Please set your exam date
Drugs Used to Treat Dysrhythmias
Study Questions
Practice Exercise 1
A nurse in an outpatient facility is assessing a client who has taken procainamide (Pronestyl) to treat dysrhythmias for the last 12 months. The nurse should assess the client for which of the following adverse effects? Select all that apply
Explanation
Procainamide is a class Ia antiarrhythmicused to manage atrial and ventricular dysrhythmias by slowing myocardial conduction, prolonging the action potential, and stabilizing the cardiac membrane. Long-term therapy requires ongoing monitoring for cardiac conduction changes and systemic toxicities, as chronic use can lead to complications affecting multiple organ systems. Understanding the adverse effects is essential for early detection, prevention of serious complications, and ensuring safe pharmacologic management.
Rationale for correct answers:
2. Widened QRS complex.Procainamide slows ventricular conduction by blocking sodium channels. This prolongation of depolarization can be detected on an electrocardiogram (ECG) as a widened QRS complex. Persistent QRS widening may increase the risk of life-threatening ventricular arrhythmias, making monitoring essential during long-term therapy.
4. Easy bruising.Procainamide can induce bone marrow suppression, including thrombocytopenia, which reduces platelet counts and increases bleeding risk. Easy bruising or spontaneous bleeding is an important indicator of hematologic toxicity and requires prompt evaluation and possible medication adjustment or discontinuation.
5. Swollen joints.Long-term procainamide therapy can trigger drug-induced lupus erythematosus (DILE), characterized by musculoskeletal complaints such as arthralgia, myalgia, and swollen joints. Recognition of these symptoms is critical to prevent prolonged patient discomfort and complications, and discontinuation of the drug is often necessary for resolution.
Rationale for incorrect answers:
1. Hypertension.Procainamide does not typically cause hypertension; instead, it can sometimes lead to hypotension, particularly when administered intravenously. Therefore, hypertension is not a standard adverse effect.
3. Narrowed QT interval.Procainamide prolongs the action potential and repolarization, which actually increases the QT interval, not narrows it. A narrowed QT interval is unrelated to procainamide therapy.
Test-taking strategy:
• Focus on the pharmacologic class of the drug and its cardiac electrophysiology effects
• Consider long-term systemic toxicities, including hematologic and autoimmune reactions
• Eliminate options inconsistent with known ECG or systemic adverse effects
Take-home points:
• Procainamide can widen the QRS complex due to slowed ventricular conduction
• Long-term use may cause hematologic toxicity, presenting as easy bruising
• Drug-induced lupus is a possible complication, often manifesting as swollen joints and arthralgia
The nurse is administering lidocaine to a client. Which condition, if present in the client, is a caution for the use of this drug?
Explanation
The nurse is administering lidocaine, a class 1b antiarrhythmic medication, and considers renal dysfunctionas a caution because impaired renal function can alter the drug’s metabolism and excretion, increasing the risk of systemic toxicity. Lidocaine works by blocking sodium channels in cardiac cells, stabilizing the myocardial membrane, and reducing excitability in ventricles, making it effective for treating ventricular dysrhythmias. Nursing assessment must focus on monitoring for early signs of toxicity, vital signs, and renal function to ensure safe administration.
Rationale for correct answer:
4. Renal dysfunction.Lidocaine is metabolized primarily by the liver but has metabolites excreted by the kidneys. In clients with renal impairment, these metabolites can accumulate, potentially leading to central nervous system toxicity (drowsiness, confusion, seizures) and cardiovascular effects such as hypotension, bradycardia, or worsening arrhythmias. Nursing considerations include performing a thorough renal assessment, monitoring serum creatinine and BUN levels, observing for neurologic or cardiac changes, and adjusting the infusion rate or dose according to renal status.
Rationales for incorrect answers:
1. Tachycardia. While lidocaine affects cardiac conduction, the presence of tachycardia is not a contraindication or primary caution for administration. Lidocaine may actually be indicated in some cases to treat ventricular tachyarrhythmias. Careful monitoring of heart rate is important, but tachycardia alone does not pose a high risk of toxicity.
2. Hypertension. Elevated blood pressure does not affect the metabolism or excretion of lidocaine. The drug’s safety is not directly impacted by systemic hypertension, although blood pressure should always be monitored during administration.
3. Ventricular dysrhythmias. These are the therapeutic indication for lidocaine, not a caution. Presence of ventricular dysrhythmias signals the need for treatment, provided there are no significant comorbidities such as severe renal or hepatic dysfunction.
Test-taking strategy:
• Focus on conditions that affect metabolism and excretion of drugs, as these increase toxicity risk.
• Distinguish between therapeutic indications and contraindications/cautions.
• Prioritize patient safety by identifying organ dysfunction that alters pharmacokinetics.
Take-home points:
• Assess renal function before and during lidocaine therapy to prevent metabolite accumulation.
• Monitor for CNS and cardiovascular signs of toxicity, including confusion, dizziness, hypotension, and arrhythmias.
• Recognize that therapeutic indications (e.g., ventricular dysrhythmias) do not automatically preclude drug administration but require careful monitoring in at-risk clients.
The nurse is providing discharge teaching to a client newly prescribed propafenone for recurrent atrial fibrillation. Which client statement indicates correct understanding of the teaching?
Explanation
The nurse is providing discharge education to a client newly prescribed propafenone, a Class IC antidysrhythmic medicationused to manage recurrent atrial fibrillationby slowing cardiac conduction through sodium channel blockade. Client teaching must emphasize realistic expectations, adherence, and early recognition of adverse effects, as propafenone has a narrow therapeutic marginand can cause proarrhythmic and hemodynamic effects. Understanding when to report symptoms is essential for preventing complications and ensuring safe long-term therapy.
Rationale for correct answer:
4. “I will report dizziness to the healthcare provider.”Dizziness is a clinically significant adverse effect of propafenone. The drug slows myocardial conduction and may reduce cardiac output, leading to hypotension, bradycardia, or transient cerebral hypoperfusion. This manifests as dizziness or light-headedness. Additionally, propafenone has beta-adrenergic blocking properties, further increasing the risk of hemodynamic instability. Prompt reporting allows the healthcare provider to assess for dose-related toxicity, conduction abnormalities, and to adjust therapy as needed.
Rationales for incorrect answers:
1. “I should stop taking the medication if I feel palpitations.”Abrupt discontinuation of propafenone is unsafe and may precipitate rebound dysrhythmias or worsening atrial fibrillation. Palpitations should be reported, not managed independently by stopping the drug, as they may indicate either inadequate control or a proarrhythmic effect requiring medical evaluation.
2. “This medication will cure my heart rhythm problem.”Propafenone does not cure atrial fibrillation. It helps control rhythm and reduce recurrence, but atrial fibrillation is typically a chronic condition requiring long-term management. This statement reflects unrealistic expectations and inadequate understanding of the drug’s role.
3. “I will take this medication only when symptoms occur.”Propafenone is prescribed on a scheduled basisto maintain therapeutic plasma levels and prevent dysrhythmia recurrence. PRN use is inappropriate and can lead to ineffective rhythm control and increased arrhythmic risk.
Test-taking strategy:
• Identify statements reflecting safe medication use and appropriate symptom reporting.
• Eliminate options suggesting abrupt discontinuation, PRN use, or cure claims.
• Prioritize client understanding of adverse effect monitoring with antidysrhythmics.
Take-home points:
• Propafenone controls atrial fibrillation but does not cure it.
• Dizziness may indicate hemodynamic or conduction effects and must be reported promptly.
• Antidysrhythmic medications should be taken exactly as prescribed and never stopped abruptly.
Practice Exercise 2
A nurse is preparing to administer propranolol (Inderal) to a hospitalized client who has a dysrhythmia.
Which of the following nursing actions should the nurse plan to take while the client is receiving propranolol?
Explanation
Propranolol is a nonselective beta-adrenergic blockerused to treat dysrhythmias, hypertension, angina, and anxiety-related tachycardiaby blocking beta-1 and beta-2 receptors. This results in decreased heart rate, reduced myocardial contractility, and lowered blood pressure. Because propranolol affects cardiovascular reflexes that normally maintain blood pressure during position changes, careful nursing interventions are required to prevent complications such as orthostatic hypotension and falls.
Rationale for correct answer:
3. Assist the client when she sits up or stands after taking this medication.Propranolol reduces sympathetic nervous system activity, which normally causes vasoconstriction when a person changes position. By blunting this response, propranolol can lead to orthostatic hypotension, particularly in hospitalized clients who may be weak, volume-depleted, or on multiple antihypertensive medications. Sudden drops in blood pressure upon standing increase the risk for dizziness, syncope, and falls.
Rationale for incorrect answers:
1. Hold propranolol for an apical pulse greater than 100/min.Beta blockers are typically held for bradycardia, commonly defined as an apical pulse below 50 to 60 beats per minute, depending on institutional policy. A pulse greater than 100/min may indicate the need for the medication rather than withholding it.
2. Administer propranolol to increase the client’s blood pressure.Propranolol lowers blood pressure by decreasing cardiac output and inhibiting renin release. Administering it to raise blood pressure is incorrect and reflects a misunderstanding of the drug’s pharmacologic effect.
4. Check for hypokalemia frequently due to the risk for propranolol toxicity.Propranolol is not associated with hypokalemia. In some cases, beta blockers may slightly increase serum potassium levels by reducing cellular uptake. Routine potassium monitoring is not required specifically for propranolol toxicity.
Test-taking strategy:
• Recall the primary cardiovascular effects of beta blockers
• Focus on safety risks related to decreased heart rate and blood pressure
• Eliminate options that contradict known pharmacologic actions
• Prioritize nursing interventions that prevent injury and complications
Take-home points:
• Propranolol can cause orthostatic hypotension due to reduced sympathetic response
• Assist clients with position changes to prevent dizziness and falls
• Beta blockers lower heart rate and blood pressure and should not be used to increase them
A client with type 1 diabetes on insulin therapy reports that he takes propranolol (Inderal) for his hypertension. The nurse will teach the client to check glucose levels more frequently because of what concern?
Explanation
Propranolol is a non-selective beta-adrenergic blockercommonly prescribed for hypertension, angina, and certain dysrhythmias. While effective for cardiovascular management, non-selective beta blockers can interfere with the autonomic warning signs of hypoglycemiain clients with diabetes, such as tachycardia, palpitations, and tremors. Clients on insulin therapy need education on frequent blood glucose monitoringand recognition of atypical hypoglycemia symptoms to prevent severe complications.
Rationale for correct answer:
4. The propranolol may mask symptoms of hypoglycemia.Beta blockers blunt the sympathetic nervous system responses that typically alert patients to falling glucose levels. Non-selective beta blockers, like propranolol, reduce adrenergic symptoms such as tachycardia, tremors, and anxiety, while hypoglycemia may still progress to confusion, seizures, or loss of consciousness. This masking effect makes self-monitoring of blood glucose more critical, and clients should be educated to recognize alternative warning signs such as sweating, dizziness, or hunger.
Rationales for incorrect answers:
1. The propranolol can produce insulin resistance.While some beta blockers may modestly affect glucose metabolism, propranolol is not primarily associated with clinically significant insulin resistance; this is not the main safety concern requiring client education.
2. The two drugs used together will increase the risk of ketoacidosis.Propranolol does not precipitate diabetic ketoacidosis in insulin-dependent clients. Ketoacidosis risk is related to insufficient insulin or severe hyperglycemia, not beta-blocker therapy.
3. Propranolol will increase insulin requirements by antagonizing the effects at the receptors.Propranolol does not directly block insulin action at receptor sites. While it may mask hypoglycemia symptoms, it does not necessitate an automatic increase in insulin dosage.
Test-taking strategy:
• Consider the pharmacologic class and systemic effects of the drug
• Focus on interactions between cardiovascular agents and diabetes management
• Prioritize safety concerns related to symptom recognition and patient education
Take-home points:
• Non-selective beta blockers like propranolol can mask typical hypoglycemia symptoms
• Clients on insulin should monitor glucose levels more frequently
• Education should emphasize recognition of atypical hypoglycemia signs such as sweating, dizziness, or hunger
A nurse is assessing a client who has been taking amiodarone for 6 months. The nurse should monitor for which potential adverse effect?
