Please set your exam date
Personality Disorders
Study Questions
Practice Exercise 1
Carol is a new nursing graduate being oriented on a medical-surgical unit by the head nurse, Mrs. Carey. When Carol describes a new technique she has learned for positioning immobile clients, Mrs. Carey states, “What are you trying to do—tell me how to do my job? We have always done it this way on this unit, and we will continue to do it this way until I say differently!” This is an example of which type of personality characteristic?
Explanation
Obsessive–compulsive personality disorder is a chronic, pervasive pattern of behavior marked by rigidity, perfectionism, and a need for control. Individuals with this personality style often struggle with flexibility and openness to new ideas. They may impose strict standards, resist change, and exhibit excessive devotion to rules and procedures. Unlike obsessive-compulsive disorder, which involves intrusive thoughts and compulsions, this personality disorder reflects enduring traits that interfere with interpersonal functioning and adaptability.
Rationale for correct answer
D. The head nurse’s rigid insistence on maintaining traditional methods and her resistance to new techniques reflect perfectionism and control, hallmark traits of obsessive–compulsive personality disorder. Her behavior shows inflexibility and a need to maintain order, even at the expense of innovation or collaboration. The statement “we have always done it this way” exemplifies the disorder’s resistance to change and excessive adherence to routine.
Rationale for incorrect answers
A. Antisocial personality disorder is marked by disregard for others’ rights, impulsivity, and deceit. It involves manipulative or exploitative behavior, often violating social norms. The nurse’s behavior lacks the callousness or criminality typical of antisocial traits.
B. Paranoid personality disorder involves suspicion and mistrust of others’ motives. While the nurse’s response may seem defensive, it lacks the pervasive distrust, hypervigilance, and belief that others are out to harm or deceive her, which are central to paranoid traits.
C. Passive–aggressive personality traits include indirect resistance, procrastination, and covert obstruction. The nurse’s response is overtly controlling and direct, not subtly undermining or avoiding confrontation. Her behavior is assertive and rule-bound, not passive or evasive.
Take Home Points
- Obsessive–compulsive personality disorder is defined by rigidity, perfectionism, and resistance to change, not by compulsions or intrusive thoughts.
- It differs from OCD, which involves anxiety-driven rituals; OCPD is a stable personality trait.
- Paranoid and passive–aggressive traits involve suspicion and indirect resistance, respectively, not overt control.
- Antisocial traits include disregard for others and social norms, which are absent in rigid, rule-bound behavior.
Donna and Katie work in the secretarial pool of a large organization. It is 30 minutes until quitting time when a supervisor hands Katie a job that will take an hour and says he wants it before she leaves. She then says to Donna, “I can’t stay over! I’m meeting Bill at 5 o’clock! Be a doll, Donna. Do this job for me!” Donna agrees, although silently she is furious at Katie because this is the third time this has happened in two weeks. Katie leaves, and Donna says to herself, “This is crazy. I’m not finishing this job for her. Let’s see how she likes getting in trouble for a change.” Donna leaves without finishing the job. This is an example of which type of personality characteristic?
Explanation
Passive–aggressive personality traits involve a chronic pattern of indirect resistance, resentment, and avoidance of direct confrontation. Individuals with this style often appear cooperative but express hostility through procrastination, stubbornness, or intentional inefficiency. Rather than openly expressing anger or disagreement, they may sabotage tasks, withhold effort, or act out covertly. This behavior often stems from underlying feelings of powerlessness, fear of conflict, or difficulty asserting needs directly.
Rationale for correct answer
C. Donna’s behavior reflects indirect hostility and resentment. Though she agrees to help, she silently refuses to complete the task, intending for Katie to face consequences. This covert defiance and avoidance of direct confrontation are classic features of passive–aggressive personality traits.
Rationale for incorrect answers
A. Antisocial traits involve disregard for others’ rights, deceit, and impulsivity. Donna’s behavior lacks the manipulative, exploitative, or rule-breaking tendencies typical of antisocial personality disorder.
B. Paranoid personality traits include suspicion and mistrust of others’ motives. Donna does not exhibit pervasive distrust or interpret Katie’s actions as malicious or threatening, which would be necessary for a paranoid diagnosis.
D. Obsessive–compulsive personality traits involve rigidity and perfectionism. Donna’s actions are not driven by a need for control or order but by emotional retaliation. Her behavior lacks the hallmark inflexibility and rule-bound thinking of obsessive–compulsive traits.
Take Home Points
- Passive–aggressive behavior is marked by indirect expression of anger, such as procrastination or intentional inefficiency.
- It differs from assertiveness, which involves direct communication of needs and boundaries.
- Obsessive–compulsive traits involve control and perfectionism, not covert defiance.
- Antisocial traits include rule-breaking and manipulation, while paranoid traits involve pervasive mistrust.
When working with a client with a personality disorder, the nurse would expect to assess which of the following?
Explanation
Personality disorders are enduring, inflexible patterns of behavior, cognition, and inner experience that deviate markedly from cultural expectations and cause significant distress or impairment. These patterns typically emerge in adolescence or early adulthood and are stable over time. Individuals often lack insight into their condition, struggle with empathy, and experience chronic interpersonal difficulties. Unlike psychotic disorders, personality disorders do not usually involve hallucinations or gross distortions of reality.
Rationale for correct answers
B. Individuals with personality disorders often exhibit interpersonal dysfunction, including unstable relationships, poor boundaries, and difficulty with trust or cooperation. These impairments are persistent and central to the diagnosis.
C. A hallmark of many personality disorders is a reduced capacity for empathy, leading to disregard for others’ feelings, needs, or perspectives. This contributes to interpersonal conflict and emotional detachment.
D. Clients typically have limited insight into their maladaptive behaviors and may externalize blame. This lack of self-awareness hinders motivation for change and complicates therapeutic engagement.
Rationale for incorrect answers
A. High levels of self-awareness are uncommon in personality disorders. These individuals often lack recognition of their behavior’s impact and may rationalize or deny their difficulties.
E. Genuine motivation to change is often absent unless external pressures (e.g., legal, relational) exist. Resistance to feedback and defensiveness are common, especially early in treatment.
F. Poor reality testing is more characteristic of psychotic disorders, not personality disorders. While some may experience transient stress-related distortions, baseline reality orientation is typically intact.
Take Home Points
- Personality disorders involve enduring patterns of interpersonal dysfunction, impaired empathy, and limited insight.
- They differ from psychotic disorders in that reality testing is generally preserved.
- Motivation to change is often low due to ego-syntonic traits and externalization of blame.
- Effective nursing care requires structured boundaries, consistency, and therapeutic communication.
Which statement about persons with personality disorders is accurate?
Explanation
Personality disorders are enduring patterns of inner experience, behavior, and cognition that deviate from cultural expectations and are pervasive, inflexible, and maladaptive. These patterns begin in adolescence or early adulthood and lead to significant distress or impairment. A defining feature is that individuals often lack insight into their condition, externalize blame, and view their difficulties as stemming from others’ actions rather than their own behavior. This ego-syntonic nature makes treatment engagement and change particularly challenging.
Rationale for correct answer
B. Individuals with personality disorders typically lack insight and view their interpersonal or occupational difficulties as caused by others. This externalization of blame and resistance to self-reflection is a core diagnostic feature and contributes to poor treatment adherence and chronic dysfunction.
Rationale for incorrect answers
A. The risk of suicide is not low in personality disorders. In fact, individuals with borderline personality disorder, in particular, have a high risk of self-harm and suicide attempts, often driven by emotional dysregulation and interpersonal instability.
C. Personality disorders are not considered purely psychological. Neurobiological, genetic, and environmental factors all contribute to their development. Structural and functional brain differences, especially in the prefrontal cortex and limbic system, have been implicated in several personality disorders.
D. The complexity of care for individuals with personality disorders is often high. Their behaviors can challenge therapeutic boundaries, provoke countertransference, and require consistent, structured interventions. These disorders are among the most difficult to treat due to their chronicity and resistance to change.
Take Home Points
- Personality disorders are ego-syntonic, meaning individuals often do not recognize their behavior as problematic.
- Suicide risk is elevated in certain personality disorders, especially borderline personality disorder.
- These disorders have multifactorial origins, including neurobiological and genetic components.
- Managing personality disorders requires structured, consistent care due to interpersonal challenges and treatment resistance.
Personality disorders are grouped in clusters according to their behavioral characteristics. In which cluster are the disorders correctly matched with their behavioral characteristics?
Explanation
Personality disorder clusters are categorized based on shared behavioral, emotional, and interpersonal traits. Cluster C includes disorders characterized by anxious or fearful behavior, such as avoidant, dependent, and obsessive–compulsive personality disorders. These individuals often exhibit chronic anxiety, fear of rejection, and a need for control or reassurance. Their interpersonal style is marked by inhibition, submissiveness, and perfectionism, which can impair functioning and relationships.
Rationale for correct answer
D. Cluster C includes avoidant, dependent, and obsessive–compulsive personality disorders, all of which share anxious and fearful traits. Avoidant individuals fear rejection, dependent individuals fear abandonment, and obsessive–compulsive individuals fear loss of control. These traits align with the cluster’s defining behavioral characteristics.
Rationale for incorrect answers
A. Antisocial, borderline, histrionic, and narcissistic disorders belong to Cluster B, not Cluster C. These disorders are marked by dramatic and erratic behaviors, not anxiety or fearfulness.
B. Avoidant, dependent, and obsessive–compulsive disorders are not part of Cluster A, which includes paranoid, schizoid, and schizotypal disorders. Cluster A is defined by eccentric and socially detached behaviors, not anxiety-driven traits.
C. Antisocial, borderline, histrionic, and narcissistic disorders are correctly grouped together but belong to Cluster B, not Cluster A. Cluster A includes disorders with odd or eccentric behaviors, not dramatic or emotional traits.
Take Home Points
- Cluster C includes avoidant, dependent, and obsessive–compulsive personality disorders, marked by anxiety and fearfulness.
- Cluster B includes antisocial, borderline, histrionic, and narcissistic disorders, characterized by dramatic and erratic behavior.
- Cluster A includes paranoid, schizoid, and schizotypal disorders, defined by eccentric and socially detached traits.
- Accurate cluster classification aids in understanding behavioral patterns and guiding therapeutic approaches.
Although there are differences among the three personality disorder clusters, there also are some traits common to all individuals diagnosed with personality disorders. Which of the following are common traits? Select all that apply
Explanation
Personality disorders are enduring patterns of maladaptive behavior, cognition, and interpersonal functioning that deviate from cultural expectations and are inflexible across situations. These traits often lead to significant distress or impairment but are typically ego-syntonic—meaning the individual does not recognize them as problematic. Common features across all personality disorders include externalization of blame, poor insight, and rigid coping strategies that focus on changing others or the environment rather than self-reflection or adaptation.
Rationale for correct answers
A. Individuals with personality disorders often externalize blame and show limited accountability for their actions. They may rationalize or deny their role in conflicts, leading to persistent interpersonal difficulties.
D. A hallmark of personality pathology is coping by attempting to manipulate or control the environment or others rather than modifying internal responses or behaviors. This reflects a rigid and maladaptive coping style.
E. Most individuals with personality disorders exhibit poor insight into their condition. They often do not perceive their behavior as problematic, which impedes motivation for change and therapeutic engagement.
Rationale for incorrect answers
B. While self-injurious behaviors are common in borderline personality disorder, they are not universal across all personality disorders. This behavior is not a shared trait among all clusters.
C. Avoidance of personal risk is characteristic of avoidant personality disorder but not a consistent feature across all personality disorders. Some, like antisocial or narcissistic types, may engage in high-risk behaviors.
Take Home Points
- Common traits across personality disorders include poor insight, externalization of blame, and rigid coping mechanisms.
- Self-injury is specific to certain disorders like borderline personality disorder, not a universal trait.
- Risk-taking behavior varies widely across personality disorder types.
- Effective care requires understanding the ego-syntonic nature of these disorders and using structured, consistent interventions.
A hospitalized client who was diagnosed with a borderline personality disorder consistently breaks the unit’s rules. How will confronting the client about this behavior help the client?
Explanation
Borderline personality disorder is a pervasive pattern of emotional instability, impulsivity, and interpersonal dysfunction. Individuals often struggle with identity disturbance, intense fear of abandonment, and difficulty regulating emotions. Their behavior may include self-harm, rule-breaking, and splitting. Confrontation in a therapeutic context helps establish boundaries and fosters insight into maladaptive patterns, which is essential for behavioral change and emotional regulation.
Rationale for correct answer
D. Confronting the client promotes self-awareness by helping them recognize the impact of their behavior on others and the environment. This approach encourages reflection and accountability, which are critical for therapeutic progress in borderline personality disorder.
Rationale for incorrect answers
A. Anger control in borderline personality disorder requires emotion regulation strategies, not just confrontation. While boundary-setting may reduce acting out, it does not directly address the underlying dysregulation.
B. Confrontation may initially increase anxiety, especially in clients with abandonment fears. Anxiety reduction requires validation, consistency, and therapeutic rapport, not direct confrontation alone.
C. Setting realistic goals involves collaborative planning and psychoeducation. Confrontation may clarify expectations but does not inherently help the client develop goal-setting skills or motivation.
Take Home Points
- Borderline personality disorder involves emotional dysregulation, impulsivity, and unstable relationships.
- Therapeutic confrontation fosters self-awareness and accountability, essential for behavioral change.
- Anxiety and anger in BPD require structured interventions beyond confrontation.
- Goal-setting in BPD should be collaborative and supported by psychoeducation and consistent boundaries.
A nurse is working in the orientation phase of a therapeutic relationship with a client who has borderline personality disorder. What will be most difficult for the client at this stage of the relationship?
Explanation
Borderline personality disorder is marked by pervasive patterns of emotional instability, identity disturbance, and intense, unstable interpersonal relationships. During the orientation phase of a therapeutic relationship, individuals with this disorder often struggle with trust, fear of abandonment, and difficulty establishing collaborative boundaries. Their fluctuating self-image and impulsivity interfere with forming consistent therapeutic alliances, making structured goal-setting particularly challenging.
Rationale for correct answer
D. Clients with borderline personality disorder often have difficulty with collaboration and trust, making it hard to set mutual goals. Their interpersonal instability and fear of rejection can lead to idealization or devaluation of the nurse, disrupting the process of establishing shared objectives in the therapeutic relationship.
Rationale for incorrect answers
A. While anxiety may be present, it is not the defining challenge in the orientation phase. Emotional dysregulation is more prominent during crises or perceived abandonment, not necessarily at the start of the relationship.
B. Difficulty terminating sessions is more characteristic of the termination phase, where separation anxiety and fear of loss become pronounced. It is not the primary challenge during orientation.
C. Although acceptance of diagnosis may be limited, it is not unique to borderline personality disorder and does not interfere with the orientation phase as significantly as the inability to form mutual therapeutic goals.
Take Home Points
- Borderline personality disorder involves unstable relationships, identity disturbance, and emotional dysregulation.
- The orientation phase is disrupted by difficulty forming collaborative, trusting therapeutic alliances.
- Termination challenges are more prominent in later phases due to fear of abandonment.
- Goal-setting requires stability and trust, which are often impaired early in the therapeutic process.
When interviewing any client with a personality disorder, the nurse would assess for which of the following?
Explanation
Personality disorders are enduring patterns of maladaptive behavior, cognition, and interpersonal functioning that cause significant impairment in social, occupational, or other important areas of life. These patterns are inflexible and pervasive across a broad range of situations. While the specific traits vary by disorder, all personality disorders share the feature of functional disruption—whether in relationships, work, or self-identity. This impairment is often chronic and resistant to change, contributing to long-term distress or dysfunction.
Rationale for correct answer
C. The defining feature of all personality disorders is functional impairment. Whether through unstable relationships, poor impulse control, or distorted self-image, these individuals experience disruption in key life domains, which is essential for diagnosis.
Rationale for incorrect answers
A. While manipulativeness may be seen in antisocial or narcissistic personality disorders, it is not a universal trait across all personality disorders. It is not a core diagnostic feature for the broader category.
B. A desire for relationships varies. Some, like avoidant or dependent types, crave connection, while others, like schizoid or paranoid types, may avoid intimacy. This trait is not consistent across all personality disorders.
D. An increased need for approval is characteristic of dependent personality disorder but not shared across all types. Others, such as narcissistic or schizoid individuals, may show little concern for others’ approval.
Take Home Points
- Functional impairment is a core diagnostic criterion for all personality disorders.
- Traits like charm, need for approval, or desire for relationships vary widely across personality types.
- Diagnosis requires evidence of enduring, inflexible patterns that disrupt major life areas.
- Assessment should focus on behavior patterns, interpersonal functioning, and insight.
Practice Exercise 2
Which behavior should a nurse expect a client diagnosed with paranoid personality disorder to exhibit?
Explanation
Paranoid personality disorder is a chronic psychiatric condition marked by pervasive distrust, suspicion, and hypervigilance toward others. Individuals with this disorder interpret others’ motives as malevolent, even without evidence. They often misread benign interactions as threatening, are reluctant to confide in others, and may bear grudges. Their interpersonal relationships are strained due to their guardedness and persistent belief that others are trying to exploit or harm them. These patterns are stable over time and begin by early adulthood, impairing social and occupational functioning.
Rationale for correct answer
D. Individuals with paranoid personality disorder exhibit persistent suspicion and hypervigilance, leading them to scrutinize others’ actions for perceived threats. They often misinterpret neutral or friendly behavior as hostile or manipulative. This cognitive distortion drives them to analyze others’ behavior obsessively, seeking hidden meanings that confirm their fears.
Rationale for incorrect answers
A. The word trust contradicts the core pathology of this disorder. These individuals rarely trust others, even those who treat them well. Their default assumption is that others have ulterior motives, making genuine trust nearly impossible.
B. Seeing goodwill where none exists is more characteristic of dependent or histrionic traits. Paranoid individuals do the opposite—they assume malevolence even when goodwill is present, due to their cognitive bias toward suspicion.
C. Acting the opposite of internal feelings is more aligned with passive-aggressive or certain neurotic defenses, not paranoid personality. Paranoid individuals are more likely to act in accordance with their suspicious thoughts, often becoming defensive or hostile.
Take Home Points
- Paranoid personality disorder is defined by pervasive distrust and suspicion without sufficient basis.
- Clients often misinterpret neutral or positive actions as hostile or threatening.
- It must be differentiated from delusional disorder (persecutory type), which involves fixed false beliefs.
- Therapeutic approaches require consistency, clear boundaries, and avoidance of overly familiar or intrusive behavior.
When working with a client with paranoid personality disorder, a nurse should:
Explanation
Paranoid personality disorder is a chronic psychiatric condition characterized by pervasive distrust, suspicion, and interpersonal detachment. These individuals are hypersensitive to perceived threats and often misinterpret benign interactions as hostile. They are reluctant to confide in others and may bear long-standing grudges. Their guardedness and fear of exploitation impair their ability to form close relationships. Therapeutic engagement requires consistency, emotional neutrality, and clear boundaries to avoid reinforcing their suspicions.
Rationale for correct answer
A. A structured, businesslike approach minimizes emotional ambiguity and helps establish predictability, which is essential for building trust with paranoid clients. This method respects their need for control and reduces perceived threats. By focusing on tasks and maintaining professional boundaries, the nurse avoids triggering the client's suspicion or misinterpretation of motives, facilitating therapeutic rapport.
Rationale for incorrect answers
B. Initiating with social conversation may be perceived as intrusive or manipulative. Paranoid clients often view friendliness as a cover for hidden agendas, which can heighten their defensiveness and hinder rapport.
C. Using jokes can be misinterpreted as ridicule or sarcasm. These clients are highly sensitive to perceived slights and may interpret humor as mocking, which can escalate mistrust and hostility.
D. Arriving late reinforces the client’s belief in hidden meanings or intentional disrespect. Timeliness is critical in maintaining consistency and demonstrating reliability, which are essential to reduce paranoid ideation.
When working with a client diagnosed with paranoid personality disorder, a nurse understands that the client most likely:
Explanation
Paranoid personality disorder is shaped by early developmental experiences that reinforce emotional detachment, mistrust, and interpersonal vigilance. These individuals often grow up in environments lacking warmth, consistency, and emotional responsiveness. Indifference or emotional neglect during formative years fosters discomfort with intimacy and a tendency to interpret others’ actions as threatening. The disorder reflects a stable pattern of maladaptive interpersonal beliefs and behaviors rooted in early relational trauma or neglect.
Rationale for correct answer
C. An upbringing marked by indifference fosters emotional withdrawal and discomfort with affection. This aligns with the interpersonal coldness and suspiciousness seen in paranoid personality disorder. The lack of nurturing and emotional engagement during early development impairs the ability to form secure attachments, leading to persistent mistrust and guardedness in adulthood.
Rationale for incorrect answers
A. While affection may have been limited, the key developmental factor is emotional indifference rather than absence of approval. Lack of approval alone does not explain the pervasive suspiciousness and interpersonal detachment.
B. A lack of empathy and nurturing is more characteristic of antisocial or narcissistic traits. Paranoid personality disorder stems more from emotional neglect and indifference than overt cruelty or lack of empathy.
D. Recognition in early childhood followed by neglect in adolescence may contribute to mood or identity disorders, but it does not explain the chronic mistrust and guardedness central to paranoid personality disorder.
Take Home Points
- Paranoid personality disorder often stems from emotionally indifferent or neglectful early environments.
- Clients may struggle with intimacy and interpret affection as manipulation or threat.
- Differentiation from antisocial traits involves absence of cruelty but presence of emotional coldness.
- Therapeutic approaches must be structured, predictable, and emotionally neutral to avoid triggering mistrust.
Which of the following should a nurse include as a primary outcome for an individual with schizoid personality disorder?
Explanation
Schizoid personality disorder is a Cluster A condition marked by pervasive detachment from social relationships and a restricted range of emotional expression. Individuals often appear emotionally cold, prefer solitary activities, and show little interest in forming close relationships. They are not distressed by their isolation and typically function best when left alone. These individuals may maintain employment and basic self-care but avoid interpersonal engagement. The disorder is chronic and ego-syntonic, meaning the person does not view their behavior as problematic. The focus of care is on maintaining independent functioning, ensuring safety, and supporting basic needs rather than altering personality traits.
Rationale for correct answer
B. The goal of care for individuals with schizoid personality disorder is to support independent functioning in the community. These individuals are often capable of managing daily tasks and employment if allowed to do so without excessive social demands. Promoting autonomy and ensuring they can meet their basic needs without relying on others aligns with both therapeutic goals and the individual’s preferences.
Rationale for incorrect answers
A. The need to validate ideas before acting is more relevant to disorders involving impulsivity or distorted thinking, such as borderline or schizotypal personality disorders. Schizoid individuals are not typically impulsive or socially reactive, and they do not seek validation from others.
C. Emotional regulation is not a primary concern in schizoid personality disorder because these individuals already exhibit emotional detachment and flat affect. They do not experience intense emotional swings or dysregulation that would necessitate this outcome.
D. Recognizing limits is more applicable to individuals with narcissistic or borderline traits who may overestimate their abilities or violate boundaries. Schizoid individuals are already withdrawn and self-limiting, often under-engaging rather than overreaching.
Which behavior should a nurse expect a client diagnosed with paranoid personality disorder to exhibit?
Explanation
Paranoid personality disorder is a Cluster A disorder characterized by pervasive distrust and suspiciousness of others. Individuals interpret others’ motives as malevolent, often without sufficient evidence. They are hypervigilant, reluctant to confide in others, and may bear grudges. These clients frequently misinterpret benign remarks or behaviors as hostile or threatening. They are not delusional but their cognitive distortions and interpersonal sensitivity lead to chronic interpersonal difficulties. The condition is ego-syntonic, meaning the person does not view their behavior as problematic, and they often resist treatment due to mistrust of providers.
Rationale for correct answer
D. Individuals with paranoid personality disorder frequently analyze others’ behaviors for hidden meanings, often interpreting neutral or positive actions as threats. This hypervigilance and misinterpretation are central features of the disorder and contribute to their social isolation and interpersonal conflict.
Rationale for incorrect answers
A. Trust is impaired in paranoid personality disorder, even toward those who treat them well. These individuals often question motives and may perceive kindness as manipulation or deceit.
B. Rather than seeing goodwill where none exists, these clients tend to perceive malevolence even when none is present. They are unlikely to interpret others’ actions positively without suspicion.
C. Acting opposite to thoughts or feelings is more characteristic of disorders involving emotional dysregulation or manipulative behavior, such as borderline or histrionic personality disorders. Paranoid individuals are more likely to act in line with their suspicious thoughts.
Take Home Points
- Paranoid personality disorder involves pervasive distrust and misinterpretation of others’ motives as threatening.
- These individuals often analyze others’ behavior for hidden meanings and are resistant to forming trusting relationships.
- Unlike psychotic disorders, paranoid personality disorder does not involve delusions but rather fixed suspicious beliefs.
- It is important to differentiate paranoid personality disorder from schizophrenia and delusional disorder, which involve psychosis.
A client diagnosed with a personality disorder insists that a grandmother, through reincarnation, has come back to life as a pet kitten. The thought process described is reflective of which personality disorder?
Explanation
Schizotypal personality disorder is a Cluster A disorder marked by pervasive social deficits, cognitive or perceptual distortions, and eccentric behavior. Individuals often exhibit magical thinking, odd beliefs, and unusual perceptual experiences that are not delusional but are culturally or personally idiosyncratic. They may believe in telepathy, reincarnation, or other supernatural phenomena. These clients often display paranoid ideation, social anxiety, and eccentric speech or appearance. Unlike schizophrenia, they do not experience full-blown psychosis, but their thought processes are notably distorted and disconnected from conventional norms.
Rationale for correct answer
B. The belief that a deceased grandmother has reincarnated as a kitten reflects magical thinking, a hallmark of schizotypal personality disorder. This type of cognitive distortion is common in schizotypal individuals, who often hold unusual beliefs that are not grounded in reality but are not considered delusional either.
Rationale for incorrect answers
A. Passive-aggressive personality disorder involves indirect expression of hostility, procrastination, and resistance to demands, not magical thinking or perceptual distortions. The behavior described does not reflect interpersonal defiance or covert aggression.
C. Borderline personality disorder is characterized by emotional instability, fear of abandonment, and identity disturbance. While transient psychotic-like symptoms may occur under stress, persistent magical beliefs are not typical.
D. Schizoid personality disorder involves emotional detachment and social withdrawal, but not cognitive or perceptual distortions. These individuals do not typically engage in magical thinking or unusual beliefs.
Take Home Points
- Schizotypal personality disorder includes magical thinking, perceptual distortions, and eccentric behavior without full psychosis.
- It must be differentiated from schizophrenia, which involves delusions and hallucinations.
- Unlike schizoid personality disorder, schizotypal clients often experience social anxiety and odd beliefs.
- Borderline personality disorder may show transient psychotic symptoms but lacks persistent magical thinking.
A client has been diagnosed with a cluster A personality disorder. Which client statement would reflect cluster A characteristics?
Explanation
Cluster A personality disorders include paranoid, schizoid, and schizotypal types. These disorders are marked by odd, eccentric, or socially detached behaviors. Clients often exhibit distorted thinking, social withdrawal, and unusual beliefs. Paranoid individuals are suspicious and mistrustful; schizoid individuals are emotionally detached and prefer solitude; schizotypal individuals show magical thinking, perceptual distortions, and eccentric behavior. These disorders are ego-syntonic, meaning the individual does not see their behavior as problematic, and they often resist treatment due to mistrust or lack of insight.
Rationale for correct answer
B. The belief that one’s dinner has been poisoned reflects the suspiciousness and mistrust typical of paranoid personality disorder, a Cluster A condition. These clients often misinterpret benign actions as malevolent and may harbor persistent, unfounded suspicions about others’ intentions.
Rationale for incorrect answers
A. Grandiose self-appraisal such as claiming to be the best chef reflects narcissistic traits, which are part of Cluster B personality disorders. These individuals seek admiration and have an inflated sense of self-importance, not the social detachment or suspiciousness seen in Cluster A.
C. Repetitive handwashing is a hallmark of obsessive-compulsive disorder, which is an anxiety-related condition, not a personality disorder. Obsessive-compulsive personality disorder (Cluster C) involves rigidity and perfectionism, but not compulsions like this.
D. Inability to eat alone suggests dependent traits, where individuals feel anxious or helpless without others. This aligns with Cluster C disorders, which are marked by anxious and fearful behavior, not the eccentricity of Cluster A.
Take Home Points
- Cluster A personality disorders involve eccentric, socially detached, or suspicious behavior patterns.
- Paranoid personality disorder is characterized by pervasive mistrust and misinterpretation of others’ intentions.
- Schizotypal personality disorder includes magical thinking and perceptual distortions without full psychosis.
- These disorders must be differentiated from Cluster B (dramatic/emotional) and Cluster C (anxious/fearful) personality disorders.
Which scenario would the nurse expect to observe if the client were diagnosed with paranoid personality disorder?
Explanation
Paranoid personality disorder is a Cluster A condition marked by pervasive distrust and suspicion of others. Individuals with this disorder often believe that others are exploiting, harming, or deceiving them, even without evidence. They are hypervigilant, reluctant to confide in others, and may interpret benign remarks or events as threatening. These clients often appear guarded, hostile, or aloof, and they may isolate themselves due to their suspiciousness. Unlike psychotic disorders, their beliefs do not reach delusional intensity, but their thought patterns are rigid and resistant to change. They are often difficult to engage in therapeutic relationships due to their mistrust.
Rationale for correct answer
A. The statement “Everyone wants to hurt me” reflects the suspiciousness and pervasive mistrust characteristic of paranoid personality disorder. These clients often isolate themselves and interpret others’ actions as threatening, even in neutral or supportive environments.
Rationale for incorrect answers
B. Exploiting others for cigarettes reflects manipulative and irresponsible behavior more typical of antisocial personality disorder, a Cluster B condition. Paranoid individuals are more likely to avoid interaction than to manipulate others.
C. Shyness and avoidance due to low self-esteem are features of avoidant personality disorder, a Cluster C condition. Paranoid individuals avoid others due to mistrust, not feelings of inadequacy.
D. Allowing others to make decisions reflects submissiveness, which is characteristic of dependent personality disorder. Paranoid individuals are controlling and mistrustful, not passive or deferential.
Take Home Points
- Paranoid personality disorder involves pervasive mistrust and misinterpretation of others’ intentions as hostile.
- These individuals often isolate themselves and are resistant to forming trusting relationships.
- It must be differentiated from avoidant personality disorder, which involves social withdrawal due to fear of rejection.
- Unlike Cluster B disorders, paranoid individuals are not manipulative or emotionally volatile.
Which diagnostic criterion describes schizotypal personality disorder?
Explanation
Schizotypal personality disorder is a Cluster A condition characterized by pervasive social and interpersonal deficits, marked by acute discomfort with close relationships, and cognitive or perceptual distortions. Individuals often display eccentric behavior, odd beliefs or magical thinking, unusual perceptual experiences, and peculiar speech. They may appear socially anxious, suspicious, or emotionally constricted. Unlike schizophrenia, they do not experience persistent delusions or hallucinations, but their thinking is often tangential or metaphorical. Their appearance or behavior may be noticeably unusual, contributing to social isolation and functional impairment.
Rationale for correct answer
D. The presence of odd or eccentric behavior or appearance is a hallmark diagnostic criterion of schizotypal personality disorder. This includes unusual dress, speech patterns, or mannerisms that deviate from social norms and contribute to interpersonal discomfort.
