Please set your exam date
Fetal Development
Study Questions
Practice Exercise
By which week of gestation is the fetal heart typically detectable via ultrasound?
Explanation
Fetal cardiac development begins early in gestation and follows a tightly regulated sequence of events that culminates in detectable cardiac activity. Cardiac tube formation, heartbeat initiation, ultrasound visualization, and valvular development are essential benchmarks. The fetal heart begins rhythmic contraction by day 22–23 post-conception, equivalent to week 5 gestation, and is typically detectable by transvaginal ultrasound by week 6 gestation. Heart rate ranges from 90–110 bpm at week 6, rising to 140–170 bpm by week 9. Visualization depends on equipment quality and maternal habitus, but week 6 remains the accepted norm in clinical guidelines.
Rationale for correct answers
B. Week 6 marks the earliest point at which transvaginal ultrasound can reliably detect fetal cardiac activity. The heart begins beating at 22–23 days post-fertilization, and by week 6 gestation, this activity is visible with sensitive ultrasound probes. The presence of cardiac motion at this stage confirms a viable intrauterine pregnancy.
Rationale for incorrect answers
A. At week 4, the fetal heart is still forming as a simple cardiac tube and has not yet initiated contractions. Although organogenesis has begun, cardiac activity cannot yet be visualized by ultrasound at this stage.
C. While fetal heart activity is clearly detectable by week 8, this is later than the earliest detectable point. Waiting until week 8 delays diagnosis of viability, particularly in early pregnancy assessments or evaluations for ectopic pregnancy.
D. By week 10, the fetal heart is well developed and easily visualized, but this is significantly later than necessary for initial viability assessments. Ultrasound at this point may assess more than viability, such as rhythm or structural anomalies.
Take home points
• Fetal cardiac activity begins at 22–23 days post-conception and is visible on ultrasound by week 6.
• Week 6 is the standard gestational age for confirming cardiac motion via transvaginal ultrasound.
• By week 8–10, fetal heart structures are more developed, but detection occurs earlier.
• Absence of cardiac activity at or after week 6 may suggest pregnancy failure if gestational dating is accurate.
A nurse is assessing a patient at 8 weeks gestation. Which system is most vulnerable to teratogens at this stage?
Explanation
Organogenesis is the phase in embryonic development during which organ systems form, making the embryo highly vulnerable to teratogens. The nervous system is the first major structure to develop, beginning in week 3, and continues through week 8 and beyond. Neural tube formation begins at day 18–21 and closes by day 28. Exposure to teratogens during this critical period can cause irreversible damage such as anencephaly or spina bifida. Folic acid deficiency is a leading cause of neural tube defects. The neural tissue remains susceptible longer than most other systems due to its prolonged development.
Rationale for correct answers
C. The nervous system is the most vulnerable to teratogens at 8 weeks gestation because this is the peak of its morphogenesis. By 8 weeks, the neural tube has closed, and rapid differentiation of the brain and spinal cord occurs. Disruption at this stage results in structural anomalies like hydrocephalus, anencephaly, or microcephaly.
Rationale for incorrect answers
A. The respiratory system begins development around week 4, but its critical period of vulnerability to teratogens occurs much later, primarily in the pseudoglandular and canalicular phases, from weeks 5 to 17 and 16 to 25 respectively. However, full maturation extends into the third trimester, making week 8 less critical for major structural anomalies.
B. The cardiovascular system begins forming at week 3 and is largely complete by week 8. Most congenital heart defects result from teratogenic exposure earlier in the first trimester. By week 8, major septation and outflow tract formation are usually complete, so this period is less vulnerable.
D. The musculoskeletal system starts developing in week 4 and continues throughout gestation. Although it is still differentiating at week 8, the most teratogen-sensitive window is earlier when somites are forming and limb buds are initiating (weeks 4 to 7). By week 8, musculoskeletal anomalies are less likely from new teratogenic insults.
Take home points
• The nervous system has the longest teratogen-sensitive period due to its early start and prolonged development.
• Week 8 is critical for brain and spinal cord differentiation, making neural tissue highly vulnerable.
• Cardiovascular defects originate earlier, typically between weeks 3 and 6.
• Teratogenic effects depend on timing, with different systems having unique windows of susceptibility.
A nurse is educating a patient about the importance of folic acid supplementation. What is the primary purpose of this nutrient in early pregnancy?
Explanation
Folic acid metabolism plays a critical role in early embryogenesis, particularly during neural tube closure. This process begins at day 18 post-conception and completes by day 28. Folic acid is required for DNA synthesis, cell division, and methylation reactions, which are essential during rapid cellular proliferation in early fetal development. The recommended daily intake is 400–800 mcg prior to conception and during the first trimester. Deficiency significantly increases the risk of neural tube defects such as spina bifida and anencephaly.
Rationale for correct answers
B. Folic acid prevents neural tube defects by supporting DNA synthesis and rapid cell division required for proper neural tube closure between days 18 and 28 post-conception. Supplementation before and during early pregnancy reduces neural tube defects by up to 70%.
Rationale for incorrect answers
A. Folic acid does not directly enhance fetal weight gain. Fetal growth is influenced by factors such as placental function, maternal nutrition overall, and gestational age, not folic acid alone.
C. While folic acid indirectly supports red blood cell production, its primary function in pregnancy is to prevent neural tube defects. Iron and vitamin B12 are more directly involved in hemoglobin synthesis.
D. Folic acid does not reduce the risk of gestational diabetes. Risk factors for gestational diabetes include obesity, family history, and insulin resistance. There is no strong evidence that folic acid modifies glucose metabolism.
Take home points
• Folic acid is essential for neural tube closure between days 18 and 28 post-conception.
• Supplementation reduces the risk of neural tube defects such as anencephaly and spina bifida.
• Recommended intake is 400–800 mcg daily before conception through the first trimester.
• Folic acid does not directly affect fetal weight gain or maternal glucose regulation.
At what gestational age does the developing organism transition from being called an embryo to a fetus?
Explanation
Embryo-to-fetus transition is marked by the completion of organogenesis and the beginning of growth and maturation phases. The embryonic period spans from implantation until the end of week 8, during which all major organ systems form. By the start of week 9, the organism is termed a fetus, reflecting the shift toward structural refinement and functional development. Critical processes such as neurulation, cardiac looping, and limb bud formation occur during this phase. The crown-rump length at this stage is approximately 30 mm, and fetal heart rate ranges between 140–170 bpm.
Rationale for correct answers
C. Week 8 marks the final week of the embryonic period, after which the developing organism is termed a fetus. This transition occurs at the beginning of week 9, following the completion of major organ system formation during the embryonic stage.
Rationale for incorrect answers
A. Week 4 is early in the embryonic period, when organogenesis has just begun. At this stage, processes such as gastrulation and early neural development are occurring, and the term "fetus" is not yet applicable.
B. Week 6 is mid-embryonic development. Organ systems, including the heart and neural tube, are actively forming, and the embryo is undergoing rapid morphogenesis. It is still scientifically referred to as an embryo.
D. Week 12 is well into the fetal period. By this time, organ systems are formed and are undergoing functional maturation. However, the transition from embryo to fetus has already occurred by the start of week 9.
Take home points
• The embryonic period ends at the close of week 8 gestation.
• The fetus begins at week 9, focusing on growth and functional maturation.
• Organogenesis occurs during weeks 3–8, making this a teratogen-sensitive phase.
• Terminology shift reflects developmental milestones, not fetal viability.
Which of the following are crucial events that occur during fertilization? Select all that apply.
Explanation
Fertilization involves a series of tightly regulated cellular events that allow a single sperm to penetrate the oocyte and initiate embryogenesis. These include capacitation, acrosomal reaction, cortical reaction, and syngamy. Capacitation occurs in the female reproductive tract and enhances sperm motility and membrane fluidity. The acrosomal reaction enables enzymatic digestion of the zona pellucida, while the cortical reaction blocks polyspermy through release of cortical granules. Normal fertilization occurs in the ampulla of the fallopian tube. Diploid zygote formation with 46 chromosomes follows nuclear fusion.
Rationale for correct answers
A. Capacitation is a prerequisite for successful fertilization. It occurs in the female reproductive tract and involves cholesterol efflux and membrane destabilization, which prepare the sperm for the acrosomal reaction.
B. The cortical reaction occurs immediately after the sperm penetrates the oocyte membrane. It involves exocytosis of cortical granules that modify the zona pellucida to prevent polyspermy, ensuring monospermic fertilization.
E. The acrosomal reaction allows the sperm to penetrate the zona pellucida by releasing hydrolytic enzymes like hyaluronidase and acrosin. This reaction is essential for sperm entry into the oocyte.
Rationale for incorrect answers
C. Implantation occurs several days after fertilization, typically between days 6–10 post-fertilization. It is not part of the fertilization process but rather a post-fertilization embryonic event involving trophoblast invasion of the endometrium.
D. Gastrulation occurs in the third week of development. It marks the formation of the three germ layers (ectoderm, mesoderm, endoderm) and is a post-implantation embryonic process, not part of fertilization.
Take home points
• Capacitation prepares sperm for fertilization by enhancing motility and membrane changes.
• Acrosomal reaction is essential for sperm penetration through the zona pellucida.
• Cortical reaction prevents polyspermy and ensures successful monospermic fertilization.
• Implantation and gastrulation are post-fertilization events and occur days later.
Practice Exercise 2
Which of the following begins to form on the fetal skin during the early second trimester?
Explanation
Fetal skin development progresses in defined stages, influenced by keratinization, hair follicle formation, and sebaceous gland activity. By the early second trimester (weeks 13–16), the fetus begins producing lanugo—fine, unpigmented hair—and vernix caseosa, a lipid-rich, white protective substance. Lanugo helps anchor vernix to the skin, while vernix caseosa provides barrier protection, prevents fluid loss, and has antimicrobial properties. Subcutaneous fat, by contrast, begins to accumulate significantly in the third trimester, particularly after week 28.
Rationale for correct answers
D. Both lanugo and vernix caseosa begin to form in the early second trimester. Lanugo appears first and facilitates the adherence of vernix caseosa, which is secreted by fetal sebaceous glands. Their formation marks key protective adaptations of fetal skin.
Rationale for incorrect answers
A. Subcutaneous fat does not begin to accumulate until the third trimester. Fat deposition accelerates after week 28 and continues until term, helping with thermoregulation and energy storage postpartum.
B. Lanugo begins to form around weeks 13–16 and is a normal early second-trimester feature. However, it is not the only structure that forms at this time, making this answer incomplete.
C. Vernix caseosa begins to develop alongside lanugo in the early second trimester. It alone does not represent the full scope of what occurs during this period, making this option incomplete.
Take home points
• Lanugo and vernix caseosa both begin forming in the early second trimester.
• Subcutaneous fat accumulates later, primarily in the third trimester.
• Vernix caseosa has antimicrobial and barrier functions in fetal skin protection.
• Lanugo helps retain vernix on the fetal skin surface.
What is "quickening" in pregnancy?
Explanation
Quickening refers to the first maternal perception of fetal movement, typically occurring between 18 and 20 weeks gestation in nulliparous women and as early as 16 weeks in multiparous women. It results from increased neuromuscular coordination, fetal strength, and uterine wall sensitivity. Quickening is influenced by placental location, with posterior placentas allowing earlier detection than anterior ones. These movements are critical indicators of neurologic integrity and fetal viability and become more regular as gestation advances.
Rationale for correct answers
A. Quickening is defined as the first sensation of fetal movement perceived by the pregnant person. It generally occurs around 18–20 weeks in first pregnancies due to lower uterine sensitivity and around 16 weeks in subsequent pregnancies due to increased awareness. The movement represents advancing fetal neuromuscular development.
