Please set your exam date
Hyperemesis Gravidarum
Study Questions
Practice Exercise 1
A nurse is educating a client diagnosed with hyperemesis gravidarum. Which hormone is primarily implicated in the pathogenesis of hyperemesis gravidarum due to its peak levels in the first trimester, and which of the following best explains the mechanism?
Explanation
Hyperemesis gravidarum is characterized by severe, persistent vomiting leading to dehydration, ketonuria, and > 5% weight loss. Rapidly rising human chorionic gonadotropin levels peak between 8 and 12 weeks gestation, cross-reacting with the thyrotropin receptor and stimulating the medullary emetic center.
Rationale for correct answer
- High serum concentrations of human chorionic gonadotropin directly stimulate the chemoreceptor trigger zone located in the area postrema. This neurohumoral activation induces severe emesis during the first trimester when hormone levels are maximal. The structural similarity between the alpha subunit of this hormone and thyroid-stimulating hormone further exacerbates metabolic disturbances.
Rationale for incorrect answers
- While progesterone levels rise significantly during pregnancy, this hormone actually causes smooth muscle relaxation rather than increased motility. This leads to delayed gastric emptying and esophageal sphincter relaxation, contributing to gastroesophageal reflux but not the primary pathogenesis of hyperemesis.
- Estrogen contributes to the general nausea of pregnancy by increasing olfactory sensitivity and altering fluid balance. However, it does not primarily enhance insulin secretion as a mechanism for vomiting, and its levels continue to rise throughout pregnancy rather than peaking in the first trimester.
- Thyroid-stimulating hormone typically decreases in early pregnancy because human chorionic gonadotropin acts as a thyroid stimulator, causing a transient hyperthyroidism. It does not act by suppressing gastric acid secretion; rather, the suppressed levels are a physiological response to the thyroid-stimulating effects of high pregnancy hormones.
Test-taking strategy
- Identify the Core Issue: The question asks for the primary hormone and mechanism responsible for hyperemesis gravidarum, focusing on first-trimester peaks.
- Analyze the Hormonal Timeline: Recall that human chorionic gonadotropin (hCG) reaches its highest concentration around 10 to 12 weeks gestation, aligning with the typical onset and peak of hyperemesis symptoms.
- Eliminate Pathophysiological Errors: Rule out Choice 1 because progesterone decreases motility via muscle relaxation. Rule out Choice 2 because estrogen does not peak in the first trimester. Rule out Choice 4 because thyroid-stimulating hormone (TSH) is usually suppressed, not the primary driver of the emetic reflex.
- Evaluate the Mechanism: The chemoreceptor trigger zone (CTZ) is the neurological center for vomiting. Link hCG to CTZ stimulation to confirm the most scientifically accurate physiological pathway for severe gestational emesis.
Take home points
- Human chorionic gonadotropin peaks during the first trimester and is the primary biological marker associated with the severity of hyperemesis gravidarum.
- The chemoreceptor trigger zone in the brainstem is activated by high hormonal concentrations, leading to the clinical manifestation of intractable vomiting.
- Hyperemesis gravidarum must be differentiated from morning sickness by the presence of significant weight loss, electrolyte imbalances, and ketonuria.
- Maternal thyroid function tests may show suppressed TSH and elevated free T4 due to the structural homology between hCG and TSH.
A nurse is reviewing laboratory findings of a client with hyperemesis gravidarum. Which of the following acid–base disturbances is most directly caused by repeated loss of gastric secretions?
Explanation
Hyperemesis gravidarum induces a severe metabolic alkalosis characterized by an arterial pH > 7.45 and an elevated serum bicarbonate. The primary driver is the active secretion of hydrogen ions into the stomach, which are subsequently expelled, preventing their normal reabsorption in the small intestine. This loss of gastric acid is coupled with hypovolemia, which triggers secondary hyperaldosteronism and further renal potassium and hydrogen ion excretion.
Rationale for correct answer
- The stomach contains a high concentration of hydrochloric acid produced by parietal cells via the hydrogen-potassium ATPase pump. Repeated emesis results in the massive loss of hydrogen and chloride ions, leading to a surplus of bicarbonate in the extracellular fluid. This shift raises the systemic pH, while the concurrent loss of chloride forces the kidneys to retain bicarbonate to maintain electrical neutrality.
Rationale for incorrect answers
- Metabolic acidosis occurs when there is a gain of non-volatile acids or a bicarbonate loss, typically through lower gastrointestinal secretions like diarrhea. In hyperemesis, the pathology is the opposite, as the body loses acid rather than base. If a client develops ketosis from starvation, they may eventually develop a metabolic acidosis, but it is not the direct result of losing gastric secretions.
- Respiratory alkalosis is defined by a primary decrease in partial pressure of carbon dioxide due to alveolar hyperventilation. While a pregnant woman may have a slightly lower baseline pCO2 due to progesterone-induced stimulation of the respiratory center, it is not the direct consequence of losing gastric fluids. Gastric secretions affect metabolic components of the acid-base balance, not the primary respiratory drive or CO2 elimination.
- Respiratory acidosis results from alveolar hypoventilation leading to the retention of carbon dioxide and a subsequent drop in pH. This condition is typically associated with obstructive lung diseases, respiratory center depression, or neuromuscular disorders. The loss of gastric secretions in hyperemesis does not cause CO2 retention; if anything, the body may slightly decrease respirations as a compensatory mechanism for metabolic alkalosis.
Test-taking strategy
- Identify the anatomical source: The question specifies the loss of gastric secretions, which are highly acidic due to hydrochloric acid content.
- Apply Acid-Base Principles: Recognize that losing an acid (H+) from the body will result in an alkalotic state, while losing a base (HCO3-) results in an acidotic state.
- Differentiate Metabolic vs. Respiratory: Since the loss is occurring through the gastrointestinal tract (a metabolic route) and not the lungs, the primary disturbance must be metabolic. This allows for the immediate elimination of choices 2 and 4.
- Evaluate Electrolyte Shifts: Consider the relationship between chloride and bicarbonate. As chloride is lost in gastric juice, the kidneys increase bicarbonate reabsorption to maintain anionic balance, reinforcing the state of metabolic alkalosis.
Take home points
- Profuse vomiting leads to metabolic alkalosis because of the direct depletion of gastric hydrogen and chloride ions.
- Contraction alkalosis occurs in these patients as the kidneys prioritize sodium and water retention over acid-base balance due to severe dehydration.
- Hypokalemia frequently accompanies this condition because potassium shifts into the cells in exchange for hydrogen ions during alkalosis.
- Laboratory findings in severe hyperemesis typically include elevated pH, elevated bicarbonate, low chloride, and low potassium.
A nurse is assessing the pathophysiology of hyperemesis gravidarum. Which of the following physiological changes contribute to persistent vomiting? Select all that apply
Explanation
Hyperemesis gravidarum involves multifactorial pathophysiology including hormonal surges and gastrointestinal dysmotility. Elevated human chorionic gonadotropin and progesterone levels decrease myoelectric gastric activity, leading to gastric dysrhythmia and severe emesis. Persistent starvation induces lipolysis, resulting in metabolic acidosis and ketonuria which further irritates the medullary emetic centers.
Rationale for correct answers
1. High concentrations of progesterone during pregnancy cause smooth muscle relaxation, which results in significantly decreased motility. This delayed transit time leads to gastric stasis and distension. Such physiological shifts directly contribute to the nausea and persistent vomiting characteristic of the condition.
2. Rapidly rising human chorionic gonadotropin levels directly stimulate the area postrema in the medulla oblongata. This region contains the chemoreceptor trigger zone, which lacks a functional blood-brain barrier. Activation of these receptors by pregnancy hormones triggers the involuntary vomiting reflex and persistent emetic episodes.
4. Intractable vomiting leads to inadequate caloric intake and subsequent glycogen depletion. The body shifts to utilizing adipose tissue for energy, which increases ketone production through fatty acid oxidation. These circulating ketones cross into the central nervous system, further exacerbating the cycle of nausea and vomiting.
Rationale for incorrect answers
3. In hyperemesis gravidarum, there is actually a decrease in sphincter tone due to the systemic effects of progesterone on smooth muscle. A high tone would provide a protective barrier against reflux and emesis. The relaxation of the lower esophageal sphincter facilitates the retrograde movement of gastric contents during vomiting.
5. Frequent emesis does not increase gastric neutralization; instead, it causes a massive loss of hydrochloric acid and hydrogen ions. This loss leads to an increase in systemic pH and metabolic alkalosis. Neutralization mechanisms like bicarbonate secretion are overwhelmed by the mechanical loss of acidic gastric secretions during persistent vomiting.
Test-taking strategy
- Analyze the Physiology: Evaluate each choice based on how it influences the gastrointestinal or neurological systems during pregnancy.
- Apply Hormonal Knowledge: Recall that progesterone is a smooth muscle relaxant. This confirms that it would decrease, not increase, motility and sphincter tone. Therefore, Choice 1 is correct and Choice 3 is incorrect.
- Identify Emetic Pathways: Recognize that the chemoreceptor trigger zone (CTZ) is the primary neurological pathway for hormone-induced vomiting. This validates Choice 2.
- Evaluate Metabolic Consequences: Consider the effect of prolonged starvation. If a patient cannot retain food, they will burn fat, producing ketones. This supports Choice 4.
- Review Acid-Base Balance: Remember that vomiting results in the loss of acid (HCl). This makes the stomach contents more likely to be acidic upon exit and the blood more alkaline, contradicting the idea of neutralization in Choice 5.
Take home points
- Progesterone-induced gastric dysrhythmia and delayed emptying are primary mechanical contributors to pregnancy-related emesis.
- Hormonal stimulation of the chemoreceptor trigger zone in the medulla is the neurological basis for severe vomiting.
- Ketosis from starvation creates a self-perpetuating cycle of nausea by further irritating the central emetic centers.
- The condition is distinguished from normal morning sickness by the presence of dehydration, ketonuria, and significant weight loss.
A nurse is caring for a client with severe hyperemesis gravidarum and notes neurological changes. Which of the following mechanisms places the client at highest risk for Wernicke’s encephalopathy?
Explanation
Hyperemesis gravidarum induces a critical thiamine deficiency through prolonged emesis and inadequate nutritional intake. This essential cofactor for pyruvate dehydrogenase is necessary for cerebral glucose metabolism; without it, the administration of intravenous dextrose precipitates acute neurotoxicity and neuronal death.
Rationale for correct answer
2. Wernicke's encephalopathy is caused by a depletion of Vitamin B1, which is a required coenzyme for the Kreb's cycle. When a severely malnourished client receives intravenous dextrose without prior thiamine supplementation, the sudden glucose load exhausts the remaining thiamine stores. This metabolic demand leads to acute cerebral ischemia and the classic triad of ataxia, ophthalmoplegia, and acute confusion.
Rationale for incorrect answers
1. While severe emesis can lead to a state of starvation, it does not typically cause persistent hypoglycemia via insulin resistance. In fact, pregnancy is a state of relative insulin resistance designed to ensure glucose availability for the fetus. While hypoglycemia can occur during fasting, it is not the primary pathophysiological mechanism that triggers the specific neurological damage seen in encephalopathy.
3. Human chorionic gonadotropin shares a structural alpha-subunit with thyroid-stimulating hormone, often leading to transient gestational hyperthyroidism. While elevated free T4 can cause tremors or tachycardia, it does not cause the specific hemorrhagic lesions in the mammillary bodies seen in Wernicke's. Thyroid levels in hyperemesis usually normalize without intervention once the hormone peaks subside after the first trimester.
4. Progesterone acts as a systemic smooth muscle relaxant, leading to delayed gastric emptying and increased venous capacitance. While this contributes significantly to the gastrointestinal symptoms and potential orthostatic hypotension in hyperemesis, it has no direct correlation with central nervous system cellular damage. It affects the peripheral autonomic and digestive systems rather than the metabolic pathways of the brain.
Test-taking strategy
- Identify the Emergency: Recognize Wernicke's encephalopathy as a life-threatening neurological complication related to nutritional deficiency in chronic vomiting or alcoholism.
- Link Nutrient to Condition: Associate Vitamin B1 (thiamine) directly with the prevention of Wernicke-Korsakoff syndrome. This makes Choice 2 the most scientifically plausible answer.
- Evaluate Iatrogenic Risks: Recall the nursing priority that "thiamine must come before glucose." Giving sugar to a thiamine-deficient brain causes a metabolic "crash" because the brain cannot process the glucose, leading to toxic byproduct accumulation.
- Rule out Hormonal Distractions: While progesterone and thyroid hormones are involved in the general pathophysiology of hyperemesis, they do not explain the sudden onset of neurological changes like ataxia or cranial nerve palsies.
Take home points
- Wernicke's encephalopathy in hyperemesis gravidarum is a medical emergency caused by severe thiamine (Vitamin B1) deficiency.
- Intravenous dextrose must never be administered to a severely malnourished patient before thiamine supplementation is provided.
- The clinical triad of the condition includes ataxia, global confusion, and ocular abnormalities such as nystagmus.
- Untreated Wernicke's encephalopathy can progress to Korsakoff syndrome, which involves permanent anterograde and retrograde amnesia.
A nurse is identifying risk factors related to the underlying pathophysiology of hyperemesis gravidarum. Which of the following conditions increase hormone-mediated stimulation of vomiting pathways? Select all that apply
Explanation
Hyperemesis gravidarum risk is directly proportional to the total concentration of circulating hormones, particularly human chorionic gonadotropin. Conditions that increase placental mass lead to supra-physiologic hormone production, which excessively stimulates the medullary centers and the chemoreceptor trigger zone. Genetic predisposition also plays a role through the GDF15 gene, which encodes a protein specifically linked to appetite regulation and the induction of nausea.
Rationale for correct answers
1. Multiple gestations, such as twins or triplets, result in a significantly larger total placental volume. This increased tissue mass produces much higher concentrations of human chorionic gonadotropin and estrogen compared to singleton pregnancies. These elevated hormonal peaks provide more intense stimulation to the vomiting centers in the brain, greatly increasing the clinical severity of emetic symptoms.
2. A molar pregnancy, or hydatidiform mole, is a gestational trophoblastic disease characterized by abnormal trophoblastic proliferation. This condition results in extremely high, pathological levels of hCG, often exceeding 100,000 mIU/mL. Such extreme hormonal concentrations are a classic trigger for early and severe hyperemesis gravidarum, necessitating immediate ultrasound and surgical evacuation of the uterus.
4. Evidence suggests a strong genetic component in the development of hyperemesis, as the condition often clusters within families. Research has identified specific genes, such as GDF15 and IGFBP7, which are expressed in the placenta and influence maternal nausea pathways. A positive family history indicates a lower biological threshold for the emetic response to normal or slightly elevated pregnancy hormones.
Rationale for incorrect answers
3. A singleton pregnancy with low hCG levels is statistically associated with a decreased risk of hyperemesis. Since hCG is the primary hormone implicated in the pathogenesis of the condition, lower levels typically result in milder symptoms or none at all. Abnormally low hCG levels are more often associated with failing pregnancies or ectopic implantations rather than the hyper-emetic state.
5. Decreased estrogen levels are not a risk factor; rather, elevated estrogen levels are known to contribute to nausea. Estrogen increases the sensitivity of the olfactory system, making the pregnant woman more reactive to food odors and environmental scents. Lower levels of this steroid hormone would generally lead to a reduction in the sensory triggers that initiate the vomiting reflex.
Test-taking strategy
- Analyze Hormonal Correlation: Recognize that hyperemesis is a "high-hormone" state. Evaluate the options to determine which ones increase hormone production.
- Identify Placental Mass: Recall that multiple gestations and molar pregnancies involve more placental tissue, leading to the highest levels of hCG. This confirms Choices 1 and 2.
- Evaluate Genetic Influence: Consider that many obstetric conditions have hereditary patterns. Identifying "family history" as a risk factor is a common correct theme in pathophysiology questions, validating Choice 4.
- Eliminate Inconsistent Options: Rule out Choice 3 and Choice 5 because they describe "low" or "decreased" states, which contradict the underlying hyper-metabolic and hyper-hormonal nature of the disease.
Take home points
- Conditions that increase placental mass, such as multifetal pregnancy, directly correlate with the severity of hyperemesis.
- Gestational trophoblastic disease (molar pregnancy) is a critical differential diagnosis for any patient with extreme first-trimester vomiting.
- The GDF15 hormone and its corresponding gene are major genetic determinants of a woman's susceptibility to severe pregnancy-related nausea.
- Clinical risk assessment should always include a review of previous pregnancies and family history to identify high-risk individuals early.
Practice Exercise 2
A nurse is assessing a pregnant client with severe nausea and vomiting. Which of the following maternal histories places the client at the highest risk for developing hyperemesis gravidarum?
Explanation
Hyperemesis gravidarum exhibits a high rate of recurrence in subsequent pregnancies, estimated between 15% and 80%. This susceptibility is likely driven by genetic polymorphisms in the GDF15 and IGFBP7 genes, which lower the threshold for emesis in response to placental hormones.
Rationale for correct answer
2. A maternal history of a previous pregnancy complicated by hyperemesis is the most significant clinical predictor for the condition. The underlying pathophysiological sensitivity to human chorionic gonadotropin remains constant across pregnancies, meaning the chemoreceptor trigger zone will likely react with the same intensity to future hormonal surges. This history necessitates early nutritional and pharmacological prophylaxis before symptoms peak in the first trimester.
Rationale for incorrect answers
1. Multiparity with uncomplicated prior pregnancies is actually associated with a decreased risk of hyperemesis. Women who have successfully navigated previous gestations without severe vomiting have demonstrated a physiological tolerance to pregnancy hormones. Nulliparity is traditionally considered a higher risk factor than asymptomatic multiparity, as the maternal body's reaction to the initial surge of hCG is less predictable.
3. A singleton pregnancy at 28 weeks gestation is well beyond the typical pathogenetic window for hyperemesis gravidarum. Symptoms of hyperemesis almost universally initiate in the first trimester, typically between 4 and 9 weeks, and peak around week 12. If severe vomiting begins in the third trimester, the nurse should investigate other etiologies such as preeclampsia or acute fatty liver of pregnancy.
4. A history of gestational diabetes mellitus involves a primary pathology of insulin resistance and pancreatic insufficiency, which is distinct from the emetic pathways. While both conditions involve metabolic stress, there is no direct evidence that glucose intolerance stimulates the medullary centers or increases hCG production. Therefore, gestational diabetes does not increase the risk of intractable vomiting in the way that placental mass or genetic history does.
Test-taking strategy
- Prioritize Recurrence: In many obstetric and medical conditions, the strongest predictor of future occurrence is a previous history of that specific condition.
- Apply Chronological Knowledge: Evaluate the timing of the symptoms. Hyperemesis is a disease of early pregnancy; recognizing that 28 weeks is too late helps eliminate Choice 3.
- Analyze Hormonal Load: Consider which factor most directly correlates with the "sensitivity" to hCG. While multiparity (Choice 1) deals with hormones, "uncomplicated" suggests low sensitivity.
- Rule out Unrelated Pathologies: Distinguish between metabolic disorders of carbohydrate metabolism (Choice 4) and those of emetic regulation. This allows for the confident selection of Choice 2.
Take home points
- The single strongest risk factor for hyperemesis gravidarum is a personal history of the condition in a prior pregnancy.
- Genetic predisposition, specifically involving the GDF15 gene, explains the high rate of recurrence among female relatives.
- Hyperemesis typically resolves by 20 weeks gestation, differentiating it from late-pregnancy nausea caused by gastrointestinal displacement.
- Early identification of high-risk clients allows for the initiation of Vitamin B6 and ginger before the onset of intractable vomiting.
A nurse is caring for a client at 10 weeks gestation with persistent vomiting. Which pregnancy-related factor most strongly contributes to the development of hyperemesis gravidarum through excessive hormonal stimulation?
Explanation
Hyperemesis gravidarum is characterized by intractable vomiting mediated by the supraphysiologic elevation of gestational hormones. The primary driver is human chorionic gonadotropin, which reaches its absolute peak between 8 and 12 weeks, inducing gastric dysrhythmia and activating the area postrema within the brainstem.
Rationale for correct answer
2. Multiple gestations, such as twins or triplets, involve a significantly larger placental mass, which directly correlates with higher circulating levels of human chorionic gonadotropin. This hormonal surge causes excessive stimulation of the chemoreceptor trigger zone, leading to more severe and persistent emetic episodes. The structural similarity between the alpha subunit of this hormone and thyroid-stimulating hormone also induces a transient hyperthyroidism that exacerbates metabolic disturbances.
Rationale for incorrect answers
1. Advanced gestational age is not a risk factor because hyperemesis is a disease of the first trimester. By the second and third trimesters, human chorionic gonadotropin levels naturally decline and stabilize, leading to the resolution of symptoms in approximately 90% of cases. If severe vomiting persists beyond 20 weeks, clinicians must investigate secondary causes such as preeclampsia or late-onset gastrointestinal disorders.
3. Reduced placental mass would result in lower concentrations of human chorionic gonadotropin and estrogen, thereby decreasing the stimulus for vomiting. Conditions associated with small placentas, such as placental insufficiency or certain chromosomal abnormalities, are less likely to present with hyperemesis gravidarum. The condition is fundamentally driven by a high trophoblastic burden and excessive hormone production.
4. Decreased estrogen levels would likely result in a reduction of nausea symptoms rather than an increase. Estrogen is known to enhance the olfactory response, making pregnant women hyper-reactive to environmental odors and food scents. High levels of estradiol are consistently associated with the pathogenesis of severe vomiting, while low levels are generally protective against the hyperemetic state.
Test-taking strategy
- Analyze the Physiological Peak: The question specifies 10 weeks gestation, which is the physiological peak for human chorionic gonadotropin (hCG).
- Apply the "More is More" Principle: Hyperemesis is a condition of excess. Therefore, the nurse should look for factors that increase, rather than decrease, hormonal or placental load. This immediately eliminates Choice 3 and Choice 4.
- Differentiate Trimesters: Recognize that "advanced gestational age" (Choice 1) refers to later pregnancy, whereas hyperemesis is an early pregnancy complication.
- Correlate Placental Mass with Symptoms: Link multiple gestations to increased hCG production. Since hCG is the primary hormone implicated in the stimulation of the vomiting centers, this confirms Choice 2 as the most scientifically sound answer.
Take home points
- The severity of hyperemesis gravidarum is directly proportional to the total concentration of circulating human chorionic gonadotropin.
- Multiple gestations and molar pregnancies are the primary risk factors due to increased trophoblastic tissue and hormone secretion.
- Hormonal peaks in the first trimester stimulate the chemoreceptor trigger zone, which lacks a blood-brain barrier.
- Symptoms typically peak between 10 and 12 weeks gestation and should resolve as hormone levels plateau later in pregnancy.
A nurse is identifying clients at increased risk for hyperemesis gravidarum. Which of the following maternal characteristics are recognized risk factors? Select all that apply
Explanation
Hyperemesis gravidarum is a complex gestational disorder likely involving a lower neurological threshold for emetic stimuli. The condition is associated with high trophoblastic mass and specific genetic markers like GDF15, which sensitize the brainstem. Maternal predisposition through pre-existing sensory or vestibular sensitivities increases the risk of intractable vomiting during the first trimester.
Rationale for correct answers
1. A history of motion sickness indicates a highly sensitive vestibular system and medullary emetic center. In the context of pregnancy, the hormonal surge of human chorionic gonadotropin acts upon an already reactive neurological pathway. This pre-existing sensitivity makes the client significantly more vulnerable to developing severe, persistent vomiting when exposed to gestational metabolic shifts.
2. Nulliparity, or being a first-time mother, is a recognized demographic risk factor for hyperemesis gravidarum. The maternal body has not been previously exposed to the rapid, supra-physiologic rise in pregnancy-related hormones like hCG and estrogen. This lack of immunological or physiological habituation often results in a more profound systemic reaction to the initial pregnancy.
3. A previous diagnosis of hyperemesis gravidarum is the strongest predictor for recurrence in subsequent pregnancies. The underlying pathophysiological sensitivity to placental hormones remains constant, and genetic studies suggest a hereditary component that lowers the emetic threshold. Early pharmacological intervention is typically required in these patients before the peak hormonal surge at 10 weeks.
5. Women with a history of migraines often have a more reactive chemoreceptor trigger zone and altered serotonin signaling. These neurological traits overlap with the pathways that mediate pregnancy-induced emesis and nausea. The same triggers that induce a migraine episode can synergize with elevated estrogen to precipitate the intractable vomiting seen in hyperemesis.
Rationale for incorrect answers
4. Multiparity without complications is generally considered a protective factor rather than a risk. A history of successful gestations without severe emesis suggests a high maternal tolerance to hormonal fluctuations and placental secretions. The risk for hyperemesis is significantly lower in women who have previously experienced normal pregnancies without significant nausea or vomiting.
Test-taking strategy
- Identify Neurological Sensitivities: Look for conditions that involve a "sensitive" brain or nervous system. Motion sickness and migraines both involve the brainstem and vomiting pathways, making Choice 1 and Choice 5 correct.
- Recognize the Strongest Predictor: Always prioritize prior history of the same condition as the primary risk factor. This confirms Choice 3.
- Evaluate Obstetric History: Distinguish between the risks of a "first-time" experience versus a "proven" history of health. Nulliparity is a stressor for many pregnancy complications, while uncomplicated multiparity suggests resilience. This validates Choice 2 and eliminates Choice 4.
- Apply Hormonal Logic: Focus on factors that correlate with a high hormonal reaction. Since Choice 4 describes a body that previously handled hormones well, it is logically inconsistent with a "risk factor" question.
Take home points
- Previous history of hyperemesis is the most significant clinical indicator for recurrence in future pregnancies.
- Pre-existing neurological conditions like migraines and motion sickness lower the threshold for hormonal stimulation of the vomiting center.
- Nulliparity increases risk as the maternal system encounters the rapid surge of hCG for the first time without prior adaptation.
Clinicians should screen for these risk factors during the initial prenatal visit to implement early dietary and lifestyle modifications.
A nurse is reviewing diagnostic findings for a client with early severe hyperemesis gravidarum. Which associated condition must be ruled out due to its link with markedly elevated human chorionic gonadotropin levels?
