Please set your exam date
Growth And Development In Infants
Study Questions
Practice Questions
The father of a 2-month-old girl is expressing concern that his infant may be getting spoiled. The nurse’s best response is:
Explanation
Erik Erikson’s theory of psychosocial developmentis a framework that explains how people evolve emotionally and socially across their lifespan. He proposed that human development unfolds in eight distinct stages, each marked by a central conflict that must be resolved for healthy psychological growth.
Rationale for correct answer:
B.According to Erikson’s theory of psychosocial development, the stage for infants is trust vs. mistrust. When caregivers consistently meet an infant's physical and emotional needs, the child learns the world is safe and predictable, forming the basis for future secure relationships and emotional regulation. Meeting needs such as feeding, comfort, and holding does not spoil an infant.
Rationale for incorrect answers:
A.“She just needs love and attention. Don’t worry; she’s too young to spoil.”This is partially correct, but lacks developmental context. While it affirms the infant can't be spoiled, it doesn’t explain the importance of consistent caregivingin promoting trust and security.
C.“Infants need to be fed and cleaned; if you’re sure those needs are met, just let her cry.”Ignoring cries, even when physical needs are met, can cause distress and erode trust. Crying is an infant’s only communication tool. Emotional comfort is a legitimate need, and withholding it can be harmful.
D.“Consistency in meeting needs is important, but you’re right, holding her too much will spoil her.”Infants cannot be spoiled by being held or comforted. This response reinforces harmful myths and undermines appropriate bonding and attachment behaviors.
Take home points
- Infants cannot be spoiled; they rely on consistent caregiving to feel secure.
- Prompt, nurturing responses to distress foster trust, emotional health, and future autonomy.
- Nurses should educate caregivers using evidence-based, developmentally appropriate guidance, especially when addressing myths rooted in cultural or generational beliefs.
Various children are being seen in the clinic for well-baby checks. By what age should a nurse expect a child to begin to use simple words to communicate needs?
Explanation
Developmental milestonesare age-specific tasks and behaviors most children can do within a certain age range. They guide parents and healthcare professionals in monitoring a child's development and identifyingpotential developmental delays. The milestones are categorized into different areas, such as motor skills, sensory development, language, and social skills.
Rationale for correct answer:
A.By 10 to 12 months, most infants begin to say simple words like “mama” or “dada” with meaning. They also understand basic instructions like “no” or “bye-bye”, use gestures like pointing or waving, and attempt to imitate speech sounds. This stage marks the beginning of expressive languageused to meet basic needs.
Rationale for incorrect answers:
B.Age 1–2 years:While vocabulary expands rapidly during this stage (up to 50+ words), first simple wordstypically begin before 12 months, making this slightly late for the initiation of verbal communication.
C.Age 6–9 month:Infants this age begin babbling(e.g., “ba-ba,” “da-da”) but these are not yet meaningful words. Communication is mostly nonverbal (smiles, cries, gestures).
D.Age 2–3 years:By this age, children usually form two- to three-word sentencesand have a vocabulary of several hundred words. This stage reflects complex communication, not the beginning of speech.
Take home points
- Infants typically say first meaningful words around 10–12 months.
- Language development is closely tied to nutritional and neurological health.
- Early language delays may indicate hearing issues, developmental delays, or nutritional deficits and should prompt further assessment.
- Nurses play a key role in monitoring milestones and guiding caregivers on what to expect and when to seek help.
A nurse in a clinic is assessing the weight of an infant. Which infant’s weight indicates to the nurse that the infant’s weight is normal for the infant’s age?
Explanation
Weight gainis a key indicator of adequate nutrition in infants. Deviations from expected weight milestones may suggest under- or overnutrition, feeding difficulties, or underlying medical conditions. Regular monitoring helps identify potential nutrient deficiencies or growth delaysearly.
Rationale for correct answer:
C.This reflects normal infant growth patterns. By 5–6 months, an infant's birth weight typically doubles. By 12 months, the weight typically triples. This pattern is a clinical benchmark for assessing healthy growth and nutritional adequacy in infancy.
Rationale for incorrect answers:
A.Tripling weight in only 6 monthssuggests excessive weight gain, which may signal overnutrition or fluid retention, especially if not accompanied by proportional height/length growth.
B.Doubling by 12 monthsis below expected growth. This may indicate inadequate nutrition, feeding difficulties, or a medical concern such as malabsorption or chronic illness.
D.The baby’s weight doubling in the first 6 months and doubling again in the next 6 months implies the weight is four times the birth weight by 12 months, which is excessive and could suggest overnutrition or metabolic issuesif unaccompanied by proportionate linear growth.
Take home points
- Expected weight gain: Double by 6 months, triple by 12 months.
- Significant deviations may indicate nutrition-related or health concerns.
- Nurses should use growth charts to track weight percentiles and educate caregivers on feeding, portioning, and appropriate milestones.
- Regular well-child checks are vital for monitoring growth and development and detecting early signs of nutrient deficiency or excess.
A student explains to an instructor that the infant period is categorized as the “oral phase” according to Freud’s theory. Which statements by the student suggest an understanding of this phase? Select all that apply
Explanation
Freud’spsychosexual theory of developmentis a foundational framework in psychology that suggests personality develops through a series of childhood stages, each focused on a different erogenous zone. According to Freud, how a child navigates these stages determines aspects of their adult personality.
Rationale for correct answers:
A.Freud’s oral stage(birth to ~18 months) is centered around the mouth as the primary source of pleasure and interaction. Infants suck not only for nourishmentbut also for comfort and gratification. This is why they seek pacifiers, thumb-sucking, and frequent feeding, even when not hungry.
E.Mouthingis a major way infants explore their environment, helping them learn about texture, shape, and taste. This aligns with Freud’s belief that the mouth is the center of pleasurein this stage.
Rationale for incorrect answers:
B.This contradicts Freud’s theory. Suckingis pleasurableeven outside feeding, which is why pacifiers or thumb-sucking soothe infants.
C.While breastfeeding may foster bonding and skin-to-skin contact, Freud’s theory is not about energy expenditure. The source of pleasure is oral stimulation, not how much effort it takes.
D.According to Freud, pacifiersare a classic example of how infants seek oral gratification for pleasure beyond nutrition.
F.An infant beginning to explore the genital area to learn sexual identity is part of Freud’s phallic stage, which occurs around ages 3–6 years, not in infancy.
Take home points
- Freud’s oral stage emphasizes that infants derive pleasure and comfort through sucking and mouthing.
- Oral gratification is crucial for both emotional development and ensuring consistent nutrient intake through feeding.
- Nurses should support appropriate oral behaviors and reassure caregivers that habits like thumb-sucking or mouthing are developmentally normal in infancy.
An 8-month-old baby girl, who is developing appropriately, is admitted to a pediatric unit for respiratory syncytial virus (RSV). The baby is crying and being held by her mother. A nurse wants to provide appropriate care based on Erikson’s developmental stages. In which stage is this baby, according to Erikson’s theory?
Explanation
Erik Erikson’s theory of psychosocial developmentis a framework that explains how people evolve emotionally and socially across their lifespan. He proposed that human development unfolds in eight distinct stages, each marked by a central conflict that must be resolved for healthy psychological growth.
Rationale for correct answer:
D.According to Erikson’s psychosocial theory, the first stage, “Trust vs. Mistrust” occurs from birth to approximately 18 months. During this period, infants learn to trust their caregivers to meet basic needs such as feeding, comfort, and emotional security. A child like this 8-month-old, when sick and in a strange environment, relies even more heavily on a trusted caregiver(in this case, the mother) for comfort.
Rationale for incorrect answers:
A.Punishment versus obedience orientationis not an Erikson stage; it's a concept from Kohlberg’s theoryof moral development and applies to preschool and school-aged children, not infants.
B.Oral stageis part of Freud’s theory, not Erikson’s. While related to infancy, it is not the correct framework for answering a question on Erikson’s stages.
C.Initiative versus guiltstage occurs in preschool-aged children(around 3–6 years old). It focuses on exploring the environment, initiating activities, and developing purpose—not relevant for an 8-month-old.
Take home points
- Erikson’s “Trust vs. Mistrust” stage spans from birth to 18 months.
- Infants develop trust when caregivers respond consistently and lovingly to their needs, especially during illness or stress.
- Nurses should support parent-infant bonding during hospitalization to reinforce emotional security and promote healing.
- Understanding developmental theory helps tailor age-appropriate nursing care in pediatric settings.
Practice Questions
A nurse at a clinic is preparing the immunizations for a 6-month-old baby. The mother says, “My baby is afraid of strangers and afraid of separating from me. My mother-in-law is upset and thinks I am
causing it.” Which response by the nurse is most appropriate?
Explanation
Separation anxietyis a normal and healthy developmental milestone that typically begins around 6 to 9 months of age. It is a natural emotional response to unfamiliar situations or people.
Rationale for correct answer:
C.Separation anxiety reflects the development of object permanence, the understanding that caregivers exist even when out of sight, a sign of a secure attachmentto the primary caregiver. This behavior should not be discouraged, and parents should be supported in responding with empathy and consistency.
Rationale for incorrect answers:
A.“Give your baby to strangers while you are present, so your baby gets used to strangers.”Forcing interaction with strangers can increase distress and erode trust. Instead, gradual exposurein a calm environment with caregiver support is more appropriate.
B.“Your mother-in-law is correct; you need to include her more in your baby’s needs.”This dismisses the mother’s valid observation of normal developmental behavior. The concern is about developmental appropriateness, not family involvement.
D.“Just let your baby cry for a while; your baby will get used to being separated from you.”Ignoring the baby’s distress may harm the secure attachment process and increase anxiety. Infants at this age need responsive caregiving to feel safe and supported.
Take home points
- Separation anxiety beginning around 6–9 months is a healthy sign of attachment and cognitive development.
- Nurses should validate caregiver concerns and provide developmentally appropriate guidance.
- Encouraging gentle exposure to new people and supportive separation routines helps build confidence and emotional resilience.
- Emotional security, like proper nutrition, is critical for a child’s overall growth and well-being.
Parents of an 8-month-old girl express concern that she cries when left with the babysitter. How does the nurse best explain this behavior?
Explanation
Cognitive developmentin children refers to how they acquire, organize, and use knowledge as they grow. It’s the unfolding of mental processes like thinking, learning, problem-solving, memory, and language. One of the most influential frameworks for understanding this is Jean Piaget’s theory, which outlines four major stages.
Rationale for correct answer:
C.Around 6 to 9 months, infants begin to understand object permanence, the concept that caregivers still exist even when out of sight. This cognitive development brings about separation anxiety, a normal developmental milestone. Crying when left with a caregiver does not signal trauma but rather reflects emotional attachment and growing awareness.
Rationale for incorrect answers:
A.“Crying when left with the sitter may indicate difficulty with building trust.”This misinterprets the behavior. The infant’s distress is not about lack of trust, but rather healthy attachment. Trust is actually forming through strong parent-child bonds.
B.“Stranger anxiety should not occur until toddler-hood; this concern should be investigated.”Stranger and separation anxietytypically emerge between 6 to 12 months, not toddlerhood. This statement suggests abnormality when the behavior is expected and age-appropriate.
D.“Perhaps the sitter doesn’t meet the infant’s needs; choose a different sitter.”While caregiver quality is always important, distress during separations at this age is common even with attentive sitters. Changing caregivers may not help and could even disrupt the development of consistent relationships.
Take home points
- Separation anxiety is normal around 8 months due to developmental milestones like object permanence.
- Crying during separation reflects a secure attachment, not mistrust or poor care.
- Nurses should reassure and educate caregivers, validating their concerns while explaining the normal course of emotional development.
- Encourage gentle routines and short separations to help infants adjust gradually.
A new graduate nurse is assessing an infant in the pediatric unit. An important milestone in the infant’s life is the development of object permanence. This milestone is represented by which of these statements?
Explanation
Developmental milestonesare age-specific tasks and behaviors most children can do within a certain age range. They guide parents and healthcare professionals in monitoring a child's development and identifyingpotential developmental delays. The milestones are categorized into different areas, such as motor skills, sensory development, language, and social skills.
Rationale for correct answer:
C. The infant turning and looking for the mother when she walks out of his viewdemonstrates object permanence, the understanding that people and objects continue to exist even when out of sight. This milestone typically begins to emerge around 6 to 8 months of ageand is a key component of cognitive development during the sensorimotor stageas described by Piaget.
Rationale for incorrect answers:
A. The infant smiling at the mother when she talks to himreflects social developmentand bonding, not object permanence. It shows recognition and responsiveness, usually emerging around 6 weeks of age.
B. The infant repeatedly flexing and extending his arms and legs when the mother picks him upindicates excitement or physical reactionto familiar handling, not a cognitive understanding of presence or absence.
D. The infant crying when the mother hands him to a babysitteris a sign of separation anxiety, which also develops around 6 to 9 months but is emotionally driven, not a direct measure of object permanence.
Take home points
- Object permanence is the ability to understand that people and things exist even when unseen.
- This milestone is typically observed when an infant looks for or searches for a hidden person or object.
- It is a key developmental step that reflects cognitive growth in the first year.
- Supportive communication helps parents recognize and value such milestones, fostering a sense of progress and connection.
A nurse is assessing an infant for attachment behavior with a parent. Which observations are important in assessing this relationship? Select all that apply
Explanation
Secure parent-infant attachmentinfluences feeding patterns and the infant’s emotional readiness to eat, both of which affect nutritional intake and growth. A strong attachment relationship ensures responsive feeding, reduces stress during meals, and supports healthy development.
Rationale for correct answers:
A.Physical closeness such as skin-to-skin, rocking, and gentle touchfosters emotional bonding and signals a secure attachment.
B.Cuddlingis a sign of nurturing and emotional connection. This physical closeness helps the infant feel safe, calm, and secure, which is key in attachment.
C.Observing how the parent soothes a crying or distressed baby reflects sensitivity and responsiveness, which are fundamental components of healthy attachment.
D.A parent who appears relaxed and confidentduring interactions is likely forming a positive attachment. Tension or avoidance may suggest bonding difficulties.
Rationale for incorrect answer:
E.Crying alone isnot a direct indicatorof attachment quality. All infants cry as a form of communication. What’s more important is how the caregiver respondsto the crying such as comforting, picking up, and soothing.
Take home points
- Healthy attachment behaviors include responsive touch, holding, eye contact, and soothing efforts.
- Nurses should assess not just the infant’s behavior, but also the parent’s sensitivity, consistency, and emotional presence.
- Strong attachment supports optimal nutrition, immune development, and emotional resilience.
- Early identification of bonding concerns allows for timely intervention and support, promoting better long-term outcomes for both infant and caregiver.
Practice Questions
The mother of a 3-month-old boy asks the nurse about starting solid foods. What is the most appropriate response by the nurse?
Explanation
Nutrient deficiencyrefers to inadequate intake or absorption of essential nutrients critical for healthy growth, immunity, and development.Infants rely heavily on breast milk or formula in the first months, and appropriate timing of solid food introduction helps meet evolving nutritional needs such as iron and zinc, and developmental milestones.
Rationale for correct answer:
D.The tongue extrusion reflex, which causes infants to push food out of their mouths with their tongue, typically fades between 4 to 6 months of age. Its disappearance signals readiness for spoon-feeding and oral motor coordination necessary for handling solids. This is why complementary feedingusually starts around 6 months, alongside continued breast/formula feeding.
Rationale for incorrect answers:
A.Solid foods should never be fed via a bottleas this increases the risk of choking and does not support oral motor development. At 3 months, the infant’s GI tract and neuromuscular maturity are not yet sufficient for solids.
B.Waiting until 12 monthsdelays key nutrientslike iron and zinc and misses a critical developmental window for introducing textures and preventing feeding difficulties.
C.Infants are not expected to handle a spoon themselves at 6 months.Rather, they begin to accept food from a spoon held by a caregiver when they demonstrate readiness signs such as disappearance of tongue thrust, good head control, and interest in food.
Take home points
- Solid foods are typically introduced around 6 months when the tongue thrust reflex disappears.
- Feeding solids with a spoon, not a bottle, is essential for safety and development.
- Early introduction (before 4 months) or late introduction (after 6–7 months) may pose nutritional and developmental risks.
- Nurses should guide parents using evidence-based recommendations and assess developmental readiness, not just age.
The nurse is providing anticipatory guidance to the mother of a 6-month-old infant. What is the best instruction by the nurse in relation to the infant’s oral health?
Explanation
Oral healthis tightly connected to nutrition. Poor oral hygiene can lead to early childhood caries, which may affect an infant’s ability to eat comfortably and get adequate nutrients. Starting oral hygiene early promotes healthy feeding and supports lifelong dental habits.
Rationale for correct answer:
C.The best practiceis to begin oral hygiene before teeth eruptby cleaning the gums with a soft, damp washcloth. Once teeth emerge (typically around 6 months), continue cleaning with a washcloth or soft infant toothbrush without toothpaste. This practice reduces bacterial growth and helps the infant get used to oral care routines.
Rationale for incorrect answers:
A.Oral care should begin before tooth eruption, not after full dentition. Delaying increases risk of early childhood caries.
B.Infantsshould not use toothpasteuntil at least age 12–18 months, and even then, only a rice-grain amountof fluoride toothpaste under supervision. Toothpaste is not neededfor early oral cleaning.
D.Rinsingis not necessary and may pose a choking hazardin young infants. Instead, cleaning with a washcloth is safer and more effective for removing milk residue and bacteria.
Take home points
- Begin oral care before teeth erupt using a damp washcloth to clean gums.
- Continue daily cleaning as new teeth come in to promote healthy oral development.
- Avoid toothpaste in infants under 12 months unless directed by a dentist.
- Early oral hygiene helps prevent nutritional disruptions due to dental discomfort or caries and builds lifelong habits.
A 9-month-old infant’s mother is questioning why cow’s milk is not recommended in the first year of life as it is much cheaper than formula. What rationale does the nurse include in her response?
Explanation
Infants are especially vulnerable to iron deficiency, which can impair cognitive, motor, and immune development. Exclusive cow’s milk before 12 months increases the risk of nutritional deficiencies, especially iron-deficiency anemia, due to poor iron content and its interference with iron absorption.
Rationale for correct answer:
B.Cow’s milk should not be introduced before 12 monthsbecause it is low in ironand can cause microscopic gastrointestinal bleeding, further increasing iron loss. It contains high levels of protein, sodium, and potassium, which can strain the immature kidneys of an infant. It lacks essential nutrients like vitamin E and essential fatty acids found in breast milk or formula.
Rationale for incorrect answers:
A.Even at 9 months, the infant’s GI system and kidneys are still immature. Substituting cow’s milk too early increases the risk of iron-deficiency anemiaand other nutrient imbalances.
C.While whole milk is appropriate after 12 months, it is still not safe before 1 year, regardless of fat content, due to the nutrient profile and iron-related concerns.
D.Diluting formula can lead to water intoxication, hyponatremia, and malnutrition. Nurses must offer safe, supportive alternativeslike referral to nutrition assistance programs rather than endorsing harmful practices.
Take home points
- Do not introduce cow’s milk before 12 months due to its poor iron content and potential to cause anemia.
- Formula or breast milk should remain the infant’s primary milk source until age 1.
- Diluting formula is unsafe and should be discouraged.
- Nurses should educate compassionately and connect families with resources for affordable infant nutrition.
The parent of a 10-month-old is being interviewed by the nurse preceding an examination by the pediatric nurse practitioner and states, “My baby loves all kinds of food, and he always drinks his milk from a sippy cup, except in the evening when he wants a bottle.” Which of the following follow-up questions is most important for the nurse to ask?
Explanation
Introducing cow’s milk before 12 monthscan lead to iron-deficiency anemia, as cow’s milk is low in iron, can irritate the gastrointestinal lining, and may interfere with iron absorption. Early introduction also displaces nutrient-dense breast milk or formula, increasing the risk of nutrient deficiencies during a critical growth phase.
Rationale for correct answer:
B.This question directly addresses the most immediate nutritional risk. At 10 months, infants should not yet be consuming cow’s milkas a primary milk source. The nurse must clarify what type of milk the infant is drinking to ensure it is breast milk or iron-fortified formulaand prevent nutrient imbalances, especially iron deficiency.
Rationale for incorrect answers:
A.While bottle weaning is important to prevent dental cariesand promote independence, it is not as urgent as assessing for the risk of early cow’s milk introduction.
C.While asking about fruits and vegetables the child has been fedis relevant to dietary variety, this does not address the primary safety concern about inappropriate milk intake and its impact on iron status.
