Please set your exam date
Respiratory Management and Mechanical Ventilation
Study Questions
Practice Exercise 1
A comatose patient with a possible cervical spine injury is intubated with a nasal endotracheal (ET) tube. The nurse recognizes that what is a disadvantage of a nasal ET tube in comparison with an oral ET tube?
Explanation
Following endotracheal intubation, understanding the advantages and disadvantages of the nasal versus oral route is crucial for maintaining airway patency and minimizing complications. A nasal endotracheal (ET) tube increases airway resistance, requiring greater respiratory effort compared with an oral ET tube. This is due to the narrower nasal passages and increased tube curvature, which make airflow less efficient.
Rationale for Correct Answer
3. Requires greater respiratory effort in breathing: Nasal ET tubes create more airflow resistance because of their longer length and smaller internal diameter. The nasal route also introduces additional anatomical curves, increasing work of breathing and making spontaneous ventilation more difficult.
Rationale for Incorrect Answers
1. Requires the placement of a bite block: Bite blocks are primarily needed for oral ET tubes to prevent the patient from occluding the tube with their teeth; they are not necessary for nasal intubation.
2. Is more likely to cause laryngeal trauma: Nasal intubation generally causes less laryngeal trauma than oral intubation because the tube bypasses the tongue and oropharynx; however, it may cause nasal or sinus injury instead.
4. Requires the placement of an additional airway to keep the trachea open: The ET tube itself maintains tracheal patency, and no additional airway adjunct is required once proper placement is confirmed.
Take-Home Points
- Nasal ET tubes increase airway resistance, making spontaneous breathing more difficult.
- Oral ET tubes are preferred when possible because they allow for larger tube diameters and lower resistance.
- Nasal tubes may be useful for patients with oral or facial trauma or those requiring long-term intubation but carry risks of nasal bleeding or sinus infection.
In preparing a patient in the ICU for oral ET intubation, what should the nurse do?
Explanation
During preparation for oral endotracheal (ET) intubation, proper patient positioning is essential to align the oral, pharyngeal, and tracheal axes for easy tube insertion. The correct position is supine with the head extended and the neck flexed, commonly called the “sniffing position.” This alignment facilitates visualization of the vocal cords and smooth passage of the tube into the trachea.
Rationale for Correct Answer
1. Place the patient supine with the head extended and the neck flexed: The “sniffing” position (neck flexed slightly forward with head extended) aligns the mouth, pharynx, and larynx to provide a straight pathway for intubation. It improves glottic visualization and increases the likelihood of successful tube placement on the first attempt.
Rationale for Incorrect Answers
2. Tell the patient that the tongue must be extruded while the tube is inserted: During intubation, the patient is typically sedated or unconscious, and the tongue should remain inside the mouth. Extruding the tongue would obstruct rather than aid insertion.
3. Position the patient supine with the head hanging over the edge of the bed to align the mouth and trachea: This hyperextension can obstruct the airway, make intubation more difficult, and risk spinal injury, especially if cervical trauma is suspected.
4. Inform the patient that while it will not be possible to talk during insertion of the tube, speech will be possible after it is correctly placed: Once the ET tube is in place, speech is impossible because the tube passes through the vocal cords, preventing phonation until it is removed.
Take-Home Points
- The “sniffing position” (neck flexed, head extended) is optimal for oral ET intubation.
- Hyperextension or tongue extrusion interferes with safe airway alignment.
- Patients cannot speak while an endotracheal tube is in place.
A patient has an oral ET tube inserted to relieve an upper airway obstruction and to facilitate secretion removal. What is the first responsibility of the nurse immediately following placement of the tube?
Explanation
Immediately following endotracheal (ET) tube placement, the nurse’s first responsibility is to verify correct tube placement to ensure the airway is patent and ventilation is effective. This is done by assessing for bilateral breath sounds and symmetric chest movement, which confirm that the tube is in the trachea and not in a mainstem bronchus or the esophagus.
Rationale for Correct Answer
4. Assess for bilateral breath sounds and symmetric chest movement: After intubation, the priority is to confirm that the tube is correctly positioned in the trachea. Bilateral and equal breath sounds, visible chest rise on both sides, and absence of gastric sounds indicate correct placement. This assessment must occur before securing the tube or performing suctioning to prevent hypoxia or aspiration due to misplaced tubing.
Rationale for Incorrect Answers
1. Suction the tube to remove secretions: Suctioning is performed after confirming correct placement. Suctioning too early could dislodge a misplaced tube or worsen hypoxia if the tube is in the esophagus.
2. Place an end-tidal CO₂ detector on the ET tube: Although using an end-tidal CO₂ detector is an important step to confirm placement, initial bedside verification through chest assessment must be done first to rapidly identify gross misplacement before further validation.
3. Secure the tube to the face with adhesive tape: The tube should only be secured after confirmation of proper placement through auscultation, observation, and device verification to prevent fixing a tube that’s incorrectly positioned.
Take-Home Points
- First priority after intubation: verify placement through bilateral breath sounds and symmetric chest movement.
- Do not secure or suction until tube placement is confirmed.
- Use end-tidal CO₂ and chest x-ray as follow-up confirmation methods.
The nurse uses the minimal occluding volume technique to inflate the cuff on an ET tube to minimize the incidence of what?
Explanation
The minimal occluding volume (MOV) technique is used during endotracheal (ET) tube cuff inflation to create a proper airway seal while minimizing pressure on the tracheal wall. The goal is to use just enough air to seal the airway during positive-pressure ventilation without excessive pressure. This technique helps prevent tracheal necrosis, which can result from prolonged high cuff pressures that impair tracheal mucosal blood flow.
Rationale for Correct Answer
3. Tracheal necrosis: Overinflation of the ET tube cuff can exert excessive pressure on the tracheal mucosa, reducing capillary perfusion and causing ischemia, ulceration, or necrosis. Using the minimal occluding volume ensures an adequate seal with minimal pressure, preventing these complications while maintaining effective ventilation.
Rationale for Incorrect Answers
1. Infection: While maintaining cuff pressure may reduce the risk of aspiration, infection prevention primarily depends on aseptic technique, oral care, and minimizing intubation duration, not on cuff inflation technique.
2. Hypoxemia: The MOV technique helps ensure a proper seal for ventilation, but hypoxemia is more commonly related to inadequate oxygen delivery, dislodgement, or airway obstruction, not cuff volume.
4. Accidental extubation: Cuff inflation does not prevent tube displacement; secure fixation of the tube and proper patient positioning are the primary measures to prevent extubation.
Take-Home Points
- The MOV technique prevents excess cuff pressure while ensuring an airtight seal.
- Excessive cuff inflation can cause tracheal ischemia and necrosis.
- Monitor cuff pressure (20–25 cm H₂O) regularly to maintain safety.
- Tube security and infection control rely on separate nursing interventions.
The nurse suctions the patient’s ET tube when the patient has what?
Explanation
Suctioning an endotracheal (ET) tube is performed only when there are clear indications of airway secretion accumulation or obstruction—not on a routine schedule. The presence of coarse rhonchi over central airways indicates mucus or secretions within the trachea or main bronchi that need to be removed to maintain a patent airway and adequate ventilation.
Rationale for Correct Answer
3. Coarse rhonchi over central airways: Coarse rhonchi are low-pitched, rattling sounds heard over large airways and are caused by secretions or mucus movement. In a patient with an ET tube, this finding signals the need for suctioning to clear the airway, improve breath sounds, and prevent hypoxemia or infection.
Rationale for Incorrect Answers
1. Peripheral wheezes in all lobes: Wheezes indicate bronchospasm or airway narrowing, not secretions. Suctioning will not relieve wheezing; bronchodilator therapy is required instead.
2. Has not been suctioned for 2 hours: Suctioning is not time-based but assessment-based. Routine suctioning can cause mucosal injury, hypoxia, and arrhythmias if done unnecessarily.
4. A need for stimulation to cough and deep breathe: Suctioning should not be used as a method to stimulate coughing; instead, encourage or assist coughing through repositioning, chest physiotherapy, or incentive spirometry if the patient is able.
Take-Home Points
- Suction only when indicated—signs include coarse rhonchi, visible secretions, increased airway pressure, or decreased oxygen saturation.
- Avoid routine suctioning to prevent mucosal trauma and hypoxemia.
- Wheezes require bronchodilators, not suctioning.
- Always hyperoxygenate before and after suctioning to minimize desaturation.
