Please set your exam date
Sensation, perception, and cognition
Study Questions
Practice Exercise 1
Which client is at greatest risk for experiencing sensory overload?
Explanation
Sensory overload occurs when a client is exposed to excessive stimuli that the brain cannot effectively process, while sensory deprivation occurs when stimuli are reduced or absent. Recognizing the difference is important in providing a supportive environment for clients at risk.
Rationale for correct answer:
4. An 80-year-old client admitted for emergency surgery: This client is at greatest risk for sensory overload because of the sudden admission, pain, multiple diagnostic tests, consent forms, and the stressful hospital environment with limited time for orientation.
Rationale for incorrect answers:
1. A 40-year-old client in isolation with no family: At risk for sensory deprivation because of reduced stimulation and social contact, not overload.
2. A 28-year-old quadriplegic client in a private room: Also at risk for sensory deprivation due to immobility, limited interaction, and minimal environmental input.
3. A 16-year-old listening to loud music: This is a normal activity for a teenager; while it may increase stimulation, it does not necessarily indicate overload in this age group.
Take home points:
- Sensory overload happens when there is too much stimulation, while sensory deprivation results from too little stimulation.
- Nurses should assess the client’s environment and health status to balance sensory input and maintain comfort and orientation.
A client is at risk for sensory deprivation. Which of the following clinical signs would the nurse observe? Select all that apply
Explanation
Clinical manifestations of sensory deprivation occurs when a client receives too little meaningful stimulation. Lack of input can negatively affect cognition, mood, and behavior, leading to changes in sleep, concentration, and emotional stability.
Rationale for correct answer:
2. Decreased attention span: Without adequate sensory input, clients may have trouble focusing, thinking clearly, or following conversations, as the brain lacks sufficient stimulation to stay engaged.
4. Excessive sleeping: Some clients respond to sensory deprivation by withdrawing and sleeping more than usual as a way to escape monotony.
5. Crying, depression: Emotional changes such as sadness, tearfulness, and depression are common in clients who are deprived of normal social and sensory input.
Rationale for incorrect answers:
1. Sleeplessness: A lack of normal stimulation can disrupt circadian rhythms, causing restlessness at night and difficulty sleeping.
3. Irritability: It can result from excessive stimuli that overwhelm the brain, leading to agitation and difficulty coping.
Take home points:
- Sensory deprivation affects sleep, cognition, mood, and emotional well-being; nurses must recognize this wide spectrum of symptoms.
- Early recognition and providing adequate stimulation (e.g., communication, activities, meaningful interaction) can prevent complications like depression and disorientation.
The nurse is assessing for sensory function. Match the assessment tool to the specific sense it will be testing.
|
|
|
|
Identifying taste Stereognosis Snellen chart Identifying aromas Tuning fork |
dropdown
dropdown
dropdown
dropdown
dropdown
|
Explanation
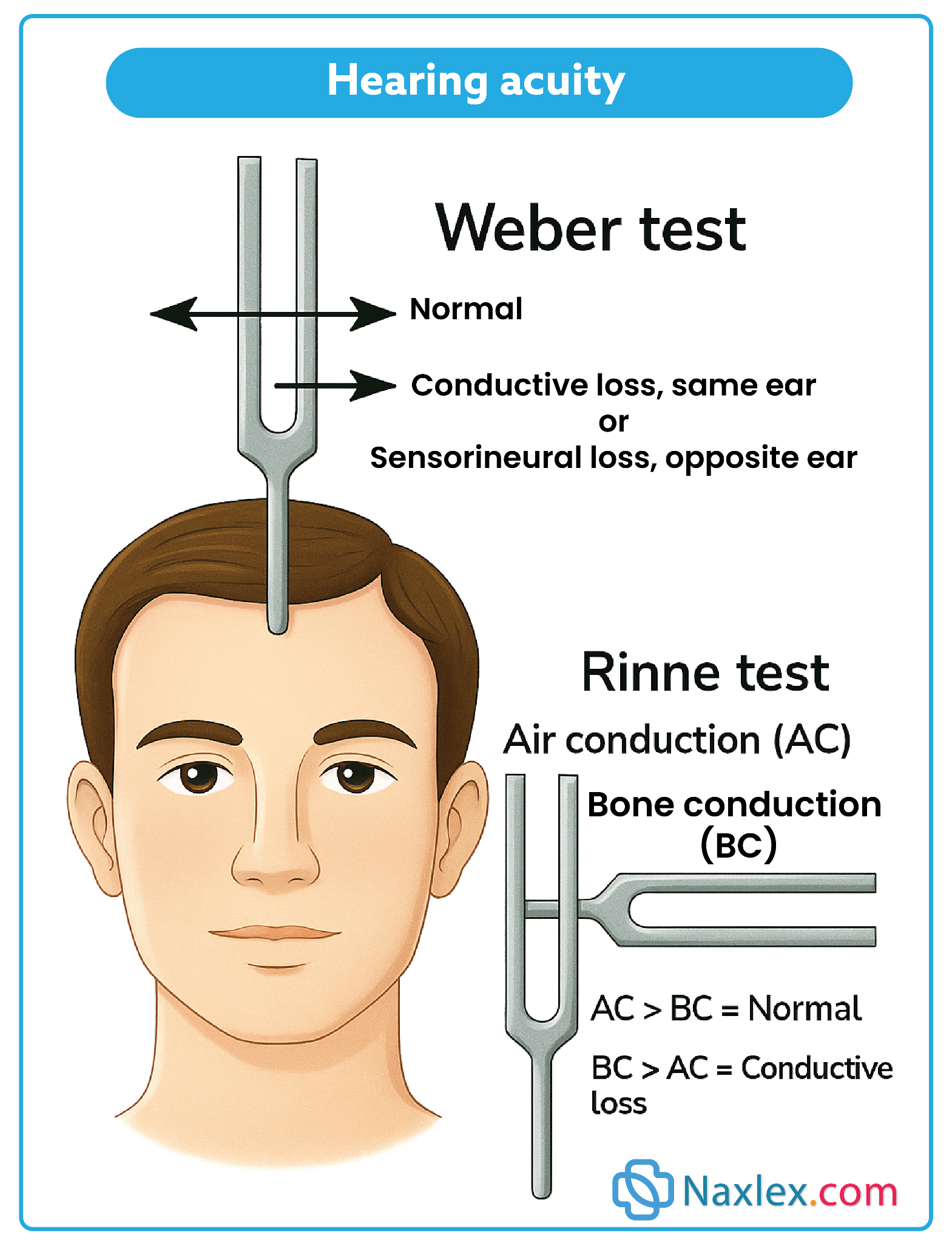
This question is assessing the nurse’s knowledge of neurological and sensory function assessments. Each tool or activity is designed to evaluate a specific sensory pathway- vision, hearing, tactile perception, olfaction, or taste - which is essential for detecting deficits and planning interventions.
Rationale for correct answer:
Identifying taste → Gustatory (5): The gustatory sense involves taste perception. Asking a client to identify flavors such as sweet, salty, or sour tests cranial nerves VII (facial) and IX (glossopharyngeal).
Stereognosis → Tactile (3): Stereognosis is the ability to identify an object placed in the hand (like a key or coin) without visual input. This assesses tactile sensation and cortical integration.
Snellen chart → Visual (1): The Snellen chart measures visual acuity by having clients read letters at a distance, assessing cranial nerve II (optic nerve).
Identifying aromas → Olfactory (4): Asking the client to recognize smells such as coffee or peppermint evaluates the olfactory sense, which tests cranial nerve I (olfactory nerve).
Tuning fork → Hearing (2): A tuning fork is used for auditory assessments such as the Rinne or Weber test, which evaluate air and bone conduction and test cranial nerve VIII (vestibulocochlear).
Take-home points:
- Each sensory assessment is linked to a specific cranial nerve and pathway, making accurate tool selection essential for neurological exams.
- Nurses should know how to differentiate sensory modalities (visual, hearing, tactile, olfactory, gustatory) to detect deficits early and intervene appropriately.
When assessing a patient’s sensory experience, which of the following would the nurse identify as the major components?
Explanation
Sensory functioning involves more than identifying the different senses or the qualities of stimuli—it depends on two essential stages: reception, where receptors detect and transmit stimuli, and perception, where the brain organizes and interprets those signals into meaningful information. Nurses assessing sensory function must evaluate both of these aspects to determine whether a client has deficits in detecting stimuli, interpreting them, or both.
Rationale for correct answer:
2. Reception and perception: Reception (detection of stimuli by receptors and transmission to the nervous system) and perception (interpretation and conscious awareness of those stimuli) are the major process components of sensory experience.
Rationale for incorrect answers:
1. The kinesthetic and visceral senses: These are types or modalities of sensation (kinesthetic = proprioception, visceral - internal organ sensation). They describe what is sensed, not the fundamental components of the sensory process.
3. The intensity, size, change, or representation of stimuli: These are characteristics of stimuli that influence sensation and perception, but they are not the primary components of the process itself.
4. Vision, hearing, smell, taste, and touch: These are the main sensory modalities, but they are examples of senses rather than the basic components of sensory experience.
Take home points:
- The two major components of sensory experience are reception and perception.
- In practice, a thorough sensory assessment requires checking both the ability to detect stimuli and the ability to interpret them correctly.
When evaluating a patient’s sensory experience, which four conditions would be essential for a person to receive data and experience the world?
Explanation
In order for a person to meaningfully interact with the environment, four conditions must be present: a stimulus to trigger the sense, receptors to detect it, intact neural pathways to carry the message, and a functioning brain to interpret the signal. Without any one of these, sensory perception becomes impaired.
Rationale for correct answer:
1. A stimulus, a receptor, an intact nerve pathway, and a functioning brain: These are the four essential conditions required for a person to receive sensory data. Without a stimulus, there is nothing to detect; without receptors, detection cannot occur; without intact pathways, the message cannot reach the brain; and without a functioning brain, perception and interpretation are impossible.
Rationale for incorrect answers:
2. The visual, auditory, olfactory–gustatory, and tactile senses: These are examples of the types of senses a person may have, but they are not the necessary conditions for sensory experience to occur.
3. The basic orienting systems arising from muscles, joints, hollow organs, and movement: These refer to kinesthetic and visceral senses, which are part of the sensory system, but they are not the foundational requirements for receiving and processing stimuli.
4. The reticular activating system, variable stimuli, memory, and motivation: The reticular activating system (RAS) influences arousal and awareness, and memory and motivation affect how experiences are processed and recalled, but these are not the essential baseline conditions for sensory reception and perception.
Take home points:
- Sensory experience depends on stimulus, receptor, intact pathway, and functioning brain- disruption of any of these impairs perception.
- Nurses must assess not just the sense organs but also the neurological pathways and cognitive functioning to get a full picture of a patient’s sensory health.
Practice Exercise 2
The nursing diagnosis Risk for Impaired Skin Integrity related to sensory-perception disturbance would best fit a client who:
Explanation
Sensory-perception disturbances prevent clients from recognizing or responding to potential injury. Sensory-perceptual deficits increase the risk of burns, wounds, and pressure injuries because the client may not feel pain, temperature, or pressure appropriately.
Rationale for correct answer:
2. Uses a wheelchair due to paraplegia: Because of paralysis, the client lacks sensation in the lower body and cannot feel discomfort from prolonged pressure. This makes them at risk for impaired skin integrity from pressure ulcers.
Rationale for incorrect answers:
1. Cut a foot by stepping on broken glass: This is an actual problem (a wound), not a potential risk and it is not directly linked to sensory-perceptual disturbance.
3. Wears glasses because of poor vision: Glasses correct the visual deficit, so the client is not at increased risk.
4. Is legally blind and smokes in bed: This situation fits Risk for Injury, since blindness plus smoking creates risk for burns, but it is not specifically related to skin integrity from sensory-perception disturbance.
Take home points:
- Match nursing diagnoses to the defining risk factor.
- Differentiate between actual problems and potential problems-risk diagnoses are about prevention, not existing conditions.
Which statement indicates the client needs a sensory aid in the home?
Explanation
A nurse should have the ability to identify clients with sensory deficits who would benefit from assistive devices to improve safety and independence. Hearing and vision impairments are common in older adults, and recognizing early cues helps prevent accidents and support daily functioning.
Rationale for correct answer:
2. “I can’t hear the doorbell.” This indicates a hearing deficit, and the client would benefit from a sensory aid such as a flashing light doorbell or hearing assistive device.
Rationale for incorrect answers:
1. “I tripped over that throw rug again.” This reflects a safety hazard, but it does not directly point to a sensory deficit. Removing the rug would address the problem, not a sensory aid.
3. “My eyesight is good if I wear my glasses.” The sensory deficit is already corrected with glasses, so no new aid is required.
4. “I can hear the TV if I turn it up high.” This suggests mild hearing loss but doesn’t necessarily confirm the need for a sensory aid, since volume adjustment may be sufficient.