D.Self-feedingsupports motor development and autonomy, but again, this is secondary to the need to verify the type of milk consumed.
Take home points
- Cow’s milk should not be introduced before 12 months due to the risk of iron-deficiency anemia and poor nutrient content for infants.
- Iron-fortified formula or breast milk should remain the primary milk source until the first birthday.
- Nurses must assess feeding practices carefully to ensure safe transitions in infant nutrition.
- Prompt, respectful caregiver education is key to preventing avoidable nutritional risks in the first year of life.
A mother brings her 5-month-old to the clinic for a well-child appointment. A nurse is doing an assessment when the mother asks when she can give her baby solid foods. What response is most appropriate?
Explanation
The timely and safe introduction of solid foods is crucial for preventing nutrient deficiencies, particularly iron and zinc, which breast milk alone may not sufficiently provide after 6 months. Delayed or premature introduction can result in malnutrition, feeding difficulties, or gastrointestinal distress.
Rationale for correct answer:
A.The nurse’s role includes assessing readiness cuesbefore advising on introducing solids. Key developmental signs of readiness include sitting with minimal support, good head and neck control, decreased tongue thrust reflex, and showing interest in food. These indicators typically appear around 4–6 months, and confirming them ensures the infant can safely manage solid foods.
Rationale for incorrect answers:
B.While the mother's observations are important, readiness should be based on developmental milestones, not feelings or assumptions alone.
C.Increased hunger may signal a growth spurt, not necessarily readiness for solids. Hunger aloneis not a reliable indicator of readiness for spoon-feeding or managing textures.
D.While collaboration with the provider is essential, the nurse is qualifiedto assess developmental readiness and provide anticipatory guidance about solid food introduction as part of routine well-child care.
Take home points
- Solid foods are typically introduced at around 6 months, but only when developmental readiness is confirmed.
- Signs of readiness include: sitting with support, decreased tongue thrust, good head control, and interest in food.
- Introducing solids too early can increase choking risk, while delaying beyond 6 months may lead to nutrient deficiencies.
- Nurses play a key role in educating caregivers and promoting safe, timely feeding transitions.
A 6-month-old child received the following play things as a gift from a relative. The nurse should advise the parents that which of the items is potentially dangerous for the child to play with?
Explanation
Developmental aids in childrenare tools, resources, or strategiesdesigned to support and enhance a child's growth and developmentacross various domains such as physical, cognitive, emotional, social, language, and motor skills. These aids can be used at home, in schools, or by healthcare professionals such as pediatricians, occupational therapists to help children reach age-appropriate developmental milestones.
Rationale for correct answer:
B. Balloonsare choking hazards, especially for infants and young toddlers. If a balloon pops or is accidentally inhaled, it can block the airway and cause suffocation. Latex balloons are especially dangerous, as they conform to the airway and are difficult to remove during choking emergencies. The American Academy of Pediatrics warns against giving balloons to children under 8 years old.
Rationale for incorrect answers:
A. While stuffed animalsshould be free of small parts like button eyes and long strings, a soft stuffed animal is generally safe for a 6-month-old, especially under supervision.
C. As long as the toy cell phoneage-appropriate with no detachable small parts or batteries accessible to the child, toy phones encourage imitation and sensory play and are generally safe for infants.
D. Shape sorteris a common, safe toy for older infants that promotes fine motor skills and cognitive development. As long as the pieces are too large to swallow, it’s appropriate for a 6-month-old.
Take home points
- Balloons are a major choking hazard and should be avoided for infants and young children.
- Choose toys that are age-appropriate, durable, and free of small parts or sharp edges.
- Educate parents calmly and supportively about toy safety, especially around choking risks.
Safe play fosters development and strengthens parent-child interaction while minimizing injury risk.
Comprehensive Questions
A nurse is caring for a 1-month-old whose mother states that she is curious as to whether her infant is developing normally. Which of the following developmental milestones would the nurse inform the mother that the infant is expected to perform at this age?
Explanation
Developmental milestonesare age-specific tasks and behaviors most children can do within a certain age range. They guide parents and healthcare professionals in monitoring a child's development and identifyingpotential developmental delays. The milestones are categorized into different areas, such as motor skills, sensory development, language, and social skills.
Rationale for correct answer:
C. At 1 month of age, infants typically demonstrate primitive reflexes and simple motor skills, such as turning their head side to sidewhen lying on their back or during tummy time. This is a normal and expected milestone reflecting early neuromuscular development.
Rationale for incorrect answers:
A. Rolling from back to fronttypically appears around 4 to 6 months. At 1 month, infants do not have the trunk and upper body strength required for rolling.
B. While a social smile may start to appear between 6 to 8 weeks, laughing out loud usually occurs closer to 3 to 4 months. A 1-month-old may exhibit reflexive smiles but not genuine social or vocal expressions of joy.
D. Holding a rattle for ten secondsindicates purposeful grasping which typically begins around 3 to 4 months. At 1 month, a baby may grasp reflexively, but cannot hold objects for extended periods or with intention.
Take home points
- A 1-month-old is expected to turn their head from side to side, especially during tummy time.
- Smiling and purposeful grasping are still emerging at this age; rolling and laughing come later.
- Understanding age-appropriate milestones helps reassure caregivers and guide anticipatory guidance.
- Nurses should use calm, supportive communication when educating caregivers about normal development.
An 8-month-old is seen in the well-child clinic. Which of the following behaviors would the nurse expect to see? Select all that apply
Explanation
Developmental milestonesare age-specific tasks and behaviors most children can do within a certain age range. They guide parents and healthcare professionals in monitoring a child's development and identifyingpotential developmental delays. The milestones are categorized into different areas, such as motor skills, sensory development, language, and social skills.
Rationale for correct answers:
A. At 8 months, infants begin to demonstrate object permanence, a key cognitive milestone. Peek-a-boois a classic behavior indicating the baby understands that objects and people still exist even when out of sight.
E. Transferring objects from hand to handis a fine motor skill typically develops between 6 and 8 months. It reflects improved coordination and bilateral hand use, and is an expected milestone for an 8-month-old.
Rationale for incorrect answers:
B. Independent walkingtypically emerges between 12 and 15 months. At 8 months, a baby may pull to stand or cruise while holding furniture but is not expected to walk alone.
C. Feeding self with a spoonrequires more advanced coordination and typically develops around 15 to 18 months. At 8 months, infants may begin finger feeding but cannot use utensils effectively.
D. Stacking two blocks into a toweris a milestone usually achieved between 15 and 18 months. An 8-month-old may bang toys together but lacks the precision to stack blocks purposefully.
Take home points:
- At 8 months, expect skills like playing peek-a-boo and transferring objects between hands.
- Walking, using utensils, and block stacking are later milestones in toddlerhood.
- Use therapeutic communication to reassure parents that each child develops at their own pace within expected ranges.
- Focusing on what is developmentally normal now prevents unrealistic expectations and supports healthy parenting confidence.
A nurse is educating a parent regarding the immunizations that a child is to receive during the first year of life. Which of the following immunizations did the nurse discuss?
Explanation
Vaccines are biological tools designed to train your immune system to recognize and defend against harmful pathogens, like viruses or bacteria without causing the actual disease. They usually contain weakened or inactivated formsof the virus or bacteria, toxoids(inactivated toxins) produced by bacteria or mRNA or subunit particlesthat trigger an immune response
Rationale for correct answer:
D.The inactivated poliovirus vaccine (IPV)is part of the routine immunization schedule in the first year of life. Doses are typically given at 2 months, 4 months, and 6–18 months of age.It protects against poliomyelitis, a serious viral infection that can cause paralysis.
Rationale for incorrect answers:
A. The MMR (measles, mumps, rubella)vaccine, is not administered during the first year. The first dose of MMR is given at 12–15 monthsof age, per CDC guidelines, because maternal antibodies may interfere with vaccine effectiveness if given earlier.
B. The MMR (measles, mumps, rubella)vaccine, is not administered during the first year. The first dose of MMR is given at 12–15 monthsof age, per CDC guidelines, because maternal antibodies may interfere with vaccine effectiveness if given earlier.
C. The MMR (measles, mumps, rubella)vaccine, is not administered during the first year. The first dose of MMR is given at 12–15 monthsof age, per CDC guidelines, because maternal antibodies may interfere with vaccine effectiveness if given earlier.
Take home points
- Polio vaccine is part of the first-year immunization schedule, typically at 2, 4, and 6 months.
- MMR (measles, mumps, rubella) is not given until after the first year (12–15 months).
- Nurses should use calm, supportive language to explain vaccine timing and importance.
- Accurate vaccine education helps reduce hesitancy and strengthens caregiver confidence in health decisions.
A nurse is educating a parent regarding the psychosocial stage of development of the infancy period. Which of the following information did the nurse include in the discussion?
Explanation
The psychosocial stage of developmentrefers to a concept from Erik Erikson's theory of psychosocial development, which outlines eight distinct stagesthat an individual passes through over their lifespan. Each stage involves a psychosocial conflictthat must be resolved for healthy psychological and social development.
Rationale for correct answer:
A. According to Erik Erikson’s psychosocial theory, the infancy stage(birth to 1 year) centers on Trust vs. Mistrust. Infants develop trust when caregivers consistently respond to their needs with warmth and prompt attention. This creates a secure foundation for emotional and social development.
Rationale for incorrect answers:
B. Ignoring a crying infant, especially in the early months, may hinder the development of trust and emotional security. Infants lack self-soothing skills and require caregiver comfort to feel safe.
C. Infants do not have the cognitive capacity to understand cause and effect or “bad behavior.” Scoldingcan be confusing and emotionally harmful at this stage.
D. Sneaking awaycan increase separation anxiety. Infants may develop mistrust if caregivers disappear without warning. Gradual transitions and brief, loving goodbyes help foster security.
Take home points:
- The key psychosocial task in infancy is developing trust through consistent, loving care.
- Timely responses to infant needs promote emotional security.
- Avoid practices like sneaking away or scolding, which can undermine trust.
- Therapeutic education should reassure and guide caregivers in building strong emotional bonds with their infants.
The nurse is visiting the home pictured below. A 6-month-old child lives in the home. Please select the image in the picture that the nurse should inform the parents presents a potential danger to the child. (HOT SPOT- THE LABELED POINTS SHOULD BE HIGHLIGHTABLE)
Explanation
Correct answer: Point A (The electrical cord hanging from the table)
Infants are naturally curiousbut lack the ability to recognize danger. As they begin to roll, crawl, and explore, homes must be carefully baby-proofed to prevent accidents and injuries. Common household hazards include choking hazards, suffocation and strangulation risks, falls, burns and scalds, poisoning, electrical hazards, sharp objects, and drowning risks.
Rationale:
Once babies develop the ability to grasp objects, they explore their environment by grasping and playing with items within their reach. If the child were placed near the table, he or she could grasp the electrical cord and attempt to chew it or to pull downon the cord and topple the lamp. Babies do not understand the potential dangers that cords present.
Take home points
- Electrical Hazards for infants include:
- Uncovered electrical outlets
- Loose wires or cords within reach
- Appliances left plugged in and accessible
A mother visits her child’s primary health-care provider for the child’s 12-month visit. The child
weighed 2,800 grams at birth. Which of the following weights is most consistent with the expected weight for this child?
Explanation
Weight gain in childrenrefers to the normal increase in body weightas a child grows and develops. It is an essential indicator of health, nutrition, and overall development. Appropriate weight gain varies by age, sex, genetic potential, and health status.
Rationale for correct answer:
C. 8,500 grams: By 12 months of age, an infant's weight is expected to be approximately three times their birth weight. Birth weight: 2,800 grams; expected 12-month weight: 2,800 × 3 = 8,400 grams. A weight of 8,500 grams is most consistent with this milestone, showing normal and healthy growth.
Rationale for incorrect answers:
A. 7,500 gramsis below the expected tripling of birth weight. It could indicate inadequate weight gainand may warrant further evaluation of the infant's nutrition and health.
B. 8,000 gramsis closer to the expected range but still slightly below the ideal target (8,400 g). It may be acceptable for some infants but is not the best match compared to 8,500 grams.
D. While 9,000 gramsmay still be within a healthy range, it is slightly above the typical tripled weight. Though not concerning, 8,500 g is closer to the expected average.
Take home points
- At 12 months, infants are expected to triple their birth weight.
- For a birth weight of 2,800 g, the expected 12-month weight is about 8,400 g.
- 8,500 grams best aligns with this developmental milestone.
- Use therapeutic communication to explain growth expectations while respecting individual variations and promoting confidence in parenting.
A mother of an 8-month-old boy states that the family is vacationing in a beach house for the next 2 weeks. Which of the following information should the nurse educate the mother about in relation to sun exposure? Select all that apply
Explanation
Sun exposurerefers to the amount of time a child’s skin is exposed to ultraviolet (UV) rays from the sun. While some sunlight is beneficial by helping the body produce vitamin D, it also carries risks, especially for children, whose skin is more delicate and sensitivethan adults.
Rationale for correct answers:
B. Broad-spectrum sunscreenoffers protection from both types of harmful ultraviolet radiation. UVA contributes to skin aging, while UVB causes sunburn. For infants over 6 months, using a broad-spectrum, SPF 30 or highersunscreen on exposed skin is recommended.
C. UV rays can damage the eyes. Sunglassesthat block 100% of UVA and UVBrays help protect the infant’s developing eyes from long-term harm like cataracts or retinal damage.
E. Lightweight, long-sleeved shirts and pantsoffer effective physical protection from the sun. A wide-brimmed hatalso helps shield the face and neck.
Rationale for incorrect answers:
A. Sunscreen should be reapplied every 2 hoursor more frequently if the child is sweating or in water, even if the sunscreen is labeled as “water-resistant.” Waiting 4–6 hours between applications is insufficient.
D. The most intense sun exposureoccurs between 10 a.m. and 4 p.m., not just 12–2 p.m. During these hours, children should be kept in the shade, wear protective clothing, and have sunscreen applied to exposed areas.
Take home points
- Infants over 6 months should use broad-spectrum sunscreen and wear protective clothing and sunglasses.
- Reapply sunscreen every 2 hours or after swimming/sweating.
- Avoid sun exposure between 10 a.m. and 4 p.m., not just midday.
- Therapeutic teaching should empower caregivers to enjoy outdoor activities safely, using clear, supportive communication.
The mother of an 11-month-old states, “My child has 8 teeth. I brush them every morning with bubble gum-flavored toothpaste. My child loves it.” Which of the following responses by the nurse is appropriate?
Explanation
Teeth care in childrenrefers to the practices, routines, and professional interventions used to maintain healthy teeth and gumsduring childhood. It plays a critical role in preventing cavities, gum disease, and other dental problems, while also supporting proper speech, nutrition, and self-esteem.
Rationale for correct answer:
D.For children under 2 years of age, it is recommended to avoid toothpaste containing fluorideunless advised by a dentist. Fluoride ingestion at this age can lead to fluorosis, a condition that causes permanent changes in the appearance of tooth enamel. The nurse should commend the mother for brushing but gently advise using a soft brush with water only, or, if using toothpaste, to use only a tiny smear (grain of rice-sized)and ensure the child does not swallow it.
Rationale for incorrect answers:
A.While brushing is encouraged, using regular toothpaste, especially in a flavor that might encourage swallowing, is not appropriate for infants under 2 unless fluoride-free and used cautiously. This response overlooks the risk of fluoride ingestion.
B.This response misleads the parent into thinking toothpaste is essential for cavity prevention at this age, which it is not. Tooth brushing itselfis the most important factor; fluoride use is age-dependent and requires caution.
C.This is a judgmental and inappropriate comment. Describing a child as being “spoiled”does not reflect therapeutic communication and can harm the caregiver’s confidence.
Take home points
- For children under 2 years, brush teeth with a soft toothbrush and water or a tiny smear of fluoride toothpaste only if recommended.
- Avoid flavored toothpaste that encourages swallowing in infants.
- Encourage and praise parents for brushing while offering gentle, evidence-based correction when needed.
- Supportive communication strengthens parent education and confidence in promoting good oral hygiene early.
A nurse is assessing a child in the well child clinic. In relation to developmental milestones, the infant can be expected to roll over from back to abdomen at approximately:
Explanation
Developmental milestonesare age-specific tasks and behaviors most children can do within a certain age range. They guide parents and healthcare professionals in monitoring a child's development and identifyingpotential developmental delays. The milestones are categorized into different areas, such as motor skills, sensory development, language, and social skills.
Rationale for correct answer:
C. Most infants can roll over from back to abdomen by around 6 months. This motor milestone reflects increased muscle strength and coordination. Rolling from abdomen to backtypically occurs earlier, around 4 months, while back to abdomentakes slightly longer due to the greater strength and control required.
Rationale for incorrect answers:
A. At 2 months of age, infants have limited head and neck controland cannot roll over. They may lift their heads briefly while prone but are not developmentally ready for rolling.
B. At 4 months, infants may roll from tummy to back, but rolling from back to abdomenis typically not achieved until closer to 6 months.
D. By 8 months, most infants have already mastered rolling and are developing more advanced motor skills, such as sitting without support and possibly crawling.
Take home points
- Rolling from back to abdomen is typically achieved around 6 months of age.
- Tummy to back rolling may occur earlier, around 4 months.
- Milestones vary slightly by child, but delayed motor skills may warrant further assessment.
- Nurses should provide age-appropriate guidance with reassurance to help caregivers support developmental progress confidently.
A nurse is educating a group of new graduate nurses on growth and development in children. The type of play in which infants engage is called:
Explanation
Developmental milestonesare age-specific tasks and behaviors most children can do within a certain age range. They guide parents and healthcare professionals in monitoring a child's development and identifyingpotential developmental delays. The milestones are categorized into different areas, such as motor skills, sensory development, language, and social skills.
Rationale for correct answer:
A. Infants engage in solitary play, which means they play alone, focusing on their own activities without interacting directly with other children. This is developmentally appropriate in infancy, as their social and cognitive skills are still developing.
Rationale for incorrect answers:
B. Parallelplayis common in toddlers (around 2–3 years old), where children play side by side but do not interact directly. It involves awareness of others but not shared play.
C. Associativeis typically seen in preschool-aged children (3–5 years). In associative play, children may share toys and talk but their play is not organized around a common goal.
D. Cooperativeplay emerges in school-age children. It involves organized, goal-directed activities where children play together with assigned roles or shared purposes.
Take home points
- Infants engage in solitary play, focusing on exploration and sensory stimulation.
- Each play type reflects a specific developmental stage and social capacity.
- Understanding these stages helps caregivers support age-appropriate play and avoid unrealistic expectations.
- Encouraging safe, stimulating environments supports healthy growth and development.
A mother questions the nurse regarding car seat safety for her infant. Which of the following information should the nurse include in the discussion?
Explanation
Car safety in childrenrefers to the use of appropriate restraints, practices, and equipmentto protect children from injury or death while riding in a motor vehicle. Because children's bodies are more vulnerable during collisions, special care is needed to ensure they are properly securedaccording to age, weight, and height.
Rationale for correct answer:
A. Placing the infant car seat rear facing in the back seat of the caris the safest position for infants and young toddlers. According to the American Academy of Pediatrics (AAP), children should ride rear-facing as long as possible, at least until 2 years of age or until they reach the highest weight or height allowed by their car seat manufacturer. The back seatis also the safest position in the vehicle.
Rationale for incorrect answers:
B. Moving the car seat to the forward-facing position when the child reaches 1 year of ageis an outdated advice. The AAP recommends delaying forward-facing until at least age 2, or longer if the child remains within the rear-facing seat’s height/weight limits.
C. While many infants use an infant “bucket” seat, transitioning to a rear-facing convertible seatis appropriate once the infant outgrows the bucket seat’s size limits, often before 12 months. Safety depends on fit and proper installation, not just age.
D. Tightening the straps of the seat so that only an adult fist fits under the strapsare too loose. Straps should be tight enough that no slack is present; you should be able to fit no more than one fingerbetween the harness and the child’s collarbone. The harness should lie flat and snugagainst the body.
Take home points
- Infants should always ride rear-facing in the back seat for as long as their seat allows.
- Delay switching to forward-facing until at least 2 years or when seat limits are exceeded.
- Ensure harness straps are flat and snug, with no slack.
- Therapeutic education empowers caregivers to make safe, informed decisions with confidence and care.
A nurse is caring for a 3-month-old infant. Based on the developmental age of the child, which motor skill should the nurse expect to see during an assessment?