Rationale for incorrect answers
A. Lack of desire for close relationships is a defining feature of schizoid personality disorder, not schizotypal. Schizoid individuals are emotionally detached but do not exhibit cognitive or perceptual distortions.
B. Persistent doubts about others’ loyalty are characteristic of paranoid personality disorder. These individuals are mistrustful and interpret others’ actions as malevolent, without the eccentricity seen in schizotypal disorder.
C. Misjudging intimacy in relationships is typical of borderline personality disorder, where individuals may rapidly idealize others and experience intense fear of abandonment, not the social awkwardness and magical thinking of schizotypal disorder.
Take Home Points
- Schizotypal personality disorder includes eccentric behavior, magical thinking, and social anxiety without full psychosis.
- It differs from schizoid personality disorder, which lacks perceptual distortions and magical beliefs.
- Paranoid personality disorder involves mistrust but not the cognitive eccentricities of schizotypal disorder.
- Borderline personality disorder features emotional instability and distorted interpersonal boundaries, not odd behavior.
A client diagnosed with schizoid personality disorder chooses solitary activities, lacks close friends, and appears indifferent to criticism. Which nursing diagnosis would be appropriate for this client’s problem?
Explanation
Schizoid personality disorder is a Cluster A condition marked by pervasive social detachment, restricted emotional expression, and preference for solitary activities. Individuals with this disorder neither desire nor enjoy close relationships, including family bonds. They appear emotionally cold, indifferent to praise or criticism, and often choose isolated lifestyles. These traits are ego-syntonic, meaning the person does not perceive them as problematic. The clinical focus is on supporting basic functioning and recognizing the discomfort these individuals feel with interpersonal engagement, rather than attempting to increase socialization or emotional expression.
Rationale for correct answer
D. The diagnosis of social isolation is appropriate because the client avoids others due to discomfort with human interaction, not due to fear or low self-esteem. This aligns with the core features of schizoid personality disorder, where the individual prefers solitude and shows emotional indifference.
Rationale for incorrect answers
A. Anxiety related to poor self-esteem is not consistent with schizoid personality disorder. These individuals are emotionally detached, not anxious or self-critical, and their lack of relationships stems from preference rather than insecurity.
B. Ineffective coping due to communication deficits implies a desire or need to engage, which schizoid individuals lack. Their indifference to criticism is not a sign of poor coping but a reflection of their emotional constriction.
C. Altered sensory perception and magical thinking are features of schizotypal personality disorder, not schizoid. Schizoid individuals do not exhibit perceptual distortions or eccentric beliefs.
Take Home Points
- Schizoid personality disorder involves emotional detachment, solitary lifestyle, and indifference to social feedback.
- Social isolation is a fitting nursing diagnosis due to the client’s discomfort with interpersonal interaction.
- It must be differentiated from schizotypal disorder, which includes perceptual distortions and magical thinking.
- Unlike avoidant personality disorder, schizoid individuals do not avoid others due to fear of rejection or low self-esteem.
An adult is diagnosed with schizotypal personality disorder. How should a nurse describe the client’s behavior?
Explanation
Schizotypal personality disorder is a pervasive pattern of social and interpersonal deficits marked by acute discomfort with close relationships, cognitive or perceptual distortions, and eccentric behavior. Individuals often display odd beliefs, magical thinking, and unusual perceptual experiences. They may appear socially anxious, have constricted affect, and exhibit paranoid ideation. These traits are stable over time and lead to significant functional impairment, particularly in interpersonal domains. Unlike schizophrenia, they do not typically experience full-blown psychosis, though they may have transient psychotic episodes under stress.
Rationale for correct answer
D. Individuals with schizotypal personality disorder are typically introverted and display emotional withdrawal due to their discomfort with close relationships and pervasive social anxiety. Their interpersonal deficits are rooted in cognitive distortions and eccentric behavior, leading to isolation and limited emotional expression. These clients often appear aloof, suspicious, and socially awkward, which aligns with the observed withdrawn demeanor.
Rationale for incorrect answers
A. The term rigid is more characteristic of obsessive-compulsive personality disorder, where individuals are preoccupied with orderliness, perfectionism, and control. Schizotypal individuals are not controlling but rather socially detached and eccentric.
B. Submissive and immature traits are more aligned with dependent personality disorder, where individuals exhibit clinginess and fear of separation. Schizotypal clients are socially distant and do not seek dependency on others.
C. Arrogant and attention-seeking behaviors are typical of narcissistic or histrionic personality disorders. Schizotypal individuals tend to avoid attention due to their discomfort in social settings and do not exhibit grandiosity or dramatic behavior.
Take Home Points
- Schizotypal personality disorder involves eccentric behavior, cognitive distortions, and social withdrawal without full psychosis.
- It must be differentiated from schizophrenia, which includes persistent hallucinations and delusions.
- Unlike avoidant personality disorder, schizotypal traits include magical thinking and perceptual distortions.
- Treatment includes supportive psychotherapy and sometimes low-dose antipsychotics for transient psychotic symptoms.
A nurse begins a relationship with a client with the diagnosis of schizotypal personality disorder. What is the initial nursing action?
Explanation
Schizotypal personality disorder is a Cluster A personality disorder marked by pervasive social deficits, cognitive-perceptual distortions, and eccentric behavior. Individuals often exhibit social anxiety, odd beliefs, and paranoid ideation. They may appear aloof, have few close relationships, and struggle with interpersonal intimacy. Speech may be vague or metaphorical, and behavior can seem eccentric or peculiar. Unlike schizophrenia, they do not have persistent psychosis, but transient psychotic episodes may occur under stress. Functioning is often impaired, especially in occupational and social domains.
Rationale for correct answer
D. The client’s behavior aligns with introversion and emotional detachment, which are hallmark traits of schizotypal personality disorder. These individuals avoid close relationships, exhibit social withdrawal, and often appear emotionally cold or indifferent. Their discomfort with intimacy and suspicion of others contributes to their isolation. The emotional constriction and interpersonal deficits are consistent with the DSM-5 diagnostic criteria.
Rationale for incorrect answers
A. The term rigid is more characteristic of obsessive-compulsive personality disorder, where individuals are preoccupied with order, perfectionism, and control. Schizotypal individuals are not controlling but rather socially anxious and withdrawn.
B. Submissiveness and immaturity are more typical of dependent personality disorder, where individuals rely excessively on others for decision-making and support. Schizotypal clients are more socially detached and suspicious, not dependent.
C. Arrogance and attention-seeking behaviors are associated with narcissistic or histrionic personality disorders. Schizotypal individuals tend to avoid attention due to their discomfort in social situations and do not seek admiration or approval.
Take Home Points
- Schizotypal personality disorder involves social withdrawal, eccentric behavior, and cognitive-perceptual distortions without persistent psychosis.
- It must be differentiated from schizophrenia, which includes sustained delusions and hallucinations.
- Unlike Cluster B disorders, schizotypal individuals avoid attention and exhibit emotional constriction.
- Treatment focuses on building trust, supporting social skills, and managing transient psychotic symptoms.
A nurse notices that a client with paranoid personality disorder demonstrates some instances of spying behaviors on other clients on the unit. Which nursing intervention should the nurse institute?
Explanation
Paranoid personality disorder is a Cluster A disorder characterized by pervasive distrust, suspiciousness, and a tendency to interpret others’ motives as malevolent. These individuals often misinterpret benign actions as threatening, are hypervigilant, and may exhibit guarded or hostile behavior. They typically lack insight into their condition and are reluctant to accept psychological explanations for their behavior. Interventions must prioritize structure, consistency, and clear boundaries to reduce perceived threats and maintain safety in therapeutic environments.
Rationale for correct answer
B. Clients with paranoid personality disorder respond best to clear structure and consistent enforcement of rules. Addressing the behavior in terms of unit expectations, rather than personal flaws, reduces defensiveness and maintains therapeutic rapport. This approach avoids challenging the client’s distorted perceptions directly, which could escalate mistrust or hostility, and instead focuses on observable behavior and unit norms.
Rationale for incorrect answers
A. Focusing on relationships may be perceived as intrusive or judgmental by a paranoid client. They are unlikely to accept that their behavior interferes with social connection, and such feedback may increase suspicion or withdrawal.
C. Encouraging self-reflection on thinking patterns is more appropriate for clients with insight, such as those with anxiety or depressive disorders. Paranoid individuals typically lack insight and may view such suggestions as accusatory or manipulative.
D. Attributing behavior to feelings or personality changes risks invalidating the client’s experience. Paranoid clients often externalize blame and are unlikely to accept emotional explanations, which may be interpreted as an attack on their character.
Take Home Points
- Paranoid personality disorder involves pervasive distrust, suspicion, and misinterpretation of others’ motives.
- Interventions should emphasize structure, consistency, and behavioral boundaries rather than emotional insight.
- Avoid challenging paranoid beliefs directly; instead, focus on observable behavior and unit expectations.
- Differentiate from schizophrenia by the absence of persistent hallucinations or delusions.
Clients with a schizotypal personality disorder are most likely to benefit from which of the following nursing interventions?
Explanation
Schizotypal personality disorder is a Cluster A disorder marked by social deficits, eccentric behavior, and cognitive-perceptual distortions. Clients often exhibit odd beliefs, magical thinking, and suspiciousness. They struggle with interpersonal relationships due to discomfort with closeness and impaired social skills. Though not psychotic, they may experience transient psychotic episodes under stress. Their speech may be vague or metaphorical, and they often appear emotionally constricted. These individuals benefit most from structured interventions that target interpersonal functioning and reduce social isolation.
Rationale for correct answer
D. Teaching social skills is essential because clients with schizotypal personality disorder often lack the ability to form and maintain relationships. Structured social skills training helps reduce isolation, improve communication, and increase functional engagement. This intervention directly addresses their interpersonal deficits and supports gradual integration into social environments.
Rationale for incorrect answers
A. Cognitive restructuring is more effective for clients with insight, such as those with anxiety or depression. Schizotypal clients often lack insight and may not respond well to interventions that challenge their distorted beliefs directly.
B. Improving community functioning is a broader goal that depends on foundational interpersonal skills. Without addressing core social deficits first, efforts to enhance community integration are likely to fail or increase stress.
C. Providing emotional support alone does not address the functional impairments in social interaction. While support is important, it must be paired with skill-building to produce meaningful behavioral change.
Take Home Points
- Schizotypal personality disorder involves eccentric behavior, social withdrawal, and cognitive-perceptual distortions.
- Social skills training is a primary intervention to improve interpersonal functioning and reduce isolation.
- Insight-oriented therapies are less effective due to limited self-awareness in these clients.
- Differentiate from schizophrenia by the absence of persistent delusions or hallucinations.
A client newly admitted to an inpatient psychiatric unit is diagnosed with schizotypal personality disorder. The client states, “I can’t believe you are not afraid of the monsters coming after us all.” Which is the most appropriate nursing response?
Explanation
Schizotypal personality disorder is a Cluster A condition marked by cognitive-perceptual distortions, eccentric behavior, and social anxiety. Clients may express odd beliefs, magical thinking, or suspiciousness, and under stress, may experience transient psychotic-like symptoms. These individuals often lack close relationships and exhibit constricted affect. While they may not have full-blown delusions, their thoughts can appear bizarre or illogical. Therapeutic communication must focus on validation, emotional containment, and maintaining trust without reinforcing distorted beliefs.
Rationale for correct answer
D. This response acknowledges the client’s distress without validating the content of the thought. It maintains therapeutic neutrality, offers support, and invites collaboration. This approach respects the client’s experience while gently redirecting focus toward emotional needs, which is essential in managing transient psychotic-like symptoms in schizotypal personality disorder.
Rationale for incorrect answers
A. Denying the client’s perception by saying don’t know what they’re talking about may increase defensiveness and mistrust. It invalidates their experience and can escalate paranoia or withdrawal.
B. Asking for more details about the monsters risks reinforcing the client’s distorted thinking. It may be interpreted as agreement or interest in the delusion, which can deepen the cognitive-perceptual distortion.
C. Redirecting to group without first addressing the client’s emotional state may feel dismissive. It overlooks the immediate need for emotional validation and containment, which is critical in early rapport-building.
Take Home Points
- Schizotypal personality disorder involves eccentric behavior, social withdrawal, and transient psychotic-like symptoms.
- Therapeutic responses should validate emotional distress without reinforcing distorted beliefs.
- Avoid direct confrontation or denial of odd thoughts; instead, focus on emotional support and safety.
- Differentiate from schizophrenia by the absence of sustained delusions or hallucinations.
A client diagnosed with paranoid personality disorder needs information regarding medications. Which nursing intervention would assist this client in understanding prescribed medications?
Explanation
Paranoid personality disorder is a Cluster A disorder marked by pervasive distrust, suspiciousness, and a tendency to interpret others’ motives as threatening. These clients often feel vulnerable in group settings and may misinterpret neutral actions as hostile. They are hypervigilant, reluctant to share personal information, and may resist interventions perceived as manipulative. Effective nursing care requires individualized communication, clear boundaries, and a nonjudgmental approach that respects the client’s need for control and privacy.
Rationale for correct answer
B. Providing one-on-one teaching in the client’s room minimizes perceived threats and respects the client’s need for privacy and control. This approach reduces anxiety, builds trust, and allows for tailored explanations without the pressure of group dynamics. It also avoids triggering suspiciousness that may arise in public or unfamiliar settings.
Rationale for incorrect answers
A. Group education may provoke anxiety or mistrust in paranoid clients. They often feel threatened in group environments and may interpret others’ behavior as targeting or judging them, impairing learning.
C. Having the physician ask during rounds may feel impersonal or coercive. Paranoid clients may perceive this as a setup or interrogation, especially in a public setting with multiple staff present.
D. Reading a handout alone does not address the client’s need for clarification or reassurance. Paranoid individuals may misinterpret written information or distrust its source, leading to increased confusion or resistance.
Take Home Points
- Paranoid personality disorder involves pervasive distrust and hypersensitivity to perceived threats.
- One-on-one teaching builds trust and reduces anxiety in clients with paranoid traits.
- Group settings and impersonal interactions may increase suspicion and hinder therapeutic engagement.
- Written materials alone are insufficient; personalized verbal communication is essential.
A nurse encourages an angry client to attend group therapy. Knowing that the client has been diagnosed with a cluster B personality disorder, which client response might the nurse expect?
Explanation
Cluster B personality disorders include antisocial, borderline, histrionic, and narcissistic types. These disorders are marked by emotional dysregulation, impulsivity, and dramatic or erratic behavior. Clients often struggle with interpersonal relationships, exhibit manipulative or attention-seeking behaviors, and may respond to perceived criticism with hostility or sarcasm. Anger and defensiveness are common, especially when confronted with therapeutic interventions. Their reactions are often externalized, and they may resist group settings due to fear of judgment or loss of control.
Rationale for correct answer
A. The sarcastic remark reflects defensiveness and hostility, which are common in Cluster B disorders. Clients may use sarcasm to deflect vulnerability and avoid emotional exposure in group therapy. This response also demonstrates a lack of insight and resistance to therapeutic engagement, consistent with the interpersonal challenges seen in these disorders.
Rationale for incorrect answers
B. Scornful responses involving bizarre content are more typical of Cluster A disorders, such as schizotypal personality disorder. Cluster B clients may be dramatic, but they do not usually exhibit magical thinking or psychotic-like speech.
C. Suspiciousness and paranoid ideation are hallmark features of Cluster A disorders, particularly paranoid personality disorder. Cluster B clients are more likely to externalize blame through emotional outbursts than through paranoid delusions.
D. Hesitant cooperation and seeking proximity suggest traits of dependent personality disorder, which falls under Cluster C. Cluster B individuals are less likely to seek closeness and more likely to challenge authority or resist group participation.
Take Home Points
- Cluster B personality disorders involve emotional instability, impulsivity, and dramatic interpersonal behavior.
- Sarcasm and hostility are common defense mechanisms used to avoid vulnerability.
- These disorders differ from Cluster A (odd/eccentric) and Cluster C (anxious/fearful) in their interpersonal style.
- Group therapy may provoke resistance due to fear of judgment or loss of control.
Which behaviors should a nurse expect when working with a client with histrionic personality disorder? Select all that apply
Explanation
Histrionic personality disorder is a Cluster B personality disorder marked by pervasive emotionality and attention-seeking behavior. Individuals with this disorder often display exaggerated emotions, are easily influenced by others, and exhibit inappropriate seductiveness. Their self-esteem is often dependent on the approval of others, and they may use dramatic speech or physical appearance to remain the center of attention. They tend to overestimate the intimacy of relationships and may become distressed when not the focus of social interactions.
Rationale for correct answers
A. Individuals with this disorder experience significant discomfort when they are not the focus of attention. This is a hallmark feature and often drives their dramatic or provocative behavior in social settings.
D. These clients frequently misinterpret the depth of relationships, believing casual acquaintances are deeply intimate. This distortion supports their need for validation and emotional closeness, even when unwarranted.
F. They often use appearance to attract attention, dressing inappropriately or flamboyantly. This behavior is not merely aesthetic but serves a psychological function to maintain social focus and approval.
Rationale for incorrect answers
B. The term apathy is inconsistent with the emotional expressiveness seen in this disorder. These individuals are often overly expressive and animated, not emotionally flat or withdrawn.
C. While they may have superficial relationships, they do not typically lack companions. Their social behavior is often gregarious, though relationships may lack depth or authenticity.
E. Suspiciousness about a partner’s fidelity is more characteristic of paranoid or borderline personality disorders. Histrionic individuals are more focused on being admired than on distrust or jealousy.
Take Home Points
- Histrionic personality disorder is defined by excessive emotionality and attention-seeking behaviors, often through dramatic or seductive actions.
- Clients may overestimate the intimacy of relationships and become distressed when not the center of attention.
- They often use physical appearance and exaggerated emotions to maintain social focus.
- It is important to differentiate this disorder from borderline and narcissistic personality disorders, which may share overlapping traits but differ in core motivations.
Practice Exercise 3
Which behaviors should a nurse expect when working with a client with histrionic personality disorder? Select all that apply
Explanation
Histrionic personality disorder is a Cluster B personality disorder marked by pervasive emotionality and attention-seeking behavior. Individuals with this disorder often display exaggerated emotions, are easily influenced by others, and exhibit inappropriate seductiveness. Their self-esteem is often dependent on the approval of others, and they may use dramatic speech or physical appearance to remain the center of attention. They tend to overestimate the intimacy of relationships and may become distressed when not the focus of social interactions.
Rationale for correct answers
A. Individuals with this disorder experience significant discomfort when they are not the focus of attention. This is a hallmark feature and often drives their dramatic or provocative behavior in social settings.
D. These clients frequently misinterpret the depth of relationships, believing casual acquaintances are deeply intimate. This distortion supports their need for validation and emotional closeness, even when unwarranted.
F. They often use appearance to attract attention, dressing inappropriately or flamboyantly. This behavior is not merely aesthetic but serves a psychological function to maintain social focus and approval.
Rationale for incorrect answers
B. The term apathy is inconsistent with the emotional expressiveness seen in this disorder. These individuals are often overly expressive and animated, not emotionally flat or withdrawn.
C. While they may have superficial relationships, they do not typically lack companions. Their social behavior is often gregarious, though relationships may lack depth or authenticity.
E. Suspiciousness about a partner’s fidelity is more characteristic of paranoid or borderline personality disorders. Histrionic individuals are more focused on being admired than on distrust or jealousy.
Take Home Points
- Histrionic personality disorder is defined by excessive emotionality and attention-seeking behaviors, often through dramatic or seductive actions.
- Clients may overestimate the intimacy of relationships and become distressed when not the center of attention.
- They often use physical appearance and exaggerated emotions to maintain social focus.
- It is important to differentiate this disorder from borderline and narcissistic personality disorders, which may share overlapping traits but differ in core motivations.
A 45-year-old male client with no psychiatric history is admitted to the emergency department after physically assaulting his wife. The client is frightened by his loss of control. He tells the nurse that he is self-employed, recently expanded his company nationally, and has many well-known friends. His wife angrily states, “That’s what is important to you; who you know and how it looks!” Despite recent financial losses, the client continues his lavish lifestyle. The nurse determines that the client’s behavior is typical of:
Explanation
Narcissistic personality disorder is a Cluster B personality disorder characterized by a pervasive pattern of grandiosity, need for admiration, and lack of empathy. Individuals often exaggerate achievements, expect special treatment, and are preoccupied with fantasies of success or power. They may exploit others, appear arrogant, and have fragile self-esteem that is vulnerable to criticism. Despite external confidence, their self-worth is often dependent on external validation and admiration.
Rationale for correct answer
C. The client demonstrates classic features of narcissistic personality disorder, including grandiosity (boasting about national business expansion and famous friends), lack of empathy (assaulting his wife), and continued lavish spending despite financial losses. His wife’s comment highlights his preoccupation with image and status, which are central to this disorder.
Rationale for incorrect answers
A. Borderline personality disorder is marked by emotional instability, fear of abandonment, and impulsive behaviors. While aggression can occur, the absence of unstable relationships, identity disturbance, and affective lability makes this less likely.
B. Schizoid personality disorder involves detachment from social relationships and restricted emotional expression. The client’s social engagement, business expansion, and concern with image are inconsistent with the social withdrawal typical of this disorder.
D. Dependent personality disorder is characterized by submissiveness, excessive need to be taken care of, and fear of separation. The client’s assertiveness, self-promotion, and independence in business contradict the passive and clingy behavior seen in this disorder.
Take Home Points
- Narcissistic personality disorder involves grandiosity, need for admiration, and lack of empathy, often masked by superficial charm.
- It must be differentiated from borderline personality disorder, which centers on emotional instability and abandonment fears.
- Schizoid personality disorder presents with social detachment and flattened affect, not attention-seeking or status preoccupation.
- Dependent personality disorder features submissiveness and fear of separation, not assertiveness or self-aggrandizement.
Individuals with antisocial personality disorder often exhibit poor judgment, emotional distance, aggression, and impulsivity. A nurse understands that besides the limbic system, which other area of the brain is implicated in causing these behaviors? Place an X on the affected area.
Explanation
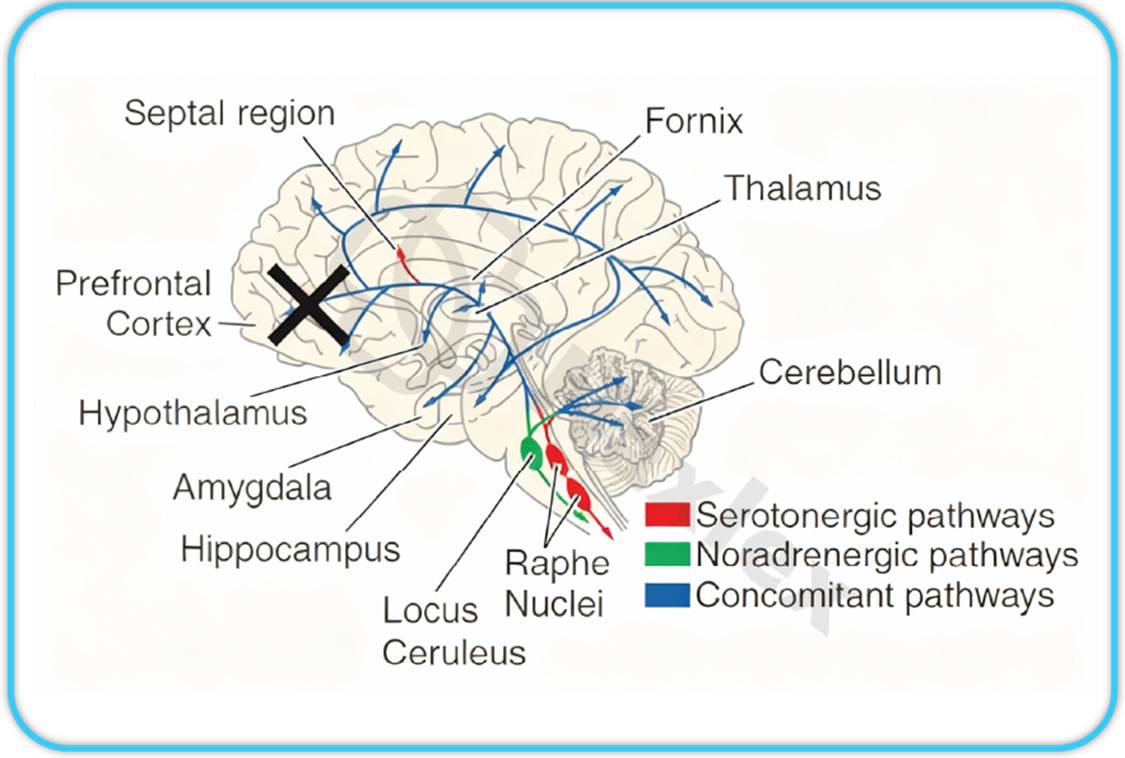
Antisocial personality disorder (ASPD) is a chronic mental condition characterized by disregard for others, violation of social norms, and impulsive aggression. It is associated with dysfunction of brain regions responsible for emotional regulation, judgment, and behavior inhibition. Neuroimaging shows reduced prefrontal activity, particularly in the orbitofrontal and ventromedial areas, leading to impaired moral reasoning and impulse control. Low serotonin and altered noradrenergic signaling also contribute to aggression and emotional detachment in affected individuals.
Rationale for correct answer
Prefrontal Cortex: The prefrontal cortex governs executive functioning, decision-making, and emotional regulation. In antisocial personality disorder, this region shows hypoactivity, impairing the ability to plan, empathize, and control impulses. The lack of inhibitory control allows unchecked limbic-driven emotions such as aggression or risk-taking to dominate behavior. Lesions or developmental deficits in this area result in socially inappropriate actions and moral insensitivity. The prefrontal cortex thus integrates higher reasoning and behavioral restraint, making its dysfunction central to ASPD traits.
Rationale for incorrect answers
Amygdala: The amygdala mediates fear and aggression, but alone it cannot explain poor moral reasoning or social decision-making. Dysfunction increases aggression but does not impair executive control.
Hippocampus: The hippocampus is essential for memory formation and spatial learning, not impulse regulation. Damage causes memory deficits but does not produce the disinhibited or antisocial behaviors of ASPD.
Hypothalamus: The hypothalamus regulates autonomic and endocrine responses, influencing hunger, sleep, and stress. Its dysfunction alters physiological states, not moral or judgmental capacities linked to social behavior.
Thalamus: The thalamus acts as a sensory relay center. While it contributes to attention and consciousness, it does not directly control emotional restraint or decision-making involved in antisocial traits.
Cerebellum: The cerebellum coordinates movement and balance. Though it plays minor roles in emotion, it primarily affects motor precision, not cognitive or moral processes related to ASPD.
Locus Ceruleus: The locus ceruleus releases norepinephrine for arousal and alertness. Dysfunction causes changes in vigilance or sleep but not the persistent behavioral disinhibition seen in ASPD.
Raphe Nuclei: The raphe nuclei produce serotonin affecting mood and arousal. While low serotonin links to impulsivity, it is a biochemical factor, not a structural cause of moral or social dysfunction.
Septal Region and Fornix: The septal region and fornix are limbic connections aiding emotion and memory integration. Dysfunction affects motivation and arousal but not higher-order decision-making or moral judgment.
Take Home Points
- The prefrontal cortex regulates judgment, inhibition, and moral reasoning, and its dysfunction leads to antisocial traits.
- The limbic system controls emotions, but prefrontal regulation prevents impulsive or aggressive actions.
- Serotonin imbalance contributes to impulsivity but structural prefrontal deficits are central to antisocial behavior.
- Differentiating ASPD from other conditions like borderline personality disorder requires assessing empathy, impulse control, and moral awareness.
A nurse is caring for a client diagnosed with borderline personality disorder who is self-mutilating. Which actions should be taken by the nurse to prevent further self-mutilation by the client? Prioritize the nurse’s actions by placing each step in the correct order.
Explanation
Borderline personality disorder is a chronic psychiatric condition characterized by pervasive instability in mood, self-image, and interpersonal relationships. Individuals often experience intense emotional pain and engage in impulsive behaviors such as self-mutilation to cope with distress. These behaviors are typically triggered by perceived rejection or abandonment and serve as maladaptive attempts to regulate overwhelming affect. Management requires a structured, consistent approach that prioritizes safety, emotional regulation, and therapeutic boundaries.
Rationale for correct order
F. Removing dangerous objects addresses the most immediate safety concern. It eliminates access to tools that could be used for self-harm, satisfying the most basic physiological need and preventing injury.
A. Frequent observation allows early detection of escalating distress and provides opportunities for timely intervention. It supports risk containment and reinforces the therapeutic presence of staff.
G. Assigning one-to-one staff ensures constant supervision and emotional containment. It reduces isolation, enhances safety, and allows for real-time support during emotional crises.
B. Securing a verbal contract engages the client in collaborative safety planning. It promotes autonomy and accountability while reinforcing the therapeutic alliance and internal control over impulses.
C. Caring for wounds without offering sympathy avoids reinforcing maladaptive behavior. It maintains therapeutic neutrality and discourages secondary gain from self-injury.
D. Encouraging discussion of feelings helps the client identify emotional triggers and patterns. It fosters insight and supports the development of healthier coping strategies.
E. Teaching anger expression is a long-term intervention. It builds emotional regulation skills and replaces maladaptive behaviors with constructive outlets, but it is not an immediate safety priority.
Take Home Points
- Borderline personality disorder requires structured, safety-first interventions before therapeutic engagement.
- Self-mutilation is often a maladaptive coping mechanism for emotional dysregulation and must be addressed without reinforcement.
- One-to-one staffing and verbal contracts support containment and therapeutic alliance but must follow environmental safety measures.
- Emotional processing and anger management are essential long-term strategies but secondary to immediate risk reduction.
Situation: Kim has a diagnosis of borderline personality disorder. She often exhibits alternating, clinging and distancing behaviors. The most appropriate nursing intervention with this type of behavior would be to:
Explanation
Borderline personality disorder is a complex psychiatric condition marked by pervasive instability in interpersonal relationships, self-image, and affect, often accompanied by marked impulsivity. Individuals with this disorder frequently experience intense fears of abandonment, leading to splitting, a defense mechanism where others are viewed as all good or all bad. These patients may alternate between clinging and distancing behaviors, which can disrupt therapeutic alliances and staff cohesion. Effective care requires consistent boundaries, structured interactions, and team-based approaches to reduce dependency and manipulation.
Rationale for correct answer
D. Rotating staff prevents the formation of exclusive attachments and reduces the risk of splitting, a hallmark defense in borderline personality disorder. This approach fosters consistency in limit-setting and models healthy interpersonal boundaries, helping the patient generalize relational skills across multiple caregivers. It also protects staff from emotional burnout and triangulation, which are common in managing these patients.
Rationale for incorrect answers
A. Encouraging a single-staff relationship reinforces dependency, which is maladaptive in borderline personality disorder. It increases the risk of idealization and devaluation cycles, undermining therapeutic neutrality and team cohesion.
B. Verbal contracts are ineffective for managing unconscious defense mechanisms like clinging and distancing. These behaviors are not under full volitional control and require structured behavioral interventions, not promises.
C. Withdrawing attention may be perceived as abandonment, intensifying the patient’s fear and worsening symptoms. This response can escalate emotional dysregulation and self-harming behaviors, which are common in this population.
Take Home Points
- Clients with borderline personality disorder often use splitting and alternating attachment behaviors as defense mechanisms against perceived abandonment.
- Rotating staff helps maintain therapeutic neutrality and prevents overdependence on a single caregiver.
- Structured, team-based approaches with consistent boundaries are essential in managing manipulative or emotionally labile behaviors.
