Please set your exam date
Safety
Study Questions
Practice Exercise 1
A nurse who is teaching a group of adults ages 20 to 40 years old about safety is going to ensure that which topic is a priority?
Explanation
Age-appropriate safety education must reflect the most common and preventable risks for the age group. Teaching priorities should align with data and public health trends.
Rationale for correct answer:
A. Automobile crashes: For adults aged 20 to 40 years, motor vehicle accidents are one of the leading causes of unintentional injury and death. Can be preventable through seat belt use, avoiding distracted/drunk driving, and obeying traffic laws.
Rationale for incorrect answers:
B. Drowning and firearms: Drowning is more common in children, while firearm safety is a broader public health issue that depends on region, occupation, and access.
C. Falls are a major concern in older adults (especially those over 65), not typically in younger, healthy adults.
D. Suicide and homicide: Mental health and violence are growing concerns, especially in young men, but as a general safety education topic, motor vehicle safety still takes precedence because of higher prevalence and universal risk.
Take home points:
- Motor vehicle accidents are a leading cause of death in adults aged 20–40.
- Automobile safety education (e.g., seat belts, DUI prevention, texting while driving) is thus top teaching priority.
When describing safety issues and related mortality to a local senior citizens group, which of the following would the nurse identify as the leading cause of accidental death for people 79 years of age and older?
Explanation
Older adults have unique vulnerability to injury-related death because of physiologic changes, comorbidities, and environmental risks.
Rationale for correct answer:
D. Falls: Falls are the predominant cause of injury-related morbidity and mortality in older adults, often leading to fractures, head injuries, loss of independence, and death.
Take home points
- Fall prevention is a top priority in geriatric care.
- Small, practical interventions (remove rugs, improve lighting, ensure assistive devices are used and fit properly) substantially reduce risk.
Rationale for incorrect answers:
A. Fires: Fires are a hazard but account for far fewer accidental deaths in the very old compared with falls.
B. Exposure to temperature extremes: Hypo-/hyperthermia can be fatal in elders but are not the leading cause of accidental death in this age group.
C. Drug overdose: Medication errors/overdose may occur, but they are not the top cause of accidental death for those ≥79.
Which action provided for legal protection of information voluntarily reported to an organization regarding safety issues?
Explanation
In the healthcare system, promoting a culture of safety includes encouraging the voluntary reporting of errors, near misses, and other safety concerns. To support this, specific legal protections have been put in place to ensure that healthcare providers can report such information without fear of legal liability or retaliation.
Rationale for correct answer:
D. Patient Safety and Quality Improvement Act of 2005: This law specifically provides legal protection for information voluntarily reported to Patient Safety Organizations (PSOs). It ensures confidentiality and protects against use of this data in lawsuits.
Rationale for incorrect answers:
A. Public Health Service Act: This act primarily supports public health activities such as disease prevention, medical research, and health education programs.
B. Report of the Institute of Medicine in 1999: The landmark report "To Err is Human: Building a Safer Health System" highlighted the prevalence of medical errors and sparked national attention on patient safety.
C. Centers for Disease Control and Prevention (CDC): The CDC focuses on controlling infectious diseases, public health emergencies, and surveillance.
Take home points:
- The Patient Safety and Quality Improvement Act of 2005 legally protects healthcare professionals who voluntarily report patient safety concerns.
- Not all influential health documents or organizations provide legal protection-understanding the difference between policy guidance and legal mandates is key in professional practice.
When planning to teach health care topics to a group of male adolescents, which topic should the nurse consider a priority?
Explanation
Adolescence is a developmental stage characterized by rapid physical, emotional, and cognitive changes, accompanied by increased risk-taking behaviors. Health teaching for adolescents should prioritize issues that significantly affect morbidity and mortality in this age group.
Rationale for correct answer:
C. Guns are the most frequently used weapon for adolescent suicide: Firearms are a leading means of suicide among male adolescents, making gun safety and suicide prevention education a top priority.
Rationale for incorrect answers:
A. Sports contribute to an adolescent’s self-esteem: While physical activity has benefits for self-esteem and overall health, it is not the highest priority when compared to immediate life-threatening risks like suicide or gun violence.
B. Sunbathing and tanning beds can be dangerous: Skin cancer prevention is important but not the most urgent concern for adolescent males compared to suicide prevention.
D. A driver’s education course is mandatory for safety: Driver safety is important, but in terms of priority, suicide and gun safety education take precedence due to higher mortality impact.
Take home points:
- Suicide is a leading cause of death among male adolescents, and firearms are the most common means used.
- Priority health education for this group should focus on suicide prevention and gun safety, addressing immediate threats to life.
A mother and her 3-year-old live in a home built in 193B. Which NANDA nursing diagnosis is most applicable for this child?
Explanation
Homes built before the mid-20th century commonly have lead-based paint (and may have deteriorating paint chips or dust). Young children (especially toddlers/preschoolers) are at high risk because of hand-to-mouth behavior and potential ingestion of paint chips or contaminated dust.
Rationale for correct answer:
C. Risk for Poisoning: The classic environmental hazard in very old homes is lead exposure/poisoning, so a NANDA diagnosis of Risk for Poisoning best captures the likely danger to a 3-year-old living in a 1932 house.
Rationale for incorrect answers:
A. Risk for Suffocation: More relevant for infants (e.g., unsafe bedding) or situations with small objects/entrapment; not the most specific hazard here.
B. Risk for Injury: While true that old homes present many injury risks, Risk for Poisoning pinpoints the specific, high-priority concern (lead).
D. Risk for Disuse Syndrome: Pertains to immobility and loss of function; not applicable to a healthy, mobile 3-year-old.
Take home points:
- For young children in pre-1950s/1970s homes, lead poisoning risk is a priority-assess for exposure and arrange blood lead screening per local guidelines.
- Teach caregivers about lead-safe practices (prevent peeling paint, wet-cleaning to reduce dust, safe renovation) and refer to public-health resources as needed.
Practice Exercise 2
The nurse is planning a health teaching session for new parents about poisoning emergencies. Which of the following would the nurse emphasize that the parents do first?
Explanation
When children ingest a potentially poisonous substance, immediate, appropriate action can reduce harm. The best first step is to obtain expert guidance (poison control or emergency services) because management varies by substance, amount, and the child’s age/condition.
Rationale for correct answer:
C. Call the poison control center: Poison control specialists give rapid, substance-specific instructions (whether to observe at home, induce no action, give an antidote, or go to ED) and can help prepare caregivers and clinicians.
Rationale for incorrect answers:
A. Use salt water to induce vomiting: Inducing vomiting at home is unsafe and generally not recommended; it can worsen injury (e.g., with corrosives or hydrocarbons).
B. Rush the child to the emergency department: In many cases the poison control center provides immediate instructions and triage advice; ED is needed if advised or if the child is symptomatic or the exposure is high-risk.
D. Routinely administer syrup of ipecac for any poison ingestion: Ipecac is no longer routinely recommended; it may be harmful and is not advised without specific medical direction.
Take home points:
- Call poison control immediately for guidance; keep the product container and the child’s age/weight available to give precise information.
- Do not induce vomiting or give home remedies unless explicitly instructed by poison control or a medical professional.
A male patient has weakened knees due to arthritis. The home healthcare nurse determines that he understands the need for safety modifications at home by which of the following?
Explanation
Home safety modifications for clients with mobility limitations (like arthritic knees) focus on reducing fall risk and making transfers easier and safer. Simple environmental changes and choice of furniture or assistive devices can greatly increase independence and prevent injury.
Rationale for correct answer:
C. Sitting primarily in chairs with armrests: Armrests provide stable leverage for standing and sitting, reducing stress on the knees and lowering fall risk.
Rationale for incorrect answers:
A. Using the towel bar for support to stand up from the commode: Towel bars are not anchored to bear body weight and can pull out, causing a fall. Use a properly installed grab bar instead.
B. Leaning on the pedestal table in his bedroom when he dresses: Pedestal or lightweight tables can tip or slide and are unsafe as weight-bearing supports.
D. Using a small stepladder to reach an item on an upper shelf: Stepladders increase fall risk for someone with weak knees; better options are a long-handled reacher or having items relocated to lower shelves.
Take home points:
- Choose stable furniture and devices designed for transfers (chairs with armrests, raised toilet seats with arm supports, properly installed grab bars).
- Avoid improvised supports and climbing; relocate frequently used items within easy reach.
While discussing home safety with the nurse, a patient admits that she always smokes a cigarette in bed before falling asleep at night. Which nursing diagnosis would be the priority for this patient?
Explanation
Smoking in bed is an immediate home-safety hazard because it’s a common cause of fatal residential fires.
Rationale for correct answer:
C. Risk for Suffocation related to unfamiliarity with fire prevention guidelines: Smoking in bed creates an acute, potentially life-threatening hazard (fire leading to smoke inhalation, burns, suffocation).
Rationale for incorrect answers:
A. Impaired gas exchange related to cigarette smoking: True as a long-term problem (COPD, chronic effects), but not the immediate priority compared with active fire risk from smoking in bed.
B. Anxiety related to inability to stop smoking: May be present, but it’s not the immediate safety priority.
D. Deficient knowledge related to lack of follow-through of recommendation to stop smoking: Education is needed, but first address the immediate life-threat (fire/suffocation); knowledge deficits are secondary.
Take home points:
Prioritize immediate safety risks (fire, smoke inhalation) over chronic sequelae when establishing nursing diagnoses and interventions.
Interventions:
- remove smoking materials from bedside
- discuss safer alternatives (smoke outside)
- provide smoking-cessation resources
- educate on fire safety, and consider home safety referrals.
A parent calls the pediatrician’s office frantic about the bottle cleaner that her 2-year-old son drank. Which of the following is the most important instruction the nurse gives to this parent?
Explanation
Accidental poisoning is a common emergency in young children due to their natural curiosity and tendency to explore their environment orally. When a caregiver contacts a nurse about a potential poisoning, the nurse must prioritize evidence-based, safe, and effective guidance based on the current best practice.
Rationale for correct answer:
C. Call the poison control center: The poison control center has toxicology experts available 24/7 who can provide specific, immediate, and safe instructions based on the exact substance ingested.
Rationale for incorrect answers:
A. Give the child milk: While milk was once considered a diluent for certain ingestions, it should not be given unless specifically advised by a poison control expert. It may interact with the substance ingested or delay appropriate treatment.
B. Give the child syrup of ipecac: Syrup of ipecac induces vomiting but is no longer recommended due to lack of evidence of benefit and risk of complications like aspiration, prolonged vomiting, and delayed treatment.
D. Take the child to the emergency department: While going to the ER may be necessary, Poison control can advise whether an ER visit is needed and what steps to take en route.
Take home points:
- Poison control centers are the best first point of contact for poisoning incidents in children-they provide immediate, expert guidance tailored to the situation.
- Outdated home remedies (like ipecac or milk) should not be used unless explicitly instructed by a medical professional, as they can worsen the situation.
The nursing assessment on a 78-year-old woman reveals shuffling gait, decreased balance, and instability. On the basis of the patient’s data, which one of the following nursing diagnoses indicates an understanding of the assessment findings?
Explanation
A comprehensive nursing assessment helps identify potential safety risks and functional limitations, especially in older adults. It’s critical for the nurse to interpret these findings accurately and formulate an appropriate nursing diagnosis. This promotes early intervention and prevents adverse outcomes, such as falls and injury.
Rationale for correct answer:
D. Risk for falls: A shuffling gait, decreased balance, and instability are classic indicators of fall risk in older adults. Identifying this risk allows nurses to implement safety measures like fall precautions and mobility aids.
Rationale for incorrect answer:
A. Activity intolerance: This diagnosis refers to a lack of physiological energy to complete activities, often due to cardiovascular or respiratory compromise.
B. Impaired bed mobility: This applies to difficulty moving in bed (turning, repositioning).
C. Acute pain: There is no indication of pain in the assessment data. Acute pain might contribute to mobility issues, but it must be explicitly assessed and reported to justify this diagnosis.
Take home points:
- “Risk for falls” is the most appropriate nursing diagnosis when a client displays mobility and balance issues, especially in the elderly.
- Always align your nursing diagnosis with the assessment findings-choose diagnoses that reflect the actual data, not assumptions or unrelated conditions.