Explanation
Developmental milestonesare age-specific tasks and behaviors most children can do within a certain age range. They guide parents and healthcare professionals in monitoring a child's development and identifyingpotential developmental delays. The milestones are categorized into different areas, such as motor skills, sensory development, language, and social skills.
Rationale for correct answer:
D.At 3 months, infants typically look at and play with their own hands and fingers, bring hands to the mouth, begin to show some head control, and may briefly hold a light object placed in their hand, but grasping is mostly reflexive. This behavior reflects early hand-eye coordinationand self-awareness, which are typical for this age.
Rationale for incorrect answers:
A.Banging objects held in hand typically appears around 7–8 months, when infants develop more purposeful control over objects and arm movement.
B.The pincer grasp(thumb and forefinger coordination) emerges around 9–10 months, not at 3 months.
C.While the palmar grasp reflexis present from birth, voluntary palmar graspingusually develops between 4–5 months. At 3 months, grasping is mostly involuntary or reflexive.
Take home points
- At 3 months, normal motor skills include playing with fingers, visual tracking, and bringing hands to the mouth.
- Pincer and palmar grasps develop later as fine motor skills mature.
- Monitoring motor milestones helps detect early nutritional or neurological concerns.
- Nurses should educate caregivers on typical developmental expectations and the importance of responsive interaction to promote sensory and motor development.
A nurse is educating a group of caregivers on nutrition among infants. An important nutritional supplement recommended to prevent rickets in infants who are exclusively breastfeeding is:
Explanation
Nutritional supplementation in childrenrefers to the addition of vitamins, minerals, or other nutrientsin the form of tablets, syrups, powders, or fortified foods, to a child’s diet to support optimal growth, development, and health. It is used when a child’s regular diet does not meet their nutritional needs due to various reasons such as poor intake, medical conditions, or increased nutritional demands.
Rationale for correct answer:
C. Infants who are exclusively breastfedare at risk for vitamin D deficiency, as breast milk alone does not provide adequate vitamin D. To prevent rickets, a bone-softening disease caused by vitamin D deficiency, the American Academy of Pediatrics recommends that all breastfed infantsreceive 400 IU of vitamin D daily, beginning within the first few days of life.
Rationale for incorrect answers:
A. While vitamin Ais important for vision and immune function, vitamin A deficiency is rare in infants who are breastfed, as breast milk contains sufficient levels.
B. Fluoridesupplementation is not needed in early infancy and is generally considered starting after 6 months, depending on the fluoride content of local water suppliesand dental risk.
D. Folic acidis critical during pregnancy to prevent neural tube defects. It is not a primary supplement needed for breastfed infants after birth.
Take home points:
- Vitamin D supplementation (400 IU daily) is essential for breastfed infants to prevent rickets.
- Begin vitamin D within the first few days of life and continue throughout breastfeeding.
- Breast milk is optimal for nutrition but lacks adequate vitamin D, necessitating this supplement.
- Clear, supportive education helps caregivers feel confident in meeting their infant’s nutritional needs.
A 4-month-old infant is brought to the well-child clinic for immunizations. The mother indicates that the infant often strains to have a bowel movement, so she has been giving him honey and has stopped feeding him iron-fortified formula, based on her sister’s recommendations. The nurse recognizes that the infant is at risk for the development of which of the following? Select all that apply
Explanation
Nutrient deficiency in childrenrefers to a lack or insufficient intake or absorptionof essential nutrients such as vitamins and minerals required for growth, development, immunity, and overall health. It can result from poor diet, illness, or increased nutritional needs during rapid growth phases.
Rationale for correct answers:
B. By discontinuing iron-fortified formula, the infant is at increased risk of iron deficiency, especially at 4 months when iron stores from birth begin to decline. Iron is essential for cognitive and physical development, and infants who don’t receive enough are at risk for anemia.
D. Honey should never be given to infants under 12 monthsdue to the risk of Clostridium botulinum spores, which can germinate in the immature gut and produce toxins. Even small amounts can lead to infant botulism which causes life-threatening muscle weakness and paralysis.
Rationale for incorrect answers:
A. There is no indication that the infant is consuming excess calories or gaining excess weight. The concern here is nutritional deficiency, not excess.
C. Ricketsis linked to vitamin D deficiency, not iron or honey. There's no mention of insufficient vitamin D or lack of sun exposure, so rickets is not the relevant risk in this case.
E. There is no evidence of cow’s milk introduction or symptoms of allergy such as rash, diarrhea, or vomiting. The infant is on formula (iron-fortified) and nothing suggests a reaction.
Take home points:
- Honey should never be given to infants under 12 months due to the risk of infant botulism.
- Iron-fortified formula is essential to prevent iron-deficiency anemia, especially after 4 months of age.
- When parents follow unsafe advice, use therapeutic, nonjudgmental education to build trust and correct practices.
- Always explore the why behind a caregiver’s decision to offer appropriate and respectful teaching.
A 10-month-old child reaches the 9- to 12-month developmental stage. Which nursing action is most appropriate for providing tactile stimulation for this child?
Explanation
Developmental milestonesare age-specific tasks and behaviors most children can do within a certain age range. They guide parents and healthcare professionals in monitoring a child's development and identifyingpotential developmental delays. The milestones are categorized into different areas, such as motor skills, sensory development, language, and social skills.
Rationale for correct answer:
D.At 9 to 12 months, children experience rapid sensory and motor development. They love to explore through touch, including during meals, are ready for finger foods and begin self-feeding, which enhances fine motor skills and sensory integration. Letting the child squash, smear, and mash foodpromotes tactile learning, encourages independence, and supports healthy eating behaviors.
Rationale for incorrect answers:
A.While gentle touch provides comfort, it is not sufficient tactile stimulation for this developmental stage. Older infants need active sensory engagementwith various textures.
B.Though helpful, a squeeze toy offers limited tactile variation. At this age, infants benefit more from interactive, hands-on experienceslike food play, water play, or textured objects.
C.Swaddlingis typically used for newbornsup to 2–3 monthsto promote sleep and reduce startle reflexes. At 10 months, swaddling may restrict movementand interfere with developmental exploration.
Take home points
- Tactile stimulation at 9–12 months should involve active exploration, especially with food, toys, and textures.
- Self-feeding is both a nutritional and developmental milestone, supporting independence and sensory integration.
- Nurses should guide caregivers to encourage safe, supervised sensory play to promote optimal development.
- Restrictive practices (like swaddling at this age) may hinder sensory and motor growth.
Exams on Growth And Development In Infants
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
-
Analyze the biologic milestones of infancy, including physical growth patterns and the maturation of organ systems.
-
Evaluate psychosocial development based on Erikson’s theory of Trust vs. Mistrust.
-
Identify cognitive milestones within Piaget’s sensorimotor phase, focusing on object permanence and cause-and-effect.
-
Assess the development of body image and gender identity as they begin to emerge in late infancy.
-
Interpret various infant temperaments and their influence on the parent-child relationship and "goodness of fit."
-
Formulate nursing interventions to assist parents in managing separation and stranger anxiety.
-
Educate caregivers on health promotion strategies, including infant nutrition, sleep hygiene, and dental care.
-
Prioritize injury prevention and immunization schedules to ensure infant safety and disease prevention.
Introduction
-
Infancy, spanning from birth to twelve months, represents the most rapid period of growth and development in the human lifespan.
-
For the pediatric nurse, understanding this stage is critical, as it sets the physiological and psychological foundation for all future health.
-
This period is characterized by a total dependence on caregivers, making the assessment of the family unit just as vital as the assessment of the infant.
-
Growth in infancy is not merely about an increase in size but is a complex orchestration of biologic maturation, where the brain, nervous system, and metabolic functions undergo profound shifts to support increasing autonomy.
-
Biologically, infants typically double their birth weight by six months and triple it by one year. However, nurses must look beyond the scale to observe psychosocial and cognitive markers.
-
According to Erikson, the primary task of infancy is the establishment of trust. When a nurse observes a parent responding to an infant's cry, they are witnessing the literal construction of a child’s worldview, that the world is a safe and predictable place.
-
Cognitively, the transition from simple reflexes to intentional movements, and eventually to the understanding that objects exist even when out of sight, marks the beginning of intellectual thought.
-
As the infant begins to recognize themselves as distinct from their mother, the early seeds of body image and gender identity are sown.
-
Socially, the infant moves from the reflexive "social smile" to complex interactions involving vocalizations and gestures. For the nurse, this stage is a window of opportunity to promote optimum development through anticipatory guidance.
-
By understanding the nuances of temperament and the stressors of teething or separation anxiety, the nurse acts as a bridge, helping parents navigate the intense demands of the first year while ensuring the infant’s safety and health are maintained through evidence-based interventions.
Promoting Optimum Growth And Development
1. Biologic development in infancy
- Infancy is a time of incredible change. Babies grow and develop at an astonishing rate. All their body systems are maturing, and they're constantly learning new skills to interact with the world around them.
Nursing insight: It's important to remember that physical and motor skill development happens in a predictable way: from head-to-toe (cephalocaudal) and from the center of the body to the periphery (proximodistal).
1.1. Proportional Changes: Growth Spurts and Milestones
Growth is super-fast, especially in the first six months.
- Weight Gain:
- For the first 5 months, infants gain about 680 grams (1.5 lbs) per month. By 5 months, their birth weight has at least doubled.
- A 6-month-old typically weighs around 7.26 kg (16 lbs).
- Weight gain slows down by half during the next 6 months.
- By their first birthday, an infant's birth weight has usually tripled, averaging around 9.75 kg (21.5 lbs).
- Breastfed babies often gain a bit less weight than formula-fed babies after 4 to 6 months, but their head circumference usually remains healthy.
- Height Increase:
- During the first 6 months, infants grow approximately 2.5 cm (1 inch) per month.
- This rate halves in the second 6 months.
- Growth in length tends to happen in sudden spurts, not a slow, steady increase.
- Average height: 65 cm (25.5 inches) at 6 months and 74 cm (29 inches) at 12 months.
- By 1 year, their birth length has increased by almost 50%. Most of this growth is in their trunk, which gives older infants their characteristic body shape.
- Head Growth:
- Rapid head growth is a key sign of brain development.
- From birth to 3 months: about 2 cm (0.75 inch) per month.
- From 4 to 6 months: about 1 cm (0.4 inch) per month.
- During the second 6 months: about 0.5 cm (0.2 inch) per month.
- Average head size: 43 cm (17 inches) at 6 months and 46 cm (18 inches) at 12 months.
- By 1 year, head size has increased by almost 33%.
Measuring Head Circumference

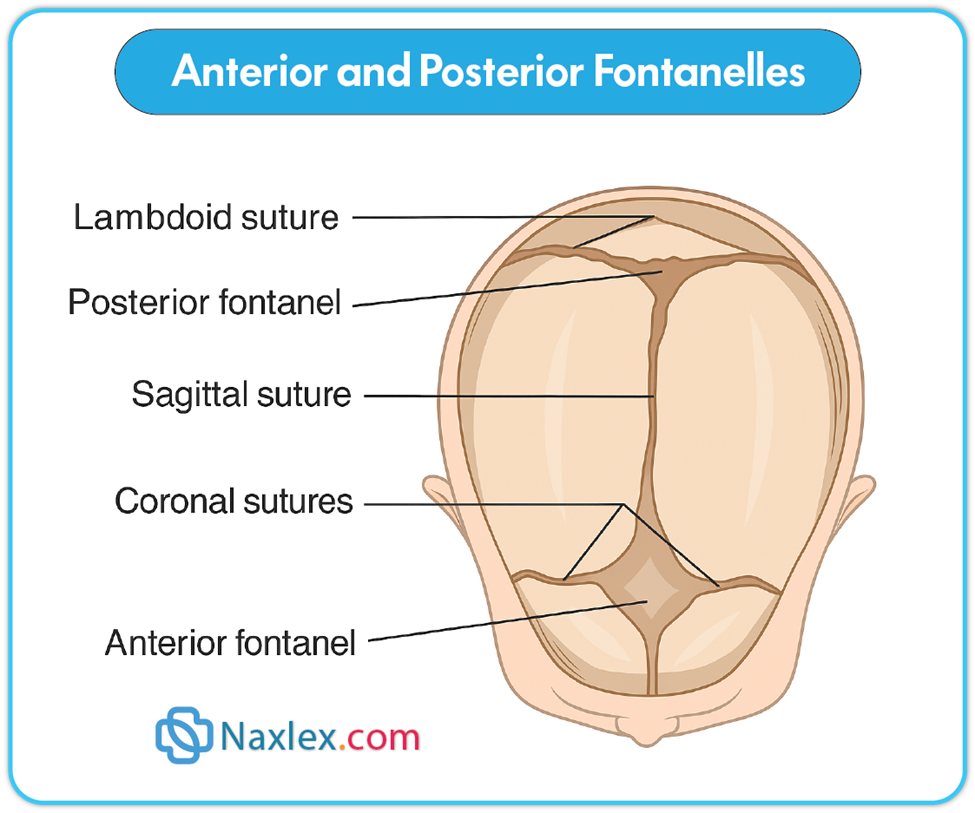
- Fontanel Closure:
- The anterior fontanel (soft spot on top of the head) typically closes between 12 to 18 months (average is 14 months).
- The posterior fontanel (soft spot at the back of the head) usually closes by 6 to 8 weeks.
Anterior and Posterior Fontanelles
Important Note: These are general guidelines. Factors like genetics, metabolism, environment, and nutrition heavily influence infant growth. Always use appropriate growth charts, such as the WHO growth charts (2006), to track an infant's individual growth, especially since these charts are based on healthy breastfed infants worldwide.
Brain Development: The expanding head size reflects the incredible growth of the nervous system. By the end of the first year, the brain has increased its weight by approximately 2.5 times. This brain maturation is what allows for the amazing developmental achievements you'll see in infants. Primitive reflexes disappear and are replaced by voluntary, purposeful movements, and new protective reflexes emerge.
Neurological Reflexes that Appear During Infancy
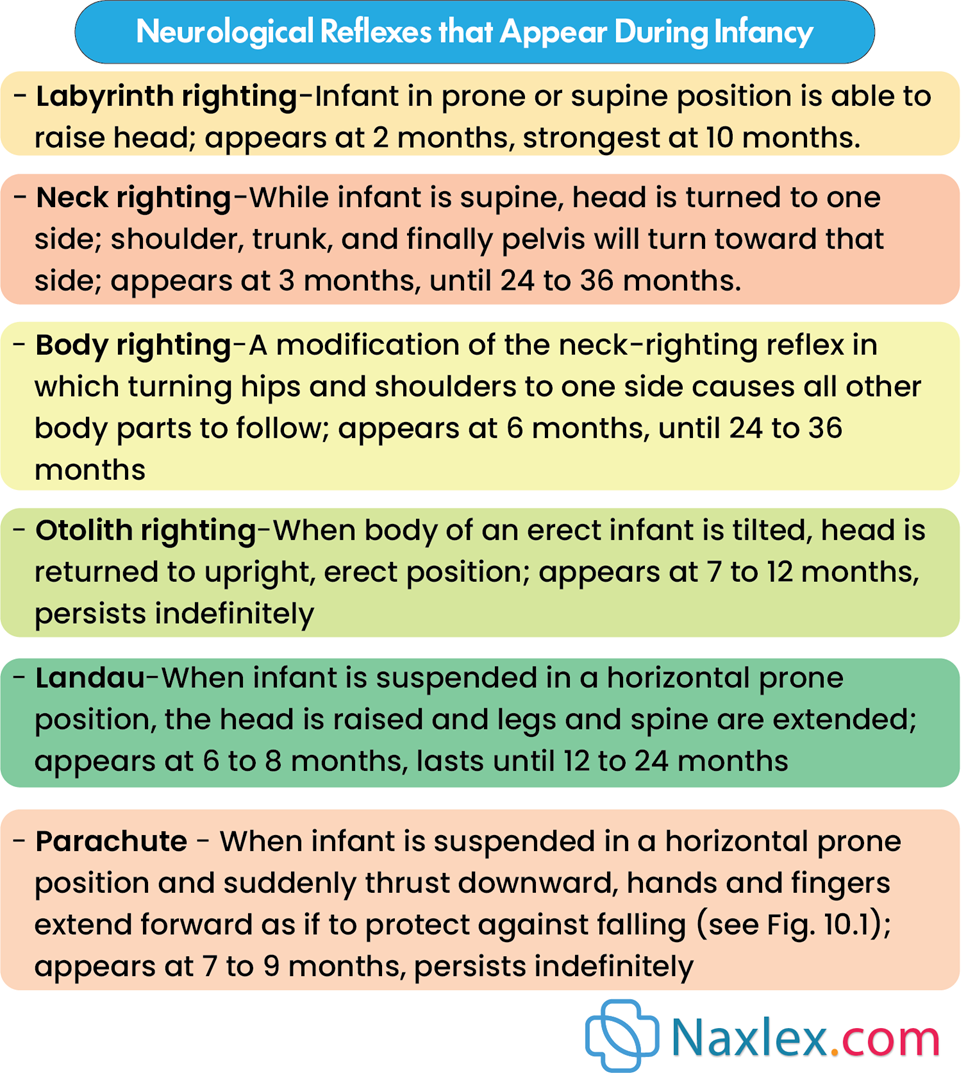
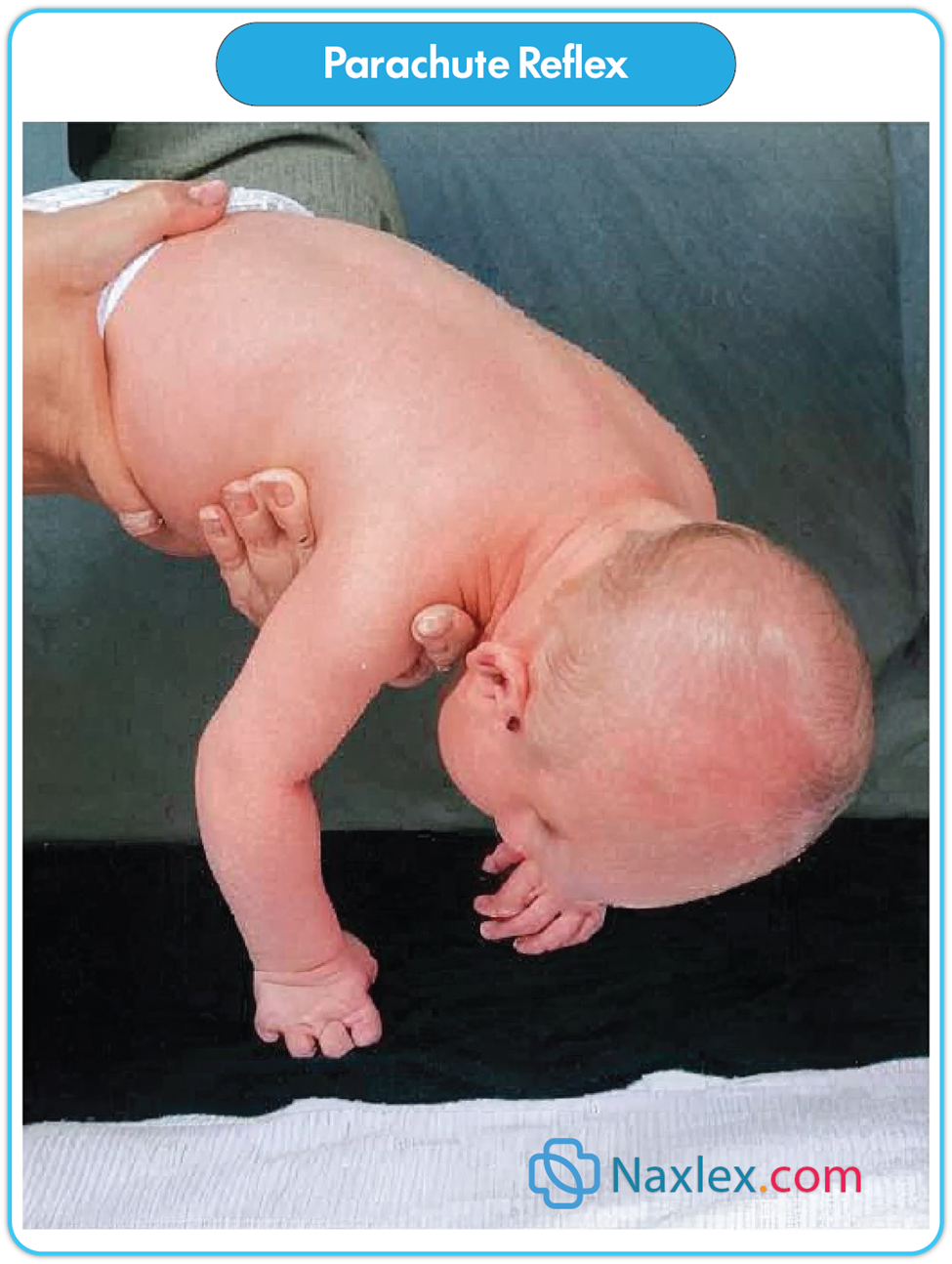
Parachute Reflex
Chest Growth: The chest starts to look more like an adult's, with the side-to-side measurement becoming larger than the front-to-back measurement. By the end of the first year, the chest circumference is roughly equal to the head circumference.
