Please set your exam date
Neurologic Diagnostic Procedures
Study Questions
Practice Exericise 1
A patient presents with a sudden, severe headache described as "the worst headache of my life," and the physician suspects a cerebral aneurysm. Which of the following diagnostic tests is the most definitive for confirming this diagnosis?
Explanation
Cerebral angiography is considered the gold standard for confirming the presence, size, and location of a cerebral aneurysm. It provides detailed visualization of cerebral blood vessels, enabling precise diagnosis and surgical planning.
Rationale for correct answer:
C. Cerebral angiography: This test offers the highest resolution imaging of intracranial vasculature, allowing clinicians to detect aneurysms with accuracy. It also helps evaluate the aneurysm’s shape and risk of rupture, making it essential for definitive diagnosis.
Rationale for incorrect answers:
A. Non-contrast CT scan: While useful for detecting subarachnoid hemorrhage from a ruptured aneurysm, it does not provide detailed vessel imaging to confirm or characterize the aneurysm itself.
B. Electroencephalogram (EEG): EEG measures electrical brain activity and is used for seizure evaluation, not aneurysm diagnosis.
D. Magnetic resonance imaging (MRI) without contrast: MRI can detect vascular abnormalities, but without contrast or specialized techniques like MRA, it is less definitive than angiography.
Take home points:
- Cerebral angiography remains the gold standard for aneurysm diagnosis.
- CT is valuable for detecting bleeding but not for detailed vascular assessment.
- Timely and accurate imaging is critical to prevent catastrophic rupture.
A nurse is preparing a patient for a cerebral angiogram. Which of the following pre-procedure actions are essential? Select all that apply
Explanation
Before a cerebral angiogram, the nurse must ensure the patient is safe for contrast dye use, appropriately prepared with NPO status, and has a baseline vascular assessment. Obtaining a detailed history helps identify any conditions or medications that may affect the procedure or recovery. Sedatives are not always required and are administered only if prescribed.
Rationale for correct answers:
A. Assessing for any known allergies to iodine-based contrast dye: Essential to prevent allergic or anaphylactic reactions to the contrast used during angiography.
B. Ensuring the patient has been NPO for 6–8 hours: Reduces the risk of aspiration during the procedure, especially if sedation is required.
C. Checking and documenting peripheral pulses in the limb to be used: Provides a baseline for comparison after the procedure to detect vascular complications.
D. Obtaining a full medical history and current medication list: Critical for identifying bleeding risks (e.g., anticoagulants) and other potential contraindications.
Rationale for incorrect answer:
E. Administering a sedative to all patients to ensure they remain still: Sedation is not universally required; some patients undergo the procedure under local anesthesia with minimal or no sedation. Administration depends on the patient’s condition and provider’s order.
Take home points:
- Always assess for contrast dye allergy before angiographic procedures.
- NPO status helps prevent aspiration if sedation is used.
- Peripheral pulse checks are vital for detecting post-procedure vascular compromise.
- Sedation is individualized, not routine for every patient.
A physician orders a cerebral CT scan for a patient who has experienced head trauma. The scan is ordered without contrast. The primary reason for this is to:
Explanation
A non-contrast CT scan is the preferred initial imaging for head trauma because acute blood appears hyperdense and is easily identifiable without the obscuring effect of contrast. This allows for rapid detection of intracranial hemorrhage, which is critical in emergency management.
Rationale for correct answer:
A. Visualize blood more easily and quickly: Contrast dye can obscure fresh blood on imaging. A non-contrast CT is fast, widely available, and highly sensitive for detecting acute intracranial bleeding, making it the gold standard in acute head injury evaluation.
Rationale for incorrect answers:
B. Identify a brain tumor: While CT scans can sometimes detect tumors, MRI is generally preferred for tumor evaluation, and contrast is often used to enhance visualization of mass lesions.
C. Assess for vascular abnormalities: CT angiography or cerebral angiography is better for vascular assessment; a plain CT is not ideal for this purpose.
D. Minimize radiation exposure to the patient: The decision to use or avoid contrast is based on diagnostic needs, not radiation exposure; contrast does not affect the radiation dose.
Take home points:
- Non-contrast CT is the first-line imaging for acute head trauma to detect bleeding.
- Contrast is avoided initially because it can mask acute hemorrhage.
- MRI and contrast-enhanced CT are more useful for tumors and vascular lesions in non-emergent settings.
Following a cerebral angiogram, a nurse is providing post-procedure care. Which of the following interventions and assessments are a priority? Select all that apply
Explanation
Post-cerebral angiogram care focuses on preventing bleeding at the puncture site, detecting neurological changes early, avoiding complications from contrast dye, and maintaining limb immobilization to promote hemostasis. Immediate ambulation is avoided to reduce the risk of bleeding.
Rationale for correct answers:
B. Checking the puncture site for bleeding or hematoma formation: This is critical to detect and manage hemorrhage early, which is a common complication due to the arterial puncture.
C. Assessing the patient's neurological status and level of consciousness: Neurological changes may indicate complications such as embolism or intracranial bleeding, requiring immediate intervention.
D. Keeping the patient's affected limb straight and immobilized for several hours: Immobilization reduces the risk of bleeding and allows the arterial puncture to heal properly.
E. Monitoring for signs of allergic reaction to the contrast dye: Allergic reactions can occur minutes to hours after exposure and may range from mild rash to severe anaphylaxis.
Rationale for incorrect answers:
A. Encouraging the patient to ambulate immediately to prevent clot formation: Early ambulation after an arterial procedure increases the risk of bleeding and hematoma formation; the patient should remain on bed rest with limb immobilization for several hours.
Take home points:
- Monitor puncture site closely for bleeding or hematoma after cerebral angiogram.
- Assess neurological status frequently to detect post-procedure complications early.
- Keep affected limb immobilized to prevent bleeding.
- Watch for delayed allergic reactions to contrast dye.
A non-contrast cerebral CT scan of a patient with a sudden onset of symptoms reveals a bright, hyperdense area in the brain. This finding is most indicative of:
Explanation
On a non-contrast CT scan, acute blood appears as a bright (hyperdense) area. This is a hallmark finding of a hemorrhagic stroke, which occurs when a blood vessel ruptures and bleeds into brain tissue. The high density is due to the clot’s protein content and the absence of dilution by cerebrospinal fluid.
Rationale for correct answer:
B. A hemorrhagic stroke: Acute intracranial bleeding appears bright on a non-contrast CT because the hemoglobin in clotted blood has high attenuation. This imaging helps differentiate hemorrhagic stroke from ischemic stroke, guiding immediate treatment decisions.
Rationale for incorrect answers:
A. An ischemic stroke: In the early stages, ischemic strokes may appear normal or show subtle hypodense changes on CT. They do not typically present as bright, hyperdense areas.
C. Multiple sclerosis: MS lesions are best detected with MRI and appear as hypodense or isodense areas on CT, not bright hyperdensities.
D. A brain abscess: Abscesses may appear as ring-enhancing lesions with contrast but are not hyperdense on non-contrast CT unless calcified or hemorrhagic.
Take home points:
- Acute blood is hyperdense on non-contrast CT and strongly suggests hemorrhage.
- CT scans are the preferred first-line imaging for suspected stroke to distinguish between hemorrhagic and ischemic types.
- Early identification of hemorrhagic stroke is essential because treatment differs drastically from ischemic stroke.
Practice Exercise 2
Which of the following best describes the primary purpose of an electroencephalogram (EEG)?
Explanation
An EEG records the brain's electrical impulses through electrodes placed on the scalp. It is primarily used to diagnose seizure disorders, assess brain function, and monitor patients during certain surgeries.
Rationale for correct answer:
B. To measure the brain’s electrical activity: EEG measures spontaneous electrical activity generated by neuronal firing, which is crucial for diagnosing epilepsy and other neurological disorders.
Rationale for incorrect answers:
A. To assess cerebral blood flow: This is done using tests like cerebral angiography or transcranial Doppler, not EEG.
C. To visualize brain structures: CT and MRI are used for structural imaging.
D. To measure intracranial pressure: ICP monitoring devices are used for this, not EEG.
Take home points:
- EEG is functional, not structural, brain testing.
- It is essential for seizure diagnosis and brain death evaluation.
- Preparation often includes avoiding caffeine and washing hair before electrode placement.
A nurse is performing a Glasgow Coma Scale assessment. Which components are evaluated? Select all that apply
Explanation
The GCS evaluates eye opening, verbal response, and motor response to assess level of consciousness. It does not directly assess pupil size or reflexes, though these may be part of a broader neurological exam.
