Please set your exam date
Gestational Hypertension
Study Questions
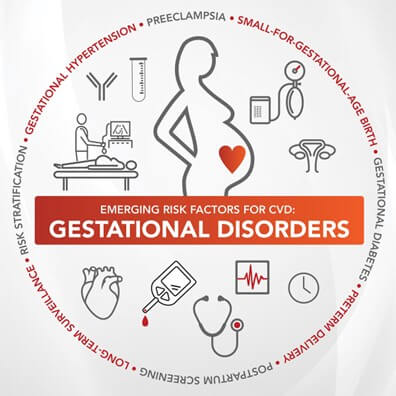
Introduction
A nurse is caring for a client who is diagnosed with gestational hypertension at 28 weeks of gestation.
Which of the following findings should alert the nurse to the possibility of preeclampsia? (Select all that apply.).
Explanation
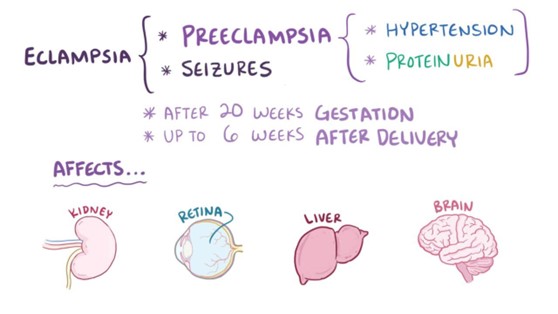
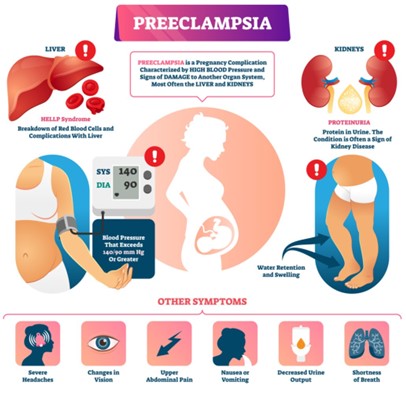
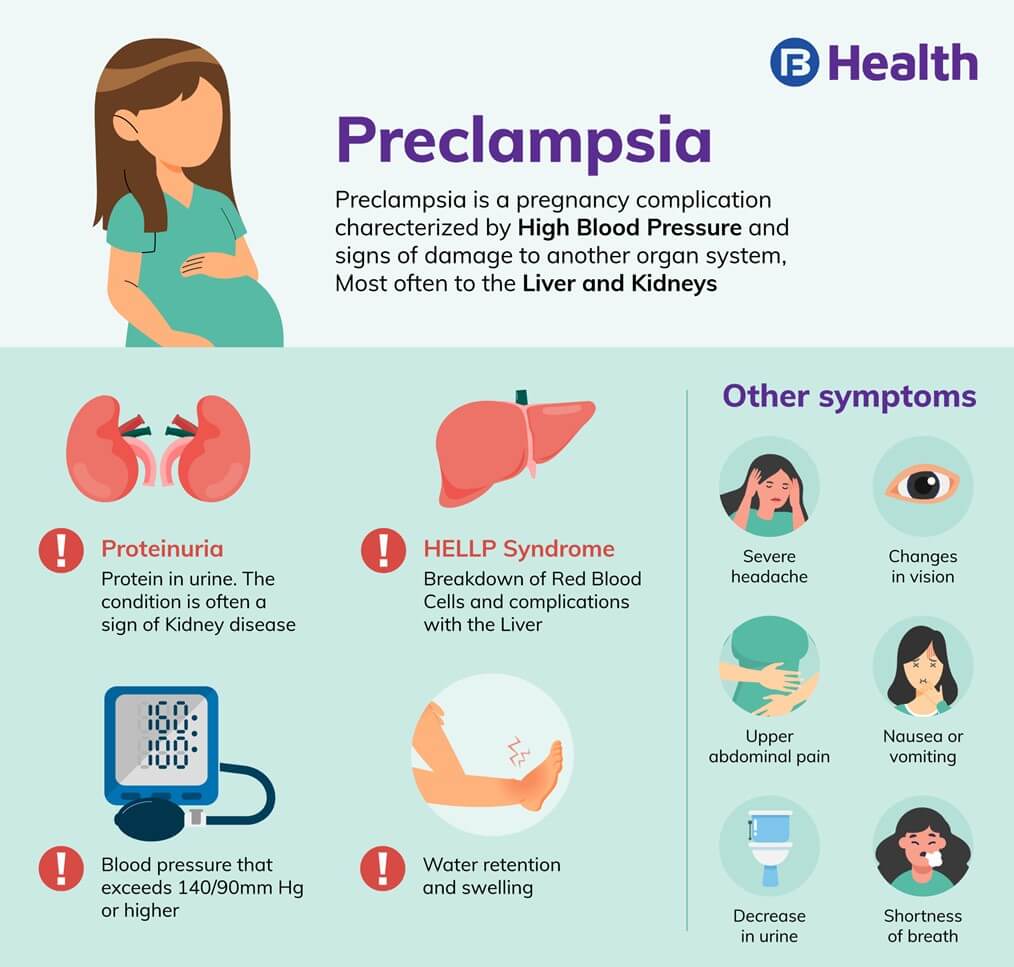
The correct answer is choice A, B, C and E.These are all possible symptoms of preeclampsia, a condition that can occur in the second half of pregnancy and cause high blood pressure, proteinuria and organ damage.
Preeclampsia can be dangerous for both the mother and the baby if not treated promptly.
Choice D is wrong because polyuria (increased urination) is not a symptom of preeclampsia.In fact, some women with preeclampsia may have reduced urine output due to kidney damage.
Normal ranges for blood pressure during pregnancy are below 140/90 mmHg.Normal ranges for protein in urine are below 300 mg per 24 hours.Normal ranges for reflexes are 1+ to 2+ on a scale of 0 to 4.
These are all possible symptoms of preeclampsia, a condition that can occur in the second half of pregnancy and cause high blood pressure, proteinuria and organ damage.
Preeclampsia can be dangerous for both the mother and the baby if not treated promptly.
Explanation
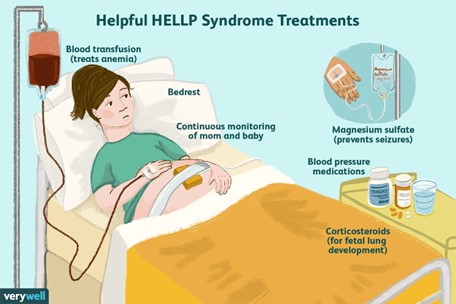
The correct answer is choice B. Platelets 80,000/mm3.This is because HELLP syndrome is a severe form of preeclampsia characterized byHemolysis,Elevated Liver enzymes, andLow Platelets.Platelets are blood cells that help with clotting, and a normal range is 150,000 to 450,000/mm3.A low platelet count (<100,000/mm3) indicates a risk of bleeding and organ damage.
Choice A is wrong because hemoglobin 12 g/dL is within the normal range for pregnant women (11 to 16 g/dL).Hemoglobin is a protein in red blood cells that carries oxygen, and hemolysis is the breakdown of red blood cells.
Choice C is wrong because AST 15 U/L is within the normal range for women (10 to 35 U/L).AST is a liver enzyme that indicates liver function, and elevated liver enzymes (>70 U/L) indicate liver damage.
Choice D is wrong because LDH 90 U/L is within the normal range for women (85 to 225 U/L).LDH is another liver enzyme that indicates liver function, and elevated LDH (>600 U/L) indicates liver damage.
A nurse is teaching a client who has gestational hypertension about the importance of bed rest.
Which of the following statements by the client indicates an understanding of the teaching?
Explanation
The correct answer is choice C.“Bed rest will help decrease the workload on my heart and improve oxygen delivery to my baby.” This is because gestational hypertension is a condition where the blood pressure is elevated after 20 weeks of pregnancy, which can affect the blood flow to the placenta and reduce the oxygen and nutrients that reach the fetus.Bed rest can help lower the blood pressure and increase the blood flow to the placenta.
Choice A is wrong because bed rest alone may not be enough to lower the blood pressure and reduce the risk of complications.Some women may need medications or hospitalization to control their blood pressure and prevent preeclampsia, a serious complication of gestational hypertension.
Choice B is wrong because bed rest does not directly affect the kidney function or prevent proteinuria, which is the presence of protein in the urine.Proteinuria is a sign of preeclampsia, not gestational hypertension.
Bed rest may help prevent the progression of gestational hypertension to preeclampsia, but it does not treat proteinuria.
Choice D is wrong because bed rest does not prevent fluid retention or reduce the swelling in the legs.
Fluid retention and swelling are common symptoms of pregnancy, not specific to gestational hypertension.They are caused by hormonal changes and increased blood volume, not by high blood pressure.
Bed rest may worsen the swelling by reducing the circulation in the legs.
A nurse is preparing to administer magnesium sulfate IV to a client who has severe preeclampsia.
Which of the following actions should the nurse take? (Select all that apply.)
Explanation
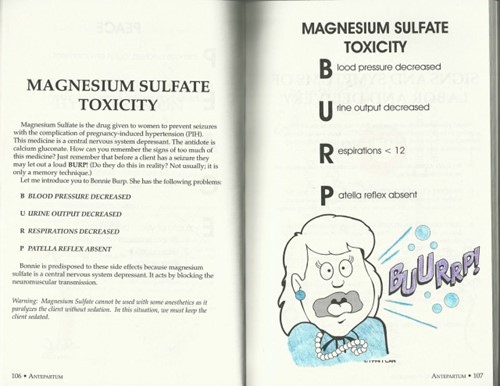
Choice A is correct because magnesium sulfate is excreted in the urine and a decreased urine output places the client at risk for magnesium toxicity.The nurse should monitor the client’s urine output hourly and report any decrease to the provider.
Choice B is wrong because hyperactive (3+ or 4+) deep tendon reflexes are a common physical finding of preeclampsia or eclampsia and do not require an action.The nurse should check the client’s deep tendon reflexes more frequently than every 4 hours to detect any signs of magnesium toxicity, such as absent or hypoactive reflexes.
Choice C is correct because calcium gluconate is the antidote for magnesium toxicity and should be readily available in case of respiratory depression, cardiac arrest, or other signs of overdose.The nurse should administer 10 mL of 10% calcium gluconate IV push over 3 to 5 minutes if needed.
