Please set your exam date
Infertility
Study Questions
Practice Exercise 1
Which hormone is primarily responsible for stimulating follicular development in the female reproductive system?
Explanation
Follicular developmentis regulated by a delicate interplay of gonadotropins, hormones, and ovarian feedbackmechanisms. The anterior pituitary releases follicle-stimulating hormone (FSH)and luteinizing hormone (LH)under the control of gonadotropin-releasing hormone (GnRH)from the hypothalamus. FSH stimulates growth of ovarian follicles, essential for estrogenproduction and ovulation. Estradiol levels normally range from 30–400 pg/mL across the menstrual cycle, while FSH typically ranges from 4.7–21.5 mIU/mL depending on cycle phase. LH spikes mid-cycle to induce ovulation. Follicular development begins in the early follicular phase and is critical for menstrual regulation and fertility.
Rationale for correct answers
B.FSH is secreted by the anterior pituitary and directly stimulates growth and maturation of ovarian follicles. It acts on granulosa cells, promoting estrogen synthesis and follicular expansion during the early follicular phase of the menstrual cycle. Rising estrogen levels then provide feedback for LH surge and ovulation.
Rationale for incorrect answers
A.LH is responsible for triggering ovulation and supporting the formation of the corpus luteum, not the initial development of follicles. It acts later in the cycle, peaking around day 14 to induce rupture of the mature follicle. It does not initiate follicular development.
C.GnRH is produced by the hypothalamus and regulates the release of both FSH and LH from the anterior pituitary. While it is essential for initiating the hormonal cascade, it does not directly stimulate ovarian follicle development. It functions upstream in the hormonal hierarchy.
D.Progesterone is secreted primarily by the corpus luteum after ovulation and is involved in preparing the endometrium for potential implantation. It inhibits FSH and LH through negative feedback and is not involved in stimulating follicular growth, but rather in the luteal phase.
Take home points
- FSH is the key hormone responsible for follicular growth in the early menstrual cycle.
- LH triggers ovulation but does not initiate follicular development.
- GnRH regulates the release of FSH and LH but has no direct effect on the ovaries.
Progesterone dominates the luteal phase and inhibits follicular development.
A nurse is assessing a patient with suspected infertility. What is the definition of primary infertility?
Explanation
Primary infertilityis defined by the failure to achieve a clinical pregnancy after 12 months or more of regular, unprotected, and heterosexualintercourse in couples who have never conceived. It involves hormonal, anatomical, or geneticcauses in either partner. Normal semen volume is 1.5–6.8 mL, total motility ≥40%, and female FSH should be <10 mIU/mL during the follicular phase. Ovulatory dysfunction, tubal blockage, or abnormal sperm parameters are the most common contributors. Evaluation should begin after 12 months in women <35 years, or after 6 months if ≥35 years.
Rationale for correct answers
B.Primary infertility is defined scientifically as the inability to conceive after 12 consecutive months of regular, unprotected sexual intercourse. This is the international standard set by the WHO and CDC for couples with no previous pregnancies. The definition excludes secondary infertility, miscarriage, or male factor causes unless specified.
Rationale for incorrect answers
A.This defines secondary infertility, not primary. Secondary infertility occurs when a couple has previously achieved a pregnancy but is now unable to conceive again despite 12 months of unprotected intercourse. The term primary infertility specifically refers to couples who have never achieved pregnancy.
C.The inability to carry a pregnancy to term relates to recurrent pregnancy loss or miscarriage, not infertility. Infertility refers to the failure to achieve conception, while pregnancy loss is a separate reproductive issue, often involving different investigations and management approaches.
D.Male factor infertility is a cause of infertility, not a definition. While male factors contribute to about 40–50% of infertility cases, the term "primary infertility" does not specify the source (male or female), only the condition of never having conceived.
Take home points
- Primary infertility means never having conceived after 12 months of unprotected intercourse.
- Secondary infertility refers to difficulty conceiving after a previous successful pregnancy.
- Inability to carry a pregnancy to term is not defined as infertility.
Male factor is a cause, not a definition, of infertility.
A 32-year-old female presents to the clinic reporting inability to conceive after 18 months of regular, unprotected sexual intercourse. Her menstrual cycles are irregular, occurring every 45-60 days. She also reports increased facial hair and acne. Which of the following conditions is most likely contributing to her infertility?
Explanation
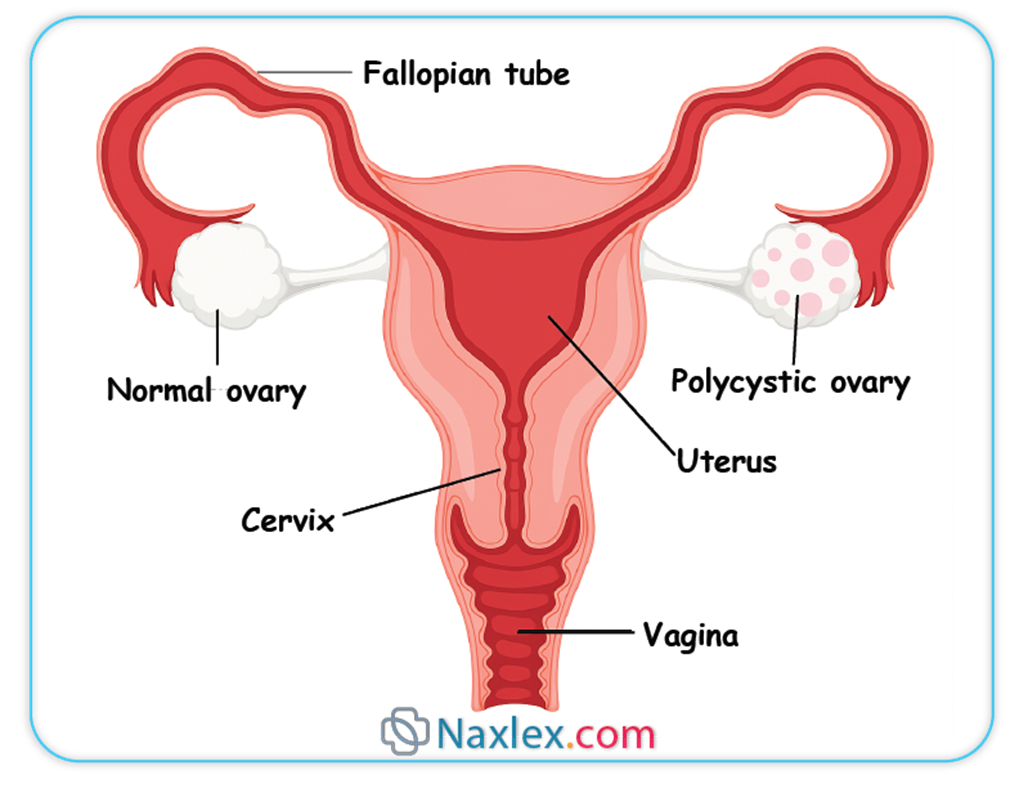
Polycystic ovary syndrome (PCOS)is a common endocrine disorder characterized by chronic anovulation, hyperandrogenism, and polycystic ovarian morphology. It affects approximately 6–10% of reproductive-aged women and is a major cause of infertility. Hallmark features include menstrual irregularities (cycles >35 days), elevated androgens (testosterone >70 ng/dL), and ovarian volume >10 mL or ≥12 follicles per ovary on ultrasound. Insulin resistance, increased LH:FSH ratio (>2:1), and elevated AMH (>4.5 ng/mL) are also common. PCOS increases the risk for type 2 diabetes, metabolic syndrome, and endometrial hyperplasia due to unopposed estrogen.
Rationale for correct answers
C.PCOS is the most likely diagnosis in a woman with infertility, irregular cycles (45–60 days), hirsutism, and acne—all signs of hyperandrogenism and anovulation. The chronic anovulation prevents regular follicular maturation and ovulation, leading to infertility. The history fits the classic diagnostic criteria (Rotterdam criteria) for PCOS.
Rationale for incorrect answers
A.Hypothalamic-pituitary dysfunction usually presents with hypogonadotropic hypogonadism—low FSH and LH—and is often triggered by stress, weight loss, or excessive exercise. These patients typically have absentrather than irregular menses, and do not display signs of androgen excess like hirsutism or acne.
B.Premature ovarian insufficiency presents with menopause before age 40, usually with elevated FSH >25 mIU/mLand amenorrhea or oligomenorrhea. It is not typically associated with hyperandrogenism, and patients may have hot flashes or night sweats. The presence of androgenic symptoms makes PCOS more likely.
D.Endometriosis commonly presents with chronic pelvic pain, dyspareunia, and dysmenorrhea, rather than androgenic symptoms or cycle lengths of 45–60 days. While it can cause infertility due to pelvic adhesions and inflammation, it does not typically feature hirsutism or acne.
Take home points
- PCOS is characterized by irregular cycles, hyperandrogenism, and chronic anovulation.
- Insulin resistance and elevated LH:FSH ratio are common in PCOS.
- Hypothalamic dysfunction presents with low gonadotropins and amenorrhea, not hyperandrogenism.
- Endometriosis causes infertility via pelvic inflammation, not hormonal imbalance.
Which of the following are causes of female infertility? Select all that apply.
Explanation
Female infertilityresults from disorders affecting ovulation, tubal patency, uterine structure, and endocrine balance. Common causes include polycystic ovary syndrome (PCOS), endometriosis, tubal obstruction, and uterine abnormalitiessuch as fibroids. Ovulatory dysfunction accounts for approximately 25–30% of cases, while tubal and uterine factors each contribute about 20–25%. FSH in the early follicular phase should be 4.7–21.5 mIU/mL; estradiol ranges from 30–400 pg/mL. Serum progesterone >3 ng/mL in mid-luteal phase confirms ovulation. Assessment includes hormonal evaluation, pelvic imaging, and ovulation tracking.
Rationale for correct answers
A.PCOSis a leading cause of female infertility due to chronic anovulation. Women present with irregular menses, elevated androgens, and disrupted follicular maturation. The hormonal imbalance interferes with ovulation and conception.
C.Endometriosiscauses infertility through pelvic adhesions, inflammation, and distorted anatomy that impair oocyte pickup and tubal transport. It may also create an inhospitable peritoneal environment for fertilization or implantation.
E.Uterine fibroids(especially submucosal or intramural types) can distort the uterine cavity, interfere with implantation, or cause early pregnancy loss. They are a structural cause of infertility in women.