Explanation
Hyperemesis gravidarum is a clinical diagnosis of exclusion, necessitating the investigation of underlying trophoblastic pathologies. Markedly elevated human chorionic gonadotropin levels, often exceeding 100,000 mIU/mL, characterize gestational trophoblastic disease. This pathological proliferation of placental tissue leads to supraphysiologic stimulation of the medullary emetic centers, manifesting as intractable vomiting and significant metabolic derangement.
Rationale for correct answer
2. A molar pregnancy, or hydatidiform mole, involves an abnormal genetic conception where the placental villi become swollen and fluid-filled, resembling clusters of grapes. This condition produces extreme concentrations of hCG that far exceed the levels found in a normal singleton pregnancy. Because this hormone is the primary trigger for the chemoreceptor trigger zone, a nurse must ensure an ultrasound is performed to rule out this pathology in any client presenting with severe, early-onset hyperemesis.
Rationale for incorrect answers
1. An ectopic pregnancy occurs when a fertilized egg implants outside the uterine cavity, most commonly in the fallopian tube. While this condition involves the production of human chorionic gonadotropin, the levels are typically lower than expected for the calculated gestational age. Low or slowly rising hormone levels are inconsistent with the pathophysiological drive behind hyperemesis, which requires high hormonal concentrations to stimulate the vomiting reflex.
3. Placenta previa is an obstetric complication where the placenta implants in the lower segment of the uterus, potentially covering the internal os. This is a condition associated with painless bleeding in the second or third trimester rather than hormonal surges in the first trimester. It does not involve an increase in trophoblastic mass or elevated hCG levels and is therefore unrelated to the development of hyperemesis gravidarum.
4. Gestational diabetes mellitus is a metabolic disorder characterized by insulin resistance and impaired glucose tolerance emerging during pregnancy. While it shares some metabolic complexities with hyperemesis, its pathogenesis is related to placental lactogen and maternal pancreatic function rather than hCG-mediated emesis. There is no clinical link between the development of gestational diabetes and the hormone-induced pathways that trigger severe first-trimester vomiting.
Test-taking strategy
- Identify the Key Driver: Focus on the phrase "markedly elevated human chorionic gonadotropin levels." In obstetrics, the most common "high-hCG" pathology is molar pregnancy.
- Rule out Timing: Hyperemesis occurs in the first trimester. Choice 3 (Placenta previa) and Choice 4 (Gestational diabetes) are typically second or third-trimester concerns.
- Analyze Hormone Trends: Distinguish between "low/rising" hCG (suggestive of Choice 1, ectopic) and "excessive/pathological" hCG (suggestive of Choice 2, molar).
- Select the Diagnosis of Exclusion: Recall that any patient with severe vomiting and an oversized uterus for gestational age must be screened for trophoblastic disease to ensure proper surgical and oncological follow-up.
Take home points
- Molar pregnancy is a critical differential diagnosis for hyperemesis gravidarum due to extreme hCG production.
- A pelvic ultrasound is the gold standard diagnostic tool to differentiate between a viable pregnancy and a hydatidiform mole.
- Ectopic pregnancies usually present with lower-than-normal hCG levels and are unlikely to cause hyperemesis.
- Management of a molar pregnancy involves surgical evacuation and monitoring of hCG levels to ensure they return to zero, preventing malignant transformation.
A nurse is providing anticipatory guidance to a client with risk factors for hyperemesis gravidarum. Which associated medical conditions are known to increase the risk? Select all that apply
Explanation
Hyperemesis gravidarum results from an interplay of hormonal surges and gastrointestinal dysmotility. The condition is strongly associated with high levels of human chorionic gonadotropin and estrogen, which alter myoelectric activity. Pre-existing gastrointestinal inflammation or metabolic imbalances can exacerbate the emetic response, leading to intractable vomiting and dehydration during the first trimester.
Rationale for correct answers
1. A chronic infection with Helicobacter pylori is significantly more prevalent in women suffering from hyperemesis gravidarum. This gram-negative bacterium causes gastric mucosal inflammation and alters gastrin secretion, which synergizes with pregnancy hormones to trigger severe emesis. Persistent infection may delay the resolution of symptoms beyond the typical first-trimester window, often requiring targeted antibiotic therapy for resolution.
2. Transient gestational hyperthyroidism occurs because the alpha-subunit of hCG is structurally identical to thyroid-stimulating hormone. In cases of extreme hCG elevation, the hormone binds to TSH receptors, causing a temporary increase in free thyroxine levels. This hypermetabolic state is a common pathophysiological finding in hyperemesis and directly correlates with the severity of the patient's nausea and vomiting.
4. Gastroesophageal reflux disease is exacerbated by the progesterone-mediated relaxation of the lower esophageal sphincter. The retrograde flow of gastric acid irritates the esophageal mucosa and can stimulate the vomiting reflex through vagal pathways. Clients with a pre-pregnancy history of this condition are at higher risk because their gastric clearance is already compromised before the hormonal shifts of pregnancy occur.
Rationale for incorrect answers
1. Chronic hypertension is a cardiovascular condition defined by persistent blood pressure ≥ 140/90 mmHg. While it increases the risk for preeclampsia and placental abruption, it does not share a common pathophysiological pathway with the emetic centers of the brain. There is no evidence that elevated systemic vascular resistance or arterial pressure influences the secretion of hCG or the sensitivity of the chemoreceptor trigger zone.
3. Iron-deficiency anemia is a common hematological finding in pregnancy due to increased fetal demand and plasma volume expansion. However, anemia itself is not a primary trigger for the medullary emetic response. In fact, oral iron supplementation is frequently discontinued in patients with hyperemesis because iron is a known gastric irritant that can worsen pre-existing nausea and vomiting.
Test-taking strategy
- Identify Gastric Irritants: Evaluate which conditions directly affect the stomach or the "vomiting center." Since Helicobacter pylori (Choice 1) and GERD (Choice 4) both involve the GI tract, they are highly likely contributors.
- Apply Hormonal Logic: Recall the structural similarity between hCG and TSH. Recognizing that a "hyper-hormonal" state like hyperemesis often causes thyroid shifts validates Choice 2.
- Differentiate Trimester-Specific Risks: Chronic hypertension (Choice 3) is a systemic vascular issue, not an emetic one. Use the "ABC" or "systemic vs local" rule to see that blood pressure does not drive the vomiting reflex.
- Analyze Treatment Side Effects: For Choice 5, remember that iron is a cause of nausea, but the deficiency itself is not the risk factor. This subtle distinction helps eliminate anemia as a pathophysiological cause of hyperemesis.
Take home points
- Helicobacter pylori infection is a known co-factor that increases the severity and duration of hyperemesis gravidarum.
- Transient gestational hyperthyroidism is a frequent biochemical finding due to the cross-reactivity of hCG with TSH receptors.
- Progesterone-induced relaxation of the esophageal sphincter makes pre-existing GERD a significant risk factor for severe emesis.
- Clinical management should include screening for GI infections and thyroid dysfunction in refractory cases of vomiting.
Practice Exercise 3
A nurse is assessing a pregnant client with suspected hyperemesis gravidarum. Which of the following clinical findings is most indicative of this condition?
Explanation
Hyperemesis gravidarum is a severe gestational disorder characterized by intractable vomiting and significant metabolic disruption. It causes systemic ketosis, profound dehydration, and electrolyte imbalances such as hypokalemia. The clinical diagnosis requires evidence of nutritional depletion and a loss of at least 5% of pre-pregnancy weight.
Rationale for correct answer
3. Clinical diagnosis of hyperemesis requires objective evidence of severe nutritional deficit. Weight loss exceeding 5% of the baseline pre-pregnancy mass is a hallmark of the condition. This metric indicates that the patient has reached a state of catabolism where caloric intake is insufficient for maternal and fetal metabolic demands.
Rationale for incorrect answers
1. Occasional nausea that is relieved by eating is a characteristic of physiological "morning sickness" rather than hyperemesis. In hyperemesis, oral intake usually precipitates further vomiting, making relief through eating impossible. This finding suggests a mild form of pregnancy-associated nausea that does not meet the criteria for pathological emesis.
2. Vomiting once daily in the evening is inconsistent with the persistent and intractable nature of hyperemesis. Hyperemesis involves continuous or multiple daily episodes that interfere with activities of daily living. A single daily episode lacks the frequency required to cause the severe dehydration and ketonuria seen in this clinical syndrome.
4. Mild dehydration with normal electrolyte levels does not reflect the severity of hyperemesis gravidarum. True hyperemesis is associated with electrolyte disturbances such as hypochloremic metabolic alkalosis and hypokalemia. Normal levels suggest that the body's homeostatic mechanisms are still intact, whereas hyperemesis involves a failure of these compensatory systems.
Test-taking strategy
- Define the Severity: Differentiate between "normal" pregnancy discomfort and a medical emergency. Hyperemesis is defined by its extreme clinical manifestations, so look for the most severe data point.
- Apply Diagnostic Criteria: Recall the "rule of 5" for hyperemesis. The medical definition specifically includes weight loss of at least 5% of pre-pregnancy weight as a primary diagnostic indicator.
- Eliminate Physiological Norms: Choice 1 and Choice 2 describe symptoms that are common and non-pathological in many early pregnancies. Rule them out as they do not indicate a disease state.
- Analyze Laboratory Expectations: In a patient with "severe" hyperemesis, electrolytes should be abnormal due to gastric acid loss. Choice 4 is eliminated because it describes "normal" laboratory findings, which contradicts the diagnosis.
Take home points
- Hyperemesis gravidarum is primarily distinguished from morning sickness by weight loss exceeding 5% of baseline body mass.
- Intractable vomiting leads to the development of ketonuria, which serves as a clinical marker for starvation.
- Persistent loss of gastric hydrochloric acid typically results in hypochloremic metabolic alkalosis.
- The condition requires aggressive fluid resuscitation and often pharmacological intervention to prevent neurological complications like Wernicke encephalopathy.
A nurse is reviewing laboratory data for a client with persistent vomiting. Which finding best supports the diagnosis of hyperemesis gravidarum rather than normal nausea and vomiting of pregnancy?
Explanation
Hyperemesis gravidarum is a pathological state characterized by intractable vomiting that leads to a state of starvation. When glucose reserves are exhausted, the body initiates lipolysis, causing the incomplete oxidation of fatty acids and the accumulation of acetoacetate and beta-hydroxybutyrate. This metabolic shift is evidenced by ketonuria, which serves as a definitive clinical marker of nutritional failure and severe dehydration.
Rationale for correct answer
3. The presence of ketonuria indicates that the client has transitioned from carbohydrate metabolism to fat catabolism due to prolonged caloric deprivation. In normal morning sickness, the woman typically retains enough nutrition to avoid ketone production. Finding ketones in the urine confirms that the emesis is severe enough to cause metabolic disruption, distinguishing it from physiological nausea.
Rationale for incorrect answers
1. A urine specific gravity of 1.010 is within the normal range (1.005 to 1.030) and indicates adequate hydration. In hyperemesis gravidarum, the nurse would expect to see a high specific gravity (≥ 1.025) due to severe fluid volume deficit and compensatory renal water reabsorption. A reading of 1.010 suggests that the kidneys are not currently under the osmotic stress associated with severe dehydration.
2. The absence of ketones in the urine would suggest that the client’s energy demands are still being met by glucose and glycogen stores. Since hyperemesis is defined by its ability to cause starvation-level metabolic changes, a negative ketone test would point away from this diagnosis. Normal nausea of pregnancy rarely results in the persistent ketosis required to be labeled as hyperemesis.
4. A stable maternal weight is a strong indicator that the client is not suffering from hyperemesis gravidarum. The diagnostic criteria specifically require a weight loss exceeding 5% of the pre-pregnancy baseline. Stable weight implies that the client is maintaining a positive or neutral caloric balance, whereas hyperemesis is fundamentally a state of progressive nutritional depletion.
Test-taking strategy
- Identify the Pathological Marker: The question asks for a finding that differentiates "pathological" from "normal." Look for a laboratory value that indicates a failure of normal homeostasis.
- Apply Metabolic Knowledge: Recall that when the body cannot get energy from food (due to vomiting), it burns fat, producing ketones. This makes Choice 3 the most medically significant finding for a diagnosis of hyperemesis.
- Rule out Normalcy: Choice 1, Choice 2, and Choice 4 all describe "normal" or "stable" findings. Since hyperemesis is an extreme and unstable condition, these options can be safely eliminated as they do not support a severe diagnosis.
- Correlate Signs and Symptoms: Associate hyperemesis with the "triad" of symptoms: weight loss, dehydration (high specific gravity), and ketonuria. Matching the choice to this known triad confirms the correct answer.
Take home points
- Ketonuria is the primary laboratory indicator of starvation and fat metabolism in hyperemesis gravidarum.
- Urine specific gravity increases in these patients as a result of profound dehydration and hemoconcentration.
- A diagnosis of hyperemesis requires objective evidence of weight loss and metabolic imbalance, not just subjective reports of nausea.
- Electrolyte panels in these clients often reveal hypokalemia and metabolic alkalosis due to the loss of gastric hydrochloric acid.
A nurse is assessing a client with severe hyperemesis gravidarum. Which of the following findings indicate significant dehydration? Select all that apply
Explanation
Hyperemesis gravidarum leads to a profound intracellular and extracellular fluid volume deficit due to the continuous loss of gastric fluids. This state of hypovolemia triggers compensatory mechanisms such as the activation of the renin-angiotensin-aldosterone system and the release of antidiuretic hormone. Clinical manifestations result from decreased hydrostatic pressure and impaired tissue perfusion, necessitating aggressive isotonic fluid resuscitation.
Rationale for correct answers
1. Persistent vomiting prevents adequate oral rehydration, leading to a systemic depletion of total body water. As interstitial fluid is drawn into the vascular compartment to maintain pressure, the mucous membranes become parched and lose their natural lubrication. This is a primary physical indicator of a dehydration state where the body can no longer maintain surface moisture.
2. Fluid loss from the interstitial spaces around the orbit causes a reduction in intraocular pressure and a loss of periorbital fat volume. This results in the characteristic clinical appearance of sunken eyes, which is a sign of advanced fluid volume deficit. It reflects a significant shift in extracellular fluid that occurs when compensatory oral intake is impossible due to intractable emesis.
4. In response to a decreased stroke volume caused by hypovolemia, the baroreceptors trigger an increase in sympathetic nervous system activity. This results in tachycardia, as the heart attempts to maintain a constant cardiac output despite a lower circulating blood volume. A heart rate exceeding 100 beats per minute in a resting pregnant client is a critical sign of cardiovascular compensation for dehydration.
Rationale for incorrect answers
3. Normal skin turgor is a finding associated with adequate hydration and elastic tissue integrity. In a client with severe hyperemesis, the nurse would instead expect to find poor turgor, demonstrated by the skin "tenting" when pinched. This occurs because the dermal layers lack the interstitial fluid necessary to snap back to their original position immediately.
5. Increased urine output, or polyuria, is inconsistent with the physiological response to dehydration. The posterior pituitary gland releases vasopressin, which instructs the kidneys to reabsorb water, leading to oliguria (output < 30 mL/hr) and highly concentrated urine. A client with severe hyperemesis will demonstrate a low volume of urine with a high specific gravity rather than an increase in excretion.
Test-taking strategy
- Identify the Physiological State: The question asks for signs of dehydration. Group the symptoms into those that show "loss" versus those that show "excess."
- Apply the "Dryness" Principle: Dehydration is fundamentally a lack of water. Choice 1 (dry membranes) and Choice 2 (sunken features) fit the physical description of a body lacking fluid.
- Evaluate Hemodynamics: Recall that when volume (preload) goes down, the heart rate must go up to compensate. This confirms Choice 4 as a classic sign of fluid deficit.
- Rule out Normal/Positive Findings: Choice 3 (normal turgor) and Choice 5 (increased output) are signs of "wellness" or "over-hydration." In the context of "severe" vomiting, these findings are physiologically impossible and should be eliminated.
Take home points
- Tachycardia and orthostatic hypotension are early cardiovascular indicators of significant volume depletion in hyperemesis.
- Poor skin turgor and sunken fontanelles or eyes represent a loss of interstitial fluid and late-stage dehydration.
- Oliguria occurs as the kidneys maximize water reabsorption in response to elevated antidiuretic hormone levels.
- Clinical assessment of dehydration must be correlated with laboratory findings such as elevated hematocrit and high urine specific gravity.
A nurse is evaluating a client at 9 weeks gestation with severe vomiting. Which diagnostic test is most appropriate to rule out a molar pregnancy?
Explanation
Hyperemesis gravidarum is a clinical diagnosis of exclusion, necessitating the systematic ruling out of trophoblastic pathologies. Gestational trophoblastic disease, specifically a molar pregnancy, involves abnormal placental proliferation that generates extreme concentrations of human chorionic gonadotropin. This supraphysiologic hormonal surge triggers the medullary emetic centers, resulting in symptoms far more severe than those of a standard singleton gestation.
Rationale for correct answer
3. An ultrasound examination is the definitive diagnostic modality used to visualize the uterine contents and differentiate between a viable fetus and pathological tissue. In a molar pregnancy, the sonogram typically reveals a characteristic snowstorm appearance, which represents hydropic villi and the absence of a gestational sac or fetal heart tones. This immediate visual confirmation is essential for determining if the severe vomiting is driven by an abnormal trophoblastic mass.
Rationale for incorrect answers
1. A complete blood count is used to assess for hemoconcentration (elevated hematocrit) and infection, but it cannot identify the source of hormonal elevation. While it helps the nurse understand the degree of dehydration caused by the vomiting, it provides no anatomical information regarding the pregnancy. It is a supportive laboratory test rather than a confirmatory tool for trophoblastic disease.
2. An electrocardiogram is indicated if the client exhibits severe electrolyte imbalances, such as hypokalemia, which can lead to cardiac dysrhythmias. While it monitors the cardiovascular effects of persistent emesis, it does not address the underlying etiology of the vomiting. It is a safety intervention for managing complications but is not a diagnostic test for molar pregnancy.
4. Liver function tests are often ordered in severe hyperemesis to monitor for transaminitis, which occurs in approximately 50% of hospitalized cases. Elevated AST and ALT levels can indicate hepatic stress from starvation or dehydration, yet these findings are non-specific. They do not distinguish between primary hyperemesis and the high-hCG state of a hydatidiform mole.
Test-taking strategy
- Identify the Diagnostic Goal: The question specifically asks for the "most appropriate" test to rule out a molar pregnancy.
- Match Tool to Anatomy: Recognize that a molar pregnancy is an anatomical abnormality of the uterus. Among the choices, only the ultrasound allows for direct visualization of the uterine cavity.
- Prioritize Confirmatory Testing: While blood tests (Choice 1 and Choice 4) show the effects of the disease, and an ECG (Choice 2) shows cardiac risk, the ultrasound identifies the cause.
- Recall Pathognomonic Signs: Associate the "snowstorm" ultrasound pattern specifically with molar pregnancy to confirm the correct choice.
Take home points
- Ultrasound is the gold standard for differentiating hyperemesis gravidarum from gestational trophoblastic disease.
- A molar pregnancy must be suspected when the uterus is larger than expected for gestational age or when hCG levels are pathologically high.
- Prompt diagnosis of a molar pregnancy is vital to prevent complications such as early-onset preeclampsia or choriocarcinoma.
- Complete blood counts and liver function tests are supplementary tools to assess the systemic impact of severe vomiting.
A nurse is differentiating hyperemesis gravidarum from other conditions. Which findings support the diagnosis of hyperemesis gravidarum? Select all that apply
Explanation
Hyperemesis gravidarum is a pathological state of intractable vomiting that results in systemic metabolic decompensation. Unlike physiological nausea, it involves a transition to catabolism as glycogen stores are depleted and the body begins to metabolize adipose tissue. This leads to the accumulation of acidic byproducts and significant fluid shifts, manifesting as clinical dehydration and biochemical instability within the extracellular compartment.
Rationale for correct answers
1. Persistent vomiting that occurs throughout the day is a hallmark of hyperemesis, distinguishing it from the "morning" sickness that typically resolves after the early hours. This continuous emetic activity prevents any meaningful absorption of nutrients or fluids, leading to a state of progressive starvation. It reflects the constant stimulation of the medullary emetic centers by high concentrations of gestational hormones.
2. Ketonuria occurs when the body lacks sufficient glucose for energy and begins breaking down fatty acids, producing ketone bodies. The presence of these metabolites in the urine is a primary diagnostic marker for hyperemesis, indicating that the patient has entered a starvation state. It serves as objective evidence of the nutritional failure caused by the inability to retain oral intake.
4. Intractable vomiting causes a massive loss of gastric hydrochloric acid and potassium, leading to a profound electrolyte imbalance. The nurse will typically identify hypokalemia, hyponatremia, and hypochloremic metabolic alkalosis on a serum chemistry panel. These findings support the diagnosis by demonstrating that the vomiting has surpassed the body's homeostatic ability to maintain chemical neutrality.
Rationale for incorrect answers
3. Weight gain during the first trimester is a sign of a healthy, progressing pregnancy where caloric intake exceeds metabolic demand. Hyperemesis gravidarum is defined by a mandatory weight loss, typically exceeding 5% of the pre-pregnancy baseline mass. A client who is gaining weight does not meet the diagnostic criteria for this severe condition, regardless of the subjective frequency of nausea.
5. Symptoms relieved by small, frequent meals are characteristic of physiological morning sickness, where stabilizing blood sugar and reducing gastric distension provide therapeutic relief. In hyperemesis, the mere sight, smell, or attempt to ingest any food usually triggers further vomiting. The lack of response to standard dietary modifications is a key clinical indicator that the condition is pathological rather than physiological.
Test-taking strategy
- Identify Pathological vs. Physiological: Look for descriptors that indicate "severity" and "abnormality." Choice 1, Choice 2, and Choice 4 all describe a breakdown of normal body function.
- Apply the 5% Rule: Recall that hyperemesis is synonymous with weight loss. This makes Choice 3 (weight gain) an automatic distractor that can be eliminated.
- Evaluate Treatment Efficacy: Consider how a "normal" pregnant woman reacts to food versus a "hyperemesis" patient. If small meals work (Choice 5), it is not a severe disease state.
- Match Laboratory Markers: Associate "starvation" with "ketones" and "vomiting" with "electrolyte shifts." This confirms that Choice 2 and Choice 4 are necessary components of the diagnosis.
Take home points
- Hyperemesis gravidarum is characterized by weight loss > 5%, ketonuria, and clinical dehydration.
- The presence of ketones in the urine is the most reliable indicator of the transition to a starvation-based metabolism.
- Electrolyte disturbances, particularly hypokalemia, are common and require intravenous replacement to prevent cardiac complications.
- Unlike morning sickness, hyperemesis is often refractory to simple dietary changes and requires pharmacological intervention.
Practice Exercise 4
A nurse is reviewing laboratory results for a client with hyperemesis gravidarum. Which of the following findings is most indicative of dehydration and metabolic alkalosis?
Explanation
Hyperemesis gravidarum induces a severe contraction alkalosis primarily driven by the mechanical loss of hydrogen and chloride ions from the gastric lumen. This state triggers renal proximal tubule bicarbonate reabsorption and secondary hyperaldosteronism, resulting in profound hypokalemia and hemoconcentration. Clinically, the body attempts to conserve volume by producing highly concentrated urine while metabolic pathways shift toward base excess.
Rationale for correct answer
2. A urine specific gravity of 1.035 indicates significant renal concentration in response to decreased circulating volume and elevated antidiuretic hormone. An arterial pH of 7.48 confirms a state of metabolic alkalosis, which is the classic acid-base disturbance resulting from the direct loss of hydrochloric acid. These two findings together provide objective evidence of both severe fluid volume deficit and compensatory metabolic shifts.
Rationale for incorrect answers
1. While a serum potassium of 3.0 mEq/L is consistent with the hypokalemia seen in persistent vomiting, an arterial pH of 7.28 indicates a state of metabolic acidosis. Acidosis in hyperemesis would only occur late due to starvation ketosis, but it is not the primary result of losing gastric secretions. The question specifically asks for findings indicative of alkalosis, making this choice physiologically inconsistent with the primary gastric loss.
3. A serum sodium of 145 mEq/L is at the upper limit of normal, which can occur in dehydration, but a blood urea nitrogen of 10 mg/dL is within the normal range (7 to 20 mg/dL). In significant dehydration, the nurse expects to see an elevated BUN due to decreased renal perfusion and pre-renal azotemia. This combination fails to demonstrate the severity of the clinical dehydration typically associated with pathological hyperemesis gravidarum.
4. Normal electrolytes and a decreased hematocrit are findings that contradict the pathophysiology of severe emesis. Persistent vomiting leads to hemoconcentration, which causes the hematocrit to rise as plasma volume decreases. The presence of normal electrolytes suggests that the client has not yet experienced the significant ionic shifts that characterize the transition from simple nausea to hyperemesis gravidarum.
Test-taking strategy
- Identify the Physiological Demand: The question requires two specific findings: one for dehydration and one for metabolic alkalosis.
- Analyze Acid-Base Balances: Recall that pH > 7.45 is alkalosis and pH < 7.35 is acidosis. This allows you to immediately eliminate Choice 1 because 7.28 is acidotic.
- Evaluate Hydration Markers: Dehydration is marked by high concentration. Urine specific gravity > 1.030 and elevated hematocrit are standard markers. Choice 2 provides a highly concentrated gravity of 1.035.
- Correlate the Findings: Only Choice 2 matches both criteria: a high specific gravity for dehydration and a high pH for alkalosis. Choice 3 and Choice 4 are eliminated because they contain "normal" values (BUN and electrolytes) which do not support a "severe" condition.
Take home points
- Metabolic alkalosis is the primary acid-base disturbance in hyperemesis due to the loss of hydrogen and chloride ions from the stomach.
- Urine specific gravity increases significantly (> 1.025) as the kidneys attempt to conserve water during states of hypovolemia.
- Hypokalemia occurs as potassium is lost in vomitus and further excreted by the kidneys in exchange for hydrogen ions during alkalosis.
- Elevated hematocrit and BUN are expected findings due to hemoconcentration and reduced renal blood flow.
A nurse is evaluating diagnostic data for a client with suspected hyperemesis gravidarum. Which laboratory finding most strongly indicates starvation?