Choice D is correct because magnesium sulfate should be administered via a piggyback infusion using an infusion pump to ensure accurate and safe delivery.The nurse should not administer magnesium sulfate as a bolus or through a primary IV line.
Choice E is wrong because the infusion rate of magnesium sulfate should not be titrated according to the client’s blood pressure, but according to the client’s serum magnesium level, which should range from 4 to 7 mEq/L.The nurse should notify the provider of any low or high serum magnesium level and adjust the infusion rate accordingly.The nurse should also administer antihypertensive medications other than magnesium for sustained hypertension.
Normal ranges:
• Urine output: at least 30 mL/hour
• Deep tendon reflexes: 1+ or 2+
• Respiratory rate: 12 to 20 breaths/minute
• Serum magnesium level: 4 to 7 mEq/L
• Blood pressure: less than 140/90 mm Hg

A nurse is assessing a client who has eclampsia and is receiving magnesium sulfate IV.
Which of the following findings should indicate to the nurse that the client is experiencing magnesium toxicity?
Explanation
The correct answer is choice A. Respiratory rate of 10/min.This indicates that the client is experiencingmagnesium toxicity, which can causemuscle weakness,lethargy, andrespiratory depression.
Magnesium sulfate is a medication used to prevent seizures in clients with eclampsia, but it can also have adverse effects if the dose is too high or the kidney function is impaired.
Choice B. Urine output of 40 mL/hr is wrong because this is within the normal range for urine output.
The minimum urine output should be at least 30 mL/hr.
Choice C. Serum magnesium level of 6 mg/dL is wrong because this is within the normal range for serum magnesium.The normal range is 1.7–2.3 mg/dL.
Choice D. Patellar reflex 2+ is wrong because this is a normal finding for deep tendon reflexes.
A decreased or absent patellar reflex could indicate magnesium toxicity, as magnesium sulfate
Causes and risk factors
A nurse is caring for a client with gestational hypertension.
What is the blood pressure reading that indicates gestational hypertension?
Explanation
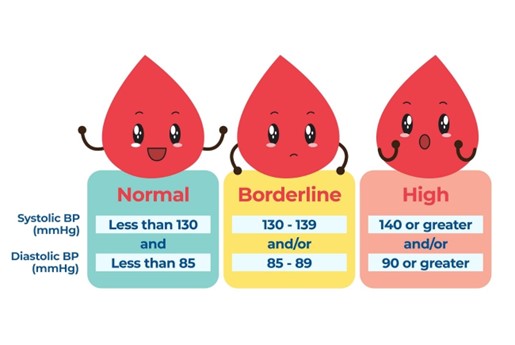
The correct answer is choice C.Gestational hypertension is defined as a blood pressure (BP) of≥140/90 mmHgon two occasions (at least 4 hours apart) after 20 weeks’ gestation in a previously normotensive woman, without the presence of proteinuria or other clinical features suggestive of preeclampsia.
Choice A is wrong because 120/80 mmHg is a normal blood pressure reading for a pregnant woman.
Choice B is wrong because 130/90 mmHg is not high enough to meet the criteria for gestational hypertension.
Choice D is wrong because 150/100 mmHg is a severe hypertension reading that would require immediate medical attention and may indicate preeclampsia or eclampsia.
Tasha Wright: Excellent questions
Tasha Wright: Excellent questions .
A nurse is caring for a client with gestational hypertension.
What is the most common cause of gestational hypertension?
Explanation
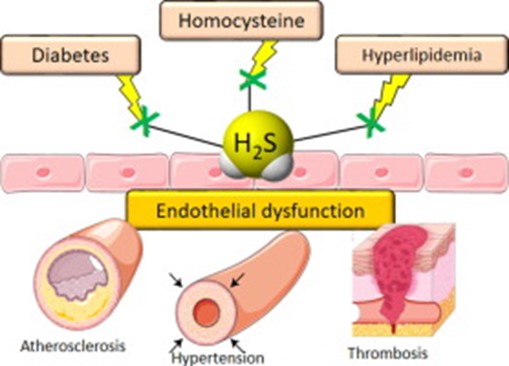
The correct answer is choice D. Vascular dysfunction.Gestational hypertension is high blood pressure that begins after 20 weeks of pregnancy and goes away after childbirth.It happens in about 6% to 8% of pregnancies.The exact cause of gestational hypertension is unknown, but it may be related to problems with the blood vessels that supply the placenta.
Vascular dysfunction means that the blood vessels are not working properly, which can affect blood flow and blood pressure.
Choice A is wrong because genetic factors are not a common cause of gestational hypertension.However, having a family history of gestational hypertension may increase the risk of developing it.
Choice B is wrong because immune system dysfunction is not a common cause of gestational hypertension.However, having an immune system disorder, such as lupus, may increase the risk of developing it.
Choice C is wrong because placental abnormalities are not a common cause of gestational hypertension.However, they may be a consequence of it, as high blood pressure can affect how the placenta develops and functions.
A nurse is caring for a client with gestational hypertension.
What are some risk factors for developing gestational hypertension?
Explanation
The correct answer is choice E.Multiple pregnancy (twins or more) is a risk factor for developing gestational hypertension.Gestational hypertension is high blood pressure that begins after 20 weeks of pregnancy and goes away after childbirth.
Choice A is wrong because first pregnancy or new partner is not a risk factor for gestational hypertension, but for preeclampsia, which is a more severe condition that involves high blood pressure and protein in the urine.
Choice B is wrong because age younger than 20 or older than 40 is a risk factor for chronic hypertension, which is high blood pressure that exists before pregnancy or early in pregnancy (before 20 weeks).
Choice C is wrong because obesity or excessive weight gain is a risk factor for chronic hypertension and preeclampsia, but not for gestational hypertension.
Choice D is wrong because family history of hypertension or preeclampsia is a risk factor for chronic hypertension and preeclampsia, but not for gestational hypertension.
A nurse is caring for a client with gestational hypertension.
What are some preexisting medical conditions that can increase the risk of developing gestational hypertension?
Explanation
The correct answer is choice D. All of the above.Gestational hypertension is high blood pressure that begins after 20 weeks of pregnancy and goes away after childbirth.It can cause complications for both the mother and the baby.
Some preexisting medical conditions that can increase the risk of developing gestational hypertension are:
• Diabetes: This condition affects how the body uses glucose (sugar) and can cause high blood pressure and damage to the blood vessels.
• Kidney disease: This condition affects how the kidneys filter waste and fluid from the blood and can cause high blood pressure and protein in the urine.
• Autoimmune disorders: These conditions occur when the immune system attacks healthy cells and tissues and can cause inflammation and damage to various organs, including the kidneys, heart and blood vessels.
Choice A is wrong because diabetes is not the only risk factor for gestational hypertension.
Choice B is wrong because kidney disease is not the only risk factor for gestational hypertension.
Choice C is wrong because autoimmune disorders are not the only risk factor for gestational hypertension.
Other risk factors for gestational hypertension may include age (less than 18 or more than 35 years old), marital status (unmarried), living in a city/town, education level (post-secondary), employment status (unemployed), obesity, first labor in consecutively pregnant women, the threat of pregnancy termination, cardiovascular system diseases, urinary tract pathology, varicose veins and ABO-sensibilization.
A nurse is caring for a client with gestational hypertension who has a history of preeclampsia in previous pregnancies.
What is the most important nursing intervention?
Explanation
The correct answer is choice A. Monitor blood pressure and urine output closely.This is the most important nursing intervention for a client with gestational hypertension because it helps to detect any signs of worsening condition or complications such as preeclampsia, eclampsia, or HELLP syndrome.Monitoring blood pressure and urine output can also help to evaluate the effectiveness of antihypertensive medications and fluid management.
Choice B is wrong because administering antihypertensive medications as ordered is not the most important nursing intervention for a client with gestational hypertension.Antihypertensive medications are only indicated for clients with severe hypertension (systolic blood pressure ≥ 160 mm Hg or diastolic blood pressure ≥ 110 mm Hg) or those with evidence of end-organ damage.Antihypertensive medications should be used with caution and under close monitoring because they can cause adverse effects such as hypotension, fetal growth restriction, or oligohydramnios.
Choice C is wrong because encouraging bed rest and limiting activity is not the most important nursing intervention for a client with gestational hypertension.Bed rest and activity restriction have not been proven to prevent or improve gestational hypertension or its complications.In fact, bed rest can increase the risk of thromboembolism, muscle wasting, bone loss, and psychological distress in pregnant women.
Bed rest and activity restriction should only be advised for clients with severe hypertension or those with signs of fetal compromise
Signs and symptoms
A nurse is assessing a pregnant woman with gestational hypertension.
Which of the following symptoms would lead the nurse to suspect that the client has developed severe preeclampsia?
Explanation
Hyperreflexia is a sign of severe preeclampsia, which is a complication of gestational hypertension that can affect the mother and the fetus.Hyperreflexia means having exaggerated reflexes that can cause muscle spasms or jerks.It can indicate increased nervous system activity due to high blood pressure.
A. Urine protein 300 mg/24 hours.This statement is wrong because urine protein 300 mg/24 hours is within the normal range for pregnant women.Proteinuria, which is a sign of preeclampsia, is defined as urine protein more than 300 mg/24 hours.
B. Blood pressure 150/96 mm Hg.
This statement is wrong because blood pressure 150/96 mm Hg is not high enough to indicate severe preeclampsia.Severe preeclampsia is diagnosed when blood pressure is 160/110 mm Hg or higher on two occasions at least four hours apart.
C. Mild facial edema.This statement is wrong because mild facial edema is a common symptom of pregnancy and not specific to preeclampsia.Severe preeclampsia may cause sudden and severe swelling in the face, hands, or feet.
A client with gestational hypertension reports severe headache.
What should the nurse do first?
Explanation
The correct answer is choice B. Assess blood pressure.This is because a severe headache can be a sign of elevated blood pressure, which can lead to preeclampsia and other complications in pregnancy.
Assessing blood pressure is the first step to determine the severity of the condition and the need for further interventions.
Choice A is wrong because administering acetaminophen may not address the underlying cause of the headache and may mask other symptoms.
Choice C is wrong because assessing for visual disturbances is not the first priority, although it can be a serious symptom of preeclampsia.