Rationale for incorrect answers
B. The rapid growth spurt occurs during the second trimester but is not related to maternal perception of fetal movement. Fetal length increases from approximately 9 cm at week 12 to 25 cm by week 20, but this process is silent to maternal sensation.
C. Braxton Hicks contractions are irregular, painless uterine contractions that begin in the second trimester but typically intensify in the third. They are not perceived as fetal movement and are unrelated to the neurologic activity of the fetus.
D. Engagement of the fetal head, also called lightening, occurs near term when the presenting part descends into the pelvic inlet. This mechanical process is different from fetal movement and occurs later, usually after 36 weeks in primigravida.
Take home points
• Quickening is the first perceived fetal movement, typically at 18–20 weeks gestation.
• It is earlier in multiparous women and later in primigravida.
• It reflects fetal neuromuscular maturation and uterine wall sensitivity.
• It must be differentiated from Braxton Hicks contractions and lightening.
During which weeks do fetal movements typically become perceptible to primigravida mothers?
Explanation
Fetal movement perception is a physiologic milestone influenced by gestational age, parity, uterine sensitivity, and placental location. In primigravida mothers, the first perception of fetal movement—quickening—typically occurs between weeks 18 and 20, though it may be reported as early as week 16. Multiparous women may notice movement earlier due to heightened neuromuscular awareness and abdominal wall laxity. Fetal movement frequency increases after week 20 and becomes more organized as the central nervous system matures. Movements are associated with intact neurologic and musculoskeletal systems and are a marker of fetal well-being.
Rationale for correct answers
B. Weeks 16–20 are when fetal movements become perceptible to most primigravida mothers. The first movements are usually felt at 18–20 weeks due to the lower sensitivity of the uterine wall and unfamiliarity with fetal activity in first-time pregnancies. This timeframe reflects neurologic maturation and increasing fetal strength.
Rationale for incorrect answers
A. Fetal movement at weeks 12–14 is minimal and not strong enough to be perceived by the mother. Although spontaneous movements occur by week 7–8 on ultrasound, they are too subtle for maternal detection this early.
C. While fetal movements are definitely present by weeks 21–24, this is later than the expected window for initial perception in primigravida mothers. Most first-time mothers have already reported quickening by this stage.
D. Weeks 25–28 are well beyond the expected time of initial fetal movement perception. Movements during this stage are more forceful and regular but should not be the first perceived movements in a normal pregnancy.
Take home points
• Primigravida mothers typically perceive fetal movement at 18–20 weeks gestation.
• Movements may be felt as early as week 16 but rarely before.
• Earlier perception is more common in multiparous women.
• Delayed perception beyond 20 weeks may require clinical evaluation.
Which diagnostic test is commonly performed in the second trimester to assess fetal development?
Explanation
Second-trimester fetal assessment focuses on evaluating structural development, growth parameters, and anomalies. The most commonly used diagnostic tool is ultrasound, particularly the anatomy scan or level II ultrasound, typically done between 18 and 22 weeks. It assesses fetal biometry, organ structure, amniotic fluid volume, placental location, and fetal sex. Normal biparietal diameter (BPD) at 20 weeks is approximately 45–52 mm, femur length (FL) is 30–32 mm, and amniotic fluid index (AFI) ranges from 8 to 18 cm. Ultrasound is non-invasive, safe, and widely accessible.
Rationale for correct answers
C. Ultrasound is the most commonly used diagnostic test in the second trimester for evaluating fetal development. The detailed anatomy scan performed at 18–22 weeks assesses organ formation, fetal measurements, and detects structural abnormalities such as neural tube or cardiac defects. It is non-invasive and provides real-time imaging.
Rationale for incorrect answers
A. Non-stress test (NST) is used in the third trimester, typically after 28 weeks, to assess fetal heart rate patterns in response to movement. It evaluates fetal well-being in high-risk pregnancies but does not assess fetal anatomy or development in the second trimester.
B. Amniocentesis can be performed in the second trimester (usually after 15 weeks), but it is not a routine assessment of fetal development. It is an invasive diagnostic test used for genetic testing, lung maturity, or infection evaluation when indicated.
D. Biophysical profile is done later in pregnancy, typically after 28 weeks, to assess fetal well-being using ultrasound and NST. It evaluates fetal breathing, tone, movement, and amniotic fluid but is not used for developmental assessment during the second trimester.
Take home points
• Ultrasound is the standard second-trimester test to assess fetal anatomy and growth.
• Detailed anatomy scans are done between 18 and 22 weeks.
• NST and biophysical profiles are third-trimester assessments of fetal well-being.
• Amniocentesis is used selectively for genetic diagnosis, not routine development screening.
Which of the following statements about the second trimester (weeks 14-27) are true? Select all that apply.
Explanation
Second trimester development (weeks 14–27) is characterized by fetal growth, organ maturation, and increasing structural refinement rather than initial organogenesis, which concludes by week 8. During this period, vernix caseosa begins forming around week 20, external genitalia become clearly distinguishable on ultrasound by weeks 16–18, and lanugo emerges but does not disappear until the third trimester. Subcutaneous fat starts accumulating in the third trimester, particularly after week 28, and is critical for postnatal thermoregulation and energy metabolism.
Rationale for correct answers
C. Vernix caseosa begins to cover the fetal skin in the second trimester, typically starting around week 20. It is secreted by sebaceous glands and composed of water, lipids, and desquamated epithelial cells, providing barrier and antimicrobial protection.
D. External genitalia are usually well-differentiated and visible on ultrasound by weeks 16–18, allowing accurate determination of fetal sex. Genital differentiation is hormonally regulated and is typically complete by the mid-second trimester.
Rationale for incorrect answers
A. Significant subcutaneous fat accumulation occurs in the third trimester, primarily after week 28. Before this, the fetus appears thin and translucent due to minimal fat stores. Fat deposition is essential for thermal insulation and energy storage after birth.
B. Lanugo begins to form during the early second trimester (around weeks 13–16) and does not disappear by the end of the trimester. It typically persists into the third trimester, disappearing closer to term, around weeks 36–38.
E. Organogenesis is the hallmark of the first trimester, concluding by week 8. The second trimester focuses on organ growth, functional maturation, and morphologic development, not initial formation.
Take home points
• Vernix caseosa begins forming by week 20 for skin protection and moisture retention.
• External genitalia are usually visible on ultrasound by weeks 16–18.
• Subcutaneous fat develops later, mainly in the third trimester.
• Organogenesis ends in the first trimester; the second focuses on maturation.
Practice Exercise 3
What is the approximate fetal weight by week 26?
Explanation
Fetal growth in the second trimester follows a predictable pattern influenced by genetic, placental, and maternal factors. By week 26, the fetus typically weighs between 600 and 800 grams, with an average crown-to-heel length of 35–36 cm. The fetal weight increases rapidly from approximately 350 grams at week 22 to over 1,000 grams by week 28. Fetal lung development, muscle mass gain, and fat deposition also begin accelerating near the end of this period. Normal fetal growth parameters are assessed using biometric measurements such as femur length, abdominal circumference, and biparietal diameter.
Rationale for correct answers
B. At 26 weeks, the average fetal weight is approximately 760 grams, well within the range of 600–800 grams. This corresponds with fetal length of about 35 cm and increasing viability due to progressive lung and CNS maturation.
Rationale for incorrect answers
A. By week 26, the fetus exceeds 400 grams. A weight of 300–400 grams corresponds more closely to fetal parameters seen around week 20–22, not week 26.
C. A weight of 1–1.2 kg is typical around week 28–30, during early third trimester. At week 26, the fetus has not yet accumulated enough fat and muscle to reach this mass.
D. Weights of 1.5–2 kg occur in the late third trimester, generally around weeks 32–34. This is beyond the expected weight for a fetus at 26 weeks.
Take home points
• The average fetal weight at week 26 is approximately 760 grams.
• Fetal growth accelerates significantly after week 24 due to fat and muscle accumulation.
• Biometric measurements assess intrauterine growth and detect fetal growth restriction.
• Fetal viability improves significantly after week 24 due to organ maturation.
Which medication is administered to enhance fetal lung maturity in cases of preterm labor?
Explanation
Fetal lung maturation is critical for extrauterine survival, particularly before 34 weeks gestation, when surfactant production is often insufficient. Betamethasone, a glucocorticoid, is administered intramuscularly to the pregnant person to stimulate type II alveolar cells to produce surfactant, primarily dipalmitoylphosphatidylcholine (DPPC). It crosses the placenta and promotes structural and biochemical maturation of the fetal lungs. The standard regimen is 12 mg intramuscularly every 24 hours for 2 doses. Benefits are greatest when birth occurs 24–48 hours after the first dose and include reduced risks of neonatal respiratory distress syndrome, intraventricular hemorrhage, and necrotizing enterocolitis.
Rationale for correct answers
B. Betamethasone is the drug of choice to enhance fetal lung maturity in preterm labor. It accelerates surfactant synthesis and lung development when administered between 24 and 34 weeks gestation, reducing neonatal respiratory morbidity.
Rationale for incorrect answers
A. Magnesium sulfate is used for neuroprotection in preterm infants <32 weeks and for seizure prophylaxis in preeclampsia, not lung maturation. It does not stimulate surfactant production.
C. Oxytocin is a uterotonic agent used to induce or augment labor, not to promote fetal lung maturity. Its administration would worsen preterm labor outcomes by promoting contractions.
D. Nifedipine is a calcium channel blocker used as a tocolytic to delay preterm labor. While it can prolong pregnancy, it does not directly influence surfactant production or lung development.
Take home points
• Betamethasone promotes fetal lung maturity by enhancing surfactant synthesis.
• It is administered between 24–34 weeks gestation in cases of preterm labor risk.
• Optimal benefit occurs within 24–48 hours of administration.
• Magnesium sulfate is for neuroprotection, not lung development.
At what gestational age is Group B Streptococcus (GBS) screening typically performed in pregnant women?
Explanation
Group B Streptococcus (GBS) screening is a universal prenatal test conducted to identify maternal colonization with Streptococcus agalactiae, which can cause early-onset neonatal sepsis, pneumonia, and meningitis. The screening is typically performed between 36 and 37 weeks gestation using a vaginal-rectal swab to best predict colonization status at delivery. Colonization can be transient, intermittent, or persistent, so testing too early may not reflect status at birth. If positive, intrapartum antibiotic prophylaxis (usually penicillin G) is recommended to reduce neonatal infection risk. GBS colonization does not typically cause maternal illness.
Rationale for correct answers
D. Screening is recommended between 36–37 weeks gestation because this timing best correlates with colonization status at delivery. Positive results prompt intrapartum antibiotic administration to prevent neonatal transmission during vaginal delivery.
Rationale for incorrect answers
A. Testing at 24–26 weeks is too early to accurately predict colonization status at term, since GBS colonization can change. Early testing may miss new colonization or clear existing transient colonization.
B. At 28–30 weeks, GBS screening is still premature. Colonization detected at this point does not reliably indicate presence at delivery, potentially leading to unnecessary or missed prophylaxis.
C. While 32–34 weeks is closer to delivery, it is still earlier than recommended. Testing at this stage may not reflect GBS status at term, reducing accuracy and predictive value.
Take home points
• GBS screening is optimally done at 36–37 weeks gestation.
• The test involves a vaginal-rectal swab to detect maternal colonization.
• Positive results require intrapartum penicillin to prevent neonatal GBS disease.
• Early testing is unreliable due to transient colonization.
Which of the following provides passive immunity to the fetus in the third trimester?
Explanation
Passive immunity in the fetus during the third trimester is primarily conferred by the transplacental transfer of maternal immunoglobulin G (IgG) antibodies. This process is facilitated by the neonatal Fc receptor (FcRn) in the placenta, which actively transports IgG from the maternal circulation to the fetal bloodstream. The transfer increases significantly after week 28, peaking near term, and provides temporary protection against pathogens such as measles, rubella, and tetanus. Other immunoglobulin classes, like IgM and IgA, do not cross the placenta. This maternal-fetal IgG transfer helps protect the neonate during the early postnatal period when the infant's immune system is still immature.