- This condition must be differentiated from dependent personality disorder, which lacks the intense affective instability and impulsivity seen in borderline personality disorder.
Kim manipulates the staff in an effort to fulfill her own desires. All of the following may be examples of manipulative behaviors in the borderline client except:
Explanation
Borderline personality disorder is characterized by pervasive instability in affect regulation, impulse control, interpersonal relationships, and self-image. Individuals often experience intense fear of abandonment and may engage in self-injurious behaviors as a maladaptive coping mechanism. These behaviors are not always manipulative but rather reflect emotional dysregulation and internal distress. Manipulation in this context typically involves interpersonal strategies to control or influence others, not self-directed harm.
Rationale for correct answer
D. Cutting after discussing discharge reflects emotional dysregulation, not manipulation. It is a self-harming behavior commonly seen in borderline personality disorder, triggered by perceived abandonment or rejection. The act is self-directed and rooted in affective instability, not a calculated attempt to control staff or outcomes.
Rationale for incorrect answers
A. Refusing to stay alone and expressing loneliness may be a form of attention-seeking behavior. When used repetitively to elicit staff presence or avoid distress, it reflects interpersonal manipulation to fulfill emotional needs.
B. Asking for cigarettes before the agreed time undermines boundaries and exploits inconsistencies in staff enforcement. This is a classic manipulative behavior aimed at testing limits and gaining immediate gratification.
C. Excessive praise of one nurse over others is a form of splitting, a defense mechanism where the client idealizes one caregiver while devaluing others. This fosters division among staff and is used to gain preferential treatment.
Take Home Points
- Self-harm in borderline personality disorder is typically a response to emotional pain, not a manipulative act.
- Manipulative behaviors are interpersonal and goal-directed, often involving boundary-testing or splitting.
- Emotional dysregulation, not manipulation, drives many self-injurious behaviors in borderline clients.
- Differentiating between manipulation and affective instability is essential for therapeutic consistency and safety planning.
“Splitting” by the client with borderline personality disorder denotes:
Explanation
Splitting is a primitive defense mechanism commonly seen in borderline personality disorder. It reflects the inability to integrate positive and negative aspects of self and others into a cohesive whole. Individuals with this disorder often oscillate between idealization and devaluation, perceiving people as either entirely good or entirely bad. This binary thinking disrupts relationships and contributes to emotional instability. Splitting is rooted in early developmental deficits in object constancy and is often triggered by perceived threats to attachment or abandonment.
Rationale for correct answer
B. Splitting is a primitive defense mechanism where individuals fail to reconcile contradictory feelings about others. In borderline personality disorder, this manifests as viewing caregivers or loved ones as either perfect or malicious, depending on emotional state. It impairs interpersonal functioning and contributes to chaotic relationships.
Rationale for incorrect answers
A. Precocious development implies advanced cognitive or emotional maturity, which contradicts the regressive nature of splitting. This defense is developmentally immature and reflects poor integration of self and object representations.
C. Brief psychotic episodes involve loss of contact with reality, such as hallucinations or delusions. Splitting, while maladaptive, does not constitute psychosis and does not impair reality testing to that extent.
D. Two distinct personalities suggest dissociative identity disorder, not borderline personality disorder. Splitting involves dichotomous thinking about others, not fragmentation of the self into separate identities.
Take Home Points
- Splitting is a defense mechanism where individuals perceive others as all good or all bad, common in borderline personality disorder.
- It differs from psychosis and dissociation, as reality testing is generally preserved.
- This behavior disrupts relationships and contributes to emotional instability and interpersonal conflict.
- Effective management includes consistent boundaries and team-based care to reduce idealization and devaluation cycles.
Situation: Jack was arrested for breaking into a jewelry store and stealing thousands of dollars’ worth of diamonds. At his arraignment, the judge ordered a psychological evaluation. He has just been admitted by court order to the locked unit. Based on a long history of maladaptive behavior, he has been given the diagnosis of antisocial personality disorder.
Which of the following characteristics would you expect to assess in Jack?
Explanation
Antisocial personality disorder is a pervasive pattern of disregard for and violation of the rights of others, beginning in childhood or early adolescence and continuing into adulthood. Individuals with this disorder often exhibit deceitfulness, impulsivity, irritability, and consistent irresponsibility. A hallmark feature is a profound lack of remorse for harmful actions. These individuals frequently rationalize or minimize their behavior and show little concern for the consequences of their actions on others. They often manipulate or exploit others for personal gain and fail to conform to social norms or lawful behavior.
Rationale for correct answer
A. Lack of guilt is a defining feature of antisocial personality disorder. These individuals show no remorse for harming others and often justify or deny wrongdoing. This emotional detachment facilitates repeated violations of societal rules and interpersonal boundaries.
Rationale for incorrect answers
B. Insight is typically absent in antisocial personality disorder. These individuals rarely acknowledge the impact of their behavior on others and often externalize blame, minimizing personal responsibility.
C. The ability to learn from past experiences is impaired. Despite repeated legal or social consequences, individuals with this disorder often continue engaging in the same maladaptive behaviors, reflecting poor behavioral adaptation.
D. Compliance with authority is generally lacking. These individuals often challenge rules, manipulate systems, and exhibit defiance toward figures of authority, including law enforcement and healthcare providers.
Take Home Points
- Antisocial personality disorder is marked by lack of remorse, deceitfulness, and disregard for others’ rights.
- Insight and behavioral learning are typically impaired, contributing to repeated legal and interpersonal violations.
- These individuals often manipulate or exploit others and show poor compliance with authority.
- It must be differentiated from narcissistic personality disorder, which involves grandiosity but not necessarily criminal behavior or lack of empathy to the same extent.
Milieu therapy is a good choice for clients with antisocial personality disorder because it:
Explanation
Milieu therapy is a structured therapeutic approach that utilizes the environment as a tool for behavioral and social learning. It emphasizes group norms, peer feedback, and shared responsibility within a controlled setting. For individuals with antisocial personality disorder, who often lack empathy, disregard social norms, and exhibit manipulative or exploitative behaviors, milieu therapy offers a microcosm of society where they can practice adaptive interpersonal skills. The therapeutic community fosters accountability, consistency, and social reinforcement, which are essential for behavioral change in this population.
Rationale for correct answer
B. Milieu therapy emulates a social community, allowing clients with antisocial traits to experience structured interpersonal interactions. It promotes harmonious living through peer feedback, shared norms, and consistent consequences, helping the client internalize social expectations and reduce maladaptive behaviors.
Rationale for incorrect answers
A. A system of punishment and rewards may reinforce external compliance without fostering internal change. Antisocial clients often manipulate such systems and fail to develop genuine prosocial values through this approach alone.
C. One-to-one therapy lacks the social modeling and peer accountability that milieu therapy provides. Antisocial clients benefit more from group-based interactions where they can observe and practice appropriate behaviors.
D. A setting with minimal client input may provoke defiance and resistance in antisocial individuals. Milieu therapy encourages participation and responsibility, which are critical for developing insight and behavioral ownership.
Take Home Points
- Milieu therapy provides a structured social environment that promotes adaptive behavior through peer interaction and shared norms.
- Antisocial personality disorder requires interventions that foster accountability and interpersonal learning, not just individual therapy.
- Punitive systems may be manipulated and fail to produce lasting behavioral change in antisocial clients.
- Client involvement in care planning enhances engagement and reduces resistance, especially in personality disorders marked by defiance.
In evaluating Jack’s progress, which of the following behaviors would be considered the most significant indication of positive change?
Explanation
Behavioral rehabilitation focuses on internal motivation, insight, and sustained change in interpersonal conduct. The most meaningful indicators of progress reflect self-directed actions that demonstrate empathy, accountability, and impulse control. Insight, initiative, and remorse are core markers of psychosocial recovery, especially in individuals with histories of aggression or poor impulse regulation. Remorse, self-control, and accountability are critical in evaluating readiness for reintegration and therapeutic progress.
Rationale for correct answer
C. Sending an apology note independently reflects insight and accountability. It shows Jack is internalizing the impact of his actions and initiating reparative behavior without external prompting, which is a hallmark of genuine behavioral change.
Rationale for incorrect answers
A. Reduced anger episodes may reflect suppression, not transformation. Frequency alone doesn’t indicate internal change or improved coping; it may be situational or externally controlled.
B. Delaying gratification without verbal abuse shows restraint, but it’s reactive and lacks the depth of insight or empathy. It’s a surface-level improvement, not a transformative behavior.
D. Stating intent to stop fighting is verbal, not behavioral. Without action, such declarations lack reliability. Change must be demonstrated through consistent, observable conduct.
Take Home Points
- Self-initiated reparative actions are stronger indicators of behavioral change than verbal promises or reduced symptoms.
- Insight and empathy are critical markers in psychiatric rehabilitation and must be observed through spontaneous prosocial behavior.
- Behavioral restraint alone does not equate to internal transformation; deeper emotional processing is essential.
- Differentiating between suppression and genuine change is key in evaluating progress in individuals with impulse control or aggression issues.
Which of the following behavioral patterns is characteristic of individuals with histrionic personality disorder?
Explanation
Histrionic personality disorder is a Cluster B disorder marked by excessive emotionality and attention-seeking behavior. Individuals often display dramatic, theatrical expressions and are uncomfortable when not the center of attention. Emotionality, attention-seeking, and suggestibility are hallmark traits. These individuals may use physical appearance or provocative behavior to draw attention and often exaggerate emotional responses to minor events.
Rationale for correct answer
B. Overreacting to minor stimuli reflects exaggerated emotionality, a core feature of histrionic personality disorder. These individuals often respond with disproportionate emotional displays to gain attention or validation.
Rationale for incorrect answers
A. Belittling oneself is more consistent with depression, not histrionic traits. Individuals with histrionic personality disorder typically seek admiration and exaggerate strengths rather than minimize them.
C. Suspicion and mistrust are features of paranoid personality disorder, not histrionic. Histrionic individuals are more likely to be trusting and overly familiar, not guarded or suspicious.
D. Lifelong social withdrawal is characteristic of schizoid personality disorder, which contrasts sharply with the sociable, attention-seeking nature of histrionic individuals.
Take Home Points
- Histrionic personality disorder is defined by exaggerated emotionality and attention-seeking behavior.
- It must be differentiated from Cluster A disorders like paranoid and schizoid personality disorders.
- Individuals often misinterpret relationships and display superficial charm and dramatic affect.
- Emotional overreaction and suggestibility are key diagnostic features in clinical evaluation.
A client arrived at the psychiatric unit from the emergency department. His diagnosis is personality disorder, and he exhibits manipulative behavior. As the nurse reviews the unit rules with him, the client asks, “Can I go to the snack shop just one time and then I will answer whatever you ask?” What is the nurse’s most appropriate response?
Explanation
Manipulative behavior is a hallmark of certain personality disorders, especially those in Cluster B, such as borderline and antisocial types. These individuals often challenge boundaries, test limits, and exploit interpersonal dynamics to gain control or avoid responsibility. Firm limit-setting, consistent enforcement of rules, and structured environments are essential to prevent reinforcement of maladaptive behaviors. Nurses must maintain therapeutic neutrality and avoid engaging in negotiations that undermine unit structure or staff authority. Consistency across staff responses is critical to reduce splitting and manipulation.
Rationale for correct answer
D. The nurse’s response demonstrates consistency and limit-setting, which are essential when managing manipulative behaviors. By stating that rules apply to everyone, the nurse avoids negotiation and reinforces structure, reducing reinforcement of manipulation and promoting fairness. This approach prevents splitting and maintains therapeutic boundaries.
Rationale for incorrect answers
A. This response reinforces manipulation by allowing the client to delay assessment in exchange for a privilege. It undermines the nurse’s authority and sets a precedent for bargaining, which destabilizes unit structure.
B. Allowing the client to go with a time limit still rewards manipulative behavior. It suggests that rules are negotiable, which can lead to further testing of boundaries and inconsistent staff responses.
C. While denying the request is appropriate, the lack of explanation makes the response rigid and potentially confrontational. Without reinforcing the rationale that rules apply to all, it may escalate resistance or hostility.
Take Home Points
- Manipulative behavior in personality disorders requires firm, consistent limit-setting to prevent reinforcement.
- Responses to manipulation must avoid negotiation and maintain therapeutic boundaries.
- Rules should be applied uniformly to all clients to prevent splitting and promote fairness.
- Personality disorders often involve testing limits; structured environments reduce maladaptive interpersonal patterns.
A nurse is discharging a client diagnosed with narcissistic personality disorder. Which employment opportunity is most likely to be recommended by the treatment team?
Explanation
Narcissistic personality disorder is characterized by pervasive patterns of grandiosity, need for admiration, and lack of empathy. Individuals often seek positions that reinforce their sense of superiority, authority, or uniqueness. They are drawn to roles that offer power, visibility, or control over others. While they may appear confident and competent, their fragile self-esteem depends on external validation. Structured environments with clear hierarchies can sometimes accommodate their interpersonal style, especially when the role aligns with their self-image.
Rationale for correct answer
D. A role like prison warden provides authority, control, and a structured environment where the individual can assert dominance and receive recognition. This aligns with narcissistic traits such as the need for admiration and power, while minimizing the need for emotional reciprocity.
Rationale for incorrect answers
A. Construction work is task-oriented and collaborative, often requiring humility and teamwork. It lacks the hierarchical recognition or status that narcissistic individuals typically seek.
B. An air traffic controller role demands intense focus, precision, and stress tolerance, but offers little interpersonal recognition or authority over others. It does not satisfy the narcissistic need for admiration or control.
C. A night watchman role is solitary and low-profile, offering minimal opportunity for admiration, influence, or status. It is unlikely to appeal to someone with narcissistic traits.
Take Home Points
- Narcissistic personality disorder involves grandiosity, need for admiration, and preference for roles with authority or visibility.
- Structured environments with clear hierarchies may suit narcissistic individuals if their need for recognition is met.
- Solitary or low-status roles are often poorly tolerated due to lack of external validation.
- Employment planning should consider personality traits to reduce interpersonal conflict and promote role satisfaction.
The nurse working with a client with antisocial personality disorder would expect which of the following behaviors? Select all that apply
Explanation
Antisocial personality disorder is characterized by a pervasive pattern of disregard for and violation of the rights of others. Individuals often exhibit deceitfulness, impulsivity, and lack of remorse. They may manipulate others for personal gain, disregard social norms, and show superficial charm to exploit relationships. Empathy is typically absent, and behaviors are often goal-directed toward self-interest without concern for consequences. These clients may appear cooperative but are often calculating and self-serving.
Rationale for correct answers
B. Individuals with antisocial traits often engage in exploitation of others to achieve personal goals. This includes manipulating peers, deceiving staff, or using coercion without guilt or empathy.
C. Seeking special privileges is common as these clients attempt to manipulate systems for personal benefit. They may use charm, threats, or deceit to bypass rules or gain advantages.
D. Superficial friendliness is a hallmark trait. These individuals may appear engaging or charismatic initially, but the behavior is often manipulative and lacks genuine emotional depth.
Rationale for incorrect answers
A. Genuine compliance is rare in antisocial personality disorder. While clients may appear cooperative, it is often strategic rather than rooted in respect for rules or authority.
E. Use of rituals is more characteristic of obsessive-compulsive or anxiety disorders. Antisocial individuals are typically impulsive and do not rely on structured behaviors to reduce anxiety.
F. Withdrawal is not typical. These clients are often socially active, using interactions to manipulate or dominate others rather than avoiding them.
Take Home Points
- Antisocial personality disorder involves manipulation, deceit, and lack of empathy, often masked by superficial charm.
- Clients may appear cooperative but are often motivated by self-interest and manipulation.
- Unlike anxiety or obsessive disorders, antisocial traits do not include ritualistic or avoidant behaviors.
- Nursing care requires firm boundaries, consistent limit-setting, and awareness of manipulation tactics.
Irresponsible, guiltless behavior is to a client diagnosed with cluster B personality disorder as avoidant, dependent behavior is to a client diagnosed with a:
Explanation
Personality disorders are enduring patterns of inner experience and behavior that deviate markedly from cultural expectations. They are grouped into clusters based on descriptive similarities. Cluster C includes disorders characterized by anxious and fearful behavior, such as avoidant, dependent, and obsessive-compulsive personality disorders. These individuals often exhibit excessive need for reassurance, hypersensitivity to criticism, and social inhibition. Their behaviors are driven by fear of rejection or abandonment, contrasting sharply with the impulsivity and disregard for others seen in Cluster B.
Rationale for correct answer
C. Cluster C includes avoidant and dependent personality disorders, both of which are marked by fear-driven behaviors. Avoidant individuals are socially inhibited due to feelings of inadequacy, while dependent individuals display submissiveness and cling to others for reassurance. These traits reflect anxious and insecure interpersonal styles.
Rationale for incorrect answers
A. Cluster A includes eccentric and odd behaviors, such as those seen in paranoid, schizoid, and schizotypal personality disorders. These clients are socially detached or suspicious, not characterized by dependency or avoidance.
B. Cluster B includes dramatic and impulsive behaviors, such as those seen in antisocial, borderline, histrionic, and narcissistic personality disorders. These clients often lack guilt and act irresponsibly, not avoidantly.
D. There is no Cluster D in the DSM-5 classification of personality disorders. The recognized clusters are A, B, and C only.
Take Home Points
- Cluster C personality disorders are characterized by anxious, fearful behaviors including avoidance and dependency.
- Cluster B disorders involve dramatic, emotional, or erratic traits such as impulsivity and lack of remorse.
- Cluster A disorders are marked by social detachment, odd beliefs, and suspiciousness.
- DSM-5 classifies personality disorders into three clusters: A (odd), B (dramatic), and C (anxious); there is no Cluster D.
A client diagnosed with a personality disorder tells the nurse, “When I was a waiter, I used to spit in the dinners of annoying customers.” This statement would be associated with which personality disorder?
Explanation
Antisocial personality disorder is defined by a pervasive pattern of disregard for the rights of others, often accompanied by deceitfulness, impulsivity, and lack of remorse. Individuals may engage in behaviors that violate social norms and ethical boundaries, including aggression, manipulation, and criminal acts. They often show guiltless attitudes toward harmful actions and may rationalize or boast about them. These behaviors typically begin in adolescence and persist into adulthood, with poor impulse control and a lack of empathy being central features.
Rationale for correct answer
D. The statement reflects remorseless and aggressive behavior toward others, consistent with antisocial traits. Spitting in food as retaliation shows a violation of social norms and lack of empathy, which are core features of this disorder.
Rationale for incorrect answers
A. Paranoid personality disorder involves suspicion, mistrust, and hypersensitivity to perceived threats, but not overtly aggressive or retaliatory acts. These individuals are more likely to isolate or defend themselves than to act out.
B. Schizoid personality disorder is marked by detachment from social relationships and limited emotional expression. These individuals are unlikely to engage in retaliatory or confrontational behaviors due to their preference for isolation.
C. Passive-aggressive personality traits involve indirect resistance and procrastination rather than overt hostility. Spitting in food is a direct and aggressive act, not consistent with passive-aggressive behavior.
Take Home Points
- Antisocial personality disorder involves aggressive, deceitful, and guiltless behaviors that violate social norms.
- Paranoid traits center on mistrust and suspicion, not overt retaliation.
- Schizoid individuals are emotionally detached and avoid social conflict.
- Passive-aggressive behavior is indirect and resistant, not openly hostile or confrontational.
A male client diagnosed with a personality disorder boasts to the nurse that he has to fight off female attention and is the highest paid in his company. These statements are reflective of which personality disorder?
Explanation
Narcissistic personality disorder is characterized by a pervasive pattern of grandiosity, need for admiration, and lack of empathy. Individuals often exaggerate achievements, expect special treatment, and display arrogance. Their self-esteem is fragile and dependent on external validation. They may present with boastful or self-aggrandizing statements and become defensive or angry when challenged. These behaviors are not rooted in psychosis but in a distorted self-concept and interpersonal exploitation.
Rationale for correct answer
D. The client’s statements reflect grandiosity and self-importance, hallmark traits of narcissistic personality disorder. Boasting about desirability and income exemplifies the exaggerated self-image and need for admiration typical of this disorder.
Rationale for incorrect answers
A. Obsessive-compulsive personality disorder involves perfectionism, rigidity, and preoccupation with control—not boastfulness or inflated self-worth. These individuals are more focused on order than on admiration.
B. Passive-aggressive traits involve indirect resistance, procrastination, and covert hostility. They do not include overt bragging or grandiose self-presentation.
C. Schizotypal personality disorder is marked by eccentric behavior, odd beliefs, and social anxiety. Clients may be socially awkward or paranoid, not boastful or self-promoting.
Take Home Points
- Narcissistic personality disorder involves grandiosity, need for admiration, and lack of empathy.
- Clients often exaggerate achievements and expect special treatment.
- Obsessive-compulsive personality disorder focuses on control and perfectionism, not self-aggrandizement.
- Schizotypal traits include eccentricity and social discomfort, not boastful or arrogant behavior.
A client diagnosed with borderline personality disorder is admitted to a psychiatric unit with recent self-inflicted cuts to both arms. Which of the following would explain this behavior? Select all that apply
Explanation
Self-mutilation in borderline personality disorder is often a maladaptive coping mechanism used to regulate overwhelming emotions, express internal pain, or respond to perceived abandonment. It is not always suicidal in intent but may reflect a desperate attempt to feel something when emotional numbness sets in. Affective instability, intense fear of rejection, and impulsivity are core features. These behaviors often occur in response to interpersonal stressors and are linked to dysregulated emotional states rather than psychosis or manipulation.
Rationale for correct answers
C. The belief that pain is preferable to emotional numbness reflects the dissociative and affective dysregulation seen in borderline personality disorder. Self-harm may serve to re-establish a sense of reality or emotional presence.
D. Feelings of abandonment are a central trigger for self-injurious behavior. Separation from significant others can provoke intense fear and emotional pain, leading to impulsive acts like cutting to relieve distress or signal need.
Rationale for incorrect answers
A. Labeling self-mutilation as manipulative oversimplifies the behavior and ignores its emotional and psychological roots. While attention-seeking may occur, the primary driver is emotional dysregulation, not calculated manipulation.
B. A safety plan is a preventive strategy, not a trigger. Self-harm typically occurs when emotional regulation fails, not because a plan is in place. The presence of a safety plan does not provoke self-injury.
E. Voices commanding self-harm suggest psychotic features, which are not typical of borderline personality disorder. While transient dissociation may occur, persistent auditory hallucinations are more consistent with psychotic disorders.
Take Home Points
- Self-mutilation in borderline personality disorder is often a response to emotional numbness or abandonment, not manipulation.
- These behaviors are impulsive and rooted in affective instability, not psychosis.
- Safety plans are protective tools, not triggers for self-harm.
- Differentiating borderline traits from psychotic symptoms is essential for accurate diagnosis and intervention.
When assessing a client diagnosed with passive-aggressive personality disorder, the nurse might identify which characteristic behavior?
Explanation
Passive-aggressive personality disorder is marked by a pervasive pattern of indirect resistance to demands or expectations from others. Individuals often express anger or resentment through procrastination, stubbornness, intentional inefficiency, or subtle sabotage. They may appear cooperative on the surface but act out covert hostility when they feel wronged or controlled. Subtle retribution is a hallmark trait, reflecting internalized resentment and avoidance of direct confrontation. These behaviors often emerge in interpersonal or occupational settings where authority or expectations are perceived as oppressive.
Rationale for correct answer
D. The client’s tendency to seek subtle revenge reflects the core dynamic of passive-aggressive behavior. Rather than confronting others directly, these individuals express hostility through indirect actions like delaying tasks or undermining efforts, especially when they feel slighted or controlled.
Rationale for incorrect answers
A. Splitting is more characteristic of borderline personality disorder, where individuals pit staff against each other to manage emotional instability. Passive-aggressive clients are more covert and do not typically engage in overt manipulation of staff dynamics.
B. Reckless disregard for safety is a defining feature of antisocial personality disorder, not passive-aggressive traits. These individuals do not typically engage in impulsive or dangerous behaviors.
C. Distrust of others is central to paranoid personality disorder. Passive-aggressive individuals may feel resentful but do not exhibit pervasive suspicion or unjustified doubts about others’ intentions.
Take Home Points
- Passive-aggressive personality disorder involves indirect expression of anger and resistance to authority.
- Subtle sabotage and procrastination are common ways these individuals express resentment.
- Splitting and impulsive risk-taking are not typical of passive-aggressive traits.
- Differentiating passive-aggressive behavior from paranoid and borderline traits is essential for accurate assessment.
A client diagnosed with antisocial personality disorder states, “My kids are so busy at home and school they don’t miss me or even know I’m gone.” Which nursing diagnosis applies to this client?
Explanation
Antisocial personality disorder is marked by a pervasive pattern of disregard for the rights of others, deceitfulness, impulsivity, and lack of remorse. Clients often rationalize or minimize the impact of their behavior, showing little concern for consequences. They may use defense mechanisms such as denial to avoid accountability or emotional discomfort. These individuals frequently externalize blame and show superficial charm while masking emotional detachment or guilt. Insight into their behavior is often limited, and they may distort reality to maintain a self-serving narrative.
Rationale for correct answer
C. The client’s statement reflects denial of emotional consequences and interpersonal impact. By claiming his children don’t miss him, he minimizes the significance of his absence and avoids acknowledging potential guilt or relational harm, which aligns with ineffective denial.
Rationale for incorrect answers
A. Injury risk is not the primary concern here. Antisocial clients are more likely to endanger others than themselves, and there is no evidence in the statement suggesting physical vulnerability or harm.
B. Self-directed violence is uncommon in antisocial personality disorder. These individuals typically externalize aggression rather than internalize distress, and the statement lacks indicators of suicidal ideation or self-harm.
D. Powerlessness implies a perceived lack of control over life circumstances. The client’s tone suggests detachment and rationalization, not helplessness or loss of control, making this diagnosis inappropriate.
Take Home Points
- Antisocial personality disorder often involves denial and minimization of interpersonal harm.
- Clients may rationalize or externalize blame to avoid emotional accountability.
- Risk for self-directed violence is more typical in mood or borderline disorders, not antisocial traits.
- Powerlessness reflects helplessness, which is inconsistent with the manipulative and self-assured tone of antisocial presentations.
A nurse is working in the orientation phase of a therapeutic relationship with a client who has borderline personality disorder. What will be most difficult for the client at this stage of the relationship?
Explanation
Borderline personality disorder is characterized by pervasive patterns of instability in interpersonal relationships, self-image, and affect, with marked impulsivity. Individuals with this disorder experience intense emotional fluctuations and fear of abandonment, which often interfere with establishing trust and consistent boundaries in relationships. During the orientation phase of a therapeutic relationship, the nurse and client begin developing trust and identifying goals. For clients with borderline personality disorder, this phase is particularly challenging due to their unstable perception of others and difficulty maintaining consistent emotions.
Rationale for correct answer
D. Individuals with borderline personality disorder struggle with boundaries and trust, which are essential in setting mutual goals during the orientation phase. Their emotional instability and fear of rejection make collaboration difficult. The client may oscillate between idealizing and devaluing the nurse, hindering the process of goal-setting and mutual agreement. Establishing realistic and shared goals requires a stable perception of self and others, which this client lacks in early therapeutic interactions.
Rationale for incorrect answers
A. Anxiety is common in many clients during early therapy sessions, but it is not the most significant challenge for those with borderline personality disorder. The central issue lies in relationship instability, not generalized anxiety.
B. Difficulty terminating sessions on time usually emerges during the working or termination phases, when dependency and fear of separation intensify. In the orientation phase, the primary struggle is establishing a stable connection.
C. Acceptance of a psychiatric diagnosis is typically a cognitive process that develops as insight increases. While denial may occur, it is not the main obstacle in forming an initial therapeutic alliance.
Take Home Points
- Clients with borderline personality disorder have unstable relationships and intense emotional responses, making early goal-setting difficult.
- Trust and boundaries are central challenges in the orientation phase of therapy.
- Emotional instability and fear of abandonment hinder consistent therapeutic engagement.
- Nurses must maintain firm structure and boundaries to promote safety and therapeutic progress.
Practice Exercise 4
Which interventions should a nurse plan for a client with avoidant personality disorder? Select all that apply.
Explanation
Avoidant personality disorder (AvPD) is characterized by social inhibition, feelings of inadequacy, and hypersensitivity to negative evaluation. Clients often desire relationships but avoid them due to fear of rejection. It is essential for the nurse to build trust, encourage self-esteem, and use cognitive-behavioral techniques to modify maladaptive thoughts.
Rationale for correct answers
A. Providing support and reassurance helps build a therapeutic alliance and reduces anxiety during interactions. This intervention fosters trust and emotional safety, which are essential for gradual engagement and participation in therapy.
B. Exploring positive self-aspects assists the client in identifying personal strengths, counteracting persistent feelings of inferiority. This approach enhances self-worth and encourages healthier interpersonal relationships.
C. Reframing enables clients to reinterpret negative experiences or beliefs from a more balanced perspective, thereby reducing distortion in self-perception and improving coping responses.
D. De-catastrophizing helps the client challenge and modify irrational fears of failure or rejection by breaking down catastrophic thinking patterns into realistic evaluations. This technique is core to cognitive restructuring.
Rationale for incorrect answer(s)
E. Identifying negative responses from others may reinforce avoidance and hypersensitivity to criticism, worsening the client’s social withdrawal. Instead, therapy should focus on reframing perceptions rather than validating perceived rejections.
Take Home Points
- Avoidant personality disorder involves chronic fear of rejection and feelings of inadequacy despite a desire for connection.
- Cognitive-behavioral strategies like reframing and de-catastrophizing help correct distorted beliefs and improve self-concept.
- Supportive therapeutic relationships and encouragement of positive self-aspects build confidence and promote social engagement.
- Interventions should reduce avoidance behaviors, not reinforce hypersensitivity to others’ judgments.
A public health nurse visits a client’s home and discovers a multitude of cluttered possessions taking up 75% of the living space, obscuring entrance into the home and access to all rooms except the bathroom. The chairs and table are covered with various objects. The nurse interprets the client’s behavior as:
Explanation
Hoarding disorder is a condition marked by persistent difficulty discarding possessions regardless of their actual value, leading to accumulation that congests living areas and significantly compromises functionality and safety. It often stems from anxiety, distorted beliefs about possessions, or obsessive fears of losing important items. This behavior can occur independently or as a feature of obsessive-compulsive disorder (OCD) or obsessive-compulsive personality disorder (OCPD).
Rationale for correct answer
D. Hoarding is associated with excessive acquisition and retention of items, resulting in unsafe, cluttered environments. It reflects underlying obsessive fears and maladaptive attachment to possessions. Clients experience marked distress at the thought of discarding items, often rationalizing their need to keep them. The behavior interferes with daily functioning, hygiene, and safety, necessitating interventions that address cognitive distortions and promote gradual decluttering.
Rationale for incorrect answers
A. Passive-aggressive personality disorder involves indirect resistance to demands and procrastination, not accumulation of objects. The main feature is hostility expressed covertly, not environmental disorganization.
B. Borderline personality disorder is characterized by instability in mood, relationships, and self-image. Though impulsive behaviors may occur, excessive hoarding is not a diagnostic hallmark of this condition.
C. Histrionic personality disorder centers on attention-seeking and exaggerated emotional expression. Individuals crave admiration and dramatize behavior; cluttered accumulation of objects does not serve that purpose.
Take Home Points
- Hoarding disorder is defined by the excessive collection and inability to discard items, leading to unsafe living conditions.
- It can occur as a distinct disorder or within the spectrum of OCD or OCPD.
