Please set your exam date
Croup Syndromes
Study Questions
Practice Exercise 1
A 5-year-old is seen in the urgent care clinic with the following history and symptoms: sudden onset of severe sore throat after going to bed, drooling and difficulty swallowing, axillary temperature of 102.2o F (39.0o C), clear breath sounds, and absence of cough. The child appears anxious and is flushed. Based on these symptoms and history, the nurse anticipates a diagnosis of:
Explanation
Acute epiglottitisis a life-threatening condition caused most commonly by Haemophilus influenzae type b (Hib), though less common now due to Hib vaccination. It involves rapid inflammation and swelling of the epiglottis, leading to airway obstruction. It primarily affects children aged 2–7 years and is a pediatric emergency.
Rationale for correct answer:
3. Acute epiglottitisis the most likely diagnosis based on the classic triad: sudden onset of high fever and severe sore throat, drooling and dysphagia and muffled or hoarse voice, anxiety, and absence of cough
The child appears anxious and flushed, which may indicate hypoxia or respiratory distress. The absence of cough and presence of drooling are critical signs distinguishing epiglottitis from other upper respiratory illnesses.
Rationale for incorrect answers
1. Group A β-hemolytic streptococcus (GABHS) pharyngitis)may cause sore throat and fever, but typically does not cause drooling or dysphagia to this degree. It also presents more gradually and doesn’t lead to sudden airway emergency.
2. Acute tracheitisoften follows an upper respiratory infection and presents similarly to croup, but drooling and sudden onsetare not common. It also typically presents with a cough and stridor.
4. Acute laryngotracheobronchitis (croup)is more common than epiglottitis but presents with a barking cough, gradual onset, and stridor. The child usually doesn’t drool or have difficulty swallowing.
Take home points
- Acute epiglottitis is a medical emergency. It can progress quickly to airway obstruction.
- Do not examine the throat or insert anything into the mouth, as this may precipitate complete airway closure.
- Look for the “tripod position,” drooling, absence of cough, and high fever in children.
- Ensure Hib vaccination is up to date to prevent this condition.
A nurse is educating a group of parents regarding the rationales for the administration of vaccinations. The nurse should advise the parents that the vaccine that prevents infections from which of the following diseases has helped to reduce the numbers of children diagnosed with bacterial croup?
Explanation
Bacterial croupis a term sometimes used to describe acute epiglottitis, a serious upper airway infection that can resemble severe viral croup but is caused by bacteria, most commonly Haemophilus influenzaetype b (Hib). Before the introduction of the Hib vaccine, epiglottitis was a leading cause of airway emergencies in children.
Rationale for correct answer:
2. Haemophilus influenzaetype b (Hib)vaccine has dramatically reduced the incidence of acute epiglottitis. Although viral croup is more common and caused by parainfluenza viruses, Hib-related epiglottitis was historically referred to as "bacterial croup" due to its upper airway involvement and rapid progression. Routine Hib vaccinationis a major public health success, significantly decreasing this once-common pediatric emergency.
Rationale for incorrect answers:
1. Hepatitis Avaccine prevents liver infection spread via the fecal-oral route. It has no connection to respiratory infections or croup.
3. Rotavirusprevents severe gastroenteritis and dehydration, particularly in infants. It is unrelated to any form of croup or upper airway disease.
4. Neisseria meningitidiscauses meningococcal meningitis and sepsis, not respiratory tract infections. While serious, it is not linked to croup or epiglottitis.
Take home points
- The Hib vaccine prevents acute epiglottitis, often referred to as bacterial croup, especially before routine immunization.
- Bacterial croup is not the same as viral croup, which is more common and less severe.
- Vaccines can indirectly reduce emergency airway events in children by preventing infections like Hib.
- Always maintain up-to-date vaccination to protect children from rare but life-threatening diseases.
A toddler has moderate respiratory distress, is mildly cyanotic, and has increased work of breathing, with a respiratory rate of 40. What is the priority nursing intervention?
Explanation
Moderate respiratory distress in toddlersmay present with increased work of breathing, tachypnea, and mild cyanosis. Cyanosis indicates hypoxemia, and a respiratory rate of 40 is elevated for a toddler (normal: ~24–40 breaths/min). These signs suggest an urgent need to support oxygenation and maintain airway patencyto prevent progression to severe distress or respiratory failure.
Rationale for correct answer:
1. Airway maintenance and 100% oxygen by maskprioritizes the ABC approach (Airway, Breathing, Circulation)in pediatric emergencies. The child has signs of oxygen deficiency such as cyanosis and increased respiratory effort, which require immediate intervention. Administering high-flow oxygenand maintaining an open airway are essential life-saving steps. Mask delivery ensures effective oxygenation, especially in a distressed toddler who may not tolerate nasal cannula.
Rationale for incorrect answers:
2. While oxygen and monitoringare important, this option fails to include airway maintenance, which is critical in a child showing signs of respiratory distress and cyanosis.
3. Although reassessmentis essential, this option omits oxygen delivery, which is urgently needed due to the child’s cyanosis and increased work of breathing.
4. Comfortis important but not a priority over airway and effective oxygenation in a child with signs of hypoxia. Comfort does not address airway patency or ventilation.
Take home points
- Always follow the ABC priority in pediatric emergencies.
- Cyanosis and increased work of breathing require immediate need for airway support and oxygen therapy.
- Use high-concentration oxygen by mask for best delivery in young children.
- Monitoring and comfort are supportive but not substitutes for life-saving interventions.
Which is the most appropriate nursing diagnosis for the child with epiglottitis?
Explanation
Epiglottitisis a life-threatening bacterial infection (commonly caused by Haemophilus influenzae type B) that leads to inflammation and swelling of the epiglottis, potentially obstructing the airway. It is a medical emergencyrequiring prompt recognition and airway management. Symptoms include sudden onset of high fever, sore throat, drooling, muffled voice, dysphagia, and inspiratory stridor.
Rationale for correct answer:
3. Ineffective airway clearance related to laryngospasm: This is the most appropriate nursing diagnosis because airway obstruction is the primary and most critical concern in epiglottitis. Inflammation and spasm of the laryngeal structures can block airflow, making airway maintenance the highest priority. Nursing care focuses on ensuring a patent airway, avoiding throat examination or procedures that could precipitate complete obstruction, and preparing for possible intubation or tracheostomy.
Rationale for incorrect answers:
1. Anxiety related to separation from the parent: While anxiety is common in hospitalized children, in this case, the airway takes precedence. Emotional comfort is important but not life-threatening.
2. Decreased cardiac output related to bradycardia: Bradycardia is not a typical manifestation of epiglottitis; tachycardia may occur due to hypoxia, but the main issue is respiratory, not cardiac output.
4. Impaired gas exchange related to noncompliant lungs: The lungs themselves are not the primary site of pathology. The issue lies in the upper airway (epiglottis), not lung compliance.
Take home points
- Airway obstruction is the leading risk in epiglottitis. Never attempt to visualize the throat without emergency airway equipment ready.
- Maintain the child in a sitting position, minimize agitation, and ensure humidified oxygen if tolerated.
- Notify the provider immediately since intubation or tracheostomy may be required.
- Routine Hib vaccination greatly reduces incidence.
The nurse is assessing a child recently brought to the emergency department. Which observations would cause the nurse to suspect epiglottitis?
Explanation
Epiglottitisis an acute, rapidly progressive, and life-threatening inflammation of the epiglottis, the flap of tissue at the base of the tongue that closes during swallowing. It is usually caused by Haemophilus influenzae type B (Hib). The inflammation leads to airway obstruction, making it a pediatric emergency.
Rationale for correct answer:
2. Droolingis a classic sign of epiglottitis. It occurs because the child cannot swallow due to painful, swollen structures and risk of airway obstruction. Along with drooling, dysphagia, distress, and dysphonia, and absence of spontaneous cough form the hallmark “4 D’s” of epiglottitis.
Rationale for incorrect answers:
1. In epiglottitis, secretions are not decreased; rather, they accumulate because the child cannot swallow, resulting in drooling.
3. Epiglottitis presents with a high feverand rapid onset of symptoms, not a mild or low-grade fever.
4. The cough is typicallyabsentin epiglottitis due to severe throat pain and airway obstruction. A spontaneous cough is more characteristic of laryngotracheobronchitis (croup).
Take home points
- Common epiglottitis signs include:
- Sudden onset of high fever
- Severe sore throat
- Dysphagia (difficulty swallowing)
- Drooling due to inability to swallow saliva
- Muffled voice ("hot potato" voice)
- Stridor and respiratory distress
- Tripod positioning (child leaning forward to facilitate breathing
Which strategy is the best plan of care for a child with acute epiglottitis?
Explanation
Acute epiglottitisis a medical emergencycaused by bacterial infection, most commonly Haemophilus influenzae type B (Hib), that leads to rapid inflammation and swelling of the epiglottis, threatening airway obstruction. Immediate management focuses on maintaining airway patencyand treating the infectionto prevent respiratory failure.
Rationale for correct answer:
3. Administering I.V. antibiotic therapyis the best plan of care once the airway is secured. I.V. antibiotics such as ceftriaxone or cefotaxime target the bacterial infection and reduce inflammation of the epiglottis. Early antibiotic therapy is critical to prevent complications such as airway obstruction, sepsis, or respiratory arrest.
Rationale for incorrect answers:
1. Encouraging oral fluids for hydrationis contraindicated in epiglottitis. Oral intake increases the risk of aspirationand airway obstructiondue to dysphagia and swelling. The child should be NPO (nothing by mouth) until the airway is secure.
2. The child should be allowed to assume a position of comfort, typically the tripod position, which optimizes airway patency and breathing. Forcing a semi-Fowler’s position may worsen distress.
4. While droplet precautionsare appropriate until the child has received 24 hours of antibiotic therapy, airway management and infection control through treatment are higher priorities. The isolation period depends on clinical progress and provider orders.