Rationale for correct answers
B. Maternal antibodies, specifically IgG, cross the placenta starting around 20 weeks but most significantly after 28 weeks. This provides the fetus with passive immunity to pathogens the mother has previously encountered or been vaccinated against, protecting the neonate until their own immune system matures.
Rationale for incorrect answers
A. The fetal liver produces immunoglobulins like IgM but cannot produce IgG in significant quantities. IgM is the first antibody synthesized by the fetus but does not confer maternal-derived passive immunity.
C. Amniotic fluid contains nutrients, hormones, and fetal waste products but does not deliver immunoglobulins systemically. While some immune cells may be present, it does not function in providing passive immunity.
D. Placental hormones (e.g., hCG, progesterone, estrogens) support pregnancy maintenance and fetal development but do not play a role in immune protection. They do not transfer antibodies or confer immune function.
Take home points
• IgG is the only antibody class that crosses the placenta to provide fetal immunity.
• Passive immunity transfer increases sharply after 28 weeks gestation.
• IgM and IgA do not cross the placenta and are synthesized by the fetus.
• Placental Fc receptors facilitate selective IgG transfer to the fetus.
What is the primary role of surfactant in the fetal lungs?
Explanation
Surfactant physiology is vital for fetal pulmonary development and neonatal respiratory function. Surfactant is a lipoprotein complex primarily composed of dipalmitoylphosphatidylcholine (DPPC), produced by type II alveolar cells beginning around week 20, with significant increases after week 32. Its main function is to reduce surface tension within the alveoli, preventing collapse during exhalation and enabling efficient lung expansion at birth. Surfactant also contributes to alveolar stability, compliance, and gas exchange. The lecithin-to-sphingomyelin (L/S) ratio, with a normal maturity value of ≥2:1, is a key indicator of fetal lung maturity.
Rationale for correct answers
B. Surfactant reduces surface tension at the air-liquid interface within alveoli, allowing them to remain open during respiration. This prevents atelectasis after the first breath, enabling effective lung inflation and gas exchange in the neonate.
Rationale for incorrect answers
A. Oxygen transport to the fetus occurs via placental gas exchange, not surfactant. Oxygenated maternal blood diffuses through the placenta to the fetal circulation, independent of pulmonary function before birth.
C. While surfactant has minor immune-modulatory functions, its primary role is not infection prevention. Other components like alveolar macrophages and immunoglobulins play a more significant role in pulmonary immune defense.
D. Fetal breathing movements are controlled by the central nervous system and are not driven by surfactant. These movements begin around week 20 and help condition respiratory muscles, but surfactant is not their initiator.
Take home points
• Surfactant reduces alveolar surface tension, preventing collapse during neonatal breathing.
• Type II alveolar cells begin surfactant production around week 20.
• Adequate surfactant levels are critical by week 34 to avoid respiratory distress syndrome.
• L/S ratio ≥2:1 indicates sufficient surfactant for postnatal respiration.
Comprehensive Questions
Which of the following is a critical nursing intervention during the first trimester to prevent congenital anomalies?
Explanation
Teratogen exposure during the first trimester poses the highest risk for congenital anomalies due to organogenesis, which occurs between weeks 3 and 8 of gestation. Teratogens disrupt cellular differentiation, DNA synthesis, and tissue morphogenesis, resulting in structural or functional fetal defects. Common teratogens include retinoic acid, ACE inhibitors, valproic acid, alcohol, tobacco, radiation, and certain infections such as rubella and toxoplasmosis. Severity depends on dose, timing, and genetic susceptibility. Avoidance and early counseling are crucial. No safe threshold exists for many teratogens, and even brief exposure can lead to anomalies during this critical developmental period.
Rationale for correct answers
C. Educating on teratogen avoidance is the most critical nursing intervention in the first trimester. This is the peak window for organ development, so exposure to substances like alcohol, tobacco, certain medications, or infections can lead to major congenital anomalies. Timely education minimizes preventable teratogenic risk.
Rationale for incorrect answers
A. Administering corticosteroids is used in the second or third trimester, typically between 24 and 34 weeks, to promote fetal lung maturity in cases of preterm labor risk. It does not prevent congenital anomalies and is not a first trimester intervention.
B. Monitoring fundal height is not applicable in the first trimester because the uterus remains a pelvic organ until around 12 weeks. Fundal height measurements begin after 20 weeks gestation as a tool for tracking fetal growth, not anomaly prevention.
D. Performing Leopold’s maneuvers is relevant in the third trimester, typically after 28 weeks, to assess fetal position and presentation. It is unrelated to early congenital anomaly prevention and not useful in the first trimester.
Take home points
• Teratogen exposure in the first trimester can cause irreversible structural defects.
• Weeks 3–8 are the most critical for organogenesis and highest teratogenic risk.
• Nursing education on substance avoidance is essential during early prenatal visits.
• Not all common interventions are appropriate or effective in the first trimester.
What is the primary role of human chorionic gonadotropin (hCG) in early pregnancy?
Explanation
Human chorionic gonadotropin (hCG) is a glycoprotein hormone produced by syncytiotrophoblasts of the developing placenta beginning around day 6–8 post-fertilization. Its primary role in early pregnancy is to maintain the corpus luteum, which in turn secretes progesterone to sustain the endometrial lining and prevent menstruation. hCG levels double every 48–72 hours in a viable early pregnancy, peaking around 100,000 mIU/mL by weeks 8–11, then gradually decline. Normal range at 4 weeks gestation is approximately 5–426 mIU/mL. hCG also promotes immune tolerance, supports placental growth, and is the basis for urine and serum pregnancy tests.
Rationale for correct answers
B. hCG maintains the corpus luteum during the first 8–10 weeks of pregnancy, ensuring continued secretion of progesterone, which is essential for maintaining the decidua and preventing uterine contraction. Without hCG support, the corpus luteum would regress and lead to pregnancy loss.
Rationale for incorrect answers
A. Fetal lung maturation is not influenced by hCG. This function is regulated by cortisol and surfactant production, which are stimulated by glucocorticoids such as betamethasone during the third trimester.
C. Fetal weight gain occurs primarily in the third trimester and is regulated by placental nutrient transfer, insulin-like growth factors, and maternal nutrition, not by hCG.
D. Labor contractions are initiated by increased oxytocin, prostaglandins, and estrogen at term. hCG has no role in triggering parturition.
Take home points
• hCG maintains corpus luteum function in early pregnancy to support progesterone production.
• Peak hCG levels occur between weeks 8–11 and decline thereafter.
• hCG is the hormone detected in pregnancy tests.
• It is produced by syncytiotrophoblast cells of the trophoblast.
What is the recommended daily folic acid supplementation for women of childbearing age to prevent neural tube defects?
Explanation
Folic acid supplementation is critical for preventing neural tube defects (NTDs) such as spina bifida and anencephaly, which arise from failure of neural tube closure by day 28 post-conception. Folate, a B-vitamin (B9), is required for DNA synthesis, methylation, and cell division. Since neural tube formation occurs early, often before pregnancy is confirmed, supplementation should begin at least 1 month prior to conception. The recommended daily intake for women of childbearing age is 400 mcg (0.4 mg) of folic acid. For women with a history of NTDs or high-risk conditions (e.g., diabetes, antiseizure therapy), the dosage increases to 4 mg daily.
Rationale for correct answers
C. The CDC and WHO recommend 400 mcg of folic acid daily for all women of childbearing potential to reduce the risk of NTDs. This amount ensures adequate folate status for early embryonic neural tube closure, which completes by the 4th week of gestation.
Rationale for incorrect answers
A. 100 mcg is insufficient for NTD prevention. This dose may be found in food but is below the therapeutic threshold required for reducing neural tube malformations.
B. 200 mcg is still subtherapeutic. Evidence-based guidelines consistently show that at least 400 mcg per day is needed for effective neural tube defect risk reduction.
D. 800 mcg is above the general recommendation. While not harmful in most cases, this higher dose is reserved for special populations or prenatal supplements and is not routinely recommended for all women unless otherwise indicated.
Take home points
• The neural tube closes by day 28; early folic acid intake is essential.
• 400 mcg daily is recommended for all women of reproductive age.
• Higher doses are used in women with prior NTD-affected pregnancies or high-risk conditions.
• Folate is vital for DNA synthesis and embryonic cell division.
At what approximate gestational age can external genitalia typically be distinguished as male or female on ultrasound?
Explanation
Fetal sexual differentiation begins early but genitalia visualization on imaging is influenced by several developmental milestones. Testosterone, secreted by fetal Leydig cells, influences external genitalia starting from week 8. However, distinct labioscrotal and phallus development features become ultrasonographically visible around week 14. The normal fetal heart rate is 110–160 bpm, and accurate sex determination depends on genital tubercle angle, with full differentiation by week 14. Chromosomal sex is determined at conception (XX or XY), but phenotypic differentiation requires hormonal influence, especially dihydrotestosterone.
Rationale for correct answers
D. By week 14, the external genitalia are typically developed enough to be distinguished by ultrasound. The scrotal sac and penile shaft in males, and labial folds in females, become distinct. Visualization accuracy improves with high-resolution transabdominal ultrasound and adequate amniotic fluid volume.
Rationale for incorrect answers
A. Week 8 marks the start of genital ridge differentiation into either testes or ovaries under influence of the SRY gene in XY embryos. However, external genitalia are still undifferentiated and identical in appearance in both sexes, making ultrasound distinction impossible.
B. By week 10, internal reproductive structures such as Müllerian and Wolffian ducts begin differentiating. However, external features remain ambiguous on imaging. At this stage, the genital tubercle is still forming and appears similar in both sexes.
C. Week 12 is the transitional phase where the external genitalia begin to show early signs of sexual differentiation. However, the features are often subtle, and accurate identification on ultrasound remains unreliable due to overlapping characteristics and suboptimal visualization.
Take home points
• Ultrasound visualization of external genitalia becomes reliable around week 14 of gestation.
• Phenotypic differentiation requires androgens such as testosterone and dihydrotestosterone.
• Chromosomal sex is determined at fertilization, but visible genitalia emerge later.
• Genital tubercle angle and shape are early markers but lack specificity before week 14.
What is the primary function of the kidneys in the fetus by week 12?
Explanation
Fetal renal development begins during week 5 of gestation with the formation of the metanephros, the permanent kidney. By week 9–12, the kidneys start producing urine, which is excreted into the amniotic cavity, making the kidneys a major contributor to amniotic fluid volume. Amniotic fluid, composed largely of fetal urine after the first trimester, is essential for lung development, fluid-electrolyte balance, and musculoskeletal movement. The fetal glomerular filtration rate (GFR) remains low compared to postnatal levels, and fetal kidneys do not filter maternal blood. Normal amniotic fluid index (AFI) ranges from 5 to 25 cm in the second and third trimesters.
Rationale for correct answers
B. By week 12, fetal kidneys begin producing urine, which is excreted into the amniotic sac. This urine significantly contributes to amniotic fluid volume, which is vital for normal fetal development, particularly pulmonary and musculoskeletal growth.
Rationale for incorrect answers
A. Red blood cells are produced by the yolk sac early in gestation, then by the liver and spleen. The fetal kidneys do not participate in hematopoiesis at any stage.
C. The fetal kidneys are immature and do not regulate systemic blood pressure effectively. Fetal blood pressure regulation is primarily under control of the placenta and fetal adrenal hormones, not the renal system.
D. Fetal kidneys do not filter maternal blood. Exchange of nutrients and waste products between mother and fetus occurs via the placenta, not through direct blood filtration by fetal organs.