Heart Growth: While the body triples in weight, the heart only doubles in weight by 1 year. It's still quite large compared to the chest cavity, taking up about 55% of the chest width.
1.2.Sensory Changes: Seeing, Hearing, and Perceiving the World
Infants' senses are constantly developing, helping them understand their surroundings.
- Vision:
- Visual acuity (how clearly they see) gradually improves.
- Binocularity (the ability of both eyes to work together to form a single image) starts developing around 6 weeks and should be well-established by 4 months. If not, it can lead to strabismus (crossed eyes) and potential permanent vision problems if not caught early.
- Depth perception (stereopsis) begins to develop between 7 to 9 months, though it might appear earlier as a safety instinct.
- The parachute reflex (an arm extension when falling) appears around 7 months, which is a protective response.
- Visual Preferences: Infants prefer looking at human faces!
- At 6 weeks: More interested in a face with eyes.
- By 10 weeks: Prefer faces with both eyes and eyebrows.
- By 20 weeks: The mouth is also important for facial recognition.
- By 6 months: They start responding to facial expressions and can tell familiar faces from strangers, which is when separation anxiety often begins.
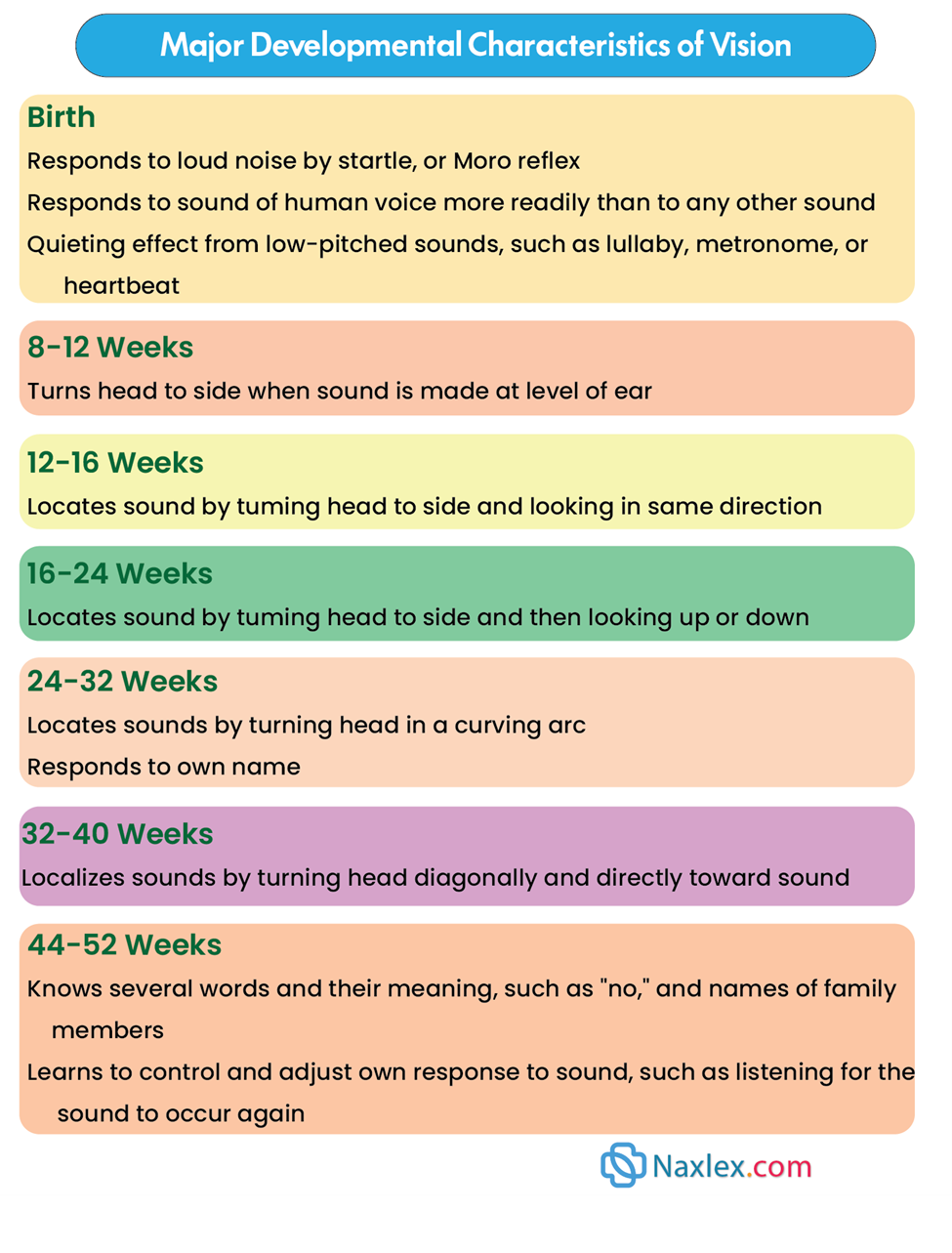
Major Developmental Characteristics of Vision
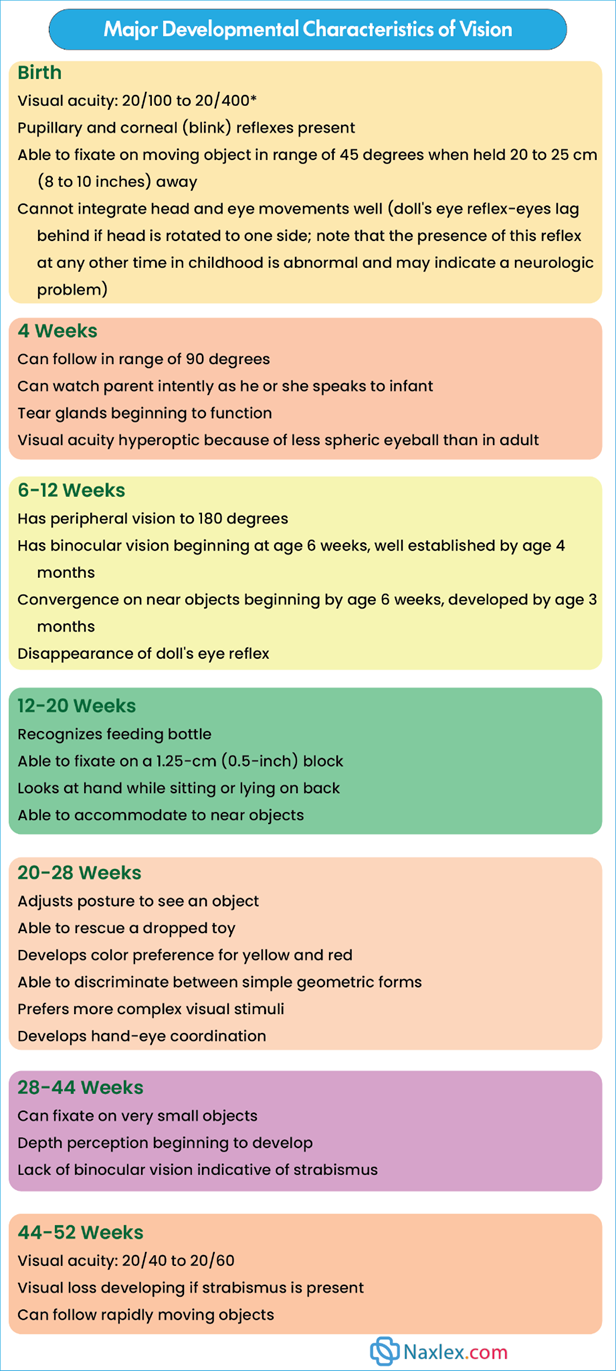
- Hearing: As the auditory pathway matures, infants go from a generalized response to sound to being able to precisely locate sounds.
Major Developmental Characteristics of Vision
1.3. Maturation of Organ Systems
Many other body systems undergo significant changes during infancy.
- Respiratory System:
- The respiratory rate slows down and becomes more stable, with breathing remaining mostly abdominal.
- Increased Risk for Respiratory Problems: Infants are more prone to severe respiratory infections because:
- Their trachea is close to the bronchi, allowing infections to spread quickly to the respiratory system and ears (due to the short, straight eustachian tube).
- Their immune system produces less IgA (an antibody that protects mucous membranes), offering less protection against infection.
- Their respiratory tract produces less mucus, which reduces humidification of inhaled air.
- The trachea and bronchi, though enlarging, remain small compared to lung size, leading to high resistance to airflow.
- Small airways are easily blocked by swelling, mucus, or foreign objects.
- Their flexible rib cage has less elastic recoil, making breathing harder during distress.
- They have a large "dead space" (air not involved in gas exchange), meaning they have to breathe twice as fast as adults to get enough oxygen.
- Cardiovascular System:
- Heart rate slows down as the infant grows, and it's common to see sinus arrhythmia (heart rate increases with inspiration, decreases with expiration).
- Blood pressure changes:
- Systolic pressure rises in the first 2 months as the left ventricle gets better at pumping blood.
- Diastolic pressure decreases for the first 3 months, then gradually rises back to near birth levels.
- BP can fluctuate with activity and emotions.
- Hematopoietic System (Blood):
- Fetal hemoglobin (HgbF) is present until about 5 months, gradually replaced by adult hemoglobin. HgbF has a shorter red blood cell (RBC) lifespan, leading to fewer RBCs.
- Physiologic Anemia: This often occurs between 3 to 6 months of age due to decreasing HgbF and its effect on erythropoietin production (a hormone that stimulates RBC production).
- Iron Stores: Maternal iron stores last about 5 to 6 months and then diminish, contributing to lower hemoglobin levels later in the first 6 months. While physiologic anemia isn't caused by a lack of iron, adequate iron is crucial when RBC production ramps up.
- Gastrointestinal System:
- Immaturity at Birth: Digestive processes are still developing. Breast milk helps compensate for limited digestive enzymes in the first few months.
- Enzymes:
- Amylase (for complex carbohydrates) is limited until about 4 to 6 months.
- Lipase (for fat digestion) is also limited, with adult levels of fat absorption not reached until 4 to 5 months.
- Trypsin (for protein breakdown) is present in sufficient amounts.
- Stomach Digestion: Relies on hydrochloric acid and rennin (which curdles milk, keeping it in the stomach longer for digestion).
- Intestinal Digestion: Pancreatic enzymes and bile in the duodenum break down protein and fat.
- Stool Appearance: Due to immature digestion, solid foods (like peas or carrots) may be seen undigested in the stool. Too much fiber can cause loose, bulky stools.
- Stomach Capacity: The stomach enlarges, allowing infants to tolerate more food. By the end of the first year, they can usually handle three meals a day, an evening bottle, and one or two bowel movements daily.
- Vulnerability: Infants are prone to diarrhea, vomiting, and dehydration with any gastric irritation.
- Liver: The liver is the most immature GI organ throughout infancy. While it can conjugate bilirubin and secrete bile after the first couple of weeks, functions like making glucose, plasma proteins, and ketones, storing vitamins, and breaking down amino acids remain relatively immature for the entire first year.
- Sucking, Swallowing, and Teeth: The development of these reflexes and the eruption of teeth prepare the infant for solid foods.
- Sucking: Can occur in the womb as early as 15-18 weeks gestation. Coordinated sucking, swallowing, and breathing patterns usually mature by 34-36 weeks.
- Nonnutritive sucking: For comfort.
- Nutritive sucking: For food intake.
- Suckling: Often used to describe breastfeeding.
- Infantile (Visceral) Swallow: Food sits in a groove on the tongue, and as the tongue presses up, milk flows down the sides of the mouth. Efficient for liquids, not solids.
- Mature (Somatic) Swallow: As the infant grows, the tongue becomes more mobile, orofacial muscles develop, and teeth erupt. The tongue stays behind the central incisors, and the jaw doesn't thrust forward. This allows for solid food consumption.
- Santmyer Swallow: A reflexive swallow when a puff of air is directed at the face. Can be useful for giving small amounts of fluids or meds, but use caution to prevent aspiration.
- Sucking: Can occur in the womb as early as 15-18 weeks gestation. Coordinated sucking, swallowing, and breathing patterns usually mature by 34-36 weeks.
- Immunologic System:
- Maternal Immunity: Full-term newborns get a lot of maternal immunoglobulin G (IgG), providing immunity for about 3 months against infections the mother was exposed to.
- Infant Immunity: IgG levels drop as maternal IgG breaks down, and the infant produces limited IgG. Infants reach only about 40% of adult IgG levels by 1 year, making them more susceptible to infections during the first 6 to 12 months.
- IgM: Significant amounts are produced at birth, but their ability to recognize specific pathogens is limited. Adult IgM levels are reached by 9 to 12 months.
- IgA, IgD, IgE: Production is much slower, reaching maximum levels in early childhood.
- Breast Milk Benefits: Breast milk contains prebiotic oligosaccharides that promote "good" bacteria (like bifidobacteria and lactobacilli), which stimulate the production of secretory IgA (sIgA). sIgA, abundant in colostrum, protects the GI tract's mucous membranes against many bacteria (like E. coli) and viruses (like rubella, poliovirus).
- Mucosa-Associated Lymphoid Tissue: Develops during infancy and helps prevent bacteria from crossing the mucosal barrier.
- Reduced Immune Factors: In early infancy, the function and quantity of T-lymphocytes, lymphokines, and other immune factors are reduced, affecting their response to some bacteria and viruses.
- Probiotics: May help establish healthy gut bacteria, preventing illnesses like antibiotic-induced diarrhea.
- Vernix Caseosa: The white, oily substance covering newborns has immune properties and helps maintain skin integrity.
- Integumentary System (Skin): The skin of a full-term infant matures during the first month, acting as a barrier to infection, helping with temperature regulation, and preventing water loss.
- Thermoregulation (Temperature Control): Becomes more efficient in infancy.
- The skin's ability to contract and muscles to shiver in response to cold increases.
- Peripheral capillaries adjust to temperature changes:
- Constrict in cold: Conserves core body temperature and reduces heat loss.
- Dilate in heat: Decreases internal body temperature through evaporation, conduction, and convection.
- Shivering (thermogenesis): Muscle contractions generate metabolic heat.
- Adipose tissue (fat): Increases in the first 6 months, providing insulation against heat loss.
- Fluid and Electrolyte Balance:
- High Body Water Content: At birth, 75% of an infant's body weight is water, and a significant portion is extracellular fluid (ECF).
- Dehydration Risk: The high proportion of ECF (blood plasma, interstitial fluid, lymph) makes infants prone to faster fluid loss and dehydration.
- The 5-10% weight loss in the first 5 days is due to ECF reduction, improved kidney function, and increasing glomerular filtration rate.
- Renal System (Kidneys):
- Immaturity: Kidney maturity isn't complete until the latter half of the second year. Filtration capacity is reduced before this time.
- Frequent Urination: Infants void frequently, and their urine has a low specific gravity (1.008 to 1.012).
- Urine Output:
- Newborns: Approximately 45 to 50 ml/kg/24 hr.
- As they grow: Increases to 60 to 80 ml/kg/24 hr.
- Insensible Water Loss: Radiant warmers, fever, and some phototherapy can cause low or no urine output in the first 24 hours. Infants should have at least 1 ml/kg/hr by the second day of life.
- Endocrine System:
- Adequate but Immature: The endocrine system is developed at birth, but its functions are immature. All endocrine organs are interconnected, so issues with one can affect others.
- Vulnerability to Imbalances: Due to functional deficiencies, infants are especially vulnerable to imbalances in fluid and electrolytes, glucose levels, and amino acid metabolism.
- Corticotropin (ACTH): Produced in limited quantities. Since the feedback between ACTH and the adrenal cortex is immature, infants have less tolerance for stressful conditions that affect fluid, electrolytes, and metabolism of fats, proteins, and carbohydrates.
- Insulin and Glucagon: Produced by the pancreas, but blood glucose levels tend to be unstable, especially under stress.
1.4. Fine Motor Development: The Skillful Hands
Fine motor skills involve the precise use of hands and fingers, especially for grasping.
- Early Grasping (Reflexive to Voluntary):
- 1-2 Months: Hands are mostly fisted (closed). Grasping is a reflex at this stage. If you put a rattle in their hand, they'll hold onto it.
- 3 Months: Hands are mostly open. Infants show an interest in grasping, often "grasping" with their eyes first, then their hands.
- 4 Months: Infants start looking from a small object to their hands and back again, showing increased hand-eye coordination.
- 5 Months: They can voluntarily grasp an object.
- Grasping Evolution (Whole Hand to Precision):
- Palmar Grasp: Initially, infants use their whole hand (like a rake) to grasp objects.
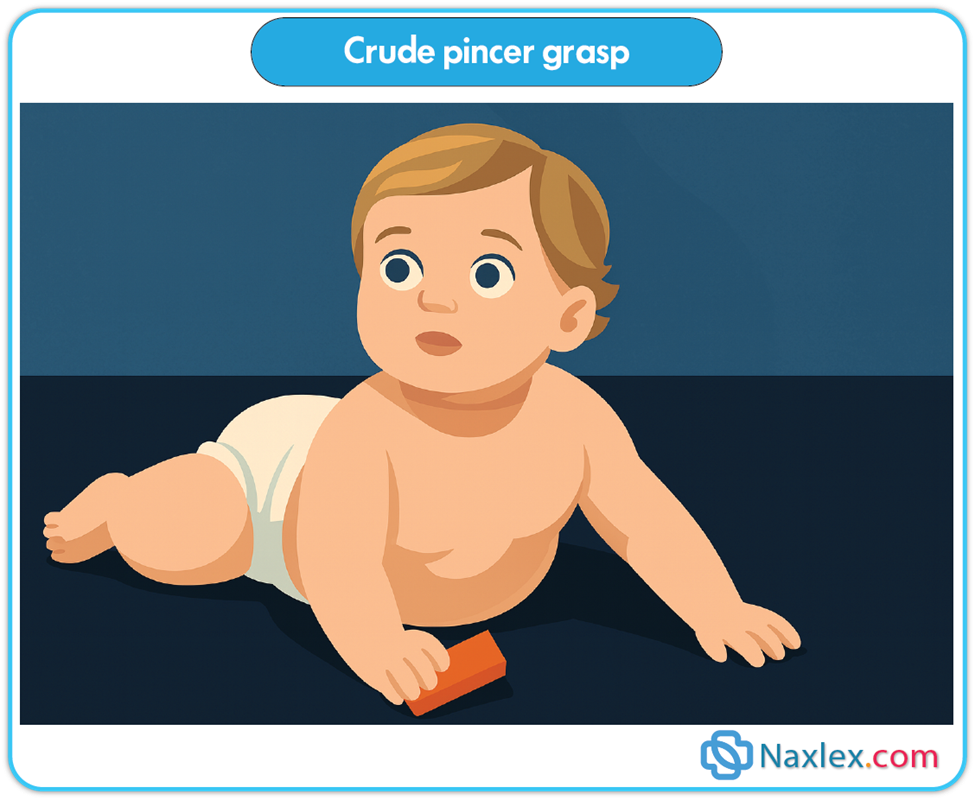
- 8-9 Months: Develop a crude pincer grasp (using the thumb and fingers, but not perfectly precise).
Crude pincer grasp
-
- 10 Months: The pincer grasp is well-established, allowing them to pick up small items like raisins or finger foods.
- 11 Months: Progress to a neat pincer grasp, with excellent thumb and index finger coordination.
Neat pincer grasp

- Increased Hand Skills:
- 6 Months: Much better at manipulating objects. They can hold their bottle, grab their feet and put them in their mouth, and feed themselves soft crackers.
- 7 Months: Can transfer objects from one hand to the other, use one hand to grasp, and hold a cube in each hand. They love to bang objects together and explore movable parts of toys.
- 10 Months: Can deliberately let go of an object and will offer it to someone.