Rationale for correct answers:
A. Eye opening response: Indicates arousal and basic brainstem function.
B. Verbal response: Reflects cerebral cortex function.
C. Motor response: Demonstrates ability to follow commands and motor cortex integrity.
Rationale for incorrect answers:
D. Pupil size: Part of cranial nerve assessment, not GCS.
E. Reflex testing: Evaluates spinal and peripheral nerve function, not included in GCS scoring.
Take home points:
- GCS ranges from 3–15, with lower scores indicating deeper coma.
- It’s a quick, standardized method for neurological assessment.
- Monitoring trends is more important than a single score.
Which of the following are priority nursing interventions for a patient undergoing intracranial pressure (ICP) monitoring? Select all that apply
Explanation
Proper positioning, leveling of the transducer, and strict asepsis are key to accuracy and infection prevention. Flushing and encouraging increased intrathoracic pressure can dangerously raise ICP.
Rationale for correct answers:
A. Level at foramen of Monro: Ensures accurate pressure readings.
B. Elevate HOB 30 degrees: Promotes venous drainage and lowers ICP.
D. Aseptic technique: Prevents life-threatening central nervous system infections.
Rationale for incorrect answers:
C. Routinely flush the system: Risk of increasing ICP or damaging brain tissue.
E. Encourage coughing/straining: These maneuvers increase ICP and should be avoided.
Take home points:
- ICP should be maintained below 20 mmHg.
- Prevention of infection and accurate measurement are top priorities.
- Positioning plays a vital role in ICP control.
Which statement about lumbar puncture is most accurate?
Explanation
A lumbar puncture is used to obtain CSF for analysis, measure CSF pressure, or administer medications. It must be delayed if increased ICP is suspected to prevent herniation.
Rationale for correct answer:
B. To collect CSF for diagnostic testing: This is the main purpose, aiding in diagnosis of infections, hemorrhage, and certain neurological conditions.
Rationale for incorrect answers:
A. Perform immediately if elevated ICP suspected: This is dangerous; it can precipitate brain herniation.
C. Contraindicated in suspected meningitis: LP is actually indicated to confirm meningitis diagnosis, unless contraindicated by raised ICP.
D. Requires general anesthesia: Most LPs are done under local anesthesia and patient cooperation.
Take home points:
- LP is valuable for diagnosing CNS infections and subarachnoid hemorrhage.
- Always assess for ICP before performing.
- Positioning and sterile technique are critical.
Which statement about lumbar puncture is most accurate?
Explanation
Good electrode contact, avoidance of stimulants, medication management, and sometimes sleep deprivation improve diagnostic accuracy.
Rationale for correct answers:
A. Wash hair: Oils interfere with electrode adhesion.
B. Avoid caffeine: Prevents altered brain activity patterns.
D. Continue medications unless told otherwise: Some EEGs assess baseline brain function while on medication.
E. Sleep deprivation: Used to increase seizure detection.
Rationale for incorrect answers:
C. Fast completely for 12 hours: Unnecessary and may cause hypoglycemia, affecting EEG results.
Take home points:
- EEG prep focuses on clean scalp, avoiding stimulants, and following medication instructions.
- Sleep deprivation protocols can help trigger abnormalities in certain cases.
- EEG is safe, painless, and non-invasive
Practice Exercise 3
A physician is concerned about a patient's potential for a skull fracture after a fall. Which of the following imaging modalities would be the most appropriate initial diagnostic study to order?
Explanation
A CT scan is the most appropriate initial imaging study for suspected skull fractures after trauma because it provides rapid, detailed visualization of both bone and brain structures. It is highly sensitive for detecting fractures and associated intracranial injuries, which are critical to identify in acute settings.
Rationale for correct answer:
C. Computed Tomography (CT) scan: CT is the preferred imaging modality in acute head trauma due to its speed, availability, and excellent bone detail, allowing for accurate fracture detection and evaluation of intracranial hemorrhage or edema.
Rationale for incorrect answers:
A. Positron Emission Tomography (PET) scan: PET is used mainly for metabolic imaging in oncology or neurology, not for acute trauma evaluation.
B. Magnetic Resonance Imaging (MRI): MRI provides excellent soft tissue detail but is time-consuming and less sensitive than CT for detecting acute fractures.
D. Conventional skull X-ray: Although it can detect fractures, skull X-rays are less sensitive and less commonly used due to inferior imaging quality compared to CT.
Take home points:
- CT scan is the first-line imaging for suspected skull fractures in trauma.
- Rapid identification of fractures and brain injury improves patient outcomes.
- MRI and PET have roles in other neurological assessments but are not appropriate for acute skull fracture diagnosis.
Which of the following statements are true regarding a Magnetic Resonance Imaging (MRI) scan of the brain? Select all that apply
Explanation
MRI is the imaging modality of choice for detailed visualization of soft tissues, including brain tumors and demyelinating diseases. It offers superior contrast resolution compared to CT, allowing better differentiation of brain structures.
Rationale for correct answers:
B. Preferred modality for soft tissue visualization: MRI provides detailed images of brain parenchyma and pathology, making it superior for detecting tumors, inflammation, and demyelination.
D. Superior contrast resolution: MRI’s ability to distinguish subtle differences in tissue contrast exceeds that of CT, which is more useful for bone and acute hemorrhage detection.
Rationale for incorrect answers:
A. Uses ionizing radiation: MRI uses strong magnetic fields and radio waves, not ionizing radiation, which makes it safer for repeated imaging.
C. Patients with pacemakers or certain metal implants: Many pacemakers and metal implants are contraindications for MRI due to risk of malfunction or injury.
E. Fast procedure: MRI scans typically take 30 minutes to over an hour, which is longer than CT scans.
Take home points:
- MRI is ideal for soft tissue brain imaging and neurological diseases.
- It does not expose patients to radiation but requires screening for implants.
- MRI offers high contrast but is more time-consuming than CT.
A patient with a history of epilepsy is being evaluated for a potential surgical resection. The goal is to identify areas of decreased brain activity where seizures originate. Which functional neuroimaging scan would be most useful for this purpose?
Explanation
A SPECT scan measures cerebral blood flow and can detect regions of altered perfusion, identifying areas of decreased or increased brain activity associated with seizure foci. This functional imaging is valuable in pre-surgical planning for epilepsy patients.
Rationale for correct answer:
C. Single-Photon Emission Computed Tomography (SPECT) scan: SPECT provides functional imaging of brain perfusion during seizures or interictal periods, helping localize seizure origins for targeted surgical intervention.
Rationale for incorrect answers:
A. Conventional skull X-ray: Provides no functional information and is inadequate for epilepsy evaluation.
B. Non-contrast CT scan: Useful for structural brain assessment but does not assess brain activity.
D. Cerebral angiogram: Visualizes cerebral vasculature but does not provide functional data about seizure activity.
Take home points:
- SPECT is a valuable tool for localizing seizure foci in epilepsy.
- Functional imaging complements structural studies like MRI.
- Accurate localization aids in improving surgical outcomes.
Which of the following are contraindications for a patient undergoing a Magnetic Resonance Imaging (MRI) scan? Select all that apply
Explanation
Certain implants and metallic foreign bodies pose serious safety risks during MRI because of the strong magnetic fields. Cochlear implants, cardiac pacemakers, and metallic foreign bodies in the eye can be displaced or damaged, leading to injury or malfunction.
Rationale for correct answers:
A. Cochlear implant: Most cochlear implants are not MRI-compatible due to magnetic components that can cause heating or movement.
D. Cardiac pacemaker: Many pacemakers are contraindicated because the MRI’s magnetic field can interfere with device function or cause device damage.
E. Metallic foreign body in the eye: Ferromagnetic objects can move during MRI, causing severe ocular injury.
Rationale for incorrect answers:
B. History of claustrophobia: This is a relative contraindication; sedation or open MRI machines can help manage anxiety.
C. Intrauterine device (IUD): Most modern IUDs are MRI-safe and do not pose a contraindication.
Take home points:
- Always screen patients for implants or metal before MRI.
- Some contraindications are absolute (pacemakers, metal in eye), others are relative (claustrophobia).
- Alternatives or precautions can often enable safe imaging when needed.
A PET scan is ordered to evaluate a patient with suspected Alzheimer's disease. The scan is primarily used to assess:
Explanation
PET scans measure the metabolic activity of brain tissue by detecting radiotracer uptake, which reflects cellular function. In Alzheimer's disease, areas of decreased metabolism, especially in the temporal and parietal lobes, help support the diagnosis.
