Please set your exam date
Nutrition
Study Questions
Practice Exercise 1
Which of the following nursing diagnoses is most appropriate for a client with a body mass index (BMI) of 35?
Explanation
A BMI of 35 kg/m² falls in the obesity range (≥30), so the diagnosis should reflect excess adiposity.
Rationale for correct answer:
2. Obesity: NANDA-I uses “Obesity” for individuals with excess body fat-objectively supported by BMI ≥30 kg/m².
Rationale for incorrect answers:
1. Imbalanced Nutrition: Less Than Body Requirements: This diagnosis is used when intake is insufficient to meet metabolic needs and is typically associated with underweight or weight loss.
3. Overweight generally corresponds to BMI 25.0–29.9 kg/m².
4. Deficient Knowledge: This may be appropriate only if assessment reveals knowledge gaps (e.g., misconceptions about nutrition/activity).
Take home points
- Match the diagnosis to objective criteria: BMI ≥30 = “Obesity”; BMI 25–29.9 =“Overweight.”
- Use “Deficient Knowledge” only with assessment evidence of learning needs-never infer it from BMI alone.
Two months ago a client weighed 195 pounds. The current weight is 182 pounds. Calculate the client’s percentage of weight loss and determine its significance.
Explanation
Unintended weight loss is important clinically clue to malnutrition, disease, or inadequate intake. Calculate percent weight loss to judge clinical significance: small absolute losses can be important when compared to baseline weight and timeframe.
Original weight = 195 lb
Current weight = 182 lb
Weight loss = 195 − 182 = 13 lb.
Percent weight loss = (weight loss ÷ original weight) × 100
= (13 ÷ 195) × 100.
= 6.666 %, round to 6.7%
Rationale for correct answer:
2. Not significant: If the weight loss has been steady during the past 2 months, that would indicate a 3.3% loss per month. Less than 5% loss in 1 month is not significant.
Rationale for incorrect answers:
1. % weight loss: the percent loss is about 6.7%. If the test wanted the percent, this is the numeric result - but by itself it does not state whether the loss is clinically significant.
3. Significant weight loss: Not significant yet, because <5% per month.
4. Severe weight loss: “Severe” usually implies a larger percentage (e.g., ≥10% over a few months or higher depending on criteria); 6.7% is significant but not typically labeled “severe.”
Take home points
- Not significant at 2 months, but concerning if trend continues -may become severe (≥10%) at 3 months.
- On significant weight loss: perform a focused assessment, involve a dietitian, and plan interventions.
When reviewing a patient’s dietary intake, the nurse would identify which nutrient as providing the most concentrated source of energy in the body?
Explanation
Nutrition is an essential component of health and healing. Nurses play a vital role in assessing nutritional intake, interpreting lab values, and teaching clients about healthy dietary guidelines.
Rationale for correct answer:
3. Fat: Provides 9 kcal/gram, making it the most concentrated energy source. It also helps with fat-soluble vitamin absorption and insulation.
Rationale for incorrect answers:
1. Protein: Provides 4 kcal/gram, mainly used for tissue building and repair, not the most concentrated energy source.
2. Carbohydrates: Also provides 4 kcal/gram, but they are the body’s primary energy source, not the most concentrated.
4. Macrominerals: Do not provide energy (no calories); instead, they are needed for metabolic processes (e.g., calcium, potassium).
Take home points:
- Fats are the most energy-dense macronutrient at 9 kcal/g.
- Carbohydrates and proteins both provide 4 kcal/g, while vitamins/minerals provide no calories.
Which statement made by the parents of a 2-month-old infant requires further education by the nurse?
Explanation
Infant nutrition in the first year is essential for growth, immunity, and neurodevelopment. The AAP (American Academy of Pediatrics) and similar guidelines recommend breast milk or iron-fortified formula exclusively until ~6 months, and avoiding cow’s milk until after 12 months.
Rationale for correct answer:
4. “I’m going to alternate formula with whole milk, starting next month.” Cow’s milk should not be given before 12 months because it lacks iron and other essential nutrients, and increases risk of anemia and intestinal bleeding.
Rationale for incorrect answers:
1. “I’ll continue to use formula for the baby until he is at least a year old.” Formula or breast milk should be the infant’s primary nutrition for the first 12 months.
2. “I’ll make sure that I purchase iron-fortified formula.” Prevents iron deficiency anemia, which is common in formula-fed infants if non-fortified formula is used.
3. “I’ll start feeding the baby cereal at 4 months.” Though some guidelines recommend exclusive breast milk or formula until ~6 months, many pediatricians allow iron-fortified cereal introduction between 4-6 months.
Take home points:
- Infants should receive only breast milk or iron-fortified formula for the first year; avoid cow’s milk until after 12 months.
- Solid foods are generally started around 4-6 months, but formula/breast milk remains the main source of nutrition through the first year.
When discussing a weight-reduction plan with Mrs. Young, the nurse would explain that 1 lb of body fat is equal to about how many calories?
Explanation
Weight management is an important part of nursing education, especially when counseling clients on safe and effective weight reduction. Nurses need to understand the basic science of calories, energy balance, and fat metabolism. A fundamental concept is that stored body fat has a predictable caloric value, and knowing this helps guide discussions on diet and exercise for weight loss.
Rationale for correct answer:
3. 3,500 cal: One pound of body fat equals approximately 3,500 calories, so a 500-calorie daily deficit leads to ~1 lb of fat loss per week.
Rationale for incorrect answers:
1. 1,500 cal: This underestimates the energy value of body fat and would mislead the client about the amount of caloric deficit needed for weight loss.
2. 2,400 cal: While closer, this still underestimates the standard accepted value of 3,500 calories per pound of fat.
4. 5,000 cal: This overestimates and may create unrealistic expectations for caloric restriction or activity.
Take home points:
- 1 pound of body fat = ~3,500 calories.
- A safe weight loss strategy is to reduce caloric intake or increase energy expenditure by about 500 calories/day.
Practice Exercise 2
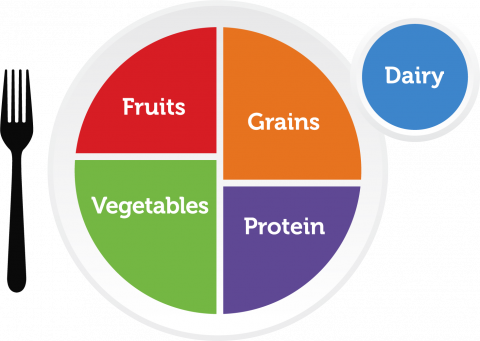
An adult reports usually eating the following each day: 3 cups dairy, 2 cups fruit, 2 cups vegetables, 5 ounces grains, and 5 ounces meat. The nurse would counsel the client to:
Explanation
Nurses should be able to compare a client’s reported food intake against the recommended daily servings from each food group to provide effective nutrition counseling. For adults, recommended servings are: Dairy: ~3 cups, fruits: ~2 cups, vegetables: ~2.5-3 cups, grains: ~6-8 ounces (at least half whole grains), protein (meat/beans): ~5-6.5 ounces.
Rationale for correct answer:
4. Increase the number of servings of grains: Adults should consume 6-8 ounces of grains daily, but this client only eats 5 ounces. Increasing grains by at least 1-3 ounces daily would ensure adequate fiber and energy.
Rationale for incorrect answers:
1. Maintain the diet; the servings are adequate: The diet is not fully adequate. Since grains are below the recommended amount, this diet is not yet balanced.
2. Increase the number of servings of dairy: The client already consumes 3 cups of dairy daily, which is within the recommended range for adults. No increase is necessary.
3. Decrease the number of servings of vegetables: The client reports 2 cups of vegetables daily, which is actually slightly below the recommended 2.5-3 cups. Reducing vegetables would worsen the deficit, not improve the diet.
Take home points:
- Compare intake to dietary guidelines (MyPlate, USDA, or equivalent national guidelines) before making nutritional recommendations.
- Grains and vegetables are often under-consumed; nurses should emphasize adequate intake of whole grains, fruits, and vegetables for balanced nutrition.
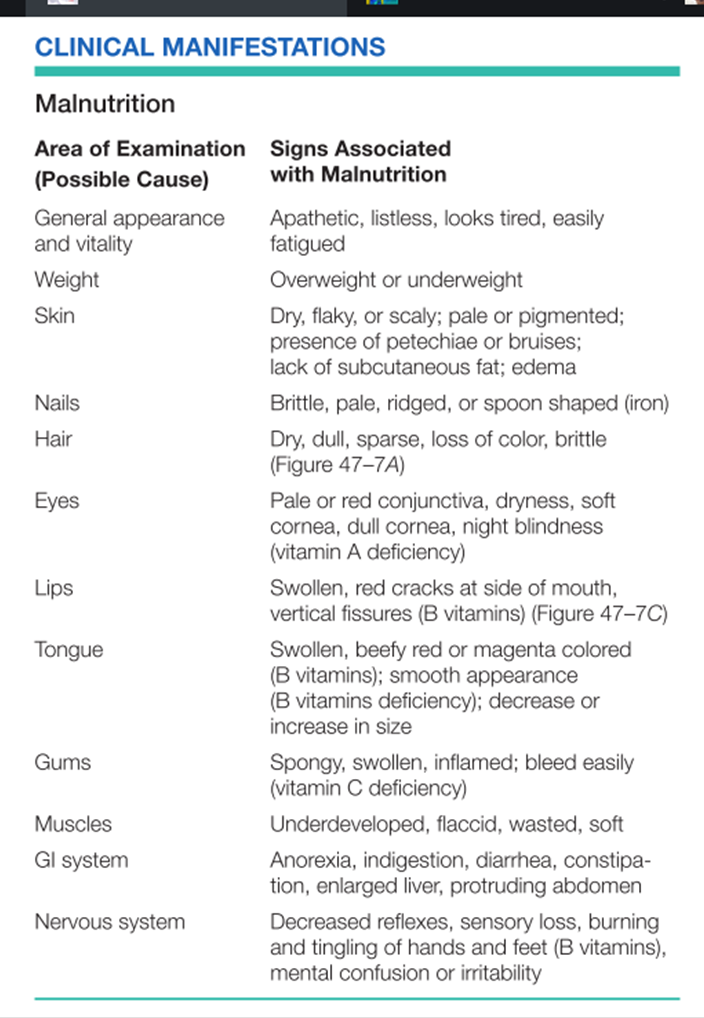
The nurse is caring for a patient with pneumonia, who has severe malnutrition. The patient’s condition places her at risk for which of the following life threatening complications during hospitalization? Select all that apply
Explanation
Severe malnutrition profoundly weakens host defenses and tissue integrity. In a hospitalized patient with pneumonia, malnutrition increases the risk of complications because of impaired immune function, poor wound healing and loss of lean body mass.
Rationale for correct answer:
2. Sepsis: Malnutrition impairs cellular and humoral immunity (fewer lymphocytes, impaired neutrophil function, reduced complement), so infections are more likely to become systemic and lead to sepsis/septic shock.
4. Skin breakdown: Protein-calorie malnutrition leads to loss of subcutaneous tissue, poor wound healing and thinning of skin, increasing risk of pressure ulcers and infected skin breakdown that can become severe.
5. Diarrhea: Malnutrition causes mucosal atrophy and altered gut immunity and microbiome; hospitalized patients are also exposed to enteric pathogens and antibiotics (risk for C. difficile).
Rationale for incorrect answers:
1. Heart disease: Chronic malnutrition can cause myocardial wasting, hypotension, and arrhythmias over time, and refeeding can precipitate cardiac problems, but heart disease as an acute inpatient complication from malnutrition and pneumonia is less likely.