Explanation
Hyperemesis gravidarum induces a metabolic transition toward catabolism when exogenous glucose delivery is insufficient to meet maternal and fetal requirements. Once hepatic glycogen stores are exhausted, the body initiates lipolysis, resulting in the hepatic oxidation of free fatty acids into ketone bodies. This biochemical shift is reflected in the urine as acetoacetate and beta-hydroxybutyrate, serving as the definitive clinical indicator of a starvation state and inadequate caloric intake.
Rationale for correct answer
2. The presence of ketonuria provides objective evidence that the client’s body has shifted to metabolizing fat for fuel due to prolonged nutritional deprivation. In physiological morning sickness, glycogenolysis is usually sufficient to maintain homeostasis, but in hyperemesis, the glycogen depletion is absolute. This finding is a diagnostic cornerstone that justifies the need for hospital admission and the initiation of intravenous dextrose or parenteral nutrition.
Rationale for incorrect answers
1. An elevated hemoglobin level is a common finding in hyperemesis gravidarum, but it is a marker of hemoconcentration rather than starvation. As the plasma volume decreases due to profound dehydration, the relative concentration of red blood cells increases. While this reflects the fluid volume status of the client, it does not provide information regarding the underlying metabolic pathways or the switch to ketosis.
3. Normal serum glucose levels are often maintained even in severe starvation states due to the body's highly efficient gluconeogenesis pathways. The liver can synthesize glucose from non-carbohydrate sources like amino acids and glycerol to protect fetal development and brain function. Therefore, a normal glucose reading does not rule out starvation, as the body may be maintaining that level by sacrificing maternal tissues.
4. A decreased white blood cell count, or leukopenia, is not a recognized feature of the pathophysiology of hyperemesis gravidarum. In fact, a client with severe dehydration and stress may actually exhibit a mild leukocytosis as a physiological response to systemic inflammation or hemoconcentration. A low count would be more suggestive of an immunological disorder or bone marrow suppression, which is unrelated to the emetic pathways.
Test-taking strategy
- Identify the Core Concept: The question specifically asks for a marker of starvation. Distinguish between "fluid loss" and "lack of food."
- Apply Biochemical Knowledge: Recall the sequence of energy use: Glucose → Glycogen → Fat. The byproduct of burning fat is ketones. This makes Choice 2 the most direct answer.
- Differentiate Findings: Choice 1 is about dehydration. Choice 3 is about homeostasis (staying "normal" despite stress). Choice 4 is about infection/immunity. By categorizing the options, you can see that only Choice 2 addresses the metabolic shift of malnutrition.
- Utilize Medical Terminology: Look for terms that indicate "breakdown" of body stores. Ketonuria is the clinical manifestation of lipolysis and ketosis, which are the hallmarks of starving tissues.
Take home points
- Ketonuria is the gold standard laboratory finding used to diagnose the starvation component of hyperemesis gravidarum.
- Glycogen depletion occurs rapidly in pregnancy due to the high metabolic demands of the growing fetus.
- Elevated hemoglobin and hematocrit should be interpreted as signs of dehydration and hemoconcentration, not nutritional status.
- Normal blood glucose levels do not exclude the possibility of severe maternal nutritional depletion.
A nurse is assessing laboratory findings in a client with severe hyperemesis gravidarum. Which abnormalities are commonly associated with this condition? Select all that apply
Explanation
Hyperemesis gravidarum induces a state of metabolic decompensation characterized by the exhaustion of glycogen stores and profound extracellular fluid volume deficit. Intractable vomiting results in the mechanical loss of hydrogen, chloride, and potassium ions, while starvation triggers lipolysis and the subsequent production of ketone bodies. These biochemical shifts lead to hypovolemic hemoconcentration and significant electrolyte derangements that threaten maternal and fetal stability.
Rationale for correct answers
1. When oral carbohydrate intake is insufficient to meet metabolic demands, the body enters a state of catabolism. The liver oxidizes fatty acids into acetoacetate and beta-hydroxybutyrate, which are excreted as ketonuria in the urine. This finding is a definitive diagnostic marker for the starvation and nutritional failure seen in severe hyperemesis, necessitating immediate fluid and caloric replacement.
2. Gastric secretions contain high concentrations of potassium, which are lost directly through persistent emesis. Furthermore, the resulting metabolic alkalosis causes a shift of potassium into the intracellular space in exchange for hydrogen ions, while secondary hyperaldosteronism increases renal potassium excretion. Hypokalemia is a dangerous complication that can lead to cardiac arrhythmias and muscular weakness if not corrected intravenously.
4. Profound vomiting leads to the loss of sodium-rich gastric and intestinal fluids, often exacerbated by the maternal intake of only plain water which further dilutes the extracellular space. Hyponatremia occurs as a result of both direct loss and the compensatory release of antidiuretic hormone, which causes the kidneys to retain water disproportionately to sodium. This electrolyte shift can lead to cerebral edema or neurological irritability in extreme cases.
5. Severe dehydration leads to a reduction in total plasma volume, causing the cellular components of the blood to become more concentrated. This results in elevated hemoglobin and hematocrit levels, a phenomenon known as hemoconcentration. These values do not reflect an actual increase in red cell mass but rather the severity of the fluid volume deficit and the degree of intravascular depletion.
Rationale for incorrect answers
3. Hyperglycemia is not a typical finding in hyperemesis gravidarum; rather, these clients are at a much higher risk for hypoglycemia. Because they cannot maintain oral intake, their blood glucose levels drop once hepatic glycogen is depleted. Insulin resistance associated with later pregnancy (gestational diabetes) is not a feature of the first-trimester emetic response, where the primary risk is a lack of glucose for cellular energy.
Test-taking strategy
- Identify the Physiological State: Recognize that hyperemesis is a state of "loss" (vomiting) and "starvation" (no intake).
- Apply Electrolyte Knowledge: Remember that vomiting causes the loss of acid and electrolytes. This confirms Choice 2 (Hypokalemia) and Choice 4 (Hyponatremia).
- Evaluate Fluid Status: Dehydration means less water in the blood. This makes the solids (hemoglobin) look higher. This validates Choice 5.
- Connect Starvation to Lab Markers: Recall that the body burns fat when it has no food. The byproduct is ketones. This validates Choice 1.
- Eliminate Inconsistent Options: Choice 3 (Hyperglycemia) describes a state of "excess sugar," which is the opposite of what happens in a starving, vomiting patient.
Take home points
- Ketonuria and elevated specific gravity are the primary urinary indicators of starvation and dehydration.
- Hypokalemia and hyponatremia are the most common electrolyte disturbances resulting from the loss of gastric contents and renal compensation.
- Hemoconcentration (elevated Hgb/Hct) serves as an objective measure of the degree of intravascular fluid volume deficit.
- Metabolic alkalosis usually precedes ketotic acidosis in the early stages of severe hyperemesis due to the loss of hydrochloric acid.
A nurse is reviewing diagnostic orders for a client at 8 weeks gestation with severe vomiting. Which diagnostic test is essential to exclude a condition associated with markedly elevated human chorionic gonadotropin levels?
Explanation
Hyperemesis gravidarum is a clinical diagnosis of exclusion, requiring the systematic elimination of trophoblastic pathologies that mimic severe emesis. Gestational trophoblastic disease, specifically a hydatidiform mole, involves the abnormal proliferation of placental tissue, resulting in supraphysiologic concentrations of human chorionic gonadotropin. These extreme hormonal peaks excessively stimulate the medullary emetic centers and the chemoreceptor trigger zone, necessitating immediate differential screening via imaging.
Rationale for correct answer
3. An ultrasound examination is the definitive modality required to visualize the uterine cavity and differentiate between a viable gestation and pathological tissue. In cases of molar pregnancy, the sonogram reveals a pathognomonic snowstorm appearance, characterized by a complex echogenic mass with multiple small cystic spaces representing hydropic villi. This visualization is critical because the hCG levels produced by a mole can be significantly higher than those of a singleton pregnancy, directly driving the severity of the vomiting.
Rationale for incorrect answers
1. A complete blood count is utilized to assess for hemoconcentration and infection, but it provides no information regarding the etiology of hormonal surges. While an elevated hematocrit can confirm the severity of dehydration, it cannot visualize the contents of the uterus to rule out abnormal placental growth. It is a supportive test for fluid management rather than a primary diagnostic tool for trophoblastic disease.
2. Liver function tests are often indicated in severe hyperemesis to monitor for transaminitis, which may occur due to starvation or hepatic stress. While these enzymes can be mildly elevated in approximately 50% of hospitalized cases, they are non-specific findings that do not identify the source of the emetic stimulus. Elevated AST or ALT levels do not help in ruling out a molar pregnancy or other gestational abnormalities.
4. An electrocardiogram is primarily used to monitor for cardiac arrhythmias secondary to electrolyte imbalances like hypokalemia. While essential for managing the systemic complications of persistent vomiting, it lacks the diagnostic capability to identify the hormonal or anatomical cause of the hyperemesis. It assesses the cardiovascular impact of the disease rather than the underlying pregnancy-related pathology.
Test-taking strategy
- Identify the Pathological Trigger: The question highlights the need to exclude a condition associated with "markedly elevated hCG." In obstetrics, the primary "high-hCG" emergency in the first trimester is a molar pregnancy.
- Match Tool to Anatomy: To rule out a molar pregnancy, the nurse must look for a tool that provides visual evidence of the uterine contents. Ultrasound is the only choice that offers anatomical visualization.
- Differentiate Cause vs. Effect: Choices 1, 2, and 4 measure the effects of vomiting (dehydration, liver stress, and heart rhythm). Only Choice 3 investigates the cause of the vomiting (the pregnancy itself).
- Select Confirmatory Evidence: Recall that a molar pregnancy is often suspected when the uterus is larger than expected and hCG is pathologically high; an ultrasound is the gold standard to confirm this suspicion.
Take home points
- Ultrasound is the essential diagnostic test to differentiate hyperemesis gravidarum from gestational trophoblastic disease.
- A molar pregnancy must be excluded in any patient with severe early-onset vomiting and excessively high hCG levels.
- The "snowstorm" pattern on ultrasound is the diagnostic hallmark of a complete hydatidiform mole.
- Prompt diagnosis of molar pregnancy is vital to prevent secondary complications such as choriocarcinoma or early-onset preeclampsia.
A nurse is monitoring renal and hydration status in a client with hyperemesis gravidarum. Which findings indicate severe dehydration? Select all that apply
Explanation
Hyperemesis gravidarum produces a state of profound intravascular volume contraction due to the persistent loss of gastric secretions. This hypovolemia triggers a cascade of compensatory responses, including the activation of the renin-angiotensin-aldosterone system and the release of antidiuretic hormone to maximize water conservation. When these mechanisms are overwhelmed, the resulting hemoconcentration and reduced renal perfusion lead to significant biochemical shifts and pre-renal azotemia.
Rationale for correct answers
1. As the plasma volume decreases due to severe fluid loss, the cellular components of the blood become disproportionately concentrated. An elevated hematocrit is a classic sign of this hemoconcentration, where the percentage of red blood cells appears higher because the total liquid volume of the blood has diminished. This finding serves as an objective measure of the severity of the client's dehydration and the need for isotonic fluid replacement.
2. Severe dehydration leads to decreased renal perfusion and a lower glomerular filtration rate. This results in elevated blood urea nitrogen and creatinine levels, a condition known as pre-renal azotemia. These laboratory markers indicate that the kidneys are struggling to filter metabolic waste products due to the lack of adequate blood flow and pressure within the renal vasculature.
4. The presence of ketones in the urine is a direct consequence of the starvation state induced by intractable vomiting. When the body cannot obtain energy from oral glucose, it metabolizes adipose tissue, producing acidic ketone bodies. While primarily a marker of nutritional status, ketonuria in this context is almost always accompanied by severe dehydration and a metabolic shift toward catabolism.
Rationale for incorrect answers
3. Decreased urine specific gravity (e.g., 1.005) is a finding associated with dilute urine and fluid overload or diabetes insipidus. In a client with severe hyperemesis, the nurse would expect an increased specific gravity (≥ 1.030). This occurs because the kidneys are actively reabsorbing as much water as possible to compensate for fluid loss, resulting in highly concentrated urine.
5. Normal serum sodium is not an indicator of severe dehydration; instead, the nurse would expect to see abnormal sodium levels. Depending on the ratio of water to solute loss, the client may exhibit hyponatremia from direct loss of gastric salts or hypernatremia due to profound water depletion. A normal value suggests that the body's homeostatic mechanisms are still maintaining balance, which is inconsistent with the definition of severe dehydration.
Test-taking strategy
- Identify the Physiological Theme: Group the choices into markers of "concentration" versus markers of "dilution." Dehydration always shifts the body toward concentration.
- Connect Volume to Lab Values: Recall that when the liquid part of blood (plasma) disappears, the solids (Hct, BUN, Creatinine) stay behind and appear elevated. This validates Choice 1 and Choice 2.
- Analyze Renal Compensation: Remember that a dehydrated kidney holds onto water. This makes urine very thick and heavy, resulting in a high specific gravity. This allows you to eliminate Choice 3.
- Correlate Starvation with Dehydration: In the specific context of hyperemesis, ketones and dehydration go hand-in-hand because both result from the inability to tolerate oral intake. This confirms Choice 4.
Take home points
- Elevated hematocrit and hemoglobin are primary indicators of hemoconcentration due to intravascular fluid loss.
- Pre-renal azotemia, evidenced by rising BUN and creatinine, reflects decreased renal perfusion during severe hypovolemic states.
- Urine specific gravity increases significantly (> 1.025) as a compensatory mechanism to prevent further water loss.
- Ketonuria serves as a marker for the metabolic transition to fat catabolism caused by prolonged caloric deprivation.
Practice Exercise 5
A nurse is caring for a client with untreated hyperemesis gravidarum. Which of the following complications is most strongly associated with prolonged thiamine deficiency?
Explanation
Hyperemesis gravidarum induces a critical state of micronutrient depletion when persistent emesis prevents the absorption of water-soluble vitamins. Thiamine, also known as Vitamin B1, is a mandatory cofactor for pyruvate dehydrogenase and alpha-ketoglutarate dehydrogenase within the Kreb's cycle. Without this coenzyme, the brain cannot metabolize glucose, leading to acute adenosine triphosphate failure and subsequent neuronal death in the brainstem and diencephalon.
Rationale for correct answer
2. Wernicke's encephalopathy is the most severe neurological complication of prolonged thiamine deficiency in hyperemesis. The condition is characterized by a classic clinical triad of global confusion, ataxia, and ophthalmoplegia (particularly nystagmus or sixth nerve palsy). Because pregnancy increases the metabolic demand for thiamine, a client with intractable vomiting can exhaust their limited hepatic stores within 2 to 3 weeks, leading to irreversible hemorrhagic lesions in the mammillary bodies.
Rationale for incorrect answers
1. Gestational diabetes is a disorder of carbohydrate metabolism caused by placental lactogen and maternal insulin resistance. While it involves glucose pathways, it is not triggered by a vitamin deficiency or persistent vomiting. In fact, severe hyperemesis is more likely to cause hypoglycemia due to starvation rather than the hyperglycemia characteristic of gestational diabetes.
3. Placenta previa is an anatomical abnormality where the placenta implants over or near the internal os of the cervix. This condition is primarily related to uterine scarring or placental surface area and is not influenced by the maternal nutritional or vitamin status. There is no known pathophysiological link between thiamine levels and the site of placental implantation in the uterine wall.
4. Preeclampsia is a multisystem hypertensive disorder characterized by endothelial dysfunction and vasospasm. While severe hyperemesis can cause renal stress, it does not cause the specific glomerular endotheliosis or systemic hypertension seen in preeclampsia. Thiamine deficiency affects the central nervous system and metabolic cycles rather than the vascular resistance and proteinuria associated with hypertensive disorders of pregnancy.
Test-taking strategy
- Link Nutrient to Disease: Establish a firm mental connection between Thiamine (B1) and Wernicke's encephalopathy. This is a high-yield medical association across many specialties, including obstetrics and addiction medicine.
- Identify the Body System: The question mentions a deficiency that causes "neurological changes" in previous contexts. Only Choice 2 is a neurological condition, whereas the others are endocrine, anatomical, or vascular.
- Evaluate Iatrogenic Risks: Recall the nursing priority that "thiamine must precede glucose." Giving intravenous dextrose to a thiamine-deficient patient will trigger Wernicke's by rapidly consuming the last remaining B1 molecules for glucose metabolism.
- Rule out Unrelated Pathologies: Use the process of elimination by recognizing that Choice 1, 3, and 4 are primary obstetric complications with distinct etiologies (hormonal, structural, and vascular) that do not involve micronutrient depletion.
Take home points
- Wernicke's encephalopathy is a medical emergency in hyperemesis gravidarum caused by severe Vitamin B1 (thiamine) deficiency.
- The clinical triad of confusion, ataxia, and ocular abnormalities requires immediate high-dose intravenous thiamine replacement.
- Nurses must never administer glucose-containing IV fluids to a malnourished hyperemesis patient until thiamine has been provided to prevent precipitating acute encephalopathy.
- If untreated, Wernicke's can progress to Korsakoff syndrome, which involves permanent memory loss and confabulation.
A nurse assesses a client with hyperemesis gravidarum who presents with tachycardia and hypotension. Which of the following is the most likely underlying cause?
Explanation
Hyperemesis gravidarum induces a profound intracellular and extracellular fluid volume deficit due to the persistent loss of gastric secretions. This hypovolemia triggers a decrease in venous return and stroke volume, necessitating a compensatory increase in heart rate via the baroreceptor reflex. Clinically, the body attempts to maintain mean arterial pressure despite a significantly contracted intravascular compartment, leading to the classic presentation of orthostatic instability.
Rationale for correct answer
2. Tachycardia and hypotension are the primary hemodynamic indicators of hypovolemia resulting from severe dehydration. When the circulating blood volume drops, the sympathetic nervous system triggers a compensatory increase in heart rate to maintain cardiac output. If the fluid loss is not replaced intravenously, the body’s compensatory mechanisms eventually fail, resulting in a drop in blood pressure and reduced tissue perfusion.
Rationale for incorrect answers
1. Transient hyperthyroidism is common in hyperemesis due to human chorionic gonadotropin (hCG) cross-reacting with thyroid-stimulating hormone receptors. While elevated thyroxine (T4) can cause a high heart rate, it is typically associated with normal or elevated blood pressure rather than hypotension. This condition reflects a hypermetabolic state but does not primarily cause the acute volume depletion that leads to low blood pressure in these patients.
3. Hypoglycemia occurs when hepatic glycogen stores are exhausted due to prolonged starvation and inadequate carbohydrate intake. While low blood sugar can cause a mild sympathetic surge resulting in tachycardia and diaphoresis, it does not typically cause a significant drop in blood pressure. Hypotension in the context of persistent vomiting is almost exclusively a result of fluid loss rather than the metabolic concentration of glucose.
4. An anxiety-related sympathetic response can trigger a rapid heart rate and tachypnea due to the "fight or flight" mechanism. However, this physiological response typically causes an increase in blood pressure (hypertension) rather than a decrease. Finding both tachycardia and hypotension together strongly points toward an objective circulatory deficit rather than a purely psychological or emotional reaction to the illness.
Test-taking strategy
- Analyze the Vital Signs: Recognize that the combination of "up" (tachycardia) and "down" (hypotension) is the classic signature of shock or severe volume depletion.
- Apply the ABCs: Prioritize Circulation (Choice 2) over metabolic (Choice 3) or endocrine (Choice 1) issues when life-threatening vital sign changes are present.
- Differentiate Sympathetic Drivers: Distinguish between causes of tachycardia. While anxiety (Choice 4) and hyperthyroidism (Choice 1) raise the heart rate, they do not satisfy the hypotension part of the clinical picture.
- Identify the Physiological Demand: Link the "vomiting" in the stem directly to "loss of volume." Since volume is required for pressure, Choice 2 is the only answer that explains both clinical findings.
Take home points
- Tachycardia and hypotension are the hallmark signs of significant intravascular volume depletion in hyperemesis gravidarum.
- Compensatory tachycardia occurs as the heart attempts to maintain cardiac output (CO = HR x SV) in the face of a low stroke volume.
- Orthostatic blood pressure changes are a sensitive early indicator of dehydration before resting hypotension develops.
- Immediate treatment involves the administration of isotonic IV fluids (0.9% Normal Saline or Lactated Ringer's) to restore circulating volume.
A nurse is monitoring a client with severe hyperemesis gravidarum. Which of the following are maternal complications associated with repeated vomiting? Select all that apply
Explanation
Hyperemesis gravidarum induces severe mechanical and metabolic stress through persistent, forceful emesis. The repeated expulsion of gastric contents leads to mucosal trauma and a profound loss of hydrogen and chloride ions, resulting in a systemic contraction alkalosis. Furthermore, the exhaustion of water-soluble vitamin stores, specifically thiamine, compromises cerebral glucose metabolism, leading to life-threatening neurological degradation.
Rationale for correct answers
1. Repeated, forceful retching creates a massive pressure gradient across the gastroesophageal junction, which can lead to esophageal tears, specifically Mallory-Weiss tears. These longitudinal mucosal lacerations manifest as hematemesis (bright red blood in vomitus) and can cause significant maternal hemorrhage. The mechanical trauma is a direct result of the high-velocity intra-abdominal pressure changes that occur during intractable vomiting episodes.
2. Prolonged vomiting prevents the absorption of Vitamin B1, leading to Wernicke's encephalopathy, a medical emergency characterized by ataxia, confusion, and ocular abnormalities. Thiamine is an essential cofactor for metabolic pathways in the brain; its depletion causes neuronal death and hemorrhagic lesions in the mammillary bodies. If not corrected with immediate thiamine supplementation, this can progress to permanent memory loss or death.
4. Intractable vomiting causes the excessive loss of hydrochloric acid from the stomach, which is the primary driver of metabolic alkalosis. As hydrogen and chloride ions are depleted, the serum bicarbonate level rises to compensate, shifting the arterial pH above 7.45. This biochemical shift is often exacerbated by hypokalemia, as the kidneys attempt to conserve hydrogen at the expense of potassium excretion.
Rationale for incorrect answers
3. Gestational diabetes mellitus is a condition of insulin resistance and glucose intolerance that typically develops in the second or third trimester. While hyperemesis causes metabolic stress, it does not trigger the pancreatic or hormonal dysfunction required for a diabetes diagnosis. In fact, severe vomiting is more likely to cause hypoglycemia due to the total absence of carbohydrate intake and glycogen depletion.
5. Placental abruption is the premature separation of the placenta from the uterine wall, usually caused by hypertension, trauma, or cocaine use. While severe vomiting involves intense abdominal muscle contraction, it is not a recognized pathophysiological cause of the vascular disruption that leads to abruption. Abruption is a vasculopathy of the retroplacental space rather than a complication of gastrointestinal or metabolic distress.
Test-taking strategy
- Categorize the Complications: Group the answers into "Mechanical" (Choice 1), "Neurological/Nutritional" (Choice 2), and "Acid-Base" (Choice 4). All three are directly linked to the act of vomiting.
- Apply the "Loss of Acid" Rule: Recall that losing stomach acid (HCl) always leads to alkalosis. This makes Choice 4 a mandatory selection for any vomiting-related question.
- Identify Micronutrient Risks: Associate "long-term vomiting" with "vitamin deficiency." Thiamine (B1) is the most critical deficiency in this context, making Choice 2 correct.
- Evaluate Trimester Timing: Hyperemesis is a first-trimester disease. Choice 3 and Choice 5 are typically complications of late pregnancy, allowing you to rule them out based on the chronological progression of gestation.
Take home points
- Mallory-Weiss tears are mechanical complications of forceful retching that can lead to upper gastrointestinal bleeding and hematemesis.
- Wernicke's encephalopathy is a preventable but fatal complication of thiamine deficiency that requires IV thiamine before any dextrose administration.
- Metabolic alkalosis (hypochloremic) is the hallmark acid-base disturbance caused by the direct loss of gastric hydrochloric acid.
- Starvation ketosis and hypoglycemia are the primary metabolic risks, distinct from the hyperglycemia seen in gestational diabetes.
A nurse is monitoring fetal outcomes in a client hospitalized for hyperemesis gravidarum. Which fetal complication is most directly related to prolonged maternal malnutrition?
Explanation
Hyperemesis gravidarum induces a state of chronic gestational starvation that compromises the maternal-fetal nutrient transfer. When maternal caloric intake is insufficient to support the metabolic demands of pregnancy, the body prioritizes essential maternal functions, leading to placental insufficiency. This nutritional deficit results in a failure of the fetus to achieve its genetically determined growth potential, primarily due to a lack of amino acids and glucose required for tissue accretion.
Rationale for correct answer
2. Intrauterine growth restriction is the primary fetal complication resulting from the persistent maternal catabolic state seen in severe hyperemesis. Prolonged malnutrition leads to a reduction in fetal insulin-like growth factor and chronic hypovolemia, which decreases uterine artery blood flow. This leads to a fetus that is small for gestational age, as the nutrient supply is inadequate to support normal cellular hyperplasia and hypertrophy during critical developmental windows.
Rationale for incorrect answers
1. Macrosomia refers to a birth weight exceeding 4,000 to 4,500 grams and is typically associated with maternal hyperglycemia and gestational diabetes. In hyperemesis gravidarum, the mother is in a state of hypoglycemia and starvation, which is the physiological opposite of the environment required for fetal overgrowth. There is no biological mechanism by which maternal caloric deprivation would lead to excessive fetal weight gain.
3. Polyhydramnios is an excess of amniotic fluid that often results from fetal gastrointestinal obstructions or maternal diabetes. Hyperemesis is more likely to be associated with oligohydramnios, or low amniotic fluid, due to maternal dehydration and reduced fetal renal perfusion. The lack of maternal fluid volume means there is less fluid available to be processed into amniotic fluid through the fetal-placental circulation.
4. Congenital heart defects are structural abnormalities that typically occur during the first 8 weeks of organogenesis. While severe nutritional deficiencies like folate can increase the risk of neural tube defects, heart defects are primarily linked to genetics, teratogens, or pre-gestational diabetes. Hyperemesis usually peaks after the most critical period of cardiac development has already passed or reached a stage where malnutrition would stunt growth rather than cause a structural malformation.
Test-taking strategy
- Identify the Physiological Theme: Match "malnutrition" with "lack of growth." Only Choice 2 describes a condition of inadequate size or growth.