Practice Exercise 3
Joint Commission guidelines regarding the use of restraints recommend which of the following?
Explanation
The Joint Commission (TJC) guidelines on the use of restraints, emphasize patient safety, dignity, and the minimization of harm. Restraints-whether physical or chemical-pose significant risks, including physical injury, psychological distress, and even death. Therefore, their use must comply with strict standards to ensure they are applied only when absolutely necessary.
Rationale for correct answer:
D. Alternative measures must be attempted first: TJC standards require that restraints be a last resort after less restrictive alternatives (such as sitter observation, environmental adjustments, or de-escalation) have been tried and documented.
Rationale for incorrect answers:
A. Vest restraints be used because they are the least restrictive type: Vest restraints are not considered the least restrictive; in fact, they pose a high risk of injury or death from strangulation.
B. Restraints should be used for 48 hours in nonpsychiatric patients: The Joint Commission requires that restraint orders for nonpsychiatric patients be renewed every 24 hours (or less), and the patient must be continually reassessed. A fixed “48 hours” policy violates these safety guidelines.
C. Restraints should be applied to prevent wandering behavior: Restraints are not indicated for preventing wandering, especially in patients with dementia. Wandering should be managed through safe environmental modifications, supervision, and redirection rather than physical restriction.
Take home points
- Restraints should only be used as a last resort, after documented attempts with less restrictive measures.
- Orders for restraints must follow strict time limits and require frequent reassessment to ensure ongoing necessity.
An older resident who is disoriented likes to wander the halls of his long-term care facility. Which of the following would be most appropriate for the nurse to use as an alternative to restraints?
Explanation
For residents with confusion or dementia, safety and dignity are priorities. Physical restraints are last-resort measures because they increase risk of injury, agitation, and loss of function. Best practice is to use least-restrictive, person-centered alternatives (environmental cues, supervision, safe wandering paths, diversion activities) to reduce wandering and the associated risks.
Rationale for correct answer:
D. Identifying his door with his picture and a balloon: Visual cues (photo, personalized decorations) help orient confused residents and reduce unsupported exits/wandering by making their room recognizable.
Rationale for incorrect answers:
A. Sitting him in a geriatric chair near the nurses’ station: Can be restrictive if used to immobilize him; it doesn’t promote orientation and may increase agitation over time.
B. Using the sheets to secure him snugly in his bed: Unsafe and constitutes an improper restraint - risk of injury, suffocation; inappropriate.
C. Keeping the bed in the high position: Dangerous- increases fall risk if he tries to climb out and can lead to serious injury; not an accepted safety practice.
Take home points:
- Use environmental, person-centered measures (personalized door signs, safe wandering routes, activity engagement) before restraints.
- Restraints and unsafe bed positions are last-resort and carry significant risk; always try supervision and reorientation first and document rationale/alternatives.
Nursing education efforts that focus on prevention of firearm injuries are important for which of the following reasons?
Explanation
Firearm injury prevention is a public-health and safety priority. Prevention education targets populations at highest risk (for homicide, suicide, unintentional injury) and focuses on safe storage, counseling, and community strategies that reduce access to lethal means for vulnerable people.
Rationale for correct answer:
B. Most homicide victims, 10 to 24 years of age, are killed with a gun: Firearms account for a large proportion of homicides among adolescents and young adults. That pattern makes firearm-safety education (safe storage, reducing youth access) especially important to lower youth mortality.
Rationale for incorrect answers:
A. The elderly population is particularly at risk for firearm injuries: Older adults are at elevated risk of firearm suicide in some countries, but they are not the primary group for firearm homicide risk.
C. The National Safety Council recommends a gun in every household to protect its members: Safety organizations emphasize risk reduction (safe storage, education), not recommending firearms as a universal household safety measure.
D. They have contributed to a decrease in injuries and deaths from guns: Education helps, but alone it has not reliably driven population-level decreases in firearm deaths; multifaceted strategies (policy, safe storage laws, access reduction, and community programs) are typically needed.
Take home points
- Firearm-safety education is especially important for preventing homicide and unintentional injury among adolescents and young adults.
- Effective prevention combines counseling on safe storage and access reduction with community/policy interventions- education alone is necessary but often not sufficient.
The nurse, at change-of-shift report, learns that one of the clients in his care has bilateral soft wrist restraints. The client is confused, is trying to get out of bed, and had pulled out the IV line, which was subsequently reinserted. Which action(s) by the nurse is appropriate? Select all that apply
Explanation
Use of physical restraints is a high-risk intervention and must follow legal/ethical standards and facility policy. Nurses must prioritize the client’s safety, use the least restrictive measure, document thoroughly, monitor neurovascular status, and provide removal/ROM and reorientation frequently.
Rationale for correct answers:
A.Document the behavior(s) that require continued use of the restraints: You must document the specific behaviors that justify restraint use (e.g., pulled IV, attempts to get OOB), the alternatives tried, the type/time of restraint, and ongoing reassessments.
C. Provide range-of-motion exercises when the restraints are removed: Periodic release of restraints (per policy, often at least every 2 hours) with ROM, repositioning, skin checks, toileting and nourishment prevents complications (contractures, skin breakdown, circulatory problems).
D. Orient the client: Reorientation, explanation of why restraints are used, and reassurance are nonpharmacologic, least-restrictive interventions that should be used continuously to reduce agitation and possibly shorten restraint duration.
E. Assess the tightness of the restraints: Regular neurovascular checks (capillary refill, pulses, sensation, color, temperature) and ensuring you can fit about two fingers between the restraint and skin are essential to prevent ischemia and nerve injury.
Rationale for incorrect answers:
B. Ensure that the restraints are tied to the side rails: Restraints must be secured to the bed frame (a immovable part) or use quick-release ties per policy - not to side rails, because side rails move and can cause entrapment or increased fall risk if the rail is raised/lowered.
Take home points:
- Use restraints only when absolutely necessary, with a physician order, and document the behavior, alternatives tried, and frequent reassessments.
- Tie restraints to the bed frame (not side rails), perform scheduled releases with ROM/skin care, and assess neurovascular status each check.
A client is being admitted to the hospital because of a seizure that occurred at his home. The client has no previous history of seizures. In planning the client’s nursing care, which of the following measures is most essential at this time of admission? Select all that apply
Explanation
When a client is admitted after experiencing a seizure-especially if it’s the first episode-ensuring immediate safety and preparedness for possible recurrence is a top nursing priority. Early interventions should focus on protecting the client from injury, maintaining airway patency, and being prepared to respond appropriately if another seizure occurs.
Rationale for correct answer:
B. Pad the bed with blankets: Padding protects the client from injury during involuntary movements of a seizure, especially if the seizure occurs while in bed.
E. Test oral suction equipment: Ensuring suction is functional prepares the nurse to clear secretions and maintain a patent airway if the client has another seizure, especially if vomiting or excessive saliva occurs.
Rationale for incorrect answers:
A. Place a padded tongue depressor at the head of the bed: Tongue depressors (padded or not) should never be placed in the mouth of a seizing client, as this can cause choking, dental injury, or airway obstruction.
C. Inform the client about the importance of wearing a medical identification tag: While important for long-term management, this is not essential during the admission phase, especially when the diagnosis is still being investigated.
D. Teach the client about epilepsy: The client has had a single seizure and does not yet have a diagnosis of epilepsy. Education should be based on confirmed conditions.
Take home points:
- Safety and airway management are top priorities during the initial care of a client who has had a seizure-bed padding and working suction equipment are essential.
- Client education and long-term planning (such as teaching about epilepsy or medical ID tags) should only begin after a confirmed diagnosis and once immediate risks are addressed.
Comprehensive Questions
A nurse sees smoke emerging from the suction equipment being used. Which is the greatest priority in the event of a fire?
Explanation
Follow the RACE protocol in fire emergencies:
- Rescue those in immediate danger
- Alarm (report the fire)
- Contain the fire
- Extinguish if possible and safe
Rationale for correct answer:
C. Protect the clients: The highest priority in the event of a fire is to protect and remove clients from immediate danger. Ensuring the safety of human life always takes precedence over property or protocol steps that can be performed afterward.
Rationale for incorrect answers:
A. Report the fire: While reporting the fire is part of the fire response protocol, it is not the first priority. Reporting comes after ensuring the safety of those in immediate danger.
B. Extinguish the fire: Attempting to extinguish a fire is only advisable if it is small and can be safely controlled. This is not the top priority because client and staff safety must be ensured before addressing the fire itself.
D. Contain the fire: Closing doors to prevent the spread of fire is important, but it is done after people in danger have been rescued and the fire has been reported.
Take home points:
- Client safety is the top priority during any emergency situation, including fires.
- Always act first to protect or remove clients from harm before any other action.
A 75-year-old client, hospitalized with a cerebrovascular accident (stroke), becomes disoriented at times and tries to get out of bed, but is unable to ambulate without help. What is the most appropriate safety measure?
Explanation
When caring for older adults who are hospitalized following a cerebrovascular accident (stroke), safety becomes a top priority-especially when the client is disoriented and at risk of falls. These individuals may have impaired mobility and cognitive function, increasing the likelihood of attempting to get out of bed without assistance. Choosing the most appropriate intervention requires balancing client safety with dignity and minimizing the use of restrictive measures.
Rationale for correct answer:
D. Use a bed exit safety monitoring device: These devices alert nursing staff immediately when the client attempts to leave the bed, allowing rapid intervention before a fall occurs. It provides real-time monitoring, supports fall prevention, and respects the client’s dignity.
Rationale for incorrect answers:
A. Restrain the client in bed: Physical restraints should only be used as a last resort when other interventions have failed and the client poses an immediate danger to themselves or others.
B. Ask a family member to stay with the client: While family presence can help reduce confusion and provide reassurance, it is not always feasible or a reliable safety intervention.
C. Check the client every 15 minutes: Frequent monitoring is useful, but it may not be timely enough to prevent a fall or injury if the client attempts to get up unassisted in between checks.
Take home points:
- Bed exit alarms are an effective, non-restrictive intervention for preventing falls in disoriented or high-risk clients who attempt to ambulate unassisted.
- Restraints should always be a last resort, used only when other safety interventions fail and the client is at immediate risk to themselves or others.
Which nursing intervention is the highest in priority for a client at risk for falls in a hospital setting?
Explanation
Preventing falls is a major nursing responsibility and involves identifying modifiable risk factors and implementing evidence-based safety interventions. Prioritizing actions that directly reduce the risk of injury and promote client safety is essential in any hospital setting.
Rationale for correct answer:
D. Place the bed in the lowest position: Lowering the bed reduces the height from which a client might fall and makes it easier for them to get in and out safely. It is a direct and effective intervention that helps prevent injury.
Rationale for incorrect answers:
A. Keep all of the side rails up: Raising all four side rails may seem protective, but it is considered a form of restraint and may increase the risk of injury if the client tries to climb over them.
B. Review prescribed medications: Medication review is essential, especially for drugs that cause dizziness or sedation. However, it is an indirect intervention and does not provide immediate protection from falls.
C. Complete the “get up and go” test: This test assesses mobility and fall risk, but it’s a screening tool, not an intervention. It’s useful for planning care but doesn’t actively prevent falls in the moment.
Take home points:
- Not all interventions are created equal-distinguishing between assessments, indirect strategies, and direct, high-impact actions is key to prioritizing nursing care.
- Lowering the bed is one of the most effective and immediate safety measures to reduce the risk and severity of falls in hospitalized clients.
The physiological changes of aging increase the risk for which of the following?
Explanation
Aging brings about a range of physiological changes that affect multiple body systems, including the musculoskeletal, sensory, and neurological systems. These changes can reduce balance, coordination, vision, and reaction time, increasing the vulnerability of older adults to certain safety hazards.
Rationale for correct answer:
C. Falls: Aging leads to decreased muscle strength, impaired balance, slowed reflexes, and changes in vision and proprioception-all of which significantly increase the risk of falls. Falls are the leading cause of injury-related death in adults aged 65 and older.
Rationale for incorrect answers:
A. Choking: While some older adults may experience difficulty swallowing (dysphagia), choking is not the most common or highest risk associated with normal aging.