Practice Exercise 2
A nurse is planning care for a client who is receiving mechanical ventilation. Which mode of ventilation increases the effort of the client’s respiratory muscles? Select all that apply
Explanation
When planning care for a client receiving mechanical ventilation, it’s essential to understand how each mode affects respiratory muscle workload. Modes that allow or require the patient to initiate breaths independently—such as Synchronized Intermittent Mandatory Ventilation (SIMV), Continuous Positive Airway Pressure (CPAP), and Pressure Support Ventilation (PSV)—increase the effort of the patient’s respiratory muscles by promoting spontaneous breathing.
Rationale for Correct Answers
2. Synchronized Intermittent Mandatory Ventilation (SIMV): In SIMV, the ventilator delivers a set number of mandatory breaths, but the patient can breathe spontaneously between them without assistance. These spontaneous breaths require the patient to use their own respiratory muscles, increasing workload compared with fully controlled modes.
3. Continuous Positive Airway Pressure (CPAP): CPAP is a spontaneous mode with no mandatory breaths. The patient breathes entirely on their own against continuous airway pressure, maintaining alveolar stability but requiring full respiratory muscle effort.
4. Pressure Support Ventilation (PSV): In PSV, each breath is patient-initiated and supported by preset pressure from the ventilator. The patient performs most of the work of breathing, and the ventilator simply decreases airway resistance, thus strengthening respiratory muscles during weaning.
Rationale for Incorrect Answers
1. Assist-control (A/C): This mode delivers a full ventilator-assisted breath for every patient-initiated or timed breath, minimizing muscle use. It provides maximum ventilatory support and minimal patient effort.
5. Independent lung ventilation: This specialized technique delivers separate ventilation to each lung (via double-lumen tubes) for patients with unilateral lung disease. It does not inherently increase respiratory effort since each lung is ventilated mechanically.
Take-Home Points
- SIMV, CPAP, and PSV increase patient respiratory muscle effort by promoting spontaneous breathing.
- Assist-control provides maximum ventilator support and minimal patient effort.
- CPAP and PSV are commonly used for weaning because they strengthen respiratory muscles.
A nurse is orienting a newly licensed nurse who is caring for a client receiving mechanical ventilation that has been placed on pressure support ventilation (PSV) mode. Which of the following statements by the newly licensed nurse demonstrates an understanding of PSV?
Explanation
Pressure Support Ventilation (PSV) is a spontaneous mode of mechanical ventilation that assists patients with their own breathing efforts by providing a preset amount of positive pressure during inspiration. This mode decreases the work of breathing while allowing the patient to maintain control over their respiratory rate and tidal volume, making it ideal for weaning.
Rationale for Correct Answer
2. “It permits spontaneous ventilation to decrease the work of breathing.”
In PSV mode, the ventilator delivers a preset level of inspiratory pressure in response to the patient’s own breaths. This pressure support helps overcome airway resistance (such as that from the endotracheal tube) and reduces the patient’s effort, thereby decreasing the work of breathing while promoting spontaneous respiration.
Rationale for Incorrect Answers
1. “It keeps the alveoli open and prevents atelectasis.” This statement describes Continuous Positive Airway Pressure (CPAP), which provides continuous pressure throughout the respiratory cycle to maintain alveolar inflation, not PSV.
3. “It is used with clients who have difficulty weaning from the ventilator.” PSV is used to facilitate, not hinder, the weaning process by gradually strengthening respiratory muscles as the patient assumes more of the breathing workload.
4. “It delivers a preset ventilatory rate and tidal volume to the client.” This describes Assist-Control (A/C) or Volume Control Ventilation (VCV) modes, where the ventilator determines the rate and volume, not PSV, which relies on patient effort to initiate and determine breath size.
Take-Home Points
- PSV supports spontaneous breathing by delivering inspiratory pressure, reducing respiratory muscle workload.
- It is commonly used during weaning from mechanical ventilation.
- The patient determines rate and tidal volume, while the ventilator provides pressure assistance.
- PSV differs from CPAP (continuous pressure) and A/C (mandatory rate and volume) modes.
Which patient’s medical diagnosis should the nurse know is most likely to need mechanical ventilation? Select all that apply
Explanation
Mechanical ventilation is required when a patient cannot maintain adequate oxygenation, ventilation, or airway protection on their own. Conditions that cause severe respiratory compromise, such as Cystic Fibrosis and Acute Respiratory Distress Syndrome (ARDS), are the most likely to require ventilatory support to sustain gas exchange and reduce the work of breathing.
Rationale for Correct Answers
2. Cystic Fibrosis: This chronic genetic disorder leads to the production of thick mucus that obstructs airways, causing severe respiratory infections and hypoventilation. During acute exacerbations or respiratory failure, mechanical ventilation supports oxygenation and CO₂ elimination until the underlying infection or obstruction is managed.
5. Acute Respiratory Distress Syndrome (ARDS): ARDS results in severe alveolar damage, noncompliant lungs, and refractory hypoxemia, making spontaneous breathing ineffective. Mechanical ventilation with PEEP (positive end-expiratory pressure) is essential to improve oxygenation and prevent alveolar collapse.
Rationale for Incorrect Answers
1. Sleep Apnea: Most patients with sleep apnea are managed with noninvasive positive airway pressure (CPAP or BiPAP) at home, not mechanical ventilation. Intubation is only required in rare, severe cases of apnea-related respiratory failure.
3. Acute Kidney Failure: Although kidney failure affects fluid and electrolyte balance, it does not directly impair ventilation. Mechanical ventilation may be needed only if fluid overload causes pulmonary edema leading to respiratory distress.
4. Type 2 Diabetes Mellitus: Diabetes alone does not affect ventilation. Respiratory support would only be indicated if a complication like diabetic ketoacidosis caused respiratory compromise.
Take-Home Points
- Mechanical ventilation is indicated for disorders causing severe hypoxemia, hypercapnia, or airway compromise.
- Cystic Fibrosis and ARDS both impair gas exchange and are leading causes for ventilator support.
- Sleep apnea is typically treated with noninvasive ventilation (CPAP/BiPAP), not intubation.
- Conditions like renal failure or diabetes only require ventilation if secondary respiratory failure develops.
What characteristics describe positive pressure ventilators? Select all that apply
Explanation
Positive pressure ventilators work by delivering air into the lungs through an artificial airway under positive pressure during inspiration. This type of ventilation is commonly used in acutely ill patients in hospital settings, as it provides complete control over oxygenation, ventilation, and airway protection.
Rationale for Correct Answers
1. Require an artificial airway: Most positive pressure ventilators require an endotracheal or tracheostomy tube to deliver air directly into the lungs. This ensures a sealed system for effective ventilation and prevents aspiration in critically ill patients.
4. Most frequently used with acutely ill patients: Positive pressure ventilation is the standard of care in intensive care units (ICUs) for patients with acute respiratory failure, ARDS, or those undergoing major surgery. It allows precise control of tidal volume, respiratory rate, and FiO₂.
Rationale for Incorrect Answers
2. Applied to the outside of the body: This describes negative pressure ventilation (e.g., iron lung), where negative pressure around the chest draws air into the lungs—used historically and rarely today. Positive pressure ventilators deliver air internally, not externally.
3. Most similar to physiologic ventilation: Negative pressure ventilation mimics normal physiology, as the diaphragm contracts and chest wall expands to draw air in. Positive pressure ventilation is the opposite, pushing air into the lungs.
5. Frequently used in the home for neuromuscular or nervous system disorders: Noninvasive negative pressure ventilators or BiPAP/CPAP devices are used in home settings for chronic respiratory insufficiency, not invasive positive pressure ventilators.
Take-Home Points
- Positive pressure ventilation pushes air into the lungs via an artificial airway (ET or tracheostomy tube).
- It is the most common form used in hospitals for acutely ill patients with respiratory failure.
- It differs from negative pressure ventilation, which mimics normal breathing mechanics.
- Home ventilation for chronic disorders usually involves noninvasive support, not invasive positive pressure systems.
What is included in the description of positive pressure ventilation? Select all that apply
Explanation
Positive pressure ventilation (PPV) delivers air into the lungs under pressure during inspiration, and its characteristics vary depending on whether the ventilator operates in a volume-controlled or pressure-controlled mode. In general, PPV involves a predetermined peak inspiratory pressure, carries a risk of over- or under-ventilation, and results in variable tidal volumes depending on the patient’s lung compliance.
Rationale for Correct Answers
1. Peak inspiratory pressure predetermined: In pressure-controlled ventilation, the ventilator delivers each breath to a preset inspiratory pressure, regardless of the volume achieved. This limits barotrauma risk but allows the delivered volume to fluctuate with compliance.