Rationale for incorrect answers
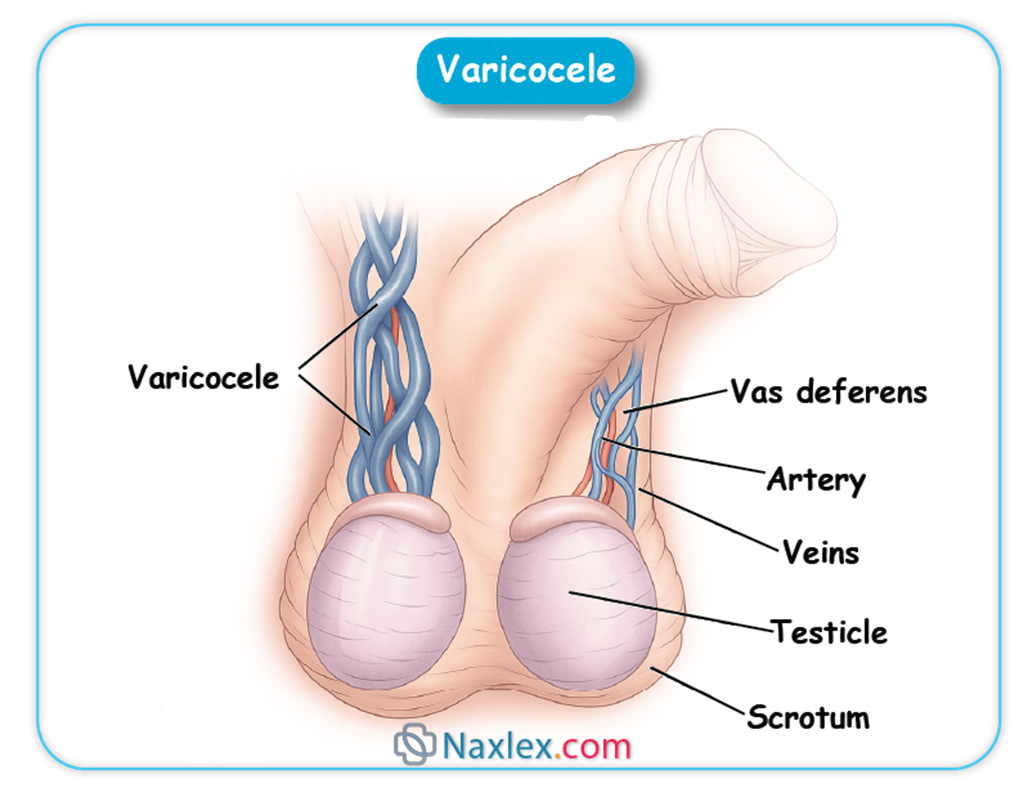
B.Varicoceleis a dilation of the pampiniform plexus in the scrotum and is a malefactor infertility cause. It impairs testicular thermoregulation and sperm quality but does not apply to female infertility.
D.Hypogonadismis a general term indicating reduced gonadal function. In females, primary hypogonadism (e.g., Turner syndrome) can cause infertility, but the term is more commonly associated with maleinfertility due to low testosterone. The question focuses on common femalecauses, making this option inapplicable without specifying female context.
Take home points
- PCOS is the most common hormonal cause of anovulatory infertility.
- Endometriosis causes infertility through pelvic inflammation and adhesions.
- Uterine fibroids can interfere with implantation and embryo development.
- Varicocele is a male infertility factor and not applicable to females.
Which of the following are common causes of ovulatory dysfunction in females? Select all that apply.
Explanation
Ovulatory dysfunctionrefers to the failure of the ovary to release an oocyte during a normal menstrual cycle and is a major cause of female infertility. It results from endocrine imbalances, hypothalamic suppression, or ovarian failure. Normal mid-luteal progesterone levels >3 ng/mL confirm ovulation. FSH levels in the early follicular phase normally range from 4.7–21.5 mIU/mL; LH is typically 5–20 mIU/mL. Common causes include PCOS, hypothalamic-pituitary dysfunction, and premature ovarian insufficiency, all of which alter gonadotropin releaseor ovarian responsiveness. Ovulatory dysfunction accounts for approximately 25–30% of female infertility cases.
Rationale for correct answers
A.PCOS is the most common cause of chronic anovulation. It is associated with hyperandrogenism, insulin resistance, and elevated LH:FSH ratio (>2:1), which disrupt follicular maturation and prevent ovulation.
B.Hypothalamic-pituitary dysfunction results in decreased GnRH secretion, leading to low or inappropriately normal FSH and LH, and subsequently insufficient ovarian stimulation. Common causes include stress, excessive exercise, and eating disorders.
D.Premature ovarian insufficiency involves early depletion of ovarian follicles before age 40. It presents with elevated FSH (>25 mIU/mL), low estradiol (<30 pg/mL), and amenorrhea or oligomenorrhea, causing loss of ovulatory cycles.
Rationale for incorrect answers
C.PID causes infertility primarily by damaging the fallopian tubes through infection-induced scarring. It is not a direct cause of ovulatory dysfunction because it does not affect the hypothalamic-pituitary-ovarian axis or folliculogenesis.
E.Uterine fibroids interfere with implantation or cause mechanical disruption of the uterine cavity but do not affect ovulation. They are structural causes of infertility rather than hormonal or ovulatory.
Take home points
- PCOS causes anovulation through hormonal imbalance and follicular arrest.
- Hypothalamic-pituitary dysfunction reduces GnRH, suppressing FSH and LH.
- POI leads to early follicular depletion and elevated FSH levels.
- PID and fibroids affect fertility but do not cause ovulatory dysfunction.
Which of the following diagnostic tests are used to evaluate female infertility? Select all that apply.
Explanation
Female infertilityis evaluated through a combination of tests that assess ovulation, hormonal profile, tubal patency, and uterine structure. Key investigations include hormonal assays like anti-Müllerian hormone (AMH)for ovarian reserve, imaging such as hysterosalpingogram (HSG)for tubal patency, and laparoscopyfor direct visualization of pelvic pathology. Normal AMH levels range from 1.0–4.0 ng/mL; values <1.0 ng/mL suggest diminished ovarian reserve. HSG is typically done between days 5–10 of the cycle, and laparoscopy is indicated for suspected endometriosis or pelvic adhesions. Evaluation of male factors is complementary but not part of the female infertility workup.
Rationale for correct answers
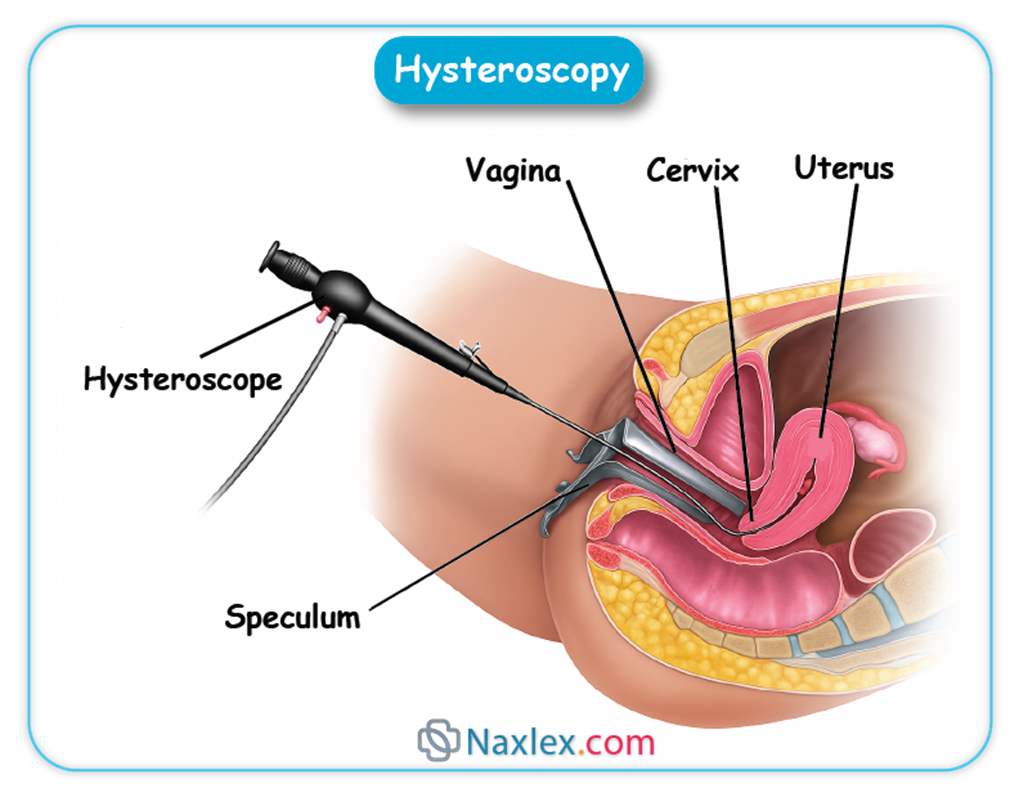
A.Hysterosalpingogram is used to evaluate uterine cavity anatomy and fallopian tube patency by injecting contrast under fluoroscopy. It helps detect tubal obstruction, adhesions, and uterine anomalies, making it a core test in female infertility assessment.
C.Anti-Müllerian hormone reflects the quantity of antral follicles and is used to assess ovarian reserve. High AMH levels (>4.5 ng/mL) may indicate PCOS, while low levels (<1.0 ng/mL) suggest diminished ovarian reserve. It is cycle-independent and highly reliable.
E.Laparoscopy allows direct visualization of pelvic organs and is considered the gold standard for diagnosing endometriosis, pelvic adhesions, and tubal disease. It is both diagnostic and therapeutic in managing structural causes of infertility.
Rationale for incorrect answers
B.Semen analysis is the primary test for maleinfertility and assesses sperm concentration, motility, and morphology. It is not used to evaluate femaleinfertility, though it is essential in a comprehensive infertility evaluation of the couple.
D.Scrotal ultrasound is used to evaluate malereproductive anatomy, particularly for detecting varicocele, testicular masses, or structural abnormalities. It plays no role in diagnosing female infertility.
Take home points
- HSG evaluates tubal patency and uterine cavity.
- AMH is a reliable marker of ovarian reserve in females.
- Laparoscopy is the gold standard for diagnosing endometriosis and adhesions.
- Semen analysis and scrotal ultrasound are used for evaluating male infertility.
Practice Exercise 2
Which diagnostic procedure is considered the gold standard for directly visualizing the pelvic organs and diagnosing endometriosis in a female patient with infertility?
