Please set your exam date
Anticoagulants and Thrombolytic Agents
Study Questions
Introduction
A nurse is caring for a client who has a history of coronary thrombosis and is taking warfarin as a long-term anticoagulant therapy. What laboratory test should the nurse monitor to evaluate the effectiveness of warfarin?
Explanation
The INR is a standardized measure of the prothrombin time (PT), which reflects the activity of the extrinsic and common pathways of coagulation.
Warfarin is an anticoagulant that inhibits the synthesis of vitamin K-dependent clotting factors (II, VII, IX, and X), which are involved in these pathways.
Therefore, the INR is used to monitor the effectiveness of warfarin therapy and adjust the dose accordingly.The target INR range depends on the indication for warfarin, but it is usually between 2 and 3.
Choice A is wrong because activated partial thromboplastin time (aPTT) reflects the activity of the intrinsic and common pathways of coagulation.
Heparin is an anticoagulant that enhances the activity of antithrombin, which inhibits factors II, IX, X, XI, and XII, which are involved in these pathways.Therefore, the aPTT is used to monitor the effectiveness of heparin therapy.
Choice C is wrong because platelet count measures the number of platelets in the blood, which are involved in primary hemostasis.Platelet count is not affected by warfarin therapy, but it can be decreased by heparin-induced thrombocytopenia (HIT), a rare but serious complication of heparin therapy.
Choice D is wrong because fibrinogen level measures the amount of fibrinogen in the blood, which is a precursor of fibrin, the main component of blood clots.Fibrinogen level is not affected by warfarin therapy, but it can be decreased by disseminated intravascular coagulation (DIC), a condition where widespread clotting and bleeding occur simultaneously.
The normal ranges for these tests are as follows:
• INR: 0.8 to 1.2
• aPTT: 25 to 35 seconds
• Platelet count: 150 to 450 x 10^9/L
• Fibrinogen level: 2 to 4 g/L
A nurse is teaching a client who is prescribed clopidogrel, an antiplatelet drug, to prevent recurrent stroke. Which of the following statements should the nurse include in the teaching? (Select all that apply.)
Explanation
Clopidogrel is an antiplatelet drug that inhibits the ability of platelets to clump together as part of a blood clot.It is used to prevent recurrent stroke and other cardiovascular events in people who are at high risk.
Choice A is correct because taking aspirin or other nonsteroidal anti-inflammatory drugs (NSAIDs) while on clopidogrel can increase the risk of bleeding.These drugs also affect platelet function and can interfere with the action of clopidogrel.
Choice B is correct because bleeding is the most common side effect of clopidogrel.Any signs of bleeding, such as nosebleeds, bruising, or black stools, should be reported to the provider as they may indicate a serious complication.
Choice C is wrong because clopidogrel can be taken with or without food.Taking it with food does not prevent gastrointestinal upset, which is another possible side effect of clopidogrel.
Choice D is wrong because clopidogrel does not affect blood pressure.However, having high blood pressure can increase the risk of stroke and other cardiovascular events, so it is important to have it checked regularly and treated if necessary.
Choice E is correct because clopidogrel should be stopped at least 5 days before any planned surgery.This is to reduce the risk of excessive bleeding during or after the surgery.The provider should be informed about the use of clopidogrel and any other medications before undergoing any surgical procedure.
A nurse is preparing to administer alteplase, a thrombolytic drug, to a client who has an acute myocardial infarction. The nurse knows that this drug works by which mechanism?
Explanation
Alteplase works by activating plasminogen, which converts to plasmin, an enzyme that degrades fibrin.Fibrin is a protein that forms the meshwork of a blood clot, so by breaking it down, alteplase helps dissolve the clot and restore blood flow.
Choice A is wrong because alteplase does not inhibit platelet aggregation and adhesion.
Platelets are blood cells that stick together and form the initial plug in a blood clot.Alteplase does not affect platelets directly, but rather targets fibrin.
Choice B is wrong because alteplase does not interfere with the coagulation cascade.
The coagulation cascade is a series of reactions that lead to the formation of fibrin from fibrinogen.Alteplase does not inhibit any of the steps in this process, but rather activates plasminogen, which is already present in the blood.
Choice D is wrong because alteplase does not block the action of platelet activators or receptors.
Platelet activators are substances that stimulate platelets to aggregate and adhere, such as thrombin, ADP, and collagen.
Platelet receptors are molecules on the surface of platelets that bind to these activators or to other platelets, such as GPIIb/IIIa and GPVI.Alteplase does not affect these molecules, but rather targets fibrin.
A nurse is reviewing the medication history of a client who is prescribed cilostazol, an antiplatelet drug, for intermittent claudication. The nurse should recognize that which of the following medications is contraindicated with cilostazol?
Explanation
Omeprazole, a proton pump inhibitor, is contraindicated with cilostazol, an antiplatelet drug, for intermittent claudication.
This is because omeprazole can inhibit the metabolism of cilostazol by affecting the hepatic/intestinal enzyme CYP2C19, which is responsible for converting cilostazol to its active metabolites.This can result in increased plasma levels of cilostazol and increased risk of bleeding and adverse effects.
Choice B is wrong because metoprolol, a beta blocker, is not contraindicated with cilostazol.
Metoprolol can be used to treat hypertension, angina, and heart failure, which are common comorbidities in patients with intermittent claudication.Metoprolol does not interact significantly with cilostazol or affect its metabolism.
Choice C is wrong because simvastatin, a statin, is not contraindicated with cilostazol.
Simvastatin can be used to lower cholesterol and prevent cardiovascular events in patients with intermittent claudication.Simvastatin does not interact significantly with cilostazol or affect its metabolism.
Choice D is wrong because glyburide, a sulfonylurea, is not contraindicated with cilostazol.
Glyburide can be used to treat type 2 diabetes mellitus, which is a common risk factor for intermittent claudication.Glyburide does not interact significantly with cilostazol or affect its metabolism.
A nurse is administering enoxaparin, a low-molecular-weight heparin, to a client who has undergone orthopedic surgery. The nurse should administer this medication by which route and at which site?
Explanation
Subcutaneous injection in the abdomen.This is because enoxaparin is a low-molecular-weight heparin that is administered subcutaneously, usually in the abdomen or outer thigh.The drug should be clear and colorless or pale yellow.The dosage for adults is typically 30mg every 12 hours for 7 to 10 days, or 40mg once a day for 3 weeks after hip replacement surgery.The needle should be inserted fully into the skin and the syringe plunger should be pressed down to inject the drug.Injection sites should be rotated and areas of active skin disease or injury should be avoided.
Choice A is wrong because intramuscular injection in the deltoid muscle is not the recommended route or site for enoxaparin.Intramuscular injection may cause bleeding, bruising, or hematoma formation.
Choice C is wrong because intravenous infusion in a peripheral vein is not the recommended route for enoxaparin.Enoxaparin can be given intravenously only as a bolus injection for acute coronary syndrome, not as an infusion.
Choice D is wrong because intradermal injection in the forearm is not the recommended route or site for enoxaparin.Intradermal injection may cause skin irritation, infection, or necrosis.
Classification of Anticoagulant medications
A nurse is caring for a client who is receiving heparin therapy. Which laboratory test should the nurse monitor to determine the effectiveness of the medication?
Explanation
Activated partial thromboplastin time (aPTT) is the laboratory test most commonly used to monitor the anticoagulant effect of unfractionated heparin therapy. The aPTT measures the time it takes for blood to clot in the presence of heparin, which inhibits thrombin and other clotting factors.The aPTT should be maintained at 1.5 to 2.5 times the normal range, which is usually 25 to 35 seconds.
Choice B is wrong because prothrombin time (PT) is the laboratory test used to monitor the anticoagulant effect of warfarin, not heparin.
Warfarin inhibits the synthesis of vitamin K-dependent clotting factors, such as factor II, VII, IX, and X.The PT should be maintained at 1.5 to 2 times the normal range, which is usually 11 to 13 seconds.
Choice C is wrong because international normalized ratio (INR) is a standardized way of reporting the PT results, which are affected by different reagents and methods.
The INR is used to monitor warfarin therapy, not heparin therapy.The INR should be maintained at 2 to 3 for most indications of warfarin therapy.
Choice D is wrong because platelet count is not a direct measure of the anticoagulant effect of heparin, but rather a potential complication of heparin therapy.
Heparin can cause heparin-induced thrombocytopenia (HIT), a serious condition that causes low platelet count and increased risk of thrombosis.Platelet count should be monitored regularly during heparin therapy to detect HIT, which usually occurs within 5 to 10 days of exposure.The normal platelet count range is 150,000 to 450,000 per microliter of blood.
A nurse is caring for a client who is receiving warfarin therapy. Which of the following medications should the nurse expect to administer if the client develops bleeding as an adverse effect of the medication? (Select all that apply.)
Explanation
Vitamin K and fresh frozen plasma are both used to reverse the effects of warfarin and stop the bleeding.Vitamin K is a cofactor for the synthesis of clotting factors in the liver, and fresh frozen plasma contains clotting factors that can replenish the depleted ones.
Choice C is wrong because protamine sulfate is an antidote for heparin, not warfarin.Choice D is wrong because factor IX complex concentrate is used to treat hemophilia B, not warfarin-induced bleeding.
Choice E is wrong because tranexamic acid is an antifibrinolytic agent that prevents the breakdown of clots, but does not reverse the effects of warfarin.
Normal ranges for PT (prothrombin time) and INR (international normalized ratio) are 11 to 13.5 seconds and 0.8 to 1.2, respectively.Warfarin therapy aims to prolong the PT and INR to prevent clot formation.
A nurse is caring for a client who is receiving enoxaparin therapy for deep vein thrombosis (DVT). Which of the following statements by the client indicates an understanding of the medication?
Explanation
Enoxaparin is an anticoagulant that helps prevent the formation of blood clots in patients with DVT.It can also cause bleeding or other side effects, so patients should monitor for any signs of bleeding and report them to their provider.
Choice A is wrong because aspirin is not contraindicated with enoxaparin.Aspirin is also an antiplatelet agent that can prevent thrombosis, and it may be used in combination with enoxaparin for certain indications, such as acute coronary syndrome.
Choice B is wrong because ibuprofen is not contraindicated with enoxaparin.Ibuprofen is a nonsteroidal anti-inflammatory drug (NSAID) that can reduce pain and inflammation, and it may be used with enoxaparin for certain conditions, such as arthritis.However, NSAIDs can also increase the risk of bleeding, so patients should use them with caution and inform their provider if they are taking them.
Choice D is wrong because enoxaparin does not need to be taken with food.Enoxaparin is given by subcutaneous injection, so food does not affect its absorption or efficacy.Patients should follow the instructions on how to inject enoxaparin properly and store it at room temperature.
A client who has atrial fibrillation is prescribed warfarin therapy. Which of the following statements by the client indicates an understanding of the medication?
Explanation
“I should report any unusual bleeding or bruising to my provider.” This statement indicates that the client understands that warfarin is an anticoagulant that can increase the risk of bleeding and that any signs of bleeding should be reported promptly.Warfarin works by inhibiting the synthesis of vitamin K-dependent clotting factors, so the client should monitor their intake of vitamin K, but not avoid it completely.Warfarin can be taken with or without food, so choice B is not correct.
Aspirin is also an anticoagulant and can increase the risk of bleeding when taken with warfarin, so the client should avoid taking it unless prescribed by the provider
A nurse is caring for a client who has a mechanical heart valve and is receiving warfarin therapy to prevent thromboembolism formation. Which of the following statements by the client indicates an understanding of the medication?
Explanation
This statement indicates that the client understands that warfarin is a blood thinner that can increase the risk of bleeding and that any signs of bleeding should be reported to the provider promptly.The client may need to have their blood tested to check the level of anticoagulation and adjust their warfarin dose accordingly.
Choice A is wrong because the client should not avoid foods that are high in vitamin K, but rather keep their intake of vitamin K consistent.
Vitamin K is needed for the production of clotting factors and warfarin works by blocking its action.If the client changes their vitamin K intake, it can affect the effectiveness of warfarin and increase the risk of clotting or bleeding.