3. Increased risk for hyperventilation and hypoventilation: Because patient lung compliance and airway resistance can change, both volume-controlled and pressure-controlled modes may deliver too much or too little ventilation, resulting in hyperventilation or hypoventilation if not closely monitored.
5. Volume delivered varies based on selected pressure and patient lung compliance: In pressure-controlled modes, tidal volume depends on the set pressure and the compliance of the lungs and chest wall—poor compliance leads to smaller volumes, while improved compliance increases volume.
Rationale for Incorrect Answers
2. Consistent volume delivered with each breath: This applies to volume-controlled ventilation, not to PPV in general. In pressure-controlled modes, delivered volume varies.
4. Preset volume of gas delivered with variable pressure based on compliance: This describes volume-controlled ventilation, where a fixed volume is delivered, but the pressure required to achieve that volume varies with lung compliance.
Take-Home Points
- Positive pressure ventilation delivers gas into the lungs using positive inspiratory pressure.
- Pressure-controlled modes: pressure is fixed, volume varies with compliance.
- Volume-controlled modes: volume is fixed, pressure varies with compliance.
Practice Exercise 3
A patient receiving mechanical ventilation is very anxious and agitated, and neuromuscular blocking agents are used to promote ventilation. What should the nurse recognize about the care of this patient?
Explanation
Patients who receive neuromuscular blocking agents (NMBAs) are paralyzed but not sedated or anesthetized by the paralytic itself. Therefore, the nurse must always address the patient and explain care because the patient may be awake, aware, and able to hear despite being unable to move or speak. Clear verbal communication preserves dignity, reduces fear, and is an essential component of compassionate care.
Rationale for Correct Answer
3. The patient should always be addressed and explanations of care given. NMBAs cause skeletal muscle paralysis but do not alter consciousness or pain perception. Patients may retain awareness and the ability to perceive auditory input. Speaking to the patient, explaining procedures, and providing reassurance help prevent psychological trauma and maintain trust, even though the patient cannot respond.
Rationale for Incorrect Answers
1. The patient will be too sedated to be aware of the details of care. This is incorrect because paralytics are not sedatives or analgesics. Sedation and pain control must be provided separately; assuming the patient is unaware risks causing distress and harm.
2. Caregivers should be encouraged to provide stimulation and diversion. While emotional support is important, excessive stimulation may be frightening when the patient cannot respond. Calm, clear verbal reassurance and minimal unnecessary stimulation are preferred.
4. Communication will not be possible with the use of neuromuscular blocking agents. Verbal communication is impossible, but alternative communication methods (e.g., explanation, yes/no signals if possible, communication boards when feasible) and ongoing verbal interaction remain crucial because the patient may still comprehend.
Take-Home Points
- NMBAs paralyze muscles but do not produce sedation or analgesia—administer sedatives and analgesics as indicated.
- Always speak to and explain care to paralyzed patients; assume they can hear and understand.
- Use calm reassurance rather than excessive stimulation; provide alternative communication methods when possible.
- Continuous monitoring for oxygenation, comfort, and appropriate sedation is essential when paralytics are in use.
While receiving prolonged mechanical ventilation, the patient developed anemia. The patient is also having difficulty being weaned from the ventilator related to recurrent pneumonia and early fatigue with weaning. What is contributing to the patient’s prolonged recovery?
Explanation
When a patient is receiving prolonged mechanical ventilation, adequate nutritional support is vital for maintaining respiratory muscle strength, immune function, and tissue healing. Inadequate nutrition leads to muscle wasting, anemia, and fatigue, all of which contribute to difficulty in weaning and delayed recovery.
Rationale for Correct Answer
3. Inadequate nutrition: Prolonged mechanical ventilation increases metabolic demand, requiring higher calorie and protein intake. When nutritional needs are unmet, respiratory muscles weaken, endurance decreases, and immune response declines, predisposing the patient to recurrent pneumonia and anemia. This combination leads to early fatigue and delayed weaning from the ventilator.
Rationale for Incorrect Answers
1. Hypoxemia: While hypoxemia can result from pneumonia or poor ventilation, it is typically a symptom of the patient’s overall condition, not the root cause of prolonged recovery.
2. Enteral feeding: This method provides essential nutrients and supports healing. It aids recovery rather than delays it, provided it meets the patient’s metabolic needs.
4. Decreased activity level: Though physical inactivity contributes to muscle weakness, the primary factor in this scenario is malnutrition, which underlies both fatigue and impaired muscle function.
Take-Home Points
- Adequate nutrition is crucial for respiratory muscle strength and successful ventilator weaning.
- Malnutrition leads to muscle atrophy, anemia, and delayed healing, increasing ventilator dependence.
- Monitor nutritional intake closely and collaborate with dietitians to meet energy and protein needs.
- Nutritional therapy plays a key role in preventing complications and promoting recovery in ventilated patients.
The nurse determines that alveolar hypoventilation is occurring in a patient on a ventilator when what happens?
Explanation
When a patient on mechanical ventilation develops alveolar hypoventilation, it means that inadequate ventilation is occurring, leading to CO₂ retention and respiratory acidosis. The buildup of CO₂ decreases blood pH and can cause cardiac dysrhythmias due to altered acid-base balance and electrolyte disturbances.
Rationale for Correct Answer
1. The patient develops cardiac dysrhythmias: Alveolar hypoventilation results in increased PaCO₂ and decreased pH. The resulting respiratory acidosis alters myocardial excitability, predisposing the patient to cardiac dysrhythmias. This is a key clinical indicator that ventilation is inadequate and CO₂ clearance is impaired.
Rationale for Incorrect Answers
2. Auscultation reveals an air leak around the ET tube cuff: An air leak may cause loss of tidal volume or poor pressure delivery, but it does not directly confirm alveolar hypoventilation unless accompanied by abnormal ABG values.
3. ABG results show a PaCO₂ of 32 mm Hg and a pH of 7.47: These findings indicate alveolar hyperventilation, not hypoventilation, because CO₂ levels are low and pH is alkalotic.
4. The patient tries to breathe faster than the ventilator setting: This suggests anxiety, pain, or ventilator dyssynchrony, not alveolar hypoventilation. The patient may actually be hyperventilating, decreasing CO₂ levels instead.
Take-Home Points
- Alveolar hypoventilation leads to CO₂ retention and respiratory acidosis.
- Cardiac dysrhythmias can occur due to acid-base imbalance from rising CO₂.
- ABGs are essential to confirm whether the problem is hypoventilation (↑PaCO₂) or hyperventilation (↓PaCO₂).
- Prompt ventilator adjustment and evaluation of airway function help restore adequate gas exchange.
What plan should the nurse use when weaning a patient from a ventilator?
Explanation
When weaning a patient from mechanical ventilation, the goal is to gradually restore independent breathing while preventing respiratory muscle fatigue. The safest and most effective approach is to use intermittent spontaneous breathing trials (SBTs), alternating with periods of mechanical support to allow rest and recovery.
Rationale for Correct Answer
2. Intermittent trials of spontaneous ventilation followed by ventilatory support to provide rest: This method allows the patient to practice spontaneous breathing while ensuring adequate rest between trials. It prevents respiratory fatigue and promotes gradual adaptation to independent ventilation. The nurse monitors for signs of distress (e.g., increased respiratory rate, tachycardia, or desaturation) and resumes full support as needed.
Rationale for Incorrect Answers
1. Decrease the delivered FiO₂ concentration: Oxygen concentration should be reduced only if oxygenation remains stable; it is not the primary strategy for ventilator weaning.
3. Substitute ventilator support with a manual resuscitation bag if the patient becomes hypoxemic: This is an emergency measure, not a weaning technique. Manual ventilation is used only during equipment failure or acute decompensation.
4. Implement weaning procedures around the clock until the patient does not experience ventilatory fatigue: Continuous weaning can cause severe fatigue and respiratory failure. Rest periods are essential to allow recovery and prevent exhaustion of respiratory muscles.
Take-Home Points
- Weaning should be a gradual, closely monitored process using spontaneous breathing trials.
- Rest periods between trials prevent fatigue and promote success.
- Monitor for signs of respiratory distress and discontinue trials if instability occurs.
- The goal is to balance respiratory workload and support recovery of independent ventilation.
A patient is to be discharged home with mechanical ventilation. Before discharge, what is most important for the nurse to do for the patient and caregiver?