Take-home points:
- Look for statements that show uncorrected sensory loss (e.g., can’t hear, can’t see) when deciding if a client needs an aid.
- Corrected impairments (like wearing glasses) don’t indicate a new aid is needed.
A client with impaired vision is admitted to the hospital. Which interventions are most appropriate to meet the client’s needs? Select all that apply
Explanation
When making environmental adjustments for clients with visual impairment, the goal is to maximize safety, orientation, and comfort by adapting care to meet sensory needs.
Rationale for correct answer:
1. Identify yourself by name: A client with impaired vision relies more on hearing, so naming yourself establishes trust, prevents confusion, and reassures the client.
3. Stay in the client’s field of vision: Clients with impaired vision may not see well even if you are in their field of vision; instead, verbal cues and safe environmental arrangements are more helpful.
4. Explain the sounds in the environment: Unfamiliar sounds may cause anxiety for visually impaired clients. Explaining what is happening (e.g., alarms, staff movement) helps orient and reassure them.
Rationale for incorrect answers:
2. Decrease background noise before speaking: This intervention is more appropriate for hearing-impaired clients, as vision loss does not affect auditory processing.
5. Keep your voice at the same level throughout the conversation: Visual impairment does not affect hearing, so altering or maintaining voice level is unnecessary; clarity and descriptive explanations are more effective.
Take home points:
- Safety and orientation are the priorities for visually impaired clients- use clear communication and explanations.
- Avoid confusing interventions intended for hearing-impaired clients, such as lowering noise or altering voice level.
An 85-year-old client has impaired hearing. When creating the care plan, which intervention should have the highest priority?
Explanation
Hearing loss can lead to social isolation, miscommunication, and safety risks, so the nurse must select interventions that most directly enhance the client’s ability to communicate and interact effectively.
Rationale for correct answer:
1. Obtaining an amplified telephone: This intervention directly supports communication, social interaction, and safety (e.g., ability to call for help in emergencies). It is the highest priority because it addresses the client’s immediate functional needs.
Rationale for incorrect answers:
2. Teaching the importance of changing his position: Position changes help with circulation or mobility but are unrelated to hearing impairment.
3. Providing reading material with large print: This supports vision, not hearing. While useful for visually impaired clients, it does not address the specific problem here.
4. Checking expiration dates on food packages: This is more relevant for clients with vision or memory deficits. It does not directly meet the needs of someone with impaired hearing.
Take home points:
- When prioritizing interventions, always choose the one that directly addresses the client’s primary deficit or risk-in this case, communication for hearing loss.
- Assistive devices such as amplified phones or hearing aids are critical in maintaining independence, safety, and quality of life for older adults with hearing impairments.
Which of the following would be most important to include in the plan of care for a patient who is 85 years old and has presbycusis?
Explanation
Presbycusis is the age-related loss of hearing, especially for high-pitched sounds. The key nursing intervention is to adapt communication methods, such as lowering vocal pitch, speaking clearly, and ensuring face-to-face conversation. These measures improve the patient’s ability to process auditory input, promote interaction, and reduce frustration or social withdrawal.
Rationale for correct answer:
2. Speaking distinctly using lower frequencies: Presbycusis is a gradual sensorineural hearing loss associated with aging, particularly affecting the ability to hear high-frequency sounds. Speaking clearly at a lower pitch and moderate pace enhances communication.
Rationale for incorrect answers:
1. Obtaining large-print written material: This intervention addresses visual impairment, not presbycusis (age-related hearing loss).
3. Decreasing tactile stimulation: Tactile input is not related to presbycusis and decreasing it may increase isolation.
4. Initiating a safety program to prevent falls: Although fall prevention is essential for older adults, it is not the most specific or direct intervention for presbycusis.
Take home points:
- Presbycusis primarily impairs the ability to hear high-frequency sounds.
- Nurses should communicate using lower-pitched, clear speech to support older patients with this condition.
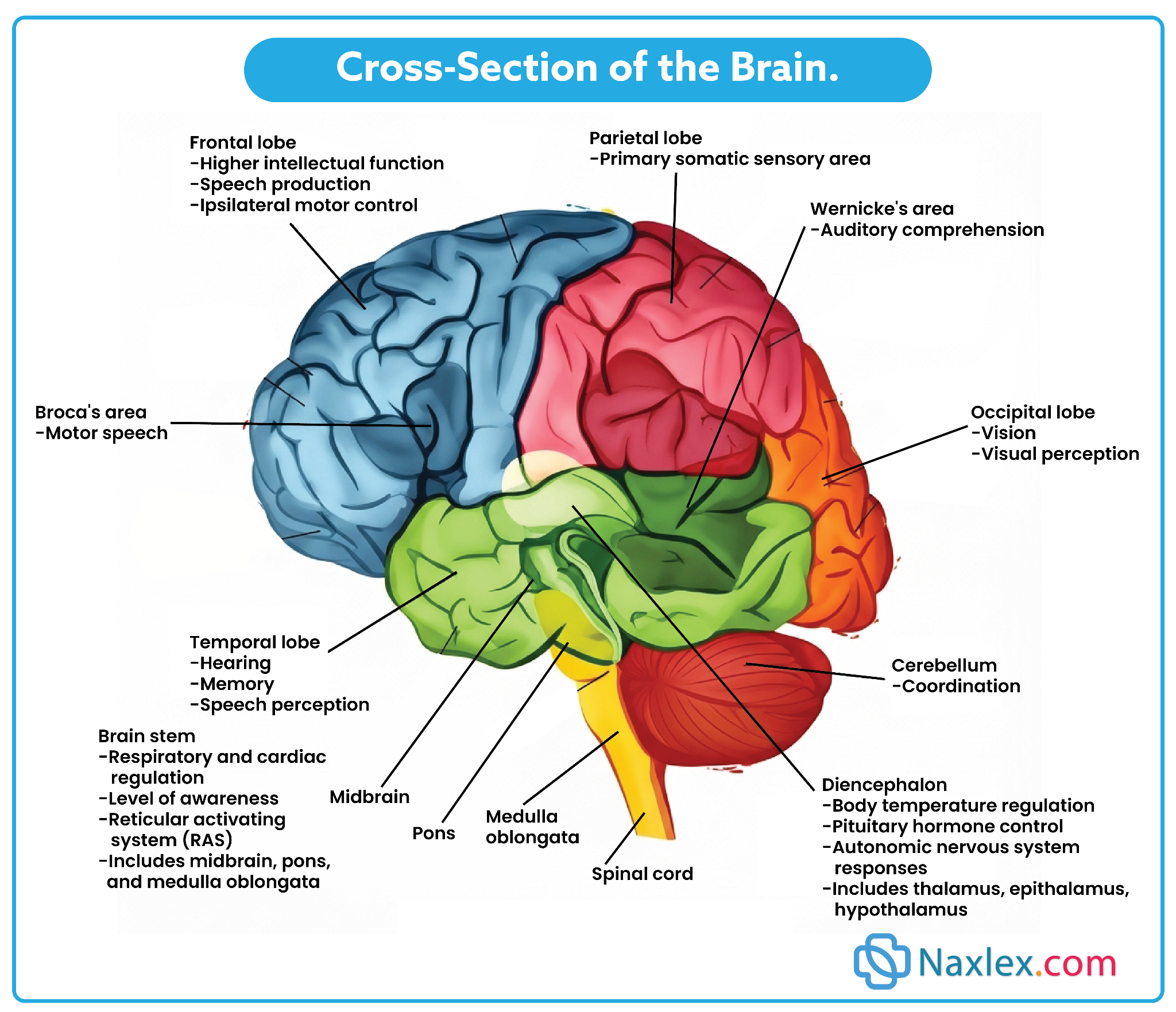
An older adult with pneumonia is admitted from a skilled nursing home to a medical unit. A review of the medical record reveals that he had a stroke affecting the right hemisphere of the brain 6 months ago and was placed in the skilled nursing home because he was unable to care for himself. Which of these assessment findings does the nurse expect to find? Select all that apply
Explanation
A stroke in the right hemisphere typically causes left-sided deficits such as neglect and visual-spatial problems (hemianopsia, depth perception issues). Right-brain damage is also associated with impulsivity and poor judgment. In contrast, left hemisphere strokes cause right-sided motor deficits and cautious, slow behaviors. Differentiating between left- and right-brain stroke effects is essential for accurate assessment and safe care.
Rationale for correct answers:
2. Inattention and neglect, especially to the left side: Right hemisphere strokes commonly cause left-sided neglect (the patient ignores or is unaware of the left side of the body/environment).
4. Visual spatial alterations such as loss of half of a visual field: Right hemisphere damage often results in left homonymous hemianopsia, where the patient loses vision in the left half of the visual field in both eyes.
Rationale for incorrect answers:
1. Slow, cautious behavioral style: This is more typical of left hemisphere stroke, where patients are often slow, cautious, and hesitant. Right hemisphere stroke patients are more likely to be impulsive and lack judgment.
3. Cloudy or opaque areas in part of the lens or the entire lens: This describes cataracts, an age-related eye disorder, not a direct effect of stroke.
5. Loss of sensation and motor function on the right side of the body: Right hemisphere strokes cause left-sided motor and sensory deficits, because the motor pathways cross over in the brainstem.
Take home points
- Right hemisphere stroke = left-sided neglect, visual-spatial deficits, impulsivity.
- Left hemisphere stroke = right-sided weakness, cautious behavior, language deficits (aphasia).
Practice Exercise 3
An alert 80-year-old client is transferred to a long-term care facility. On the second night, he becomes restless and agitated. What is the most appropriate nursing diagnosis?
Explanation
Older adults in new environments often experience acute confusion (delirium) due to sudden changes, stress, and disorientation. The transfer to a different setting can change the amount or patterning of incoming stimuli accompanied by a diminished, exaggerated, distorted, or impaired response to such stimuli. Recognizing the difference between delirium, dementia, and other thought disturbances is key for accurate nursing diagnoses and interventions.
Rationale for correct answer:
3. Acute Confusion: The sudden onset of agitation and restlessness after a transfer suggests delirium, a temporary and reversible condition often triggered by environmental change, hospitalization, or acute illness.
Rationale for incorrect answers:
1. Chronic Confusion: Chronic confusion refers to dementia or long-term irreversible decline, which is not supported since the client was alert before transfer.
2. Impaired Memory: This would imply difficulty recalling past events or new information, but the main issue here is sudden restlessness and agitation, not memory loss.
3. Disturbed Thought Processes: This diagnosis relates more to long-term psychiatric or neurological issues affecting reasoning or perception, not the sudden change seen here.
Take-home points:
- Acute confusion (delirium) is characterized by sudden onset, fluctuating course, and is usually reversible if the cause is addressed.
- Nurses must differentiate acute confusion from chronic confusion (dementia) to ensure timely intervention and prevent complication.
A hospitalized client is disoriented and believes she is in a train station. Which response from the nurse is the most appropriate?
Explanation
When applying therapeutic communication in reality orientation, nurses must acknowledge a client’s feelings while gently re-orienting them to person, place, and time. Confrontation or ridicule increases anxiety and worsens disorientation.
Rationale for correct answer:
4. “It may seem like a train station sometimes, but this is Valley Hospital.” This acknowledges the client’s perception while gently reorienting them to reality.
Rationale for incorrect answers:
1. “You wouldn’t be getting a bath at the train station.” This is dismissive and confrontational, which may increase confusion and agitation.
2. “Let’s finish your bath before the train arrives.” This reinforces the delusion rather than reorienting the client to reality.
3. “Don’t you know where you are?” This is scolding and non-therapeutic; it shames the client instead of supporting them.
Take-home points:
- Best communication with disoriented clients- validate feelings and reorient to reality.
- Avoid responses that are confrontational, sarcastic, or that reinforce delusions.
A client is exhibiting signs and symptoms of acute confusion/ delirium. Which strategy should the nurse implement to promote a therapeutic environment?
Explanation
In environmental management for clients with delirium (acute confusion), the goal is to reduce disorientation and agitation by providing a calm, structured, and supportive setting. A disorganized, cluttered environment increases confusion.
Rationale for correct answer:
3. Keep the room organized and clean: A tidy, clutter-free, and consistent environment decreases confusion, prevents accidents, and supports reorientation for clients with delirium.
Rationale for incorrect answers:
1. Keep lights in the room dimmed during the day to decrease stimulation: Dim lighting can worsen disorientation, especially during the day when natural light helps maintain orientation to time.
2. Keep the environmental noise level high to increase stimulation: Excessive noise increases agitation, worsens confusion, and contributes to sensory overload in delirious clients.
4. Use restraints for client safety: Restraints increase agitation and confusion, are a last-resort intervention, and do not promote a therapeutic environment.
Take home points:
- Clients with delirium benefit most from a calm, structured, and organized environment to reduce confusion and agitation.
- Avoid interventions that increase disorientation (dim lights, noise, restraints), and instead promote orientation through environmental consistency.