Choice B is wrong because warfarin can be taken with or without food.Food does not affect the absorption or metabolism of warfarin.
Choice D is wrong because the client should avoid taking aspirin while taking warfarin, unless prescribed by their provider.
Aspirin is another blood thinner that works by inhibiting platelets.Taking both warfarin and aspirin can increase the risk of bleeding significantly, especially in older adults.
Heparins
A nurse is preparing to administer subcutaneous heparin to a client with deep vein thrombosis. What is the appropriate technique for this procedure?
Explanation
Inject heparin at a 90-degree angle into the abdomen, at least 2 inches away from the umbilicus.This is the appropriate technique for administering subcutaneous heparin, as it ensures that the drug reaches the fat layer under the skin and reduces the risk of bleeding and bruising.
Choice B is wrong because heparin should not be injected into the deltoid muscle, as it may cause tissue damage and nerve injury.Heparin should also not be aspirated before injecting, as it may cause hematoma formation.
Choice C is wrong because heparin should not be injected at a 90-degree angle into the thigh, as it may cause pain and irritation.The thigh is also not a preferred site for heparin injection, as it has less fat tissue than the abdomen.
Choice D is wrong because heparin should not be injected at a 45-degree angle into the upper arm, as it may cause nerve damage and hematoma formation.Heparin should also not be massaged after injection, as it may increase the risk of bleeding and bruising.
A nurse is reviewing the laboratory results of a client who is receiving intravenous unfractionated heparin. The nurse notes that the client’s activated partial thromboplastin time (aPTT) is 120 seconds. What are the appropriate nursing actions in this situation? Select all that apply.
Explanation
A. Stop the heparin infusion immediately.This is correctbecause heparin is an anticoagulant that prevents blood clotting by inhibiting the formation of thrombin.
The activated partial thromboplastin time (aPTT) is a test that measures how long it takes for the blood to clot.
The normal range for aPTT is25 to 35 seconds.
A high aPTT indicates that the blood is taking too long to clot, which increases the risk of bleeding.
Therefore, the heparin infusion should be stopped to prevent further bleeding.
•
B. Administer protamine sulfate as ordered.This is correctbecause protamine sulfate is an antidote for heparin overdose.
It binds to heparin and neutralizes its anticoagulant effect.
Protamine sulfate should be administered as ordered by the health care provider to reverse the heparin overdose and restore normal clotting time.
•
C. Notify the health care provider of the result.This is correctbecause the health care provider should be informed of the abnormal aPTT result and the actions taken by the nurse.
The health care provider may order further tests or adjust the heparin dosage or frequency based on the client’s condition and response to treatment.
•
D. Draw a prothrombin time (PT) and international normalized ratio (INR) level.This is wrongbecause PT and INR are tests that measure the effect of warfarin, another anticoagulant, on blood clotting.
They are not affected by heparin and are not relevant for this client.
•
E. Monitor the client for signs and symptoms of bleeding.This is wrongbecause this is not an appropriate action in this situation.
The nurse should not wait for signs and symptoms of bleeding to occur, but should act immediately to stop the heparin infusion, administer protamine sulfate, and notify the health care provider.
Monitoring for bleeding is a preventive measure that should be done before and during heparin therapy, not after an overdose has occurred.
A nurse is educating a client who is prescribed low molecular weight heparin (LMWH) for home use. The client asks, “What is the difference between LMWH and regular heparin?” What is an appropriate response by the nurse?
Explanation
Low molecular weight heparin (LMWH) is a type of anticoagulant medication that prevents blood clots.
LMWH has several advantages over regular heparin, such as:
• LMWH has a lower risk of bleeding than regular heparin.LMWH has a more specific action on the clotting factors and less effect on platelets, which reduces the risk of bleeding complications.
• LMWH does not require frequent blood tests like regular heparin.LMWH has a more predictable and consistent effect than regular heparin, which means that the dose does not need to be adjusted based on blood tests.Regular heparin requires frequent monitoring of the activated partial thromboplastin time (aPTT) to ensure therapeutic levels.
• LMWH has a more predictable effect than regular heparin.LMWH has a longer half-life and a higher bioavailability than regular heparin, which means that it works more reliably and lasts longer in the body.Regular heparin has a variable response and can be affected by factors such as age, weight, and renal function.
Therefore, the nurse should explain to the client that LMWH is a safer and more convenient option than regular heparin for home use.
A nurse is caring for a client who develops heparin-induced thrombocytopenia (HIT) while receiving unfractionated heparin for pulmonary embolism. The nurse anticipates that the health care provider will order which of the following medications to treat this condition?
Explanation
Argatroban, which is a direct thrombin inhibitor that works by binding to thrombin. This is because argatroban is an alternative anticoagulant that can be used for patients with HIT, as it does not cause platelet aggregation or activation. Argatroban directly inhibits thrombin, which is the enzyme that converts fibrinogen to fibrin and activates platelets.
Choice A is wrong because warfarin, which is an oral anticoagulant that works by blocking vitamin K, is contraindicated in patients with HIT, as it can cause skin necrosis and limb gangrene due to microvascular thrombosis.
Warfarin also has a delayed onset of action and requires monitoring of the international normalized ratio (INR).
Choice B is wrong because aspirin, which is an antiplatelet agent that works by inhibiting cyclooxygenase, is also contraindicated in patients with HIT, as it can increase the risk of bleeding and does not prevent thrombosis.
Aspirin also has a long-lasting effect on platelet function and can interact with other drugs.
Choice D is wrong because streptokinase, which is a thrombolytic agent that works by converting plasminogen to plasmin, is not indicated for patients with HIT, as it can cause severe bleeding complications and allergic reactions.
Streptokinase also has a short half-life and requires continuous infusion.
A nurse is administering protamine sulfate to a client who has received an overdose of heparin. What are some important nursing considerations for this medication?
Explanation
Protamine sulfate should be given slowly intravenously within 30 minutes of heparin administration. This is because protamine sulfate is a strong base that neutralizes the anticoagulant effect of heparin, which is a strong acid. Protamine sulfate should be given within 30 minutes of heparin administration to prevent excessive bleeding or hemorrhage.Protamine sulfate should be given slowly intravenously to avoid adverse effects such as hypotension, bradycardia, pulmonary edema, and anaphylaxis.
Choice B is wrong because protamine sulfate should not be given rapidly or intramuscularly.Rapid administration can cause severe hypotension and shock, and intramuscular administration can cause local irritation and hematoma formation.
Choice C is wrong because protamine sulfate should not be given more than 60 minutes after heparin administration.The half-life of heparin is 60 to 90 minutes, and the anticoagulant effect of heparin will usually wear off within a few hours after discontinuation.Giving protamine sulfate after 60 minutes may cause excess anticoagulation or “heparin rebound” due to the longer half-life of protamine sulfate.
Choice D is wrong for the same reasons as choice B.Protamine sulfate should not be given rapidly or intramuscularly.
Vitamin K antagonists
A nurse is caring for a patient who is taking warfarin (Coumadin). Which of the following laboratory values should the nurse monitor regularly?
Explanation
The nurse should monitor the INR regularly for a patient who is taking warfarin (Coumadin), which is an anticoagulant that inhibits the synthesis of vitamin K-dependent clotting factors in the liver. The INR is a standardized measure of the prothrombin time (PT), which reflects the time it takes for blood to clot.The INR should be between2 and 3for most patients on warfarin therapy, unless otherwise specified by the provider.
Choice A is wrong becausehemoglobinis the protein in red blood cells that carries oxygen.
It is not affected by warfarin therapy and does not indicate the risk of bleeding or clotting.
Choice B is wrong becausehematocritis the percentage of blood volume that is occupied by red blood cells.
It is also not affected by warfarin therapy and does not indicate the risk of bleeding or clotting.
Choice C is wrong becauseplatelet countis the number of platelets in the blood.
Platelets are cell fragments that help with blood clotting by forming a plug at the site of injury.
Warfarin does not affect platelet production or function, but rather inhibits the clotting factors that are needed to stabilize the platelet plug.
Choice D is wrong becauseprothrombin time (PT)is the time it takes for blood to clot in the presence of a specific reagent.
It is affected by warfarin therapy, but it is not standardized and may vary depending on the reagent and the laboratory.
A nurse is caring for a patient who is taking warfarin (Coumadin). Which of the following instructions should the nurse include in the patient teaching?
Explanation
Warfarin (Coumadin) is an anticoagulant that works by inhibiting the synthesis of vitamin K-dependent clotting factors. Vitamin K is found in foods such as green leafy vegetables, broccoli, liver, and soybeans.Eating foods that are high in vitamin K can decrease the effectiveness of warfarin and increase the risk of blood clots.
Choice B is wrong because warfarin can be taken with or without food.
Taking the medication with food does not affect its absorption or action.
Choice C is wrong because stopping warfarin abruptly can increase the risk of thromboembolism.
If the patient experiences bleeding, they should notify their health care provider and follow their instructions.
They may need to adjust their dose or switch to another medication.
Choice D is wrong because aspirin is also an anticoagulant that inhibits platelet aggregation.
Taking aspirin with warfarin can increase the risk of bleeding and bruising.
The patient should avoid taking aspirin or other nonsteroidal anti-inflammatory drugs (NSAIDs) unless prescribed by their health care provider.
The patient who is taking warfarin should also have regular blood tests to monitor their international normalized ratio (INR), which measures how long it takes for their blood to clot.The target INR range for most patients is 2 to 3.
The patient should report any signs of bleeding, such as nosebleeds, gum bleeding, blood in urine or stool, or prolonged bleeding from cuts or wounds.
They should also report any signs of thrombosis, such as chest pain, shortness of breath, leg pain or swelling, or stroke symptoms.They should wear a medical alert bracelet or carry a card that identifies them as taking warfarin.
A client who is taking warfarin (Coumadin) reports experiencing nosebleeds and easy bruising. Which of the following statements by the client indicates a need for further teaching?
Explanation
This statement indicates a need for further teaching because aspirin is an antiplatelet drug that can increase the risk of bleeding when taken with warfarin (Coumadin), an anticoagulant.The patient should avoid aspirin and other nonsteroidal anti-inflammatory drugs (NSAIDs) and use acetaminophen (Tylenol) or other pain relievers that do not affect blood clotting.
Choice A is wrong because it is a correct statement.The patient should avoid activities that could cause injury, such as contact sports, shaving with a razor, or using sharp objects, because they could lead to bleeding complications while on warfarin (Coumadin).
Choice C is wrong because it is a correct statement.The patient should report any unusual bleeding to their healthcare provider, such as nosebleeds, easy bruising, blood in urine or stool, heavy menstrual bleeding, or bleeding gums.
These could be signs of excessive anticoagulation or adverse effects of warfarin (Coumadin).
Choice D is wrong because it is a correct statement.The patient should use a soft-bristled toothbrush and floss gently to prevent gum bleeding while on warfarin (Coumadin).The patient should also avoid dental procedures without consulting their healthcare provider first.
The normal range for INR (international normalized ratio), a test that measures how long it takes blood to clot, is 0.75-1.25 for people who are not taking warfarin (Coumadin).For people who are taking warfarin (Coumadin), the therapeutic range is usually 2-3, depending on the condition being treated.The patient’s INR level should be monitored regularly to adjust the dose of warfarin (Coumadin) and prevent bleeding or clotting complications.
A nurse is caring for a client who is taking warfarin (Coumadin). Which of the following statements by the client indicates an understanding of the medication?
Explanation
Warfarin (Coumadin) is an anticoagulant medication that prevents blood clots from forming or growing larger. It works by inhibiting the synthesis of vitamin K-dependent clotting factors in the liver. Warfarin can increase the risk of bleeding, so patients should monitor for signs of bleeding and report them to their healthcare provider.Some signs of bleeding are bruising, nosebleeds, gum bleeding, blood in urine or stool, and heavy menstrual bleeding.
Choice A is wrong because patients taking warfarin should not avoid foods that are high in vitamin K, but rather maintain a consistent intake of vitamin K.