Explanation
Before discharging a patient who will require home mechanical ventilation, the nurse’s primary responsibility is to ensure that the caregiver is competent and confident in managing the ventilator and caring for the patient safely. Comprehensive education and hands-on training are critical to prevent complications and ensure continuity of care at home.
Rationale for Correct Answer
1. Teach the caregiver to care for the patient with a home ventilator: Caregiver education is the most important step before discharge. The nurse must teach ventilator operation, troubleshooting alarms, suctioning, airway care, infection prevention, and emergency procedures. The caregiver should demonstrate proficiency and confidence in these skills to ensure safe home management and reduce hospital readmissions.
Rationale for Incorrect Answers
2. Help the caregiver to plan for placement of the patient in a long-term care facility: This may be an option if home care is not feasible, but it is not appropriate if the goal is to discharge the patient home.
3. Stress the advantages for the patient in being cared for in the home environment: Although beneficial, discussing advantages does not ensure the caregiver’s readiness or competence to manage home ventilation.
4. Have the caregiver arrange for around-the-clock home health nurses for the first several weeks: Continuous nursing care is not always available or necessary; the focus should be on training and empowering the primary caregiver to handle daily care safely.
Take-Home Points
- Education and demonstration are key before discharging a ventilated patient home.
- The caregiver must understand ventilator use, suctioning, and emergency management.
- Competency validation ensures safety and prevents respiratory emergencies at home.
Comprehensive Questions
While suctioning the ET tube of a spontaneously breathing patient, the nurse notes that the patient develops bradycardia with premature ventricular contractions. What should the nurse do first?
Explanation
During endotracheal suctioning, a patient may develop bradycardia with premature ventricular contractions (PVCs) due to vagal stimulation and transient hypoxia. The priority intervention is to stop suctioning immediately and reoxygenate the patient with 100% oxygen using a bag-valve-mask (BVM) until the heart rate stabilizes and oxygenation improves.
Rationale for Correct Answer
4. Stop suctioning and ventilate the patient with a BVM device with 100% oxygen until the heart rate returns to baseline: This response directly addresses the cause of the bradycardia and PVCs—hypoxia and vagal stimulation. Providing 100% oxygen restores oxygen saturation, reverses vagal-induced bradycardia, and prevents further dysrhythmias. Reoxygenation before and after suctioning is essential for patient safety.
Rationale for Incorrect Answers
1. Stop the suctioning and assess the patient for spontaneous respirations: Although assessment is important, the priority is to restore oxygenation immediately rather than simply observe the patient.
2. Attempt to resuction the patient with reduced suction pressure and pass time: Resuctioning at this point would worsen hypoxia and bradycardia. Suctioning should be resumed only after stabilization and reoxygenation.
3. Stop the suctioning and ventilate the patient with slow, small-volume breaths using a BVM device: Ventilating with small-volume breaths does not ensure adequate reoxygenation. The patient needs 100% oxygen to rapidly reverse the hypoxic state.
Take-Home Points
- Bradycardia and PVCs during suctioning indicate vagal stimulation and hypoxia.
- Immediately stop suctioning and administer 100% oxygen with a BVM until stability returns.
- Always preoxygenate for 30 seconds before suctioning and reoxygenate afterward.
- Continuous cardiac and oxygen monitoring is crucial during suctioning of intubated patients.
What precautions should the nurse take during mouth care and repositioning of an oral ET tube to prevent and detect tube dislodgement? Select all that apply
Explanation
When performing mouth care or repositioning an oral endotracheal (ET) tube, the nurse must take specific precautions to prevent accidental tube dislodgement and ensure airway security. Coordination between caregivers and continuous assessment of tube placement and breath sounds are essential to detect displacement early and maintain effective ventilation.
Rationale for Correct Answers
1. Confirm bilateral breath sounds after care: Checking for equal and bilateral breath sounds immediately after repositioning or oral care ensures that the ET tube has not shifted or migrated into one bronchus. Unequal or absent breath sounds can indicate tube displacement, requiring prompt repositioning.
5. One staff member holds the tube and one performs care: This is a critical safety measure. Having one nurse stabilize the ET tube while another provides oral care or repositioning prevents accidental extubation or tube movement. It maintains correct tube depth and placement throughout the procedure.
Rationale for Incorrect Answers
2. Use suction pressures less than 120 mm Hg: While this is an important airway suctioning precaution, it does not specifically prevent or detect tube dislodgement during oral care.
3. Use water swabs to prevent mucosal drying: This measure maintains oral hygiene, not ET tube placement stability.
4. Use humidified inspired gas to help thin secretions: Humidification prevents secretion thickening but does not protect against tube dislodgement.
6. Move secretions into larger airways with turning every 2 hours: Turning promotes lung expansion and secretion movement but is unrelated to detecting tube displacement during oral care.
Take-Home Points
- Always stabilize the ET tube during repositioning and oral care to prevent dislodgement.
- Two-person technique is the safest method for handling the tube during care.
- Reassess breath sounds and tube depth after any repositioning or manipulation.
- Early detection of tube migration or extubation prevents hypoxia and ensures patient safety.
A patient with an oral ET tube has a nursing diagnosis of risk for aspiration related to presence of artificial airway. What are appropriate nursing interventions for this patient? Select all that apply
Explanation
A patient with an oral endotracheal (ET) tube is at high risk for aspiration because the airway defense mechanisms—such as the epiglottis and cough reflex—are bypassed. Nursing care must focus on preventing oropharyngeal secretions and gastric contents from entering the airway, ensuring proper cuff function, and maintaining optimal positioning.
Rationale for Correct Answers
2. Ensure that the cuff is properly inflated: A well-inflated ET tube cuff seals the trachea, preventing secretions from the upper airway or gastric contents from leaking into the lungs. Cuff pressure should be maintained within the recommended range (20–25 cm H₂O) to balance airway protection with tracheal safety.
3. Suction the patient’s mouth frequently: Regular oropharyngeal suctioning helps remove accumulated secretions that could leak past the cuff or be aspirated when the patient is repositioned or the cuff deflates slightly.
5. Raise the head of the bed 30 to 45 degrees unless the patient is unstable: This semi-Fowler’s position minimizes the risk of aspiration by using gravity to keep gastric and oropharyngeal contents away from the airway. It’s a standard component of ventilator-associated pneumonia (VAP) prevention bundles.
Rationale for Incorrect Answers
1. Assess gag reflex: The gag reflex is not a reliable indicator of aspiration risk in an intubated patient, as the ET tube bypasses the normal swallowing mechanism. Assessing it is unnecessary and may cause discomfort or coughing.
4. Keep the ventilator tubing cleared of condensed water: While important for infection control and ventilator function, draining condensate from the tubing does not directly prevent aspiration.
Take-Home Points
- Maintain cuff pressure, perform frequent oral suctioning, and elevate the head of the bed to reduce aspiration risk.
- Always use aseptic technique when suctioning to prevent infection.
- Incorporate these measures into VAP prevention protocols for mechanically ventilated patients.
Although the oxygen saturation is above 92%, an orally intubated, mechanically ventilated patient is restless and very anxious. What intervention should be used first to decrease the risk of accidental extubation?
Explanation
A mechanically ventilated, orally intubated patient who is restless and anxious is at risk for accidental extubation, even if oxygen saturation is adequate. The first priority is to reduce agitation safely through sedation and continuous presence of a caregiver or nurse, addressing both comfort and safety before considering restraints.
Rationale for Correct Answer
3. Administer sedatives and have a caregiver stay with the patient: Sedation decreases anxiety and restlessness, reducing the likelihood of self-extubation or tube displacement. A caregiver or nurse provides constant supervision, ensuring rapid intervention if the patient attempts to pull at the tube. This approach addresses the root cause of agitation while maintaining patient safety.
Rationale for Incorrect Answers
1. Obtain an order and apply soft wrist restraints: Restraints should be a last resort after sedation and close monitoring fail. Applying restraints first does not address anxiety, may increase agitation, and carries ethical considerations.
2. Remind the patient that he needs the tube inserted to breathe: Verbal reassurance alone is insufficient for a patient who is physiologically and psychologically distressed and may not fully comprehend due to sedation or confusion.
4. Move the patient to an area close to the nurses’ station for closer observation: While closer observation may help, it does not reduce agitation or prevent self-extubation by itself; sedation and continuous presence are more effective first-line interventions.
Take-Home Points
- Sedation and constant supervision are first-line measures to prevent accidental extubation in anxious, intubated patients.
- Restraints are a secondary measure and should be used only if sedation and monitoring are insufficient.
- Always assess agitation, pain, and discomfort in ventilated patients to guide safe interventions.