Explanation
A client who has been taking amiodaronefor several months is at risk for multiple long-term adverse effectsdue to the drug’s lipophilic nature, large volume of distribution, and iodine content. Amiodarone is a class III antiarrhythmic agentused to manage life-threatening ventricular and supraventricular arrhythmias by prolonging the cardiac action potential and refractory period. Chronic therapy requires ongoing monitoringfor organ toxicity, particularly affecting the eyes, lungs, thyroid, liver, and skin, because amiodarone accumulates in tissues over time, leading to potential cumulative toxicity.
Rationale for correct answer:
3. “Photophobia.”One of the most common ocular adverse effects of long-term amiodarone therapy is corneal microdeposits, which can lead to photophobia, blurred vision, and halos around lights. These ocular changes are usually benign and reversible upon discontinuation, but clients may experience discomfort and visual sensitivity that warrants assessment and regular ophthalmologic evaluation. Nurses should instruct clients to report any changes in vision, wear sunglasses for protection, and schedule routine eye exams to detect early ocular toxicity.
Rationales for incorrect answers:
1. “Hyperglycemia.”Amiodarone does not typically alter glucose metabolism or produce hyperglycemia. While thyroid dysfunction secondary to amiodarone can indirectly affect metabolism, hyperglycemia is not a primary or expected adverse effect.
2. “Dysphagia.”Difficulty swallowing is not a recognized effect of amiodarone. Any report of dysphagia should prompt assessment for unrelated conditions, such as esophageal disorders, rather than attributing it to the medication.
4. “Urticaria.”Cutaneous reactions to amiodarone are generally limited to photosensitivity, blue-gray skin discoloration, or rash, not urticaria. This option misrepresents the typical dermatologic effects of the drug.
Test-taking strategy:
• Focus on long-term, tissue-accumulating adverse effects of amiodarone rather than acute side effects.
• Link ocular complaints, such as photophobia, to known corneal deposits.
• Exclude options that are not pharmacologically supported by amiodarone’s mechanism or common toxicity profile.
Take-home points:
• Monitor for ocular toxicity, including photophobia and visual disturbances, in clients on long-term amiodarone.
• Encourage routine eye examinations and protective measures such as sunglasses.
• Recognize that hyperglycemia, dysphagia, and urticaria are not expected adverse effects of amiodarone.
A client is in the clinic for a follow-up visit. He has been taking amiodarone (Cordarone) for almost 1 year, and today he tells the nurse, “I am noticing some blue color around my face, neck, and upper arms. Is that normal?” Which is the nurse's correct response?
Explanation
The nurse is caring for a client who has been taking amiodarone, a class III antiarrhythmic medicationused to treat ventricular and supraventricular dysrhythmias by prolonging the cardiac action potential and refractory period. Amiodarone has multiple systemic effects due to its lipophilic nature and long half-life, leading to potential adverse effects in the skin, lungs, thyroid, eyes, and liver. Client education focuses on monitoring for toxicity, reporting unusual findings promptly, and understanding which effects require immediate provider notification.
Rationale for correct answer:
3. “This can happen with amiodarone. I will let your doctor know about it right away.”Blue-gray discoloration of the skin, particularly in areas exposed to sunlight such as the face, neck, and arms, is a rare but documented adverse effect of long-term amiodarone therapy. This occurs due to photosensitivity and deposition of drug metabolites in the dermis, which can be permanent if exposure continues. Promptly reporting this finding to the healthcare provider ensures proper evaluation, possible dose adjustment, and counseling on sun protection and skin monitoring, which is crucial to preventing further complications and ensuring safe continuation of therapy.
Rationales for incorrect answers:
1. “This is an expected side effect and should go away soon.” While amiodarone has common side effects such as photosensitivity and mild skin reactions, blue-gray pigmentation is not transient and may be permanent if exposure continues. Minimizing sun exposure and consulting the provider is necessary; stating it will resolve soon is inaccurate.
2. “This is a harmless effect. As long as the medication is working, we’ll just monitor your skin.”Blue-gray skin discoloration is clinically significant and indicates chronic photosensitivity and drug deposition, which warrants evaluation. Passive monitoring without provider notification is unsafe because it may precede other systemic toxicity.
4. “How much sun exposure have you had recently?”While sun exposure can exacerbate photosensitivity, asking this alone does not address the seriousness of the skin change or prompt provider notification, which is required for appropriate management.
Test-taking strategy:
• Recognize statements that indicate potential drug toxicity versus harmless side effects.
• Prioritize interventions that promptly involve the healthcare provider for assessment and management.
• Identify long-term, irreversible adverse effects as requiring immediate attention.
Take-home points:
• Amiodarone can cause blue-gray skin discoloration, especially in sun-exposed areas.
• Clients should report unusual skin changes immediately to the provider.
• Management includes sun protection, medication review, and possible dose adjustment or discontinuation to prevent further complications.
Practice Exercise 3
A client with atrial fibrillation is being started on sotalol. Which nursing action is appropriate before administering the first dose?
Explanation
Sotalol is a Class III antidysrhythmic with nonselective beta-adrenergic blocking propertiesused in the management of atrial fibrillation and other tachydysrhythmias. Because sotalol significantly affects cardiac repolarizationand is eliminated almost entirely by the kidneys, safe initiation requires careful pre-administration assessment. Nursing responsibilities focus on identifying factors that increase the risk of drug accumulation, QT prolongation, and life-threatening ventricular dysrhythmias, particularly torsades de pointes.
Rationale for correct answer:
1. Assess serum creatinine level
Sotalol is primarily excreted unchanged by the kidneys. Impaired renal function leads to drug accumulation, prolonged half-life, and increased risk of QT interval prolongation, which can precipitate torsades de pointes, a potentially fatal ventricular dysrhythmia. Assessing serum creatinine allows the nurse and provider to evaluate renal clearance and determine whether dose adjustment or delayed initiationis necessary.
Rationales for incorrect answers:
2. Obtain a baseline blood glucose level
Although sotalol has beta-blocking effects that may mask symptoms of hypoglycemia, blood glucose monitoring is not the most critical assessment prior to the first dose. This action is secondary to renal and cardiac safety considerations.
3. Encourage increased oral fluid intake
While adequate hydration supports general cardiovascular and renal health, increased oral fluid intake does not directly address the primary risks associated with sotalol initiation. It does not prevent QT prolongation or drug accumulation.
4. Administer potassium supplementation prophylactically
Electrolyte balance, particularly potassium and magnesium levels, is important when using antidysrhythmics. However, prophylactic supplementation without documented hypokalemia is inappropriate and may cause hyperkalemia. Electrolytes should be assessed and corrected only if abnormal, not supplemented routinely.
Test-taking strategy:
• Identify the drug’s primary route of elimination and major safety risks.
• Prioritize assessments that prevent life-threatening adverse effects.
• Focus on renal function and cardiac conduction when initiating Class III antidysrhythmics.
Take-home points:
• Sotalol is renally excreted; impaired kidney function greatly increases toxicity risk.
• Baseline and ongoing serum creatinine monitoring is essential before and during therapy.
• Preventing QT prolongation and torsades de pointes is the nurse’s top priority when initiating sotalol.
A nurse is caring for a client whose supraventricular tachycardia (SVT) was treated with verapamil (Calan) IV. The client’s pulse rate is now 98/min and his blood pressure is 74/44 mg Hg. For which of the following IV medications should the nurse anticipate a prescription?
Explanation
Verapamil is a non-dihydropyridine calcium channel blockerthat works by inhibiting calcium influx through L-type calcium channelsin cardiac and smooth muscle cells. It is commonly used intravenously for the management of supraventricular tachycardia (SVT)because it slows AV nodal conduction, decreases heart rate, and reduces myocardial contractility. While effective, IV verapamil can precipitate severe hypotension, bradycardia, and myocardial depression, particularly due to excessive calcium channel blockade. When profound hypotension develops after IV verapamil administration, treatment focuses on reversing calcium channel blockade and supporting cardiac output.
Rationale for the correct answer:
1. Calcium gluconate. Calcium gluconate is the antidotal therapy for hemodynamic instability caused by calcium channel blockers such as verapamil. Verapamil blocks calcium entry into myocardial and vascular smooth muscle cells, leading to reduced myocardial contractility, vasodilation, and hypotension. Administration of IV calcium gluconate increases extracellular calcium concentration, which partially overcomes the competitive blockade at calcium channels. This restores calcium-dependent processes, improving cardiac contractility, vascular tone, and blood pressure.
Rationales for incorrect answers:
2. Sodium bicarbonate.Sodium bicarbonate is used primarily to treat metabolic acidosis, certain drug toxicities (such as tricyclic antidepressant overdose), or severe hyperkalemia. It has no role in reversing calcium channel blockade and would not correct the underlying cause of hypotension in this scenario.
3. Potassium chloride. Potassium chloride is indicated for hypokalemia, which may contribute to dysrhythmias. However, potassium does not counteract verapamil’s negative inotropic or vasodilatory effects. Administering potassium in a hypotensive client without documented hypokalemia could worsen cardiac conduction abnormalities.
4. Magnesium sulfate. Magnesium sulfate is commonly used for torsades de pointes, preeclampsia, or certain ventricular dysrhythmias. While magnesium can influence cardiac conduction, it does not reverse the calcium channel blockade-induced hypotension seen with verapamil toxicity and is therefore not the priority medication.
Test-taking strategy:
• Identify the cause of the adverse effect: in this case, excessive calcium channel blockade.
• Match the complication (severe hypotension) with the physiologic antidote.
• Eliminate options that treat unrelated electrolyte or acid–base disturbances.
Take-home points:
• IV verapamil can cause profound hypotension due to decreased myocardial contractility and vasodilation.
• Calcium gluconate is the first-line antidote for calcium channel blocker–induced hemodynamic instability.
• Always prioritize interventions that directly reverse the drug’s mechanism of action when managing medication-related emergencies.
A nurse is caring for a client on verapamil. The nurse understands that the medication should be used with extra caution in clients with which cardiovascular condition?
Explanation
Verapamil is a calcium channel blocker that slows conduction through the atrioventricular node, decreases myocardial contractility, and dilates coronary and peripheral arteries. It is used to treat hypertension, supraventricular tachycardia, and angina. However, because it has negative inotropic effects, it can exacerbate pre-existing heart failureby further decreasing cardiac contractility and cardiac output. Understanding the drug’s hemodynamic effects is essential for safe administration and client monitoring.
Rationale for correct answer:
3. Heart failure.Verapamil’s negative inotropic properties can reduce the heart’s pumping ability, worsening symptoms in clients with heart failure. This can lead to fluid retention, pulmonary congestion, and decreased tissue perfusion. Nurses must assess for signs of worsening heart failure, such as dyspnea, edema, and weight gain, before and during verapamil therapy. Its use is contraindicated in severe left ventricular dysfunction and should be used cautiously in mild to moderate cases.
Rationales for incorrect answers:
1. Hypertension.Verapamil is frequently used to manage hypertension through arterial vasodilation. It reduces systemic vascular resistance, which lowers blood pressure effectively, making it appropriate for this condition.
2. Tachycardia.Verapamil slows heart rate by depressing AV nodal conduction, making it suitable for treating certain tachyarrhythmias such as supraventricular tachycardia. It is not contraindicated unless accompanied by severe heart failure or AV block.
4. Angina.Verapamil is effective for vasospastic and effort-related angina by dilating coronary arteries and reducing myocardial oxygen demand. It is a first-line or adjunct therapy in clients with stable or Prinzmetal’s angina.
Test-taking strategy:
• Focus on the pharmacologic effects of calcium channel blockers, especially negative inotropy
• Identify conditions where reduced cardiac contractility could worsen the disease state
• Exclude conditions that are indications for the drug rather than contraindications
Take-home points:
• Verapamil decreases myocardial contractility and AV nodal conduction
• Avoid or use caution in clients with heart failure due to risk of exacerbation
• It is safe and effective for hypertension, angina, and certain tachyarrhythmias when heart failure is not present
A client is in the emergency department with new-onset rapid-rate atrial fibrillation. The nurse is about to add a continuous infusion of diltiazem (Cardizem) at 5 mg/hr but must first give a bolus of 0.25 mg/kg over 2 minutes. The client weighs 220 pounds. The medication comes in a vial of 25 mg/5 mL. How many milligrams will the client receive for the bolus dose and how many milliliters will the nurse draw up for this dose?
