Please set your exam date
Pain assessment and management in children
Study Questions
Practice Exercise 1
A 7-year-old child who recently had an appendectomy is experiencing pain. This type of pain is best described as:
Explanation
Acute pain is a sudden onset pain related to tissue injury, surgery, or illness, typically lasting less than 3 months and resolving as healing occurs. In children, it can cause increased heart rate, rapid breathing, anxiety, and reluctance to move. Appendectomy pain in the immediate postoperative period fits this description.
Rationale for correct answer:
C. Acute pain: The child’s pain is directly related to a recent surgical procedure and is expected to improve as recovery progresses. This type of pain responds well to analgesics and nonpharmacologic comfort measures.
Rationale for incorrect answers:
A. Neuropathic pain is caused by nerve injury or dysfunction, often described as burning, tingling, or shooting; not typical after a straightforward appendectomy.
B. Chronic pain persists beyond normal healing time (usually >3 months) and is not expected in a normal postoperative course.
D. Mixed-pain involves both nociceptive and neuropathic components; may be seen in complex injuries or conditions but is not expected after a routine appendectomy in a healthy child.
Take home points
- Acute pain follows surgery, injury, or illness and usually resolves with healing.
- Effective pain management in children includes age-appropriate pain scales, timely medication, and comfort measures.
- Prompt treatment of acute pain improves healing, reduces anxiety, and prevents progression to chronic pain.
Which of the following is a primary characteristic of chronic pain?
Explanation
Chronic pain is pain that continues beyond the expected period of healing, usually longer than 3 months. It may persist despite treatment and may not always have an identifiable cause. Chronic pain can affect physical, emotional, and social functioning, and often requires a multidisciplinary management approach.
Rationale for correct answer:
C. Pain persisting for more than three months is the standard clinical definition used to distinguish chronic pain from acute pain. Chronic pain can occur with or without ongoing tissue injury and often requires long-term strategies for relief and coping.
Rationale for incorrect answers:
A. Sudden onset and short-lived pain describes acute pain, not chronic pain.
B. Pain that serves as a warning of tissue damage is a key function of acute pain, whereas chronic pain often persists after tissue healing.
D. Chronic pain may occur without an obvious injury or after the original injury has healed such as fibromyalgia, and phantom limb pain.
Take home points
- Chronic pain lasts >3 months or beyond normal healing time.
- May be continuous or intermittent and not always linked to visible injury.
- Management focuses on function improvement, coping strategies, and quality of life, not just pain elimination.
A child with Complex Regional Pain Syndrome (CRPS) is likely experiencing which type of pain?
Explanation
Complex Regional Pain Syndrome (CRPS) is a chronic pain condition that usually develops after an injury or surgery but is disproportionate to the original event. CRPS often presents with burning pain, hypersensitivity, swelling, temperature changes, and skin color changes in the affected limb.
Rationale for correct answer:
B. CRPS pain results from abnormal nerve signaling rather than ongoing tissue damage making it a neuropathic pain. This explains the intense, burning, or shooting sensations and the sensory changes characteristic of the condition.
Rationale for incorrect answers:
A. Musculoskeletal pain originates from muscles, bones, or joints; CRPS involves nerve dysfunction, not just musculoskeletal structures.
C. CRPS is a chronic, long-lasting condition, not a short-term response to injury.
D. While some patients with CRPS may have overlapping nociceptive pain from the initial injury, the defining feature is neuropathic.
Take home points
- CRPS is a neuropathic pain disorder often triggered by minor trauma or surgery.
- Symptoms include burning pain, hypersensitivity, and autonomic changes (color, temperature, sweating).
- Early recognition and intervention improve outcomes and may prevent permanent disability.
A nurse is caring for a child with sickle cell disease. This is an example of:
Explanation
Pain in children is a complex, subjective experience that includes both physical sensations and emotional responses. It can be caused by illness, injury, medical procedures, or chronic conditions, and children may express it differently depending on their age, development, and communication abilities.
Rationale for correct answer:
C. Sickle cell disease involves both chronic pain, from ongoing vaso-occlusive damage to tissues, and acute pain episodes (pain crises from sudden vaso-occlusion and ischemia). A vaso-occlusive crisis combines features of both types, making it a classic example of mixed-pain in pediatrics.