- Preventing self-extubation reduces risk of hypoxia, airway trauma, and ventilator complications.
Which mode of ventilation is used with critically ill patients and allows the patient to self-regulate the rate and depth of spontaneous respirations but may also deliver a preset volume and frequency of breaths?
Explanation
Synchronized Intermittent Mandatory Ventilation (SIMV) is a mode commonly used for critically ill patients that combines mandatory ventilator breaths with spontaneous breaths. This allows the patient to self-regulate the rate and depth of their breathing while still receiving preset volume and frequency support as needed.
Rationale for Correct Answer
4. Synchronized intermittent mandatory ventilation (SIMV): In SIMV, the ventilator delivers a set number of mandatory breaths at a preset volume or pressure, synchronized with the patient’s spontaneous efforts. Between mandatory breaths, the patient can breathe spontaneously, controlling rate and tidal volume, which promotes respiratory muscle use and supports gradual weaning.
Rationale for Incorrect Answers
1. Assist-control ventilation (ACV): Delivers a full ventilator-assisted breath for every patient-initiated or timed breath, minimizing spontaneous effort. The patient has less control over rate and depth.
2. Pressure support ventilation (PSV): Only provides pressure assistance for patient-initiated breaths. There are no mandatory breaths; it cannot deliver preset volume or frequency.
3. Pressure-controlled inverse ratio ventilation (PC-IRV): Used in severe ARDS to improve oxygenation by prolonging inspiratory time. It is a fully controlled mode, not allowing spontaneous regulation of rate and depth.
Take-Home Points
- SIMV allows combination of ventilator support and spontaneous breathing, promoting muscle strength and weaning.
- ACV provides maximum support, minimizing patient effort.
- PSV assists spontaneous breaths but does not provide mandatory support.
- Selecting the appropriate mode balances oxygenation, ventilation, and respiratory muscle preservation in critically ill patients.
A patient in acute respiratory failure is receiving ACV with a positive end-expiratory pressure (PEEP) of 10 cm H₂O. What sign alerts the nurse to undesirable effects of increased airway and thoracic pressure?
Explanation
Positive end-expiratory pressure (PEEP) improves oxygenation by preventing alveolar collapse, but excessive PEEP increases intrathoracic pressure, which can impair venous return and reduce cardiac output. The earliest and most significant sign of this hemodynamic effect is decreased blood pressure.
Rationale for Correct Answer
1. Decreased blood pressure: Elevated intrathoracic pressure from high PEEP reduces venous return to the heart, lowering cardiac output and causing hypotension. This is an important early indicator of PEEP-induced hemodynamic compromise that requires prompt assessment and adjustment of ventilator settings.
Rationale for Incorrect Answers
2. Decreased PaO₂: PEEP is designed to improve oxygenation; a decrease in PaO₂ usually indicates a problem with lung compliance, secretions, or oxygen delivery, not direct hemodynamic compromise from PEEP.
3. Increased crackles: Crackles suggest pulmonary edema or fluid overload, which is not an immediate or reliable indicator of high PEEP effects.
4. Decreased spontaneous respirations: In ACV, the ventilator delivers full breaths; spontaneous respirations are minimal or absent and do not indicate PEEP-related hemodynamic compromise.
Take-Home Points
- High PEEP increases intrathoracic pressure, which can decrease venous return and cardiac output, causing hypotension.
- Monitor blood pressure and assess for signs of hemodynamic instability during PEEP therapy.
- Adjust PEEP carefully to balance oxygenation benefits with cardiovascular effects.
What should the nurse recognize as a factor commonly responsible for sodium and fluid retention in the patient on mechanical ventilation?
Explanation
Patients receiving mechanical ventilation often experience sodium and fluid retention due to increased antidiuretic hormone (ADH) release. Positive pressure ventilation increases intrathoracic pressure, reducing venous return and stimulating neurohormonal responses that promote water and sodium retention to maintain circulatory volume.
Rationale for Correct Answer
1. Increased release of ADH: Positive pressure ventilation decreases left atrial filling and cardiac output, triggering ADH secretion from the posterior pituitary. ADH increases water reabsorption in the kidneys, leading to fluid retention, mild hyponatremia, and potential edema, which are commonly observed in ventilated patients.
Rationale for Incorrect Answers
2. Increased release of atrial natriuretic factor: This hormone promotes sodium and water excretion, not retention. It is usually decreased in patients with positive pressure ventilation due to altered atrial stretch.
3. Increased insensible water loss via the airway: While mechanical ventilation can increase water loss from humidified gases, this results in fluid loss, not sodium and fluid retention.
4. Decreased renal perfusion with release of renin: Although renal hypoperfusion can trigger RAAS activation, ADH release is a more direct and consistent mechanism responsible for ventilation-related fluid retention.
Take-Home Points
- Positive pressure ventilation can trigger ADH-mediated fluid retention.
- Monitor for weight gain, edema, and hyponatremia in ventilated patients.
- Balance fluid therapy carefully to maintain hemodynamic stability without exacerbating retention.
A nurse is caring for a client who is experiencing respiratory distress. Which of the following are early clinical manifestations of hypoxemia? Select all that apply
Explanation
Early recognition of hypoxemia is essential in patients with respiratory distress, as initial signs are often subtle. The earliest manifestations usually involve neurologic and cardiovascular changes, such as confusion, pallor, and elevated blood pressure, reflecting compensatory responses to inadequate oxygen delivery.
Rationale for Correct Answers
1. Confusion: The brain is highly sensitive to low oxygen levels. Early hypoxemia often presents with altered mental status, anxiety, or confusion before more obvious physical signs develop.
2. Pale skin: Peripheral vasoconstriction occurs to preserve blood flow to vital organs, leading to pallor as an early visible sign of decreased tissue oxygenation.
5. Elevated blood pressure: The body initially compensates for hypoxemia by increasing sympathetic activity, causing tachycardia and elevated blood pressure to maintain tissue perfusion.
Rationale for Incorrect Answers
3. Bradycardia: Bradycardia is a late sign of hypoxemia, often occurring only after prolonged oxygen deprivation or severe hypoxia.
4. Hypotension: Hypotension is also a late manifestation, reflecting circulatory collapse after compensatory mechanisms fail.
Take-Home Points
- Early hypoxemia presents as neurologic changes, pallor, and elevated blood pressure.
- Bradycardia and hypotension are late signs indicating severe oxygen deprivation.
- Rapid assessment and intervention can prevent progression to respiratory failure or cardiac arrest.
A nurse is orienting a newly licensed nurse on performing routine assessment of a client who is receiving mechanical ventilation via an endotracheal tube. Which of the following should the nurse include in the teaching?
Explanation
Routine assessment of a patient receiving mechanical ventilation via an endotracheal tube (ETT) requires frequent monitoring to ensure adequate ventilation, early detection of complications, and tube placement verification. Assessing breath sounds every 1 to 2 hours allows the nurse to identify problems such as tube migration, obstruction, or pneumothorax promptly.
Rationale for Correct Answer
4. Assess breath sounds every 1 to 2 hours: Frequent auscultation helps detect unequal or absent breath sounds, which may indicate ETT displacement, mucus plugging, or lung collapse. This assessment is critical for ensuring adequate oxygenation and ventilation and should be part of routine care for all mechanically ventilated patients.
Rationale for Incorrect Answers
1. Apply a vest restraint if self-extubation is attempted: Restraints are used only as a last resort and not as part of routine assessment. Priority interventions should focus on sedation, monitoring, and safety precautions.
2. Monitor ventilator settings every 8 hours: Ventilator settings should be monitored continuously or at least every 1–2 hours, not only every 8 hours, to detect sudden changes in ventilation or patient-ventilator synchrony.
3. Document tube placement in centimeters at the angle of the jaw: ETT placement is typically documented at the lip or teeth, not the jaw, and should be checked frequently rather than once during orientation.
Take-Home Points
- Frequent auscultation of breath sounds (every 1–2 hours) is essential to detect early complications.
- Continuous monitoring of ventilator settings and patient response ensures safe mechanical ventilation.
- Tube security and placement must be verified frequently to prevent accidental extubation or malposition.
- Restraints and sedation are secondary safety measures, not routine assessment steps.
The purpose of adding PEEP to positive pressure ventilation is to:
Explanation
Positive end-expiratory pressure (PEEP) is added to mechanical ventilation to prevent alveolar collapse at the end of expiration, increase functional residual capacity (FRC), and improve oxygenation. It is particularly useful in patients with acute respiratory distress syndrome (ARDS) or hypoxemic respiratory failure.