- 11 Months: Enjoy putting objects into containers and taking them out.
- 1 Year: Will attempt to build a tower of two blocks but usually don't succeed yet.
1.5. Gross Motor Development: Movement and Mobility
Gross motor skills involve large muscle movements, like posture, head control, sitting, crawling, standing, and walking.
- Early Reflexes and Posture:
- Full-term newborns can briefly hold their head in midline when held vertically and can lift and turn their head side-to-side when on their tummy.
- Caution: Never place an infant prone on a soft surface like a pillow, as they lack the head control to lift their head out of a depression, risking suffocation.
- Righting Reflexes: These reflexes help with postural responses (flexion/extension) and enable activities like rolling, assuming a crawl position, and maintaining body alignment.
- Neck-righting reflex: Helps them roll from back to stomach (body turns with the head).
- Otolith and labyrinth-righting reflexes: Help them lift their head.
- Asymmetric Tonic Neck Reflex (ATNR): Present from birth to 3 months, this reflex actually prevents rolling over.
- Symmetric Tonic Neck Reflex (STNR): When the head/neck extend, arms extend, and legs bend (helps with crawling position). Due to strong leg flexor tone, infants might initially crawl backward before moving forward. This reflex fades as true crawling (with independent limb movement) develops.
- Head Control:
- Newborn: Marked head lag when pulled to sit. Can lift and turn head when prone, but only momentarily hold it in midline when suspended.
- 3 Months: Can hold their head up well, even beyond the plane of their body.
- 4 Months: Can lift their head and chest 90 degrees when on their tummy, bearing weight on their forearms. Only slight head lag when pulled to sit.
- 4-6 Months: Head control is well-established.
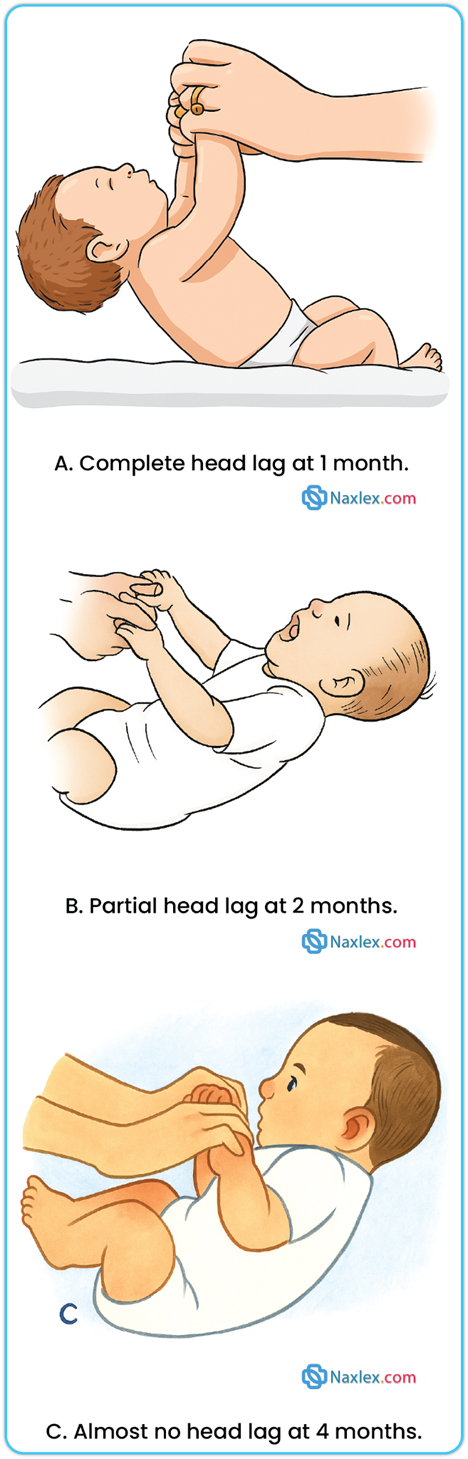
A. Complete head lag at 1 month. B. Partial head lag at 2 months. C. Almost no head lag at 4 months.
- Rolling Over:
- Infants often roll accidentally early on due to their rounded back.
- 5 Months: Can voluntarily roll from tummy to back.
- 6 Months: Can voluntarily roll from back to tummy.
- 7 Months: The parachute reflex appears, providing a protective response when falling.
- Sitting: Becoming Upright:
- First 2-3 Months: Back is uniformly rounded.
- 3-4 Months: Cervical (neck) curve forms as head control is established.
- 4 Months (approx.): Lumbar (lower back) curve appears as they begin to sit. Can be propped in a sitting position.
- 7 Months: Can sit alone, often leaning forward on their hands for support.
- 8 Months: Can sit unsupported very well and explore their surroundings from this position.
- 10 Months: Can maneuver from a tummy-lying position to a sitting position.
Nursing insight: If an infant isn't pulling to a standing position by 11-12 months, they should be evaluated for potential developmental hip dysplasia.
- Locomotion: Moving Around:
- 4-6 Months: Increasing arm coordination. Initial locomotion might involve propelling themselves backward by pushing with their arms.
- 6-7 Months: Can bear all their weight on their legs with assistance.
- 9 Months: Progress from crawling (belly on floor) to creeping (on hands and knees, belly off floor). At this age, they also stand while holding onto furniture and can pull themselves up to stand, but may struggle to get back down without falling.
- 11 Months: Walk while holding onto furniture (cruising) or with both hands held.
- 1 Year: May be able to walk with one hand held. Many infants take their first independent steps around their first birthday!
2. Psychosocial development: developing a sense of trust (Erik Erikson)
Erik Erikson's first stage of psychosocial development (birth to 1 year) focuses on the infant acquiring a sense of trust while overcoming mistrust.
- Core Concept of Trust: This is about infants learning that their needs for feeding, comfort, stimulation, and care will be consistently met. It builds trust in themselves, others, and the world.
- The Crucial Element: The quality of the relationship between the primary caregiver (parent) and the infant, and the care the infant receives, are paramount. Simply providing food and shelter isn't enough for a strong sense of self-trust.
- Mutual Regulation of Frustration: Both infant and parent learn to manage frustration together. When this "synchrony" (working together smoothly) doesn't happen, mistrust can develop.
- Sources of Mistrust:
- Parental Immaturity: If a parent is emotionally immature or doesn't understand the infant's cues.
- Too Much or Too Little Gratification:
- Too much: If needs are always met before the infant signals readiness, they don't learn to control their environment.
- Too little (prolonged delay): Leads to constant frustration and mistrust of others.
- Consistency of care is essential!
- Sources of Mistrust:
- Foundation for the Future: The trust developed in infancy provides a secure base for all future developmental stages, allowing infants to approach new situations with less fear.
- Oral-Social Stages (Within the first year): Erikson divides the first year into two stages related to oral experiences:
- First 3-4 Months: Food intake is the most important social activity. Infants have little tolerance for frustration or delayed gratification. Primary narcissism (total self-concern) is high. However, as vision, motor skills, and vocalization improve, infants use more advanced behaviors to interact (e.g., reaching arms up to be held instead of just crying).
- Second Stage (Beyond 4 months):
- Grasping: This becomes a way of "reaching out" to others. While initially a reflex, the reciprocal act of parents holding and touching the infant during grasping provides pleasurable tactile stimulation, which is extremely important for developing trust. The quality of the interpersonal relationship is more important than just the amount of food or sucking time.
- Biting: A more active and aggressive way of interacting. Infants learn they can hold onto their own and exert control.
- Conflict Example: During breastfeeding, biting causes the mother to withdraw the breast, but it also relieves teething discomfort and gives the infant a sense of power.
- Resolution: This conflict can be resolved by using pacifiers or teething toys, allowing the infant to continue pleasurable breastfeeding. Successfully navigating this conflict strengthens the mother-child bond as the infant recognizes the mother as the most significant person in their life.
3. Cognitive development in infancy: piaget's sensorimotor phase (birth to 12 months)
Piaget's theory helps us understand how infants "know" and learn about their world. The period from birth to 24 months is called the sensorimotor phase, because infants learn through their senses and motor actions. We'll focus on the first four stages, covering birth to 12 months.
During this phase, infants move from simple reflexes to purposeful, repetitive actions, and eventually to imitation.
3.1. Key Intellectual Achievements in Infancy:
There are three major cognitive milestones during the sensorimotor phase:
- Separation:
- Infants learn that they are separate from other objects and people in their environment.
- They realize that others, not just themselves, control certain aspects of the environment. This means they start to understand they need to adjust their actions for things to work out mutually.
- Connection: This concept ties into Erikson's idea of trust and the mutual regulation of frustration (learning to manage disappointments together).
- Object Permanence:
- This is the understanding that objects still exist even when they are out of sight.
- Example: If you hide a toy under a blanket, an infant with object permanence will actively look for it.
- This skill typically develops around 9 to 10 months of age, which aligns with their increased ability to move around and explore.
- Use of Symbols (Mental Representation):
- This is the ability to think about an object or situation without actually seeing or experiencing it at that moment.
- It's the beginning of understanding concepts like time and space.
- Example: An infant might pretend to feed a doll, even if there's no real food present, showing they can mentally represent the action.
3.2. Piaget's Sensorimotor Stages (Birth to 12 Months):
Stage 1: Reflexive Behavior (Birth to 1 Month)
- Focus: The infant primarily uses their inborn reflexes to interact with the world.
- Examples: Sucking, rooting, grasping, and crying.
- Learning: The repetition of these reflexes starts to form associations. For example, when they cry (hunger), a nipple is put in their mouth, they suck, feel satisfied, and then sleep. They are "assimilating" (taking in) this experience, linking the sound of crying with the feeling of satisfaction.
- This stage lays the groundwork for recognizing patterns and orderly sequences of events.
Stage 2: Primary Circular Reactions (1 to 4 Months)
- Focus: Reflexive behaviors start to be replaced by voluntary acts. Infants begin to repeat actions that they find pleasurable or interesting, especially those involving their own body.
- Examples: Sucking their thumb, repeatedly grasping and releasing their own fingers.
- Learning: This is the beginning of accommodation – where infants adjust their behaviors based on new information from the environment.
- Before: They might cry until the nipple is in their mouth.
- Now: They learn that hearing a parent's voice means the nipple is coming, so they might stop crying before the nipple even arrives.
- They start to understand causality (cause and effect) and that events happen in a sequence. They actively take in sensory information (sight, sound, touch) and use their developing motor skills.
Stage 3: Secondary Circular Reactions (4 to 8 Months)
- Focus: Infants now repeat actions that produce interesting results in the environment, not just on their own body. They are becoming more aware of the effects of their actions on external objects.
- Examples: Shaking a rattle to hear a noise, banging toys, pulling strings to make something move. They're doing this not just for the act itself, but for the response it creates.
- Key Developments:
- Quality and Quantity: They notice that "more" or "less" shaking produces different sounds.
- Causality, Time, Intentionality, Separateness: These concepts begin to develop.
- New Behaviors:
- Imitation: By the second half of the first year, they can imitate simple sounds and gestures.
- Play: They enjoy repeating actions they've mastered. Much of their waking time is spent in sensorimotor play.
- Affect (Emotion): Their emotions become more evident as they develop a sense of permanence.
- Emerging Object Permanence: During the first 6 months, if an object is out of sight, it's "out of mind." But in this stage, they start to remember objects even when they can't see them. Object permanence is crucial for parent-child attachment and is linked to the development of separation anxiety around 6 to 8 months.
Stage 4: Coordination of Secondary Schemas (8 to 12 Months)
- Focus: Infants combine and coordinate their previous knowledge and skills to achieve new goals. This is a transitional stage where they build on what they've learned.
- Increasing Motor Skills: Their improved motor skills (like crawling) allow them to explore the environment much more extensively.
- Problem-Solving:
- They begin to understand that an object isn't gone just because it's hidden.
- They actively try to remove obstacles to find a hidden object. This is the beginning of intellectual reasoning – they can see a problem and intentionally try to solve it.
- Symbol Association: They start to associate symbols with events, even if their understanding is still very personal (e.g., "bye-bye" meaning "Mommy is going to work"). They learn about objects through direct interaction with them.
- Advanced Intentionality: They will now actively try to overcome barriers to get what they want (or avoid what they don't want). If something is in their way, they'll attempt to climb over it or push it aside, rather than just giving up like before.
4. Development of Body Image
Body image development closely follows how an infant learns about the world through their senses and movements.
- Early Sensations (Kinesthetic and Tactile):
- An infant's first understanding of their body comes from how it moves (kinesthetic) and how it feels to touch (tactile).
- The mouth is the primary source of pleasurable sensations (e.g., sucking).
- Other body parts become sources of pleasure: hands and fingers are sucked, feet are played with.
- Comfort and Reinforcement: When their physical needs are met (e.g., fed, changed), infants feel comfort and satisfaction with their body. Caregivers' responses (e.g., smiling back when the infant smiles) reinforce these positive feelings.
- Self-Image and Object Permanence:
- Achieving object permanence (understanding that things exist even when out of sight) is crucial for developing a self-image.
- By the end of the first year, infants recognize that they are distinct individuals separate from their parents.
- They become increasingly interested in their own image, especially in a mirror.
- Body Awareness through Movement: As motor skills improve, infants learn how useful their body parts are: hands bring objects to the mouth, legs help them move. These experiences teach them about themselves.
- Nursing Point: It's important for parents and nurses to convey positive messages to infants about their bodies.
5. Development of gender identity
Gender identity is a person's internal sense of being male, female, both, or neither.
- Early Influences: Gender identity is thought to begin even before birth due to complex hormonal influences that also shape brain development.
- Establishment: A child's gender identity (as male or female) is generally established by 2 to 3 years of age.
- Multifactorial: Environmental, biological, and sociocultural factors all play a role.
- From birth, the child is given a name, and caregivers interact with them in specific ways based on their assigned gender.
- Touch is vital: Skin-to-skin contact, sucking, and mouthing are important.
- Self-Exploration: Infants explore their own bodies for pleasure; male infants commonly have erections and can experience genital self-stimulation.
- Nursing Point: Parents' responses to these early expressions of sexuality are very important. A healthy, accepting response by parents helps shape a child's evolving attitudes toward their own body and sexuality.
6. Social development
Infants' social development starts with simple reflexes and quickly becomes heavily influenced by their interactions with primary caregivers. They show increasing attachment, improve communication, and engage in personal-social behaviors. Play is a major way infants socialize and learn.
6.1. Attachment: Forming Crucial Bonds
Attachment is the deep emotional bond that forms between an infant and their primary caregiver.
- Importance of Human Contact: Physical contact is extremely important for infant development. Parenting is a learned skill, not an instinct.
- Continuous Process: Attachment begins even before birth and continues to develop throughout the first year.
- The "Mother" Figure: While the term "mother" is often used, it refers to the consistent caregiver (who could be a father, grandparent, or other family member) with whom the child has the strongest bond.
- Father-Child Attachment:
- Fathers also go through similar stages of attachment.
- They are more involved in childcare when mothers are employed.
- Inexperienced first-time fathers are just as capable of forming strong attachments.
- Fathers of high-risk infants show love and affection, especially with close physical contact (like holding).
- Fathers play a significant role in supporting the mother's well-being during the perinatal period, especially with high-risk infants.
- A father's relationship with the infant also impacts the mother's emotional well-being.
- Other Caregivers: In single-parent families, a grandparent or other significant person may become the primary caregiver. Nurses need to recognize that attachment can vary based on caregiving arrangements.
- Insecure Attachment:
- If an infant doesn't receive consistent, loving care and a safe environment, they may develop an insecure attachment.
- This can lead to psychosocial difficulties that can persist into childhood and adulthood.
- Maternal depression during the perinatal period can negatively affect the infant's neuroendocrine development, growth, and overall development.
- Requirements for Attachment: Two cognitive abilities are needed for attachment to fully develop:
- The ability to tell the primary caregiver apart from other people.
- The achievement of object permanence.
-
- These abilities prepare the infant for separation from the parent, which is another crucial aspect of attachment. Separation-individuation (becoming a distinct individual) should happen in harmony with emotional attachment.
- Stages of Attachment Formation:
- First few weeks: Infants respond to anyone indiscriminately.
- 8-12 weeks: Infants show more crying, smiling, and vocalizing towards the mother (or primary caregiver) but still respond to others.
- Around 6 months: Infants show a distinct preference for the mother. They follow her more, cry when she leaves, enjoy playing with her most, and feel most secure in her arms.
- About 1 month later: Many infants begin to attach to other family members, often the father.
- Behaviors Indicating Attachment:
- Crying, smiling, and vocalizing more to the primary caregiver.
- Looking more at the primary caregiver, even from a distance.
- Crying when the caregiver leaves the room.
- Approaching the caregiver using locomotion (crawling, creeping, walking).
- Clinging to the caregiver, especially when strangers are present.
- Exploring their environment while using the caregiver as a "secure base" to return to.
Effects of Prolonged Separation:
- Attachment is critical for optimal child development. Researchers like John Bowlby, John Robertson, and René Spitz documented the negative effects of prolonged early separation without quality substitute care.
- Bowlby's Findings (1969): Severe cognitive and physical impairment, especially if emotional deprivation occurs in the first 3 years. Effects can be reversed if deprivation stops early (before 2 years), but severe, prolonged deprivation starting early in the first year can lead to permanent issues like:
- Inability to form trusting, intimate relationships.
- Language impairment.
- Difficulty with abstract thinking.
- Robertson (1953) & Bowlby (1969): Identified typical behavioral reactions of hospitalized infants separated from their mothers (e.g., separation anxiety).
- Spitz's Findings (1945): Studied institutionalized children (one nurse for eight infants). Despite loving care, lack of individual attention and stimulation led to:
- Delayed physical growth.
- Increased susceptibility to disease.
- Decreased developmental scores over two years.
- Normal development occurred with one-to-one attention from a mother substitute.
- Severe Attachment Disorders: These are serious psychological and developmental problems from unhealthy or absent attachment.
- Risk Factors: Abuse, neglect, parental alcoholism/mental illness/substance abuse, lack of consistent caregiver (foster care, institutionalization, abandonment, incarceration).
- Types:
- Reactive Attachment Disorder (RAD): Children may not cuddle, fail to seek comfort when distressed, show minimal social or emotional reciprocity, and have unexplained fearfulness or irritability.
- Disinhibited Social Engagement Disorder (DSED): Children may inappropriately approach unfamiliar adults, lack suspicion of strangers, and have poor impulse control.
- Without early intervention, some children may struggle to develop a conscience and may develop antisocial personality disorder. (Note: These are distinct from autism or other pervasive developmental disorders).
- Nursing Implications:
- Assess each family, understanding that stress doesn't always lead to harm, and children can adapt.
- Evaluate individual risk factors and coping abilities (e.g., using temperament questionnaires).
- When prolonged parental separation occurs, help families find suitable, warm, responsive, and interactive caregiver substitutes to minimize negative effects.
- Emphasize the child's "plasticity" (ability to change) and "resilience" (ability to bounce back) to minimize parental guilt.
6.2. Separation Anxiety: Missing the Caregiver
- When it Develops: Between 4 and 8 months, as infants gain self-awareness and understanding of the mother as a separate being, and object permanence develops.
- Manifestation: A predictable sequence of behaviors:
- Early on: Protesting when placed in their crib.
- Soon after: Objecting when the mother leaves the room. They might not notice if absorbed in play, but will protest when they realize she's gone.
- Increasing Awareness: Become very alert to the caregiver's activities and whereabouts.
- 11-12 Months: Can anticipate an imminent departure by watching caregiver behaviors and will protest before they leave. Parents often learn to delay alerting the child until just before leaving.
6.3. Stranger Fear (Stranger Anxiety): Discriminating Familiar from Unfamiliar
- When it Develops: Between 6 and 8 months, as infants form attachments and can distinguish familiar people from strangers.
- Behaviors: Common signs include:
- Clinging to the parent.
- Crying.
- Turning away from strangers.
6.4. Language Development: From Cries to Words
- First Communication: Crying:
- Initially, crying is a reflexive biological sign of urgency and displeasure (e.g., hunger).
- It's also a social event that influences the parent-infant relationship.
- Early Weeks: Mostly reflexive, related to physical needs.
- Cry for 1-1.5 hours/day up to 3 weeks.
- Increases to 2-4 hours by 6 weeks.
- Tends to decrease by 12 weeks.
- Increased Crying (First few months): Unexplained fussiness might be related to energy discharge and central nervous system maturation.
- End of First Year: Infants cry for attention, from fear (especially stranger fear), and from frustration due to developing but still inadequate motor skills.