Take home points
• Fetal kidneys begin producing urine by weeks 9–12.
• Urine becomes the main source of amniotic fluid after the first trimester.
• Amniotic fluid supports lung development and fetal movement.
• Fetal kidneys do not regulate blood pressure or filter maternal blood.
What is the primary role of the placenta during fetal development?
Explanation
Placental function is central to fetal development, beginning after implantation and becoming fully functional by the end of the first trimester. The placenta serves as a semi-permeable barrier, allowing nutrient and gas exchange, waste elimination, and hormone production. It transfers oxygen, glucose, amino acids, and fatty acids to the fetus and removes carbon dioxide, urea, and other waste products. It also synthesizes essential hormones such as hCG, progesterone, estrogen, and human placental lactogen (hPL) to support pregnancy and fetal growth. While it offers partial immune protection, it does not fully block pathogens like rubella virus or Toxoplasma gondii.
Rationale for correct answers
C. The placenta facilitates bidirectional exchange of nutrients, oxygen, and waste between maternal and fetal circulations and produces hormones like hCG, progesterone, estrogen, and hPL, which are vital for maintaining pregnancy and supporting fetal development.
Rationale for incorrect answers
A. Fetal red blood cells are produced by the yolk sac, liver, and bone marrow during different stages of development, not the placenta. The placenta does not have a hematopoietic function.
B. Fetal temperature is regulated by maternal homeostasis, not by the placenta. The fetus remains slightly warmer (~0.5°C) than the maternal core temperature due to high metabolic activity.
D. While the placenta acts as a partial barrier, it does not prevent all infections. Pathogens such as cytomegalovirus, rubella, herpes simplex virus, varicella-zoster, HIV, and Toxoplasma gondii can cross the placenta and cause congenital infections.
Take home points
• The placenta is responsible for gas, nutrient, and waste exchange.
• It produces hCG, progesterone, estrogen, and hPL.
• It is not a site of red blood cell production.
• It offers limited protection against infections.
A nurse is measuring fundal height at 16 weeks gestation. What is the expected measurement?
Explanation
Fundal height measurement is a non-invasive clinical tool used to assess uterine growth and indirectly estimate fetal development. It is measured in centimeters from the pubic symphysis to the top of the uterine fundus. From weeks 18 to 32, the fundal height in centimeters typically equals the gestational age in weeks ±2 cm. Before 20 weeks, the uterus gradually rises through the abdomen. By 16 weeks, the fundus is typically located midway between the pubic symphysis and the umbilicus, and the expected measurement is approximately 14–18 cm.
Rationale for correct answers
B. At 16 weeks gestation, the uterus has ascended into the abdomen, and the expected fundal height is between 14 and 18 cm. This corresponds anatomically to a position halfway between the pubic symphysis and the umbilicus.
Rationale for incorrect answers
A. A fundal height of 8–10 cm is expected at approximately 12 weeks gestation, when the uterus is still just palpable above the pubic symphysis. At 16 weeks, this measurement would indicate uterine growth lag.
C. A measurement of 20–22 cm correlates with about 20–22 weeks gestation. At this point, the fundus is typically at the level of the umbilicus, not applicable to a 16-week pregnancy.
D. A fundal height of 24–26 cm is appropriate for 24–26 weeks gestation, when the fundus is well above the umbilicus. This would be significantly advanced for a 16-week pregnancy and may indicate incorrect dating or conditions like polyhydramnios.
Take home points
• Fundal height in cm generally matches gestational age in weeks between 18–32 weeks.
• At 16 weeks, fundal height should be 14–18 cm and located midway between symphysis and umbilicus.
• Lower-than-expected height may indicate fetal growth restriction or incorrect dating.
• Higher-than-expected height may suggest multiple gestation or polyhydramnios.
Which reflex becomes more coordinated in the fetus during weeks 17–20?
Explanation
Fetal reflex development follows a specific neurological sequence and reflects central nervous system maturation. Between weeks 17–20, the sucking reflex becomes increasingly coordinated as the brainstem and cranial nerves mature. This reflex involves cranial nerves V (trigeminal), VII (facial), IX (glossopharyngeal), X (vagus), and XII (hypoglossal) and is essential for postnatal feeding. Fetal swallowing of amniotic fluid, observed on ultrasound, reflects functional development of oromotor coordination. Although sucking may begin as early as week 14, it becomes coordinated and repetitive by weeks 17–20, laying the foundation for effective breastfeeding after birth.
Rationale for correct answers
B. The sucking reflex becomes more coordinated between weeks 17–20 as cranial nerves responsible for oral motor function mature. This coordination is critical for future feeding and is often visualized on ultrasound as fetal swallowing or thumb-sucking behavior.
Rationale for incorrect answers
A. The grasping reflex appears later, typically after week 26, and becomes more pronounced in the third trimester. It involves finger flexion in response to stimulation and is mediated by spinal and cortical circuits.
C. The stepping reflex does not develop in utero. It emerges postnatally, around birth to 6 weeks, as a primitive response when the soles touch a flat surface.
D. The rooting reflex, which helps infants locate a nipple by turning the head toward stimuli on the cheek, begins developing in the third trimester and is generally seen postnatally at full term, not coordinated at 17–20 weeks.
Take home points
• The sucking reflex becomes coordinated by 17–20 weeks gestation.
• It is essential for postnatal feeding and involves multiple cranial nerves.
• Grasping and rooting reflexes appear later in gestation or after birth.
• Reflex development reflects CNS and cranial nerve maturation.
What developmental milestone is typically reached around week 26, where the fetus can open its eyes?
Explanation
Fetal eyelid development follows a defined timeline that reflects neurological and anatomical maturation. The eyelids fuse by approximately week 10 to protect the developing eye and remain fused to allow for proper corneal and conjunctival differentiation. By around week 26, the eyelids separate, allowing the fetus to open and close the eyes in response to light and other stimuli. This milestone is associated with optic nerve myelination and increasing visual system activity, though vision remains immature. The retina is still developing, and light perception is limited. This separation coincides with increased blink-startle responses and maturation of REM-like eye movements.
Rationale for correct answers
B. Separation of the eyelids typically occurs by week 26, allowing the fetus to begin opening its eyes. This marks a significant milestone in fetal neurological and sensory development, including initiation of visual reflexes and responses to light.
Rationale for incorrect answers
A. Taste bud development begins much earlier, around weeks 7–8, and by week 14, taste receptors are already functional. While taste sensation continues to mature, this is not a unique milestone of week 26.
C. Formation of fingerprints (dermal ridges) is completed by weeks 17–19, during the second trimester. This unique feature arises due to genetic and intrauterine influences on skin patterning.
D. Complete lung maturation does not occur by week 26. Type II alveolar cells begin surfactant production around weeks 24–28, but full structural and functional lung maturity typically is not achieved until week 36–37.
Take home points
• Fetal eyelids fuse around week 10 and reopen by week 26.
• Eye opening indicates sensory and CNS maturation.
• Fingerprints form between weeks 17–19, earlier than eye opening.
• Lung maturation continues into late third trimester.
A nurse is performing Leopold’s maneuvers at 28 weeks gestation. What is the purpose of this assessment?
Explanation
Leopold’s maneuvers are a systematic four-step abdominal palpation technique used during the second and third trimesters to assess fetal position, lie, and presentation. These maneuvers help determine the fundal content, fetal back location, presenting part, and engagement in the maternal pelvis. Performed after week 24, they become more reliable as the uterus enlarges and fetal parts are more palpable. Knowing fetal position assists in evaluating labor progression and identifying malpresentation (e.g., breech, transverse). Normal fetal lie is longitudinal, and cephalic presentation is most common by term.
Rationale for correct answers
B. Leopold’s maneuvers assess fetal lie (longitudinal or transverse), presentation (cephalic or breech), and position (e.g., left occiput anterior) by palpating the uterus systematically. At 28 weeks, this helps anticipate delivery planning and detect malpresentation.
Rationale for incorrect answers
A. Amniotic fluid volume is assessed via ultrasound, not by Leopold’s maneuvers. The amniotic fluid index (AFI) is measured in centimeters, with normal range between 5–25 cm during the second and third trimesters.
C. Fetal heart rate is evaluated using Doppler ultrasound or fetoscope, not palpation. Leopold’s maneuvers may assist in locating the best site for auscultation but do not measure heart rate directly.
D. Placental location is assessed by ultrasound imaging, particularly via transabdominal or transvaginal scan, especially to rule out conditions like placenta previa. Palpation cannot reliably locate the placenta.
Take home points
• Leopold’s maneuvers are palpation techniques used to assess fetal lie and presentation.
• They are most reliable after 24–28 weeks gestation.
• Amniotic fluid volume and placental location require ultrasound.
• Fetal heart rate is assessed using Doppler or fetoscope, not palpation.
Which of the following are functions of the trophoblast cells in early pregnancy? Select all that apply.
Explanation
Trophoblast function is central to early pregnancy, beginning immediately after blastocyst implantation. These cells differentiate into cytotrophoblasts and syncytiotrophoblasts, which invade the endometrial lining, allowing for implantation and formation of the placenta. Syncytiotrophoblasts secrete human chorionic gonadotropin (hCG), which supports the corpus luteum to maintain progesterone levels until placental steroidogenesis is established. Trophoblasts are not involved in surfactant production or neural development. Normal hCG levels in early pregnancy double approximately every 48–72 hours and peak around 100,000 mIU/mL by 10 weeks gestation.
Rationale for correct answers
A. Trophoblasts, specifically syncytiotrophoblasts, secrete hCG starting at implantation. hCG maintains the corpus luteum during early pregnancy, which secretes progesterone to support the endometrium.
B. Trophoblast cells give rise to the placenta, forming both fetal components such as the chorionic villi and contributing to maternal-fetal interface development.
E. Trophoblasts penetrate the endometrial epithelium, enabling implantation of the blastocyst. This process involves enzymatic digestion of maternal tissue and establishment of early uteroplacental circulation.
Rationale for incorrect answers
C. Surfactant is produced by type II alveolar cells in the fetal lungs starting around weeks 24–28, not by trophoblasts. It reduces surface tension in alveoli to aid postnatal lung expansion.
D. Neural tube closure is a function of the ectoderm, occurring around days 21–28 post-fertilization. Trophoblasts are extraembryonic cells and do not contribute to neuroectodermal development.
Take home points
• Trophoblasts facilitate implantation by invading maternal endometrium.
• They secrete hCG to maintain the corpus luteum and progesterone production.
• Trophoblasts form the fetal component of the placenta.
• They are not involved in neural or pulmonary development.
Which of the following are risk factors for neural tube defects? Select all that apply.
Explanation
Neural tube defects (NTDs) are severe congenital malformations resulting from the incomplete closure of the neural tube during the third to fourth week of gestation, specifically between days 21–28. The most common forms include spina bifida, anencephaly, and encephalocele. NTDs are associated with several maternal and environmental risk factors. Folic acid deficiency impairs methylation and DNA synthesis, both critical for neural tube closure. Maternal diabetes, especially poorly controlled pregestational diabetes, increases oxidative stress and teratogenic risk. Anticonvulsant medications, such as valproic acid and carbamazepine, interfere with folate metabolism and increase NTD incidence. Normal folic acid supplementation is 400 mcg/day preconceptionally and in early pregnancy.
Rationale for correct answers
A. Maternal diabetes, particularly if poorly controlled, leads to increased oxidative stress and altered glucose metabolism, which disrupt early embryogenesis, including neural tube formation.
B. Folic acid deficiency is the most established risk factor for NTDs. Folate is vital for nucleotide synthesis and methylation. Low folate levels impair neural tube closure during early embryonic development.
D. Anticonvulsant medications, especially valproate and carbamazepine, are teratogenic due to their interference with folate metabolism, significantly increasing the risk for NTDs.