In a boarding home where most patients have slight to moderate visual or hearing impairment and some are periodically confused, which of the following would be the nurse’s first priority in caring for sensory concerns?
Explanation
Safety is the immediate, overarching nursing priority (Maslow’s hierarchy- physiological/safety needs first). In a boarding home where many residents have visual/hearing impairments and intermittent confusion, the greatest risk is injury, falls, accidents, or worsening sensory loss from lack of aids or unsafe environment. Preventing further sensory deterioration both protects residents now and preserves function long-term.
Rationale for correct answer:
1. Maintaining safety and preventing sensory deterioration: Focuses on immediate risk reduction (falls, accidents, miscommunication) and on preserving residual senses by ensuring assistive devices, safe environment, and appropriate sensory stimulation or protection. These actions reduce harm and enable later rehabilitation or psychosocial interventions.
Rationale for incorrect answers:
2. Insisting that every patient participate in as many self-care activities as possible: Promoting independence is important for function and dignity, but “insisting” ignores individual ability, safety and cognitive status. Encouragement and graded participation after safety/assessment are appropriate, but forcing participation could increase risk of harm.
3. Emphasizing and reinforcing individual patient strengths: Strength-based approaches support self-esteem, motivation and engagement in care, and help with adaptation to sensory loss. However, they don’t address immediate safety risks and should follow or run alongside core safety measures.
4. Encouraging reminiscence and life review in groups: Group reminiscence promotes socialization, orientation and emotional well-being (especially for those with cognitive changes), but it’s an intervention for psychosocial health rather than immediate safety. It’s appropriate once the environment and sensory needs are secure.
Take home points:
- Safety first: always prioritize interventions that reduce immediate risk and preserve residual senses.
- Use strength-based supports and psychosocial activities tailored to each resident’s sensory/cognitive ability to maximize independence and quality of life.
Comprehensive Questions
When planning the care for a patient related to disturbed sensory perception, the nurse would integrate knowledge of which system as responsible for monitoring and regulating incoming sensory stimuli to maintain, enhance, or inhibit cortical arousal?
Explanation
The role of the reticular activating system (RAS) in sensory processing- it acts as a filter and regulator of sensory stimuli, preventing sensory overload or deprivation by controlling which stimuli reach conscious awareness. In nursing practice, understanding the RAS is crucial when planning interventions for patients with disturbed sensory perception, such as those experiencing confusion, delirium, or sensory deprivation.
Rationale for correct answer:
3. Reticular activating system: The RAS, located in the brainstem, is responsible for mediating arousal and regulating the amount and quality of sensory input that reaches the cerebral cortex, ensuring the brain is neither overloaded nor deprived.
Rationale for incorrect answers:
1. General adaptation system: This system relates to the body’s physiological response to stress (fight-or-flight) and is not primarily responsible for sensory arousal.
2. Kinesthetic/visceral system: This relates to awareness of body position and internal organ sensation, not to the regulation of cortical arousal.
4. Sensory/perceptual system: This refers generally to the senses (vision, hearing, taste, smell, touch) but does not specifically regulate cortical arousal.
Take home points:
- The RAS is the key regulator of sensory input and cortical arousal.
- Nurses must manage the patient’s environment to ensure appropriate stimulation-neither too much nor too little.
You notice that Mr. Wong, who has cataracts, is sitting closer to the television than usual. The nurse would interpret the etiologic basis of his sensory problem is an alteration in which of the following?
Explanation
Cataracts affect the lens of the eye, leading to blurred vision because light cannot properly reach the retina. This is a classic example of an alteration in sensory reception, not in neural conduction or cortical interpretation. Nurses should recognize signs such as moving closer to objects or straining to see as indicators of impaired sensory reception.
Rationale for correct answer:
2. Sensory reception: Cataracts cause clouding of the lens, which interferes with the reception of visual stimuli at the sensory organ level (the eye). Thus, the sensory receptor (eye structures) is impaired.
Rationale for incorrect answers:
1. Environmental stimuli: The problem is not due to the absence of stimuli in the environment (the television still provides adequate visual input), but rather the patient’s inability to receive it clearly.
3. Nerve impulse conduction: The optic nerve and conduction pathways remain intact; the problem lies before conduction occurs.
4. Impulse translation: The brain’s ability to interpret stimuli (translation/perception) is not affected; the problem is at the level of input reception.
Take home points:
- Cataracts impair sensory reception at the level of the lens, not nerve conduction or brain processing.
- Observing patient behavior (e.g., sitting closer to the TV) provides important clues to underlying sensory deficits.
Peter Almone is in the late stages of AIDS, which is now affecting his brain as well other major organ systems. He confides to you that he feels terribly alone because most of his friends are afraid to visit. The nurse determines that which of the following would be the least likely underlying etiology for his sensory problems?
Explanation
There is a multifactorial nature of sensory problems in serious illness. In late-stage AIDS, neurological involvement, emotional distress, and impaired perception can all contribute to sensory changes. However, lack of stimulation is the least likely underlying factor since the problem arises more from internal disease processes and psychological effects rather than a complete absence of environmental input.
Rationale for correct answer:
4. Emotional responses: While emotional changes (such as feeling lonely, sad, or anxious) are effects of sensory deprivation, they are not the underlying etiology. They result from the problem rather than cause it.
Rationale for incorrect answers:
1. Stimulation: Peter is receiving decreased environmental stimuli (friends not visiting), so lack of stimulation is a likely contributing factor.
2. Reception: AIDS with multi-organ involvement can affect sensory reception, making this another likely cause.
3. Transmission-perception-reaction: Impaired brain function from AIDS will directly interfere with impulse transmission, perception, and reaction.
Take home points:
- Etiologies of sensory problems are primarily related to stimulation, reception, and transmission-perception-reaction.
- Emotional responses are consequences of sensory deprivation, not underlying causes.
Which factor is least likely to place a patient at high risk for sensory deprivation?
Explanation
Sensory deprivation, occurs when a person cannot receive, process, or is not exposed to sufficient stimuli. Although impaired response affects communication, it does not directly limit sensory input. Therefore, the greatest risks come from reduced stimulation, impaired reception, or impaired processing of stimuli.
Rationale for correct answer:
4. Impaired ability to respond to environmental stimuli: While this may affect interaction, it does not directly reduce the patient’s reception or perception of stimuli. The patient still receives and processes input, making this the least likely factor for deprivation.
Rationale for incorrect answers:
1. An environment with decreased or monotonous stimuli: A lack of varied sensory input (e.g., isolated hospital room, long-term care facility) is a major risk factor for sensory deprivation.
2. Impaired ability to receive environmental stimuli: Deficits such as hearing or vision loss reduce sensory input and increase risk for deprivation.
3. Impaired ability to process environmental stimuli: Neurological conditions (e.g., brain injury, dementia) limit the brain’s ability to interpret stimuli, leading to sensory deprivation.
Take home points:
- Sensory deprivation arises mainly from lack of stimulation, impaired reception, or impaired processing.
- Impaired ability to respond is a secondary factor, not a primary cause of deprivation.
Which patient would the nurse assess as being at greatest risk for sensory deprivation?
Explanation
When identifying patients most vulnerable to sensory deprivation, the elderly stroke patient confined at home has reduced mobility, decreased environmental interaction, and possible neurological impairment, putting him at highest risk. By contrast, patients engaged with peers, experiencing acute stimulation, or in enriched environments have lower risk.
Rationale for correct answer:
1. An elderly man confined to bed at home after a stroke: This patient is at highest risk because he is immobile, isolated, and has potential neurological deficits from the stroke that impair reception and processing of stimuli.
Rationale for incorrect answers:
2. An adolescent in an oncology unit working on homework supplied by friends: Despite hospitalization, this patient has ongoing stimulation through schoolwork and peer interaction, reducing risk of deprivation.
3. A woman in labor: Labor provides intense and varied sensory stimulation, not deprivation.
4. A toddler in a playroom awaiting same-day surgery: Although awaiting surgery, the toddler is in a stimulating environment (playroom) that provides adequate sensory input.
Take home points:
- Isolation, immobility, and neurological impairment are the strongest predictors of sensory deprivation.
- Patients in stimulating environments (social or physical) are less likely to experience deprivation, even if hospitalized.
A patient in an intensive care burn unit for 1 week is in pain much of the time and has his face and both arms heavily bandaged. His wife visits every evening for 15 minutes at 6, 7, and 8 PM. A heart monitor beeps for a patient on one side, and another patient moans frequently. Assessment would suggest that that the patient probably is experiencing which of the following?
Explanation
Sensory overload, a common risk in intensive care settings. Continuous noise, alarms, pain, and emotional distress can overwhelm the nervous system, leading to agitation, confusion, or withdrawal. Nurses play a crucial role in modifying the environment-reducing noise, clustering care, and promoting supportive family presence-to help restore balance.
Rationale for correct answer:
4. Both sensory deprivation and overload: This patient’s bandages may result in deficient sensory stimulation (sensory deprivation), and the monitors and other sounds in the intensive care burn unit may cause a sensory overload.
Rationale for incorrect answers:
1. Sufficient sensory stimulation: The patient is not in balance; he is overwhelmed by constant noise, pain, and stress.
2. Deficient sensory stimulation: Although bandages limit tactile input and visits are brief, the overall environment is not deprived but instead overloaded.
3. Excessive sensory stimulation: The combination of persistent pain, constant auditory stimuli (beeping monitor, moaning patient), and a stressful ICU environment results in sensory overload. However, this patient’s bandages may result in deficient sensory stimulation.
Take home points:
- ICU environments often cause sensory overload due to constant stimuli and stress.
- Nurses must reduce unnecessary noise and promote structured support to protect patients’ sensory well-being.
Richard’s spinal cord was severed, and he is paralyzed from the waist down. When obtaining data about this patient, which component of the sensory experience would be most important to assess?
Explanation
The importance of assessing transmission in spinal cord injuries- although receptors in the skin and muscles below the waist may still detect stimuli, the severed cord prevents those signals from reaching the brain. The nurse’s role is to monitor the extent of sensory and motor loss and to implement safety measures to prevent injury to insensate areas.
Rationale for correct answer:
1. Transmission of tactile stimuli: With a severed spinal cord, the major concern is whether tactile (touch, pressure, pain, temperature) stimuli can be transmitted from below the injury site to the brain. Transmission is the key component affected.
Rationale for incorrect answers:
2. Adequate stimulation in the environment: The environment may be stimulating, but the problem lies in the patient’s ability to transmit signals from receptors below the injury level.
3. Reception of visual and auditory stimuli: These senses are intact since the injury affects only lower spinal cord function.
4. General orientation and ability to follow commands: Orientation and cognition are not impaired by the spinal cord injury.
Take home points:
- In spinal cord injury, the critical issue is impaired transmission of sensory stimuli, not reception or cognition.
- Care planning must focus on protection from injury and compensatory strategies for sensory loss.
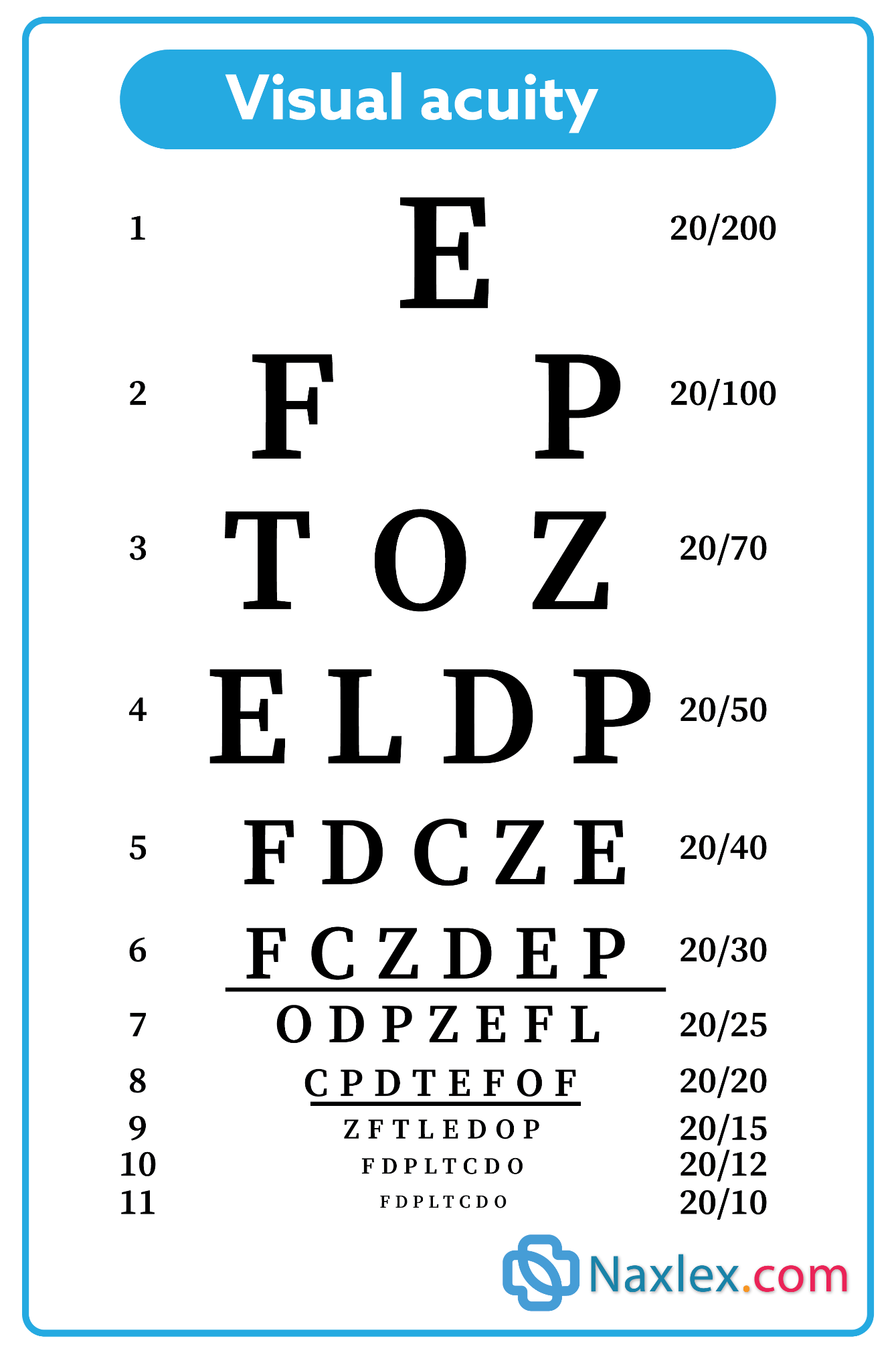
An 11-year-old 6th grader whose grades have dropped has difficulty completing her work on time, frequently rubs her eyes, and squints. Her visual acuity on a Snellen’s eye chart was 160/20. Which nursing diagnosis would be most appropriate?