- Apply the "Rule of Opposites": Recognize that Choice 1 (macrosomia) and Choice 3 (polyhydramnios) are associated with "excess" (too much sugar, too much fluid), which contradicts the "deficit" state of hyperemesis.
- Rule out Chronological Errors: Organogenesis of the heart (Choice 4) is often nearly complete by the time hyperemesis becomes severe enough to cause systemic malnutrition.
- Focus on Nutrient Flow: Remember that a starving mother cannot provide the building blocks for a large baby. This logic directly points to Choice 2 as the only reasonable outcome for a nutrient-deprived fetus.
Take home points
- Intrauterine growth restriction (IUGR) is the most common fetal consequence of severe, untreated maternal malnutrition.
- Fetal outcomes in hyperemesis are generally favorable if the mother receives aggressive nutritional and fluid support.
- Low birth weight and preterm delivery risks increase significantly if maternal weight gain remains below 7 kg (15 lbs) total.
- Chronic maternal dehydration can lead to reduced amniotic fluid levels, necessitating serial ultrasound monitoring.
A nurse is assessing a client with hyperemesis gravidarum for signs of severe dehydration. Which findings indicate this complication? Select all that apply
Explanation
Hyperemesis gravidarum induces a profound intracellular and extracellular fluid volume deficit due to the continuous loss of gastric secretions. This state of hypovolemia triggers compensatory mechanisms such as the activation of the renin-angiotensin-aldosterone system and the release of antidiuretic hormone. Clinical manifestations result from decreased hydrostatic pressure and impaired tissue perfusion, necessitating aggressive isotonic fluid resuscitation.
Rationale for correct answers
1. Persistent vomiting prevents adequate oral rehydration, leading to a systemic depletion of total body water. As interstitial fluid is drawn into the vascular compartment to maintain pressure, the mucous membranes become parched and lose their natural lubrication. This is a primary physical indicator of a dehydration state where the body can no longer maintain surface moisture.
2. Fluid loss from the interstitial spaces around the orbit causes a reduction in intraocular pressure and a loss of periorbital fat volume. This results in the characteristic clinical appearance of sunken eyes, which is a sign of advanced fluid volume deficit. It reflects a significant shift in extracellular fluid that occurs when compensatory oral intake is impossible due to intractable emesis.
4. In response to a decreased stroke volume caused by hypovolemia, the baroreceptors trigger an increase in sympathetic nervous system activity. This results in tachycardia, as the heart attempts to maintain a constant cardiac output despite a lower circulating blood volume. A heart rate exceeding 100 beats per minute in a resting pregnant client is a critical sign of cardiovascular compensation for dehydration.
Rationale for incorrect answers
3. A urine specific gravity of 1.010 is within the normal range (1.005 to 1.030) and indicates that the kidneys are excreting relatively dilute urine. In severe dehydration, the nurse expects a high specific gravity, typically ≥ 1.025, as the kidneys maximize water reabsorption. A reading of 1.010 suggests that the renal homeostatic mechanisms are not currently responding to a state of profound fluid volume deficit.
5. Normal skin turgor is a finding associated with adequate hydration and elastic tissue integrity. In a client with severe hyperemesis, the nurse would instead expect to find poor turgor, demonstrated by the skin "tenting" when pinched. This occurs because the dermal layers lack the interstitial fluid necessary to snap back to their original position immediately after being manipulated.
Test-taking strategy
- Identify the Physiological State: The question asks for signs of dehydration. Group the symptoms into those that show "loss" versus those that show "excess."
- Apply the "Dryness" Principle: Dehydration is fundamentally a lack of water. Choice 1 (dry membranes) and Choice 2 (sunken features) fit the physical description of a body lacking fluid.
- Evaluate Hemodynamics: Recall that when volume (preload) goes down, the heart rate must go up to compensate. This confirms Choice 4 as a classic sign of fluid deficit.
- Rule out Normal/Positive Findings: Choice 3 (normal gravity) and Choice 5 (normal turgor) are signs of "wellness" or "adequate hydration." In the context of "severe" vomiting, these findings are physiologically impossible and should be eliminated.
Take home points
- Tachycardia and orthostatic hypotension are early cardiovascular indicators of significant volume depletion in hyperemesis.
- Poor skin turgor and sunken eyes represent a loss of interstitial fluid and late-stage dehydration.
- Oliguria occurs as the kidneys maximize water reabsorption in response to elevated antidiuretic hormone levels.
- Clinical assessment of dehydration must be correlated with laboratory findings such as elevated hematocrit and high urine specific gravity.
Practice Exercise 6
A nurse is caring for a client hospitalized with severe hyperemesis gravidarum. Which of the following is the most immediate nursing priority?
Explanation
Hyperemesis gravidarum induces an acute hemodynamic crisis characterized by profound intravascular volume depletion and metabolic derangement. This state of hypovolemia compromises maternal cardiac output and uterine perfusion, necessitating the rapid restoration of the circulating compartment. Immediate isotonic resuscitation is the clinical priority to prevent acute kidney injury and cardiovascular collapse, preceding all other pharmacological or nutritional interventions.
Rationale for correct answer
2. Initiating intravenous fluid therapy is the most immediate priority to stabilize the client’s cardiovascular status and correct profound dehydration. Severe vomiting causes a massive loss of extracellular fluid, leading to hemoconcentration and electrolyte instability that can trigger cardiac arrhythmias. Intravenous access allows for the rapid administration of crystalloids, which are essential for restoring renal perfusion and reversing the starvation-induced ketosis associated with hyperemesis.
Rationale for incorrect answers
1. Administering pyridoxine (Vitamin B6) orally is a common first-line treatment for nausea, but it is inappropriate for a client with severe hyperemesis. Oral medications are unlikely to be absorbed in a patient experiencing intractable vomiting and may actually trigger further emetic episodes. In a hospitalized client with evidence of systemic dehydration, the parenteral route must be established before oral vitamins can be considered therapeutic.
3. Providing emotional reassurance is an important component of holistic nursing care, but it does not address the life-threatening physiological imbalances present. Psychological support is a secondary intervention that should be implemented only after the client is hemodynamically stable and out of acute physical distress. In the hierarchy of needs, the correction of fluid and electrolyte deficits takes precedence over psychosocial comfort in an emergency setting.
4. Offering small, frequent meals is the standard recommendation for mild morning sickness but is contraindicated in the acute phase of hyperemesis. A client with severe vomiting requires a period of gut rest (NPO status) to minimize stimulation of the emetic centers. Reintroducing oral intake before the patient has been rehydrated and stabilized intravenously often exacerbates the metabolic crisis and delays clinical recovery.
Test-taking strategy
- Apply the ABCs: Prioritize Circulation. Among the choices, only Choice 2 directly addresses the circulatory deficit (hypovolemia) caused by the disease.
- Determine the Route of Choice: For a patient who is "severely" vomiting, any oral intervention (Choice 1 and Choice 4) is likely to fail and is therefore not a priority.
- Use Maslow's Hierarchy: Address physiological needs (fluid balance) before safety/social needs (emotional reassurance). This quickly eliminates Choice 3.
- Identify the Acute vs. Chronic Phase: Recognize that "hospitalized" and "severe" imply an acute phase. Interventions that work for chronic/mild nausea do not apply to an emergency resuscitation scenario.
Take home points
- Intravenous fluid resuscitation with isotonic crystalloids is the primary intervention for severe hyperemesis to restore intravascular volume.
- Gut rest (NPO status) is initially required to allow the gastric mucosa to recover and to prevent further emetic triggers.
- Thiamine must be administered during rehydration to prevent the development of Wernicke's encephalopathy.
- Success of fluid therapy is measured by improved urine output (> 30 mL/hr), decreased specific gravity, and resolution of tachycardia.
A nurse prepares to administer dextrose-containing IV fluids to a client with hyperemesis gravidarum. Which of the following actions is most critical to prevent neurologic complications?
Explanation
Hyperemesis gravidarum induces a critical state of micronutrient depletion where glycogen exhaustion triggers metabolic shifts. Thiamine acts as a mandatory coenzyme for the pyruvate dehydrogenase complex within the aerobic glucose oxidation pathway. Introduction of high-load carbohydrate substrates without sufficient B1 stores precipitates acute neuronal oxidative stress and ATP failure.
Rationale for correct answer
3. Administering thiamine before dextrose is the most critical action to prevent the precipitation of acute Wernicke encephalopathy. Thiamine is a vital cofactor for metabolic enzymes that process carbohydrates into cellular energy. If a concentrated glucose load is provided to a depleted patient, the remaining B1 is rapidly consumed, leading to catastrophic neurotoxicity and hemorrhagic lesions in the brain.
Rationale for incorrect answers
1. Assessing blood glucose levels is a standard nursing assessment but does not prevent the specific neurological damage caused by thiamine deficiency. While the nurse needs to identify hypoglycemia, this data point does not mitigate the risk of encephalopathy if glucose is infused alone. The underlying metabolic requirement for thiamine exists regardless of the baseline serum glucose concentration at the time of admission.
2. Administering ondansetron first addresses the symptomatic emesis but has no pharmacological impact on the metabolic or neurological status of the client. This serotonin antagonist works on the chemoreceptor trigger zone to reduce nausea. It is a secondary priority compared to the prevention of permanent central nervous system damage caused by iatrogenic thiamine depletion during intravenous resuscitation.
4. Monitoring urine ketones provides objective evidence of fat catabolism and the depth of the starvation state. While this allows the nurse to track the severity of the disease, it is an assessment rather than a preventative intervention. Knowing that ketonuria is present confirms the patient is at high risk, which reinforces the urgent necessity of providing thiamine.
Test-taking strategy
- Identify the Critical Risk: The question focuses on "neurologic complications" in a malnourished patient. In nursing exams, this phrase is almost always a reference to thiamine deficiency and Wernicke encephalopathy.
- Recall the Order of Operations: Memorize the rule that "B1 comes before D5." Never give dextrose (glucose) to a patient with chronic vomiting or starvation until thiamine has been administered.
- Differentiate Priorities: Rule out Choice 2 (ondansetron) because it treats symptoms, not the life-threatening metabolic underlying cause.
- Eliminate Assessments: Choice 1 and Choice 4 are data-gathering steps. When a question asks for a "most critical action" to prevent a specific complication, look for an intervention that stops the pathology.
- Analyze the Iatrogenic Trigger: Recognize that providing the "cure" (dextrose) can actually cause the "harm" (brain damage) if the metabolic cofactor is missing.
Take home points
- Thiamine (Vitamin B1) must always precede or accompany the first dose of dextrose-containing IV fluids in hyperemesis.
- Iatrogenic Wernicke encephalopathy is caused by the rapid consumption of residual thiamine during a sudden glucose load.
- The classic triad of Wernicke includes global confusion, ataxia, and ocular abnormalities like nystagmus.
- Failure to provide thiamine can result in Korsakoff syndrome, which involves irreversible memory loss and confabulation.
A nurse is evaluating the effectiveness of fluid replacement therapy in a client with hyperemesis gravidarum. Which of the following findings indicate improvement? Select all that apply
Explanation
Hyperemesis gravidarum necessitates aggressive isotonic resuscitation to reverse the systemic effects of profound volume depletion. Effective therapy restores the intravascular compartment, thereby increasing renal perfusion and suppressing the hormonal triggers for water conservation. As the body transitions from a catabolic state back to aerobic metabolism, biochemical markers of starvation and dehydration normalize, reflecting a restoration of hemodynamic stability and cellular hydration.
Rationale for correct answers
1. A urine output of 35 mL/hr indicates that the kidneys are receiving adequate perfusion and that the circulating volume has been sufficiently restored. In a dehydrated state, the body produces oliguria (< 30 mL/hr) as a compensatory mechanism to preserve fluid. Reaching this threshold confirms that the glomerular filtration rate has normalized and the immediate threat of pre-renal acute kidney injury has subsided.
2. The resolution of ketonuria is a definitive sign that the client has moved out of a starvation state. Once intravenous fluids provide sufficient glucose or allow for the resumption of oral intake, the body ceases the lipolysis of adipose tissue. The disappearance of ketones in the urine proves that metabolic homeostasis is being restored and that the catabolic breakdown of maternal stores has halted.
4. Stable blood pressure without orthostatic changes indicates that the autonomic nervous system is no longer struggling to compensate for a low stroke volume. The absence of a drop in pressure upon standing suggests that the intravascular volume is full enough to maintain cerebral perfusion against gravity. This is a critical indicator of successful volume expansion and cardiovascular stabilization.
Rationale for incorrect answers
3. Decreased skin turgor is a classic sign of dehydration, evidenced by "tenting" of the skin when pinched. An improvement in hydration status would manifest as elastic skin turgor that snaps back immediately to its original position. Finding decreased turgor implies that the interstitial fluid levels remain depleted and that the replacement therapy has not yet reached a therapeutic endpoint.
5. Persistent tachycardia is a sign that the heart is still working harder to compensate for a perceived or actual lack of volume. As rehydration succeeds, the resting heart rate should decrease toward the client's baseline as the stroke volume increases. Continued tachycardia suggests either ongoing hypovolemia, pain, or a secondary metabolic issue like transient gestational hyperthyroidism that has not yet resolved.
Test-taking strategy
- Identify the Goal: The question asks for signs of "improvement." Categorize each choice as either a "sign of health" or a "sign of disease."
- Use Numeric Benchmarks: Recall that the minimum safe urine output for an adult is 30 mL/hr. Since 35 mL/hr (Choice 1) exceeds this, it is a positive sign.
- Analyze Metabolic Shifts: Understand that ketonuria is a marker of failure (starvation). Therefore, its "resolution" (Choice 2) is a marker of success.
- Evaluate Vital Sign Trends: Improvement in volume status results in "stable" or "decreasing" vitals. Choice 4 (stable pressure) fits this trend, while Choice 5 (persistent tachycardia) indicates a lack of progress.
- Watch for Opposites: Choice 3 (decreased turgor) is the opposite of what you want. Always look for "brisk" or "normal" turgor as the goal.
Take home points
- Successful rehydration is evidenced by a urine output ≥ 30 mL/hr and a decrease in urine specific gravity.
- The absence of ketones in the urine indicates that the patient has exited the catabolic state of starvation.
- Hemodynamic stability is confirmed when orthostatic hypotension and resting tachycardia resolve.
- Normalization of skin turgor and moist mucous membranes are the primary physical indicators of restored interstitial fluid.
A nurse provides dietary teaching to a client diagnosed with hyperemesis gravidarum. Which of the following recommendations is most appropriate?
Explanation
Hyperemesis gravidarum necessitates a nutritional rehabilitation strategy focused on minimizing gastric distension and optimizing glycemic stability. The transition from a catabolic state requires small-volume, high-density intake to prevent the activation of the medullary emetic centers. High-protein substrates facilitate slower gastric emptying and provide sustained amino acid availability, while limiting adipose tissue mobilization.
Rationale for correct answer
3. Eating small, frequent meals high in protein is the most effective dietary intervention to stabilize blood glucose and reduce nausea. High-protein foods may decrease gastric dysrhythmia and provide better symptomatic relief than high-carbohydrate alternatives in some gestations. Frequent small portions prevent gastric overdistension, which is a potent trigger for the mechanical stretch receptors that initiate the emetic reflex arc.
Rationale for incorrect answers
1. Consuming large meals three times daily is contraindicated because massive gastric volume increases intraluminal pressure and triggers immediate vomiting. Hyperemesis patients suffer from delayed gastric emptying, meaning large volumes lead to prolonged stasis and fermentation. This traditional eating pattern fails to provide the constant, steady stream of nutrients required to suppress starvation-induced ketosis and maintain metabolic neutrality.
2. Avoiding all solid foods is an inappropriate long-term strategy that can exacerbate malnutrition and lead to muscle wasting. While a brief period of gut rest may be required during acute resuscitation, the goal is a gradual return to solid intake. Relying solely on liquids often leads to inadequate caloric density and may actually worsen nausea due to rapid gastric transit and subsequent hypoglycemia.
4. Increasing intake of fatty foods is strongly discouraged because lipids significantly delay gastric emptying times and relax the lower esophageal sphincter. High-fat content increases the risk of acid reflux and creates a sensation of "fullness" that triggers the chemoreceptor trigger zone. Patients with hyperemesis typically exhibit a profound intolerance to the odors and textures of greasy or highly seasoned adipose-rich dietary items.
Test-taking strategy
- Identify the Goal: The objective is to find a dietary pattern that minimizes nausea while maximizing absorption.
- Apply Gastric Physiology: Recall that distension causes vomiting. This immediately rules out Choice 1 (large meals).
- Evaluate Macronutrients: Understand that fats (Choice 4) slow down the stomach too much, while proteins (Choice 3) provide stable energy. Protein is the "friend" of the nauseated stomach.
- Analyze Nutritional Sustainability: Total avoidance of solids (Choice 2) is a "starvation" move. In nursing, we always move toward rehabilitation and self-sufficiency unless the patient is in an acute crisis.
- Look for "Small and Frequent": This is a classic NCLEX-style "buzzword" for almost all gastrointestinal or metabolic conditions requiring dietary management, including GERD, dumping syndrome, and pregnancy-related emesis.
Take home points
- Small, frequent meals (every 2 to 3 hours) prevent the gastric distension and hypoglycemia that trigger vomiting episodes.
- High-protein, low-fat foods are better tolerated because they do not significantly delay gastric emptying or cause reflux.
- Dry carbohydrates (e.g., crackers) upon awakening can help stabilize blood sugar before rising from bed to prevent morning triggers.
- Separating liquid and solid intake (drinking between meals rather than with them) reduces the total volume in the stomach at any one time.
A nurse is caring for a client with refractory hyperemesis gravidarum. Which of the following interventions are appropriate? Select all that apply
Explanation
Refractory hyperemesis gravidarum represents a clinical failure of first-line antiemetics and fluid resuscitation, necessitating escalated therapeutic modalities. This condition involves persistent metabolic instability where maternal homeostasis cannot be maintained through oral or standard parenteral routes. Management focuses on providing adequate caloric density via bypass of the gastrointestinal tract and suppressing the systemic inflammatory or autoimmune triggers that potentially exacerbate the emetic response.
Rationale for correct answers
1. Initiating total parenteral nutrition (TPN) is indicated when a client remains unable to tolerate any oral or enteral intake for > 7 days or has lost > 10% of their body weight. TPN provides essential amino acids, lipids, and glucose directly into the central venous system, bypassing the stomach and preventing further maternal tissue catabolism. This intervention is a life-saving measure to ensure fetal growth and prevent severe maternal malnutrition in refractory cases.
2. Administering corticosteroids such as methylprednisolone is a recognized treatment for refractory hyperemesis that has not responded to standard antiemetics. These agents are strictly avoided before 10 weeks gestation due to a potential risk of fetal cleft lip and palate during organogenesis. After this period, they function by reducing systemic inflammation and potentially stabilizing the chemoreceptor trigger zone, though they are considered a last-resort pharmacological option.
4. Providing a low-stimulus environment is a non-pharmacological priority to prevent triggering the highly sensitized emetic center. Sensory inputs such as strong odors, bright lights, and loud noises can act as external afferent stimuli that precipitate a vomiting episode. By minimizing environmental stressors, the nurse reduces the physiological threshold for nausea, allowing the client’s nervous system to remain in a more stable, parasympathetic state.
Rationale for incorrect answers
3. Withholding thiamine supplementation is a dangerous and inappropriate action that increases the risk of permanent neurological damage. Any client with prolonged vomiting or starvation must receive B1 to prevent Wernicke's encephalopathy, especially before receiving glucose. Thiamine is a mandatory cofactor for cerebral energy metabolism, and its omission can lead to irreversible ataxia, confusion, and ophthalmoplegia.
5. Encouraging high-fat meals is contraindicated because lipids significantly delay gastric emptying and decrease lower esophageal sphincter tone. Fatty acids trigger the release of cholecystokinin, which further slows intestinal motility and exacerbates the sensation of bloating and nausea. For a client with refractory symptoms, a high-fat diet would likely precipitate immediate vomiting and worsen the underlying gastrointestinal dysrhythmia.
Test-taking strategy
- Identify the Phase of Care: The word "refractory" means standard treatments failed. Look for "advanced" interventions like TPN (Choice 1) and steroids (Choice 2).
- Evaluate Safety Contraindications: Recall the "Thiamine First" rule. This makes Choice 3 (withholding) an automatic error in any clinical scenario involving malnutrition.
- Match Diet to Pathology: Hyperemesis involves slow stomach emptying. Since fats slow it down more, Choice 5 is incorrect. High-protein, low-fat is the rule.
- Prioritize Environment: For a sensitized brain, "low-stimulus" (Choice 4) is a standard nursing intervention for neurological or severe metabolic irritability.
Take home points
- Total parenteral nutrition is reserved for clients with severe weight loss and failure of enteral management.
- Corticosteroids are only used after 10 weeks gestation to avoid the risk of fetal oral-facial clefting.
- Thiamine supplementation is mandatory in all refractory cases to prevent iatrogenic neurological complications.
- A quiet, odor-free environment is essential to minimize external triggers for the emetic reflex.
Practice Exercise 7
A nurse is assessing a client admitted with hyperemesis gravidarum. Which of the following findings most strongly indicates severe dehydration?
Explanation
Hyperemesis gravidarum induces an acute extracellular fluid volume deficit resulting from the intractable expulsion of gastric hydrochloric acid and water. This hypovolemia triggers a compensatory shift of interstitial fluid into the intravascular compartment, leading to observable mucosal desiccation and reduced intraocular pressure. Severe cases progress to hemoconcentration and impaired tissue perfusion as the homeostatic baroreceptor response becomes overwhelmed by continuous fluid loss.
Rationale for correct answer
3. The presence of sunken eyes and dry mucous membranes indicates a significant depletion of the interstitial fluid compartment. As total body water decreases, the periorbital fat pads lose hydration, and the salivary glands fail to maintain oral lubrication. These physical findings serve as definitive clinical evidence that the body has moved beyond simple thirst into a state of systemic fluid volume deficit.
Rationale for incorrect answers
1. A urine specific gravity of 1.010 falls within the normal physiological range of 1.005 to 1.030 and suggests adequate renal hydration. In a state of severe dehydration, the nurse expects a markedly elevated specific gravity, typically ≥ 1.030, as the kidneys maximize water reabsorption. This finding would actually contradict a diagnosis of severe dehydration, as it indicates the urine is not being concentrated to preserve volume.
2. Normal skin turgor is a sign of adequate fluid balance where the dermal and subcutaneous layers remain elastic and hydrated. In severe dehydration, the nurse would instead observe "tenting," where the skin fails to return to its original position after being pinched. Because this choice represents a healthy finding, it cannot be used to indicate a complication as severe as pathological dehydration in a hyperemesis client.
4. A heart rate of 72 beats per minute is a normal resting find for most adults and indicates cardiovascular stability. Severe dehydration typically triggers a compensatory tachycardia (HR > 100 bpm) as the sympathetic nervous system attempts to maintain cardiac output in the face of low stroke volume. The absence of an elevated pulse suggests that the circulating volume is currently sufficient to meet the body's metabolic and hemodynamic demands.
Test-taking strategy
- Identify the Physiological State: The question asks for signs of "severe dehydration." Categorize each option as either "normal" or "abnormal."
- Eliminate Normal Findings: Choice 1 (1.010 SG), Choice 2 (Normal turgor), and Choice 4 (72 bpm) are all within normal limits. In a question asking for a "severe" complication, correct answers must be pathological.
- Match Pathology to Condition: Only Choice 3 describes a pathological change. Sunken eyes and dry membranes are classic physical assessment findings for volume depletion.
- Apply Hemodynamic Principles: Recall that when volume goes down, the heart rate must go up. Since Choice 4 shows a normal heart rate, it is an incorrect indicator for a hypovolemic state.
- Correlate Renal Function: Remember that the kidney's job in dehydration is to save water, which makes urine "heavy" and "dark." A low or middle specific gravity like 1.010 proves the kidney is still wasting water, which doesn't happen in severe dehydration.
Take home points
- Sunken eyes and dry mucous membranes are late-stage physical indicators of significant interstitial fluid loss.
- Tachycardia and orthostatic hypotension are the primary cardiovascular compensations for a decreased intravascular volume.
- Laboratory confirmation of severe dehydration includes a urine specific gravity ≥ 1.030 and an elevated hematocrit due to hemoconcentration.
- Oliguria (urine output < 30 mL/hr) is a critical renal indicator that fluid resuscitation is urgently required to prevent acute kidney injury.
A nurse is monitoring a client with hyperemesis gravidarum receiving intravenous fluids. Which of the following findings indicate effective hydration? Select all that apply
Explanation
Hyperemesis gravidarum triggers a hypovolemic state that necessitates aggressive isotonic fluid resuscitation to restore the intravascular and interstitial compartments. Effective hydration therapy reverses the secondary hyperaldosteronism and suppresses antidiuretic hormone secretion, thereby allowing for normal renal filtration and electrolyte balance. As the body moves from a state of catabolism back to aerobic carbohydrate metabolism, biochemical markers of starvation and volume deficit normalize.
Rationale for correct answers
1. A urine output of 35 mL/hr is a primary indicator of improved renal perfusion and adequate circulating volume. In severe dehydration, the kidneys produce oliguria (less than 30 mL/hr) as they maximize water reabsorption to maintain blood pressure. Reaching a minimum threshold of 30 mL/hr confirms that the glomerular filtration rate has been restored through effective intravenous fluid volume expansion.
2. The resolution of orthostatic hypotension demonstrates that the autonomic nervous system and baroreceptors no longer need to overcompensate for a low stroke volume. When a client can move from a supine to a standing position without a significant drop in blood pressure (greater than 20 mmHg systolic), it indicates that the intravascular space is sufficiently filled. This finding signifies a return to hemodynamic stability and a reduction in the risk of syncope.
4. Decreased urine ketones reflect the transition from fat catabolism back to glucose-based energy production. When a client is adequately hydrated and receiving dextrose-containing fluids, the body stops breaking down adipose tissue, which prevents the formation of acidic ketone bodies. This serves as a definitive marker that the metabolic crisis and starvation state associated with hyperemesis are being successfully reversed.