Explanation
Endometriosisis a chronic gynecologic condition characterized by ectopic endometrial tissue, often found on the ovaries, peritoneum, and pelvic organs. It causes chronic pelvic pain, dysmenorrhea, dyspareunia, and infertility. The gold standard for diagnosis is direct visualizationof lesions via laparoscopy, often with biopsy. Lesions may appear as “powder burn” or “blue-black” implants. Endometriosis affects fertility by causing pelvic adhesions, tubal distortion, and an inflammatory environment. CA-125 may be elevated (>35 U/mL) but is nonspecific. Ultrasound may detect endometriomas, but superficial implants are usually invisible on imaging.
Rationale for correct answers
C.Laparoscopy is the gold standard because it allows direct visualization of pelvic structures and biopsy of suspected endometrial implants. It can assess extent and severity of disease, detect adhesions, and facilitate surgical treatment during the same procedure.
Rationale for incorrect answers
A.HSG evaluates the uterine cavity and tubal patency using contrast dye under fluoroscopy. It does not allow visualization of peritoneal or ovarian implants and cannot confirm endometriosis.
B.Transvaginal ultrasound is useful for identifying ovarian endometriomas (chocolate cysts) but cannot detect superficial peritoneal implants or adhesions. It is not diagnostic for endometriosis unless a mass is present.
D.Sonohysterography (SIS) is used to assess the uterine cavity using saline infusion and ultrasound. It detects polyps and fibroids but does not visualize the peritoneum or diagnose endometriosis.
Take home points
- Laparoscopy is the definitive diagnostic method for endometriosis.
- HSG evaluates tubal patency but not pelvic implants.
- Transvaginal ultrasound may detect endometriomas but misses superficial disease.
- SIS is used for uterine cavity evaluation, not peritoneal assessment.
What is the minimum sperm count considered normal in a semen analysis?
Explanation
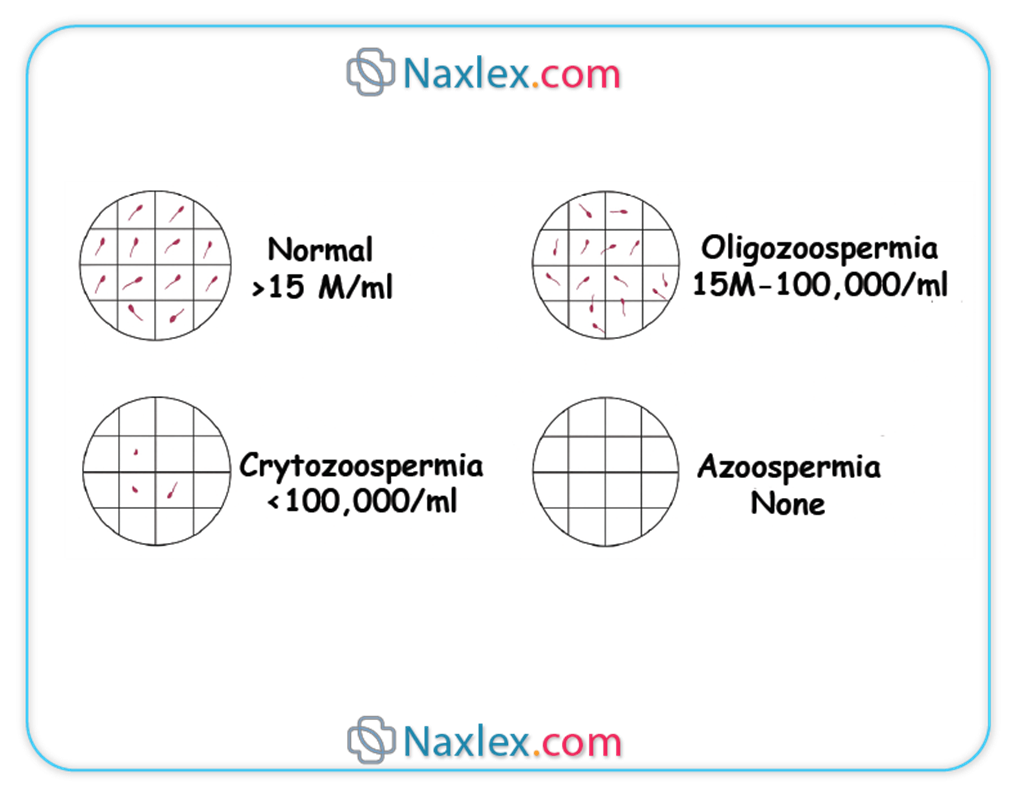
Semen analysisis the cornerstone diagnostic test for assessing male fertilityand includes evaluation of sperm concentration, motility, morphology, volume, and vitality. The World Health Organization (WHO)2021 reference values define the lower limits of normal for semen parameters. A normal sperm concentrationis ≥15 million/mL, total motile sperm ≥40%, progressive motility ≥32%, and normal morphology ≥4% (strict Kruger criteria). Semen volume should be ≥1.4 mL. Abstinence of 2–7 days before the test is recommended to ensure accurate results. Low counts (<15 million/mL) are termed oligozoospermiaand may contribute to infertility.
Rationale for correct answers
C.The WHO 2021 criteria define the minimum normal sperm concentration as 15 million/mL. This threshold reflects the lowest 5th percentile of fertile men and is used globally in fertility assessments. Below this level, the probability of spontaneous conception declines significantly.
Rationale for incorrect answers
A.A concentration of 5 million/mL is well below the WHO cutoff and is classified as moderate to severe oligozoospermia. Fertility is typically impaired at this level, and further investigation is required.
B.While higher than 5 million/mL, 10 million/mL is still below the normal reference range. This value may result in reduced fertility and is not considered normal by WHO standards.
D.Although 20 million/mL was previously used as the lower reference limit in earlier WHO guidelines, the current accepted cutoff is 15 million/mL. Therefore, 20 million/mL is normal, but not the minimum.
Take home points
- Normal sperm concentration is ≥15 million/mL based on WHO 2021.
- Sperm motility should be ≥40% and progressive motility ≥32%.
- Morphology is normal if ≥4% of sperm are morphologically normal.
- Oligozoospermia is diagnosed when sperm count is <15 million/mL.
Which of the following parameters are typically assessed in a routine semen analysis? Select all that apply.
Explanation
Semen analysisis the primary diagnostic test for evaluating male fertilityand assesses the quantity, quality, and functionalityof sperm. It involves measurement of sperm concentration, motility, morphology, volume, and pH, all of which are critical to determine fertilization potential. According to WHO 2021 criteria, normal values include sperm concentration ≥15 million/mL, total motility ≥40%, progressive motility ≥32%, morphology ≥4% normal forms (strict Kruger criteria), volume ≥1.4 mL, and pH between 7.2–8.0. Abnormalities in these parameters may indicate oligozoospermia, asthenozoospermia, teratozoospermia, or other functional deficits.
Rationale for correct answers
A.Sperm concentration, measured in millions per milliliter, assesses the density of sperm in the ejaculate. A normal value is ≥15 million/mL. Low concentration indicates oligozoospermia and may affect fertility.
B.Sperm motility evaluates the percentage of moving sperm and their ability to move progressively toward the egg. Total motility should be ≥40%, with progressive motility ≥32%. Poor motility (asthenozoospermia) reduces fertilization capability.
C.Sperm morphology is assessed under strict Kruger criteria, with ≥4% normal forms considered acceptable. Abnormal shapes can impair the ability to fertilize an egg.
D.Semen pH assesses the acidity or alkalinity of the ejaculate. Normal pH ranges from 7.2–8.0. Deviations may indicate infection (alkaline) or ejaculatory duct obstruction (acidic).
Rationale for incorrect answers
E.Serum testosterone is a hormonalparameter and not part of a routine semen analysis. It is measured separately when evaluating endocrine causes of male infertility, especially in cases of low libido, erectile dysfunction, or signs of hypogonadism.
Take home points
- Routine semen analysis includes sperm concentration, motility, morphology, volume, and pH.
- WHO 2021 criteria define normal values for all semen parameters.
- Serum testosterone is not part of routine semen testing.
Abnormalities in morphology or motility can exist despite normal concentration.
Practice Exercise 3
Which of the following lifestyle modifications should a nurse emphasize to a male patient seeking to improve his sperm health?
Explanation
Male infertilityis commonly associated with abnormal sperm parameters, including reduced concentration, motility, and morphology. Lifestyle factors such as smoking, alcohol, heat exposure, and intense physical stress disrupt the hypothalamic-pituitary-gonadalaxis and impair spermatogenesis. Normal semen values include sperm concentration ≥15 million/mL, total motility ≥40%, progressive motility ≥32%, morphology ≥4% normal forms, volume ≥1.4 mL, and pH 7.2–8.0. Oxidative stress from toxins like nicotine and ethanol reduces sperm DNA integrity, while scrotal hyperthermia from tight clothing or heat exposure impairs sperm production.
Rationale for correct answers
C.Smoking and alcohol are well-established negative influences on sperm health. Nicotine increases oxidative stress and DNA fragmentation, while alcohol disrupts testosterone synthesis and impairs spermatogenesis. Limiting alcohol intake and quitting smoking improves sperm count, motility, and morphology.
Rationale for incorrect answers
A.Increased hot tub usage exposes the testes to high temperatures. The scrotum normally maintains a temperature 2–4°C below core body temperature. Prolonged heat exposure impairs Sertoli cell function, disrupts spermatogenesis, and reduces sperm quality.
B.Tight-fitting underwear elevates testicular temperature, contributing to scrotal hyperthermia. Sustained heat exposure reduces sperm concentration and motility by affecting the seminiferous epithelium and hormone regulation in the testes.
D.High-intensity endurance exercise, especially daily, elevates cortisol levels and suppresses the hypothalamic-pituitary-gonadal axis. This leads to reduced luteinizing hormone and testosterone levels, which impairs spermatogenesis and may result in oligozoospermia or azoospermia in extreme cases.
Take home points
- Smoking and alcohol impair sperm DNA and hormonal balance.
- Heat exposure reduces sperm count and motility.
- Intense endurance exercise suppresses testosterone production.
- Sperm production requires testicular temperatures below core body temperature.
A nurse is monitoring a patient undergoing IVF. What is a potential complication of controlled ovarian stimulation?