Rationale for incorrect answers:
A. Pain crises have an acute component, but sickle cell patients also live with baseline chronic pain between crises.
B. They do have chronic pain from repeated tissue injury, but the acute crisis pain is a separate, superimposed episode.
D. Sickle cell pain is not surgery-related, so post-operative pain does not apply.
Take home points
- Acute pain: Sudden onset, short duration, protective warning sign (e.g., postoperative, injury).
- Chronic pain: Lasts >3 months, persists beyond normal healing (e.g., juvenile arthritis).
- Mixed-pain: Coexistence of acute and chronic elements (e.g., sickle cell disease, cancer pain).
Practice Exercise 2
A nurse is preparing to administer an intramuscular injection to a 1-year-old. Which biobehavioral intervention would be most appropriate to reduce the pain?
Explanation
Biobehavioral interventions are powerful, evidence-based strategies that help reduce pain in children by addressing the biological, psychological, and social dimensions of pain.
Rationale for correct answer:
C. Sucrose given orally a few minutes before an injection has been shown to reduce pain behaviors in infants and young toddlers. It stimulates sweet taste receptors, triggering endogenous opioid release, which has a calming and analgesic effect. It is simple, quick, and safe when used appropriately.
Rationale for incorrect answers:
A. A 1-year-old lacks the cognitive ability to understand a detailed explanation; verbal preparation is more effective in older children.
B. Candy does not have the same analgesic effect as sucrose solution, and choking hazards make it inappropriate for a 1-year-old.
D. Guided imagery requires cognitive and imaginative skills that a 1-year-old has not yet developed.
Take-home points
- Oral sucrose is an evidence-based analgesic for infants during short painful procedures.
- Combine sucrose with comfort positioning and parental presence for best results.
- Cognitive distraction techniques are better suited for older children.
The gold standard for pain assessment in a child who can communicate is:
Explanation
Pain assessment in children is the process of evaluating the presence, intensity, and impact of pain using age-appropriate tools and observations.
Rationale for correct answer:
B. The child’s self-report is considered the gold standard for pain assessment if the child is developmentally able to communicate. Pain is a subjective experience, only the person feeling it can truly describe its intensity, location, and nature. Validated self-report tools for children include the Faces Pain Scale – Revised (FPS-R), the Oucher scale, and numeric rating scales (for older children).
Rationale for incorrect answers:
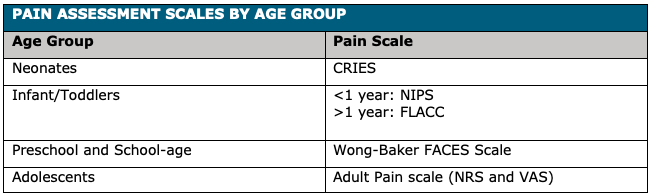
A. The FLACC (Face, Legs, Activity, Cry, Consolability) scale is a behavioral scale is used for children unable to self-report, such as infants or non-verbal children.
C. The parent's report is helpful for gaining insight, especially in non-verbal children, but it’s secondary to the child’s own report when possible.
D. The nurse's observation is useful as part of a comprehensive assessment, but it’s not as accurate as self-report for children who can communicate.
Take-home points
- Always use self-report first for children who can communicate; adapt the tool to the child’s developmental level.
- Behavioral and physiological measures are backup options when self-report isn’t possible.
- Accurate pain assessment drives appropriate management and improves trust with the child and family.
A 9-year-old child is receiving morphine for postoperative pain via a PCA pump. The most critical side effect to monitor for is:
Explanation
Morphine is a powerful opioid analgesic used to treat moderate to severe pain, especially when other pain relief methods are ineffective or not tolerated. It works by binding to mu-opioid receptors in the brain and spinal cord, altering the perception and emotional response to pain
Rationale for correct answer:
D. Respiratory depression is the most critical and potentially life-threatening side effect of opioid use, including morphine administered via PCA (patient-controlled analgesia). Opioids depress the brain’s respiratory center, which can reduce respiratory rate and tidal volume, leading to hypoxia.
Rationale for incorrect answers:
A. Nausea and vomiting are common opioid side effects but not immediately life-threatening; managed with antiemetics.
B. Constipation is a predictable long-term effect of opioids, preventable with stool softeners and laxatives; not an acute emergency.
C. Itching usually occurs due to histamine release from opioids; uncomfortable but not critical.
Take home points
- In pediatric opioid therapy, airway and breathing always take priority.
- Continuous monitoring for respiratory depression is mandatory with PCA use, especially in opioid-naïve children.
- Educate caregivers and staff on early warning signs: slowed breathing, decreased responsiveness, and oxygen desaturation.