Blood pressure should be assessed first to determine the risk of eclampsia and other adverse outcomes.
Choice D is wrong because assessing for proteinuria is not the first priority, although it can be a diagnostic criterion for preeclampsia.
Blood pressure should be assessed first to determine the severity of the condition and the need for further interventions.
A nurse is caring for a client with gestational hypertension who reports chest pain and shortness of breath.
What should the nurse do first?
Explanation
The correct answer is choice A. Administer oxygen.
The client is experiencing signs of pulmonary edema, which is a complication of gestational hypertension.
Oxygen therapy can help improve oxygenation and reduce the workload of the heart.
The nurse should also monitor the client’s vital signs, urine output, and magnesium sulfate level.
Choice B. Assess blood pressure.
This is an important action, but not the first priority.
The nurse should assess blood pressure after administering oxygen and stabilizing the client.
Choice C. Assess for visual disturbances.
This is a symptom of severe preeclampsia, but not an immediate threat to the client’s life.
The nurse should assess for visual disturbances as part of the ongoing evaluation of the client’s condition.
Choice D. Assess for proteinuria.
This is a diagnostic criterion for preeclampsia, but not a priority action in this situation.
The nurse should assess for proteinuria as part of the routine urinalysis.
Normal ranges for blood pressure are less than 140/90 mm Hg, and for proteinuria are less than 300 mg/24 hours.
A client with gestational hypertension reports abdominal pain and tenderness.
What should the nurse do first?
Explanation
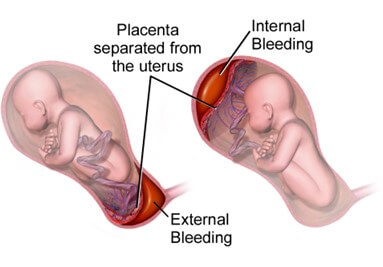
The correct answer is choice B. Assess blood pressure.The nurse should do this first because gestational hypertension is a condition that causes high blood pressure after 20 weeks of pregnancyand can lead to complications such as placental abruptionor preeclampsia.
Abdominal pain and tenderness can be signs of these complications, so the nurse should check the blood pressure to determine the severity of the situation and plan further interventions.
Choice A is wrong because administering acetaminophen may not relieve the pain and may mask other symptoms.
Choice C is wrong because visual disturbances are not the most urgent symptom to assess in this case.
Choice D is wrong because assessing for proteinuria is not the first priority, although it is important to diagnose preeclampsia.
A nurse is caring for a client with gestational hypertension who reports swelling of the face, hands or feet and decreased urine output or protein in urine.
What should the nurse do first?
Explanation
The correct answer is choice B. Assess blood pressure.The nurse should first assess the client’s blood pressure because gestational hypertension is a condition that causes high blood pressure after 20 weeks of pregnancyand can lead to complications such as preeclampsia and abruptio placentae.High blood pressure is a classic sign of preeclampsia, along with proteinuria, edema, headache and blurred vision.
Therefore, the nurse should monitor the client’s blood pressure closely and report any abnormal findings to the health care provider.
Choice A is wrong because administering acetaminophen is not indicated for gestational hypertension and may mask signs of infection or inflammation.
Choice C is wrong because assessing for visual disturbances is not the priority action for gestational hypertension.
Visual disturbances are a symptom of severe preeclampsia or eclampsia, which are more serious conditions that require immediate medical attention.
Choice D is wrong because assessing for proteinuria is not the first action for gestational hypertension.
Proteinuria is a sign of preeclampsia, which may develop from gestational hypertension, but it is not present in all cases.
The nurse should first assess the blood pressure and then check for proteinuria if indicated by the provider or protocol.
Diagnosis and tests
A nurse is assessing a pregnant woman with gestational hypertension.
Which of the following blood pressure readings would lead the nurse to suspect that the client has gestational hypertension?
Explanation
The correct answer is choice B.Choice B is correct because gestational hypertension is defined as a blood pressure (BP) of≥140/90 mmHgon two occasions (at least 4 hours apart) after 20 weeks’ gestation in a previously normotensive woman, without the presence of proteinuria or other clinical features suggestive of preeclampsia.
Choice A is wrong because 130/80 mmHg is within the normal range for blood pressure in pregnancy.
Choice C is wrong because 120/70 mmHg is also within the normal range for blood pressure in pregnancy.
Choice D is wrong because 110/60 mmHg is on the lower end of the normal range for blood pressure in pregnancy and does not indicate hypertension.
Normal blood pressure in pregnancy is usually between 110/70 and 120/80 mmHg.Blood pressure can vary throughout the day and may change with activity, stress, or position
A client is diagnosed with gestational hypertension.
Which of the following tests should the nurse expect to be ordered?
Explanation
The correct answer is choiceC.
An ultrasound to measure fetal growth and amniotic fluid volume is a test that the nurse should expect to be ordered for a client with gestational hypertension.This is because gestational hypertension can cause intrauterine growth restriction and oligohydramnios, which are conditions that affect the fetal development and well-being.
ChoiceAis wrong because urinalysis to check for proteinuria is not a specific test for gestational hypertension, but rather for preeclampsia, which is a more severe complication of gestational hypertension.Proteinuria indicates impaired kidney function due to high blood pressure.
ChoiceBis wrong because blood tests to check for liver enzymes are also not specific for gestational hypertension, but for HELLP syndrome, which is another severe complication of preeclampsia.Elevated liver enzymes indicate impaired liver function due to high blood pressure.
ChoiceDis wrong because nonstress test or biophysical profile to monitor fetal heart rate and movements are not tests that are ordered for gestational hypertension alone, but for any high-risk pregnancy that requires close monitoring of the fetal status.These tests can detect signs of fetal distress or hypoxia.
A nurse is caring for a client with gestational hypertension.
Which of the following symptoms would indicate that the client is developing preeclampsia?
Explanation
The correct answer is choice B.Proteinuria greater than 300 mg in a 24-hour urine collection is one of the criteria for diagnosing preeclampsia, along with hypertension and edema.
Proteinuria indicates that the kidneys are not functioning properly due to the increased blood pressure.
Choice A is wrong because blood pressure of 140/90 mmHg or higher is a sign of gestational hypertension, not preeclampsia.Gestational hypertension is a risk factor for developing preeclampsia, but it does not necessarily mean that the client has preeclampsia.
Choice C is wrong because mild facial edema is a common finding in normal pregnancy and does not indicate preeclampsia.Edema in preeclampsia is usually generalized and severe.
Choice D is wrong because hyperreflexia is a sign of eclampsia, not preeclampsia.Eclampsia is a complication of preeclampsia that involves seizures and coma.
Hyperreflexia indicates increased nervous system irritability due to the high blood pressure.
Normal ranges for blood pressure and proteinuria in pregnancy are:
• Blood pressure: less than 140/90 mmHg
• Proteinuria: less than 300 mg/24 hours
A nurse is caring for a client with gestational hypertension who is at risk for preterm labor.
Which of the following medications should the nurse expect to be ordered?
Explanation
The correct answer is choice C. Nifedipine.Nifedipine is a calcium channel blocker that can be used to treat gestational hypertension and prevent preterm labor by relaxing the smooth muscles of the uterus and blood vessels.It also lowers blood pressure and reduces the risk of preeclampsia.
Choice A is wrong because magnesium sulfate is used to prevent seizures in severe preeclampsia or eclampsia, not to prevent preterm labor.It can also cause adverse effects such as respiratory depression, hypotension, and decreased reflexes.
Choice B is wrong because oxytocin is used to induce or augment labor, not to prevent it.It can also cause adverse effects such as uterine hyperstimulation, fetal distress, and water intoxication.
Choice D is wrong because misoprostol is used to ripen the cervix and induce labor, not to prevent it.It can also cause adverse effects such as uterine rupture, diarrhea, and fever.
A nurse is teaching a client with gestational hypertension about self-care measures to manage her condition at home.
Which of the following instructions should the nurse include?
Explanation
This is because gestational hypertension can cause complications for both the mother and the baby, such as preeclampsia, placental abruption, and intrauterine growth restriction.
Monitoring blood pressure at home can help detect any changes or signs of worsening condition and prompt early intervention.
Choice A is wrong because limiting fluid intake to less than 1 liter per day can cause dehydration and increase blood viscosity, which can worsen hypertension and increase the risk of thrombosis.
Fluid intake should be adequate and balanced to maintain hydration and electrolyte balance.
Choice B is wrong because lying on the left side can help reduce pressure on the inferior vena cava and improve blood flow to the uterus and the kidneys.
Lying on the right side or supine can impair venous return and increase blood pressure.
Choice D is wrong because acetaminophen is a safe and effective analgesic and antipyretic for pregnant women.
It does not affect blood pressure or cause harm to the fetus.
Other medications, such as nonsteroidal anti-inflammatory drugs (NSAIDs) or aspirin, should be avoided as they can increase the risk of bleeding, renal impairment, or premature closure of the ductus arteriosus.
Nursing interventions and Management
A nurse is caring for a client with gestational hypertension who is receiving magnesium sulfate.
What is the main purpose of administering this medication?
Explanation
The correct answer is choice B. To prevent seizures.Magnesium sulfate is a medication that is used to prevent seizures in women with gestational hypertension or preeclampsia.
Seizures can be life-threatening for both the mother and the baby.Magnesium sulfate also has a mild antihypertensive effect, but it is not the main purpose of administering this medication.
Choice A is wrong because magnesium sulfate does not lower blood pressure significantly.Other antihypertensive drugs, such as hydralazine, are used to control blood pressure in women with gestational hypertension or preeclampsia.
Choice C is wrong because magnesium sulfate does not induce labor.It may actually delay labor by relaxing the uterine muscles.Other medications, such as oxytocin, are used to induce labor when needed.
Choice D is wrong because magnesium sulfate does not increase urine output.It may actually decrease urine output by causing fluid retention and renal impairment.Urine output should be monitored closely in women receiving magnesium sulfate to detect signs of toxicity.
A client with severe preeclampsia is admitted to the hospital.
Which of the following signs would indicate that she is at risk for developing eclampsia?
Explanation
The correct answer is choice A. Headache and blurred vision.These are signs ofcerebral edemaor swelling of the brain, which can lead toeclampsia, a life-threatening complication of preeclampsia that causes seizures.