Explanation
Visual deficits can impair a child’s academic and social roles. In this case, poor vision (160/20) is preventing her from effectively completing her role as a student, evidenced by declining grades, eye rubbing, and squinting. The nursing diagnosis should directly connect the impairment to her most affected role rather than unrelated areas such as body image or growth.
Rationale for correct answer:
2. Ineffective Role Performance (Student) related to visual impairment: The primary problem is that her visual deficit is interfering with her ability to carry out her main developmental role-functioning successfully as a student.
Rationale for incorrect answers:
1. Deficient Knowledge related to visual impairment: The issue is not that the child lacks knowledge about her condition, but rather that her school performance is being directly affected by the impairment.
3. Disturbed Body Image related to visual impairment: There is no indication that she feels negatively about her appearance or body image.
4. Delayed Growth and Development related to visual impairment: There is no evidence that her overall growth or developmental milestones are delayed; the problem is specifically linked to academic performance.
Take home points:
- Nursing diagnoses should be specific to the area most impacted by the sensory impairment.
- In children, vision problems often manifest as academic decline and role performance issues before they are formally diagnosed.
Of the four items listed below, which nursing intervention would be best to prevent sensory alterations for a man with a severe hearing deficit who reads lips well?
Explanation
Social engagement is the best preventive measure for sensory deprivation in patients with hearing loss. Since the patient reads lips well, structured opportunities for socialization in small groups will help maintain his orientation, prevent isolation, and preserve cognitive and emotional well-being.
Rationale for correct answer:
3. Provide daily opportunity for him to participate in a social hour with six or eight people: Social interaction provides meaningful stimulation, prevents isolation, and supports his ability to lip-read, which compensates for his hearing deficit.
Rationale for incorrect answers:
1. Turn the radio or television volume up very loud and close the door to his room: This increases noise but does not provide meaningful interaction or help with lip reading. It may actually cause frustration and isolation.
2. Prevent embarrassment and emotional discomfort as much as possible: While supportive, this is too vague and does not actively address the prevention of sensory deprivation.
4. Encourage daily participation in exercise and physical activity: Exercise is beneficial for overall health but does not specifically prevent sensory alterations linked to hearing loss.
Take home points:
- For patients with sensory impairments, social interaction is a powerful intervention to prevent sensory deprivation.
- Nursing care should build on the patient’s strengths (lip reading) to maintain quality of life and reduce isolation.
The nursing diagnosis for 8-month-old Sally was Disturbed Sensory Perception: Sensory Deprivation related to inadequate parenting. Since that time, both parents have attended parenting classes. However, both parents work while Sally stays with her 86-year-old grandmother, who has reduced vision. The parents provide appropriate stimulation in the evening. At an evaluation conference at age 11 months, Sally lays on the floor sucking her thumb and rocking her body. Her facial expression is dull, and she vocalizes only in a low monotone (“uh-h-h”). Which statement accurately reflects evaluation about the child’s sensory deprivation?
Explanation
Adequate sensory stimulation (visual, auditory, tactile, and social) is critical for normal growth and development. Infants deprived of such input may develop maladaptive behaviors like rocking, thumb-sucking, monotone vocalizations, and lack of responsiveness. Evaluation must focus on the child’s current status rather than caregiver intentions. Early identification and intervention are crucial to prevent developmental delays.
Rationale for correct answer:
3. Sally’s sensory deprivation is still severe: Sally’s rocking, dull facial expression, and monotone vocalizations at 11 months indicate significant ongoing deprivation. At this age, infants should be engaging socially, showing curiosity, babbling with varied sounds, and interacting with their environment. The behaviors described are maladaptive responses to lack of adequate stimulation.
Rationale for incorrect answers:
1. Her parents lack motivation to provide necessary stimulation: The parents have demonstrated motivation by attending parenting classes and providing stimulation when they are available. The issue lies more in the adequacy and consistency of stimulation throughout the day, not in motivation.
2. Her grandmother is unable to improve Sally’s care: While the grandmother’s poor vision may limit her ability to give sufficient sensory input, this choice places blame rather than assessing Sally’s condition. The focus of evaluation should be on the child’s ongoing deprivation.
4. This is normal behavior for a child of Sally’s age: At 11 months, normal infants are mobile (crawling or trying to walk), actively exploring, showing social smiles, and producing multiple sounds. Rocking with a dull affect and low monotone sounds is not developmentally appropriate.
Take home points:
- Child’s behavior is the key indicator.
- Infants need regular, age-appropriate sensory and social input throughout the day to ensure healthy emotional, cognitive, and physical development.
Which nursing interventions would be least appropriate for an elderly woman in a nursing home with a nursing diagnosis of Disturbed Sensory Perception: Chronic Sensory Deprivation related to the effects of aging? She had walked out the door unobserved and was hit by a car.
Explanation
Aging often brings vision and hearing decline, reduced mobility, and social isolation, which can lead to sensory deprivation. Effective nursing interventions aim to enhance orientation, stimulate senses, and provide safe, meaningful activities. Ineffective or passive approaches (such as ignoring confusion) worsen disorientation and increase risk of harm.
Rationale for correct answer:
1. Ignore when the patient is confused or go along to prevent embarrassment: This approach neglects the patient’s need for orientation and safety. It reinforces disorientation and fails to support adaptation. In cases of sensory deprivation, active interventions such as reorientation, reality testing, and structured activities are needed- not avoidance.
Rationale for incorrect answers:
2. Encourage self-care and independent decisions: Promotes autonomy, self-worth, and sensory engagement. Supporting independence helps counteract deprivation by giving the patient meaningful activities and control over daily life.
3. Take walks around the grounds and to the garden daily: Exposure to nature, light, fresh air, and exercise stimulates multiple senses and helps improve mood and orientation. Supervised walks also reduce isolation while ensuring safety.
4. Provide daily contact with children, community people, and pets: Socialization and interaction with others (including animals) provide multisensory input, emotional support, and help prevent loneliness and depression, which worsen sensory deprivation.
Take home points:
- Active orientation and engagement strategies are essential for elderly clients with sensory deprivation.
- Safe activities, social contact, and self-care help preserve dignity, reduce isolation, and improve quality of life in elderly residents.
A new nurse is going to help a patient walk down the corridor and sit in a chair. The patient has an eye patch over the left eye and poor vision in the right eye. What is the correct order of steps to help the patient safely walk down the hall and sit in the chair?
Explanation
To ensure safe ambulation techniques for visually impaired clients, nurses must use guiding methods that prioritize safety, independence, and dignity, such as offering the arm, walking slightly ahead, and providing clear verbal and tactile cues.
Rationale for correct answer:
3. Guide the patient’s hand to your arm, resting just above the elbow: This is the standard guiding technique for visually impaired clients. It provides stability and allows the nurse to lead safely.
4. Position yourself one-half step in front of the patient: Being slightly ahead enables the nurse to lead while the patient follows smoothly, sensing movement changes.
2. Walk at a relaxed pace: A steady, relaxed pace ensures safety and allows the patient to follow naturally without rushing.
1. Tell the patient when you are approaching the chair: The patient needs orientation before attempting to sit. Giving this cue prepares them mentally and physically.
5. Position the patient’s hand on the back of the chair: This gives the patient tactile orientation to the chair and promotes independence and safety when sitting down.
Take home points
- Always use guiding techniques: Offer your arm, walk slightly ahead, and give verbal/tactile cues.
- Promote independence and orientation: Help the client feel the chair so they can sit safely on their own.
A patient with progressive vision impairments had to surrender his driver’s license 6 months ago. He comes to the medical clinic for a routine checkup. He is accompanied by his son. His wife died 2 years ago, and he admits to feeling lonely much of the time. Which of the following interventions reduce loneliness? Select all that apply
Explanation
Effective interventions for reducing loneliness in older adults with sensory loss include facilitating social contact, improving accessibility (transportation), and strengthening support systems. Dismissing loneliness or creating distance worsens isolation.
Rationale for correct answer:
1. Sharing information about senior transportation services: Promotes mobility and independence, reduces isolation, and allows access to community/social activities.
4. Providing information about local social groups in the patient’s neighborhood: Facilitates new friendships, peer support, and engagement, all of which reduce loneliness.
5. Recommending that the patient consider making living arrangements that will put him closer to family or friends: Living near supportive relationships decreases isolation, provides companionship, and enhances emotional well-being.
Rationale for incorrect answers:
2. Reassuring the patient that loneliness is a normal part of aging: Dismissing loneliness as “normal” invalidates feelings and does not help the patient cope. Nurses should offer support and solutions, not minimize concerns.
3. Maintaining distance while talking to avoid overstimulating the patient: Distance increases isolation and makes communication harder, especially for clients with vision loss. Close, respectful interaction enhances connection.
Take home points
- Address loneliness proactively: Offer practical resources like transport, social groups, or housing near family/friends.
- Validate, don’t dismiss: Loneliness is not “normal aging”; interventions should focus on connection and meaningful engagement.
A nurse is performing an assessment on a patient admitted to the unit following treatment in the emergency department for severe bilateral eye trauma. During patient admission the nurse’s priority interventions include which of the following? Select all that apply
Explanation
This scenario assesses nursing priorities in acute care for a patient with new, severe visual impairment. The nurse’s role is to ensure immediate hospital safety (accessible environment, orientation), reduce anxiety, and maintain effective communication across the care team. Long-term teaching about home safety or prevention of future injury is important but not urgent at the time of admission.
Rationale for correct answer:
3. Placing necessary objects such as the nurse call system and water in front of the patient to prevent falls caused by reaching: Ensures safety by minimizing unnecessary movement, prevents falls, and promotes independence despite visual impairment.
4. Orienting the patient to the environment to reduce anxiety and prevent further injury to the eyes: Orientation reduces disorientation and anxiety. Clear explanation of surroundings prevents accidental injury due to impaired vision.
5. Alerting other nurses and health care providers about patient’s visual status during hand-off reports: Communicating the patient’s visual impairment ensures continuity of safe care and reduces risk of accidents or miscommunication.
Rationale for incorrect answers:
1. Conducting a home-safety assessment and identifying hazards in the patient’s living environment: Important for discharge planning, but not an immediate admission priority. At this stage, the patient needs stabilization and orientation in the hospital setting.
2. Reinforcing eye safety at work and in activities that place the patient at risk for eye injury@ This is a long-term teaching intervention, appropriate later in recovery or at discharge, not during acute admission after trauma.
Take-home points
- Immediate priorities focus on safety and orientation in the hospital, not future education.
- Clear communication of visual status to staff prevents errors and ensures consistent, safe care.
A nurse is performing a home care assessment on a patient with a hearing impairment. The patient reports, “I think my hearing aid is broken. I can’t hear anything.” After determining that the patient’s hearing aid works and that the patient is having trouble managing the hearing aid at home, which of the following teaching strategies does the nurse implement? Select all that apply
Explanation
Nurses must teach practical, hands-on skills on safe hearing aid management such as battery replacement, volume adjustment, and maintenance while emphasizing ear health. Unsafe practices (hot water, chemical cleaners) should be avoided to protect the device and patient.