Vitamin K is found in green leafy vegetables, such as spinach, kale, broccoli, and cabbage.Vitamin K can counteract the effects of warfarin and lower its effectiveness, so sudden changes in vitamin K intake can alter the patient’s response to warfarin.
Choice B is wrong because patients taking warfarin should not take aspirin for pain relief.
Aspirin is a nonsteroidal anti-inflammatory drug (NSAID) that can also inhibit platelet aggregation and increase the risk of bleeding.
Patients taking warfarin should avoid NSAIDs and other medications that can interact with warfarin, such as antibiotics, antifungals, anticonvulsants, and herbal supplements.Patients should consult their healthcare provider before taking any new medications or supplements.
Choice D is wrong because patients taking warfarin should not use a hard-bristled toothbrush.
A hard-bristled toothbrush can cause gum bleeding and increase the risk of oral infection.
Patients taking warfarin should use a soft-bristled toothbrush and floss gently to prevent gum bleeding.They should also avoid dental procedures that can cause bleeding, such as extractions, implants, or scaling.
A client who is taking warfarin (Coumadin) reports experiencing black tarry stools and abdominal pain. Which of the following statements by the client indicates a need for further teaching?
Explanation
This statement indicates a need for further teaching because taking an antacid can interfere with the absorption of warfarin and affect its effectiveness. The client should not self-medicate with any over-the-counter drugs without consulting their healthcare provider first.
Choice A is wrong because reporting black tarry stools and abdominal pain to the healthcare provider immediately is the appropriate action.These symptoms may indicate gastrointestinal bleeding, which is a serious adverse effect of warfarin.
Choice B is wrong because stopping the medication if these symptoms persist is not advisable.Warfarin should not be discontinued abruptly without medical supervision, as this can increase the risk of thrombosis.
Choice D is wrong because increasing the intake of green leafy vegetables is not harmful.
Green leafy vegetables are rich in vitamin K, which is the antidote for warfarin overdose.However, the client should maintain a consistent intake of vitamin K and avoid sudden changes in their diet.
Direct oral anticoagulants (DOACs)
A nurse is caring for a client who is receiving direct oral anticoagulants (DOACs). Which of the following adverse effects should the nurse monitor for?
Explanation
Gastrointestinal disturbances are a common adverse effect of direct oral anticoagulants (DOACs), which include nausea, vomiting, diarrhea, constipation, indigestion, and abdominal pain. These symptoms may be mild or severe, and may require dose adjustment or discontinuation of the DOAC.
Choice A is wrong because hypertension is not a known adverse effect of DOACs.In fact, some DOACs may lower blood pressure by reducing arterial stiffness.
Choice B is wrong because bradycardia is not a known adverse effect of DOACs.DOACs do not affect the cardiac conduction system or the autonomic nervous system.
Choice D is wrong because hypoglycemia is not a known adverse effect of DOACs.DOACs do not interfere with glucose metabolism or insulin secretion.
A nurse is caring for a client who is receiving direct oral anticoagulants (DOACs). Which of the following instructions should the nurse include in the teaching? Select all that apply.
Explanation
These are the instructions that the nurse should include in the teaching for a client who is receiving direct oral anticoagulants (DOACs).
Here is why:
Choice A is correct because DOACs increase the risk of bleeding and injury.The client should avoid activities that may cause trauma, such as contact sports, shaving with a razor, or using a toothpick.
Choice B is correct because DOACs should be taken at the same time every day to maintain a consistent level of anticoagulation.This helps to prevent fluctuations in the effect of the drug and reduces the risk of stroke or bleeding.
Choice C is correct because signs and symptoms of bleeding, such as bruising, bleeding gums, nosebleeds, blood in urine or stool, or prolonged bleeding from cuts, should be reported immediately to the health care provider.Bleeding can be a serious complication of DOACs and may require urgent treatment or reversal.
Choice D is correct because alcohol and aspirin can increase the risk of bleeding when taken with DOACs.
Alcohol can affect the liver function and interfere with the metabolism of DOACs.Aspirin can inhibit platelet function and impair the blood clotting process.
Choice E is wrong because monitoring vital signs regularly is not necessary for clients who are receiving DOACs.
Unlike warfarin, DOACs do not require frequent blood tests or dose adjustments based on the international normalized ratio (INR).However, the client should have periodic tests to check their kidney and liver function, as well as their blood count.
A nurse is caring for a client who is receiving direct oral anticoagulants (DOACs). The client reports experiencing abdominal pain and nausea. Which of the following statements by the client requires further assessment by the nurse?
Explanation
This statement by the client requires further assessment by the nurse because antacids can interfere with the absorption and effectiveness of direct oral anticoagulants (DOACs), which are used to prevent blood clots and stroke. The nurse should ask the client about the type, frequency, and dosage of antacids they are taking and inform the provider.
Choice A is wrong because taking the medication as prescribed is expected and does not indicate a problem.
Choice B is wrong because diarrhea can be a common side effect of DOACs and does not require further assessment unless it is severe or persistent.
Choice D is wrong because eating green leafy vegetables does not affect the action of DOACs, unlike vitamin K antagonists such as warfarin.
The client does not need to limit their intake of foods rich in vitamin K.
A nurse is caring for a client who is receiving direct oral anticoagulants (DOACs). The client reports experiencing dizziness and lightheadedness when standing up quickly. Which of the following statements by the client requires further assessment by the nurse?
Explanation
This statement by the client requires further assessment by the nurse because diarrhea can cause dehydration and electrolyte imbalance, which can affect the renal function and the clearance of direct oral anticoagulants (DOACs).Renal impairment can increase the risk of bleeding and adverse effects of DOACs. The nurse should monitor the client’s fluid intake and output, serum creatinine, electrolytes, and signs of bleeding. The nurse should also advise the client to report any persistent or severe diarrhea to their prescriber.
Choice A is wrong because taking the medication as prescribed is expected and does not indicate any problem with DOACs.
Choice C is wrong because over-the-counter antacids are generally safe to use with DOACs and do not affect their efficacy or safety.
However, the nurse should educate the client about potential drug interactions with other over-the-counter or herbal products and encourage them to consult their prescriber before taking any new medications.
Choice D is wrong because eating green leafy vegetables does not affect the anticoagulant effect of DOACs, unlike warfarin, which is influenced by dietary vitamin K intake.
The nurse should encourage the client to eat a balanced diet and maintain a consistent intake of vitamin K-rich foods.
A nurse is caring for a client who is receiving direct oral anticoagulants (DOACs). The client reports experiencing chest pain and shortness of breath. Which of the following actions should the nurse take first?
Explanation
The client is experiencing signs of a pulmonary embolism, which is a life-threatening complication of anticoagulant therapy. The priority action is to improve oxygenation and prevent hypoxia.Administering oxygen therapy can help achieve this goal.
Choice B is wrong because nitroglycerin is used to treat angina, not pulmonary embolism.
Nitroglycerin dilates the coronary arteries and reduces the workload of the heart, but it does not address the underlying cause of the chest pain and shortness of breath in this case.
Choice C is wrong because obtaining an electrocardiogram (ECG) is not the first action to take.
An ECG can help diagnose cardiac arrhythmias, ischemia, or infarction, but it does not provide immediate treatment for the client’s condition.
Choice D is wrong because aspirin is contraindicated in clients who are receiving direct oral anticoagulants (DOACs).
Aspirin increases the risk of bleeding and can interfere with the action of DOACs.DOACs are a newer class of anticoagulants that do not require regular blood testing or dietary restrictions like warfarin.Some examples of DOACs are rivaroxaban, edoxaban, apixaban, and dabigatran.
Direct thrombin inhibitors (DTIs)
A nurse is caring for a client who is receiving bivalirudin IV for a PCI procedure. Which of the following laboratory tests should the nurse monitor to evaluate the effectiveness of the drug?
Explanation
ECT.ECT stands for ecarin clotting time, which is a test that measures the anticoagulant effect of bivalirudin, a direct thrombin inhibitor.Bivalirudin is used for patients undergoing percutaneous coronary intervention (PCI) to prevent thrombotic complications.ECT is the most sensitive and specific test for monitoring bivalirudin therapy.
Choice A is wrong because PT stands for prothrombin time, which is a test that measures the extrinsic pathway of coagulation and the effect of warfarin, a vitamin K antagonist.PT is not affected by bivalirudin.
Choice B is wrong because INR stands for international normalized ratio, which is a standardized way of reporting PT results and the effect of warfarin.INR is also not affected by bivalirudin.
Choice C is wrong because aPTT stands for activated partial thromboplastin time, which is a test that measures the intrinsic pathway of coagulation and the effect of heparin, an indirect thrombin inhibitor.aPTT can be used to monitor bivalirudin therapy, but it is less sensitive and specific than ECT.
A nurse is teaching a client who has a new prescription for dabigatran to prevent stroke. Which of the following instructions should the nurse include? (Select all that apply.)
Explanation
Dabigatran is an anticoagulant that prevents blood clots and stroke.It can cause bleeding as a side effect, so the client should report any signs of bleeding, such as bruising, hematuria, or melena.The client should also use a soft toothbrush and an electric razor to prevent injury and bleeding.Dabigatran should be stored in its original container to maintain potency and protect it from moisture.
Choice A is wrong because dabigatran does not need to be taken with food to prevent gastrointestinal upset.It can be taken with or without food.
Choice E is wrong because dabigatran does not require regular blood tests to monitor the drug level.Unlike warfarin, dabigatran has a predictable anticoagulant effect and does not need frequent dose adjustments.
A nurse is reviewing the medication history of a client who is prescribed argatroban for HIT. Which of the following statements by the client indicates a need for further teaching?
Explanation
This statement by the client indicates a need for further teaching because aspirin can increase the risk of bleeding when taken with argatroban, which is an anticoagulant drug used to treat or prevent thrombosis in patients with heparin-induced thrombocytopenia (HIT). The client should avoid taking aspirin or other nonsteroidal anti-inflammatory drugs (NSAIDs) unless prescribed by their health care provider.
Choice A is wrong because avoiding alcohol while taking argatroban is a correct statement.
Alcohol can also increase the risk of bleeding and should be avoided or limited by the client.
Choice C is wrong because notifying the dentist that the client is taking argatroban is a correct statement.
The client should inform their dentist and other health care providers about their medication history before any invasive procedures, as they may need to adjust or stop their argatroban dose to prevent excessive bleeding.
Choice D is wrong because checking the blood pressure regularly at home is a correct statement.
The client should monitor their blood pressure and other signs of bleeding, such as bruising, nosebleeds, blood in urine or stool, or prolonged bleeding from cuts or wounds.
The client should also report any symptoms of thrombosis, such as chest pain, shortness of breath, leg pain or swelling, or stroke-like symptoms.
A nurse is preparing to administer lepirudin IV to a client who has DVT. Which of the following actions should the nurse take?
Explanation
Lepirudin is a direct thrombin inhibitor that is used as an anticoagulant in patients with heparin-induced thrombocytopenia (HIT).It is administered as an initial intravenous bolus dose followed by a continuous intravenous infusion for 2-10 days or longer if clinically needed.The infusion rate should be adjusted to the activated partial thromboplastin time (aPTT), which is a measure of the blood’s clotting ability. An infusion pump can ensure a constant and accurate delivery of the drug at the desired rate.
Choice A is wrong because flushing the IV line with heparin before and after giving lepirudin can increase the risk of bleeding and worsening HIT.Heparin is the cause of HIT and should be avoided in patients with this condition.
Choice C is wrong because administering lepirudin as a bolus injection over 15 seconds can result in a rapid and excessive anticoagulation effect, which can increase the risk of bleeding and hemorrhage.Lepirudin should be given as a bolus injection over 15-20 minutes, followed by a continuous infusion.
Choice D is wrong because monitoring the client’s platelet count daily is not sufficient to assess the efficacy and safety of lepirudin therapy.The platelet count is not affected by lepirudin and does not reflect its anticoagulant activity.The aPTT should be monitored at least once daily and more frequently in patients with renal impairment or increased bleeding risk.The normal platelet count range is 150,000 to 450,000 platelets per microliter of blood.