- Have naloxone readily available as an opioid antagonist in case of severe respiratory depression.
Which of the following is an example of a coanalgesic drug?
Explanation
Analgesics are medications designed to relieve pain without causing loss of consciousness. They work by targeting different parts of the pain pathway, either at the site of injury, in the spinal cord, or in the brain.
Rationale for correct answer:
C. Coanalgesic drugs (also called adjuvant analgesics) are medications not primarily designed for pain relief but have pain-modifying properties, especially for neuropathic pain. Certain antidepressants, such as tricyclic antidepressants (e.g., amitriptyline) and SNRIs (e.g., duloxetine), can modulate pain pathways by enhancing serotonin and norepinephrine activity in the CNS.
Rationale for incorrect answers:
A. Ibuprofen is a nonsteroidal anti-inflammatory drug (NSAID), classified as a non-opioid analgesic, not a coanalgesic.
B. Morphine is an opioid analgesic, directly used for pain relief, not an adjuvant.
D. Acetaminophen is a non-opioid analgesic/antipyretic; not considered a coanalgesic.
Take home points
- Coanalgesics are especially useful for neuropathic pain and pain unresponsive to standard analgesics.
- Examples include antidepressants, anticonvulsants, corticosteroids, and muscle relaxants.
- Pain management often requires a multimodal approach, combining opioids, non-opioids, and coanalgesics for optimal effect and minimal side effects.
Comprehensive Questions
When caring for their infant, a parent asks you, “Is Emily in a lot of pain? How would you know since she can’t really tell you?” The best answer to this question is:
Explanation
Infants do feel pain, and their nervous systems are capable of transmitting pain signals from birth. Because they cannot verbalize their discomfort, healthcare providers use standardized infant pain assessment tools (such as the FLACC scale or Neonatal Infant Pain Scale) to interpret behavioral and physiological cues.
Rationale for correct answer:
D. “Although we try to give her medicine before she feels pain, we watch her very closely and use different techniques to help relieve the pain.” This is correct because pain prevention (preemptive analgesia) is a best practice, but infants still require ongoing monitoring. Combining medication with nonpharmacologic comfort measures (swaddling, skin-to-skin, gentle rocking) improves pain control and emotional security.
Rationale for incorrect answers:
A. “Infants don’t feel pain as we do because their pain receptors are not fully developed yet.” Infants’ pain receptors and pathways are functional at birth. In fact, preterm and newborn infants may have increased pain sensitivity because inhibitory pain pathways are immature.
B. “The nurses give pain medication before she really feels the pain.” While preemptive analgesia is ideal for predictable procedures, not all pain can be prevented, and ongoing assessment is still required.
C. “We assess her pain using an infant pain assessment tool and give the medicine as needed.” While true, it does not highlight the proactive approach of giving pain relief before pain escalates and using multiple comfort techniques.
Take home points
- Infants do feel pain, and untreated pain can have lasting developmental effects.
- Use validated infant pain assessment tools to guide treatment.
- Combine pharmacologic and nonpharmacologic measures for optimal comfort.
- Ongoing monitoring is crucial, even when preemptive pain control is in place.
Which of the following pain scales is most suitable for children with cognitive impairment?
Explanation
Pain assessment in infants relies on behavioral and physiologic indicators interpreted through validated tools. These tools help guide timely interventions, especially in nonverbal patients, ensuring pain is recognized and managed appropriately.
Rationale for correct answer:
C. NCCPC (Parent and health caregiver questionnaire assessing acute and chronic pain): Designed for nonverbal children, including those with cognitive impairments, using caregiver observations for both acute and chronic pain. Relies on input from parents and caregivers who know the child’s usual behaviors.
Rationale for incorrect answers:
A. CRIES (Crying, Requiring increased oxygen, Inability to console, Expression, and Sleeplessness): Used for neonates (0–6 months), especially postoperative, assessing pain through five observable indicators.
B. FLACC (child’s face, legs, activity, cry, and consolability): Suitable for infants and young children (2 months–7 years) who cannot self-report. Scores each category 0–2 for a total of 0–10.
D. NPASS (Neonatal pain, agitation, and sedation scale for infants from 3 to 6 months) This is validated for preterm and term neonates up to 100 days old. It evaluates both pain/agitation and sedation levels.
E. Numerical pain scale
Take home points
- CRIES is ideal for postoperative neonates.
- FLACC works well for infants through early childhood when self-report isn’t possible.
