Please set your exam date
Pediatric Anatomy And Physiology Of The Respiratory Tract
Study Questions
Comprehensive Questions
A small degree of inflammation in a child's airway can lead to a disproportionately large increase in airway resistance compared to an adult. Which of the following is the primary reason for this?
Explanation
The primary reason a small degree of inflammation in a child’s airway causes a disproportionately large increase in airway resistance is the significantly narrower airway diameter. According to Poiseuille’s law, resistance to airflow is inversely proportional to the fourth power of the radius, meaning even a slight reduction in airway size greatly increases resistance.
Rationale for correct answer:
4. A child’s airway is much narrower than an adult’s, so swelling or mucus buildup reduces the radius substantially, causing a dramatic increase in resistance and work of breathing. This makes conditions like croup or bronchiolitis more severe in young children.
Rationale for incorrect answers:
1. While children do have higher metabolic rates and oxygen demands, this is not the main reason for the exaggerated effect of inflammation on airway resistance.
2. The cartilaginous and flexible trachea in infants contributes to collapsibility but does not explain the disproportionate rise in resistance from swelling.
3. Greater diaphragmatic reliance affects breathing mechanics but not the mathematical relationship between airway narrowing and resistance.
Take home points
- Airway resistance is highly sensitive to changes in radius, especially in children due to their small baseline diameters.
- Even minor airway swelling (e.g., 1 mm circumferential edema) can reduce the cross-sectional area by more than half in a child.
- Rapid recognition and management of pediatric airway inflammation is critical to prevent respiratory distress and hypoxia.
Which of the following are anatomical features that make infants and children more susceptible to respiratory distress and disease? Select all that apply
Explanation
Infants and children have multiple anatomical and physiological characteristics that increase their vulnerability to respiratory distress and disease. These features make them less able to compensate for airway compromise, infection, or increased oxygen demands.
Rationale for correct answers:
1. Fewer and smaller alveoli: At birth, the lungs have a limited number of alveoli, which grow in number and size over early childhood. This reduces the surface area for gas exchange, making them more prone to hypoxia during illness.
2. More compliant, cartilaginous chest wall: A softer chest wall can lead to retractions and inefficient ventilation when respiratory effort increases.
3. Higher, more anterior larynx: This anatomical position makes airway obstruction more likely and complicates airway management during resuscitation or intubation.
Rationale for incorrect answers:
4. Infants actually have a higher metabolic rate and oxygen consumption (about twice that of adults per kg body weight). This increases their vulnerability to hypoxia when breathing is compromised.
Take home points
- Pediatric airways are smaller, more collapsible, and more easily obstructed than adult airways.
- Immature lung development limits gas exchange capacity.
- High oxygen needs and low reserves mean children can deteriorate rapidly.
- Early recognition and intervention are essential to prevent severe hypoxia.
The primary function of the mucociliary clearance system is to:
Explanation
The mucociliary clearance system is a key innate defense mechanism of the respiratory tract, designed to trap and remove inhaled particles, pathogens, and debris before they reach the lower airways and alveoli.
Rationale for correct answer:
1. The respiratory epithelium contains mucus-producing goblet cells and ciliated cells. Mucus traps inhaled contaminants, and coordinated ciliary beating moves the mucus upward toward the pharynx, where it can be swallowed or expectorated. This process helps prevent infections and maintains airway cleanliness.
Rationale for incorrect answers:
2. While moisture in the alveoli facilitates gas exchange, this is not the main role of the mucociliary clearance system, alveolar moisture regulation is handled by surfactant and fluid balance mechanisms, not cilia and mucus.
3. Adaptive immunity involves lymphocytes and antigen-specific responses, which are separate from the mechanical clearance provided by the mucociliary system.
4. Angiotensin-converting enzyme (ACE) production occurs mainly in the pulmonary capillary endothelium, not as part of mucociliary clearance.
Take home points
- The mucociliary escalator is an essential first-line defense in the respiratory tract.
- Smoking, dehydration, and certain diseases (e.g., cystic fibrosis, primary ciliary dyskinesia) can impair this system, increasing infection risk.
- Efficient mucociliary function is especially important in children, whose immune systems are still developing.
Which statement about the defense mechanisms of the pediatric respiratory tract is correct?
Explanation
Lymphoid tissues such as the tonsils and adenoids form part of the Waldeyer’s ring and play a vital role in local immune surveillance of the upper respiratory tract, detecting and responding to inhaled or ingested pathogens.