Rationale for incorrect answers
C. Excessive caffeine intake has not been definitively linked to neural tube defects. While high caffeine levels may be associated with other outcomes like miscarriage or low birth weight, they are not proven NTD risk factors.
E. Advanced maternal age increases the risk of chromosomal abnormalities such as trisomy 21, but it is not a direct risk factor for NTDs. NTD risk is more closely linked to nutritional and metabolic factors.
Take home points
• NTDs occur between days 21–28 of embryogenesis.
• Risk factors include folic acid deficiency, maternal diabetes, and certain anticonvulsants.
• Normal folic acid requirement is 400 mcg/day to prevent NTDs.
• Advanced age and caffeine are not primary contributors to NTDs.
Which of the following are signs of miscarriage in the first trimester? Select all that apply.
Explanation
Miscarriage (also called spontaneous abortion) is the loss of a pregnancy before 20 weeks of gestation, with most cases occurring in the first trimester (before 13 weeks). The most common cause is chromosomal abnormalities, followed by maternal conditions like thyroid disorders, infections, or uterine anomalies. Clinical signs include vaginal bleeding, abdominal cramping, and loss of pregnancy symptoms such as nausea and breast tenderness. Diagnosis is supported by ultrasound and quantitative hCG levels, which should double every 48–72 hours in a viable early pregnancy. A fetal heart rate is considered normal between 110–160 beats per minute.
Rationale for correct answers
A. Vaginal bleeding in the first trimester, especially when persistent or heavy, is a common sign of threatened or inevitable miscarriage. It may be accompanied by passage of clots or tissue.
B. Severe abdominal cramping or back pain is a hallmark of miscarriage due to uterine contractions and cervical dilation. It often intensifies as the pregnancy tissue is expelled.
D. Loss of pregnancy symptoms, such as resolution of nausea or breast soreness before the end of the first trimester, may indicate hormonal decline following embryonic demise.
Rationale for incorrect answers
C. Increased fundal height is not a sign of miscarriage. In fact, a decreasing or non-rising fundal height may be more indicative of pregnancy loss or intrauterine growth restriction.
E. A fetal heart rate of 140 beats per minute is within the normal range (110–160 bpm) and strongly indicates a viable pregnancy. Its presence rules out miscarriage at that moment.
Take home points
• First trimester miscarriage presents with bleeding, cramping, and loss of pregnancy symptoms.
• Chromosomal abnormalities are the most common cause.
• Normal fetal heart rate (110–160 bpm) rules out miscarriage.
• Miscarriage is confirmed by ultrasound and declining hCG levels.
Which of the following organ systems are developing during the embryonic period (weeks 3-8)? Select all that apply.
Explanation
Embryonic organogenesis occurs during weeks 3–8 of gestation, a period marked by rapid cellular differentiation, morphogenesis, and high vulnerability to teratogens. During this stage, the three germ layers—ectoderm, mesoderm, and endoderm—differentiate into major organ systems. The central nervous system forms from the ectoderm beginning with neural tube closure by day 28. The cardiovascular system is the first functional organ system, with the primitive heart beating by day 22. Limb buds appear by week 4, followed by elongation and digital separation. The digestive system originates from endoderm, with gut tube formation by week 4. The reproductive system, although genetically determined early, structurally differentiates later, during the fetal period.
Rationale for correct answers
A. The central nervous system begins developing early in the embryonic period. The neural plate forms in week 3, and the neural tube closes by week 4, initiating brain and spinal cord development.
B. The cardiovascular system starts forming in week 3. By day 22, the primitive heart tube begins beating and circulates blood, making it the earliest functioning organ system.
C. Limb buds become visible by week 4. By week 8, limb differentiation is advanced, including the formation of digits through programmed cell death (apoptosis) in the hand and foot plates.
D. The digestive system begins forming in week 4 from the endodermal germ layer. The primitive gut is divided into foregut, midgut, and hindgut, which later give rise to organs like the stomach, intestines, and liver.
Rationale for incorrect answers
E. The reproductive system, while genetically established at fertilization (XX or XY), begins structural differentiation later, primarily during the fetal period (after week 9). Gonadal development becomes histologically apparent between weeks 10–12.
Take home points
• Organogenesis occurs between weeks 3–8, known as the embryonic period.
• CNS, cardiovascular, digestive, and limb development all begin during this stage.
• The heart starts beating by day 22, making it the first functioning organ.
• Reproductive organs differentiate structurally later, during the fetal period.
Which of the following are important nursing considerations related to fetal development in the third trimester (weeks 28-40)? Select all that apply.
Explanation
Third trimester nursing care (weeks 28–40) centers on fetal maturation, maternal readiness for delivery, and monitoring for complications like preterm labor or infections. At this stage, the fetus undergoes rapid brain growth, lung surfactant production, and weight gain, reaching approximately 3,000–3,500 grams by term. Nurses must ensure Rho(D) immune globulin (RhoGAM) is administered at 28 weeks for Rh-negative mothers to prevent alloimmunization. Group B Streptococcus (GBS) screening is performed between 36–37 weeks. Preterm labor signs include uterine contractions, pelvic pressure, and cervical changes before 37 weeks. Fetal kick count education is essential, with fewer than 10 movements in 2 hours considered abnormal.
Rationale for correct answers
A. RhoGAM is administered at 28 weeks to Rh-negative mothers to prevent maternal antibody formation against Rh-positive fetal red blood cells, which can lead to hemolytic disease in future pregnancies.
B. Monitoring for preterm labor is critical during the third trimester. Early recognition of signs like uterine contractions every 10 minutes or cervical dilation enhances neonatal outcomes through timely interventions.
D. GBS screening is recommended at 36–37 weeks to identify maternal colonization. If positive, intrapartum antibiotics reduce the risk of neonatal GBS sepsis.
E. Educating mothers about fetal movement monitoring helps detect fetal distress. A common method is counting at least 10 movements in 2 hours; decreased movement may signal hypoxia.
Rationale for incorrect answers
C. Folic acid supplementation is essential preconceptionally and during the first trimester to prevent neural tube defects, which occur by day 28 of gestation. It is not a primary focus in the third trimester.
Take home points
• RhoGAM is given at 28 weeks to Rh-negative mothers to prevent alloimmunization.
• GBS screening occurs at 36–37 weeks to prevent neonatal infection.
• Preterm labor signs require immediate attention before 37 weeks.
• Kick counts help assess fetal well-being in late pregnancy.
Exams on Fetal Development
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
Upon completion of this comprehensive review, the nursing student will be able to:
• Articulate the intricate processes of human fertilization, implantation, and early embryonic development.
• Delineate the sequential developmental milestones of the fetus across all three trimesters of gestation.
• Identify critical physiological changes occurring within the developing fetus, encompassing organogenesis, growth, and maturation.
• Recognize the impact of various teratogens on fetal development during sensitive periods of gestation.
• Formulate evidence-based nursing interventions and patient education strategies pertinent to each trimester of pregnancy.
• Comprehend the significance of diagnostic assessments utilized throughout gestation to monitor fetal well-being and identify potential complications.
• Integrate knowledge of fetal development into holistic maternal-newborn nursing care, optimizing outcomes for both mother and neonate.
Introduction
The trajectory of human fetal development is a complex and exquisitely orchestrated biological process, commencing with the fusion of gametes and culminating in the birth of a neonate capable of extrauterine existence. This profound journey, spanning approximately 40 weeks of gestation, involves intricate cellular differentiation, tissue morphogenesis, and organ system maturation. A comprehensive understanding of these developmental phenomena is paramount for professional nursing practice within the maternal-newborn specialty. This document aims to provide an extensive, scientifically rigorous overview of fetal development, emphasizing key physiological milestones, potential vulnerabilities, and essential nursing considerations, thereby equipping nursing students with the requisite knowledge for exemplary patient care and academic success.
First Trimester: Weeks 1-13
The first trimester represents a period of rapid and profound developmental changes, laying the foundational structures for all subsequent growth and maturation.
1. Fertilization and Implantation
• Gamete Genesis and Transport:
➤ Spermatogenesis involves the continuous production of spermatozoa within the seminiferous tubules of the testes, a process typically lasting approximately 70 days. Mature spermatozoa possess a distinct morphology, including a head containing the haploid nucleus, a midpiece replete with mitochondria for ATP generation, and a flagellum for propulsive motility.
➤ Oogenesis, the developmental process of ova, initiates prenatally with primordial germ cells differentiating into oogonia. Meiosis I is arrested in prophase I until the onset of puberty. During each ovarian cycle, under hormonal influence, one primary oocyte completes meiosis I to yield a large secondary oocyte and a diminutive first polar body. Meiosis II is subsequently arrested in metaphase II, only completing upon successful fertilization.
➤ Ovulation typically occurs around day 14 of a standardized 28-day menstrual cycle, wherein the mature secondary oocyte is expelled from the ruptured graafian follicle and expeditiously captured by the fimbriae of the fallopian tube.
➤ Spermatozoa, deposited in the posterior vaginal fornix during coitus, undertake a formidable journey through the cervical canal, across the endometrial cavity, and into the fallopian tubes. Spermatozoal viability within the female reproductive tract can persist for up to 72 hours, although their fertilizing capacity significantly diminishes beyond 24 hours. Conversely, the ovum maintains its fertilizable capacity for a more limited window of approximately 12-24 hours post-ovulation.
• Fertilization:
➤ Fertilization, defined as the intricate fusion of a single spermatozoon with a secondary oocyte, most commonly transpires within the ampulla of the fallopian tube.
➤ Capacitation: This is a crucial physiological conditioning process that spermatozoa undergo within the female reproductive tract, culminating in enhanced motility and preparing them for the subsequent acrosomal reaction. It entails the enzymatic removal of a glycoprotein coat and seminal plasma proteins from the acrosomal region of the sperm head.
➤ Acrosomal Reaction: Upon encountering the corona radiata and the underlying zona pellucida, the glycoprotein layer surrounding the ovum, the capacitated sperm's acrosome releases an array of hydrolytic enzymes, notably hyaluronidase and acrosin. These enzymes facilitate the localized degradation of the extracellular matrix, enabling sperm penetration through these protective layers.
➤ Sperm Penetration: A singular spermatozoon successfully traverses the zona pellucida and subsequently fuses with the oocyte's plasma membrane.
➤ Cortical Reaction: The binding and entry of the first spermatozoon into the oocyte cytoplasm instantaneously trigger the cortical reaction. This exocytotic event involves the release of specialized cortical granules from the oocyte's periphery into the perivitelline space. The contents of these granules induce biochemical alterations in the zona pellucida, rendering it impermeable to subsequent spermatozoa and thereby critically preventing polyspermy (fertilization by multiple sperm, which would result in a non-viable triploid zygote).
➤ Completion of Meiosis II: The influx of calcium ions following sperm penetration stimulates the secondary oocyte to promptly complete its second meiotic division. This results in the formation of a mature ovum (ootid), containing the female pronucleus, and the extrusion of a second polar body.
➤ Pronuclei Formation and Fusion: The haploid nucleus of the fertilizing spermatozoon decondenses to form the male pronucleus, while the newly formed ovum's nucleus becomes the female pronucleus. These two pronuclei replicate their DNA and subsequently fuse, establishing a single diploid nucleus. The resultant unicellular entity, now possessing a full complement of 46 chromosomes (23 from each gamete), is designated a zygote.