Explanation
Controlled ovarian stimulation (COS)is a pharmacologic technique used in in vitro fertilization (IVF)to induce multi-follicular development. It involves administration of gonadotropinslike FSH or hMG to stimulate the ovaries, often followed by a trigger (hCG or GnRH agonist) to induce ovulation. A significant risk of COS is ovarian hyperstimulation syndrome (OHSS), which results from exaggerated ovarian response. OHSS is characterized by increased vascular permeability, third spacing, and ovarian enlargement. Severe OHSS presents with hemoconcentration (hematocrit >45%), elevated estradiol (>3,500 pg/mL), and ascites. Risk factors include high AMH (>3.5 ng/mL), PCOS, and high antral follicle count.
Rationale for correct answers
B.OHSS is a well-known complication of IVF, triggered by excessive ovarian response to gonadotropins. Elevated VEGF levels from granulosa cells increase capillary permeability, leading to ascites, pleural effusions, and hypovolemia. Severe forms may involve electrolyte imbalance, oliguria, and thromboembolism.
Rationale for incorrect answers
A.Hypothyroidism is an endocrine disorder affecting ovulatory function and fertility but is not caused by IVF or ovarian stimulation. It is associated with high TSH (>4.0 mIU/L) and low free T4 (<0.8 ng/dL), and may contribute to menstrual irregularities and miscarriage risk.
C.Hyperprolactinemia results from pituitary dysfunction, medication (e.g., antipsychotics), or hypothyroidism. It suppresses GnRH and impairs ovulation, but it is not a complication of IVF or gonadotropin use.
D.Varicocele is a dilation of the pampiniform plexus and is a male factor infertility cause. It does not occur in females and is unrelated to IVF procedures or ovarian stimulation.
Take home points
- OHSS is a complication of ovarian stimulation during IVF.
- Symptoms include ascites, hemoconcentration, and enlarged ovaries.
- PCOS and high AMH increase OHSS risk.
- Hypothyroidism and hyperprolactinemia affect fertility but are not IVF complications.
A nurse is explaining the procedure of Intrauterine Insemination (IUI) to a couple. Where is the washed and concentrated sperm typically placed during this procedure?
Explanation
Intrauterine insemination (IUI)is a form of assisted reproductive technology (ART)used to treat certain types of infertility, including unexplained infertility, mild male factor infertility, and cervical factor infertility. The procedure involves placing washed and concentrated spermdirectly into the uterine cavityaround the time of ovulation. The sperm is typically processed to remove seminal plasma, prostaglandins, and debris, enhancing motilityand reducing the risk of uterine cramping or immune reaction. The timing is coordinated with ovulation, often using a urinary LH surge or hCG trigger injection. A typical insemination uses 0.3–0.5 mL of prepared sperm.
Rationale for correct answers
C.In IUI, the sperm is placed directly into the uterine cavityusing a sterile catheter passed through the cervix. This technique increases the number of motile sperm reaching the fallopian tubes and reduces the distance they must travel to fertilize the egg.
Rationale for incorrect answers
A.Direct placement into the fallopian tuberefers to a different procedure called gamete intrafallopian transfer (GIFT), which is no longer commonly used due to invasiveness and lower success rates compared to IVF and IUI.
B.Placement into the ovarian follicleis not performed in any standard fertility treatment. Follicular aspiration occurs in IVF, where oocytes are retrieved from follicles—not inseminated directly.
D.Placement into the vaginal canalis the natural site during intercourse or artificial insemination via intracervical methods. However, IUI bypasses the cervix and vagina to improve fertilization chances by depositing sperm directly into the uterus.
Take home points
- IUI deposits sperm directly into the uterus near ovulation.
- It bypasses cervical mucus and vaginal environment, improving fertilization chances.
- GIFT involves tubal placement, not used in IUI.
- Follicles are not inseminated directly in any fertility procedure.
Which of the following are Assisted Reproductive Technologies (ART)? Select all that apply.
Explanation
Assisted reproductive technologies (ART)are medical procedures that involve the direct manipulation of gametes or embryosto achieve fertilization and pregnancy. ART bypasses natural fertilization pathways and includes advanced techniques like in vitro fertilization (IVF)and intracytoplasmic sperm injection (ICSI). ART is distinct from fertility-enhancing medications, which stimulate ovulation, and surgical interventions, which address anatomical abnormalities. ART is used in cases of tubal obstruction, male factor infertility, unexplained infertility, and failed ovulation induction. Success depends on age, ovarian reserve, and embryo quality.
Rationale for correct answers
A.Intrauterine insemination (IUI) is a form of ART where washed and concentrated sperm are placed directly into the uterus to improve the chance of fertilization. It is often used in conjunction with ovulation induction.
C.In vitro fertilization (IVF) involves retrieval of oocytes, fertilization outside the body, and transfer of the embryo into the uterus. It is one of the most widely used ART methods.
E.Intracytoplasmic sperm injection (ICSI) is a specialized form of IVF in which a single sperm is injected directly into the cytoplasm of an egg. It is used for severe male factor infertility or failed fertilization in prior IVF cycles.
Rationale for incorrect answers
B.Clomiphene citrate is an ovulation induction medication that stimulates the hypothalamic-pituitary-ovarian axis by blocking estrogen receptors. It is not ART because it does not involve handling of gametes or embryos.
D.Varicocelectomy is a surgical procedure to correct varicocele and improve sperm quality. It is a surgical treatment for male infertility but not an ART, as it does not involve assisted fertilization.
Take home points
- ART involves direct manipulation of gametes or embryos.
- IVF and ICSI are the primary ART procedures used worldwide.
- IUI is considered ART as it bypasses the cervical barrier.
- Fertility drugs and surgeries are supportive but not ART.
Which of the following are important aspects of the nursing role in infertility care? Select all that apply.
Explanation
Nursing role in infertility carefocuses on education, emotional support, and care coordinationthroughout the often complex and emotionally taxing infertility journey. Nurses play a central role in explaining diagnostic procedures, guiding patients through treatment protocols like IVFor IUI, and providing psychological support. They do not perform surgical procedures or independently prescribe medications unless certified as advanced practice nurses under specific regulatory authority. Nurses also act as liaisons between patients and specialists, ensuring timely communication and adherence to treatment plans.
Rationale for correct answers
A.Nurses provide comprehensive education on fertility processes, procedures like IVF, and medication protocols. They ensure that patients understand timelines, instructions, and risks involved in treatment, improving adherence and outcomes.
B.Infertility is emotionally distressing. Nurses offer counseling, normalize emotional responses, and refer to mental health services when needed. They support individuals and couples experiencing grief, anxiety, and frustration.
C.Nurses coordinate care by scheduling tests, tracking cycle timing, and facilitating communication between reproductive endocrinologists, labs, and other providers, which is essential in time-sensitive fertility treatments.
Rationale for incorrect answers
D.Prescribing fertility medications such as gonadotropins or clomiphene citrate is beyond the scope of practice for most registered nurses. This responsibility lies with physicians or advanced practice providers (e.g., nurse practitioners with prescriptive authority).
E.Surgical sperm retrieval (e.g., testicular sperm aspiration or extraction) is a urologic procedure performed by physicians, not nurses. Nurses may assist in perioperative care but do not perform surgery.
Take home points
- Nurses educate, support, and advocate for patients undergoing infertility treatment.
- Emotional support is crucial due to the psychological burden of infertility.
- Nurses coordinate appointments, labs, and communication during ART procedures.
Prescribing medications and performing surgical retrieval are outside standard nursing roles.
Comprehensive Questions
What is the prevalence of infertility among couples worldwide?
Explanation
Infertilityis defined as the inability to conceive after 12 monthsof regular, unprotected intercourse. It affects both men and women and may result from ovulatory dysfunction, tubal pathology, uterine abnormalities, or male factor infertility. According to the World Health Organization (WHO), 1 in 6 couplesglobally are affected by infertility during their reproductive lifetime. Primary infertility refers to inability to achieve a pregnancy, while secondary infertility is the failure to conceive after a previous pregnancy. Age, lifestyle, infections, and environmental exposures significantly influence fertility.
Rationale for correct answers
B.Global epidemiological data from the WHO estimates that 1 in 6 couples—approximately 17% of the population—experience infertility during their lifetime. This includes both developed and developing countries and highlights infertility as a major public health concern.
Rationale for incorrect answers
A.The 1 in 10 estimate underrepresents the current global prevalence. Earlier estimates suggested this figure, but updated data confirms a higher rate.
C.While 1 in 4 women may experience infertility during specific periods of their reproductive years, this does not reflect couple-based prevalence. The correct global couple-based prevalence is 1 in 6.
D.The 1 in 8 statistic (12.5%) is closer to historical data specific to certain high-income countries but is not the current global average reported by WHO.
Take home points
- Global infertility affects 1 in 6 couples during reproductive years.
- WHO defines infertility as failure to conceive after 12 months of unprotected sex.
- Both male and female factors contribute equally to infertility.
- Age, lifestyle, and underlying health issues increase infertility risk.
Which condition is characterized by anovulation, hyperandrogenism, and polycystic ovaries on ultrasound?
Explanation
Polycystic ovary syndrome (PCOS)is a complex endocrine disordermarked by anovulation, hyperandrogenism, and the presence of polycystic ovarieson ultrasound. It is the most common cause of ovulatory dysfunctionand female infertility. Diagnostic criteria (Rotterdam criteria) require 2 of 3: oligo/anovulation, clinical/biochemical hyperandrogenism (e.g., hirsutism, elevated total testosterone >50 ng/dL), and polycystic ovarian morphology (≥12 follicles measuring 2–9 mm or ovarian volume >10 mL on ultrasound). LH:FSH ratio is often elevated (>2:1), and AMH levels are typically high (>4.5 ng/mL) due to increased antral follicles. Insulin resistance is frequently associated and increases the risk for metabolic syndrome.
Rationale for correct answers
B.PCOS is characterized by the triad of anovulation, hyperandrogenism, and polycystic ovarian morphology. The patient's irregular cycles, signs of androgen excess (acne, hirsutism), and ultrasound findings confirm the diagnosis. Elevated LH:FSH ratio and AMH are common lab findings.
Rationale for incorrect answers
A.Endometriosis involves ectopic implantation of endometrial tissue, typically presenting with chronic pelvic pain, dysmenorrhea, and infertility. It is not characterized by anovulation or hyperandrogenism and does not present with polycystic ovaries on ultrasound.
C.Premature ovarian insufficiency (POI) involves cessation of ovarian function before age 40. It presents with amenorrhea, elevated FSH (>25 IU/L), and low estradiol (<20 pg/mL). Ovaries are usually small and hypoactive—not polycystic.