3. Hemorrhage: Significant bleeding would usually require specific coagulopathy (e.g., severe vitamin K deficiency or liver failure).
Take home points:
- Monitor closely for signs of infection- malnourished patients can deteriorate quickly to sepsis.
- Prevent skin breakdown and GI complications proactively: nutrition support, frequent repositioning/pressure-area care, strict infection control and cautious antibiotic use.
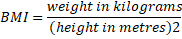
Which of the following would the nurse need to keep in mind when teaching a patient about the current MyPyramid Food Guide?
Explanation
The MyPyramid Food Guide was designed to educate individuals on balanced eating, portion control, and the importance of nutrient-dense food choices.
Rationale for correct answer:
3. Consumption of nutrient-dense foods is promoted: MyPyramid emphasizes choosing foods rich in vitamins, minerals, and fiber rather than empty calories.
Rationale for incorrect answers:
1. Meat and dairy products are located at the peak: Unlike the older food pyramid, MyPyramid shows food groups in vertical bands, not with meat and dairy at the top.
2. All food groups are equally emphasized: Different widths represent relative proportions, so some groups (like grains and vegetables) are emphasized more.
4. The Pyramid focuses on deficiencies in our diet: It focuses on balance, variety, moderation, and physical activity, not just deficiencies.
Take home points:
- MyPyramid encourages nutrient-dense choices and balanced portions across food groups.
- It also highlights physical activity as part of a healthy lifestyle.
Which laboratory test result would the nurse interpret as indicating that a patient is at risk for poor nutritional status?
Explanation
Laboratory data are valuable in assessing nutritional status, as they provide objective indicators of protein stores, immune function, and metabolic processes. Recognizing abnormal lab results helps nurses identify clients at risk for malnutrition.
Rationale for correct answer:
1. Decreased serum albumin level: Low albumin is a strong indicator of poor protein intake or malnutrition.
Rationale for incorrect answers:
2. Increased lymphocyte count: Malnutrition usually decreases immune cell production; an increase does not indicate poor nutrition.
3. Decreased blood urea nitrogen (BUN) level: While low BUN can be associated with low protein intake, it is not as reliable as serum albumin.
4. Increased platelet count: Platelet count is more related to hematologic or inflammatory conditions, not nutritional status.
Take-Home Points:
- Low serum albumin is a key indicator of malnutrition or poor protein status.
- Lab values should always be interpreted alongside clinical assessment for an accurate picture of nutrition.
The nurse completing anthropometric measurements for a patient collects which of the following information?
Explanation
Anthropometric measurements are physical assessments used to evaluate a person’s nutritional status and growth patterns. These measurements provide objective data that help in determining whether a patient is underweight, overweight, or at risk of malnutrition.
Rationale for correct answer:
1. Height and weight: These are the primary anthropometric measurements and are used to calculate BMI and monitor changes in nutritional status.
Rationale for incorrect answers:
2. Serum hemoglobin and hematocrit levels: These are biochemical measurements, not anthropometric. They help evaluate anemia and iron status.
3. Diet history: This is part of the dietary assessment, not anthropometric measurement.
4. Intake and output: These are clinical measurements used to monitor fluid balance, not anthropometry.
Take home points:
- Anthropometric measurements mainly include height, weight, BMI, skinfolds, and circumferences.
- Biochemical and dietary assessments are different categories of nutritional assessment and should not be confused with anthropometry.
Practice Exercise 3
Which of the following are allowed on a full liquid diet? Select all that apply
Explanation
A full liquid diet includes foods that are liquid at room temperature or become liquid when melted, and are used for patients transitioning from clear liquids to more solid foods.
Rationale for correct answer:
2. Chocolate pudding: Pudding is smooth, liquid-like, and acceptable.
3. Tomato juice: Juices are permitted on a full liquid diet.
4. Hard candy dissolves in the mouth and is allowed.
6. Cream of Wheat cereal: Hot cereals that are smooth and pourable are allowed.
8. Fruit “smoothies”: Smoothies that are blended smooth without pulp or seeds can be included in a full liquid diet.
Rationale for incorrect answers:
1. Scrambled eggs are soft solids, not liquids at room temperature. Not allowed on a full liquid diet.
5. Mashed potatoes are soft solids and require chewing; they belong to a soft diet, not full liquid.
7. Oatmeal cereal has texture and is not fully liquid; not allowed.
Take home points:
- Full liquid diet include foods liquid at room temperature (pudding, juices, smooth cereals, smoothies).
- Solid or textured foods like eggs, potatoes, or oatmeal are not permitted.
What is the best indication of proper placement of a nasogastric tube in the stomach?
Explanation
Misplacement of a nasogastric tube into the lungs is a serious risk that can cause aspiration pneumonia. Nurses must use reliable methods to confirm placement before administering fluids or medications.
Rationale for correct answer:
3. pH of the aspirate is less than 5: Gastric contents are acidic (pH ≤ 5), making this the most reliable bedside method.
Rationale for incorrect answers:
1. Client is unable to speak: Inability to speak may suggest airway involvement but is not a reliable or safe confirmation of gastric placement.
2. Client gags during insertion: Gagging is common during insertion but does not confirm stomach placement.
4. Fluid is easily instilled into the tube: Fluid may enter the lungs as easily as the stomach, so this is unsafe and unreliable.
Take home points:
- The best bedside test for NG tube placement is pH testing of aspirate (<5).
- Other signs like gagging, speaking, or fluid flow are unreliable.
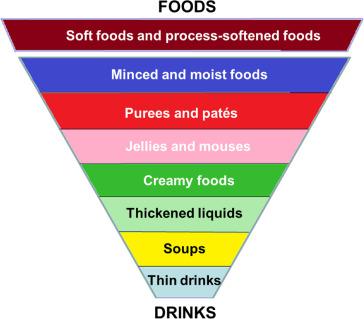
An older Asian client has mild dysphagia from a recent stroke. The nurse plans the client’s meals based on the need to:
Explanation
When a patient has dysphagia after a stroke, the priority is safe oral intake while maintaining nutrition and respecting cultural preferences. Careful texture modification, positioning, and involvement of a speech-language therapist are central. Offering familiar, culturally acceptable foods in safe textures improves intake and cooperation.
Rationale for correct answer:
3. Include as many of the client’s favorite foods as possible: Familiar foods increase appetite and intake. The nurse should, however, modify the texture or preparation as recommended by SLP (e.g., pureed, chopped, thickened liquids) to ensure safety while preserving cultural preferences.
Rationale for incorrect answers:
1. Have at least one serving of thick dairy (e.g., pudding, ice cream) per meal: Thickened liquids or texture-modified foods may be used when ordered, but mandating a serving of dairy per meal is not standard and could worsen tolerance or add unwanted calories/fat.
2. Eliminate the beer usually ingested every evening: Avoiding alcohol is reasonable (it can impair swallowing/co-ordination and increase aspiration risk), but meal planning focuses on safe textures, positioning, and culturally acceptable choices- not only alcohol cessation.
4. Increase the calories from lipids to 40%: Increasing fat to an arbitrary 40% of calories is not a standard approach and could be unhealthy. Nutritional strategy should be individualized.
Take home points
- Prioritize safe texture modification and positioning (e.g., upright during meals, chin-tuck as advised) while offering culturally familiar foods to maximize intake.
- Collaborate with speech-language pathology and nutrition (dietitian) to tailor meal textures and ensure adequate nutrition without increasing aspiration risk.
Which of the following meals would the nurse recommend to the client as highest in calcium, iron, and fiber?
Explanation
Calcium, iron, and fiber-three critical nutrients for maintaining musculoskeletal, hematologic, and gastrointestinal health. Nurses need to identify which meals best meet these requirements to promote overall client wellness.
Rationale for correct answer:
4. 3 ounces tuna plus 1 ounce cheese sandwich on whole-wheat bread plus a pear: Calcium- Cheese is high in calcium. Iron- Tuna provides iron. Fiber- Whole-wheat bread and pear provide excellent dietary fiber.
Rationale for correct answer:
1. 3 ounces cottage cheese with 1/3 cup raisins and 1 banana: While this meal has calcium and some fiber, it is relatively low in iron compared to other options.
2. 1/2 cup broccoli with 3 ounces chicken and 1/2 cup peanuts: Decent in fiber, moderate in iron, lower in calcium.
3. 1/2 cup spaghetti with 2 ounces ground beef and 1/2 cup lima beans plus 1/2 cup ice cream: Ice cream adds calcium but is high in fat and sugar
Take home points:
- Balanced meals with protein, fruits/vegetables, and whole grains are more likely to meet multiple nutrient needs (calcium, iron, fiber).
- Dairy (calcium), meat/fish (iron), and whole grains/fruits (fiber) are the key groups to think about when selecting nutrient-rich meals.
A patient is receiving both PN and EN. When would the nurse collaborate with the health care provider and request a discontinuation of PN?
Explanation
When patients receive both parenteral nutrition (PN) and enteral nutrition (EN), the goal is to transition to enteral feeding as soon as it supplies adequate calories and protein.
Rationale for correct answer:
4. When 75% of the patient’s nutritional needs are met by the tube feedings: Guidelines generally recommend discontinuing PN when enteral feedings consistently meet a substantial portion of caloric/protein needs so the patient won’t become nutritionally deficient once PN is stopped.
Rationale for incorrect answers:
1. When 25% of the patient’s nutritional needs are met by the tube feedings: Discontinuing PN when only a small fraction of needs is met will leave the patient nutritionally inadequate.
2. When bowel sounds return: Return of bowel sounds is a positive sign of GI activity but does not guarantee adequate caloric/protein intake by EN. Bowel sounds alone are insufficient to stop PN.
3. When the central line has been in for 10 days: Duration of line placement is not the criterion for stopping PN. Prolonged central access increases infection risk, but discontinuation depends on nutritional adequacy, not a fixed number of days.
Take home points:
- Stop PN when EN reliably provides the majority of caloric/protein needs (≈60–75%).
- Plan for safe weaning (watch glucose and electrolytes; consider taper or D10 if abrupt stop risks hypoglycemia).
Comprehensive Questions
What is the proper technique with gravity tube feeding?
Explanation
Gravity tube feeding relies on hydrostatic pressure to deliver formula from a bag through the feeding tube. Safe technique includes correct bag height to regulate flow, positioning the patient to reduce aspiration risk, checking residuals per policy, and warming formula to room temperature for tolerance.
Rationale for correct answer:
1. Hang the feeding bag 1 foot higher than the tube’s insertion point into the client: This provides adequate hydrostatic pressure for a controlled gravity flow while reducing need for excessive bolus pressure. Always regulate flow with the roller clamp and monitor the patient.
Rationale for incorrect answers:
2. Administer the next feeding only if there is less than 25 mL of residual volume from the previous feeding: A 25 mL cutoff is unrealistically low. Traditional thresholds for holding feedings have been much higher.
3. Place client in the left lateral position: The safest position for enteral feeding to reduce aspiration is upright (high-Fowler’s) or at least a 30°-45° elevated head of bed.
4. Administer feeding directly from the refrigerator: Cold formula can cause cramping and poor tolerance; feeding solutions should be warmed to room temperature before administration.
Take home points
- Position the patient upright (head of bed 30°- 45°) during and for at least 30 - 60 minutes after gravity tube feeding to lower aspiration risk.
- Use the roller clamp to control the gravity flow; always follow facility policy for residual-volume checks and feeding procedures.