B. Electrical hazards are more environmental in nature and not directly increased by aging itself.
D. Substance abuse: While substance misuse can occur in older adults (e.g., prescription misuse), it is not primarily due to physiological aging and is less prevalent compared to younger populations.
Take home points:
- Falls are the most common and dangerous consequence of the physiological changes associated with aging-prevention must be a top nursing priority.
- When assessing safety risks in older adults, focus on age-related changes in mobility, vision, and balance, rather than environmental or behavioral risks alone.
A physician writes an order to apply a wrist restraint to a patient who has been pulling out a surgical wound drain. Place the following steps for applying the restraint in the correct order.
Explanation
Step 1: Determine that restraint alternatives fail to ensure patient’s safety.
Restraints are never a first-line intervention. Nurses must assess and document that all less restrictive alternatives (like distraction, sitter, or repositioning) have been tried and failed.
Step 2: Identify the patient using proper identifier.
Patient identification using at least two identifiers (e.g., name and date of birth) ensures that care is delivered to the correct person, preventing potential errors.
Step 3: Explain what you plan to do.
Communication promotes trust and cooperation. Even if the patient is confused, explaining actions respects their dignity and may reduce agitation.
Step 4: Pad the patient’s wrist.
Padding prevents skin breakdown, bruising, and nerve damage by distributing pressure.
Step 5: Wrap a limb restraint around wrist or ankle with soft part toward skin and secure.
The restraint must be applied properly (soft side to skin, quick-release knot to bed frame) to ensure effectiveness and safety.
Take home points:
- Always attempt alternatives before restraints and document the failure of these measures; restraint use must be justified and time-limited.
- Patient safety and dignity are key-proper identification, explanation, and padding are essential steps before applying any restraint.
The nurse found a 68-year-old female patient wandering in the hall. The patient says she is looking for the bathroom. Which interventions are appropriate to ensure the safety of the patient? Select all that apply
Explanation
Older adults in hospital settings often experience disorientation, especially at night, which increases their risk for falls and injury. A patient found wandering in search of the bathroom may be experiencing confusion, urgency, or a change in routine. Nursing interventions must focus on safety, dignity, and fall prevention while promoting independence.
Rationale for correct answer:
B. Leave a night light on in the bathroom: Adequate lighting can reduce disorientation and help the patient safely locate the bathroom, especially at night.
E. Assign a staff member to stay with the patient: One-on-one observation may be needed for patients at high risk for wandering or falls, especially if disoriented.
F. Provide scheduled toileting during the night shift. Anticipating and meeting toileting needs can reduce unsupervised wandering and accidents.
G. Keep the pathway from the bed to the bathroom clear: A clear environment decreases tripping hazards and supports the patient’s safe ambulation.
Rationale for incorrect answers:
A. Insert a urinary catheter: Indwelling urinary catheters should be avoided unless absolutely necessary due to the risk of infection and reduced mobility.
C. Ask the physician to order a restraint. Restraints should be a last resort, used only when the patient poses a danger to self or others and other interventions have failed.
D. Keep the bed in low position with upper and lower side rails up. While a low bed is helpful, raising all side rails can act as a form of restraint and may increase injury risk if the patient tries to climb over.
Take home points:
- Prioritize environmental modifications and scheduled toileting for older adults who wander or are at risk of falls, rather than relying on restraints or catheters.
- Effective fall prevention includes supervision, adequate lighting, and a clutter-free path—all of which promote both safety and patient autonomy.
A child in the hospital starts to have a grand mal seizure while playing in the playroom. What is your most important nursing intervention during this situation?
Explanation
A grand mal (tonic-clonic) seizure involves loss of consciousness, muscle rigidity, and rhythmic jerking movements. The nurse’s primary responsibility during a seizure is to maintain the child’s safety and prevent injury while allowing the seizure to run its course. Immediate interventions should focus on environmental safety and airway protection-not on forcibly stopping the seizure.
Rationale for correct answer:
D. Clear the area around the child to protect the child from injury. Moving objects away reduces the risk of head trauma or bodily injury from uncontrolled muscle movements.
Rationale for incorrect answers:
A. Begin cardiopulmonary resuscitation (CPR). CPR is not appropriate during a seizure unless the child has stopped breathing and has no pulse after the seizure ends.
B. Restrain the child to prevent injury. Physical restraint can cause more harm, including fractures or soft tissue injury, and does not stop a seizure.
C. Place a tongue blade over the tongue to prevent aspiration. Forcing an object into a seizing person’s mouth is dangerous and may cause choking, dental injury, or aspiration.
Take home points:
- During a seizure, do not restrain the child or insert objects into their mouth-this increases the risk of injury or aspiration.
- The priority is to protect the child from injury by clearing the surroundings, placing something soft under the head if possible, and positioning them on their side once the seizure subsides to maintain airway patency.
How does the nurse support a culture of safety? Select all that apply
Explanation
A culture of safety in healthcare emphasizes shared responsibility, open communication, and proactive strategies to prevent harm. Nurses play a critical role in promoting this culture by reporting errors, near misses, and unsafe conditions without fear of blame.
Rationale for correct answers:
A. Completing incident reports when appropriate: Incident reports document adverse events and help facilities analyze root causes, implement corrective actions, and improve safety practices.
B. Completing incident reports for a near miss: Near misses offer valuable learning opportunities and are just as important to report as actual errors, as they highlight system vulnerabilities.
C. Communicating product concerns to an immediate supervisor: Reporting faulty or unsafe equipment/products can prevent harm to multiple patients and staff.
Rationale for incorrect answers:
D. Identifying the person responsible for an incident: Focusing on individual blame discourages reporting and erodes trust. Modern safety culture emphasizes systems thinking, not punishment.
Take home points:
- A true culture of safety encourages open reporting of errors and near misses to improve systems-not to assign blame.
- Nurses support safety by documenting incidents, communicating concerns, and participating in quality improvement efforts.
A school nurse is preparing a talk on healthcare topics for adolescents. Which of the following would be important for the nurse to include?
Explanation
Adolescence is a critical developmental period where individuals begin exploring autonomy, often engaging in risky behaviors, including substance use. School nurses play a pivotal role in promoting health literacy and prevention by addressing relevant topics such as alcohol use, tobacco, peer pressure, and decision-making.
Rationale for correct answer:
B. Reaching a BAL (Blood Alcohol Level) of 0.08 within 2 hours constitutes binge drinking: The CDC defines binge drinking as consuming enough alcohol to raise the BAL to 0.08 g/dL-typically 4 drinks for females or 5 for males in about 2 hours.
Rationale for incorrect answer:
A. Less than 10% of students report regular tobacco use: Understates the significance of nicotine use, especially in the form of vaping, which is a major concern today.
C. Teenagers are more likely to drink and drive: While some teens engage in drinking and driving, overall rates have declined due to education, legal consequences, and increased parental monitoring. Adults aged 21–34 are statistically more likely to drive under the influence.
D. Peer pressure has an insignificant effect on adolescent substance use: Peer influence is one of the strongest predictors of adolescent behavior, especially in relation to experimentation with substances.
Take home points:
- Adolescents must be educated using accurate, current health statistics and definitions, especially regarding risky behaviors like binge drinking and substance use.
- Peer pressure is a major contributor to adolescent risk-taking behaviors, and addressing it directly in educational programs is essential for prevention.
A nurse is assessing the following children. Which child would the nurse identify as having the greatest risk for choking and suffocating?
Explanation
Choking and suffocation are among the leading causes of unintentional injury and death in infants and young children. Their small airways, underdeveloped chewing abilities, and natural curiosity make them especially vulnerable to hazards in their environment.
Rationale for correct answer:
A. A toddler playing with his 9-year-old brother’s construction set: Small toy parts from older children’s toys (like a construction set) are a significant choking hazard for toddlers, who are prone to putting objects in their mouths.
Rationale for incorrect answers:
B. A 4-year-old eating yogurt for lunch: Yogurt is a soft, smooth-textured food and unlikely to cause choking in a child with developed chewing and swallowing skills.
C. An infant covered with a small blanket and asleep in the crib: While soft bedding is a suffocation risk and is discouraged in infant sleep safety guidelines, a small blanket may not pose as immediate a threat as small, ingestible objects in a toddler’s environment.
D. A 3-year-old drinking a glass of juice: Liquids like juice generally do not pose a choking hazard unless consumed too rapidly or if the child is laughing or crying while drinking.
Take home points:
- Toddlers are at highest risk for choking when exposed to toys or items not age-appropriate, especially those with small, detachable parts.
- Nurses must assess the child’s developmental stage and environment to proactively identify and eliminate choking and suffocation hazards.
An 87-year-old man is admitted to the hospital for cellulitis of the left arm. He ambulates with a walker and takes a diuretic medication to control symptoms of fluid retention. Which intervention is most important to protect him from injury?
Explanation
Older adults on diuretics often have nocturia and may be at increased risk of orthostatic hypotension (lightheadedness when standing). Combined with limited mobility (uses a walker), the greatest safety concern are falls.
Rationale for correct answer:
C. Provide a bedside commode: A bedside commode reduces the need for the patient to walk to the bathroom (especially at night), directly lowering fall risk.
Rationale for incorrect answers:
A. Leave the bathroom light on: Helpful (improves visibility) but less effective than eliminating the need to walk to the bathroom; the patient still must ambulate.
B. Withhold the client’s diuretic medication: Inappropriate without a provider’s order. Withholding could cause fluid overload and is not an acceptable independent nursing intervention; if medication side effects are suspected, report and collaborate with prescriber.
D. Keep the side rails up: Side rails can act as restraints, increase risk of entrapment or injury if the patient attempts to climb over them, and don’t prevent the primary risk (walking to the bathroom).
Take home points:
- Match fall-prevention to the risk: when toileting is the hazard, provide a bedside commode or frequent toileting assistance.
- Never withhold prescribed meds without provider direction; instead communicate concerns (e.g., nocturia, orthostatic symptoms) so dosing/timing can be adjusted safely.
Medication errors can place the client at significant risk. Which practice(s) will help decrease the possibility of errors? Select all that apply
Explanation
Medication errors are a significant threat to patient safety and can result in serious harm or even death. Preventing these errors requires a multifaceted approach that addresses human factors, system design, and workplace culture.
Rationale for correct answer:
C. Establish a reporting system for “near misses”: Near-miss reporting helps identify vulnerabilities in the system before they cause actual harm, enabling preventive measures to be implemented.
D. Communicate effectively: Clear communication among healthcare team members reduces the chance of misunderstandings in medication orders, dosing, or timing.
E. Create a culture of trust: A non-punitive environment encourages reporting of mistakes and near misses, leading to improvements in systems and processes.
Rationale for incorrect answers:
A. Hire only competent nurses: While hiring qualified nurses is important, this alone does not guarantee prevention of medication errors. Errors can still occur due to workload, poor communication, or systemic issues.
B. Improve the nurse’s ability to multitask: Encouraging multitasking can actually increase the risk of medication errors because it may cause distraction and reduce focus on critical tasks.
Take home points:
- Prevention of medication errors requires systemic safety measures, not just individual competence.
- Effective communication, a culture of trust, and reporting systems for near misses are key strategies to reduce risk.
The nurse is teaching parents of a toddler about the use of car seats. The nurse demonstrates an understanding of this measure by stating that car seats are mandatory in which of the following conditions?
Explanation
Child passenger safety is a major public-health priority. Laws and recommendations require appropriate child restraints (rear-facing seats, forward-facing harnesses, boosters) to reduce injury and death in vehicle crashes.
Rationale for correct answer:
A.In all 50 states: All U.S. states and territories have laws requiring child safety seats or appropriate restraints for young children; requirements (age/weight/height and type of seat) differ by state, but some form of mandatory child restraint law exists nationwide.
Rationale for incorrect answers:
B. In 36 of the 50 states: This is outdated and underestimates current legislative coverage; more states have enacted child restraint laws.
C. If a seat belt is not available: Child car-seat laws do not hinge on the presence/absence of an adult seat belt; they require age/size-appropriate child restraints regardless of seat-belt availability.
D. On interstate highways: Child restraint laws apply to general vehicle travel, not only interstates; the requirement is for all motor-vehicle use as defined by state statutes.
Take home points:
- Teach caregivers that child restraints are required by law in every state, but they must follow their state’s specific rules and current AAP recommendations.