Rationale for correct answer:
2. Lymphoid tissue like tonsils and adenoids provide local immune surveillance and defense. These structures contain immune cells (B and T lymphocytes) that detect antigens entering through the nose and mouth, initiating immune responses to help prevent infection spread.
Rationale for incorrect answers:
1. Alveolar macrophages are part of the innate immune system, not adaptive immunity. They engulf and destroy pathogens and debris but do not produce specific antibodies.
3. Infants’ cough and sneeze reflexes are actually less forceful and less coordinated than adults’, making clearance of secretions less efficient.
4. Secretory Immunoglobulin A (sIgA) is part of the active mucosal immune system, not passive immunity. Passive immunity is typically acquired via maternal antibodies (e.g., IgG via placenta, IgA via breast milk).
Take home points
- The pediatric respiratory tract uses multiple defense layers: mechanical (mucociliary clearance), reflexive (cough/sneeze), and immune (lymphoid tissue, sIgA, macrophages).
- Tonsils and adenoids are particularly important in early childhood but can also be a site of chronic infection or hypertrophy leading to obstruction.
What is the primary muscle of respiration in a newborn infant, and why is this significant?
Explanation
The diaphragm is the primary muscle of respiration in newborn infants. This is significant because their intercostal muscles are underdeveloped, and their rib cages are highly compliant, so they rely almost entirely on diaphragmatic movement for ventilation.
Rationale for correct answer:
3. In newborns, diaphragmatic contraction creates negative pressure to draw air into the lungs. If the diaphragm tires due to illness, hypoxia, or increased work of breathing, ventilation can rapidly deteriorate since accessory muscle use is limited.
Rationale for incorrect answers:
1. Sternocleidomastoid muscles are accessory muscles used during respiratory distress, not for quiet breathing in healthy infants.
2. Intercostal muscles are not fully developed in newborns and provide minimal contribution to chest wall stability or ventilation.
4. Abdominal muscles assist in forced exhalation and coughing but are not the primary drivers of quiet respiration.
Take home points
- Infants’ dependence on the diaphragm makes them vulnerable to respiratory fatigue in prolonged distress.
- Conditions that impair diaphragmatic function (e.g., sepsis, neuromuscular disorders, fatigue from tachypnea) can cause rapid deterioration.
- Early recognition of increased work of breathing is essential, as infants have limited reserves.
Which of these factors contributes to infants’ and children's increased risk for upper airway obstruction as compared with adults?
Explanation
Infants and young children have anatomical and physiological differences in their upper airways compared to adults that increase their risk for airway obstruction. These differences include a smaller and more flexible airway structure and narrower passages, which make them more vulnerable to swelling and obstruction.
Rationale for correct answer:
1. Underdeveloped cricoid cartilage and narrow nasal passages contribute significantly to the increased risk of upper airway obstruction in infants and children. The cricoid cartilage is the narrowest part of a child’s airway and is less rigid than in adults, making it more prone to collapse or swelling. Narrow nasal passages can become easily blocked by secretions or inflammation, further compromising airflow.
Rationale for incorrect answers:
2. Tonsils in children tend to be relatively large, not small, and can contribute to obstruction. The nasal passages are narrow, but this option misses the critical role of cricoid cartilage development.
3. The child’s larynx is funnel-shaped, not cylindrical, with the narrowest point at the cricoid cartilage. While sinuses develop over time, their underdevelopment doesn’t directly increase risk of upper airway obstruction.
4. Children actually have proportionally larger tongues relative to their oral cavity, which can contribute to obstruction, so “smaller tongue” is inaccurate.
Take home points
- Infants and children have a funnel-shaped, narrower airway with a less rigid cricoid cartilage, making them more susceptible to airway obstruction.
- Narrow nasal passages add to the risk by limiting airflow, especially during inflammation.
- Understanding these anatomical differences is critical when assessing respiratory distress in pediatric patients.