A 55-year-old female is about 9 kg (20 lb) over her desired weight. She has been on a “low-calorie” diet with no improvement. Which statement reflects a healthy approach to the desired weight loss? “I need to:
Explanation
Safe, sustainable weight loss emphasizes gradual lifestyle changes: regular physical activity, balanced calorie control, and behavior modification.
Rationale for correct answer:
1. Increase my exercise to at least 30 minutes every day: Regular moderate exercise (about 30 minutes most days) combined with sensible dietary changes supports weight loss, improves metabolic health, and is a recommended, sustainable strategy.
Rationale for incorrect answers:
2. Switch to a low-carbohydrate diet: Low-carbohydrate diets can produce short-term weight loss for some, but they are not universally superior and may be hard to maintain; the healthier recommended approach is balanced calorie reduction plus activity.
3. Keep a list of my forbidden foods on hand at all times: Strictly forbidding foods can promote guilt, bingeing, and an unhealthy relationship with food. A flexible, portion-controlled approach and behavior strategies are preferable.
4. Buy more organic and less processed foods: Choosing less-processed whole foods can help, but “organic” alone does not guarantee lower calories nor ensure weight loss; portion control and overall caloric balance matter most.
Take home points
- Sustainable weight loss - modest, consistent calorie reduction plus regular physical activity (e.g., ~30 min/day) and behavior changes.
- Avoid extreme or rigid dieting rules; focus instead on balanced meals, portion control, and lifestyle patterns one can maintain long term.
Which of the sites on the diagram below indicates the correct location for the tip of a small-bore nasally placed feeding tube?
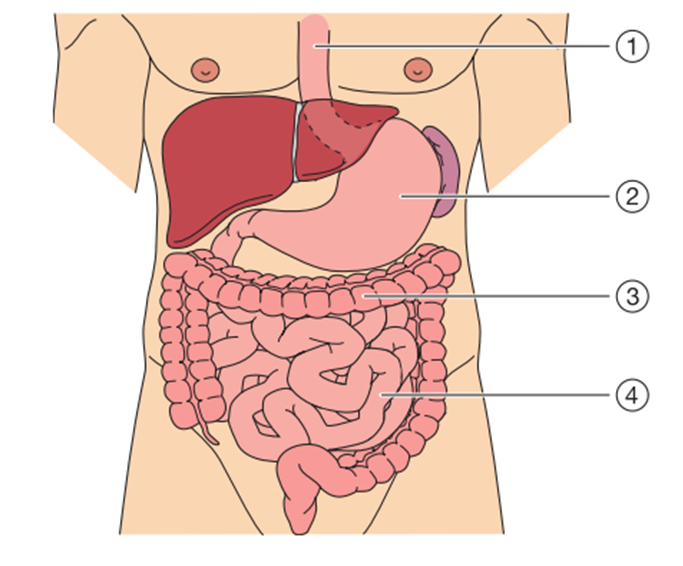
Explanation
Safe placement of a small-bore nasally placed feeding tube (Dobhoff tube or similar) is crucial for effective nutrition delivery and to prevent complications such as aspiration pneumonia.
Rationale for correct answer:
2. The stomach is the most common site for small-bore nasogastric feeding tube placement. It allows for bolus or continuous feeding, easy monitoring, and is the safest initial site. Placement is verified by X-ray before feeding begins.
Rationale for incorrect answers:
1. The esophagus is the passageway from the throat to the stomach. If a feeding tube tip remains here, formula could easily reflux into the airway and cause aspiration.
3. Feeding tubes are not advanced into the large intestine. The large bowel’s function is fluid absorption and stool formation, not nutrient absorption.
4. In some cases, feeding tubes are advanced past the stomach into the duodenum or jejunum, especially for patients at high risk of aspiration (e.g., impaired gastric emptying, severe reflux). While this is appropriate, it requires specialized placement.
Take home points:
- Small-bore nasogastric feeding tubes are most commonly placed in the stomach.
- Placement in the small intestine (jejunum/duodenum) is used for patients at high aspiration risk, but never in the esophagus or large intestine.
The nurse is preparing to perform a blood glucose monitoring test on a patient. Place the steps for performing the procedure in the correct sequence.
Explanation
Point-of-care blood glucose monitoring must combine infection control, correct technique, and device accuracy. Steps done in the right order reduce false readings and prevent transmission of infection.
Rationale for correct answer:
- (3) Instruct patient to perform hand hygiene with soap and water.
Prevents contamination from sugar or other residues on the fingers, which could give falsely high readings. - (6) Check code on test strip vial.
Ensures the test strips are calibrated correctly for the glucometer. - (1) Press button on meter to confirm match codes.
Confirms that the meter’s internal code matches the strip code for accuracy. - (8) Perform hand hygiene and put on clean gloves.
Protects both nurse and patient from bloodborne pathogens and infection transmission. - (4) Clean patient finger with antiseptic swab.
Disinfects the puncture site. Important: allow to dry to avoid dilution of blood with alcohol. - (7) Holding lancet to finger, press release button on machine.
Obtains capillary blood sample safely and effectively. - (2) Bringing meter to test strip, allow blood drop to wick onto test strip.
Ensures an adequate sample is absorbed by the strip for analysis. - (5) Interpret results and document.
Completes the procedure and ensures accurate communication of results for clinical decision-making.
Take home points:
- Correct sequence matters: code verification comes before gloves and antiseptic.
- Always finish with interpretation and documentation- this closes the loop on safe patient care.
The nurse is caring for a patient with dysphagia and is feeding her a pureed chicken diet. Suddenly the patient begins to choke. What is the priority nursing intervention?
Explanation
Patients with dysphagia are at high risk for aspiration. When a patient being fed suddenly chokes, the immediate priority is to stop the offending activity so nothing more enters the airway and you can assess and manage the airway.
Rationale for correct answer:
4. Stop feeding her: Stopping the feeding immediately prevents additional material entering the airway and allows you to quickly assess the patient, call for help if needed, and institute airway-clearance measures.
Rationale for incorrect answers:
1. Suction her mouth and throat: May be needed if secretions or visible food are present and the patient cannot clear them, but suctioning is secondary to first stopping the feed and assessing the airway/level of obstruction.
2. Turn her on her side: Turning to the side helps drain secretions and reduces risk of aspiration into the lungs (useful after stopping the feed), but it is not the first immediate action.
3. Put on oxygen at 2 L nasal cannula: Oxygen can help if the patient becomes hypoxic, but oxygen does not remove an obstruction. Do not delay airway clearance to apply oxygen.
Take home points:
- Immediately stop the feed at the first sign of choking.
- Then assess airway, breathing, and level of consciousness and act (encourage cough, Heimlich, suction, or CPR) according to the patient’s response.
The nurse is changing the PN tubing. What action should the nurse take to prevent an air embolus?
Explanation
Changing parenteral nutrition (PN) tubing involves central venous access in many patients. Any open central line connection can allow air to be entrained into the venous system; increasing intrathoracic/central venous pressure during the change and positioning the patient appropriately reduces that risk.
Rationale for correct answer:
1. Have the patient turn on the left side and perform a Valsalva maneuver: The Valsalva increases intrathoracic and central venous pressure so air is less likely to be sucked into the central venous catheter during disconnection. Placing the patient on the left side helps trap any entrained air in the right atrium/ventricle and away from the pulmonary outflow.
Rationale for incorrect answers:
2. Have the patient cough vigorously when tubing is disconnected: Coughing can transiently raise intrathoracic pressure but is uncontrolled and may dislodge lines or cause complications.
3. Have the patient take a deep breath and hold it: Holding a deep breath raises intrathoracic pressure somewhat, but a true Valsalva (forced expiration against a closed glottis or “bear down”) is more effective.
4. Place patient in supine position with head of bed elevated 90 degrees: Head-up positioning lowers central venous pressure and increases the risk of air being entrained.
Take home points:
When manipulating central lines or changing PN tubing:
- clamp the catheter when possible
- prime tubing carefully to remove air
- have the patient perform a Valsalva or exhale-and-hold during disconnection to raise central venous pressure
A patient is receiving an enteral feeding at 65 mL/h. The GRV in 4 hours was 125 mL. What is the priority nursing intervention?
Explanation
Gastric residual volume (GRV) is measured to help assess gastric emptying and aspiration risk in patients on enteral feeding. Interpretation depends on the facility’s protocol and accepted thresholds; small residuals are usually acceptable and do not require stopping the feed.
Rationale for correct answer:
3. Continue the feedings; this is normal gastric residual for this feeding: Most clinical protocols consider a GRV of <200–250 mL acceptable and do not require holding feeds.
Rationale for incorrect answers:
1. Assess bowel sounds: Reasonable if you suspect intolerance, but with a GRV of 125 mL (which is below common stop thresholds), immediate assessment of bowel sounds is not the priority action.
2. Raise the head of the bed to at least 45 degrees: Always keep the HOB elevated during enteral feeding to reduce aspiration risk; if not already elevated this is important, but it is not the priority response to a normal GRV of 125 mL.
4. Hold the feeding until you talk to the primary care provider: Not necessary for this residual value and may interrupt nutrition unnecessarily; hold-and-report is usually reserved for higher residuals or signs of intolerance.
Take home points:
- GRV threshold - common thresholds: 200–250 mL
- Always keep the head of bed elevated during feedings, monitor for signs of intolerance (abdomen distension, vomiting, aspiration)
Which action can a nurse delegate to AP?
Explanation
Delegation is guided by the “Five Rights of Delegation” (right task, circumstance, person, direction, and supervision). In general, APs (assistive personnel) can perform routine, stable, non-invasive tasks.
Rationale for correct answer:
1. Performing glucose monitoring every 6 hours on a stable patient: APs may be trained and delegated to perform point-of-care blood glucose monitoring in stable clients because it is a standardized procedure, and the nurse interprets and acts on the results.
Rationale for incorrect answers:
2. Teaching the patient about the need for enteral feeding: Teaching requires professional nursing knowledge, critical thinking, and individualized instruction. Cannot be delegated to AP.
3. Administering enteral feeding bolus after tube placement has been verified: Feeding via tube involves risk of aspiration and requires assessment and verification skills, which cannot be delegated.
4. Evaluating the patient’s tolerance of the enteral feeding: Evaluation is part of the nursing process (assessment and judgment) and cannot be delegated to AP.
Take home points:
- APs can perform stable, routine, non-invasive tasks (e.g., vital signs, I&O, ADLs, glucose checks in stable clients).
- The nurse retains responsibility for tasks involving teaching, assessment, critical judgment, and evaluation
A nurse sees an AP perform the following interventions for a patient receiving continuous enteral feedings. Which action would require immediate attention by the nurse?
Explanation
Continuous enteral feedings increase aspiration risk and require careful positioning and securement. When delegating or observing AP care, the nurse must intervene immediately for actions that increase aspiration or dislodge the tube.
Rationale for correct answer:
2. Placing patient supine while giving a bath: Supine position during ongoing feedings greatly increases risk of reflux and aspiration. The head of bed should be elevated (usually 30–45°) during continuous enteral feeding.
Rationale for incorrect answers:
1. Fastening tube to the gown with new tape: Appropriate and good practice to prevent tube dislodgement as long as the tube is secured without tension and the tape is applied correctly.
3. Monitoring the patient’s weight as ordered: Appropriate nursing activity; weight monitoring is part of routine assessment for nutritional status and tube-feeding effectiveness.
4. Ambulating patient with enteral feedings still infusing: Often acceptable if the feeding is on a pump, tubing is secured, and patient stability/transfer protocols are followed.