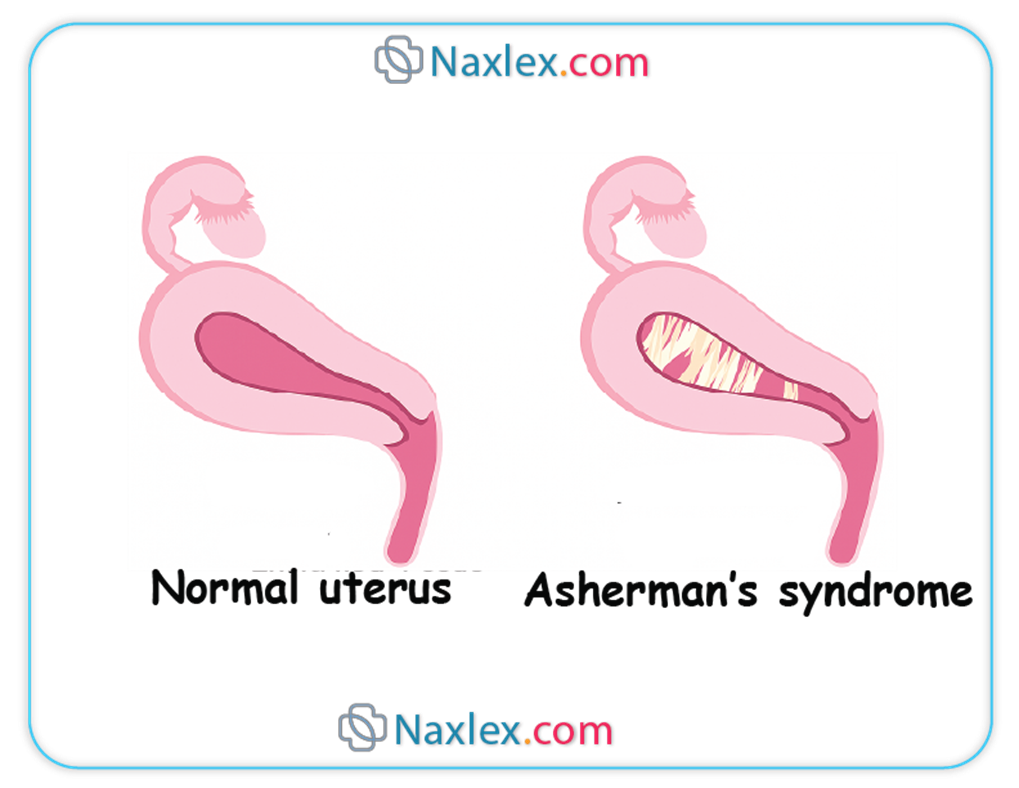
D.Asherman’s syndrome is caused by intrauterine adhesions following uterine surgery or infection. It presents with secondary amenorrhea and infertility but does not involve hyperandrogenism or polycystic ovaries.
Take home points
- PCOS is diagnosed with at least two of: anovulation, hyperandrogenism, and polycystic ovaries.
- High AMH and LH:FSH ratio support PCOS diagnosis.
- Endometriosis causes infertility but is not linked to androgen excess.
POI and Asherman’s cause amenorrhea but with distinct etiologies and imaging.
A nurse is reviewing the semen analysis results for a male patient. The report indicates a sperm concentration of 10 million sperm/mL. Which term best describes this finding?
Explanation
Oligospermiarefers to a low sperm concentrationin the ejaculate and is a major cause of male factor infertility. According to WHO 2021 guidelines, a normal sperm concentration is ≥15 million/mL. Values below this threshold are classified as oligospermia, while complete absence of sperm is termed azoospermia. Other semen parameters assessed include motility(normal ≥40% total), progressive motility(≥32%), morphology(≥4% normal forms), volume(≥1.4 mL), and pH(7.2–8.0). Causes of oligospermia include varicocele, hormonal imbalances, genetic abnormalities, and toxic exposures(e.g., heat, smoking, radiation).
Rationale for correct answers
C.A sperm concentration of 10 million/mL is below the WHO lower reference limit of 15 million/mL and is classified as oligospermia. This indicates reduced sperm density, which may impair the chances of natural conception.
Rationale for incorrect answers
A.Azoospermia is the complete absence of sperm in the ejaculate. It is diagnosed when no sperm are seen in centrifuged semen samples and is not consistent with a count of 10 million/mL.
B.Asthenozoospermia refers to reduced sperm motility. It is diagnosed when total motility is <40% or progressive motility is <32%. The question does not provide any data on motility.
D.Teratozoospermia refers to abnormal sperm morphology, specifically when <4% of sperm have normal forms according to strict Kruger criteria. Morphology is not mentioned in this result.
Take home points
- Oligospermia is defined as sperm concentration <15 million/mL.
- WHO 2021 provides updated reference values for semen analysis.
- Azoospermia means no sperm are present in ejaculate.
- Asthenozoospermia and teratozoospermia involve motility and morphology, respectively.
Which medication is a selective estrogen receptor modulator used to induce ovulation?
Explanation
Clomiphene citrateis a selective estrogen receptor modulator (SERM)used as a first-line ovulation induction agent, especially in women with anovulationdue to polycystic ovary syndrome (PCOS). It works by competitively inhibiting estrogen receptors in the hypothalamus, blocking negative feedback and leading to increased secretion of gonadotropin-releasing hormone (GnRH). This stimulates the anterior pituitary to release follicle-stimulating hormone (FSH)and luteinizing hormone (LH), which promote follicular developmentand ovulation. The standard dose is 50–150 mg orally for 5 days starting on day 2–5 of the menstrual cycle. Ovulation usually occurs 5–10 days after the last dose. Side effects include hot flashes, mood swings, and risk of multiple gestation.
Rationale for correct answers
C.Clomiphene citrate is a SERM that induces ovulation by increasing FSH and LH through estrogen receptor antagonism in the hypothalamus. It is especially effective in PCOS-related anovulation and is often the first-line pharmacologic therapy.
Rationale for incorrect answers
A.Letrozole is an aromatase inhibitor, not a SERM. It inhibits estrogen synthesis, reducing negative feedback on the hypothalamus, thereby increasing FSH secretion. It is increasingly used as an alternative to clomiphene, particularly in PCOS, but it acts via a different mechanism.
B.Gonadotropins (FSH, LH, hMG) directly stimulate the ovaries and are used in advanced ovulation induction or ART like IVF. They are not SERMs and require careful monitoring due to higher OHSS risk.
D.Progesterone is used for luteal phase supportor to treat luteal phase defects. It does not induce ovulation but is given after ovulation or embryo transfer to support endometrial receptivity.
Take home points
- Clomiphene citrate is a SERM used to induce ovulation.
- It works by blocking estrogen receptors in the hypothalamus, increasing FSH and LH.
- Letrozole is not a SERM; it is an aromatase inhibitor.
- Gonadotropins stimulate the ovaries directly but are not first-line due to cost and monitoring needs.
Which of the following are common surgical interventions for male infertility? Select all that apply.
Explanation
Male infertility surgical management
Male infertility surgical managementtargets anatomical or obstructive causes of impaired sperm delivery, varicocele repair, and sperm retrieval. Varicoceleaffects 15% of all men and up to 40% of infertile men, impairing spermatogenesisby increasing testicular temperature. Obstructive azoospermia from vasectomy or congenital blockages may need microsurgical correctionor testicular sperm extraction (TESE). Normal semen parameters: volume ≥1.5 mL, sperm concentration ≥15 million/mL, motility ≥40%, morphology ≥4%.
Rationale for correct answers
B.Varicocelectomy is the surgical ligation of dilated scrotal veins. It improves sperm parameters by reducing testicular heat stress and oxidative damage, often restoring fertility in men with clinically palpable varicocele and abnormal semen analysis.
C.Vasectomy reversal (vasovasostomy or vasoepididymostomy) reconnects the severed vas deferens to restore sperm flow. It is indicated in obstructive azoospermia due to prior vasectomy and can result in return of sperm to ejaculate.
D.Surgical sperm retrieval methods like testicular sperm extraction (TESE) or percutaneous epididymal sperm aspiration (PESA) are used in men with azoospermia. Retrieved sperm are used in intracytoplasmic sperm injection (ICSI) for assisted reproduction.
Rationale for incorrect answers
A.Myomectomy is a surgical procedure to remove uterine fibroids (leiomyomas) and is used in women to improve fertility when fibroids distort the endometrial cavity. It is not related to male infertility.
E.Hysteroscopy is a diagnostic and therapeutic procedure for evaluating the female uterine cavity. It is used in women for polyp removal, adhesiolysis, and evaluation of intrauterine pathology. It has no role in male reproductive treatment.
Take home points
- Varicocelectomy is indicated for varicocele-associated impaired spermatogenesis.
- Vasectomy reversal is used in obstructive azoospermia due to vasectomy.
- TESE and related sperm retrieval techniques are options for azoospermic men undergoing ART.
- Myomectomy and hysteroscopy are exclusively female fertility procedures.
Which hormonal imbalance in a female patient is directly treated with dopamine agonists like bromocriptine or cabergoline to improve ovulation?
Explanation
Hyperprolactinemiais a condition characterized by elevated serum prolactin levels, typically >25 ng/mL in women, which disrupts gonadotropin-releasing hormone (GnRH)secretion and results in anovulation, amenorrhea, and infertility. Common causes include pituitary adenomas (prolactinomas), hypothyroidism, and certain medications (e.g., antipsychotics, SSRIs). High prolactin suppresses pulsatile GnRH, lowering FSHand LH, which impairs follicular developmentand estrogen production. Treatment includes dopamine agonistssuch as bromocriptineand cabergoline, which inhibit prolactin secretion from the anterior pituitary, restore ovulation, and often shrink adenomas.
Rationale for correct answers
B.Hyperprolactinemia is treated with dopamine agonists like bromocriptine and cabergoline. These drugs stimulate dopamine receptors in the pituitary to suppress prolactin production, allowing GnRH, LH, and FSH to normalize and ovulation to resume.
Rationale for incorrect answers
A.Hypothyroidism can cause secondary hyperprolactinemia by increasing thyrotropin-releasing hormone (TRH), which stimulates prolactin secretion. However, it is treated with levothyroxine, not dopamine agonists. Correction of TSH levels (<4.0 mIU/L) will usually reduce prolactin indirectly.