Take home points
- Airway maintenance and I.V. antibiotic therapy are the top priorities in acute epiglottitis.
- Never attempt throat inspection since it can precipitate complete airway blockage.
- Keep emergency airway equipment and intubation capability at the bedside.
- NPO status until airway patency is assured.
A 3-year-old child is given a preliminary diagnosis of acute epiglottitis. Which nursing intervention is appropriate?
Explanation
Acute epiglottitisis a life-threatening bacterial infectionof the upper airway, most commonly caused by Haemophilus influenzae type B (Hib). It leads to rapid swelling of the epiglottis and surrounding tissues, which can cause sudden airway obstruction.
Rationale for correct answer:
3. Don’t attempt to visualize the epiglottis: Attempting to visualize the throat with a tongue blade or any object can trigger laryngospasm or complete airway obstructiondue to the extreme sensitivity and swelling of the inflamed tissues. The airway must be managed only in a controlled setting, such as an operating room, with intubation or tracheostomy equipment immediately available.
Rationale for incorrect answers:
1. Obtain a throat culture immediately: Introducing a swab may stimulate reflex laryngospasm and precipitate total airway blockage. Cultures should only be obtained after the airway is secure.
2. Place the child in a side-lying position: The child should be allowed to assume a position of comfort(usually sitting upright or tripod position). Forcing another position can increase distress and worsen obstruction.
4. Use a tongue blade to look inside the throat: This can cause complete airway obstruction. Never use a tongue depressor to inspect the throat of a child suspected of having epiglottitis.
Take home points
- Never attempt to visualize or manipulate the throat in a child with suspected epiglottitis.
- Keep emergency airway equipment ready (intubation or tracheostomy).
- Do not leave the child unattended; keep the parent present to minimize anxiety.
- Administer humidified oxygen and prepare for I.V. antibiotics once the airway is secured.
An infant is brought to the clinic for her 6-month vaccines. The nurse tells the mother that administration of which vaccine is an appropriate step for prevention of epiglottitis?
Explanation
Epiglottitisis a severe, rapidly progressive bacterial infection that causes inflammation and swelling of the epiglottis, leading to potential airway obstruction. The most common causative organism is Haemophilus influenzae type B (Hib). Before widespread vaccination, epiglottitis was a major cause of pediatric airway emergencies, particularly in children aged 2–6 years.
Rationale for correct answer:
2. TheHaemophilus influenzae type B (Hib) vaccine directly protects against Haemophilus influenzae type B, the primary pathogen responsible for epiglottitis. The vaccine is administered at 2, 4, 6, and 12–15 monthsof age as part of the routine immunization schedule. It also prevents other serious Hib-related illnesses, including meningitis, pneumonia, cellulitis, and septic arthritis.
Rationale for incorrect answers:
1. Diphtheria vaccineprotects against Corynebacterium diphtheriae, which causes diphtheria, a throat infection that forms a gray pseudomembrane, not epiglottitis.
3. Measles vaccineprevents Rubeola (measles), a viral illness characterized by cough, coryza, conjunctivitis, Koplik spots, and rash, not epiglottitis.
4. Oral poliovirus vaccine (OPV)prevents poliomyelitis, a viral disease affecting the nervous system, leading to paralysis, and is not related to Haemophilus influenzaeinfection or epiglottitis.
Take home points
- Hib vaccine is the most effective preventive measure against epiglottitis and other invasive Hib infections.
- Routine vaccination at 2, 4, 6, and 12–15 months is essential.
- Since Hib vaccination became standard, epiglottitis has become rare in immunized populations.
- Always verify the child’s immunization status during health visits to ensure complete protection.
A nurse in the emergency department is caring for a 4-year-old client sited in a tripod position with a muffled voice, drooling and a respiratory rate of 68 breaths/minute. Which of the following actions should the nurse implement first?
Explanation
This child is exhibiting classic signs of acute epiglottitis, a life-threatening bacterial that causes severe inflammation and swelling of the epiglottis. Hallmark symptoms include: muffled ("hot potato") voice, drooling, stridor or respiratory distress, and tachypnea.
Rationale for correct answer:
3. Airway protection is the first and most urgent priority. Children with epiglottitis can rapidly deteriorate and experience complete airway obstruction. The child’s tripod position,respiratory rate of 68and droolingsignal severe distress. Intubation should be performed in a controlled environment, ideally in the OR with pediatric anesthesia and ENT on standby.
Rationale for incorrect answers:
1. IV accessis important for medications and fluids but should not delay airway management in a child at risk for obstruction. Furthermore, delay of IV access is often recommended until the airway has been secure since agitating the child could result in laryngeal spasms worsening the condition.
2. Administer IV ceftriaxone as orderedis essential for treating the underlying infection, but administering them before securing the airway is dangerous if the airway closes.
4. Prepare the child for a lateral neck radiographcan help confirm diagnosis, but delaying airway intervention to obtain imaging can be fatal. Moving a distressed child could worsen airway compromise.
Take home points
- Acute epiglottitis is an airway emergency. Immediate airway support is critical.
- Do not delay airway intervention for IV access, antibiotics, or diagnostic tests.
- Classic signs: muffled voice, drooling, tripod positioning, and no cough.
- Always prioritize ABC (Airway, Breathing, Circulation), airway first.
A nurse is precepting a student nurse caring for a child with epiglottitis. Which of the following actions by the student nurse requires intervention? Select all that apply
Explanation
Epiglottitisis a medical emergency characterized by sudden inflammation of the epiglottis causing airway obstruction. Management focuses on maintaining airway patency and minimizing distress.
Rationale for correct answers:
1. Placing the child in a supine positioncan worsen airway obstruction. Children with epiglottitis prefer to sit upright or lean forward (tripod position) to ease breathing.
2. Throat examination or swabbingcan trigger laryngospasm and complete airway obstruction; it is contraindicated unless performed by an experienced provider in a controlled environment.
4. Encouraging the child to drink small sips of warm watermay increase risk of choking or aspiration due to difficulty swallowing and airway compromise. Fluids are usually withheld until airway is secure.
Rationale for incorrect answers:
3. Availing intubation equipment at the bedsideis essential preparation to manage sudden airway obstruction.
5. Allowing the caregiver to stay with the childprovides comfort and reduces anxiety, which can help prevent airway spasm.
Take home points
- Avoid any procedures or positions that may distress the child or worsen airway obstruction.
- Keep the child calm and in a position of comfort (usually upright or tripod).
- Do not attempt throat examination or swabbing outside a controlled setting.
- Always prepare for emergency airway management with equipment and skilled personnel readily available.
A nurse is caring for a 3-year-old client with epiglottitis. Which of the following equipment should the nurse avail in the client’s bedside? Select all that apply
Explanation
Epiglottitisis a rapidly progressing, life-threatening condition characterized by inflammation and swelling of the epiglottis, which can cause sudden airway obstruction. Because of the high risk of airway compromise, emergency airway management equipment must be immediately available at the bedside.
Rationale for correct answers:
1. A tracheostomy trayshould be readily available because if intubation is impossible due to severe upper airway swelling, an emergency surgical airway (tracheostomy) may be necessary to secure the airway.
3. Bag-valve mask(BVM)is essential for providing assisted ventilation if the child develops respiratory failure or apnea before or during airway management.
4. Supplemental oxygenshould be available to maintain adequate oxygenation and relieve hypoxia caused by airway obstruction.
Rationale for incorrect answers:
2. Use of a tongue depressoris contraindicated because it can trigger gagging, laryngospasm, or complete airway obstructionin a child with epiglottitis. The inflamed epiglottis is very sensitive, and oral examination should be avoided unless performed by an experienced provider in a controlled environment.
5. Albuterol nebulizationis not indicated in epiglottitis because the airway obstruction is caused byinflammation and swelling of the epiglottis, not bronchospasm or lower airway disease. Nebulizer treatments may increase agitation and worsen respiratory distress.
Take home points
- Always have emergency airway management equipment ready at the bedside for a child with epiglottitis.
- Avoid oral airway examination or interventions that can provoke airway spasm.
- Supplemental oxygen and ventilation support should be immediately accessible.
- Nebulized bronchodilators are not useful in epiglottitis and may be harmful.
Practice Exercise 2
A child is seen in the emergency department. The nurse hears a high-pitched squeal every time the child inhales. The parent states that the child’s fever is very high and, in addition, the child is gasping for breath and sitting in the tripod position. Which of the following actions would be appropriate for the nurse to perform at this time?
Explanation
The child’s presentation of a high-pitched inspiratory squeal (stridor), high fever, gasping for breath, and tripod positioningare classic signs of severe upper airway obstruction, possibly caused by epiglottitis or another critical airway emergency. This situation requires urgent medical interventionto secure the airway and stabilize the child.
Rationale for correct answer:
4. The child is showing signs of respiratory distress with potential airway obstruction, which is a life-threatening emergency. Immediate medical attention is necessary to prepare for airway management and advanced interventions, including possible intubation or emergency airway procedures. Delays in obtaining help increase the risk of airway compromise and respiratory failure.
Rationale for incorrect answers:
1. Offering liquids to a child with airway obstruction and respiratory distress risks aspiration and worsened airway compromise. The child may be unable to swallow safely.
2. Inspecting the throat with a flashlight and tongue bladecan trigger gagging or laryngospasm, leading to sudden airway obstruction and respiratory arrest in a child with suspected epiglottitis or similar airway obstruction. Throat inspection should only be performed by experienced providers in a controlled environment with airway equipment ready.
3. While vital signs and lung auscultation are important, the immediate priority is securing airway and emergency care. Assessment should not delay urgent intervention.
Take home points
- Signs of airway obstruction with respiratory distress require immediate medical attention and emergency airway management.