- The behavior often provides anxiety relief and a sense of control, but ultimately impairs functioning.
- Treatment includes cognitive-behavioral therapy, harm reduction, and gradual organization strategies rather than forced cleanup.
The nurse is assisting a client with a dependent personality disorder to work on the goal of developing healthy relationships with family members. Which nursing intervention should the nurse initiate to help the client develop healthy relationships?
Explanation
Dependent personality disorder (DPD) is characterized by an excessive and pervasive need to be cared for, leading to submissive behavior and fear of separation. Individuals with DPD rely heavily on others for decision-making, approval, and support, often avoiding responsibility or independence. Their self-esteem is closely tied to others’ opinions, and they experience significant anxiety when alone or required to act autonomously.
Rationale for correct answer
C. Practicing disagreement helps the client build autonomy and assertiveness, key deficits in dependent personality disorder. This technique encourages independent thinking, decision-making, and self-confidence—essential for developing balanced, healthy relationships that are not based on submissiveness or approval-seeking.
Rationale for incorrect answers
A. Structuring each part of the day spent alone reinforces dependence, as it limits opportunities for the client to experience autonomy and internal control over choices and activities.
B. Establishing a nurse-client contract promotes cooperation, but it focuses on treatment compliance rather than interpersonal growth or assertiveness, making it insufficient for fostering independent relationships.
D. Talking about self during outside activities may enhance socialization, but without assertiveness and autonomy, it does not specifically address dependency patterns or the tendency to seek validation.
Take Home Points
- Dependent personality disorder involves excessive reliance on others for emotional and decision-making support.
- The therapeutic goal is to promote independence, self-confidence, and assertive communication.
- Role-playing and practicing disagreement help clients learn to express opinions without fear of disapproval.
- Healthy relationships require mutual respect and equality, not control or overreliance on others for self-worth.
Which of the following underlying emotions is commonly seen in an avoidant personality disorder?
Explanation
Avoidant personality disorder (AvPD) is a chronic pattern of social inhibition, feelings of inadequacy, and hypersensitivity to criticism. Individuals desire social relationships but avoid them due to fear of rejection, embarrassment, or being judged negatively. This fear drives avoidance of interpersonal contact, maintaining a cycle of isolation and low self-esteem.
Rationale for correct answer
B. The predominant emotional state in avoidant personality disorder is fear—specifically, fear of rejection, humiliation, and disapproval. This intense apprehension causes individuals to withdraw from social interaction despite craving connection, leading to impaired functioning in personal and occupational areas.
Rationale for incorrect answers
A. Depression may occur secondarily due to chronic isolation and low self-worth but is not the central emotion driving the disorder’s behaviors. It is an outcome, not the root cause.
C. Guilt is not a core feature of avoidant personality disorder. Guilt typically arises in conditions involving moral conflict or perceived wrongdoing, which are not characteristic of AvPD.
D. Insecurity is a cognitive manifestation, not the primary emotion. It reflects self-doubt and low confidence, but the driving emotional force behind avoidance remains fear of rejection and criticism.
Take Home Points
- Fear of rejection and criticism is the hallmark emotional driver of avoidant personality disorder.
- Individuals with AvPD avoid relationships despite desiring closeness due to anticipatory anxiety.
- Secondary symptoms like depression and insecurity develop from prolonged isolation and fear.
- Treatment focuses on reducing avoidance through cognitive restructuring, gradual exposure, and supportive therapy to rebuild confidence.
Which of the following diagnostic criteria define avoidant personality disorder? Select all that apply.
Explanation
Avoidant personality disorder (AvPD) is defined by a pervasive pattern of social inhibition, feelings of inadequacy, and hypersensitivity to criticism that begins by early adulthood and occurs across various contexts. These individuals strongly desire close relationships but avoid social interaction due to fears of rejection or ridicule. Their behavior is driven by fear and low self-esteem rather than disinterest in others.
Rationale for correct answers
A. Avoiding intimate relationships due to fear of shame or ridicule is a defining feature of AvPD. Such individuals often withdraw from relationships to protect themselves from perceived humiliation, even though they desire closeness.
C. Being unwilling to engage with others unless certain of being liked reflects the avoidance and hypersensitivity to rejection central to this disorder. This cautious approach leads to limited social networks and loneliness.
E. Viewing oneself as socially inept and inferior is a core self-perception in AvPD. This negative self-image reinforces avoidance behaviors and perpetuates isolation and low self-confidence.
Rationale for incorrect answers
B. Difficulty making decisions without reassurance characterizes dependent personality disorder, where the individual relies excessively on others for guidance and support, not avoidance from fear of criticism.
D. Perfectionism that interferes with task completion is typical of obsessive-compulsive personality disorder, where excessive orderliness and control dominate functioning, not avoidance due to fear.
Take Home Points
- Avoidant personality disorder features social inhibition, hypersensitivity to rejection, and feelings of inadequacy.
- Fear of criticism and ridicule leads to avoidance of interpersonal relationships despite the desire for affection.
- Self-perception of inferiority and social ineptness perpetuates isolation and low self-esteem.
- It is distinct from dependent and obsessive-compulsive personality disorders, which are driven by dependency and perfectionism respectively.
A nurse is caring for a client with an obsessive-compulsive personality disorder that involves rituals. What should the nurse conclude about the ritual?
Explanation
Obsessive-compulsive personality disorder (OCPD) is characterized by perfectionism, control, and preoccupation with orderliness, often at the expense of flexibility and efficiency. When accompanied by ritualistic behaviors, these rituals serve to reduce internal tension and anxiety caused by intrusive thoughts. Although the behaviors may appear irrational to others, they are experienced by the client as necessary for maintaining emotional control and preventing perceived harm.
Rationale for correct answer
D. The ritual seems illogical but necessary to the person because it temporarily relieves anxiety created by obsessive thoughts. The act becomes a coping mechanism, reinforcing the cycle of compulsion by providing short-term relief despite its irrational nature. This repetitive behavior is not voluntary but driven by anxiety reduction and an overwhelming sense of duty or correctness.
Rationale for incorrect answers
A. The ritual does not merely have a useless purpose; to the client, it serves a critical psychological function of anxiety relief. Labeling it as useless fails to recognize the underlying compulsive drive.
B. The ritual is not performed after long urging but rather automatically when intrusive thoughts arise. Clients feel compelled to act immediately to decrease distress, not after external prompting.
C. The ritual does not appear to be performed willingly; it is ego-dystonic, meaning the individual recognizes it as unreasonable but feels powerless to stop, leading to significant internal conflict.
Take Home Points
- Obsessive-compulsive personality disorder involves rigid perfectionism and preoccupation with control, sometimes accompanied by compulsive rituals.
- Rituals provide short-term anxiety relief but reinforce long-term compulsive cycles.
- Clients perform rituals out of compulsion, not choice, recognizing their irrationality but feeling unable to resist.
- Treatment focuses on cognitive-behavioral therapy and exposure with response prevention to reduce compulsive behaviors and anxiety.
Practice Exercise 5
Which intervention describes an important component in the treatment of clients diagnosed with personality disorders?
Explanation
Personality disorders are enduring patterns of inner experience and behavior that deviate markedly from cultural expectations, affecting cognition, affectivity, interpersonal functioning, and impulse control. These disorders are pervasive, inflexible, and typically emerge in adolescence or early adulthood. Individuals often experience significant distress or impairment in functioning, particularly in interpersonal relationships. Treatment focuses on developing adaptive coping mechanisms, improving emotional regulation, and fostering healthy interpersonal interactions through consistent therapeutic approaches.
Rationale for correct answer
B. Self-awareness is crucial because clients with personality disorders often provoke strong emotional reactions in healthcare providers due to manipulative, dependent, or hostile behaviors. Nurses must maintain professional boundaries, recognize countertransference, and use therapeutic communication to build trust and consistency. This awareness allows the nurse to remain objective, avoid enabling maladaptive behaviors, and reinforce adaptive responses, which is essential for effective treatment and stabilization.
Rationale for incorrect answers
A. Psychotropic medications may help manage specific symptoms such as anxiety, depression, or impulsivity, but they do not treat the underlying personality structure. They are adjuncts, not primary interventions, and cannot replace psychotherapeutic modalities.
C. Group therapy can be beneficial for social learning and feedback but may not always be the preferred or safest approach, particularly for clients with severe paranoia or borderline traits, who may misinterpret others’ behaviors. Individual therapy remains fundamental for developing insight and trust before group participation.
D. Addressing comorbidities such as substance use, anxiety, or mood disorders is essential. Ignoring these conditions can hinder progress, as they often exacerbate maladaptive patterns and interfere with therapeutic engagement and recovery.
Take Home Points
- Self-awareness and boundary setting by nurses are critical for maintaining a therapeutic relationship with clients who have personality disorders.
- Medications are supportive but not curative for personality disorders; psychotherapy remains the cornerstone of treatment.
- Group therapy may be helpful but should be individualized based on the client’s diagnosis, insight level, and ability to tolerate interpersonal stress.
- Comorbid psychiatric or substance-related disorders must be addressed concurrently to achieve optimal treatment outcomes.
A college student is brought to the mental health clinic by the parents. The diagnosis is borderline personality disorder. Which factors in the client’s history support this diagnosis? Select all that apply.
Explanation
Borderline personality disorder is a pervasive pattern of instability in interpersonal relationships, self-image, and affects, with marked impulsivity beginning in early adulthood. It is characterized by intense mood swings, chronic feelings of emptiness, fear of abandonment, and recurrent self-destructive behaviors. Clients often alternate between idealization and devaluation of others, experience difficulty regulating emotions, and engage in maladaptive coping mechanisms such as self-injury to relieve internal tension.
Rationale for correct answers
A. Impulsiveness is a defining feature of borderline personality disorder, manifesting in areas such as spending, substance abuse, unsafe sex, or binge eating. It reflects poor emotional regulation and impaired judgment under stress.
B. Lability of mood is common due to emotional instability; clients experience intense episodic dysphoria, irritability, or anxiety that can last a few hours to days. This instability contributes to chaotic relationships and poor self-concept.
E. Self-destructive behavior, including self-mutilation or suicidal gestures, is a hallmark of borderline personality disorder. It often arises from an inability to manage intense emotions or from a fear of real or perceived abandonment.
Rationale for incorrect answers
C. Ritualistic behavior is associated with obsessive-compulsive disorder, not borderline personality disorder. It involves repetitive actions aimed at reducing anxiety, which differs from the emotional dysregulation seen in BPD.
D. Retardation of psychomotor activity is characteristic of major depressive disorder or certain medical conditions. Borderline personality disorder typically involves heightened emotional reactivity and impulsive activity rather than slowed movements.
Take Home Points
- Borderline personality disorder presents with impulsivity, mood instability, and self-harming behaviors as core features.
- Emotional lability and intense relationships stem from fear of abandonment and poor emotional control.
- Ritualistic or slowed motor behaviors are not features of BPD but of other psychiatric conditions.
- Treatment focuses on emotional regulation, distress tolerance, and establishing consistent therapeutic boundaries.
A nurse understands that milieu therapy can be helpful for a client with antisocial personality disorder because it:
Explanation
Antisocial personality disorder is characterized by a pervasive pattern of disregard for, and violation of, the rights of others. Individuals often demonstrate manipulative behaviors, lack empathy, and fail to conform to social norms or laws. They may display deceitfulness, impulsivity, irritability, and irresponsibility. Treatment focuses on helping clients recognize the impact of their behaviors on others and promoting prosocial interactions through structured, consistent environments like milieu therapy.
Rationale for correct answer
D. Milieu therapy provides a controlled, therapeutic social environment that simulates a community, allowing clients to practice appropriate interpersonal behaviors. Through peer feedback and social reinforcement, individuals with antisocial traits can learn to interact respectfully and develop a sense of responsibility toward others, supporting gradual internalization of social norms and empathy.
Rationale for incorrect answers
A. Limits are indeed necessary but represent only one component of milieu therapy. Limit-setting alone does not encompass the broader therapeutic purpose of promoting adaptive social functioning within a community context.
B. Reality orientation and one-on-one interaction are more relevant for clients with psychotic or cognitive disorders. Individuals with antisocial personality disorder benefit more from group-based interventions emphasizing social learning and accountability.
C. A highly structured environment can help maintain order and safety, but excessive structure without social engagement may reinforce authority resistance and manipulation rather than encourage internal behavioral change.
Take Home Points
- Milieu therapy uses a therapeutic social environment to promote adaptive interpersonal behaviors.
- Clients with antisocial personality disorder benefit from community-based feedback and consistent consequences.
- Limit-setting is essential but should occur within a supportive, socially interactive context.
- Overly rigid or isolated interventions are less effective than socially focused, reality-based therapeutic environments.
A hospitalized client who was diagnosed with a borderline personality disorder consistently breaks the unit’s rules. How will confronting the client about this behavior help the client?
Explanation
Borderline personality disorder (BPD) is a complex psychiatric condition marked by emotional instability, impulsive behavior, and disturbed interpersonal relationships. Individuals with BPD often display difficulty regulating emotions and maintaining consistent self-identity. They frequently engage in behaviors that test boundaries or defy limits, often due to intense fear of abandonment or rejection. Confronting maladaptive behaviors in a therapeutic manner helps promote self-awareness and insight into the consequences of their actions, essential for developing healthier coping mechanisms and emotional regulation.
Rationale for correct answer
D. Confronting the client promotes self-awareness by helping them recognize the relationship between their behaviors and the resulting consequences. Clients with borderline personality disorder often lack insight into their maladaptive patterns and emotional triggers. Direct, calm confrontation by the nurse encourages reflection, increases accountability, and supports the development of adaptive coping skills. This approach facilitates growth in emotional regulation and improves interpersonal effectiveness, key treatment goals in BPD.
Rationale for incorrect answers
A. Anger management is a therapeutic outcome but not the immediate purpose of confrontation. Confrontation addresses awareness of behaviors rather than directly controlling anger; behavioral therapy focuses on anger control later through skill development.
B. Anxiety reduction is not the goal of confrontation. Addressing rule-breaking behavior can initially increase anxiety because it challenges the client's defenses. Long-term anxiety reduction occurs through establishing trust and consistent boundaries, not confrontation itself.
C. Goal setting is part of broader therapeutic planning, but confrontation focuses on behavioral accountability. While realistic goals are essential in therapy, the direct purpose of confrontation is to increase self-insight, not to formulate or set goals.
Take Home Points
- Borderline personality disorder involves emotional dysregulation, impulsivity, and unstable relationships.
- Therapeutic confrontation fosters self-awareness and accountability for behavior.
- Consistent, calm limit-setting promotes emotional stability and trust in treatment settings.
- Differentiation from antisocial personality disorder lies in emotional volatility rather than lack of remorse.
Which statement about persons with personality disorders is accurate?
Explanation
Personality disorders are enduring patterns of maladaptive behavior, emotional responses, and interpersonal functioning that deviate markedly from societal expectations. These behaviors are deeply ingrained, ego-syntonic, and inflexible, often leading to significant impairment in relationships, work, and self-identity. Unlike individuals with mood or psychotic disorders, those with personality disorders usually lack insight into their behavior, frequently perceiving that their distress arises from others rather than from themselves. Treatment focuses on helping them develop self-awareness and adaptive interpersonal skills.
Rationale for correct answer
B. Individuals with personality disorders often view their behaviors and thoughts as normal, making them ego-syntonic. Because of this, they rarely perceive their own behavior as problematic, instead attributing difficulties to others’ actions or attitudes. This lack of insight complicates therapy and hinders motivation for change. Interpersonal conflicts are common, as clients externalize responsibility for their struggles, reinforcing maladaptive relationship patterns and emotional instability.
Rationale for incorrect answers
A. The risk of suicide is not low in personality disorders. In fact, individuals—particularly those with borderline personality disorder—have a significantly elevated suicide risk due to impulsivity, emotional dysregulation, and chronic feelings of emptiness.
C. Personality disorders are not purely psychological; research shows biological, genetic, and neurochemical factors contribute alongside environmental influences. Dysfunctions in brain regions involved in impulse control and emotion regulation have been documented, indicating complex biopsychosocial origins.
D. Symptoms can be disabling, and treatment is often challenging. Clients may exhibit manipulative, resistant, or demanding behaviors, making therapeutic relationships complex. Their maladaptive patterns significantly impair social and occupational functioning, requiring structured and consistent care.
Take Home Points
- Personality disorders are ego-syntonic, meaning individuals often do not recognize their behavior as problematic.
- Suicide risk can be high, especially in borderline personality disorder.
- Biological, psychological, and environmental factors all contribute to personality disorders.
- Management requires structured, consistent therapeutic approaches with clear boundaries to ensure effective care.
Practice Exericise 6
After being treated in the ED for self-inflicted lacerations to the wrists and arms, a client with a diagnosis of borderline personality disorder is admitted to the psychiatric unit. Which nursing intervention takes priority?
Explanation
Borderline personality disorder (BPD) is a complex mental condition characterized by unstable mood, self-image, and interpersonal relationships. Individuals often experience intense emotional swings, impulsivity, and recurrent self-harming behaviors. The disorder involves impaired emotional regulation and an unstable sense of identity, leading to patterns of fear of abandonment, self-injury, or suicidal ideation. The priority in managing these clients is ensuring safety, as self-harm and impulsive acts pose immediate life-threatening risks.
Rationale for correct answer
B. The most critical nursing action is to ensure safety by frequent observation. Clients with borderline personality disorder are at high risk for self-harm or suicide, particularly following emotional distress or interpersonal conflict. Close observation allows early intervention if the client attempts to injure themselves again, thereby preventing life-threatening behavior. Safety monitoring fulfills the physiological need for survival, which takes precedence over emotional or psychosocial care interventions.
Rationale for incorrect answers
A. Administering tranquilizing drugs is not the first-line action unless the client displays acute agitation or psychosis. Medications may help control mood instability but do not prevent self-injury or suicidal behavior, which is the immediate concern.
C. Encouraging the client to verbalize hostile feelings is therapeutic but not the priority intervention during the acute phase after self-harm. Emotional expression can be explored after the client is physically safe and stabilized.
D. Exploring alternative ways of handling frustration is a rehabilitative approach used in later stages of therapy. Initially, the focus must be on observation and safety to prevent recurrence of self-inflicted injuries.
Take Home Points
- The primary nursing priority in borderline personality disorder after self-harm is ensuring client safety through close and continuous observation.
- Emotional exploration and coping strategy development are secondary to stabilization.
- Medication management may support mood control but is not a substitute for safety monitoring.
- Interventions progress from meeting physiological needs to addressing psychological and interpersonal aspects as stability improves.
A 15-year-old client living in a residential facility has a nursing diagnosis of ineffective coping related to abuse as evidenced by defiant responses to adult rules. Which of the following interventions would address this nursing diagnosis appropriately? Select all that apply.
Explanation
Ineffective coping is a maladaptive response pattern in which an individual fails to use appropriate strategies to manage stressors or emotional distress. In adolescents with a history of abuse, this may manifest as defiance, manipulation, or aggression toward authority figures. Such behaviors reflect underlying feelings of anger, mistrust, and low self-esteem. Effective management involves providing consistent boundaries, emotional expression, and therapeutic communication to help the adolescent develop healthier coping mechanisms and emotional regulation.
Rationale for correct answers
A. Setting limits on manipulative behavior establishes boundaries that promote a sense of security and predictability. Adolescents with ineffective coping often test authority as a way to regain control; firm and consistent limits help them learn responsibility and trust within safe parameters.
B. Refusing to engage in controversial or argumentative encounters prevents power struggles and reinforces emotional control. This approach models calm communication and avoids reinforcing negative attention-seeking behaviors while maintaining a therapeutic alliance.
D. Encouraging the discussion of angry feelings facilitates emotional expression and helps the client verbalize instead of acting out anger. It allows exploration of past trauma, reduces internal tension, and builds adaptive coping skills through supportive communication.
Rationale for incorrect answers
C. Administering tranquilizing medications is not appropriate unless the client exhibits acute agitation or poses a danger to self or others. Medication use does not directly address underlying coping deficits or behavioral issues.
E. Removing dangerous objects is indicated only when there is violence or suicidal intent. Since this client’s problem involves defiance rather than self-harm, environmental restriction is unnecessary and could increase resistance or mistrust.
Take Home Points
- Ineffective coping in abused adolescents is best managed through consistent limits, supportive communication, and emotional validation.
- Avoiding power struggles fosters trust and models appropriate emotional regulation.
- Encourage the expression of anger and frustration safely to prevent acting-out behaviors.
- Medication or environmental control is secondary and used only when safety risks are present.
A client diagnosed with a borderline personality disorder is given a nursing diagnosis of disturbed personal identity related to unmet dependency needs as evidenced by the inability to be alone. Which nursing intervention would be appropriate?
Explanation
Disturbed personal identity, or identity disturbance, occurs when an individual has a fragmented or unstable sense of self, often resulting from unmet dependency and attachment issues. In borderline personality disorder, this manifests as chronic feelings of emptiness, identity confusion, and reliance on others to define one’s worth. Clients often experience intense fear of abandonment and difficulty maintaining a consistent self-concept. Nursing interventions focus on helping clients establish internal values and beliefs that promote self-awareness and identity stability.
Rationale for correct answer
D. Helping the client identify values and beliefs promotes self-concept development and personal identity formation. This intervention encourages introspection and assists the client in distinguishing their own feelings, opinions, and preferences from those of others, reducing dependency behaviors. It supports long-term psychological growth and fosters autonomy essential for recovery.
Rationale for incorrect answers
A. Asking directly about suicidal thoughts is appropriate when assessing safety, but it does not address issues of identity or dependency. While suicide risk must always be monitored, this intervention is unrelated to the specific nursing diagnosis of disturbed personal identity.
B. Maintaining a low level of stimuli is a strategy for anxiety or agitation, not identity disturbance. This action may help calm the client temporarily but does not promote self-awareness or personal growth.
C. Frequent orientation to reality is indicated for psychosis or confusion, not borderline personality disorder. Clients with BPD are typically reality-oriented but struggle with emotional instability and self-perception, making this intervention irrelevant.
Take Home Points
- Disturbed personal identity in borderline personality disorder arises from unmet dependency and a fragile sense of self.
- Supporting value clarification helps clients define their own beliefs and develop stable identity boundaries.
- Identity-focused interventions promote autonomy and reduce reliance on external validation.
- Orientation or environmental control techniques are not effective for identity disturbances without perceptual impairment.
A client diagnosed with an antisocial personality disorder is given a nursing diagnosis of self-esteem disturbance related to extreme poverty as evidenced by continual boasting and grandiosity. Which nursing intervention would be appropriate?
Explanation
Self-esteem disturbance in individuals with antisocial personality disorder (ASPD) is characterized by a fragile and inflated self-image that compensates for deep feelings of inadequacy. Clients may demonstrate arrogance, manipulation, and a lack of empathy as defenses against internal insecurity. These behaviors often arise from chronic deprivation, neglect, or failure to meet basic psychological needs, leading to distorted self-perception and poor emotional insight. Effective nursing care focuses on developing self-awareness, accountability, and empathy to foster genuine self-esteem rather than superficial grandiosity.
Rationale for correct answer
B. Encouraging self-awareness through critical examination of feelings and behaviors helps the client gain insight into maladaptive coping patterns and the underlying feelings of inferiority masked by boasting or manipulation. This process promotes internal reflection, responsibility, and authentic self-esteem development. It shifts focus from external validation to personal accountability, which is central to managing antisocial traits.
Rationale for incorrect answers
A. Offering to remain with the client during initial interactions is useful for those with anxiety or social withdrawal, not for antisocial personality disorder. These clients often display excessive confidence and do not require supportive presence for social engagement.
C. Recognizing “splitting” staff is crucial in borderline personality disorder, not antisocial. ASPD clients manipulate others for personal gain but do not typically engage in splitting behavior characterized by idealization and devaluation of staff members.
D. Allowing the client to take responsibility for self-care is appropriate for promoting independence, but in this case, it does not address the self-esteem disturbance or the psychological mechanisms sustaining the client’s grandiosity. The focus should be on self-reflection and emotional understanding first.
Take Home Points
- Antisocial personality disorder involves inflated self-image masking deep insecurity and lack of empathy.
- Encouraging self-awareness and emotional insight is key to improving genuine self-esteem.
- “Splitting” behaviors are typical of borderline, not antisocial, personality disorders.
- Long-term therapeutic goals focus on accountability, empathy development, and recognition of consequences.
A nursing student is learning about narcissistic personality disorder. Which student statement indicates that learning has occurred?
Explanation
Narcissistic personality disorder (NPD) is characterized by a pervasive pattern of grandiosity, need for admiration, and lack of empathy. Individuals with this disorder have an exaggerated sense of self-importance, overestimate their abilities, and expect special treatment. Their fragile self-esteem makes them extremely sensitive to criticism, leading to feelings of shame or humiliation when not admired. The core disturbance lies in a distorted self-concept and an inability to view others as separate individuals with equal worth.
Rationale for correct answer
D. A grandiose sense of self-importance is a defining feature of narcissistic personality disorder. Clients often overvalue their talents and accomplishments, believing they are unique or superior. This exaggerated self-view serves as a psychological defense against underlying feelings of inadequacy and low self-worth.
Rationale for incorrect answers
A. Peculiarities of ideation are typical of schizotypal personality disorder, which involves eccentric thinking, magical beliefs, and perceptual distortions, not the grandiosity or admiration-seeking seen in narcissism.
B. Constant need for approval is more consistent with dependent personality disorder, where clients rely excessively on others for reassurance and decision-making, unlike narcissistic individuals who seek admiration rather than approval.
C. Impulsivity and self-destructive tendencies are associated with borderline personality disorder, characterized by emotional instability and fear of abandonment, not with narcissistic traits of superiority and control.
Take Home Points
- Narcissistic personality disorder involves pervasive grandiosity, admiration-seeking, and lack of empathy.
- The inflated self-image masks deep insecurity and low self-esteem.
- Unlike dependent or borderline personalities, narcissistic individuals seek admiration, not reassurance or closeness.
- Insight-oriented therapy and empathy training may support emotional regulation and self-awareness.
A client with a diagnosis of borderline personality disorder has negative feelings toward the other clients on the unit and considers them all to be “bad.” Which defense was the client using when this statement was made?
Explanation
Splitting is a primitive defense mechanism commonly seen in individuals with borderline personality disorder (BPD). It involves an inability to integrate positive and negative aspects of oneself or others into a cohesive whole. As a result, people are viewed as either entirely good or entirely bad, with no middle ground. This black-and-white thinking often leads to unstable relationships, emotional lability, and frequent shifts in idealization and devaluation. Splitting serves as a way to manage intense anxiety and fear of abandonment by simplifying complex emotional experiences.
Rationale for correct answer
A. The client’s statement that others are all “bad” demonstrates polarization, which defines splitting. This mechanism allows the individual to cope with conflicting feelings by categorizing people or experiences as all good or all bad. In BPD, this arises from difficulty tolerating ambivalence, resulting in unstable interpersonal relationships and intense emotional reactions.
Rationale for incorrect answers
B. Ambivalence refers to simultaneous opposing emotions toward the same person or situation. It reflects emotional conflict but not the rigid separation of good and bad qualities characteristic of splitting.
C. Passive aggression involves indirect expression of hostility, such as procrastination or resistance, rather than overtly labeling others as bad. It is a behavioral response, not a cognitive distortion like splitting.
D. Reaction formation occurs when an individual behaves in a way opposite to their true feelings, such as expressing affection toward someone they actually dislike. This differs from splitting, where individuals categorize people into extremes without emotional reversal.
Take Home Points
- Splitting is a hallmark defense mechanism in borderline personality disorder.
- It reflects an inability to integrate both positive and negative perceptions of self or others.
- This defense contributes to unstable relationships and intense emotional shifts.
- Treatment focuses on helping clients recognize and integrate conflicting feelings for healthier emotional regulation.
A client is diagnosed with a borderline personality disorder. What is a realistic initial intervention for this client?
Explanation
Borderline personality disorder (BPD) is characterized by pervasive instability in relationships, self-image, and affect, often accompanied by impulsive behaviors and fear of abandonment. Clients with BPD typically struggle with emotional regulation and boundaries, frequently oscillating between idealization and devaluation of others. Early in treatment, the therapeutic focus must be on establishing structure, predictability, and safety within the nurse-client relationship to reduce anxiety and maintain behavioral control.
Rationale for correct answer
A. Establishing clear boundaries is the most realistic and essential initial intervention for clients with BPD. Consistent limits help prevent manipulation, splitting, and dependence, while providing a secure framework that promotes trust and emotional containment. Structure allows the nurse to maintain professionalism and avoid enmeshment, supporting the client’s gradual development of internal controls and stability.
Rationale for incorrect answers
B. Exploring job possibilities is premature, as vocational planning requires emotional stability and consistent functioning. Early treatment should focus on safety, boundaries, and basic emotional regulation before addressing long-term goals.
C. Discussing victimization may evoke overwhelming emotions and intensify instability early in therapy. This should occur later, once a trusting and structured therapeutic relationship is established and the client has learned basic coping skills.
D. Spending excessive time with the nurse fosters dependency and reinforces boundary issues, which are central to BPD. Frequent, brief, and predictable contacts are more therapeutic and prevent overattachment or manipulation.
Take Home Points
- Initial nursing care for BPD emphasizes structure, consistency, and firm boundaries.
- Boundaries promote safety, reduce manipulation, and help stabilize relationships.
- Emotional exploration should begin only after trust and control are established.
- Excessive nurse availability increases dependency and interferes with therapeutic progress.
A client with a personality disorder tells a nurse, “I want to tell you something, but you must promise to keep it a secret.” Which response could lead to splitting among the staff?
Explanation
Splitting is a common defense mechanism used by individuals with personality disorders, especially borderline personality disorder. It involves perceiving others as either entirely good or entirely bad, without the ability to integrate both positive and negative qualities. This defense often leads to manipulation, emotional conflict, and division among staff members as the client attempts to gain control or special treatment by pitting team members against each other. Effective management requires consistent communication and a unified team approach to prevent staff polarization.
Rationale for correct answer
B. Saying that comments will be kept confidential because the nurse is the client’s “advocate” fosters splitting. This response gives the impression of a special relationship and secrecy, isolating the nurse from the team and reinforcing the client’s manipulative pattern. It undermines team consistency and increases mistrust between staff members, contributing to interpersonal conflict on the unit.
Rationale for incorrect answers
A. Stating that the nurse is part of a team that shares important information reinforces open communication and teamwork. It sets clear limits and prevents the client from using secrecy to divide staff, thus avoiding splitting.
C. Refusing to promise confidentiality upholds honesty and professional boundaries. It ensures transparency and maintains consistency among caregivers, protecting against manipulation and staff conflict.
D. Explaining that information will be handled in the client’s best interests and shared appropriately with the team promotes trust while maintaining ethical standards. It prevents the client from perceiving any one staff member as exclusively loyal or protective.
Take Home Points
- Splitting is a defense mechanism in which individuals view others as all good or all bad.
- Avoiding secretive or exclusive communication prevents division among staff.
- Consistent teamwork and clear communication reduce manipulation and maintain therapeutic structure.
- Nurses must uphold professional boundaries while remaining supportive and transparent.
The clients on a mental health unit go on a supervised day trip to a baseball game. When returning to the bus, a client with a narcissistic personality disorder insists on leaving the group to get an autograph from a player. What is the most appropriate response by the nurse?