Explanation
Step 1: Convert the client's weight from pounds to kilograms. To convert pounds to kilograms, divide the weight by 2.2. 220 lbs / 2.2 = 100 kg.
Step 2: Calculate the required dose in milligrams (mg). Multiply the client's weight in kilograms by the ordered dose (0.25 mg/kg). 100 kg * 0.25 mg/kg = 25 mg.
Step 3: Identify the concentration of the available medication. The vial contains 25 mg in 5 mL (25 mg/5 mL).
Step 4: Calculate the volume in milliliters (mL) needed for the dose. Divide the desired dose by the concentration on hand (or use the ratio). (25 mg / 25 mg) * 5 mL = 5 mL.
Final answer: The client will receive a bolus dose of 25 mg, and the nurse will draw up 5 mL.
Test-Taking Strategy:
- Always perform weight conversions as the very first step of your calculation to avoid using the wrong numerical base for the rest of the problem.
- Identify and ignore "filler" information, such as the 5 mg/hr infusion rate, which is not needed to calculate the bolus dose.
- Use the "Desired over Have" formula (Desired 25 mg / Have 25 mg * Volume 5 mL) to quickly verify the final volume.
Take-Home Points:
- Diltiazem is a calcium channel blocker used to slow the ventricular rate in patients with atrial fibrillation.
- Bolus doses of potent cardiac medications must be administered slowly over the specified timeframe (in this case, 2 minutes) to prevent sudden hypotension.
- Continuous monitoring of blood pressure and heart rate is mandatory when initiating a diltiazem bolus and subsequent infusion.
A client with a rapid, irregular heart rhythm is being treated in the emergency department with adenosine. During administration of this drug, the nurse will be prepared to monitor the client for which effect?
Explanation
A client with a rapid, irregular heart rhythmmay be experiencing supraventricular tachycardia (SVT), a condition characterized by a sudden onset of abnormally fast heartbeats originating above the ventricles. Adenosineis an antiarrhythmic agentused in acute care to terminate SVT by temporarily blocking atrioventricular (AV) nodal conduction. Its extremely short half-life (less than 10 seconds) allows it to act quickly and transiently, making it ideal for rapid rhythm conversion. Nursing monitoring during administration is critical because adenosine can cause transient cardiovascular effects, including brief asystole or heart block, which may be alarming to clients if unprepared.
Rationale for correct answer:
2. “A brief period of systole.”Adenosine works by slowing conduction through the AV node, which can result in a momentary pause in cardiac electrical activity, appearing as transient asystole or systole on the monitor. This effect is expected, short-lived, and usually resolves spontaneously within seconds, but the nurse must be prepared to reassure the client and monitor for return of a normal sinus rhythm. This brief interruption allows the heart to reset its electrical conduction and terminate the abnormal tachycardic rhythm. Continuous cardiac monitoring and IV access are essential for safety during administration.
Rationales for incorrect answers:
1. “Nausea and vomiting.” These are not common or expected acute effects of adenosine. While mild nausea may occur occasionally, it is not the primary concern during IV administration and does not necessitate immediate monitoring.
3. “Muscle tetany.”Adenosine does not affect skeletal muscle function or calcium channels in a manner that produces tetany. Monitoring for this is unnecessary.
4. “Hypertension.”Adenosine typically causes transient hypotension, not hypertension, due to its vasodilatory and AV nodal slowing effects. Therefore, preparing for hypertension is inappropriate.
Test-taking strategy:
• Focus on the pharmacologic action of adenosine and its effects on cardiac conduction.
• Expect transient asystole or pauses and distinguish them from adverse reactions requiring intervention.
• Remember the drug’s extremely short half-life; effects are brief and self-limiting.
Take-home points:
• Adenosine can cause a brief period of asystole during administration; monitor continuously.
• Clients may feel momentarily light-headed, chest pressure, or palpitations during this pause; reassurance is important.
• The drug is short-acting and effective for terminating SVT, but preparation for emergency support is always essential.
A client is receiving digoxin for treatment of atrial fibrillation. When you enter the room to give the medication, you find the client irritable and complaining of nausea and blurred vision. She’s also disoriented to place and time. The most appropriate action at this time is to:
Explanation
The nurse is caring for a client who has been taking amiodarone, a class III antiarrhythmic drugused to treat life-threatening ventricular and supraventricular dysrhythmias by prolonging cardiac repolarization and refractory periods. Due to its lipophilic properties and long half-life, amiodarone can accumulate in multiple tissues, leading to systemic effects, including dermatologic, pulmonary, hepatic, and thyroid toxicity. Client education emphasizes early recognition of adverse effects, timely reporting, and preventive strategiesto reduce complications while continuing therapy safely.
Rationale for correct answer:
3. “This can happen with amiodarone. I will let your doctor know about it right away.”Blue-gray skin discoloration in sun-exposed areas is a rare but documented adverse effect of long-term amiodarone therapy. It occurs due to photosensitivity and deposition of drug metabolites in the dermis, and the pigmentation may be permanent if exposure continues. Promptly notifying the healthcare provider ensures assessment, evaluation for other systemic toxicities, reinforcement of sun protection strategies, and discussion of whether dose modification or discontinuation is needed.
Rationales for incorrect answers:
1. “This is an expected side effect and should go away soon.”Blue-gray pigmentation is not transient and may persist despite continued therapy. Describing it as temporary is misleading and may delay provider intervention.
2. “This is a harmless effect. As long as the medication is working, we’ll just monitor your skin.” While amiodarone efficacy is important, this skin change indicates potential chronic photosensitivity and tissue accumulation, which requires provider evaluation. Passive monitoring alone is unsafe.
4. “How much sun exposure have you had recently?”Although sun exposure worsens pigmentation, asking this does not address the seriousness of the adverse effect or prompt appropriate clinical action. Immediate provider notification is required.
Test-taking strategy:
• Identify statements that indicate serious, potentially irreversible adverse effects.
• Prioritize responses that involve the healthcare provider promptly.
• Distinguish between minor side effects and clinically significant toxicity.
Take-home points:
• Amiodarone may cause blue-gray pigmentation, particularly in sun-exposed areas.
• Clients must report unusual skin changes immediately.
• Management includes sun protection, provider evaluation, and possible dose adjustment or discontinuation.
The client is receiving digoxin for treatment of heart failure. Which finding would suggest to the nurse that heart failure is improving?
Explanation
The nurse is caring for a client receiving digoxin, a cardiac glycosideused to manage heart failure and certain dysrhythmias. Digoxin works by increasing myocardial contractility (positive inotropy) and decreasing conduction through the atrioventricular node, which improves cardiac output and reduces heart failure symptoms. Monitoring for therapeutic effectiveness involves assessing signs of improved perfusion, fluid balance, and symptom relief, which guide ongoing management and medication titration.
Rationale for correct answer:
2. “Absence of peripheral edema.”One of the hallmark signs of improved heart failure is a reduction in fluid retention, particularly peripheral edema. As cardiac output improves with digoxin therapy, venous return and renal perfusion increase, promoting diuresis and decreasing swelling in the extremities. Monitoring for diminished edema is a direct and clinically reliable indicator that heart failure is improving and therapy is effective.
Rationales for incorrect answers:
1. “Pale and cool extremities.”These findings suggest poor perfusion, which is a sign of ongoing heart failure and inadequate cardiac output. They do not indicate improvement and may signal worsening of the condition.
3. “Urine output of 60 mL/4 h.”This is below normal expected output (typically 30 mL/h or 120 mL/4 h) and may indicate decreased renal perfusion, a sign of persistent heart failure or pre-renal compromise. It does not reflect improvement.
4. “Complaints of increasing dyspnea.” Worsening shortness of breath indicates progression or exacerbation of heart failure, suggesting inadequate symptom control. Improvement would be evidenced by decreased dyspnea on exertion and improved activity tolerance.
Test-taking strategy:
• Identify clinical indicators that reflect improved cardiac function and fluid balance.
• Distinguish between signs of ongoing heart failure versus signs of therapeutic improvement.
• Focus on objective, measurable outcomes, such as edema reduction, urine output, and symptom relief.
Take-home points:
• Absence of peripheral edema is a key indicator of improved heart failure.
• Worsening perfusion, decreased urine output, or increasing dyspnea suggest ongoing or worsening heart failure.
• Monitoring objective and subjective signs guides assessment of digoxin effectiveness and overall heart failure management.
Comprehensive Questions
A nurse is caring for four clients who are each taking digoxin (Lanoxin). The client who is taking which of the following medications concurrently is at risk for digoxin toxicity?
Explanation
Digoxinis a cardiac glycoside used in the management of heart failure and certain dysrhythmias. It has a narrow therapeutic index. Digoxin is primarily eliminated unchanged by the kidneysand is a substrate for P-glycoprotein, a transport protein involved in drug absorption and renal excretion. Many clinically significant drug interactions occur when a concurrent medication interferes with digoxin clearance, resulting in accumulation and toxic effects.
Rationale for correct answer:
4. Amiodarone (Cordarone) for ventricular dysrhythmias.Amiodarone significantly increases serum digoxin levels and is one of the most clinically important drug interactions associated with digoxin toxicity. Amiodarone inhibits P-glycoprotein, reducing digoxin efflux from intestinal cells and decreasing renal tubular secretion. This results in increased digoxin absorption and reduced elimination, causing serum concentrations to rise even when the digoxin dose remains unchanged. In addition, amiodarone has an extremely long half-life, allowing its inhibitory effects to persist for weeks. Coadministration can raise digoxin levels by up to 100 percent, often requiring a 50 percent dose reduction. This combination places the client at a high risk for toxicity and requires close monitoring.
Rationale for incorrect answers:
1. Procainamide (Pronestyl) for premature ventricular contractions.Procainamide affects cardiac conduction by blocking sodium channels but does not significantly interfere with digoxin metabolism, renal clearance, or P-glycoprotein activity. Although both drugs affect the heart, procainamide does not meaningfully increase digoxin serum levels and is not strongly associated with digoxin toxicity.
2. Ranitidine (Zantac) for peptic ulcer disease.Ranitidine is an H2-receptor antagonist with minimal effects on hepatic enzymes and drug transport systems. Unlike cimetidine, it does not significantly alter digoxin absorption or elimination, making toxicity unlikely.
3. Phenytoin (Dilantin) for a seizure disorder.Phenytoin induces hepatic enzymes and may actually lower digoxin levels rather than increase them. Digoxin is not primarily metabolized by the liver, and phenytoin does not inhibit P-glycoprotein, reducing the risk of toxicity.
Test-taking strategy:
• Identify medications known to inhibit digoxin clearance
• Focus on drugs with strong pharmacokinetic interactions
• Prioritize agents with documented effects on P-glycoprotein
• Eliminate medications that do not significantly affect renal elimination
Take-home points:
• Digoxin toxicity is commonly caused by drug interactions that reduce elimination
• Amiodarone markedly increases digoxin levels and requires dose adjustment
• Close monitoring is essential when digoxin is combined with antiarrhythmic agents
A client with type 1 diabetes on insulin therapy reports that he takes propranolol (Inderal) for his hypertension. The nurse will teach the client to check glucose levels more frequently because of what concern?
Explanation
Propranolol is a non-selective beta-adrenergic blockercommonly prescribed for hypertension, angina, and certain dysrhythmias. While effective for cardiovascular management, non-selective beta blockers can interfere with the autonomic warning signs of hypoglycemiain clients with diabetes, such as tachycardia, palpitations, and tremors. Clients on insulin therapy need education on frequent blood glucose monitoringand recognition of atypical hypoglycemia symptoms to prevent severe complications.
Rationale for correct answer:
4. The propranolol may mask symptoms of hypoglycemia.Beta blockers blunt the sympathetic nervous system responses that typically alert patients to falling glucose levels. Non-selective beta blockers, like propranolol, reduce adrenergic symptoms such as tachycardia, tremors, and anxiety, while hypoglycemia may still progress to confusion, seizures, or loss of consciousness. This masking effect makes self-monitoring of blood glucose more critical, and clients should be educated to recognize alternative warning signs such as sweating, dizziness, or hunger.