- Avoid oral examinations or giving fluids in children with suspected epiglottitis or severe airway obstruction.
- Prompt recognition and action can prevent respiratory failure and death.
The parent of an 18-month-old-child calls the child’s primary health-care provider and states, “My child coughed all night long. She doesn’t seem to be too sick, and she has no temperature. What can I do to help her and the rest of us to sleep tonight?” Which of the following responses is appropriate for the nurse to make?
Explanation
A nighttime cough in a young child without fever often indicates mild upper respiratory irritation or postnasal drip. Non-pharmacologic comfort measures can help reduce coughing and promote better sleep without unnecessary medication.
Rationale for correct answer:
3. Raising the head of the baby’s crib can help reduce coughingby promoting drainage of nasal secretions and reducing postnasal drip that irritates the throat. This simple intervention is safe, non-invasive, and can improve the child’s comfort and sleep quality.
Rationale for incorrect answers:
1. Steam vaporizersplaced too close can cause burns or be a safety hazard. Cold mist humidifiers used properly can help, but the placement should be safe and not directly next to the child’s face or crib.
2. Nonprescription cough and cold medicinesare not recommended for children under 2 years due to lack of efficacy and potential serious side effects. The FDA advises against their use in infants and toddlers.
4. Antibioticsare not appropriate without signs of bacterial infection such as fever or purulent symptoms. Most coughs in toddlers are viral and self-limiting.
Take home points
- For mild nighttime cough without fever in toddlers, non-pharmacologic measures like elevating the head of the crib can improve comfort.
- Avoid over-the-counter cough and cold medicines in children under 2 due to safety concerns.
- Antibiotics should not be prescribed unless bacterial infection is clearly suspected.
Which of these factors contributes to infants’ and children's increased risk for upper airway obstruction as compared with adults?
Explanation
Infants and young children have anatomical and physiological differences in their upper airways compared to adults that increase their risk for airway obstruction. These differences include a smaller and more flexible airway structure and narrower passages, which make them more vulnerable to swelling and obstruction.
Rationale for correct answer:
1. Underdeveloped cricoid cartilage and narrow nasal passagescontribute significantly to the increased risk of upper airway obstruction in infants and children. The cricoid cartilageis the narrowest part of a child’s airway and is less rigid than in adults, making it more prone to collapse or swelling. Narrow nasal passagescan become easily blocked by secretions or inflammation, further compromising airflow.
Rationale for incorrect answers:
2. Tonsils in children tend to be relatively large, not small, and can contribute to obstruction. The nasal passages are narrow, but this option misses the critical role of cricoid cartilage development.
3. The child’s larynx is funnel-shaped, not cylindrical, with the narrowest point at the cricoid cartilage. While sinuses develop over time, their underdevelopment doesn’t directly increase risk of upper airway obstruction.
4. Children actually have proportionally larger tonguesrelative to their oral cavity, which can contribute to obstruction, so “smaller tongue” is inaccurate.
Take home points
- Infants and children have a funnel-shaped, narrower airway with a less rigid cricoid cartilage, making them more susceptible to airway obstruction.
- Narrow nasal passages add to the risk by limiting airflow, especially during inflammation.
- Understanding these anatomical differences is critical when assessing respiratory distress in pediatric patients.
A parent brings her child to the pediatrician’s office because of difficulty breathing and a “barking” cough. These signs are associated with which of the following conditions?
Explanation
Croup (laryngotracheobronchitis)is a viral infection (commonly caused by the parainfluenza virus) that leads to inflammation and narrowing of the larynx and trachea, resulting in upper airway obstruction.
It typically affects children between 6 months and 3 years old. Symptoms are often worse at night and may follow an upper respiratory infection.
Rationale for correct answer:
4. The hallmark signs, barking cough and difficulty breathing, are classic indicators of croup. The cough results from laryngeal swelling, and inspiratory stridor occurs due to narrowing of the upper airway. Treatment typically includes humidified air, corticosteroids (e.g., dexamethasone), and, in moderate to severe cases, nebulized epinephrine to reduce airway edema.
Rationale for incorrect answers:
1. Cystic fibrosisis a genetic disorder causing thick mucus secretions affecting the lungs and pancreas. It presents with chronic cough, recurrent infections, and malabsorption, not a barking cough or acute airway obstruction.
2. Asthma causes wheezing, shortness of breath, and chest tightness due to lower airway bronchoconstriction, not a barking cough or stridor.
3. Epiglottitispresents with drooling, dysphagia, high fever, tripod positioning, and absence of cough not a barking cough. It’s a medical emergency due to risk of complete airway obstruction.
Take home points
- Barking cough and stridor are hallmark signs of croup which is viral and usually mild to moderate.
- Drooling, no cough, and high fever are symptoms of epiglottitis a bacterial emergency.
- Wheezing and chest tightness are typical of asthma.
- Chronic productive cough and malabsorption are symptoms of cystic fibrosis.
Which action is the best intervention for parents to take if their child is experiencing an episode of “midnight croup,” or acute spasmodic laryngitis?
Explanation
Acute spasmodic laryngitis (midnight croup)is a sudden-onset, viral-induced laryngeal inflammation that typically occurs at night in children aged 1–3 years. It presents with a barking, seal-like cough, inspiratory stridor, and respiratory distress. This condition is usually mild and self-limiting, often managed at home with supportive care.
Rationale for correct answer:
3. Cool misthelps reduce mucosal swellingand soothe inflamed airways, easing breathing and decreasing cough intensity. Exposure to cool, humid air, such as from a cool-mist vaporizer or stepping outside into the night air, can relieve laryngeal spasm and inflammation. This is the first-line, noninvasive management for mild croup episodes at home.
Rationale for incorrect answers:
1. Giving oral fluidsduring acute respiratory distress increases the risk of aspiration. Oral intake should be avoided until the child’s breathing improves and the airway is stable.
2. Warm, dry aircan worsen airway inflammationand dry out secretions, making symptoms worse. The goal is cool, moist air, not warm air.
4. Although warm mistwas once recommended, cool mist is now preferred because it is safer and equally effective. Warm mist can sometimes increase swelling in the inflamed airway and poses a burn risk.
Take home points
- Cool, humidified air is the best nonpharmacologic intervention for mild croup (spasmodic laryngitis).
- Avoid warm air and warm fluids during acute distress.
- Monitor for signs of worsening airway obstruction such as stridor at rest, retractions, cyanosis, and drooling, these require emergency medical evaluation.
- Calm reassurance and keeping the child in an upright position can also reduce airway spasms and distress.
Which sign should alert a nurse that an 18-month-old child with croup is experiencing increased respiratory distress?
Explanation
Croup (laryngotracheobronchitis)is a viral infectioncommonly caused by the parainfluenza virusthat causes inflammation and narrowing of the larynx, trachea, and bronchi, leading to upper airway obstruction. Typical signs include barking cough, inspiratory stridor, and hoarseness.
Rationale for correct answer:
2. Intercostal retractionsindicate increased work of breathing and use of accessory muscles due to airway narrowing or obstruction. This is a sign of worsening respiratory distress in a child with croup and warrants immediate evaluation and possible medical intervention such as nebulized epinephrine or corticosteroids. Retractions occur because the child’s compliant chest wall is pulled inward during inspiration as airway resistance increases.
Rationale for incorrect answers:
1. The barking, seal-like coughis a typical feature of croup, but by itself does not indicate worsening distress. It is a baseline symptom, not a progression sign.
3. Clubbing of the fingersindicates chronic hypoxemia from long-term respiratory disease such as cystic fibrosis, or congenital heart disease. It does not develop acutely in croup.
4. Increased anterior-posterior chest diameteroccurs with chronic obstructive conditions such as asthma or cystic fibrosis due to air trapping over time, not with acute viral croup.
Take home points
- Retractions, nasal flaring, stridor at rest, and restlessness signal increasing respiratory distress in children with croup.
- Prompt recognition and intervention are essential to prevent airway compromise.
- Mild croup: barking cough, stridor only with activity.
- Severe croup: stridor at rest, marked retractions, agitation, possible cyanosis, requires emergency treatment.
Which precaution is recommended when caring for children with respiratory infections such as croup?
Explanation
Croup(laryngotracheobronchitis)is a viral respiratory infection, most often caused by the parainfluenza virus. It is highly contagiousand spreads through respiratory dropletsand direct contactwith contaminated surfaces.
Rationale for correct answer:
1. Hand hygieneis the most effective infection-control measure for preventing the spread of viral respiratory illnesses such as croup. Viruses are easily transmitted through touching contaminated hands, toys, or surfaces, and frequent hand washing with soap and water minimizes transmission. Hand hygiene should be performed before and after contact with the child or their environment.
Rationale for incorrect answers:
2. Isolationis not routinely required for croup unless another specific infection (like RSV or influenza) is suspected or confirmed. Standard precautionswith hand hygiene and droplet precautions if coughing/sneezing are usually sufficient.
3. Whileteaching children to use tissues ishelpful for older children, an 18-month-old or young child may not effectively use tissues or practice good respiratory hygiene. Teaching tissues alone is not adequate to prevent transmission.
4. Keeping siblings in the same room increases the risk of cross-infection, as croup is contagious. Siblings, especially those who are young or immunocompromised, should be kept apart during the illness.
Take home points
- Hand washing is the single most effective way to prevent the spread of respiratory infections like croup.
- Standard precautions should be followed by avoiding close contact, cleaning toys/surfaces, and encouraging covering the mouth when coughing.
- Droplet precautions may be added in healthcare settings if the child is coughing or sneezing.
- Good hygiene practices protect both family members and healthcare providers from infection.
What is the best time to administer a nebulizer treatment to a child with croup?