Explanation
Narcissistic personality disorder (NPD) is marked by an exaggerated sense of self-importance, an excessive need for admiration, and a lack of empathy for others. Individuals with NPD often believe that normal rules or expectations do not apply to them and may act entitled or superior. They seek attention and recognition to maintain their inflated self-image. Nursing management focuses on setting firm, consistent limits while maintaining a calm, professional, and non-confrontational approach to prevent escalation or humiliation, which these clients cannot tolerate.
Rationale for correct answer
C. Informing the client in a matter-of-fact tone that everyone must stay with the group establishes clear boundaries without confrontation. This approach reinforces rules consistently while minimizing attention to the client’s attention-seeking behavior. It models respectful authority, maintains group safety, and reduces the likelihood of power struggles, which could reinforce the client’s need for control or superiority.
Rationale for incorrect answers
A. Physically restraining the client without cause is inappropriate unless there is immediate danger. This action could provoke anger, increase resistance, and damage trust, escalating the situation unnecessarily.
B. Using a loud or authoritative tone draws attention to the client, reinforcing their need for admiration and control. It can also embarrass or provoke the client, leading to defiance or aggression.
D. Telling the client the player will not give autographs introduces unnecessary information and may lead to argument or denial. It also fails to address the behavioral issue—following group expectations and respecting boundaries.
Take Home Points
- Clients with narcissistic personality disorder require firm, consistent, and calm limit setting.
- Avoid emotional or confrontational responses that feed attention-seeking behaviors.
- Matter-of-fact communication maintains boundaries while preserving dignity and safety.
- The goal is to promote compliance with rules without reinforcing entitlement or superiority.
Which nursing intervention is most important for a client who has the diagnosis of antisocial personality disorder?
Explanation
Antisocial personality disorder (ASPD) is characterized by a pervasive pattern of disregard for and violation of the rights of others, impulsivity, and lack of remorse. Individuals often manipulate, deceive, or exploit others for personal gain. They frequently ignore rules, show little empathy, and fail to learn from negative experiences. Nursing management focuses on establishing structure and consistent boundaries, as these clients respect authority only when clear consequences are enforced.
Rationale for correct answer
C. Providing clear boundaries and consequences is the most important intervention for clients with antisocial personality disorder. This approach ensures safety and prevents manipulation by maintaining structure and predictability. Firm limit-setting helps the client recognize that behaviors have consequences and that privileges are earned through acceptable conduct. Consistency among staff is essential to prevent manipulation and maintain therapeutic control.
Rationale for incorrect answers
A. Teaching and role-modeling assertiveness are appropriate for clients who lack confidence or have difficulty expressing needs, such as those with dependent or avoidant disorders, not for manipulative antisocial clients.
B. Using a gentle and reassuring approach can be misinterpreted as weakness, encouraging manipulation or exploitation. Clients with ASPD often test limits and may take advantage of overly permissive staff.
D. A democratic and overly empathetic style is not effective with antisocial clients. These individuals require firm, direct communication and consistent enforcement of rules rather than negotiation or shared decision-making, which they may manipulate.
Take Home Points
- Antisocial personality disorder requires firm boundaries and consistent consequences to reduce manipulation.
- A structured environment promotes safety and accountability.
- Overly gentle or permissive approaches increase the risk of exploitation.
- Consistency among staff prevents manipulation and reinforces behavioral control.
A patient becomes frustrated and angry when trying to get his MP3 player and headset to function properly and angrily throws it across the room, nearly hitting a peer with it. Which intervention(s) would be the most therapeutic? Select all that apply.
Explanation
Therapeutic communication is a structured, patient-centered approach used to support emotional regulation, insight, and behavioral change. It emphasizes empathy, active listening, and nonjudgmental engagement to promote self-awareness, reduce distress, and foster coping skills. In psychiatric and behavioral settings, therapeutic communication is essential for de-escalating agitation, preventing aggression, and reinforcing adaptive responses to frustration. It avoids punitive or authoritarian tones and instead encourages reflection, problem-solving, and emotional validation.
Rationale for correct answers
C. Helping the patient operate the device demonstrates empathy and problem-solving, reducing frustration by addressing the root cause. It models supportive behavior and reinforces trust in the caregiver-patient relationship.
D. Exploring the patient’s feelings promotes emotional insight, allowing the patient to verbalize internal states rather than act out. This intervention fosters self-regulation and helps identify triggers for future prevention.
G. Encouraging recognition of tension and seeking help builds coping capacity and emotional literacy. It teaches proactive strategies for managing distress and reinforces autonomy in self-regulation.
Rationale for incorrect answers
A. Seclusion is a restrictive intervention reserved for imminent danger. Using it prematurely undermines therapeutic rapport and may escalate feelings of isolation or punishment.
B. Threatening loss of privileges is a punitive approach that increases defensiveness and shame. It lacks supportiveness and does not teach alternative coping mechanisms.
E. Pointing out consequences without emotional processing is confrontational. It may provoke resistance and fails to address underlying emotional dysregulation or skill deficits.
F. Avoiding frustration entirely delays skill development. Exposure with support is necessary for building resilience and adaptive functioning in real-world settings.
Take Home Points
- Therapeutic communication prioritizes empathy, emotional insight, and skill-building over punishment or avoidance.
- Seclusion and threats should only be used when safety is compromised, not for frustration or emotional dysregulation.
- Emotional processing and tension recognition are foundational for teaching self-regulation and preventing future outbursts.
- Avoidance of frustration delays coping development; supported exposure fosters resilience and behavioral growth.
Comprehensive Questions
A client with borderline personality has a history of unsuccessful suicidal behavior. After creating a safe environment for this client, the nurse should implement which intervention?
Explanation
Borderline personality disorder is marked by pervasive instability in mood, self-image, and interpersonal relationships, often accompanied by impulsivity and recurrent suicidal behavior. Clients may experience intense emotional dysregulation, fear of abandonment, and transient psychotic symptoms under stress. Verbalization of internal experiences helps externalize distress, reduce impulsive actions, and allows for therapeutic intervention. Safety is prioritized through structured communication and emotional containment.
Rationale for correct answer
D. Encouraging the client to verbalize disturbing thoughts promotes emotional regulation and early intervention. It allows the nurse to assess for escalating risk, validate the client’s experience, and implement safety measures. This approach supports therapeutic alliance and reduces impulsive self-harm.
Rationale for incorrect answers
A. Focusing on resentment may intensify negative affect and reinforce maladaptive rumination. This can escalate emotional dysregulation and does not provide immediate containment or safety for suicidal ideation.
B. Addressing the source of pain is a long-term therapeutic goal, not an acute intervention. In early stabilization, this may overwhelm the client and increase vulnerability to self-harm without adequate coping strategies.
C. Asking the client to document problematic conditions may be cognitively demanding during emotional crises. It lacks immediacy in addressing suicidal ideation and may not provide the emotional support needed in acute phases.
Take Home Points
- Clients with borderline personality disorder benefit from structured, supportive environments that prioritize emotional safety.
- Encouraging verbalization of distress helps prevent impulsive self-harm and builds therapeutic trust.
- Acute interventions should focus on containment, not deep emotional processing or cognitive tasks.
- Long-term therapy may address core issues like abandonment fears, trauma, and interpersonal dysfunction, but not during crisis stabilization.
A nurse should anticipate that a client diagnosed with antisocial personality disorder may use the primary ego defense mechanism of:
Explanation
Antisocial personality disorder is characterized by a pervasive pattern of disregard for the rights of others, impulsivity, and lack of remorse. Individuals often exhibit manipulative behavior, superficial charm, and poor empathy. They frequently externalize blame and show limited insight into their actions. Their defense mechanisms are typically primitive and serve to deflect responsibility or justify harmful behavior. These individuals may engage in criminal acts, violate social norms, and rationalize their behavior to avoid guilt or accountability.
Rationale for correct answer
B. Individuals with antisocial traits often use projection to attribute their own unacceptable impulses or behaviors to others. This allows them to avoid accountability and maintain a distorted self-image. In clinical settings, they may accuse others of being manipulative or dishonest, reflecting their own tendencies. Projection is a primitive defense mechanism that aligns with the psychological immaturity seen in antisocial personality disorder.
Rationale for incorrect answers
A. Compensation involves making up for perceived deficiencies in one area by excelling in another. It is more common in individuals with intact self-awareness and goal-directed behavior, not in antisocial traits where denial and blame-shifting dominate.
C. Sublimation is a mature defense mechanism where unacceptable impulses are transformed into socially acceptable actions. Antisocial individuals rarely channel aggression or deceit into constructive outlets, making sublimation inconsistent with their behavioral profile.
D. Rationalization is a higher-level defense used to justify actions with logical explanations. While antisocial individuals may attempt to explain their behavior, their primary defense is more primitive and externalizing, such as projection, rather than internal justification.
Take Home Points
- Antisocial personality disorder involves primitive defenses like projection, externalizing blame, and lack of remorse.
- Projection is common in personality disorders with poor insight and impaired interpersonal functioning.
- Sublimation and compensation are mature defenses not typically used by individuals with antisocial traits.
- Differentiating antisocial personality disorder from narcissistic or borderline traits requires attention to defense mechanisms and interpersonal patterns.
A nurse is caring for a client diagnosed with paranoid personality disorder in an acute care facility. Which intervention should the nurse use to control the client’s suspiciousness?
Explanation
Paranoid personality disorder is marked by pervasive distrust and suspiciousness of others, often interpreting benign actions as malicious. These individuals are hypervigilant, reluctant to confide, and may react with hostility to perceived threats. They often misinterpret intentions, hold grudges, and resist authority. Therapeutic approaches must prioritize consistency, transparency, and non-confrontational communication. Pharmacologic interventions are rarely primary unless comorbid conditions exist. Building trust is slow and requires careful attention to boundaries and predictability.
Rationale for correct answer
A. Individuals with paranoid traits benefit from clear and consistent communication that avoids ambiguity or deception. This reduces perceived threats and helps establish a predictable therapeutic environment. Avoiding hidden meanings or sarcasm is essential to prevent misinterpretation and escalation of suspiciousness. Structured, honest interactions foster a sense of safety and reduce defensive behaviors.
Rationale for incorrect answers
B. Pharmacologic therapy is not the primary intervention for paranoid personality disorder unless there is a comorbid psychiatric condition such as depression or psychosis. Medication does not directly address the core interpersonal mistrust and rigidity.
C. Social interactions may increase anxiety and suspicion in individuals with paranoid traits. They often perceive others as threatening or manipulative, making group settings counterproductive unless carefully structured and monitored.
D. Basic needs should be met consistently, but this alone does not address the core issue of suspiciousness. While routine care builds some trust, it lacks the targeted communication strategies needed to reduce paranoid ideation.
Take Home Points
- Paranoid personality disorder requires structured, transparent, and non-deceptive communication to reduce mistrust.
- Pharmacologic therapy is not first-line unless comorbid conditions are present.
- Group interactions may worsen paranoia and should be approached cautiously.
- Consistency in care builds trust but must be paired with clear messaging to address suspiciousness.
A nurse is caring for a client with borderline personality disorder. Which intervention should the nurse perform?
Explanation
Borderline personality disorder is characterized by pervasive instability in relationships, self-image, and affect, often accompanied by impulsivity and intense fear of abandonment. Clients may exhibit splitting, emotional lability, and manipulative behaviors to test boundaries or avoid perceived rejection. They often struggle with identity disturbance and chronic feelings of emptiness. Therapeutic approaches require firm, consistent limits, validation of emotions, and avoidance of reinforcing maladaptive behaviors. Safety concerns may arise due to self-harm or suicidal gestures, but behavioral interventions are prioritized over physical restraints.
Rationale for correct answer
A. Clients with borderline traits often engage in manipulative behaviors such as splitting staff or testing boundaries. Setting firm, consistent limits helps reduce chaos and reinforces therapeutic structure. Limit-setting is essential to maintain safety, reduce emotional dysregulation, and prevent staff burnout. It also models healthy interpersonal boundaries and supports emotional containment.
Rationale for incorrect answers
B. Allowing the client to set limits undermines therapeutic structure and may reinforce maladaptive control-seeking behaviors. These clients often lack internal regulation and benefit from external consistency.
C. Restraints are not a routine intervention for borderline personality disorder. They are reserved for acute safety threats and may escalate distress or reinforce feelings of abandonment and punishment.
D. Acting-out behavior should never be encouraged. It reflects poor impulse control and emotional dysregulation. Reinforcing such behavior increases risk of harm and undermines therapeutic goals.
Take Home Points
- Borderline personality disorder requires firm, consistent limit-setting to manage manipulative and impulsive behaviors.
- Emotional dysregulation and fear of abandonment are core features that drive interpersonal instability.
- Physical restraints are reserved for acute safety concerns and should be used cautiously.
- Encouraging acting-out behaviors worsens emotional instability and undermines therapeutic progress.
When working with a client with a narcissistic personality disorder, the nurse would use which of the following approaches?
Explanation
Narcissistic personality disorder is defined by a pervasive pattern of grandiosity, need for admiration, and lack of empathy. Individuals often exaggerate achievements, expect special treatment, and react poorly to criticism. They may appear arrogant or entitled, but underlying this is a fragile self-esteem. Therapeutic approaches must avoid feeding into grandiosity or challenging it directly. Instead, neutral, structured, and non-emotional interactions help maintain boundaries and reduce power struggles. Emotional engagement or excessive praise can reinforce maladaptive patterns.
Rationale for correct answer
C. A matter-of-fact approach maintains therapeutic neutrality and avoids reinforcing the client’s need for admiration or emotional validation. This style helps preserve boundaries and reduces the likelihood of narcissistic injury or manipulation. It allows the nurse to deliver care without engaging in power dynamics or emotional entanglement, which are common triggers for individuals with narcissistic traits.
Rationale for incorrect answers
A. Cheerful interactions may be misinterpreted as admiration or approval, reinforcing the client’s grandiosity. It can also provoke entitlement or unrealistic expectations of special treatment.
B. Friendly approaches risk blurring professional boundaries and may invite manipulation or idealization. Narcissistic clients often exploit warmth to seek validation or control interactions.
D. Supportive tones may inadvertently reinforce dependency or entitlement. While empathy is important, overt emotional support can escalate demands and reduce therapeutic effectiveness in narcissistic dynamics.
Take Home Points
- Narcissistic personality disorder requires neutral, structured, and emotionally detached interactions to maintain boundaries.
- Matter-of-fact communication reduces reinforcement of grandiosity and prevents emotional entanglement.
- Excessive warmth or praise may escalate entitlement or manipulation in narcissistic clients.
- Differentiating narcissistic traits from histrionic or borderline features involves assessing emotional regulation and interpersonal expectations.
The nurse would assess for which of the following characteristics in a client with narcissistic personality disorder?
Explanation
Narcissistic personality disorder is defined by a pervasive pattern of grandiosity, need for admiration, and lack of empathy. Individuals often display arrogance, exaggerate achievements, and expect special treatment. Beneath this exterior lies a fragile self-esteem, making them vulnerable to criticism. They often exploit others for personal gain and show little regard for others’ feelings. Their interpersonal relationships are superficial, and they may become enraged or dismissive when their inflated self-image is challenged. Unlike borderline or paranoid traits, their core defense is entitlement and superiority, not fear or mistrust.
Rationale for correct answer
A. The hallmark of narcissistic personality disorder is entitlement, where the individual believes they deserve special privileges and admiration without reciprocation. This belief fuels interpersonal conflict, as they expect others to comply with their expectations and may react with rage or disdain when not treated as superior. Entitlement is central to their interpersonal dysfunction and is a key diagnostic feature.
Rationale for incorrect answers
B. Fear of abandonment is characteristic of borderline personality disorder, not narcissistic traits. While narcissistic individuals may react strongly to rejection, it stems from wounded pride rather than abandonment anxiety.
C. Hypersensitivity to rejection is more aligned with avoidant personality disorder. Narcissistic individuals may react to criticism with anger or devaluation, but not due to social inhibition or fear of disapproval.
D. Suspiciousness is a core feature of paranoid personality disorder. Narcissistic individuals may be defensive, but they do not typically exhibit pervasive mistrust or interpret others’ actions as malevolent.
Take Home Points
- Entitlement is a defining feature of narcissistic personality disorder, driving interpersonal conflict and expectations of special treatment.
- Narcissistic individuals may react to criticism with rage or devaluation, but not due to abandonment fears.
- Differentiating narcissistic traits from borderline or avoidant personality disorders requires assessing the motivation behind interpersonal reactions.
- Suspiciousness and mistrust are more consistent with paranoid personality disorder, not narcissistic pathology.
The most important short-term goal for a client who tries to manipulate others would be to:
Explanation
Manipulative behavior in clinical settings often stems from underlying personality traits such as borderline, antisocial, or narcissistic features. These individuals may use indirect tactics to control others, avoid responsibility, or gain attention. Manipulation is frequently driven by unmet emotional needs, poor insight, and impaired interpersonal boundaries. Addressing this behavior requires structured interventions that promote accountability, emotional regulation, and self-awareness. Short-term goals focus on recognition of behavior patterns before deeper therapeutic work can begin.
Rationale for correct answer
A. The most effective short-term goal is for the client to acknowledge their manipulative behavior. This reflects emerging insight and is foundational for therapeutic progress. Without recognition, interventions lack traction. Acknowledgment allows for the development of healthier coping strategies and opens the door to behavioral change and emotional regulation.
Rationale for incorrect answers
B. Feelings expression is important but premature if the client lacks insight into their manipulative patterns. Verbalizing emotions without accountability may reinforce maladaptive behaviors or deflect responsibility.
C. Arguments may be a symptom of manipulation, but stopping them is a behavioral outcome, not a cognitive goal. Without recognizing the underlying behavior, cessation of arguments may be superficial or temporary.
D. Relationships require long-term emotional work and behavioral consistency. Sustaining them is a distant goal that depends on foundational changes, including acknowledgment of manipulative tendencies and development of empathy.
Take Home Points
- Manipulative behavior often reflects poor insight and impaired interpersonal boundaries, requiring structured therapeutic goals.
- Acknowledging manipulative actions is the first step toward behavioral change and emotional regulation.
- Expressing feelings is valuable but must follow recognition of maladaptive patterns to be therapeutic.
- Long-term relational goals depend on short-term cognitive shifts and consistent behavioral accountability.
A client diagnosed with a personality disorder states, “You are the very best nurse on the unit and not at all like that mean nurse who never lets us stay up later than 9 p.m.” This statement would be associated with which personality disorder?
Explanation
Borderline personality disorder is marked by intense instability in relationships, affect, and self-image. Clients often experience rapid shifts in emotional states, impulsivity, and chronic fears of abandonment. A hallmark feature is splitting, a primitive defense mechanism where individuals categorize others as entirely good or entirely bad. This black-and-white thinking leads to idealization and devaluation, often directed toward caregivers. Their interpersonal relationships are chaotic, and they may alternate between clinging and rejecting behaviors based on perceived threats to attachment.
Rationale for correct answer
A. The statement reflects splitting, where the client idealizes one nurse while devaluing another. This is a classic interpersonal pattern in borderline personality disorder, driven by unstable affect and fear of abandonment. The exaggerated praise and simultaneous criticism are attempts to manage internal emotional turmoil and maintain perceived security in relationships.
Rationale for incorrect answers
B. Schizoid personality disorder is characterized by detachment and limited emotional expression. Individuals with this disorder avoid close relationships and are unlikely to express strong opinions or emotional comparisons between caregivers.
C. Passive-aggressive traits involve indirect resistance and covert hostility, such as procrastination or intentional inefficiency. The client’s statement lacks the subtle defiance or undermining typical of passive-aggressive behavior.
D. Paranoid personality disorder involves pervasive distrust and suspicion. While these individuals may criticize others, their statements are typically rooted in fear of harm or betrayal, not emotional idealization or relational splitting.
Take Home Points
- Splitting is a hallmark defense mechanism in borderline personality disorder, leading to idealization and devaluation.
- Borderline clients often express intense emotional reactions and unstable interpersonal attachments.
- Schizoid personality disorder presents with emotional detachment and limited interpersonal engagement.
- Paranoid personality disorder involves mistrust and suspicion, not emotional instability or relational idealization.
Which of the following diagnostic criteria define borderline personality disorder? Select all that apply.
Explanation
Borderline personality disorder is a pervasive pattern of instability in interpersonal relationships, self-image, and affect, with marked impulsivity. Individuals often experience intense emotional swings, chronic feelings of emptiness, and engage in self-harming or suicidal behaviors. A core feature is frantic efforts to avoid abandonment, whether real or perceived. These clients may exhibit identity disturbance, impulsivity in areas like spending or sex, and unstable relationships marked by idealization and devaluation.
Rationale for correct answers
B. Frantic efforts to avoid abandonment are central to borderline personality disorder. These behaviors may include clinging, manipulation, or emotional outbursts when separation is perceived, even if imagined.
C. Recurrent suicidal gestures and self-mutilation are diagnostic criteria. These behaviors often serve as emotional regulation attempts or expressions of internal pain, and are not always linked to suicidal intent.
E. Chronic feelings of emptiness reflect the identity disturbance and emotional void common in borderline personality disorder. Clients may describe feeling hollow, disconnected, or lacking a stable sense of self.
Rationale for incorrect answers
A. Arrogant and haughty behaviors are characteristic of narcissistic personality disorder, not borderline. Borderline individuals may idealize or devalue others but do not typically present with grandiosity.
D. Preoccupation with fears of being left to care for oneself is more aligned with dependent personality disorder. While borderline clients fear abandonment, the focus is emotional loss rather than functional incapacity.
Take Home Points
- Borderline personality disorder includes fear of abandonment, emotional instability, and self-harming behaviors.
- Chronic emptiness and identity disturbance are key features that differentiate it from other personality disorders.
- Narcissistic traits involve grandiosity and entitlement, not emotional dysregulation or self-harm.
- Dependent personality disorder centers on fears of being unable to function alone, not emotional abandonment.
When assessing a client diagnosed with histrionic personality disorder, the nurse might identify which characteristic behavior?
Explanation
Histrionic personality disorder is marked by pervasive patterns of excessive emotionality and attention-seeking behavior. Individuals often display dramatic, flirtatious, and exaggerated expressions, with a strong need to be the center of attention. They may use physical appearance to draw attention, show rapidly shifting emotions, and be easily influenced by others. Relationships are often perceived as more intimate than they actually are. Unlike narcissistic or schizotypal traits, histrionic features are rooted in emotional expressiveness and social approval-seeking.
Rationale for correct answer
D. The hallmark of histrionic personality disorder is attention-seeking behavior, often expressed through flamboyant dress, exaggerated emotions, and theatrical speech. The client’s need for approval and admiration drives these behaviors.
Rationale for incorrect answers
A. The presence of magical thinking and odd beliefs is characteristic of schizotypal personality disorder, not histrionic. Schizotypal individuals often exhibit eccentric behavior and cognitive distortions, not emotional dramatization.
B. A grandiose sense of self-importance is typical of narcissistic personality disorder. These individuals seek admiration but lack the emotional expressiveness and dependency seen in histrionic traits.
C. Perfectionism and preoccupation with order are features of obsessive-compulsive personality disorder. These clients are rigid, controlling, and focused on rules, not on emotional display or attention-seeking.
Take Home Points
- Histrionic personality disorder is defined by excessive emotionality and attention-seeking, often through dramatic and seductive behavior.
- It must be differentiated from narcissistic personality disorder, which centers on grandiosity and lack of empathy.
- Schizotypal personality disorder involves cognitive distortions and eccentricity, not emotional expressiveness.
- Obsessive-compulsive personality disorder is marked by rigidity, perfectionism, and control, not flamboyance or approval-seeking.
A client diagnosed with borderline personality disorder superficially cut both wrists, is disruptive in group, and is “splitting” staff. Which nursing diagnosis would take priority?
Explanation
Borderline personality disorder is characterized by pervasive instability in interpersonal relationships, self-image, and affect, often accompanied by impulsivity. Clients may engage in self-harming behaviors, such as superficial cutting, as a maladaptive way to regulate intense emotions or to express distress. These acts are not always suicidal but may serve to relieve internal tension or elicit care. Splitting—viewing others as all good or all bad—is a defense mechanism reflecting fear of abandonment and difficulty with emotional regulation. Disruption in group settings and manipulation of staff are common behavioral manifestations.
Rationale for correct answer
A. The client’s superficial wrist cutting indicates a pattern of self-mutilation, which is a hallmark behavior in borderline personality disorder. This behavior is often used to express emotional pain or gain attention, and it poses an immediate safety risk, making it the priority diagnosis.
Rationale for incorrect answers
B. While coping deficits are present in borderline personality disorder, they are not the most urgent concern when active self-harm is evident. Safety takes precedence over emotional processing or therapeutic insight.
C. Although abandonment fears and splitting behaviors are common in borderline personality disorder, they are not life-threatening. These dynamics contribute to interpersonal instability but do not supersede the risk of physical harm.
D. The wrist cutting described is non-lethal and superficial, which does not meet the threshold for prioritizing suicide risk. There is no mention of suicidal ideation or a lethal plan, making self-mutilation the more immediate concern.
Take Home Points
- Borderline personality disorder often involves self-mutilation as a coping mechanism for emotional dysregulation.
- Splitting is a defense mechanism rooted in fear of abandonment and contributes to staff manipulation.
- Suicide risk must be differentiated from non-lethal self-harm behaviors in borderline clients.
- Priority nursing diagnoses focus on immediate safety threats before addressing coping or interpersonal issues.
Which client situation requires the nurse to prioritize the implementation of limit setting?
Explanation
Limit setting is a therapeutic intervention used to maintain boundaries, promote safety, and reinforce appropriate behavior in psychiatric and behavioral health settings. It is especially critical when a client’s actions threaten physical or emotional safety, violate ethical standards, or disrupt therapeutic relationships. Limit setting must be clear, consistent, and enforced without punitive tone. It is not merely about correcting behavior but about protecting staff and clients while maintaining therapeutic structure. Immediate implementation is required when behaviors are intrusive, aggressive, or sexually inappropriate.
Rationale for correct answer
A. Sexual advances toward staff represent a boundary violation and pose a risk to safety and therapeutic integrity. These behaviors must be addressed immediately with firm, clear limits to prevent escalation and protect staff from harassment.
Rationale for incorrect answers
B. The client’s comment about food rules reflects manipulation, not a safety threat. While it may undermine staff consistency, it does not require immediate limit setting unless it escalates into disruptive behavior.
C. Provoking a paranoid patient is inappropriate, but the priority is de-escalation and redirection rather than limit setting. The focus should be on preventing conflict and ensuring both clients are safe, not enforcing behavioral boundaries.
D. Refusing medication for secondary gain is a form of passive resistance. While it requires therapeutic intervention, it does not pose an immediate safety risk or boundary violation that demands prioritized limit setting.
Take Home Points
- Limit setting is prioritized when client behavior threatens safety, violates boundaries, or disrupts therapeutic relationships.
- Sexual advances toward staff require immediate intervention to protect ethical and professional standards.
- Manipulative or provocative behaviors may need redirection or therapeutic engagement but not urgent limit setting.
- Medication refusal for secondary gain should be addressed through motivational interviewing and care planning, not immediate behavioral limits.
A suicidal client is diagnosed with borderline personality disorder. Which short-term outcome is most beneficial for the client?
Explanation
Borderline personality disorder is marked by intense emotional instability, impulsivity, and self-harming behaviors often triggered by interpersonal stress or fear of abandonment. Clients may struggle to regulate emotions and resort to self-injury as a maladaptive coping mechanism. Suicidal ideation may coexist with non-lethal self-harm, making emotional expression and regulation critical therapeutic targets. The short-term goal in acute care is to reduce self-injury by promoting safe emotional outlets and building trust. Long-term goals may include interpersonal insight and behavioral change, but immediate focus is on safety and emotional regulation.
Rationale for correct answer
B. The most beneficial short-term outcome is the ability to express feelings without resorting to self-injury, which directly addresses the client’s suicidal risk and emotional dysregulation. This goal is realistic, measurable, and safety-focused for discharge planning.
Rationale for incorrect answers
A. While being free from self-injury is ideal, it is not a realistic short-term goal for a suicidal borderline client. The emphasis should be on reducing harm and building coping strategies, not complete abstinence.
C. Socializing with peers may support therapeutic engagement but does not directly address the client’s suicidal ideation or self-harming behavior. It is secondary to emotional safety and regulation.
D. Acknowledging interpersonal role requires insight and reflection, which are long-term therapeutic goals. In acute care, the priority is stabilizing emotional expression and preventing self-harm.
Take Home Points
- Borderline personality disorder involves emotional dysregulation and self-harm, often triggered by interpersonal stress.
- Short-term goals should focus on reducing self-injury through safe emotional expression.
- Long-term goals may include interpersonal insight and behavioral change but are not prioritized in crisis stabilization.
- Social engagement and insight are supportive but secondary to safety and emotional regulation in suicidal clients.
A client diagnosed with antisocial personality disorder is observed smoking in a non-smoking area. Which initial nursing intervention is appropriate?
Explanation
Antisocial personality disorder is characterized by a pervasive pattern of disregard for the rights of others, impulsivity, and violation of social norms. Clients often manipulate, deceive, or break rules without remorse. They may rationalize harmful behavior and resist authority. In inpatient settings, these individuals often test limits and challenge rules. Therapeutic management requires consistent enforcement of rules and immediate consequences to reduce manipulation and maintain unit structure. Limit setting must be direct, firm, and nonjudgmental to preserve safety and therapeutic boundaries.
Rationale for correct answer
A. Immediate confrontation of the behavior is essential to reinforce boundaries and uphold institutional rules. Antisocial clients respond best to clear, consistent consequences rather than indirect or delayed interventions.
Rationale for incorrect answers
B. Reporting to the primary nurse delays intervention and allows the behavior to go unaddressed in the moment. Timely, direct response is critical to prevent reinforcement of rule-breaking.
C. A general reminder to the group avoids accountability and fails to address the specific client’s behavior. Antisocial individuals often exploit vague or indirect interventions.
D. Teaching coping skills is important but not the priority in this context. The issue is not anxiety but deliberate rule violation, which requires behavioral correction before therapeutic engagement.
Take Home Points
- Antisocial personality disorder involves rule-breaking, impulsivity, and disregard for others, often requiring firm behavioral management.
- Immediate, direct confrontation is essential to maintain structure and prevent manipulation.
- Indirect or delayed interventions undermine therapeutic boundaries and reinforce antisocial behaviors.
- Teaching coping skills is secondary to enforcing rules and ensuring safety in clients with antisocial traits.
A client has the diagnosis of histrionic personality disorder. Which behavior should the nurse expect when assessing this client?
Explanation
Histrionic personality disorder is marked by excessive emotionality, attention-seeking, and dramatic behavior. Clients often display exaggerated expressions, are highly extroverted, and may use physical appearance or provocative behavior to gain attention. They are uncomfortable when not the center of attention and may rapidly shift emotions. Relationships are often perceived as more intimate than they are. Unlike narcissistic or antisocial traits, histrionic features are rooted in emotional expressiveness and social approval-seeking rather than manipulation or grandiosity.
Rationale for correct answer
C. The client’s extroverted and dramatic presentation aligns with the core features of histrionic personality disorder. These individuals thrive on attention and often exaggerate emotions to maintain social engagement and approval.
Rationale for incorrect answers
A. The egotistical and boastful traits are more consistent with narcissistic personality disorder, where self-importance and entitlement dominate, rather than emotional expressiveness.
B. Perfectionistic and rigid behaviors are hallmarks of obsessive-compulsive personality disorder. These clients are focused on control and order, not emotional display or attention-seeking.
D. Manipulative and aggressive traits are more typical of antisocial personality disorder, where rule-breaking and exploitation are central. Histrionic clients may be suggestible but not overtly aggressive.