Rationale for incorrect answers
3. Persistent tachycardia is a sign that the cardiovascular system is still under stress or attempting to compensate for an ongoing volume deficit. As hydration becomes effective, the heart rate should gradually decrease toward the client's baseline as the stroke volume increases and the sympathetic drive diminishes. A heart rate that remains elevated (greater than 100 bpm) suggests that resuscitation is either incomplete or that other factors like pain or anxiety are present.
5. Concentrated, dark urine is a hallmark sign of ongoing dehydration and the body's attempt to conserve every milliliter of fluid. Effective hydration would instead result in pale yellow or straw-colored urine with a low specific gravity (1.005 to 1.015). Finding highly concentrated urine implies that the kidneys are still responding to high levels of antidiuretic hormone and that the client remains in a state of fluid volume deficit.
Test-taking strategy
- Identify the Physiological Goal: The question asks for signs of "effective" treatment. Categorize choices as "positive/healthy" versus "negative/pathological" trends.
- Recall Renal Benchmarks: Use the standard nursing rule that 30 mL/hr is the minimum acceptable urine output for an adult. Since 35 mL/hr (Choice 1) is above this, it indicates success.
- Analyze the Pulse-Volume Relationship: Remember that as volume (preload) increases, the heart does not have to beat as fast to maintain cardiac output. Therefore, persistent tachycardia (Choice 5) is a sign of failure, not success.
- Evaluate Metabolic Outcomes: Ketonuria is a byproduct of the starvation seen in hyperemesis. Its "decrease" or "resolution" (Choice 4) proves the patient is metabolizing nutrients correctly again.
- Match Physical Findings to Hydration: Think about what happens when you drink plenty of water. Your urine gets lighter, and you don't feel dizzy when you stand up. This validates Choice 2 and invalidates Choice 5.
Take home points
- Successful fluid replacement is evidenced by a urine output exceeding 30 mL/hr and the normalization of urine specific gravity.
- Resolution of orthostatic hypotension and a decreasing heart rate are the primary indicators of restored intravascular volume.
- The disappearance of ketones in the urine signals the end of the starvation-induced catabolic state.
- Moist mucous membranes and brisk skin turgor are the physical assessment goals for rehydration therapy.
A nurse notes confusion and unsteady gait in a client with severe hyperemesis gravidarum. Which of the following complications should the nurse suspect?
Explanation
Hyperemesis gravidarum induces a critical state of micronutrient depletion when persistent emesis prevents the absorption of water-soluble vitamins. Thiamine, also known as Vitamin B1, is a mandatory cofactor for enzymes within the aerobic glucose oxidation pathway. Without this coenzyme, the brain cannot metabolize glucose, leading to acute adenosine triphosphate failure and subsequent neuronal death in the brainstem and diencephalon.
Wernicke’s encephalopathy is the most severe neurological complication of prolonged thiamine deficiency in hyperemesis. The condition is characterized by a classic clinical triad of global confusion, ataxia, and ophthalmoplegia such as nystagmus. Because pregnancy increases the metabolic demand for thiamine, a client with intractable vomiting can exhaust their limited hepatic stores within 2 to 3 weeks, leading to irreversible hemorrhagic lesions in the mammillary bodies.
Rationale for correct answer
3. Wernicke's encephalopathy is the only complication listed that directly results from the nutritional and vitamin depletion inherent to severe hyperemesis. The symptoms of unsteady gait (ataxia) and confusion are pathognomonic for thiamine deficiency when they occur in a starving patient. This condition is a medical emergency because it can progress to permanent memory loss or death if not treated with immediate intravenous thiamine.
Rationale for incorrect answers
1. A stroke typically presents with focal neurological deficits, such as hemiparesis or facial drooping, rather than a global state of confusion. While dehydration can increase the risk of thrombosis, the specific combination of ataxia and encephalopathy in a vomiting patient is much more characteristic of a metabolic deficiency. Stroke symptoms usually appear suddenly and are related to a specific vascular territory in the brain.
2. A migraine disorder is characterized by severe, often unilateral, throbbing headaches accompanied by photophobia and phonophobia. While migraines can cause nausea and vomiting, they do not cause a persistent unsteady gait or global cognitive confusion between episodes. The primary pathology of a migraine is vascular and neurological irritability rather than the systemic micronutrient depletion seen in hyperemesis.
4. A seizure disorder involves paroxysmal, uncontrolled electrical activity in the brain that results in altered consciousness or convulsions. While a post-ictal state can include confusion, a persistent ataxic gait is not a standard feature of chronic epilepsy. Seizures in a pregnant client with hyperemesis would more likely be a result of severe hyponatremia or magnesium imbalance rather than thiamine loss.
Test-taking strategy
- Link Symptoms to Nutrient: Associate the "Confusion + Ataxia" duo specifically with Thiamine (B1). This is a high-yield association for any patient with long-term vomiting or malnutrition.
- Identify the Condition: Recognize that Wernicke’s encephalopathy (Choice 3) is the primary neurological "killer" in hyperemesis cases.
- Evaluate Iatrogenic Risks: Recall that giving dextrose (sugar) before thiamine can actually trigger this condition by using up the last bit of Vitamin B1.
- Differentiate by Presentation: Rule out Choice 1 (stroke) because it is usually one-sided, and Choice 2 (migraine) because it is primarily a pain disorder.
- Prioritize Acute vs Chronic: While all choices are neurological, only Choice 3 is a direct complication of the nutritional failure described in the stem.
Take home points
- Wernicke’s encephalopathy is caused by a severe deficiency of thiamine (Vitamin B1) due to prolonged vomiting.
- The clinical triad of confusion, ataxia, and ocular abnormalities requires immediate high-dose intravenous thiamine replacement.
- Nurses must never administer glucose-containing IV fluids to a malnourished patient until thiamine has been provided.
- Untreated Wernicke’s can lead to Korsakoff syndrome, which involves permanent anterograde and retrograde amnesia.
A nurse is developing a plan of care for a client with hyperemesis gravidarum. Which of the following nursing assessments are essential? Select all that apply
Explanation
Hyperemesis gravidarum represents a systemic metabolic and hemodynamic challenge characterized by the persistent loss of gastric secretions. This condition results in a significant intravascular volume deficit and the exhaustion of maternal nutritional stores, which can lead to starvation ketosis. Nursing management focuses on the objective quantification of fluid balance and the assessment of compensatory mechanisms to prevent secondary renal and fetal complications.
Rationale for correct answers
1. Monitoring daily weight is the most objective and sensitive measure of total body fluid status in a client with hyperemesis. A loss of > 5% of pre-pregnancy mass is a diagnostic hallmark of the condition and indicates significant nutritional and fluid depletion. Trends in weight provide the healthcare team with immediate feedback on the efficacy of parenteral nutrition and rehydration protocols.
2. Assessing skin turgor provides a direct clinical evaluation of the interstitial fluid compartment and overall tissue hydration. In severe dehydration, the skin loses its natural elasticity, resulting in a phenomenon known as "tenting" when the skin is pinched. This physical assessment helps the nurse identify the severity of the fluid volume deficit before more advanced hemodynamic collapse occurs.
3. Measuring urine output is essential for evaluating renal perfusion and the adequacy of the circulating blood volume. The kidneys produce oliguria (output < 30 mL/hr) as a compensatory response to hypovolemia via the activation of the renin-angiotensin-aldosterone system. Monitoring output allows the nurse to titrate intravenous fluid rates and ensure the prevention of pre-renal acute kidney injury.
4. Monitoring fetal heart rate is a priority to ensure that maternal dehydration and malnutrition have not compromised placental perfusion. Maternal hypovolemia can lead to decreased uterine blood flow, which may manifest as fetal tachycardia or decreased variability. Regular auscultation or electronic monitoring confirms fetal well-being and provides reassurance that the pregnancy remains viable despite maternal metabolic stress.
Rationale for incorrect answers
5. Evaluating respiratory depth only is an incomplete and inadequate nursing assessment for a client with complex acid-base disturbances. While respiratory patterns may change to compensate for metabolic alkalosis or ketosis, the nurse must monitor rate, rhythm, and oxygen saturation as well. A narrow focus on depth ignores critical indicators of systemic stability and the potential for respiratory depression secondary to severe electrolyte imbalances.
Test-taking strategy
- Identify the Condition Type: Hyperemesis is a fluid and electrolyte disorder. Priority assessments must focus on volume markers (Weight, Turgor, Output).
- Assess the Client as a Pair: In obstetrics, always look for an answer that includes the fetus. Choice 4 is essential because any maternal illness affects the gestational unit.
- Watch for "Absolutist" Language: Words like only in Choice 5 are almost always red flags in nursing exams. They indicate an overly narrow scope that misses broader clinical priorities.
- Match Assessment to Pathology: Connect "vomiting" to "weight loss" and "dehydration." This makes Choices 1, 2, and 3 mandatory for a comprehensive plan of care.
- Think ABCs: Circulation is heavily impacted here. Measuring output and weight are the gold standards for monitoring the "C" in the ABC hierarchy for this patient.
Take home points
- Daily weights are the primary longitudinal indicator of nutritional and fluid volume status in hyperemesis.
- Urine output must be maintained above 30 mL/hr to ensure adequate renal perfusion and avoid azotemia.
- Physical signs like poor skin turgor and dry mucous membranes indicate a significant interstitial fluid deficit.
- Fetal monitoring is necessary to detect potential placental insufficiency caused by maternal hypovolemia.
A nurse is providing psychosocial support to a client with hyperemesis gravidarum. Which of the following nursing actions is most appropriate?
Explanation
Hyperemesis gravidarum induces a state of chronic neuroendocrine and psychological stress that extends beyond the physical symptoms of emesis. The persistent nature of the condition often leads to secondary depressive disorders and anxiety due to the loss of functional independence and disruption of social roles. Nursing interventions must address the psychosomatic interface by validating the maternal experience of suffering and identifying the impact of chronic illness on maternal-fetal attachment and mental well-being.
Rationale for correct answer
3. Acknowledging the psychological impact of prolonged illness is the most appropriate action because it validates the client's feelings of distress and isolation. Chronic, intractable vomiting is physically exhausting and often leads to feelings of hopelessness or anxiety regarding the safety of the fetus. By using therapeutic communication to address these emotional burdens, the nurse fosters a supportive environment that can improve the client's coping mechanisms and overall treatment adherence.
Rationale for incorrect answers
1. Advising the client that symptoms are expected in pregnancy is a form of dismissal that trivializes a potentially life-threatening condition. While "morning sickness" is common, hyperemesis gravidarum is a pathological state that requires medical hospitalization. This statement minimizes the client's physical suffering and can lead to a breakdown in the therapeutic relationship, as the client may feel the nurse does not understand the severity of the illness.
2. Minimizing discussion of emotional distress is counterproductive and can exacerbate the psychological burden of the disease. Unaddressed anxiety and depression can worsen the physiological perception of nausea through the gut-brain axis. Ignoring the emotional components of hyperemesis fails to provide holistic care and misses critical opportunities to screen for serious mental health complications like post-traumatic stress disorder related to the pregnancy.
4. Encouraging the client to avoid family involvement is inappropriate because social support is a vital protective factor during high-risk pregnancies. Family members can provide emotional comfort, assist with activities of daily living, and help manage the household while the client is incapacitated. Isolation can lead to increased maternal anxiety and depression, whereas a strong support system is associated with better psychological outcomes for the mother and family unit.
Test-taking strategy
- Identify Therapeutic Communication: Look for the answer that uses validation and empathy. Choice 3 is the only option that focuses on acknowledging the client's internal experience.
- Avoid Dismissive Language: Rule out Choice 1 because it "normalizes" a serious medical condition. In nursing, we never tell a patient with a severe pathology that their symptoms are "expected" or "normal."
- Promote Holistic Care: Eliminate Choice 2. Nursing care must always address the mind and the body. Any action that "minimizes" the psychological side of a disease is usually incorrect.
- Evaluate Support Systems: Choice 4 is incorrect because family support is generally viewed as a positive resource in maternal-child nursing unless there is specific evidence of abuse or toxic dynamics.
- Match Strategy to Chronic Illness: For any prolonged condition, the correct psychosocial approach is to recognize the long-term emotional toll the illness takes on the patient's identity and life.
Take home points
- Hyperemesis gravidarum is associated with high rates of secondary depression, anxiety, and social isolation.
- Therapeutic communication that validates the client's physical and emotional suffering is essential for holistic recovery.
- Emotional distress can exacerbate physical nausea, making psychological support a key component of physiological stabilization.
- Family involvement should be encouraged to provide a robust support network for the client during and after hospitalization.
Comprehensive Questions
A nurse is caring for a client with hyperemesis gravidarum who has persistent vomiting. Which of the following laboratory findings is most indicative of metabolic alkalosis?
Explanation
Hyperemesis gravidarum induces a severe extracellular fluid volume deficit and electrolyte depletion through the intractable expulsion of hydrochloric acid. The loss of hydrogen and chloride ions from the gastric mucosa triggers a systemic metabolic shift characterized by an elevated bicarbonate concentration and arterial pH. To maintain electrical neutrality, the kidneys excrete potassium in exchange for hydrogen ions, leading to profound hypokalemia and contraction alkalosis.
Rationale for correct answer
1. A serum potassium of 2.8 mEq/L and an arterial pH of 7.50 are the hallmark biochemical markers of metabolic alkalosis in this clinical context. The pH value exceeds the normal physiological limit of 7.45, confirming a state of alkalemia caused by the massive loss of gastric acid. Hypokalemia occurs as a direct result of compensatory renal mechanisms and the secondary hyperaldosteronism triggered by the profound dehydration and volume contraction.
Rationale for incorrect answers
2. A serum sodium of 140 mEq/L and an arterial pH of 7.35 represent values within the normal physiological reference range for a healthy adult. A pH of 7.35 is at the lowest end of the normal range and does not reflect the alkalosis expected with persistent vomiting. Normal laboratory values would not be expected in a client with severe hyperemesis who has reached the stage of systemic acid-base derangement.
3. A serum potassium of 4.0 mEq/L and a pH of 7.28 indicate a state of metabolic acidosis, which is the opposite of the condition described. A pH below 7.35 represents acidemia, which might occur later in starvation due to the buildup of ketone bodies but contradicts the primary alkalosis. This finding is inconsistent with the acute loss of gastric hydrochloric acid typically seen in the early phases of hyperemesis.
4. A serum sodium of 135 mEq/L and a pH of 7.32 also indicate a mild acidosis or a compensated state that does not match the question. While hyponatremia can occur due to the loss of gastric salts, the pH of 7.32 indicates an excess of hydrogen ions in the blood. In the context of active, forceful vomiting, the arterial pH should be significantly elevated due to the depletion of gastric acid.
Test-taking strategy
- Identify the Acid-Base Goal: The question asks for "metabolic alkalosis." In medical terms, alkalosis always means an arterial pH greater than 7.45.
- Filter by pH Values: Immediately look at the pH in each choice. Choice 1 (7.50) is the only option that shows alkalemia. Choices 2, 3, and 4 show either normal or acidic pH levels.
- Correlate with Electrolytes: Recall that vomiting causes the loss of hydrochloric acid (HCl). When the body loses acid, the pH goes up.
- Recognize the Potassium Relationship: Remember that hypokalemia (low potassium) is the standard electrolyte partner to metabolic alkalosis. Choice 1 shows a low potassium of 2.8 mEq/L, which matches the pathology perfectly.
- Eliminate Normalcy: Rule out Choice 2 because a patient with "persistent vomiting" will not have perfect, normal lab values; there must be a visible derangement.
Take home points
- Metabolic alkalosis is defined by an arterial pH > 7.45 and an elevated serum bicarbonate level.
- Persistent vomiting causes the loss of gastric hydrochloric acid, leading to an excess of base in the blood.
- Hypokalemia (Potassium < 3.5 mEq/L) typically accompanies metabolic alkalosis as the kidneys attempt to conserve hydrogen.
- Severe dehydration and volume contraction exacerbate alkalosis through the activation of the renin-angiotensin-aldosterone system.
A client with hyperemesis gravidarum reports fruity-smelling breath and deep, rapid respirations. Which metabolic condition should the nurse suspect?
Explanation
Hyperemesis gravidarum induces a state of carbohydrate deprivation when persistent emesis prevents the absorption of dietary glucose. Once hepatic glycogen stores are exhausted, typically within 24 hours of starvation, the body initiates the catabolic breakdown of adipose tissue for energy. This lipolysis results in the hepatic synthesis of ketone bodies, specifically acetoacetate and beta-hydroxybutyrate, which accumulate in the systemic circulation.
Rationale for correct answer
2. The presence of fruity-smelling breath and deep, rapid respirations indicates that the client has transitioned into a state of ketosis. This occurs because the breakdown of fatty acids produces acetone, which is volatile and excreted through the lungs, creating a distinct fruity odor. The altered respiratory pattern, known as Kussmaul breathing, is a compensatory mechanism to blow off carbon dioxide and mitigate the metabolic acidosis caused by the acidic ketone bodies.
Rationale for incorrect answers
1. Metabolic alkalosis is common in the early stages of hyperemesis due to the direct loss of hydrochloric acid from the stomach. However, alkalosis typically causes hypoventilation (slow, shallow breathing) as the body attempts to retain carbon dioxide to lower the pH. It does not produce the fruity odor or the rapid, deep breathing associated with the accumulation of acidic metabolic byproducts like ketones.
3. Diabetic ketoacidosis (DKA) shares the same clinical signs of fruity breath and Kussmaul respirations but is driven by insulin deficiency and profound hyperglycemia. While a pregnant client can have DKA, the underlying cause in this scenario is starvation from hyperemesis rather than a primary pancreatic disorder. In hyperemesis, the blood glucose level is typically low or normal, whereas in DKA, it is significantly elevated.
4. Respiratory acidosis results from the retention of carbon dioxide due to alveolar hypoventilation, often seen in chronic obstructive pulmonary disease or narcotic overdose. This condition would manifest as a decreased respiratory rate and depth, leading to hypercapnia and a low pH. It does not involve the metabolic production of acetone, and therefore, it would not be associated with fruity-smelling breath or the rapid breathing pattern described.
Test-taking strategy
- Identify Pathognomonic Signs: Recognize that "fruity breath" is the classic medical descriptor for acetone excretion. This immediately points to a condition involving ketones.
- Connect Breathing to Acidosis: Deep, rapid respirations (Kussmaul breathing) are the body's way of fighting an acidic blood pH. Since vomiting usually causes alkalosis, the presence of this breathing pattern means the patient has shifted into starvation acidosis.
- Differentiate the Cause: Choose between Choice 2 and Choice 3. In a patient with "hyperemesis" (vomiting/starvation), Ketosis is the direct result of not eating. DKA requires a history of diabetes or high blood sugar.
- Match Physiological Responses: Eliminate Choice 1 and Choice 4 because their respiratory compensations (breathing slower) are the exact opposite of what the patient is doing (breathing faster).
- Focus on the Stem Context: The stem provides a diagnosis of "hyperemesis gravidarum," which is a nutritional crisis. The answer must reflect the metabolic consequence of starvation.
Take home points
- Fruity-smelling breath is caused by the pulmonary excretion of acetone, a byproduct of fat metabolism.
- Kussmaul respirations are a compensatory respiratory response to metabolic acidosis (ketosis).
- Starvation ketosis in hyperemesis occurs once glucose and glycogen stores are completely depleted.
- Monitoring urine for ketones is a priority nursing assessment to track the severity of the maternal catabolic state.
A nurse is preparing to administer intravenous therapy to a client with severe hyperemesis gravidarum. Which fluid should be given first to prevent Wernicke’s encephalopathy?
Explanation
Hyperemesis gravidarum induces a critical state of micronutrient depletion where glycogen exhaustion triggers metabolic shifts. Thiamine acts as a mandatory coenzyme for the pyruvate dehydrogenase complex within the aerobic glucose oxidation pathway. Introduction of high-load carbohydrate substrates without sufficient B1 stores precipitates acute neuronal oxidative stress and ATP failure.
Rationale for correct answer
4. Administering thiamine before glucose-containing fluids is the most critical intervention to prevent the precipitation of acute Wernicke encephalopathy. Thiamine is a vital cofactor for metabolic enzymes that process carbohydrates into cellular energy. If a concentrated glucose load is provided to a depleted patient, the remaining B1 is rapidly consumed, leading to catastrophic neurotoxicity and hemorrhagic lesions in the brain.
Rationale for incorrect answers
1. Dextrose 5% in water is contraindicated as the initial fluid for a malnourished client because it provides a glucose substrate without the necessary metabolic cofactors. Infusing dextrose alone can trigger a sudden shift in carbohydrate metabolism that exhausts the body's last thiamine reserves. This iatrogenic error is the primary cause of hospital-acquired Wernicke encephalopathy in patients with prolonged starvation.
2. Lactated Ringer’s solution is an isotonic crystalloid often used for volume expansion, but it does not address the specific vitamin deficiency required to protect the central nervous system. While it provides electrolytes like potassium and calcium, it lacks the thiamine necessary to prevent neurological degradation. It is a secondary choice for hydration but is not the specific intervention requested to prevent encephalopathy.
3. Normal saline 0.9% is an appropriate fluid for initial volume resuscitation and does not carry the same immediate risk as dextrose. However, simply giving saline does not actively prevent the neurological damage if the patient is already thiamine deficient. The "most critical" action remains the specific administration of Vitamin B1 prior to the introduction of any calorie-dense intravenous infusions.
Test-taking strategy
- Identify the Critical Risk: The question focuses on "Wernicke’s encephalopathy" in a malnourished patient. In nursing exams, this phrase is almost always a reference to thiamine deficiency.
- Recall the Order of Operations: Memorize the clinical rule that "B1 comes before D5." Never give dextrose (glucose) to a patient with chronic vomiting or starvation until thiamine has been administered.
- Differentiate Priorities: Rule out Choice 2 and Choice 3 because while they are safe, they are not specific treatments for the mentioned neurological complication.
- Identify the Iatrogenic Trigger: Recognize that providing the "cure" (dextrose) can actually cause the "harm" (brain damage) if the metabolic cofactor is missing.
- Focus on the Nutrient: Look for the specific vitamin associated with neurological stability in alcoholics and hyperemesis patients.
Take home points
- Thiamine (Vitamin B1) must always precede or accompany the first dose of dextrose-containing IV fluids in hyperemesis.
- Iatrogenic Wernicke encephalopathy is caused by the rapid consumption of residual thiamine during a sudden glucose load.
- The classic triad of Wernicke includes global confusion, ataxia, and ocular abnormalities like nystagmus.
- Failure to provide thiamine can result in Korsakoff syndrome, which involves irreversible memory loss and confabulation.
A nurse is teaching a client with hyperemesis gravidarum about dietary management. Which recommendation is most appropriate?
Explanation
Hyperemesis gravidarum necessitates a nutritional rehabilitation strategy focused on minimizing gastric distension and optimizing glycemic stability. The transition from a catabolic state requires small-volume, high-density intake to prevent the activation of the medullary emetic centers. High-protein substrates facilitate slower gastric emptying and provide sustained amino acid availability, while limiting adipose tissue mobilization.
Rationale for correct answer
2. Eating small, frequent meals high in protein is the most effective dietary intervention to stabilize blood glucose and reduce nausea. High-protein foods may decrease gastric dysrhythmia and provide better symptomatic relief than high-carbohydrate alternatives in some gestations. Frequent small portions prevent gastric overdistension, which is a potent trigger for the mechanical stretch receptors that initiate the emetic reflex arc.
Rationale for incorrect answers
1. Consuming large meals three times daily is contraindicated because massive gastric volume increases intraluminal pressure and triggers immediate vomiting. Hyperemesis patients suffer from delayed gastric emptying, meaning large volumes lead to prolonged stasis and fermentation. This traditional eating pattern fails to provide the constant, steady stream of nutrients required to suppress starvation-induced ketosis and maintain metabolic neutrality.
3. Avoiding all solid foods is an inappropriate long-term strategy that can exacerbate malnutrition and lead to muscle wasting. While a brief period of gut rest may be required during acute resuscitation, the goal is a gradual return to solid intake. Relying solely on liquids often leads to inadequate caloric density and may actually worsen nausea due to rapid gastric transit and subsequent hypoglycemia.
4. Increasing intake of high-fat foods is strongly discouraged because lipids significantly delay gastric emptying times and relax the lower esophageal sphincter. High-fat content increases the risk of acid reflux and creates a sensation of "fullness" that triggers the chemoreceptor trigger zone. Patients with hyperemesis typically exhibit a profound intolerance to the odors and textures of greasy or highly seasoned adipose-rich dietary items.
Test-taking strategy
- Identify the Goal: The objective is to find a dietary pattern that minimizes nausea while maximizing absorption.
- Apply Gastric Physiology: Recall that distension causes vomiting. This immediately rules out Choice 1 (large meals).
- Evaluate Macronutrients: Understand that fats (Choice 4) slow down the stomach too much, while proteins (Choice 3) provide stable energy. Protein is the "friend" of the nauseated stomach.
- Analyze Nutritional Sustainability: Total avoidance of solids (Choice 2) is a "starvation" move. In nursing, we always move toward rehabilitation and self-sufficiency unless the patient is in an acute crisis.
- Look for "Small and Frequent": This is a classic NCLEX-style "buzzword" for almost all gastrointestinal or metabolic conditions requiring dietary management, including GERD, dumping syndrome, and pregnancy-related emesis.
Take home points
- Small, frequent meals (every 2 to 3 hours) prevent the gastric distension and hypoglycemia that trigger vomiting episodes.
- High-protein, low-fat foods are better tolerated because they do not significantly delay gastric emptying or cause reflux.
- Dry carbohydrates (e.g., crackers) upon awakening can help stabilize blood sugar before rising from bed to prevent morning triggers.
- Separating liquid and solid intake (drinking between meals rather than with them) reduces the total volume in the stomach at any one time.
A nurse is monitoring a client with hyperemesis gravidarum. Which electrolyte imbalance is most likely to cause cardiac arrhythmias?
Explanation
Hyperemesis gravidarum induces a severe electrolyte depletion through the intractable expulsion of hydrochloric acid and potassium-rich gastric secretions. This hypovolemia triggers secondary hyperaldosteronism, which further accelerates renal potassium wasting in an attempt to conserve sodium and water. The resulting deficit compromises the resting membrane potential of excitable tissues, particularly within the cardiac conduction system, leading to dangerous electrical instability.