Rationale for correct answers:
1. Demonstrate hearing aid battery replacement: Many hearing aid problems stem from dead or improperly placed batteries. Demonstrating replacement helps the patient gain independence and confidence in troubleshooting.
2. Review method to check volume on hearing aid: Teaching the patient to adjust and verify volume settings ensures optimal device use and prevents frustration from misinterpreted device malfunction.
4. Discuss the importance of having wax buildup in the ear canal removed: Earwax is a common cause of impaired hearing aid function. Patients should be taught to seek safe removal by a professional instead of attempting self-cleaning with unsafe objects.
Rationale for incorrect answers:
3. Demonstrate how to wash the earmold and microphone with hot water: Hearing aids should not be exposed to hot water, which damages electronic components. The correct method is wiping with a soft, dry cloth or using manufacturer-approved cleaning methods.
5. Recommend a chemical cleaner to remove difficult buildup: Harsh cleaners can damage delicate electronic components. Only manufacturer-approved tools or methods should be recommended.
Take-home points
- Teach safe, practical skills: battery replacement, volume checks, and addressing earwax are key to effective hearing aid use.
- Avoid unsafe methods: never use hot water or chemicals on hearing aids - use only manufacturer-recommended cleaning techniques.
Exams on Sensation, perception, and cognition
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
- Discuss the components of the sensory-perception process.
- Describe factors that influence sensory function.
- Identify clinical signs and symptoms of sensory deprivation and overload.
- Describe essential components in assessing a client’s sensory perception function.
- Discuss factors that place a client at risk for sensory disturbances.
- Develop nursing diagnoses and outcome criteria for clients with impaired sensory function.
- Discuss nursing interventions to promote and maintain sensory function.
- Identify strategies to promote a therapeutic environment for the client with acute confusion/delirium.
Introduction
An individual’s senses are essential for growth, development, and survival.
Making sense of one’s situation, learning new information, and recalling memories of the past are activities that make each person a unique individual. Performance of these activities relies on intact cognition, sensation, and perceptual abilities.
Sensory stimuli give meaning to events in the environment. Any alteration in people’s sensory functions can affect their ability to function within the environment.
Nurses are in the position to use knowledge of sensory functioning to support positive outcomes for patients.
Components Of The Sensory Experience
The sensory process involves two components: reception and perception.
Sensory reception is the process of receiving stimuli or data.
Sensory perception involves the conscious organization and translation of the data or stimuli into meaningful information.
These stimuli are either external or internal to the body.
- External stimuli are visual (sight), auditory (hearing), olfactory (smell), tactile (touch), and gustatory (taste). Gustatory stimuli can be internal as well.
- Other types of internal stimuli are kinesthetic or visceral. Kinesthetic refers to awareness of the position and movement of body parts. Visceral organs may produce stimuli that make a person aware of them (e.g., a full stomach).
For an individual to be aware of the surroundings, four aspects of the sensory process must be present:
- Stimulus: This is an agent or act that stimulates a nerve receptor.
- Receptor: A nerve cell acts as a receptor by converting the stimulus to a nerve impulse.
- Impulse conduction: The impulse travels along nerve pathways either to the spinal cord or directly to the brain.
- Perception: Perception, or awareness and interpretation of stimuli, takes place in the brain, where specialized brain cells interpret the nature and quality of the sensory stimuli.
1.1 Arousal Mechanism
For the person to receive and interpret stimuli, the brain must be alert, also referred to as arousal.
The reticular activating system (RAS) in the brainstem is thought to mediate the arousal mechanism.
The RAS has two components: the reticular excitatory area (REA) and the reticular inhibitory area (RIA). The REA is responsible for arousal and wakefulness.
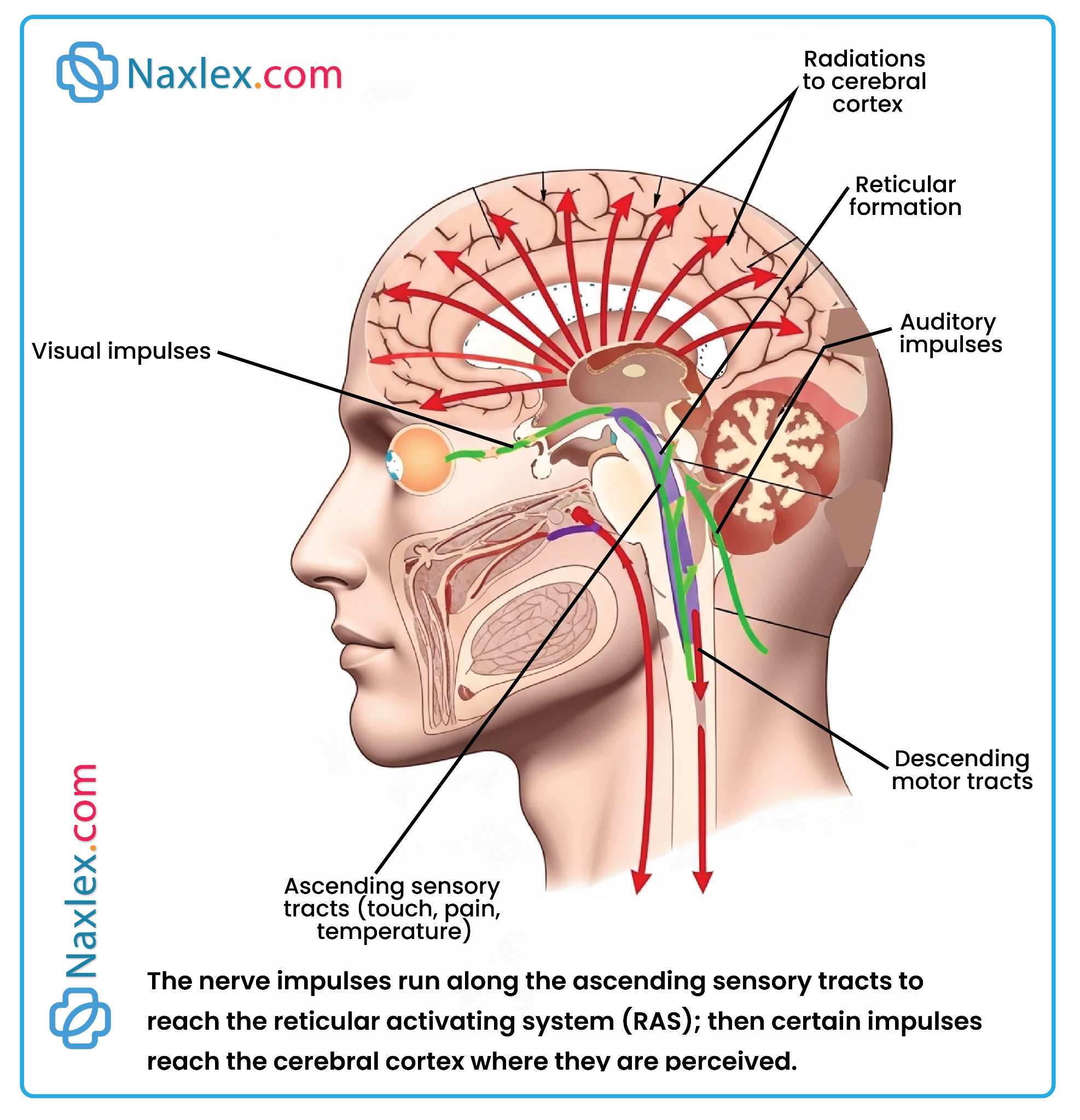
Sensoristasis is the term used to describe the state in which a person is in optimal arousal.
Awareness is the ability to perceive internal and external stimuli, and to respond appropriately through thought and action.
|
States of Awareness |
|
|
State |
Description |
|
Full consciousness |
Alert; oriented to time, place, person; understands verbal and written words |
|
Disoriented |
Not oriented to time, place, or person |
|
Confused |
Reduced awareness, easily bewildered; poor memory, misinterprets stimuli; impair ed judgment |
|
Somnolent |
Extreme drowsiness but will respond to stimuli |
|
Semi-comatose |
Can be aroused by extreme or repeated stimuli |
|
Coma |
Will not respond to verbal stimuli |
1.2 Factors affecting sensory function
A number of factors affect sensory reception and perception:
- Developmental stage:
Perception of sensation is critical to the intellectual, social, and physical development of infants and children.
Infants learn to recognize the face of their mother or caregiver and establish bonding essential to later emotional development. Young children respond to music by singing and dancing as they begin to interact with their peers in groups.
- Culture:
An individual’s culture often determines the amount of stimulation that a person considers usual or “normal.”
In addition, the normal amount of stimulation associated with ethnic origin, religious affiliation, and income level, for example, also affects the amount of stimulation an individual desires and believes to be meaningful.
Cultural deprivation, or cultural care deprivation, is a lack of culturally assistive, supportive, or facilitative acts.
- Stress:
During times of increased stress, people may find their senses already overloaded and thus seek to decrease sensory stimulation.
- Medications and Illness:
Certain medications can alter an individual’s awareness of environmental stimuli.
- Narcotics, antiepileptic agents, and sedatives, for example, can decrease awareness of stimuli. Some antidepressants can also alter perceptions of stimuli.
- The nurse is responsible for protecting the client from injury that can result from impaired sensory perception.
Some medications, if taken in large doses or over a long period of time, become ototoxic, injuring the auditory nerve and causing hearing loss that may be irreversible
Certain diseases, such as atherosclerosis, restrict blood flow to the receptor organs and the brain, thereby decreasing awareness and slowing responses.
- Lifestyle and personality:
Lifestyle influences the quality and quantity of stimulation to which an individual is accustomed.
- A client who is employed in a large company may be accustomed to many diverse stimuli, whereas a client who is self-employed and works in the home is exposed to fewer, less diverse stimuli.
People’s personalities also differ in terms of the quantity and quality of stimuli with which they are comfortable.
- Some people delight in constantly changing stimuli and excitement, whereas others prefer a more structured life with few changes.
1.3 Sensory alterations
People become accustomed to certain sensory stimuli, and when these change markedly an individual may experience discomfort.
Nurses have become increasingly aware of the behaviors that may result from different stimuli. They now pay more attention to color, sound, privacy, and social interaction for clients so that the stimuli more closely resemble those in the home environment.
Factors that contribute to alterations in behavior include sensory deprivation, sensory overload, and sensory deficits.
- Sensory Deprivation:
Sensory deprivation is generally thought of as a decrease in or lack of meaningful stimuli.
When a person experiences sensory deprivation, the balance in the reticular activating system is disturbed. The RAS is unable to maintain normal stimulation to the cerebral cortex.
Because of this reduced stimulation, a person becomes more acutely aware of the remaining stimuli and often perceives these in a distorted manner. The person often experiences alterations in perception, cognition, and emotion.
Clinical manifestations:
- Excessive yawning, drowsiness, sleeping
- Decreased attention span, difficulty concentrating, decreased problem solving
- Impaired memory
- Periodic disorientation, general confusion, or nocturnal confusion
- Preoccupation with somatic complaints, such as palpitations
- Hallucinations or delusions
- Crying, annoyance over small matters, depression
- Apathy, emotional liability
- Sensory overload:
Sensory overload generally occurs when a person is unable to process or manage the amount or intensity of sensory stimuli.
Three factors contribute to sensory overload:
- Increased quantity or quality of internal stimuli, such as pain, dyspnea, or anxiety
- Increased quantity or quality of external stimuli, such as a noisy health care setting, intrusive diagnostic studies, or contacts with many strangers
- Inability to disregard stimuli selectively, perhaps as a result of nervous system disturbances or medications that stimulate the arousal mechanism.
Sensory overload can prevent the brain from ignoring or responding to specific stimuli. Because of the many stimuli, the individual has difficulty perceiving the environment in a way that makes sense. As a result the individual’s thoughts race in many directions, causing restlessness and anxiety.
Clinical manifestations:
- Complaints of fatigue, sleeplessness
- Irritability, anxiety, restlessness
- Periodic or general disorientation
- Reduced problem-solving ability and task performance
- Increased muscle tension
- Scattered attention and racing thoughts
- Sensory deficits:
A sensory deficit is impaired reception, perception, or both, of one or more of the senses. Blindness and deafness are sensory deficits.
When the loss of sensory function is gradual, individuals often develop behaviors to compensate for the loss; sometimes these behaviors are unconscious. For example, a person with gradual hearing loss in the right ear may unconsciously turn the left ear toward a speaker.
However, sudden loss of one of the senses can result in disorientation, and compensatory behavior often takes days or weeks to develop.
Clients with sensory deficits are at risk for both sensory deprivation and sensory overload.
Example: Individuals with visual problems may be unable to read, watch television, or recognize nurses by sight, which could lead to sensory deprivation. On the other hand, blind people often have highly structured home environments, and the diversity and unfamiliarity of the hospital environment can create sensory overload.