Take Home Points
- Histrionic personality disorder involves exaggerated emotionality and a strong need to be the center of attention.
- It must be differentiated from narcissistic traits, which focus on grandiosity and entitlement.
- Obsessive-compulsive personality disorder centers on control and perfectionism, not emotional expressiveness.
- Antisocial personality disorder features manipulation and aggression, unlike the socially engaging nature of histrionic traits.
A client with borderline personality disorder receives the wrong meal tray for lunch and angrily states, “The next time I see the dietician, I am going to throw this tray at her!” What is the nurse’s most appropriate response?
Explanation
Borderline personality disorder is a complex psychiatric condition marked by pervasive instability in mood, self-image, and interpersonal relationships. Clients often exhibit intense emotional reactions, impulsivity, and fear of abandonment. They may use splitting, projection, and externalization to cope with distress. Therapeutic communication must be firm, empathetic, and nonjudgmental, with clear boundaries. Staff consistency and validation of feelings without reinforcing maladaptive behaviors are essential. Impulsivity, emotional dysregulation, and interpersonal conflict are hallmark features.
Rationale for correct answer
C. This response uses empathy and limit-setting, which are essential in managing borderline personality disorder. It validates the client’s frustration while clearly stating that aggressive behavior is unacceptable. This approach maintains therapeutic rapport and reinforces behavioral boundaries without escalating the situation.
Rationale for incorrect answers
A. The word calm may invalidate the client’s emotional experience and minimize their distress. Suggesting that trays get mixed up ignores the emotional intensity and risks escalating the situation by appearing dismissive.
B. The word inappropriate introduces judgment and punishment, which can trigger feelings of rejection and abandonment in borderline clients. Sending the client out of the dining room may reinforce maladaptive behaviors and damage therapeutic trust.
D. The word seclusion implies a punitive consequence and may escalate the client’s fear of abandonment or loss of control. This response lacks empathy and may provoke further acting out rather than de-escalating the situation.
Take Home Points
- Borderline personality disorder requires firm, empathetic communication that validates feelings while setting behavioral limits.
- Avoid punitive or judgmental language, which may escalate emotional dysregulation and reinforce maladaptive coping.
- Therapeutic responses should balance empathy with boundaries to maintain safety and trust.
- Differentiate borderline personality disorder from antisocial and histrionic disorders by focusing on emotional instability and fear of abandonment.
A nurse is caring for a client with antisocial personality disorder. What client characteristic should the nurse consider when formulating a plan of care?
Explanation
Antisocial personality disorder is a chronic psychiatric condition characterized by a pervasive pattern of disregard for and violation of the rights of others. Clients often exhibit deceitfulness, impulsivity, irritability, and lack of remorse. They may manipulate others for personal gain and show poor compliance with social norms. Impulsivity, lack of empathy, and irresponsibility are core features. These individuals often fail to plan ahead and struggle with delayed gratification, making structured behavioral interventions and firm boundaries essential in care planning.
Rationale for correct answer
C. The client’s inability to delay gratification reflects the impulsivity and poor behavioral control typical of antisocial personality disorder. This trait contributes to risk-taking, noncompliance, and difficulty adhering to long-term goals, which must be considered when designing care plans.
Rationale for incorrect answers
A. Extreme anxiety is not a hallmark of antisocial personality disorder. These clients typically show low levels of anxiety and may appear indifferent or unconcerned about consequences.
B. Punishment rarely leads to rapid learning in antisocial clients due to their low sensitivity to negative consequences and lack of remorse. Behavioral change requires consistent reinforcement and structured consequences.
D. A strong sense of responsibility toward others is absent in antisocial personality disorder. These individuals often exploit others and lack empathy, making them unreliable in interpersonal commitments.
Take Home Points
- Antisocial personality disorder is marked by impulsivity, lack of empathy, and disregard for social norms.
- Clients often struggle with delayed gratification and may require structured, consequence-based interventions.
- Unlike anxiety disorders, antisocial traits include emotional detachment and low remorse.
- Differentiate from borderline personality disorder by noting the absence of emotional instability and fear of abandonment.
The nursing staff is discussing the best way to develop a relationship with a new client who has antisocial personality disorder. What characteristic of clients with antisocial personality should the nurses consider when planning care?
Explanation
Antisocial personality disorder is a pervasive psychiatric condition marked by disregard for societal norms and the rights of others. Clients often display manipulative behaviors, superficial charm, and a profound lack of remorse. They may exploit others for personal gain and show minimal concern for the emotional or physical consequences of their actions. Deceitfulness, impulsivity, and lack of empathy are central traits. These individuals often have intact communication skills but use them manipulatively, making trust-building and boundary-setting critical in care planning.
Rationale for correct answer
C. The defining feature of antisocial personality disorder is a profound lack of empathy, which underlies manipulative and exploitative behaviors. This absence of emotional concern for others must be considered when establishing therapeutic boundaries and ensuring safety.
Rationale for incorrect answers
A. Ritualistic behaviors are more characteristic of obsessive-compulsive personality disorder, not antisocial traits. Antisocial clients are typically impulsive and unconcerned with routine or order.
B. While they may appear independent, this trait is not diagnostically significant. Their independence is often superficial and used to avoid accountability or manipulate others.
D. Communication skills are usually intact in antisocial clients. They may be articulate and socially adept, using these abilities to deceive or manipulate rather than due to any deficit.
Take Home Points
- Antisocial personality disorder is defined by lack of empathy, impulsivity, and disregard for others’ rights.
- Clients often have intact communication skills used manipulatively, not due to deficits.
- Ritualistic behaviors suggest obsessive-compulsive traits, not antisocial pathology.
- Effective care requires firm boundaries, consistent consequences, and awareness of manipulative dynamics.
A client with a diagnosis of antisocial personality disorder is being discharged from the hospital. The client asks the nurse, “Can I have your phone number so that I can call you for a date?” What is the nurse’s best response?
Explanation
Antisocial personality disorder is marked by a pervasive pattern of disregard for others’ rights, lack of empathy, and manipulative or exploitative behavior. These individuals often violate social norms, show impulsivity, and may engage in deceit or aggression. They typically lack remorse and may attempt to charm or manipulate authority figures for personal gain. Therapeutic boundaries are essential in managing interactions with such clients to prevent exploitation and maintain professional integrity.
Rationale for correct answer
C. Professional boundaries must be maintained with clients diagnosed with antisocial personality disorder due to their manipulative tendencies. This response clearly defines the therapeutic relationship and prevents personal entanglement. It avoids emotional engagement and reinforces the nurse’s role, protecting both parties from inappropriate dynamics.
Rationale for incorrect answers
A. The word permitted implies that dating clients is a rule violation rather than a professional boundary issue. This response lacks the therapeutic clarity needed to reinforce the nurse-client relationship and may invite further negotiation.
B. The term ethics is vague and may provoke debate or challenge from a client with antisocial traits. It does not firmly establish the therapeutic boundary and may be interpreted as a personal moral stance rather than a professional standard.
D. The word glad introduces emotional engagement, which is inappropriate in this context. It may reinforce the client’s manipulative behavior and blur professional boundaries, making the nurse appear personally invested.
Take Home Points
- Antisocial personality disorder requires firm, clear boundaries due to manipulative and exploitative behaviors.
- Therapeutic relationships must remain professional and emotionally neutral to prevent boundary violations.
- Responses to inappropriate client advances should reinforce the nurse’s role and avoid emotional language.
- Differentiate antisocial personality disorder from borderline personality disorder, which involves emotional instability and fear of abandonment rather than calculated manipulation.
Josie, a 27-year-old patient, complains that most of the staff do not like her or care what happens to her, but you are special and she can tell that you are a caring person. She talks with you about being unsure of what she wants to do with her life and her “mixed-up feelings” about relationships. When you tell her that you will be on vacation next week, she becomes very angry. Two hours later, she is found using a curling iron to burn her underarms and explains that it “makes the numbness stop.” Given this presentation, which personality disorder would you suspect?
Explanation
Borderline personality disorder is characterized by pervasive instability in interpersonal relationships, self-image, and affect, along with marked impulsivity. Individuals often experience intense fear of abandonment, rapidly shifting emotions, and chronic feelings of emptiness. They may idealize caregivers or providers, then quickly devalue them when they perceive rejection. Self-injurious behaviors, such as cutting or burning, are common coping mechanisms to manage emotional pain or dissociation. These patients often form intense attachments to specific caregivers, leading to boundary-testing and emotional volatility.
Rationale for correct answer
B. Emotional dysregulation and self-harm are hallmark features of borderline personality disorder. Josie’s idealization of the nurse, intense reaction to perceived abandonment, and use of self-injury to “stop the numbness” are classic signs. Her unstable relationships, identity disturbance, and affective instability further support this diagnosis.
Rationale for incorrect answers
A. The focus of obsessive-compulsive personality disorder is on control, orderliness, and perfectionism, not emotional instability or self-harm. These individuals are rigid and preoccupied with rules, not prone to impulsive or self-destructive behavior.
C. Antisocial personality disorder is marked by disregard for others’ rights, deceit, and lack of remorse. Josie’s emotional vulnerability, fear of abandonment, and self-harm are inconsistent with the manipulative, unemotional traits of antisocial behavior.
D. Schizotypal personality disorder involves eccentric behavior, cognitive distortions, and social anxiety. While these individuals may be socially isolated, they do not typically exhibit the intense emotional reactivity or self-injury seen in borderline personality disorder.
Take Home Points
- Borderline personality disorder presents with emotional instability, fear of abandonment, and recurrent self-harm.
- Self-injury in BPD is often a maladaptive coping mechanism to relieve emotional numbness or distress.
- BPD must be differentiated from antisocial personality disorder, which lacks emotional depth and remorse.
- Obsessive-compulsive and schizotypal personality disorders do not typically involve impulsivity or self-injurious behavior.
Lacey, a 19-year-old patient, shows you multiple fresh, serious (but non-life-threatening) self-inflicted cuts on her forearm. Which response would be most therapeutic?
Explanation
Self-injurious behavior is often a maladaptive coping mechanism used to regulate overwhelming emotions, relieve psychological numbness, or express internal distress. It is commonly associated with borderline personality disorder, depression, and trauma-related conditions. These behaviors are not typically suicidal but signal significant emotional dysregulation. Therapeutic responses must be nonjudgmental, maintain safety, and promote emotional insight. The goal is to validate the patient’s experience while guiding them toward healthier coping strategies and emotional processing.
Rationale for correct answer
D. Therapeutic engagement and emotional insight are central to this response. It prioritizes wound care while encouraging reflection on emotional triggers. Writing down thoughts fosters self-awareness and sets the stage for a meaningful therapeutic discussion, helping the patient explore underlying distress.
Rationale for incorrect answers
A. The word sorry may blur professional boundaries and reinforce emotional dependency. While empathetic, this response lacks structure and may not promote emotional insight or future coping strategies.
B. The focus on searched introduces a punitive tone and may escalate distress. Although safety is important, this approach lacks therapeutic engagement and may alienate the patient.
C. Labeling the behavior as attention-seeking is invalidating and stigmatizing. It undermines the emotional pain driving the behavior and damages the therapeutic alliance, potentially worsening the patient’s distress.
Take Home Points
- Self-injury is often a coping mechanism for emotional dysregulation, not a suicidal gesture.
- Therapeutic responses should validate distress, ensure safety, and promote emotional insight.
- Avoid punitive or judgmental language when addressing self-harm; it can escalate emotional instability.
- Encourage structured reflection and discussion to help patients identify triggers and develop healthier coping strategies.
Alicia, a 31-year-old patient, is flirting with a peer. She is overheard asking him to convince staff to give her privileges to leave the inpatient mental health unit. Later, she offers you a backrub in exchange for receiving her 10:00 p.m. Xanax an hour early. Which response(s) to such behaviors would be most therapeutic? Select all that apply.
Explanation
Manipulative behavior in psychiatric settings often reflects underlying unmet needs, poor coping strategies, and distorted interpersonal boundaries. It may be linked to personality disorders, especially borderline personality disorder, where individuals use charm, seduction, or threats to gain control or avoid distress. Therapeutic responses must maintain professional boundaries, reinforce adaptive behaviors, and avoid reinforcing maladaptive patterns. Staff must remain consistent, avoid splitting, and use structured interventions to promote insight and accountability. Limit-setting and modeling appropriate communication are essential to prevent escalation and maintain unit safety.
Rationale for correct answers
A. This response promotes insight and accountability by labeling the behavior and exploring healthier alternatives. It avoids judgment and supports therapeutic engagement, helping Alicia recognize the impact of her actions and develop more adaptive strategies.
B. Role-playing is a behavioral intervention that teaches Alicia alternative ways to meet her needs. It reinforces appropriate communication and empowers her to practice new skills in a safe, structured environment, enhancing her interpersonal effectiveness.
E. Setting clear boundaries and consequences is essential in managing manipulative behavior. This response maintains therapeutic structure, prevents reinforcement of inappropriate actions, and communicates expectations without emotional reactivity.
Rationale for incorrect answers
C. This response fosters a punitive and divisive atmosphere, undermining trust among patients and staff. It risks escalating conflict and reinforces Alicia’s perception of rejection, which may worsen her behavior.
D. Bargaining with manipulative behavior compromises professionalism and blurs boundaries. It reinforces the idea that inappropriate actions can yield rewards, undermining therapeutic goals and staff consistency.
F. Ignoring the behavior may inadvertently reinforce it through intermittent reward. Without feedback or redirection, Alicia may escalate her actions to gain attention or privileges, compromising unit safety and therapeutic integrity.
Take Home Points
- Manipulative behavior often reflects unmet emotional needs and poor coping mechanisms, especially in personality disorders.
- Therapeutic responses must be structured, consistent, and focused on promoting insight and adaptive behavior.
- Role-playing and limit-setting are effective strategies to redirect inappropriate behavior and reinforce boundaries.
- Differentiating manipulative behavior from psychosis or impulsivity is critical for appropriate intervention and care planning.
A client who has borderline personality disorder says that a male nursing student was flirting with her and tried to kiss and touch her breasts. The student denies the accusation but says, “She asked me if I thought she was attractive, and I said yes.” What is the best way to handle this situation?
Explanation
Borderline personality disorder is characterized by pervasive instability in interpersonal relationships, self-image, and affect, often accompanied by marked impulsivity. Patients may exhibit splitting, intense emotional reactions, and manipulative or seductive behaviors, especially in response to perceived rejection or abandonment. These behaviors can lead to false accusations or boundary violations. Staff must maintain professional boundaries, document incidents objectively, and avoid emotional entanglement. Clinical education should emphasize structured responses, supervision, and incident reporting to protect both patients and trainees.
Rationale for correct answer
A. This response is both protective and educational. It acknowledges the potential for boundary-testing behavior in patients with borderline traits and guides the student toward appropriate documentation and supervisory support. It reinforces professional boundaries and ensures institutional oversight.
Rationale for incorrect answers
B. While reflection is important, minimizing the incident as a mere learning experience risks underestimating the seriousness of the allegation. It fails to initiate formal documentation or supervisory involvement, which are essential in such cases.
C. Confronting the patient directly may escalate conflict and compromise therapeutic rapport. It also risks violating professional boundaries and may be perceived as coercive or intimidating, especially in psychiatric settings.
D. Suggesting that “nothing is likely to come of it” undermines the credibility of the reporting process and may discourage future disclosures. It also bypasses proper institutional channels and fails to support the student appropriately.
Take Home Points
- Borderline personality disorder may involve seductive, manipulative, or accusatory behaviors that challenge professional boundaries.
- Staff and students must maintain clear boundaries and avoid emotional entanglement or direct confrontation.
- All allegations of misconduct must be documented and reported through appropriate institutional channels.
- Clinical education should emphasize structured supervision, incident reporting, and therapeutic neutrality in managing complex psychiatric behaviors.
A female presents with a history of repeated episodes of slashing her wrists and attempted suicide and now presents with a similar history. What is the diagnosis?
Explanation
Borderline personality disorder is a pervasive pattern of instability in interpersonal relationships, self-image, and affect, with marked impulsivity. It often manifests with recurrent suicidal behavior, gestures, or threats, and self-mutilating acts such as cutting. These behaviors are typically triggered by perceived abandonment or emotional dysregulation. Patients may also exhibit intense mood swings, chronic feelings of emptiness, and identity disturbance. The disorder is more common in females and often coexists with mood, anxiety, and substance use disorders. Management includes dialectical behavior therapy (DBT), mood stabilizers, and structured therapeutic environments.
Rationale for correct answer
D. The presence of repeated self-harm and suicide attempts, particularly in the context of emotional distress, is highly characteristic of borderline personality disorder. These behaviors are often used as maladaptive coping mechanisms to manage overwhelming affect or interpersonal conflict.
Rationale for incorrect answers
A. Schizotypal personality disorder is marked by eccentric behavior, social anxiety, and cognitive or perceptual distortions, not recurrent self-harm or suicidal behavior.
B. Histrionic personality disorder involves attention-seeking and excessive emotionality, but it does not typically include recurrent suicidal gestures or self-mutilation.
C. Dependent personality disorder is characterized by submissiveness and fear of separation, but it lacks the impulsivity and recurrent self-injurious behavior seen in borderline personality disorder.
Take Home Points
- Borderline personality disorder often presents with recurrent self-harm and suicidal behaviors triggered by emotional dysregulation.
- It must be differentiated from other personality disorders that lack impulsivity and self-injurious patterns.
- Management includes DBT, mood stabilizers, and structured therapeutic relationships.
- Accurate diagnosis is essential to avoid mislabeling behaviors as manipulative or attention-seeking without addressing underlying pathology.
A 25-year-old woman was brought to the casualty after taking an overdose of diazepam following a broken relationship. History revealed that she had many such relationships in the past and also has cut marks over her wrists. What is the most likely diagnosis?
Explanation
Borderline personality disorder is marked by pervasive instability in relationships, affect, and self-image, often accompanied by impulsivity and recurrent self-harming behaviors. Individuals may experience intense emotional reactions to perceived abandonment, leading to suicidal gestures or overdoses. They often have a history of unstable interpersonal relationships and may engage in self-mutilation as a maladaptive coping strategy. These behaviors are not necessarily driven by a desire to die but rather to regulate overwhelming emotions or elicit care. The condition is more prevalent in young women and requires structured, empathetic, and consistent therapeutic approaches.
Rationale for correct answer
C. The combination of impulsive overdose, wrist cutting, and unstable romantic relationships strongly supports borderline personality disorder. These behaviors reflect emotional dysregulation and fear of abandonment, hallmark features of the disorder.
Rationale for incorrect answers
A. Narcissistic personality disorder involves grandiosity and need for admiration, but does not typically present with self-harm or impulsive suicidal behavior following relationship loss.
B. Histrionic personality disorder features attention-seeking and dramatic emotional expression, but lacks the recurrent self-injurious behavior and emotional instability seen in borderline personality disorder.
D. A severe depressive episode may include suicidal ideation, but the pattern of repetition and impulsivity, along with unstable relationships and self-mutilation, points more specifically to a personality disorder rather than a mood episode.
Take Home Points
- Borderline personality disorder often presents with impulsive self-harm and emotional instability triggered by interpersonal stress.
- It must be differentiated from mood disorders and other personality disorders that lack recurrent self-injurious behavior.
- Management includes dialectical behavior therapy, mood stabilizers, and structured therapeutic boundaries.
- Accurate diagnosis is essential to guide appropriate treatment and avoid mislabeling behaviors as purely depressive or manipulative.
A defect in empathy or in the capacity to appreciate other people’s feelings, especially to comprehend how others feel about the consequences of one’s own actions, is the core feature of which disorder?
Explanation
A defect in empathy and disregard for others’ feelings is central to dissocial personality disorder, a condition marked by persistent antisocial behavior, lack of remorse, and failure to conform to social norms. Individuals often manipulate or exploit others and show callousness toward the consequences of their actions. They may have a history of conduct disorder in childhood and continue to violate the rights of others into adulthood. This disorder is associated with increased risk of criminality, substance abuse, and poor interpersonal relationships.
Rationale for correct answer
B. The defining feature of dissocial personality disorder is a profound lack of empathy and disregard for others’ emotions, especially regarding the impact of one’s actions. This aligns directly with the question stem, which highlights impaired emotional comprehension and interpersonal insensitivity. Individuals often rationalize harmful behavior and show no remorse, making this the most scientifically accurate choice.
Rationale for incorrect answers
A. Schizoid personality disorder is marked by emotional detachment, social withdrawal, and limited interest in relationships. However, it does not involve active disregard for others’ feelings or consequences of actions. These individuals prefer solitude but do not typically harm or manipulate others.
C. Paranoid personality disorder involves pervasive suspicion and mistrust of others, often interpreting benign actions as malicious. While interpersonal difficulties are common, the core issue is not a lack of empathy but rather hypervigilance and misinterpretation of intent.
D. Emotionally unstable personality disorder (often borderline type) features intense emotional instability, impulsivity, and fear of abandonment. Although empathy may fluctuate during emotional crises, the primary deficit is not a consistent inability to appreciate others’ feelings, but rather difficulty regulating one’s own emotions.
Take Home Points
- Dissocial personality disorder is defined by persistent antisocial behavior, lack of empathy, and disregard for social norms.
- It must be differentiated from schizoid personality disorder, which involves emotional detachment but not interpersonal harm.
- Paranoid personality disorder centers on mistrust and suspicion, not emotional insensitivity.
- Emotionally unstable personality disorder involves emotional dysregulation and impulsivity, not a core empathy deficit.
All the characteristics mentioned below are seen in schizoid personality disorder except:
Explanation
Schizoid personality disorder is a pervasive pattern of detachment from social relationships and a restricted range of emotional expression. Individuals with this disorder often appear emotionally cold, prefer solitary activities, and lack interest in forming close relationships. They may be aloof and indifferent to praise or criticism, but they are not typically hostile or judgmental toward others. Many are introspective, spending time in fantasy or intellectual pursuits, but they do not exhibit prejudice or strong opinions about others.
Rationale for correct answer
A. The term bigoted implies strong, intolerant prejudice against others, which is not characteristic of schizoid personality disorder. These individuals are socially withdrawn and emotionally indifferent, but they do not harbor hostile or discriminatory attitudes. Their detachment is passive, not antagonistic.
Rationale for incorrect answers
B. Emotional coldness is a hallmark of schizoid personality disorder. These individuals show limited emotional expression and often appear indifferent to social interactions or emotional cues from others.
C. Being aloof—distant and disengaged—is consistent with schizoid traits. They avoid close relationships and prefer isolation, often seeming uninterested in others’ lives or emotions.
D. Introspective tendencies are common in schizoid personality disorder. These individuals often retreat into internal worlds, engaging in solitary intellectual or creative activities, and may be absorbed in abstract thinking.
Take Home Points
- Schizoid personality disorder involves emotional detachment, social withdrawal, and preference for solitude.
- It must be differentiated from paranoid personality disorder, which includes mistrust and suspicion.
- Unlike dissocial personality disorder, schizoid individuals do not violate others’ rights or show callousness.
- Bigotry is not a feature of schizoid personality disorder; their detachment is passive, not hostile.
Exams on Personality Disorders
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
- Objectives
- Introduction
- Description, Classification and Etiology
- Description, Classification and Etiology
- Practice Exercise 1
- Cluster a – Odd or Eccentric Disorders
- Practice Exercise 2
- Cluster B – Dramatic, Emotional, or Erratic Disorders
- Practice Exercise 3
- Cluster C – Anxious or Fearful Disorders
- Practice Exercise 4
- Risk Factors for Personality Disorders
- Treatment for Personality Disorders
- Practice Exercise 5
- Comorbidity and Differential Diagnosis
- Nursing Care Process for Personality Disorders
- Practice Exericise 6
- Summary
- Comprehensive Questions
Notes Highlighting is available once you sign in. Login Here.
Objectives
The learner will be able to:
- Articulate the scientific definition, core characteristics, and basic concepts of personality disorders.
- Analyze the current understanding of biopsychosocial and etiological factors contributing to the development of personality disorders.
- Categorize personality disorders according to the three clusters (A, B, and C) and describe the general behavioral features of each cluster.
- Identify the specific neurobiological correlates and areas of the brain hypothesized to be associated with the characteristic behaviors of each personality disorder.
- Describe the clinical presentations, predisposing factors, and specific nursing interventions for all personality disorders in Cluster A, B, and C.
- Formulate appropriate nursing diagnoses and realistic, measurable outcomes for clients exhibiting symptoms of personality disorders.
- Apply evidence-based nursing interventions, including promoting safety and de-escalation techniques, for clients with various personality disorders.
- Recognize and address the common maladaptive coping strategies and defense mechanisms utilized by individuals with personality disorders.
- Discuss the various pharmacological and non-pharmacological treatment modalities, including different types of psychotherapy and milieu therapy, used in the management of personality disorders.
- Differentiate between personality disorders and other psychiatric conditions, recognizing common comorbidities and utilizing appropriate differential diagnosis.
Introduction
- Personality disorders represent a category of mental disorders characterized by an enduring, pervasive, and inflexible pattern of inner experience and outward behavior that significantly deviates from the expectations of the individual’s culture, leading to distress or functional impairment.
- These patterns are typically fixed and manifest across a broad range of personal and social situations, often becoming evident in adolescence or early adulthood and remaining stable over time.
- The development of a personality disorder is thought to result from a complex interaction of genetic predispositions, neurobiological factors, and adverse environmental influences.
- The classification system organizes these disorders into three distinct clusters based on descriptive similarities, which aids in understanding and treatment planning.
- Effective Mental Health Nursing requires a scientific and comprehensive understanding of the diverse clinical presentations, underlying mechanisms, and specific therapeutic interventions tailored to each disorder to promote client safety and improved quality of life.
Description, Classification and Etiology
3.1. Description of Personality Disorders
A personality disorder is a chronic and pervasive condition involving maladaptive patterns of perceiving, relating to, and thinking about the environment and oneself.
- These rigid and unhealthy patterns typically cause significant distress or impairment in social, occupational, or other important areas of functioning.
- According to the DSM-5-TR, the pattern must manifest in two or more of the following areas:
- Cognition (ways of perceiving and interpreting self, other people, and events).
- Affectivity (the range, intensity, lability, and appropriateness of emotional response).
- Interpersonal functioning.
- Impulse control.
- The pattern must be stable and long-lasting, with an onset traceable at least to adolescence or early adulthood.
3.2. Basic Concepts and Defining Characteristics
- Pervasiveness: The maladaptive traits are evident across a wide range of personal and social contexts.
- Inflexibility/Rigidity: The individual is unable to adapt their behavior or emotional responses to changing circumstances, leading to repeated conflicts.
- Ego-syntonicity: The behaviors, thoughts, and attitudes are often consistent with the individual's self-image and goals, meaning they perceive their patterns as normal or acceptable, rather than viewing them as a problem (unlike ego-dystonic disorders, such as obsessive-compulsive disorder).
- This lack of insight often makes treatment challenging, as the client may externalize blame for their difficulties.
- Maladaptive Traits: The core features are exaggerated, pathological variations of common personality traits that hinder effective functioning.
- Difficulty in Relationships: A defining feature is an inability to maintain healthy, stable, and reciprocal relationships due to the core pathology.
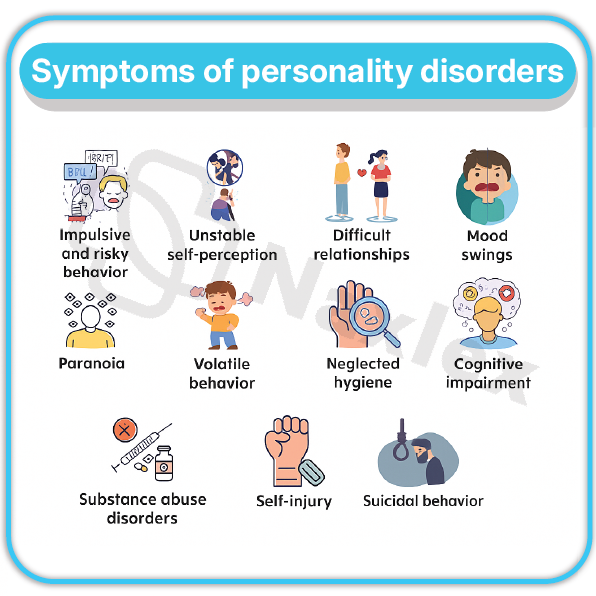
3.3. Etiologic Factors
The etiology of personality disorders is considered a complex integration of biological, psychological, and sociocultural influences.
- Biological Factors (Neurobiological/Genetic):
- Genetics: Twin and family studies demonstrate a heritable component, particularly for Schizotypal (sharing genetic overlap with Schizophrenia) and Antisocial and Borderline personality disorders.
- Neurotransmitters: Dysregulation of serotonin (5-HT) is implicated, particularly in impulsivity, aggression, and affective instability observed in Borderline and Antisocial personality disorders.
- Neurobiology: Structural and functional brain abnormalities are frequently observed (see Section 3.5).
- Psychological Factors (Psychodynamic/Developmental):
- Early Childhood Trauma: High rates of childhood abuse (sexual, physical, emotional) and neglect are consistently reported, particularly in borderline personality disorder.
- Insecure Attachment: Disrupted early attachment with primary caregivers is theorized to impair the development of self-identity and stable relationships.
- Object Relations Theory: Maladaptive patterns of internalized self-representations and relationship-representations (objects) are central to the development of pathology. For example, Splitting (the inability to integrate positive and negative aspects of self and others) is a key concept in borderline personality disorder.
- Sociocultural Factors:
- Environmental influences, such as family dysfunction, peer relationships, and broader cultural expectations, can significantly shape the expression of personality traits and contribute to maladaptive patterns.
3.4. Classification into Clusters
Personality disorders are categorized into three clusters based on descriptive similarities:
|
Cluster |
General Description |
Associated Disorders |
|
A |
Odd or Eccentric |
Paranoid, Schizoid, Schizotypal |
|
B |
Dramatic, Emotional, or Erratic |
Antisocial, Borderline, Histrionic, Narcissistic |
|
C |
Anxious or Fearful |
Avoidant, Dependent, Obsessive-Compulsive |
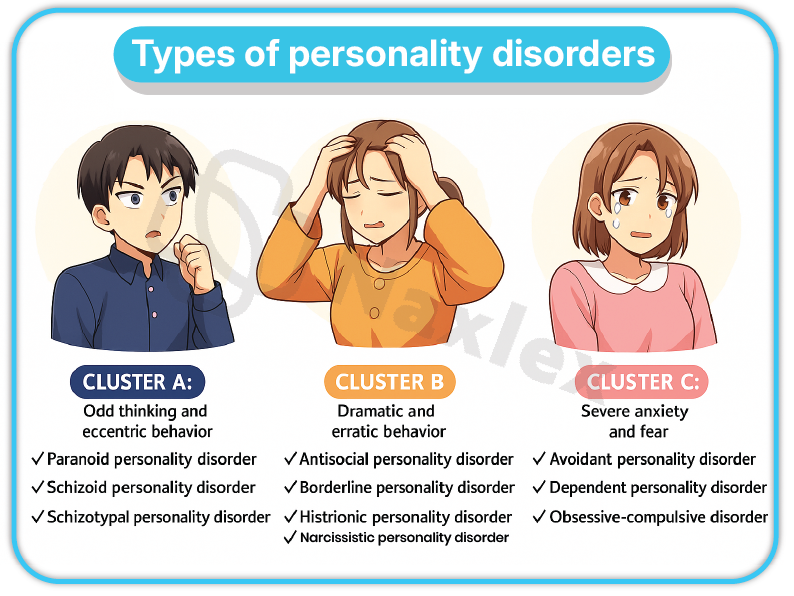
3.5. Areas of the Brain Associated with Personality Disorder Behaviors
Specific behaviors seen in personality disorders have been linked to functional and structural alterations in key brain regions:
- Frontal Lobe (Prefrontal Cortex):
- Involved in executive functions, planning, impulse control, working memory, and social cognition.