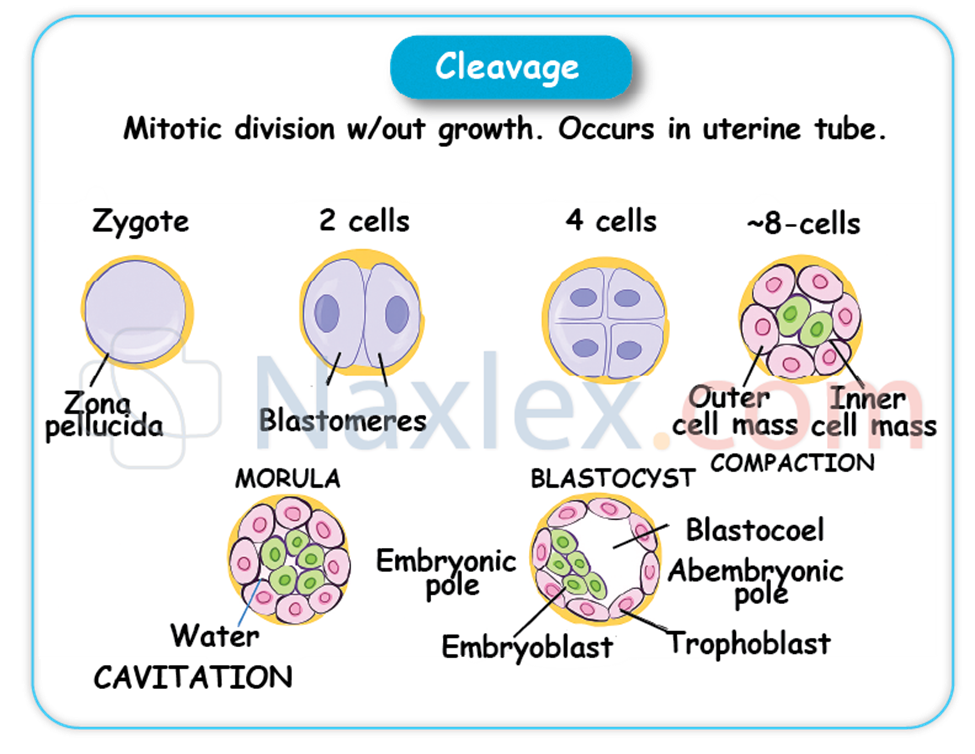
• Cleavage and Morula Formation:
➤ Following fertilization, the zygote commences a series of rapid mitotic divisions, collectively termed cleavage, as it embarks on its journey down the fallopian tube towards the uterine cavity.
➤ These divisions are characterized by an increase in cell number (blastomeres) without a concomitant increase in the overall size of the conceptus.
➤ By approximately 3-4 days post-fertilization, the cleaving zygote typically comprises 12-32 blastomeres, forming a compact, solid ball resembling a mulberry, which is termed the morula.
• Blastocyst Formation:
➤ As the morula enters the uterine cavity, fluid from the uterine glands begins to permeate its intercellular spaces, coalescing to form a progressively expanding fluid-filled cavity known as the blastocoel (or blastocyst cavity).
➤ This cavitation process transforms the morula into a blastocyst, a developmental stage typically achieved by day 4-5 post-fertilization.
➤ The blastocyst differentiates into two primary, functionally distinct cell populations:
◆ Trophoblast: This is the outer epithelial layer of cells that will predominantly contribute to the formation of the embryonic portion of the placenta. Trophoblast cells are pivotal in mediating the intricate processes of implantation and subsequent nutrient and gas exchange between the maternal and fetal circulations.
◆ Inner Cell Mass (Embryoblast): This is an eccentrically positioned cluster of pluripotent cells located within the blastocoel. The embryoblast is destined to develop into the embryo proper and several extraembryonic membranes.
• Implantation:
➤ Implantation, the critical process by which the blastocyst firmly embeds itself into the prepared endometrial lining (now termed the decidua due to its gestational modifications), typically occurs approximately 6-10 days after fertilization. The most common site for implantation is the posterior superior wall of the uterine fundus.
➤ The trophoblast cells, particularly the syncytiotrophoblast, secrete proteolytic enzymes that enzymatically erode the compact layer of the decidua, facilitating the invasive embedding of the blastocyst.
➤ Human Chorionic Gonadotropin (hCG): Crucially, the syncytiotrophoblast cells commence the secretion of human chorionic gonadotropin (hCG) shortly after implantation. This glycoprotein hormone is indispensable for rescuing and maintaining the corpus luteum in the ovary. The corpus luteum, under the sustained stimulation of hCG, continues to produce vital progesterone, which is essential for sustaining the integrity of the endometrial lining and inhibiting the onset of menstruation. This hormonal support is critical for the early maintenance of pregnancy. The detection of elevated hCG levels in maternal serum or urine forms the biochemical basis for current pregnancy tests.
Nursing Insights:
• Practical Application: Patient Education on Conception: A comprehensive understanding of the precise timing of ovulation and the lifespan of spermatozoa and ova is fundamental for nurses when providing patient education regarding optimizing conception efforts or implementing natural family planning methods. For instance, advising couples to engage in coitus around the estimated time of ovulation, considering sperm viability, can significantly increase the likelihood of fertilization.
• Practical Application: Preventing Polyspermy: The cortical reaction is a highly specialized biological mechanism. Nurses should appreciate that while not directly intervened upon in clinical practice, its failure could lead to non-viable pregnancies, reinforcing the precision of early human development.
• Practical Application: Confirming Pregnancy and Early Management: The detection of hCG through qualitative or quantitative assays serves as the earliest biochemical confirmation of pregnancy. Nurses utilize this principle daily, interpreting positive home pregnancy tests and ordering serum quantitative hCG levels to monitor early pregnancy progression or evaluate potential complications such as ectopic pregnancy or miscarriage. Serial hCG levels are often monitored to assess the viability and progression of the early gestation.
2. Embryonic Period (Weeks 3-8)
This period is characterized by unparalleled cellular proliferation, intricate differentiation, and complex morphogenesis, culminating in the establishment of all major organ systems. Consequently, it represents the most sensitive and critical window of vulnerability to teratogenic insults.
• Development of the Bilaminar Disc (Week 2):
➤ During the second week of development, the embryoblast undergoes further differentiation, forming two distinct, apposed germ layers, giving rise to the bilaminar embryonic disc:
◆ Epiblast: This dorsal, columnar cell layer is directly adjacent to the developing amniotic cavity and will serve as the progenitor for the three primary germ layers during gastrulation.
◆ Hypoblast: This ventral, cuboidal cell layer is adjacent to the primary yolk sac.
➤ Concurrently, the amniotic cavity expands within the epiblast, providing a protective fluid-filled environment for the developing embryo.
• Gastrulation and Formation of the Trilaminar Embryonic Disc (Week 3):
➤ Gastrulation is a profoundly significant developmental event occurring during the third week, involving extensive cell migration, rearrangement, and differentiation. During this process, the epiblast cells migrate through the primitive streak to form three distinct primary germ layers, establishing the trilaminar embryonic disc:
◆ Ectoderm: This outermost germ layer differentiates to form the central nervous system (including the brain, spinal cord, and cranial nerves), the epidermis and its appendages (skin, hair, nails, sweat glands), mammary glands, the anterior pituitary gland, the enamel of teeth, and the sensory epithelia of the eyes, ears, and nose.
◆ Mesoderm: This middle germ layer is highly diverse, giving rise to the entire musculoskeletal system (muscles, bones, cartilage, connective tissues), the cardiovascular system (heart, blood vessels, blood cells, lymphatic vessels), the urogenital system (kidneys, gonads, reproductive ducts), the spleen, the adrenal cortex, and the dermis of the skin.
◆ Endoderm: This innermost germ layer forms the epithelial lining of the entire gastrointestinal tract (from pharynx to anus), the epithelial lining of the respiratory system (trachea, bronchi, lungs), the parenchyma of associated glands such as the liver and pancreas, the thyroid and parathyroid glands, and the thymus.
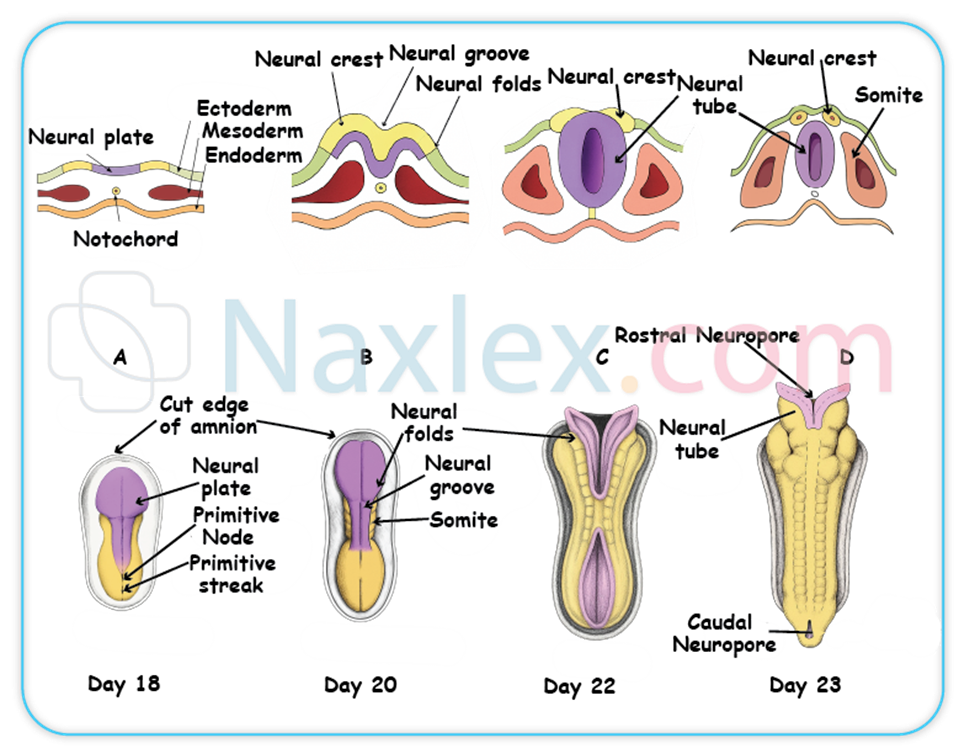
• Neurulation (Weeks 3-4):
➤ Neurulation is the process by which the neural plate forms, folds, and fuses to create the neural tube. This critical process commences during the third week and completes by the end of the fourth week.
➤ The ectoderm overlying the notochord (a transient, mesoderm-derived rod-like structure that serves as a primary inducer) thickens to form the neural plate.
➤ The neural plate then invaginates centrally, forming the neural groove, flanked by neural folds.
➤ The neural folds subsequently elevate and fuse dorsally, effectively closing off to form the neural tube.
➤ The neural tube is the primordium of the entire brain and spinal cord.
➤ Neural tube defects (NTDs), such as spina bifida (incomplete closure of the caudal neural tube) and anencephaly (incomplete closure of the cranial neural tube, resulting in absence of major parts of the brain and skull), arise from incomplete fusion of the neural tube. Folic acid supplementation (specifically 400 mcg daily for all women of childbearing age, and 4 mg daily for those with a prior history of NTD-affected pregnancy) is unequivocally critical for the primary prevention of NTDs.
• Cardiovascular Development (Weeks 3-8):
➤ The primitive heart tube begins to form from cardiogenic mesoderm during the third week and initiates rudimentary circulation by the end of week 3 or early week 4, making the cardiovascular system the first major organ system to become functionally active.
➤ By week 5, the tubular heart has folded and begins to beat rhythmically, propelling blood through the embryonic circulation.
➤ By week 6, fetal cardiac activity is typically definitively detectable via transvaginal ultrasound, providing objective evidence of embryonic viability.
➤ During this period, the heart undergoes septation to form the four distinct chambers, and major blood vessels (e.g., aorta, pulmonary artery) develop.

• Other Organogenesis:
➤ Limb Buds: Upper limb buds emerge at the end of week 4, followed closely by the appearance of lower limb buds during week 5. These buds elongate and flatten to form paddle-like structures.