Rationale for correct answer:
C. The metabolic activity and function of different brain regions: PET provides functional imaging by showing how active various parts of the brain are, which is crucial in neurodegenerative diseases like Alzheimer's where metabolism decreases in affected regions.
Rationale for incorrect answers:
A. Structural integrity: MRI or CT scans evaluate structural brain changes, not PET.
B. Brain bleed: CT is preferred to detect hemorrhages.
D. Vascular flow: Cerebral angiography or CT/MR angiography assess blood flow, not PET.
Take home points:
- PET scans assess brain metabolism and function, not structure.
- They are useful in differentiating Alzheimer’s from other dementias.
- PET complements other imaging modalities in comprehensive neurological assessment.
Comprehensive Questions
A nurse is caring for a client post-lumbar puncture who reports a throbbing headache when sitting upright for meals. Which of the following are appropriate actions by the nurse? Select all that apply
Explanation
A lumbar puncture (LP), also known as a spinal tap, is a procedure used to collect cerebrospinal fluid (CSF) for diagnostic or therapeutic purposes. One of the most common complications following this procedure is a post-lumbar puncture headache, which is typically positional and worsens when the client is sitting upright. The headache results from a leak of CSF at the puncture site, leading to decreased intracranial pressure. Nursing care focuses on alleviating symptoms and promoting healing of the puncture site. Appropriate interventions include analgesic administration, hydration, and maintaining the client in a supine position to reduce CSF leakage and discomfort.
Rationale for Correct Answers:
B. Assist client to eat meals while lying flat in bed: Lying flat decreases the gravitational pull that exacerbates CSF leakage and helps reduce the intensity of the headache. It also facilitates clot formation at the puncture site, promoting healing.
C. Administer an opioid medication: Opioid analgesics are often used when non-opioid medications are insufficient to relieve pain. They provide effective symptom control while the underlying CSF leak resolves.
D. Encourage client to increase fluid intake: Increasing fluids supports the production of cerebrospinal fluid and may speed recovery. Hydration can also help maintain normal intracranial volume and pressure.
Rationale for Incorrect Answers:
A. Use the Glasgow Coma Scale when assessing the client: The Glasgow Coma Scale (GCS) is primarily used to assess neurological status and level of consciousness in clients with head injury or suspected brain dysfunction. It is not indicated solely for managing post-lumbar puncture headaches.
E. Place client in a “cannonball” position: This position is used to facilitate needle insertion during the LP procedure. After the procedure, it does not alleviate symptoms and may cause discomfort or worsen the headache.
Key Takeaways:
• Post-lumbar puncture headaches are positional and related to CSF leakage.
• Lying flat, hydration, and analgesics are key nursing interventions.
• Positions used during the LP procedure or unnecessary neurologic assessments are not helpful in managing headache symptoms.
.A nurse is caring for a client who experienced a traumatic head injury and has an intraventricular catheter (ventriculostomy) for ICP monitoring. The nurse should monitor the client for which of the following complications related to the ventriculostomy?
Explanation
An intraventricular catheter (ventriculostomy) is a device used to monitor intracranial pressure (ICP) and drain excess cerebrospinal fluid (CSF) in clients with severe brain injury. While it provides valuable real-time data on ICP, it also carries a significant risk of infection because it involves direct access to the brain's ventricles. Meningitis or ventriculitis can occur if strict aseptic technique is not maintained. Nurses must closely observe for signs of infection, such as fever, change in mental status, or purulent drainage from the catheter site.
Rationale for Correct Answer:
B. Infection: Ventriculostomy catheters provide a direct route for pathogens into the central nervous system. This places the client at risk for life-threatening infections like meningitis or ventriculitis, which require immediate recognition and intervention.
Rationale for Incorrect Answers:
A. Headache: While headaches can occur with increased ICP or CSF drainage, they are not specific to ventriculostomy-related complications. Headaches are common and nonspecific and not considered a direct complication of the catheter itself.
C. Aphasia: Aphasia is a neurologic deficit related to brain injury, particularly in the dominant hemisphere, but it is not a complication of ventriculostomy. It reflects damage from the trauma itself, not the monitoring device.
D. Hypertension: Hypertension may occur as a compensatory response to increased ICP (as part of Cushing’s triad), but it is not a direct complication of the ventriculostomy catheter. It signals a systemic or neurologic response, not an issue with the catheter.
Key Takeaways:
• Infection is the most serious and common complication of ventriculostomy use.
• Nurses must maintain sterile technique and monitor closely for signs of CNS infection.
• Other symptoms like headache or hypertension may relate to the injury, not the catheter itself.
A nurse is assessing a client for changes in the level of consciousness using the Glasgow Coma Scale. The client opens his eyes when spoken to, speaks incoherently, and moves his extremities when pain is applied. Which of the following is the correct scoring by the nurse using the Scale that indicates the client has a moderate head injury?
Explanation
The Glasgow Coma Scale (GCS) is a tool used by healthcare professionals to assess a client's level of consciousness following a neurological injury such as traumatic brain injury. It evaluates three components: eye opening (E), verbal response (V), and motor response (M), with a total score ranging from 3 to 1E. A score between 9 and 12 indicates a moderate head injury. The client's responses—eye opening to voice, confused verbal response, and withdrawal from pain—match a GCS score of 11, confirming moderate brain injury severity. Accurate scoring is essential for determining the appropriate level of care and monitoring progression.
Rationale for Correct Answer:
B. E3 + V4 + M4 = 11: The client opens their eyes to verbal stimuli (E3), responds with confused conversation (V4), and withdraws from pain (M4). These responses total a GCS of 11, which falls in the range of moderate head injury. This score reflects the client’s partial awareness and purposeful motor responses, warranting close monitoring for improvement or deterioration.
Rationale for Incorrect Answers:
A. E2 + V3 + M5 = 10: This score would indicate eye opening only to pain (E2), inappropriate words (V3), and withdrawal from pain (M5). However, the client opens eyes to speech, not pain, and speaks in complete but confused sentences (not just inappropriate words), making this an inaccurate representation.
C. E4 + V5 + M6 = 15: This score indicates normal neurologic function—spontaneous eye opening, oriented verbal responses, and command-following motor responses. It reflects a client with no head injury, which does not match the described presentation.
D. E2 + V2 + M4 = 8: This score represents a severe head injury, including eye opening to pain only (E2), incomprehensible sounds (V2), and withdrawal to pain (M4). The client in this case is more responsive than this scoring suggests.
Key Takeaways:
• A GCS score of 9–12 indicates a moderate traumatic brain injury.
• Accurate interpretation of behavioral cues is essential for determining neurologic status.
• Eye, verbal, and motor responses must be assessed separately and scored accordingly for reliable evaluation.
A nurse is developing a plan of care for a client who is scheduled for a cerebral angiogram with contrast dye. Which of the following statements by the client should the nurse report to the provider? Select all that apply
Explanation
A cerebral angiogram is a diagnostic imaging procedure that uses iodinated contrast dye and fluoroscopy to visualize cerebral blood flow. Prior to the procedure, the nurse must assess for conditions that could pose a risk or require modification of care, such as pregnancy, bleeding risk from anticoagulants, or allergies to contrast agents. Some client-reported statements, especially those related to contrast dye sensitivity and anticoagulation, require immediate provider notification.
Rationale for Correct Answers:
A. “I think I may be pregnant.”: Exposure to radiation and contrast dye during a cerebral angiogram may pose potential harm to a developing fetus. This possibility should be investigated and reported before proceeding.
B. “I take Coumadin.”: Warfarin is an anticoagulant that increases the client’s risk for bleeding during the procedure. The provider must evaluate coagulation status and possibly pause or adjust therapy.
D. “I am allergic to shrimp.”: Although a seafood allergy does not automatically mean an iodine allergy, a history of shrimp allergy may be associated with contrast dye sensitivity. The provider should assess further and consider premedication to prevent a hypersensitivity reaction.
Rationale for Incorrect Answers:
C. “I take antihypertensive medication.”: Antihypertensive medications are generally safe and may even be beneficial for clients undergoing angiography. There is no need to stop these medications unless directed by the provider.
E. “I am allergic to latex.”: Latex allergy is important to document, but it is not a specific concern related to angiography with contrast dye. Latex-free equipment is widely available, and this allergy does not require cancellation or modification of the procedure itself.
Key Takeaways:
• Always report possible pregnancy, use of anticoagulants, and contrast dye allergy risks before cerebral angiography.
• Latex allergy, while relevant, does not pose a direct risk during contrast administration.