Take home points:
- Never allow a patient to be supine during continuous enteral feeding - always keep HOB elevated (30-45°) to reduce aspiration risk.
- Secure the tube properly and monitor safety during ambulation; intervene immediately for positioning or securement practices that increase aspiration/dislodgement risk.
A patient is receiving total parenteral nutrition (TPN). What are the primary interventions the nurse should follow to prevent a central line infection? Select all that apply
Explanation
Total parenteral nutrition (TPN) requires central venous access and strict aseptic technique because the central line is a major route for bloodstream infections.
Rationale for correct answer:
1. Change the dressing using sterile technique: Sterile dressing changes reduce microbial colonization at the insertion site and lower risk of central line-associated bloodstream infection (CLABSI).
3. Change the TPN tubing every 24 hours: Frequent tubing changes (usually every 24 hours for lipid-containing or TPN administration sets) help prevent microbial contamination and reduce CLABSI risk.
Rationale for incorrect answers:
2. Change TPN containers every 48 hours: TPN containers and lipid admixtures are typically changed every 24 hours to limit bacterial growth; leaving containers longer (e.g., 48 hrs) increases infection risk.
4. Monitor glucose levels to watch and assess for glucose intolerance. — Important for metabolic monitoring of TPN (hyper/hypoglycemia) but not a primary intervention to prevent central line infection.
5. Elevate head of the bed 45 degrees to prevent aspiration: Good for aspiration prevention, but unrelated to preventing central line infections.
Take home points:
Preventing central line infections centers on aseptic technique:
- sterile dressing changes
- proper skin antisepsis
- hub/port disinfection before access
- routine tubing/container changes per policy (commonly every 24 hours for TPN).
Mr. Yow is refusing to eat. Which intervention would be most helpful in stimulating his appetite?
Explanation
Appetite stimulation in hospitalized clients can be challenging due to illness, hospital routines, and unfamiliar foods. Nurses play a crucial role in promoting nutrition by addressing barriers such as pain, treatment schedules, and food preferences.
Rationale for correct answer:
2. Encouraging food from home when possible: Familiar foods can enhance appetite, provide comfort, and increase food intake.
Rationale for incorrect answers:
1. Administering pain medication after meals: Pain should be controlled before meals to improve comfort and willingness to eat. Giving it after meals does not promote appetite.
3. Scheduling his respiratory therapy before each meal: Treatments before meals may tire or stress the client, reducing appetite. They should ideally be scheduled after meals.
4. Reinforcing the importance of his eating exactly what is delivered to him: Strict enforcement can create resistance and does not address appetite stimulation. Flexibility is more effective.
Take home points:
- Appetite is best stimulated with comfort measures such as familiar, preferred foods.
- Nursing interventions should reduce barriers to eating (pain, fatigue, dislike of hospital food) rather than enforce strict compliance.
Mrs. James has progressed to a full liquid diet. Which items would the nurse expect to see on the patient’s meal tray?
Explanation
A full liquid diet is prescribed for clients transitioning from clear liquids to more substantial foods. It includes all clear liquids plus foods that are liquid at room temperature or melt into liquid. The goal is to provide adequate nutrition while being gentle on the digestive system until the client can tolerate solid foods.
Rationale for correct answer:
4. Custard and a glass of milk: Both are part of a full liquid diet, as they are smooth and liquid at room temperature.
Rationale for incorrect answers:
1. Apple juice and bouillon: These are clear liquids, not full liquids.
2. Water ice and ginger ale: These are also clear liquids; not sufficient for a full liquid diet.
3. Puréed beef and cream of broccoli soup: Puréed meat is considered mechanical soft or blenderized diet, not full liquid. Cream soup is acceptable, but puréed meat is not.
Take home points:
- A full liquid diet includes milk, custards, puddings, cream soups, and liquid nutritional supplements-not just clear liquids.
- Understanding diet progression (clear → full liquid → soft → regular) is essential for safe nutritional management.
When explaining parenteral nutrition, the nurse would describe this method as providing nutrients to the patient by way of which of the following?
Explanation
Parenteral nutrition (PN) is a specialized method of providing nutrition for clients who cannot use their gastrointestinal tract due to disease, surgery, or dysfunction. Unlike enteral nutrition, which delivers nutrients directly into the stomach or intestines, parenteral nutrition bypasses the digestive system completely.
Rationale for correct answer:
2. Intravenous access: Parenteral nutrition is administered directly into the bloodstream, most often via a central venous catheter (total parenteral nutrition, TPN) or sometimes through peripheral veins (peripheral parenteral nutrition, PPN).
Rationale for incorrect answers:
1. Gastrostomy tube: A gastrostomy tube delivers nutrition directly into the stomach through a surgically created opening. This is an example of enteral nutrition, not parenteral nutrition.
3. Nasogastric tube: A nasogastric tube passes through the nose into the stomach for feeding. This also represents enteral nutrition.
4. Jejunostomy tube: A jejunostomy tube delivers nutrition into the jejunum, another method of enteral feeding, not parenteral.
Take home points:
- Parenteral nutrition always uses intravenous access-not the GI tract.
- PN is reserved for clients with impaired GI function when enteral feeding is not possible or contraindicated.
Mr. White has been admitted to the alcoholic referral unit in the local hospital. Based on an understanding of the effects of alcohol on the GI tract, which of the following would the nurse be most alert for nutritionally?
Explanation
Chronic alcohol use profoundly affects nutrition. Alcohol interferes with absorption, storage, and metabolism of essential vitamins and minerals, particularly the B vitamins. Nurses caring for clients with alcohol dependence must anticipate and manage nutritional deficiencies to prevent complications such as anemia, neuropathy, or Wernicke-Korsakoff syndrome.
Rationale for correct answer:
1. Vitamin B malnutrition: Alcohol interferes with absorption and metabolism of B vitamins (especially thiamine, folate, and B12), leading to neurological and hematological problems.
Rationale for incorrect answers:
2. Obesity: Although alcohol is calorie-dense, most chronic alcoholics tend to suffer from malnutrition rather than obesity.
3. Dehydration: Alcohol has a diuretic effect, but the key nutritional issue is vitamin deficiency, not fluid imbalance.
4. Vitamin C deficiency: Less commonly associated with alcoholism compared to Vitamin B deficiencies.
Take home points:
- Alcoholism is strongly associated with Vitamin B deficiencies, particularly thiamine.
- Thiamine supplementation is essential to prevent complications such as Wernicke’s encephalopathy.
A patient has a nasogastric tube inserted for feeding purposes. Using the stomach as a reservoir for food is advantageous in preventing what complication?
Explanation
Enteral nutrition through nasogastric (NG) tubes is a common nursing intervention for patients who cannot eat orally. The stomach acts as a natural reservoir, allowing gradual delivery of nutrients. Understanding the physiologic advantage of gastric feeding helps nurses prevent complications such as dumping syndrome and metabolic imbalances.
Rationale for correct answer:
1. Dumping syndrome: The stomach regulates the flow of food into the small intestine, reducing the risk of rapid emptying that causes diarrhea, cramping, and hypoglycemia.
Rationale for incorrect answers:
2. Duodenal ulcers: NG feeding does not prevent ulcer formation. Ulcers are primarily linked to H. pylori infection, NSAID use, or acid imbalance.
3. Hyperglycemia: Hyperglycemia is more related to the composition of feedings and metabolic regulation, not the site of feeding.
4. Gastric ulcers: Feeding into the stomach does not specifically prevent gastric ulcers.
Take home points:
- The stomach acts as a reservoir that prevents dumping syndrome by regulating nutrient flow.
- NG feeding must be monitored carefully for tolerance, aspiration, and correct placement.
Exams on Nutrition
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
To:
- Identify essential nutrients and their dietary sources.
- Describe normal digestion, absorption, and metabolism of carbohydrates, proteins, and lipids.
- Identify factors influencing nutrition.
- Identify nutritional variations throughout the life cycle.
- Evaluate a diet using a food guide pyramid.
- Discuss essential components and purposes of nutritional assessment and nutritional screening.
- Identify risk factors for and clinical signs of malnutrition.
- Describe nursing interventions to promote optimal nutrition.
- Discuss nursing interventions to treat clients with nutritional problems.
- Verbalize the steps used in: a. Inserting a nasogastric tube. b. Removing a nasogastric tube. c. Administering a tube feeding. d. Administering a gastrostomy or jejunostomy tube feeding
Introduction
Nutrition is the sum of all the interactions between an organism and the food it consumes. In other words, nutrition is what a person eats and how the body uses it.
Nutrients are organic and inorganic substances found in foods that are required for body functioning.
Adequate food intake consists of a balance of nutrients: water, carbohydrates, proteins, fats, vitamins, and minerals.
Foods differ greatly in their nutritive value (the nutrient content of a specified amount of food), and no one food provides all essential nutrients.
Essential Nutrients
The energy-providing nutrients are carbohydrates, fats, and proteins.
Carbohydrates, fats, protein, minerals, vitamins, and water are referred to as macronutrients, because they are needed in large amounts (e.g., hundreds of grams) to provide energy.
Micronutrients are those vitamins and minerals that are required in small amounts (e.g., milligrams or micrograms) to metabolize the energy-providing nutrients.
3.1 CARBOHYDRATES
Carbohydrates are composed of the elements carbon (C), hydrogen (H), and oxygen (O) and are of two basic types: simple carbohydrates (sugars) and complex carbohydrates (starches and fiber).
Natural sources of carbohydrates also supply vital nutrients, such as protein, vitamins, and minerals that are not found in processed foods.
Processed carbohydrate foods are relatively low in nutrients in relation to the large number of calories they contain.
Types of carbohydrates:
Sugars: may be monosaccharides (single molecules) or disaccharides (double molecules). Of the three monosaccharides (glucose, fructose, and galactose), glucose is by far the most abundant simple sugar.
Starches: Starches are the insoluble, nonsweet forms of carbohydrate. They are polysaccharides. Nearly all starches exist naturally in plants, such as grains, legumes, and potatoes.
Fiber: Fiber, a complex carbohydrate derived from plants, supplies roughage, or bulk, to the diet. However, fiber cannot be digested by humans.
Carbohydrate digestion & metabolism
- Major enzymes of carbohydrate digestion include ptyalin (salivary amylase), pancreatic amylase, and the disaccharidases: maltase, sucrase, and lactase.
- The desired end products of carbohydrate digestion are monosaccharides.
- Carbohydrate metabolism is a major source of body energy.
- Insulin, a hormone secreted by the pancreas, enhances the transport of glucose into cells.
- Carbohydrates are stored either as glycogen or as fat. Glycogen is a large polymer (compound molecule) of glucose.
- Almost all body cells can store glycogen; however, most is stored in the liver and skeletal muscles, where it is available for conversion back into glucose.
3.2 PROTEINS
Amino acids, organic molecules made up primarily of carbon, hydrogen, oxygen, and nitrogen, combine to form proteins.
Amino acids are categorized as essential or nonessential.
Essential amino acids are those that cannot be manufactured in the body and must be supplied as part of the protein ingested in the diet. Nine essential amino acids- histidine, isoleucine, leucine, lysine, methionine, phenylalanine, tryptophan, threonine, and valine-are necessary for tissue growth and maintenance.
Nonessential amino acids are those that the body can manufacture. Nonessential amino acids include alanine, aspartic acid, cystine, glutamic acid, glycine, hydroxyproline, proline, serine, and tyrosine.
Proteins may be complete or incomplete.
- Complete proteins contain all of the essential amino acids plus many nonessential ones. Most animal proteins, including meats, poultry, fish, dairy products, and eggs, are complete proteins.