A nurse is caring for a client who has an overdose of dabigatran and is experiencing life-threatening bleeding. Which of the following drugs should the nurse anticipate administering as an antidote?
Explanation
• Dabigatran is a direct thrombin inhibitor that prevents the formation of blood clots.
It is used to treat atrial fibrillation, deep vein thrombosis, and pulmonary embolism.However, it can also cause bleeding complications, especially in high doses or in clients who have renal impairment, liver disease, or other risk factors.
• Idarucizumab is a monoclonal antibody that binds to dabigatran and reverses its anticoagulant effect.It is the only specific antidote for dabigatran overdose and should be administered intravenously as soon as possible.
• Choice A. Vitamin K is wrong because it is not an antidote for dabigatran.Vitamin K is used to reverse the effect of warfarin, a vitamin K antagonist that inhibits the synthesis of clotting factors.
• Choice B. Protamine sulfate is wrong because it is not an antidote for dabigatran.Protamine sulfate is used to reverse the effect of heparin, an indirect thrombin inhibitor that enhances the activity of antithrombin.
• Choice D. Aminocaproic acid is wrong because it is not an antidote for dabigatran.Aminocaproic acid is used to treat bleeding caused by excessive fibrinolysis, such as in hemophilia or after surgery.
Thrombolytic agents:
Thrombolytic agents
A nurse is preparing to administer alteplase, a second-generation thrombolytic agent, to a client with an acute ischemic stroke. Which of the following actions should the nurse take before administering the medication?
Explanation
The nurse should take all of the following actions before administering alteplase, a second-generation thrombolytic agent, to a client with an acute ischemic stroke:
• Check the client’s blood pressure and pulse.Alteplase can cause bleeding and hypotension, so the nurse should monitor the client’s vital signs closely and report any abnormal findings to the provider.
• Obtain a baseline complete blood count (CBC) and coagulation studies.Alteplase can increase the risk of hemorrhage, so the nurse should check the client’s platelet count, hemoglobin, hematocrit, prothrombin time (PT), international normalized ratio (INR), and activated partial thromboplastin time (aPTT) before and during therapy.The normal ranges for these tests are as follows:
➤ Platelet count: 150,000–400,000/mm3
➤ Hemoglobin: 13.5–17.5 g/dL for males; 12.0–15.5 g/dL for females
➤ Hematocrit: 38.8–50.0% for males; 34.9–44.5% for females
➤ PT: 11–13.5 seconds
➤ INR: 0.8–1.1
➤ aPTT: 25–35 seconds
• Assess the client’s neurological status using a standardized scale.Alteplase can improve the neurological outcome of ischemic stroke by dissolving the clot and restoring blood flow to the brain.However, it can also cause intracranial hemorrhage, which can worsen the neurological deficit.Therefore, the nurse should use a scale such as the National Institutes of Health Stroke Scale (NIHSS) or the Glasgow Coma Scale (GCS) to evaluate the client’s level of consciousness, motor function, sensory function, speech, vision, and other neurological functions before and after administering alteplase.
A nurse is reviewing the contraindications for thrombolytic therapy for a client with a peripheral arterial occlusion. Which of the following conditions would make the client ineligible for this therapy? (Select all that apply.)
Explanation
These are all contraindications for thrombolytic therapy, which is the administration of agents directly into an artery to break down thrombus.Thrombolytic therapy presents a serious risk for bleeding and requires careful monitoring.
Therefore, any condition that increases the risk of bleeding or hemorrhage would make the client ineligible for this therapy.
These conditions include:
• History of peptic ulcer disease: Peptic ulcers are erosions in the lining of the stomach or duodenum that can bleed and perforate.
Thrombolytic therapy could worsen the bleeding and cause life-threatening complications.
• Recent dental extraction: Dental extraction involves removing a tooth from its socket in the bone.
This can cause bleeding and infection in the oral cavity.
Thrombolytic therapy could increase the bleeding and delay the healing process.
• Chronic atrial fibrillation: Atrial fibrillation is an irregular and often rapid heart rate that can cause blood clots to form in the heart chambers.
Thrombolytic therapy could dislodge these clots and cause embolism in the brain, lungs, or other organs.
• Pregnancy: Pregnancy is a state of hypercoagulability that increases the risk of thrombosis.However, thrombolytic therapy is contraindicated in pregnancy because it can cause bleeding complications for both the mother and the fetus.
Choice E, diabetes mellitus, is not a contraindication for thrombolytic therapy.Diabetes mellitus is a chronic condition that affects the metabolism of glucose and insulin.It can increase the risk of cardiovascular diseases and stroke, but it does not directly affect the clotting cascade or the risk of bleeding.
Therefore, diabetes mellitus alone would not make the client ineligible for thrombolytic therapy.However, other factors such as blood pressure, blood glucose level, and renal function should be monitored closely during thrombolytic therapy.
A nurse is reviewing the contraindications for thrombolytic therapy for a client with a peripheral arterial occlusion. Which of the following conditions would make the client ineligible for this therapy? (Select all that apply.)
Explanation
A. History of peptic ulcer disease: Peptic ulcers increase the risk of gastrointestinal bleeding, making thrombolytics dangerous for these clients.
B. Recent dental extraction: Any recent surgery, including dental procedures, can lead to excessive bleeding due to clot dissolution from thrombolytics.
C. Chronic atrial fibrillation: Atrial fibrillation increases the risk of thromboembolism, but it is not a contraindication for thrombolytics. Clients with AFib may already be on anticoagulation therapy, which requires monitoring, but thrombolytics are still used in certain cases (e.g., ischemic stroke).
D. Pregnancy:Pregnancy is a relative contraindication due to the risk of placental abruption, fetal loss, and severe maternal bleeding.
E. Diabetes mellitus:Diabetes itself does not increase the risk of bleeding, so it is not a contraindication. However, diabetic clients with complications (e.g., retinopathy) require careful assessment.
A nurse is monitoring a client who is receiving streptokinase, a first-generation thrombolytic agent, for a pulmonary embolism. The nurse observes that the client has developed a rash, fever, and hypotension after receiving the medication.
Which of the following actions should the nurse take first?
Explanation
The client has developed signs of an allergic reaction to streptokinase, which can be life-threatening.Streptokinase is a drug that can cause bleeding, allergic reactions, and general discomfort.Allergic reactions can include nausea, vomiting, and low blood pressure.The first step in managing anaphylaxis is to remove the trigger if possible.
Therefore, stopping the infusion of streptokinase is the most appropriate action.
Choice B is wrong because administering epinephrine is not the first action to take.Epinephrine is a medication that can help reduce an allergic response by constricting blood vessels and relaxing airways.
However, it should be used after stopping the infusion of streptokinase and only if the client has an auto-injector or a doctor’s order.
Choice C is wrong because notifying the health care provider is not the first action to take.
The client needs immediate treatment to prevent shock and respiratory failure.
Calling 999 for an ambulance is more urgent than notifying the health care provider.
Choice D is wrong because drawing blood samples for antibody testing is not the first action to take.
Antibody testing can help diagnose a previous exposure to streptokinase, but it does not help.
A nurse is caring for a client who has received a thrombolytic agent for an acute ischemic stroke. The nurse notes that the client’s activated partial thromboplastin time (aPTT) is 120 seconds. What is the most appropriate action by the nurse?
Explanation
The nurse should notify the health care provider because an activated partial thromboplastin time (aPTT) of 120 seconds is significantly elevated and indicates a high risk of bleeding.The normal range for aPTT is 25 to 35 seconds. A thrombolytic agent is a medication that dissolves blood clots and restores blood flow to the brain after an acute ischemic stroke. However, it can also cause excessive bleeding and hemorrhage, which can be life-threatening.
Choice A is wrong because the finding is not normal and requires immediate intervention.
Choice B is wrong because vitamin K is an antidote for warfarin, an oral anticoagulant, not for a thrombolytic agent.
Vitamin K would not reverse the effects of a thrombolytic agent.
Choice C is wrong because protamine sulfate is an antidote for heparin, an injectable anticoagulant, not for a thrombolytic agent.
Protamine sulfate would not reverse the effects of a thrombolytic agent.
More questions
A nurse is caring for a client who has variant angina and is prescribed verapamil. Which of the following are expected outcomes of this medication? (Select all that apply.)
Explanation
Verapamil is a calcium channel blocker that is used to treat variant angina by dilating the coronary arteries and relieving the chest pain caused by spasms.It also reduces blood pressure and heart rate, but these are not the expected outcomes for variant angina.
Choice A is wrong because verapamil decreases heart rate, not increases it.This can help reduce the oxygen demand of the heart, but it is not the main goal of therapy for variant angina.
Choice B is wrong because verapamil decreases contractility, not increases it.This can also help reduce the oxygen demand of the heart, but it is not the main goal of therapy for variant angina.
Choice D is wrong because verapamil reduces blood pressure, not increases it.This can help lower the workload of the heart, but it is not the main goal of therapy for variant angina.
Normal ranges for heart rate are 60 to 100 beats per minute, for blood pressure are 120/80 mm Hg or lower, and for contractility are measured by ejection fraction, which is normally 55% or higher.
A patient is receiving heparin therapy during hemodialysis for chronic renal failure and develops heparin-induced thrombocytopenia (HIT). The nurse anticipates that which medication will be ordered for this patient?
Explanation
This is because argatroban is a direct thrombin inhibitor that can be used as an alternative anticoagulant for patients with heparin-induced thrombocytopenia (HIT).HIT is an immune-mediated disorder that occurs when antibodies form against heparin and platelet factor 4, leading to platelet activation and thrombosis.The diagnosis of HIT is based on clinical criteria and laboratory tests.
Choice A is wrong because warfarin is a vitamin K antagonist that interferes with the synthesis of clotting factors II, VII, IX, and X.Warfarin is contraindicated in patients with HIT because it can worsen the thrombotic complications and cause skin necrosis.Warfarin should only be started after the platelet count has recovered and the patient is adequately anticoagulated with a non-heparin agent.
Choice B is wrong because clopidogrel is an antiplatelet agent that inhibits the ADP receptor on platelets, preventing their aggregation.Clopidogrel is not effective for the treatment of HIT, as it does not target the underlying mechanism of thrombin generation.Clopidogrel may also increase the risk of bleeding in patients with HIT.
Choice D is wrong because alteplase is a fibrinolytic agent that converts plasminogen to plasmin, which breaks down fibrin clots.Alteplase is not indicated for the treatment of HIT, as it does not prevent further thrombosis and may cause severe bleeding complications.Alteplase may be used as a last resort for life-threatening thrombosis in patients with HIT who do not respond to other therapies.
A patient who has atrial fibrillation is taking warfarin and has an INR of 2.5.The patient reports having frequent headaches and asks for an over-the-counter pain reliever.The nurse will recommend which medication?
Explanation
The patient reports having frequent headaches and asks for an over-the-counter pain reliever.The nurse will recommend acetaminophen, which is the safest pain reliever while taking warfarin.Acetaminophen does not interfere with the anticoagulant effect of warfarin and does not increase the risk of bleeding.
Choice A is wrong because ibuprofen is a nonsteroidal anti-inflammatory drug (NSAID) that can enhance the anticoagulant effect of warfarin and increase the likelihood of harmful bleeding.
NSAIDs can also cause stomach ulcers, kidney damage, and high blood pressure.
Choice B is wrong because naproxen is another NSAID that has the same risks as ibuprofen.
Naproxen should be avoided by patients taking warfarin.
Choice D is wrong because aspirin is also an anticoagulant that can increase the risk of bleeding when taken with warfarin.
Aspirin can also cause stomach irritation, ulcers, and allergic reactions.
The normal range for INR is 2 to 3 for patients with atrial fibrillation who are taking warfarin.
An INR of 2.5 indicates that the patient’s blood is taking longer to clot than normal, but not too long.
The patient should have regular blood tests to monitor their INR and adjust their warfarin dose if needed.
A nurse is caring for a client who has pulmonary embolism and is receiving alteplase via continuous IV infusion.The nurse should monitor for which adverse effects of this medication? (Select all that apply.)