Rationales for incorrect answers:
1. The propranolol can produce insulin resistance.While some beta blockers may modestly affect glucose metabolism, propranolol is not primarily associated with clinically significant insulin resistance; this is not the main safety concern requiring client education.
2. The two drugs used together will increase the risk of ketoacidosis.Propranolol does not precipitate diabetic ketoacidosis in insulin-dependent clients. Ketoacidosis risk is related to insufficient insulin or severe hyperglycemia, not beta-blocker therapy.
3. Propranolol will increase insulin requirements by antagonizing the effects at the receptors.Propranolol does not directly block insulin action at receptor sites. While it may mask hypoglycemia symptoms, it does not necessitate an automatic increase in insulin dosage.
Test-taking strategy:
• Consider the pharmacologic class and systemic effects of the drug
• Focus on interactions between cardiovascular agents and diabetes management
• Prioritize safety concerns related to symptom recognition and patient education
Take-home points:
• Non-selective beta blockers like propranolol can mask typical hypoglycemia symptoms
• Clients on insulin should monitor glucose levels more frequently
• Education should emphasize recognition of atypical hypoglycemia signs such as sweating, dizziness, or hunger
A client is given a prescription for propranolol (Inderal) 40 mg bid. What is the most important instruction the nurse should give to this client?
Explanation
A nurse is teaching a client who has been prescribed propranolol, a non-selective beta-adrenergic blockerused to manage hypertension, angina, and certain dysrhythmias. Effective client education is essential to prevent serious complications, ensure therapeutic effectiveness, and promote adherence. One of the most critical aspects of propranolol therapy is the gradual tapering of the dosewhen discontinuing treatment to avoid rebound cardiovascular effects.
Rationale for correct answer:
2. “Do not stop taking this medication abruptly; the dosage must be decreased gradually if it is discontinued.” Abrupt cessation of propranolol can lead to rebound tachycardia, hypertension, and exacerbation of angina, and in some cases may precipitate myocardial infarction in high-risk clients. Tapering allows the cardiovascular system to adjust slowly, minimizing risks associated with sudden withdrawal. This instruction is crucial for client safety and adherence to the prescribed regimen.
Rationales for incorrect answers:
1. “Take this medication on an empty stomach, as food interferes with its absorption.”Propranolol can be taken with or without food. While food may slightly delay absorption, it does not significantly affect therapeutic outcomes, so this instruction is not essential.
3. “If the client experiences any disturbances in hearing, the client should notify the health care provider immediately.”Propranolol is not ototoxic. Hearing disturbances are unrelated to beta-blocker therapy and do not require specific monitoring in this context.
4. “The client may become very sleepy while taking this medication, do not drive.”Fatigue or mild drowsiness may occur, but it is not the most critical teaching point for propranolol. While safety precautions are useful, preventing rebound cardiovascular events through proper tapering is far more important.
Test-taking strategy:
• Prioritize teaching points that prevent serious, life-threatening complications.
• Distinguish between common, mild side effects and critical safety precautions.
• Remember that abrupt discontinuation of beta blockers can trigger severe cardiovascular events.
Take-home points:
• Always taper propranolol gradually to avoid rebound angina, tachycardia, or hypertension.
• Fatigue and mild drowsiness may occur, but they are secondary considerations compared to abrupt withdrawal risks.
• Propranolol can be taken with or without food, and ototoxicity is not a concern.
A client was admitted from the emergency department after receiving treatment for dysrhythmias and will be started on amiodarone (Cordarone, Pacerone) because of lack of therapeutic effects from his other antidysrhythmic therapy. When the nurse checks with him in the afternoon, he complains of feeling light-headed and dizzy. What will the nurse assess first?
Explanation
A client is being started on amiodarone, a class III antiarrhythmicused for the management of ventricular and supraventricular dysrhythmias when other therapies are ineffective. Amiodarone works by prolonging the cardiac action potential and refractory period, which stabilizes cardiac rhythm. Nursing assessment during administration is critical because the drug can cause hemodynamic instability, including hypotension and bradycardia. When a client reports dizziness or light-headedness, immediate assessment should focus on vital signs, as these symptoms may indicate cardiovascular compromise.
Rationale for correct answer:
4. “Whether the client’s pulse and blood pressure are within normal limits.”Light-headedness and dizziness in a client receiving amiodarone may be early signs of hypotension or bradycardia, which are common adverse effects due to negative chronotropic and vasodilatory properties of the drug. Assessing the pulse and blood pressure first allows the nurse to identify hemodynamic instability promptly and initiate appropriate interventions, such as adjusting medication dosage, implementing safety precautions, or notifying the healthcare provider. Prioritizing vital signs ensures client safety and rapid response to potentially life-threatening events.
Rationales for incorrect answers:
1. “Whether there is the possibility of sleep deprivation from the stress of admission to the hospital.”While sleep deprivation may contribute to fatigue or dizziness, it is not an immediate life-threatening cause. Vital signs should be assessed first to rule out acute cardiovascular compromise.
2. “Whether an allergic reaction is occurring with anticholinergic-like symptoms.” Amiodarone rarely causes allergic reactions with anticholinergic symptoms. Focusing on this at this moment delays identification of hemodynamic instability, which is more urgent.
3. “Whether the amiodarone level is not yet therapeutic enough to treat the dysrhythmias.” Therapeutic plasma levels develop over time; dizziness and light-headedness are not usually due to subtherapeutic drug levels but are more likely adverse effects of the current dose, making this assessment less urgent.
Test-taking strategy:
• Prioritize assessments that identify life-threatening or hemodynamically significant complications first.
• Recognize that dizziness and light-headedness in clients on antiarrhythmics often indicate hypotension or bradycardia.
• Consider pharmacologic properties and adverse effect profiles when determining initial nursing assessments.
Take-home points:
• Amiodarone can cause hypotension and bradycardia; monitor vital signs frequently.
• Early recognition of cardiovascular compromise ensures prompt intervention and safety.
• Always assess acute symptoms in the context of drug therapy before exploring less critical causes.
The nurse is assessing a client who has been taking quinidine who asks about adverse effects. Which of these are potential adverse effects of quinidine? Select all that apply
Explanation
A client taking quinidine, a class IA antiarrhythmic medication, should be educated about its potential adverse effectsdue to its sodium channel-blocking propertiesand impact on cardiac conduction, gastrointestinal function, and auditory perception. Quinidine is used to treat supraventricular and ventricular arrhythmiasby slowing depolarization, prolonging the action potential, and decreasing myocardial excitability. Long-term therapy requires careful monitoringfor both cardiac and systemic toxicities, as adverse effects can affect adherence and overall safety.
Rationale for correct answers:
2. “Tinnitus.”Quinidine is associated with cinchonism, a syndrome of quinoline-related toxicity that includes tinnitus, headache, dizziness, and blurred vision. Tinnitus is often one of the first signs of quinidine toxicity, making it important for the nurse to assess and teach the client to report ringing in the ears or hearing changes promptly.
4. “Diarrhea.”Gastrointestinal adverse effects are common with quinidine due to its direct irritant effect on the GI tract. Clients may experience nausea, vomiting, abdominal cramping, and diarrhea, which are often dose-related. Nursing education should include managing GI discomfort, monitoring hydration, and contacting the provider for severe symptoms.
5. “Anorexia.”Quinidine can also cause loss of appetite, which is another manifestation of GI disturbance. This may be subtle but can impact nutritional intake and weight, especially in long-term therapy.
Rationales for incorrect answers:
1. “Muscle pain.”Muscle pain, or myopathy, is not a recognized adverse effect of quinidine. While other antiarrhythmics or cardiovascular medications may contribute to musculoskeletal complaints, quinidine primarily affects the heart, GI system, and auditory system.
3. “Dyspnea.”Shortness of breath is not a typical effect of quinidine unless secondary to an underlying cardiac condition. Quinidine does not directly cause respiratory compromise and should not be expected as a drug-induced effect.
Test-taking strategy:
• Identify common systemic adverse effects of quinidine, focusing on cinchonism and gastrointestinal effects.
• Eliminate options unrelated to quinidine’s known toxicity profile.
• Remember that early signs of toxicity, such as tinnitus, require prompt assessment and intervention to prevent progression.
Take-home points:
• Tinnitus is an early sign of quinidine toxicity and should be reported immediately.
• Gastrointestinal adverse effects, including diarrhea and anorexia, are common and may affect adherence.
• Muscle pain and dyspnea are not typical adverse effects of quinidine and should prompt assessment for other causes.
The nurse is teaching a client about taking an antidysrhythmic drug, which of the following statements by the nurse are correct? Select all that apply
Explanation
The nurse is teaching a client about antidysrhythmic drug therapy, which is used to control abnormal heart rhythmsby altering cardiac electrical conduction, automaticity, or refractoriness. Effective teaching focuses on proper administration, adherence, recognition of adverse effects, and safety precautions. Understanding how to take the medication ensures therapeutic effectiveness while minimizing complications such as toxicity, gastrointestinal upset, or therapeutic failure.
Rationale for correct answer:
2. “Do not chew sustained-release capsules.”Sustained-release formulations are designed to release medication slowly over time, maintaining therapeutic plasma levels and preventing peaks that could increase toxicity risk. Chewing these capsules destroys the release mechanism, potentially resulting in rapid absorption, increased side effects, and decreased safety. Clients should be instructed to swallow these capsules whole.
5. “If stomach upset occurs, you may take the medication with food.”Some antidysrhythmic drugs can cause gastrointestinal irritation when taken on an empty stomach. Taking the medication with food can help minimize nausea, dyspepsia, or abdominal discomfort without significantly affecting absorption, ensuring the client maintains adherence and avoids skipping doses.
Rationales for incorrect answers:
1. “Take the medication with an antacid if stomach upset occurs.”Antacids can interfere with the absorption of certain antidysrhythmic drugs, reducing their therapeutic effect. Instead of using antacids routinely, taking the drug with food is the preferred method to minimize gastrointestinal upset.
3. “If a weight gain of 5 pounds occurs within 1 week, notify your physician at the next office visit.”Rapid weight gain may indicate fluid retention, which is clinically significant and warrants immediate notification rather than waiting until the next scheduled visit, particularly in clients with potential heart failure. Delayed reporting can lead to complications.
5. “If you experience severe adverse effects, stop the drug and notify your physician.”Abruptly stopping an antidysrhythmic medication can precipitate rebound arrhythmias or exacerbation of the underlying dysrhythmia, which may be life-threatening. Clients should contact their provider before discontinuing to ensure a safe plan.
Test-taking strategy:
• Focus on statements that ensure safe, effective drug administration.
• Identify instructions that prevent toxicity, maintain therapeutic levels, and manage minor adverse effects safely.
• Distinguish between safe interventions (food, swallowing capsules whole) versus unsafe practices (chewing, stopping abruptly, using antacids).
Take-home points:
• Do not chew or crush sustained-release antidysrhythmic capsules.
• Taking medication with food is acceptable to reduce gastrointestinal upset.
• Report severe side effects promptly but never stop therapy abruptly without provider guidance.
The client’s serum digoxin level is 3.0 ng/mL. What does the nurse know about this serum digoxin level?
Explanation
The nurse is monitoring a client taking digoxin, a cardiac glycosideused to treat heart failure and certain atrial dysrhythmias. Therapeutic monitoring of serum digoxin levels is crucial because the therapeutic window is narrow, and levels above the recommended range increase the risk of digoxin toxicity, which can have serious cardiac and systemic consequences. Understanding normal and toxic levels allows the nurse to recognize early signs of toxicity, intervene appropriately, and prevent life-threatening complications.
Rationale for correct answer:
1. “It is in the high (elevated) range.”The therapeutic serum digoxin range for heart failure is typically 0.5–2.0 ng/mL. A serum level of 3.0 ng/mL exceeds the upper limit, indicating elevated digoxin levels. At this concentration, the client is at significant risk for digoxin toxicity, which may present as arrhythmias, nausea, vomiting, visual changes (e.g., blurred vision, yellow-green halos), and confusion. Immediate assessment and collaboration with the healthcare provider are warranted, including possible withholding of the drug, monitoring for toxicity, and evaluating contributing factors such as renal function or drug interactions.