➤ Eye and Ear Placodes: Early developmental precursors of the sensory organs, specifically the optic placodes (future eyes) and otic placodes (future ears), become discernible.
➤ Gastrointestinal Tract: The primitive gut tube differentiates into foregut, midgut, and hindgut. Liver and pancreatic buds, crucial for digestive and metabolic functions, emerge from the endoderm.
➤ Respiratory System: The laryngotracheal groove forms, and lung buds emerge from the foregut, initiating the development of the bronchial tree.
➤ Kidney Development: A sequence of kidney precursors appears: the pronephros (transient), followed by the mesonephros, before the definitive kidney, the metanephros, begins its formation.

Nursing Insights:
• Practical Application: Teratogen Counseling: The embryonic period (weeks 3-8) is the most vulnerable to teratogens due to the simultaneous rapid organogenesis of all major body systems. Nurses must provide rigorous and comprehensive patient education regarding the avoidance of known teratogens, including alcohol, illicit drugs, certain prescription and over-the-counter medications (e.g., isotretinoin, thalidomide), excessive radiation exposure, and specific infectious agents (e.g., rubella, cytomegalovirus). For example, a pregnant patient presenting for their first prenatal visit at 7 weeks gestation needs explicit counseling on discontinuing alcohol consumption immediately due to the risk of Fetal Alcohol Spectrum Disorders.
• Practical Application: Folic Acid Adherence: Nurses must vehemently emphasize the critical role of folic acid supplementation in the periconceptional period to prevent neural tube defects. This involves counseling all women of childbearing potential, not just those planning pregnancy, on daily supplementation, as neural tube closure occurs very early in gestation, often before pregnancy is even recognized. Documenting patient adherence to folic acid supplementation is a vital nursing responsibility.
• Practical Application: Early Pregnancy Viability Assessment: The visualization of fetal cardiac activity via transvaginal ultrasound as early as 6 weeks gestation is a pivotal finding for confirming pregnancy viability and providing significant reassurance to expectant parents. Nurses preparing patients for such scans should explain what to expect and be prepared to address the emotional responses to this early visualization of life.
3. Fetal Period (Weeks 9-13)
By the commencement of the fetal period at week 9, all major organ systems have been established in rudimentary form. This subsequent period is predominantly characterized by exponential growth, accelerated maturation, and functional refinement of these existing structures.
• Differentiation and Growth:
➤ From week 9 onward, the developing organism is unequivocally referred to as a fetus.
➤ This period witnesses a rapid linear increase in crown-rump length and a substantial gain in overall body mass. By the completion of week 12, the fetus typically measures approximately 6-7 cm in crown-rump length and possesses a body mass of around 14 grams.
➤ During these early fetal weeks, the head remains disproportionately large in relation to the developing trunk and limbs, reflecting the accelerated growth and differentiation of the brain.
• Organ System Maturation:
➤ Cardiovascular System: The four-chambered heart is fully formed, and cardiac septation is complete. The unique fetal circulatory patterns, incorporating critical shunts such as the ductus arteriosus (connecting the pulmonary artery to the aorta), foramen ovale (an opening between the right and left atria), and ductus venosus (bypassing the liver), are well-established to optimize oxygen delivery in the intrauterine environment.
➤ Renal System: The metanephros, the definitive kidney, becomes functional and commences urine production. This fetal urine is subsequently excreted into the amniotic fluid, playing a vital role in contributing to and maintaining its volume. By week 12, the kidneys are demonstrable as functionally active.
➤ Gastrointestinal System: The intestines, which undergo a transient physiological herniation into the umbilical cord during the embryonic period, complete their retraction into the abdominal cavity by approximately week 10. The liver, a significant hematopoietic organ at this stage, begins to produce bile.
➤ External Genitalia: Gross differentiation of the external genitalia progresses sufficiently to allow for the reliable determination of fetal sex via ultrasound examination by week 12-14.
➤ Musculoskeletal System: The limbs are well-formed with identifiable digits (fingers and toes). While fetal movements are present and discernible on ultrasound, they are generally not yet strong enough to be perceived by the expectant mother.
➤ Endocrine System: The thyroid gland initiates the production of thyroid hormones, crucial for fetal growth and neurological development. The pancreas begins to synthesize insulin.
➤ Hematopoietic System: The primary site of erythropoiesis (red blood cell production) transitions from the yolk sac to the developing liver, signifying the increasing sophistication of fetal organ function.
Nursing Insights:
• Practical Application: Transition from Embryo to Fetus: Nurses should effectively communicate to parents that the transition from "embryo" to "fetus" at week 9 signifies the completion of major organ formation. This typically corresponds to a decreased, though not absent, susceptibility to gross congenital anomalies, shifting the developmental focus towards growth and functional maturation.
• Practical Application: Fetal Kidney Function and Amniotic Fluid: The understanding that fetal urine production is the primary contributor to amniotic fluid volume after the first trimester is critical. Nurses should recognize that oligohydramnios (abnormally low amniotic fluid) can be an indicator of underlying fetal renal dysfunction or urinary tract obstruction. Conversely, polyhydramnios (excessive amniotic fluid) may suggest impaired fetal swallowing or other anomalies.
• Practical Application: Sex Determination and Communication: While sex determination by ultrasound at 12-14 weeks can be an exciting milestone for expectant parents, nurses must approach this topic with sensitivity. Some parents may prefer not to know, or the visualization may be challenging, requiring careful communication to manage expectations and provide accurate information.
Second Trimester: Weeks 14-27
The second trimester is frequently referred to as the "golden trimester" in maternal health, attributable to a notable reduction in the common discomforts of early pregnancy for the expectant mother and a period characterized by substantial fetal growth and intricate refinement of developing organ systems.
1. Continued Growth and Maturation
• Growth and Proportions:
➤ This trimester is marked by a prodigious increase in fetal length and overall body mass. By the cessation of week 27, the fetus typically attains a crown-heel length of approximately 37 cm and weighs around 1000 grams (1 kg), reflecting exponential growth.
➤ Fetal body proportions gradually normalize; while cephalic growth continues, the accelerated development of the trunk and limbs leads to a more proportionate and recognizable human form.
➤ Fundal Height Measurement: The uterine fundal height, meticulously measured in centimeters from the symphysis pubis to the superior aspect of the uterine fundus, generally correlates precisely with the gestational age in weeks after the 20th week of gestation (e.g., 20 cm at 20 weeks). At 16 weeks gestation, the anticipated fundal height measurement is approximately 14-18 cm. This clinical assessment provides a rapid, non-invasive estimation of fetal growth and gestational age.
• Integumentary System:
➤ Lanugo: A fine, soft, downy hair, known as lanugo, begins to uniformly cover the fetal body. This serves as a primary insulating layer, aiding in thermoregulation within the aqueous amniotic environment.

➤ Vernix Caseosa: A unctuous, white, and protective substance, comprised of desquamated epithelial cells and sebaceous gland secretions, commences its formation and uniformly coats the fetal skin around week 19-20. The vernix caseosa acts as a crucial barrier, safeguarding the delicate fetal skin from chronic maceration and desiccation by the amniotic fluid, and also contributes to postnatal thermoregulation.

➤ Subcutaneous fat deposition initiates during this period, contributing to a more rounded and less translucent appearance of the fetal integument.
• Musculoskeletal System:
➤ The process of ossification and subsequent hardening of the fetal skeleton continues progressively.
➤ Fetal musculature gains strength and tone, leading to increasingly coordinated and purposeful movements.
➤ Quickening: The maternal perception of initial fetal movements, termed quickening, typically occurs around weeks 16-20 for primigravida mothers (those experiencing their first pregnancy). Multigravida mothers, having prior experience, often perceive quickening earlier due to heightened awareness of sensations. This is a profound and emotionally significant milestone for expectant parents.
• Sensory Development:
➤ The eyes are structurally well-developed, and the eyelids typically remain fused shut until approximately 26 weeks of gestation, after which they separate and can open.
➤ The auditory system continues its intricate maturation, enabling the fetus to respond to external sound stimuli.
➤ Taste buds are actively differentiating and maturing on the fetal tongue.
• Respiratory System:
➤ The pulmonary system undergoes continued branching of bronchioles and proliferation of alveolar ducts.
➤ Surfactant Production: Type II pneumocytes, specialized alveolar cells within the fetal lungs, initiate the production of surfactant (a complex lipoprotein that functions to reduce surface tension at the air-liquid interface within the alveoli, preventing alveolar collapse during expiration) around week 24. Although present, surfactant levels at this stage are not yet sufficient to support independent, sustained extrauterine respiration. Adequate surfactant is paramount for successful lung expansion and gas exchange post-birth.
• Hematopoietic System:
➤ The primary site of red blood cell production undergoes a significant physiological shift from the liver to the developing bone marrow.
Nursing Insights:
• Practical Application: Fetal Movement Education: Nurses must comprehensively educate expectant mothers on the significance of quickening and, subsequently, the importance of daily fetal movement counts (kick counts) as a simple yet effective non-invasive method for assessing fetal well-being. A reduction in perceived movements warrants immediate evaluation. For example, instruct a patient to lie on their side and count movements for an hour; if fewer than 10 distinct movements are felt, advise them to consume a sugary beverage and re-count, contacting their provider if still fewer than 10 movements occur within two hours.
• Practical Application: Explaining Fetal Skin Coverings: When parents inquire about the appearance of their newborn, nurses should explain the physiological roles of lanugo and vernix caseosa. This can alleviate potential concerns regarding their presence at birth, emphasizing their protective functions in utero rather than indicating an abnormality.
• Practical Application: Pulmonary Maturity and Preterm Birth: The knowledge of surfactant production onset around 24 weeks is crucial for understanding fetal viability at earlier gestational ages. Nurses caring for patients at risk of preterm labor will anticipate and administer antenatal corticosteroids (e.g., betamethasone) to accelerate fetal lung maturity, demonstrating a direct correlation between scientific understanding and clinical intervention.
2. Fetal Milestones
• Week 14: The fetus demonstrates active, coordinated movements, including suck and swallow movements, indicative of advancing neurological maturation.
• Week 16: Fetal sex is typically reliably determinable via high-resolution ultrasound. The external genitalia are visually distinct. The uterine fundus is palpable approximately midway between the symphysis pubis and the umbilicus.
• Week 18: Fetal heart tones are typically audible with a traditional fetoscope, providing an audibly reassuring sign of fetal viability.
• Week 20: Quickening is almost universally perceived by primigravida mothers. Both lanugo and vernix caseosa become evident. The fetus measures approximately 25 cm in crown-heel length.
• Week 24: The pulmonary system achieves a critical milestone with the initiation of significant surfactant production. At this gestational age, the fetus is considered to reach the threshold of viability, meaning it possesses a reasonable chance of survival outside the uterus with advanced intensive medical support.
• Week 26: The fetal eyelids separate, allowing the eyes to open and close. Distinct fetal sleep-wake cycles emerge, reflecting neurological maturation. The fetus demonstrates responsiveness to auditory stimuli.
• Diagnostic Tests:
➤ Ultrasound (Mid-Pregnancy Anomaly Scan, typically 18-22 weeks): This is a comprehensive, detailed anatomical assessment to meticulously evaluate fetal structures for congenital anomalies, ascertain precise fetal growth parameters, confirm placental location, and measure amniotic fluid volume. This ultrasound is paramount for early detection of potential structural abnormalities.
➤ Amniocentesis: This invasive diagnostic procedure may be performed between weeks 15-20 to obtain amniotic fluid for genetic analysis. It is indicated for the diagnosis of chromosomal abnormalities (e.g., Down syndrome), specific genetic disorders, or neural tube defects, particularly in high-risk pregnancies (e.g., advanced maternal age, abnormal genetic screening results, family history of genetic conditions).