Explanation
Alteplase is a fibrinolytic agent that dissolves blood clots and restores blood flow.However, it also increases the risk of bleeding from any site, such as the nose, gums, injection sites, or internal organs.Therefore, the nurse should monitor the client for signs of bleeding, such as bruising, hematuria, hematemesis, melena, or decreased hemoglobin and hematocrit levels.
Choice A is wrong because hypotension is not a common adverse effect of alteplase.Hypotension may occur due to blood loss from bleeding or other causes, such as dehydration, sepsis, or cardiac dysfunction.
Choice C is wrong because dysrhythmias are not a common adverse effect of alteplase.Dysrhythmias may occur due to pulmonary embolism itself, which can cause hypoxia, acidosis, and increased pulmonary artery pressure.
Choice D is wrong because nausea is not a common adverse effect of alteplase.Nausea may occur due to other factors, such as anxiety, pain, or medications.
Choice E is wrong because fever is not a common adverse effect of alteplase.Fever may occur due to infection, inflammation, or other causes.
A nurse is caring for a client who has atrial fibrillation and is receiving warfarin therapy to prevent thromboembolism formation. The nurse should monitor which of the following laboratory values to determine the effectiveness of the medication?
Explanation
Warfarin is an anticoagulant that inhibits the synthesis of vitamin K-dependent clotting factors. The INR is a standardized measure of the prothrombin time (PT), which reflects the degree of anticoagulation.The therapeutic range for INR is 2 to 3 for most conditions, and higher for some mechanical heart valves.
Choice A) Activated partial thromboplastin time (aPTT) is wrong because it is used to monitor heparin therapy, not warfarin therapy.
Heparin is another anticoagulant that works by activating antithrombin III, which inhibits thrombin and factor Xa.The therapeutic range for aPTT is 1.5 to 2.5 times the normal value, which is 30 to 40 seconds.
Choice B) Prothrombin time (PT) is wrong because it is not a standardized measure of the warfarin effect.
The PT can vary depending on the reagents and methods used by different laboratories.The INR was developed to eliminate this variability and provide a consistent measure of the warfarin effect.
Choice D) Platelet count is wrong because it is not affected by warfarin therapy.
Warfarin does not affect the number or function of platelets, only the clotting factors.Platelet count can be used to monitor other conditions that affect hemostasis, such as thrombocytopenia or thrombocytosis.
A nurse is caring for a client who has deep vein thrombosis and is receiving enoxaparin therapy subcutaneously once daily at home. The nurse should instruct the client to report which of the following findings immediately?
Explanation
This is because swelling in one leg could indicate a new or worsening deep vein thrombosis (DVT), which is a serious condition that can lead to pulmonary embolism or other complications. The client should report this finding to the provider immediately and seek medical attention.
Choice A) Bruising at injection site is wrong because bruising is a common and expected side effect of enoxaparin therapy, especially if the client is using the same injection site repeatedly.
The client should be instructed to rotate the injection sites and apply gentle pressure after each injection to minimize bruising.
Choice B) Redness at injection site is wrong because redness is also a common and expected side effect of enoxaparin therapy, as it indicates a local inflammatory response to the medication.
The client should be advised to avoid rubbing or scratching the injection site and to apply a cold compress if needed.
Choice D) Mild pain at injection site is wrong because mild pain is also a common and expected side effect of enoxaparin therapy, as it reflects the needle insertion and the medication delivery.
The client should be reassured that the pain will subside shortly and to use a different injection site for the next dose.
Normal ranges for enoxaparin therapy are based on the client’s weight, indication, and renal function.
The usual dose for DVT prophylaxis is 40 mg subcutaneously once daily, and the usual dose for DVT treatment is 1 mg/kg subcutaneously every 12 hours.
The client should have regular blood tests to monitor the anti-factor Xa level, which should be between 0.5 and 1.0 IU/mL for DVT prophylaxis and between 0.6 and 1.0 IU/mL for DVT treatment.
The client should also have regular platelet counts to check for heparin-induced thrombocytopenia (HIT), which is a rare but serious complication of enoxaparin therapy that causes a drop in platelets and an increased risk of thrombosis.
The normal platelet count range is 150,000 to 450,000/mm3.
A client who has atrial fibrillation is prescribed dabigatran etexilate mesylate (Pradaxa). The nurse should instruct the client to report which of the following findings immediately? (Select all that apply.)
Explanation
Dabigatran etexilate mesylate (Pradaxa) is a medication that prevents blood clots and reduces the risk of stroke in patients with atrial fibrillation.
However, it can also cause bleeding as a side effect.
Therefore, the nurse should instruct the client to report any signs of unusual bleeding or bruising, blood in urine or stool, or abdominal pain or swelling immediately.These could indicate a serious complication such as gastrointestinal bleeding, hemorrhage, or internal organ damage.
Choice D, headache or dizziness, is not a correct answer.
Although these symptoms could be caused by dabigatran, they are not as serious or urgent as bleeding.
They could also be due to other factors such as dehydration, low blood pressure, or stress.The nurse should advise the client to monitor these symptoms and seek medical attention if they persist or worsen.
Choice E, shortness of breath, is not a correct answer.
Shortness of breath is not a common side effect of dabigatran.
However, it could be a symptom of atrial fibrillation or its complications such as heart failure or stroke.The nurse should educate the client about the signs and symptoms of these conditions and instruct them to call 911 if they experience chest pain, palpitations, fainting, or weakness.
The nurse recognizes what absolute contraindication to the administration of a thrombolytic to a patient having an acute myocardial infarction?
Explanation
A history of stroke is an absolute contraindication to the administration of a thrombolytic to a patient having an acute myocardial infarction (AMI).This is because thrombolytics can increase the risk of intracranial hemorrhage and worsen the neurological outcome.
Choice A is wrong because history of hypertension is not an absolute contraindication, but a relative one.This means that the benefits of thrombolytic therapy may outweigh the risks in some cases, depending on the severity and duration of hypertension.
Choice C is wrong because history of peptic ulcer disease is also a relative contraindication, not an absolute one.Thrombolytics can increase the risk of gastrointestinal bleeding, but this can be managed with proton pump inhibitors or histamine-2 blockers.
Choice D is wrong because history of diabetes mellitus is not a contraindication at all to thrombolytic therapy.In fact, some studies have shown that diabetic patients with AMI may benefit more from thrombolytic therapy than non-diabetic patients.
Which patients below would be at a HIGH risk for developing adverse effects of Heparin drug therapy? Select all that apply:
Explanation
Heparin is an anticoagulant that inhibits blood clotting and prevents harmful clots from forming in blood vessels.However, heparin can also cause some serious side effects, such as bleeding, bruising, low platelet count, allergic reactions, and osteoporosis.
Therefore, patients who are at a high risk for developing these adverse effects should be monitored closely and have their heparin dose adjusted accordingly.
Choice A is correct because a patient who is post-op day 1 from brain surgery has a high risk of bleeding from the surgical site or intracranially.Heparin can increase this risk and cause life-threatening hemorrhage.
Therefore, this patient should not receive heparin unless absolutely necessary and under strict supervision.
Choice B is wrong because a patient with a pulmonary embolism (PE) is a candidate for heparin therapy.
A PE is a blood clot that blocks the blood flow to the lungs and can cause respiratory failure and death.Heparin can prevent the clot from becoming larger and causing more damage, and also prevent new clots from forming.
Therefore, this patient would benefit from heparin therapy and is not at a high risk of adverse effects.
Choice C is correct because a patient with active peptic ulcer disease (PUD) has a high risk of bleeding from the stomach or duodenum.
PUD is a condition where the lining of the digestive tract is eroded by stomach acid and bacteria.Heparin can worsen this condition and cause ulcer bleeding or perforation.
Therefore, this patient should avoid heparin therapy unless absolutely necessary and under strict supervision.
Choice D is wrong because a patient with uncontrolled atrial fibrillation (AF) is a candidate for heparin therapy.
AF is an irregular heartbeat that can cause blood clots to form in the heart chambers and travel to other organs, such as the brain or lungs.Heparin can prevent these clots from forming and reduce the risk of stroke or PE.
Therefore, this patient would benefit from heparin therapy and is not at a high risk of adverse effects.
Normal ranges of heparin depend on the type of heparin used (unfractionated heparin or low molecular weight heparin), the method of administration (intravenous or subcutaneous), and the indication for use (prophylaxis or treatment).Generally, the therapeutic range for heparin level is 0.3 - 0.7 U/mL, measured by anti-Xa assay.However, this range may vary depending on the pregnancy stage and the type of heparin used.The dose of heparin should be individualized according to the results of suitable laboratory tests and clinical response.
A patient is ordered to start an IV continuous Heparin drip. Prior to starting the medication, the nurse would ensure what information is gathered correctly before initiating the drip? Select all that apply: *.
Explanation
The nurse would need to know the patient’s weight and aPTT level before starting the IV continuous Heparin drip.
Here is why:
• Weight: Heparin dosing is based on the patient’s weight, so the nurse would want to make sure the documented weight of the patient is current and accurate.The initial bolus and infusion rate are calculated using the patient’s weight in kilograms.
• aPTT: Heparin works by enhancing the activation of antithrombin III, which prevents the activation of thrombin and the conversion of fibrinogen to fibrin.Heparin affects the intrinsic pathway of clotting, and its therapeutic effect is monitored by measuring the activated partial thromboplastin time (aPTT).The normal range for aPTT is about 30-40 seconds, and the therapeutic range for Heparin is 1.5-2.5 times the normal value.The nurse would need to check the baseline aPTT before starting the drip, and then collect an aPTT level every 6 hours per protocol to adjust the infusion rate as needed.
The other choices are wrong because:
• Vital signs: Although vital signs are important to monitor for any patient, they are not specific to Heparin therapy.Heparin does not affect blood pressure, heart rate, respiratory rate, or temperature directly.
• PT/INR: These are coagulation tests that measure the extrinsic pathway of clotting, which is affected by Vitamin K antagonists such as Warfarin.Heparin does not affect the PT/INR levels, so they are not relevant for Heparin therapy.
• EKG: An electrocardiogram (EKG) is a test that measures the electrical activity of the heart.It can help diagnose cardiac arrhythmias, ischemia, infarction, electrolyte imbalances, and other cardiac conditions.
Heparin does not affect the electrical conduction of the heart, so an EKG is not necessary before starting Heparin therapy
A nurse is caring for a patient who is receiving heparin therapy via continuous IV infusion for treatment of deep vein thrombosis (DVT). The nurse should monitor which of the following laboratory values to evaluate therapeutic effectiveness of heparin therapy?
Explanation
The correct answer is choice A) Activated partial thromboplastin time (aPTT).This is because aPTT is the most commonly used laboratory test to monitor the therapeutic effect of heparin therapy.
Heparin is an anticoagulant that inhibits the formation of thrombin and fibrin, which are essential for blood clotting.Heparin therapy is indicated for the treatment of deep vein thrombosis (DVT), which is a condition where blood clots form in the deep veins of the legs or pelvis.
Choice B) Prothrombin time (PT) is wrong because PT is used to monitor the therapeutic effect of warfarin therapy, not heparin therapy.
Warfarin is another anticoagulant that inhibits the synthesis of vitamin K-dependent clotting factors.Warfarin therapy is also indicated for the treatment of DVT, but it has a different mechanism of action and monitoring than heparin therapy.
Choice C) International normalized ratio (INR) is wrong because INR is a standardized way of reporting PT results that accounts for the variability of different laboratory methods.INR is also used to monitor the therapeutic effect of warfarin therapy, not heparin therapy.
Choice D) Platelet count is wrong because platelet count is not directly affected by heparin therapy.However, platelet count should be monitored periodically in patients receiving heparin therapy to detect heparin-induced thrombocytopenia (HIT), which is a rare but serious complication of heparin therapy that causes a drop in platelet count and an increased risk of thrombosis.
Choice E) Hemoglobin is wrong because hemoglobin is not directly affected by heparin therapy.However, hemoglobin should be monitored periodically in patients receiving heparin therapy to detect bleeding complications, which are the most common adverse effects of heparin therapy.
