Please set your exam date
Perioperative Nursing Care
Study Questions
Practice Exercise 1
The nurse is preparing Mrs. Ogg for surgery for treatment of a ruptured spleen as the result of an automobile crash. The nurse knows that this type of surgery belongs in which of the following categories?
Explanation
Surgical procedures are classified by urgency (elective, urgent, emergency) and by extent/risk (minor vs major). Knowing these categories helps nurses anticipate surgical urgency, preparation needs, and potential risks.
Rationale for correct answer:
3. Major, emergency: This surgery involves significant risk, requires entry into the abdominal cavity, and is performed immediately to control hemorrhage and prevent death. It fits both the major and emergency categories.
Rationale for incorrect answers:
1. Minor, diagnostic: Minor diagnostic procedures are usually planned, low-risk, and involve minimal tissue disruption (eg, biopsy, endoscopy).
2. Minor, elective: Elective surgeries are scheduled in advance and are not life-saving (eg, hernia repair, cosmetic procedures).
4. Major, palliative: Palliative procedures aim to relieve symptoms without curing (eg, debulking tumors).
Take home points:
- Major surgery involves significant tissue disruption and higher risks.
- Emergency surgery is unplanned, done immediately, and lifesaving.
A group of students are reviewing the purposes of general anesthesia in preparation for a test. The students demonstrate a need for additional study when they identify which of the following as a purpose?
Explanation
General anesthesia causes a reversible loss of consciousness along with analgesia, amnesia, muscle relaxation, and suppression of reflexes. It is distinct from local/regional anesthesia, which only blocks sensation in a specific body part without affecting consciousness.
Rationale for correct answer:
4. Localized loss of sensation: This is the purpose of local or regional anesthesia, not general anesthesia. Students identifying this as a purpose of general anesthesia show a knowledge gap.
Rationale for incorrect answers:
1. Loss of consciousness: General anesthesia induces complete unconsciousness, rendering the patient unaware of pain and surroundings.
2. Relaxation of skeletal muscles: General anesthesia provides muscle relaxation, which facilitates intubation and surgical manipulation.
3. Reduction of reflex action: It suppresses reflexes (like gag or cough reflex) to allow safe surgical and anesthetic procedures.
Take home points:
- General anesthesia- unconsciousness, amnesia, analgesia, reflex suppression, and muscle relaxation.
- Local anesthesia- localized numbness without loss of consciousness; confusing the two indicates a gap in understanding.
A nurse has been asked to witness a patient signature on an informed consent form for surgery. For which one of these patients would the document be valid?
Explanation
Valid informed consent requires capacity (ability to understand and decide), comprehension (understands risks/benefits/alternatives), and voluntariness (not coerced). A witness’s role is to verify the signature is the patient’s and that the patient appears to sign voluntarily and knowingly.
Rationale for correct answer:
2. A 45-year-old patient who is oriented and alert: Adult, alert, and oriented patients who demonstrate understanding and voluntariness have capacity to consent; the witness may attest the signature.
Rationale for incorrect answers:
1. A 92-year-old patient who is severely confused: Severe confusion indicates lack of decision-making capacity; such a patient cannot give valid informed consent. A legal surrogate or court order is required.
3. A 10-year-old patient who is oriented and alert: Minors generally cannot provide legal consent, except in specific legal exceptions (e.g., emancipated minor, some treatment categories).
4. A 36-year-old patient who has had a narcotic premedication: Recent narcotic premedication can impair consciousness, judgement, and comprehension. If the patient is sedated or cognitively impaired by meds, consent is not valid.
Take home points:
- Only witness consent when the patient is an adult who is alert, oriented, and not impaired by drugs, confusion, or intoxication.
- Minors and cognitively impaired patients generally cannot consent
Practice Exercise 2
Which test is the best resource for determining the preoperative status of a client’s liver function?
Explanation
The liver metabolizes many anesthetics and produces clotting factors; impairment increases risks of bleeding, drug toxicity, infection, and poor wound healing. Preoperative evaluation should screen for hepatocellular injury (ALT/AST), cholestasis/excretory problems (bilirubin), and synthetic function/coagulation (albumin, PT/INR).