• Routine medications like antihypertensives are generally not contraindicated unless otherwise instructed.
A nurse is providing education to a client who is to undergo an electroencephalogram (EEG) the next day. Which of the following information should the nurse include in the teaching?
Explanation
An electroencephalogram (EEG) is a noninvasive procedure that evaluates electrical activity in the brain. Clients scheduled for a sleep-deprived EEG are often instructed to stay awake most of the night before the test to increase the chance of detecting abnormal brain wave activity. Sleep deprivation can help provoke seizures or abnormal discharges, improving diagnostic accuracy for epilepsy or other neurological conditions.
Rationale for Correct Answer:
B. “Try to stay awake most of the night prior to the procedure.”: Clients are often advised to reduce sleep before an EEG to enhance the sensitivity of the test, especially when evaluating seizure disorders. Sleep-deprived EEGs help uncover abnormalities that may not appear in a standard, well-rested recording.
Rationale for Incorrect Answers:
A. “Do not wash your hair the morning of the procedure.”: Clients should be instructed to wash their hair the night before or the morning of the test and avoid using conditioners, sprays, or gels. Clean, product-free hair improves electrode contact with the scalp.
C. “The procedure will take approximately 15 minutes.”: A standard EEG typically lasts 30 to 60 minutes, not 1E. Additional time may be needed for preparation or if extended monitoring is ordered.
D. “You will need to lie flat for 4 hours after the procedure.”: EEG is a noninvasive and painless procedure that does not require any recovery time or post-procedure positioning. Clients can resume normal activities immediately unless sedatives were used.
Key Takeaways:
• Sleep deprivation before EEG enhances detection of abnormal brain activity.
• Clients should wash hair prior to the EEG and avoid hair products.
• EEG is painless, noninvasive, and typically lasts longer than 15 minutes with no special recovery required.
A client scheduled for magnetic resonance imaging (MRI) has arrived at the radiology department. The nurse who prepares the client for the MRI should prioritize which of the following actions?
Explanation
An MRI uses strong magnetic fields and radio waves to create detailed images of the body. The most critical safety measure is ensuring the removal of all metal-containing objects, as metal can become a projectile hazard, cause burns, or interfere with image quality. This includes jewelry, hearing aids, belts, and sometimes certain implants. The nurse must prioritize metal screening above all other preparations to prevent serious injury.
Rationale for Correct Answer:
B. Removing all metal-containing objects: Metal objects pose a severe risk in the MRI suite due to the powerful magnetic field. Removing metal is the first priority for safety and must be done before entering the scanner room. This step also ensures image accuracy.
Rationale for Incorrect Answers:
A. Withholding stimulants 24 to 48 hours prior to exam: This is not necessary for most MRI procedures. It may apply to specialized tests like EEGs or cardiac stress testing but not standard MRIs.
C. Instructing the client to void prior to the MRI: While a full bladder may cause some discomfort, it is not dangerous and does not interfere with MRI function. Voiding is not the priority.
D. Initiating an IV line for administration of contrast: This may be required if the MRI is ordered with contrast, but not all MRIs require contrast. Even when needed, IV access is secondary to safety screening for metal.
Key Takeaways:
• Metal screening is the top priority before any MRI to prevent injury and ensure image quality.
• MRIs use magnetic fields, not radiation—making metal objects and implants high-risk items.
• Other preparations like voiding or IV access are important but not as critical as ensuring metal safety compliance.
The client in the ED has just had a diagnostic lumbar puncture. To reduce the incidence of a post-lumbar puncture headache, what is the nurses most appropriate action? Post lp headache
Explanation
A post-lumbar puncture headache occurs due to leakage of cerebrospinal fluid (CSF) from the puncture site, which leads to reduced intracranial pressure. The most evidence-based nursing action to reduce the risk of this complication is to position the client supine with the head of the bed flat immediately after the procedure. This position supports CSF pressure equilibrium and promotes closure of the dural puncture.
Rationale for Correct Answer:
B. Position the client supine with the head of bed flat: Lying flat reduces gravitational CSF leakage and encourages clot formation at the puncture site. This position is typically maintained for 4 to 8 hours to lower the incidence of post-lumbar puncture headaches, especially in the first critical hours after the procedure.
Rationale for Incorrect Answers:
A. Position the client prone: Although used in some cases, the prone position is not the standard recommendation for post-lumbar puncture care. It may provide pressure over the site but does not facilitate CSF pressure balance as effectively as lying supine.
C. Position the client left side-lying: This position is commonly used during the lumbar puncture for needle insertion but is not effective post-procedure for headache prevention.
D. Administer acetaminophen as ordered: Acetaminophen can relieve a headache after it occurs, but it does not prevent a post-lumbar puncture headache. Prevention is priority in the immediate post-procedural period.
Key Takeaways:
• The supine, flat position is best for preventing post-lumbar puncture headache.
• Post-LP headaches are caused by CSF leakage, and position helps promote closure of the puncture site.
• Analgesics treat symptoms but do not prevent the complication.
A trauma client in the ICU has been declared brain dead. What diagnostic test is used in making the determination of brain death?
Explanation
Brain death is a clinical and legal diagnosis indicating the irreversible cessation of all brain activity, including the brainstem. While the diagnosis is primarily clinical, confirmatory tests may be used to support the findings—especially in cases where the full clinical exam cannot be completed. Electroencephalography (EEG) is the most commonly used test to confirm brain death by demonstrating the absence of electrical activity in the cerebral cortex over a sustained period of time.
Rationale for Correct Answer:
B. Electroencephalography (EEG): EEG is a diagnostic test that measures electrical activity in the brain. In brain death, the EEG will show no detectable cerebral activity, confirming the absence of brain function. It is a key confirmatory test, particularly when confounding factors are present.
Rationale for Incorrect Answers:
A. Magnetic resonance imaging (MRI): While MRI provides detailed structural imaging of the brain, it does not assess functional brain activity. It may show evidence of brain injury but is not used to confirm brain death.
C. Electromyelography (EMG): EMG is used to evaluate neuromuscular disorders and peripheral nerve function. It does not measure brain activity and is not relevant to brain death determination.
D. Computed tomography (CT): Like MRI, CT scans provide structural imaging, which may reveal brain swelling or herniation but do not assess cerebral activity. Therefore, CT is not diagnostic for brain death.
Key Takeaways:
• EEG is the preferred confirmatory test for brain death, detecting absence of cerebral activity.
• Imaging studies like MRI and CT show brain structure but not function.
• Brain death diagnosis relies on both clinical criteria and electrophysiological confirmation when needed.
A client is scheduled for CT scanning of the head because of a recent onset of neurologic deficits. What should the nurse tell the client in preparation for this test?
Explanation
A computed tomography (CT) scan of the head is a noninvasive diagnostic tool that produces cross-sectional images of the brain to assess for stroke, bleeding, or masses. To ensure clear images, the client must lie still throughout the procedure to avoid motion artifacts, which can distort the results. While the scan is relatively quick and painless, patient cooperation is key to image accuracy.
Rationale for Correct Answer:
C. You will need to lie still throughout the procedure: Movement during the CT scan can blur the images, making them less useful for identifying subtle neurological changes. Lying still is essential for image clarity and diagnostic accuracy.
Rationale for Incorrect Answers:
A. No metal objects can enter the procedure room: This applies more strictly to MRI scans, where magnetic fields can attract metal. CT scanners use X-rays, not magnets, so metal is not as strictly contraindicated—although clients may be asked to remove certain objects like jewelry to improve image quality.
B. You need to fast for 8 hours prior to the test: Fasting is only required for CT scans involving IV contrast, and even then, the duration is usually 2–4 hours, not H. If contrast is not used, fasting is not needed at all.
D. There will be a lot of noise during the test: CT scanners produce some sound but are much quieter than MRI machines. Excessive noise is not a concern for this type of imaging.
Key Takeaways:
• Stillness during a CT scan is critical for accurate imaging.
• CT does not require metal restrictions or noise precautions like MRI.
• Fasting is only necessary if contrast dye is to be used, and even then, only for a few hours.
A client for whom the nurse is caring has positron emission tomography (PET) scheduled. In preparation, what should the nurse explain to the client?
Explanation
A positron emission tomography (PET) scan is a functional imaging study that uses a radioactive tracer (often glucose-based) to detect metabolic activity in the body. This scan can be used to identify areas of abnormal brain function, tumors, or degenerative disease. Because the radioactive glucose is injected intravenously, some clients may experience dizziness, lightheadedness, or headache during or after the test as a mild, transient reaction to the tracer or the metabolic shift.