- Parental Interpretation: Many parents learn to distinguish different cries and interpret their infant's needs.
- Nursing Point: Crying can be very distressing for parents (e.g., colic). Explain that variation in crying is normal. Offer guidance on consoling techniques (holding, swaddling, massage, rocking, gentle stimulation).
- From Cries to Vocalizations:
- Vocalizations heard during crying eventually become syllables and words (e.g., "mama" during vigorous crying).
- 5-6 Weeks: Make small throaty sounds.
- 2 Months: Produce single vowel sounds (ah, eh, uh).
- 3-4 Months: Add consonants (n, k, g, p, b); coo, gurgle, and laugh aloud.
- 6 Months: Imitate sounds; add consonants (t, d, w); combine syllables (e.g., "dada"), but they don't yet understand the meaning of the word.
- 9-10 Months: Comprehend the meaning of "no" and obey simple commands with gestures.
- 1 Year: Can say 3-5 words with meaning and may understand as many as 100 words.
- Nursing Insight: Language development relies on both expressive skills (making thoughts known) and receptive skills (understanding spoken words). Ensure infants are exposed to expressive speech, and carefully evaluate any delays for potential hearing loss.
6.5. Personal-Social Behavior: Connecting with the World
Personal-social behavior refers to how a child responds to their environment. It's heavily influenced by external stimuli and forms the basis for essential life skills like feeding, potty training, independence, and cooperative play.
- Infant's Influence on Environment: Infants actively shape their environment and elicit responses from caregivers.
- They show a visual preference for the human face.
- As early as 1 week old, they intently watch a parent speak, diminishing other activity, bobbing their head, and moving their mouth as if trying to respond.
- Developing Social Responses:
- 6-8 Weeks: The social smile appears in response to pleasurable stimuli. This is a powerful milestone that encourages more interaction from family members.
- 3 Months: Show significant interest in their surroundings: excitement when a toy is presented, refusal to be left alone, recognition of parents, and expressing pleasure by squealing.
- 4 Months: Laugh aloud and enjoy new, surprising stimuli.
- Increasing Independence and Control:
- 6 Months: Become very personable. They play games like peek-a-boo, signal to be picked up by extending their arms, and show displeasure when a toy is taken away or their face is washed. They increasingly demonstrate their ability to control their environment.
- The development of fine and gross motor skills gives them much greater independence in movement.
- Understanding Discipline and Emotions:
- Second half of the first year: Infants begin to understand simple discipline, like the meaning of "no" or a scolding tone.
- They comprehend different facial expressions and are sensitive to the emotional changes in others.
- Imitation:
- 7 Months: Imitate actions and noises.
- 8 Months: Imitate sounds.
- 10 Months: Imitate games like pat-a-cake and peek-a-boo.
- Increasing Independence (11 Months +):
- They become more independent, learning to feed themselves (though with much spilling) using fingers, spoons, and cups.
- They can help with dressing (e.g., putting a foot out for a shoe, pushing an arm through a sleeve).
- They not only understand "no" but also shake their head to indicate "no."
- They can follow simple directions and love to "perform" for others to get attention.
6.6. Play: The Infant's Way of Learning and Socializing
Play is a crucial part of an infant's social and cognitive development.
- Early Play (Narcissistic & Body-Focused):
- Initially, an infant's play is narcissistic (self-centered), revolving around their own body.
- Body parts like hands, fingers, and feet are primary objects of play and pleasure.
- Progressive Sophistication:
- Birth to 3 Months: Responses are global and undifferentiated. Pleasure is shown by quieting (1 month), smiling (2 months), and squealing (3 months). Play is "dependent" (they respond to you).
- 3 to 6 Months: Show more focused interest in stimuli. They begin to play alone with a rattle or stuffed toy, or with others. They interact much more during play.
- 4 Months: Laugh aloud, show preferences for certain toys, and get excited by food or favorite objects. They recognize and smile/vocalize at their image in a mirror.
- 6 Months to 1 Year: Play involves advanced sensorimotor skills.
- They play actual games like peek-a-boo and pat-a-cake.
- They demonstrate verbal repetition and imitate simple gestures.
- Play becomes more selective regarding toys and "playmates." Although play is solitary (one-sided), infants choose who they interact with.
- 6-8 Months: Often refuse to play with strangers.
- Parents are favorites! Infants know how to get their attention:
- 6 Months: Extend arms to be picked up.
- 7 Months: Cough to make their presence known.
- 10 Months: Pull a parent's clothing.
- 12 Months: Call parents by name. This is a huge step from the newborn who only cried to signal needs.
- Importance of Stimulation:
- Stimulation is as vital for psychosocial growth as food is for physical growth.
- Nurses guide parents on appropriate play for infants based on developmental milestones.
- Just putting a mobile over a crib or toys in a play yard isn't enough for optimal social, emotional, and intellectual development.
- Media Use: The American Academy of Pediatrics recommends discouraging media (other than video-chatting) for children under 18 months. This is because it doesn't provide appropriate sensory stimulation or improve language skills.
- Interactive Play: Play must involve interpersonal contact and provide recreational and educational stimulation. Infants need to be played with, not just allowed to play alone.
- Solitary Play: While infant play is often called "solitary," this doesn't mean they don't want interaction. It just refers to the one-sided nature of their play at this stage. The quality of personal interaction is far more important than the specific toys.
Play During Infancy
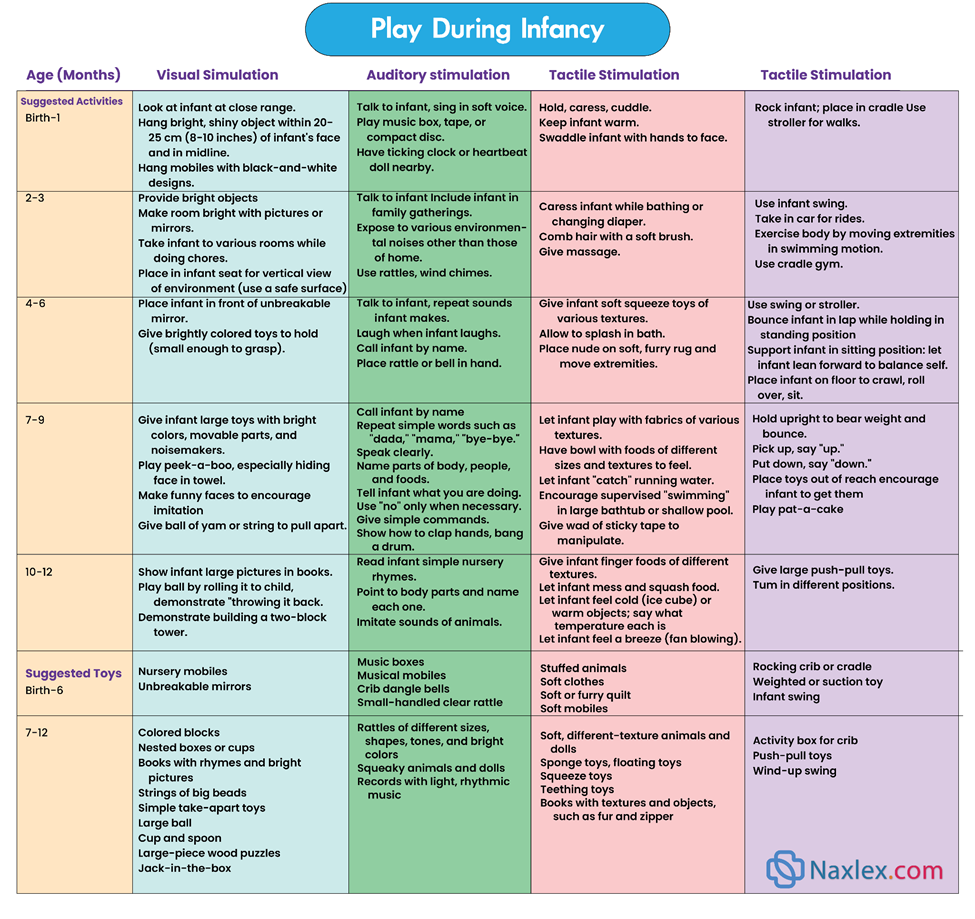
Temperament
An infant's temperament (their behavioral style) significantly influences how they interact with parents and family.
- Parental Perception is Key: When assessing temperament, what matters most is the parents' perception of the child and how well the child's actual temperament "fits" with the parents' expectations.
- "Goodness of Fit": If there's a lot of "dissonance" (lack of harmony) between the child's temperament and the parents' ability to accept and deal with it, there's a higher risk for future parent-child conflicts.
- Nature vs. Nurture: While temperament has a strong biological component, the environment (especially the family) can modify it. Family interaction is a circular process: each member affects others and the family unit.
- Nursing Role: Nurses play a crucial role in helping families understand their infant's temperament and how it relates to family dynamics and overall well-being.
- Temperament and Parental Depression:
- Some research links maternal depression (especially postpartum depression) to a "difficult" infant temperament, which can negatively affect the mother-infant relationship.
- Infant sleep problems combined with temperament can also impact maternal-infant bonding.
- Fathers can also experience postnatal depression, especially when infants have a difficult temperament, or due to other factors like previous pregnancy loss, parenting distress, marital issues, or feeling ineffective as a parent.
- A lack of reciprocity (mutual give-and-take) between infant and mother increases the risk of discord.
- Assessing Temperament:
- Several tools exist to measure infant temperament (e.g., Revised Infant Temperament Questionnaire, Infant Behavior Questionnaire, Early Infancy Temperament Questionnaire).
- Nursing Tip: When discussing test results with parents, avoid labeling infants as "difficult." Instead, describe them using characteristics like "intense" or "less predictable."
- How Nurses Can Help: Knowing an infant's temperament allows nurses to:
- Provide parents with information that helps them see their child from a better perspective.
- Offer a more organized view of the child's behavior, potentially correcting parental misperceptions.
- Guide parents on appropriate childrearing techniques tailored to their child's temperament.
- Relieving Guilt: Simply informing parents that certain "difficult" traits might be innate can greatly reduce feelings of guilt and incompetence.
Importance of Developmental Knowledge for Nurses:
- Assessment: Knowledge of developmental sequences allows nurses to assess normal growth and identify minor or abnormal deviations.
- Parental Guidance: It helps parents develop realistic expectations for their child's abilities and provides guidelines for suitable play and stimulation. Parents who lack this knowledge might set inappropriate expectations.
- Strengthening Relationships: Emphasizing the child's developmental age over their chronological age strengthens the parent-child relationship by fostering trust and reducing frustration.
- Conclusion: A thorough understanding and appreciation of children's growth and development are absolutely essential for nursing practice.
Nursing Insight: Remember while the sequence of milestones is generally the same, the rate at which children achieve them can vary. This is why developmental screening for all children is crucial.
Coping With Concerns Related To Normal Growth And Development
1.0. Infancy is a period of rapid growth, but it also comes with unique challenges for both infants and parents. Nurses play a crucial role in providing anticipatory guidance and support.
1.1. Separation Anxiety and Stranger Fear
These are normal, healthy signs of a strong parent-child attachment, not undesirable behavior. However, they can be challenging for families.
- Understanding the Behavior:
- Separation anxiety is when an infant becomes distressed when a primary caregiver leaves.
- Stranger fear (or stranger anxiety) is when an infant reacts negatively to unfamiliar people.
- These fears develop as infants achieve object permanence and can distinguish familiar from unfamiliar faces.
- Challenges for Parents: Parents may feel confined to home as the infant protests being left with caregivers or at daycare.
- Nursing Interventions/Guidance:
- Normalize the behavior: Reassure parents that this is a healthy, desirable, and necessary part of emotional development.
- Familiarity with others: Encourage parents to have close friends or relatives visit often so the infant becomes comfortable with other trusted adults.
- Safe stranger experiences: Allow infants to explore strangers at their own pace. If parents hold the child close but turn them slightly away, the infant can observe while feeling secure.
- Factors influencing stranger fear intensity (for nurses/strangers):
- Gender, Age, Size: Female, younger, and smaller people (or those who kneel/sit) are less stressful.
- Approach: Avoid loud, sudden, or intrusive approaches (e.g., don't immediately reach out).
- Proximity to Parent: Being closer to the parent (e.g., on their lap) is less stressful.
- Best Approach for Strangers (including nurses):
- Talk softly.
- Meet the child at eye level (to appear smaller).
- Maintain a safe distance.
- Avoid sudden, intrusive gestures (like holding arms out or smiling broadly right away).
- Reassurance of Parent's Presence: Help parents understand that reassuring the infant of their continued presence helps the infant learn that the parent still exists even when not physically seen. Techniques include:
- Talking to the infant when leaving the room.
- Letting them hear your voice on the telephone.
- Using transitional objects (e.g., a favorite blanket or toy).
- Acknowledge Difficulty: This period is trying but necessary, as parents cannot always be with the infant. Bedtime fears (fear of going to bed or being alone in the dark) commonly emerge during the second half of the first year.
1.2. Limit Setting and Discipline
As infants gain motor skills and mobility, setting safe limits becomes essential.
- Early Discipline:
- Parents can begin discipline using a negative voice and stern eye contact.
- Time-out can be effective for older infants, adjusted to their abilities (e.g., a play yard is better than a chair for most infants).
- Early intervention: Emphasize that starting effective disciplinary methods earlier makes it easier to continue them.
- Understanding Infant Limitations:
- Parents must recognize that infants (and toddlers) do not understand cause-and-effect relationships between dangerous objects and harm. Adequate protection from hazards is crucial.
- Reassure parents that infant behavior is exploratory, not oppositional, and is primarily driven by needs for warmth, love, food, security, and comfort.
- "Spoiling" Myth Debunked:
- Parents often worry that too much attention or meeting an infant's needs will "spoil" them. There is no substantial evidence to support this. Meeting basic needs does not spoil a child.
- Research shows that more responsive parents (who pick up crying babies promptly) have infants who cry less later on, not more.
- True "spoiling" is defined as "excessive self-centered and immature behavior resulting from the failure of parents to enforce consistent, age-appropriate limits." It involves demanding their own way, being inconsiderate, and manipulative.
- Indulgence combined with clear expectations and limits does not cause spoiling. It's indulgence without guidelines for acceptable behavior that leads to unrealistic expectations.
- Normal Behaviors Mistaken for Spoiling:
- Crying in early infancy (with or without colic).
- Crying due to unmet basic physical needs (e.g., soiled diaper, hunger, need for physical contact).
- Toddler behaviors like negativism ("no"), persistent exploration, and temper tantrums (these are normal developmental stages).
- Children experiencing extreme stress from marital discord, abuse (physical, emotional, sexual), substance abuse, or parental mental illness.
- Nursing Role:
- Provide anticipatory guidance on expected but challenging behaviors.
- Reassure parents that loving their infant without fear of spoiling is healthy.
- As infants grow, help parents set limits to prevent normal disruptive behaviors from becoming problems.
- Injury Prevention: This starts by helping parents understand normal infant development. Reiterate that infants cry because a need isn't met, not to intentionally irritate.
- Warning: A fussy or irritable infant is at risk for traumatic brain injury or shaken baby syndrome if caregivers don't understand the nature of infant crying.
1.3. Alternative Child Care Arrangements
Finding safe and competent child care is a significant concern for many parents, especially working mothers.
- Shift in Care: More children are now cared for in group settings or other arrangements outside the home.
- Types of Child Care:
- In-home care: A babysitter (live-in or daily), cooperative arrangements (e.g., exchange babysitting), or family day care (in caregiver's home, usually licensed for up to 6 children, including the provider's own young children). Large family homes care for 8-12.
- Center-based care: Licensed day care facilities caring for 6+ children for 6+ hours/day.
- Work-based group care: Offered by employers.
- Sick-child care: Programs (often in hospitals or workplaces) for when a child is ill.
- Guiding Parents in Selection (Nursing Responsibility):
- Help parents find suitable facilities with qualified staff.
- State licensing agencies: Provide lists of centers, public records (health, safety, fire reports, evaluations, complaints, employee qualifications).
- Accreditation: Check if programs belong to voluntary accreditation systems like the National Academy of Early Childhood Programs (NAECP), which serves as a model for optimal care.
- References: Other parents' references can be helpful if they've thoroughly investigated and remain involved.
- Areas to Evaluate:
- Daily program.
- Teacher qualifications.
- Nurturing qualities of caregivers.
- Student-to-staff ratio.
- Discipline policy.
- Emergency protocols (fire, tornado).
- Environmental safety precautions.
- Provision of meals.
- Sanitary conditions.
- Adequate indoor/outdoor space per child.
- Fee schedule (minimum fees may mean minimum services).
- Crucial: Personal observation of the facility is irreplaceable. Meet the director and caregivers.
- Parental Rights: Parents should always have the right to visit their child, and regular conferences should occur.
- Babysitters: Apply the same scrutiny. Get references, and observe interaction. For older infants, a gradual introduction to a new caregiver is beneficial.
- Health Practices in Child Care:
- This is a growing concern parents often overlook.
- Children in daycare, especially under 3, have more illnesses (diarrhea, ear infections, respiratory infections, hepatitis A, meningitis, cytomegalovirus).
- Strongest predictor of illness risk is the number of unrelated children in the room.
- Proactive infection control and staff education reduce illness.
- SIDS Prevention: Parents must discuss safe sleep positions and environments for infants with caregivers, as SIDS cases have occurred in daycares.
- Nurse's Role in Infection Control & Injury Prevention in Child Care:
- Advise parents on center sanitation and safety practices.
- Actively educate staff on minimizing infection transmission and injury.
- Key Diapering/Toileting Guidelines (AAP):
- Handwashing by children and staff after diapering/toileting.
- Use disposable or properly designed reusable diapers.
- Change soiled diapers promptly.
- Never rinse reusable diapers (fecal contents can be flushed).
- Send soiled reusable diapers home in a sealed plastic bag.
- Properly clean diaper-changing surfaces after each use.
- Use child-sized toilets or modified toilet seats for easier cleaning.
- Sanitize toilets, seats, potty chairs, and diaper-changing areas with a fresh 1:64 bleach solution (1/4 cup bleach to 1 gallon water), applied for 2 minutes, then rinsed.
- Other AAP Guidelines: Daycare centers should follow guidelines on hand hygiene, cleaning equipment/toys, food handling, human milk handling, pet care, and when children should be kept home due to illness. They should also share information about reportable infectious diseases.
1.4. Thumb Sucking and Pacifier Use
Sucking is a primary pleasure for infants, often not fully satisfied by feeding alone.
- Natural Need: Infants deprived of sucking (e.g., cleft lip repair) may suck their tongues. Some are born with sucking blisters from in utero activity.
- Parental Concern: Investigate parents' feelings before offering advice if they are overly concerned about finger, thumb, or pacifier sucking.
- Pacifier Use and Breastfeeding:
- Recent research shows no negative effect of pacifier use on breastfeeding. While historically discouraged for breastfed infants, experts now suggest pacifier use may signal a mother's decision to stop breastfeeding rather than causing it directly.
- Important: Pacifier use should not replace actual feeding or suckling. The infant should control feeding pace and termination.
- Pacifier Benefits and Risks:
- Risk: Associated with an increased risk of otitis media (ear infections) in several studies.
- Benefits (AAP/AAFP Recommendations):
- Recommended during the first 6 months for pain management during painful procedures (non-nutritive sucking has an analgesic effect for neonates).
- Strong evidence for SIDS prevention. The exact mechanism is unknown, but pacifier use is recommended for non-breastfed infants as desired, and for breastfed infants once breastfeeding is established.
- Weaning: Recommend weaning from pacifier during the second 6 months of life.
- Pacifier Safety:
- Stress safety considerations when buying pacifiers.
- Caution parents against altering pacifiers.
- Avoid "bling" or decorative gems that can be dislodged and swallowed/aspirated.
- Thumb Sucking:
- No need to restrain non-nutritive sucking of fingers/thumbs during infancy and early childhood.
- Malocclusion (dental problems) may occur if thumb sucking persists past age 4 or when permanent teeth erupt.
- Pacifiers are sometimes seen as less damaging because they are usually discarded earlier (2-3 years) than thumb sucking might cease.
- Cultural variations exist for both.
- Peak: Thumb sucking peaks at 18-20 months, most common when hungry, tired, or insecure.
- Warning Sign: Persistent thumb sucking in a listless, apathetic child warrants investigation; it could signal emotional problems, boredom, isolation, or lack of stimulation.
- Preterm Infants: Non-nutritive sucking (including pacifier use) can improve sucking skills and shorten the time to full breastfeeding in preterm infants. It should not be withheld from them.
