Please set your exam date
Drugs Used for Diuresis
Study Questions
Exams on Drugs Used for Diuresis
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
- Describe the definition and primary therapeutic purposes of diuretics in clinical practice.
- Identify the major classes of diuretics and their specific nephron sites of action.
- Explain the mechanism of action and pharmacologic effects of carbonic anhydrase inhibitors.
- Discuss the mechanism, clinical significance, and adverse effects of loop diuretics.
- Summarize the mechanism, indications, and monitoring requirements for thiazide diuretics.
- Explain how potassium-sparing diuretics conserve potassium while promoting mild diuresis.
- Describe the rationale, mechanisms, and clinical benefits of combination diuretic products.
- Identify common and serious adverse effects associated with each class of diuretics.
- Outline nursing interventions, monitoring strategies, and patient education for diuretic therapy.
- Evaluate therapeutic effectiveness and safety of diuretics using fluid balance, electrolytes, and clinical outcomes.
Introduction
Definition
Diuretics are medications that increase urine output by acting on specific segments of the nephron to promote the excretion of sodium and water.
By reducing intravascular volume, diuretics decrease blood pressure, preload, and edema, making them essential in cardiovascular, renal, and endocrine disorders.
Primary Purposes of Diuretic Therapy
Diuretics are prescribed to:
- Reduce fluid overload in conditions such as heart failure, renal disease, and liver cirrhosis
- Manage hypertension by lowering circulating blood volume
- Decrease edema (peripheral, pulmonary, cerebral)
- Correct or prevent electrolyte imbalances in specific clinical situations
- Reduce intraocular pressure and intracranial pressure (select agents)
Sites of Action in the Nephron
Each class of diuretics works at a different location within the nephron, which determines its potency and electrolyte effects:
- Proximal Convoluted Tubule (PCT): Carbonic anhydrase inhibitors
- Loop of Henle (Ascending Limb): Loop diuretics
- Distal Convoluted Tubule (DCT): Thiazide diuretics
- Collecting Duct: Potassium-sparing diuretics
Understanding the site of action helps predict:
- Degree of diuresis
- Electrolyte losses
- Acid–base effects
- Drug combinations used in therapy
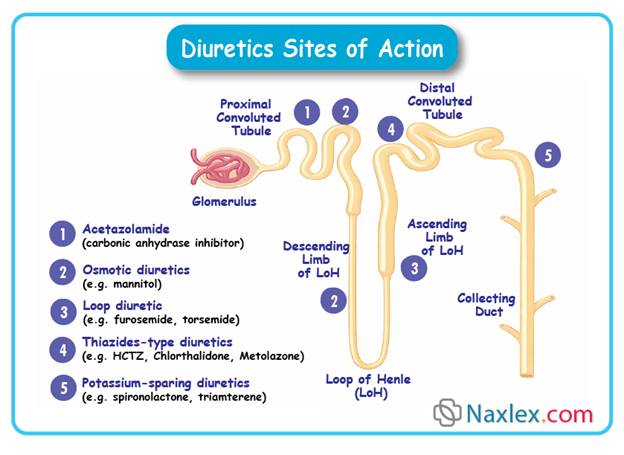
Major Classes of Diuretics
Diuretics are broadly classified into:
- Carbonic Anhydrase Inhibitors
- Example: Acetazolamide
- Loop Diuretics
- Sulfonamide-type: Furosemide, Bumetanide, Torsemide
- Non-sulfonamide: Ethacrynic acid
- Thiazide and Thiazide-Like Diuretics
- Examples: Hydrochlorothiazide, Chlorthalidone, Metolazone
- Potassium-Sparing Diuretics
- Aldosterone antagonists: Spironolactone
- Sodium channel blockers: Amiloride, Triamterene
- Combination Diuretic Products
- Fixed-dose combinations to enhance efficacy and minimize potassium imbalance
Most diuretics work by blocking sodium reabsorption at specific nephron sites.
Because water follows sodium, inhibition of sodium reabsorption leads to increased water excretion.