Rationale for Correct Answer:
D. The test may result in dizziness or lightheadedness: Although generally safe, PET scans involve radioactive tracer injection, and clients can experience temporary side effects like dizziness or fatigue. These symptoms are usually mild and resolve quickly, but clients should be informed and monitored.
Rationale for Incorrect Answers
A. The test will temporarily limit blood flow through the brain: PET scans do not limit blood flow; instead, they assess blood flow and glucose metabolism. This statement is inaccurate and misleading.
B. An allergy to iodine precludes getting the radio-opaque dye: PET tracers are not iodine-based. Iodine allergy is relevant for contrast CT scans, but not a contraindication for PET scans.
C. The client will need to endure loud noises during the test: Unlike MRI, PET scans are quiet. There may be some mechanical sounds from the machine, but loud noises are not characteristic of PET imaging.
Key Takeaways:
• PET scans evaluate metabolic activity, not structure, using radioactive tracers.
• Clients may feel lightheaded or dizzy due to tracer injection, but this is usually brief.
• PET scans are quiet, and iodine allergy is not relevant to this procedure.
A client is scheduled for a myelogram and the nurse explains to the client that this is an invasive procedure, which assesses for any lesions in the spinal cord. The nurse should explain that the preparation is similar to which of the following neurologic tests?
Explanation
A myelogram is an invasive diagnostic procedure used to visualize the spinal cord, nerve roots, and surrounding subarachnoid space using contrast dye injected into the spinal canal via lumbar puncture. Because of this, the preparation and positioning for a myelogram closely resemble those of a lumbar puncture, including obtaining informed consent, checking for allergies to contrast dye, and proper positioning during and after the procedure.
Rationale for Correct Answer:
A. Lumbar puncture: A myelogram requires injection of contrast dye into the subarachnoid space through a lumbar puncture. Therefore, preparation (e.g., client positioning, sterile technique, consent, allergy screening) and aftercare (e.g., monitoring for headache or CSF leak) are very similar to a standard lumbar puncture.
Rationale for Incorrect Answers:
B. MRI: MRI is a noninvasive imaging procedure that uses magnetic fields and does not involve puncturing the spinal canal or injecting contrast into the CSF unless performed with special contrast protocols.
C. Cerebral angiography: This procedure involves injection of contrast dye into cerebral arteries, typically via a femoral catheter, and does not involve accessing the spinal canal.
D. EEG: EEG is noninvasive and involves placement of electrodes on the scalp to monitor electrical activity in the brain. It does not use contrast dye or invasive techniques.
Key Takeaways:
• Myelogram preparation is most similar to a lumbar puncture due to shared technique and spinal access.
• Contrast dye is used in both procedures, requiring allergy assessment and informed consent.
• Other tests like EEG, MRI, and cerebral angiography differ significantly in terms of invasiveness and preparation.
The critical care nurse provides care for a client who is admitted for the treatment of head trauma and prescribed mannitol to reduce intracranial pressure (ICP). Which electrolyte is the priority for the nurse to monitor?
Explanation
Mannitol is an osmotic diuretic commonly used in clients with increased intracranial pressure (ICP) to reduce cerebral edema by drawing fluid from the brain into the vascular system. However, this diuresis can cause significant fluid and electrolyte imbalances, particularly affecting sodium levels. Hypernatremia or hyponatremia may develop depending on the patient's fluid status, so sodium must be closely monitored to prevent neurological deterioration or worsening cerebral edema.
Rationale for Correct Answer:
D. Sodium: Mannitol causes osmotic diuresis, which may result in hypernatremia if excessive water loss occurs or hyponatremia if free water replacement is inadequate. Either imbalance can worsen neurologic status, making sodium the most critical electrolyte to monitor in these patients.
Rationale for Incorrect Answers:
- Potassium: Although mannitol can cause some renal electrolyte losses, potassium disturbances are less common and less urgent than sodium changes in the context of mannitol therapy.
- Chloride: Chloride may be altered as it accompanies sodium loss or retention, but it is not typically the primary concern in mannitol administration.
- Magnesium: Magnesium levels can be affected by diuretics, but neurologic implications of sodium imbalance take priority in clients with increased ICP.
Key Takeaways:
• Sodium is the priority electrolyte to monitor when administering mannitol due to the risk of diuresis-induced imbalances.
• Both hypernatremia and hyponatremia can worsen neurologic status and must be addressed promptly.
• While other electrolytes are also monitored, sodium directly affects cerebral fluid balance and ICP.
A nurse is teaching a group of students the main structures that play a role with altering intracranial pressure. Which of the following structures should the nurse include? Select all that apply
Explanation
The components that contribute to intracranial pressure (ICP) are described by the Monro-Kellie doctrine: brain tissue, cerebrospinal fluid (CSF), and blood. The dura mater, as part of the meningeal layers, also influences ICP dynamics.
Rationale for Correct Answers:
A. Brain: The brain tissue itself is one of the primary components of intracranial volume and contributes directly to ICP.
C. Cerebrospinal Fluid: CSF circulates within the ventricles and subarachnoid space and significantly influences ICP.
D. Blood: Cerebral blood volume impacts ICP through changes in arterial or venous flow.
F. Dura mater: The dura mater helps contain the intracranial contents and plays a structural role in pressure regulation.
Rationale for Incorrect Answers:
B. Neurons: While part of brain tissue, individual neurons are not discussed separately in ICP dynamics.
E. Periosteum: This membrane covers the outer surface of bone and is not involved in intracranial volume or pressure regulation.
Key Takeaways:
• Intracranial pressure is determined by the volume of brain tissue, blood, and CSF within the skull.
• The Monro-Kellie doctrine helps explain compensatory changes among these components.
• Structures outside the cranial cavity, such as the periosteum, do not impact ICP.
A nurse is caring for 4 clients. Which of the clients below is at the highest risk for increased intracranial pressure?
Explanation
Traumatic brain injury (TBI) is a serious disruption in normal brain function caused by an external force, such as a blow to the head, fall, or penetrating injury. It ranges in severity from mild concussions to severe brain damage and can lead to temporary or permanent cognitive, physical, and psychological impairments. TBI is a leading cause of disability and death worldwide, often requiring urgent assessment, neuroimaging, and interventions to reduce intracranial pressure and preserve neurologic function.
Rationale for Correct Answer:
B. TBI often leads to cerebral edema or bleeding, both of which increase ICP and can cause brain herniation if unmanaged.
Rationale for Incorrect Answers:
A. Severe hypotension typically lowers cerebral perfusion pressure but does not increase ICP directly.
C. Myocardial infarction can have neurological complications (e.g., hypoxic injury) but does not usually raise ICP.
D. Eye surgery may cause localized swelling or pressure but is unlikely to result in elevated ICP unless there are specific complications.
Key Takeaways:
• Traumatic brain injury is the leading cause of increased ICP.
• ICP elevation can lead to herniation and death if untreated.
• Systemic issues like hypotension or MI don't usually elevate ICP directly.
A client with increased ICP has the following vital signs: blood pressure 99/60, HR 65, Temperature 10A.6°F, respirations 14, oxygen saturation of 95%. ICP reading is 21 mmHg. Based on these findings you would:
Explanation
Hyperthermia, or elevated body temperature, is a concerning finding in clients with increased intracranial pressure (ICP). It may result from damage to the hypothalamus, the brain's temperature-regulating center, especially in traumatic brain injury, hemorrhagic stroke, or central nervous system infections. Elevated temperature can increase cerebral metabolic demand, which in turn raises cerebral blood flow and worsens ICP.
Rationale for Correct Answer:
C. Cooling interventions help control fever, which can worsen ICP by increasing cerebral metabolism and blood flow.
Rationale for Incorrect Answers:
A. Vasopressors are not appropriate unless the patient is in shock. BP is low but not severely, and raising BP can worsen cerebral edema.
B. Oxygen is within normal range (95%), so additional oxygen is not necessary.
D. Suctioning can increase ICP transiently and should be used cautiously and only when airway clearance is needed.
Exams on Neurologic Diagnostic Procedures
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
- Objectives
- Introduction
- Cerebral Angiogram
- Cerebral Computed Tomography (CT) Scan
- Practice Exericise 1
- Electroencephalography (EEG)
- Glasgow Coma Scale (GCS)
- Intracranial Pressure (ICP) Monitoring
- Lumbar Puncture (Spinal Tap)
- Practice Exercise 2
- Magnetic Resonance Imaging (MRI) Scan
- PET and SPECT Scans
- Radiography (X-Ray)
- Practice Exercise 3
- Comprehensive Questions
Notes Highlighting is available once you sign in. Login Here.