Rationale for correct answer
2. Hypokalemia is the most likely electrolyte derangement to precipitate life-threatening cardiac arrhythmias in hyperemesis. Potassium is the primary intracellular cation responsible for repolarizing the myocardium during the cardiac cycle. When serum levels drop below 3.5 mEq/L, the heart becomes hyper-irritable, potentially leading to premature ventricular contractions, flattened T-waves, and even lethal ventricular fibrillation if not corrected.
Rationale for incorrect answers
1. Hyperkalemia refers to an excess of potassium and is typically associated with renal failure or excessive tissue trauma rather than vomiting. While high potassium also causes arrhythmias and peaked T-waves, it is physiologically inconsistent with the chronic fluid and acid loss seen in hyperemesis. A client with persistent emesis is losing cations through the stomach and urine, making an elevated potassium level extremely unlikely.
3. Hypernatremia is an elevation in serum sodium often caused by pure water loss or excessive salt intake. While it can cause neurological symptoms like seizures or altered mental status, it is not the primary driver of cardiac rhythm disturbances in this population. Hyperemesis more frequently results in hyponatremia due to the loss of sodium in gastric juices and the compensatory release of antidiuretic hormone.
4. Hypermagnesemia involves an excess of magnesium, which can lead to respiratory depression and a loss of deep tendon reflexes. This condition is usually iatrogenic, occurring during the treatment of preeclampsia, rather than as a complication of vomiting. In hyperemesis, the nurse is more likely to encounter hypomagnesemia, which can actually worsen the severity of the concurrent hypokalemia and increase the risk of torsades de pointes.
Test-taking strategy
- Identify the Organ System: The question asks about "cardiac arrhythmias." Potassium is the "king" of cardiac electrical stability.
- Match Direction to Loss: Vomiting is a "loss" condition. Therefore, you should look for "hypo-" conditions. This eliminates Choice 1, 3, and 4.
- Link Symptoms to Ions: Associate Potassium with the heart, Sodium with the brain, and Magnesium/Calcium with the nerves and muscles.
- Recall the Chemistry of Emesis: Gastric juice is rich in H+, Cl-, and K+. Losing it leads directly to Choice 2.
- Apply the "Most Likely" Filter: While many imbalances occur, hypokalemia is the most common and most dangerous hemodynamic threat in a vomiting patient.
Take home points
- Hypokalemia (Potassium < 3.5 mEq/L) is a critical complication of hyperemesis that requires immediate IV replacement.
- Cardiac monitoring (ECG) is indicated for any client with severe electrolyte derangements to screen for U-waves or ST-segment depression.
- Potassium replacement should only be initiated after confirming adequate urine output (at least 30 mL/hr) to avoid iatrogenic hyperkalemia.
- Concurrent hypomagnesemia often makes hypokalemia resistant to treatment, requiring magnesium replacement as well.
A nurse is assessing a client admitted with hyperemesis gravidarum. Which vital sign indicates early hypovolemia?
Explanation
Hyperemesis gravidarum induces a state of intravascular volume depletion through the persistent loss of gastric secretions. When circulating volume decreases, the baroreceptors in the carotid sinus and aortic arch detect a reduction in mean arterial pressure. This triggers a sympathetic nervous system response, resulting in the release of catecholamines to maintain cardiac output through increased heart rate, a process known as compensatory tachycardia.
Rationale for correct answer
2. Tachycardia is the most sensitive early clinical indicator of hypovolemia in the pregnant client. As the stroke volume declines due to fluid loss, the heart must beat faster to maintain a constant cardiac output and ensure placental perfusion. A resting heart rate exceeding 100 beats per minute often precedes a drop in systolic blood pressure, as the body utilizes chronotropic compensation to stabilize the hemodynamic status during the initial phase of dehydration.
Rationale for incorrect answers
1. Bradycardia is a slow heart rate (less than 60 beats per minute) and is generally not an indicator of acute fluid loss. This finding is more commonly associated with athletic conditioning, certain medications like beta-blockers, or late-stage neurological injury. In a client with hyperemesis, the physiological stress and volume deficit would trigger the opposite response, as a slow heart rate would lead to a catastrophic drop in perfusion pressure.
3. Hypertension refers to an elevated blood pressure and is usually a sign of conditions like preeclampsia or chronic vascular disease rather than dehydration. While sympathetic activation can cause a brief, transient rise in pressure, prolonged hypovolemia eventually leads to hypotension. A high blood pressure reading would suggest a different pathology or perhaps a state of acute pain or anxiety, rather than the volume depletion characteristic of severe vomiting.
4. A low-grade fever of 37.2°C (99°F) is a non-specific finding that may occur with dehydration due to reduced heat dissipation from the skin. However, it is not a primary or reliable indicator of hypovolemia when compared to cardiovascular changes. Fever is more typically a hallmark of infectious processes or inflammatory responses, whereas the clinical priority in hyperemesis is identifying the hemodynamic shifts that precede circulatory collapse.
Test-taking strategy
- Identify the Physiological Theme: The question asks for an "early" sign of "low volume." Think about how the heart reacts to "empty pipes."
- Apply the Compensation Rule: When blood volume (preload) goes down, the heart rate must go up to keep blood moving. This makes Choice 2 the only logical physiological response to early blood loss or dehydration.
- Eliminate Late Signs: Remember that hypotension (low blood pressure) is often a "late" sign of shock. The "early" sign is always the body's attempt to fix the pressure, which is tachycardia.
- Rule out Normal/Irrelevant Data: Choice 4 is essentially a normal variation and doesn't tell you anything specific about the vascular compartment.
- Differentiate Pathologies: Choice 3 (Hypertension) is the opposite of what happens when you lose fluid. Think of a garden hose; if you turn off the water, the pressure doesn't go up.
Take home points
- Tachycardia is the earliest cardiovascular sign of hypovolemia as the body compensates for decreased stroke volume.
- Orthostatic hypotension (a drop in BP when standing) often accompanies tachycardia in the early stages of dehydration.
- Blood pressure may remain within normal limits initially due to intense peripheral vasoconstriction.
- A heart rate > 100 bpm in a resting pregnant client necessitates immediate assessment of fluid and electrolyte status.
A client with hyperemesis gravidarum is prescribed Ondansetron. The nurse should monitor the client for which potential fetal complication?
Explanation
Ondansetron acts as a selective 5-HT3 receptor antagonist that prevents the binding of serotonin in the peripheral and central nervous system to suppress the emetic reflex. This pharmacological agent can interfere with the repolarization phase of the cardiac action potential by blocking the rapid component of the delayed rectifier potassium current. In the developing fetus, this interference can disrupt the established electrical conduction pathways, potentially leading to significant cardiovascular instability or life-threatening rhythms if exposure occurs during critical development.
Rationale for correct answer
2. Cardiac arrhythmias are the primary fetal concern associated with ondansetron exposure, particularly when maternal administration occurs in high doses. The drug’s mechanism of QT interval prolongation is not restricted to maternal physiology and can cross the placental barrier to affect fetal cardiac myocytes. Prolonged exposure can lead to bradycardia or atrioventricular dissociation, which increases the risk of fetal hydrops or intrauterine fetal demise.
Rationale for incorrect answers
1. Neural tube defects are structural abnormalities that occur within the first 28 days of gestation, often due to folate deficiency or genetic factors. Ondansetron is typically prescribed after the organogenesis phase has begun or peak hyperemesis has set in, which is often after the neural tube has already closed. There is no established biopathway linking serotonin receptor antagonism to the failure of neural tube closure during the first month of pregnancy.
3. Low birth weight is a generalized outcome often resulting from maternal malnutrition or placental insufficiency in untreated hyperemesis. While ondansetron aims to improve maternal caloric intake by stopping emesis, the drug itself is not a direct cause of growth restriction. In fact, successful antiemetic therapy is more likely to prevent low birth weight by allowing the mother to maintain a positive nitrogen balance and adequate glucose levels.
4. Hyperbilirubinemia is a condition of excess bilirubin in the neonatal period, typically caused by ABO incompatibility or physiological liver immaturity. Ondansetron does not interfere with fetal bilirubin metabolism or the breakdown of erythrocytes in the fetal circulation. This complication is more closely linked to maternal-fetal blood group mismatches or preterm delivery rather than the administration of serotonin antagonists for nausea and vomiting.
Test-taking strategy
- Link Drug to Side Effect: Associate ondansetron (Zofran) with QT prolongation and arrhythmias. This is a "must-know" side effect for this drug class in all patient populations.
- Prioritize the Heart: In pharmacology questions, structural defects (Choice 1) are rare, while rhythm disturbances (Choice 2) are common concerns for drugs that affect ion channels.
- Differentiate Cause and Effect: Recognize that Choice 3 (low birth weight) is a result of the disease (hyperemesis), not the treatment (ondansetron).
- Rule out Neonatal Issues: Choice 4 occurs after birth and is not a standard complication of antiemetic exposure during the antepartum period.
Take home points
- Ondansetron is associated with a small but significant risk of QT interval prolongation in both mother and fetus.
- Baseline and serial ECG monitoring may be required for mothers with pre-existing electrolyte imbalances or cardiac history.
- Current clinical guidelines recommend using ondansetron only after first-line therapies (B6 and doxylamine) have failed.
- Nurses should monitor for symptoms of fetal distress, such as bradycardia, during high-dose intravenous ondansetron therapy.
A nurse is caring for a client with hyperemesis gravidarum who has ketonuria and elevated hematocrit. Which intervention is priority?
Explanation
Hyperemesis gravidarum induces a severe extracellular fluid volume deficit characterized by the loss of gastric water and hydrochloric acid. This hypovolemia results in hemoconcentration, where the plasma volume decreases relative to the cellular components, leading to an elevated hematocrit reading. Simultaneously, the body enters a catabolic state of starvation once glycogen stores are exhausted, forcing the breakdown of adipose tissue and the subsequent excretion of ketone bodies in the urine.
Rationale for correct answer
2. Initiating IV fluid replacement is the highest priority to correct the life-threatening physiological imbalances of dehydration and ketosis. Intravenous resuscitation with isotonic crystalloids rapidly expands the intravascular compartment, which reduces hemoconcentration and lowers the hematocrit back to normal levels. By providing necessary fluid and often dextrose, the nurse halts the catabolism of fats, thereby resolving the ketonuria and protecting maternal renal and neurological function.
Rationale for incorrect answers
1. Providing emotional support is a secondary nursing action that should occur only after the client has been hemodynamically stabilized. While the psychological distress of hyperemesis is significant, it does not address the immediate risks of renal failure or metabolic acidosis. In a clinical scenario with objective signs of dehydration (elevated hematocrit), physiological needs take precedence over psychosocial needs according to Maslow's Hierarchy.
3. Encouraging small, frequent meals is a dietary strategy for mild nausea but is inappropriate for a client with ketonuria. A client in a state of active ketosis typically requires a period of gut rest (NPO status) to stop the cycle of vomiting and allow for intravenous stabilization. Attempting to introduce oral intake before the patient is rehydrated often leads to further emetic episodes and worsening metabolic derangement.
4. Monitoring fetal heart rate is an essential component of obstetric care but is not the immediate priority when the mother is in a metabolic crisis. The best way to ensure fetal well-being in this situation is to correct the maternal hypovolemia that is compromising placental perfusion. Fetal monitoring is an assessment that identifies a problem, whereas IV therapy is the intervention that treats the underlying cause of both maternal and fetal distress.
Test-taking strategy
- Prioritize Physiological over Psychosocial: Following Maslow's Hierarchy, Choice 2 (IV fluids) addresses the physical survival of the patient, while Choice 1 addresses emotional needs.
- Identify the most Acute Need: The stem provides laboratory evidence of dehydration (elevated hematocrit) and starvation (ketonuria). Both require immediate "replacement" or "input," which points directly to Choice 2.
- Apply the ABCs: Circulation is compromised by low volume (hypovolemia). IV fluids are the primary treatment for the Circulation component of the ABCs.
- Assess Route of Administration: A patient who is vomiting to the point of ketonuria cannot tolerate oral interventions (Choice 3). Parenteral (IV) access is the only reliable route for resuscitation.
- Distinguish Assessment from Intervention: Choice 4 is an assessment (monitoring). When a question asks for a "priority intervention" for a known problem, choose the action that fixes the problem.
Take home points
- IV fluid resuscitation is the gold standard for treating severe dehydration and ketosis in hyperemesis.
- Elevated hematocrit (hemoconcentration) and ketonuria are objective indicators that a client requires hospital-level stabilization.
- Restoration of fluid volume is necessary to maintain maternal blood pressure and ensure adequate placental blood flow.
- Normalization of lab values (negative ketones and lower hematocrit) is the primary goal of the initial 24 hours of therapy.
A client with hyperemesis gravidarum is at risk for Wernicke’s encephalopathy. Which of the following are early neurological manifestations?
Explanation
Hyperemesis gravidarum induces a critical state of micronutrient depletion where the persistent expulsion of gastric contents prevents the absorption of water-soluble vitamins. Thiamine, or Vitamin B1, is a mandatory cofactor for enzymes within the aerobic glucose oxidation pathway. Without this coenzyme, the brain cannot metabolize glucose, leading to acute adenosine triphosphate failure and subsequent neuronal death in the brainstem and diencephalon.
Wernicke encephalopathy is the most severe neurological complication of prolonged thiamine deficiency in hyperemesis. The condition is characterized by a classic clinical triad of global confusion, ataxia, and ophthalmoplegia such as nystagmus. Because pregnancy increases the metabolic demand for thiamine, a client with intractable vomiting can exhaust their limited hepatic stores within 2 to 3 weeks, leading to irreversible hemorrhagic lesions in the mammillary bodies.
Rationale for correct answers
1. Confusion is a primary neurological manifestation of Wernicke encephalopathy resulting from impaired cerebral energy metabolism. The client may exhibit disorientation, apathy, or a significantly decreased level of consciousness as the diencephalon suffers from thiamine depletion. This global cognitive impairment serves as a critical warning sign that the central nervous system is experiencing acute metabolic failure and requires immediate intravenous thiamine replacement.
2. Ataxia refers to an unsteady, uncoordinated, or broad-based gait caused by dysfunction in the cerebellum and vestibular system. In the context of hyperemesis, this motor deficit indicates that the thiamine deficiency has progressed to affect the structural integrity of the hindbrain. Identifying ataxia is essential because it is a pathognomonic feature of the Wernicke triad and distinguishes nutritional encephalopathy from simple dehydration or lethargy.
3. Ophthalmoplegia, particularly nystagmus or lateral rectus palsy, occurs due to lesions in the cranial nerve nuclei that control ocular movement. The eyes may exhibit involuntary rhythmic oscillations or an inability to move outward, reflecting damage to the abducens nerve. This ocular finding is a definitive diagnostic marker that, when combined with confusion and ataxia, confirms the presence of life-threatening thiamine deficiency.
Rationale for incorrect answers
4. Headache is a common, non-specific symptom in hyperemesis gravidarum that often results from dehydration, stress, or caffeine withdrawal. While a headache can be distressing, it is not a specific or diagnostic feature of the thiamine-induced neurological destruction seen in Wernicke encephalopathy. Using headache as a primary indicator would lead to inaccurate clinical screening, as it does not reflect the focal brainstem or cerebellar involvement characteristic of the condition.
5. Nausea is the underlying symptom of hyperemesis gravidarum itself and serves as the cause of the nutritional deficiency rather than a neurological manifestation of the encephalopathy. While persistent nausea leads to the starvation state, it does not provide information about the integrity of the central nervous system. Assessing nausea alone would fail to identify the transition from a gastrointestinal crisis to a permanent neurological emergency involving brain tissue damage.
Test-taking strategy
- Identify the Pathognomonic Triad: Memorize the "classic triad" for Wernicke: Confusion, Ataxia, and Ocular changes. These three symptoms (Choices 1, 2, 3) are the gold standard for this diagnosis.
- Link Nutrient to Symptom: Associate Thiamine (B1) with the brain's ability to "use sugar." If the brain can't use sugar, it gets "confused" and the body loses "coordination" (ataxia).
- Eliminate General Symptoms: Rule out Choice 4 and Choice 5 because they are too common. In high-stakes nursing questions, look for the symptoms that are unique to the specific complication mentioned.
- Assess the Anatomical Site: Wernicke affects the brainstem and cerebellum. Ataxia and eye movements are controlled there, which validates Choices 2 and 3.
- Prioritize Life-Threatening Indicators: While all choices may be present in a sick patient, only the first three represent the irreversible damage associated with encephalopathy.
Take home points
- The clinical triad of Wernicke encephalopathy consists of global confusion, ataxia, and ophthalmoplegia.
- Thiamine deficiency in hyperemesis can lead to irreversible brain damage (Korsakoff syndrome) if not treated within hours.
- Nurses must assess gait and eye movements in any client with weight loss > 5% and prolonged vomiting.
- Thiamine 100 mg to 500 mg IV must be administered before any glucose-containing fluids to prevent worsening the encephalopathy.
A nurse is assessing a client with severe hyperemesis gravidarum. Which of the following are clinical signs of dehydration?
Explanation
Hyperemesis gravidarum induces an acute extracellular fluid volume deficit resulting from the intractable expulsion of gastric hydrochloric acid and water. This hypovolemia triggers a compensatory shift of interstitial fluid into the intravascular compartment to maintain perfusion, leading to observable mucosal desiccation and reduced intraocular pressure. Severe cases progress to hemoconcentration as the homeostatic baroreceptor response becomes overwhelmed by continuous fluid loss.
Rationale for correct answers
1. Dry mucous membranes are a primary clinical sign of dehydration resulting from the depletion of the interstitial fluid compartment. As total body water decreases, the salivary glands fail to maintain oral lubrication, leading to a "sticky" or parched appearance of the tongue and buccal mucosa. This finding serves as definitive clinical evidence that the body has moved into a state of systemic fluid volume deficit.
2. Sunken eyes occur when the periorbital fat pads and the vitreous body lose hydration and volume due to prolonged fluid loss. The reduction in intraocular pressure causes the globes to recede within the orbits, creating a hollowed appearance. This is typically considered a sign of moderate to severe dehydration and indicates that compensatory mechanisms are failing to protect the most sensitive tissue compartments.
4. Tachycardia is the most sensitive early cardiovascular indicator of hypovolemia as the body attempts to maintain cardiac output. As the stroke volume declines due to fluid loss, the heart must beat faster to ensure adequate systemic and placental perfusion. A heart rate > 100 beats per minute in a resting client confirms that the sympathetic nervous system has been activated to compensate for the decreased blood volume.
Rationale for incorrect answers
3. Normal skin turgor is a sign of adequate fluid balance where the dermal and subcutaneous layers remain elastic and hydrated. In severe dehydration, the nurse would instead observe "tenting," where the skin fails to return to its original position after being pinched. Because this choice represents a healthy finding, it cannot be used to indicate a complication as severe as pathological dehydration in a hyperemesis client.
5. Increased urine output is physiologically impossible in a state of severe dehydration unless the patient has a concurrent condition like diabetes insipidus. The kidneys respond to hypovolemia by releasing antidiuretic hormone and activating the renin-angiotensin-aldosterone system to conserve water. This results in oliguria (output < 30 mL/hr) and highly concentrated urine, rather than an increase in fluid excretion.
Test-taking strategy
- Identify the Physiological State: Categorize each option as a sign of "volume up," "volume down," or "normal volume."
- Eliminate Normalcy: Rule out Choice 3 (Normal turgor) because the question specifically asks for signs of a pathological state (dehydration).
- Apply Renal Physiology: Remember that the kidney's job in dehydration is to save water. This immediately invalidates Choice 5 (Increased output).
- Look for "Dry" Indicators: Choice 1 and Choice 2 are classic physical assessment findings for the loss of water from the "padding" and "lining" of the body.
- Assess the Heart's Response: Recall that when volume (preload) is low, the heart rate must go up to maintain blood pressure. This validates Choice 4 (Tachycardia).
Take home points
- Dry mucous membranes and sunken eyes are visible markers of interstitial and intracellular fluid loss.
- Tachycardia and orthostatic hypotension are the primary hemodynamic compensations for decreased intravascular volume.
- Dehydration leads to oliguria and increased urine specific gravity (≥ 1.030) as the kidneys attempt to conserve water.
- Poor skin turgor (tenting) over the sternum or forearm is a late-stage physical indicator of severe volume depletion.
A nurse is identifying risk factors for hyperemesis gravidarum. Which of the following are recognized risk factors? Select all that apply
Explanation
Hyperemesis gravidarum is associated with elevated concentrations of human chorionic gonadotropin (hCG) and estrogen, which stimulate the chemoreceptor trigger zone in the brainstem. Conditions that increase the total placental mass or the sensitivity of the vestibular system significantly predispose the client to intractable vomiting. Physiological hyperthyroidism of pregnancy, mediated by the structural similarity between hCG and thyroid-stimulating hormone, may also play a secondary role in the pathogenesis of severe emetic symptoms.
Rationale for correct answers
1. Multiple gestation is a recognized risk factor because the presence of more than one fetus leads to a significantly higher total placental mass and increased serum hCG levels. These elevated hormonal concentrations place a greater metabolic and chemical burden on the maternal medullary emetic centers. Statistics indicate that women carrying twins or triplets have a markedly higher incidence of severe nausea compared to those with singleton pregnancies.
2. Molar pregnancy, or gestational trophoblastic disease, involves the abnormal proliferation of trophoblastic tissue which produces extreme levels of hCG. The rapid and excessive hormonal surge often results in the early and severe onset of hyperemesis symptoms. Nurses must screen clients with severe vomiting for this condition using ultrasound to differentiate a viable pregnancy from a hydatidiform mole.
3. A history of migraines is a predisposing factor that suggests a baseline sensitivity of the central nervous system to hormonal or sensory triggers. Women who suffer from migraines may have a more reactive vestibular system or altered serotonin metabolism, both of which are involved in the emetic reflex. This neurological predisposition makes the individual more susceptible to the nausea-inducing effects of pregnancy-related hormonal shifts.
Rationale for incorrect answers
4. A male fetus is not a recognized risk factor for the development of hyperemesis gravidarum. Clinical research has actually demonstrated a stronger correlation between female fetuses and severe nausea, likely due to the additional estrogenic load associated with female gestations. Carrying a male fetus does not typically involve the specific hormonal elevations required to trigger the intractable vomiting seen in this condition.
5. Obesity is generally not classified as a primary risk factor for the onset of hyperemesis gravidarum. While high body mass index is associated with other gestational complications like preeclampsia and gestational diabetes, it does not correlate with the hCG-driven pathology of hyperemesis. In fact, many clinical observations note that hyperemesis is frequently seen in women with a lower or normal baseline body mass index.
Test-taking strategy
- Identify the Hormonal Link: Recognize that hyperemesis is driven by "too much" hCG. Choice 1 (multiple babies) and Choice 2 (molar pregnancy) both cause massive hCG spikes.
- Recall Neurosensory Links: Think of hyperemesis as a "sensitive brain" issue. This helps you group it with other sensitivity disorders like migraines (Choice 3) or motion sickness.
- Filter Gender Trends: Remember the "Girl Rule"—hyperemesis is more common with female fetuses. This eliminates Choice 4.
- Distinguish Complications: Don't confuse hyperemesis with metabolic syndrome. Choice 5 (obesity) is a risk for "sugar and pressure" problems, not typically "vomiting" problems.
- Look for "Placental Volume": Any condition that makes the placenta bigger or more active increases the risk. This validates both Choices 1 and 2.
Take home points
- Conditions that increase hCG levels, such as multiple gestations and molar pregnancies, are primary risk factors for hyperemesis.
- A personal or family history of hyperemesis, migraines, or motion sickness increases an individual's susceptibility.
- Women carrying a female fetus have a higher statistical risk of developing severe nausea and vomiting.
- Hyperemesis is fundamentally a hormonal and neurochemical disorder rather than one driven by maternal weight or lifestyle.
A nurse is reviewing the laboratory results of a client admitted with hyperemesis gravidarum. Which of the following findings are commonly associated with this condition? Select all that apply
Explanation
Hyperemesis gravidarum induces a state of profound metabolic and hemodynamic instability resulting from the intractable loss of gastric secretions. The continuous expulsion of hydrochloric acid, water, and electrolytes triggers a compensatory shift in maternal homeostasis, leading to a transition from carbohydrate to fat metabolism. This results in the accumulation of acidic byproducts and a relative increase in the concentration of formed elements within the blood as the plasma volume contracts during acute hypovolemia.
Rationale for correct answers
1. Ketonuria is a hallmark finding of hyperemesis resulting from the body's transition into a state of starvation ketosis. Once hepatic glycogen stores are exhausted (typically within 24 hours), the body initiates lipolysis to meet metabolic demands, producing ketone bodies such as acetoacetate. The presence of these ketones in the urine (1+ to 4+) confirms that maternal carbohydrate reserves are depleted and the body is in a catabolic state.
2. Hypokalemia (serum potassium < 3.5 mEq/L) occurs due to the direct loss of potassium in gastric juice and secondary renal wasting. As the body becomes dehydrated, the activation of the renin-angiotensin-aldosterone system causes the kidneys to retain sodium and water at the expense of potassium excretion. Severe hypokalemia is a critical finding as it can precipitate life-threatening cardiac arrhythmias and muscle weakness.
3. Hyponatremia (serum sodium < 135 mEq/L) develops from the significant loss of sodium in emesis combined with the compensatory release of antidiuretic hormone. ADH causes the kidneys to reabsorb free water, which further dilutes the remaining extracellular sodium concentration. This electrolyte imbalance can lead to neurological symptoms such as lethargy, confusion, or even seizures if the decline in sodium is rapid and severe.
5. Elevated hemoglobin is a classic sign of hemoconcentration resulting from a decrease in total intravascular volume. When the liquid portion of the blood (plasma) is lost through vomiting and inadequate intake, the cellular components become more densely packed. This relative elevation does not indicate an increase in red cell production but rather serves as an objective marker of the severity of maternal dehydration.
Rationale for incorrect answers
4. Hyperglycemia is not a typical finding in hyperemesis gravidarum; rather, clients are more prone to hypoglycemia. Due to intractable vomiting and the inability to maintain oral intake, maternal glucose levels frequently drop as glycogen stores are consumed. Elevated blood sugar is more characteristic of gestational diabetes, whereas hyperemesis is fundamentally a condition of nutrient and energy deficiency.