- NCCPC is useful for nonverbal or cognitively impaired children.
- NPASS is for neonates, including preterm infants, not older infants.
As the nurse is getting Nathan ready for surgery, his doctor asked you to explain preemptive analgesic to Nathan’s mother. Which response leads you to believe his mother needs more teaching?
Explanation
Preemptive analgesia is the administration of pain medication before the onset of pain, especially before surgery or procedures, to minimize pain intensity afterward. It aims to reduce central sensitization, improve comfort, and possibly shorten recovery time. However, it does not guarantee the patient will “feel nothing”, some discomfort may still occur, though it is usually less intense.
Rationale for correct answer:
B. “This medication will control Nathan’s pain so he doesn’t feel anything.” While preemptive analgesia can significantly reduce pain, it may not eliminate it completely. Pain perception varies, and additional postoperative pain management is often required.
Rationale for incorrect answers:
A. “I understand that preemptive analgesia is giving Nathan pain medication before he has pain and could be given before surgery.” This reflects the definition and timing of preemptive analgesia.
C. “Giving this medicine early may help prevent complications after surgery.” Effective early pain control can reduce complications such as shallow breathing, immobility, or delayed healing caused by uncontrolled pain.
D. “By controlling Nathan’s pain, he will be more comfortable and may be able to go home sooner.” Improved comfort can facilitate earlier mobilization and discharge.
Take home points
- Preemptive analgesia is given before pain starts, often before surgery.
- It aims to reduce pain severity and improve recovery outcomes.
- It does not guarantee complete absence of pain.
- Combining preemptive analgesia with ongoing multimodal pain management yields the best results.
The nurse is giving a 5-year-old child a vaccine injection. The child cries loudly during the procedure. Which of the following interventions would be appropriate for the nurse to perform after the injection?
Explanation
After a painful or stressful procedure, emotional support and positive reinforcement are essential for young children. Providing comfort and a small reward, such as a sticker, helps reduce fear and build resilience for future healthcare experiences.
Rationale for correct answer:
D. Comforting the child and offering a sticker provides positive reinforcement and acknowledges the child’s bravery. This developmentally appropriate response helps the child associate medical procedures with support and care, rather than fear and punishment.
Rationale for incorrect answers:
A. Telling a child that "big children are quiet" is shaming and dismissive. It implies that the child did something wrong by crying, which is a normal emotional reaction at this age.
B. Explaining why vaccines are given may be more appropriate before the procedure, but afterward, the child is likely focused on the pain or distress, not the rationale. At 5 years old, the child may not fully comprehend the explanation either.
C. Informing the child that the provider ordered the vaccine may seem like an attempt to deflect responsibility and does nothing to comfort or validate the child's feelings.
Take home points
- Preschool and early school-age children benefit from comfort, reassurance, and tangible rewards after stressful events.
- Crying is a normal, age-appropriate reaction to pain; it should not be shamed or discouraged.
- Focus post-procedure care on emotional recovery, not explanation or discipline.
- Positive reinforcement builds cooperation and trust in medical settings, making future encounters easier for both the child and the caregiver.
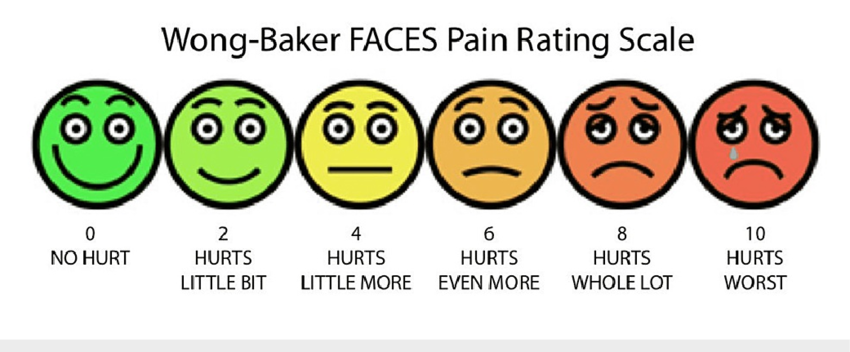
The Wong-Baker Faces Pain Rating Scale is an appropriate pain assessment tool for a child of what age?
Explanation
The Wong-Baker Faces Pain Rating Scale is a self-report tool that uses facial expressions paired with numerical ratings to help children describe their pain intensity. It is most reliable in school-age children and adolescents.