Objectives
- Identify the major diagnostic tests used to assess neurological function, including CT, MRI, EEG, PET, lumbar puncture, and cerebral angiography.
- Describe the nursing responsibilities before, during, and after common neurologic procedures, such as lumbar puncture and myelogram.
- Interpret findings from diagnostic tools like the Glasgow Coma Scale and understand their clinical significance in assessing level of consciousness.
- Explain the pathophysiology and clinical presentation of traumatic brain injury, including signs of increased intracranial pressure (ICP).
- Recognize potential complications of neurologic procedures, such as infection, CSF leakage, post-lumbar puncture headache, or allergic reactions to contrast dye.
- Prioritize nursing interventions for clients with increased ICP, including positioning, medication administration, and temperature management.
- Differentiate between invasive and noninvasive neurologic diagnostic tests and identify their indications.
- Evaluate client statements or conditions that require provider notification before neurologic procedures.
Introduction
• Neurologic assessment and diagnostic procedures are used to evaluate neurologic function by testing
indicators such as mental status, motor functioning, electrical activity, and intracranial pressure.
• Neurologic assessment and diagnostic procedures that nurses should be knowledgeable about include:
✔ Cerebral angiogram
✔ Cerebral computed tomography (CT) scan
✔ Electroencephalography (EEG)
✔ Glasgow Coma Scale (GCS)
✔ Intracranial pressure (ICP) monitoring
✔ Lumbar puncture (spinal tap)
✔ Magnetic resonance imaging (MRI) scan
✔ Positron emission tomography (PET) and single-photon emission computed tomography (SPECT) scans
✔ Radiography (x-ray)
Cerebral Angiogram
A cerebral angiogram provides visualization of the cerebral blood vessels.
✔ Digital subtraction angiography “subtracts” the bones and tissues from the images, providing
x-rays with only the vessels apparent.
✔ The procedure detects defects, narrowing, or obstruction of arteries or blood vessels in brain.
✔ The procedure is performed within the radiology department because iodine-based contrast dye is injected into an artery during the procedure.
• Indications
✔ A cerebral angiogram is used to assess the blood flow to and within the brain, identify aneurysms, and define the vascularity of tumors (useful for surgical planning). It may also be used therapeutically to inject medications that treat blood clots or to administer chemotherapy.
• Preprocedure
✔ If the client is pregnant, a determination of the risks to the fetus versus the benefits of the
information obtained by this procedure should be made.
✔ Nursing Actions
‣ Instruct the client to refrain from consuming food or fluids for 4 to 6 hr prior to the procedure.
‣ Assess for allergy to shellfish or iodine, which would require the use of a different contrast media. Any history of bleeding or taking anticoagulant medication requires additional
considerations and additional monitoring to ensure clotting after the procedure.
‣ Assess BUN and serum creatinine to determine kidney’s ability to excrete the dye.
‣ Ensure that the client is not wearing any jewelry.
‣ A mild sedative for relaxation is occasionally administered prior to and during the procedure
and vital signs are continuously monitored during the procedure.
✔ Client Education
‣ Instruct the client about the importance of not moving during the procedure and about the
need to keep the head immobilized.
‣ Instruct the client to void immediately before the test.
‣ Instruct the client about a metallic taste in the mouth, a warm sensation over the face, jaw,
tongue, lips, and behind the eyes from the dye injected during procedure.
• Intraprocedure
✔ The client is placed on a radiography table, where the client’s head is secured.
✔ A catheter is placed into an artery (usually in the groin or the neck), dye is injected, and x-ray
pictures are taken.
✔ Once all pictures are taken, the catheter is removed and a arterial closure device is used or pressure is held over the artery to control bleeding by thrombus formation sealing the artery.
• Postprocedure
✔ Nursing Actions
‣ The area is closely monitored to ensure that clotting occurs.
‣ Movements are restricted depending on the type of procedure used to seal the artery to prevent
rebleeding at the catheter site.
• Complications
✔ Bleeding
‣ There is a risk for bleeding or hematoma formation at the entry site.
‣ Nursing Actions
☐ Check the insertion site frequently.
☐ Check the affected extremity distal to the puncture site for adequate circulation (e.g., color,
temperature, pulses, and capillary refill).
☐ If bleeding does occur, apply pressure over the artery and notify the provider.
Cerebral Computed Tomography (CT) Scan
• A CT scan provides cross-sectional images of the cranial cavity. A contrast media may be used to enhance the images.
• Indications
✔ A CT scan can be used to identify tumors and infarctions, detect abnormalities, monitor response to treatment, and guide needles used for biopsies.
• Preprocedure
✔ If the client is pregnant, a determination of the risks to the fetus versus the benefits of the
information obtained by this procedure should be made.
✔ Nursing Actions
‣ If contrast media and/or sedation is expected:
☐ Instruct the client to refrain from consuming food or fluids for at least 4 hr prior to
the procedure.
☐ Assess for allergy to shellfish or iodine, which would require the use of a different
contrast media.
☐ Assess renal function (BUN and creatinine), because contrast media is excreted by
the kidneys.
‣ Because this procedure is performed with the client in a supine position, placing pillows in
the small of the client’s back may assist in preventing back pain. The head must be secured to
prevent unnecessary movement during the procedure.
‣ Ensure that the client’s jewelry is removed prior to this procedure. In general, clients wear a
hospital gown to prevent any metals from interfering with the x-rays.
• Intraprocedure
✔ The client must lie supine with the head stabilized during the procedure.
✔ Although CT scanning is painless, sedation may be provided.
• Postprocedure
✔ Nursing Actions
‣ There is no follow-up care associated with a CT scan.
‣ If contrast media is injected, monitor for allergic reaction and changes in kidney function.
‣ If sedation is administered, monitor the client until stable.
Electroencephalography (EEG)
• This noninvasive procedure assesses the electrical activity of the brain and is used to determine if there are abnormalities in brain wave patterns.
• Indications
✔ EEGs are most commonly performed to identify and determine seizure activity, but they are also useful for detecting sleep disorders and behavioral changes.
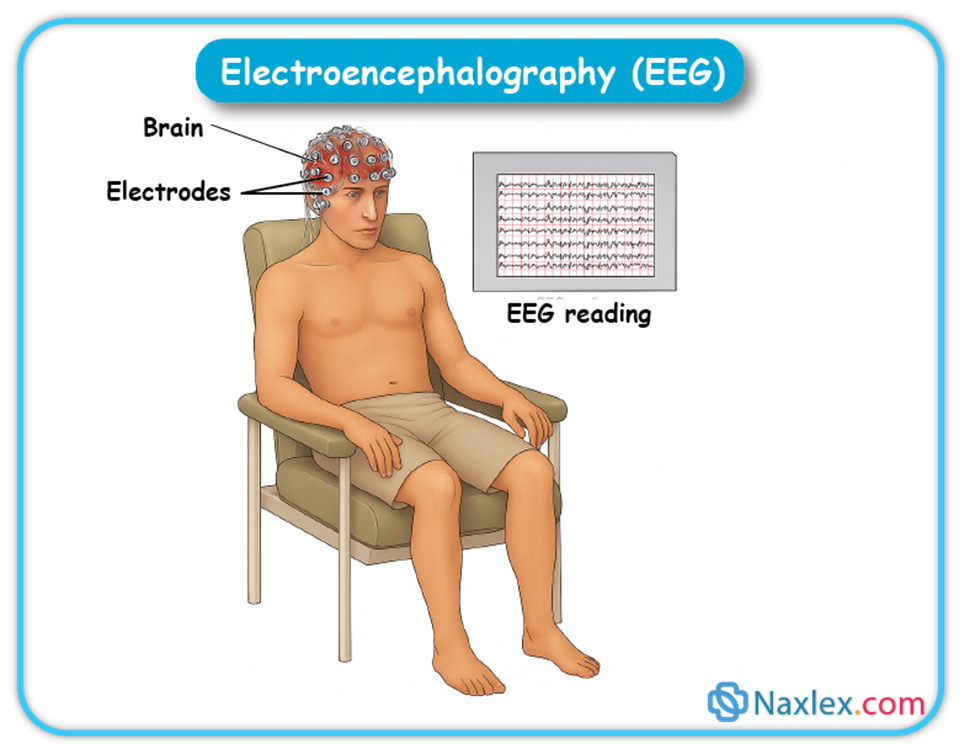
Preprocedure
✔ Nursing Actions
‣ Review medications with the provider to determine if they should be continued prior to
this procedure.