Test-taking strategy
- Identify the Physiological Theme: Hyperemesis is a "loss" disease. Focus on laboratory values that represent depletion (Hypo-) or concentration (Elevated Hgb).
- Connect Starvation to Lab Markers: Recall that "vomiting = not eating = burning fat." This makes Choice 1 (Ketonuria) a mandatory selection for this condition.
- Analyze Fluid Shifts: Understand that when the "water" leaves the blood, the "solids" stay behind. This explains why Choice 5 (Elevated Hgb) is a sign of dehydration, not health.
- Match Electrolytes to Gastric Loss: Gastric juices are rich in salt and acid. Losing them leads to "Low Sodium" (Choice 3) and "Low Potassium" (Choice 2).
- Rule out Excesses: Choice 4 (Hyperglycemia) describes an "excess" of fuel, which contradicts the "starvation" state of a patient who cannot keep food down.
Take home points
- Ketonuria (presence of ketones in urine) is a primary indicator of starvation and fat catabolism in hyperemesis.
- Hypokalemia and hyponatremia are common electrolyte derangements that require careful intravenous replacement.
- Hemoconcentration (elevated hematocrit and hemoglobin) serves as an objective measure of intravascular fluid volume deficit.
- Metabolic alkalosis is the initial acid-base disturbance, which may shift to metabolic acidosis if ketosis becomes severe.
A nurse is planning care for a client with hyperemesis gravidarum. Which of the following nursing interventions are appropriate for managing nausea? Select all that apply
Explanation
Hyperemesis gravidarum necessitates a multimodal therapeutic approach to suppress the overactive emetic reflex arc and stabilize the maternal gastrointestinal environment. Management focuses on pharmaceutical antagonism of serotonin receptors in the chemoreceptor trigger zone and the modulation of afferent neural pathways. By reducing environmental and mechanical triggers, the nurse aims to raise the emetic threshold and facilitate a return to metabolic homeostasis.
Rationale for correct answers
1. Administering ondansetron is an appropriate pharmacological intervention as it acts as a selective 5-HT3 receptor antagonist. By blocking serotonin receptors on the vagus nerve and in the area postrema of the brainstem, it effectively interrupts the signaling pathway that triggers forceful emesis. This medication is a standard second-line therapy when first-line options like pyridoxine (Vitamin B6) fail to provide adequate relief for refractory nausea.
2. Using acupressure wristbands (such as Sea-Bands) is a non-pharmacological strategy that targets the P6 (Neiguan) point on the inner wrist. Stimulation of this pressure point is thought to modulate the parasympathetic nervous system and reduce the perception of nausea without the risk of systemic side effects. It provides a low-risk, supplementary option for clients seeking complementary therapies to manage persistent gestational emesis.
4. Providing a calm, low-stimulus environment is essential to minimize external sensory triggers that can aggravate the medullary emetic center. Strong odors, bright lights, and loud noises can act as potentiating stimuli that precipitate vomiting in a highly sensitized client. By creating a quiet and odor-free space, the nurse reduces the physiological stress on the client's nervous system, promoting relaxation and symptomatic stability.
Rationale for incorrect answers
3. Encouraging large meals is contraindicated as gastric overdistension is a primary mechanical trigger for the emetic reflex. In clients with hyperemesis, gastric motility is often delayed, meaning large volumes lead to prolonged stasis and increased intraluminal pressure. This would directly exacerbate the symptoms and likely lead to immediate expulsion of the food, worsening the dehydration and nutritional deficit.
5. Offering high-fat foods is inappropriate because lipids significantly slow the rate of gastric emptying and relax the lower esophageal sphincter. A high-fat intake prolongs the presence of food in the stomach, increasing the likelihood of reflux and nausea. For successful dietary rehabilitation, the focus should instead be on high-protein and dry carbohydrate choices, which are processed more efficiently by the compromised digestive system.
Test-taking strategy
- Identify Therapy Categories: This question includes both pharmacological and non-pharmacological interventions. Ensure you look for "holistic" options like environment and acupressure.
- Apply the "Small and Frequent" Rule: In almost all NCLEX-style GI questions, "large meals" are always the wrong choice.
- Filter by Macronutrients: Remember that fat is the enemy of a nauseated stomach. Protein is the preferred substrate for stabilizing gastric rhythms.
- Assess Sensory Triggers: For a patient with severe nausea, anything that lowers "stress" on the senses (Choice 4) is a priority nursing action.
- Evaluate Complementary Care: Acknowledge that the NCLEX and nursing boards often value evidence-based non-drug options like acupressure (Choice 2).
Take home points
- 5-HT3 antagonists like Ondansetron are effective for suppressing the central and peripheral triggers of emesis.
- Non-pharmacological interventions like P6 acupressure and ginger are useful adjuncts to standard medical therapy.
- Environmental control (minimizing odors and noise) is a critical nursing priority for a sensitized emetic center.
- Dietary management must avoid high-fat and large-volume intake to prevent gastric stasis and distension.
A nurse is educating a client with severe hyperemesis gravidarum about potential fetal risks. Which of the following complications may result from this condition? Select all that apply
Explanation
Hyperemesis gravidarum presents a significant metabolic threat to the developing fetus due to the persistent state of maternal starvation and dehydration. The disruption of the maternal-fetal nutritional interface leads to the depletion of glucose and amino acid supplies required for cellular hyperplasia and hypertrophy. Furthermore, chronic hypovolemia can result in persistent uterine artery vasoconstriction, which compromises the delivery of oxygen and essential nutrients to the placental bed.
Rationale for correct answers
1. Intrauterine growth restriction (IUGR) is a recognized complication because the fetus may not receive the caloric density required for optimal development. When maternal glycogen stores are exhausted and the body enters a catabolic state, the fetus is deprived of the primary energy substrates needed for growth. This prolonged nutritional deficit can lead to a fetus that fails to reach its biological growth potential, often manifesting as a birth weight below the 10th percentile for gestational age.
2. Low birth weight is a frequent outcome in pregnancies complicated by severe hyperemesis, especially when maternal weight loss exceeds 5 percent of pre-pregnancy mass. The lack of protein and fat intake prevents the accumulation of fetal adipose tissue during the third trimester. Research consistently correlates the severity of maternal malnutrition with a reduction in the total birth weight of the neonate, increasing the risk for neonatal hypoglycemia and thermoregulation issues.
3. Preterm birth is a potential complication triggered by the physiological stress and inflammatory environment associated with severe dehydration and electrolyte imbalances. Maternal starvation leads to the production of ketones and a shift in the neuroendocrine axis that can stimulate premature uterine activity. Additionally, the medical necessity to deliver the fetus early may arise if maternal organ systems, such as the kidneys or liver, begin to fail due to the intractable nature of the condition.
Rationale for incorrect answers
4. Macrosomia, defined as a birth weight > 4000 grams, is associated with gestational diabetes and excessive maternal weight gain, not hyperemesis. Hyperemesis represents a state of caloric deficiency and wasting, which is the physiological opposite of the over-nutrition required to produce a macrosomic infant. A client struggling to maintain any oral intake is statistically unlikely to deliver an infant with excessive adipose tissue accumulation.
5. Congenital anomalies are structural defects that typically occur during the period of organogenesis (the first 10 weeks of gestation). While hyperemesis occurs during this timeframe, it is fundamentally a nutritional and fluid disorder rather than a teratogenic one. Most clinical studies have not found a significant increase in the baseline rate of structural malformations among infants born to mothers with hyperemesis, provided that critical micronutrients like folic acid and thiamine are eventually replaced.
Test-taking strategy
- Identify the Physiological Theme: Hyperemesis is a "deficiency" state. Look for choices that reflect "smallness" or "loss" (Choices 1 and 2).
- Connect Nutrition to Growth: Recall that without maternal glucose and protein, the fetus cannot gain weight. This makes IUGR and Low Birth Weight mandatory selections.
- Assess Stress Responses: Understand that any severe systemic illness in the mother (like dehydration or ketosis) acts as a trigger for preterm labor (Choice 3).
- Rule out Opposites: Eliminate Choice 4 (Macrosomia) because it is a "growth excess" condition, which contradicts the "growth restriction" typical of vomiting and starvation.
- Distinguish Pathogenesis: Recognize that Choice 5 (Anomalies) usually relates to genetics or toxins, not simple vomiting, unless it leads to a specific, severe vitamin deficiency.
Take home points
- Intrauterine growth restriction (IUGR) occurs when maternal malnutrition limits the nutrients available for fetal cellular development.
- Preterm birth in hyperemesis is often linked to the metabolic stress of dehydration and maternal ketosis.
- Infants of mothers with severe weight loss (> 5%) have a significantly higher risk of being born small for gestational age (SGA).
- Aggressive nutritional support (Parenteral or Enteral) can mitigate these fetal risks by restoring maternal glucose and nitrogen balance.
A nurse is caring for a client with hyperemesis gravidarum who requires intravenous therapy. Which of the following interventions are critical to prevent Wernicke’s encephalopathy? Select all that apply
Explanation
Hyperemesis gravidarum represents a critical metabolic state where the continuous depletion of water-soluble vitamins puts the central nervous system at risk. Thiamine acts as an essential coenzyme for the pyruvate dehydrogenase complex within the aerobic glucose oxidation pathway. Introduction of high-load carbohydrate substrates without sufficient B1 stores precipitates acute neuronal oxidative stress and ATP failure, particularly in the brainstem.
Rationale for correct answers
1. Administering thiamine before dextrose-containing fluids is the most critical intervention to prevent the iatrogenic precipitation of Wernicke encephalopathy. Thiamine is a mandatory cofactor for metabolic enzymes that process glucose into cellular energy. If concentrated dextrose is infused into a depleted patient, the remaining B1 is rapidly exhausted, leading to catastrophic neurotoxicity and cellular death in the mammillary bodies.
2. Monitoring neurological status is essential for the early identification of subtle changes in mentation or consciousness that precede permanent brain damage. The nurse must perform serial assessments of orientation, alertness, and cognitive function to ensure that the maternal brain is not suffering from metabolic failure. Early detection of decreased responsiveness allows for the immediate escalation of parenteral thiamine therapy before lesions become irreversible.
4. Assessing for confusion and ataxia focuses on identifying two of the three pathognomonic signs of the Wernicke clinical triad. Ataxia, or an unsteady gait, indicates cerebellar dysfunction, while confusion reflects global cerebral energy failure. Identifying these neuromuscular deficits is a priority nursing action to differentiate simple lethargy from a life-threatening nutritional emergency requiring intensive vitamin replacement.
Rationale for incorrect answers
3. Providing oral glucose supplements is inappropriate for a client with severe hyperemesis who is already in a state of intractable vomiting. Oral intake will likely be expelled immediately, failing to provide any metabolic benefit and potentially triggering further gastric irritation. Furthermore, providing any form of glucose without first ensuring adequate thiamine levels carries the same neurological risk as intravenous dextrose.
5. Encouraging high-carbohydrate meals is contraindicated during the acute phase of hyperemesis when Wernicke risk is highest. Carbohydrates increase the metabolic demand for thiamine, and if the client's B1 stores are already low, a sudden carbohydrate load can trigger encephalopathy. Additionally, high-carbohydrate loads are often poorly tolerated by the gastric mucosa in a client suffering from persistent nausea and vomiting.
Test-taking strategy
- Identify the Mechanism: Wernicke is caused by a thiamine (B1) deficiency. Any correct answer must relate to replacing B1 or checking for brain damage.
- Recall the Clinical Rule: Memorize the phrase "B1 before D5." Never give dextrose (sugar) before thiamine (Choice 1) in a starved patient.
- Select Diagnostic Triad: Look for the classic symptoms: Confusion, Ataxia, and Ocular changes. This validates Choice 4.
- Evaluate Route of Delivery: A hyperemesis patient cannot use the "oral" route reliably. Eliminate Choice 3 and Choice 5 because they rely on the stomach, which is the site of the primary pathology.
- Prioritize Safety: Choice 2 is a broad, safe assessment that covers the "Neuro" part of the ABCs for a metabolic patient.
Take home points
- Thiamine (Vitamin B1) must be administered prior to any glucose-containing IV fluids to prevent Wernicke encephalopathy.
- The classic diagnostic triad includes global confusion, ataxia (unsteady gait), and ophthalmoplegia (nystagmus).
- Iatrogenic encephalopathy occurs when a glucose load exhausts the last remaining maternal thiamine reserves.
- Prompt recognition and high-dose IV thiamine can reverse early symptoms and prevent permanent Korsakoff syndrome.
Exams on Hyperemesis Gravidarum
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
- Objectives
- Introduction
- Pathophysiology Of Hyperemesis Gravidarum
- Practice Exercise 1
- Risk Factors And Epidemiology
- Practice Exercise 2
- Clinical Manifestations And Diagnostic Criteria
- Practice Exercise 3
- Laboratory And Diagnostic Findings
- Practice Exercise 4
- Maternal And Fetal Complications
- Practice Exercise 5
- Medical And Nursing Management
- Practice Exercise 6
- Nursing Assessment And Priority Interventions
- Practice Exercise 7
- Summary
- Comprehensive Questions
Notes Highlighting is available once you sign in. Login Here.
Objectives
At the completion of this section, the nursing student will be able to:
- Explain the complex pathophysiological mechanisms involved in hyperemesis gravidarum using scientific medical terminology.
- Analyze the role of hormonal, gastrointestinal, neurological, metabolic, endocrine, psychological, and genetic factors in the development of hyperemesis gravidarum.
- Correlate pathophysiological changes with clinical manifestations and laboratory abnormalities observed in affected clients.
- Apply pathophysiological knowledge to clinical nursing decision-making, prioritization of care, and early identification of complications.
- Demonstrate NCLEX-level critical thinking by answering application-based practice questions related to the pathophysiology of hyperemesis gravidarum.
Introduction
Hyperemesis gravidarum is a severe, pathological form of nausea and vomiting of pregnancy characterized by persistent, intractable vomiting that leads to significant maternal dehydration, electrolyte imbalance, nutritional deficiencies, ketosis, and weight loss exceeding 5% of pre-pregnancy weight. Unlike normal nausea and vomiting of pregnancy, hyperemesis gravidarum results in systemic physiological derangements requiring medical intervention and often hospitalization.
This condition typically presents during the first trimester, with peak severity between 9–12 weeks of gestation, coinciding with maximal elevations in pregnancy-related hormones. Hyperemesis gravidarum affects approximately 0.3–2% of pregnancies and represents a leading cause of early pregnancy hospitalization.
From a nursing perspective, understanding the multifactorial pathophysiology is essential for early recognition, prevention of complications, and implementation of targeted interventions to protect both maternal and fetal well-being.
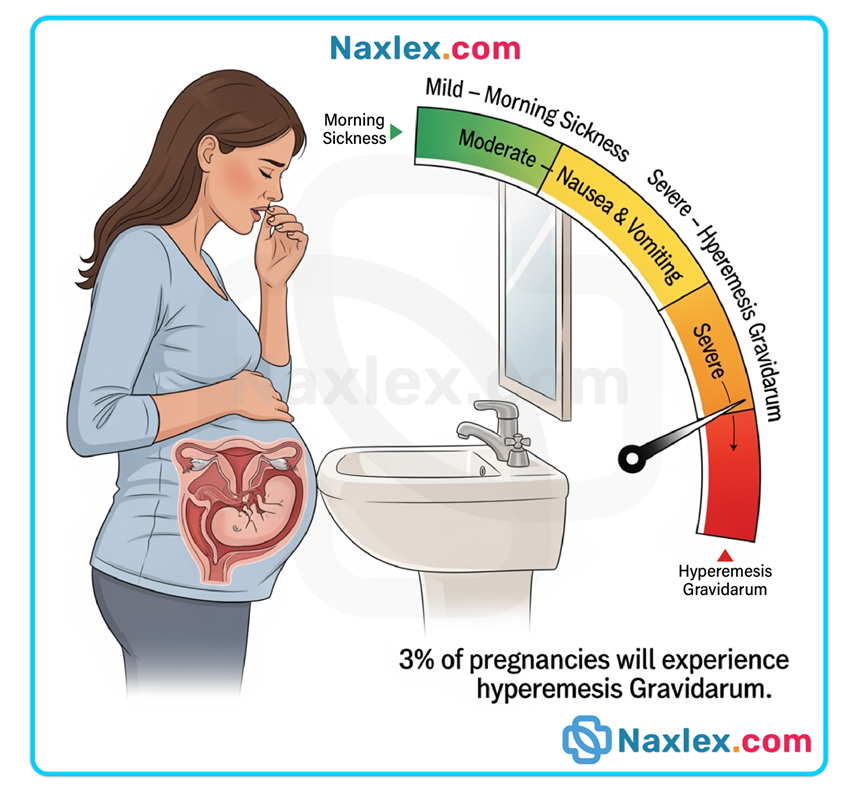
Pathophysiology Of Hyperemesis Gravidarum
Hyperemesis gravidarum is caused by a multisystem interaction involving endocrine, gastrointestinal, neurological, metabolic, and psychological pathways. No single mechanism fully explains the condition; rather, it results from synergistic physiological disturbances.
1.1 Hormonal Factors
Hormonal alterations in early pregnancy play a central role in the development of hyperemesis gravidarum.
- Human Chorionic Gonadotropin (hCG):
- hCG levels peak during the first trimester, temporally correlating with symptom onset and severity.
- hCG stimulates the chemoreceptor trigger zone (CTZ) in the medulla oblongata, increasing nausea and vomiting.
- Structural similarity between hCG and thyroid-stimulating hormone (TSH) leads to transient gestational hyperthyroidism, exacerbating nausea.
- Elevated hCG is associated with:
- Multiple gestations
- Molar pregnancy
- Female or male fetal sex (variable evidence)
- Estrogen:
- Increases olfactory sensitivity, heightening nausea triggered by odors.
- Delays gastric emptying and increases gastrointestinal sensitivity.
- Progesterone:
- Relaxes smooth muscle throughout the gastrointestinal tract.
- Reduces gastric motility and delays gastric emptying.
- Decreases lower esophageal sphincter tone, increasing reflux and emesis.
Nursing Insights
- Severe vomiting in the first trimester should prompt evaluation for conditions associated with excessive hCG, including molar pregnancy.
- Nurses must recognize that thyroid function abnormalities in hyperemesis gravidarum are usually transient and hormone-mediated, not primary thyroid disease.
1.2 Gastrointestinal and Neurological Mechanisms
Neurological and gastrointestinal dysfunction significantly contribute to symptom severity.
- Central Nervous System Involvement:
- Activation of the chemoreceptor trigger zone (CTZ) responds to circulating hormones and metabolic byproducts.
- The vomiting center integrates signals from:
- Vestibular system
- Gastrointestinal tract
- Cerebral cortex
- Gastrointestinal Changes:
- Decreased gastric motility leads to gastric distention and nausea.
- Delayed gastric emptying worsens vomiting frequency.
- Repeated emesis causes:
- Esophageal irritation
- Risk of esophageal tears
- Electrolyte depletion
- Autonomic Nervous System Dysregulation:
- Increased parasympathetic stimulation intensifies nausea.
- Heightened vagal tone contributes to persistent vomiting.
Nursing Insights
- Persistent vomiting without relief throughout the day suggests central neurological involvement, not typical morning sickness.
- Nurses should monitor for signs of esophageal injury, including hematemesis and chest discomfort.
1.3 Metabolic and Endocrine Changes
Sustained vomiting leads to profound metabolic disturbances.
- Fluid and Electrolyte Imbalances:
- Loss of hydrochloric acid causes metabolic alkalosis.
- Common electrolyte abnormalities include:
- Hypokalemia
- Hyponatremia
- Hypochloremia
- Starvation and Ketosis:
- Inadequate caloric intake results in fat metabolism.
- Ketone production leads to ketonuria and ketonemia.
- Ketosis further stimulates the vomiting center, creating a vicious cycle.
- Vitamin Deficiencies:
- Thiamine (Vitamin B1) depletion occurs rapidly.
- Administration of glucose without thiamine precipitates Wernicke’s encephalopathy.
Nursing Insights
- Thiamine must always be administered before dextrose-containing fluids.
- Ketonuria is a hallmark indicator of starvation and disease severity.
1.4 Psychological and Genetic Influences
Psychological and genetic predispositions modulate symptom expression.
- Psychological Factors:
- Stress and anxiety amplify nausea via cortical stimulation of the vomiting center.
- Depression and emotional distress worsen symptom perception.
- Genetic Factors:
- Increased incidence among first-degree relatives.
- Association with genes involved in:
- Placental development
- Hormonal sensitivity
- Conditioned Responses:
- Learned aversions to foods and smells perpetuate vomiting.
Nursing Insights
- Emotional validation and psychological support reduce symptom severity.
- Nurses should assess coping mechanisms and provide nonjudgmental support, recognizing that symptoms are physiological, not voluntary.
Risk Factors And Epidemiology
Hyperemesis gravidarum is a multifactorial disorder with clearly identified epidemiological trends and predisposing risk factors. Recognition of these risk factors allows nurses to identify high-risk clients early, initiate anticipatory guidance, and implement preventive interventions to reduce maternal and fetal morbidity.
1.1 Maternal Risk Factors
Several maternal characteristics significantly increase susceptibility to hyperemesis gravidarum due to genetic, physiological, and psychosocial influences.
- History of Hyperemesis Gravidarum
- The strongest predictor of recurrence in subsequent pregnancies.
- Recurrence rates range from 15–80%, indicating a strong individual predisposition.
- Genetic Predisposition
- Increased incidence among first-degree relatives.
- Suggests inherited sensitivity to pregnancy-related hormonal changes.
- Nulliparity
- First-time pregnant clients experience higher rates due to:
- Lack of physiological adaptation to pregnancy hormones
- Increased psychological stress
- First-time pregnant clients experience higher rates due to:
- Advanced Maternal Age
- Altered metabolic and endocrine responsiveness may exacerbate symptoms.
- Psychological Factors
- Anxiety, depression, and high stress levels amplify symptom severity through:
- Cortical stimulation of the vomiting center
- Increased autonomic nervous system activation
- Anxiety, depression, and high stress levels amplify symptom severity through:
- History of Motion Sickness or Migraines
- Indicates heightened vestibular sensitivity.
- Shared neurological pathways with nausea and vomiting mechanisms.
Nursing Insights
- A detailed obstetric history is essential, as prior hyperemesis gravidarum strongly predicts recurrence.
- Nurses should proactively screen for anxiety and depression, as psychological distress worsens symptom severity and prolongs hospitalization.
1.2 Pregnancy-Related Risk Factors
Pregnancy-specific conditions that elevate hormone levels or placental mass significantly increase the likelihood of hyperemesis gravidarum.
- Multiple Gestations
- Increased placental tissue leads to elevated hCG levels.
- Greater hormonal stimulation of the chemoreceptor trigger zone.
- Molar Pregnancy
- Abnormally high hCG production.
- Often associated with severe, early-onset hyperemesis gravidarum.
- Requires prompt ultrasound evaluation.
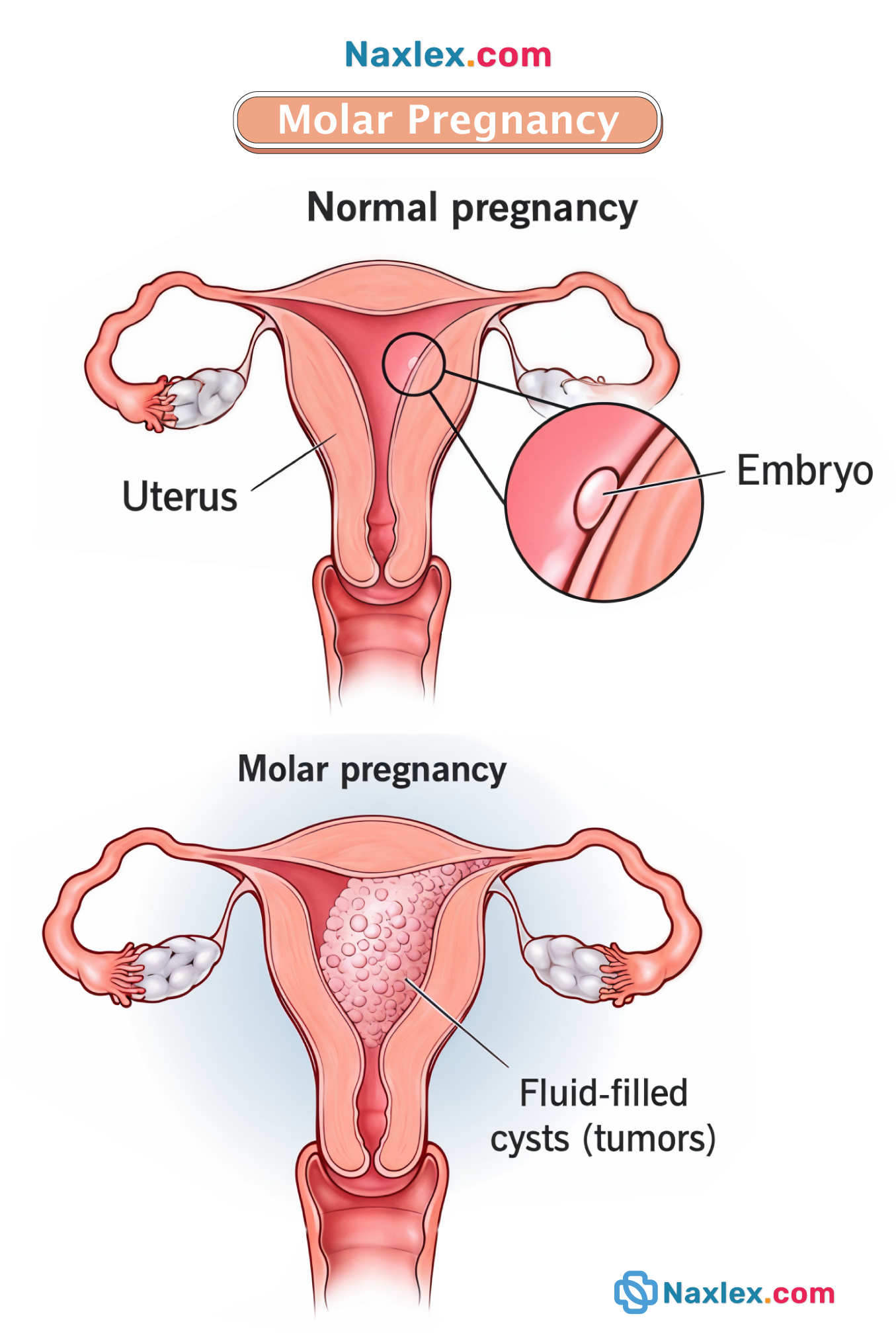
- Fetal Sex
- Some studies associate female fetuses with increased risk due to higher estrogen exposure.