C.Elevated FSH levels typically indicate diminished ovarian reserveor primary ovarian insufficiency, and are not treated with dopamine agonists. High FSH (>10–15 IU/L) reflects low feedback from estrogen or inhibin and requires other fertility strategies, including ART.
D.Low estrogen can result from many causes, including hypothalamic amenorrhea or menopause. Treatment depends on the underlying cause but does not involve dopamine agonists. Estrogen replacement or ovulation induction may be appropriate.
Take home points
- Hyperprolactinemia impairs ovulation by suppressing GnRH.
- Dopamine agonists like cabergoline lower prolactin and restore fertility.
- Hypothyroidism may cause secondary hyperprolactinemia but is treated with levothyroxine.
Elevated FSH and low estrogen reflect ovarian dysfunction, not prolactin excess.
Which condition is associated with dilated scrotal veins?
Explanation
A.Varicocele is directly characterized by dilated scrotal veins. The venous dilation disrupts thermoregulation of the testes, leading to impaired sperm quality and infertility. It is the most common correctable cause of male infertility.
Rationale for incorrect answers
B.Azoospermia is the absence of sperm in ejaculate, which can be due to obstructive or non-obstructive causes. While varicocele may contribute to azoospermia, azoospermia itself is not defined by dilated veins.
C.Klinefelter syndrome is a genetic condition (47,XXY) associated with small testes, gynecomastia, and infertility due to testicular failure. It is not associated with dilated scrotal veins.
D.Oligospermia is defined as sperm concentration <15 million/mL. While varicocele may contribute to oligospermia, the term itself refers to low sperm count and not to venous dilation.
Take home points
- Varicocele involves dilated pampiniform plexus veins in the scrotum.
- It is a common, correctable cause of male infertility.
- Diagnosis is clinical and confirmed by scrotal ultrasound.
- Treatment improves sperm quality and fertility outcomes.
A 28-year-old female presents with a history of recurrent miscarriages. A uterine imaging study reveals a congenital anomaly where a fibrous wall divides the uterine cavity. Which uterine factor is most likely responsible for her recurrent pregnancy losses?
Explanation
Uterine septumis a congenital Müllerian anomalywhere a fibrous or fibromuscular bandincompletely resorbs during embryologic development, resulting in a longitudinal partition of the uterine cavity. It is the most common uterine anomaly associated with recurrent pregnancy loss, accounting for up to 60% of Müllerian anomalies. The septum is typically avascular, limiting implantation and fetal nourishment, increasing the risk of first-trimester miscarriages, preterm labor, and malpresentation. Diagnosis is best made via MRI, 3D ultrasound, or hysterosalpingography, and confirmed by hysteroscopy, which also allows for surgical resection (metroplasty).
Rationale for correct answers
C.A uterine septum is a congenital anomaly characterized by a fibrous wall dividing the endometrial cavity. Its poor vascularization contributes to implantation failure or early pregnancy loss. Hysteroscopic metroplasty can restore normal uterine anatomy and improve pregnancy outcomes.
Rationale for incorrect answers
A.Uterine fibroids (leiomyomas) are benign smooth muscle tumors. Submucosal fibroids may contribute to miscarriage, but fibroids do not typically present as a fibrous wall dividing the cavity. Intramural and subserosal fibroids are less implicated in recurrent losses.
B.Asherman’s syndrome involves intrauterine adhesions, usually acquired after curettage or infection. It leads to secondary amenorrhea, infertility, or miscarriage, but is not congenital or defined by a septum-like structure on imaging.
D.Endometrial polyps are localized overgrowths of endometrial glands and stroma. They may cause abnormal uterine bleeding or subfertility but do not present as a fibrous partition of the uterine cavity and are not a leading cause of recurrent miscarriage.
Take home points
- Uterine septum is the most common congenital uterine anomaly linked to recurrent pregnancy loss.
- It is a fibrous or fibromuscular division of the uterine cavity with poor vascularity.
- Diagnosis is via hysteroscopy, 3D ultrasound, or MRI.
- Surgical resection significantly improves pregnancy outcomes.
What is the primary purpose of preimplantation genetic testing (PGT)?
Explanation
Preimplantation genetic testing (PGT)is a laboratory procedure used during in vitro fertilization (IVF)to screen embryos for genetic abnormalitiesbefore uterine transfer. It involves biopsy of embryonic cells, typically at the blastocyst stage (day 5–6), followed by genetic analysis. The goal is to detect aneuploidy, monogenic disorders, or structural chromosomal rearrangements. PGT helps select chromosomally normal embryos, reducing the risk of implantation failure, recurrent miscarriage, and genetic disease transmission. Indications include advanced maternal age, recurrent pregnancy loss, previous child with a genetic disorder, or known parental chromosomal abnormality.
Rationale for correct answers
C.PGT is specifically designed to evaluate embryos for chromosomal or genetic abnormalities prior to implantation. It improves IVF outcomes by transferring embryos most likely to result in a healthy pregnancy.
Rationale for incorrect answers
A.Ovulation induction is achieved with agents such as clomiphene citrate, letrozole, or gonadotropins. PGT is unrelated to the hormonal stimulation or ovulation process.
B.Tubal patency is assessed using hysterosalpingogram (HSG)or sonohysterography, not genetic testing. PGT evaluates embryo genetics, not fallopian tube function.
D.Sperm motility is influenced by factors such as varicocele, hormonal status, and lifestyle. PGT does not modify sperm motility; it screens embryos post-fertilization.
Take home points
- PGT screens embryos for chromosomal or genetic defects before implantation.
- Common indications include advanced maternal age or known parental genetic disorders.
- It is performed during IVF, usually at the blastocyst stage.
- PGT improves implantation and reduces miscarriage by selecting euploid embryos.
What is the definition of secondary infertility?
Explanation
Secondary infertilityis defined as the inability to conceive or carry a pregnancy to term after previously achieving a pregnancy, regardless of the outcome (live birth, miscarriage, or ectopic). It affects many couples and shares similar causes with primary infertility, including ovulatory dysfunction, tubal disease, uterine abnormalities, and male factor infertility. Contributing factors include age-related decline in fertility, especially after age 35, endometriosis, adhesions from prior surgeries or infections, and lifestyle changes. Evaluation involves assessment of ovulation, tubal patency, uterine anatomy, and semen analysis. Normal female hormone parameters: FSH <10 IU/L, LH 5–20 IU/L, prolactin <25 ng/mL, and TSH 0.5–4.5 mIU/L.
Rationale for correct answers
C.Secondary infertility refers to the inability to conceive after a prior conception. This distinguishes it from primary infertility, where no prior pregnancy has occurred. The definition applies even if the prior pregnancy did not result in a live birth.
Rationale for incorrect answers
A.This defines primary infertility, which refers to couples who have never achieved a pregnancy despite 12 months of unprotected intercourse.
B.This describes the timeline for initiating infertility evaluationin women >35, but it is not a definition of secondary infertility. The diagnosis is independent of how long attempts have been made.
D.This implies recurrent pregnancy loss, which is a distinct condition. While miscarriage may occur in secondary infertility, the definition hinges on the inability to conceive, not to maintain pregnancy.
Take home points
- Secondary infertility occurs after a prior conception.
- It shares causes with primary infertility, including ovulatory, tubal, uterine, and male factors.
- Prior surgeries or infections may lead to acquired fertility issues.
- Evaluation and treatment should be individualized based on history and testing.
Which of the following female uterine factors can interfere with implantation or maintenance of pregnancy? Select all that apply.
Explanation
A.Uterine fibroids, particularly submucosal ones, disrupt the endometrial lining, leading to poor implantation, abnormal placentation, or miscarriage. They may also alter uterine contractility and blood flow.
B.A uterine septum is a congenital malformation composed of fibrous tissue with poor vascular supply. It increases the risk of early miscarriage and implantation failure.
C.Asherman’s syndrome is the presence of intrauterine adhesions, often from prior curettage or infection. It results in reduced endometrial function and poor implantation due to scarred endometrial surfaces.
D.Endometrial polyps are focal overgrowths of endometrial glands and stroma. They can distort the uterine cavity, act as a physical barrier to implantation, and alter local cytokine and hormone signaling.
Rationale for incorrect answers
E.Cervical stenosis impairs sperm transport and may obstruct embryo transfer in ART. It can also cause hematometra or dysmenorrhea due to blocked menstrual outflow. However it does not prevent implantation or maintenance of pregnancy.
Take home points
- Structural uterine abnormalities interfere with implantation and pregnancy maintenance.
- Fibroids and polyps distort the endometrial cavity and reduce fertility.
- A uterine septum is the most common Müllerian anomaly linked to miscarriage.
- Asherman’s syndrome and cervical stenosis reduce endometrial receptivity or access.
Which of the following hormones are involved in the hypothalamic-pituitary-ovarian (HPO) axis? Select all that apply.
Explanation
Hypothalamic-pituitary-ovarian (HPO) axisis a complex hormonal feedback system that regulates the female reproductive cycle, ovulation, and hormonal balance. The hypothalamussecretes gonadotropin-releasing hormone (GnRH)in a pulsatile manner, which stimulates the anterior pituitaryto release follicle-stimulating hormone (FSH)and luteinizing hormone (LH). These gonadotropins act on the ovaries, promoting follicular development, ovulation, and the production of estradioland progesterone. Progesteronefrom the corpus luteum provides negative feedback to the hypothalamus and pituitary to regulate further hormone release. Normal serum FSH: 3–10 IU/L; LH: 5–20 IU/L (mid-cycle peak ~40 IU/L); progesterone (luteal phase): 5–20 ng/mL.
Rationale for correct answers
A.GnRH is secreted by the hypothalamus in a pulsatile fashion, initiating the HPO axis. It controls the release of FSH and LH from the anterior pituitary.
B.FSH stimulates follicular growth in the ovaries and promotes estrogen production by granulosa cells, essential for follicle maturation and endometrial proliferation.
D.LH surges mid-cycle, triggering ovulation and luteinization of the dominant follicle. It also stimulates theca cells to produce androgens, which are converted to estrogens.
E.Progesterone is secreted by the corpus luteum after ovulation. It prepares the endometrium for implantation and exerts negative feedback on GnRH, FSH, and LH.
Rationale for incorrect answers
C.Testosterone is not a primary hormone in the HPO axis. While it is produced in small amounts by the ovaries and adrenal glands and contributes to libido, its primary role is in the hypothalamic-pituitary-gonadal axis in males, not in regulating ovulation in females.