- Emphasize correct installation, appropriate seat type for age/weight/height, and registering the car seat.
Which of the following would be most important for the nurse to keep in mind regarding the use of side rails for a confused patient?
Explanation
Side rails may seem like a straightforward safety measure, but for confused or cognitively impaired patients they can become a hazard (entrapment, injury, or even a form of restraint).
Rationale for correct answer:
D. A person of small stature is at increased risk for injury from entrapment: Small patients (or those with limited mobility) have a higher risk of becoming entrapped between rails or between the rail and mattress, which can cause injury or asphyxia.
Rationale for incorrect answers:
A. They prevent confused patients from wandering: Side rails do not reliably prevent wandering; they can give a false sense of security and may prompt a patient to climb over rails, increasing fall risk.
B. A history of a previous fall from a bed with raised side rails is insignificant: A prior fall in that context is highly significant and should prompt re-evaluation of bed setup and alternatives-it's an important safety cue.
C. Alternative measures are ineffective to prevent wandering: Many effective alternatives exist (low beds, bed/chair alarms, frequent rounding, sitter, environmental modifications, toileting schedule, reorientation), and these should be tried before using rails.
Take home points:
- Treat side rails as a potential restraint and assess risk of entrapment-especially for small or frail patients.
- Use least-restrictive alternatives (frequent checks, alarms, bedside commode, sitter) before resorting to rails and document the justification and monitoring.
When discussing emergency preparedness with a group of first responders, which of the following would be important to include about preparation for a terrorist attack?
Explanation
First responders must be prepared for the medical consequences of terrorist events (explosions, chemical/radiation releases, biological attacks). Preparedness includes knowledge of likely injury patterns, medical management priorities, and coordination with public health assets and stockpiled countermeasures.
Rationale for correct answer:
D. Blast lung injury is a serious consequence following detonation of an explosive device: Explosive blasts can cause primary blast injuries to the lungs (pulmonary contusion, hemorrhage, edema), which can be life-threatening and require specific clinical recognition and management.
Rationale for incorrect answers:
A. Posttraumatic stress disorders can be expected in most survivors of a terrorist attack: Many survivors experience acute stress reactions; PTSD is a known long-term risk but does not develop in most survivors.
B. The FDA has collaborated with drug companies to create stockpiles of emergency drugs: Federal preparedness does include strategic stockpiles (e.g., the Strategic National Stockpile) and public–private partnerships; the primary stockpile is managed by HHS/ASPR/CDC rather than the FDA.
C. Even small doses of radiation result in bone marrow depression and cancer: Acute bone-marrow depression occurs with high radiation doses (radiation sickness). Small doses may slightly increase long-term cancer risk but do not cause immediate marrow failure.
Take home points
- Expect specific primary blast injuries (including blast lung) after explosions; early recognition and supportive respiratory care are critical.
- Preparedness relies on accurate understanding of roles and resources.
- Training should emphasize realistic injury patterns and coordinated response rather than overstated generalizations.
When assessing a temperature rectally, the nurse would use extreme care when inserting the thermometer to prevent which of the following?
Explanation
Rectal temperature assessment provides a core body temperature, often considered highly accurate. However, it is also the most invasive route and carries certain risks, especially in vulnerable populations such as infants, children, and clients with cardiac conditions. Inserting a rectal thermometer stimulates the vagus nerve.
Rationale for correct answer:
B. A decrease in heart rate: Stimulating the vagus nerve during rectal temperature measurement can lead to bradycardia (a decreased heart rate).
Rationale for incorrect answers:
A. An increase in heart rate: Rectal insertion stimulates the vagus nerve, which causes a parasympathetic response. This response typically results in a decrease.
C. A decrease in blood pressure: While vagal stimulation can affect blood pressure, the primary concern during rectal temperature measurement is bradycardia, not hypotension.
D. An increase in respirations: Respiratory rate is generally not directly affected by rectal temperature measurement. An increase in respirations may occur due to fever or pain.
Take-home points:
- Rectal temperature assessment can stimulate the vagus nerve, leading to bradycardia, so nurses must insert the thermometer gently and shallowly.
- Avoid rectal temperature in newborns, cardiac patients, or those with rectal abnormalities to prevent serious complications.
A nurse is assessing vital signs on several hospitalized children. The nurse would plan to use the oral route to assess temperature for which patient?
Explanation
The route used to measure temperature (oral, rectal, axillary, tympanic, temporal) must be chosen based on age, level of consciousness, safety, and clinical condition.
Rationale for correct answer:
C. 15-year-old healthy adolescent: A 15-year-old is developmentally and physically able to hold the thermometer correctly under the tongue and follow instructions, making the oral route appropriate and accurate.
Rationale for incorrect answers:
A. 6-month-old infant: Infants are too young for oral temperature assessment due to safety risks, such as biting the thermometer, and inability to hold it in place properly.
B. Patient receiving oxygen therapy by mask: Clients on oxygen via face mask should not have oral temperatures taken because it requires removal of the mask, which interrupts oxygen delivery and may lead to hypoxia.
D. Unconscious patient: The oral route is contraindicated in unconscious or unresponsive clients due to risk of choking, aspiration, or injury.
Take-home points:
- The oral temperature route is suitable for alert, cooperative clients aged 4 years and older, especially adolescents.
- Avoid oral temperature in infants, unconscious clients, and those on oxygen masks, due to safety and accuracy concerns.
Exams on Safety
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
- Objectives
- Introduction
- Factors Affecting Patient Safety
- Common Potential Hazards Throughout The Life Span
- Types Of Accidents
- Nursing Diagnosis
- Nursing Assessment
- Practice Exercise 1
- Preventing Specific Hazards I
- Practice Exercise 2
- Preventing Specific Hazards II
- Restraints
- Practice Exercise 3
- Summary
- Comprehensive Questions
Notes Highlighting is available once you sign in. Login Here.
Objectives
- Describe the factors affecting environmental safety.
- Describe methods to assess a client’s risk for injury.
- Identify common potential hazards throughout the life span.
- Describe the categories of safety risks in a health care agency.
- Describe nursing interventions specific to a patients’ age for reducing risk of falls, fires, poisonings, radiation and electrical hazards.
- Discuss implementation of seizure precautions.
- Discuss the use and legal implications of restraints
- Describe alternatives to restraints.
Introduction
Safety, often defined as freedom from psychological and physical injury, is a basic human need.
Registered nurses (RNs) are responsible for providing the client with a safe environment through the delivery of professional, quality nursing care that incorporates safety precautions, infection control practices, and hygiene assistance.
A safe environment:
- Reduces the risk for illness and injury
- Helps to contain the cost of health care by preventing extended lengths of treatment
- Improves or maintaining a patient’s functional status
- Increases the patient’s sense of well-being.
A safe environment protects the staff as well, allowing them to function optimally.
Vulnerable groups who often require help in achieving a safe environment include infants, children, older adults, the ill, the physically and mentally disabled, the illiterate, and the poor.
Factors Affecting Patient Safety
The ability of people to protect themselves from injury is affected by several factors. Nurses need to assess each of these factors when they plan care or teach clients to protect themselves.
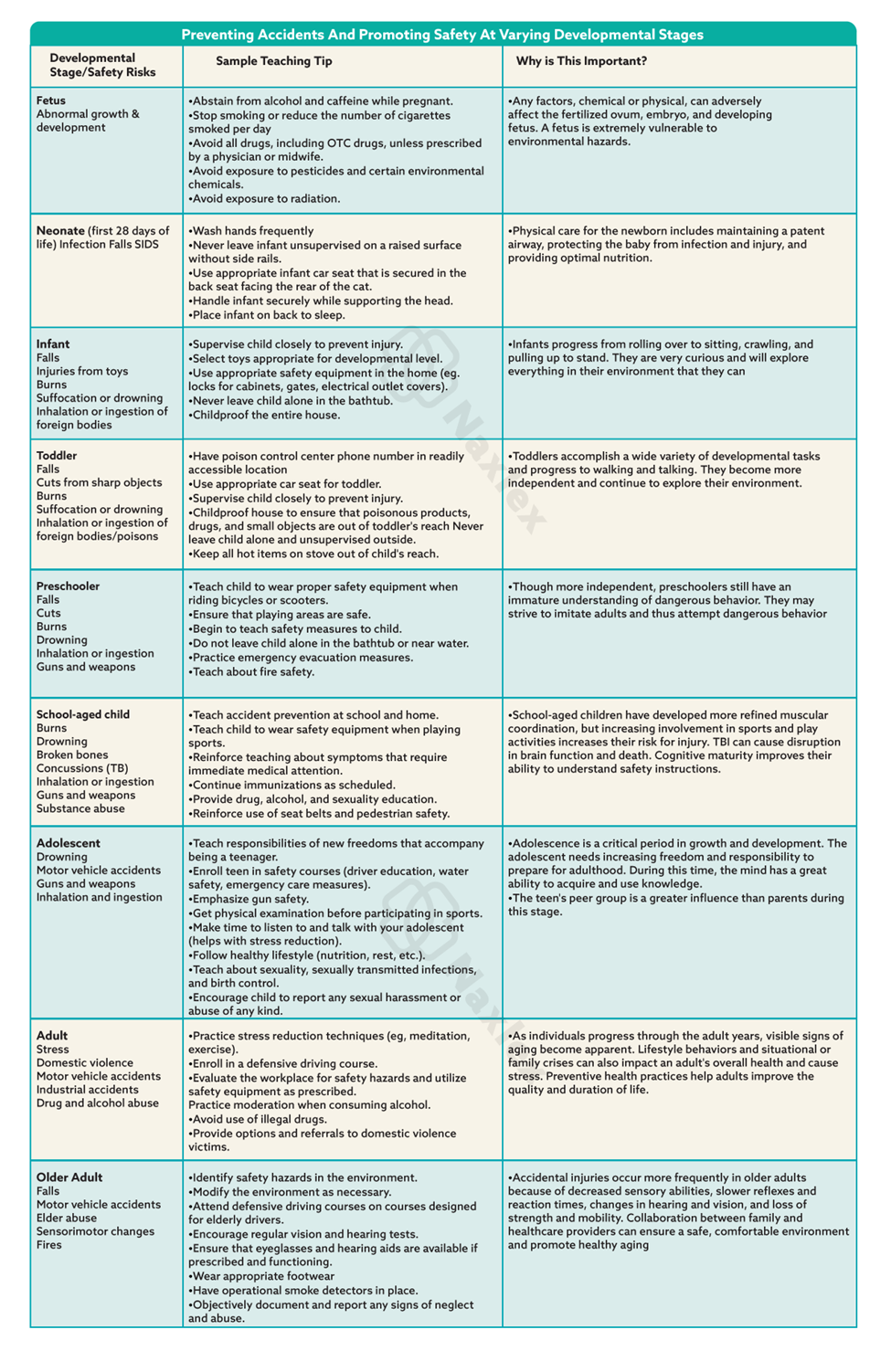
- Age and development: For the very young, learning about the environment is essential to avoid what is potentially harmful. Older adults can have difficulty with movement and diminished sensory-neurologic acuity, which can contribute to the likelihood of injury.
- Lifestyle: Includes unsafe work environments; residence in neighborhoods with high crime rates; access to firearms; insufficient income to purchase safety equipment or make necessary repairs; and access to illicit drugs.
- Mobility and health status: paralysis, muscle weakness, diminished balance, and lack of coordination place clients at risk for injury.
- Ability to communicate: Individuals with diminished ability to receive and convey information are at risk for injury. They include clients with aphasia, language barriers, or the ability to read.
- Emotional state: Stressful situations can reduce a person’s level of concentration, cause errors of judgment, and decrease awareness of external stimuli. Extreme emotional states can alter the ability to perceive environmental hazards.
- Sensory-perceptual alterations: People with impaired touch perception, hearing, taste, smell, and vision are highly susceptible to injury.
- Cognitive awareness: include people lacking sleep; people who are unconscious or semiconscious; disoriented people; people who perceive stimuli that do not exist; and people whose judgment is altered by disease or medications, such as narcotics, tranquilizers, hypnotics, and sedatives.
- Safety awareness: Lack of knowledge about unfamiliar equipment, such as oxygen tanks, intravenous tubing, and hot packs, is a potential hazard.