Nursing Management
1.1 Assessing
Nursing assessment of sensory-perceptual functioning includes six components:
- nursing history
- mental status examination
- physical examination
- identification of clients at risk
- the client’s environment
- the client’s social support network.
Nursing History:
During the nursing history the nurse assesses the client’s current sensory perceptions, usual functioning, sensory deficits, and potential problems.
Examples of interview questions to elicit data about the client’s sensory-perceptual functioning include:
VISUAL
- How would you rate your vision (excellent, good, fair, or poor)?
- Do you wear eyeglasses or contact lenses?
- Describe any recent changes in your vision.
- Do you have any difficulty seeing near or far objects?
- Do you have any difficulty seeing at night? Have you ever experienced blurred vision, double vision, spots moving in front of your eyes, blind spots, light sensitivity, flashing lights, or halos around objects?
- When did you last visit an eye doctor?
AUDITORY
- How would you rate your hearing (excellent, good, fair, or poor)?
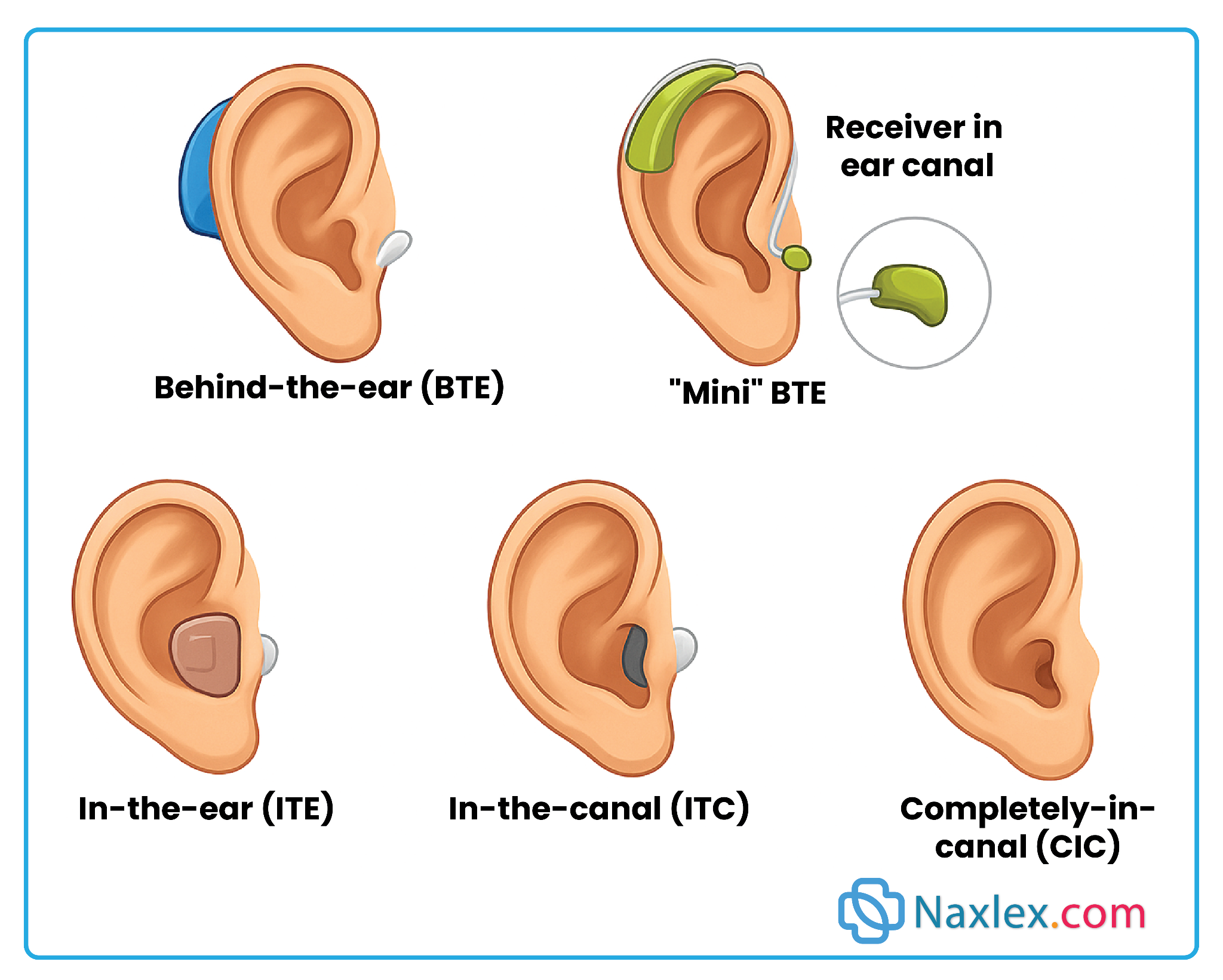
- Do you wear a hearing aid?
- Describe any recent changes in your hearing.
- Can you locate the direction of sounds and distinguish various voices?
- Do you experience any dizziness or vertigo? Do you experience any ringing, buzzing, humming, crackling noises, or fullness in the ears?
GUSTATORY
- Have you experienced any changes in taste (e.g., difficulty in differentiating sweet, sour, salty, and bitter tastes)?
- Do you enjoy the taste of foods as you did previously?
OLFACTORY
- Have you experienced any changes in smell?
- Do things (foods, flowers, perfumes, and so on) smell the same as previously?
- Can you distinguish foods by their odors and tell when something is burning?
- Have you experienced any changes in appetite? (Changes in appetite may be related to an impaired sense of smell.)
TACTILE
- Are you experiencing any pain or discomfort?
- Have you experienced any decrease in your ability to perceive heat, cold, or pain in your limbs?
- Do you have any numbness or tingling in your extremities?
KINESTHETIC
- Have you noticed any difficulty in perceiving the position of parts of your body?
Mental Status Examination:
Mental status is critical to any evaluation of the sensory-perceptual process.
Data on mental status, including level of consciousness, orientation, memory, and attention span, are usually obtained during the nursing history.
It is important to note that sensory alterations can cause changes in cognitive functioning and vice versa.
Physical examination:
Physical assessment determines whether the senses are impaired.
The examination should reveal the client’s specific visual and hearing abilities; perception of heat, cold, light touch, and pain in the limbs; and awareness of the position of the body parts.
Specific sensory tests include the following:
- Visual acuity, using a Snellen chart or other reading material such as a newspaper, and visual fields
- Hearing acuity, by observing the client’s conversation with others and by performing the whisper test and the Weber and Rinne tuning fork tests
- Olfactory sense, by asking the client to identify specific aromas
- Gustatory sense, by asking the client to identify three tastes such as lemon, salt, and sugar
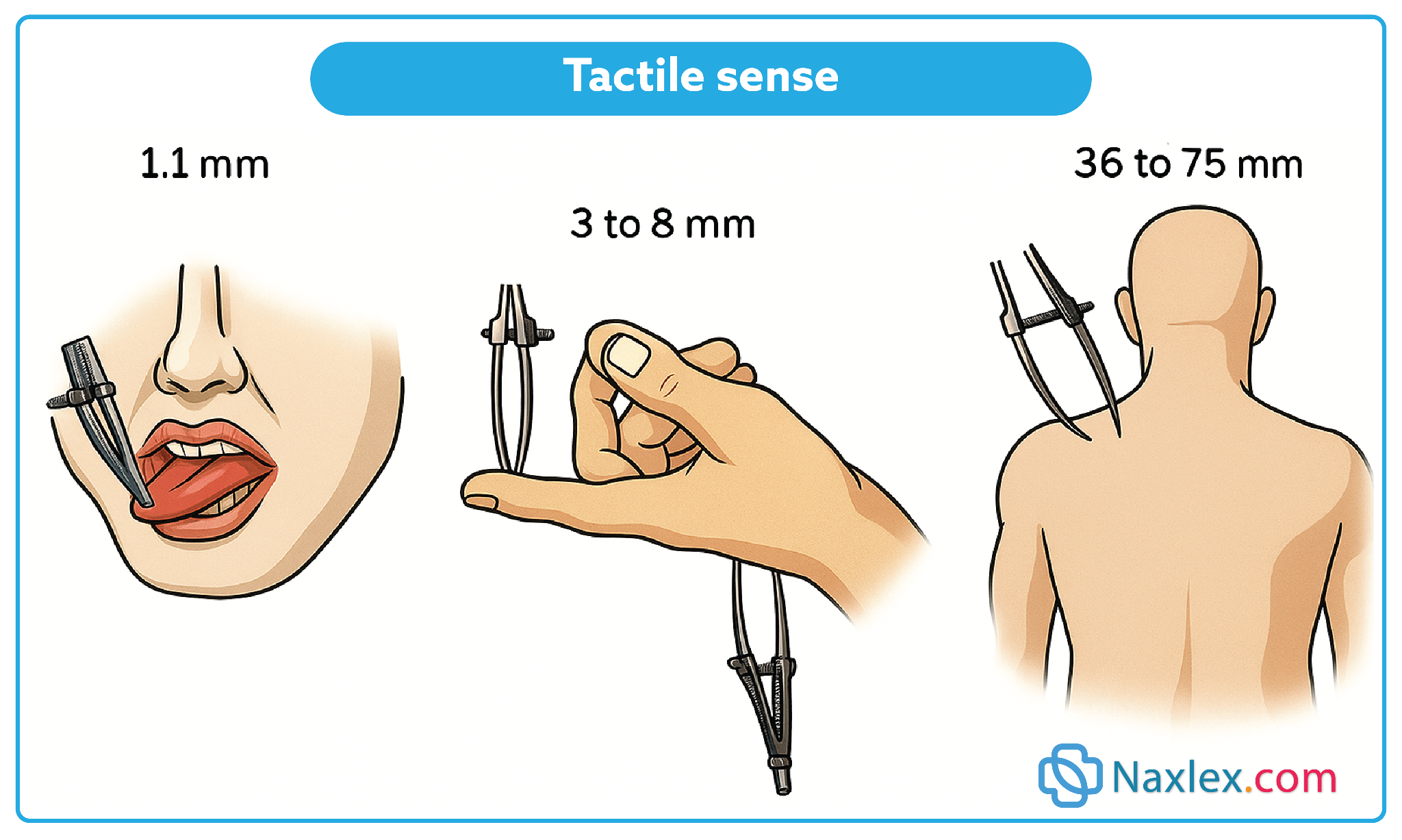
- Tactile sense, by testing light touch, sharp and dull sensation, two point discrimination, hot and cold sensation, vibration sense, position sense, and stereognosis.
Identification of clients at risk:
Clients at risk for sensory-perceptual alterations need to be identified to ensure that preventive measures can be initiated.
Sensory Deprivation:
Clients Who:
- are confined in a non stimulating or monotonous environment in the home or health care agency
- have impaired vision or hearing
- have mobility restrictions such as quadriplegia or paraplegia with bed rest, traction apparatus
- are unable to process stimuli (e.g., clients who have brain damage or who are taking medications that affect the central nervous system)
- have emotional disorders (e.g., depression) and withdraw within themselves
- have limited social contact with family and friends (e.g., clients from a different culture).
Sensory Overload:
Clients Who:
- have pain or discomfort
- are acutely ill and have been admitted to an acute care facility
- are being closely monitored in an intensive care unit (ICU) and have intrusive tubes such as IVs, catheters, or nasogastric or endotracheal tubes
- have decreased cognitive ability (e.g., head injury).
Client Environment:
A nurse should assess the client’s environment for quantity, quality, and type of stimuli.
The environment may produce insufficient stimuli, placing the client at risk for sensory deprivation, or excessive stimuli, placing the client at risk for sensory overload.
Because appropriate or meaningful stimuli decrease the incidence of sensory deprivation, the nurse must consider the client’s health care environment for the presence of the following stimuli:
-
- Electronic devices (computers, DVD/CD players, television, smart phones)
- Clock or calendar
- Reading material (or toys for children)
- Number and compatibility of roommates
- Number of visitors.
Client’s social support network:
The degree of isolation a person feels is significantly influenced by the quality and quantity of support from family members and friends.
A nurse should assess
- whether the client lives alone
- who visits and when
- any signs indicating social deprivation, such as withdrawal from contact with others to avoid embarrassment or dependence on others, negative self-image
1.2 Diagnosing
The approved NANDA diagnostic labels for perception and cognition are:
- Acute Confusion: abrupt onset of reversible disturbances of consciousness, attention, cognition, and perception that develop over a short period of time.
- Chronic Confusion: irreversible, long-standing, and/or progressive deterioration of intellect and personality characterized by decreased ability to interpret environmental stimuli; decreased capacity for intellectual thought processes; and manifested by disturbances of memory, orientation, and behavior.
- Impaired Memory: inability to remember or recall bits of information or behavior skills.