- Incomplete proteins lack one or more essential amino acids (most commonly lysine, methionine, or tryptophan) and are usually derived from vegetables.
Protein digestion:
Digestion of protein foods begins in the stomach, where the enzyme pepsin breaks protein down into smaller units.
However, most protein is digested in the small intestine. The pancreas secretes the proteolytic enzymes trypsin, chymotrypsin, and carboxypeptidase; glands in the intestinal wall secrete aminopeptidase and dipeptidase.
These enzymes break protein down into smaller molecules and eventually into amino acids.
Protein storage and metabolism:
The liver uses amino acids to synthesize specific proteins (e.g., liver cells and the plasma proteins albumin, globulin, and fibrinogen). Plasma proteins are a storage medium that can rapidly be converted back into amino acids. Other amino acids are transported to tissues and cells throughout the body where they are used to make protein for cell structures.
Protein metabolism includes three activities: anabolism (building tissue), catabolism (breaking down tissue), and maintaining nitrogen balance.
3.3 LIPIDS
Lipids are organic substances that are greasy and insoluble in water but soluble in alcohol or ether. Fats are lipids that are solid at room temperature; oils are lipids that are liquid at room temperature.
Fatty acids, made up of carbon chains and hydrogen, are the basic structural units of most lipids.
Fatty acids are described as saturated or unsaturated, according to the relative number of hydrogen atoms they contain.
- Saturated fatty acids are those in which all carbon atoms are filled to capacity (i.e., saturated) with hydrogen; an example is butyric acid, found in butter.
- An unsaturated fatty acid is one that could accommodate more hydrogen atoms than it currently does. It has at least two carbon atoms that are not attached to a hydrogen atom; instead, there is a double bond between the two carbon atoms.
- Fatty acids with one double bond are called monounsaturated fatty acids; those with more than one double bond (or many carbons not bonded to a hydrogen atom) are polyunsaturated fatty acids
Classification of lipids:
Based on their chemical structure, lipids are classified as simple or compound.
- Glycerides, the simple lipids, are the most common form of lipids. They consist of a glycerol molecule with up to three fatty acids attached.
- Triglycerides (which have three fatty acids) account for more than 90% of the lipids in food and in the
- Cholesterol is a fatlike substance that is both produced by the body and found in foods of animal origin.
Lipid digestion and metabolism:
- Although chemical digestion of lipids begins in the stomach, they are digested mainly in the small intestine, primarily by bile, pancreatic lipase, and enteric lipase, an intestinal enzyme.
- The end products of lipid digestion are glycerol, fatty acids, and cholesterol.
- These are immediately reassembled inside the intestinal cells into triglycerides and cholesterol esters (cholesterol with a fatty acid attached to it), which are not water soluble.
- For these reassembled products to be transported and used, the small intestine and the liver must convert them into soluble compounds called lipoproteins
- Converting fat into usable energy occurs through the use of the enzyme hormone-sensitive lipase, which breaks down triglycerides in adipose cells, releasing glycerol and fatty acids into the blood.
3.4 MICRONUTRIENTS
A vitamin is an organic compound that cannot be manufactured by the body and is needed in small quantities to catalyze metabolic processes. Thus, when vitamins are lacking in the diet, metabolic deficits result.
Vitamins are generally classified as fat soluble or water soluble.
- Water-soluble vitamins include C and the B-complex vitamins: B1 (thiamine), B2 (riboflavin), B3 (niacin or nicotinic acid), B6 (pyridoxine), B9 (folic acid), B12 (cobalamin), pantothenic acid, and biotin. The body cannot store water-soluble vitamins; thus, people must get a daily supply in the diet
- Fat-soluble vitamins include A, D, E, and K. The body can store these vitamins, although there is a limit to the amounts of vitamins E and K the body can store.
Minerals are found in organic compounds, as inorganic compounds, and as free ions.
- Macrominerals are those that people require daily in amounts over 100 mg. They include calcium, phosphorus, sodium, potassium, magnesium, chloride, and sulfur.
- Microminerals are those that people require daily in amounts less than 100 mg. They include iron, zinc, manganese, iodine, fluoride, copper, cobalt, chromium, and selenium.
Energy Balance
Energy balance is the relationship between the energy derived from food and the energy used by the body.
Energy Intake
The amount of energy that nutrients or foods supply to the body is their caloric value.
A calorie is a unit of heat energy. A small calorie (c, cal) is the amount of heat required to raise the temperature of 1 gram of water 1 degree Celsius.
A large calorie (Calorie, kilocalorie [Kcal]) is the amount of heat energy required to raise the temperature of 1 gram of water 15 to 16 degrees Celsius and is the unit used in nutrition.
In the metric system, the measure is the kilojoule (kJ). One Calorie (Kcal) equals 4.18 kilojoules.
The energy liberated from the metabolism of food has been determined to be:
- 4 Calories/gram (17 kJ) of carbohydrates
- 4 Calories/gram (17 kJ) of protein
- 9 Calories/gram (38 kJ) of fat
- 7 Calories/gram (29 kJ) of alcohol.
Energy Output
Metabolism refers to all biochemical and physiological processes by which the body grows and maintains itself.
The basal metabolic rate (BMR) is the rate at which the body metabolizes food to maintain the energy requirements of a person who is awake and at rest.
Resting energy expenditure (REE) is the amount of energy required to maintain basic body functions; in other words, the calories required to maintain life- 1 cal/kg of body weight/h for men and 0.9 cal/kg/h for women.
4.1 BODY WEIGHT AND BODY MASS STANDARDS
Ideal body weight (IBW) is the optimal weight recommended for optimal health.
To determine an individual’s approximate IBW, the nurse can consult standardized tables or can quickly calculate a value using the Rule of 5 for women and the Rule of 6 for men.
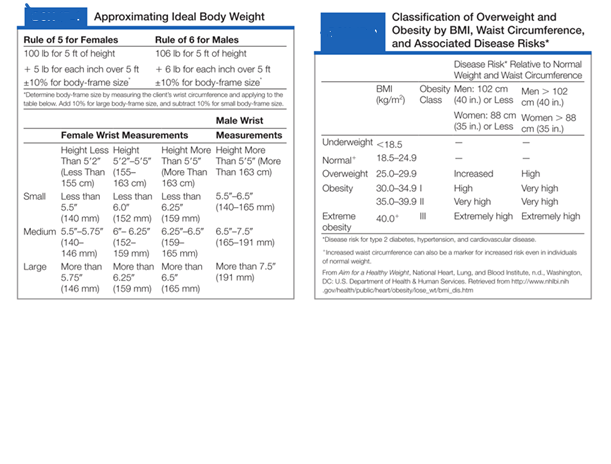
Many health professionals consider the body mass index to be a more reliable indicator of a person’s healthy weight. However, the results must be used with caution in people who have fluid retention (e.g., ascites or edema), athletes, or older adults.
To calculate the BMI:
Factors Affecting Nutrition
An individual’s food preferences and habits are often a major factor affecting actual food intake.
1. Development
- Infants & Adolescents: Higher nutrient needs due to rapid growth.
- Older Adults: Lower caloric needs, risk of CHD, osteoporosis, HTN - dietary adjustments needed.
2. Sex
- Men: Higher calories & protein (larger muscle mass).
- Women: Higher iron needs (menstruation); increased calories/fluids during pregnancy & lactation.
3. Ethnicity & Culture
- Food preferences shaped by tradition (e.g., rice, pasta, curry).
- Nurses should avoid labeling foods as “good/bad”; encourage variety & moderation.
4. Beliefs About Food
- Media & cultural beliefs influence diet.
- Food fads may be harmless or dangerous. Nurses should explore underlying needs and guide toward healthier options.
5. Personal Preferences
- Likes/dislikes shaped by experiences, taste, smell, texture, color, and familiarity.
- Some people are adventurous with food; others prefer routine.
6. Health
- Illnesses/diseases (GI, liver, pancreas, autoimmune, dysphagia, dental issues) impair nutrition.
- Cancer therapies (chemo, radiotherapy) cause ulcers, nausea, malabsorption, fatigue, anorexia.
- Intolerances: lactose intolerance, gluten sensitivity.
7. Alcohol Consumption
- High in calories; contributes to fat storage.
- Excessive use leads to nutrient deficiencies, poor absorption, increases vitamin B needs.
- Moderate use may have some protective effects (e.g., CVD), but risks often outweigh benefits.
8. Advertising
- Promotes processed/fast foods over fruits & vegetables.
- Strong influence on children’s food choices.
9. Religious Practices
- Dietary restrictions vary (e.g., no pork in Islam/Judaism, no meat on certain days in Catholicism).
- Nurses should plan care respecting these practices.
10. Lifestyle
- Busy individuals rely on convenience/fast food; home-based individuals may cook more.
- Work schedules (night shifts) affect eating patterns.
- Physical activity increases metabolic needs more than mental activity.
11. Economics
- Low income- limited access to fresh, healthy foods.
- High income- more proteins/fats, fewer complex carbs.
- Nurses should not assume availability of cooking/storage facilities.
12. Medications & Therapy
- Drugs may alter appetite, taste, absorption, excretion.
- Nutrients can affect drug absorption (e.g., calcium reduces tetracycline absorption).
- Older adults at higher risk for drug–food interactions.
- Herbal supplements may cause adverse effects or interactions.
13. Psychological Factors
- Stress, depression, loneliness leads to overeating or undereating.
- Severe conditions: anorexia nervosa & bulimia, common in adolescents.
5.1 CULTURALLY RESPONSIVE CARE
Nutritional Practices and Preferences Among Different Cultures:
AFRICAN AMERICAN HERITAGE
- Gifts of food are common and should never be rejected.
- Diets are often high in fat, cholesterol, and sodium.
- Being overweight may be viewed as positive.
- Popular vegetables include black-eyed peas, okra, sweet potatoes, peanuts, corn, hot and sweet peppers, green and lima beans, and collard, turnip, and mustard greens.
ARAB HERITAGE
- Many spices and herbs are used such as cinnamon, allspice, cloves, mint, ginger, and garlic.
- Meats are often skewer roasted or slow simmered; most common are lamb and chicken.
- Bread is served at every meal.
- Muslims do not eat pork, and all meats must be cooked well done.
- Food is eaten (and clients fed) with the right hand.
- Beverages are drunk after the meal, not during; alcohol is prohibited.
- Muslims fast during daylight hours during the month of Ramadan (the ninth month of the year based on the lunar calendar).
CHINESE HERITAGE
- Foods are served at meals in a specific order.
- Each region in China has its own traditional diet.
- Traditional Chinese may not want ice in their drinks.
- Foods are chosen to balance yin and yang in order to avoid indigestion.
- Soy sauce is used instead of salt.
JEWISH HERITAGE
- Dietary laws govern killing, preparation, and eating of foods.
- Meat and animal milk are not eaten at the same time; dairy substitutes (e.g., margarine) are permitted.
- Pork is one meat that is forbidden to eat.
- All blood must be drained from meats.
- Always wash hands before eating.
MEXICAN HERITAGE
- Rice, beans, and tortillas are core, essential foods.
- Larger body size may be viewed as a positive attribute.
- Sweet fruit drinks, including adding sugar to juice, are popular.
- The main meal of the day is at noontime.
- Foods are chosen according to hot and cold theory.
NAVAJO HERITAGE
- Rites of passage and ceremonies are celebrated with food.
- Herbs are used to treat many illnesses.
- Sheep are the major source of meat.
- Squash and corn are major vegetables.