Common Potential Hazards Throughout The Life Span
Developing fetus:
Exposure to:
- Maternal smoking, alcohol consumption, addictive drugs.
- X-rays (first trimester)
- Pesticides
Newborns and infants:
- Falling
- Choking
- Suffocation in crib
- Burns from hot water or other spilled hot liquids
- Placement in the prone position
- Automobile crashes, crib or playpen injuries
- Suffocation when entangled in cords
- Electric shock, poisoning
Toddlers:
- Physical trauma from falling
- Running into objects
- Aspiration of small toys
- Getting cut by sharp objects
- Automobile crashes
- Burns; poisoning; drowning; and electric shock
Preschoolers:
- Injury from traffic, playground equipment, and other objects
- Choking, suffocation, and obstruction of airway or ear canal by foreign objects
- Poisoning
- Drowning; fire and burns
- Harm from other people or animals
Adolescents:
- Vehicular (automobile, bicycle) crashes
- Recreational injuries
- Firearms, substance abuse
- Sexually transmitted diseases.
Older adults:
- Falls
- Burns
- Pedestrian and automobile crashes
Types Of Accidents
In the health care setting, accidents are categorized by their causative agent: client behaviors, therapeutic procedures, or equipment:
1. Client behavior accidents occur when the client’s behavior or actions precipitate the incident, for example, poisonings, burns, and self-inflicted cuts and bruises.
2. Therapeutic procedure accidents occur during the delivery of medical or nursing interventions, for example, medication errors, client falls during transfers, contamination of sterile instruments or wounds, and improper performance of nursing activities.
3. Equipment accidents result from the malfunction or improper use of medical equipment, for example, electrocution and fire.
Nursing Diagnosis
The primary nursing diagnosis risk for injury exists when the client is at risk for injury as a result of environmental conditions interacting with the individual’s adaptive and defensive resources.
NANDA (North American Nursing Diagnosis Association) has six defined subcategories of specific risk factors for this diagnostic labeling:
- Risk for suffocation: An accentuated risk of accidental suffocation.
- Risk for poisoning: An accentuated risk of accidental exposure to, or ingestion of, drugs or dangerous products in doses sufficient to cause poisoning
- Risk for trauma: An accentuated risk of accidental tissue injury (e.g., wound, burn, fracture)
- Risk for aspiration: Risk for entry of gastrointestinal secretions, oropharyngeal secretions, solids, or fluids into the tracheobronchial passages
- Risk for disuse syndrome: Risk for deterioration of body or body systems as the result of prescribed or unavoidable musculoskeletal inactivity
- Risk for latex allergy response: Risk for allergic response to natural latex rubber products
Nursing Assessment
During the assessment process thoroughly assess each patient and critically analyze findings to ensure that you make patient-centered clinical decisions required for safe nursing care.
Patients usually do not purposefully put themselves in jeopardy. When they are uninformed or inexperienced, threats to their safety occur.
To conduct a thorough patient assessment, consider possible threats to a patient’s safety, including the immediate environment and any individual risk factors.
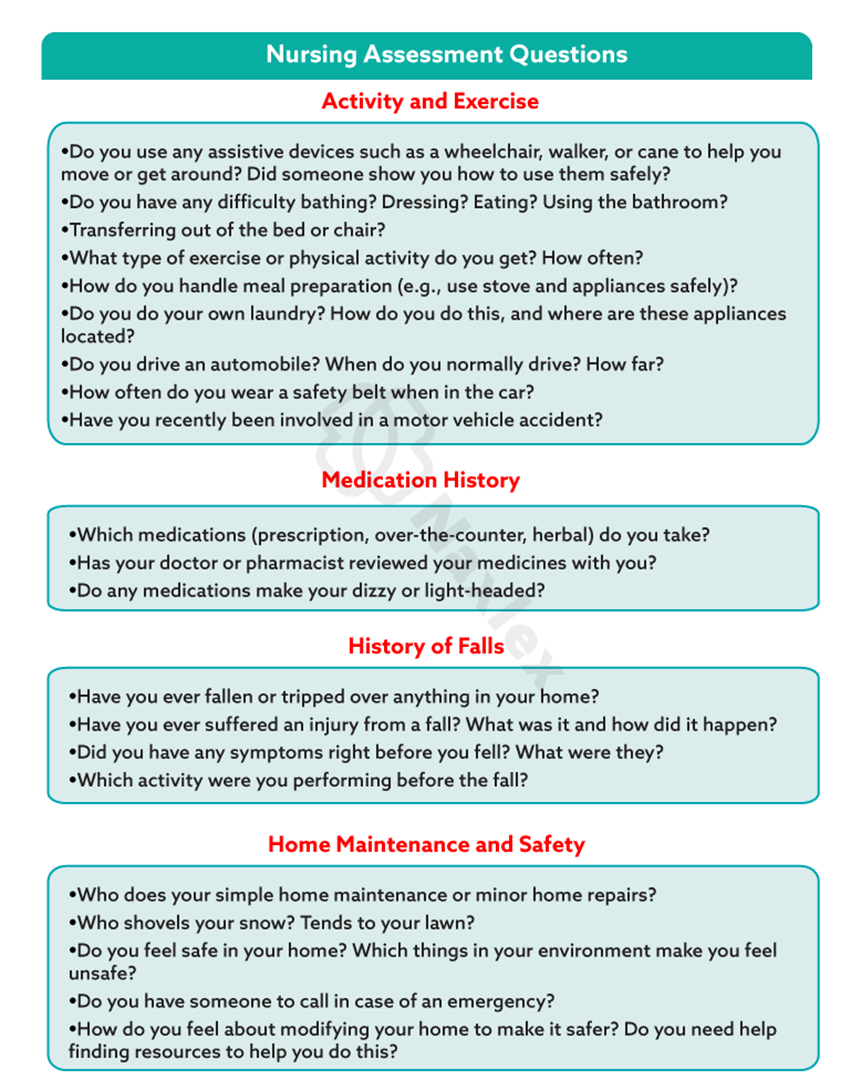
Health care environment:
When the patient is cared for within a health care facility, you need to determine if any hazards exist in the immediate care environment.
- placement of equipment (e.g., drainage bags, IV pumps) or furniture
- positioning of the patient’s bed
- assistance with ambulation
- multiple tubes or IV lines
- call bell within reach
Risk for Medical Errors:
Be alert to factors within your own work environment that create conditions in which medical errors are more likely to occur.
- overwork and fatigue
- patient’s identification by using two identifiers
Nursing insights:
- Nurses need awareness of what constitutes a safe environment for specific individuals and for groups of people in the home, community, and workplace.
- Hazards to safety occur at all ages and vary according to the age and development of the individual.
Preventing Specific Hazards I
Falls
People of any age can fall, but infants and older adults are particularly prone to falling and causing serious injury. Falls are the leading cause of injuries among older adults.
It is important to assess clients for fall risk on admission, whenever a change in physical or mental status occurs, on transfer, and before discharge.
Fall risk appraisal:
|
Risk Factor |
Points |
|
Age 60-69 years (1 point) 70-79 years (2 points) ≥80 years (3 points |
|
|
Fall History One fall within 6 months before admission (5 points) |
|
|
Elimination (Bowel and Urine) Incontinence (2 points) Urgency or frequency (2 points) Urgency/frequency and incontinence (4 points) |
|
|
Medications: Includes PCA/Opiates, Anticonvulsants, Antihypertensives, Diuretics, Hypnotics, Laxatives, Sedatives, and Psychotropics On one high fall–risk drug (3 points) On two or more high fall–risk drugs (5 points) Sedated procedure within past 24 hours (7 points) |
|
|
Patient Care Equipment: Any Equipment That Tethers Patient (e.g., IV Infusion, Chest Tube, Indwelling Catheters, SCDs) One present (1 point) Two present (2 points) 3 or more present (3 points) |
|
|
Mobility (Multi-select, Choose All That Apply and Add Points Together) Requires assistance or supervision for mobility, transfer, or ambulation (2 points) Unsteady gait (2 points) Visual or auditory impairment affecting mobility (2 points) |
|
|
Cognition (Multi-select, Choose All That Apply and Add Points Together) Altered awareness of immediate physical environment (1 point) Impulsive (2 points) Lack of understanding of one’s physical and cognitive limitations (4 points) |
|
|
TOTAL: Moderate risk = 6-13 total points High risk = >13 total points |
|
NB: The data obtained from the client’s fall risk appraisal will identify which clients require special nursing measures to prevent falls.
Fall Prevention strategies
1. Assessment
- Perform client injury risk appraisal and identify fall risks. Update status of fall risks daily and as needed on a nursing care plan.
- Assess effects of medications administered that increase risk of falling.
2. Client teaching
- On admission, orient clients to their surroundings and explain the call system.
- Instruct client and significant others on correct use of hospital equipment.
- Instruct client with risk for falls to call for assistance when ambulating or performing activities of daily living (ADL).
3. Environmental interventions:
- Keep the environment tidy; keep light cords from underfoot and furniture out of the way.
- Carefully assess the client’s ability to ambulate and transfer.
- Provide walking aids and assistance as required.
- Encourage the client to use the call light to request assistance. Ensure that the light is within easy reach.
- Place bedside tables and overbed tables near the bed or chair so that clients do not overreach and consequently lose their balance.
- Always keep hospital beds in the low position and wheels locked when not providing care so that clients can move in or out of bed easily.
- Encourage clients to use grab bars mounted in toilet and bathing areas and railings along corridors.
- Make sure nonskid bath mats are available in tubs and showers.
- Encourage the client to wear nonskid footwear.
- Closely supervise the clients at risk for falls, especially at night.
- Use individualized interventions (e.g., alarm sensitive to client position) rather than side rails for confused clients.
- Use mechanical or electronic ceiling lifts to transfer dependent clients.
4. Direct nursing care:
- Respond promptly to call lights and verbal requests for assistance.
- Provide assistance with ADL.
- Maintain close supervision by performing hourly safety assessments.
- Encourage significant others to stay with high-risk clients.
- Provide proper equipment for ambulation and elimination needs.
- Document in the client’s medical record.
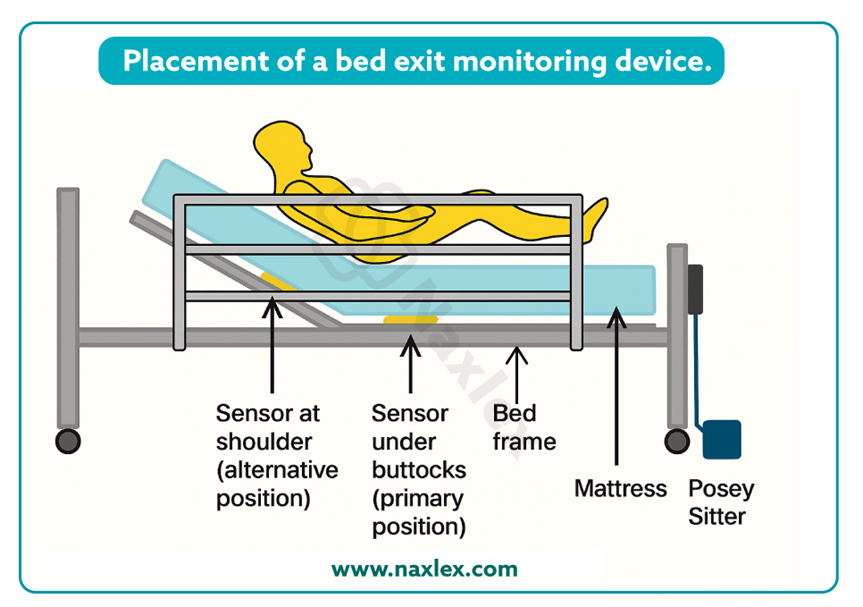
The alarm device is position sensitive; that is, when it approaches a near-vertical position (such as in walking, crawling, or kneeling as the client attempts to get out of bed), the audio alarm will be triggered.
Fire safety
Fire is a potential danger to all people in an institutional or a home environment. It occurs with the interaction of three elements: sufficient heat to ignite the fire, combustible material, and oxygen to support the fire.
Common causes of fire are:
- smoking in bed
- discarding cigarette butts in trash cans
- faulty electrical equipment
Immobilized or incapacitated clients are at increased risk during a fire.