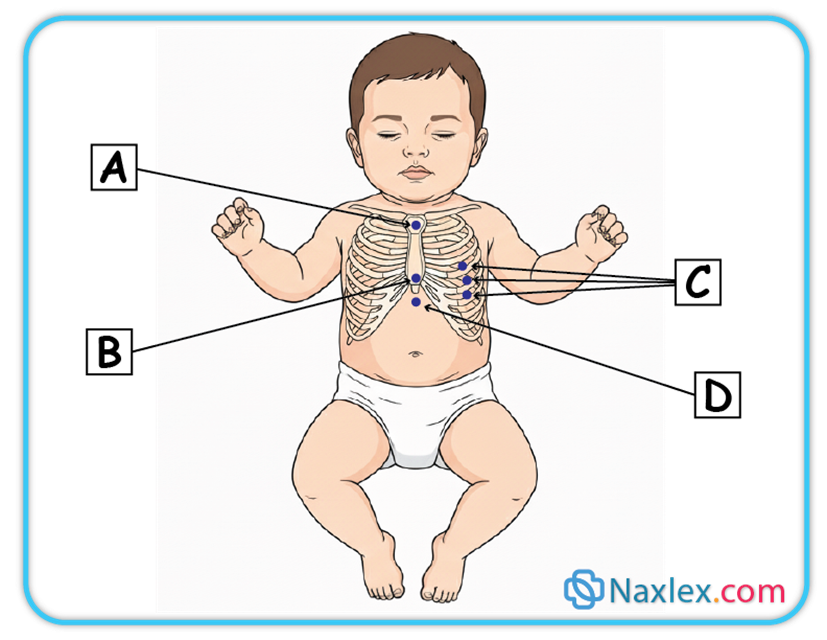
A nurse notes substernal retractions when assessing a child. At which area on the illustration did the nurse make this observation?
Explanation
Retractions are a clinical sign of increased work of breathing, often seen in infants and children. They occur when soft tissues around the chest wall are pulled inward during inspiration due to negative intrathoracic pressure, usually because the child is struggling to get enough air into the lungs.
Rationale for correct answer:
4. D: Substernal retractions are inward pulling of the soft tissue just beneath the sternum/xiphoid (subxiphoid/epigastric area). This reflects increased negative intrathoracic pressure and is common in moderate- severe respiratory distress.
Rationale for incorrect answers:
1. A: This represents suprasternal retractions, typically seen at the sternal notch with upper-airway obstruction (e.g., croup, laryngomalacia). Not “substernal.”
2. B: The xiphoid itself is the bony tip; retractions are named for the soft tissue below it (subxiphoid/substernal). At the xiphisternum isn’t the same as below the sternum.
3. C: Those are intercostal retractions along the lateral chest wall, not beneath the sternum.
Take home points
- Retractions are classified by location: suprasternal (above sternum), intercostal (between ribs), subcostal (below ribs), and substernal (below sternum).
- The more severe the respiratory distress, the more locations you may see retractions in simultaneously.
- Substernal retractions often point to lower airway or lung pathology (e.g., bronchiolitis, asthma, pneumonia).
Exams on Pediatric Anatomy And Physiology Of The Respiratory Tract
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
- Identify the key anatomical and physiological differences between the pediatric and adult respiratory systems.
- Describe the structure and functions of the pediatric respiratory tract.
- Explain the components of a comprehensive respiratory assessment in children.
- Detail the common diagnostic procedures used to evaluate pediatric respiratory function.
- List and describe the various defense mechanisms of the respiratory tract.
Introduction
- The respiratory system is vital for gas exchange, supplying O2 and removing CO2.
- In children, this system undergoes rapid development and exhibits significant anatomical and physiological differences from adults, making them uniquely vulnerable to respiratory illnesses.
- Understanding these differences is crucial for effective pediatric nursing care, as minor pathology can quickly lead to severe respiratory distress or failure.
- Respiratory disorders are the leading cause of hospitalization for children under five.
Variation In Pediatric Anatomy And Physiology
Children are not just "small adults." Their distinct anatomy and physiology predispose them to respiratory issues:
|
Feature |
Pediatric Variation |
Clinical Implication |
|
Airway Size |
Narrower diameter, especially the trachea and bronchi. |
Smaller decrease in radius causes a much greater increase in airway resistance (Poiseuille's Law: resistance is inversely proportional to r4). Quickly prone to obstruction from edema or mucus. Even mild swelling can compromise a baby's airway significantly. |
|
Larynx & Glottis |
Higher in the neck (C3-C4 vs. C5-C6 in adults); funnel-shaped (narrowest point is the cricoid ring in infants). |
This shape makes them prone to subglottic stenosis and makes intubation challenging. |
|
Tongue |
Proportionately larger than in adults. |
Easily occludes the pharynx when muscle tone is decreased (e.g., during sleep, sedation, or illness). |
|
Epiglottis |
Longer, floppier, and more U-shaped. |
Greater risk for acute epiglottitis and obstruction. |
|
Chest Wall |
More cartilaginous, compliant, and less rigid (ribs are horizontal). |
Offers poor leverage for the intercostal muscles; chest wall retractions are common during distress and are a sign of respiratory effort. |
|
Diaphragm |
Primary muscle of respiration; muscle fibers are less fatigue-resistant. |
Fatigue occurs faster, leading to respiratory failure. Monitor for signs of diaphragmatic fatigue (e.g., reduced grunting, paradoxical breathing). |
|
Metabolic Rate & O2 Consumption |
Higher (about 2x that of an adult per kg of body weight). |
They require more O2; any compromise leads to hypoxia faster. |
|
Alveoli |
Fewer in number and smaller at birth; increase rapidly up to age 8. |
Less surface area for gas exchange, reducing reserve capacity. |
|
Obligate Nose Breathers |
Infants (especially those under 4-6 months) |
Nasal congestion (e.g., from a common cold) is a major problem causing significant feeding and respiratory distress. Nasal suctioning (e.g., with a bulb syringe) and saline drops before feeds/sleep are vital interventions. |
Respiratory Tract Structure
The respiratory tract is divided into upper and lower sections:
A. Upper Respiratory Tract (Above the Larynx)
- Nose and Nasal Cavity: Filters, warms, and humidifies air. Contains ciliated mucosa.