- Hypo-frontality (reduced activity or volume) is commonly associated with Antisocial Personality Disorder (linked to poor judgment and impulsivity) and deficits in emotion regulation in Borderline Personality Disorder.
- Limbic System (Amygdala and Hippocampus):
- The amygdala is central to fear processing and emotional arousal. Dysregulation is linked to emotional lability and heightened threat perception in disorders like Borderline (hypersensitivity to negative stimuli) and Paranoid (distrust).
- The hippocampus is involved in memory formation; trauma-related changes here may contribute to emotional dysregulation.
- Anterior Cingulate Cortex (ACC):
- Crucial for emotional regulation, error detection, and attention. Alterations here are implicated in emotional dysregulation and cognitive biases across several disorders, including Borderline and Obsessive-Compulsive Personality Disorder.
- Temporal Lobe:
- Involved in auditory processing and cognitive-perceptual distortions. Alterations are sometimes noted in Schizotypal Personality Disorder, contributing to unusual perceptual experiences.
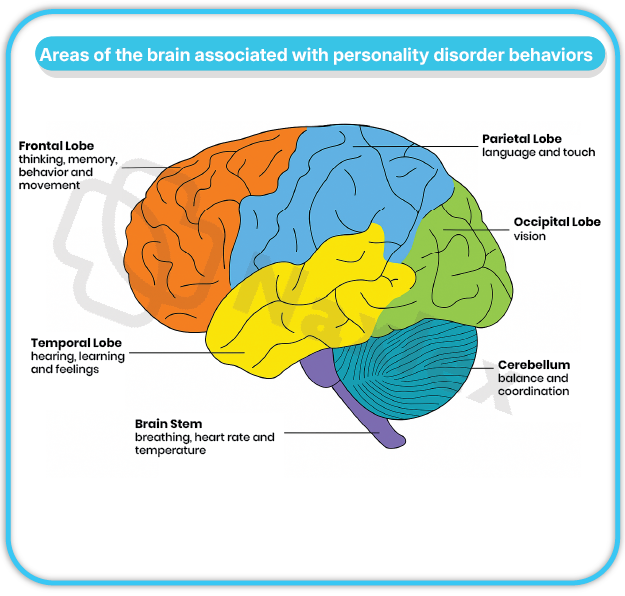
Nursing Insights
- Ego-syntonic vs. Ego-dystonic: RN candidates must recognize that a key reason individuals with personality disorders rarely seek treatment is that their symptoms are typically ego-syntonic—they view the world and their reactions as normal and often blame others for their problems.
- This contrasts sharply with most other mental illnesses (e.g., Depression, OCD, Generalized Anxiety Disorder), which are often ego-dystonic (the symptoms are inconsistent with one’s self-concept and cause distress), motivating the client to seek relief.
- This difference dictates the therapeutic approach, requiring the nurse to focus initially on the consequences of the client's behavior rather than the client's internal perception of the behavior.
Cluster a – Odd or Eccentric Disorders
- Cluster A disorders are characterized by behaviors that are often described as odd or eccentric.
- Individuals in this cluster frequently display social awkwardness, emotional detachment, and peculiar patterns of thinking and perceiving.
- There is a notable overlap in symptomatology with Schizophrenia, suggesting a possible shared genetic vulnerability, although the Cluster A disorders are less severe and do not involve psychosis (e.g., persistent delusions or hallucinations) in the absence of severe stress.
5.1. PARANOID PERSONALITY DISORDER (PPD)
- Definition: A pervasive distrust and suspiciousness of others such that their motives are interpreted as malevolent, beginning by early adulthood and present in a variety of contexts.
- Epidemiological Statistics: Estimated prevalence in the general population is approximately 2.3% to 4.4%. It is more commonly diagnosed in males than females and may be seen more often in individuals with a family history of Schizophrenia or delusional disorder.
Clinical Picture: Characteristics
- Suspiciousness and Distrust: A belief that others are exploiting, harming, or deceiving them, even in the absence of evidence.
- Preoccupation with Justification: They are preoccupied with unjustified doubts about the loyalty or trustworthiness of friends or associates.
- Reluctance to Confide: They are reluctant to confide in others for fear that the information will be used maliciously against them.
- Interpreting Hidden Meanings: They often read demeaning or threatening hidden meanings into benign remarks or events.
- Persistent Grudges: They persistently bear grudges and are unforgiving of perceived insults, injuries, or slights.
- Perceiving Attacks: They perceive attacks on their character or reputation that are not apparent to others and are quick to react angrily or to counterattack.
- Suspicion of Partner: Recurrent, unjustified suspicions regarding the fidelity of a spouse or sexual partner.
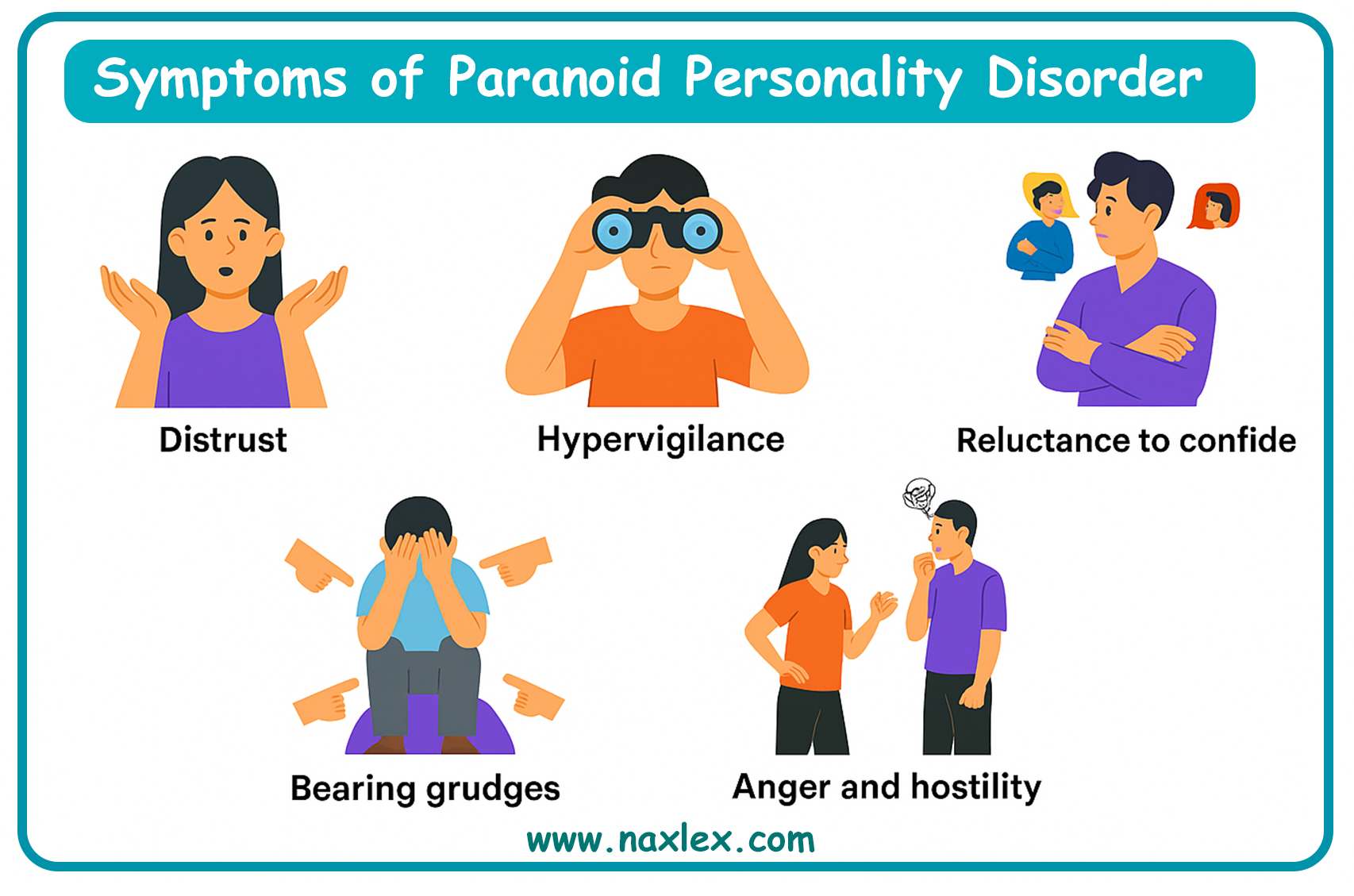
Predisposing Factors
- Heredity: Possible genetic link to schizophrenia.
- Childhood Trauma/Abuse: Experience of severe emotional trauma, neglect, or physical abuse in childhood may contribute to the development of deep-seated distrust.
- Psychological: An individual's projection of their own hostility and aggression onto others may fuel the paranoid ideation.
Diagnoses
- Primary Diagnoses: Disturbed thought process (related to pervasive suspiciousness) and Impaired social interaction (related to inability to trust).
- Secondary/Supportive Diagnoses: Risk for violence: Directed at others (related to defensive rage when perceived as threatened).
Nursing Interventions
- Maintain Professionalism: Use a formal, business-like approach and keep a courteous but neutral affect to avoid being perceived as overly familiar or invasive.
- Honesty and Consistency: Be scrupulously honest and adhere strictly to schedules and commitments to build the minimal trust possible.
- Avoid Group Therapy (Initially): Group settings may increase anxiety and exacerbate suspiciousness due to the need to interact with multiple unknown individuals.
- Respect Need for Space: Give the client adequate personal space and avoid whispering or laughing in their presence, which can be misinterpreted as conspiracy.
- Medication: Antianxiety agents or atypical antipsychotics may be used for symptom management (e.g., severe anxiety, hypervigilance, agitation).
5.2. SCHIZOID PERSONALITY DISORDER (SPD)
- Definition: A pervasive pattern of detachment from social relationships and a restricted range of emotional expression in interpersonal settings, beginning by early adulthood.
- Epidemiological Statistics: Prevalence is estimated to be between 3.1% and 4.9% in the general population. It may be slightly more common in males.
Clinical Picture: Characteristics
- Detachment and Solitude: Neither desires nor enjoys close relationships, including being part of a family. They consistently choose solitary activities.
- Lack of Interest in Others: They have little, if any, interest in having sexual experiences with another person.
- Anhedonia: Takes pleasure in few, if any, activities.
- Emotional Coldness: Shows emotional coldness, detachment, or flat affect; they appear indifferent to both praise and criticism.
- Interpersonal Deficits: Lacks close friends or confidants other than first-degree relatives.
- Fantasy Over Action: Often immerse themselves in non-human interests, such as mathematics, or engage in excessive fantasy.
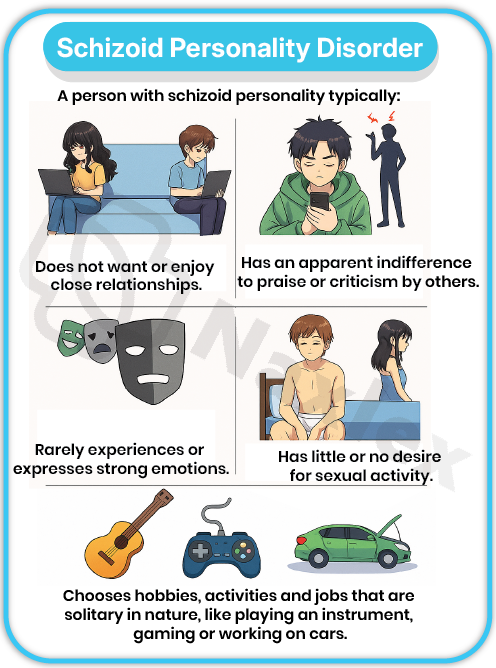
Predisposing Factors
- Genetics: Possible familial pattern, potentially sharing a distant genetic link to schizophrenia, but a distinct entity.
- Early Development: A cold, neglectful childhood environment that failed to provide the opportunity for emotional attachment and bonding.
- Temperament: Innate shyness and a preference for solitary activities may be present from a very young age.
Diagnoses
- Primary Diagnoses: Impaired social interaction (related to preference for solitude and emotional detachment) and Social isolation (related to lack of desire for close relationships).
- Secondary/Supportive Diagnoses: Ineffective coping (related to reliance on fantasy and social withdrawal).
Nursing Interventions
- Respect Isolation: Recognize and respect the client's need for social isolation; the goal is not to force socialization but to improve function.
- Improve Social Functioning (Gradual): If social intervention is deemed necessary, encourage interaction focused on their interests (e.g., talking about hobbies), not personal life.
- Focus on Concrete Assistance: Offer assistance with practical problems or basic self-care, as direct problem-solving is preferred over emotional support.
- Psychotherapy: Group therapy is usually not appropriate initially, as it causes too much anxiety. Individual therapy should focus on building a non-demanding, non-intrusive therapeutic alliance.
- Medication: Low-dose antipsychotics or antidepressants may be used to treat co-occurring anxiety or depressive symptoms, or to improve emotional expression.
Nursing Insights
- Cluster A Distinction from Schizophrenia: While Cluster A disorders share features like social withdrawal and peculiar thinking with Schizophrenia, it is critical for nurses to differentiate them.
- The key distinction is the absence of persistent psychotic symptoms (e.g., frank delusions, hallucinations, disorganized speech) in Cluster A disorders.
- A client with Schizotypal PD may have ideas of reference, but not fixed delusions of reference.
- They may have unusual perceptual experiences, but not true, sustained hallucinations.
- This distinction guides treatment, as antipsychotic medication is rarely a primary treatment unless severe co-morbid symptoms or a brief, transient psychotic episode is present.
5.3. SCHIZOTYPAL PERSONALITY DISORDER (STPD)
- Definition: A pervasive pattern of social and interpersonal deficits marked by acute discomfort with, and reduced capacity for, close relationships, as well as by cognitive or perceptual distortions and eccentricities of behavior.
- Epidemiological Statistics: Estimated prevalence is about 3.9% in the general population. It is slightly more common in males and is generally considered to be the most prevalent of the Cluster A disorders. It is thought to be part of the "schizophrenia spectrum."
Clinical Picture: Characteristics
- Cognitive and Perceptual Distortions:
- Ideas of Reference: Incorrect interpretations of external events as having a special meaning for oneself (but not of delusional intensity).
- Odd Beliefs/Magical Thinking: Beliefs that are inconsistent with subcultural norms, such as clairvoyance, telepathy, "sixth sense," or bizarre fantasies.
- Unusual Perceptual Experiences: Sensations that may include illusions, such as sensing a presence when alone (but not true hallucinations).
- Eccentric Appearance/Behavior: Behavior or appearance that is odd, eccentric, or peculiar (e.g., wearing ill-fitting, soiled, or unusual clothing).
- Suspiciousness/Paranoid Ideation: Mistrust of others and their motives (less intense than PPD).
- Inappropriate/Constricted Affect: Emotional responses may be inappropriate or limited; they may look stiff or aloof.
- Lack of Close Relationships: Severe social anxiety that does not diminish with familiarity and tends to be associated with paranoid fears rather than negative judgments about self.
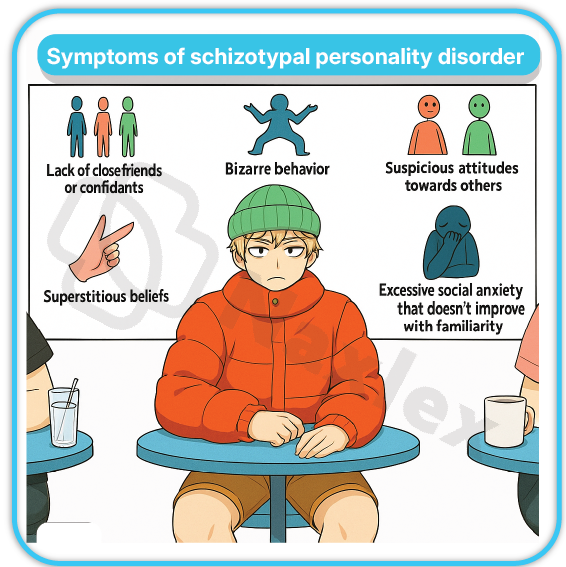
Predisposing Factors
- Genetics: Considered the personality disorder with the strongest genetic link to schizophrenia; individuals often have first-degree relatives with schizophrenia.
- Neurobiological: Possible deficits in inhibitory mechanisms and information processing, similar to but less severe than those seen in schizophrenia.
- Environmental: History of childhood neglect, abuse, or early separation from caregivers.
Diagnoses
- Primary Diagnoses: Disturbed thought process (related to magical thinking and ideas of reference), Impaired social interaction (related to social anxiety and eccentric behavior).
- Secondary/Supportive Diagnoses: Chronic low self-esteem (related to social isolation and feeling different).
Nursing Interventions
- Respect Need for Solitude: Acknowledge the need for space while encouraging small, realistic steps toward increasing social interactions, especially related to self-care and unit activities.
- Clarity in Communication: Use clear, concrete, and simple language when communicating to counteract their tendency toward circumstantiality, vagueness, or over-elaboration.
- Avoid Challenging Odd Beliefs: Do not directly challenge the client's magical thinking or strange beliefs; instead, gently reorient to reality-based topics and focus on the client's objective distress and functional outcomes.
- Medication: Low-dose atypical antipsychotics (e.g., risperidone, olanzapine) may be used to treat cognitive and perceptual symptoms, while antidepressants may manage associated anxiety and dysphoria.
- Psychotherapy: Cognitive-Behavioral Therapy (CBT) can help test the reality of their perceptions and develop social skills.
Cluster B – Dramatic, Emotional, or Erratic Disorders
- Cluster B disorders are characterized by patterns of behavior that are often perceived as dramatic, overly emotional, or unpredictable (erratic).
- Individuals in this cluster frequently struggle with impulse control and emotional regulation, leading to tumultuous interpersonal relationships.
- These disorders are often associated with the highest rates of hospitalization, criminal justice involvement, and overall functional impairment due to their volatile nature.
7.1 HISTRIONIC PERSONALITY DISORDER (HPD)
- Definition: A pervasive pattern of excessive emotionality and attention-seeking behavior, beginning early adulthood and present in a variety of contexts.
- Epidemiological Statistics: Estimated prevalence is approximately 2-3% in the general population. It is more frequently diagnosed in females, although this may be influenced by diagnostic bias.
Clinical Picture: Characteristics
- Center of Attention: The individual is uncomfortable in situations where they are not the center of attention. They often use physical appearance to draw attention to themselves.
- Seductive/Provocative Behavior: Interactions with others are often characterized by inappropriately sexually seductive or provocative behavior.
- Rapidly Shifting Emotions: Displays rapid shifting and shallow expression of emotions (affective lability). Emotions may appear exaggerated or theatrical.
- Speech Style: Has a style of speech that is excessively impressionistic and lacking in detail.
- Suggestibility: Easily influenced by others or circumstances (highly suggestible).
- Interprets Relationships as Closer: Considers relationships to be more intimate than they actually are (e.g., calling a new acquaintance a "dear, close friend").
- Somatization: May frequently seek medical attention or have vague, dramatized physical complaints.
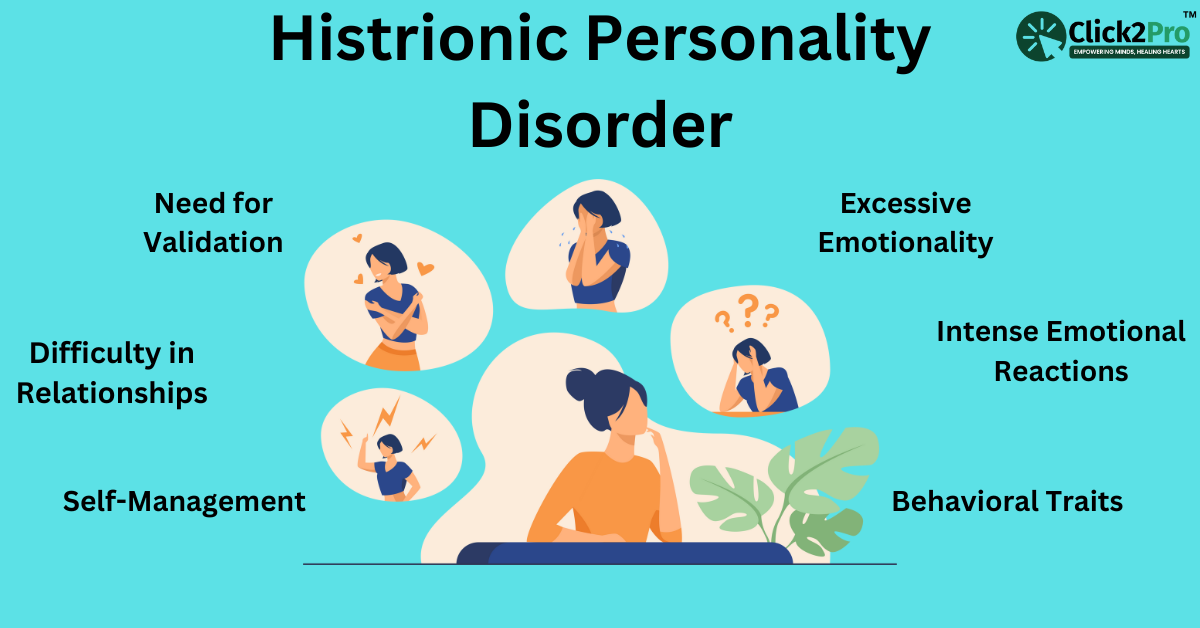
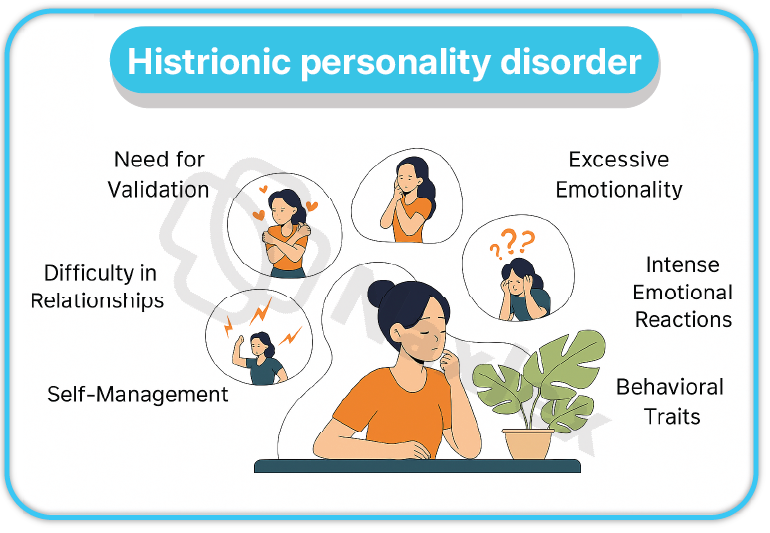
Predisposing Factors
- Genetics: Evidence suggests a familial link with other Cluster B disorders, possibly related to shared traits of emotional instability.
- Psychological: Psychoanalytic theory posits parental failure to validate the child's sense of self, leading to an adult seeking external validation through dramatic displays.
- Neurobiological: Possible link to increased norepinephrine and serotonergic dysfunction.
Diagnoses
- Primary Diagnoses: Ineffective coping (related to use of manipulative or attention-seeking behaviors) and Impaired social interaction (related to inappropriate behaviors).
- Secondary/Supportive Diagnoses: Chronic low self-esteem (related to seeking approval from others).
Nursing Interventions
- Set Clear Limits: The nurse must set and maintain professional, firm limits on sexually suggestive or demanding attention-seeking behavior.
- Positive Reinforcement: Reinforce and encourage appropriate, non-dramatic communication and behavior. Ignore attention-seeking behavior (when possible and safe) to extinguish the maladaptive pattern.
- Improve Self-Esteem: Help the client clarify their true feelings, which are often masked by external drama. Focus on strengths and genuine accomplishments, not physical appearance.
7.2 NARCISSISTIC PERSONALITY DISORDER (NPD)
- Definition: A pervasive pattern of grandiosity (in fantasy or behavior), a need for admiration, and a lack of empathy, beginning by early adulthood.
- Epidemiological Statistics: Estimated prevalence is between 0.5% and 5% in the general population. It is more frequently diagnosed in males, with rates of up to 75% being male.
Clinical Picture: Characteristics
- Grandiosity: Has a grandiose sense of self-importance, exaggerating achievements and talents and expecting to be recognized as superior without commensurate achievements.
- Fantasy: Preoccupied with fantasies of unlimited success, power, brilliance, beauty, or ideal love.
- Sense of Entitlement: Believes they are "special" and unique and should only associate with, or be understood by, other special or high-status people. Requires excessive admiration.
- Exploitation: Is interpersonally exploitative, taking advantage of others to achieve their own ends.
- Lack of Empathy: Is unwilling or unable to recognize or identify with the feelings and needs of others.
- Envy: Is often envious of others or believes that others are envious of them.
- Arrogance: Shows arrogant, haughty behaviors or attitudes.
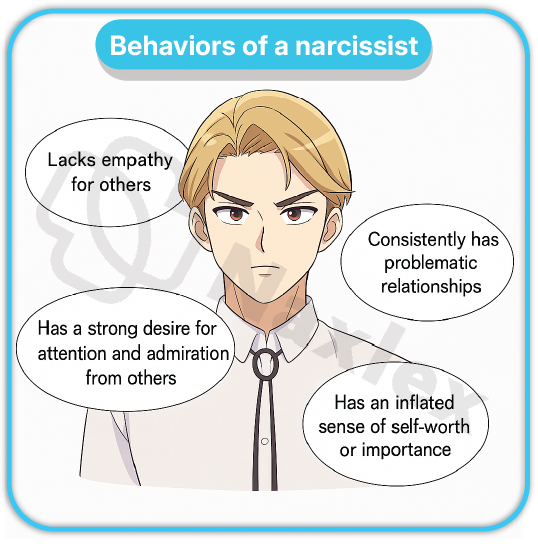
Predisposing Factors
- Psychological: A primary psychological theory suggests that NPD stems from failure to develop a realistic sense of self-worth, potentially due to parental overindulgence or, conversely, highly critical parenting that demanded perfection.
- Societal: Contemporary society's emphasis on individualism, success, and celebrity status may contribute to or amplify narcissistic traits.
Diagnoses
- Primary Diagnoses: Chronic low self-esteem (although masked by grandiosity) and Impaired social interaction (related to exploitative behavior and lack of empathy).
- Secondary/Supportive Diagnoses: Ineffective coping (related to hypersensitivity to criticism).
Nursing Interventions
- Neutral Demeanor: Maintain a neutral, respectful, but non-adulatory approach to avoid feeding into the client’s grandiosity.
- Limit Setting: Institute strict limit-setting on any exploitative or demanding behavior towards staff or other clients.
- Avoid Confrontation: Avoid becoming defensive or engaging in power struggles, which can trigger narcissistic rage. Criticism must be measured and delivered in a non-judgmental manner.
- Self-Awareness: Help the client recognize the true source of their grandiosity, the underlying fear of failure and need for validation.
Nursing Insights
- Managing Narcissistic Rage and Therapeutic Alliance: The RN must anticipate that criticism, even perceived as mild, can shatter the NPD client's fragile self-esteem, leading to narcissistic rage (intense anger, devaluing, and aggression).
- The therapeutic alliance is often strained because the client expects special treatment and devalues the nurse if they perceive the nurse as inferior.
- A key nursing strategy is to consistently reinforce that all clients are treated equitably and to focus on behavioral goals rather than challenging their grandiosity directly, which is often counterproductive.
7.3 ANTISOCIAL PERSONALITY DISORDER (ASPD)
- Definition: A pervasive pattern of disregard for and violation of the rights of others, occurring since age 15, as indicated by three or more specified criteria (e.g., failure to conform to social norms, deceitfulness, impulsivity). Previously, it was called Psychopathy or Sociopathy.
- Epidemiological Statistics: Estimated prevalence is approximately 0.2% to 3.3% in the general population. The diagnosis is made much more often in males than in females.
- Prerequisite: The individual must have evidence of Conduct Disorder onset before age 15 years.
Clinical Picture: Characteristics
- Criminality: Failure to conform to social norms with respect to lawful behaviors, often repeatedly performing acts that are grounds for arrest.
- Deceit and Manipulation: Repeated lying, use of aliases, or conning others for personal profit or pleasure.
- Irresponsibility: Consistent irresponsibility, as indicated by repeated failure to sustain consistent work behavior or honor financial obligations.
- Lack of Remorse: Indifference to or rationalizing having hurt, mistreated, or stolen from another. Absence of guilt is a cardinal feature.
- Impulsivity and Recklessness: Impulsivity or failure to plan ahead; reckless disregard for the safety of self or others.
- Aggressiveness: Irritability and aggressiveness, often indicated by repeated physical fights or assaults.

Predisposing Factors
- Biological: Significant genetic component; individuals often have a family history of ASPD, substance abuse, or somatization disorder.
- Neurobiological: Low levels of Serotonin and high levels of Dopamine are implicated in aggressive and impulsive behaviors.
- Cortical Arousal: Studies show lower-than-normal autonomic nervous system arousal, requiring greater stimulation to achieve normal arousal levels (the need for high-risk behaviors).
- Environmental: Severe poverty, parental deprivation or neglect, and inconsistent or abusive parenting practices.
- Temperament: Diagnosed with childhood Conduct Disorder (e.g., cruelty to animals, destruction of property).
Diagnoses
- Primary Diagnoses: Risk for other-directed violence (related to inability to tolerate frustration) and Ineffective coping (related to impulsivity and self-serving behaviors).
- Secondary/Supportive Diagnoses: Impaired social interaction (related to manipulative behavior).
Nursing Interventions
- Safety First: Prioritize the safety of other clients and staff by maintaining constant awareness of the client's behavior and potential for manipulation or aggression.
- Consistent Limits: Establish and enforce strict, clear, and consistent rules and expectations, communicated non-emotionally. All staff must adhere to the plan to prevent the client from exploiting staff splits.
- Manage Manipulation: Identify manipulative behaviors (e.g., flattery, bargaining, provoking staff conflict) and address them immediately by reiterating the limits.
- Focus on Consequences: Hold the client accountable for their actions and focus on the immediate consequences of their behaviors, rather than attempting to instill empathy.
- Group Therapy: May be beneficial in a structured, long-term setting if participation is non-manipulative, as the peer feedback can be highly effective.
7.4 BORDERLINE PERSONALITY DISORDER (BPD)
- Definition: A pervasive pattern of instability of interpersonal relationships, self-image, and affects, and marked impulsivity, beginning by early adulthood.
- Epidemiological Statistics: Estimated prevalence is between 1.6% and 5.9% in the general population. It is one of the most common personality disorders and is diagnosed predominantly in females (up to 75%).
- Risk: High risk for self-mutilation (non-suicidal self-injury, NSSI) and recurrent suicidal behavior, gestures, or threats.
Clinical Picture: Characteristics
- Frantic Efforts to Avoid Abandonment: Intense fear of real or imagined abandonment, leading to desperate behaviors to prevent separation.
- Unstable Relationships (Splitting): A pattern of unstable and intense interpersonal relationships characterized by alternating between extremes of idealization (e.g., "the best nurse ever") and devaluation (e.g., "the worst, most incompetent nurse"). This is known as splitting.