Interventions aimed at reducing the risk of fire:
- Clearly marking fire exits
- Knowing locations of fire extinguishers and their operation
- Practicing fire evacuation procedures
- Posting emergency phone numbers by all telephones
- Keeping open spaces and hallways clear of clutter
- Checking electrical cords and outlets for exposed or damaged wires
- Reporting identified electrical hazards
- Educating clients about fire hazards
In the event of a fire:
Nursing interventions during a fire are directed at protecting the client from injury and containing the fire.
When smoke or fire is detected, two mnemonics can help the nurse remember the steps to follow. First is the RACE protocol:
- Rescue: If the area is safe to enter, protect and evacuate clients who are in immediate danger.
- Alarm: Pull the fire alarm and report the fire details and location to the hospital’s fire emergency extension.
- Confine: Contain the fire by closing the doors to all rooms and the fire doors at each entrance to the unit.
- Extinguish: Extinguish the fire. Use the appropriate type of fire extinguisher (see the PASS mnemonic) OR Evacuate the area if the fire is too large for a fire extinguisher.
The nurse follows the mnemonic PASS when using a fire extinguisher:
- Pull out the extinguisher’s safety pin.
- Aim the hose at the base of the fire.
- Squeeze or press the handle to discharge the material onto the fire.
- Sweep the hose from side to side across the base of the fire until the fire appears to be out.
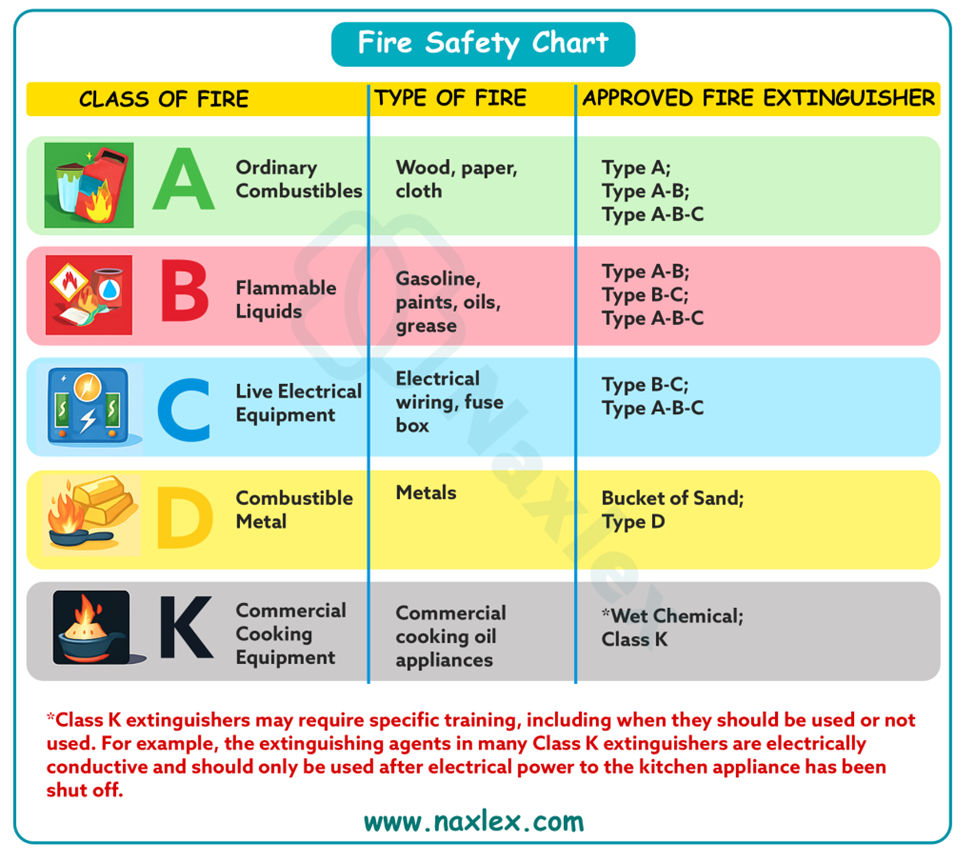
Extinguishing the fire requires knowledge of three categories of fire, classified according to the type of material that is burning:
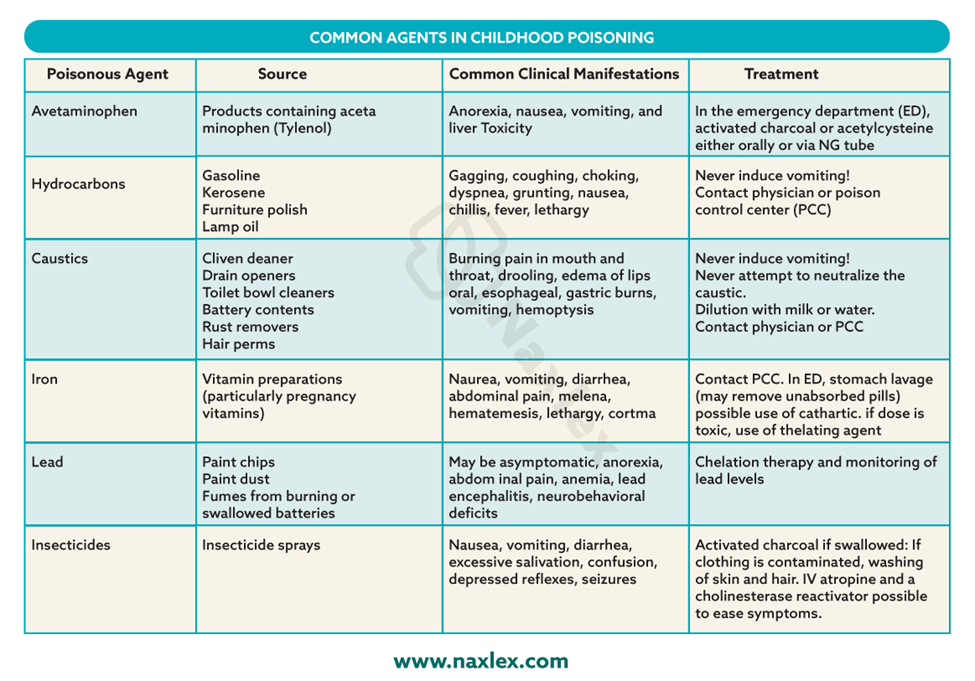
Poisoning
A poison is any substance that causes an alteration in the client’s health, such as injury or death, when inhaled, injected, ingested, or absorbed by the body.
Antidotes and treatments are available for some but not all types of poisonings.
Causes of poisonings are:
• Inadequate supervision of children
• Ingestion of household plants
• Improper storage of toxic substances
• Insect or snake bites
• Accidental ingestion of a toxic substance or medication overdose- due to failing eyesight/ impaired memory.
• Carbon monoxide poisoning
Carbon monoxide poisoning: Carbon monoxide (CO) is an odorless, colorless, tasteless gas that is very toxic. Exposure to CO can cause symptoms that include headaches, dizziness, weakness, nausea, vomiting, or loss of muscle control. Prolonged exposure to CO can lead to unconsciousness, brain damage, or death.
Preventing poisoning:
- Lock potentially toxic agents, in a cupboard, or attach special plastic hooks to the insides of cabinet doors to keep them securely closed.
- Do not let children watch you open the latches.
- Store medications in child-resistant containers.
- Do not take medications in front of children.
- Avoid storing toxic liquids or solids in food containers.
- Do not remove container labels or reuse empty containers to store different substances.
- Do not rely on cooking to destroy toxic chemicals in plants.
- Teach children never to eat any part of an unknown plant.
- Do not keep poisonous plants in the home, and avoid planting poisonous plants in the yar
- Place poison warning stickers designed for children on containers with toxic substances.
- Read and follow label directions on all products before using them.
- Keep syrup of ipecac on hand at all times.
- Display the phone number of the poison control center near or on all telephones in the home so that it is available to babysitters, family, and friends.
Interventions in accidental poisoning:
1. Assess for signs or symptoms of ingestion of harmful substance:
- nausea, vomiting
- foaming at the mouth, drooling
- difficulty breathing
- sweating, and lethargy.
2. Terminate exposure to the poison by having the person empty his or her mouth of pills, plant parts, or other material.
3. If poisoning is caused by skin or eye contact, irrigate the skin or eye with copious amounts of cool tap water for 15 to 20 minutes.
4. In the case of an inhalation exposure, safely remove the victim from the potentially dangerous environment.
5. Identify the type and amount of substance ingested to help determine the correct type and amount of antidote needed.
6. Call the local poison control center or the national toll-free poison control center number (1-800-222-1222) before attempting any intervention.
7. If the victim has collapsed or stopped breathing, call 911 for emergency transportation to the hospital. Initiate CPR if indicated until emergency personnel arrive.
8. Position the victim with head turned to the side to reduce risk for aspiration.
9. Never induce vomiting if the victim has ingested the following poisonous substances: lye, household cleaners, hair care products, grease or petroleum products, furniture polish, paint thinner, or kerosene.
10. Never induce vomiting in an unconscious or convulsing victim because vomiting increases risk for aspiration.
Electrical hazards
All electric equipment must be properly grounded. Grounding prongs offer a path of least resistance to stray electric currents.
The electric plug of grounded equipment has three prongs. The two short prongs transmit the power to the equipment. The third, longer prong is the grounding device, which carries short circuits or stray electric current.
Faulty equipment such as equipment with a frayed cord presents a danger of electric shock or may start a fire.
Actions to reduce electrical hazards:
- Check cords for fraying or other signs of damage before using an appliance. Do not use it if damage is apparent.
- Avoid overloading outlets and fuse boxes with too many appliances.
- Use only grounded outlets and plugs.
- Always pull a plug from the wall outlet by firmly grasping the plug and pulling it straight out. Pulling a plug by its cord can damage the cord and plug unit.
- Never use electric appliances near sinks, bathtubs, showers, or other wet areas, because water readily conducts electricity.
- Keep electric cords and appliances out of the reach of young children.
- Place protective covers over wall outlets to protect young children.
- Have all non-insulated wiring in the home altered to meet safety standards.
- Carefully read instructions before operating electric equipment. Clients who do not understand how to operate the equipment should seek advice.
- Always disconnect appliances before cleaning or repairing them.
- Unplug any appliance that has given a tingling sensation or shock and have an electrician evaluate it for stray current.
- Keep electric cords coiled or taped to the ground away from areas of traffic to prevent others from damaging the cords or tripping over them.
If a client receives an electrical shock:
- Turn off or remove the electric source before touching the client.
- The client’s pulse should be checked.
- If the client has no pulse, CPR should be initiated.
- If the client has a pulse, the nurse should assess vital signs, mental status, and skin integrity for burns.
- A prescribing practitioner should be notified of the event.
- The nurse should note points of entry and exit of electrical current to assess for potential complications.
Preventing Specific Hazards II
Radiation
Clients are exposed to radiation during diagnostic testing and therapeutic interventions.
Injury can occur from radiation if there is overexposure or exposure to untargeted tissues.
Radiation therapy destroys cancer cells, with minimal exposure of normal cells to the damaging effects of radiation; the damaged cells die or become unable to divide.
Radiation therapy is effective on tissues directly within the path of the radiation beam.
Side effects include local skin changes and irritation, alopecia (hair loss), fatigue (most common side effect of radiation), and altered taste sensation; the effects vary according to the site of treatment.
Types of radiation therapy:
External beam radiation (also called teletherapy) and internal radiation (also called brachytherapy) are the types of radiation therapy most commonly used to treat cancer.
a) External beam radiation (teletherapy):
The actual radiation source is external to the client.
1. Instruct the client regarding self-care of the skin.
2. The client does not emit radiation and does not pose a hazard to anyone else.
b) Brachytherapy
1. The radiation source comes into direct, continuous contact with tumor tissues for a specific time.
2. The radiation source is within the client; for a period of time, the client emits radiation and can pose a hazard to others.
3. Brachytherapy includes an unsealed source or a sealed source of radiation.
Unsealed radiation source
a. Administration is via the oral or IV route or by instillation into body cavities.
b. The source is not confined completely to one body area, and it enters body fluids and eventually is eliminated via various excreta, which are radioactive and harmful to others. Most of the source is eliminated from the body within 48 hours; then neither the client nor the excreta is radioactive or harmful.