Explanation
Croup (laryngotracheobronchitis)is a viral infectioncommonly caused by the parainfluenza virusthat causes inflammation and narrowing of the larynx, trachea, and bronchi, leading to upper airway obstruction. Typical signs include barking cough, inspiratory stridor, and hoarseness. Nebulized treatmentssuch as racemic epinephrinehelp reduce airway edemaand ease breathing.
Rationale for correct answer:
1. During naptime: Administering the nebulizer while the child is calm or asleep reduces agitation, crying, and airway stress, which can worsen obstruction in croup. Ensures effective delivery of the medication without struggle or additional respiratory distress. Children are often more tolerant of nebulization when relaxed, which improves outcomes.
Rationale for incorrect answers:
2. During playtime: The child may be active and uncooperative, making treatment less effective and potentially stressful.
3. After the child eats: Treatment immediately after meals may increase risk of vomiting or aspiration.
4. After the parents leave: Young children need parental reassurance during respiratory treatment. Administering nebulizers in the parent’s absence can increase anxiety and worsen symptoms.
Take home points
- Calm, relaxed children respond better to nebulizer treatments.
- Administering during naptime minimizes stress and agitation, improving airway safety and medication effectiveness.
- Always monitor respiratory status during and after the treatment.
- Ensure parental presence and reassurance to reduce anxiety.
A nurse in the pediatric unit is caring for a child with croup. Which of the following interventions should the nurse include in the plan of care? Select all that apply
Explanation
Croup is an inflammatory condition causing upper airway narrowing that leads to respiratory distress in children. Treatment focuses on reducing airway swelling and ensuring adequate oxygenation.
Rationale for correct answers:
1. Nebulized epinephrinecauses vasoconstrictionof the swollen mucosa, reducing airway edema and improving breathing rapidly in moderate to severe cases of croup.
2. Dexamethasoneis a corticosteroid that helps reduce airway inflammationover several hours, leading to sustained improvement in symptoms.
4. Supplemental oxygen, especially humidified, helps relieve hypoxia and soothes irritated airways, supporting respiratory effort.
Rationale for incorrect answers:
3. Warm mist therapy is no longer routinely recommended as evidence does not show clear benefit, and some children tolerate it poorly. Cool mistmay be more soothing but is not the priority intervention.
5. Activity should be limited during respiratory distress to prevent worsening of symptoms and conserve energy.
Take home points
- Nebulized epinephrine and corticosteroids are cornerstone therapies to reduce airway swelling in croup.
- Humidified oxygen supports oxygenation but is not a substitute for medications.
- Avoid activities that increase oxygen demand during acute illness.
A nurse is caring for a child with croup presenting with a barking cough. The parents are concerned about the child’s alarming cough. Which of the following explanation behind the cough should the nurse provide?
Explanation
Croupis a viral infection that causes inflammation and swelling of the upper airway structures, especially the larynx, trachea, and sometimes bronchi, resulting in the characteristic barking cough and respiratory symptoms.
Rationale for correct answer:
3. “The cough is caused by inflammation and swelling in the trachea and the bronchi, leading to airway narrowing.”The hallmark barking coughof croup occurs because inflammation narrows the airway, causing turbulent airflow and irritation that triggers the cough reflex. This swelling reduces the airway diameter, producing the distinctive "seal-like" sound and respiratory distress.
Rationale for incorrect answers:
1. “The cough indicates a severe allergic reaction that is causing the airways to constrict rapidly.”While allergic reactions can cause airway constriction, the croup cough is not due to an allergic process but an inflammatory viral infection.
2. “The cough is a reflex to clear mucus and other secretions from the lungs in children with a respiratory illness.”The cough in croup is primarily due to upper airway narrowing, not just mucus clearance from the lungs.
4. “The child is making this sound due to anxiety and distress about their condition.”Anxiety may worsen respiratory symptoms but is not the cause of the characteristic barking cough.
Take home points
- The barking cough in croup is caused by inflammation and swelling of the upper airway leading to narrowing.
- Understanding this helps caregivers appreciate the importance of treatment to reduce airway edema.
- Reassure parents that the cough is a sign of the body’s response to airway irritation, not anxiety or allergy.
A nurse is proving discharge education to the caregivers of a toddler managed with croup. Which of the following caregiver statements indicate effective teaching? Select all that apply
Explanation
Croupis a common respiratory illness in toddlers characterized by a barking cough, often caused by viral inflammation leading to airway narrowing. Discharge teaching focuses on home management and recognizing signs of worsening illness.
Rationale for correct answers:
1. Cool mist helps soothe inflamed airwaysand can reduce airway irritation, making breathing easier. It is a safe, non-invasive home therapy to help alleviate symptoms.
3. Stridor at restindicates significantairway obstructionand respiratory distress that requires urgent medical evaluation to prevent respiratory failure.
4. Adequate hydration thins mucus secretions, prevents dehydration, and supports overall recovery.
Rationale for incorrect answers:
2. Over-the-counter cough syrups are not recommended for young children due to limited efficacy and potential side effects.
5. Aspirinis contraindicated in children because of the risk of Reye’s syndrome, a serious and potentially fatal condition.
Take home points
- Use cool-mist humidifiers and maintain hydration to support symptom relief in croup.
- Recognize signs of respiratory distress such as stridor at rest and seek emergency care promptly.
- Avoid cough syrups and aspirin in young children.
Comprehensive Questions
Which sign in a 3-year-old child with acute epiglottitis indicates that the client’s respiratory distress is increasing?
Explanation
Acute epiglottitisis a life-threatening bacterial infection(commonly due to Haemophilus influenzae type B) that causes inflammation and swelling of the epiglottis, leading to rapid airway obstruction. It primarily affects children aged 2–6 years and presents with sudden onset of high fever, drooling, dysphagia, muffled voice, and inspiratory stridor.
Rationale for correct answer:
3. Increasing heart rateis an early and sensitive indicator of worsening hypoxia and respiratory distressin children. As oxygen levels drop, the heart rate rises in an attempt to maintain oxygen delivery to vital organs. If untreated, tachycardia may later progress to bradycardia and cardiac arrest, a late and ominous sign of severe hypoxia.
Rationale for incorrect answers:
1. A barking (seal-like) coughis characteristic of croup (laryngotracheobronchitis), not epiglottitis. Children with epiglottitis typically have no coughor a muffled voicedue to painful swallowing and airway swelling.
2. While irritabilitymay occur as a response to hypoxia, it is a nonspecific early sign. The increase in heart rate provides a more objective and direct indicator of escalating respiratory distress.
4. Coughingis usually absent in epiglottitis because of pain and airway obstruction. Productive coughs are more typical in lower respiratory infections, such as pneumonia or bronchitis.
Take home points
- Tachycardia and restlessness are early signs of hypoxia; bradycardia and cyanosis are late, preterminal signs.
- In epiglottitis, airway obstruction can progress rapidly hence continuous monitoring of respiratory rate, heart rate, and oxygen saturation is essential.
- Avoid procedures that agitate the child; maintain airway equipment and intubation readiness at the bedside.
- Early recognition and I.V. antibiotic therapy after securing the airway are key to recovery.
While examining a child with acute epiglottitis, a nurse should have which item available?
Explanation
Acute epiglottitisis a medical emergencycaused primarily by Haemophilus influenzae type B (Hib)infection. The inflamed epiglottis can rapidly swell, leading to sudden and complete airway obstruction.
Typical presentation includes sudden onset of high fever, drooling, severe sore throat, dysphagia, muffled voice, stridor, tripod positioning, and absence of cough.
Rationale for correct answer:
2. Intubation equipment: The nurse must have intubation or tracheostomy equipment immediately available when examining a child with suspected epiglottitis. The airway can obstruct suddenly and completely, even with minimal stimulation. Intubation should be performed only by an experienced provider (e.g., anesthesiologist, critical care physician) in a controlled environment. Equipment should include an appropriate-size endotracheal tube, laryngoscope, suction setup, and emergency tracheostomy kit.
Rationale for incorrect answers:
1. Cool mist tent: Humidified air may provide comfort in mild respiratory conditions (e.g., croup), but in epiglottitis, it is not the priority. Airway maintenance supersedes all comfort measures.
3. Tongue blades: Using a tongue blade to inspect the throat can trigger laryngospasm or complete airway obstruction. The throat must never be examined until airway control is secured.
4. Viral culture medium: Epiglottitis is caused by a bacterial pathogen, not a virus, so viral cultures are unnecessary and would delay emergency treatment.
Take home points
- Always have emergency airway equipment ready when epiglottitis is suspected.
- Never attempt to visualize the throat or insert objects into the mouth.
- Do not leave the child unattended. Always keep the parent nearby to reduce anxiety.
- Prepare for immediate intubation and administer I.V. antibiotics once the airway is secure.
A 2-year-old child is brought to the emergency department in respiratory distress. The child is drooling, sitting upright and leaning forward with chin thrust out, mouth open, and tongue protruding. Which nursing intervention is most appropriate?
Explanation
Acute epiglottitisis a life-threatening bacterial infection, most commonly caused by Haemophilus influenzae type B (Hib), that leads to rapid inflammation and swelling of the epiglottis, causing airway obstruction. Typical presentation includes sudden onset of high fever, drooling, severe sore throat, dysphagia, muffled voice, stridor, tripod positioning, absence of cough, anxiety and restlessness due to respiratory distress.
Rationale for correct answer:
4. Support the child in an upright position on the parent’s lap: This position helps maximize airway patencyand reduce respiratory effort. Allowing the child to remain with the parent provides comfort, minimizing crying and agitation, which can worsen airway obstruction. The nurse should stay calm, avoid unnecessary interventions, and notify the healthcare provider immediately for airway management (possible intubation).
Rationale for incorrect answers:
1. Check the child’s gag reflex with a tongue blade: Inserting anything into the mouth may trigger laryngospasm and complete airway obstruction. The throat should never be examined unless the airway is secure and emergency personnel are present.