- Risk for Acute Confusion: at risk for alterations in consciousness, attention, cognition, and perception that develops over a short time period.
Depending on the data obtained, alterations in sensory-perception function may affect other areas of human functioning and indicate other diagnoses. Examples of nursing diagnoses for which sensory-perception disturbances are the etiology include the following:
- Impaired Home Maintenance related to sensory-perception disturbance (declining visual abilities).
- Impaired Verbal Communication related to sensory-perception disturbance (specify). For example:
- Sensory deprivation
- Sensory overload
- Hearing impairment
- Altered level of consciousness
- Risk for Impaired Skin Integrity related to sensory-perception disturbance (altered tactile sensation)
- Risk for Injury related to sensory-perception disturbance (specify). For example:
- Visual impairment (e.g., decreased depth perception)
- Reduced tactile sensation secondary to neurologic or circulatory alterations
- Decreased sense of smell
- Hearing impairment
- Decreased kinesthetic sense
- Social Isolation related to sensory-perception disturbance (specify). For example:
- Impaired vision
- Impaired hearing
1.3 Planning
Planning includes goals associated with the care of clients independent of setting and those specific to the home environment.
Planning Independent of Setting:
The overall outcome criteria for clients with sensory-perception alterations are to:
- Prevent injury.
- Maintain the function of existing senses.
- Develop an effective communication mechanism.
- Prevent sensory overload or deprivation.
- Reduce social isolation.
- Perform activities of daily living (ADLs) independently and safely
Planning for Home Care
To provide for continuity of care, a nurse must consider a client’s needs for assistance with care in the home or residential treatment setting.
Discharge planning incorporates a reassessment of the client’s abilities for self-care, the availability and skills of support people, financial resources, and the need for referrals and home health services.
A major aspect of discharge planning involves the instructional needs of the client and family.
1.4 Implementing
Nurses can assist clients with sensory alterations by promoting healthy sensory function, helping clients manage acute sensory deficits, and adjusting environmental stimuli.
A. PROMOTING HEALTHY SENSORY FUNCTION:
Detecting sensory problems early is one step toward preventing serious problems. The arousal mechanism for sensation is normally present at birth; however, it is undifferentiated. The special senses are also present at birth, although some changes in function occur during the growth process.
Early Hearing Detection and Intervention (EHDI) Tracking and Surveillance System goals have been established by the Centers for Disease Control and Prevention (CDC) (2014).
The seven goals are:
- Goal 1: All newborns will be screened for hearing loss before 1 month of age.
- Goal 2: All infants who screen positive will require a diagnostic audiologic examination before the age of 3 months.
- Goal 3: All infants identified with hearing loss will receive early intervention services prior to age 36 months.
- Goal 4: Infants with late, progressive, or acquired hearing loss will be identified early.
- Goal 5: Infants with hearing loss will have a primary care provider who will collaborate and coordinate care with the EHDI Tracking and Surveillance System at the CDC.
- Goal 6: Each state is responsible for completing the EHDI Tracking and Surveillance System.
- Goal 7: Every state will have a complete EHDI Tracking and Surveillance System to minimize loss of clients and to maintain current information on every infant identified as having a hearing loss.
Women who are considering pregnancy should be advised of the importance of prenatal testing for syphilis and confirmation of a positive rubella titer, because maternal syphilis and rubella infection can both cause hearing impairments in newborns.
Periodic vision screening of all newborns and children is recommended to detect congenital blindness, strabismus, and refractive errors.
Impaired Vision
- Nursing care
- Orient to room layout; keep environment uncluttered.
- Keep pathways clear; do not rearrange furniture without informing client.
- Place self-care items and call light within easy reach; keep bed low.
- Assist ambulation by walking slightly ahead, allowing client to grasp arm.
- Common vision diseases
- Macular degeneration – leading cause of blindness in adults >65.
- Cataracts – lens opacities, slow/painless, leading cause of blindness worldwide.
- Glaucoma – optic nerve damage from increased intraocular pressure; 2nd leading cause of blindness in US.
- Diabetic retinopathy – microvascular damage in type 1 & 2 DM.
- Consequences
- Difficulty with ADLs & IADLs - increase disability.
- Risk of depression (due to disability, loss of autonomy, or fear).
- Loss of leisure activities (e.g., reading).
Impaired Hearing
- Nursing care
- Check alarms (IV pumps, monitors) frequently.
- Encourage use of devices: amplified/low-frequency alarms, flashing lights (doorbells, phones, smoke detectors).
- The sounds of doorbells and alarm clocks may be amplified or changed to a lower frequency or buzzer-like sound.
- Speak slowly, clearly; avoid noisy/reverberant environments.
- Consider effect of fast speech and accents on understanding.
- Consequences
- Communication barriers.
- Risk of missed alarms.
- Social isolation.
Impaired Olfactory Sense
- Risks
- Chemical exposure (ammonia, gas leaks).
- Food poisoning (inability to smell spoiled food).
- Safety teaching
- Maintain stoves/heaters in good working order.
- Inspect food by color, texture, expiration dates.
Impaired Tactile Sense
- Risks
- Burns (reduced temperature sensation).
- Pressure ulcers (reduced pressure sensation).
- Safety teaching
- Adjust hot water heater to safe levels.
- Test bath water with thermometer.
- Reposition frequently to prevent skin breakdown.
B. MANAGING ACUTE SENSORY IMPAIRMENTS:
When assisting clients who have a sensory impairment, a nurse needs to:
- encourage the use of sensory aids to support residual sensory function
- promote the use of other senses
- communicate effectively
- ensure client safety.
- Encouraging the Use of Sensory Aids:
Many sensory aids are available for clients who have visual and hearing deficits.
In all situations, the assistance of support people needs to be enlisted whenever possible to help the client deal with the deficit.
VISUAL
- Braille or recorded books Eyeglasses of the correct prescription, clean and in good repair
- Adequate room lighting, including night-lights
- Sunglasses or shades on windows to reduce glare
- Bright contrasting colors in the environment
- Magnifying glass
- Phone dialer with large numbers
- Clock and wristwatch with large numbers
- Color code or texture code on stoves, washer, medicine containers, and so on
- Colored or raised rims on dishes
- Reading material with large print
- Service dog
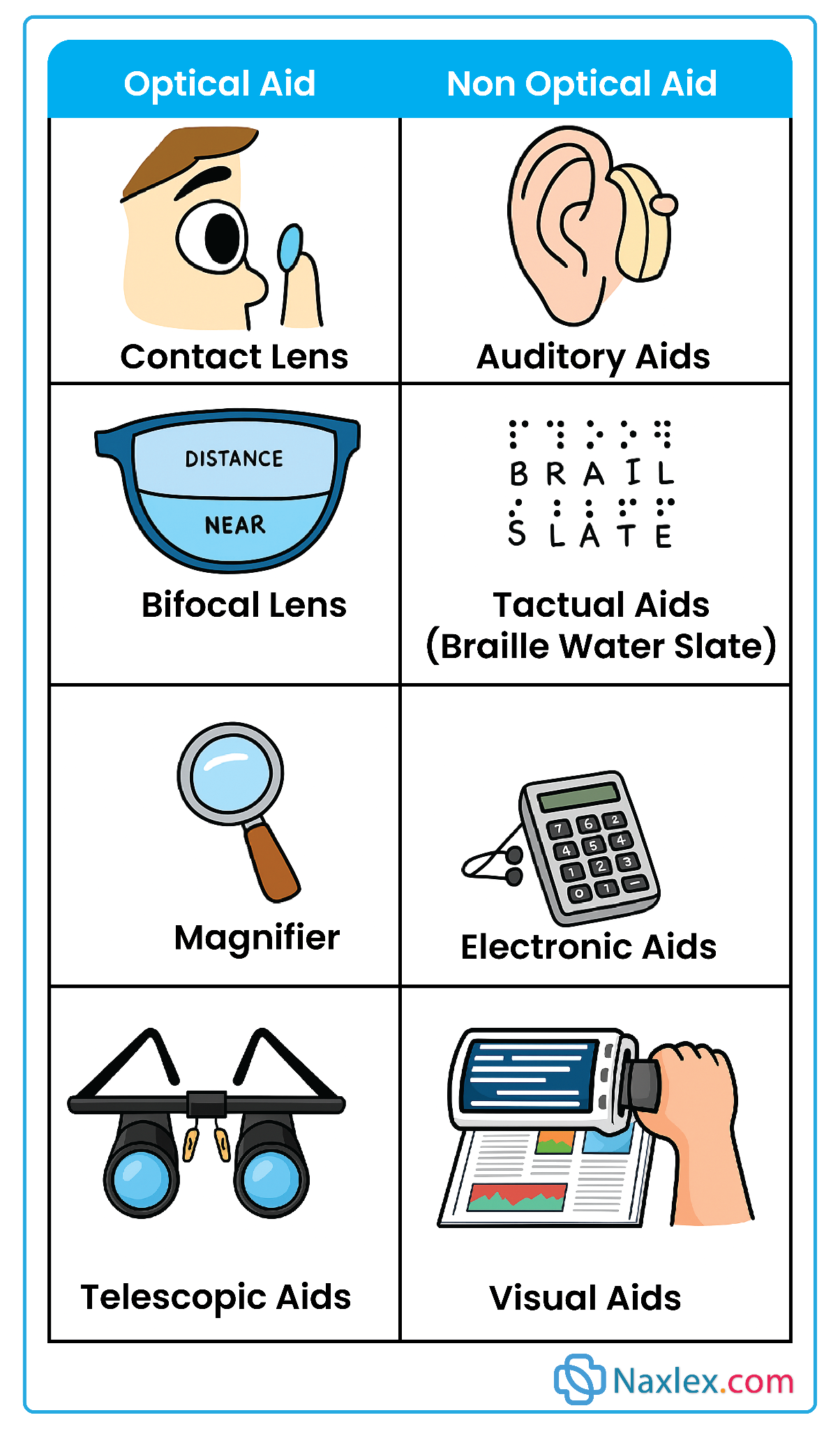
HEARING
- Hearing aid in good order
- Lip reading
- Sign language
- Amplified telephones
- Telecommunication device for the deaf (TDD)
- Amplified telephone ringers and doorbells
- Flashing alarm clocks
- Flashing smoke detectors
- Promoting the use of other senses:
When one sense is lost, a nurse can teach the client to use other senses to supplement the loss. However, the type of stimulation needs to be adapted in accordance with the client’s specific deficit.
For example, for the client with a visual impairment, stimulation of hearing, taste, smell, and touch can be encouraged.
|
Sense |
Stimulation Strategies |
|
Auditory |
Radio, audiotapes (music/books), clocks that chime, music boxes, wind chimes |
|
Gustatory |
Varied diet (flavors, temperatures, textures); sip water between foods; eat foods separately |
|
Olfactory |
Fresh flowers, scented candles (safe use), room fragrances, brewing coffee, baking; recall pleasant/familiar odors |
|
Tactile |
Hugs, massage, hair brushing, grooming; varied fabric textures (clothing, upholstery); pets |
- Communicating effectively:
Communication with clients who have sensory impairments should convey respect, enhance the person’s self-esteem, and ensure the exchange of correct information
Visual impairment:
- Always announce your presence when entering the client’s room and identify yourself by name.
- Stay in the client’s field of vision if the client has a partial vision loss.
- Speak in a warm and pleasant tone of voice. Some people tend to speak louder than necessary when talking to a person who is blind.
- Always explain what you are about to do before touching the person.
- Explain the sounds in the environment.
- Indicate when the conversation has ended and when you are leaving the room.
Hearing impairment:
- Before initiating conversation, convey your presence by moving to a position where you can be seen or by gently touching the person.
- Decrease background noises (e.g., television) before speaking.
- Talk at a moderate rate and in a normal tone of voice.
- Address the person directly. Do not turn away in the middle of a remark or story. Make sure the person can see your face easily and that it is well lighted.
- Avoid talking when you have something in your mouth, such as chewing gum. Avoid covering your mouth with your hand.
- Keep your voice at about the same volume throughout each sentence, without dropping the voice at the end of each sentence.
- Always speak as clearly and accurately as possible. Articulate consonants with particular care.
- Do not “overarticulate”; mouthing or overdoing articulation is just as troublesome as mumbling. Pantomime or write ideas, or use sign language or finger spelling as appropriate.
- Use longer phrases, which tend to be easier to understand than short ones. For example, “Would you like a drink of water?” presents much less difficulty than “Would you like a drink?” Word choice is important: “Fifteen cents” and “fifty cents” may be confused, but “half a dollar” is clear.
- Pronounce every name with care.
- Change to a new subject at a slower rate, making sure that the person follows the change to the new subject. A key word or two at the beginning of a new topic is a good indicator.
Patients with aphasia
- Listen to the patient and provide sufficient time to communicate.
- Do not shout or speak loudly (hearing loss is not the problem).
- If patient has problems with comprehension, use simple, short questions and facial gestures to give additional clues.