The normal range for aPTT is 25 to 35 seconds, but the therapeutic range for heparin therapy is usually 1.5 to 2.5 times the normal range, depending on the indication and protocol.
The normal range for PT is 11 to 13 seconds, and the therapeutic range for warfarin therapy is usually an INR of 2 to 3, depending on the indication and protocol
A nurse is caring for a patient who has been prescribed enoxaparin (Lovenox) subcutaneously for prophylaxis against deep vein thrombosis (DVT). The nurse should instruct the patient to:
Explanation
The correct answer is choice D) Use a soft-bristled toothbrush.
This is because enoxaparin (Lovenox) is an anticoagulant that prevents blood clots by thinning the blood.Therefore, patients who take enoxaparin should avoid activities that can cause bleeding, such as using a hard-bristled toothbrush, flossing, shaving, or cutting their nails.
Choice A) Avoid foods that are high in vitamin K is wrong because vitamin K interacts with warfarin, another anticoagulant, but not with enoxaparin.Vitamin K helps the blood clot, so patients who take warfarin should avoid foods that are high in vitamin K, such as leafy green vegetables, broccoli, or liver.
Choice B) Administer injections into areas with decreased subcutaneous tissue is wrong because enoxaparin should be injected into areas with adequate subcutaneous tissue, such as the abdomen or the thighs.Injecting into areas with decreased subcutaneous tissue can cause bruising, pain, or hematoma formation.
Choice C) Massage injection sites after administration is wrong because massaging the injection sites can cause bleeding, bruising, or irritation.Patients who take enoxaparin should not rub or press on the injection sites after administration.
A client has been prescribed warfarin (Coumadin) for treatment of deep vein thrombosis (DVT). Which of the following instructions should the nurse include in patient teaching? Select all that apply.
Explanation
Warfarin (Coumadin) is a blood thinner that prevents blood clots from forming or growing larger.
It is used to treat or prevent deep vein thrombosis (DVT), a condition in which a blood clot forms in a vein deep in the body, usually in the legs.
It can also prevent pulmonary embolism (PE), a condition in which a blood clot breaks off and travels to the lungs, blocking blood flow and causing breathing problems.
Patients taking warfarin should follow these instructions:
• Avoid foods that are high in vitamin K.
Vitamin K is needed for the production of some clotting factors in the liver.
Warfarin blocks the action of vitamin K, and thus reduces the clotting ability of the blood.
However, if the intake of vitamin K varies significantly from day to day, it can affect the stability of the warfarin effect.Foods that are high in vitamin K include green leafy vegetables, such as spinach, kale, broccoli, cabbage, and lettuce, as well as some vegetable oils, such as soybean and canola.Patients should not avoid these foods completely, but they should keep their intake consistent and inform their doctor or pharmacist if they make any changes to their diet.
• Report any unusual bleeding to healthcare provider.
Warfarin can increase the risk of bleeding, especially if the dose is too high or if it interacts with other medications or supplements.Patients should notify their doctor or seek emergency care if they have any signs of bleeding, such as bruising, red or black stools, blood in the urine, coughing up blood, vomiting blood, nosebleeds, heavy menstrual bleeding, headaches, dizziness, weakness, or swelling.They should also inform their doctor of any other medications or supplements they are taking, including over-the-counter products and herbal remedies.
• Use an electric razor when shaving.
Warfarin can make the skin more prone to bleeding from minor cuts or injuries.
Patients should use an electric razor when shaving to reduce the risk of nicking themselves and causing bleeding.They should also use a soft toothbrush and avoid flossing if it causes bleeding.They should wear gloves when handling sharp objects or working in the garden.
Choice B and E are wrong because:
• Take aspirin for pain relief.
Aspirin is a medication that also prevents blood clots by inhibiting platelets, which are cells that stick together to form clots.Taking aspirin with warfarin can increase the risk of bleeding significantly and is not recommended unless prescribed by a doctor for a specific reason.Patients should avoid taking aspirin or other nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen or naproxen, for pain relief unless advised by their doctor.They should also check the labels of any over-the-counter medications or supplements they use and avoid those that contain aspirin or NSAIDs.
• Wear shoes that fit well and avoid tight clothing.
This instruction is not related to warfarin therapy and does not affect its efficacy or safety.
However, it may be a general advice for patients with DVT to prevent further complications or discomfort.Wearing shoes that fit well and avoiding tight clothing can help improve blood circulation in the legs and prevent swelling or pain.Patients with DVT should also elevate their legs when possible and wear compression stockings if prescribed by their doctor.
A patient has been prescribed rivaroxaban (Xarelto) for deep vein thrombosis (DVT). Which statement by the patient indicates understanding of medication teaching?
Explanation
This statement indicates that the patient understands that rivaroxaban (Xarelto) is an anticoagulant that can increase the risk of bleeding and bruising.The patient should avoid activities that may cause injury, such as contact sports, sharp objects, or falls.
Choice A is wrong because aspirin is also an antiplatelet drug that can further increase the risk of bleeding when taken with rivaroxaban.The patient should not take aspirin or any other nonsteroidal anti-inflammatory drugs (NSAIDs) without consulting the prescriber.
Choice C is wrong because rivaroxaban can be taken with or without food.The patient does not need to take the medication with food to prevent stomach upset or absorption problems.
Choice D is wrong because rivaroxaban should be taken as prescribed and not stopped abruptly without consulting the prescriber.Stopping the medication can increase the risk of blood clots and stroke.The patient should not stop taking the medication even if they feel better or have no symptoms.
A patient has been prescribed dabigatran (Pradaxa) for atrial fibrillation (AF). Which laboratory test should be monitored while on this medication?
Explanation
Activated partial thromboplastin time (aPTT).
Dabigatran (Pradaxa) is a direct oral anticoagulant (DOAC) that inhibits thrombin, a key enzyme in the coagulation cascade.
Dabigatran prolongs the aPTT, which is a measure of the intrinsic and common pathways of coagulation.The aPTT can be used to monitor the anticoagulant effect of dabigatran, although routine monitoring is not required.
Choice A) Prothrombin time (PT) is wrong because PT measures the extrinsic and common pathways of coagulation, which are not affected by dabigatran.
PT is used to monitor warfarin therapy, not dabigatran.
Choice B) International normalized ratio (INR) is wrong because INR is a standardized version of PT that is used to monitor warfarin therapy, not dabigatran.
INR is not affected by dabigatran.
Choice D) Platelet count is wrong because platelet count is a measure of the number of platelets in the blood, which are involved in primary hemostasis.
Platelet count is not affected by dabigatran, which acts on secondary hemostasis.
Normal ranges for these tests are:
• aPTT: 25 to 35 seconds
• PT: 11 to 13.5 seconds
• INR: 0.8 to 1.2
• Platelet count: 150,000 to 450,000 per microliter of blood
A nurse is caring for a patient who has been prescribed apixaban (Eliquis) for deep vein thrombosis (DVT). Which instructions should be included in patient teaching? Select all that apply.
Explanation
Apixaban (Eliquis) is a blood thinner that prevents blood clots from forming or growing larger.
It is used to treat or prevent deep vein thrombosis (DVT), a condition in which a blood clot forms in a vein deep in the body, usually in the legs.
It can also prevent pulmonary embolism (PE), a condition in which a blood clot breaks off and travels to the lungs, blocking blood flow and causing breathing problems.
Patients taking apixaban should follow these instructions:
• Avoid activities that may cause injury.
Apixaban can increase the risk of bleeding, so patients should be careful not to cut or bruise themselves.
They should use a soft toothbrush, an electric razor, and avoid contact sports or other activities that may cause bleeding.They should also wear a medical alert bracelet or carry an identification card that states they are taking apixaban.
• Report signs and symptoms of bleeding immediately.Patients should notify their doctor or seek emergency care if they have any signs of bleeding, such as unusual bruising, red or black stools, blood in the urine, coughing up blood, vomiting blood, nosebleeds, heavy menstrual bleeding, headaches, dizziness, weakness, or swelling.
• Do not take aspirin or other nonsteroidal anti-inflammatory drugs (NSAIDs).
These drugs can also increase the risk of bleeding and interfere with the effects of apixaban.
Patients should avoid taking aspirin, ibuprofen, naproxen, or other NSAIDs unless prescribed by their doctor.They should also check the labels of any over-the-counter medications or supplements they use and avoid those that contain aspirin or NSAIDs.
Choice B and D are wrong because:
• Take medication with food.Apixaban can be taken with or without food.Taking it with food does not affect its absorption or efficacy.
Therefore, this instruction is not necessary for patients taking apixaban.
• Monitor vital signs regularly.Apixaban does not affect blood pressure, heart rate, or oxygen saturation.
Therefore, monitoring vital signs regularly is not required for patients taking apixaban.However, patients should still follow their doctor’s advice on how often to check their blood tests, such as hemoglobin, hematocrit, and platelets.
A nurse is reviewing the medication list of a client who is prescribed dabigatran and has a history of peptic ulcer disease. The nurse should recognize that which of the following medications can increase the risk of bleeding in this client?
Explanation
Omeprazole is a proton pump inhibitor (PPI) that reduces the production of stomach acid.
Dabigatran is an anticoagulant that prevents blood clots from forming.
Both drugs can increase the risk of bleeding in the gastrointestinal tract, especially in clients with peptic ulcer disease.Therefore, they should not be used together unless absolutely necessary.
Choice B. Ranitidine is wrong because ranitidine is a histamine-2 receptor antagonist (H2RA) that also reduces the production of stomach acid, but to a lesser extent than PPIs.Ranitidine does not interact significantly with dabigatran and does not increase the risk of bleeding.
Choice C. Sucralfate is wrong because sucralfate is a mucosal protectant that forms a barrier over ulcers and protects them from acid and enzymes.Sucralfate does not affect the coagulation system and does not increase the risk of bleeding.
Choice D. Misoprostol is wrong because misoprostol is a synthetic prostaglandin that inhibits gastric acid secretion and increases bicarbonate and mucus production.
Misoprostol is used to prevent ulcers in clients who take NSAIDs, which can cause ulcers and bleeding.
Misoprostol does not interact with dabigatran and does not increase the risk of bleeding.
A nurse is caring for a client who is receiving argatroban IV for HIT and requires urgent surgery. The nurse should stop the infusion at least how many hours before the surgery?
Explanation
Argatroban is a direct thrombin inhibitor (DTI) that is used as an alternative anticoagulant for patients with heparin-induced thrombocytopenia (HIT) who require urgent surgery. Argatroban has a half-life of about 40 to 50 minutes and is cleared by the liver.The infusion should be stopped at least 4 hours before the surgery to allow adequate time for the anticoagulant effect to wear off.The activated partial thromboplastin time (aPTT) should be monitored before and after the infusion to assess the degree of anticoagulation.
Choice A is wrong because 2 hours is not enough time to stop the argatroban infusion before surgery.
The patient may still have a high risk of bleeding if the aPTT is prolonged.
Choice C is wrong because 6 hours is longer than necessary to stop the argatroban infusion before surgery.
The patient may have a higher risk of thrombosis if the anticoagulation effect is too low.
Choice D is wrong because 8 hours is much longer than necessary to stop the argatroban infusion before surgery.
The patient may have a very low level of anticoagulation and a high risk of thrombosis if the infusion is stopped for too long.
A nurse is teaching a client who has a new prescription for bivalirudin about potential adverse effects of the drug. Which of the following effects should the nurse include? (Select all that apply.)
Explanation
The nurse should include headache and dyspnea as potential adverse effects of bivalirudin.According to the drug information from various sources, bivalirudin can cause common side effects such as headache, nausea, low or high blood pressure, chest pain, abdominal pain, and shortness of breath (dyspnea).
These side effects should be reported to the provider if they are severe or persistent.
Choice B is wrong because fever is not a common side effect of bivalirudin.
However, fever can be a sign of infection or an allergic reaction to the drug, which should be reported to the provider immediately.
Choice C is wrong because chest pain is not an adverse effect of bivalirudin, but rather a symptom of angina, which is one of the conditions that bivalirudin is used to treat.