Sealed radiation source
a. A sealed, temporary or permanent radiation source (solid implant) is implanted within the tumor target tissues.
b. The client emits radiation while the implant is in place, but the excreta are not radioactive.
Radiation safety:
1. Know the protocols and guidelines of the health care agency.
2. Label potentially radioactive material.
3. To reduce exposure to radiation, do the following.
- Limit the time spent near the source.
- Make the distance from the source as great as possible.
- Use a shielding device such as a lead apron.
4. Monitor radiation exposure with a film (dosimeter) badge.
5. Place the client who has a radiation implant in a private room.
6. Never touch dislodged radiation implants/ body fluids from client.
7. Keep all linens in the client’s room until the implant is removed.
8. Label all potentially radioactive material.
9. Dispose of radioactive substances in special containers.
Seizures
A seizure is a single temporary event that consists of uncontrolled electrical neuronal discharge of the brain that interrupts normal brain function.
Causes of seizures:
The etiology or cause of the seizure can be different based on the age of the client.
- Trauma during birth is the leading cause of seizures in newborns.
- Infants and children develop seizures as a result of fever, trauma, and infections of the central nervous system.
- Adults- most commonly related to structural abnormalities of the brain such as tumors, strokes, and trauma.
Types of seizures:
Partial seizures (also called focal) involve electrical discharges from one area of the brain.
Generalized seizures affect the whole brain.
NB: Clients are at risk for injury if they experience seizures that involve the entire body such as grand mal (tonic-clonic) seizures or any seizure that includes loss of consciousness.
Seizure precautions:
Seizure precautions are safety measures taken by the nurse to protect clients from injury should they have a seizure.
Include:
1. Assessment
Assess the patient's seizure history and knowledge of precipitating factors.
Assess medication history and patient’s adherence.
Assess for medical and surgical conditions, including electrolyte disturbances
2. Environmental considerations
Pad the bed of any client who might have a seizure.
Secure blankets or other linens around the head, foot, and side rails of the bed.
Put oral suction equipment and oxygen equipment in place and test to ensure that it is functional.
3. In the event of a seizure:
Note time, stay with patient, and call for help.
Track duration of seizure.
Notify health care provider immediately. Have staff member bring an emergency cart to the bedside.
Position the patient safely. If standing or sitting, guide the patient to the floor and protect the head by cradling in the nurse's lap or placing a pad under head. Turn the patient onto one side, head tilted slightly forward.
Clear surrounding area of furniture. If the patient is in bed, remove pillows and raise side rails.
Do not restrain the patient; hold limbs loosely if they are flailing.
Loose clothing such as a collar or belt.
Maintain the patient's airway and suction as needed.
1. Post seizure:
Assist patient to position of comfort in bed with side rails up (one rail down for easy exit).
Place the bed in the lowest position.
Place the call light or intercom system within reach.
Provide a quiet, non-stimulating environment.
Record thoroughly in nurses’ notes your observations before, during, and after seizure.
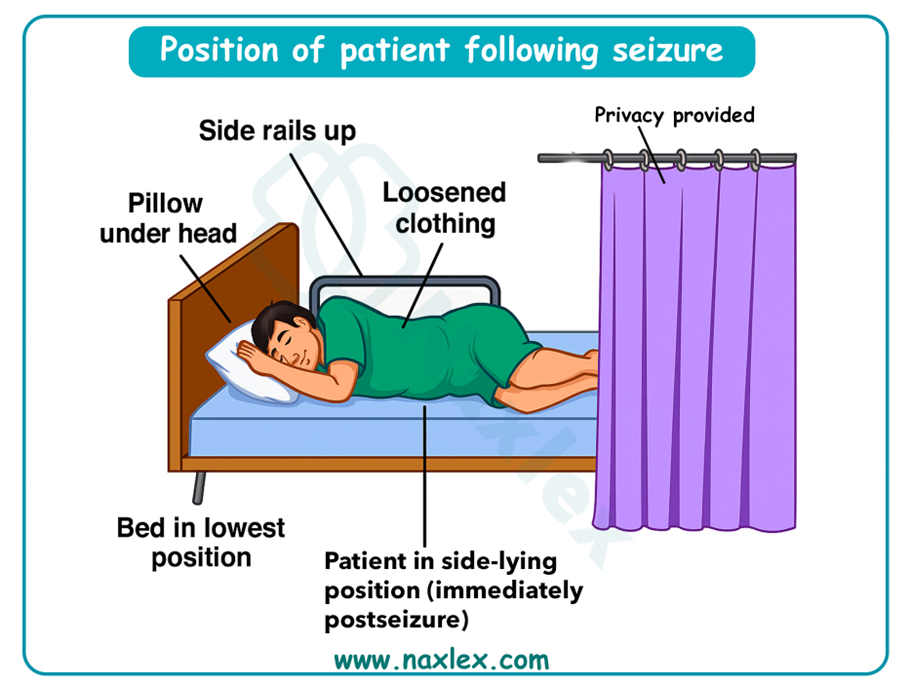
Firearms
The following basic firearm safety rules must be implemented for any gun:
- Store all guns in sturdy locked cabinets without glass and make sure the keys are inaccessible to children.
- Store the bullets in a different location from the guns.
- Tell children never to touch a gun or stay in a friend’s house where a gun is accessible.
- Teach children never to point the barrel of a gun at anyone.
- Ensure the firearm is unloaded and the action is open when handing it to someone else.
Restraints
Restraints are devices used to limit the physical activity of a client or a part of the body.
All patients have the right to be free from restraint or seclusion, of any form, imposed as a means of coercion, discipline, convenience, or retaliation by staff.
Restraint or seclusion may only be imposed to ensure the immediate physical safety of the patient, a staff member, or others and must be discontinued at the earliest possible time.
Restraints can be classified as:
- physical restraints
- chemical restraints
- use of seclusion
Physical restraints: Any manual method, physical or mechanical device, material, or equipment that immobilizes or reduces the ability of a patient to move his or her arms, legs, body, or head freely.
Examples: Leather or cloth wrist and ankle restraints, soft belts or vests, hand mitts, pelvic ties, gerichairs, and overchair tables.
Chemical restraints: Using a medication to control behavior or to restrict the client’s freedom of movement.
Seclusion: This is the involuntary confinement of a client alone in a room or area from which the client is physically prevented from leaving.
Seclusion may only be used for the management of violent or self-destructive behavior that is an immediate threat to the client’ s physical safety.
Risks of improper use of restraints:
Improper use of restraints and lack of monitoring can lead to injury and death and to psychological harm. Restraints can cause injury to clients through:
- Hazards of immobility (e.g., muscle atrophy, bone loss, contractures, pressure ulcers, constipation, and decreased appetite)
- Confusion, boredom and loneliness, depression, and loss of dignity.
- Death can result due to strangulation, suffocation, broken necks, burns, pneumonia, and sepsis.
Standards for Use of Restraints:
- Restraints should be used only after every other possible means of ensuring safety have been unsuccessful and documented.
- There must be a face-to-face evaluation of the client within 1 hour by the physician or LIP, or an RN or physician assistant (PA) who has been trained.
- A written restraint order for an adult with violent or self-destructive behavior, following evaluation, is valid for only 4 hours for up to a total of 24 hours.
- Primary care provider’s order for restraints include: delineation of the reason for, specific time frame (only for violent or self-destructive behavior), and type of restraint necessary.
- Restrained clients must be monitored regularly.
- Restraint or seclusion must be discontinued at the earliest possible time.
- “As-needed” (prn) orders for restraints are prohibited.
Selecting a restraint:
5 criteria:
- It restricts the client’s movement as little as possible.
- It is safe for the particular client.
- It does not interfere with the client’s treatment or health problems.
- It is readily changeable.
- It is as discreet as possible
Applying restraints:
- Obtain consent from the client or guardian.
- Assure the client and the client’s support people that the restraint is temporary and protective.
- Pad bony prominences (e.g., wrists and ankles) before applying a restraint over them.
- Always tie a limb restraint with a knot (e.g., a clove hitch) that will not tighten when pulled.
- Tie the ends of a body restraint to the part of the bed that moves to elevate the head.
- Never tie the ends to a side rail or to the fixed frame of the bed if the bed position is to be changed.
- Apply a restraint so that it can be released quickly in case of an emergency and with the body part in a normal anatomic position.
- Check restraint for constriction by inserting two fingers under restraint.
- Assess skin integrity per agency protocol (e.g., every 2 hours), and provide range-of-motion (ROM) exercises and skin care when restraints are removed.
- Assess and assist with basic needs: nutrition, hydration, hygiene, elimination.
- Reassess the continued need for the restraint.
- Immediately report to the nurse in charge and record on the client’ s chart any persistent reddened or broken skin areas under the restraint.
- At the first indication of cyanosis or pallor, coldness of a skin area, or a client’s complaint of a tingling sensation, pain, or numbness, loosen the restraint and exercise the limb.
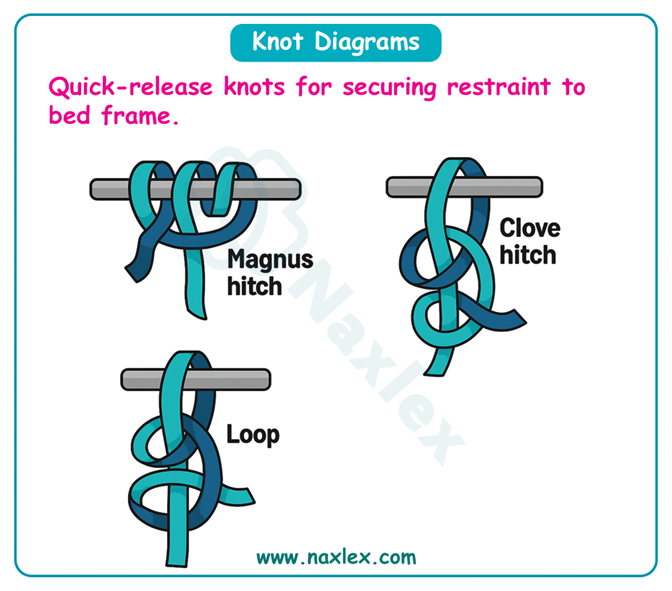
Alternatives to restraints:
- Ask family members or significant others to stay with the client.
- Reduce stimulation (e.g., noise, lights); play soothing music.
- Assign nurses in pairs to act as “buddies” so that one nurse can observe the client when the other leaves the unit.
- Place unstable clients in an area that is constantly or closely supervised.
- Prepare clients before a move to limit relocation shock and resultant confusion.
- Use rocking chairs to help confused clients expend some of their energy so that they will be less inclined to wander.
- To quiet agitated clients, try a warm beverage, soft lights, a back rub, or a walk.
- Use “environmental restraints,” such as pieces of furniture or large plants as barriers, to keep clients from wandering beyond appropriate areas.
- Place a picture or other personal item on the door to clients’ rooms to help them identify their room.
- Try to determine the causes of the client’s sundowner-syndrome.
Nursing insights:
Measures to ensure the safety of people of all ages focus on:
(a) observation or prediction of situations that are potentially harmful
(b) client education that empowers clients to safeguard themselves and their families from injury.
Summary
- Nurses need awareness of what constitutes a safe environment for specific individuals and for groups of people in the home, community, and workplace.
- Hazards to safety occur at all ages and vary according to the age and development of the individual.
- Nurses assess clients at risk for injury through methods such as nursing history and physical examination, risk assessment tools, and home hazard appraisal.
Comprehensive Questions
Falls
People of any age can fall, but infants and older adults are particularly prone to falling and causing serious injury. Falls are the leading cause of injuries among older adults.
It is important to assess clients for fall risk on admission, whenever a change in physical or mental status occurs, on transfer, and before discharge.