Rationale for correct answer:
3. ALT, AST, bilirubin: ALT/AST reflect hepatocellular injury; bilirubin reflects excretory function/cholestasis. Together they are the best single-resource panel here to judge preop liver status and prompt further testing
Rationale for incorrect answers:
1. Serum electrolytes: Assess fluid/electrolyte and acid–base balance (e.g., Na⁺, K⁺, Cl⁻, HCO₃⁻). While severe cirrhosis can cause hyponatremia, electrolytes are not specific measures of hepatic function.
2. BUN, Creatinine: Primarily evaluate renal function and drug clearance by the kidneys. Important preoperatively, especially if combined liver-kidney disease is suspected, but these do not measure liver injury.
4. Serum albumin: A marker of hepatic synthetic function and nutritional status. Useful for chronic liver disease severity, but with a long half-life (~20 days) it’s less sensitive to acute changes and, alone, gives an incomplete picture of preop liver risk.
Take home points:
- For preop liver assessment, prioritize a liver panel (ALT, AST, bilirubin ± ALP/GGT) and add PT/INR and albumin to gauge synthetic function.
- Abnormal liver tests change surgical/anesthetic risk and management; investigate and optimize before proceeding when possible.
A client who is having a mastectomy expresses sadness about losing her breast. Based on this information, the nurse would identify that the client is at risk for which nursing diagnosis?
Explanation
Grieving is a process that includes sadness, yearning, and adjustment as the person works through what the loss means for identity and role. Disturbed body image is a different concept: it implies a disturbed self-image often accompanied by shame or revulsion.
Rationale for correct answer:
2. Grieving: A normal reaction to an expected significant loss (loss of a breast, body image, role, or sense of femininity). Sadness expressed about losing the breast is characteristic of grieving.
Rationale for incorrect answers:
1. Disturbed Body Image: Defined as confusion in the mental picture of oneself; commonly shows shame, embarrassment, guilt, or revulsion about appearance.
3. Fear: Characterized by dread, alarm, or apprehension about threats; the client’s sadness does not primarily indicate fear.
4. Ineffective Coping: Shown by inability to ask for help, inappropriate defenses, or failure to meet role expectations.
Take home points:
- Grieving is a normal response to anticipated loss.
- Distinguish grief (sadness, adjustment) from disturbed body image (shame/repulsion) and from ineffective coping (maladaptive behaviors).
Which statement by the client indicates that the preoperative teaching regarding gallbladder surgery has been effective?
Explanation
Preoperative teaching focuses on safety priorities that reduce immediate perioperative risks. NPO status is fundamental because a full stomach increases the risk of aspiration during induction of anesthesia. Other instructions that prevent complications: deep-breathing and coughing to prevent pulmonary complications, calf exercises to reduce DVT risk, and correct understanding of anticoagulant management.
Rationale for correct answer:
4. “The nurse showed me how to contract and relax my calf muscles.” This demonstrates effective teaching about preventing venous stasis and DVT, which are key postoperative complications, especially after abdominal surgery.
Rationale for incorrect answers:
1. “I cannot eat or drink anything after midnight.” Current ASA (American Society of Anesthesiologists) guidelines allow clear fluids up to 2 hours before elective surgery and a light meal up to 6 hours before.