➤ Maternal Serum Alpha-Fetoprotein (MSAFP) Screening (15-20 weeks): This maternal blood test is a screening tool used to assess the risk for neural tube defects (elevated MSAFP) and certain chromosomal abnormalities, notably Down syndrome (decreased MSAFP in conjunction with other markers in a quad screen). It is a screening, not diagnostic, test.
Nursing Insights:
• Practical Application: Explaining Diagnostic Test Results: Nurses are often the primary point of contact for patients receiving results from diagnostic tests like the mid-pregnancy ultrasound, amniocentesis, and MSAFP screening. It is imperative to provide accurate, empathetic explanations of the findings, implications, and subsequent management plans. For example, if an MSAFP is elevated, explain it is a screening test and does not mean the fetus definitely has an NTD, but warrants further diagnostic testing such as a targeted ultrasound.
• Practical Application: Counseling on Viability: While acknowledging fetal viability around 24 weeks is important, nurses must also provide realistic counseling regarding the prognosis for survival and the potential for long-term morbidity in extremely preterm infants. Emphasize that while medical advancements improve outcomes, the highest likelihood of healthy survival is achieved with advancing gestational age.
• Practical Application: Promoting Prenatal Care Adherence: Regularly scheduled second-trimester prenatal visits are crucial for monitoring maternal and fetal well-being. Nurses reinforce the importance of these visits, which include fundal height measurements, fetal heart tone auscultation, and preparation for the mid-pregnancy ultrasound, ensuring comprehensive care.
Third Trimester: Weeks 28-40+
The third trimester represents the culminating phase of intrauterine development, characterized by intensive fetal growth, substantial weight accrual, and the final functional maturation of all organ systems, meticulously preparing the fetus for the physiological demands of extrauterine existence.
1 Advanced Fetal Maturation
• Weight Gain and Fat Accumulation:
➤ The fetus experiences a pronounced growth spurt during the third trimester, gaining approximately half of its total birth weight during the last 8-10 weeks of gestation.
➤ There is a significant and progressive deposition of subcutaneous adipose tissue (fat), which serves as a crucial insulating layer for thermoregulation post-birth and provides vital energy reserves for neonatal adaptation.
➤ By week 26, the approximate fetal weight ranges from 600-800 grams. By the completion of gestation at term (week 40), the average fetal weight is typically within the range of 2.5-4 kg.
• Respiratory System Maturation:
➤ The pulmonary system continues its intricate maturation, involving the development of more complex alveolar sacs and a sustained increase in the production of surfactant.
➤ Surfactant production reaches levels considered sufficient to support independent and effective extrauterine lung function in the majority of fetuses around week 34-36. This critical protein-lipid complex lowers surface tension within the alveoli, preventing their collapse upon exhalation and ensuring adequate gas exchange.
➤ Fetal breathing movements (FBMs) become more regular and vigorous, playing a crucial role in the development and conditioning of the pulmonary musculature and fluid clearance from the airways.
• Nervous System Development:
➤ This trimester is marked by exponential brain growth and development, including continued gyration and sulcation, which increase the cortical surface area.
➤ The process of myelination of nerve fibers progresses rapidly, particularly in the central nervous system, enhancing the speed and efficiency of neural impulse transmission, thereby improving coordination and reflex integration.
➤ The central nervous system assumes greater control over vital physiological functions, including thermoregulation and respiratory drive.
➤ Coordinated reflexes, such as the sucking reflex, become more refined around weeks 32-34, essential for successful oral feeding after birth.
• Immunological Development:
➤ Passive Immunity: A critical protective mechanism is established through the active transfer of maternal immunoglobulin G (IgG) antibodies across the placenta to the fetus. This transfer predominantly occurs during the third trimester, commencing significantly around week 33. These maternal antibodies confer passive immunity to the neonate, providing temporary protection against common bacterial and viral infections to which the mother has developed immunity, safeguarding the infant during the initial vulnerable months of extrauterine life.
• Gastrointestinal System:
➤ Fetal digestive enzymes are present and functional.
➤ Meconium, the first intestinal discharge of the neonate, accumulates within the fetal intestines. This sterile, greenish-black, viscous substance is composed of shed epithelial cells, lanugo, intestinal secretions, and bile pigments.
• Renal System:
➤ The fetal kidneys are fully functional and play a substantial role in maintaining the appropriate volume of amniotic fluid through continuous urine production and excretion.
• Sensory Organs:
➤ The pupillary light reflex is established.
➤ The auditory system is fully developed, enabling the fetus to consistently react to external auditory stimuli, including maternal voice and environmental sounds.
Nursing Insights:
• Practical Application: Fetal Movement Monitoring (Kick Counts): Nurses must diligently educate expectant mothers on the consistent monitoring of fetal movements (often referred to as "kick counts") as a simple, non-invasive, and effective daily assessment of fetal well-being, particularly in the third trimester. A significant decrease or cessation of fetal movements necessitates immediate medical evaluation. Instructing the patient to choose a consistent time each day, lie on her side, and count distinct movements (e.g., report if fewer than 10 movements occur within 2 hours) is a standard protocol.
• Practical Application: Antenatal Corticosteroid Administration: When managing a patient at risk for preterm labor, nurses understand the critical importance of administering betamethasone (or dexamethasone). This corticosteroid medication, given intramuscularly to the mother, accelerates fetal lung maturity by stimulating surfactant production, significantly reducing the incidence and severity of respiratory distress syndrome in preterm neonates. Nurses monitor for potential side effects and ensure timely administration within the therapeutic window.
• Practical Application: Explaining Neonatal Immunity: Nurses should counsel parents about the concept of passive immunity acquired from the mother, explaining that it provides temporary protection. This knowledge helps parents understand why routine childhood immunizations are crucial even if the baby received maternal antibodies, as these antibodies gradually wane.
2 Preparation for Birth
• Fetal Position and Presentation:
➤ As the fetus rapidly grows and occupies an increasing proportion of the intrauterine space, it typically assumes a characteristic position within the uterus.
➤ The most common and physiologically advantageous fetal position for vaginal birth is vertex (cephalic) presentation, where the fetal head is positioned inferiorly, towards the maternal pelvis.
➤ Lightening: This maternal sensation, often described as the fetus "dropping," occurs when the fetal head descends and engages into the maternal pelvis. This typically transpires a few weeks prior to term in primigravida individuals and often closer to the actual onset of labor in multigravida individuals. Physiologically, lightening can alleviate maternal dyspnea by reducing pressure on the diaphragm, but it concurrently increases pressure on the bladder, leading to more frequent urination.
• Amniotic Fluid Volume:
➤ The volume of amniotic fluid generally peaks around week 32-36 of gestation, subsequently undergoing a gradual physiological decrease as term approaches.
➤ Deviations from normal amniotic fluid volume, specifically oligohydramnios (abnormally low amniotic fluid, often associated with uteroplacental insufficiency or fetal renal anomalies) or polyhydramnios (excessive amniotic fluid, potentially indicative of fetal gastrointestinal anomalies or gestational diabetes), can serve as significant indicators of underlying fetal or maternal complications, necessitating further diagnostic evaluation and management.
• Placental Maturation and Aging:
➤ While the placenta continues to grow throughout gestation, it exhibits physiological signs of aging as term approaches and especially beyond term. These changes include calcifications and decreased vascularity, which can lead to diminished efficiency in nutrient and gas exchange. This phenomenon is termed placental insufficiency, and it can compromise fetal well-being in post-term pregnancies.
• Maternal Assessment for Fetal Well-being:
➤ Leopold's Maneuvers: This systematic series of four abdominal palpation techniques is a fundamental nursing skill performed typically after 28 weeks of gestation. Leopold's maneuvers enable the clinician to accurately determine fetal presentation (e.g., vertex, breech), fetal position (e.g., left occiput anterior), the fetal lie (longitudinal, transverse, oblique), and provide an estimation of fetal weight. This assessment is critical for planning labor management.
➤ Non-Stress Test (NST): The NST is a non-invasive antepartum fetal surveillance test performed to assess fetal well-being. It involves monitoring the fetal heart rate (FHR) response to spontaneous fetal movements. A reactive NST, characterized by two or more FHR accelerations (defined as an increase of at least 15 beats per minute above baseline, lasting at least 15 seconds) within a 20-minute period, indicates adequate fetal oxygenation and an intact autonomic nervous system.
➤ Biophysical Profile (BPP): The BPP is a comprehensive, non-invasive assessment tool that combines the Non-Stress Test with real-time ultrasonography. It evaluates five parameters: fetal breathing movements, gross body movements, fetal tone, amniotic fluid volume, and the reactive NST. Each parameter is scored 0 or 2, with a maximum score of 10. A score of 8-10 is generally considered reassuring for fetal well-being.
• Signs of Labor:
➤ Nurses are instrumental in educating patients on the crucial differentiation between true labor (characterized by regular, progressively stronger, and longer uterine contractions leading to cervical effacement and dilation) and false labor (Braxton Hicks contractions, which are irregular, do not increase in intensity, and resolve with rest or position change).
➤ Other important pre-labor and early labor signs include progressive cervical ripening, passage of the "bloody show" (mucus plug mixed with blood), and rupture of membranes (spontaneous amniotomy).
Nursing Insights:
• Practical Application: Mastering Leopold's Maneuvers: Nurses must develop proficiency in performing Leopold's maneuvers, as this skill directly impacts labor and delivery care. For instance, identifying a breech presentation necessitates preparing for potential external cephalic version or planned cesarean delivery, whereas a vertex presentation guides the expectation of a vaginal birth. Practicing this palpation technique on multiple patients enhances accuracy.
• Practical Application: Preterm Labor Recognition and Response: Nurses provide explicit instructions to patients on recognizing the subtle and overt signs and symptoms of preterm labor (e.g., regular uterine contractions, pelvic pressure, low backache, increased vaginal discharge, vaginal spotting) and emphasizing the critical importance of prompt medical evaluation should these symptoms arise. Early recognition and intervention can significantly impact neonatal outcomes.
• Practical Application: Explaining Antenatal Surveillance: When fetal surveillance tests such as NSTs and BPPs are ordered, nurses are responsible for thoroughly explaining the purpose, procedure, and interpretation of these tests to expectant parents. For example, explain that a non-reactive NST does not necessarily mean distress but requires further evaluation, often with a BPP or contraction stress test, to gain more comprehensive insight into fetal status. This transparency alleviates anxiety and promotes informed decision-making.
Summary
The remarkable journey of fetal development, commencing from a singular zygote and culminating in a highly complex human neonate prepared for independent extrauterine existence, is a testament to extraordinarily intricate biological programming. The first trimester, encompassing the pivotal events of fertilization, implantation, and the critical embryonic period (weeks 3-8), is characterized by profoundly rapid cellular division and the foundational establishment of all major organ systems. This embryonic phase is unequivocally the most susceptible window for teratogenic insults, necessitating rigorous patient education on avoidance. The second trimester (weeks 14-27) transitions into a period of substantial fetal growth, intricate refinement of organ systems, and the emotionally significant maternal perception of fetal movements. Finally, the third trimester (weeks 28-40+) is defined by exponential fetal weight gain, the critical final maturation of the pulmonary and neurological systems, and a comprehensive physiological preparation for the demands of birth and subsequent extrauterine life. Throughout these gestational trimesters, a series of critical physiological milestones—including the development of a beating heart, functional kidneys, and adequate surfactant production—are essential for the eventual success of independent survival. Nursing care across the entire gestational continuum necessitates a comprehensive understanding of these developmental stages, emphasizing proactive health promotion, meticulous risk reduction strategies, precise patient education, and the skillful application and interpretation of various diagnostic assessments. This holistic approach ensures optimal maternal and fetal outcomes, embodying competent and compassionate maternal-newborn nursing practice.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Fetal Development
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