Rationale for Correct Answer
1. Increase functional residual capacity and improve oxygenation: PEEP maintains alveolar patency, preventing atelectasis and improving gas exchange. By increasing FRC, more alveoli participate in oxygenation, which enhances PaO₂ and overall tissue oxygen delivery.
Rationale for Incorrect Answers
2. Increase FiO₂ in an attempt to wean the patient and avoid O₂ toxicity: FiO₂ is the fraction of inspired oxygen delivered, not affected by PEEP. PEEP improves oxygenation mechanically without altering FiO₂.
3. Determine if the patient is in synchrony with the ventilator or needs to be paralyzed: Ventilator synchrony is assessed through patient comfort, respiratory effort, and waveforms, not PEEP.
4. Determine if the patient is able to be weaned and avoid the risk of pneumomediastinum: PEEP is not a weaning tool. Excessive PEEP can increase the risk of barotrauma, including pneumomediastinum, rather than prevent it.
Take-Home Points
- PEEP improves oxygenation by maintaining alveolar recruitment and increasing functional residual capacity.
- Appropriate PEEP levels help reduce shunting and improve gas exchange in hypoxemic patients.
- Excessive PEEP can lead to barotrauma and hypotension, so careful titration and monitoring are essential.
- PEEP is distinct from FiO₂ adjustments and is part of ventilator management strategies to optimize oxygenation safely.
The nursing management of a patient with an artificial airway includes:
Explanation
Nursing management of a patient with an artificial airway requires careful attention to airway patency, patient safety, and monitoring for complications. Suctioning, while necessary, can stimulate the vagus nerve or irritate the myocardium, potentially causing cardiac dysrhythmias, making monitoring during the procedure essential.
Rationale for Correct Answer
3. Observing for cardiac dysrhythmias during suctioning: Suctioning an ET or tracheostomy tube can cause vagal stimulation, hypoxemia, or irritation of the myocardium, leading to bradycardia, PVCs, or other dysrhythmias. Continuous cardiac monitoring and pulse oximetry during suctioning allows for prompt recognition and intervention if complications occur.
Rationale for Incorrect Answers
1. Maintaining ET tube cuff pressure at 30 cm H₂O: Recommended cuff pressure is generally 20–25 cm H₂O to prevent tracheal injury while ensuring a seal; 30 cm H₂O is too high and increases the risk of tracheal necrosis.
2. Routine suctioning of the tube at least every 2 hours: Suctioning should be performed as needed based on secretions, breath sounds, and patient tolerance, not routinely on a fixed schedule, to reduce mucosal trauma and hypoxemia.
4. Preventing tube dislodgment by limiting mouth care to lubrication of the lips: Proper oral hygiene and tube stabilization are necessary to prevent infection and accidental extubation. Limiting care to lip lubrication does not adequately protect the airway.
Take-Home Points
- Monitor for cardiac dysrhythmias during airway suctioning due to vagal stimulation or hypoxia.
- Cuff pressures should be maintained at 20–25 cm H₂O to balance sealing and tissue safety.
- Suctioning should be based on patient need, not fixed intervals.
- Oral care and tube stabilization are critical to prevent infection and accidental extubation.
The nurse monitors the patient with positive pressure mechanical ventilation for:
Explanation
Patients receiving positive pressure mechanical ventilation are at risk for cardiovascular compromise because increased intrathoracic pressure can impede venous return to the heart, reducing cardiac output. The nurse should monitor for hypotension, tachycardia, and signs of poor perfusion.
Rationale for Correct Answer
3. Signs of cardiovascular insufficiency because pressure in the chest impedes venous return: Positive pressure ventilation increases intrathoracic pressure, which decreases venous return to the right atrium, leading to reduced stroke volume and cardiac output. Monitoring blood pressure, heart rate, urine output, and perfusion is essential to detect cardiovascular compromise early.
Rationale for Incorrect Answers
1. Paralytic ileus because pressure on the abdominal contents affects bowel motility: While critically ill patients may develop ileus, it is not directly caused by positive pressure ventilation.
2. Diuresis and sodium depletion because of increased release of atrial natriuretic peptide: Positive pressure ventilation actually stimulates ADH release, leading to fluid retention, not sodium depletion.
4. Respiratory acidosis in a patient with COPD because of alveolar hyperventilation and increased PaO₂ levels: Respiratory acidosis occurs with hypoventilation, not hyperventilation. Alveolar hyperventilation lowers PaCO₂ and increases PaO₂, which does not cause acidosis.
Take-Home Points
- Positive pressure ventilation can compromise cardiovascular function due to decreased venous return.
- Monitor for hypotension, tachycardia, and low urine output as indicators of reduced cardiac output.
- Adjust ventilator settings carefully to optimize oxygenation without adversely affecting hemodynamics.
A patient on mechanical ventilation suddenly triggers a high-pressure alarm. Which of the following should the nurse assess first?
Explanation
A high-pressure alarm on a mechanical ventilator indicates that airway resistance has increased or there is reduced lung compliance. The nurse’s first action should be to assess the patient’s airway for obstructions such as secretions, kinks in the tube, or biting of the ET tube, as these are the most common and immediately correctable causes.
Rationale for Correct Answer
1. The patient’s airway for secretions or kinking: Obstruction in the airway is the most common cause of a high-pressure alarm. Rapid assessment and intervention, such as suctioning or repositioning the ET tube, can restore ventilation and prevent hypoxia. Immediate patient assessment is priority over equipment checks.
Rationale for Incorrect Answers
2. The ventilator’s tubing connections: Loose or disconnected tubing usually triggers a low-pressure alarm, not high-pressure. While checking equipment is important, it is secondary to assessing the patient.
3. The humidifier water level: Low or high water in the humidifier may affect humidification but is unlikely to trigger a high-pressure alarm.
4. The patient’s urine output in the past hour: Urine output is unrelated to ventilator pressure alarms and is not an immediate concern in this context.
Take-Home Points
- High-pressure alarms usually indicate airway obstruction or decreased lung compliance.
- Immediate assessment of the patient’s airway is the first priority.
- Common interventions include suctioning secretions, repositioning the ET tube, or checking for kinks.
- Equipment and ventilator settings should be evaluated after patient safety is ensured.
The nurse is caring for a patient who is being weaned from mechanical ventilation. Which finding indicates that the patient is not yet ready for extubation?
Explanation
During weaning from mechanical ventilation, the nurse assesses respiratory strength, effort, and gas exchange to determine readiness for extubation. A high respiratory rate with shallow respirations indicates respiratory fatigue and inadequate ventilation, suggesting the patient is not yet ready for extubation.
Rationale for Correct Answer
2. Respiratory rate of 36 breaths/min and shallow respirations: A rapid, shallow breathing pattern reflects increased work of breathing and fatigue. This is a sign of poor ventilatory reserve, indicating the patient may fail extubation if removed from the ventilator prematurely.
Rationale for Incorrect Answers
1. Vital capacity of 12 mL/kg and strong cough reflex: Adequate vital capacity and a strong cough indicate the patient has sufficient lung expansion and airway clearance ability, supporting readiness for extubation.
3. Oxygen saturation consistently above 94% on FiO₂ 0.4: Adequate oxygenation on moderate FiO₂ suggests the patient can maintain sufficient gas exchange without high ventilatory support.
4. Negative inspiratory force (NIF) of −30 cm H₂O: NIF values more negative than −20 cm H₂O indicate adequate respiratory muscle strength for spontaneous breathing.
Take-Home Points
- Rapid, shallow breathing is a warning sign of ventilatory fatigue and extubation failure risk.
- Assess vital capacity, cough strength, oxygenation, and NIF to determine readiness for weaning.
- Extubation should only be attempted when the patient demonstrates adequate respiratory strength, effort, and oxygenation.
A patient receiving assist-control ventilation develops respiratory alkalosis on the latest arterial blood gas (ABG) results. What adjustment should the nurse anticipate the provider will make?
Explanation
Respiratory alkalosis in a patient receiving assist-control ventilation (ACV) usually results from hyperventilation, which causes excessive CO₂ elimination. The primary intervention is to reduce the ventilator rate to allow CO₂ to accumulate to normal levels, restoring acid-base balance.
Rationale for Correct Answer
1. Decrease the ventilator rate: Lowering the respiratory rate reduces minute ventilation, allowing PaCO₂ to rise and correcting respiratory alkalosis. This adjustment directly targets the cause of excessive alveolar ventilation.