5.2 NUTRITIONAL VARIATIONS THROUGHOUT THE LIFE CYCLE
Neonate to 1 Year
- Nutrition from breast milk or formula; ~80–100 mL/kg/day.
- Small stomach - feeds every 2.5-4 hrs, fed “on demand.”
- Introduce solids at 4–6 months (cereals, fruits, vegetables, meats; 1 food/5 days).
- Iron supplementation at ~6 months; avoid cow’s milk & honey <12 months.
- Begin weaning by 12–24 months; risk of bottle-mouth syndrome. The term describes decay of the teeth caused by constant contact with sweet liquid from the bottle.
Toddler (1–3 yrs)
- Eats 3 meals/day + snacks; developing self-feeding skills.
- Energy needs: 1,000–1,400 kcal/day; ~1,250 mL fluids/day.
- Common deficiencies: iron, calcium, vitamins A & C.
- Mealtime tips: small portions, variety, avoid food as reward, pleasant atmosphere.
Preschooler (3–5 yrs)
- Eats adult foods; needs healthy snacks (fruit, cheese, yogurt, veggies).
- ~1,500 mL fluids/day; still learning utensil use.
- Active → may rush meals; enjoys helping with food prep.
School-Age Child (6–12 yrs)
- Needs 1,600–2,200 kcal/day; protein-rich breakfast essential for school performance.
- Risk of obesity (increased junk food, decreased activity, peer pressure).
- Parents should model healthy eating, encourage balanced meals/snacks.
Adolescent (12–18 yrs)
- High needs: calories, protein, calcium, vit D, iron, B vitamins.
- Calcium 1,200–1,500 mg/day - peak bone mass.
- Tend to snack/diet irregularly; often choose high-calorie fast foods.
- Risks: obesity, anorexia nervosa, bulimia (linked to control, body image, depression).
- Encourage healthy snacks & shared responsibility for choices.
Young Adult (18–40 yrs)
- Needs balanced intake from all food groups.
- Women: 18 mg iron/day; folate supplementation to prevent neural tube defects.
- Calcium and Vitamin D for bone health.
- Risk: obesity, hypertension, CV disease-promote low-fat, low-cholesterol diet + exercise.
Middle-Aged Adult (40–65 yrs)
- Continue balanced diet; decrease calories (decreased metabolic rate & activity).
- Protein, calcium, vit D still important.
- Women (post-menopause): Increase calcium + vit D to prevent osteoporosis.
- Risks: obesity, diabetes, HTN, arthritis.
- Avoid fatty/fried foods; encourage exercise, behavior modification if overweight.
Older Adult (65+)
- Same nutrition needs but fewer calories (decreased metabolism, decreased activity).
- Increase Carbs for fiber/bulk; consider nutrient-dense foods.
- Barriers: tooth loss, decreased taste/smell, decreased saliva/gastric juice, isolation, decreased income, limited mobility/transportation.
- Psychosocial factors (loneliness, depression, loss of spouse) impact nutrition.
Dietary Guidelines For Americans
- Shift to more plant-based foods such as vegetables, fruits, grains, beans, and nuts.
- Significantly reduce foods with added sugars and solid fats.
- Engage in regular physical activity.
- Consume foods, including milk products, each day that increase commonly insufficient nutrients: vitamin D, calcium, potassium, and fiber.
- Keep daily total fat intake within 20% to 35% of total calories, less than 7% from saturated fatty acids and less than 300 mg cholesterol.
- Consume less than 1,500 mg of sodium per day.
- If you drink alcohol, do so in moderation (one drink per day for women and two drinks per day for men).
7.1 THE FOOD GUIDE PYRAMID AND MYPLATE
The Food Guide Pyramid is a graphic aid developed by the USDA as a guide in making daily food choices. On the pyramid, the food groups-grains, vegetables, fruits, milk, and meat and beans-are drawn from the base of the pyramid to the apex.
This indicates that activity, moderation, personalization, proportionality, variety, and gradual improvement are the keys to good nutrition.
MyPlate icon as a simpler reminder of how to implement the dietary guidelines. Promote getting more fruits and vegetables, whole grains, and low-fat dairy foods into the diet.
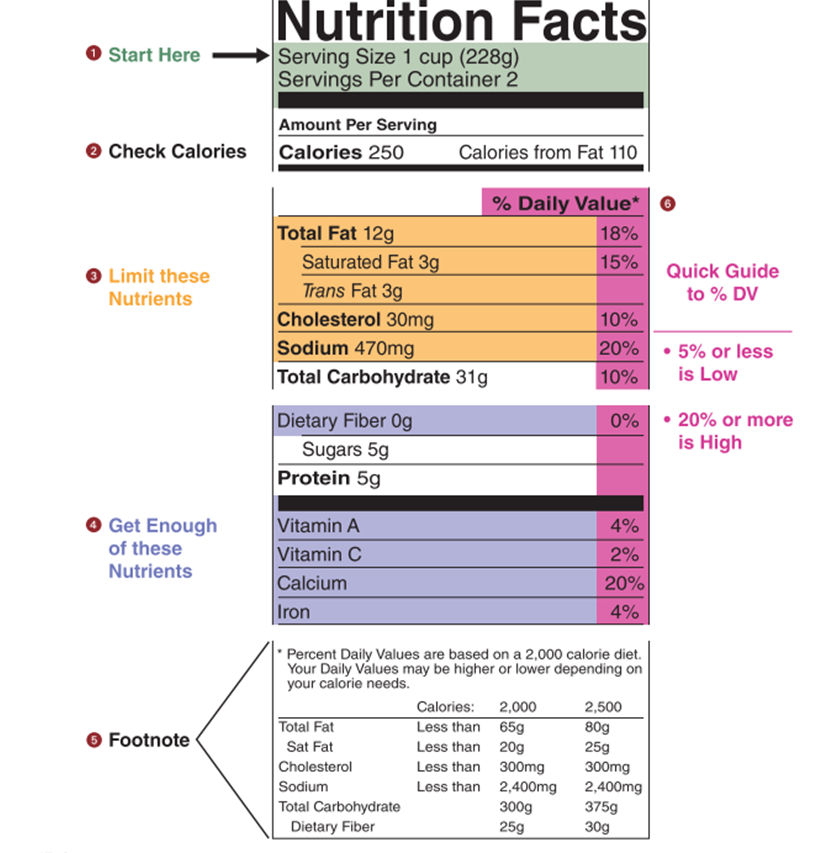
7.2 RECOMMENDED DIETARY INTAKE
Dietary reference intakes (DRIs) are the standards for nutrient recommendations that include the following values:
- Estimated average requirement (EAR): the average daily nutrient intake value estimated to meet the requirement of half the healthy individuals in a particular life stage and gender group
- Recommended dietary allowance (RDA): the average daily nutrient intake level sufficient to meet the nutrient requirement of nearly all (97% to 98%) healthy individuals in a particular life stage and gender group
- Adequate intake (AI): used when RDA cannot be determined; a recommended average daily nutrient intake level based on observed or experimentally determined approximations or estimates of nutrient intake for a group (or groups) of healthy people that are assumed to be adequate
- Tolerable upper intake level (UL): the highest average daily nutrient intake level likely to pose no risk of adverse health effects to almost all individuals in a particular life stage and gender group. As intake increases above the UL, the potential risk of adverse health effects increases.
Consumers most commonly learn recommended dietary intake information from the U.S. Food and Drug Administration (FDA) nutrition labels. Food labeling is required for most prepared foods, such as breads, cereals, canned and frozen foods, snacks, desserts, and drinks.
7.3 ALTERED NUTRITION
Malnutrition is commonly defined as the lack of necessary or appropriate food substances, but in practice includes both undernutrition and overnutrition.
Overnutrition refers to a caloric intake in excess of daily energy requirements, resulting in storage of energy in the form of adipose tissue. A person is said to be overweight when the BMI is between 25 and 29.9 kg/m2 and obese when the BMI is >30 kg/m2
Undernutrition refers to an intake of nutrients insufficient to meet daily energy requirements because of inadequate food intake or improper digestion and absorption of food.
Protein-calorie malnutrition (PCM), seen in starving children of underdeveloped countries, is now also recognized as a significant problem of clients with long-term deficiencies in caloric intake (e.g., those with cancer and chronic disease).
Characteristics of PCM are depressed visceral proteins (e.g., albumin), weight loss, and visible muscle and fat wasting.
Nursing Management
8.1 ASSESSING
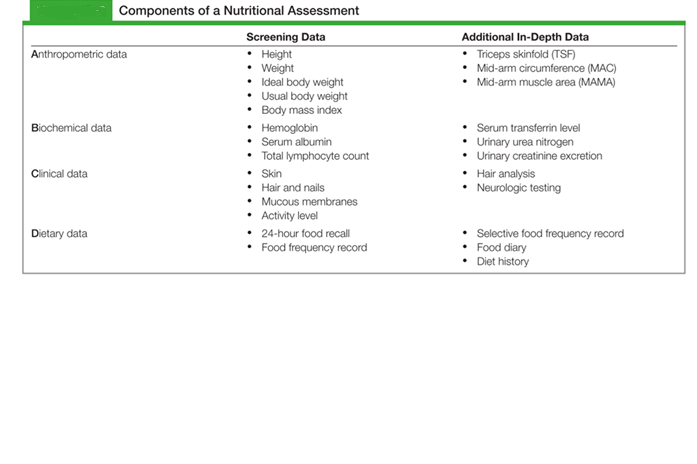
A nutritional assessment identifies clients at risk for malnutrition and those with poor nutritional status.
Components of a nutritional assessment and may be remembered as ABCD data: anthropometric, biochemical, clinical, and dietary.
Nursing insights: Risk factors for nutritional problems
DIET HISTORY
- Chewing or swallowing difficulties (including ill-fitting dentures, dental caries, and missing teeth)
- Inadequate food budget
- Inadequate food intake
- Inadequate food preparation facilities
- Inadequate food storage facilities
- Intravenous fluids (other than total parenteral nutrition for 10 or more days)
- Living and eating alone Physical disabilities
- Restricted or fad diets
MEDICAL HISTORY
- Adolescent pregnancy or closely spaced pregnancies
- Alcohol or substance abuse
- Catabolic or hypermetabolic condition: burns, trauma
- Chronic illness: end-stage renal disease, liver disease, AIDS, pulmonary disease (e.g., COPD), cancer
- GI problems: anorexia, dysphagia, nausea, vomiting, diarrhea, constipation
- Neurologic or cognitive impairment
- Oral and GI surgery
- Unintentional weight loss or gain of 10% within 6 months
MEDICATION HISTORY
- Antacids
- Antidepressants
- Antihypertensives
- Anti-inflammatory agents
- Antineoplastic agents Aspirin
- Digitalis Diuretics (thiazides)
- Laxatives
- Potassium chloride
NUTRITIONAL SCREENING
- Purpose: Quick assessment to identify risk for malnutrition.
- Nurses role: Perform screening; dietitians handle full assessments.
- High-risk indicators (Medicare standards for nursing homes):
- ≥5% weight loss in 1 month
- ≥7.5% in 3 months
- ≥10% in 6 months
1. Screening Tools
- PG-SGA: Classifies clients (well, moderately, severely malnourished); originally for cancer patients.
- NSI: Focuses on older adults; 9 warning signs checklist.
2. Nursing History (Key Data Collected)
- Age, sex, activity level
- Appetite/weight changes
- Chewing/swallowing difficulties
- Mouth/teeth condition, dentures
- Physical limitations (shopping, cooking, feeding self)
- Cultural/religious food practices
- Living situation, income, overall health
- Medications
3. Anthropometric Measurements
- TSF (Triceps Skinfold): Estimates fat stores.