Rationale for correct answer:
3. A 14-year-old child has the cognitive ability to self-report pain using a scale. The Wong-Baker Faces Scale is simple, widely recognized, and effective for adolescents.
Rationale for incorrect answers:
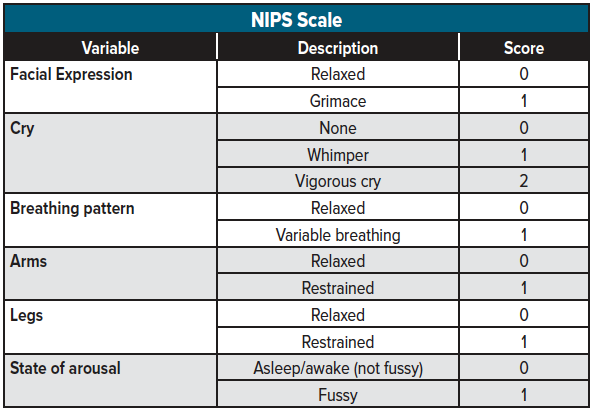
1. An infant cannot self-report pain. Behavioral and physiologic assessment tools like FLACC or CRIES are more appropriate.
2. While some 3-year-olds can use the scale, many may not yet have the cognitive maturity to understand and accurately use it. The scale is more reliable in slightly older children.
4. A preverbal child with cognitive impairment cannot self-report; observational tools like FLACC or the Non-Communicating Children’s Pain Checklist are better suited.
Take home points
- Wong-Baker Faces Scale is a self-report pain tool, best for children who can understand symbolic representation.
- Infants and nonverbal children require behavioral/physiologic scales.
- Choose pain tools based on age, developmental stage, and communication ability.
Exams on Pain assessment and management in children
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
- Differentiate between acute, chronic, and mixed-pain conditions in pediatric patients.
- Identify appropriate observational pain tools for infants and non-verbal children.
- Select age-appropriate self-report pain rating scales for verbal children.
- Assess the unique challenges and strategies for measuring pain in special populations or those with cognitive impairments.
- Evaluate the role of biobehavioral interventions in a holistic pain management plan.
- Compare the indications and side effects of non-opioids, opioids, and coanalgesic medications.
- Analyze the benefits and risks of various delivery methods, including PCA and epidural analgesia.
- Determine the critical monitoring parameters for preventing and managing analgesic-related side effects.
Introduction
- Health supervision, also known as well-child care, is a proactive, preventative approach to healthcare that focuses on the ongoing needs of children from birth through adolescence.
- Unlike sick visits, which address acute illnesses, well-child visits are designed to promote optimal physical, cognitive, and psychosocial development.
- These regular visits are a cornerstone of modern pediatrics, aiming to keep children healthy rather than just treating them when they are sick.
- The primary objective of health supervision is to ensure a child's optimal physical, mental, and developmental well-being. The main goals include:
- Preventing Illness and Injury: This is the most crucial goal. Well-child visits provide an opportunity to administer necessary immunizations and offer guidance on injury prevention (e.g., car seat safety, poison control).
- Monitoring Growth and Development: The healthcare provider tracks a child's growth using charts for weight, height, and head circumference. They also assess developmental milestones, such as language skills, motor skills, and cognitive abilities.
- Early Detection and Screening: These visits are essential for identifying health problems early, before they become serious. Screenings may include tests for hearing, vision, anemia, lead poisoning, and developmental disorders.
- Health Promotion and Education: Healthcare providers provide anticipatory guidance to parents and caregivers. This includes advice on nutrition, sleep habits, behavior, and what to expect as the child grows.
- Building a Relationship: Regular visits help establish a trusting relationship between the child, the family, and the healthcare provider. This creates a safe space for parents to ask questions and discuss concerns.
Types of pain
3.1. Acute Pain Conditions
Acute pain is sudden in onset and typically short-lived, with a clear cause. It serves as a warning signal of actual or potential tissue damage.
- Needlestick Pain: A common cause of acute pain and anxiety in children, often associated with immunizations or blood draws. The pain is sharp and localized, and the associated fear can be a significant barrier to care.
- Postoperative Pain: Pain that occurs after a surgical procedure. It is a predictable and often severe type of acute pain, which, if not managed effectively, can delay recovery, prolong hospital stays, and increase the risk of developing chronic pain.
- Nursing Insight: Proactive pain management for acute pain, especially post-op, is crucial. Administering analgesics on a schedule prevents the pain from escalating, making it easier to manage.