1.5.Teething
The eruption of deciduous (primary) teeth can be a challenging period.
- Timeline:
- Age of eruption varies, but the order is predictable.
- First teeth: Lower central incisors (around 6-10 months, average 8 months). Followed by upper central incisors.
- Rule of Thumb: Age in months - 6 = Number of teeth (e.g., 8 months - 6 = 2 teeth).
Sequence of Eruption of Primary Teeth
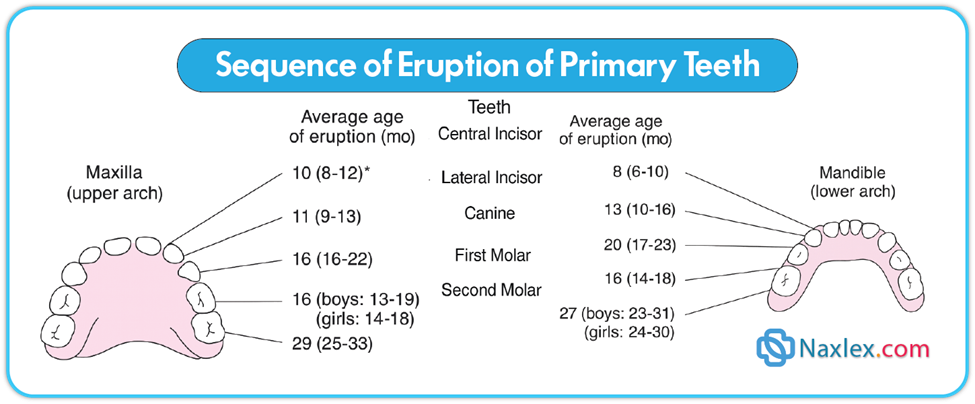
- Physiologic Process: Discomfort is common as the tooth crown breaks through the gum.
- Common Symptoms:
- Drooling.
- Increased finger sucking/biting on hard objects.
- Irritability.
- Difficulty sleeping.
- Mild temperature elevation.
- Ear rubbing.
- Decreased appetite for solid foods.
- Nursing Insight: Signs of illness (fever >39°C [102°F], vomiting, diarrhea) are NOT typical teething symptoms and warrant further investigation for actual illness.
- Nursing Interventions/Pain Relief:
- Cold is soothing:
- Frozen teething rings.
- Ice cube wrapped in a washcloth.
- Topical Anesthetic Ointments: Available over-the-counter, but most contain benzocaine, which can cause a rare but serious disorder called methemoglobinemia if ingested. Use ONLY under direct advice and supervision of a healthcare provider.
- Systemic Analgesics: If irritability affects sleeping/feeding, acetaminophen or ibuprofen (if age-appropriate) can be given for no more than 3 days. Advise parents this is temporary and to contact the practitioner if symptoms persist or worsen.
- Avoid:
- Teething powders.
- Cutting or rubbing gums with aspirin or liquor (risk of ingestion, infection, aspiration).
- Hard candy (choking hazard).
- Amber teething necklaces: Should NOT be worn by infants/young children due to choking/suffocation risk and beads becoming dislodged and ingested.
- Cold is soothing:
Promoting Optimum Health During Infancy
1.0. Optimal health in infancy lays the foundation for a lifetime of well-being. Nurses play a critical role in guiding parents, especially regarding nutrition.
1.1. Nutrition: Fueling Growth and Development
Discussions about infant nutrition ideally begin prenatally, with the choice of breastfeeding or formula feeding. This section focuses on nutrition during the first 12 months, as infants grow and develop the skills needed for solid foods.
Concerns in Infant Feeding:
Experts are concerned that many infants aren't fed appropriately, leading to potential health issues:
- Early Introduction of Solids: Infants may be given solid foods before their digestive systems are ready to fully absorb them. Studies show about 24% of infants consume cereal, fruit, or vegetables by 4 months, despite recommendations for 4-6 months.
- Consequence: Early introduction of solid food before 4 months is correlated with obesity later in life.
- Inappropriate Drinks: Giving "empty calorie" drinks (like juice or soda) instead of nutrient-rich infant milk can contribute to childhood obesity, cardiovascular disease, iron deficiency anemia, vitamin D deficiency, and rickets.
- Long-term Impact: Poor infant nutrition can negatively affect growth and development and increase the risk of chronic health conditions.
- Nursing Role: Nurses must be proactive in teaching parents about appropriate infant nutrition and habits to ensure healthy growth and development.
Developmental Milestones Associated With Feeding
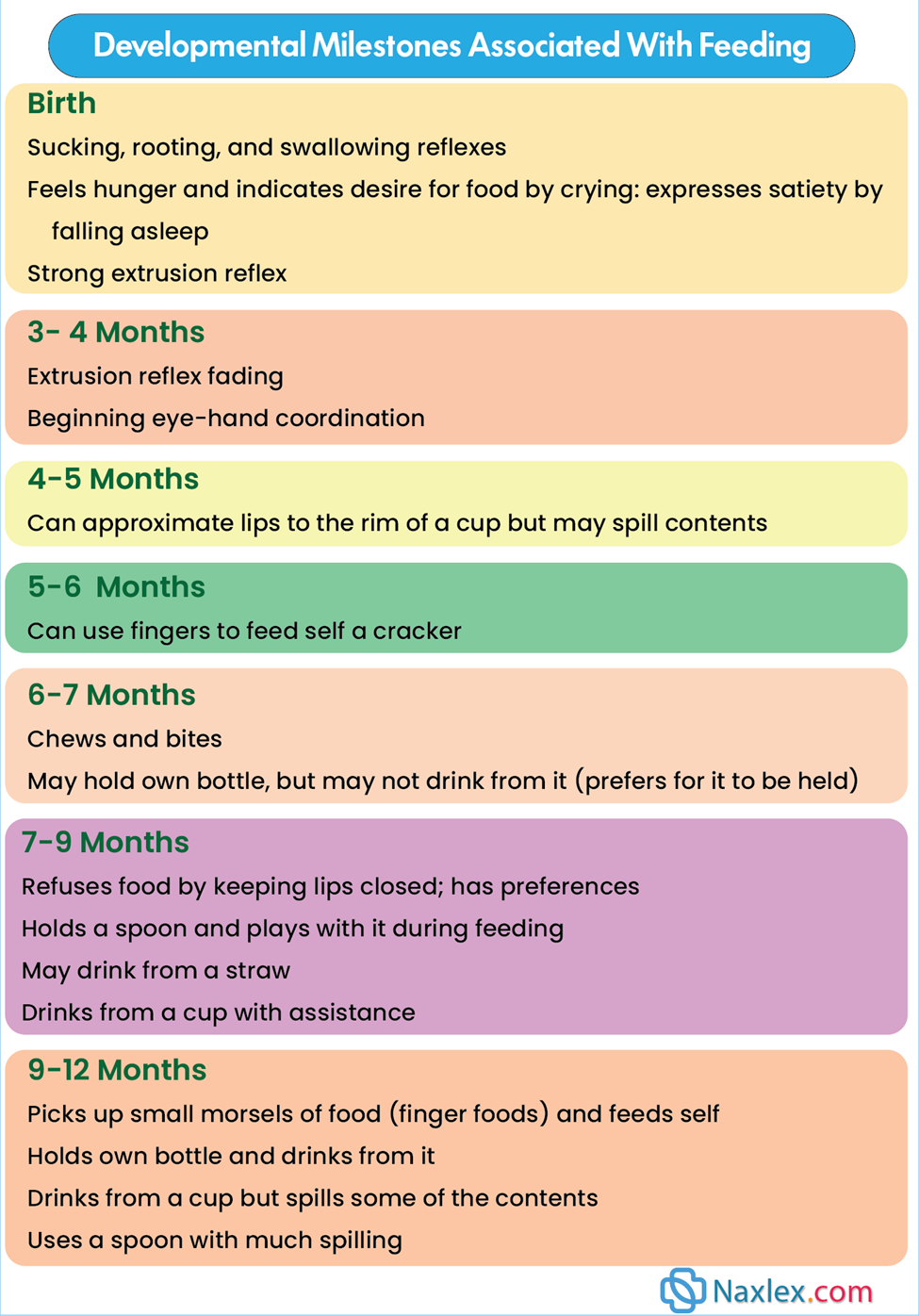
The First 6 Months: Liquid Gold and Formula
- Human Milk is Ideal: Human milk (breast milk) is the most desirable and complete diet for the first 6 months.
- Contraindications to Breastfeeding: Mothers who are HIV-positive, using illicit drugs (heroin, cocaine, methamphetamines, PCP), taking antimetabolites or radioactive medications, or have certain maternal illnesses (e.g., T-cell leukemia/lymphoma). Always consult a healthcare provider regarding maternal medications.
- Vitamin and Mineral Supplementation:
- Generally, healthy, term breastfed infants from well-nourished mothers don't need supplements, with a few exceptions.
- Vitamin D: The American Academy of Pediatrics (AAP) recommends all infants (including exclusively breastfed) receive a daily supplement of 400 IU of vitamin D starting in the first few days of life to prevent rickets and vitamin D deficiency. This continues until the infant consumes at least 1 liter (or 1 quart) per day of vitamin D-fortified formula. Non-breastfed infants consuming less than 1 liter/day of fortified formula also need this supplement.
- Iron: If an infant is exclusively breastfed after 4 months (when fetal iron stores deplete), iron supplementation (1 mg/kg/day) is recommended until appropriate iron-containing complementary foods (like iron-fortified cereal) are introduced.
- Vitamin B12: May be needed if the mother's intake is inadequate.
- Fluids (First 4 Months): Infants, whether breastfed or bottle-fed, do not require additional fluids (especially water or juice) during the first 4 months. Excessive water intake can lead to water intoxication and hyponatremia.
- Unacceptable Milks:
- Unmodified whole cow's milk, low-fat cow's milk, skim milk, other animal milks, and imitation milk drinks are not acceptable as primary nutrition sources for infants. They are difficult to digest, risk contamination, and lack necessary components for growth.
- Whole milk can cause iron deficiency anemia (possibly due to occult GI blood loss) and is deficient in iron, zinc, and vitamin C, with a high renal solute load, making it undesirable for infants under 12 months.
- Skim or low-fat milk is unacceptable due to inadequate essential fatty acids and excessively high protein/electrolyte (like sodium) concentrations.
- Dietary fat should not be restricted in infancy unless medically supervised.
- Honey: Avoid honey in the first 12 months due to the risk of infant botulism. Do not coat pacifiers with honey.
- Commercial Iron-Fortified Formula: An acceptable alternative to breastfeeding, providing all necessary nutrients for the first 6 months.
- Working Mothers and Breastfeeding:
- Encourage employed mothers to continue breastfeeding, setting realistic goals.
- Barriers: Lack of employer/co-worker support, inadequate pumping/storage facilities, insufficient time.
- Strategies: Pumping when away from home and bottle-feeding expressed milk (with or without formula supplementation) can be successful.
- Expressed Breast Milk Storage:
- Refrigerator (4°C / 39°F): Use within 48 hours.
- Freezer (-18°C / 0°F or lower): Up to 6 months (varies by freezer type). Prevent freezer burn.
- Warming Breast Milk/Formula:
- NEVER thaw or rewarm in a microwave oven due to uneven heating and risk of oral burns.
- Thawing: Place container under lukewarm water bath (40.5°C / 105°F), use a commercial warmer, or refrigerate overnight.
- Pumping Schedule: To maintain supply, pumping every 3-4 hours may be needed when away from home.
- Introduction of Solids (4-6 Months):
- Not recommended before 4-6 months. The infant GI tract and nutritional needs are not ready.
- Developmental Unreadiness: The strong extrusion reflex (pushing food out with the tongue) is present, infants instinctively suck, and limited motor skills prevent deliberate refusal of food.
- Risks of Early Introduction: May reduce breastfeeding frequency or lead to early cessation.
- Juices/Nonnutritive Drinks (First 6 Months):
- Caution parents against excessive use. These provide "empty calories," replace milk nutrients, and can lead to growth/health problems.
- Fruit juices are not required and have no proven benefits for infants under 6 months.
- Bottled Water for Formula:
- Safe alternative to tap water if tap water has high contaminants (e.g., lead).
- Do not assume bottled water is sterile unless stated.
- Fluoridated bottled water is generally not needed unless local tap water is low in fluoride, in which case fluoride supplementation is recommended after 6 months.
The Second 6 Months: Solids and Continued Milk
- Primary Nutrition: Human milk or iron-fortified formula remains the primary source of nutrition.
- If breastfeeding stops, use iron-fortified formula.
- "Follow-up formulas" marketed for older infants offer no advantage and provide excessive protein.
- Adding Solid Foods: This is the major change in feeding habits.
- Readiness (4-6 months):
- GI tract matured for more complex nutrients and less sensitive to allergens.
- Tooth eruption begins, aiding biting/chewing.
- Extrusion reflex disappears, and swallowing is coordinated.
- Well-developed head control allows sitting with support and turning head away to refuse food.
- Improved voluntary grasping and eye-hand coordination for self-feeding.
- Increased independence: desires to hold bottle, "help" with feeding.
- Readiness (4-6 months):
- Food Allergies: Previous advice was to avoid potentially allergenic foods until after 6-8 months, but this is now debated.
- Selection and Introduction of Solid Foods:
- Purpose: To supply nutrients not found in milk/formula.
- First Food: Iron-fortified infant cereal (e.g., rice cereal due to easy digestibility, low allergenic potential).
- Mix with formula, expressed breast milk, or water. After 6 months, juice can be added for vitamin C (enhances iron absorption).
- Continue until 18 months due to iron content.
- Introduction Method: Introduce one new solid food every 5 to 7 days to identify any reactions. Avoid cereal combinations initially.
- Order of Foods (Arbitrary): Strained fruits, then vegetables, then meats. Some recommend vegetables before fruits.
- Finger/Teething Foods:
- 6 Months: Crackers, zwieback.
- 8-9 Months: Junior foods, nutritious finger foods (firmly cooked vegetables, raw fruit pieces except grapes, cheese).
- 1 Year: Well-cooked table foods.
- Juice (from a cup): Can be offered after 6 months as a vitamin C source, sometimes replacing one milk feeding.
- Avoid: Juices high in fructose/sorbitol (apple, pear, prune, sweet cherry, peach, grape) can cause abdominal pain/diarrhea.
- AAP Recommendation: Fruit juice intake not to exceed 4-6 oz/day for children 1-6 years old. Only 100% fruit juice should be offered. Not warmed (destroys vitamin C). Keep covered and refrigerated.
- Dental Health: Offer juice from a cup, not a bottle, to prevent dental caries.
- Solids are for Taste/Chewing: During the second 6 months, solids are mainly for taste and chewing experience. The majority of calories still come from breast milk or formula. Solids are NOT a substitute for milk until after 12 months.
- Portion Sizes: Varies by infant. Generally, 1 tablespoon per year of age (so for infants under 12 months, 1/2 to 3/4 tablespoon, possibly 2 tablespoons served). Smaller portions can help prevent future overeating habits.
- Low-Calorie Foods/Fats: Avoid low-calorie milks and foods unless medically prescribed. Infancy is crucial for growth, and dietary fat restriction should be very cautious.
- Unacceptable Fats: Fried potatoes, candy, ice cream, cake, soda, other sweetened drinks. These don't provide appropriate fat intake and contribute to obesity.
- Recommendation: Limit serving size of dietary fats rather than eliminating them.
- Commercial vs. Homemade Baby Food: Commercial is convenient, no added salt/sugar, but expensive. Homemade is simple and inexpensive.
- Safety and Digestibility of Solids:
- Hazardous: Raw fruits with seeds, hard vegetables, nuts (choking/aspiration risks).
- Preparation: Beans, grain cereals, and vegetables should be well cooked and mashed.
- Homemade Food: Prefer fresh or frozen; canned foods (unless specifically for infants) may have too much sodium/sugar.
- Sweeteners: Refined sugar can be used if needed (avoid honey/corn syrup due to botulism risk).
- Supplements: Don't rely on food supplements as primary mineral sources. Encourage a variety of fruits, vegetables, and whole grains rich in natural iron.
Weaning: Transitioning to a Cup
Weaning is the process of moving from breast or bottle feeding to a cup.
- Psychological Significance: In Western societies, this is a significant task, as infants give up a major source of oral pleasure.
- Cultural Variations: Other cultures link weaning to specific life events (e.g., teething) or reaching a certain age.
- Timing: No single "best" time, but most infants show readiness during the second half of the first year. Weaning should be guided by the infant's needs.
- Signs of Readiness:
- Learning that "good things come from a spoon."
- Increasing desire for freedom of movement (less desire to be held for feedings).
- Improved control over actions, able to manipulate a cup.
- Imitation becomes a strong motivator (8-9 months), enjoying using a cup like others.
- Weaning Process:
- Gradual: Replace one bottle or breastfeeding at a time.
- Nighttime feeding is usually the last to go.
- Before 5-6 months: If breastfeeding ends, wean to a bottle (not in bed) to meet sucking needs.
- After 5-6 months (or 12-14 months): Weaning can be directly to a cup.
- Sugary Liquids: Any liquid with sucrose or other sugars (like fruit juice) should always be given in a cup, not a bottle.
1.2. Sleep and activity: rest, exploration, and development
Infant sleep patterns vary, and their natural drive for activity is paramount for development.
- Sleep Patterns:
- Variation: Active infants typically sleep less than milder ones.
- 3 Months: Most infants sleep approximately 15 total hours daily, with 9-11 hours nocturnal sleep and about three 1-2 hour daytime naps.
- Consolidation: Nighttime sleep hours increase, and daytime naps decrease during the first 12 months. By 1 year, infants sleep approximately 11.7 hours at night and may take one or two naps.
- Breastfed vs. Bottle-fed: Breastfed infants generally sleep for shorter periods and wake more frequently, especially at night.
- Factors Associated with Frequent Night Awakenings: Being a boy, breastfeeding, difficult temperament, and maternal depression. A pattern of less frequent awakenings is often seen by 6 months.
- (For sleep position and sleep problems, refer to Chapter 11.)
- Activity and Exploration:
- Most infants are naturally active and do not need encouragement to be mobile.
- Problematic Devices: Excessive use of devices like play yards, strollers, commercial swings, and walkers can limit an infant's natural curiosity and motor skill development. These restrict movement and prevent exploration.
- Walkers are dangerous: They do not enhance walking or coordination. They are dangerous if they tip over or are used near stairs, porches, decks, in-ground pools, or floor furnaces.
1.3. Dental health: starting early for a healthy smile
Good dental hygiene begins even before the first tooth erupts and is heavily influenced by early feeding practices.
- Early Counseling:
- Nurses should counsel parents early about maternal dental health and infant feeding practices that increase the risk of poor dental health.
- Avoid:
- Propping milk bottles or giving bottles in bed.
- Fruit juices in a bottle, especially before 6 months.
- These practices contribute to enamel erosion and early childhood caries (previously called "baby bottle tooth decay").
- Oral Hygiene Practices:
- First Teeth: Once primary teeth erupt, clean gums and teeth by wiping with a damp cloth. Toothbrushing is too harsh initially.
- Stabilization: Caregivers can cradle the infant with one arm to stabilize them, using the free hand to clean teeth.
- Making it Pleasant: Sing or talk to the infant during oral hygiene.
- Dental Home:
- Infants should have a brief oral health examination by 6 months from a qualified pediatric health practitioner.
- Identify high-risk infants for caries and provide oral health counseling.
- An infant should have an established dental home by 1 year of age.
- Toothbrushing (as more teeth erupt):
- Use a small, soft-bristled toothbrush.
- Water is preferred to toothpaste initially, as infants will swallow toothpaste.
- Fluoridated Toothpaste (AAPD Recommendations):
- "Smear" of fluoridated toothpaste for children younger than 2 years.
- Pea-size amount for those 2 to 5 years old.
- Fluoride Supplementation:
- Fluoride is essential for caries-resistant teeth.
- Needed beginning at 6 months of age if the infant does not receive water with adequate fluoride content.
- AAPD Recommendation (6 months to 3 years): 0.25 mg fluoride daily if water fluoride content is less than 0.3 ppm.
- Note: Fluoride dosage has decreased over time due to increased dental fluorosis from excessive ingestion.
- Bottled Water: If used for formula reconstitution, it should be fluoride-free or have low levels of fluoride.
- Dietary Considerations for Dental Health:
- Avoid foods with concentrated sugar (sucrose).