2. Allow the child to cry to keep the lungs expanded: Crying increases airway edema and oxygen demand, potentially precipitating complete obstruction. The goal is to keep the child calm and quiet.
3. Check the airway for a foreign body obstruction:Although drooling and respiratory distress may resemble choking, in this case the classic tripod position and drooling point to epiglottitis, not a foreign body. Any airway manipulation could be fatal.
Take home points
- Never attempt to visualize or manipulate the throat in suspected epiglottitis.
- Keep emergency airway equipment (intubation and tracheostomy setup) immediately available.
- Do not leave the child unattended; stay calm and allow the parent to remain close.
- Prepare for immediate intubation and I.V. antibiotic therapy once the airway is secure.
Which assessment is of greatest concern in a 15-month-old?
Explanation
Acute epiglottitisis a medical emergencymost often caused by Haemophilus influenzae type B (Hib). It results in rapid swelling of the epiglottis, leading to airway obstruction. Typical presentation includes sudden onset of high fever, drooling, severe sore throat, dysphagia, muffled voice, stridor, tripod positioning, absence of cough, anxiety and restlessness due to respiratory distress.
Rationale for correct answer:
2. The child is in the tripod position and has diminished breath sounds and a muffled cough: This finding indicates severe airway obstruction and impending respiratory failure. Tripod position and muffled cough are hallmark signs of epiglottitis. Diminished breath soundssignal that air movement is critically reduced, a life-threatening emergency requiring immediate airway management and preparation for intubation. The child should not be examined or agitated; emergency airway equipment should be ready, and the provider notified immediately.
Rationale for incorrect answers:
1. The child is lying down and has moderate retractions, low-grade fever, and nasal congestion: This is consistent with nasopharyngitis (common cold) or mild upper respiratory infection, not an emergency. The airway is patent.
3. The child is sitting up and has coarse breath sounds, coughing, and fussiness: These findings are more consistent with bronchiolitis or viral croup, which cause airway inflammation but typically have a characteristic cough and coarse sounds, not a muffled voice or tripod positioning.
4. The child is restless and crying, has bilateral wheezes, and is feeding poorly: This presentation suggests asthma or reactive airway disease, not epiglottitis. While concerning, wheezing indicates air is still moving, unlike the silent chest seen in impending obstruction from epiglottitis.
Take home points
- Tripod position, muffled voice, and diminished breath sounds signify airway emergency.
- Do not attempt throat inspection or use a tongue blade since this can trigger complete obstruction.
- Keep emergency intubation and tracheostomy equipment ready at the bedside.
- Calm the child, avoid unnecessary interventions, and notify the provider immediately.
Which is diagnostic for epiglottitis?
Explanation
Epiglottitisis a life-threatening bacterial infection(commonly caused by Haemophilus influenzae type B) that leads to inflammation and swelling of the epiglottis, potentially causing complete airway obstruction. It most often affects children aged 2–6 years and presents with sudden onset of high fever, drooling, dysphagia, muffled voice, and tripod positioning.
Rationale for correct answer:
3. A lateral neck x-raycan confirm the diagnosis by revealing the classic “thumbprint sign”, which represents an enlarged, swollen epiglottis protruding into the airway. This imaging study helps differentiate epiglottitis from croup, which shows a “steeple sign” (subglottic narrowing). Importantly, the x-ray should only be performed after the airway is stabilized and under controlled conditions with emergency equipment and personnel available.
Rationale for incorrect answers:
1. Blood testsuch as CBC or cultures may show infection but are nonspecific and not diagnostic. They are typically performed after the airway is secure.
2. Swabbing or inspecting the throatare contraindicated since it can trigger laryngospasmand complete airway obstructiondue to tissue irritation.
4. Although signs and symptoms such as drooling, tripod position, muffled voice, or stridor are strongly suggestive, a definitive diagnosis requires visualization or imaging. They should be safely done through a lateral neck x-ray or direct laryngoscopy in a controlled setting.
Take home points
- Lateral neck x-ray showing the “thumbprint sign” confirms epiglottitis.
- Never use a tongue blade or obtain a throat swab since both can precipitate complete obstruction.
- Ensure emergency airway equipment is available before any diagnostic procedure.
- Immediate I.V. antibiotics and airway management are key to treatment.
What should be the nurse’s first action with a child who has a high fever, dysphagia, drooling, tachycardia, and tachypnea?
Explanation
These findings, high fever, dysphagia, drooling, tachycardia, and tachypnea, are classic signs of acute epiglottitis, a life-threatening airway emergency. The inflamed epiglottis can rapidly obstruct the airway, leading to respiratory arrest if not managed immediately.
Rationale for correct answer:
2. The priority is airway maintenancewhich takes precedence over all other actions. The nurse should ensure the airway remains openand support the child in an upright position, avoiding any agitation or procedures that might worsen obstruction. Notify the provider and prepare emergency airway equipment (intubation or tracheostomy tray) immediately. Oxygen may be given by blow-by, but no invasive airway procedures (like suctioning or tongue inspection) should be attempted until the airway is secured by an experienced provider.
Rationale for incorrect answers:
1. Starting an IVrequires restraint and may agitate the child, causing airway spasm and obstruction. IV access should only be obtained after the airway is secured.
3. Attempting a detailed assessment, especially of the throat, is dangerous, even minor throat manipulation can trigger complete airway obstruction. The assessment should be brief, observational, and noninvasiveuntil airway stability is ensured.
4. Although lateral neck radiographscan confirm the diagnosis (showing the thumbprint sign), it should only be done after airway stabilization and in a controlled setting (e.g., radiology or OR) with emergency equipment available.
Take home points
- Airway management is the top priority in suspected epiglottitis.
- Do not attempt throat examination or IV insertion before securing the airway.
- Prepare for emergency intubation or tracheostomy. Ensure skilled personnel and equipment are available.
- Administer oxygen cautiously and notify the provider immediately for airway intervention.
Which is the nurse’s best response to the parent of a child diagnosed with epiglottitis who asks what the treatment will be?
Explanation
Epiglottitisis a bacterial infection causing inflammation and swelling of the epiglottis, leading to airway obstruction. It is most commonly caused by Haemophilus influenzae type B (Hib), though Streptococcusand Staphylococcusspecies can also be responsible. This is a medical emergency that requires immediate airway management and antibiotic therapy to eliminate infection and prevent recurrence.
Rationale for correct answer:
1. Once the airway is secured, treatment includes IV broad-spectrum antibioticssuch as ceftriaxone or cefotaxime, followed by oral antibiotics to complete a7–10-day course. Antibiotics are essential to eradicate the infection, reduce inflammation, and prevent complications like sepsis or meningitis. Supportive care includes oxygen, IV fluids, and close airway monitoring in an intensive care setting.
Rationale for incorrect answers:
2. Tonsillectomyis not indicated for epiglottitis. The tonsils are not involved in this infection, and surgery could worsen airway swelling or obstruction.
3. Ribavirinis an antiviral medication used for respiratory syncytial virus (RSV), not for bacterial infections like epiglottitis.
4.Epiglottitis requires urgent intervention. Without prompt treatment, airway obstruction and death can occur rapidly. Observation alone is unsafe and inappropriate.
Take home points
- Immediate airway management is the top priority in epiglottitis.
- IV antibiotics such as ceftriaxone and cefotaxime are the mainstay of treatment.
- Never perform throat examination or delay antibiotics for diagnostic testing.
- Hib vaccination is the key preventive measure.
A mother is crying and tells the nurse that she should have brought her son in yesterday when he said his throat was sore. Which is the nurse’s best response to this parent whose child is diagnosed with epiglottitis and is in severe distress and in need of intubation?
Explanation
Epiglottitisis a life-threatening bacterial infection(commonly caused by Haemophilus influenzae type B) that causes rapid inflammation and swelling of the epiglottis, leading to airway obstruction. The illness progresses suddenly and severely, often within hours, and requires immediate airway management and IV antibiotic therapy.
Rationale for correct answer:
4. “Epiglottitis is rapidly progressive; you could not have predicted his symptoms would worsen so quickly.”This response provides emotional support and reassurance to the parent. It helps alleviate guilt by explaining that the condition worsens very rapidly, often within hours, and that early recognition is difficult. The nurse is showing empathy, validating the parent’s feelings while maintaining focus on the child’s urgent care needs.
Rationale for incorrect answers:
1. “Children this age rarely get epiglottitis; you should not blame yourself.”While reassuring, this statement is inaccurate. Epiglottitis most commonly affects children ages 2 to 6 years. It also minimizes the parent’s emotions rather than addressing them therapeutically.
2. “It is always better to have your child evaluated at the first sign of illness rather than wait until symptoms worsen.”This is non-therapeutic and blaming, implying that the parent’s delay contributed to the severity of the illness. It increases guilt instead of offering comfort.
3. “Epiglottitis is slowly progressive, so early intervention may have decreased the extent of your son’s symptoms.”This is factually incorrect since epiglottitis progresses rapidly, not slowly. Such misinformation may increase the parent’s distress.
Take home points
- Epiglottitis is a medical emergency that can progress from mild sore throat to severe airway obstruction within hours.
- The nurse’s role includes both clinical vigilance and emotional support for the family.
- Therapeutic communication focuses on reassurance, empathy, and education without assigning blame.
- Early recognition and prompt airway management are critical for survival.
Which child is in the greatest need of emergency medical treatment?
Explanation
Epiglottitisis a life-threatening bacterial infection—most commonly due to Haemophilus influenzae type B (Hib), that causes inflammation and swelling of the epiglottis, leading to airway obstruction. Typical presentation includes sudden onset of high fever, drooling, severe sore throat, dysphagia, muffled voice, stridor, tripod positioning, absence of cough, anxiety and restlessness due to respiratory distress.