Rationales for incorrect answers:
2. “It is in the low (decreased) range.”This is inaccurate because a level below 0.5 ng/mL would indicate subtherapeutic dosing. A level of 3.0 ng/mL is above the therapeutic window, not below it.
3. “It is within the normal range.”Therapeutic levels for digoxin are 0.5–2.0 ng/mL; therefore, 3.0 ng/mL is above the normal range and considered elevated.
4. “It is in the low average range.”Low average levels are generally between 0.5–1.0 ng/mL. This client’s level is well above that range, making this statement incorrect.
Test-taking strategy:
• Recall the therapeutic range for digoxin (0.5–2.0 ng/mL) and recognize that levels above 2.0 ng/mL indicate toxicity risk.
• Link elevated serum levels with clinical signs of digoxin toxicity.
• Prioritize interventions such as monitoring cardiac rhythm, assessing for symptoms, and contacting the provider.
Take-home points:
• The therapeutic serum digoxin range is 0.5–2.0 ng/mL; levels above 2.0 ng/mL are high and toxic.
• Elevated levels increase the risk for life-threatening arrhythmias and systemic toxicity.
• Immediate nursing actions include assessment, monitoring, and collaboration with the healthcare provider to prevent complications.
The nurse is caring for several clients on antidysrhythmic medications. The nurse would be sure to assess which essential parameter?
Explanation
Antidysrhythmicdrugs are used to treat abnormal cardiac rhythms by modifying the electrical conduction system of the heart. These medications can affect heart rate, rhythm, and conduction velocity, making pulse assessment a primary indicator of therapeutic effectiveness. Regular monitoring allows the nurse to identify whether the drug is successfully restoring or maintaining normal sinus rhythm and to detect potential bradycardia, tachycardia, or other dysrhythmias early.
Rationale for correct answer:
1. Pulse.The pulse provides a direct measure of heart rate and rhythm, which are the primary clinical indicators of antidysrhythmic therapy efficacy. A therapeutic response is typically reflected by a pulse within the target rate range, absence of irregular rhythms, and improved cardiac output. Continuous or frequent pulse assessment ensures early detection of both under-treatment and drug-induced arrhythmias, enhancing patient safety.
Rationales for incorrect answers:
2. Blood pressure.While blood pressure is an important vital sign and may be indirectly affected by antidysrhythmic drugs, it does not specifically indicate whether the arrhythmia is controlled. Hypotension may occur as a side effect, but it is not the primary measure of therapeutic effect.
3. Drug level.Monitoring serum drug levels is relevant for certain antidysrhythmics like digoxin or procainamide to prevent toxicity, but it does not directly measure whether the arrhythmia is being treated successfully. Therapeutic effect is best assessed clinically through heart rate and rhythm.
4. Hourly urine output.Urine output reflects renal perfusion and fluid balance, not the efficacy of an antidysrhythmic agent. It may be monitored in clients with cardiac dysfunction, but it is not a primary parameter for evaluating therapeutic effect of antiarrhythmic therapy.
Test-taking strategy:
• Focus on the primary clinical effect of the medication (e.g., rhythm control for antidysrhythmics)
• Differentiate between parameters used for efficacy monitoring versus toxicity or side effect monitoring
• Prioritize vital signs directly related to the drug’s intended outcome
Take-home points:
• Pulse assessment is the key indicator of antidysrhythmic drug effectiveness
• Monitor for rate, rhythm regularity, and any new dysrhythmias
• Other parameters such as blood pressure and drug levels support safety but do not measure therapeutic effect directly
A nurse is caring for a client with a dysrhythmia. The nurse understands that common adverse effects of antidysrhythmic medications include which of the following? Select all that apply
Explanation
Antidysrhythmic medications work by altering the electrical conduction of the heart through effects on sodium, potassium, calcium channels, or autonomic input. While they control abnormal heart rhythms, these effects can also reduce cardiac output or affect vascular resistance, leading to adverse reactions. Awareness of these side effects allows nurses to implement safety measures, monitor the client appropriately, and provide patient education.
Rationale for correct answer:
1. Hypotension.Many antidysrhythmic agents, including beta blockers and calcium channel blockers, decrease myocardial contractility or cause peripheral vasodilation, leading to hypotension. This is a common adverse effect and requires monitoring of blood pressure before and during therapy.
3. Dizziness.Reduced cardiac output or hypotension can result in decreased cerebral perfusion, causing dizziness or lightheadedness. Clients should be instructed to rise slowly from sitting or lying positions and report persistent dizziness.
4. Weakness.Generalized weakness may occur due to reduced perfusion of skeletal muscles or systemic effects on energy metabolism. It is a common complaint that can affect activities of daily living and warrants monitoring.
Rationales for incorrect answers:
2. Hypertension.Antidysrhythmic drugs rarely cause hypertension as a primary adverse effect. Most agents reduce heart rate, conduction, or vascular resistance, which typically lowers rather than raises blood pressure.
5. Panic attacks.While clients may experience anxiety or palpitations, panic attacks are not a direct pharmacologic effect of antidysrhythmic medications and are not commonly associated with their use.
Test-taking strategy:
• Focus on the hemodynamic effects of antidysrhythmic drugs, such as decreased contractility and vasodilation
• Identify symptoms that result from reduced cardiac output or perfusion
• Eliminate options unrelated to cardiovascular or systemic effects
Take-home points:
• Monitor blood pressure closely for hypotension when administering antidysrhythmic agents
• Teach clients to report dizziness, weakness, or syncope promptly
• Understand that hypertension and panic attacks are not typical direct adverse effects of these drugs
The nurse is assessing a client for possible evidence of digitalis toxicity. The nurse acknowledges that which is included in the signs and symptoms for this toxicity?
Explanation
The nurse is assessing a client taking digoxin, a cardiac glycosideused to treat heart failure and certain atrial dysrhythmias. Monitoring for digitalis toxicityis critical because digoxin has a narrow therapeutic index, meaning the range between therapeutic and toxic levels is small. Toxicity can lead to life-threatening arrhythmias, gastrointestinal disturbances, and neurological symptoms. Accurate assessment of apical pulse rate and rhythmis a key component in early detection and prevention of serious complications.
Rationale for correct answer:
4. “Apical pulse of 48 beats/min and irregular rate.”Bradycardia (pulse <60 bpm) and irregular rhythms are hallmark signs of digitalis toxicity, even before other systemic manifestations appear. Digoxin slows conduction through the atrioventricular (AV) node and increases vagal tone, which can result in significant bradyarrhythmias. Early recognition of a slow, irregular pulse allows the nurse to hold the medication, notify the healthcare provider, and monitor for additional symptoms such as nausea, vomiting, visual changes, and confusion, which are common in toxicity.
Rationales for incorrect answers:
1. “Apical pulse rate of 100 beats/min.”Tachycardia is not a primary indicator of digitalis toxicity. While digoxin can cause arrhythmias, a fast, regular pulse is more likely associated with underlying disease or compensatory mechanisms rather than toxicity.
2. “Apical pulse of 72 beats/min with an irregular rate.”Although an irregular rate may indicate conduction issues, a heart rate within the normal range (60–100 bpm) is generally not suggestive of toxicity unless accompanied by other symptoms.
3. “Apical pulse of 90 beats/min and an irregular rate.”Similar to option 2, an irregular rate at a normal heart rate does not strongly indicate toxicity; digoxin toxicity more commonly causes bradyarrhythmias rather than mild irregularities with normal rates.
Test-taking strategy:
• Focus on the classic cardiovascular manifestations of digitalis toxicity, particularly bradycardia and arrhythmias.
• Recognize that irregular, slow pulses in clients on digoxin require immediate attention.
• Correlate pulse assessment findings with other toxicity signs and risk factors for a comprehensive evaluation.
Take-home points:
• Bradycardia and irregular apical pulses are key indicators of digitalis toxicity.
• Early recognition of toxicity prevents life-threatening complications, including severe arrhythmias.
• Always assess apical pulse for 1 full minute before administration and consider holding digoxin if bradycardia or irregular rhythm is present.
A client is taking a potassium-depleting diuretic and digoxin. The nurse expects that a low potassium level (hypokalemia) could have what effect on digoxin (Lanoxin)?
Explanation
The nurse is caring for a client taking digoxinin combination with a potassium-depleting diuretic. Digoxin is a cardiac glycosidethat increases myocardial contractility and is used in heart failure and atrial dysrhythmias. Because digoxin has a narrow therapeutic window, electrolyte imbalances, particularly hypokalemia, can dramatically alter its effects and increase the risk of toxicity, including life-threatening arrhythmias. Understanding this interaction is critical for safe administration and monitoring.
Rationale for correct answer:
1. “Increase serum digoxin sensitivity level.”Hypokalemia potentiates the effects of digoxin by enhancing its binding to the sodium-potassium ATPase pump in cardiac cells. Low serum potassium allows digoxin to bind more readily, which increases its pharmacologic effect even at normal digoxin levels. This heightened sensitivity increases the risk for digitalis toxicity, manifesting as bradycardia, arrhythmias, nausea, vomiting, visual disturbances, and confusion. Therefore, clients on digoxin with concurrent potassium-depleting diuretics, such as thiazides or loop diuretics, require frequent monitoring of potassium levels and appropriate supplementation if hypokalemia is detected.
Rationales for incorrect answers:
2. “Decrease serum digoxin sensitivity level.”Hypokalemia does not reduce digoxin sensitivity; instead, it potentiates its effects. Assuming decreased sensitivity could lead to inappropriate dosing or missed toxicity signs.
3. “Have no effect on serum digoxin sensitivity level.” Electrolyte imbalances, particularly low potassium, significantly alter digoxin activity. Ignoring this relationship increases the risk of adverse cardiac events.
4. “Cause a low average serum digoxin sensitivity level.” This statement is misleading; hypokalemia does not lower sensitivity but rather increases the effect and toxicity potential of digoxin.
Test-taking strategy:
• Focus on electrolyte interactions with digoxin, particularly potassium, magnesium, and calcium levels.
• Identify the mechanism by which hypokalemia enhances digoxin’s effect.
• Recognize the clinical significance of concurrent potassium-depleting diuretics in clients receiving digoxin.
Take-home points:
• Hypokalemia increases digoxin sensitivity, heightening the risk for toxicity.
• Monitor serum potassium and digoxin levels closely in clients taking digoxin and potassium-wasting diuretics.
• Teach clients to report signs of digoxin toxicity, including nausea, visual changes, fatigue, or irregular heartbeats.
A client is on acebutolol (Sectral) for dysrhythmias. The nurse understands that which of the following is the primary purpose of the drug?
Explanation
The nurse is administering acebutolol (Sectral), a beta-adrenergic blockerused to manage cardiac dysrhythmias. Beta blockers are primarily used to control heart rate, reduce myocardial contractility, and decrease cardiac workload. Understanding the specific receptor targetsof beta blockers is essential for safe and effective management of dysrhythmias, hypertension, and other cardiovascular conditions. Acebutolol is a cardioselective beta-1 blocker, meaning it primarily affects the heart while having minimal effects on the lungs.
Rationale for correct answer:
3. “Block beta1-adrenergic receptors in cardiac tissues.”Acebutolol selectively blocks beta1-adrenergic receptors located in the heart. By inhibiting beta1 stimulation, it reduces heart rate, decreases myocardial contractility, and slows atrioventricular conduction, which helps control dysrhythmias such as ventricular tachycardia or premature ventricular contractions. This receptor selectivity minimizes bronchial and vascular side effects, which are more likely with nonselective beta blockers. Blocking beta1 receptors also reduces myocardial oxygen demand, which can help prevent ischemia in clients with underlying coronary artery disease.
Rationales for incorrect answers:
1. “Increase beta1 and beta2 receptors in cardiac tissues.”Beta blockers do not increase receptor numbers; they antagonize the effects of catecholamines at beta1 receptors, decreasing heart rate and contractility. Increasing receptors is not a therapeutic mechanism of beta blockers.