Key principles:
- Greater sodium blockade = greater diuretic effect
- Electrolyte losses depend on nephron location
- Potent diuresis increases the risk of hypovolemia and electrolyte imbalance
Therapeutic Uses of Diuretics
Common clinical indications include:
- Heart failure (acute and chronic)
- Hypertension
- Pulmonary edema
- Chronic kidney disease
- Nephrotic syndrome
- Ascites due to liver disease
- Glaucoma
- Increased intracranial pressure
Carbonic Anhydrase Inhibitors
Examples:
• acetazolamide (Diamox)
• methazolamide (Neptazane)
Mechanism of Action & Drug Effects:
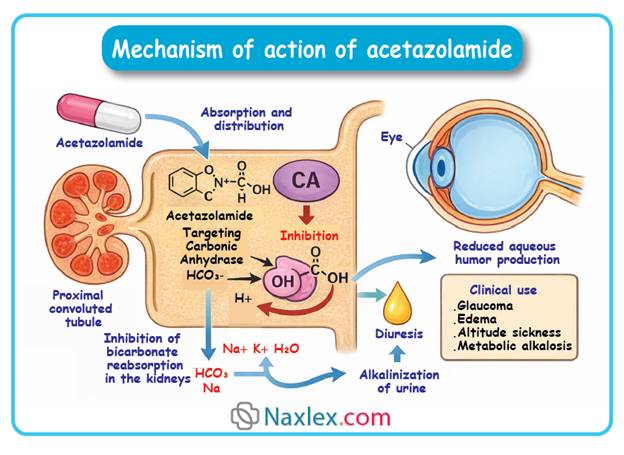
Carbonic anhydrase inhibitors act by inhibiting carbonic anhydrase in the proximal renal tubule.
This enzyme normally catalyzes the conversion of carbon dioxide and water to bicarbonate and hydrogen ions.
Inhibition leads to:
• Decreased reabsorption of bicarbonate → increased urinary bicarbonate excretion.
• Increased excretion of sodium, potassium, and water → mild diuresis.
• Alkalinization of urine and mild metabolic acidosis due to bicarbonate loss.
• Reduced intraocular pressure (secondary effect; relevant in glaucoma).
Key pharmacologic effects in diuresis:
• Mild diuretic effect – less potent than loop or thiazide diuretics.
• Reduction of extracellular fluid volume.
• Limited natriuresis compared with other diuretics; primarily used in specific indications.
• Alters urinary pH – may affect drug excretion and electrolyte balance.
Clinical Significance:
Carbonic anhydrase inhibitors are primarily used when mild diuresis is needed or in combination therapy.
They are rarely used as first-line diuretics for chronic fluid overload because of limited efficacy.
Useful in conditions requiring urinary alkalinization, reduction of intraocular pressure, or metabolic alkalosis correction.
Indications (for diuretic use):
• Edema associated with mild fluid retention.
• Adjunct therapy in heart failure when other diuretics are insufficient.
• Prevention or treatment of metabolic alkalosis.
• Treatment of glaucoma-related fluid overload (secondary benefit).
Nursing relevance:
• Monitor fluid balance – intake/output, weight, and signs of dehydration.
• Assess electrolytes, particularly potassium and sodium, due to increased excretion.
• Observe for signs of metabolic acidosis.
Adverse Effects:
Common effects:
• Polyuria
• Fatigue or drowsiness
• Mild hypokalemia and sodium loss
Serious or rare effects:
• Metabolic acidosis – may exacerbate underlying conditions
• Severe electrolyte imbalance – especially with prolonged use or combination therapy
• Nephrolithiasis – due to alkaline urine promoting stone formation
Nursing Tip:
Encourage patients to maintain adequate fluid intake to reduce the risk of dehydration and kidney stones.
Contraindications / Precautions:
• Severe renal or hepatic impairment
• Pre-existing electrolyte imbalance
• Adrenocortical insufficiency
• Sulfonamide hypersensitivity
Drug Interactions:
• Digoxin – risk of toxicity increases with hypokalemia
• Other diuretics – additive electrolyte disturbances
• Amphetamines – urinary alkalinization may reduce excretion of some drugs
• Lithium – increased risk of lithium toxicity
Nursing Insight:
• Administer with food to reduce gastrointestinal upset.
• Monitor electrolytes closely during therapy.
• Educate patients on recognizing early signs of hypokalemia (muscle weakness, cramps, arrhythmias).
• Encourage adherence even if mild diuresis is not immediately noticeable.
• Adjust dosing based on renal function and patient response.