Rationale for correct answer:
2. A 6-year-old who has high fever, no spontaneous cough, and frog-like croaking: These are classic signs of acute epiglottitis and signal imminent airway obstruction. The absence of a cough differentiates it from croup, and the frog-like croak indicates severe upper airway involvement. The child is in extreme danger of airway closure and requires immediate airway management and emergency medical treatment, often including intubation or tracheostomy and IV antibiotics.
Rationale for incorrect answers:
1. A 3-year-old who has a barky cough, is afebrile, and has mild intercostal retractions: This presentation is typical of mild viral croup (laryngotracheobronchitis). The child is stable and can usually be managed with humidified air or nebulized epinephrine, not an emergency.
3. A 7-year-old who has abrupt onset of moderate respiratory distress, a mild fever, and a barky cough: Although the child has distress, the presence of a barky cough indicates croup, not epiglottitis. Treatment includes corticosteroids and nebulized epinephrine, but it’s not as emergent as airway obstruction from epiglottitis.
4. A 13-year-old who has a high fever, stridor, and purulent secretions: This presentation suggests bacterial tracheitis, a serious but slower-progressing condition than epiglottitis. Requires IV antibiotics and airway monitoring, but it does not progress to complete airway obstruction as rapidly as epiglottitis.
Take home points
- Epiglottitis is an emergency. Look for high fever, drooling, no cough, muffled or croaking voice.
- Never attempt to examine the throat since this may trigger complete airway obstruction.
- Immediate airway stabilization and IV antibiotics are priorities.
- Rapid recognition and intervention are life-saving in epiglottitis.
A 4-year-old female child presents to the emergency department with a sore throat, difficulty swallowing, and a suspected diagnosis of acute epiglottitis. Which information should be included in the initial assessment of the child? Select all that apply
Explanation
Acute epiglottitisis a life-threatening bacterial infection(commonly caused by Haemophilus influenzae type B) resulting in rapid swelling of the epiglottis and potential airway obstruction. Initial assessment focuses on airway stability, respiratory status, and overall clinical condition, while avoiding procedures that may trigger laryngospasm or complete obstruction.
Rationale for correct answers:
2. Vital signsare essential to assess respiratory rate, heart rate, oxygen saturation, and temperature. Provides baseline data to monitor severity and guide interventions.
3. Past medical historyhelps identify risk factors, previous respiratory illnesses, immunization status (especially Hib), and allergies. Relevant for planning treatment and monitoring.
4. Assessing breath soundshelps detect airway compromise, stridor, or decreased airflow. Noninvasive assessment is safe if done gently without triggering airway obstruction.
5. Drooling, difficulty swallowing, or refusal to eat/drinkindicates airway compromise and severity of epiglottitis. Important for deciding airway management priority.
Rationale for incorrect answer:
1. Throat cultureis contraindicated in acute epiglottitis. Attempting to visualize or swab the throat may precipitate complete airway obstruction. Diagnosis is made clinically and/or by lateral neck x-ray once the airway is stabilized.
Take home points
- Airway assessment and stabilization are the top priorities in epiglottitis.
- Noninvasive observations like vital signs, swallowing ability, chest auscultation, and past history are safe and essential.
- Do not perform throat cultures or use tongue blades until the airway is secured by a skilled provider.
Early recognition and prompt IV antibiotics and airway management save lives.
During the recovery stages of croup, a nurse should explain which intervention to parents?
Explanation
During the recovery stages of croup, the airway inflammation is decreasing, but the child may still be at risk for sudden worsening of symptoms, particularly at night or with viral reinfection. Parents need to be able to monitor for early signs of respiratory distress to ensure prompt intervention if symptoms recur.
Rationale for correct answer:
2. Recognizing signs of respiratory distress: Parents should be taught to observe for stridor at rest, retractions, nasal flaring, cyanosis, or increased work of breathing. Early recognition allows timely medical evaluation and prevents potential airway compromise. Education on when to seek immediate care is a key part of discharge teaching after croup.
Rationale for incorrect answers:
1. Limiting oral fluid intake: This is inappropriate since adequate hydration helps thin secretions and support recovery. Fluids should not be restricted.
3. Providing three nutritious meals per day: While nutrition is important, meal frequency is not critical during acute recovery. The priority is airway monitoring and hydration, not strict meal scheduling.
4. Allowing the child to go to the playground: Vigorous activity can increase respiratory demand and aggravate airway inflammation. Outdoor play should be gradual and based on the child’s energy and breathing after full recovery.
Take home points
- The primary focus during recovery from croup is airway safety and early recognition of respiratory distress.
- Educate parents on signs of worsening stridor, retractions, and cyanosis.
- Ensure children remain hydrated, avoid strenuous activity, and follow up with the healthcare provider as needed.
- Most children recover fully with supportive care, but vigilance during the first few days post-illness is crucial.
Which instruction should a nurse give the parents of a 2-year-old child who wakes in the night with a barking cough?
Explanation
Acute spasmodic laryngitis (“midnight croup”)is a sudden-onset, viral upper airway infection that typically affects children aged 6 months to 3 years. It presents with barking, seal-like cough, inspiratory stridor, mild to moderate respiratory distress.It often occurs at night and worsens suddenly. Most episodes are self-limiting and can be managed safely at home with supportive care unless distress becomes severe.
Rationale for correct answer:
1. Cool, humidified airfrom a humidifier, cool mist vaporizer, or stepping outside into cool night air, reduces laryngeal swelling, eases breathing, and relieves the barking cough.This is the first-line, noninvasive intervention for nighttime croup episodes at home. Parents should remain calm, keep the child upright, and observe for worsening symptoms.
Rationale for incorrect answers:
2. Most mild croup episodes are not emergencies. Emergency servicesare needed only if the child shows severe distress such as stridor at rest, retractions, cyanosis, or lethargy.
3. Warm, dry aircan increase airway inflammation and worsen symptoms. Cool, humid air is more effective for reducing airway swelling.
4. Rescue breathingis not indicated for mild croup. Only if the child stops breathing or becomes unresponsive should emergency measures like CPR be initiated.
Take home points
- Midnight croup is usually mild and self-limiting.
- Cool, humidified air is the most effective first-line intervention at home.
- Keep the child calm and upright; agitation can worsen airway obstruction.
- Seek emergency care if stridor occurs at rest, retractions worsen, or the child becomes cyanotic, lethargic, or unable to swallow fluids.
Which nursing concern should be a priority for the nurse when working with the family of a toddler being treated for acute laryngotracheobronchitis?
Explanation
Acute laryngotracheobronchitis (croup)is a viral upper airway infectioncausing inflammation of the larynx, trachea, and bronchi. It typically affects toddlers (6 months–3 years) and presents with barking cough, stridor, respiratory distress, and agitation or anxiety due to difficulty breathing
Rationale for correct answer:
4. Fear or anxiety related to dyspnea and noisy breathing: The child’s labored, noisy breathing is distressing for both the child and the family. Anxiety can aggravate airway obstruction because crying increases airway resistance in a partially obstructed upper airway. Addressing emotional needs and providing reassurance is essential alongside airway management.
Rationale for incorrect answers:
1. Potential for impaired family coping: While family coping may be affected, it is secondary to the immediate concern of child’s respiratory distress.
2. Impaired growth and development delays related to acute onset of illness: Acute croup is short-term, and mild illness does not significantly impact growth or development.
3. Impaired social isolation related to confinement in hospital: Hospitalization may temporarily affect socialization, but it is not a priority concern compared with airway compromise and family anxiety.
Take home points
- Airway distress and fear are closely linked in toddlers with croup; managing emotional and physical needs simultaneously is critical.
- Nursing interventions include:
- Calm reassurance to the child and parents
- Upright positioning to ease breathing
- Minimizing agitation (avoid invasive procedures unless necessary)
A child with difficulty breathing and a “barking cough’ is displaying signs associated with which condition?
Explanation
Acute laryngotracheobronchitis (croup)is a viral upper airway infectioncausing inflammation of the larynx, trachea, and bronchi. It typically affects toddlers (6 months–3 years) and presents with barking cough, stridor, respiratory distress, and agitation or anxiety due to difficulty breathing
Rationale for correct answer:
4. The barking cough is the classic hallmark of croupand helps differentiate it from other pediatric respiratory conditions. Respiratory distress is typically mild to moderate, and management includes humidified air, corticosteroids, and nebulized epinephrine if severe.
Rationale for incorrect answers:
1. Cystic fibrosisis a chronic genetic disorder affecting lungs and pancreas, presenting with persistent cough, thick mucus, and recurrent infections, not an acute barking cough.
2. Asthmais characterized by wheezing, chest tightness, and shortness of breath due to lower airway obstruction; does not cause a barking cough.
3. Epiglottitisis a bacterial emergency causing drooling, dysphagia, high fever, and absence of cough. Airway obstruction is rapid, and the child usually sits upright in tripod position, not displaying a barking cough.
Take home points
- Barking cough and stridor are symptoms of croup.
- Drooling, dysphagia, and high fever suggest epiglottitis an emergency.
- Persistent productive cough with poor growth may indicate cystic fibrosis.
- Recognizing these hallmark features helps prioritize interventions and ensure airway safety.
The parent of a child with croup tells the nurse that her other child just had croup and it cleared up in a couple of days without intervention. She asks the nurse why this child is exhibiting worse symptoms and needs to be hospitalized. Which is the nurse’ s best response?
Explanation
Croup (laryngotracheobronchitis)severity varies based on age, airway size, and immune response. Children under 3 years have smaller, more pliable airways, which are easily obstructed by inflammation and edema. Their immune systems are still developing, which may contribute to more pronounced symptoms and higher risk of respiratory distress compared with older children.
Rationale for correct answer:
4. “Children younger than 3 years usually exhibit worse symptoms because their immune systems are not as developed.”This response is factually correct and helps the parent understand why severity varies among children. It reassures the parent that the child’s hospitalization is based on age-related risk and airway safety, not neglect or unusual illness. Provides education and context without blaming the parent.