Chest pain can also indicate a heart attack or other serious cardiac problems, which require immediate medical attention.
Choice D is wrong because backache is not a common side effect of bivalirudin.
However, backache can be a sign of bleeding in the kidneys or other organs, which can be a serious complication of bivalirudin therapy.
Therefore, any unusual pain or swelling in the back or abdomen should be reported to the provider as soon as possible.
The nurse is caring for a patient who has received alteplase [Activase]. It is most important for the nurse to take which action?
Explanation
This is because alteplase [Activase] is a thrombolytic drug that dissolves blood clots and can cause bleeding complications, especially intracranial hemorrhage.Neurologic assessment is essential to detect any signs of bleeding in the brain, such as altered level of consciousness, headache, or focal deficits.
Choice A is wrong because applying pressure to needleless access sites after giving medications is a standard precaution to prevent bleeding and infection.It is not specific to alteplase [Activase] therapy.
Choice C is wrong because administering heparin when partial thromboplastin time (PTT) is less than 70 seconds is not recommended for patients who have received alteplase [Activase].
Heparin is an anticoagulant that can increase the risk of bleeding and should be used with caution in patients who have received thrombolytic therapy.The PTT should be monitored closely and heparin should be withheld if the PTT is above the therapeutic range.
Choice D is wrong because giving aspirin when platelet count is greater than 150,000/mm3 is not indicated for patients who have received alteplase [Activase].
Aspirin is an antiplatelet drug that can also increase the risk of bleeding and should be avoided in patients who have received thrombolytic therapy.
The platelet count should be monitored closely and aspirin should be withheld if the platelet count is below the normal range (150,000 to 450,000/mm3).
The patient has been receiving heparin therapy for deep vein thrombosis (DVT). The patient’s activated partial thromboplastin time (aPTT) result is 90 seconds (therapeutic range: 60-80 seconds). What will be included in patient care? (Select all that apply.).
Explanation
A patient with a high aPTT result is at risk for bleeding, so assessing for signs and symptoms of bleeding is important.
Holding heparin therapy per protocol is also appropriate, as heparin is the cause of the prolonged aPTT.
The other choices are wrong because:
• Choice B is wrong because continuing heparin therapy at the current rate will increase the risk of bleeding and further prolong the aPTT.
• Choice C is wrong because decreasing heparin therapy per protocol is not enough to reverse the effects of heparin.
Heparin should be stopped until the aPTT returns to the therapeutic range.
• Choice E is wrong because increasing heparin therapy per protocol will worsen the situation and cause more bleeding and coagulation problems.
The normal range for aPTT is 25 to 35 seconds, and the therapeutic range for heparin therapy is 60 to 80 seconds.A result of 90 seconds indicates excessive anticoagulation and increased bleeding risk.
A nurse is caring for a patient who has been prescribed warfarin [Coumadin] in addition to IV heparin therapy after experiencing an acute myocardial infarction (MI). The patient asks why both medications are necessary if they do similar things in preventing clots from forming in his body.
Which response by the nurse best explains why both medications are necessary? (Select all that apply.).
Explanation
Heparin works faster than warfarin, so it is given until warfarin reaches an effective level in your blood.
Heparin has a shorter duration of action than warfarin, so it is easier to reverse if bleeding occurs.
Choice B is wrong because heparin and warfarin do not have a synergistic effect.
They work on different clotting factors, but they do not enhance each other’s effects.
Choice C is wrong because the route of administration is not relevant to the rationale for using both medications.
Heparin and warfarin can be given by different routes, but that does not explain why they are both necessary.
Choice D is wrong because warfarin does not help dissolve existing clots.
Warfarin prevents the synthesis of vitamin K-dependent clotting factors, but it does not break down clots that have already formed.
Exams on Anticoagulants and Thrombolytic Agents
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
- Define anticoagulants, antiplatelets, and thrombolytics and their indications
- Compare and contrast the mechanisms of action, pharmacokinetics, and adverse effects of different anticoagulants
- Identify the antidotes, monitoring parameters, and nursing implications for anticoagulant therapy
- Compare and contrast the mechanisms of action, pharmacokinetics, and adverse effects of different thrombolytic agents
- Identify the contraindications, precautions, and nursing implications for thrombolytic therapy
- Apply critical thinking and clinical reasoning skills to answer MCQs related to anticoagulants and thrombolytic agents
Introduction

-Anticoagulants, antiplatelets, and thrombolytics are drugs that affect the process of blood clotting or coagulation
-Coagulation is a complex cascade of reactions that involves platelets, clotting factors, fibrinogen, and fibrin
-Coagulation is essential for preventing excessive bleeding from injuries, but it can also cause pathological conditions such as thrombosis and embolism
-Thrombosis is the formation of a blood clot (thrombus) within a blood vessel, which can obstruct blood flow and cause tissue ischemia or necrosis
-Embolism is the detachment of a thrombus or other material (e.g., air, fat, bacteria) that travels through the bloodstream and lodges in a smaller vessel, causing occlusion and infarction
-Anticoagulants are drugs that prevent or delay the formation of new clots or the growth of existing clots by interfering with one or more steps of the coagulation cascade
-Antiplatelets are drugs that inhibit platelet aggregation or adhesion by blocking the action of platelet activators (e.g., collagen, thrombin, ADP) or receptors (e.g., glycoprotein IIb/IIIa)
-Thrombolytics are drugs that dissolve existing clots by activating plasminogen, which converts to plasmin, an enzyme that degrades fibrin
Classification of Anticoagulant medications
-Anticoagulants are indicated for the prevention and treatment of various thromboembolic disorders, such as deep vein thrombosis (DVT), pulmonary embolism (PE), atrial fibrillation (AF), stroke, myocardial infarction (MI), and mechanical heart valves
-Anticoagulants can be classified into four main groups:
- heparins,
- vitamin K antagonists,
- direct oral anticoagulants (DOACs), and
- direct thrombin inhibitors (DTIs)
Heparins
- Heparins are polysaccharides derived from animal sources that bind to antithrombin III (ATIII), a natural inhibitor of thrombin and factor Xa
- Heparins can be unfractionated heparin (UFH) or low molecular weight heparin (LMWH)
- UFH has a variable molecular weight and a short half-life of 1 to 2 hours. It is administered intravenously (IV) or subcutaneously (SC) and requires frequent monitoring of activated partial thromboplastin time (aPTT)
- LMWH has a lower molecular weight and a longer half-life of 4 to 6 hours. It is administered SC and does not require routine monitoring of aPTT. It has a more predictable anticoagulant effect and fewer adverse effects than UFH
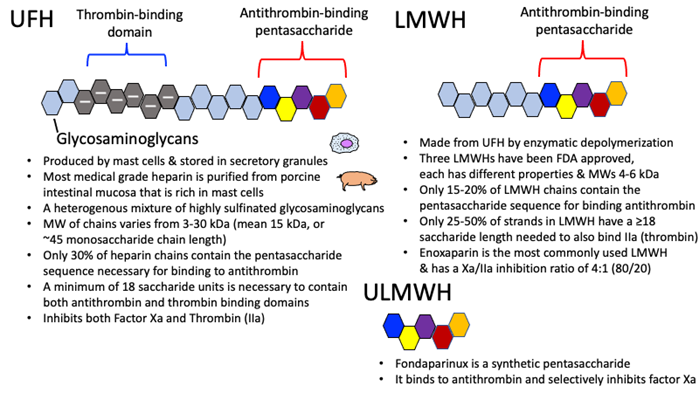
- The main adverse effect of heparins is bleeding. Other adverse effects include hypersensitivity reactions, osteoporosis, alopecia, and heparin-induced thrombocytopenia (HIT)
- HIT is a serious complication characterized by a paradoxical drop in platelet count due to antibody-mediated platelet activation and aggregation. It can lead to arterial or venous thrombosis and requires immediate discontinuation of heparin
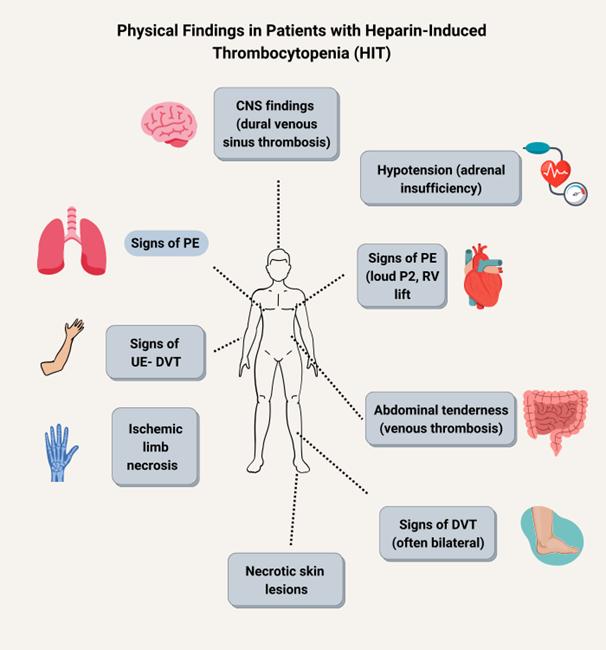
- The antidote for heparin overdose is protamine sulfate, which neutralizes heparin by forming a complex with it. Protamine should be given slowly IV within 30 minutes of heparin administration

- The dosage of heparin is based on body weight and adjusted according to the target therapeutic range of aPTT. The normal aPTT is 40 seconds, and the therapeutic range is 1.5 to 2 times normal, or between 60 to 80 seconds
- The nursing implications for heparin therapy include:
- Assessing the patient’s history of bleeding disorders, allergies, renal function, pregnancy status, and other medications that may interact with heparin
- Monitoring the patient’s vital signs, hemoglobin, hematocrit, platelet count, and aPTT regularly
- Administering heparin by the prescribed route and using a calibrated infusion pump for IV heparin
- Rotating the injection sites for SC heparin and avoiding the abdomen near the umbilicus, scars, bruises, or masses
- Applying gentle pressure to the injection site after SC heparin and avoiding rubbing or massaging the area
- Educating the patient about the signs and symptoms of bleeding, thrombosis, and HIT and instructing them to report them immediately
- Advising the patient to avoid activities that may increase the risk of bleeding or injury, such as contact sports, shaving with a razor, or using a hard toothbrush
- Instructing the patient to avoid alcohol, aspirin, NSAIDs, and herbal supplements that may increase bleeding tendency
Vitamin K antagonists
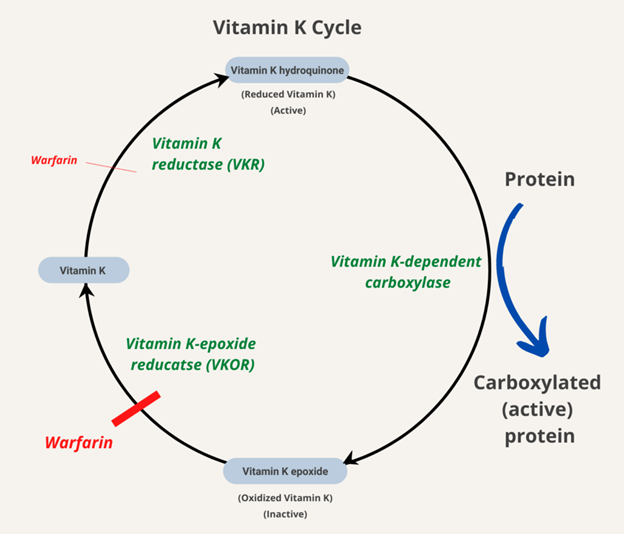
Vitamin K antagonists are drugs that inhibit the synthesis of vitamin K-dependent clotting factors (II, VII, IX, X) in the liver
- The most commonly used vitamin K antagonist is warfarin (Coumadin)
- Warfarin is indicated for the prevention and treatment of thromboembolic disorders such as DVT, PE, AF, stroke, MI, and mechanical heart valves
- Warfarin has a delayed onset of action of 2 to 5 days and a long half-life of 20 to 60 hours. It is administered orally and requires frequent monitoring of prothrombin time (PT) and international normalized ratio (INR)
- The main adverse effect of warfarin is bleeding. Other adverse effects include skin necrosis, purple toe syndrome, alopecia, and fetal harm
- The antidote for warfarin overdose is vitamin K (phytonadione), which reverses the effect of warfarin by restoring the synthesis of clotting factors. Vitamin K can be given orally or IV depending on the severity of bleeding. IV vitamin K should be given slowly over 30 minutes to avoid anaphylaxis
- The dosage of warfarin is based on body weight and adjusted according to the target therapeutic range of INR. The normal INR is 1.0, and the therapeutic range depends on the indication. For most indications, the therapeutic range is 2.0 to 3.0. For mechanical heart valves or recurrent systemic embolism, the therapeutic range is 2.5 to 3.5
- The nursing implications for warfarin therapy include:
- Assessing the patient’s history of bleeding disorders, allergies, liver function, pregnancy status, and other medications that may interact with warfarin
- Monitoring the patient’s vital signs, hemoglobin, hematocrit, platelet count, PT, and INR regularly
- Administering warfarin at the same time every day and following the prescribed dosage regimen