- Speak of things familiar and of interest to patient.
- If patient has problems speaking, ask questions that require simple yes-or-no answers or blinking of the eyes. Offer pictures or a communication board so patient can point.
- Speak slowly and give patient time to understand; be calm and patient; do not pressure or tire the patient.
- Avoid patronizing and childish phrases.
Nursing insight: Communicating with a patients with an artificial airway
- Use pictures, objects, or word cards so patient can point.
- Offer a pad and pencil or Magic Slate for patient to write messages.
- Do not shout or speak loudly.
- Give patient time to write messages because patients tire easily.
- Provide an artificial voice box (vibrator) for patient with a laryngectomy to use to speak.
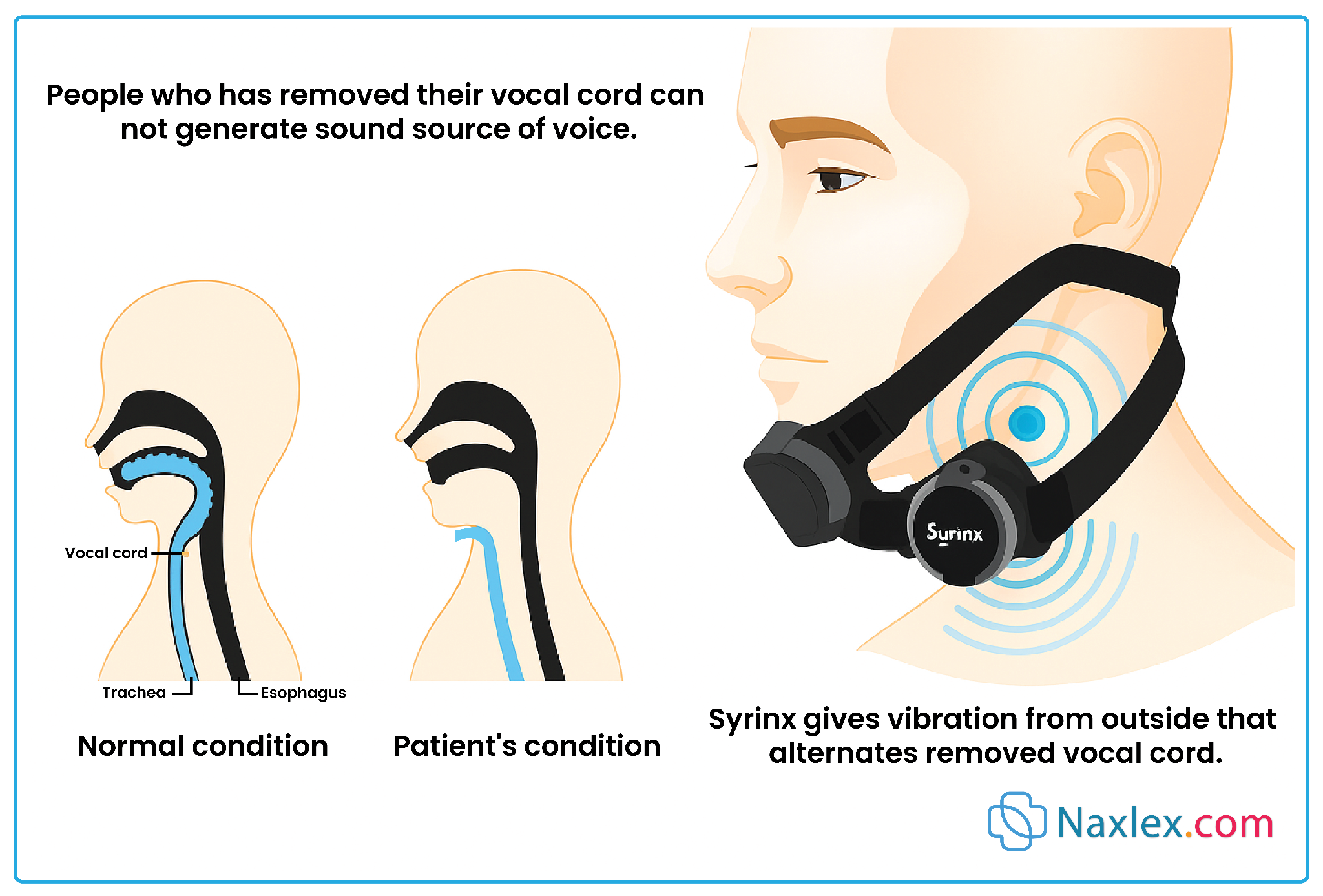
- Adjusting Environmental Stimuli
Preventing Sensory Overload
- Reduce stimuli:
- Dark glasses, window shades/drapes-reduce visual input.
- Earplugs, soft music, earphones- reduce auditory input.
- Keep wounds clean/dry- minimize odors.
- Organize care: Cluster activities; provide rest intervals.
- Control environment: Limit visitors (number & length).
- Explain sounds: Helps clients interpret alarms/noises (e.g., IV beeping).
- Promote coping: Teach relaxation techniques to reduce anxiety.
Preventing Sensory Deprivation
- Visual & auditory stimulation: Newspapers, books, music, TV.
- Tactile stimulation: Pets, objects pleasant to touch.
- Orientation aids: Clocks distinguishing day/night by color.
- Olfactory stimulation: Fresh flowers, plants.
- Social interaction: Regular visits from family, friends, community/church groups.
Nursing insight:
Essential Oils and CNS Health
-
- Chamomile (Anthemis nobilis): Alleviates physical and mental stress
- Lavender (Lavandula angustifolia): Calming, sedative effect
- Mandarin (Citrus reticulata): Relieves anxiety
- Peppermint (Mentha piperita): Stimulant; strengthens adrenal cortex
- Yarrow (Achillea millefolium): Promotes sleep
1.5 Evaluating
Using the measurable and desired outcomes developed during the planning stage as a guide, the nurse collects the data needed to judge whether client goals and outcomes have been achieved.
The Confused Client
Confusion can occur in clients of all ages, but it is most commonly seen in older people.
Confusion often presents with subtle symptoms, but it is important for the nurse to differentiate between acute confusion (delirium) and chronic confusion (dementia).
Delirium has an abrupt onset and a cause that, when treated, reverses the confusion. Dementia, often called chronic confusion, has symptoms that are gradual and irreversible (e.g., Alzheimer’s disease).
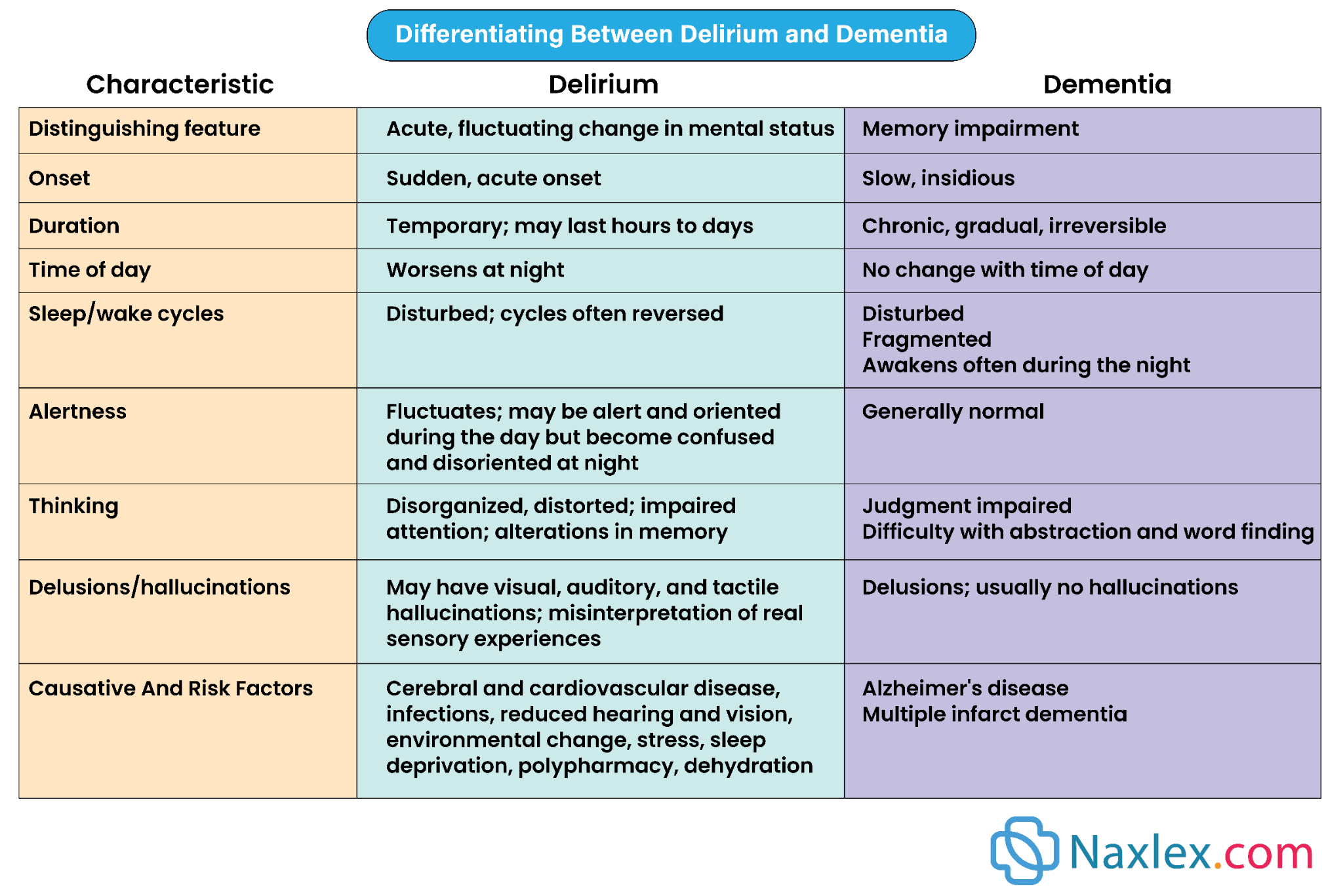
Acute Confusion amd Delirium
- Acute Confusion: Nursing diagnosis based on client’s experience and behavior, often from intoxication, infection, or dementia.
- Delirium: Medical term, common in older adults, especially post-surgery (≈40%).
Risk Factors
- Increased age
- Cognitive or sensory impairment
- Comorbidities (COPD, dementia, stroke, hypertension)
- Poor nutrition
- Depression, low education level
- Polypharmacy (anticholinergics, sedatives, narcotics)
- Environmental triggers (pain, sleep deprivation, hospital stress, sensory overload)
Clinical Features of Delirium
- Reduced ability to focus, sustain, or shift attention
- Cognitive changes (memory loss, disorientation, perceptual disturbances)
- Acute onset, fluctuating course within 24 hrs
Subtypes
- Hyperactive: Agitation, restlessness, disorientation
- Hypoactive: Quiet, apathetic, confused (may mimic depression/dementia)
- Mixed: Alternates between hyperactive and hypoactive
Assessment Tools
- CAM (Confusion Assessment Method)- gold standard
- Family CAM or FAM-CAM- is a screening tool in which family members are interviewed to maximize the detection of delirium in clients. Helps to identify acute onset, fluctuations in the delirium course, inattention, disorganized thought processes, diminished level of consciousness, disorientation, perceptual changes, and hallucinations
- Other tools include the Mini-Mental State Examination (MMSE), the Delirium Index (DI), and the NEECHAM Confusion Scale.
Nursing Interventions (Therapeutic Environment)
- Use name tags; introduce self consistently
- Assign consistent caregivers
- Reorient with time, place, and person
- Use calendar, clock, clear signage, and familiar items
- Speak calmly and clearly, allow processing time
- Encourage safe family visits
- Maintain routine schedules for meals, sleep, care
- Control pain and ensure adequate sleep
- Reduce noise and clutter; maintain adequate lighting
- Keep eyeglasses/hearing aids accessible
- Eliminate unnecessary medications
Summary
- The sensory experience consists of two components: sensory reception and sensory perception.
- Sensory stimuli can be either external or internal. Visual, auditory, olfactory, tactile, and gustatory stimuli orient a person to the external environment.
- Kinesthetic and visceral stimuli orient the person to the internal environment. Kinesthetic stimuli make the person aware of the position and movement of body parts.
- Factors affecting sensory stimulation include developmental stage, culture, stress, medications, illness, and lifestyle and personality.
- Sensory deprivation occurs when a person receives decreased sensory input or monotonous or meaningless sensory input.
- Sensory overload occurs when a person experiences excessive sensory input and is unable to process or manage the stimuli. The person feels overwhelmed and not in control.
- Goals for clients with sensory-perception disturbances include
- preventing injury
- maintaining the function of existing senses
- developing an effective communication mechanism
- preventing sensory deprivation or overload
- reducing social isolation
- performing ADLs independently and safely.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Sensation, perception, and cognition
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