- MAC (Mid-Arm Circumference): Fat + muscle + bone.
- MAMA (Mid-Arm Muscle Area): Lean body mass, calculated from TSF & MAC.
- Use: Detects chronic nutrition changes (slow, months to years).
- Limitations: Affected by hydration, aging, illness.
4. Biochemical Data (Lab Tests)
- Serum proteins
- Hemoglobin: Screens for iron deficiency anemia.
- Albumin: Reflects long-term protein status (half-life 18–20 days).
- Transferrin/TIBC: More sensitive to short-term changes (8–9 days).
- Prealbumin: Most sensitive to rapid protein changes (half-life 2 days).
- Urinary Tests
- Urea nitrogen: Indicates protein metabolism & nitrogen balance.
- Creatinine: Reflects muscle mass (↓ with malnutrition).
- Total lymphocyte count: ↓ with protein depletion (weakened immunity).
5. Clinical Data (Physical Exam)
- Focus on fast-growing tissues: skin, hair, nails, eyes, mucosa.
- Signs of malnutrition are nonspecific (e.g., dry hair may be sun damage).
- Must confirm with labs and dietary data.
6. Weight Assessment
- Compare Current Body Weight (CBW) with Usual Body Weight (UBW).
- % weight loss = [(UBW − CBW) ÷ UBW] × 100
- UBW is a better indicator than “ideal body weight” during illness.
7. Dietary Data Collection Methods
- 24-Hour Recall -quick, but may not reflect usual intake.
- Food Frequency Record -how often food groups are eaten.
- Food Diary -3-7 days of measured intake (more accurate).
- Diet History -detailed interview; most comprehensive.
8.2 DIAGNOSING
Nursing Diagnoses (NANDA Examples)
- Imbalanced Nutrition: Less Than Body Requirements
- Obesity / Overweight
- Readiness for Enhanced Nutrition
- Related diagnoses:
- Activity Intolerance (iron deficiency anemia)
- Constipation (low fiber/fluid)
- Low Self-Esteem (obesity)
- Risk for Infection (low protein - immune suppression)
8.3 PLANNING
Planning Goals
- Maintain/restore nutritional status
- Promote healthy eating habits
- Prevent malnutrition complications
- Support weight gain or loss as needed
Home Care Considerations:
- Assistance with feeding, shopping, and meal prep.
- Education on nutrition therapy.
8.4 IMPLEMENTING
Nursing interventions to promote optimal nutrition for hospitalized clients are often provided in collaboration with the primary care provider who writes the diet orders and the dietitian who informs clients about special diets.
The nurse:
- reinforces this instruction
- creates an atmosphere that encourages eating
- provides assistance with eating
- monitors the client’s appetite and food intake
- administers enteral and parenteral feedings
- consults with the primary care provider and dietitian about nutritional problems that arise
Special Dietary Requirements
10.1 TEXTURE/CONSISTENCY MODIFIED:
|
Type of diet |
Indications |
Examples |
|
Clear liquid diet |
Initial feeding after complete bowel rest. Initially to feed a malnourished person Bowel preparation for surgery or diagnostic tests Post-operatively Gastroenteritis |
water, bouillon, fat-free clear broth, clear fruit juices, carbonated beverages, gelatin, lemonade, ice pops, and regular or decaffeinated coffee or tea. Hard candy without filling |
|
Full liquid diet |
Transition diet after clear liquids following surgery difficulty chewing, swallowing, or tolerating solid foods |
all clear liquids and items such as plain ice cream, sherbet, breakfast drinks, milk, pudding and custard, plain yogurt, soups, fruit juices |
|
Mechanical soft diet |
Clients who have difficulty chewing, have dental problems, surgery of the head or neck, or dysphagia |
pureed, mashed, ground, or finely chopped. cream soups, ground or diced meats, flaked fish, cottage cheese, rice, potatoes, pancakes, light breads, cooked vegetables, canned or cooked fruits, bananas, peanut butter, and nonfried eggs |
|
Soft diet |
Clients who have difficulty chewing or swallowing. Ulcerations of the mouth or gums, oral surgery, broken jaw, plastic surgery of the head or neck, or dysphagia, or for the client who has had a stroke |
pastas, casseroles, tender meats, canned fruit, cooked vegetables, cakes, and cookies without nuts or coconut |
10.2 QUANTITATIVE NUTRIENT BASED MODIFICATIONS:
|
Type of diet |
Indications |
Examples |
|
Low-fiber diet |
inflammatory bowel disease, partial obstructions of the intestinal tract, gastroenteritis, diarrhea, or other gastrointestinal disorders |
white bread, refined cooked cereals, cooked potatoes without skins, white rice, and refined pasta |
|
High fiber diet |
constipation, irritable bowel syndrome when the primary symptom is alternating constipation and diarrhea, and asymptomatic diverticular disease |
fruits and vegetables and whole-grain products. |
|
Fat restricted diet |
malabsorption disorders, pancreatitis, gallbladder disease, and gastroesophageal reflux |
Restrict total amount of fat, including saturated, trans, polyunsaturated, and monounsaturated. |
|
High-calorie, high-protein diet |
severe stress, burns, wound healing, cancer, human immunodeficiency virus, acquired immunodeficiency syndrome, chronic obstructive pulmonary disease, respiratory failure, or any other type of debilitating disease |
Whole milk and milk products, peanut butter, nuts and seeds, beef, chicken, fish, pork, and eggs |
|
Sodium restricted diet |
hypertension, heart failure, renal disease, cardiac disease, and liver disease |
Encourage intake of fresh foods rather than processed food. Salt substitutes. |
|
Low-Potassium diet |
Impaired renal function, hypoaldosteronism, Addison’s disease, angiotensin-converting enzyme inhibitor medications, immunosuppressive medications, potassium-sparing diuretics, and chronic hyperkalemia |
applesauce, green beans, cabbage, lettuce, peppers, grapes, blueberries, cooked summer squash, cooked turnip greens, pineapple, and raspberries |
|
High-potassium diet |
renal tubular acidosis, gastrointestinal losses (diarrhea, vomiting), intracellular shifts, potassium-depleting diuretics, antibiotics, mineralocorticoid or glucocorticoid excess resulting from primary or secondary aldosteronism, Cushing’s syndrome, or exogenous corticosteroid use. |
All meats (red meat and chicken) and fish (salmon, cod, flounder, and sardines) Soy products and veggie burgers Vegetables (broccoli, peas, lima beans, tomatoes, potatoes [particularly their skins], sweet potatoes, and winter squash) Fruits (citrus, cantaloupe, bananas, kiwi, prunes, and dried apricot) |
|
Protein restricted diet |
renal disease and end-stage liver disease |
pastas, bread, cookies, wafers, and gelatin made with wheat starch, |
|
Low purine diet |
gout, kidney stones, and elevated uric acid levels |
anchovies, herring, mackerel, sardines, scallops, organ meats, gravies, meat extracts, wild game, goose, and sweetbreads. |
|
High calcium diet |
bone growth and in adulthood to prevent osteoporosis |
milk, cheese, yogurt, tofu Green leafy vegetables) Salmon and sardines Almonds, Brazil nuts, sunflower seeds, tahini, and dried beans Blackstrap molasses |
10.3 SPECIFIC CONDITIONS
|
Type of diet |
Indication |
Examples |
|
Renal diet |
Acute kidney injury or chronic kidney disease and for those requiring hemodialysis or peritoneal dialysis. |
Controlled amounts of protein, sodium, phosphorus, calcium, potassium. Most clients receiving dialysis need to restrict fluids. |
|
Cardiac diet |
Atherosclerosis, diabetes mellitus, hyperlipidemia, hypertension, myocardial infarction, nephrotic syndrome, and renal failure. |
Dietary Approaches to Stop Hypertension (DASH) diet recommended: fruits, vegetables, whole grains, low-fat dairy foods, meat, fish, poultry, nuts, and beans; it is limited in sugar sweetened foods and beverages, red meat, sodium, and fats. |
|
Diabetes Plate Method |
Clients with diabetes mellitus, hypoglycemia, hyperglycemia, and obesity. |
Fill half the plate with non-starchy vegetables, a quarter of the plate with lean protein foods and a quarter of the plate with complex carbohydrate foods. Drink water or a low-calorie drink. |
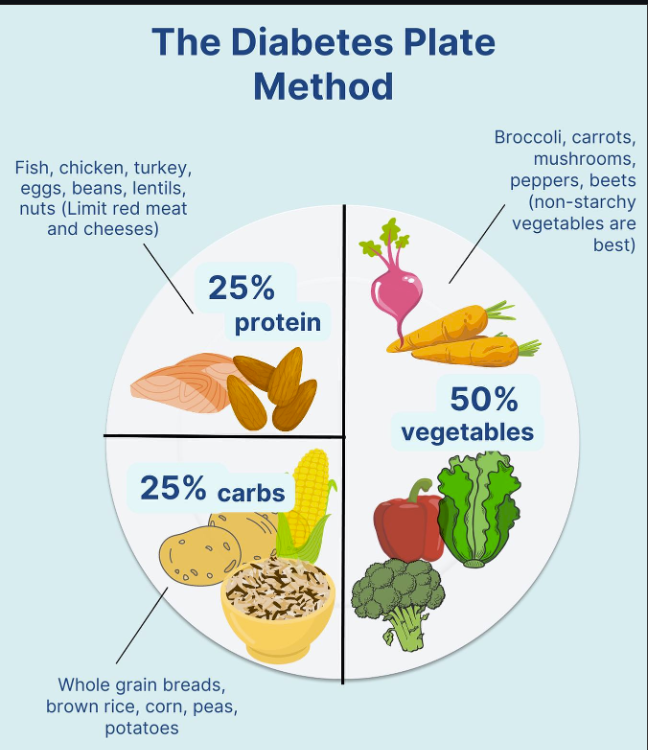
10.4 STIMULATING THE APPETITE
Physical illness, unfamiliar or unpalatable food, environmental and psychological factors, and physical discomfort or pain may depress the appetites of many clients.
- Provide familiar food that the person likes. Often the relatives of clients are pleased to bring food from home but may need some guidance about special diet requirements.
- Select small portions so as not to discourage the client.
- Avoid unpleasant or uncomfortable treatments immediately before or after a meal.
- Provide a tidy, clean environment that is free of unpleasant sights and odors. A soiled dressing, a used bedpan, an uncover ed irrigation set, or even used dishes can negatively affect the appetite.
- Encourage or provide oral hygiene before mealtime. This improves the client’s ability to taste.
- Relieve illness symptoms that depress appetite before mealtime; for example, give an analgesic for pain or an antipyretic for a fever or allow rest for fatigue.
- Reduce psychological stress. A lack of understanding of therapy, the anticipation of an operation, and fear of the unknown can cause anorexia. Often, the nurse can help by discussing feelings with the client, giving information and assistance, and allaying fears.
10.5 ENTERAL NUTRITION
Enteral nutrition (EN), also referred to as total enteral nutrition (TEN), is provided when the client cannot ingest foods or the upper GI tract is impaired and the transport of food to the small intestine is interrupted.
Enteral feedings are administered through nasogastric and small-bore feeding tubes, or through gastrostomy or jejunostomy tubes.
Nasogastric tube:
A nasogastric tube is inserted through one of the nostrils, down the nasopharynx, and into the alimentary tract.