3.2. Chronic Pain Conditions
Chronic pain persists for more than three months or beyond the expected period of healing. It can significantly impact a child's quality of life, school attendance, and emotional health.
- Headaches: Common in children and can be classified as migraines or tension-type headaches. Assessment includes identifying triggers, frequency, and severity.
- Abdominal Pain: Often functional in nature, meaning there is no underlying organic cause, though it requires thorough medical evaluation to rule out conditions like inflammatory bowel disease.
- Musculoskeletal Pain: Includes conditions like juvenile idiopathic arthritis (JIA) or growing pains. The pain can affect mobility and daily activities.
- Neuropathic Pain Syndromes: Result from damage to the nervous system. The pain is often described as burning, shooting, or tingling. Conditions include complex regional pain syndrome (CRPS).
- Nursing Insight: Chronic pain management requires a holistic, multidisciplinary approach. Nursing care extends beyond medication to include emotional support, education on coping mechanisms, and collaboration with physical therapists and psychologists.
3.3. Mixed-Pain Conditions
Mixed-pain conditions involve elements of both acute and chronic pain. The pain is often severe, persistent, and challenging to manage.
- Burn Pain: This is a combination of acute pain from the initial injury, ongoing pain from dressing changes and debridement, and chronic neuropathic pain as the skin heals.
- Cancer Pain: Can be acute (e.g., from surgery or a procedure) or chronic (e.g., from tumor growth or treatments like chemotherapy and radiation).
- Sickle Cell Pain: Characterized by episodic, severe, acute pain crises (vaso-occlusive crises) that can also lead to chronic pain over time.
Measuring pain in children
5.1. Observational Pain Measures
For infants and nonverbal children, nurses must rely on observational pain measures. These scales assess a child's behavioral and physiological responses to pain.
- FLACC Scale: Used for children from 2 months to 7 years. It stands for Face, Legs, Activity, Cry, and Consolability. The nurse rates each category from 0-2, with a total score from 0-10.
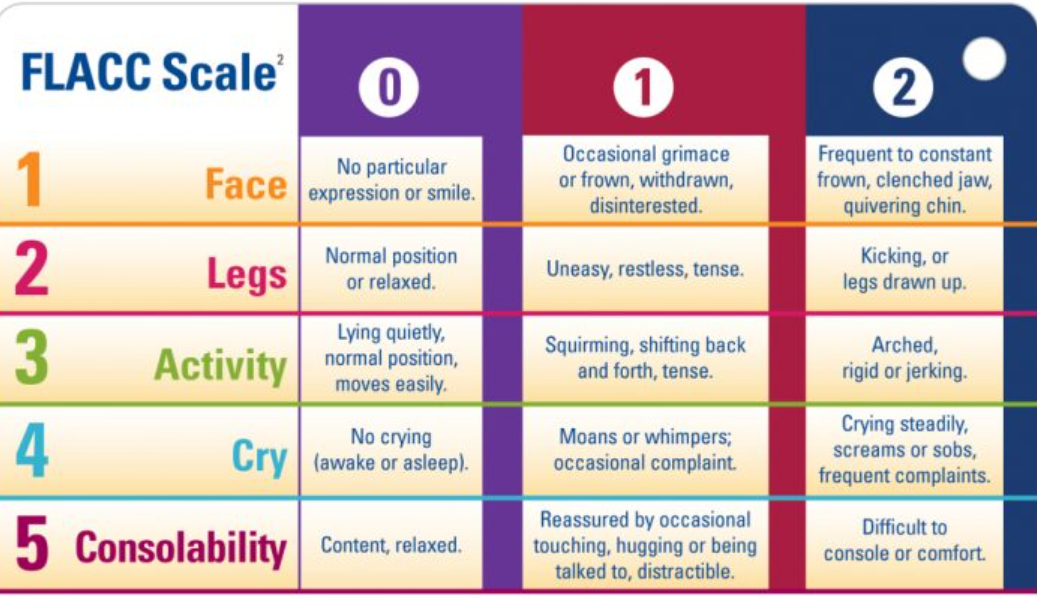
- CRIES Scale: Used for neonates. It assesses Crying, Requires O2, Increased vital signs, Expression, and Sleeplessness.