Fall risk appraisal:
|
Risk Factor |
Points |
|
Age 60-69 years (1 point) 70-79 years (2 points) ≥80 years (3 points |
|
|
Fall History One fall within 6 months before admission (5 points) |
|
|
Elimination (Bowel and Urine) Incontinence (2 points) Urgency or frequency (2 points) Urgency/frequency and incontinence (4 points) |
|
|
Medications: Includes PCA/Opiates, Anticonvulsants, Antihypertensives, Diuretics, Hypnotics, Laxatives, Sedatives, and Psychotropics On one high fall–risk drug (3 points) On two or more high fall–risk drugs (5 points) Sedated procedure within past 24 hours (7 points) |
|
|
Patient Care Equipment: Any Equipment That Tethers Patient (e.g., IV Infusion, Chest Tube, Indwelling Catheters, SCDs) One present (1 point) Two present (2 points) 3 or more present (3 points) |
|
|
Mobility (Multi-select, Choose All That Apply and Add Points Together) Requires assistance or supervision for mobility, transfer, or ambulation (2 points) Unsteady gait (2 points) Visual or auditory impairment affecting mobility (2 points) |
|
|
Cognition (Multi-select, Choose All That Apply and Add Points Together) Altered awareness of immediate physical environment (1 point) Impulsive (2 points) Lack of understanding of one’s physical and cognitive limitations (4 points) |
|
|
TOTAL: Moderate risk = 6-13 total points High risk = >13 total points |
|
NB: The data obtained from the client’s fall risk appraisal will identify which clients require special nursing measures to prevent falls.
Fall Prevention strategies
1. Assessment
- Perform client injury risk appraisal and identify fall risks. Update status of fall risks daily and as needed on a nursing care plan.
- Assess effects of medications administered that increase risk of falling.
2. Client teaching
- On admission, orient clients to their surroundings and explain the call system.
- Instruct client and significant others on correct use of hospital equipment.
- Instruct client with risk for falls to call for assistance when ambulating or performing activities of daily living (ADL).
3. Environmental interventions:
- Keep the environment tidy; keep light cords from underfoot and furniture out of the way.
- Carefully assess the client’s ability to ambulate and transfer.
- Provide walking aids and assistance as required.
- Encourage the client to use the call light to request assistance. Ensure that the light is within easy reach.
- Place bedside tables and overbed tables near the bed or chair so that clients do not overreach and consequently lose their balance.
- Always keep hospital beds in the low position and wheels locked when not providing care so that clients can move in or out of bed easily.
- Encourage clients to use grab bars mounted in toilet and bathing areas and railings along corridors.
- Make sure nonskid bath mats are available in tubs and showers.
- Encourage the client to wear nonskid footwear.
- Closely supervise the clients at risk for falls, especially at night.
- Use individualized interventions (e.g., alarm sensitive to client position) rather than side rails for confused clients.
- Use mechanical or electronic ceiling lifts to transfer dependent clients.
4. Direct nursing care:
- Respond promptly to call lights and verbal requests for assistance.
- Provide assistance with ADL.
- Maintain close supervision by performing hourly safety assessments.
- Encourage significant others to stay with high-risk clients.
- Provide proper equipment for ambulation and elimination needs.
- Document in the client’s medical record.
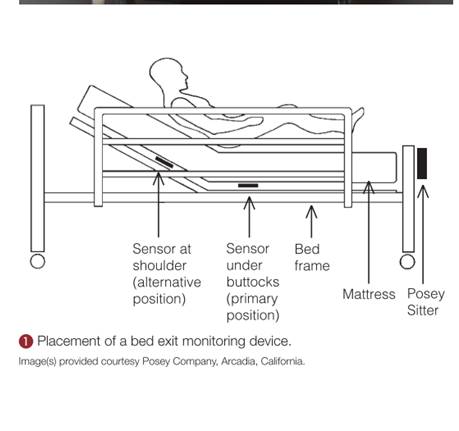
The alarm device is position sensitive; that is, when it approaches a near-vertical position (such as in walking, crawling, or kneeling as the client attempts to get out of bed), the audio alarm will be triggered.
Fire safety
Fire is a potential danger to all people in an institutional or a home environment. It occurs with the interaction of three elements: sufficient heat to ignite the fire, combustible material, and oxygen to support the fire.
Common causes of fire are:
- smoking in bed
- discarding cigarette butts in trash cans
- faulty electrical equipment
Immobilized or incapacitated clients are at increased risk during a fire.
Interventions aimed at reducing the risk of fire:
- Clearly marking fire exits
- Knowing locations of fire extinguishers and their operation
- Practicing fire evacuation procedures
- Posting emergency phone numbers by all telephones
- Keeping open spaces and hallways clear of clutter
- Checking electrical cords and outlets for exposed or damaged wires
- Reporting identified electrical hazards
- Educating clients about fire hazards
In the event of a fire:
Nursing interventions during a fire are directed at protecting the client from injury and containing the fire.
When smoke or fire is detected, two mnemonics can help the nurse remember the steps to follow. First is the RACE protocol:
- Rescue: If the area is safe to enter, protect and evacuate clients who are in immediate danger.
- Alarm: Pull the fire alarm and report the fire details and location to the hospital’s fire emergency extension.
- Confine: Contain the fire by closing the doors to all rooms and the fire doors at each entrance to the unit.
- Extinguish: Extinguish the fire. Use the appropriate type of fire extinguisher (see the PASS mnemonic) OR Evacuate the area if the fire is too large for a fire extinguisher.
The nurse follows the mnemonic PASS when using a fire extinguisher:
- Pull out the extinguisher’s safety pin.
- Aim the hose at the base of the fire.
- Squeeze or press the handle to discharge the material onto the fire.
- Sweep the hose from side to side across the base of the fire until the fire appears to be out.
Extinguishing the fire requires knowledge of three categories of fire, classified according to the type of material that is burning:
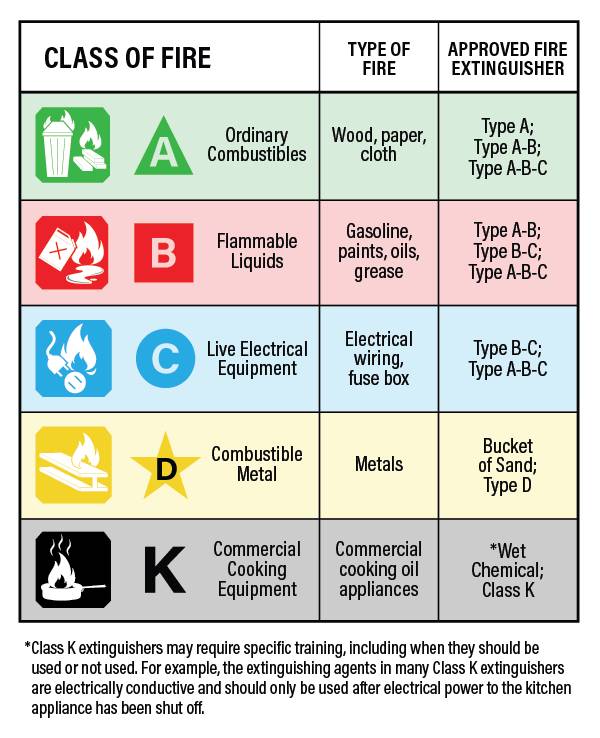
Poisoning
A poison is any substance that causes an alteration in the client’s health, such as injury or death, when inhaled, injected, ingested, or absorbed by the body.
Antidotes and treatments are available for some but not all types of poisonings.
Causes of poisonings are:
• Inadequate supervision of children
• Ingestion of household plants
• Improper storage of toxic substances
• Insect or snake bites
• Accidental ingestion of a toxic substance or medication overdose- due to failing eyesight/ impaired memory.
• Carbon monoxide poisoning
Carbon monoxide poisoning: Carbon monoxide (CO) is an odorless, colorless, tasteless gas that is very toxic. Exposure to CO can cause symptoms that include headaches, dizziness, weakness, nausea, vomiting, or loss of muscle control. Prolonged exposure to CO can lead to unconsciousness, brain damage, or death.
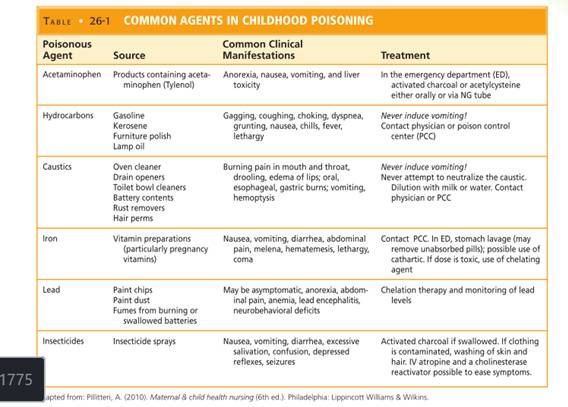
Preventing poisoning:
- Lock potentially toxic agents, in a cupboard, or attach special plastic hooks to the insides of cabinet doors to keep them securely closed.
- Do not let children watch you open the latches.
- Store medications in child-resistant containers.
- Do not take medications in front of children.
- Avoid storing toxic liquids or solids in food containers.
- Do not remove container labels or reuse empty containers to store different substances.
- Do not rely on cooking to destroy toxic chemicals in plants.
- Teach children never to eat any part of an unknown plant.
- Do not keep poisonous plants in the home, and avoid planting poisonous plants in the yar
- Place poison warning stickers designed for children on containers with toxic substances.
- Read and follow label directions on all products before using them.
- Keep syrup of ipecac on hand at all times.
- Display the phone number of the poison control center near or on all telephones in the home so that it is available to babysitters, family, and friends.
Interventions in accidental poisoning:
1. Assess for signs or symptoms of ingestion of harmful substance:
- nausea, vomiting
- foaming at the mouth, drooling
- difficulty breathing
- sweating, and lethargy.
2. Terminate exposure to the poison by having the person empty his or her mouth of pills, plant parts, or other material.
3. If poisoning is caused by skin or eye contact, irrigate the skin or eye with copious amounts of cool tap water for 15 to 20 minutes.
4. In the case of an inhalation exposure, safely remove the victim from the potentially dangerous environment.
5. Identify the type and amount of substance ingested to help determine the correct type and amount of antidote needed.
6. Call the local poison control center or the national toll-free poison control center number (1-800-222-1222) before attempting any intervention.
7. If the victim has collapsed or stopped breathing, call 911 for emergency transportation to the hospital. Initiate CPR if indicated until emergency personnel arrive.
8. Position the victim with head turned to the side to reduce risk for aspiration.
9. Never induce vomiting if the victim has ingested the following poisonous substances: lye, household cleaners, hair care products, grease or petroleum products, furniture polish, paint thinner, or kerosene.
10. Never induce vomiting in an unconscious or convulsing victim because vomiting increases risk for aspiration.
Electrical hazards
All electric equipment must be properly grounded. Grounding prongs offer a path of least resistance to stray electric currents.
The electric plug of grounded equipment has three prongs. The two short prongs transmit the power to the equipment. The third, longer prong is the grounding device, which carries short circuits or stray electric current.
Faulty equipment such as equipment with a frayed cord presents a danger of electric shock or may start a fire.
Actions to reduce electrical hazards:
- Check cords for fraying or other signs of damage before using an appliance. Do not use it if damage is apparent.
- Avoid overloading outlets and fuse boxes with too many appliances.
- Use only grounded outlets and plugs.
- Always pull a plug from the wall outlet by firmly grasping the plug and pulling it straight out. Pulling a plug by its cord can damage the cord and plug unit.
- Never use electric appliances near sinks, bathtubs, showers, or other wet areas, because water readily conducts electricity.
- Keep electric cords and appliances out of the reach of young children.
- Place protective covers over wall outlets to protect young children.
- Have all non-insulated wiring in the home altered to meet safety standards.
- Carefully read instructions before operating electric equipment. Clients who do not understand how to operate the equipment should seek advice.
- Always disconnect appliances before cleaning or repairing them.
- Unplug any appliance that has given a tingling sensation or shock and have an electrician evaluate it for stray current.
- Keep electric cords coiled or taped to the ground away from areas of traffic to prevent others from damaging the cords or tripping over them.
If a client receives an electrical shock:
- Turn off or remove the electric source before touching the client.
- The client’s pulse should be checked.
- If the client has no pulse, CPR should be initiated.
- If the client has a pulse, the nurse should assess vital signs, mental status, and skin integrity for burns.
- A prescribing practitioner should be notified of the event.
- The nurse should note points of entry and exit of electrical current to assess for potential complications.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Safety
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