Choice B is wrong because nausea and vomiting are common symptoms of pregnancy and do not indicate a risk for eclampsia.
Choice C is wrong because edema and weight gain are also common in pregnancy and may be due to fluid retention or increased blood volume.
They are not specific signs of preeclampsia or eclampsia.
Choice D is wrong because proteinuria and oliguria are signs ofkidney damagedue to preeclampsia, but they do not directly increase the risk of eclampsia.However, they may indicate severe preeclampsia that requires close monitoring and treatment.
Normal ranges for blood pressure, proteinuria, platelet count, and liver enzymes are as follows:
• Blood pressure: less than 140/90 mm Hg
• Proteinuria: less than 300 mg per 24 hours
• Platelet count: 150,000 to 400,000 per microliter
• Liver enzymes: AST less than 40 U/L, ALT less than 45 U/L
A nurse is monitoring a client with gestational hypertension for signs of fluid retention and edema.
Which of the following assessments would be most helpful?
Explanation
The correct answer is choice C. Weighing the client daily at the same time.This is because weight gain and edema are common signs of fluid retention and preeclampsia, a serious complication of gestational hypertension.Weighing the client daily at the same time can help monitor the fluid status and detect any sudden changes that may indicate worsening preeclampsia.
Choice A is wrong because measuring abdominal girth daily is not a reliable indicator of fluid retention or edema, as it can also be affected by fetal growth, uterine size, and maternal fat distribution.
Choice B is wrong because checking for pitting edema in the lower extremities is not a specific sign of preeclampsia, as it can also occur in normal pregnancies due to increased blood volume and venous pressure.
Choice D is wrong because auscultating lung sounds for crackles is not a helpful assessment for fluid retention and edema, as it is a late sign of pulmonary edema, which is a rare but life-threatening complication of severe preeclampsia.

A nurse is teaching a client with gestational hypertension about dietary modifications.
Which of the following instructions would be appropriate?
Explanation
The correct answer is choice C. Avoid foods high in sodium such as canned soups and processed meats.This is because sodium can increase blood pressure and fluid retention, which are complications of gestational hypertension.
Choice A is wrong because increasing calcium intake does not prevent bone loss in gestational hypertension.Calcium supplementation may be beneficial for preventing preeclampsia, which is a more severe form of gestational hypertension.
Choice B is wrong because limiting fluid intake to 1 liter per day can cause dehydration and electrolyte imbalance, which can harm both the mother and the fetus.Fluid intake should be adequate to maintain hydration and urine output.
Choice D is wrong because eating foods rich in iron is not related to gestational hypertension.
Iron intake may be important for preventing anemia, which can occur in pregnancy due to increased blood volume and fetal demands.
A nurse is preparing a client with gestational hypertension for delivery.
Which of the following factors would indicate that the client is ready for delivery?
Explanation
The correct answer is choice D. All of the above.
All of these factors would indicate that the client is ready for delivery because they pose a risk to the mother or the fetus or both.
Choice A is wrong because blood pressure that is uncontrollable despite medication can lead to complications such as preeclampsia, eclampsia, or HELLP syndrome.
Choice B is wrong because fetal distress detected by nonstress test or biophysical profile can indicate hypoxia, acidosis, or cord compression.
Choice C is wrong because term is reached (37 weeks or more) does not necessarily mean that the client is ready for delivery.Other factors such as cervical dilation, effacement, and station also need to be considered.
Normal ranges for blood pressure are 120/80 mmHg or lower for systolic and 80/60 mmHg or lower for diastolic.Normal ranges for nonstress test are two or more fetal heart rate accelerations of at least 15 beats per minute above baseline lasting at least 15 seconds in a 20-minute period.Normal ranges for biophysical profile are a score of 8 to 10 out of 10 based on five parameters: fetal breathing movements, fetal movements, fetal tone, amniotic fluid volume, and nonstress test.
Comparison with other types of hypertension during pregnancy
A nurse is reviewing the chart of a client who has gestational hypertension.
Which of the following findings should the nurse expect to see?
Explanation
The correct answer is choice A. Proteinuria of 2+ is a sign of preeclampsia, a serious complication of gestational hypertension that can affect the mother and the fetus.Preeclampsia is diagnosed by high blood pressure and protein in the urine after 20 weeks of pregnancy.
Choice B is wrong because gestational hypertension usually begins after 20 weeks of pregnancy, not before.
Choice C is wrong because blood pressure of 150/95 mmHg is not enough to diagnose gestational hypertension.The blood pressure must be greater than or equal to 140/90 mmHg on two occasions at least four hours apart.
Choice D is wrong because gestational hypertension does not resolve within 48 hours postpartum.It may last up to 12 weeks after delivery.

A nurse is caring for a client who has chronic hypertension and is pregnant.
The nurse should monitor the client for which of the following complications?
Explanation
The correct answer is choice A. Superimposed preeclampsia.This is a condition where a woman with chronic hypertension develops preeclampsia during pregnancy.Preeclampsia is a complication of pregnancy that involves high blood pressure, protein in the urine, and organ damage.
Choice B.Eclampsia is wrong because it is a severe form of preeclampsia that causes seizures and coma.
It is not a complication of chronic hypertension alone.
Choice C.HELLP syndrome is wrong because it is a life-threatening complication of preeclampsia that involves hemolysis, elevated liver enzymes, and low platelets.
It is not specific to chronic hypertension.
Choice D.Placenta previa is wrong because it is a condition where the placenta covers the cervix and causes bleeding during pregnancy or delivery.
It is not related to chronic hypertension or preeclampsia.
A nurse is teaching a group of pregnant clients about preeclampsia.
Which of the following statements by a client indicates a need for further teaching?
Explanation
The correct answer is choice D.Increasing salt intake to prevent fluid retention is a wrong statement because salt can worsen fluid retention and increase blood pressure, which are both signs of preeclampsia.People with preeclampsia should follow a low-salt diet and drink plenty of fluids.
Choice A is correct because changes in vision, such as blurriness, light sensitivity or dark spots, can indicate brain trouble due to preeclampsia.People with preeclampsia should report any vision changes to their provider as soon as possible.
Choice B is correct because aspirin and ibuprofen are nonsteroidal anti-inflammatory drugs (NSAIDs) that can increase blood pressure and affect kidney function, which are both complications of preeclampsia.People with preeclampsia should avoid taking NSAIDs during pregnancy unless prescribed by their provider.
Choice C is correct because lying on the left side can help lower blood pressure and improve blood flow to the placenta, which can benefit both the mother and the baby in preeclampsia.People with preeclampsia should lie on their left side if they have a headache or other symptoms.

A nurse is assessing a client who has eclampsia and is receiving magnesium sulfate IV.
Which of the following findings should alert the nurse to possible magnesium toxicity?
Explanation
The correct answer is choice A.Respiratory rate of 10 breaths/min is a sign ofmagnesium toxicity, which can occur in clients receiving magnesium sulfate IV for eclampsia.
The nurse should stop the infusion and notify the provider immediately.
Choice B is wrong because urine output of 40 mL/hr is within the normal range and does not indicate magnesium toxicity.
Choice C is wrong because deep tendon reflexes of 2+ are normal and do not indicate magnesium toxicity.
Diminished or absent deep tendon reflexes are a sign of magnesium toxicity.
Choice D is wrong because serum magnesium level of 6 mg/dL is within the normal range and does not indicate magnesium toxicity.The normal range for serum magnesium level is 1.7 to 2.3 mg/dL.
A nurse is providing discharge instructions to a client who had gestational hypertension and delivered a healthy newborn.
Which of the following statements should the nurse include in the teaching?
Explanation
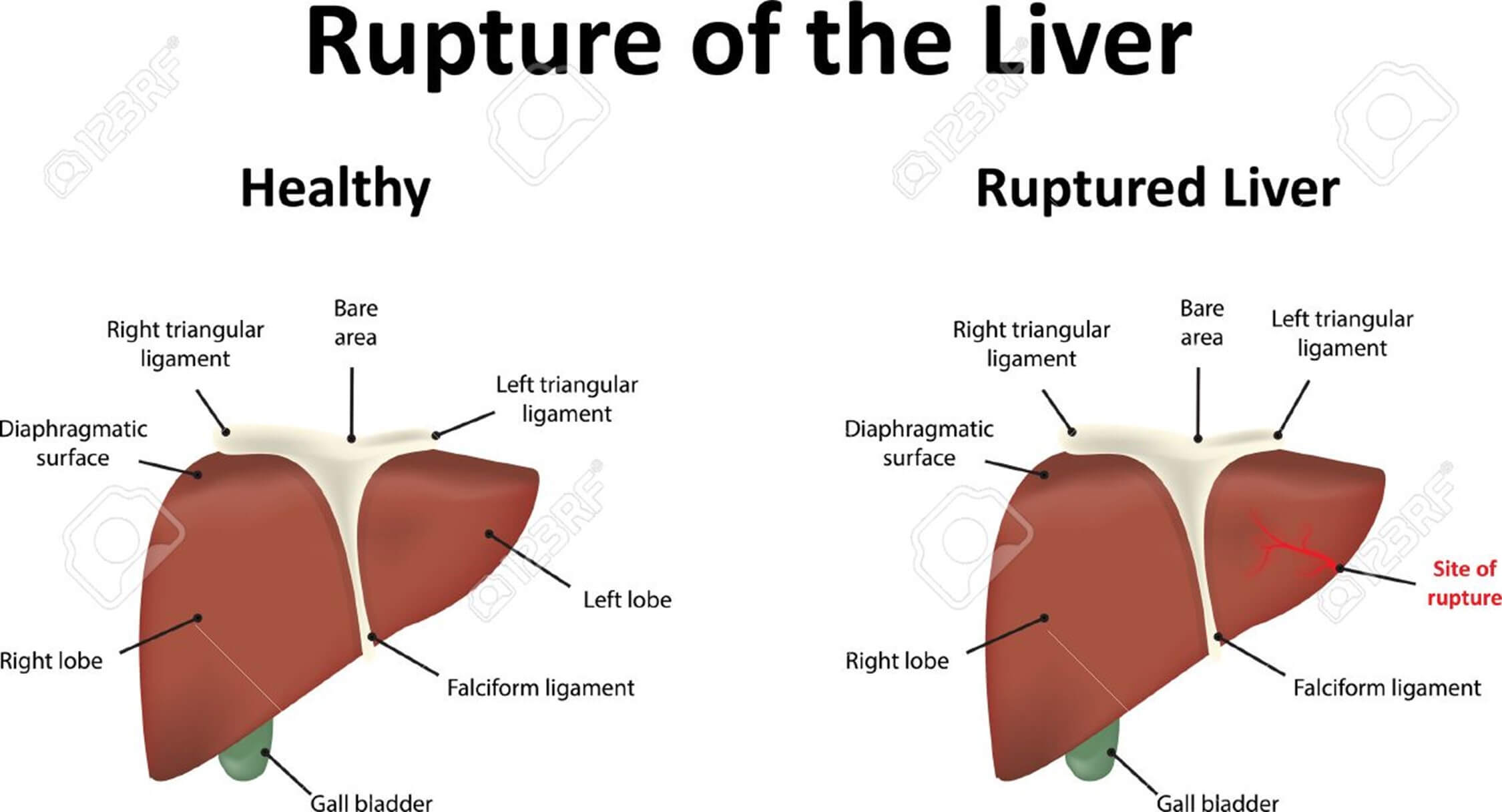
The correct answer is choice C. The nurse should include in the teaching that the client should report any blurred vision or abdominal pain to their provider.These are signs of severe preeclampsia, which can occur after delivery and can lead to serious complications such as eclampsia, stroke, or liver rupture.