2. “Increase the flow of oxygen to cardiac tissues.”While reducing heart rate and contractility indirectly decreases myocardial oxygen demand, beta blockers do not directly increase oxygen flow to cardiac tissues. Oxygen delivery is influenced by coronary perfusion and blood oxygen content, not by receptor blockade.
4. “Block beta2-adrenergic receptors in cardiac tissues.” Beta2 receptors are primarily located in the lungs and vascular smooth muscle. Acebutolol is cardioselective for beta1 and minimally affects beta2, so this statement is inaccurate for its primary therapeutic purpose.
Test-taking strategy:
• Identify whether the beta blocker is cardioselective (beta1) or nonselective (beta1 and beta2).
• Focus on the primary mechanism in the heart rather than secondary or indirect effects.
• Eliminate options that describe receptor increase or pulmonary effects, which are unrelated to cardioselective beta blockers.
Take-home points:
• Acebutolol blocks beta1-adrenergic receptors to manage dysrhythmias effectively.
• Cardioselectivity minimizes bronchial and vascular side effects.
• Beta blockers reduce heart rate, myocardial contractility, and oxygen demand, stabilizing cardiac rhythm and workload.
The nurse is caring for a client who recently suffered a myocardial infarction (MI) and now is experiencing ectopy and runs of ventricular tachycardia (VT). The client reports having feelings of palpitations during the ectopy and has been started on an antidysrhythmic.
The nurse reviewed the classifications of drugs that can be used to treat dysrhythmias and knows they include which mechanisms of action? Select all that apply
Explanation
The nurse is reviewing antidysrhythmic drug classificationsfor a client who recently experienced a myocardial infarction (MI)and is now showing ectopy and runs of ventricular tachycardia (VT). Antidysrhythmic drugs work by modifying electrical conduction, automaticity, and refractorinessin cardiac tissues. Understanding the mechanism of actionfor each drug class helps the nurse anticipate therapeutic effects, monitor for adverse reactions, and provide safe client care. These drugs are categorized based on their primary effect on ion channels or adrenergic receptorsin the heart.
Rationale for correct answers:
1. Beta-adrenergic blocking.Beta blockers inhibit beta1-adrenergic receptors in the heart, reducing sympathetic stimulation. This decreases heart rate, myocardial contractility, and conduction velocity through the atrioventricular (AV) node, stabilizing the heart rhythm and preventing tachyarrhythmias after an MI.
2. Calcium channel blocking.Calcium channel blockers, particularly the non-dihydropyridine class (verapamil, diltiazem), inhibit calcium influx during the action potential, slowing AV node conduction and reducing myocardial contractility. This helps manage supraventricular tachyarrhythmias and can indirectly influence ventricular rates.
4. Sodium channel blocking. Sodium channel blockers, such as lidocaine and procainamide, decrease the rate of depolarization in fast-response myocardial cells, slowing conduction and stabilizing excitable cardiac tissues. This is especially useful in ventricular ectopy and VT post-MI.
5. Potassium channel blocking.Drugs like amiodarone and sotalol prolong repolarization by blocking potassium efflux, extending the refractory period and preventing reentrant dysrhythmias. This mechanism is critical in controlling both atrial and ventricular tachyarrhythmias.
Rationales for incorrect answer:
3. Chloride channel blocking.Chloride channel blockade is not a recognized mechanism for controlling cardiac dysrhythmias. While chloride ions play roles in other tissues, targeting chloride channels does not produce clinically significant antiarrhythmic effects, making this option incorrect.
Test-taking strategy:
• Focus on established classes of antidysrhythmics: Classes I (sodium), II (beta blockers), III (potassium), IV (calcium).
• Eliminate options unrelated to cardiac electrophysiology.
• Remember that post-MI clients often receive drugs that stabilize ventricular conduction and reduce automaticity.
Take-home points:
• Antidysrhythmic drugs act on sodium, potassium, calcium channels, and beta-adrenergic receptors to manage dysrhythmias.
• Chloride channels are not a target for antiarrhythmic therapy.
• Understanding each drug’s mechanism helps predict effects, adverse reactions, and monitoring priorities.
The nurse reviewing the laboratory results of a 68-year-old female client receiving amiodarone hydrochloride for paroxysmal atrial fibrillation knows which of the following laboratory tests are monitored for clients on antidysrhythmic agents? Select all that apply
Explanation
The nurse is reviewing laboratory resultsfor a 68-year-old female client receiving amiodarone hydrochloridefor paroxysmal atrial fibrillation. Amiodarone is a potent class III antiarrhythmicthat works by prolonging the action potential and refractory period of cardiac cells, but it also has significant multi-system effects, particularly on the thyroid, liver, and lungs. Because of these potential toxicities, routine laboratory monitoringis essential to ensure early detection of adverse effects, safe drug therapy, and optimal clinical outcomes.
Rationale for correct answers:
1. Alanine aminotransferase (ALT).Amiodarone can cause hepatotoxicity, including asymptomatic elevations of liver enzymes or clinically significant hepatitis. ALT is a sensitive marker of hepatocellular injury, and elevated levels may necessitate dose adjustment or discontinuation of therapy. Monitoring ALT allows timely identification of hepatic toxicity.
3. Aspartate aminotransferase (AST).AST is another enzyme released with liver cell injury. Although less specific than ALT, elevations in AST may indicate hepatic stress or injury related to long-term amiodarone therapy. Tracking both ALT and AST provides a comprehensive view of liver function.
4. Thyroid-stimulating hormone (TSH).Amiodarone is iodine-rich and can disrupt normal thyroid function, causing either hypothyroidism or hyperthyroidism. Regular monitoring of TSH is essential to detect thyroid dysfunction early, as thyroid abnormalities can worsen arrhythmias or affect drug metabolism.
Rationales for incorrect answers:
2. Creatine kinase–MB (CK-MB).CK-MB is a cardiac-specific enzyme used to diagnose myocardial infarction, not for monitoring adverse effects of antidysrhythmic drugs. Routine CK-MB measurement is unnecessary unless acute myocardial injury is suspected.
5. Prostate-specific antigen (PSA).PSA screening is unrelated to amiodarone therapy and does not reflect cardiac, hepatic, or thyroid toxicity. Monitoring PSA provides no useful information for clients on antidysrhythmic agents.
Test-taking strategy:
• Identify laboratory tests that reflect known organ toxicities of the drug in question.
• Eliminate tests used for unrelated organ systems or conditions.
• Focus on liver and thyroid function monitoring for amiodarone therapy.
Take-home points:
• Monitor ALT and AST for potential hepatotoxicity during amiodarone therapy.
• Monitor TSH regularly to detect thyroid dysfunction, a common adverse effect of amiodarone.
• Tests like CK-MB and PSA are not routinely indicated for monitoring antidysrhythmic drug toxicity.
The client in the scenario was started on the antidysrhythmic flecainide and asks the nurse what they need to be aware of while taking this drug. What common adverse effects should the nurse mention to the client?
Explanation
The nurse is teaching a client who has been started on flecainide, a class IC antiarrhythmic, for management of dysrhythmias. Flecainide works by slowing the fast sodium channels in cardiac cells, thereby decreasing conduction velocityand helping to stabilize abnormal heart rhythms. While effective, flecainide is associated with a variety of adverse effects, particularly neurological and gastrointestinal, which clients should recognize to ensure safety and promote adherence to therapy. Educating clients on common and expected side effectshelps prevent unnecessary anxiety and ensures prompt reporting of serious symptoms.
Rationale for correct answers:
1. Headache.Headaches are a frequent and expected adverse effect of flecainide. They may result from vascular changes or CNS effects secondary to altered cardiac output or sodium channel modulation. Clients should be informed that mild headaches can occur and usually do not require discontinuation but should be reported if severe or persistent.
3. Nausea.Flecainide can cause gastrointestinal upset, including nausea, vomiting, or mild abdominal discomfort. These effects are typically dose-related and can often be mitigated by taking the medication with food. Clients should be advised to report persistent nausea, as it can affect hydration and adherence.
5. Dizziness.Dizziness is another common adverse effect due to reduced cardiac output or hypotension associated with the antiarrhythmic effects of flecainide. Clients should be cautioned to rise slowly from sitting or lying positions and avoid activities that require alertness until they understand how the drug affects them.
Rationales for incorrect answers:
2. Exertional dyspnea.While severe cardiac or pulmonary effects could cause dyspnea, exertional dyspnea is not a common or expected adverse effect of flecainide. If it occurs, it may indicate an underlying cardiovascular complication rather than a direct drug effect.
4. Sinus rhythm.Sinus rhythm is a therapeutic goal, not an adverse effect. Flecainide is intended to restore normal rhythm, so this is not something the client would experience as a side effect.
6. Photosensitivity.Photosensitivity is not associated with flecainide use and is not included in standard client teaching.
7. Constipation.Constipation is uncommon with flecainide therapy and is not considered a typical adverse effect of this medication.
Test-taking strategy:
• Focus on common neurological and gastrointestinal side effects of class IC antiarrhythmics.
• Distinguish between expected adverse effects and therapeutic goals or unrelated symptoms.
• Emphasize client safety and adherence in teaching plans.
Take-home points:
• Flecainide commonly causes headache, nausea, and dizziness.
• Educate clients to report severe or persistent symptoms that may indicate complications.
• Advise clients to take precautions with activities requiring alertness and to take the drug with food if gastrointestinal upset occurs.
A nurse assessing a 48-year-old male client for signs of cardiovascular disease looks for which of these symptoms? Indicate with an X the assessment signs that indicate one of the six cardinal signs of cardiovascular disease or whether it is unrelated.
Explanation
|
CLIENT ASSESSMENT |
CARDINAL SIGN OF CARDIOVASCULAR DISEASE |
UNRELATED SIGN |
|
Client complaining of not sleeping well |
X |
|
|
Client became weak and dizzy when attempting to stand |
X |
|
|
Client complaining of blurred vision |
X |
|
|
Client reports difficulty breathing when lying flat |
X |
|
|
Client having urinary retention |
X |
|
|
Client experiencing palpitations |
X |
|
|
Client having pitting edema around the ankles |
X |
|
|
Client reported decreases in physical activity |
X |
|
|
Client complaining of pain across the chest |
X |
|
|
Client reporting ringing in the ears |
X |
The nurse is assessing a 48-year-old client for signs and symptoms of cardiovascular disease (CVD), which requires recognizing the six cardinal manifestations of CVD: chest pain, palpitations, dyspnea (shortness of breath), syncope or dizziness, edema, and decreased exercise tolerance. Accurate identification ensures timely intervention, proper monitoring, and individualized care planning to reduce morbidity and prevent complications. Distinguishing unrelated complaints avoids misinterpretation and unnecessary investigations.
Rationale for correct answers:
Client became weak and dizzy when attempting to stand.This reflects syncope or pre-syncope, a cardinal sign of cardiovascular disease often related to decreased cardiac output, orthostatic hypotension, or arrhythmias.
Client reports difficulty breathing when lying flat.Dyspnea on lying down (orthopnea)is a hallmark of left-sided heart failure, a cardinal sign that indicates impaired left ventricular function and pulmonary congestion.
Client experiencing palpitations.Palpitations reflect arrhythmias or abnormal cardiac conduction, a cardinal sign of cardiovascular disease that may indicate atrial fibrillation, tachycardia, or other dysrhythmias.
Client having pitting edema around the ankles. Peripheral edema, particularly pitting edema, is a cardinal sign of right-sided heart failure, caused by fluid accumulation due to poor venous return.
Client reported decreases in physical activity.Reduced exercise tolerance signals cardiac compromise, another cardinal manifestation of cardiovascular disease, often due to decreased cardiac output and tissue perfusion.
Client complaining of pain across the chest.Chest pain or angina is a classic cardinal symptom, indicating myocardial ischemia or other cardiac pathology.
Rationales for incorrect answers:
Client complaining of not sleeping well.While sleep issues may affect cardiovascular risk long term, insomnia is not a cardinal sign of CVD and is nonspecific.
Client complaining of blurred vision.Vision changes may relate to hypertension or diabetes but are not primary indicators of cardiovascular disease.
Client having urinary retention.This is a genitourinary issue xand unrelated to cardiac pathology.