Take home points
- The HPO axis controls ovulation and hormone regulation in the menstrual cycle.
- GnRH stimulates FSH and LH, which act on the ovaries.
- Progesterone provides negative feedback post-ovulation.
Testosterone is not a core hormone in the female HPO axis.
Which of the following are male factor infertility conditions? Select all that apply.
Explanation
Male factor infertilityaccounts for approximately 30%-50% of infertility cases and is primarily due to abnormalities in sperm production, sperm function, or sperm delivery. Normal sperm concentrationis ≥15 million/mL, with normal motility≥40% and morphology≥4% (Kruger strict criteria). Causes include varicocele, infections, genetic defects (e.g., Klinefelter syndrome), and hormonal imbalances (e.g., low FSH/LH/testosterone). Lifestyle factors like smoking, alcohol, anabolic steroids, and environmental toxins can impair spermatogenesis.
Rationale for correct answers
A.Oligospermia is defined as a sperm count below 15 million/mL. It directly contributes to male infertility due to reduced availability of sperm for fertilization. It may be caused by testicular dysfunction, hormonal disorders, or varicocele.
C.Azoospermia refers to the complete absence of sperm in the ejaculate, a severe form of male factor infertility. It may be obstructive (e.g., vas deferens blockage) or non-obstructive (e.g., testicular failure).
E.Varicocele is an abnormal dilation of the pampiniform venous plexus in the scrotum and is a common reversible cause of male infertility. It impairs thermoregulation of the testis, affecting spermatogenesis and sperm quality.
Rationale for incorrect answers
B.Endometriosis is a gynecological condition where endometrial tissue grows outside the uterus. It causes female infertility due to inflammation, adhesions, and impaired oocyte quality, not related to male reproductive factors.
D.Polycystic ovary syndrome (PCOS) is a female endocrine disorder characterized by hyperandrogenism, oligo/anovulation, and polycystic ovaries. It is a leading cause of female infertility and is unrelated to male reproductive abnormalities.
Take home points
- Oligospermia and azoospermia are direct male factor infertility conditions involving low or absent sperm counts.
- Varicocele is a treatable male infertility cause due to testicular venous congestion.
- Endometriosis and PCOS are exclusively female infertility conditions.
- Evaluation of infertility requires differentiation between male and female causes using semen analysis and hormonal testing.
Exams on Infertility
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
Define the concepts of primary and secondary infertility from a clinical and epidemiological perspective.
• Delineate the multifaceted etiology of both female and male factor infertility, including specific pathophysiological mechanisms.
• Describe the comprehensive diagnostic evaluation protocols for couples experiencing infertility, including specific laboratory and imaging modalities.
• Identify and explain the various medical, surgical, and assisted reproductive technologies (ART) used in the management of infertility.
• Analyze the critical psychosocial and ethical considerations inherent to infertility care.
• Formulate a nursing care plan that integrates evidence-based practices, patient education, and emotional support for individuals and couples navigating infertility.
Introduction
Infertility is a complex, multifactorial disease of the reproductive system, defined by the failure to achieve a clinical pregnancy after 12 months or more of regular, unprotected sexual intercourse. This timeframe is reduced to 6 months for females aged 35 years or older. Infertility affects a significant portion of the global population, with estimates suggesting that it impacts approximately one in six couples worldwide. The etiology is diverse, with approximately one-third of cases attributed to female factors, one-third to male factors, and the remaining cases resulting from combined factors or remaining unexplained. A thorough and systematic diagnostic evaluation is imperative for identifying the underlying cause, which then guides the selection of appropriate therapeutic interventions. The nursing role in infertility care is pivotal, extending beyond clinical procedures to encompass patient education, emotional support, and ethical guidance.
Infertility: Definition And Etiology
1. Primary and Secondary Infertility
• Primary infertility is the inability to conceive in a nulliparous individual or couple after 12 months of regular, unprotected coitus.
• Secondary infertility is the inability to conceive after a couple has previously achieved a clinical pregnancy, regardless of the outcome of that pregnancy.
2. Epidemiology and Risk Factors
• Infertility affects a substantial global population, with a prevalence of approximately one in six couples, underscoring its public health significance.
• Risk factors are numerous and include both modifiable and non-modifiable elements.
➤ Advanced maternal age is a primary non-modifiable risk factor, as oocyte quality and quantity decline with age.
➤ Lifestyle factors, such as smoking, excessive alcohol consumption, and substance abuse, negatively impact gamete quality in both sexes.

➤ Obesity and extreme underweight can disrupt hormonal balance and lead to ovulatory dysfunction in females and compromised spermatogenesis in males.
➤ Environmental toxins and occupational exposures have been implicated in reproductive dysfunction.
• Nursing Insights: The nurse must perform a comprehensive health history, including a detailed assessment of lifestyle behaviors, occupational exposures, and chronological age, to identify potential risk factors and formulate a patient-centered care plan.
3. Female Factor Infertility
• Female factors contribute to approximately one-third of all infertility cases and often involve complex interactions between hormonal, anatomical, and genetic components.
3.1. Ovulatory Dysfunction
• This is the most frequent cause of female infertility, characterized by anovulation or oligo-ovulation.
• Polycystic Ovary Syndrome (PCOS) is a prevalent endocrine disorder characterized by anovulation, hyperandrogenism, and the presence of polycystic ovaries on ultrasound. This condition disrupts the normal follicular development and release.
• Hypothalamic-Pituitary Dysfunction results from issues in the central nervous system, often caused by stress, excessive exercise, or extreme weight loss, leading to a disruption in the gonadotropin-releasing hormone (GnRH) pulse generator and subsequent low levels of follicle-stimulating hormone (FSH) and luteinizing hormone (LH).
• Premature Ovarian Insufficiency (POI), also known as premature menopause, involves the cessation of ovarian function before the age of 40, characterized by amenorrhea and elevated FSH levels.
• Hyperprolactinemia is a condition of elevated prolactin levels, which can suppress GnRH, FSH, and LH, leading to anovulation.
3.2. Tubal and Peritoneal Factors
• Tubal obstruction or damage is a significant cause of infertility, preventing the union of the oocyte and sperm.
• Pelvic Inflammatory Disease (PID), often caused by untreated sexually transmitted infections (STIs) such as Chlamydia and Gonorrhea, can lead to chronic inflammation and scarring of the fallopian tubes.
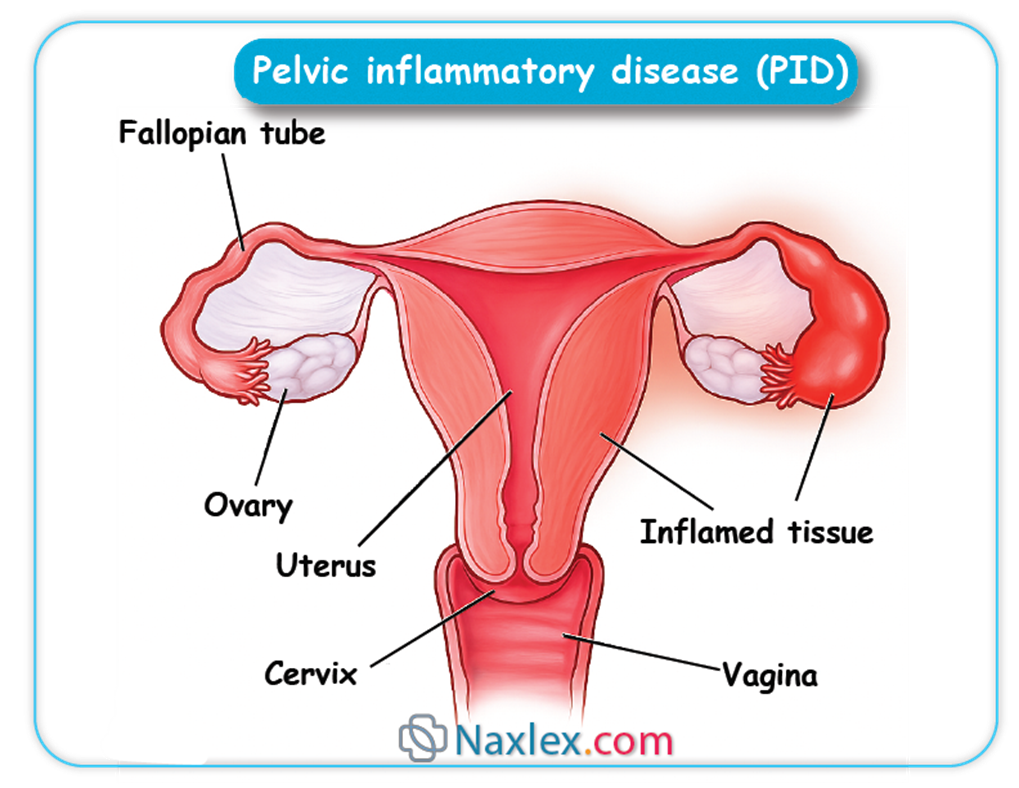
• Endometriosis is a chronic inflammatory condition where endometrial-like tissue grows outside the uterus, leading to adhesions, inflammation, and anatomical distortion of the pelvic organs, which can obstruct tubal patency and alter the peritoneal environment.
• Nursing Insights: Patient education on the prevention of STIs and the importance of early treatment is crucial for mitigating the risk of tubal factor infertility. The nurse should also be aware of the signs and symptoms of PID, such as pelvic pain and fever, and the potential long-term reproductive consequences.
3.3. Uterine and Cervical Factors
• Uterine abnormalities, both congenital and acquired, can interfere with implantation and maintenance of a pregnancy.
• Congenital anomalies, such as a uterine septum, can impair blood flow to the endometrial lining.
• Acquired conditions, such as submucosal fibroids or endometrial polyps, can disrupt the endometrial cavity.
• Asherman's syndrome is characterized by intrauterine adhesions or synechiae, often resulting from a prior uterine surgery, such as a dilation and curettage (D&C), which can compromise endometrial receptivity.
• Cervical factors involve issues with the cervix, such as cervical stenosis or the production of hostile cervical mucus, which can impede sperm transport.
4. Male Factor Infertility
• Male factors are responsible for approximately one-third of infertility cases, involving a wide range of conditions that affect spermatogenesis, sperm transport, and ejaculatory function.
4.1. Seminal Abnormalities
• These are the most common causes of male infertility and are identified through a semen analysis.
• Oligospermia is a sperm concentration below the normal reference range (less than 15 million sperm/mL).
• Azoospermia is the complete absence of sperm in the ejaculate.