Rationale:
By inhibiting carbonic anhydrase, these drugs increase urinary excretion of bicarbonate, sodium, potassium, and water, providing mild diuresis. Electrolyte monitoring and patient education are critical to prevent complications.
Monitoring & Evaluation:
• Fluid balance – daily weights, intake/output
• Serum electrolytes – sodium, potassium, bicarbonate
• Renal function – serum creatinine, BUN
• Acid-base status – monitor for metabolic acidosis
• Clinical response – reduction in edema and improvement in fluid overload symptoms
Loop Diuretics
Examples:
Sulfonamide-type:
• furosemide (Lasix)
• bumetanide (Bumex)
• torsemide (Demadex)
Non-sulfonamide:
• ethacrynic acid (Edecrin)
Mechanism of Action & Drug Effects:
Loop diuretics act primarily on the thick ascending limb of the loop of Henle.
They inhibit the Na⁺-K⁺-2Cl⁻ symporter, preventing reabsorption of sodium, potassium, and chloride.
This results in:
• Profound diuresis – rapid and potent fluid removal.
• Increased urinary excretion of sodium, potassium, chloride, calcium, and magnesium.
• Reduction of extracellular fluid volume – effective in edema and volume overload.
• Decreased blood pressure secondary to volume depletion.
• Mild vasodilation – contributes to decreased preload and afterload in heart failure.
Key pharmacologic effects in diuresis:
• Rapid onset of action – especially when given IV.
• Highly efficacious even in renal impairment.
• Potent natriuresis – superior to thiazides for severe fluid overload.
Clinical Significance:
Loop diuretics are first-line agents for acute edema and severe fluid overload.
They are essential in conditions requiring rapid diuresis and in patients with impaired renal function, as they remain effective when GFR is low.
Indications (for diuretic use):
• Pulmonary edema – especially secondary to heart failure.
• Peripheral edema – due to chronic heart failure, nephrotic syndrome, or cirrhosis.
• Hypertension – primarily when fluid overload contributes.
• Hypercalcemia – enhances calcium excretion.
Nursing relevance:
• Monitor fluid balance – intake/output, daily weight, edema.
• Assess electrolytes – particularly potassium, sodium, magnesium, and calcium.
• Observe for hypotension due to rapid volume depletion.
Adverse Effects:
Common effects:
• Hypokalemia – may cause muscle weakness or arrhythmias
• Hyponatremia
• Hypomagnesemia
• Orthostatic hypotension
Serious or rare effects:
• Ototoxicity – usually with high IV doses or rapid administration
• Severe dehydration – especially in elderly or renal-impaired patients
• Electrolyte imbalance leading to arrhythmias or seizures
Nursing Tip:
Monitor electrolytes closely and encourage potassium-rich foods or supplementation when appropriate.
Contraindications / Precautions:
• Anuria – ineffective if urine output absent
• Severe electrolyte depletion – can exacerbate hypokalemia or hyponatremia
• Sulfa allergy – caution with sulfonamide-type loop diuretics
• Hepatic coma – risk of worsening encephalopathy due to electrolyte imbalance
Drug Interactions:
• Digoxin – increased risk of toxicity with hypokalemia
• Aminoglycosides – additive ototoxicity risk
• Lithium – altered renal clearance can increase toxicity
• Other diuretics – additive electrolyte disturbances
• NSAIDs – may reduce diuretic efficacy
Nursing Insight:
• Administer IV doses slowly to reduce ototoxicity risk.
• Educate patients on signs of electrolyte imbalance – muscle cramps, weakness, palpitations.
• Monitor daily weights and fluid status closely.
• Adjust doses based on renal function and response.
• Encourage adherence and explain the need for follow-up labs.
Rationale:
Loop diuretics inhibit the Na⁺-K⁺-2Cl⁻ symporter, producing potent diuresis and electrolyte excretion. Rapid fluid removal improves edema and pulmonary congestion, but monitoring is essential to prevent complications.
Monitoring & Evaluation:
• Fluid balance – daily weight, intake/output
• Serum electrolytes – sodium, potassium, magnesium, calcium
• Renal function – BUN, creatinine
• Blood pressure – monitor for hypotension
• Clinical assessment – edema reduction, pulmonary status, signs of dehydration or arrhythmia
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Drugs Used for Diuresis
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