- Educating the patient about the signs and symptoms of bleeding and instructing them to report them immediately
- Advising the patient to avoid activities that may increase the risk of bleeding or injury, such as contact sports, shaving with a razor, or using a hard toothbrush
- Instructing the patient to avoid alcohol, aspirin, NSAIDs, and herbal supplements that may increase bleeding tendency or interfere with warfarin metabolism
- Teaching the patient to maintain a consistent intake of vitamin K-rich foods such as green leafy vegetables,broccoli, cabbage, and brussels sprouts, as they may affect the response to warfarin
- Informing the patient to wear a medical alert bracelet or carry a card that indicates they are taking warfarin
Direct oral anticoagulants (DOACs)

- Direct oral anticoagulants (DOACs) are drugs that directly inhibit factor Xa or thrombin in the coagulation cascade
- DOACs include factor Xa inhibitors (e.g., rivaroxaban, apixaban, edoxaban) and direct thrombin inhibitors (e.g., dabigatran)
- DOACs are indicated for the prevention and treatment of thromboembolic disorders such as DVT, PE, AF, stroke, and MI
- DOACs have a rapid onset of action of 2 to 4 hours and a short half-life of 8 to 15 hours. They are administered orally and do not require routine monitoring of PT or INR
- The main adverse effect of DOACs is bleeding. Other adverse effects include gastrointestinal disturbances, rash, and hypersensitivity reactions
- The antidotes for DOAC overdose are specific reversal agents that bind to the drug and prevent its activity. For factor Xa inhibitors, the antidote is andexanet alfa (Andexxa). For dabigatran, the antidote is idarucizumab (Praxbind)
- The dosage of DOACs is based on body weight and renal function and adjusted according to the indication and patient characteristics. The dosing frequency may vary from once daily to twice daily depending on the drug
- The nursing implications for DOAC therapy include:
- Assessing the patient’s history of bleeding disorders, allergies, renal function, pregnancy status, and other medications that may interact with DOACs
- Monitoring the patient’s vital signs, hemoglobin, hematocrit, platelet count, and renal function regularly
- Administering DOACs at the same time every day and following the prescribed dosage regimen
- Educating the patient about the signs and symptoms of bleeding and instructing them to report them immediately
- Advising the patient to avoid activities that may increase the risk of bleeding or injury, such as contact sports, shaving with a razor, or using a hard toothbrush
- Instructing the patient to avoid alcohol, aspirin, NSAIDs, and herbal supplements that may increase bleeding tendency or interfere with DOAC metabolism
- Teaching the patient to swallow the tablets whole without crushing or chewing them
- Informing the patient to wear a medical alert bracelet or carry a card that indicates they are taking DOACs
Direct thrombin inhibitors (DTIs)
- Direct thrombin inhibitors (DTIs) are drugs that directly bind to and inhibit thrombin, the final enzyme in the coagulation cascade that converts fibrinogen to fibrin
- DTIs include parenteral agents (e.g., bivalirudin, argatroban, lepirudin) and oral agents (e.g., dabigatran)
- DTIs are indicated for the prevention and treatment of thromboembolic disorders such as DVT, PE, AF, stroke, MI, and HIT
- DTIs have a rapid onset of action of 15 to 30 minutes and a short half-life of 2 to 4 hours. They are administered IV or orally and require monitoring of aPTT or ecarin clotting time (ECT)
- The main adverse effect of DTIs is bleeding. Other adverse effects include headache, nausea, diarrhea, and hypersensitivity reactions
- The antidote for DTI overdose is idarucizumab (Praxbind) for dabigatran. There is no specific antidote for other DTIs
- The dosage of DTIs is based on body weight and renal function and adjusted according to the indication and patient characteristics. The dosing frequency may vary from once daily to several times daily depending on the drug
- The nursing implications for DTI therapy include:
- Assessing the patient’s history of bleeding disorders, allergies, renal function, pregnancy status, and other medications that may interact with DTIs
- Monitoring the patient’s vital signs, hemoglobin, hematocrit, platelet count, aPTT, or ECT regularly
- Administering DTIs by the prescribed route and using a calibrated infusion pump for IV DTIs
- Educating the patient about the signs and symptoms of bleeding and instructing them to report them immediately
- Advising the patient to avoid activities that may increase the risk of bleeding or injury, such as contact sports, shaving with a razor, or using a hard toothbrush
- Instructing the patient to avoid alcohol, aspirin, NSAIDs, and herbal supplements that may increase bleeding tendency or interfere with DTI metabolism
- Teaching the patient to swallow the tablets whole without crushing or chewing them
- Informing the patient to wear a medical alert bracelet or carry a card that indicates they are taking DTIs
Thrombolytic agents
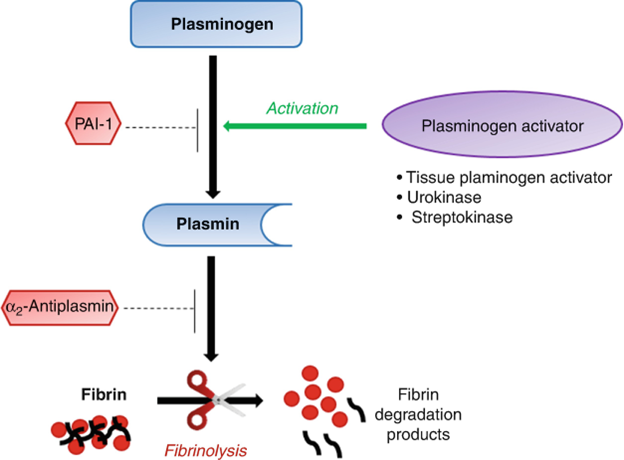
- Thrombolytic agents are drugs that dissolve existing clots by activating plasminogen, which converts to plasmin, an enzyme that degrades fibrin
- Thrombolytic agents are indicated for the management of acute thromboembolic disorders such as PE, ischemic stroke, MI, and peripheral arterial occlusion
- Thrombolytic agents can be classified into three generations: first-generation (e.g., streptokinase), second-generation (e.g., alteplase), and third-generation (e.g., tenecteplase)
- First-generation thrombolytics are non-specific activators of plasminogen that can cause systemic fibrinolysis and bleeding. They are derived from bacteria and can cause allergic reactions. They are rarely used in clinical practice
- Second-generation thrombolytics are more specific activators of plasminogen that bind to fibrin in clots. They have a short half-life of 5 to 10 minutes and require continuous infusion. They are more effective and safer than first-generation thrombolytics
- Third-generation thrombolytics are more specific activators of plasminogen that bind to fibrin in clots. They have a longer half-life of 20 to 30 minutes and can be given as a single bolus injection. They are more effective and safer than second-generation thrombolytics
- The main adverse effects of thrombolytic agents are bleeding and allergic reactions. Bleeding can occur at any site, but the most serious are intracranial hemorrhage, gastrointestinal hemorrhage, and retroperitoneal hemorrhage. Allergic reactions can include fever, chills, rash, hypotension, and anaphylaxis
- The contraindications for thrombolytic therapy are conditions that increase the risk of bleeding or have a poor prognosis, such as:
- Active bleeding or history of bleeding disorders
- Recent surgery, trauma, or invasive procedures
- Severe hypertension or history of cerebrovascular disease
- Malignancy or terminal illness
- Pregnancy or recent childbirth
- Aortic dissection or pericarditis
- Peptic ulcer disease or varices
- The precautions for thrombolytic therapy are conditions that may increase the risk of bleeding or complications, such as:
- Age over 75 years or weight less than 60 kg
- Renal or hepatic impairment
- Diabetes mellitus or hyperlipidemia
- Recent use of anticoagulants, antiplatelets, or NSAIDs
- Infective endocarditis or septic thrombophlebitis
- The nursing implications for thrombolytic therapy include:
- Assessing the patient’s history of bleeding disorders, allergies, renal function, pregnancy status, and other medications that may interact with thrombolytic agents
- Monitoring the patient’s vital signs, hemoglobin, hematocrit, platelet count, fibrinogen level, PT, INR, aPTT, and ECT regularly
- Administering thrombolytic agents by the prescribed route and following the protocol for dosage and infusion rate. The dosage and infusion rate may vary depending on the drug and the indication. For example, alteplase for ischemic stroke is given as a bolus of 0.9 mg/kg (maximum 90 mg) followed by an infusion of the remaining dose over 60 minutes. For MI, alteplase is given as a bolus of 15 mg followed by an infusion of 0.75 mg/kg (maximum 50 mg) over 30 minutes and then another infusion of 0.5 mg/kg (maximum 35 mg) over 60 minutes
- Educating the patient about the signs and symptoms of bleeding and allergic reactions and instructing them to report them immediately
- Advising the patient to avoid activities that may increase the risk of bleeding or injury, such as contact sports, shaving with a razor, or using a hard toothbrush
- Instructing the patient to avoid alcohol, aspirin, NSAIDs, and herbal supplements that may increase bleeding tendency or interfere with thrombolytic metabolism
- Teaching the patient to swallow the tablets whole without crushing or chewing them
- Informing the patient to wear a medical alert bracelet or carry a card that indicates they are taking thrombolytic agents
Conclusion
- Anticoagulants and thrombolytic agents are drugs that affect the process of blood clotting or coagulation by preventing or dissolving clots
- Anticoagulants and thrombolytic agents are indicated for various thromboembolic disorders such as DVT, PE, AF, stroke, MI, and mechanical heart valves
- Anticoagulants and thrombolytic agents have different mechanisms of action, pharmacokinetics, adverse effects, and monitoring parameters. They also have specific antidotes, contraindications, precautions, and nursing implications
- Anticoagulants and thrombolytic agents require careful assessment, administration, and education of the patient to ensure safety and efficacy
- Anticoagulants and thrombolytic agents are commonly tested in ATI/HESI nursing proctored MCQ exams. The exam questions may require the application of critical thinking and clinical reasoning skills to select the best answer
Summary
- Anticoagulants prevent or delay clot formation by interfering with the coagulation cascade
- Anticoagulants include heparins, vitamin K antagonists, DOACs, and DTIs
- Anticoagulants are used for the prevention and treatment of thromboembolic disorders
- Anticoagulants can cause bleeding and other adverse effects
- Anticoagulants have antidotes such as protamine, vitamin K, andexanet, and idarucizumab
- Anticoagulants require monitoring of aPTT, PT, INR, or ECT depending on the drug
- Anticoagulants have nursing implications such as assessment, administration, and education of the patient
- Thrombolytics dissolve clots by activating plasminogen to plasmin
- Thrombolytics include first-generation, second-generation, and third-generation agents
- Thrombolytics are used for the management of acute thromboembolic disorders
- Thrombolytics can cause bleeding and allergic reactions
- Thrombolytics have antidotes such as idarucizumab for dabigatran
- Thrombolytics require monitoring of fibrinogen level, PT, INR, aPTT, or ECT depending on the drug
- Thrombolytics have nursing implications such as assessment, administration, and education of the patient
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Anticoagulants and Thrombolytic Agents
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now