- Evidence remains variable and not diagnostic.
- Early Gestational Age
- Symptoms peak during 9–12 weeks gestation, correlating with maximal hCG levels.
Nursing Insights
- Severe vomiting early in pregnancy should raise suspicion for molar pregnancy, especially when accompanied by uterine size greater than dates.
- Nurses must advocate for diagnostic imaging when clinical severity exceeds expected gestational norms.
1.3 Associated Medical Conditions
Certain medical conditions are associated with increased risk due to hormonal sensitivity, immune response, or gastrointestinal involvement.
- Helicobacter pylori Infection
- Strongly associated with hyperemesis gravidarum.
- Increases gastric inflammation and nausea.
- Thyroid Disorders
- hCG-mediated stimulation of thyroid receptors can cause transient hyperthyroidism.
- Thyroid dysfunction exacerbates nausea and vomiting.
- Gastrointestinal Disorders
- Preexisting conditions such as:
- Gastroesophageal reflux disease
- Peptic ulcer disease
- Increase symptom severity due to baseline gastric sensitivity.
- Preexisting conditions such as:
- Metabolic Conditions
- Poor nutritional reserves predispose to rapid ketosis and dehydration.
Nursing Insights
- Nurses should recognize that thyroid abnormalities in hyperemesis gravidarum are usually secondary to hCG stimulation, not primary thyroid disease.
- Assessment for Helicobacter pylori may be indicated in refractory cases.
Clinical Manifestations And Diagnostic Criteria
Hyperemesis gravidarum presents with progressive, systemic clinical manifestations that extend beyond normal nausea and vomiting of pregnancy. Accurate identification relies on comprehensive maternal assessment, recognition of severity, and exclusion of alternative diagnoses. Early nursing recognition is critical to prevent life-threatening metabolic, neurological, and fetal complications.
1.1 Maternal Signs and Symptoms
Maternal manifestations result from persistent vomiting, dehydration, electrolyte imbalance, and malnutrition.
- Gastrointestinal Manifestations
- Persistent, uncontrollable nausea and vomiting occurring throughout the day
- Vomiting unrelieved by dietary intake
- Inability to tolerate oral fluids or foods
- Hypersensitivity to odors and visual stimuli
- Epigastric pain secondary to gastric irritation
- Nutritional and Metabolic Manifestations
- Weight loss >5% of pre-pregnancy weight
- Ketonuria due to fat metabolism
- Signs of starvation including fatigue and weakness
- Fluid Volume Deficit Indicators
- Dry mucous membranes
- Sunken eyes
- Decreased skin turgor
- Oliguria with concentrated urine
- Urine specific gravity >1.030
- Cardiovascular and Hemodynamic Changes
- Tachycardia
- Orthostatic hypotension
- Hypotension in severe dehydration
- Neurological Manifestations
- Dizziness and lightheadedness
- Confusion or altered mental status
- Ataxia and nystagmus indicating thiamine deficiency
- Risk of Wernicke’s encephalopathy
- Psychological Manifestations
- Anxiety related to symptom severity
- Depression due to prolonged illness
- Feelings of helplessness and guilt
Nursing Insights
- Persistent vomiting with ketonuria and weight loss differentiates hyperemesis gravidarum from normal nausea and vomiting of pregnancy.
- Neurological changes represent a medical emergency and require immediate intervention.
1.2 Severity Classification
Severity is classified based on degree of dehydration, metabolic derangement, and nutritional compromise.
|
Severity Level |
Clinical Characteristics |
|
Mild |
Persistent nausea with occasional vomiting, minimal weight loss |
|
Moderate |
Frequent vomiting, weight loss up to 5%, ketonuria, dehydration |
|
Severe |
Continuous vomiting, weight loss >5%, electrolyte imbalance, ketonuria, neurological symptoms |
- Severe hyperemesis gravidarum often requires hospitalization for:
- Intravenous fluid replacement
- Electrolyte correction
- Nutritional support
Nursing Insights
- Severity classification guides level of care, including outpatient versus inpatient management.
- Early escalation prevents progression to organ dysfunction.
1.3 Diagnostic Criteria and Differential Diagnosis
Diagnosis is clinical, supported by laboratory findings and exclusion of other causes.
Diagnostic Criteria
- Persistent vomiting not related to other medical conditions
- Weight loss exceeding 5% of pre-pregnancy weight
- Ketonuria indicating starvation
- Electrolyte imbalance (hypokalemia, hyponatremia)
- Dehydration requiring medical intervention
Differential Diagnosis
- Normal nausea and vomiting of pregnancy
- Symptoms improve with dietary intake
- No ketonuria or significant weight loss
- Gastrointestinal Disorders
- Gastroenteritis
- Peptic ulcer disease
- Pancreatitis
- Endocrine Disorders
- Thyroid disease
- Diabetic ketoacidosis
- Pregnancy-Related Conditions
- Molar pregnancy
- Multiple gestations
- Neurological Causes
- Increased intracranial pressure
- Migraine disorders
Nursing Insights
- Ultrasound is essential to exclude molar pregnancy in early severe cases.
- Nurses must advocate for comprehensive evaluation when symptoms are disproportionate to gestational age.
Laboratory And Diagnostic Findings
Laboratory and diagnostic evaluation in hyperemesis gravidarum is essential to confirm severity, identify life-threatening metabolic derangements, and exclude alternative medical or obstetric conditions. Findings reflect prolonged vomiting, starvation, dehydration, and endocrine disturbances. Nurses play a critical role in interpreting trends, not isolated values, and correlating them with clinical status.
1.1 Electrolyte and Metabolic Abnormalities
Persistent emesis leads to loss of gastric contents, intravascular volume depletion, and secondary metabolic disturbances.
- Electrolyte Imbalances
- Hypokalemia < 3.5 mEq/L.
- Caused by potassium loss through vomiting and renal compensation
- Increases risk for cardiac dysrhythmias and muscle weakness
- Hyponatremia < 135 mEq/L.
- Results from excessive free water intake without electrolyte replacement
- Contributes to neurological symptoms including confusion and lethargy
- Hypochloremia < 98 mEq/L.
- Due to loss of hydrochloric acid
- Associated with metabolic alkalosis
- Hypokalemia < 3.5 mEq/L.
- Acid–Base Imbalance
- Metabolic alkalosis
- Primary disturbance caused by loss of gastric hydrochloric acid
- Characterized by arterial pH >7.45
- Metabolic acidosis
- May occur later due to starvation ketosis
- Metabolic alkalosis
- Hematologic Changes
- Elevated hemoglobin and hematocrit
- Reflect hemoconcentration from dehydration
- Elevated hemoglobin and hematocrit
- Renal Function Indicators
- Elevated blood urea nitrogen (BUN) and creatinine
- Indicate reduced renal perfusion and dehydration
- Elevated blood urea nitrogen (BUN) and creatinine
Nursing Insights
- Hypokalemia is a high-risk abnormality requiring continuous cardiac monitoring.
- A rising hematocrit without bleeding strongly suggests severe dehydration, not polycythemia.
1.2 Urinalysis and Ketone Assessment
Urinalysis provides rapid assessment of hydration status and starvation.
- Ketonuria
- Presence of ketones confirms fat metabolism due to inadequate carbohydrate intake
- Indicates starvation state and disease severity
- Urine Specific Gravity
- 1.030 suggests severe dehydration
- Reflects renal conservation of water
- Urine Output
- Oliguria <30 mL/hr indicates inadequate renal perfusion
Nursing Insights
- Persistent ketonuria despite IV fluids suggests inadequate caloric replacement.
- Urine ketone monitoring guides effectiveness of nutritional therapy.
1.3 Imaging and Exclusion of Other Conditions
Diagnostic imaging and targeted testing are used to exclude conditions that mimic or worsen hyperemesis gravidarum.
- Ultrasound Examination
- Confirms intrauterine pregnancy
- Rules out:
- Molar pregnancy
- Multiple gestations
- Evaluates fetal viability and gestational age
- Thyroid Function Tests
- Detect transient gestational hyperthyroidism
- Elevated free thyroxine (T4) with suppressed thyroid-stimulating hormone (TSH)
- Additional Diagnostic Studies (When Indicated)
- Liver function tests to exclude hepatitis
- Serum glucose to rule out diabetic ketoacidosis
- Amylase and lipase to assess pancreatitis
Nursing Insights
- Ultrasound is mandatory in early severe cases to rule out molar pregnancy.
- Thyroid abnormalities in hyperemesis gravidarum are usually secondary, not primary thyroid disease.
Maternal And Fetal Complications
Hyperemesis gravidarum is a severe pregnancy-related disorder characterized by persistent nausea and vomiting resulting in significant maternal and fetal morbidity when untreated or inadequately managed. Complications arise from prolonged malnutrition, dehydration, electrolyte imbalance, vitamin deficiencies, and metabolic derangements.
1.1 Maternal Complications
Maternal complications are primarily the result of persistent vomiting, fluid volume deficit, nutritional depletion, and metabolic imbalance, affecting multiple organ systems.
Fluid and Electrolyte Complications
- Severe dehydration
- Results from prolonged fluid losses exceeding intake.
- Leads to:
- Hypovolemia
- Reduced uteroplacental perfusion
- Acute kidney injury
- Electrolyte imbalances
- Hypokalemia < 3.5 mEq/L.
- Due to gastric potassium loss.
- Can precipitate:
- Cardiac dysrhythmias
- Muscle weakness
- Hyponatremia < 135 mEq/L.
- Caused by excessive free water intake or vomiting.
- Increases risk for seizures.
- Hypochloremia < 98 mEq/L.
- Due to loss of hydrochloric acid via emesis.
- Hypokalemia < 3.5 mEq/L.
Acid–Base Disturbances
- Metabolic alkalosis
- Caused by excessive loss of gastric hydrochloric acid.
- Characterized by:
- Elevated arterial pH >7.45
- Elevated bicarbonate levels
- Starvation ketosis
- Occurs with prolonged inadequate caloric intake.
- Leads to ketonemia and ketonuria.
Nutritional and Vitamin Deficiency Complications
- Thiamine (Vitamin B1) deficiency
- Can result in Wernicke’s encephalopathy, a life-threatening neurological disorder.
- Manifestations include:
- Confusion
- Ophthalmoplegia
- Ataxia
- Folate deficiency
- May contribute to megaloblastic anemia.
- Protein-energy malnutrition
- Leads to muscle wasting and fatigue.
Gastrointestinal and Mechanical Complications
- Esophagitis
- Due to repeated exposure to gastric acid.
- Mallory–Weiss tears
- Longitudinal mucosal tears caused by forceful vomiting.
- Present with hematemesis.
- Gastroesophageal reflux disease exacerbation
Cardiovascular and Renal Complications
- Hypotension and tachycardia
- Reflect intravascular volume depletion.
- Acute kidney injury
- Due to reduced renal perfusion.
- Elevated blood urea nitrogen (BUN) and creatinine.
Psychological and Psychosocial Complications
- Depression and anxiety
- Result from prolonged illness, social isolation, and loss of function.
- Impaired maternal–fetal bonding
- Increased risk for hospitalization-related stress
Nursing Insights (Maternal Complications)
- Early recognition of hypokalemia is critical due to its association with fatal arrhythmias.
- Thiamine must be administered before dextrose-containing IV fluids to prevent Wernicke’s encephalopathy.
- Persistent vomiting with hematemesis requires immediate escalation to the primary health care provider.
- Orthostatic vital signs are a sensitive indicator of hypovolemia.
- Daily weights provide the most accurate assessment of fluid balance.
1.2 Fetal and Neonatal Complications
Fetal complications result primarily from chronic maternal malnutrition, dehydration, and placental hypoperfusion.
Fetal Growth and Development Complications
- Intrauterine growth restriction (IUGR)
- Due to inadequate maternal caloric and protein intake.
- Low birth weight (<2500 g)
- Preterm birth
- Secondary to maternal stress and metabolic imbalance.
Placental and Oxygenation Complications
- Reduced uteroplacental blood flow
- Due to maternal hypovolemia.
- Chronic fetal hypoxia
- Leads to poor fetal growth and distress.
Neonatal Complications
- Neonatal hypoglycemia
- Electrolyte imbalances
- Poor neonatal adaptation
- Due to prolonged intrauterine malnutrition.
Long-Term Neurodevelopmental Risks
- Severe maternal malnutrition during early pregnancy may be associated with:
- Cognitive delays
- Behavioral disorders
- Impaired motor development
Table: Summary of Maternal vs Fetal Complications
|
Category |
Maternal Complications |
Fetal/Neonatal Complications |
|
Fluid Balance |
Dehydration, hypovolemia |
Reduced placental perfusion |
|
Electrolytes |
Hypokalemia, hyponatremia |
Neonatal electrolyte imbalance |
|
Nutrition |
Wernicke’s encephalopathy |
Low birth weight |
|
Growth |
Muscle wasting |
Intrauterine growth restriction |
|
Outcomes |
Hospitalization |
Preterm birth |
Nursing Insights (Fetal and Neonatal Complications)
- Persistent maternal ketonuria is a marker of fetal starvation.
- Fetal heart rate monitoring evaluates uteroplacental sufficiency.
- Early nutritional intervention improves neonatal birth outcomes.
- Severe hyperemesis increases the need for serial growth ultrasounds.
- Nurses play a critical role in early referral for nutritional support, including enteral or parenteral therapy.
Medical And Nursing Management
Hyperemesis gravidarum is a potentially life-threatening obstetric condition requiring aggressive, systematic medical and nursing management to prevent maternal metabolic derangements, neurologic injury, and fetal compromise. Management is individualized based on severity, gestational age, maternal response, and presence of complications.
1.1 Fluid and Electrolyte Replacement
Severe and persistent vomiting results in hypovolemia, electrolyte depletion, and acid–base imbalance. Restoration of intravascular volume is the immediate priority.
Goals of Fluid Therapy
- Restore circulating blood volume
- Correct electrolyte imbalances
- Reverse ketosis
- Improve renal perfusion
- Prevent hypovolemic shock
Commonly Used Intravenous Fluids
- 0.9% Sodium Chloride (Normal Saline)
- Initial fluid of choice
- Corrects hypovolemia and hyponatremia
- Lactated Ringer’s
- Provides balanced electrolyte replacement
- Avoid in severe metabolic alkalosis
- Dextrose-containing solutions
- Added only after thiamine administration
- Used to reverse starvation ketosis
Electrolyte Abnormalities Addressed
- Hypokalemia
- Due to gastric potassium loss
- Requires IV or oral potassium supplementation
- Hyponatremia
- Caused by prolonged vomiting and hypotonic intake
- Hypochloremia
- From loss of hydrochloric acid (HCl)
- Metabolic alkalosis
- Due to hydrogen ion loss via emesis
Nursing Interventions
- Initiate large-bore IV access
- Monitor:
- Vital signs every 2–4 hours
- Intake and output hourly
- Urine output ≥30 mL/hr
- Assess:
- Orthostatic hypotension
- Capillary refill
- Skin turgor and mucous membranes
- Strict daily weights at the same time each day
Nursing Insights
- Thiamine must be administered before dextrose to prevent Wernicke’s encephalopathy, a potentially irreversible neurologic emergency.
- Tachycardia and hypotension in a client with hyperemesis gravidarum indicate severe hypovolemia, not anxiety.
- Dark, concentrated urine with specific gravity >1.030 reflects significant dehydration.
1.2 Pharmacological Management
Pharmacotherapy aims to control nausea and vomiting, reduce hospitalization, and allow nutritional intake.
Antiemetic Medications
|
Drug Class |
Medication |
Mechanism |
|
Vitamin |
Pyridoxine (Vitamin B6) |
Reduces nausea |
|
Antihistamine |
Doxylamine |
Blocks H1 receptors |
|
Dopamine antagonist |
Metoclopramide |
Enhances gastric emptying |
|
Phenothiazine |
Promethazine |
Central antiemetic effect |
|
Serotonin antagonist |
Ondansetron |
Blocks 5-HT3 receptors |
Adjunct Medications
- Thiamine (Vitamin B1)
- Prevents Wernicke’s encephalopathy
- Corticosteroids
- Reserved for refractory cases
- Used after 10 weeks gestation
- H2 blockers or Proton Pump Inhibitors
- Reduce gastric irritation
Medication Administration Considerations
- IV route preferred during acute phase
- Transition to oral route once vomiting controlled
- Monitor for:
- Sedation
- Extrapyramidal symptoms
- QT interval prolongation (ondansetron)
Nursing Insights
- Ondansetron is effective but requires risk–benefit evaluation due to possible fetal cardiac effects.
- Combining pyridoxine with doxylamine is considered first-line therapy.
- Persistent vomiting despite antiemetics signals need for escalation of care.
1.3 Nutritional Support and Dietary Modifications
Malnutrition is a major risk due to prolonged inadequate intake.
Dietary Recommendations
- Small, frequent meals every 1–2 hours
- High-protein, low-fat foods
- Bland foods (crackers, toast, rice)
- Cold or room-temperature foods to reduce odor
- Avoid spicy, greasy, or fatty foods
Advanced Nutritional Support
- Enteral feeding (nasogastric or nasojejunal)
- Preferred over parenteral when tolerated
- Total Parenteral Nutrition (TPN)
- Indicated when:
- 10% weight loss
- Persistent ketonuria
- Oral and enteral feeding not tolerated
- Indicated when:
Nursing Insights
- Protein intake stabilizes blood glucose and reduces nausea.
- TPN increases risk for infection, thrombosis, and hyperglycemia and requires close monitoring.
- Weight loss >5% of pre-pregnancy weight indicates severe disease.
1.4 Complementary and Non-Pharmacological Therapies
Non-pharmacologic measures enhance symptom control and patient comfort.
Therapeutic Interventions
- Acupressure at P6 (Neiguan) point
- Ginger supplementation
- Aromatherapy avoidance
- Calm, low-stimulus environment
- Emotional reassurance and support
Nursing Insights
- Stress and anxiety exacerbate nausea through neuroendocrine pathways.
- Validation of symptoms reduces psychological distress and improves adherence.
- Family involvement improves outcomes and emotional coping.
1.5 Inpatient and Outpatient Management Criteria
Outpatient Management Indications
- Mild symptoms
- No electrolyte imbalance
- Able to tolerate oral intake
- Stable vital signs
Inpatient Management Indications
- Persistent vomiting
- Ketonuria
- Electrolyte abnormalities
- Weight loss >5%
- Hematemesis or neurologic symptoms
Nursing Insights
- Ketonuria reflects starvation, not diabetes, in hyperemesis gravidarum.
- Early admission prevents progression to severe complications.
Nursing Assessment And Priority Interventions
Nursing care for clients with hyperemesis gravidarum requires systematic, continuous assessment to identify life-threatening complications, guide timely interventions, and promote maternal–fetal stability. The nurse plays a critical role in early recognition of deterioration, prevention of complications, and psychosocial support.
1.1 Comprehensive Maternal Assessment
A comprehensive maternal assessment establishes baseline severity, identifies complications, and guides the plan of care.
Subjective Assessment
- Frequency, duration, and severity of vomiting
- Number of emesis episodes per 24 hours
- Presence of bile or blood (hematemesis)
- Ability to tolerate oral intake
- Triggers:
- Odors
- Fatty or spicy foods
- Motion
- Associated symptoms:
- Dizziness
- Fatigue
- Palpitations
- Headache
- Visual disturbances
- Psychosocial assessment:
- Anxiety level
- Depression symptoms
- Impact on daily functioning
- Support system availability
Objective Physical Assessment
- Vital Signs
- Tachycardia (>100 bpm) indicating hypovolemia
- Hypotension, including orthostatic changes
- Temperature to rule out infection (≥38°C / 100.4°F)
- Hydration Status
- Dry mucous membranes
- Poor skin turgor
- Sunken eyes
- Delayed capillary refill
- Weight Assessment
- Compare current weight with pre-pregnancy baseline
- Weight loss >5% indicates severe disease
- Neurological Assessment
- Level of consciousness
- Confusion
- Ataxia
- Ophthalmoplegia (concern for Wernicke’s encephalopathy)
- Abdominal Assessment
- Epigastric tenderness
- Abdominal distention
- Bowel sounds
Laboratory Review
- Urinalysis for ketonuria
- Electrolytes:
- Sodium
- Potassium
- Chloride
- Blood urea nitrogen (BUN) and creatinine
- Hemoglobin and hematocrit (hemoconcentration)
- Liver enzymes if persistent vomiting
Nursing Insights
- Persistent tachycardia and orthostatic hypotension are late signs of dehydration and require immediate intervention.
- Ketonuria reflects starvation, not hyperglycemia, in hyperemesis gravidarum.
- Neurological changes in a vomiting pregnant client are never normal and must raise concern for thiamine deficiency.
1.2 Ongoing Monitoring Parameters
Continuous monitoring ensures early detection of deterioration and evaluates response to therapy.
Fluid Balance Monitoring
- Strict intake and output measurement
- Urine output ≥30 mL/hr indicates adequate renal perfusion
- Daily weights
- Same scale
- Same time
- Same clothing
- Urine specific gravity
- 1.030 indicates dehydration
Vital Signs Monitoring
- Monitor every 2–4 hours in acute phase
- Assess for:
- Tachycardia
- Hypotension
- Orthostatic changes
Electrolyte and Metabolic Monitoring
- Monitor serum potassium closely
- Hypokalemia increases risk for cardiac dysrhythmias
- Monitor sodium levels for dilutional or depletional hyponatremia
- Monitor acid–base status
- Metabolic alkalosis common due to gastric acid loss
Fetal Surveillance
- Assess fetal heart rate once viable gestational age reached
- Monitor fetal growth in prolonged cases
- Assess uterine activity if dehydration severe
Neurological Monitoring
- Assess orientation, gait, and eye movements
- Monitor for:
- Confusion
- Memory impairment
- Ataxia
Nursing Insights
- Declining urine output is often the earliest indicator of worsening dehydration.
- Hypokalemia must be corrected cautiously and monitored via cardiac rhythm.
- Fetal compromise often reflects maternal metabolic instability, not primary fetal pathology.
1.3 Client Education and Psychosocial Support
Hyperemesis gravidarum significantly affects mental health, family dynamics, and quality of life.
Client Education
- Explain disease process using clear, non-judgmental language
- Reinforce importance of:
- Medication adherence
- Thiamine supplementation
- Early reporting of decreased urine output
- Teach trigger avoidance strategies
- Instruct on dietary modifications:
- Small, frequent meals
- High-protein foods
- Avoid fatty and spicy foods
Psychosocial Support
- Acknowledge severity and legitimacy of symptoms
- Encourage expression of frustration and fear
- Involve family in care planning
- Screen for anxiety and depression
- Provide reassurance regarding fetal outcomes when managed appropriately
Nursing Insights
- Minimizing symptoms damages trust and worsens psychological distress.
- Emotional support improves treatment adherence and outcomes.
Hyperemesis gravidarum is associated with increased risk for antenatal depression and postpartum mood disorders.
Summary
Hyperemesis Gravidarum (HG) is a severe form of nausea and vomiting in pregnancy that exceeds typical morning sickness, leading to significant maternal and fetal complications if untreated. It primarily occurs in the first trimester and can persist longer in severe cases. Key points for nursing students:
- Definition: Persistent, uncontrollable nausea and vomiting resulting in dehydration, electrolyte imbalance, weight loss >5% of pre-pregnancy weight, and nutritional deficiencies.
- Etiology: Multifactorial including hormonal, gastrointestinal, neurological, metabolic, genetic, and psychological factors.
- Hormonal: Human chorionic gonadotropin (hCG) is most strongly implicated, along with progesterone and estrogen.
- Gastrointestinal: Delayed gastric emptying, smooth muscle relaxation, and reduced motility contribute to nausea.
- Neurological: Sensitivity of the chemoreceptor trigger zone and vomiting center in the medulla oblongata.
- Metabolic: Loss of fluids and electrolytes causes metabolic alkalosis, ketonuria, hypokalemia, and hypovolemia.
- Genetic/Psychological: Family history and high stress levels may exacerbate symptoms.
- Risk Factors:
- Multiple gestations
- Molar pregnancy
- Nulliparity
- History of migraines
- Female fetus
- Clinical Manifestations:
- Persistent vomiting
- Dehydration (sunken eyes, dry mucous membranes, poor skin turgor)
- Weight loss >5% of pre-pregnancy weight
- Electrolyte imbalances (hypokalemia, hyponatremia, chloride loss)
- Ketonuria
- Tachycardia, hypotension
- Complications:
- Maternal: Wernicke’s encephalopathy, esophageal tears, dehydration, electrolyte disturbances, malnutrition
- Fetal: Intrauterine growth restriction (IUGR), low birth weight, preterm birth
- Diagnostic Criteria:
- Persistent vomiting >3 times/day
- Weight loss >5% of pre-pregnancy weight
- Dehydration signs
- Laboratory evidence: ketonuria, electrolyte imbalances
- Nursing Assessment:
- Vital signs, including orthostatic BP
- Fluid balance: intake/output, urine specific gravity
- Laboratory monitoring: electrolytes, BUN, creatinine, ketones
- Weight monitoring
- Fetal well-being
- Nursing Interventions:
- Initiate IV fluid therapy (isotonic or lactated Ringer’s)
- Administer thiamine (Vitamin B1) before glucose to prevent Wernicke’s encephalopathy
- Antiemetic therapy: Ondansetron, Metoclopramide
- Nutritional support: small, frequent, high-protein meals; consider enteral or parenteral nutrition in severe cases
- Emotional support and education
- Low-stimulus environment to reduce nausea triggers
Nursing Insights:
- Early recognition is critical to prevent maternal-fetal complications.
- Monitor for subtle signs of dehydration before overt hypotension or tachycardia appears.
- Ensure electrolyte replacement is accurate to avoid cardiac arrhythmias.
- Educate the client on dietary modifications and the importance of small, frequent meals.
- Assess for psychological distress and provide support; stress can worsen HG symptoms.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Hyperemesis Gravidarum
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