Rationale for Incorrect Answers
2. Increase the FiO₂ level: FiO₂ affects oxygenation, not CO₂ elimination. Increasing FiO₂ does not correct alkalosis caused by hyperventilation.
3. Increase the tidal volume: Increasing tidal volume would further increase CO₂ elimination, worsening respiratory alkalosis rather than correcting it.
4. Add positive end-expiratory pressure (PEEP): PEEP improves oxygenation and alveolar recruitment, but it does not correct PaCO₂ or respiratory alkalosis.
Take-Home Points
- Respiratory alkalosis in mechanically ventilated patients is usually caused by hyperventilation.
- Decreasing the ventilator rate is the primary adjustment to normalize PaCO₂.
- Monitor ABGs after ventilator adjustments to ensure correction without compromising oxygenation.
- Always assess patient comfort, anxiety, and pain, as these can contribute to hyperventilation.
During endotracheal intubation, the nurse’s priority action to confirm correct tube placement immediately after insertion is to:
Explanation
Immediately after endotracheal tube (ETT) insertion, the nurse must confirm correct tube placement to ensure ventilation and oxygenation. Assessing bilateral breath sounds and observing for symmetrical chest rise provides rapid, reliable evidence that the tube is in the trachea rather than the esophagus.
Rationale for Correct Answer
2. Assess bilateral breath sounds and observe for symmetrical chest rise: Auscultation of both lungs and observation of chest movement immediately confirm tracheal placement. Absence of breath sounds on one side may indicate mainstem bronchus intubation, and absent breath sounds bilaterally suggests esophageal placement, both of which require immediate correction.
Rationale for Incorrect Answers
1. Obtain a chest X-ray: A chest X-ray is the gold standard for confirming tube depth but is not immediate. Initial verification must be done at the bedside before ventilating.
3. Check the patient’s oxygen saturation after 10 minutes: Waiting 10 minutes delays recognition of malposition, risking hypoxia. Immediate assessment is required.
4. Inflate the cuff and secure the tube: While necessary for stabilizing the airway, cuff inflation alone does not confirm correct tracheal placement.
Take-Home Points
- Immediate confirmation of ETT placement is critical to prevent hypoxia or gastric insufflation.
- Bilateral breath sounds and chest rise are rapid bedside assessments for correct placement.
- Chest X-ray should follow to verify tube depth, but is not the first step.
- Always monitor oxygen saturation and ventilator parameters after securing the tube.
The nurse is caring for a patient with an endotracheal tube. Which of the following findings requires immediate intervention?
Explanation
An absence of condensation in the ventilator tubing may indicate that the patient is not receiving adequate tidal volume, that the ventilator circuit is disconnected, or that airway obstruction is present. This finding requires immediate intervention to ensure ventilation and oxygenation are maintained.
Rationale for Correct Answer
2. Absence of condensation in the ventilator tubing: Condensation is a normal indicator of humidified gas flow during mechanical ventilation. A sudden absence may signal tube obstruction, disconnection, or ventilator malfunction, which can lead to rapid hypoxia. Immediate assessment and correction are necessary.
Rationale for Incorrect Answers
1. Cuff pressure of 20 cm H₂O: This is within the recommended safe range (20–25 cm H₂O) to prevent air leaks while minimizing tracheal injury.
3. Small amount of oral secretions present: This is expected in patients with an ET tube and is managed with routine suctioning.
4. Oxygen saturation of 95% on 40% FiO₂: This indicates adequate oxygenation and does not require immediate action.
Take-Home Points
- Immediate assessment is required if ventilator indicators suggest airway obstruction or disconnection.
- Condensation in the tubing serves as a quick visual cue for airflow and humidification.
- Maintain ET tube cuff pressures within 20–25 cm H₂O for safety.
- Monitor secretions, oxygen saturation, and ventilator function continuously to prevent complications.
Exams on Respiratory Management and Mechanical Ventilation
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
- Objectives
- Introduction
- Endotracheal Intubation
- Practice Exercise 1
- Mechanical Ventilation
- Key Ventilator Settings
- Practice Exercise 2
- Ventilator Alarms And Troubleshooting
- Nursing Management Of Mechanically Ventilated Patient
- Weaning And Extubation
- Practice Exercise 3
- Summary
- Comprehensive Questions
Notes Highlighting is available once you sign in. Login Here.
Objectives
- List the necessary equipment and critical steps for preparing a patient for Rapid Sequence Intubation (RSI).
- State the four crucial methods for confirming proper Endotracheal Tube (ETT) placement.
- Differentiate between the primary modes of mechanical ventilation (A/C, SIMV, PSV) and their clinical uses.
- Explain the significance of the four key critical ventilation parameters (VT, Rate, FiO2, PEEP).
- Apply the Ventilator-Associated Pneumonia (VAP) bundle to minimize patient risk.
- Perform assessment and troubleshooting of acute respiratory distress in the mechanically ventilated patient.
Introduction
This guide provides a comprehensive overview of the crucial nursing responsibilities related to endotracheal intubation (ETI) and the management of patients on mechanical ventilation (MV). These interventions are fundamental in critical care, often representing the difference between life and death for patients in acute respiratory failure. This resource is designed to solidify your knowledge of procedural preparation, continuous patient monitoring, interpretation of ventilator settings, and rapid troubleshooting, ensuring safe and effective care in the intensive care unit.
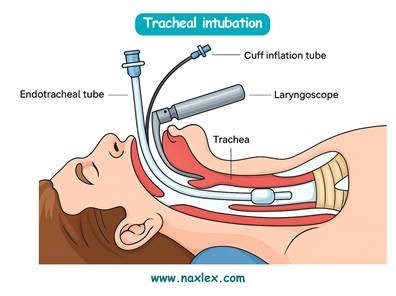
Endotracheal Intubation
Endotracheal Intubation (ETI): Principles and Nursing Role
Endotracheal Intubation (ETI) is the process of placing a flexible tube into the trachea to maintain a patent airway and provide mechanical ventilation. For a nurse, ETI represents a critical moment in patient care, demanding preparation, rapid assessment, and precise intervention.
Indications and Goals of Intubation
The primary goal of ETI is to support the patient's oxygenation and ventilation until the underlying cause of respiratory failure is resolved.
- Airway Protection: Preventing aspiration in patients with decreased level of consciousness, such as from drug overdose, stroke, or trauma.
- Respiratory Failure: Inability to maintain adequate oxygenation (PaO2) or ventilation (PaCO2), often requiring positive pressure support.
- Apnea or Severe Respiratory Distress: Complete cessation of breathing or severe exhaustion that precedes failure, for example, during a severe asthma exacerbation.
- General Anesthesia: Used to protect the airway and facilitate ventilation during surgical procedures.
Nursing Role: Before Intubation
Preparation is crucial for a successful and rapid intubation, often referred to as Rapid Sequence Intubation (RSI).
- Gather Equipment: Ensure all equipment is organized and functional.
- Suction: Test wall suction and have a Yankauer catheter and inline suction available.
- Oxygen: Have a 100% oxygen delivery system (bag-valve mask or Ambu bag) ready and connected.
- Airway Supplies: Laryngoscope (check light source), various endotracheal tube (ETT) sizes—typically 7.0-8.5 mm for adults—a stylet, and a syringe to inflate the cuff.
- Securement: Have a commercially available ETT holder or tape prepared.
- Be prepared to administer pre-medication, induction agents, and paralytics. A common RSI sequence involves a sedative/hypnotic, such as propofol or midazolam, followed immediately by a paralytic like succinylcholine or rocuronium.
- Position the patient in the "sniffing position" (neck flexed, head extended) to align the oral, pharyngeal, and tracheal axes for optimal visualization of the vocal cords.
Nursing Role During Intubation
The nurse monitors the patient and assists the provider, ensuring proper tube placement is confirmed immediately.
- Monitor Vitals: Continuously monitor heart rate, blood pressure, and oxygen saturation. Brief periods of desaturation during the attempt are expected.
- Cricoid Pressure: Apply gentle pressure on the cricoid cartilage (known as the Sellick maneuver) to occlude the esophagus, reducing the risk of gastric inflation and aspiration.
- Confirmation of Placement: Once the ETT is placed and the cuff is inflated, the following steps must be performed simultaneously to confirm tracheal placement and rule out dangerous esophageal placement:
- Auscultation: Listen for bilateral breath sounds over the lung fields and absence of sounds over the stomach (epigastrium).
- Capnography: The most reliable method. Check for the presence of end-tidal CO2 (EtCO2) indicated by a gold color on a colorimetric device or a waveform on the monitor. Sustained CO2 detection confirms tracheal placement.