- Identity Disturbance: Markedly and persistently unstable self-image or sense of self.
- Impulsivity: Impulsivity in at least two areas that are potentially self-damaging (e.g., spending, sex, substance abuse, reckless driving, binge eating).
- Affective Instability: Chronic feelings of emptiness. Recurrent suicidal behavior, gestures, threats, or self-mutilating behavior (NSSI).
- Inappropriate Anger: Inappropriate, intense anger or difficulty controlling anger (e.g., frequent temper tantrums, constant bitterness).
- Transient Paranoia/Dissociation: Transient, stress-related paranoid ideation or severe dissociative symptoms.
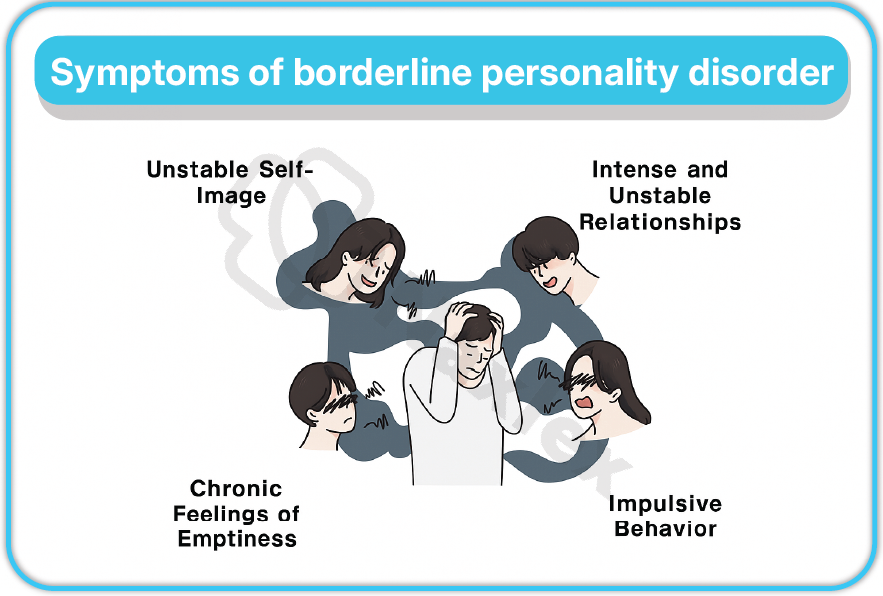
Predisposing Factors
- Biological:
- Neurobiological: Structural and functional brain deficits, particularly in the prefrontal cortex (impaired impulse control) and the amygdala (hyper-responsive emotional processing).
- Neurotransmitters: Significant evidence of Serotonin (5-HT) dysfunction linked to impulsivity and mood dysregulation.
- Psychological (Biosocial Theory): Marsha Linehan's theory proposes that BPD results from an interaction between a biological emotional vulnerability (innate, high sensitivity/intensity) and an invalidating environment (childhood abuse, neglect, or chronic emotional invalidation).
- Trauma: A history of childhood sexual abuse, physical abuse, or neglect is reported in a majority of clients.
Diagnoses
- Primary Diagnoses: Risk for self-mutilation/self-directed violence (related to inability to self-soothe) and Ineffective emotional regulation (related to affective instability).
- Secondary/Supportive Diagnoses: Disturbed personal identity (related to unstable self-image).
Nursing Interventions
- Safety Contract: Prioritize client safety; formulate a no-harm contract or safety plan regarding suicidal ideation and self-mutilation. Observe client closely as dictated by risk.
- Consistency and Boundaries: Maintain strict and consistent professional boundaries and communication among all staff to minimize the client's use of splitting to manipulate the environment.
- Validation: Use therapeutic communication that validates the client's feelings ("I hear you are feeling abandoned and terrified right now") while maintaining limits on behavior ("However, throwing the tray is not acceptable").
- Dialectical Behavior Therapy (DBT): Assist the client in learning and applying DBT skills, which is the gold-standard treatment. DBT focuses on mindfulness, distress tolerance, emotion regulation, and interpersonal effectiveness.
- Medication: Pharmacotherapy (SSRIs, mood stabilizers, atypical antipsychotics) is used primarily to manage symptoms of mood instability, impulsivity, and anxiety, rather than curing the disorder.
Cluster C – Anxious or Fearful Disorders
- Cluster C disorders are characterized by a predominant theme of anxiety or fearfulness.
- Individuals in this cluster often display a high level of stress, worry, and avoidance, resulting in difficulty with social and occupational functioning due to their need for control, perfection, or reassurance.
- These disorders often share features with anxiety disorders but involve a pervasive, inflexible personality pattern.
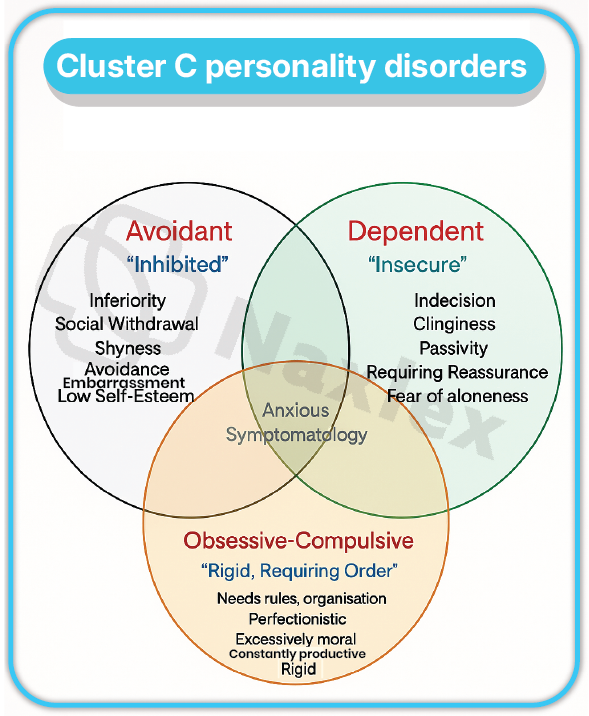
9.1. AVOIDANT PERSONALITY DISORDER (AvPD)
- Definition: A pervasive pattern of social inhibition, feelings of inadequacy, and hypersensitivity to negative evaluation, beginning by early adulthood.
- Epidemiological Statistics: Estimated prevalence is approximately 2.4% in the general population. It is equally common in males and females.
Clinical Picture: Characteristics
- Avoidance of Activities: Avoids occupational activities that involve significant interpersonal contact due to fears of criticism, disapproval, or rejection.
- Unwillingness to Get Involved: Is unwilling to get involved with people unless certain of being liked.
- Restraint in Relationships: Shows restraint within intimate relationships because of the fear of being shamed or ridiculed.
- Preoccupied with Rejection: Is preoccupied with being criticized or rejected in social situations.
- Inhibition: Views self as socially inept, personally unappealing, or inferior to others.
- Unlike Schizoid: While they avoid social contact like the Schizoid client, the Avoidant client desperately wants social interaction but is too fearful of rejection.
Predisposing Factors
- Temperament: Inherited temperament of shyness and high anxiety.
- Parental Abuse: Severe parental criticism and rejection, leading to feelings of worthlessness and a deep-seated belief that they are fundamentally unlovable.
Diagnoses
- Primary Diagnoses: Chronic low self-esteem (related to fear of negative evaluation) and Social isolation (related to fear of rejection).
- Secondary/Supportive Diagnoses: Anxiety (related to social situations).
Nursing Interventions
- Non-Threatening Approach: Use a friendly, gentle, reassuring, and accepting approach to establish trust.
- Do Not Force Socialization: Do not push the client into social situations; slowly and cautiously encourage new activities, using positive reinforcement for successful social engagement.
- Cognitive Restructuring: Help the client identify the negative self-talk and catastrophic thinking ("If I talk, I will be ridiculed") and challenge these automatic thoughts.
- Anxiety Management: Teach relaxation techniques and breathing exercises to manage acute anxiety associated with social fears.
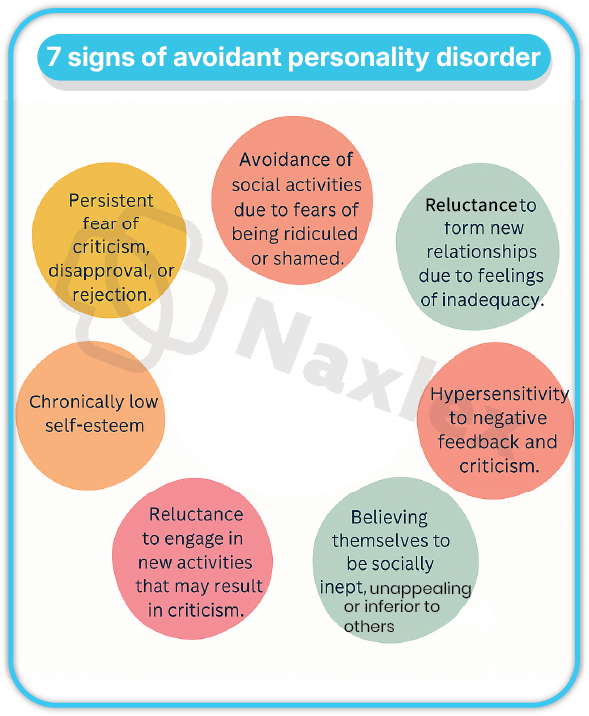
9.2 DEPENDENT PERSONALITY DISORDER (DPD)
- Definition: A pervasive and excessive need to be taken care of that leads to submissive and clinging behavior and fears of separation, beginning by early adulthood.
- Epidemiological Statistics: Estimated prevalence is approximately 0.5% in the general population, making it one of the less common disorders. It may be diagnosed slightly more often in females.
Clinical Picture: Characteristics
- Difficulty Making Decisions: Has difficulty making everyday decisions without an excessive amount of advice and reassurance from others.
- Needs Others to Assume Responsibility: Needs others to assume responsibility for most major areas of their life.
- Difficulty Expressing Disagreement: Has difficulty expressing disagreement with others because of fear of loss of support or approval.
- Difficulty Initiating Projects: Has difficulty initiating projects or doing things on their own (due to lack of self-confidence).
- Excessive Efforts to Get Nurturance: Goes to excessive lengths to obtain nurturance and support from others, to the point of volunteering to do things that are unpleasant.
- Fear of Being Alone: Feels uncomfortable or helpless when alone because of exaggerated fears of being unable to care for themselves.
- Urgent Relationship Search: Urgently seeks another relationship as a source of care and support when a close relationship ends.
Predisposing Factors
- Parenting Style: Parenting styles that foster and reward dependence, rather than promoting autonomy, can predispose to DPD.
- Genetics: Possible genetic link to co-occurring anxiety or mood disorders.
Diagnoses
- Primary Diagnoses: Ineffective coping (related to lack of self-confidence and excessive need for reassurance) and Risk for injury (related to excessive submission to others).
- Secondary/Supportive Diagnoses: Powerlessness (related to perception of inability to manage life events).
Nursing Interventions
- Promote Autonomy: The nursing plan must encourage the client to make their own decisions regarding their care (e.g., choice of clothing, unit activities) to foster self-reliance.
- Assertiveness Training: Help the client identify situations where they need to take responsibility and teach them assertiveness skills to express opinions and disagreement appropriately.
- Avoid Rescue Behavior: The nurse must avoid fostering or participating in the client’s dependent behavior; resist the urge to “rescue” the client.
- Gradual Increase in Responsibility: Start with small tasks the client can successfully complete and gradually increase the responsibility required.
9.3 OBSESSIVE-COMPULSIVE PERSONALITY DISORDER (OCPD)
- Definition: A pervasive pattern of preoccupation with orderliness, perfectionism, and mental and interpersonal control, at the expense of flexibility, openness, and efficiency, beginning by early adulthood.
- Epidemiological Statistics: Estimated prevalence is approximately 2.1% to 7.9%, potentially making it the most common personality disorder. It is diagnosed twice as often in males as in females.
- Key Distinction: OCPD is ego-syntonic (the client views their perfectionism as desirable) and does not involve true obsessions and compulsions (e.g., ritualistic handwashing to neutralize anxiety) like obsessive-compulsive disorder (OCD), which is ego-dystonic.
Clinical Picture: Characteristics
- Preoccupation with Rules: Is preoccupied with details, rules, lists, order, organization, or schedules to the extent that the major point of the activity is lost.
- Perfectionism Interferes with Task Completion: Perfectionism that interferes with task completion (e.g., unable to finish a project because self-standards are not met).
- Excessive Devotion to Work: Is excessively devoted to work and productivity to the exclusion of leisure activities and friendships.
- Inflexibility and Stubbornness: Is rigid and stubborn, often overly conscientious, scrupulous, and inflexible about matters of morality, ethics, or values.
- Hoarding: Is unable to discard worn-out or worthless objects even when they have no sentimental value.
- Reluctance to Delegate: Is reluctant to delegate tasks or to work with others unless they submit exactly to the person's way of doing things.
- Miserly Spending: Adopts a miserly spending style toward both self and others; money is viewed as something to be hoarded for future catastrophes.
Predisposing Factors
- Psychological: Psychoanalytic theory views OCPD as fixation at the anal stage of development (ages 1 to 3), focusing on control issues.
- Family Influence: Parental control and over-control, characterized by overly critical, demanding standards, and conditional approval.
Diagnoses
- Primary Diagnoses: Impaired social interaction (related to rigidity and preoccupation with rules) and Anxiety (related to inability to tolerate uncertainty or imperfection).
- Secondary/Supportive Diagnoses: Ineffective coping (related to perfectionism that prevents task completion).
Nursing Interventions
- Allow Control: Allow the client to maintain a reasonable amount of control over their routine as long as it does not interfere with the therapeutic milieu.
- Schedule Flexibility: Encourage the client to schedule leisure and social activities as a deliberate part of their routine to counterbalance their work-devotion.
- Avoid Power Struggles: Avoid engaging in power struggles over trivial details. Use rational thought and logic to calmly help the client see the need for change.
- Cognitive Restructuring: Help the client recognize that their excessive rigidity is counterproductive and that minor mistakes do not lead to catastrophic outcomes.
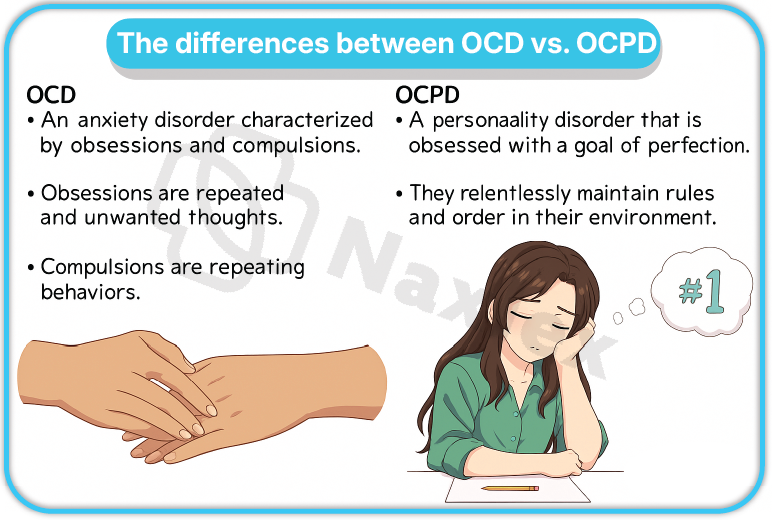
Nursing Insights
- OCPD vs. OCD: A crucial distinction for the RN is that Obsessive-Compulsive Personality Disorder (OCPD) is characterized by traits (perfectionism, rigidity, orderliness) that the individual values and considers helpful (ego-syntonic).
- Conversely, Obsessive-Compulsive Disorder (OCD) involves true obsessions (recurrent, intrusive thoughts) and compulsions (repetitive behaviors) that the individual finds distressing and wants to eliminate (ego-dystonic).
- The client with OCPD rarely presents for treatment unless a co-occurring disorder (like depression or anxiety) develops, or their rigidity causes severe occupational distress.
Risk Factors for Personality Disorders
- The development of personality disorders is multifactorial, stemming from the interplay of genetic, neurobiological, psychological, and environmental influences.
Genetic and Biological Risk Factors
-
- Family History: Having a first-degree relative with a personality disorder or a related mental illness (e.g., schizophrenia, mood disorders) significantly increases risk.
- Temperament: Inherited temperamental traits, such as high novelty-seeking (linked to Cluster B), low harm-avoidance, and emotional hypersensitivity, are early biological markers.
- Neurochemical Imbalance: Dysregulation of key neurotransmitter systems, especially serotonin (impulsivity, aggression, mood instability) and dopamine (cognitive-perceptual distortions), contributes to symptom expression.
- Brain Structure/Function: Deficits in the prefrontal cortex (executive function, impulse control) and hyperactivity/dysregulation of the amygdala (emotional processing, fear response) are strong risk factors, particularly for Borderline and Antisocial PDs.
Psychosocial and Environmental Risk Factors
-
- Childhood Trauma: Experiencing physical, sexual, or emotional abuse or neglect is a profound risk factor, particularly for Borderline PD, where up to 70% of clients report a history of abuse.
- Invalidating Environment: Growing up in an environment where a child's feelings are consistently minimized, dismissed, or punished (invalidated) impairs the ability to learn effective emotional regulation.
- Parenting Style: Inconsistent, overly authoritarian, or overly permissive parenting styles can fail to establish clear behavioral limits or foster healthy attachment.
- Poverty and Violence: Exposure to chronic socioeconomic stress, community violence, and parental substance use increases vulnerability.
- Impaired Attachment: Disrupted or insecure attachment to primary caregivers inhibits the development of mentalization (the capacity to understand one's own and others' behavior in terms of underlying mental states, such as feelings, beliefs, and desires).
Treatment for Personality Disorders
- Treatment for personality disorders is complex, often requiring a long-term, multimodal approach focused on modifying deeply ingrained maladaptive patterns. Pharmacological agents primarily treat co-morbid symptoms, while psychotherapy is the cornerstone of treatment.
Psychotherapy
-
- Dialectical Behavior Therapy (DBT):
- Gold Standard for Borderline Personality Disorder (BPD).
- Developed by Marsha Linehan, it combines cognitive and behavioral techniques with mindfulness practices.
- Focuses on teaching four core skills: Mindfulness, Distress Tolerance, Emotion Regulation, and Interpersonal Effectiveness.
- Utilizes a highly structured approach involving individual therapy, group skills training, phone coaching, and a consultation team.
- Schema-Focused Therapy (SFT):
- An integrative approach (combining CBT, attachment theory, Gestalt, and psychodynamic concepts) effective for BPD and other PDs (Narcissistic, Avoidant).
- Targets chronic, self-defeating schemas (early maladaptive patterns of thinking and relating) that originate in childhood trauma or unmet needs.
- Mentalization-Based Treatment (MBT):
- Focuses on improving the client's capacity to mentalize, or understand their own and others' behavior in terms of mental states.
- Particularly useful for BPD, where stress often leads to a temporary loss of mentalizing capacity.
- Cognitive Behavioral Therapy (CBT):
- Useful for modifying specific maladaptive cognitions (e.g., core beliefs of being unlovable in AvPD or schemas of grandiosity in NPD).
- Can help reduce rigidity and perfectionism in OCPD and manage anxiety across Cluster C.
- Psychodynamic Therapy: Focuses on exploring unconscious conflicts, early object relations, and patterns of projection/defense mechanisms to gain insight into current dysfunctional relationships.
- Dialectical Behavior Therapy (DBT):
Milieu Therapy
-
- Therapeutic Community: The environment itself is used as a tool for change, particularly in inpatient or partial hospitalization settings.
- Structure and Consistency: Provides a highly structured, predictable environment with clear, enforced rules and expectations to counteract the chaos and impulsivity of Cluster B disorders.
- Peer Pressure: Utilizes the therapeutic power of the peer group to provide feedback on behaviors and hold members accountable, which is often more effective than staff confrontation for disorders like ASPD.
- Immediate Feedback: Facilitates the provision of immediate, non-judgmental feedback on maladaptive interpersonal behaviors as they occur, allowing for real-time practice of new skills.
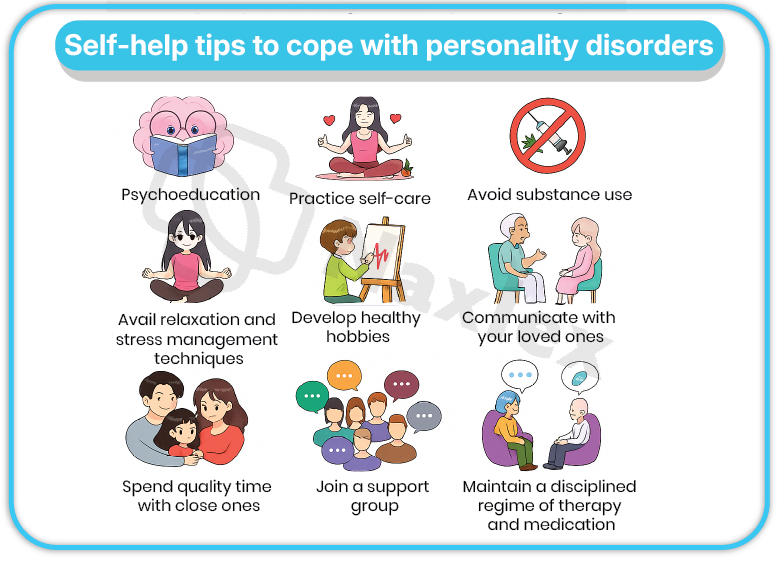
Comorbidity and Differential Diagnosis
Personality disorders rarely occur in isolation and are frequently complicated by co-occurring Axis I disorders, leading to increased symptom severity, poor treatment outcomes, and higher rates of suicide.
- Cluster A (PPD, Schizoid, Schizotypal): High comorbidity with Substance Use Disorders and other Psychotic Disorders (Schizotypal is highest risk for developing Schizophrenia).
- Cluster B (BPD, ASPD, HPD, NPD):
- BPD: Highest comorbidity with Major Depressive Disorder, Bipolar Disorder, Post-Traumatic Stress Disorder (PTSD), and Substance Use Disorders.
- ASPD: Nearly universal comorbidity with Substance Use Disorders and Gambling Disorder.
- Cluster C (AvPD, DPD, OCPD): High comorbidity with Anxiety Disorders (especially Social Anxiety Disorder in AvPD, and Generalized Anxiety Disorder in DPD) and Major Depressive Disorder.
Differential Diagnosis
- The key to differential diagnosis is determining whether the client's symptoms are pervasive, stable, and rigid (Personality Disorder) or episodic and distinct from their usual functioning (Other Axis I/II Disorder).
|
Personality Disorder Feature |
Differential Diagnosis |
Key Distinguishing Feature |
|
Pervasive Suspicion (PPD) |
Delusional Disorder (Persecutory Type) |
PPD has ideas of reference and pervasive distrust; Delusional Disorder involves a fixed, non-bizarre delusion that is held with absolute conviction. |
|
Social Isolation (Schizoid) |
Social Anxiety Disorder (SAD) |
Schizoid clients prefer isolation and lack interest in others (egosyntonic); SAD clients want relationships but avoid them due to fear (egodystonic). |
|
Emotional Lability, Impulsivity (BPD) |
Bipolar Disorder (Type II) |
BPD mood shifts are typically triggered by interpersonal events and last hours, not days/weeks; Bipolar mood shifts are spontaneous, sustained, and less reactive. |
|
Perfectionism (OCPD) |
Obsessive-Compulsive Disorder (OCD) |
OCPD is egosyntonic (viewed as helpful trait, without true obsessions/compulsions); OCD is egodystonic (intense anxiety from intrusive obsessions/compulsions). |
|
Antisocial Behavior (ASPD) |
Conduct Disorder (CD) |
CD is the prerequisite diagnosis before age 15; ASPD is the manifestation after age 18. |
Nursing Care Process for Personality Disorders
14.1. Assessment
- Comprehensive History: Obtain a detailed history of the client's past behavior, focusing on impulse control, relationship patterns (especially splitting and boundary violations), history of self-harm/suicide attempts, and use of defense mechanisms.
- Objective Data: Observe behavior during interactions:
- Cluster A: Suspiciousness, social withdrawal, flat affect.
- Cluster B: Manipulative behavior, excessive demandingness, seductive language, intense emotional lability, history of multiple physical injuries (NSSI, accidents).
- Cluster C: Excessive anxiety, rigidity, deferential (dependent) or perfectionistic behavior (OCPD).
- Risk Assessment: Crucial for BPD and ASPD. Assess for suicidal ideation, intent, plan, access to means, and history of self-mutilation or violence towards others.
- Identify Defense Mechanisms: Note the pervasive use of immature defenses like splitting (BPD), denial (ASPD), projection (PPD), and isolation of affect (OCPD).
14.2. Diagnoses
- Cluster A: Impaired Social Interaction, Disturbed Thought Process (PPD, STPD).
- Cluster B: Risk for Self-Mutilation/Self-Directed Violence (BPD), Risk for Other-Directed Violence (ASPD), Chronic Low Self-Esteem (NPD, HPD), Ineffective Emotional Regulation (BPD).
- Cluster C: Anxiety, Chronic Low Self-Esteem (AvPD, DPD), Ineffective Coping (OCPD).
14.3. Outcomes Identification for Each Personality Disorder
The overall goal is a reduction in maladaptive behaviors and an improvement in social and occupational functioning. Outcomes must be realistic, measurable, and behavioral.
|
Disorder (Cluster) |
Example Outcome |
|
PPD (A) |
Client will verbalize a reduction in suspicious ideation by acknowledging the nurse's consistency and trustworthiness within 2 weeks. |
|
Schizoid/Schizotypal (A) |
Client will participate in one self-care activity and one structured unit activity daily without undue anxiety by discharge. |
|
Borderline (B) |
Client will refrain from self-injurious behavior and utilize at least two DBT distress tolerance skills (e.g., TIPP, paced breathing) when feeling overwhelmed in 7 days. |
|
Antisocial (B) |
Client will adhere to all unit rules and contractual limits without incident or manipulation for 7 consecutive days. |
|
Narcissistic (B) |
Client will acknowledge one realistic personal limitation or error when completing a task by the end of the shift. |
|
Dependent (C) |
Client will independently make three minor decisions regarding their care or schedule daily without seeking reassurance. |
|
OCPD (C) |
Client will complete a designated task or assignment without excessive focus on minor details, prioritizing efficiency over perfection by the end of the week. |
14.4. Implementing Interventions
Promoting Safety
- Self-Harm/Suicide (BPD): Conduct rigorous and frequent safety checks, remove all harmful objects, institute one-to-one observation if risk is imminent, and constantly reassess risk factors. All threats or gestures must be taken seriously.
- Violence (ASPD, PPD): Observe for escalating agitation (e.g., pacing, clenched fists, increased paranoia). Reduce environmental stimuli. Ensure adequate physical space (maintain 2-3 arm lengths distance). Follow de-escalation protocols immediately upon identifying early signs of anger.
- Boundary Management: Maintain strict, consistent, and predictable professional boundaries with all clients, especially Cluster B, to prevent manipulation, splitting, and exploitation. All staff must be aware of the plan and consistently enforce limits.
De-Escalating
- Maintain Calm and Neutrality: Use a calm, low-pitched voice and non-threatening body posture. Do not argue, raise your voice, or show defensiveness, which can be perceived as a challenge.
- Acknowledge Feelings: Validate the client's feeling ("I see you are very angry right now") before addressing the behavior ("Throwing the chair is not permissible").
- Set Clear Limits: State the expectation and the consequence clearly, simply, and non-punitively ("If you cannot remain calm, you will need to take a time-out in your room").
- Offer Choices: Provide simple, limited choices when possible to allow the client to regain a sense of control ("Would you like to walk to the quiet room now, or in 5 minutes?").
- Medication: If verbal de-escalation fails, prepare for the administration of prescribed rapid-acting sedatives or tranquilizers (e.g., benzodiazepines, atypical antipsychotics) in collaboration with the medical team.
14.5. Coping Strategies/Mechanisms
- Defense Mechanisms: Individuals with personality disorders rely heavily on primitive or immature defense mechanisms, which shield them from anxiety but distort reality and impair interpersonal function.
|
Defense Mechanism |
Description |
Associated PDs |
Nursing Intervention |
|
Splitting |
The inability to view self and others as having both good and bad qualities simultaneously, resulting in idealization/devaluation. |
BPD (Cardinal Feature) |
Maintain staff consistency and immediately address efforts to pit staff against each other. |
|
Projection |
Attributing one's own unacceptable thoughts or feelings to another person. |
PPD (Blaming others for hostile thoughts), BPD |
Avoid defensiveness; gently focus on the client's internal feelings first. |
|
Denial |
Refusal to accept reality or fact. |
ASPD (Denying responsibility or guilt for harm caused) |
Focus on behavioral consequences; avoid challenging denial directly (it can increase aggression). |
|
Passive Aggression |
Expressing aggression indirectly, often through procrastination, stubbornness, or inefficiency. |
OCPD, Dependent PD |
Gently confront the indirect hostility and encourage direct communication of needs or anger. |
|
Acting Out |
Expressing unconscious emotional conflicts or unacceptable impulses through action rather than reflection. |
BPD, ASPD, HPD |
Teach and reinforce alternative, verbal methods for expressing intense emotion. |
Summary
- Personality disorders are characterized by pervasive, inflexible, and maladaptive patterns of inner experience and behavior that cause significant distress or impairment, categorized into three clusters: Cluster A (Odd/Eccentric: Paranoid, Schizoid, Schizotypal), Cluster B (Dramatic/Erratic: Antisocial, Borderline, Histrionic, Narcissistic), and Cluster C (Anxious/Fearful: Avoidant, Dependent, Obsessive-Compulsive).
- Etiology is complex, involving neurobiological deficits (e.g., frontal lobe/amygdala dysfunction, serotonin imbalance) and profound environmental trauma (e.g., invalidation, abuse), particularly for BPD.
- Nursing care is highly challenging, requiring the consistent application of therapeutic boundaries and structure to manage the client's maladaptive defense mechanisms, such as splitting (BPD) and projection (PPD).
- The gold standard treatment for BPD is Dialectical Behavior Therapy (DBT), which focuses on enhancing mindfulness, emotion regulation, and interpersonal effectiveness skills.
- Safety is the paramount concern for Cluster B disorders, specifically managing the high risks of self-harm, suicide, and violence through continuous assessment and consistent, non-emotional limit-setting within a therapeutic milieu.
- The primary nursing goal is to help clients replace their deep-seated, often egosyntonic, maladaptive patterns with functional coping strategies, promoting autonomy in Cluster C, accountability in Cluster B, and reality-based socialization in Cluster A.
|
CLUSTER A (ODD OR ECCENTRIC) |
CRITERIA |
|
Paranoid Personality Disorder |
The person: |
|
Schizoid Personality Disorder |
The person: |
|
Schizotypal Personality Disorder |
The person: |
|
CLUSTER B (DRAMATIC, ERRATIC AND EMOTIONAL) |
CRITERIA |
|
Antisocial Personality Disorder |
The person: |
|
Borderline Personality Disorder |
The person: |
|
Histrionic Personality Disorder |
The person: |
|
Narcissistic Personality Disorder |
The person: |
|
CLUSTER C (ANXIOUS AND FEARFUL) |
CRITERIA |
|
Avoidant Personality Disorder |
The person: |
|
Dependent Personality Disorder |
The person: |
|
Obsessive-Compulsive Personality Disorder |
The person: |
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Personality Disorders
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