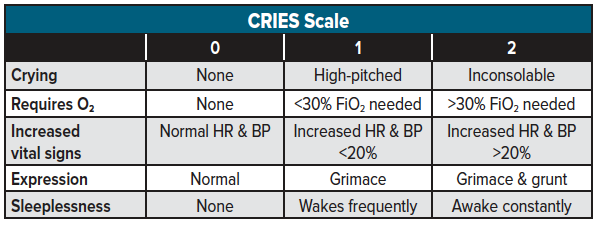
- NIPS Scale: Used for infants up to 1 year. It assesses facial expression, crying, breathing patterns, arm and leg movements, and state of arousal.
Nursing Insight: Consistent use of a single, validated observational tool by all healthcare providers ensures reliable and accurate pain assessment.
5.2. Special Populations
- Preterm Infants: Use specialized scales like the Premature Infant Pain Profile (PIPP), which considers gestational age and behavioral states.
- Cognitively Impaired Children: May not be able to use self-report scales. Nurses should use observational tools and rely on caregivers who know the child's typical behaviors. The Non-Communicating Children's Pain Checklist (NCCPC) is a useful tool.
- Children Postanesthesia: Nurses must monitor for signs of pain as the child emerges from anesthesia and is unable to self-report.
- Children in the Pediatric Intensive Care Unit (PICU): Pain assessment can be complicated by sedation, mechanical ventilation, and multiple procedures. Use tools like the Critical-Care Pain Observation Tool (CPOT).
5.3. Self-Report Pain Rating Scales
For children over 3-4 years old, self-report is the gold standard for pain assessment.
- Wong-Baker Faces Pain Rating Scale: Consists of six faces ranging from a smiling face for "no pain" to a crying face for "worst pain." It is suitable for children as young as 3.
- Faces Pain Scale-Revised (FPS-R): A similar scale with seven faces, but without the smile or tears. It is anchored with a 0-10 numerical scale and is considered more neutral.
- Word-Graphic Rating Scale: Uses a series of descriptive words (e.g., "no pain," "a little pain," "worst pain") for children who can read.
- The NCCPC (Non-Communicating Children's Pain Checklist) is a behavioral pain scale used by parents and caregivers to assess acute and chronic pain in children who are unable to express their pain verbally. It is particularly useful for children with cognitive impairments, developmental disabilities, or severe neurological conditions.
- Nursing Insight: Take the time to explain the scale to the child, ensuring they understand how to use it correctly to represent their pain level.
5.4. Multidimensional Measures
These scales assess pain from multiple perspectives, including location, quality, intensity, and impact on a child's life.
- Pediatric Pain Questionnaire (PPQ): Assesses the child's and parent's perception of the pain.
- Functional Disability Inventory (FDI): Measures how pain impacts a child's daily functioning.
- Pediatric Quality of Life Inventory (PedsQL): Assesses the child's health-related quality of life.
- Pediatric Migraine Disability Assessment Scale (PedMIDAS): Specifically for children with migraines, it measures the impact of headaches on school, home, and social activities.
Prevention and treatment of pain in children
6.1. Biobehavioral Interventions
These are non-pharmacologic strategies that focus on the child's psychological and behavioral responses to pain.
- Distraction: Using toys, games, bubbles, or music to divert a child's attention from a painful procedure.
- Relaxation Techniques: Deep breathing exercises, guided imagery, or muscle relaxation.
- Massage and Positioning: Gentle touch can reduce muscle tension and provide comfort. Proper positioning in infants can reduce procedural pain.
- Sweet-Tasting Solutions: For infants, a few drops of sucrose solution on the tongue before a procedure (e.g., heel stick) can provide a calming, analgesic effect.
6.2. Pharmacologic Management of Pain
- Pharmacologic management follows the World Health Organization (WHO) pain ladder, starting with non-opioids and escalating as needed.
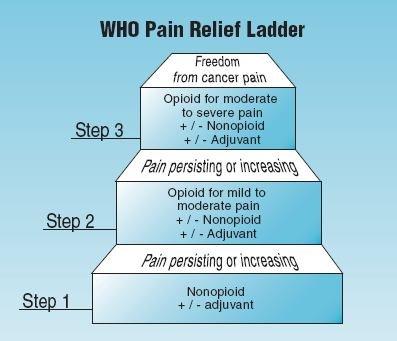
Non-opioids:
- Acetaminophen: A first-line agent for mild-to-moderate pain. It is an effective antipyretic and analgesic.
- Nonsteroidal Anti-inflammatory Drugs (NSAIDs): (e.g., ibuprofen, naproxen). Useful for inflammatory pain.