Rationale for incorrect answers:
1. “Some children just react differently to viruses. It is best to treat each child as an individual.”While partially true, it is too vague and does not explain why younger children are at higher risk for severe croup.
2. “Younger children have wider airways that make it easier for bacteria to enter and colonize.”Younger children have narrower, not wider, airways, which contributes to obstruction, not bacterial colonization. Croup is viral, not bacterial in most cases.
3. “Younger children have short and wide eustachian tubes, making them more susceptible to respiratory infections.”This is true for otitis media, but not relevant to croup, which affects the larynx and trachea, not the middle ear.
Take home points
- Age <3 years is a major risk factor for severe croup due to small, easily obstructed airways and immature immune systems.
- Parents should understand that hospitalization is for airway safety and monitoring, not necessarily because the virus is more severe.
- Education and reassurance help reduce parental anxiety and improve adherence to care recommendations.
A 5-year-old is brought to the ED with a temperature of 99.5°F (37.5°C), a barky cough, stridor, and hoarseness. Which nursing intervention should the nurse prepare for?
Explanation
Acute laryngotracheobronchitis (croup)is a viral upper airway infectioncausing inflammation of the larynx, trachea, and bronchi. It typically affects toddlers (6 months–3 years) and presents with barking cough, stridor, respiratory distress, and agitation or anxiety due to difficulty breathing
Rationale for correct answer:
2. Nebulized racemic epinephrinecauses vasoconstriction in the upper airway, reducing edemaand relieving stridor and respiratory distress. It is indicated for children with stridor at rest or moderate distress, which fits this child’s presentation. The child should be monitored for rebound symptoms and oxygen saturation.
Rationale for incorrect answers:
1. IV accessmay be necessary if the child deteriorates, needs medications, or fluids, but it is not the first intervention in mild-to-moderate croup.
3. Tracheostomyis not indicated for typical viral croup. Emergency airway intervention is rarely needed and only reserved for severe airway obstruction.
4. Tonsillectomyis not a treatment for croup, which is viral and self-limiting. Surgery is irrelevant in this acute presentation.
Take home points
- Racemic epinephrine is the treatment of choice for moderate to severe croup with stridor at rest.
- Children should be calm, upright, and monitored closely after administration.
- Supportive care with humidified air and corticosteroids is also indicated.
- Emergency airway equipment should be available in case of deterioration, but invasive measures are rarely needed.
Exams on Croup Syndromes
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
- Differentiate between the clinical presentation, etiology, and priority nursing interventions for epiglottitis and acute laryngotracheobronchitis (croup), recognizing each as a distinct pediatric respiratory emergency or illness.
- Identify the pathophysiological processes that lead to airway obstruction in both conditions, specifically noting the anatomical location of swelling.
- Recognize the high-risk clinical signs associated with impending airway compromise in both syndromes.
- Formulate appropriate nursing diagnoses and evidence-based interventions for the therapeutic management of children with epiglottitis and croup.
- Prioritize the "DO's and DON'Ts" of nursing care, focusing on maintaining a patent airway and minimizing anxiety to prevent further respiratory distress.
- Educate parents/caregivers on preventive measures and when to seek immediate medical attention for worsening symptoms.
- Describe the appropriate diagnostic evaluation and therapeutic management protocols, including pharmacological and non-pharmacological interventions.
- Anticipate and manage potential complications of both epiglottitis and croup.
Introduction
- Croup Syndromes are a group of respiratory illnesses characterized by hoarseness, a distinctive "barking" or "seal-like" cough, inspiratory stridor, and varying degrees of respiratory distress, resulting from inflammation and swelling in the larynx, trachea, and sometimes the bronchi.
- They primarily affect young children due to their naturally smaller airway diameters, making them highly susceptible to obstruction from even minor edema.
- The two most critical conditions under this umbrella are epiglottitis and acute laryngotracheobronchitis (croup), which require rapid and accurate differentiation as their etiologies, treatment priorities, and prognoses differ significantly.
- The pediatric airway is funnel-shaped, and the narrowest part is the subglottic area (below the vocal cords).
- Swelling here, as in croup, dramatically increases airway resistance. In contrast, Epiglottitis involves swelling of the supraglottic structures (above the vocal cords), which can cause a complete, rapid, and life-threatening obstruction.
- Recognizing and acting upon signs of progressive respiratory distress is the paramount responsibility of the RN in managing pediatric croup syndromes.
Epiglottitis
- Epiglottitis is an acute, severe, rapidly progressive, and potentially life-threatening inflammation and swelling of the supraglottic structures, particularly the epiglottis. It is a medical emergency that can lead to complete airway obstruction within hours.
Incidence
- Historically more common, the incidence has significantly decreased in countries with routine use of the Haemophilus influenzae type b (Hib) vaccine. It primarily affects children between 2 and 5 years old, but cases still occur in older children and adults.
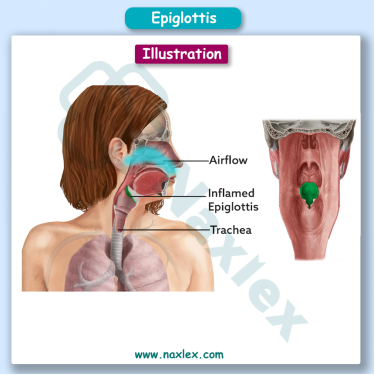
Pathophysiology
- Bacterial invasion (most commonly by Haemophilus influenzae type b) causes inflammatory edema of the epiglottis and surrounding supraglottic tissues (aryepiglottic folds). The swollen, cherry-red epiglottis obstructs the entrance to the trachea, leading to life-threatening airway compromise.
Etiology
- Most common cause: Haemophilus influenzae type b (Hib).
- Less common causes: Streptococcus pneumoniae, Staphylococcus aureus.
- Noninfectious causes: caustic ingestion, thermal injury, smoke inhalation, foreign body aspiration.
Epidemiology
- Significant decline due to widespread Hib vaccination since the 1980s.
- Still occurs, especially in unvaccinated or underimmunized children.
- It is a medical emergency due to potential for sudden airway obstruction and respiratory arrest.
Clinical Manifestations (The 4 D's)
Onset is typically abrupt and rapidly progressive. The child often appears toxic and acutely ill.
- Dysphonia- muffled voice, often described as a "hot potato" voice.
- Dysphagia- difficulty swallowing.
- Drooling due to pain and inability to swallow secretions.
- Distress- severe respiratory distress, often sitting in the tripod position—sitting up, leaning forward with neck extended, to maximize airway patency.
- High fever, >102.2°F or 39°C.
- Inspiratory stridor which is a late sign.
- Cough is typically absent or very mild, a key differentiator from Croup.
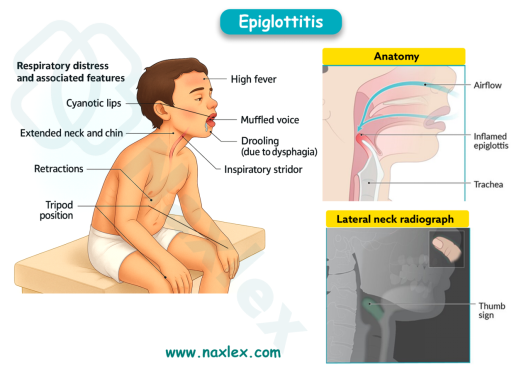
Diagnostic Evaluation
- Lateral Neck Radiograph: May show a classic "thumb sign" (a swollen epiglottis). X-rays are often avoided or deferred until the airway is secured, as movement can precipitate obstruction.
- Visual Inspection (Laryngoscopy): Definitive diagnosis, revealing a swollen, cherry-red epiglottis. This should only be performed in a setting with immediate capability for intubation (e.g., OR or ICU).
- Blood Culture: To identify the causative organism (often positive for Hib).
Therapeutic Management
|
DO'S |
DON'TS |
|
Maintain a calm, quiet environment. Minimize anxiety. |
Do not attempt to visualize the throat with a tongue depressor or throat culture. (Can trigger laryngospasm/complete obstruction) |
|
Keep the child in a position of comfort (usually sitting upright/tripod). |
Do not force the child to lie down. |
|
Secure the airway immediately (often via endotracheal intubation in the OR) by the most experienced personnel available. |
Do not perform unnecessary procedures (IV insertion, blood draw) until the airway is secured. |
|
Provide humidified oxygen as needed. |
Do not leave the child unattended. |
|
Administer IV antibiotics (e.g., Ceftriaxone) as prescribed, as it is bacterial. |
|
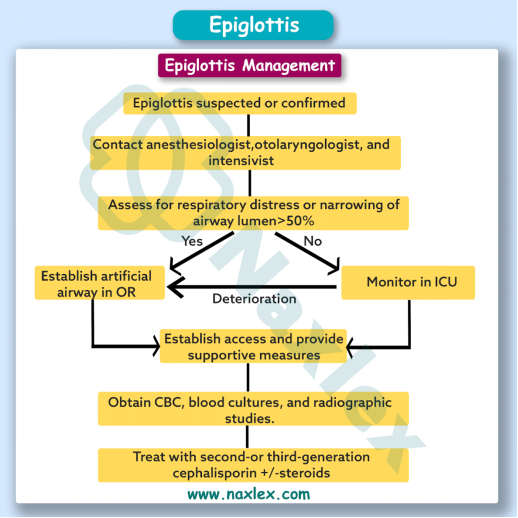
Nursing Diagnoses
- Ineffective Airway Clearance related to supraglottic swelling. (PRIORITY)
- Anxiety (Child and Parental) related to sudden onset and difficulty breathing.
- Hyperthermia related to the infectious process.
Preventive Measures
- Hib Vaccine: Routine administration of the Haemophilus influenzae type b vaccine is the most effective preventive measure.