Choice A is wrong because the client should have their blood pressure checked again within 7 to 10 days after delivery, and then again at 6 weeks postpartum.
Six months is too long to wait for a follow-up.
Choice B is wrong because the client can breastfeed safely even if they have high blood pressure or are taking antihypertensive medications.Breastfeeding has many benefits for both the mother and the baby, and most antihypertensive drugs are compatible with breastfeeding.
Choice D is wrong because oral contraceptives are not recommended for women who have had gestational hypertension or preeclampsia, especially if they have other risk factors such as obesity, smoking, or thrombophilia.Oral contraceptives can increase the risk of thromboembolic events and hypertension in these women.Non-hormonal or progestogen-only methods of contraception are preferred.
Outcomes and prognosis
A nurse is caring for a client with gestational hypertension who is receiving magnesium sulfate intravenously.
What is the primary reason for administering magnesium sulfate to this client?
Explanation
The correct answer is choice B. To prevent seizures.Magnesium sulfate is primarily used for its anticonvulsive effects in treating hypertensive disorders of pregnancy.It helps to prevent and manage seizures during stabilization and until 24 hours after delivery.
Choice A is wrong because magnesium sulfate does not lower the blood pressure.It may have a mild vasodilatory effect, but it is not the main mechanism of action.Antihypertensive drugs such as nifedipine are used to lower the blood pressure in gestational hypertension.
Choice C is wrong because magnesium sulfate does not induce labor.It may have a tocolytic effect, which means it can relax the uterine muscles and delay preterm labor.
Choice D is wrong because magnesium sulfate does not increase urine output.It may cause fluid retention and edema, which are adverse effects that need to be monitored.Diuretics are used to increase urine output, but they are not recommended for hypertensive disorders during pregnancy.
A nurse is reviewing the laboratory results of a client with gestational hypertension who has developed preeclampsia.
Which of the following findings would indicate the presence of HELLP syndrome?
Explanation
The correct answer is choice C.Elevated serum transaminases indicate liver damage, which is one of the features of HELLP syndrome.HELLP syndrome is a rare pregnancy complication that is a type of preeclampsia and has similar symptoms.It stands for hemolysis, elevated liver enzymes, and low platelet count.
Choice A is wrong because elevated serum creatinine indicates kidney damage, which is not specific for HELLP syndrome.Kidney damage can occur in preeclampsia or eclampsia as well.
Choice B is wrong because elevated serum uric acid is also not specific for HELLP syndrome.It can be a marker of preeclampsia or eclampsia, but it is not part of the diagnostic criteria for HELLP syndrome.
Choice D is wrong because elevated serum glucose is not related to HELLP syndrome.It can be a sign of gestational diabetes, which is a different pregnancy complication.
Normal ranges for serum transaminases are 10 to 40 U/L for AST and 7 to 56 U/L for ALT.Normal ranges for serum creatinine are 0.5 to 1.1 mg/dL for women.Normal ranges for serum uric acid are 2.4 to 6.0 mg/dL for women.Normal ranges for serum glucose are 70 to 100 mg/dL for fasting and less than 140 mg/dL for postprandial.
A nurse is teaching a client with gestational hypertension about the signs and symptoms of placental abruption.
Which of the following statements by the client indicates a need for further teaching?
Explanation
The correct answer is choice D. Drinking plenty of fluids if there is decreased fetal movement is wrong because it will not improve the condition of the baby or the placenta.Decreased fetal movement can be a sign of fetal distress due to placental abruption and needs immediate medical attention.
Choice A is correct because vaginal bleeding is a common symptom of placental abruption and indicates that the placenta has separated from the uterus.
Choice B is correct because monitoring blood pressure at home regularly is important for women with gestational hypertension, as high blood pressure is a risk factor for placental abruption.
Choice C is correct because lying down on the left side can improve blood flow to the uterus and the baby, and may help relieve abdominal pain caused by placental abruption.
A nurse is preparing to discharge a client with gestational hypertension who delivered a healthy baby two days ago.
Which of the following instructions should the nurse include in the discharge teaching?
Explanation
The correct answer is choice B. You should continue taking your antihypertensive medication as prescribed.This is because gestational hypertension can persist for several days or weeks after delivery and may increase your risk of complications such as stroke or heart failure.You should also monitor your blood pressure at home and report any abnormal readings to your provider.
Choice A is wrong because you should not avoid breastfeeding your baby unless your provider advises you to do so.Breastfeeding has many benefits for both you and your baby and does not affect your blood pressure.
Choice C is wrong because you do not need to limit your sodium intake to less than 2 grams per day unless your provider tells you to do so.There is no evidence that sodium restriction lowers blood pressure or prevents preeclampsia in pregnant women.
Choice D is wrong because you should have a follow-up appointment with your provider within one week after delivery, not six weeks.This is to check your blood pressure, review your medication, and screen for any postpartum complications.
A nurse is assessing a client with gestational hypertension who is at 34 weeks of gestation.
The nurse notes that the client’s blood pressure is 160/100 mmHg, her urine protein is 3+, and she has mild edema in her lower extremities.
The nurse also observes that the client has brisk deep tendon reflexes and clonus.
How should the nurse interpret these findings?
Explanation
The correct answer is choice B. The client has severe preeclampsia and needs immediate delivery.Severe preeclampsia is diagnosed when the blood pressure is at least 160/100 mmHg, the urine protein is 3+ or more, and there are signs of organ damage or central nervous system involvement, such as brisk deep tendon reflexes and clonus.These findings indicate a high risk of eclampsia, which is a life-threatening condition characterized by seizures.Immediate delivery is the only definitive treatment for preeclampsia and eclampsia.
Choice A is wrong because the client has more than mild preeclampsia.Mild preeclampsia is diagnosed when the blood pressure is at least 140/90 mmHg, the urine protein is 1+ or 2+, and there are no signs of organ damage or central nervous system involvement.Close monitoring may be appropriate for mild preeclampsia, depending on the gestational age and fetal status.
Choice C is wrong because the client does not have eclampsia yet.Eclampsia is diagnosed when the client has preeclampsia and seizures.Magnesium sulfate and anticonvulsants are used to prevent and treat seizures in eclampsia, but they do not cure preeclampsia.Delivery is still necessary to resolve the condition.
Choice D is wrong because the client does not have chronic hypertension.Chronic hypertension is high blood pressure that was present before pregnancy or that occurs before 20 weeks of gestation.The client’s blood pressure was normal before pregnancy and increased after 20 weeks of gestation, indicating gestational hypertension or preeclampsia.
Antihypertensive medication adjustment may be needed for chronic hypertension
More Questions On This Topic
Which of the following factors increases a woman’s risk for developing gestational hypertension.
Explanation
The correct answer is choice D. All of the above.All of these factors increase a woman’s risk for developing gestational hypertension.
Choice A is wrong because nulliparity (having no previous pregnancies) is a risk factor for gestational hypertension.Rates in nulliparous women range from 6% to 17% while rates in multiparous women range from 2% to 4%.
Choice B is wrong because age younger than 20 years is a risk factor for gestational hypertension.Pregnant women more than 40 years or less than 18 years are at risk of gestational hypertension.
Choice C is wrong because history of chronic renal disease is a risk factor for gestational hypertension.High blood pressure can also cause problems during and after delivery, such as preeclampsia, eclampsia, stroke, and placental abruption.
Gestational hypertension is blood pressure greater than or equal to 140/90 that begins during the latter half of pregnancy (typically after 20 weeks) and goes away after childbirth.It can put the mother and her baby at risk for problems during the pregnancy, such as preterm delivery and low birth weight.
What is the most common cause of death in women with eclampsia.
Explanation
The correct answer is choice A. Cerebral hemorrhage.Eclampsia is a severe complication of preeclampsia that causes seizures and can lead to stroke or death.Cerebral hemorrhage is bleeding in the brain that can result from high blood pressure and swelling in the brain caused by eclampsia.It is one of the most common causes of death in women with eclampsia.
Choice B. Pulmonary edema is wrong because it is not the most common cause of death in women with eclampsia.
Pulmonary edema is fluid accumulation in the lungs that can impair breathing and oxygen exchange.It can occur as a complication of eclampsia, but it is less frequent than cerebral hemorrhage.
Choice C. Liver rupture is wrong because it is not the most common cause of death in women with eclampsia.
Liver rupture is a rare but serious complication of eclampsia that involves bleeding from the liver due to increased pressure and damage to the liver tissue.It can cause severe abdominal pain, shock and death.
Choice D. Disseminated intravascular coagulation (DIC) is wrong because it is not the most common cause of death in women with eclampsia.
DIC is a condition where the blood clotting system becomes overactive and forms clots throughout the body, leading to bleeding and organ failure.It can occur as a complication of eclampsia, but it is less common than cerebral hemorrhage.
Normal ranges for blood pressure are below 140/90 mmHg and for proteinuria are below 300 mg/24 hours or below 30 mg/dL in a urine sample.