✔ Client Education
‣ Instruct the client to wash his hair prior to the procedure and eliminate all oils, gels, and sprays.
‣ If indicated, instruct the client to be sleep-deprived because this provides cranial stress,
increasing the possibility of abnormal electrical activity, such as seizure potentials, occurring
during the procedure.
• Intraprocedure
✔ The procedure generally takes 1 hr.
✔ There are no risks associated with this procedure.
✔ With the client resting in a chair or lying in bed, small electrodes are placed on the scalp and
connected to a brain wave machine or computer.
✔ Electrical signals produced by the brain are recorded by the machine or computer in the form of wavy lines. This documents brain activity.
✔ Notations are made when stimuli are presented or when sleep occurs. (Flashes of light or pictures may be used during the procedure to assess the client’s response to stimuli.)
✔ An EEG provides information about the ability of the brain to function and highlights areas
of abnormality.
• Postprocedure
✔ Client Education
‣ Instruct the client that normal activities may be resumed.
Glasgow Coma Scale (GCS)
• This assessment concentrates on neurologic function and is useful to determine the level of
consciousness and monitor response to treatment. The GCS is reported as a number, which allows health care providers to immediately determine if neurologic changes have occurred.
• Indications
✔ GCS scores are helpful in determining changes in the level of consciousness for clients
with head injuries, space occupying lesions or cerebral infarctions, and encephalitis. This is
important because complications related to neurologic injuries may occur rapidly and require
immediate treatment.
• Interpretation of Findings
✔ The best possible GCS score is 15. In general, total scores of the GCS correlate with the degree or level of coma.
✔ Less than 8 – Associated with severe head injury and coma
✔ 9 to 12 – Indicate a moderate head injury
✔ Greater than 13 – Reflect minor head trauma
• Procedure
✔ The GCS is calculated by using appropriate stimuli (a painful stimulus may be necessary) and then assessing the client’s response in three areas.
‣ Eye opening (E) – The best eye response, with responses ranging from 4 to 1
☐ 4 = Eye opening occurs spontaneously.
☐ 3 = Eye opening occurs secondary to voice.
☐ 2 = Eye opening occurs secondary to pain.
☐ 1 = Eye opening does not occur.
‣ Verbal (V) – The best verbal response, with responses ranging from 5 to 1
☐ 5 = Conversation is coherent and oriented.
☐ 4 = Conversation is incoherent and disoriented.
☐ 3 = Words are spoken, but inappropriately.
☐ 2 = Sounds are made, but no words.
☐ 1 = Vocalization does not occur.
‣ Motor (M) – The best motor response, with responses ranging from 6 to 1
☐ 6 = Commands are followed.
☐ 5 = Local reaction to pain occurs.
☐ 4 = There is a general withdrawal to pain.
☐ 3 = Decorticate posture (adduction of arms, flexion of elbows and wrists) is present.
☐ 2 = Decerebrate posture (abduction of arms, extension of elbows and wrists) is present.
☐ 1 = Motor response does not occur.
✔ Responses within each subscale are added, with the total score quantitatively describing the client’s level of consciousness. E + V + M = Total GCS
‣ In critical situations, where head injury is present and close monitoring is required, subscale
results may also be documented. Thus, a GCS may be reported as either a single number,
indicating the sum of the subscales (3 to 15), or as 3 numbers, one from each subscale
result, and the total (E3 V3 M4 = GCS 13). This allows providers to determine specific
neurologic function.
‣ Intubation limits the ability to use GCS summed scores. If intubation is present, the GCS may
be reported as two scores, with modification noted. This is generally reported as “GCS 5t”
(with the t representing the intubation tube).
Intracranial Pressure (ICP) Monitoring
• An ICP monitor is a device inserted into the cranial cavity that records pressure and is connected to a monitor that shows a picture of the pressure waveforms.
✔ Monitoring ICP facilitates continual assessment and is more precise than vague clinical
manifestations.
✔ The insertion procedure is always performed by a neurosurgeon in the operating room, emergency department, or critical care unit. This procedure is rarely used unless the client is comatose, so there is minimal need for pain medication and preprocedural teaching.
• Three Basic Types of ICP Monitoring Systems
✔ Intraventricular catheter (also called a ventriculostomy)
‣ A fluid-filled catheter is inserted into the anterior horn of the lateral ventricles (most often
on the right side) through a burr hole. The catheter is connected to a sterile drainage system
with a three-way stopcock that allows simultaneous monitoring of pressures by a transducer
connected to a bedside monitor and drainage of CSF.
✔ Subarachnoid screw or bolt
‣ A special hollow, threaded screw or bolt is placed into the subarachnoid space through a
twist‑drill burr hole in the front of the skull, behind the hairline. The bolt is connected by
fluid‑filled tubing to a transducer leveled at the approximate location of the lateral ventricles.
✔ Epidural or subdural sensor
‣ A fiber-optic sensor is inserted into the epidural space through a burr hole. The fiber-optic
device measures changes in the amount of light reflected from a pressure-sensitive diaphragm
in the catheter tip. The cable is connected to a precalibrated monitor that displays the
numerical value of ICP. This method of monitoring is noninvasive because the device does not
penetrate the dura.
• Indications
✔ ICP monitoring is useful for early identification and treatment of increased intracranial pressure. Clients who are comatose and/or have GCS scores of 8 are candidates for ICP monitoring.
✔ Client Presentation
‣ Symptoms of increased ICP include severe headache, deteriorating level of consciousness,
restlessness, irritability, dilated or pinpoint pupils, slowness to react, alteration in breathing
pattern (Cheyne Stokes respirations, central neurologic hyperventilation, apnea), deterioration
in motor function, and abnormal posturing (decerebrate, decorticate, flaccidity).
• Interpretation of Findings
✔ Normal ICP is 10 to 15 mm Hg. Persistent elevation of ICP extinguishes cerebral circulation, which will result in brain death if not treated urgently.
• Preprocedure
✔ The head is shaved around the insertion location. The site is then cleansed with an
antibacterial solution.
• Intraprocedure
✔ Local anesthetic can be used to numb the area if the client’s GCS indicates some level of
consciousness (GCS 8 to 11).
✔ Insertion and care of any ICP monitoring device requires surgical aseptic technique to reduce the risk for CNS infection.
• Postprocedure
✔ Nursing Actions
‣ Maintain system integrity at all times. There is a risk of serious, life-threatening infection.
‣ Inspect the insertion site at least every 24 hr for redness, swelling, and drainage. Change the
sterile dressing covering the access site per facility protocol.
‣ ICP monitoring equipment must be balanced and recalibrated per facility protocols.
‣ After the insertion procedure, observe ICP waveforms, noting the pattern of waveforms and
monitoring for increased ICP (a sustained elevation of pressure above 15 mm Hg).
‣ Assess the client’s clinical status and monitor routine and neurologic vital signs every hour
as needed.
• Complications
✔ Infection and bleeding
‣ The insertion and maintenance of an ICP monitoring system can cause infection and bleeding.
‣ Nursing Actions
☐ Follow strict surgical aseptic technique.
☐ Perform sterile dressing changes per facility protocol.
☐ Keep drainage systems closed.
☐ Limit monitoring to 3 to 5 days.
☐ Irrigate the system only as needed to maintain patency.
Lumbar Puncture (Spinal Tap)
• A lumbar puncture is a procedure during which a small amount of cerebrospinal fluid (CSF) is
withdrawn from the spinal canal and then analyzed to determine its constituents.
• Indications
✔ This procedure is used to detect the presence of certain diseases (multiple sclerosis, syphilis,
meningitis), infection, and malignancies. A lumbar puncture may also be used to reduce CSF
pressure, instill a contrast medium or air for diagnostic tests, or administer medication or
chemotherapy directly to spinal fluid.