Client reporting ringing in the ears.Tinnitus is not a sign of cardiovascular disease; it may relate to ear pathology or medications.
Test-taking strategy:
• Recall the six cardinal signs of cardiovascular disease: chest pain, palpitations, dyspnea, syncope/dizziness, edema, decreased exercise tolerance.
• Focus on symptoms that reflect direct cardiac compromise or impaired perfusion.
• Exclude unrelated or nonspecific symptoms that may reflect other organ systems.
Take-home points:
• Cardiovascular assessment prioritizes six cardinal signs: chest pain, palpitations, dyspnea, syncope, edema, and decreased exercise tolerance.
• Accurate identification guides interventions and monitoring for acute and chronic CVD.
• Distinguishing unrelated symptoms reduces unnecessary testing and improves clinical focus.
Exams on Drugs Used to Treat Dysrhythmias
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
- Define cardiac dysrhythmias and their underlying electrical disturbances.
- Describe the impact of dysrhythmias on cardiac output and tissue perfusion.
- State the primary goals of antidysrhythmic therapy, including rate and rhythm control.
- Classify antidysrhythmic drugs using the Vaughan Williams system.
- Explain the mechanisms of action of major antidysrhythmic drug classes.
- Match antidysrhythmic drugs to clinical indications (supraventricular vs. ventricular).
- Identify major adverse effects, including proarrhythmia and hemodynamic instability.
- Recognize key contraindications and precautions for antidysrhythmic therapy.
- Apply essential nursing monitoring strategies, including ECG and vital signs.
- Evaluate therapeutic effectiveness based on rhythm control and symptom improvement.
Introduction
Cardiac dysrhythmias, also referred to as arrhythmias, are abnormalities in heart rate, rhythm, or impulse conduction that arise from disturbances in the cardiac electrical system.
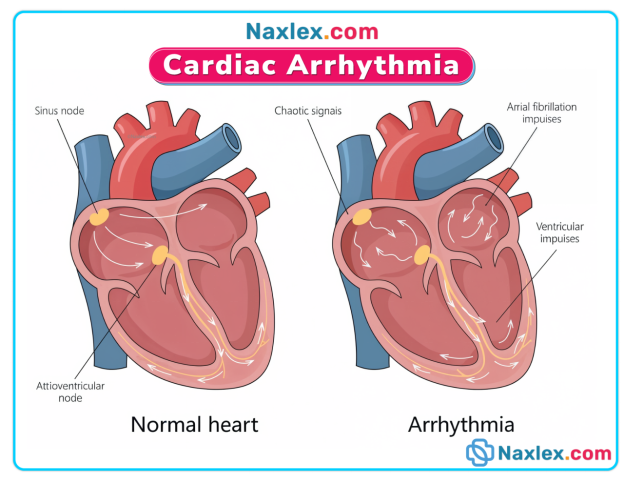
These disorders may originate in the sinoatrial (SA) node, atrioventricular (AV) node, atrial myocardium, or ventricular myocardium and can significantly alter the heart’s ability to pump blood effectively.
Dysrhythmias range from transient and asymptomatic conditions to severe, life-threatening events that compromise cardiac output, impair tissue perfusion, and increase the risk of stroke, heart failure, and sudden cardiac death.
The pharmacologic management of dysrhythmias is directed toward several key therapeutic goals:
- restoration and maintenance of normal sinus rhythm,
- control of ventricular rate,
- suppression of ectopic pacemaker activity
- prevention of recurrent or fatal arrhythmias.
Antiarrhythmic medications exert their effects by modifying the movement of ions across cardiac cell membranes or by altering autonomic influences on the heart.
These drugs are traditionally classified according to the Vaughan Williams classification system (Classes I–IV), with additional agents categorized as miscellaneous antiarrhythmics.
Antidysrhythmic medications are associated with significant risks, including proarrhythmic effects, hemodynamic instability, and organ toxicity.
Most of the medications possess a narrow therapeutic index and as a result, careful patient selection, individualized dosing, and vigilant monitoring are essential components of safe therapy.
Continuous electrocardiographic monitoring, assessment of vital signs, and evaluation of laboratory values such as electrolytes and drug serum levels are critical to detecting adverse effects early and ensuring therapeutic effectiveness.
Procainamide
Drug Name
- Generic: Procainamide
- Brand Names: Pronestyl, Procanbid
Classification
- Pharmacologic class: Class IA sodium channel blocker
- Therapeutic class: Antidysrhythmic
Mechanism of Action (MOA)
- Slows electrical conduction through the atria, ventricles, and AV node
- Decreases automaticity of the SA node
- Prolongs repolarization (increases refractory period)
- NCLEX focus: Stabilizes cardiac membranes to prevent abnormal rhythms
Indications
- Supraventricular tachycardia (SVT)
- Ventricular tachycardia
- Atrial fibrillation or flutter
Routes of Administration
- Oral (sustained-release)
- Intravenous
Pharmacologic Effects
- Restoration and maintenance of normal sinus rhythm
- Prevention of recurrent dysrhythmias
- Reduction in ventricular ectopy
Common Adverse Effects
- Hypotension
- GI upset, nausea
- Rash, fever (related to systemic lupus-like syndrome)
Serious Adverse Reactions
- Cardiotoxicity: QRS widening >50%, prolonged QT and PR intervals
- Neutropenia, thrombocytopenia
- Systemic lupus erythematosus-like syndrome
Contraindications & Precautions
- Hypersensitivity to procainamide or quinidine
- Complete heart block, atypical ventricular tachycardia
- Pregnancy Risk Category C
- Use cautiously in liver/renal dysfunction, partial AV block, heart failure
Nursing Interventions
- Monitor BP, heart rate, ECG continuously
- Assess for signs of infection or bleeding
- Monitor for SLE-like symptoms (rash, fever, joint pain)
- Ensure therapeutic serum levels (4–8 mcg/mL)
Monitoring
- Weekly CBC for first 12 weeks, then periodically
- ECG monitoring
- Serum procainamide levels
Patient Education
- Take medication as prescribed; do not crush sustained-release tablets
- Report fever, rash, joint pain, signs of infection
- Monitor and record pulse and BP
Antidote / Reversal Agents
- Symptomatic management of hypotension or arrhythmias
Drug Interactions
- Additive effects with other antidysrhythmics - increased toxicity
- Anticholinergic meds - blurred vision, constipation, urinary retention
- Antihypertensives - additive hypotension
Lidocaine
Drug Name
- Generic: Lidocaine
- Brand Name: Xylocaine
Classification
- Pharmacologic class: Class IB sodium channel blocker
- Therapeutic class: Antidysrhythmic
Mechanism of Action (MOA)
- Decreases automaticity of ventricular cells
- Slows conduction in ischemic myocardium
- Shortens repolarization
- NCLEX focus: Used for acute ventricular dysrhythmias
Indications
- Short-term treatment of ventricular tachycardia
- Ventricular fibrillation
- Post-MI dysrhythmias
Routes of Administration
- Intravenous (IV)
- Topical (for local anesthesia)
Pharmacologic Effects
- Suppression of abnormal ventricular rhythms
- Stabilization of myocardial membrane
Common Adverse Effects
- CNS effects: drowsiness, confusion, paresthesia
- Nausea, vomiting
Serious Adverse Reactions
- Seizures
- Respiratory arrest
- Severe hypotension
Contraindications & Precautions
- Stokes-Adams syndrome, severe heart block
- Pregnancy Risk Category B
- Use cautiously in liver/renal dysfunction, HF, second-degree AV block
Nursing Interventions
- Continuous ECG monitoring
- Monitor for CNS toxicity (confusion, tremors, seizures)
- Ensure resuscitation equipment available
Monitoring
- Monitor lidocaine serum levels
- Vital signs, ECG
Patient Education
- Report numbness, dizziness, or visual changes
- Only used short-term for IV therapy
- Avoid activities requiring alertness if dizzy
Antidote / Reversal Agents
- Treat seizures with IV phenytoin or diazepam
- Supportive care for hypotension or bradycardia
Drug Interactions
- Cimetidine, beta-blockers, phenytoin - decreased metabolism - toxicity
Propafenone
Drug Name
- Generic: Propafenone
- Brand Name: Rythmol
Classification
- Pharmacologic class: Class IC sodium channel blocker
- Therapeutic class: Antidysrhythmic
Mechanism of Action (MOA)
- Decreases conduction velocity
- Reduces excitability of cardiac cells
- NCLEX focus: Slows ventricular conduction to treat SVT
Indications
- Supraventricular tachycardia (SVT)
- Atrial fibrillation
Routes of Administration
- Oral
Pharmacologic Effects
- Conversion to normal sinus rhythm
- Reduction in SVT episodes
Common Adverse Effects
- Dizziness, weakness
- Bradycardia
- Heart failure exacerbation
Serious Adverse Reactions
- Severe bradycardia
- Worsening heart failure
- Cardiogenic shock
Contraindications & Precautions
- AV block, severe hypotension, severe HF
- Pregnancy Risk Category C
- Use cautiously in liver/renal dysfunction
Nursing Interventions
- Monitor ECG, BP, HR
- Observe for signs of heart failure
- Administer with food to reduce GI upset
Monitoring
- ECG, electrolytes
- Digoxin and anticoagulant levels if co-administered
Patient Education
- Report dizziness, chest pain, or edema
- Take at same time daily
- Avoid abrupt discontinuation
Drug Interactions
- Digoxin, oral anticoagulants - increased serum levels
- Quinidine, amiodarone - increased toxicity
Propranolol
Drug Name
- Generic: Propranolol
- Brand Name: Inderal
Classification
- Pharmacologic class: Class II beta-adrenergic blocker
- Therapeutic class: Antidysrhythmic / antianginal / antihypertensive
Mechanism of Action (MOA)
- Blocks beta-1 receptors - decreases HR, conduction velocity
- Decreases sympathetic stimulation of heart
- NCLEX focus: Controls rate in atrial arrhythmias
Indications
- Atrial fibrillation/flutter
- Paroxysmal SVT
- Hypertension, angina
Routes of Administration
- Oral, IV
Pharmacologic Effects
- Slower HR
- Decreased atrial ectopic activity
- Prevention of SVT recurrence
Common Adverse Effects
- Fatigue
- Bradycardia
- Hypotension
Serious Adverse Reactions
- Heart failure
- AV block
Contraindications & Precautions
- Bradycardia, >1st degree AV block, HF
- Pregnancy Risk Category C
- Caution in asthma, diabetes, liver/thyroid dysfunction
Nursing Interventions
- Monitor apical pulse and BP
- Hold dose if pulse <60/min or symptomatic
- Monitor ECG
Monitoring
- ECG
- Blood glucose in diabetic patients
Patient Education
- Take at same time daily
- Do not stop abruptly
- Report dizziness, SOB, swelling
Drug Interactions
- Verapamil, diltiazem - additive cardiosuppression
- May mask hypoglycemia
Amiodarone
Drug Name
- Generic: Amiodarone
- Brand Names: Cordarone, Pacerone
Classification
- Pharmacologic class: Class III potassium channel blocker
- Therapeutic class: Antidysrhythmic
Mechanism of Action (MOA)
- Prolongs repolarization and refractory period of myocardial cells
- Slows conduction through SA and AV nodes
- Decreases automaticity and contractility
- NCLEX focus: Maintains sinus rhythm in atrial and ventricular arrhythmias
Indications
- Recurrent ventricular fibrillation
- Ventricular tachycardia
- Conversion of atrial fibrillation (oral route)
Routes of Administration
- Oral, IV
Pharmacologic Effects
- Restoration and maintenance of normal sinus rhythm
- Reduction of ventricular and supraventricular arrhythmias
Common Adverse Effects
- Hypotension
- Bradycardia, AV block
- GI upset, nausea
Serious Adverse Reactions
- Pulmonary toxicity (fibrosis)
- Liver dysfunction, thyroid dysfunction
- Visual disturbances (photophobia, blurred vision, potential blindness)
- AV block, heart failure exacerbation
Contraindications & Precautions
- AV block, bradycardia, newborns, infants
- Pregnancy Risk Category D
- Use cautiously in liver, thyroid, pulmonary dysfunction, HF, fluid/electrolyte imbalance
Nursing Interventions
- Baseline chest X-ray, pulmonary function, liver and thyroid function tests
- Monitor ECG, BP, HR, signs of HF (dyspnea, edema, JVD, crackles)
- Advise clients to report visual disturbances, cough, dyspnea
- IV administration via central line if possible