What is a priority nursing intervention for a woman with severe preeclampsia who is receiving hydralazine IV.
Explanation
The correct answer is choice B. Monitor fetal heart rate continuously.This is because hydralazine is a vasodilator that lowers blood pressure and may cause tachycardia.Tachycardia can affect the fetal heart rate and oxygenation, so continuous monitoring is essential to detect any signs of fetal distress.
Choice A is wrong because hydralazine does not cause orthostatic hypotension, but rather a reflex increase in heart rate and cardiac output.
Orthostatic hypotension is more likely to occur with other antihypertensive drugs such as alpha-blockers or diuretics.
Choice C is wrong because encouraging oral fluid intake may worsen the fluid retention and edema that are common in preeclampsia.Fluid intake should be restricted to avoid pulmonary edema and cerebral edema.
Choice D is wrong because administering oxygen via nasal cannula is not a priority intervention for a woman with severe preeclampsia who is receiving hydralazine IV.Oxygen therapy may be indicated if the woman develops signs of hypoxia, such as dyspnea, cyanosis, or low oxygen saturation.However, oxygen therapy should be used with caution as it may increase oxidative stress and placental vasoconstriction.
A nurse is caring for a client with gestational hypertension who has been prescribed magnesium sulfate to prevent seizures related to preeclampsia.
Which of the following assessments should the nurse prioritize?
Explanation
The correct answer is choice D) Level of consciousness and reflexes.This is because magnesium sulfate can cause toxicity and affect the central nervous system, leading to decreased level of consciousness and loss of reflexes.These are signs that the dose of magnesium sulfate should be reduced or stopped.
The nurse should prioritize assessing these parameters to prevent seizures and avoid magnesium toxicity.
Choice A) Respiratory rate and depth is wrong because magnesium sulfate can also cause respiratory depression, but this is a less common and less sensitive indicator of toxicity than level of consciousness and reflexes.
Choice B) Urine output and color is wrong because magnesium sulfate can also cause renal impairment, but this is not directly related to preventing seizures.However, urine output should be monitored to ensure adequate hydration and renal function.
Choice C) Blood pressure and heart rate is wrong because magnesium sulfate can also cause hypotension and bradycardia, but these are not the primary goals of therapy.Blood pressure and heart rate should be monitored to assess the severity of preeclampsia and the response to antihypertensive medications.
A nurse is caring for a client with gestational hypertension who has been prescribed labetalol (Normodyne) to control blood pressure during pregnancy.
Which of the following statements by the client indicates an understanding of the medication?
Explanation
The correct answer is choice C) “I should report any dizziness or lightheadedness while taking this medication.” This is because labetalol can lower blood pressure and cause orthostatic hypotension, which can lead to falls and injuries.The patient should be advised to change positions slowly and monitor their blood pressure regularly while taking labetalol.
Choice A is wrong because labetalol can be taken with or without food.Taking it on an empty stomach does not affect its absorption or efficacy.
Choice B is wrong because labetalol does not affect potassium levels in the blood.Foods high in potassium are not contraindicated while taking this medication.
Choice D is wrong because swelling in the feet or hands can be a sign of worsening preeclampsia, which is a serious complication of hypertension in pregnancy.The patient should not stop taking labetalol without consulting their doctor, as this can cause rebound hypertension and endanger the mother and the fetus.The patient should seek medical attention if they experience swelling, headache, vision changes, abdominal pain, or reduced fetal movements.
A nurse is caring for a client with gestational hypertension who has been prescribed methyldopa (Aldomet) to control blood pressure during pregnancy.
Which of the following side effects should the nurse monitor for?
Explanation
Methyldopa is a drug that lowers blood pressure by reducing the activity of the sympathetic nervous system.
One of the possible side effects of methyldopa is hypotension, which means abnormally low blood pressure.Hypotension can cause dizziness, fainting, and shock.
Choice A) Bradycardia is wrong because methyldopa does not affect the heart rate directly.Bradycardia means a slow heart rate, which can be caused by other drugs or conditions.
Choice C) Hyperkalemia is wrong because methyldopa does not affect the potassium levels in the blood.Hyperkalemia means high potassium levels, which can be caused by kidney problems or other drugs.
Choice D) Hyperglycemia is wrong because methyldopa does not affect the glucose levels in the blood.Hyperglycemia means high glucose levels, which can be caused by diabetes or other conditions.
Normal ranges for blood pressure are 90/60 mmHg to 120/80 mmHg, for heart rate are 60 to 100 beats per minute, for potassium are 3.5 to 5.0 mmol/L, and for glucose are 70 to 100 mg/dL.
Which of the following is a sign or symptom of gestational hypertension?
Explanation
The correct answer is choice D) Swelling of the face, hands or feet.This is one of the signs and symptoms of gestational hypertension, which is high blood pressure that begins after 20 weeks of pregnancy and goes away after delivery.Gestational hypertension can lead to complications for both the mother and the baby, such as preeclampsia, which is a severe condition that causes protein in the urine and other problems.
Choice A) Severe headache is wrong because it is not a specific sign of gestational hypertension, but it can be a symptom of preeclampsia, which is a possible complication of gestational hypertension.
Choice B) Chest pain is wrong because it is not a common sign of gestational hypertension, but it can be a sign of a serious heart problem or a pulmonary embolism, which is a blood clot in the lungs.Chest pain during pregnancy should be evaluated by a doctor as soon as possible.
Choice C) Nausea or vomiting is wrong because it is not a typical sign of gestational hypertension, but it can be a symptom of preeclampsia or other conditions such as hyperemesis gravidarum, which is severe nausea and vomiting during pregnancy that can lead to dehydration and weight loss.
Normal blood pressure ranges for pregnant women are below 120/80 mm Hg.Gestational hypertension is diagnosed when the blood pressure is greater than or equal to 140/90 mm Hg after 20 weeks of pregnancy.
Which of the following signs and symptoms may indicate worsening condition or preeclampsia in a client with gestational hypertension?
Explanation
The correct answer ischoice A, B, D and E.These are all signs and symptoms that may indicate worsening condition or preeclampsia in a client with gestational hypertension.Preeclampsia is a complication of pregnancy that is marked by high blood pressure and presence of proteins in urine.
Choice C is wrong because chest pain or shortness of breath are not typical symptoms of preeclampsia, but they may indicate other serious conditions such as heart problems or pulmonary edema.
If a client with gestational hypertension experiences these symptoms, they should seek immediate medical attention.
Normal ranges for blood pressure and proteinuria are:
• Blood pressure: less than 140/90 mm Hg.
• Proteinuria: less than 300 mg in a 24-hour urine collection or less than 30 mg/dL in a random urine sample.
Which of the following signs and symptoms may indicate worsening condition or preeclampsia in a client with gestational hypertension?
Explanation
The correct answer is choice B, D and E. These are signs and symptoms of preeclampsia, a serious complication of gestational hypertension that can affect the mother and the baby.Preeclampsia is marked by high blood pressure and protein in urine or other signs of organ damage.
Choice A is wrong because swelling of the face, hands or feet is a common symptom of pregnancy and does not necessarily indicate preeclampsia.However, sudden or severe swelling can be a warning sign and should be checked by a healthcare provider.
Choice C is wrong because severe headache is a symptom of preeclampsia, not gestational hypertension.Gestational hypertension is high blood pressure that develops after 20 weeks of pregnancy and does not have protein in urine or other signs of organ damage.
Some normal ranges for blood pressure during pregnancy are:
• Systolic (top number): less than 140 mm Hg
• Diastolic (bottom number): less than 90 mm Hg
Some normal ranges for protein in urine during pregnancy are:
• Less than 300 mg per 24 hours
• Less than 0.3 g per liter
A client is diagnosed with preeclampsia and is receiving magnesium sulfate IV for seizure prophylaxis.
The nurse should monitor which of the following laboratory values?
Explanation
The correct answer is choice A) Serum magnesium level.Magnesium sulfate is a mineral that reduces seizure risks in women with preeclampsia.It is often given intravenously and can also be used to prolong pregnancy for up to two days.However, magnesium sulfate can also cause side effects and toxicity, such as respiratory depression, muscle weakness, and cardiac arrest.Therefore, the nurse should monitor the serum magnesium level to ensure that it is within the therapeutic range of 4 to 7 mg/dL.
Choice B) Serum potassium level is wrong because magnesium sulfate does not affect the potassium level significantly.
Potassium is an electrolyte that regulates the nerve and muscle function, especially the heart.
The normal range of potassium level is 3.5 to 5.0 mEq/L.
Choice C) Serum sodium level is wrong because magnesium sulfate does not affect the sodium level significantly.
Sodium is another electrolyte that helps maintain fluid balance and blood pressure.
The normal range of sodium level is 135 to 145 mEq/L.
Choice D) Serum calcium level is wrong because magnesium sulfate does not affect the calcium level significantly.
Calcium is a mineral that is important for bone health, blood clotting, and muscle contraction.
The normal range of calcium level is 8.5 to 10.2 mg/dL.
Which of the following interventions should be included in the plan of care for a client with severe preeclampsia? (Select all that apply.)
Explanation
The correct answer is choices A, B, C and D.These are all interventions that can help lower blood pressure, prevent seizures, and monitor the health of the mother and the baby in severe preeclampsia.
Choice E is wrong because continuous fetal heart rate monitoring is not necessary for severe preeclampsia unless there are signs of fetal distress or labor.Intermittent auscultation or nonstress test can be used instead to assess fetal well-being.
Normal ranges for blood pressure are below 140/90 mmHg, for urine output are 30 mL/hour or more, for platelet count are 150,000 to 450,000 per microliter, and for liver enzymes are 7 to 56 units per liter for AST and 0 to 35 units per liter for ALT.Magnesium sulfate levels should be maintained between 4 to 7 mg/dL to prevent toxicity.Fetal heart rate should be between 110 to 160 beats per minute.
Which of the following findings would indicate that a client with preeclampsia is experiencing HELLP syndrome?
Explanation
The correct answer is choice C) Elevated serum bilirubin levels.This is because bilirubin is a product of hemolysis (the breakdown of red blood cells), which is one of the components of HELLP syndrome.Elevated serum bilirubin levels indicate that there is excessive hemolysis occurring in the body, which can lead to jaundice and liver damage.