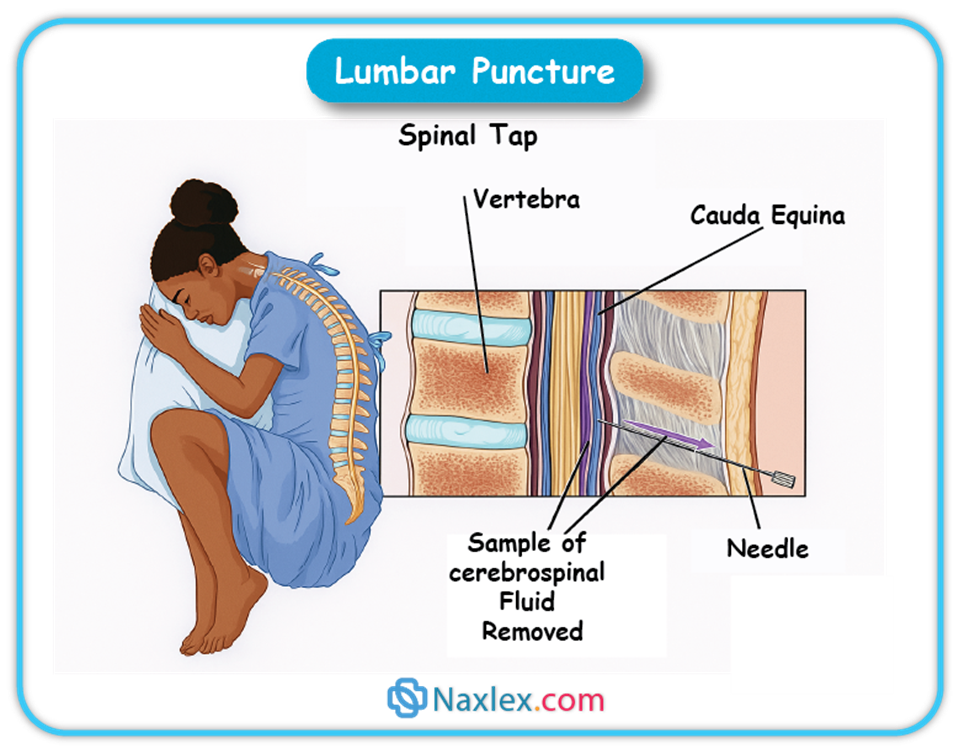
• Preprocedure
✔ The risks versus the benefits of a lumbar puncture should be discussed with the client prior to
undertaking this procedure.
‣ A lumbar puncture may be associated with rare but serious complications, especially when
performed in the presence of increased ICP (brain herniation).
‣ Lumbar punctures for clients with bleeding disorders or taking anticoagulants may result in
bleeding that compresses the spinal cord.
✔ Nursing Actions
‣ Ensure that all the client’s jewelry has been removed and that the client is wearing only a
hospital gown.
‣ Instruct the client to void prior to the procedure.
‣ Clients should be positioned to stretch the spinal canal. This may be done by having the client
assume a “cannonball” position while on one side or by having the client stretch over an
overbed table if sitting is preferred.
• Intraprocedure
✔ The area of the needle insertion is cleansed, and a local anesthesia is injected.
✔ This is not a painful procedure; there should be little need for pain or relaxing medication other than the local anesthesia.
✔ The needle is inserted and the CSF is withdrawn, after which the needle is removed.
✔ A manometer may be used to determine the opening pressure of the spinal cord, which is useful if increased pressure is a consideration.
• Postprocedure
✔ CSF is sent to the pathology department for analysis.
✔ Nursing Actions
‣ Monitor the puncture site. The client should remain lying for several hours to ensure that the
site clots and to decrease the risk of a post-lumbar puncture headache, caused by CSF leakage.
✔ Client Education
‣ Once stable, advise the client that normal activities may be resumed.
• Complications
✔ CSF leakage
‣ If clotting does not occur to seal the dura puncture site, CSF may leak, resulting in a headache
and increasing the potential for infection.
✔ Nursing Action
‣ Encourage the client to lie flat in bed, provide fluids for hydration, and administer
pain medication.
‣ Prepare the client for an epidural blood patch to seal off the hole in the dura if the
headache persists.
Magnetic Resonance Imaging (MRI) Scan
• An MRI scan provides cross-sectional images of the cranial cavity. A contrast media may be used to enhance the images.
✔ Unlike CT scans, MRI images are obtained using magnets, thus the consequences associated with radiation are avoided. This makes this procedure safer for women who are pregnant.
✔ The use of magnets precludes the ability to scan a client who has an artificial device (pacemakers, surgical clips, intravenous access port). If these are present, shielding may be done to prevent injury.
✔ MRI-approved equipment must be used to monitor vital signs and provide ventilator/oxygen
assistance to clients undergoing MRI scans.
• Indications
✔ MRI scans may be used to detect abnormalities, monitor response to treatment, and guide needles used for biopsies.
✔ MRIs are capable of discriminating soft tissue from tumor or bone. This makes the MRI scan more effective at determining tumor size and blood vessel location.
• Preprocedure
✔ Nursing Actions
‣ Assess for allergy to shellfish or iodine, which would require the use of a different contrast media.
‣ Ensure that the client’s jewelry is removed prior to this procedure. The client should wear a
hospital gown to prevent any metals from interfering with the magnet.
‣ If sedation is expected, the client should refrain from food or fluids for 4 to 8 hr prior to
the procedure.
‣ Determine if the client has a history of claustrophobia and explain the tight space and noise.
‣ Question the client about any implants containing metal (e.g., pacemaker, orthopedic joints,
artificial heart valves, intrauterine devices, aneurysm clips).
‣ Health care providers (and family members) who are in the scanning area while the magnet is
on must remove all jewelry, pagers, and phones to prevent damage to themselves or the magnet.
‣ Because this procedure is performed with the client in a supine position, placing pillows in
the small of the client’s back may assist in preventing back pain. The head must be secured to
prevent unnecessary movement during the procedure.
• Intraprocedure
✔ The client must lie supine with the head stabilized.
✔ MRI scanning is noisy, and earplugs or sedation may be provided.
• Postprocedure
✔ Nursing Actions
‣ No follow-up care is required after an MRI scan.
‣ If contrast media is injected, monitor the site to ensure that clotting has occurred and monitor
for any signs of an allergic reaction.
‣ If sedation is administered, monitor the client until stable.
PET and SPECT Scans
• PET and SPECT scans are nuclear medicine procedures that produce three-dimensional images of the head. These images can be static (depicting vessels) or functional (depicting brain activity).
✔ A glucose-based tracer is injected into the blood stream prior to the PET scan. This initiates
regional metabolic activity, which is then documented by the PET scanner. A radioisotope is used for SPECT scanning.
✔ A CT scan may be performed after a PET/SPECT scan, as this provides information regarding brain activity and pathological location (e.g., brain injury, death, neoplasm).
• Indications
✔ A PET/SPECT scan capture of regional metabolic is most useful in determining tumor activity
and/or response to treatment. PET/SPECT scans are also able to determine the presence of
dementia, indicated by the inability of the brain to respond to the tracer.
• Preprocedure
✔ PET/SPECT scans use radiation, thus the risk/benefit consequences to any client who may be
pregnant must be discussed.
✔ Nursing Actions
‣ Assess for a history of diabetes mellitus. While this condition does not preclude a PET/SPECT
scan, alterations in the client’s medications may be necessary to avoid hyperglycemia or
hypoglycemia before and after this procedure.
• Intraprocedure
✔ While the pictures are being obtained, the client must lie flat with the head restrained.
✔ This procedure is not painful and sedation is rarely necessary.
• Postprocedure
✔ Nursing Actions
‣ If radioisotopes are used, assess for allergic reaction.
‣ There is no follow-up care after a PET/SPECT scans.
‣ Because the tracer is glucose based and short acting (less than 2 hr), it is broken down within
the body as a sugar, not excreted.
Radiography (X-Ray)
• An x-ray uses electromagnetic radiation to capture images of the internal structures of an individual.
✔ A structure’s image is light or dark relative to the amount of radiation the tissue absorbs. The
image is recorded on a radiograph, which is a black and white image that is held up to light for
visualization. Some are recorded digitally and are available immediately.
✔ X-rays must be interpreted by a radiologist, who documents the findings.
• Indications
✔ X-ray examinations of the skull and spine can reveal fractures, curvatures, bone erosion and
dislocation, and possible soft tissue calcification, all of which can damage the nervous system.
• Preprocedure
✔ Nursing Actions
‣ There is no special preprocedure protocol for x-rays that do not use contrast. X-rays are often
the first diagnostic tool used after an injury (rule out cervical fracture in head trauma), and they
can be done without any preparation.
‣ Determine if female clients are pregnant.
‣ Ensure that the client’s jewelry is removed and that no clothes cover the area.
✔ Client Education
‣ Explain that the amount of radiation used in contemporary x-ray machines is very small.
• Intraprocedure
✔ Client Education
‣ Instruct the client to remain still during the procedure.
• Postprocedure
✔ Nursing Actions
‣ No postprocedure care is required.
✔ Client Education
‣ Inform the client when results will be available.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Neurologic Diagnostic Procedures
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