Traditional firm, large-bore nasogastric tubes (i.e., those larger than 12 Fr in diameter) are placed into the stomach. Examples are the Levin tube, a flexible rubber or plastic, single-lumen tube with holes near the tip, and the Salem sump tube, with a double lumen.
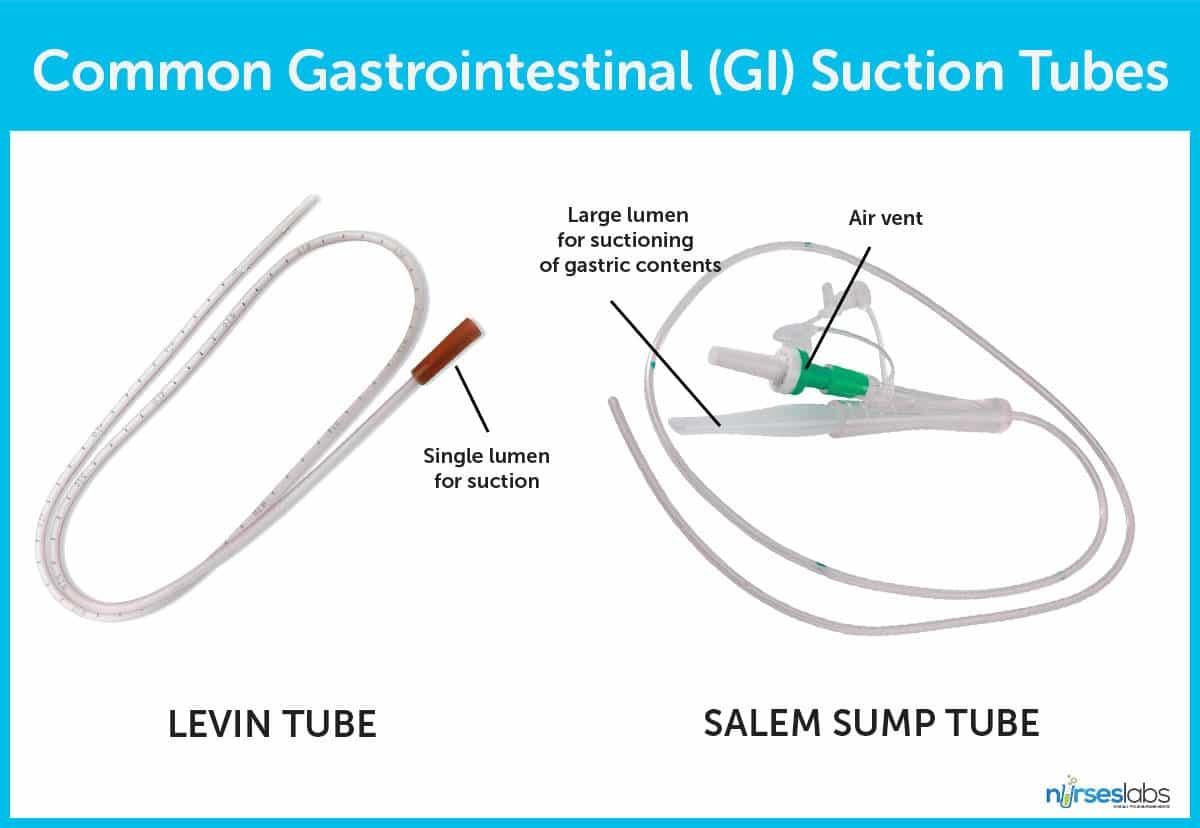
Insertion of an NG tube:
-
- Perform hand hygiene and observe other appropriate infection prevention procedures (e.g., clean gloves).
- Assess the client’s nares.
- Apply clean gloves.
- Ask the client to hyperextend the head, and, using a flashlight, observe the intactness of the tissues of the nostrils, including any irritations or abrasions.
- Examine the nares for any obstructions or deformities by asking the client to breathe through one nostril while occluding the other.
- Select the nostril that has the greater airflow.
- Prepare the tube.
- If a small-bore tube is being used, ensure stylet or guidewire is secured in position- An improperly positioned stylet or guidewire can traumatize the nasopharynx, esophagus, and stomach.
- If a large-bore tube is being used, place the tube in a basin of warm water while preparing the client. This allows the tubing to become more pliable and flexible.
- Determine how far to insert the tube.
- Use the tube to mark off the distance from the tip of the client’s nose to the tip of the earlobe and then from the tip of the earlobe to the tip of the xiphoid.
- Insert the tube- Lubricate the tip of the tube well with water-soluble lubricant or water to ease insertion.
- Insert the tube, with its natural curve downward, into the selected nostril. Direct the tube along the floor of the nostril and toward the midline.
- If the tube meets resistance, withdraw it, relubricate it, and insert it in the other nostril.
- Once the tube reaches the oropharynx (throat), the client will feel the tube in the throat and may gag and retch. Ask the client to tilt the head forward, and encourage the client to drink and swallow. Tilting the head forward facilitates passage of the tube into the posterior pharynx and esophagus rather than into the larynx; swallowing moves the epiglottis over the opening to the larynx.
- If the client continues to gag and the tube does not advance with each swallow, withdraw it slightly, and inspect the throat by looking through the mouth.
- Ascertain correct placement of the tube.
- Nasogastric tubes are radiopaque, and position can be confirmed by x-ray. If a SBFT is used, leave the stylet or guidewire in place until correct position is verified by x-ray.
- Aspirate stomach contents, and check the pH, which should be acidic. Aspirate can also be tested for bilirubin.
- Historically, nurses placed a stethoscope over the client’s epigastrium and injected 10 to 30 mL of air into the tube while listening for a whooshing sound. This method does not guarantee tube position.
11. Secure the tube by taping it to the bridge of the client’s nose.
Nasoenteric (nasointestinal) tube
A longer tube than the nasogastric tube (at least 40 cm [15.75 in.] for an adult), is inserted through one nostril down into the upper small intestine
Nasoenteric tubes are used for clients who are at risk for aspiration. Clients at risk for aspiration are those who manifest the following:
- Decreased level of consciousness
- Poor cough or gag reflexes
- Inability to participate in the procedure
- Restlessness or agitation.
Gastrostomy and jejunostomy devices
Are used for long-term nutritional support, generally more than 6 to 8 weeks. Tubes are placed surgically or by laparoscopy through the abdominal wall into the stomach (gastrostomy) or into the jejunum (jejunostomy).
A percutaneous endoscopic gastrostomy (PEG) or percutaneous endoscopic jejunostomy (PEJ) is created by using an endoscope to visualize the inside of the stomach, making a puncture through the skin and subcutaneous tissues of the abdomen into the stomach, and inserting the PEG or PEJ catheter through the puncture.
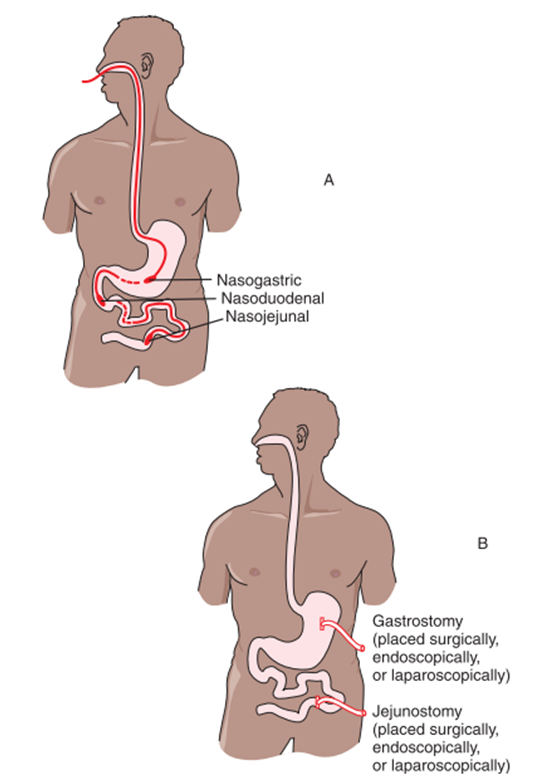
Enteral Feedings:
The type and frequency of feedings and amounts to be administered are ordered by the primary care provider.
Enteral feedings can be given intermittently or continuously.
Intermittent feedings are the administration of 300 to 500 mL of enteral formula several times per day. The stomach is the preferred site for these feedings, which are usually administered over at least 30 minutes. Initial intermittent feedings should be no more than 120 mL.
Bolus intermittent feedings are those that use a syringe to deliver the formula into the stomach.
Continuous feedings are generally administered over a 24-hour period using an infusion pump (often referred to as a kangaroo pump) that guarantees a constant flow rate. Initial intermittent feedings should be no more than 60 mL per hour.
Cyclic feedings are continuous feedings that are administered in less than 24 hours (e.g., 12 to 16 hours). These feedings, often administered at night, allow the client to attempt to eat regular meals through the day.
Enteral feedings are administered to clients through open or closed systems.
- Open systems use an open-top container or a syringe for administration. Open systems should have no more than 8 to 12 hours of formula poured at one time.
- Closed systems consist of a prefilled container that is spiked with enteral tubing and attached to the enteral access device. Prefilled containers can hang safely for 48 hours if sterile technique is used.
Nursing insights: Refeeding syndrome
A combination of fluid and electrolyte shifts that can occur after a lengthy period of malnutrition or starvation. This syndrome can occur when the starving body converts from creating glucose from carbohydrates to creating it from protein stores since carbohydrate was unavailable. The body’s reaction to the sudden presence of glucose and synthesis of protein leads to the shifts.
People at high risk for developing refeeding syndrome are those with chronic alcoholism, anorexia nervosa, massive weight loss, cancer clients receiving chemotherapy, or anyone who has gone 7 to 10 days without food.
Serum potassium, calcium, phosphate, and magnesium levels must be checked and supplemented until within normal levels before feeding.
10.6 PARENTERAL NUTRITION
Parenteral nutrition, also referred to as total parenteral nutrition (TPN) or intravenous hyperalimentation, is the IV infusion of dextrose, water, fat, proteins, electrolytes, vitamins, and trace elements.
Because TPN solutions are hypertonic (highly concentrated in comparison to the solute concentration of blood), they are injected only into high-flow central veins.
Peripheral parenteral nutrition (PPN) is delivered into the smaller peripheral veins. PPN cannot handle as concentrated a solution as central lines, but can accommodate lipids
Indications for TPN
- Severe malnutrition
- Severe burns
- Bowel disorders (ulcerative colitis, enteric fistula)
- Acute renal/hepatic failure
- Metastatic cancer
- Major surgery with NPO > 5 days
Summary
- Essential nutrients are grouped into categories: carbohydrates, proteins, lipids, vitamins, and minerals.
- Nutrients serve three basic purposes: forming body structures (such as bones and blood), providing energy, and helping to regulate the body’s biochemical reactions.
- The amount of energy that nutrients or foods supply to the body is their caloric value.
- Ideal body weight (IBW) is the optimal weight recommended for optimal health.
- Body mass index (BMI) and percent body fat are indicators of changes in body fat stores. They indicate whether a person’s weight is appropriate for height and may provide a useful estimate of nutrition.
- Assessment of nutritional status may involve all or some of the following: nutritional screening, nursing history data, anthropometric measurements, biochemical (laboratory) data, clinical data (physical examination), calculation of the percentage of weight loss, and a dietary history.
- Enteral feedings, administered through nasogastric, nasointestinal, gastrostomy, or jejunostomy tubes, are provided when the client is unable to ingest foods or the upper GI tract is impaired
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Nutrition
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