Choice A) Elevated serum creatinine levels is wrong because creatinine is a marker of kidney function, not liver function or hemolysis.While kidney failure can occur as a complication of HELLP syndrome, it is not a diagnostic criterion.
Choice B) Elevated serum uric acid levels is wrong because uric acid is also a marker of kidney function, not liver function or hemolysis.Uric acid levels can be elevated in preeclampsia, but not specifically in HELLP syndrome.
Choice D) Elevated serum glucose levels is wrong because glucose is not related to liver function or hemolysis.Glucose levels can be elevated in gestational diabetes, but not in HELLP syndrome.
Normal ranges for these tests are:
• Serum bilirubin: 0.3 to 1.2 mg/dL
• Serum creatinine: 0.6 to 1.1 mg/dL
• Serum uric acid: 2.4 to 6.0 mg/dL
• Serum glucose: 70 to 100 mg/dL
A nurse is reviewing the laboratory results of a client with gestational hypertension who has been diagnosed with HELLP syndrome.
Which of the following findings would the nurse expect to see?
Explanation
The correct answer is choice D. Hemoglobin 6 g/dL, platelets 25,000/mm3, AST 120 U/L, ALT 100 U/L.
This is because HELLP syndrome is a pregnancy complication that causes hemolysis (breaking down of red blood cells), elevated liver enzymes (indicating liver injury), and low platelet count (impairing blood clotting).
Choice A is wrong because hemoglobin 12 g/dL, platelets 150,000/mm3, AST 20 U/L, ALT 18 U/L are all within normal ranges and do not indicate HELLP syndrome.
Choice B is wrong because hemoglobin 10 g/dL, platelets 100,000/mm3, AST 40 U/L, ALT 35 U/L are mildly abnormal and may suggest mild preeclampsia but not HELLP syndrome.
Choice C is wrong because hemoglobin 8 g/dL, platelets 50,000/mm3, AST 80 U/L, ALT 70 U/L are moderately abnormal and may suggest moderate preeclampsia or incomplete HELLP syndrome but not full HELLP syndrome.
Normal ranges for these laboratory tests are:
• Hemoglobin: 11.5 to 16.5 g/dL for women.
• Platelets: 150,000 to 450,000/mm3 for adults.
• AST: 10 to 40 U/L for adults.
• ALT: 7 to 56 U/L for adults.
A nurse is administering nifedipine to a client with gestational hypertension as prescribed by the provider.
Which of the following actions would the nurse take to ensure safe administration of this medication?
Explanation
The correct answer is choice A. Check blood pressure before and after giving the medication.Nifedipine is an antihypertensive medication that is used to treat gestational hypertension.It lowers blood pressure by relaxing the blood vessels and reducing the workload of the heart.Checking blood pressure before and after giving the medication helps to monitor the effectiveness and safety of the treatment.
Choice B is wrong because grapefruit juice can interact with nifedipine and increase its blood levels, which can cause excessive lowering of blood pressure or other side effects.Grapefruit juice should be avoided when taking nifedipine.
Choice C is wrong because nifedipine does not affect the pulse rate significantly.Holding the medication if pulse rate is below 60 beats per minute is more appropriate for beta-blockers, such as labetalol, which are another class of antihypertensive medications that can slow down the heart rate.
Choice D is wrong because nifedipine does not cause hypoglycemia.Monitoring blood glucose levels for signs of hypoglycemia is more relevant for medications that lower blood sugar, such as insulin or oral antidiabetic agents.
Normal ranges for blood pressure and pulse rate during pregnancy are 110-140/60-90 mmHg and 60-100 beats per minute, respectively.Normal range for blood glucose level during pregnancy is 70-110 mg/dL.
(Select all that apply).
A nurse is providing discharge teaching to a client with gestational hypertension who delivered a healthy baby two days ago.
Which of the following statements by the client would indicate a need for further teaching?
Explanation
The correct answer is choice C. Choice C is wrong because breastfeeding is not contraindicated for women with gestational hypertension.Breastfeeding has many benefits for both the mother and the baby, and it does not affect blood pressure.
Choice A is correct because blood pressure medication should be continued as prescribed until the next check-up.Stopping medication abruptly can cause a rebound increase in blood pressure and increase the risk of complications.
Choice B is correct because headache, blurred vision, or abdominal pain are signs of severe preeclampsia, a serious complication of gestational hypertension that can affect the brain, liver, and kidneys.These symptoms should be reported to the provider immediately.
Choice D is correct because limiting salt intake and drinking plenty of fluids can help lower blood pressure and prevent fluid retention.
Salt can cause the body to hold on to excess water, which increases blood volume and blood pressure.Fluids can help flush out excess salt and keep the body hydrated.
Choice E is correct because weighing oneself daily and reporting any sudden weight gain to the provider can help monitor fluid balance and detect signs of preeclampsia.A weight gain of more than 2 pounds in a week or 5 pounds in a month may indicate fluid accumulation and increased blood pressure.
A nurse is caring for a client who has severe preeclampsia and is receiving hydralazine IV bolus for blood pressure management.
Which of the following adverse effects should the nurse monitor for? (Select all that apply.)
Explanation
The correct answer is choice A and B. Hydralazine is a drug that lowers blood pressure by relaxing the blood vessels.It can cause some side effects such astachycardia(fast heart rate) andheadache.
These are common and may go away during treatment.
However, if they are severe or persistent, the nurse should monitor the client and report to the doctor.
Choice C is wrong because nausea is not a common side effect of hydralazine.
It may be caused by other factors such as pregnancy or infection.
Choice D is wrong because hyperkalemia (high potassium level in the blood) is not a side effect of hydralazine.
It may be caused by other drugs such as angiotensin-converting enzyme inhibitors or potassium-sparing diuretics.
Choice E is wrong because oliguria (low urine output) is not a side effect of hydralazine.
It may be a sign of kidney damage or dehydration.
The nurse should monitor the client’s fluid intake and output and report any changes to the doctor.
A nurse is reviewing laboratory results for a client who has HELLP syndrome.
Which of the following findings should the nurse expect? (Select all that apply.)
Explanation
The correct answer is choice A, B, C and D.These choices reflect the laboratory findings that are expected in a client who has HELLP syndrome.HELLP syndrome is a rare pregnancy complication that is a type of preeclampsia and has similar symptoms.It can cause serious blood and liver problems.
Choice A is correct because hemoglobin of 9 g/dL indicates hemolysis, which is the breaking down of red blood cells.The normal range of hemoglobin for pregnant women is 11 to 16 g/dL.
Choice B is correct because platelets of 90,000/mm3 indicate thrombocytopenia, which is a low platelet count.The normal range of platelets for pregnant women is 150,000 to 400,000/mm3.
Choice C is correct because AST of 120 U/L indicates elevated liver enzymes, which reflect liver injury.The normal range of AST for pregnant women is 10 to 40 U/L.
Choice D is correct because LDH of 600 U/L indicates elevated lactate dehydrogenase, which is a marker of hemolysis.The normal range of LDH for pregnant women is 140 to 280 U/L.
Choice E is wrong because WBC of 15,000/mm3 indicates leukocytosis, which is not a feature of HELLP syndrome.The normal range of WBC for pregnant women is 5,000 to 15,000/mm3.
A nurse is preparing to administer an IV loading dose of magnesium sulfate to a client who has preeclampsia with severe features.
Which of the following actions should the nurse take?
Explanation
The correct answer is choice D. Have calcium gluconate available at the bedside as an antidote.Magnesium sulfate is used to prevent and treat seizures in women with severe preeclampsia or eclampsia.However, it can also cause toxicity and respiratory depression if the serum level is too high.Calcium gluconate is the antidote for magnesium sulfate toxicity and should be readily available at the bedside.
Choice A is wrong because the medication should be administered over 20-30 minutes using an infusion pump.
A shorter infusion time may increase the risk of adverse effects.
Choice B is wrong because the client should be placed in a lateral position to improve uteroplacental perfusion and reduce the risk of aspiration.
Choice C is wrong because the client’s blood pressure should be monitored every 5 minutes during the infusion, not every 15 minutes.
Blood pressure is an indicator of the severity of preeclampsia and the effectiveness of magnesium sulfate therapy.
A nurse is caring for a client with gestational hypertension who is at risk for developing preeclampsia.
Which of the following interventions should the nurse implement to prevent this complication? (Select all that apply.).
Explanation
The correct answer is choice A, C and D.These interventions can help prevent or delay the development of preeclampsia by reducing blood pressure, monitoring fetal well-being and assessing for signs of worsening condition.
Choice B is wrong because corticosteroids are not used to prevent preeclampsia, but to enhance fetal lung maturity in case of preterm delivery.
Choice E is wrong because a diet high in protein and low in carbohydrates is not recommended for gestational hypertension or preeclampsia.A balanced diet with adequate calcium, magnesium and antioxidants is advised.
A nurse is evaluating the effectiveness of magnesium sulfate therapy for a client with severe preeclampsia who is in labor.
Which of the following findings would indicate that the therapy is effective?
Explanation
The correct answer is choice B. The client’s urine output is at least 30 mL/hr.This indicates that the therapy is effective because magnesium sulfate can cause renal impairment and fluid retention, which can worsen the condition of preeclampsia.
A normal urine output is a sign that the kidneys are functioning well and that the fluid balance is maintained.
Choice A is wrong because the client’s blood pressure may not normalize even with magnesium sulfate therapy.
Magnesium sulfate is mainly used to prevent seizures, not to lower blood pressure.Other antihypertensive medications may be needed to control blood pressure in severe preeclampsia.
Choice C is wrong because the client’s deep tendon reflexes are expected to decrease with magnesium sulfate therapy, as it is a central nervous system depressant.
A normal reflex response is 2+, but a lower response (1+ or 0) may indicate magnesium toxicity, which can cause respiratory depression, cardiac arrest, and coma.
Choice D is wrong because the client’s respiratory rate should be monitored closely with magnesium sulfate therapy, as it can also cause respiratory depression.
A normal respiratory rate is 12 to 20 breaths per minute, but a lower rate (less than 12) may indicate magnesium toxicity, which requires immediate treatment with calcium gluconate.
A nurse is reviewing the risk factors for gestational hypertension with a group of pregnant clients at a prenatal clinic.