Complications
- Complete airway obstruction leading to respiratory arrest.
- Pneumonia
- Pulmonary edema.
- Meningitis or septic arthritis due to systemic spread of the bacterial infection.
Epiglottitis Summary
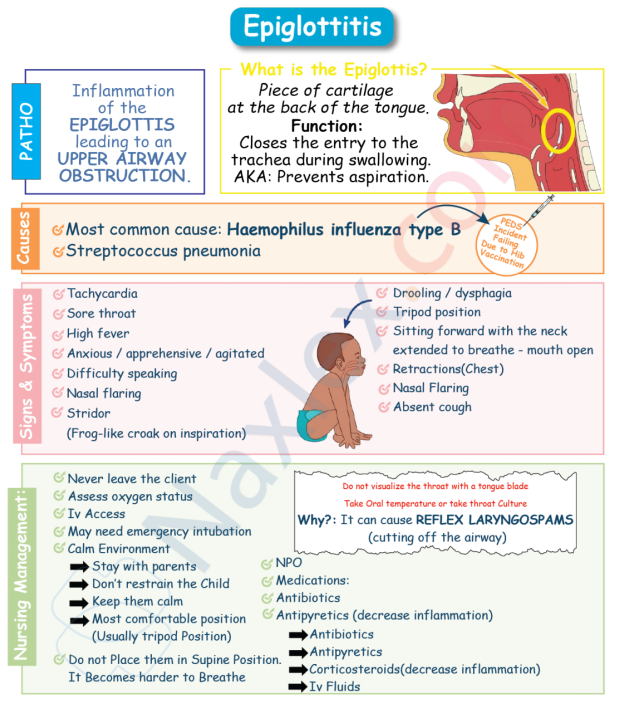
Acute Laryngotracheobronchitis
Acute Laryngotracheobronchitis (Croup) is an acute viral infection causing inflammation and edema of the larynx, trachea, and bronchi (subglottic area). This swelling below the vocal cords creates the characteristic symptoms.
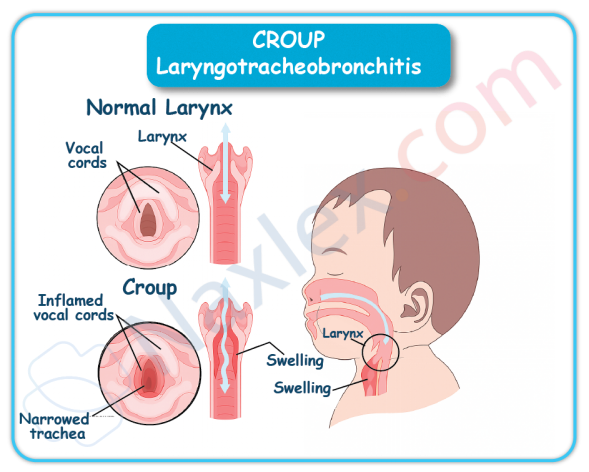
Incidence
- It is the most common cause of acute inspiratory stridor in children. It typically affects children between 6 months and 3 years of age.
Pathophysiology
- A viral infection leads to inflammation and edema of the subglottic mucosa and tracheal lining. The edema causes narrowing of the airway ("steeple sign" on X-ray) and increased mucus production, resulting in the classic "barking" cough and inspiratory stridor.
Etiology
Croup is most commonly caused by viral infections, but bacterial pathogens may also be involved in some cases.
Viral Agents (most common):
- Parainfluenza virus (types 1, 2, 3)
- Respiratory syncytial virus (RSV)
- Influenza A and B
- Adenovirus
- Enteroviruses
- Human metapneumovirus
Atypical and Bacterial Causes (less common):
- Mycoplasma pneumoniae
- Herpes simplex virus
- Staphylococcus aureus
- Streptococcus pyogenes
- Streptococcus pneumoniae
Epidemiology
- Most frequent during late fall and winter months. It is highly contagious and often follows a general upper respiratory infection (URI).
Clinical Manifestations
Onset is typically gradual, often preceded by a URI for a few days. Symptoms are generally worse at night.
- Classic "seal-like" or "barking" cough often described as croupy.
- Inspiratory stridor especially with crying or agitation, but in severe cases, at rest.
- Hoarseness due to laryngeal involvement.
- Low-grade fever or may be afebrile.
Mild to moderate respiratory distress evidenced by nasal flaring or retractions.
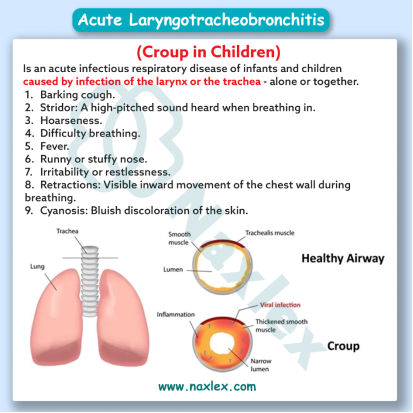
Nursing Insight: Continuous stridor at rest, signs of fatigue, cyanosis, or altered mental status suggest impending respiratory failure.
Diagnostic Evaluation
- Clinical Presentation: Diagnosis is usually made based on the characteristic cough and symptoms.
- Pulse Oximetry: To monitor oxygen saturation.
- Anteroposterior (AP) Neck Radiograph: May reveal the characteristic "steeple sign" (subglottic narrowing) due to tracheal edema.
- Westley Croup Score: Used to assess the severity of symptoms (stridor, retractions, air entry, color, level of consciousness).
Therapeutic Management
|
DO'S |
DON'TS |
|
Maintain a calm, comfortable environment. Minimize agitation, which can worsen stridor. |
Do not perform painful procedures or restraining unless absolutely necessary, as crying/agitation increases O2 consumption and airway edema. |
|
Administer Corticosteroids (e.g., oral or IM Dexamethasone) to decrease airway inflammation. This is standard care for all severity levels. |
Do not give cough suppressants or cold medicines, as they may thicken secretions. |
|
Administer Nebulized (Racemic) Epinephrine for moderate to severe stridor at rest. (Action is rapid but temporary; child must be monitored for 2-3 hours post-treatment). |
Do not let the child become dehydrated; encourage fluid intake. |
|
Provide humidified cool air/mist (e.g., cool mist tent or taking the child outside into the cool night air/to a running shower-filled bathroom). |
Do not ignore signs of worsening respiratory distress (stridor at rest, decreased level of consciousness). |
Nursing Insight: Always ensure emergency airway equipment (e.g., bag-valve mask, intubation set) is ready at the bedside for children with severe croup.
Nursing Diagnoses
- Ineffective Airway Clearance related to subglottic edema and mucus production.
- Impaired Gas Exchange related to airway obstruction (in severe cases).
- Deficient Knowledge (Parental) regarding home management and signs of complications.
Preventive Measures
- Since it is mostly viral, prevention focuses on standard hand hygiene and avoiding contact with those who have URIs. No specific vaccine exists.
Complications
- Hypoxia in severe, untreated cases.
- Dehydration due to increased respiratory effort and fever.
- Bacterial tracheitis a serious bacterial superinfection
Laryngotracheobronchitis Summary
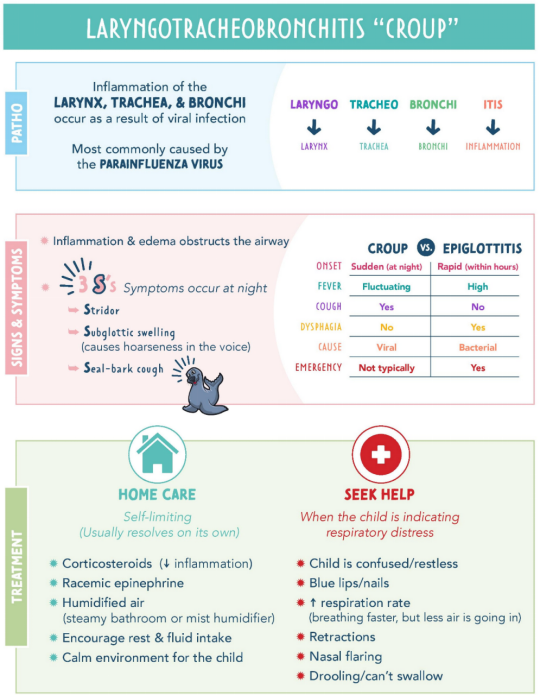
Summary
- Croup syndromes encompass a spectrum of upper airway obstructive diseases in children, with epiglottitis and acute laryngotracheobronchitis (croup) being the most crucial for the RN to distinguish.
- Epiglottitis is a rapid, bacterial, supraglottic emergency where the priority is securing the airway and preventing sudden collapse. Its hallmark signs are the 4 D's (drooling, dysphonia, dysphagia, distress), often with no cough.
- Croup is a gradual, viral, subglottic illness characterized by the classic "barking" cough and hoarseness. The nursing care for croup focuses on reducing inflammation with corticosteroids and nebulized epinephrine, minimizing agitation, and ensuring adequate hydration.
- Never inspect the throat of a child suspected of having epiglottitis, as this can trigger a fatal airway spasm.
- The RN's role is critical in rapid assessment, differentiation of the two syndromes, minimizing child anxiety, and advocating for the correct, time-sensitive medical intervention to preserve airway patency.
Comparison to Other Croup Syndromes
|
Feature |
Epiglottitis |
LTB (Croup) |
|
Age |
2–7 years |
<5 years |
|
Onset |
Sudden |
Gradual |
|
Fever |
High |
Low to moderate |
|
Drooling |
Present |
Absent |
|
Cough |
Usually absent |
Barking cough |
|
Voice |
Muffled or soft |
Hoarse |
|
Stridor |
Worse when supine |
Present |
|
Appearance |
Toxic |
Non-toxic |
|
Positioning |
Tripod |
May lie down |
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Croup Syndromes
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