Monitoring
- Liver function tests, thyroid panel
- ECG for QT prolongation and AV conduction
- Monitor electrolytes and pulmonary function
Patient Education
- Avoid grapefruit juice
- Report shortness of breath, chest pain, swelling, or vision changes
- Adverse effects may persist after discontinuation
Antidote / Reversal Agents
- No specific antidote; manage toxicity symptomatically
Drug Interactions
- Increases levels of quinidine, procainamide, digoxin, diltiazem, warfarin
- Caution with diuretics, antibiotics, other antiarrhythmics → dysrhythmia risk
- Additive bradycardia with beta blockers, verapamil, diltiazem
Sotalol
Drug Name
- Generic: Sotalol
- Brand Name: Betapace
Classification
- Pharmacologic class: Class III potassium channel blocker
- Therapeutic class: Antidysrhythmic / beta-blocker properties
Mechanism of Action (MOA)
- Prolongs repolarization, slows conduction through AV node
- Nonselective beta-blocker activity reduces sympathetic stimulation
- NCLEX focus: Controls ventricular and supraventricular arrhythmias
Indications
- Ventricular arrhythmias
- Atrial fibrillation/flutter
Routes of Administration
- Oral
Pharmacologic Effects
- Maintenance of sinus rhythm
- Prevention of recurrent ventricular tachycardia/fibrillation
Common Adverse Effects
- Fatigue
- Bradycardia
- Hypotension
Serious Adverse Reactions
- Torsades de pointes (QT prolongation)
- Heart block, HF exacerbation
Contraindications & Precautions
- Bradycardia, heart block, HF, prolonged QT interval
- Pregnancy Risk Category C
- Use cautiously in renal dysfunction
Nursing Interventions
- Monitor ECG, HR, BP
- Assess for signs of HF
- Adjust dose based on renal function
Monitoring
- ECG for QT interval
- Serum potassium and magnesium
- Renal function tests
Patient Education
- Report dizziness, fainting, palpitations
- Take at the same time daily
- Avoid sudden position changes (orthostatic hypotension)
Drug Interactions
- Additive QT prolongation with other antiarrhythmics or macrolides
- Avoid grapefruit juice
Dofetilide
Drug Name
- Generic: Dofetilide
- Brand Name: Tikosyn
Classification
- Pharmacologic class: Class III potassium channel blocker
- Therapeutic class: Antidysrhythmic
Mechanism of Action (MOA)
- Prolongs action potential duration and refractory period
- Reduces automaticity in atrial tissue
- NCLEX focus: Conversion and maintenance of normal sinus rhythm in atrial fibrillation
Indications
- Atrial fibrillation and atrial flutter
- Maintenance of sinus rhythm
Routes of Administration
- Oral
Pharmacologic Effects
- Suppression of atrial dysrhythmias
- Restoration and maintenance of normal rhythm
Common Adverse Effects
- Headache, dizziness
- Fatigue
Serious Adverse Reactions
- Torsades de pointes
- Severe bradycardia
Contraindications & Precautions
- QT prolongation
- Severe renal dysfunction
- Pregnancy Risk Category C
Nursing Interventions
- Baseline ECG and renal function
- Monitor ECG for QT interval
- Dose adjustment based on creatinine clearance
Monitoring
- ECG, renal function tests
- Serum potassium and magnesium
Patient Education
- Report palpitations, fainting, dizziness
- Avoid OTC medications that prolong QT
- Take exactly as prescribed
Drug Interactions
- Other QT-prolonging medications (e.g., quinidine, erythromycin)
Verapamil
Drug Name
- Generic: Verapamil
- Brand Name: Calan
Classification
- Pharmacologic class: Class IV calcium channel blocker
- Therapeutic class: Antidysrhythmic / antihypertensive / antianginal
Mechanism of Action (MOA)
- Inhibits calcium influx in SA and AV nodes
- Decreases AV node conduction
- NCLEX focus: Slows ventricular response in atrial fibrillation/flutter
Indications
- Atrial fibrillation/flutter
- SVT
- Hypertension
- Angina
Routes of Administration
- Oral, IV
Pharmacologic Effects
- Reduced heart rate
- Slower AV conduction
- Decreased myocardial oxygen demand
Common Adverse Effects
- Bradycardia
- Hypotension
- Constipation
Serious Adverse Reactions
- Heart failure exacerbation
- AV block
- Severe hypotension
Contraindications & Precautions
- 1st-degree AV block without pacemaker
- Severe hypotension, HF
- Pregnancy Risk Category C
Nursing Interventions
- Monitor ECG, BP, HR
- Monitor for peripheral edema and SOB
- Use caution with concurrent beta-blockers
Monitoring
- ECG
- Liver and renal function
Patient Education
- Change positions slowly to prevent dizziness
- Report swelling or shortness of breath
- Avoid grapefruit juice
Drug Interactions
- Additive cardiosuppression with beta blockers
- May potentiate digoxin and carbamazepine
Diltiazem
Drug Name
- Generic: Diltiazem
- Brand Name: Cardizem
Classification
- Pharmacologic class: Class IV calcium channel blocker
- Therapeutic class: Antidysrhythmic / antihypertensive / antianginal
Mechanism of Action (MOA)
- Blocks calcium channels in cardiac tissue
- Decreases AV node conduction and myocardial contractility
- NCLEX focus: Controls ventricular rate in SVT and AF
Indications
- SVT
- Atrial fibrillation/flutter
- Hypertension, angina
Routes of Administration
- Oral, IV
Pharmacologic Effects
- Slower heart rate
- Improved cardiac output
- Reduced oxygen demand
Common Adverse Effects
- Hypotension
- Bradycardia
- Dizziness, headache
Serious Adverse Reactions
- Heart failure exacerbation
- AV block
Contraindications & Precautions
- 1st-degree AV block without pacemaker
- Pregnancy Risk Category C
- Severe hypotension
Nursing Interventions
- Monitor ECG, HR, BP
- Assess for edema, SOB
- Use caution with beta-blockers
Monitoring
- ECG
- Liver and renal function tests
Patient Education
- Take with food if GI upset occurs
- Avoid grapefruit juice
- Change positions slowly
Drug Interactions
- Additive bradycardia with beta blockers
- May increase digoxin levels
Adenosine
Drug Name
- Generic: Adenosine
- Brand Name: Adenocard
Classification
- Pharmacologic class: Miscellaneous antiarrhythmic
- Therapeutic class: Antidysrhythmic
Mechanism of Action (MOA)
- Slows conduction through AV node
- Terminates reentrant SVT
- NCLEX focus: Emergency conversion of SVT
Indications
- Paroxysmal SVT
- Wolff-Parkinson-White syndrome
Routes of Administration
- Intravenous (rapid bolus)
Pharmacologic Effects
- Immediate termination of SVT
- Restoration of normal sinus rhythm
Common Adverse Effects
- Flushing
- Dyspnea, chest discomfort
- Short-lived bradycardia
Serious Adverse Reactions
- Severe bradycardia
- AV block
- Hypotension
Contraindications & Precautions
- Second- and third-degree AV block
- Pregnancy Risk Category C
- Use cautiously in asthma
Nursing Interventions
- Administer as rapid IV bolus followed by saline flush
- Monitor ECG continuously
- Have resuscitation equipment ready
Monitoring
- Continuous ECG
- Vital signs
Patient Education
- Effects are short-lived (<1 min)
- May feel chest pressure or flushing
- No long-term adverse effects
Drug Interactions
- Caffeine and theophylline → blocks effects
- Dipyridamole intensifies effect
Digoxin
Drug Name
- Generic: Digoxin
- Brand Name: Lanoxin
Classification
- Pharmacologic class: Cardiac glycoside
- Therapeutic class: Antidysrhythmic / inotropic
Mechanism of Action (MOA)
- Increases force of myocardial contraction
- Slows AV node conduction
- NCLEX focus: Controls ventricular rate in AF, improves cardiac output in HF
Indications
- Heart failure
- Atrial fibrillation/flutter
- Paroxysmal SVT
Routes of Administration
- Oral, IV
Pharmacologic Effects
- Slower, more regular heart rate
- Increased cardiac output
- Reduction in symptoms of HF
Common Adverse Effects
- Nausea, vomiting, fatigue
- Bradycardia
Serious Adverse Reactions
- Digoxin toxicity → dysrhythmias, vision changes, GI upset
- Severe bradycardia
Contraindications & Precautions
- Ventricular tachycardia/fibrillation not due to HF
- Pregnancy Risk Category C
- Use cautiously with AV block, renal disease, hypokalemia
Nursing Interventions
- Monitor apical pulse for 1 min before administering
- Hold if HR <60/min
- Monitor for signs of toxicity (nausea, visual changes, arrhythmias)
Monitoring
- Serum digoxin: therapeutic 0.5–0.8 ng/mL
- Potassium: 3.5–5.0 mEq/L
- ECG monitoring
Patient Education
- Take pulse before each dose
- Eat high-potassium foods
- Avoid OTC drugs that alter HR
Antidote / Reversal Agents
- Digoxin immune Fab (Digibind)
Drug Interactions
- Amiodarone, quinidine, verapamil → increase digoxin levels
- Corticosteroids, diuretics → risk of hypokalemia → toxicity
- Antacids may reduce absorption
Nursing Evaluation of Medication Effectiveness (All Antiarrhythmics)
- Absence of dysrhythmias
- Return to baseline ECG, pulse rate, and regular rhythm
- Improved clinical manifestations: chest pain, shortness of breath, palpitations
- Maintenance of stable hemodynamics
Summary
- Cardiac dysrhythmias result from abnormalities in cardiac impulse formation or conduction and may significantly impair cardiac output and tissue perfusion.
- Primary goals of antidysrhythmic therapy include:
- Restoration and maintenance of normal sinus rhythm
- Control of ventricular rate
- Suppression of ectopic pacemaker activity
- Prevention of recurrent or life-threatening arrhythmias
- Antidysrhythmic drugs are classified mainly by the Vaughan Williams system:
- Class I (Sodium channel blockers)
- IA: Procainamide – slows conduction, prolongs repolarization
- IB: Lidocaine – suppresses ventricular dysrhythmias, especially post-MI
- IC: Propafenone – markedly slows conduction, used for SVT and AF
- Class II (Beta-blockers)
- Propranolol – reduces sympathetic stimulation, controls atrial rate
- Class III (Potassium channel blockers)
- Amiodarone, Sotalol, Dofetilide – prolong repolarization and refractory period
- Class IV (Calcium channel blockers)
- Verapamil, Diltiazem – slow AV nodal conduction and ventricular response
- Miscellaneous agents
- Adenosine – rapid termination of SVT
- Digoxin – rate control in AF and improved contractility in HF
- Class I (Sodium channel blockers)
- Key pharmacologic actions include:
- Alteration of ion movement across cardiac cell membranes
- Modification of automaticity, conduction velocity, and refractoriness
- Reduction of sympathetic nervous system influence
- Major risks of antidysrhythmic therapy:
- Proarrhythmia (worsening or new dysrhythmias)
- Hemodynamic instability (hypotension, bradycardia, heart block)
- Organ toxicity (pulmonary, hepatic, thyroid, hematologic)
- Most antidysrhythmics have a narrow therapeutic index, requiring:
- Individualized dosing
- Close ECG monitoring
- Regular assessment of serum drug levels and electrolytes
- Priority nursing responsibilities:
- Continuous ECG and vital sign monitoring
- Early recognition of toxic effects and conduction abnormalities
- Monitoring electrolytes (K⁺, Mg²⁺) and renal/hepatic function
- Patient education on adherence, symptom reporting, and drug interactions
- Evaluation of effectiveness is demonstrated by:
- Resolution or reduction of dysrhythmias
- Stable heart rate and rhythm
- Improved symptoms such as palpitations, dyspnea, chest discomfort
- Maintenance of adequate cardiac output and hemodynamic stability
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Drugs Used to Treat Dysrhythmias
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