- Counsel parents about the detrimental effects of frequent and prolonged bottle-feeding or breastfeeding during sleep (nursing caries).
- Discourage coating pacifiers with honey or using hard-candy pacifiers (cariogenic, botulism risk from honey, aspiration risk from candy).
1.4.Safety promotion and injury prevention: protecting vulnerable infants
Injuries are a leading cause of death and non-fatal harm during infancy. Constant vigilance and anticipatory guidance are crucial.
- Injury Statistics:
- Leading cause of death (1-4 years): Unintentional injuries (accidents).
- Fifth leading cause of death (birth-12 months): Accidents.
- Top 3 accidental causes of death in infants: Suffocation, motor vehicle-related injuries, and drowning.
- Leading cause of non-fatal injuries in infants: Falls (account for about half of hospitalizations).
- Common sources of falls: Cribs, highchairs, baby walkers, changing tables, bouncers.
- Core Principles:
- Constant vigilance, awareness, and supervision are essential as infants gain locomotor and manipulative skills and develop insatiable curiosity.
- Injury prevention and parent education must be delivered on a growth and developmental basis.
- It's impossible to completely sterilize the environment, but many childhood deaths are due to preventable injuries.
- Nursing Role: Nurses must be aware of potential injury causes for each age group to provide anticipatory, preventive teaching.
- For example, discuss infant injury prevention guidelines (refer to Box 10.5 from the text) before the child reaches that susceptible age.
- Ideally, preventive teaching begins during pregnancy.
- Home Safety:
- One-third of all childhood injuries occur at home.
- Use a home safety checklist (like the one in the Family-Centered Care box) to increase parental awareness of hazards and encourage implementation of safety devices.
- Hands-on displays (cabinet latches, toilet seat locks) can familiarize parents with inexpensive safety products.
- The acronym SAFE PAD can help identify common types of injuries and associated objects.
- Motor Vehicle Injuries: Crucial for Infant Safety
Motor vehicle crashes are a major threat, but proper restraint dramatically reduces fatalities.
- Impact of Car Seats: Child safety seats have reduced fatalities by up to 71% in infants younger than 1 year.
- Ongoing Problem: Many infants are still injured or die due to improper restraint (inappropriate type or incorrect use).
- Studies show high incidence of incorrect car seat placement and installation.
- Lack of proper restraint is a major factor in fatal accidents.
- Mandate: All infants must be secured in federally approved restraints. Holding an infant or placing them unsecured in a seat is never safe.
- Rear-Facing is Safest:
- Infant restraints are either infant-only or convertible (infant-toddler) models.
- Both are semi-reclined and face the rear of the car.
- This position offers the best protection for an infant's disproportionately heavy head and weak neck. It spreads crash forces across the entire back, neck, and head, supporting the spine. A forward-facing seat would cause the head to whip forward, stressing the neck.
- Recommendation: All infants and toddlers should ride in rear-facing car safety seats until they reach age 2 years OR the weight limit recommended by the car seat manufacturer. Some infant-only seats go up to 35 lbs.
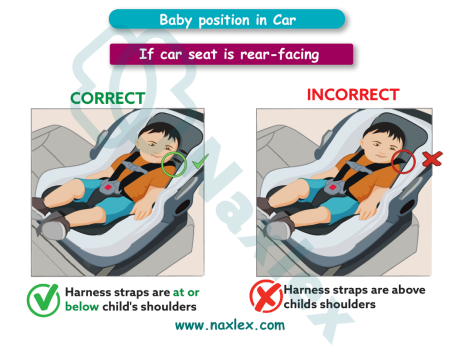
- Installation and Harnessing:
- Restraint is anchored with the vehicle's seat belt or the LATCH (lower anchor and tether for children) system.
- The restraint has a harness system to secure the infant. Some require a chest clip.
- Newer vehicles (post-1999) have tether straps for car seat anchors.
- LATCH System Weight Limit Change: Since 2014, if the combined weight of the child and car seat is more than 65 lbs (29.5 kg), parents should use the shoulder-lap belt restraint instead of the LATCH system for maximum protection.
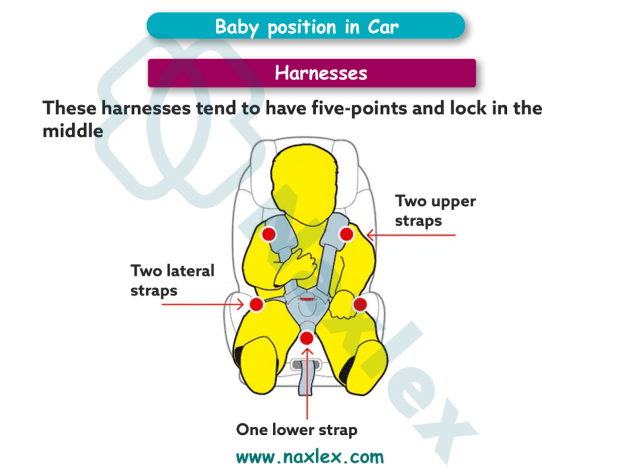
- Air Bag Danger:
- NEVER place a rear-facing infant safety seat in the front seat of a car equipped with an air bag on the passenger side. Deployment can cause severe injury or death because rear-facing seats extend closer to the dashboard.
-
- The back seat is always the safest place for children.
- Proper Use for Effectiveness:
- Dress infants in outfits with sleeves and legs to allow the harness to hold securely.
- A tightly rolled small blanket or towel on either side of the head can minimize movement.
- Padding between the infant's legs and crotch prevents slouching.
- Crucial: Do NOT place thick, soft padding under the infant or behind their back, as it will compress during impact, loosening the harness straps.
- Preterm Infants: Before discharge, preterm infants should be placed in their car seat as they would be in the car, and monitored for heart rate and oxygen saturation to detect airway occlusion.
- Burn safety and sun exposure
- Children should be kept out of direct sunlight, especially between 10 a.m. and 4 p.m.
- For the first 6 months of life, infants should have no sun exposure unless it is unavoidable.
- Methods should be used to protect children from sun exposure (e.g., they should wear clothing covering the skin, UVA and UVB protectants, and sunglasses).
- Sun protectants should be applied at least every 2 hours and always reapplied if child gets wet.
- Fire and smoke alarms should be located throughout the home.
- Yearly fire drills should be conducted with all members of the family.
- Dangerous items (e.g., matches, electrical cords, and electrical sockets) should be kept out of reach of children.
- Hot water heaters should be set at 120°F or lower.
- Pot handles should be turned away from the front of the stove.
- The knobs on stoves and ovens should be covered with child covers.
- Adults should stay away from children when eating or drinking hot substances or when smoking cigarettes.
- Children should be kept away from such things as grills, fi replaces, stoves, and radiators.
- Lead poisoning prevention
- At 9 months of age, blood lead screening should be performed, with hematocrit and hemoglobin assessments and with blood lead levels.
- Parents should be advised to wash their children’s hands and face frequently, especially before eating, to prevent ingestion of lead.
- Parents should be advised to clean their homes regularly to remove potential sources of lead.
Injury Prevention During Infancy
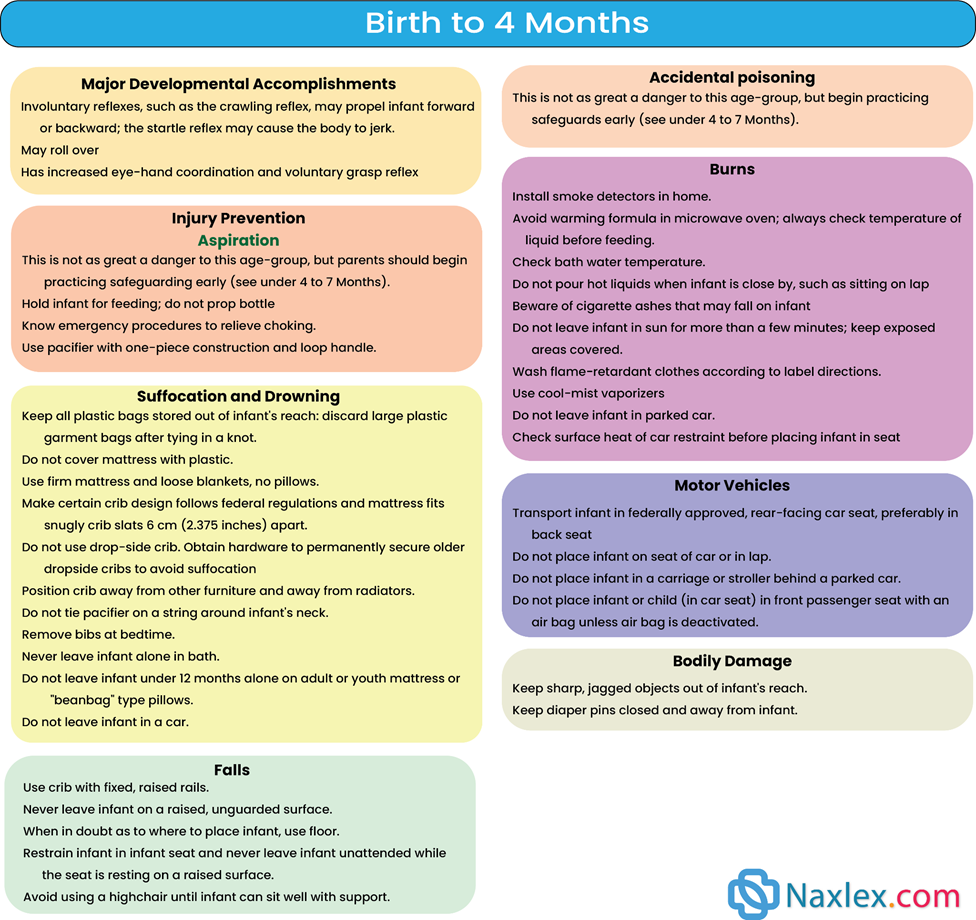
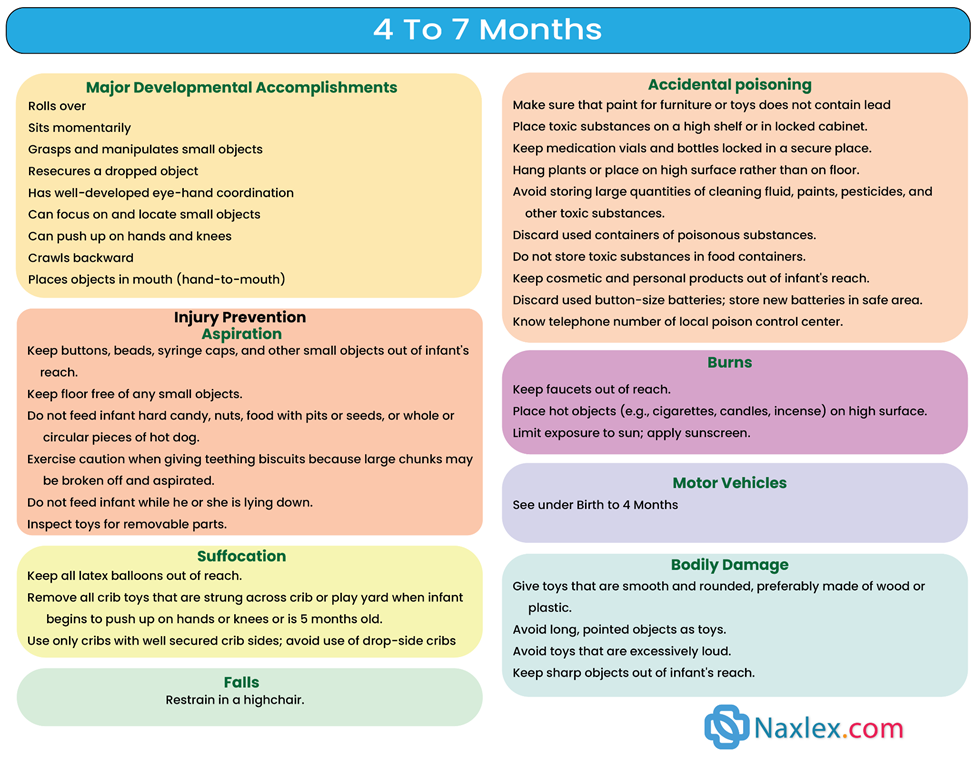
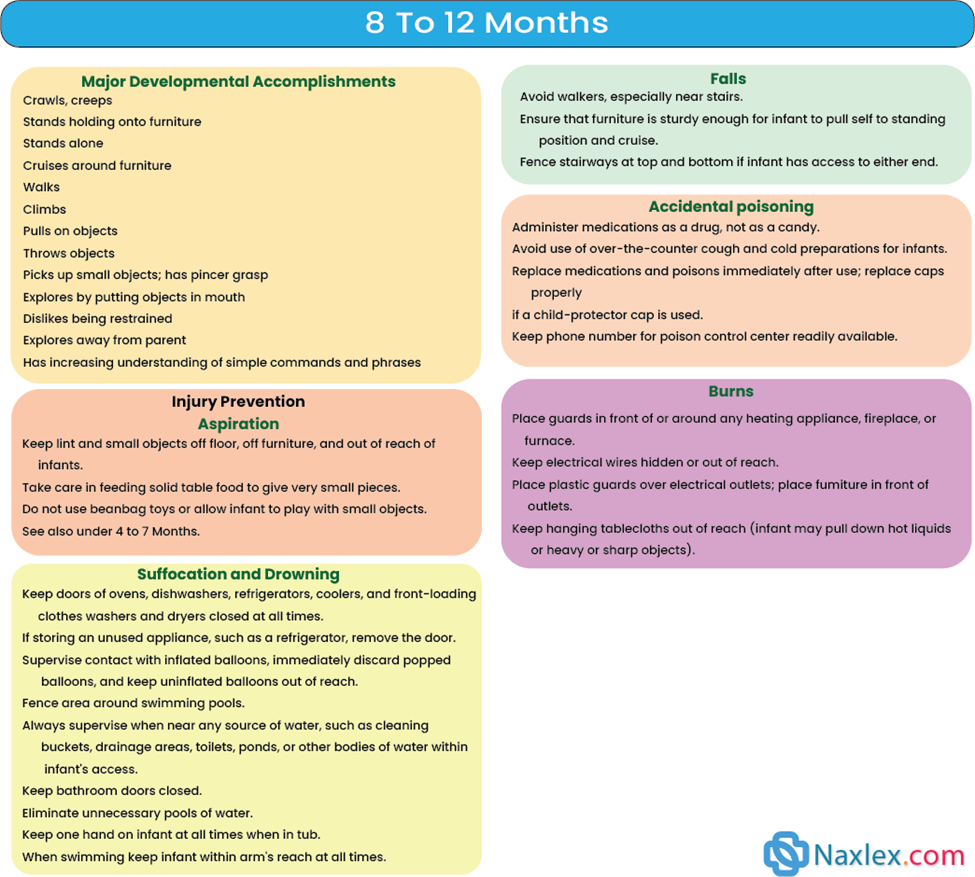 1.5. Immunization
1.5. Immunization
- The latest immunization schedule published by the Advisory Committee on Immunization Practices (ACIP) of the CDC should always be checked.
Recommended Immunization for the First Year of Life
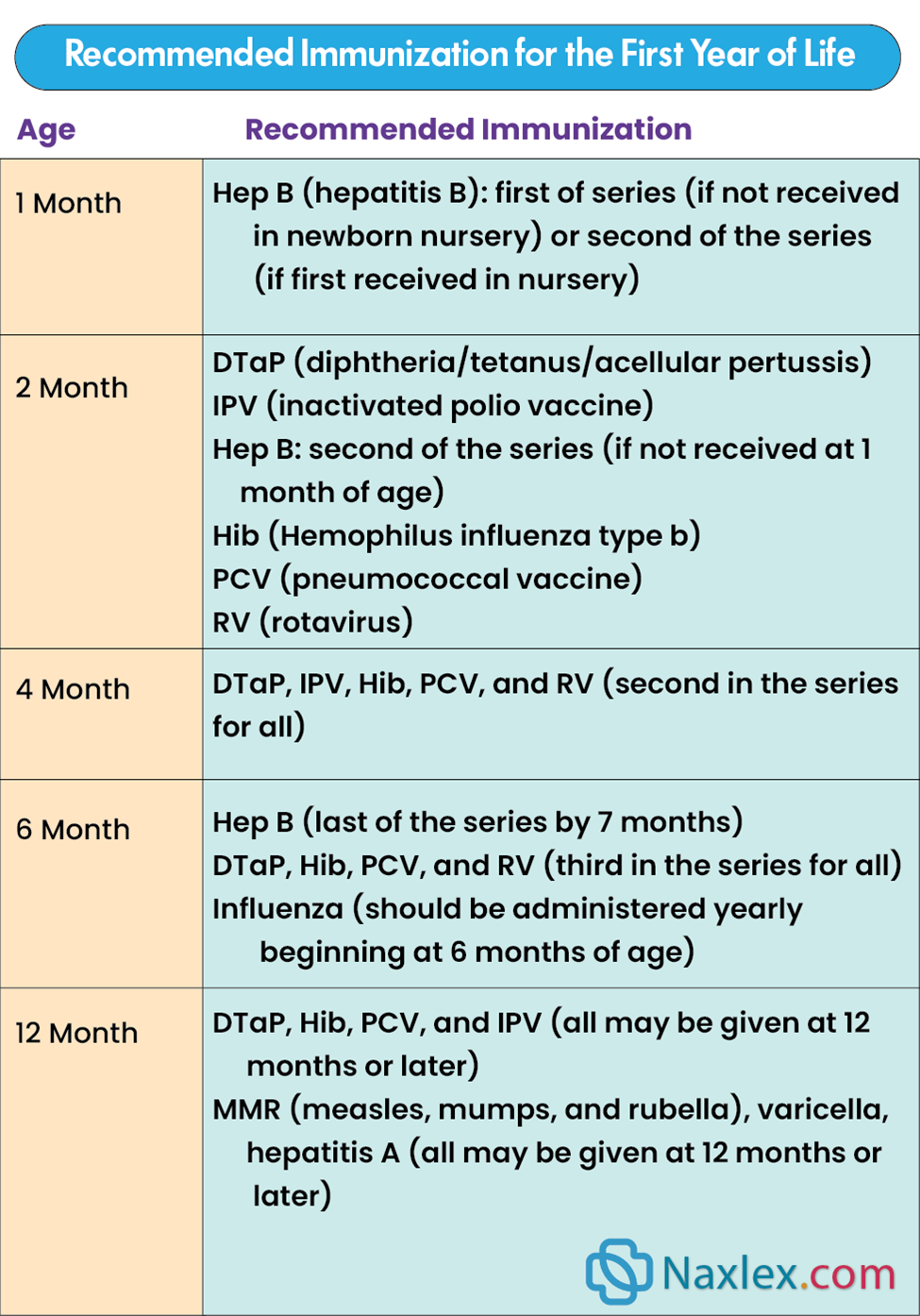
Summary
-
The mastery of infant growth and development requires a holistic nursing approach that balances clinical monitoring with parental support.
-
Biologic development is the most visible indicator of health, yet the nurse must be equally skilled in identifying the subtle shifts in psychosocial and cognitive domains.
-
Central to this is the concept of temperament; by identifying whether an infant is "easy," "slow-to-warm-up," or "difficult," the nurse can provide tailored strategies to improve the "goodness of fit" between the parent’s expectations and the child’s natural disposition. This decreases parental frustration and fosters a more secure attachment.
-
Addressing normal developmental concerns is a major component of pediatric nursing care. Nurses must prepare parents for the inevitable onset of separation and stranger anxiety, explaining these as positive signs of healthy attachment rather than behavioral problems.
-
Furthermore, guidance on limit setting, discipline, and the use of transitional objects, like pacifiers or thumb-sucking, helps parents establish healthy boundaries while meeting the infant's oral-sensory needs.
-
Teething, though a minor physiological event, often causes significant family stress, requiring the nurse to recommend safe, evidence-based comfort measures.
-
Promoting optimum health during infancy centers on the pillars of nutrition, safety, and prevention. The transition from breast milk or formula to solid foods is a critical nutritional milestone that requires careful timing and education.
-
The nurse must advocate for a safe sleep environment to prevent SIDS and emphasize the importance of the primary immunization series to protect the vulnerable infant from communicable diseases.
-
By integrating dental hygiene and rigorous injury prevention, such as car seat safety and "child-proofing", the nurse ensures that the infant’s rapid physical gains are protected by a proactive and informed care environment.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Growth And Development In Infants
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