- Pharynx: Passageway for air and food (nasopharynx, oropharynx, laryngopharynx).
- Tonsils and Adenoids: Lymphoid tissue; prominent in children, providing immune defense but can obstruct the airway when hypertrophied.
- Larynx (Voice Box): Contains the vocal cords; separates the upper and lower tract.
B. Lower Respiratory Tract (Below the Larynx)
- Trachea (Windpipe): Cartilaginous tube extending to the carina (bifurcation point). In children, it is shorter.
- Bronchi: The right main bronchus is shorter, wider, and straighter than the left, making it the more common site for aspiration of foreign bodies.
- Bronchioles: Small air passages lacking cartilage; rely on surrounding tissue for support. Prone to collapse and spasm (e.g., in asthma/bronchiolitis).
- Alveoli: Microscopic air sacs where gas exchange occurs.
Middle and Lower Airway
Functions Of The Respiratory Tract
- Gas Exchange: Primary function is the delivery of O2 to the blood and removal of CO2.
- Air Conditioning: Warming, filtering, and humidifying inhaled air.
- Acid-Base Balance: Regulates CO2 levels (CO2 is acidic). Faster/deeper breathing decreases CO2 (raising pH); slower/shallower breathing increases CO2 (lowering pH).
- Speech and Olfaction: Vocal cord vibration and sense of smell.
- Defense: Protection against pathogens and foreign matter.
Assessment Of Respiration Function
A rapid, systematic assessment is critical for identifying impending respiratory failure.
A. Physical Assessment Components
|
Observation |
Explanation |
Significance |
|
Respiration |
Rate (Tachypnea is often the first sign of distress). Depth (shallow or deep). Rhythm (regular or irregular). |
Count respirations for a full minute in infants/young children due to their irregular patterns. |
|
Retractions |
Visible sinking of the chest wall with inspiration due to the use of accessory muscles to overcome high airway resistance or poor lung compliance. Types: Suprasternal, Supraclavicular, Intercostal, Subcostal.
|
Mild: Intercostal only. Severe: Multiple areas, including supraclavicular/suprasternal. Indicates significant respiratory effort. |
|
Nasal Flaring |
Widening of the nostrils on inspiration. |
An attempt to decrease nasal airway resistance and increase the amount of air inhaled. A significant sign of distress, especially in infants. |
|
Head Bobbing |
Accessory muscle use where the head lifts with inspiration and falls with exhalation. |
Sign of severe distress and exhaustion, often seen in infants. |
|
Noisy Breathing |
Any sound other than clear breath sounds (e.g., stridor, grunting, wheezing). |
Localizes the problem (upper vs. lower airway). |
|
Stridor |
A high-pitched, harsh sound heard primarily on inspiration. |
Indicative of upper airway obstruction (e.g., Croup, foreign body, epiglottitis). Requires immediate attention. |
|
Grunting |
A short, low-pitched sound heard on expiration as the child attempts to keep the alveoli open. |
Sign of alveolar collapse/poor lung compliance (e.g., pneumonia, RDS). Self-preservation mechanism (like PEEP). |
|
Wheezing |
A high-pitched, musical whistling sound heard primarily on expiration. |
Indicative of lower airway obstruction/narrowing (e.g., Asthma, Bronchiolitis). Due to air attempting to pass through constricted bronchioles. |
|
Color Changes (Skin/Mucous Membranes) |
Pallor (early sign due to vasoconstriction). Cyanosis (late sign of O2 deprivation; central cyanosis in the lips/mucous membranes is an emergency). Cyanosis
|
Cyanosis is often a very late sign in children because they have a high Hgb concentration. Do not wait for cyanosis! |
|
Chest Pain |
Pain in the chest, often sharp and worse with deep breaths/cough (pleuritic). |
Can be related to coughing, infection (pleurisy), or inflammation. |
|
Clubbing |
Bulbous enlargement of the fingertips/toes. |
Sign of chronic hypoxia (e.g., Cystic Fibrosis, congenital heart disease). Takes time to develop. |
|
Cough |
Reflex to clear the airway. Characterized by quality (dry, wet/productive, "seal-like" in Croup) and timing. |
A sudden onset of a non-productive cough, especially in a toddler, suggests foreign body aspiration until proven otherwise. |
Diagnostic Procedures
A. Pulmonary Function Tests (PFTs)
- Purpose: Measure lung volumes, capacities, flow rates, and gas exchange.