- Visualization: Observe for bilateral chest rise and fall.
- Condensation: Look for condensation (fogging) in the ETT during exhalation.
Nursing Role After Intubation
- Securement: Secure the ETT immediately with a commercial ETT holder or tape at the measured depth, for example, 23 cm at the lip.
- Chest X-ray: Obtain a stat chest X-ray to confirm the final position of the ETT tip, which should rest 2-4 cm above the carina.
- Documentation: Document the tube size, the depth of the tube at the lip or gumline, initial CO2 readings, and the patient's response.
- Begin Ventilation: Connect the patient to the mechanical ventilator and ensure initial prescribed settings are accurate.
Mechanical Ventilation
Mechanical Ventilation (MV) is the process by which a machine (ventilator) assists or completely replaces spontaneous breathing.
Goals and Physiologic Effects
- Maintain Alveolar Ventilation: Ensure adequate PaCO2 and pH.
- Improve Oxygenation: Increase PaO2 and SaO2.
- Reduce Work of Breathing: Allow respiratory muscles to rest and recover.
- Physiologic Impact: MV, especially with Positive End-Expiratory Pressure (PEEP), increases intrathoracic pressure, which can decrease venous return to the heart, potentially leading to hypotension, a critical side effect.
Key Ventilator Settings
Ventilator modes dictate the control the machine has over the patient's breathing.
- Assist-Control (A/C) or Continuous Mandatory Ventilation (CMV):
- Function: The ventilator delivers a preset tidal volume (VT) or pressure and a preset rate. If the patient spontaneously breathes, the ventilator assists by delivering the full mandatory breath.
- Use: Used for patients requiring full respiratory support (heavily sedated or paralyzed).
- Risk: Hyperventilation and respiratory alkalosis if the patient triggers many breaths.
- Synchronized Intermittent Mandatory Ventilation (SIMV):
- Function: The ventilator delivers a preset tidal volume (VT) or pressure at a preset rate. Mandatory breaths are synchronized with the patient's spontaneous effort. Spontaneous breaths taken between mandatory breaths are limited to the patient's own effort, receiving no machine assistance.
- Use: Used for weaning; allows the patient to exercise respiratory muscles.
- Pressure Support Ventilation (PSV):
- Function: All breaths are spontaneous. The ventilator applies a preset amount of positive pressure to the patient’s spontaneous inspiratory effort to overcome the resistance of the ETT and reduce the work of breathing.
- Use: A comfort or weaning mode; the patient must have a reliable respiratory drive.
Critical Ventilation Parameters
- Tidal Volume (VT)
- Definition: Volume of gas delivered with each breath.
- Typical Range: 6-10 mL/kg (Ideal Body Weight)
- Nursing Significance: Keep low (4-8 mL/kg) for ARDS to prevent barotrauma.
- Rate (f)
- Definition: Number of breaths the ventilator delivers per minute.
- Typical Range: 10-20 breaths/min
- Nursing Significance: Affects PaCO2 (ventilation). Increasing the rate decreases CO2.
- FiO2
- Definition: Fraction of inspired oxygen (concentration).
- Typical Range: 0.21-1.0 (21% to 100%)
- Nursing Significance: Use the lowest possible setting (<0.5 - 0.6) to maintain PaO2 to prevent oxygen toxicity.
- PEEP
- Definition: Positive End-Expiratory Pressure. Pressure applied at the end of expiration.
- Typical Range: 5-15 cm H2O
- Nursing Significance: Prevents alveolar collapse. High PEEP can reduce cardiac output and cause hypotension.
Ventilator Alarms And Troubleshooting
The nurse is responsible for immediate assessment and intervention when an alarm sounds. NEVER silence an alarm without investigating the cause.
- High-Pressure Alarm: Indicates an obstruction or increased resistance to airflow.
- Causes: Secretions or mucus plug (the patient needs suctioning), biting the ETT (insert a bite block), coughing, pneumothorax, or water/kink in the tubing.
- Action: Assess the patient first, then the tube/circuit. Suction if needed.
- Low-Pressure Alarm: Indicates a leak or disconnection in the system.
- Causes: ETT cuff leak, tubing disconnection from the ETT or ventilator, or displacement of the ETT.
- Action: Check all connections. If the patient is disconnected, immediately use the Ambu bag to manually ventilate with 100% O2 and call for help.
Nursing Management Of Mechanically Ventilated Patient
Nursing care for a ventilated patient is intensive, continuous, and focused on preventing complications.
Ventilator-Associated Events (VAP) Prevention Bundle
The VAP bundle is a set of evidence-based nursing interventions applied collectively to reduce the risk of ventilator-associated pneumonia (VAP).
- Head of Bed (HOB) Elevation: Maintain HOB at 30-45 degrees to prevent aspiration and VAP.
- Daily Sedation Interruption (SIT) and Weaning Trials (SAT): The nurse collaborates with the provider/respiratory therapist to stop sedative infusions daily to assess the patient's neurological readiness for weaning. This is critical to decrease ventilation time.
- Peptic Ulcer Prophylaxis: Administer prescribed medications, such as proton pump inhibitors or H2 blockers, to prevent stress ulcers.
- Deep Venous Thrombosis (DVT) Prophylaxis: Administer anticoagulants, for instance enoxaparin, and use pneumatic compression devices.
- Oral Care: Perform meticulous mouth care, typically with an antiseptic solution like chlorhexidine, every 2-4 hours to reduce the bacterial burden that can lead to VAP.
- Inline Suctioning: Suction the patient only when indicated (visible secretions, coarse breath sounds, high-pressure alarm). Use a closed inline system to maintain a closed circuit and reduce infection risk.
Troubleshooting Respiratory Distres
When a ventilated patient suddenly develops acute respiratory distress (e.g., fighting the vent, low O2 sat, high peak pressures), use the DOPE mnemonic for rapid assessment:
- D: Dislodgement: Is the ETT displaced, perhaps pulled out or advanced into the right mainstem bronchus?
- O: Obstruction: Is the ETT obstructed by secretions, a kink, or the patient biting?
- P: Pneumothorax: Has a tension pneumothorax developed, indicated by sudden O2 drop, unilateral or absent breath sounds, tracheal deviation, or hemodynamic collapse?
- E: Equipment Failure: Is the ventilator or circuit malfunctioning, such as a disconnection or power failure?
Psychosocial Care
- Communication: Since the patient cannot speak, use alternative methods: writing pads, picture boards, or gestures. Ensure the call light is within reach.
- Sedation Management: Maintain adequate sedation to ensure comfort and cooperation with the ventilator, but avoid over-sedation which prolongs MV. Monitor with validated scales like the RASS.
- Environment: Minimize noise and light, and manage the patient’s fear and delirium.
Weaning And Extubation
Weaning is the process of gradually reducing ventilatory support and readying the patient for tube removal.
Weaning Parameters
The patient must meet established criteria, including:
- Resolution of the acute cause of respiratory failure.
- Stable hemodynamics (off or minimal vasopressors).
- Adequate gas exchange.
- Spontaneous Breathing Trial (SBT): The patient breathes spontaneously for a short period, typically 30-120 minutes, using minimal support, such as PSV 5 cm H2O and PEEP 5 cm H2O.
Nursing Role During Extubation
- Pre-Procedure: Explain the procedure. Have 100% O2, suction, and reintubation equipment immediately available. Hyperoxygenate the patient.
- Procedure: Suction the ETT and mouth above the cuff to minimize aspiration risk. The cuff is deflated fully, and the tube is removed during the patient's peak inspiration.
- Post-Procedure: Immediately provide O2 via face mask or nasal cannula.
- Monitoring (Critical): Assess for signs of respiratory distress, stridor (a high-pitched, crowing sound indicating upper airway edema), hoarseness, and decreased O2 saturation. Stridor may require rapid intervention with nebulized epinephrine or reintubation.
Summary
- Endotracheal Intubation is a rapid, high-stakes procedure where meticulous preparation (RSI) and prompt confirmation of tube placement are non-negotiable.
- Once ventilated, patient safety hinges on the nurse's ability to understand the physiologic impact of MV settings (VT, PEEP) and modes (A/C, SIMV).
- The nursing role is proactive, centered on the VAP prevention bundle, and reactive, demanding mastery of the DOPE mnemonic for troubleshooting sudden emergencies.
- Effective MV management is a critical care balance of providing life support, preventing complications, and diligently assessing the patient's readiness for extubation.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Respiratory Management and Mechanical Ventilation
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