Opioids:
- Used for moderate-to-severe pain. Morphine is the gold standard. Fentanyl is often used for short procedures. Hydromorphone is another potent option.
Coanalgesic Drugs:
- Medications used to enhance the effect of primary analgesics or treat specific types of pain. Examples include anxiolytics, antidepressants, and anti-seizure medications (for neuropathic pain).
Choosing the Pain Medication Dose:
- Doses are based on the child's weight and are often calculated in milligrams per kilogram (mg/kg).
Choosing the Timing of Analgesic:
- Medications should be given on a scheduled basis (around the clock) for continuous pain, rather than waiting for the child to report pain.
Choosing the Method of Administration:
- Oral: Preferred route when possible.
- Intravenous (IV): Used for moderate-to-severe pain or when the oral route is not feasible.
- Intramuscular (IM): Avoided due to pain and unreliable absorption.
Patient-Controlled Analgesia (PCA):
- Allows the child to self-administer small, preset doses of pain medication (usually an opioid) by pressing a button. This is suitable for children as young as 5-6 years old who understand the concept.
Epidural Analgesia:
- A catheter is placed in the epidural space to deliver a continuous infusion of local anesthetics and/or opioids. Provides excellent regional pain control, especially for lower body and abdominal surgeries.
Transmucosal and Transdermal Analgesia:
- Transmucosal: Fentanyl lollipops or lozenges are used for acute procedural pain.
- Transdermal: Fentanyl patches are used for chronic pain management. EMLA cream (a topical anesthetic) is applied to the skin before needlesticks to numb the area.
Monitoring Side Effects:
- For opioids, nurses must closely monitor for respiratory depression, sedation, constipation, nausea, and vomiting. Use of a sedation scale is essential.
Specific Strategies for Special Populations:
- Pain Prevention for Needlestick: Use EMLA cream, distraction, and sweet-tasting solutions.
- Care During Painful and Invasive Procedures: Provide procedural sedation, use comfort positioning, and involve child life specialists.
- Biobehavioral Interventions with Postsurgical Pain: Combine pharmacologic agents with distraction and relaxation to enhance pain relief and reduce anxiety.
- Pain Management in Obese and Overweight Children: Use ideal body weight for dosing certain medications (e.g., opioids) to prevent overdosing.
- Treatment of Chronic Pain: Requires a multidisciplinary approach involving pharmacologic, physical therapy, and psychological interventions.
- Pain with Pediatric Cancer: Often requires potent opioids and coanalgesics.
- Pain Prevention and Treatment for Children with Sickle Cell Disease: Involves both chronic pain management and acute crisis management with hydration, warmth, and opioids.
- Pain Treatment During End-of-Life Care: The focus shifts to providing comfort and relieving suffering, often with higher doses of opioids.
Nursing Insight: Always verify medication dosages, especially weight-based calculations, with another nurse. Monitor for side effects and be prepared to intervene, particularly for respiratory depression with opioids.
Summary
- Effective pediatric pain management is a critical component of compassionate healthcare, requiring a nuanced understanding of how children experience and communicate distress.
- Because children vary significantly in their developmental stages and verbal abilities, nurses must move beyond a "one size fits all" approach.
- The clinical management of pediatric pain begins with identifying its nature, which is generally categorized into acute, chronic, or mixed conditions.
- Acute pain is typically sudden and time-limited, often resulting from injury or surgery, whereas chronic pain persists beyond the expected healing time, as seen in juvenile idiopathic arthritis.
- Mixed conditions, such as sickle cell anemia, often involve elements of both.
- To quantify this experience, providers utilize observational measures for infants and non-verbal children, focusing on facial expressions and body movements, while relying on self-report scales for older children who can articulate their discomfort.
- Special populations, including children with cognitive impairments, require tailored observational tools to ensure their distress is not overlooked.
- Comprehensive assessments may also include multidimensional measures that evaluate how pain impacts a child's sleep, mood, and daily activities.
- Treatment involves a synergy of biobehavioral interventions, such as distraction and relaxation, and a robust pharmacological framework. This framework ranges from non-opioids like acetaminophen to opioids for severe pain, supplemented by coanalgesic drugs to enhance relief.
- Safe administration is paramount and nurses must carefully choose the dose, timing, and route, whether via patient-controlled analgesia (PCA), epidural, or transdermal patches, while strictly monitoring for side effects.
- For special populations, these strategies are further refined to balance maximum efficacy with the highest safety standards, ensuring that every child receives individualized and humane care.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Pain assessment and management in children
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