- Methods: Spirometry is the most common, measuring Forced Vital Capacity (FVC) and Forced Expiratory Volume in 1 second (FEV1).
- Pediatric Consideration: Requires cooperation, so reliable PFTs are typically performed in children over age 6.
B. Radiology
- Chest X-ray (CXR): Provides an image of the lungs, heart, and bony structures. Used to diagnose pneumonia, atelectasis, pneumothorax, and view foreign bodies.
- CT/MRI: Used for more detailed imaging of masses, congenital anomalies, or complex infections.
C. Blood Gas Determination (Arterial Blood Gas - ABG or Venous Blood Gas - VBG)
- Purpose: Assesses the adequacy of O2, ventilation, and acid-base status (pH, HCO3).
- Interpretation: A rising PaCO2 (hypercapnia) indicates impending respiratory failure in a child who is tiring out.
D. Non-Invasive Monitoring
- Pulse Oximetry (SpO2): Measures the percentage of hemoglobin saturated with oxygen. The easiest and most common method to monitor O2 status. Ensure proper probe placement (fingers, toes, earlobe) for an accurate reading. Movement or poor circulation can cause false low readings.
- Capnography (End-Tidal CO2 - EtCO2): Measures the maximum CO2 concentration at the end of exhalation. Excellent for monitoring ventilation status and is a reliable, continuous indicator of breathing adequacy.
Capnography Interpretation
E. Other Diagnostic Procedures
- Sputum/Nasal Swabs: To identify pathogens (e.g., RSV, Influenza, Mycoplasma).
- Bronchoscopy: Direct visualization of the airway, often used for removing foreign bodies or for biopsies.
Defenses Of The Respiratory Tract
The respiratory tract has multiple lines of defense to protect the delicate gas exchange surfaces:
- Lymphoid Tissues (Tonsils & Adenoids): Located at the entrance of the pharynx, they trap inhaled pathogens and produce immune cells.
- Epiglottis: A flap of cartilage that covers the entrance to the trachea during swallowing, preventing aspiration of food/liquid into the lungs.
- Mucous Blanket: A sticky layer secreted by goblet cells that lines the airway, trapping dust, pollen, and microorganisms.
- Ciliary Action (Mucociliary Escalator): Tiny hair-like projections (cilia) beat rhythmically, pushing the mucus blanket (and trapped debris) up and out of the lower airway toward the pharynx to be swallowed or coughed out.
- Cough: A vital involuntary reflex that clears the lower airways of mucus and foreign materials.
- Position Changes (Movement): Mobilization and frequent turning help to redistribute air and promote the drainage of secretions, preventing atelectasis and pneumonia.
- Lymphatics: A network of vessels and nodes that filter and trap pathogens and fluid from the lungs, promoting systemic immunity.
- Humoral Defenses: Immune components found in the blood and secretions, including:
- Immunoglobulin A (IgA): Found in respiratory secretions, providing localized immunity.
- Macrophages: Immune cells that engulf and destroy foreign particles, especially in the alveoli.
Summary
- The pediatric respiratory system is characterized by small, collapsible airways, a highly compliant chest wall, and higher O2 demands.
- These differences mean children have less respiratory reserve and are highly susceptible to obstruction and rapid deterioration.
- Nurses must have a keen understanding of age-specific anatomy, be proficient in recognizing subtle signs of distress (like retractions and nasal flaring), and intervene quickly to prevent respiratory failure.
- Key clinical differences include the obligate nose breathing of infants, the funnel shape of the larynx, and the faster fatigue of the diaphragm.
- Early recognition and intervention are the cornerstones of successful pediatric respiratory care.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Pediatric Anatomy And Physiology Of The Respiratory Tract
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now