Which of the following factors should the nurse include? (Select all that apply.).
Explanation
The correct answer is choice A, B, C and E.These are all risk factors for gestational hypertension according to various sources.
Some possible explanations for each choice are:
• Choice A: Maternal age over 35 years.Older women are more likely to have chronic hypertension, diabetes, or other conditions that increase the risk of gestational hypertension.
• Choice B: First pregnancy.Women who are pregnant for the first time are more likely to develop gestational hypertension than women who have had previous pregnancies.
• Choice C: Multiple gestation.Women who are carrying twins, triplets, or more are more likely to have gestational hypertension because of the increased placental mass and blood volume.
• Choice D: History of diabetes mellitus.This is not a risk factor for gestational hypertension, but it is a risk factor for preeclampsia, which is a more severe form of hypertension that involves proteinuria and organ damage.
Preeclampsia can develop from gestational hypertension or occur independently.
• Choice E: African American race.African American women are more likely to have gestational hypertension than women of other races or ethnicities.
This may be due to genetic, environmental, or social factors that affect blood pressure regulation.
Normal ranges for blood pressure during pregnancy are less than 140/90 mmHg.Gestational hypertension is diagnosed when blood pressure is greater than or equal to 140/90 mmHg after 20 weeks of pregnancy and there is no proteinuria or other signs of preeclampsia.Gestational hypertension usually goes away after delivery, but it can increase the risk of complications for both the mother and the baby.
Exams on Gestational Hypertension
Custom Exams
Login to Create a Quiz
Click here to loginGestational Hypertension
Lessons
 Naxlex
Just Now
Naxlex
Just Now
Login to View Gestational Hypertension Study Video
Notes Highlighting is available once you sign in. Login Here.
Objectives
- Define gestational hypertension and its causes, risk factors and complications.
- Describe the signs and symptoms of gestational hypertension and how it is diagnosed.
- Explain the nursing interventions and management for gestational hypertension and its complications.
- Discuss the patient education and counseling for gestational hypertension and its prevention.
- Compare and contrast gestational hypertension with other types of hypertension during pregnancy.
- Evaluate the outcomes and prognosis of gestational hypertension for the mother and the fetus.
Introduction
- Gestational hypertension is a type of high blood pressure that develops after 20 weeks of pregnancy and goes away after delivery.
- High blood pressure is defined as a systolic pressure of 140 mmHg or higher or a diastolic pressure of 90 mmHg or higher.
- Gestational hypertension can affect the blood flow to the placenta and the fetus, leading to growth restriction, low birth weight, preterm delivery or stillbirth.
- Gestational hypertension can also increase the risk of preeclampsia, a serious condition that causes high blood pressure, proteinuria, edema and organ damage.
- Gestational hypertension can also increase the risk of maternal complications such as stroke, heart failure, kidney failure or placental abruption.
Causes and risk factors
- The exact cause of gestational hypertension is unknown, but it may be related to genetic factors, immune system dysfunction, placental abnormalities or vascular dysfunction.
- Some risk factors for developing gestational hypertension include:
- First pregnancy or new partner
- Age younger than 20 or older than 40
- Obesity or excessive weight gain
- Family history of hypertension or preeclampsia
- Multiple pregnancy (twins or more)
- Preexisting medical conditions such as diabetes, kidney disease or autoimmune disorders
- History of gestational hypertension or preeclampsia in previous pregnancies
Signs and symptoms
- Gestational hypertension may not cause any noticeable symptoms, so it is important to monitor blood pressure regularly during prenatal visits.
- Some signs and symptoms of gestational hypertension that may indicate worsening condition or preeclampsia include:
- Severe headache
- Vision changes such as blurring, flashing lights or spots
- Chest pain or shortness of breath
- Nausea or vomiting
- Abdominal pain or tenderness
- Swelling of the face, hands or feet
- Decreased urine output or protein in urine
Diagnosis and tests
- Gestational hypertension is diagnosed when blood pressure is 140/90 mmHg or higher on two occasions at least four hours apart after 20 weeks of pregnancy.
- Other tests that may be done to assess the condition of the mother and the fetus include:
- Urinalysis to check for proteinuria, which indicates kidney damage
- Blood tests to check for liver enzymes, platelets, creatinine and uric acid, which indicate organ damage
- Ultrasound to measure fetal growth and amniotic fluid volume
- Nonstress test or biophysical profile to monitor fetal heart rate and movements
Nursing interventions and Management
- The main goals of nursing interventions and management for gestational hypertension are to prevent complications, lower blood pressure and deliver a healthy baby.
- Some nursing interventions and management strategies include:
- Monitoring blood pressure, weight, urine output and proteinuria regularly
- Administering antihypertensive medications as prescribed, such as labetalol, nifedipine or methyldopa
- Administering magnesium sulfate as prescribed to prevent seizures in severe cases or preeclampsia
- Monitoring fetal well-being with ultrasound, nonstress test or biophysical profile
- Providing bed rest in a quiet and dark environment with left lateral position to improve blood flow to the placenta and reduce blood pressure
- Encouraging fluid intake of at least 2 liters per day to prevent dehydration and maintain renal function
- Restricting sodium intake to less than 2 grams per day to reduce fluid retention and edema
- Providing emotional support and reassurance to the mother and her partner
- Preparing for delivery when indicated by the provider, such as when blood pressure is uncontrollable, fetal distress occurs or term is reached
Patient education and counselling
- Patient education and counseling for gestational hypertension are essential to prevent complications, promote compliance and improve outcomes.
- Some patient education and counseling topics include:
- The causes, risk factors and complications of gestational hypertension and preeclampsia
- The signs and symptoms of worsening condition or preeclampsia that require immediate medical attention
- The importance of regular prenatal visits and blood pressure monitoring at home
- The medications prescribed for lowering blood pressure and preventing seizures, their dosages, side effects and interactions
- The lifestyle modifications such as bed rest, fluid intake, sodium restriction and stress management
- The delivery options such as induction of labor, cesarean section or vaginal birth after cesarean section (VBAC)
- The postpartum care such as breastfeeding, contraception and follow-up visits
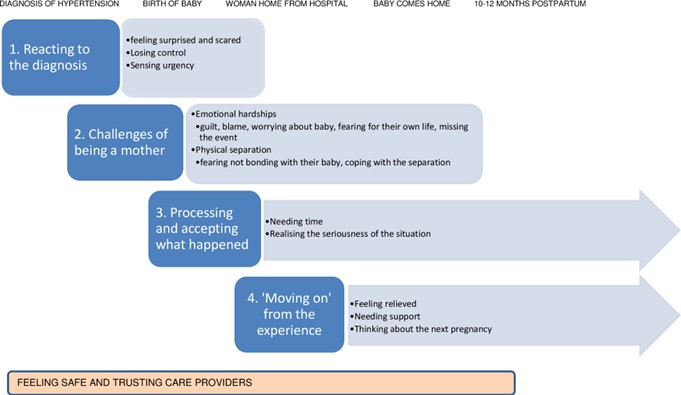
Comparison with other types of hypertension during pregnancy
Gestational hypertension is different from other types of hypertension during pregnancy in terms of onset, duration and complications.
The following table summarizes the differences between gestational hypertension and other types of hypertension during pregnancy:
|
Type |
Onset |
Duration |
Complications |
|
Gestational hypertension |
After 20 weeks |
Resolves after delivery |
Preeclampsia |
|
Chronic hypertension |
Before 20 weeks |
Persists after delivery |
Superimposed preeclampsia |
|
Preeclampsia |
After 20 weeks |
Resolves after delivery |
Eclampsia |
|
Eclampsia |
After 20 weeks |
Resolves after delivery |
HELLP syndrome |
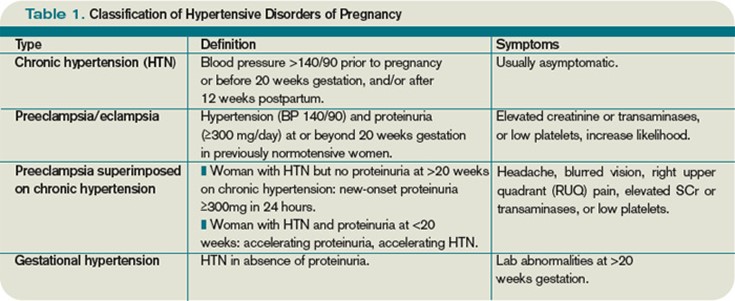
Outcomes and prognosis
- The outcomes and prognosis of gestational hypertension depend on the severity of the condition, the presence of complications and the timing of delivery.
- Most cases of gestational hypertension have good outcomes if managed properly with antihypertensive medications, magnesium sulfate and close monitoring.
- However, some cases may progress to preeclampsia, which can lead to life-threatening complications such as eclampsia (seizures), HELLP syndrome (hemolysis, elevated liver enzymes and low platelets) or placental abruption (separation of the placenta from the uterine wall).
- The best way to prevent these complications is to deliver the baby as soon as possible when indicated by the provider.
- The prognosis for the mother is usually good after delivery, but she may have an increased risk of developing chronic hypertension or cardiovascular disease later in life.
- The prognosis for the fetus depends on the gestational age at delivery, the fetal growth restriction and the presence of congenital anomalies^ ^.
- The fetus may have an increased risk of preterm birth, low birth weight, neonatal intensive care unit admission or perinatal mortality^ ^.
Summary
- Gestational hypertension is high blood pressure that develops after 20 weeks of pregnancy.
- It can affect the blood flow to the placenta and the fetus, leading to growth restriction, low birth weight or stillbirth.
- It can also increase the risk of preeclampsia, a serious condition that causes high blood pressure, proteinuria, edema and organ damage.
- It can also increase the risk of maternal complications such as stroke, heart failure or placental abruption.
- It is diagnosed when blood pressure is 140/90 mmHg or higher on two occasions at least four hours apart after 20 weeks of pregnancy.
- It is managed with antihypertensive medications, magnesium sulfate, bed rest, fluid intake, sodium restriction and close monitoring.
- It requires patient education on signs and symptoms that require immediate medical attention.
- It is different from other types of hypertension during pregnancy in terms of onset, duration and complications.
- It has good outcomes if managed properly but may progress to preeclampsia which can lead to life-threatening complications.
- It requires delivery when indicated by the provider to prevent complications.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Gestational Hypertension
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now