• Asthenozoospermia refers to reduced sperm motility.
• Teratozoospermia is characterized by an abnormal sperm morphology.
Crytozoospermia
4.2. Endocrine Disorders
• Disorders of the hypothalamic-pituitary-gonadal axis can lead to impaired sperm production.
• Hypogonadotropic hypogonadism results from a deficiency in GnRH, FSH, and LH, leading to low testosterone levels and inadequate spermatogenesis.
• Hyperprolactinemia can also suppress gonadotropin secretion in males, similar to its effect in females.
4.3. Anatomical and Genetic Factors
• Varicocele, a condition of dilated scrotal veins, is a common anatomical cause, as it can elevate scrotal temperature and negatively impact sperm quality.
• Obstructive azoospermia can result from congenital absence of the vas deferens (often associated with cystic fibrosis mutations) or from a prior vasectomy.
• Klinefelter syndrome (47, XXY karyotype) is a genetic condition that causes testicular dysfunction and often leads to azoospermia.
• Nursing Insights: The nurse should provide clear, sensitive education on the purpose and preparation for a semen analysis, including the required abstinence period. The nurse also plays a key role in explaining the diagnostic findings and therapeutic options in a manner that mitigates the potential feelings of guilt or inadequacy often associated with male factor infertility.
5. Unexplained Infertility
• This diagnosis is assigned when a comprehensive workup of both partners, including ovulation assessment, semen analysis, and tubal patency evaluation, reveals no identifiable cause.
• This diagnosis can be emotionally challenging for couples, and the nurse must provide empathetic support while explaining that empirical treatment strategies, such as ovulation induction or ART, are often successful.
Diagnostic Evaluation Of Infertility
The diagnostic workup is a systematic process to identify the underlying causes of infertility, typically commencing with less invasive procedures and progressing to more complex ones.
1. Female Diagnostic Procedures
1.1. Hormonal Assays
• FSH and LH levels: These are measured on cycle day 3 to assess ovarian reserve and hypothalamic-pituitary function. An elevated day 3 FSH level is indicative of diminished ovarian reserve.
• Anti-Müllerian Hormone (AMH) level: This is a key biomarker for ovarian reserve, as it correlates with the number of remaining antral follicles. It can be measured at any point in the menstrual cycle.
• Progesterone level: A serum progesterone level is measured during the mid-luteal phase (approximately 7 days post-ovulation) to confirm that ovulation has occurred.
• Thyroid-stimulating hormone (TSH) and Prolactin: These are assessed to rule out thyroid dysfunction and hyperprolactinemia, which can both disrupt the menstrual cycle.
1.2. Imaging Studies
• Transvaginal Ultrasound (TVUS): This is a non-invasive procedure used to visualize the uterus, ovaries, and adnexa. It is essential for assessing uterine anatomy, endometrial thickness, and antral follicle count.
• Hysterosalpingogram (HSG): An HSG is a fluoroscopic procedure where a radiopaque dye is injected through the cervix. It is considered the gold standard for evaluating the patency of the fallopian tubes and the contour of the uterine cavity.
• Hysteroscopy: This is a minimally invasive surgical procedure where a thin, lighted telescope is inserted through the cervix to directly visualize the uterine cavity. It is superior to HSG for diagnosing and treating intrauterine abnormalities like polyps, fibroids, or adhesions.
• Laparoscopy: This is a surgical procedure involving a small incision to insert a laparoscope into the peritoneal cavity, providing direct visualization of the pelvic organs. It is the gold standard for diagnosing and treating endometriosis and pelvic adhesions.
Nursing Insights: The nurse's role is critical in patient preparation and education for these procedures. For an HSG, the nurse must ensure the patient is not pregnant and is scheduled for the follicular phase of the cycle. For surgical procedures like hysteroscopy or laparoscopy, the nurse must provide pre-operative teaching, including NPO status, and post-operative care instructions.
2. Male Diagnostic Procedures
2.1. Semen Analysis
• This is the cornerstone of male fertility evaluation and assesses multiple parameters.
• Sperm Concentration: The number of sperm per milliliter of ejaculate.
• Sperm Motility: The percentage of sperm that are moving and the quality of their movement.
• Sperm Morphology: The percentage of sperm with normal shape and size, assessed using strict criteria (e.g., Kruger's criteria).
• Semen Volume and pH: These parameters are also evaluated to assess the function of the seminal vesicles and prostate.
• Nursing Insights: The nurse provides explicit instructions for semen collection, emphasizing the need for a specific abstinence period (2-5 days) and the importance of collecting the entire ejaculate. The sample must be delivered to the lab within a narrow timeframe to ensure accurate results.
2.2. Endocrine Evaluation
• Serum testosterone, FSH, and LH levels are measured to assess the hypothalamic-pituitary-testicular axis, particularly in cases of severe oligospermia or azoospermia.
2.3. Genetic Testing and Imaging
• Genetic testing for karyotype abnormalities (e.g., Klinefelter syndrome) or cystic fibrosis mutations may be indicated in cases of severe male factor infertility.
• Scrotal ultrasound is a non-invasive imaging modality used to evaluate testicular size, detect masses, and identify varicoceles.
Medical And Surgical Management Of Infertility
Therapeutic interventions for infertility are tailored to the specific diagnosis and can range from non-invasive medication regimens to complex surgical and reproductive technologies.
1. Ovulation Induction
• This is the first-line treatment for ovulatory dysfunction.
• Clomiphene citrate is a selective estrogen receptor modulator (SERM) that blocks estrogen receptors in the hypothalamus, leading to an increase in GnRH, FSH, and LH, thereby stimulating follicular development.
• Letrozole is an aromatase inhibitor that lowers estrogen levels, similarly increasing GnRH and gonadotropins, and is often preferred for patients with PCOS due to a lower risk of multiple pregnancies and ovarian hyperstimulation syndrome (OHSS).
• Gonadotropins, which contain FSH and/or LH, are injectable hormones used for controlled ovarian stimulation in patients who do not respond to oral agents or are undergoing ART.
• Nursing Insights: The nurse is responsible for teaching the patient the proper administration of injectable medications, monitoring for adverse effects such as OHSS, and scheduling follow-up ultrasounds to track follicular development.
2. Surgical Interventions
• Surgical procedures are often indicated for anatomical causes of infertility.
• Laparoscopy can be used to treat endometriosis, lyse adhesions, and correct tubal abnormalities.
• Hysteroscopy is used to remove uterine septa, polyps, or submucosal fibroids.
• Varicocelectomy is a surgical procedure to repair a varicocele in males, which may improve sperm parameters.
3. Assisted Reproductive Technologies (ART)
• ART encompasses procedures that involve the in vitro handling of gametes or embryos.
3.1. Intrauterine Insemination (IUI)
• This procedure involves placing washed and concentrated sperm directly into the uterine cavity, bypassing the cervix.
• IUI is indicated for mild male factor infertility, cervical factor infertility, or unexplained infertility.
3.2. In Vitro Fertilization (IVF)
• IVF is a multi-step process where oocytes are retrieved from the ovaries, fertilized with sperm in a laboratory, and the resulting embryo is transferred to the uterus.
• This is the most effective ART and is indicated for tubal factor infertility, severe male factor infertility, advanced maternal age, and failed cycles of less invasive treatments.

3.3. Intracytoplasmic Sperm Injection (ICSI)
• ICSI is a specialized procedure often performed in conjunction with IVF, where a single, morphologically normal sperm is injected directly into an oocyte.
• This is indicated for severe male factor infertility, such as extreme oligospermia or asthenozoospermia, or for couples with a history of failed fertilization in previous IVF cycles.
Psychosocial And Ethical Considerations
Psychosocial Impact
• Infertility is a chronic, often protracted condition that has significant psychosocial ramifications for individuals and couples.
• Common emotional responses include grief, anxiety, depression, and a profound sense of loss.
• The demanding nature of treatments, including frequent clinic visits, injections, and the financial burden, can lead to marital strain and social isolation.
• The nurse's role is to provide empathetic, non-judgmental support and to screen for signs of emotional distress. Referral to support groups, such as Resolve: The National Infertility Association, and mental health professionals is an essential component of comprehensive care.
Ethical and Legal Issues
• ART introduces complex ethical and legal questions that the nurse must be prepared to address.
• Embryo disposition, including the fate of cryopreserved embryos, is a critical issue that requires couples to make difficult decisions.
• Third-party reproduction, which involves the use of donor gametes (sperm or oocytes) or a gestational carrier, raises questions of parental rights and genetic lineage.
• Preimplantation Genetic Testing (PGT), which screens embryos for chromosomal abnormalities or specific genetic disorders, presents ethical dilemmas regarding embryo selection.
Nursing Role in Providing Support
• Patient Education: The nurse serves as the primary educator, providing clear and accurate information about diagnostic procedures, treatment protocols, and potential side effects in a compassionate manner.
• Emotional Support: Creating a safe and therapeutic environment where patients can express their fears and frustrations without judgment is paramount. The nurse validates the patient's feelings and normalizes their experience.
• Advocacy: The nurse acts as a patient advocate, ensuring the patient's preferences are respected, and their questions are answered by the healthcare team.
• Coordination of Care: Given the complex nature of infertility treatment, the nurse is often the central point of contact, coordinating appointments, lab work, and communication between the patient and multiple specialists.
Summary
Infertility is a pervasive and complex reproductive disease affecting millions of couples worldwide. It is clinically defined as the inability to achieve pregnancy after a specified period of unprotected intercourse, with different criteria for women under and over 35 years of age. The etiology is diverse and can be attributed to female factors, such as ovulatory dysfunction (PCOS, POI), tubal disease (endometriosis, PID), and uterine abnormalities (fibroids, Asherman's syndrome). Male factor infertility commonly results from seminal abnormalities (oligospermia, azoospermia) or anatomical issues like varicocele. A comprehensive diagnostic evaluation is essential and involves a series of hormonal assays, imaging studies like HSG and laparoscopy, and a detailed semen analysis. Management options are individualized based on the diagnosis and include medical treatments like ovulation induction with agents such as clomiphene citrate and letrozole, surgical interventions to correct anatomical issues, and advanced assisted reproductive technologies (ART) such as IUI, IVF, and ICSI. The psychosocial and ethical dimensions of infertility are profound, with patients often experiencing significant emotional distress. Nurses play an indispensable role in providing comprehensive education, empathetic support, and ethical guidance to help patients navigate this challenging journey.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Infertility
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