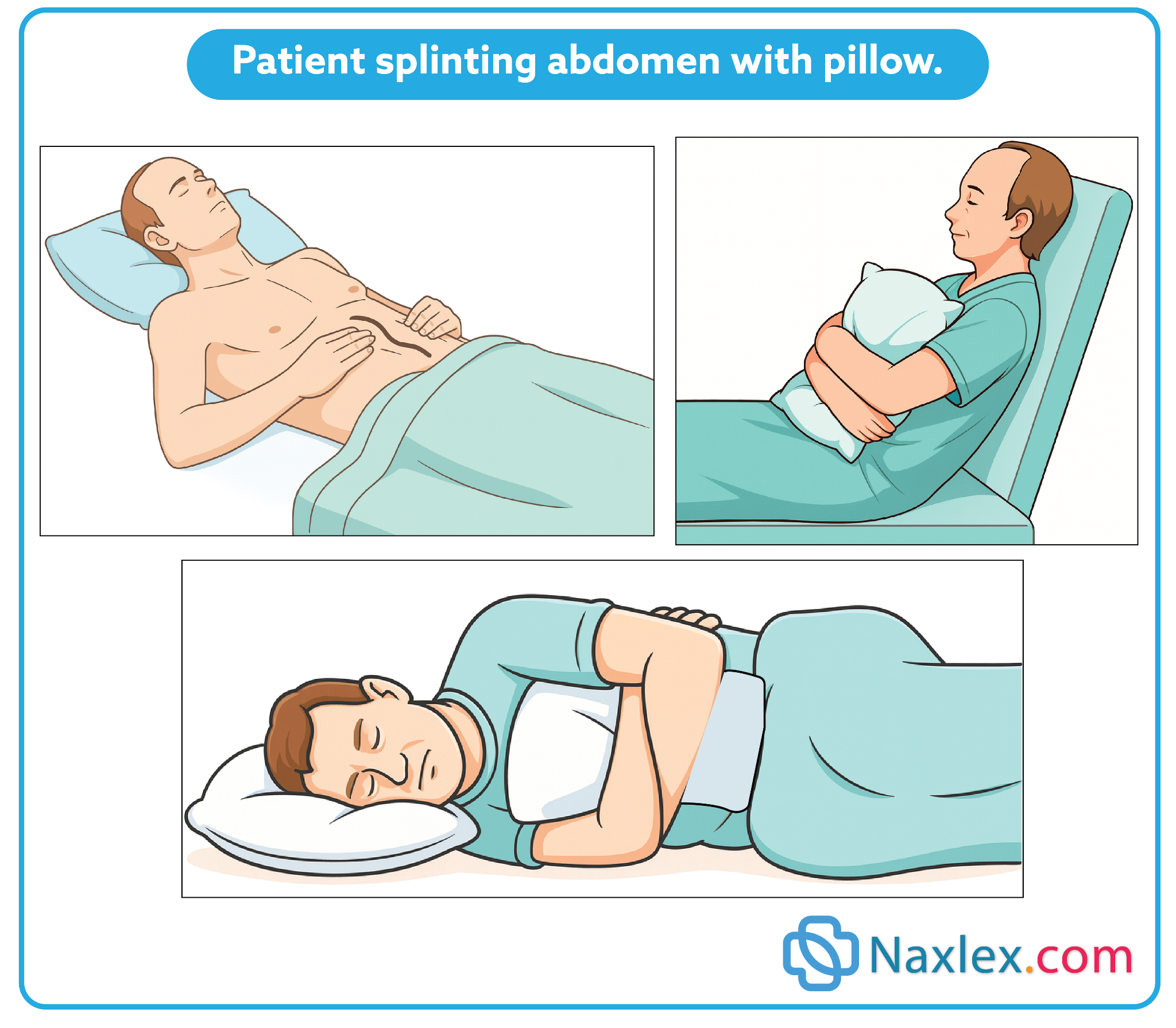
2. “I’m not going to cough after surgery because it might open my incision.” Clients are taught to cough and deep-breathe postoperatively to prevent atelectasis and pneumonia. Nurses also teach splinting the incision with a pillow or hands to support the wound during coughing.
3. “I might have a stroke if I stop taking my anticoagulant.” Anticoagulants are usually stopped several days before surgery to minimize bleeding risk. The client’s statement reflects misunderstanding of perioperative medication management.
Take home points:
- Best indicator of effective preoperative teaching: patient verbalizes accurate prevention strategies.
- NPO guidelines have evolved - clear fluids may be allowed closer to surgery, so “NPO after midnight” is not always correct.
A nurse is teaching a man scheduled to have same day surgery. Which teaching method would be most effective in preoperative teaching for ambulatory surgery?
Explanation
Ambulatory surgery requires focused, practical preoperative teaching because patients are admitted and discharged quickly. The most effective single method is clear, concise written instructions that the patient can take home and consult after discharge.
Rationale for correct answer:
4. Written instructions: For same-day/ambulatory surgery, clear written instructions (NPO, meds, arrival time, postop care, warning signs, contact info) are most effective because patients can refer to them at home when implementing postoperative care and when questions arise.
Rationale for incorrect answers:
1. Lectures are passive and may provide too much information at once; they are less practical for brief, preop teaching when the patient needs concise, usable instructions.
2. Discussion is interactive and good for clarifying questions, but in the ambulatory setting time is limited and patients may not remember verbal details once they leave.
3. Audiovisuals: Videos can efficiently demonstrate techniques and reinforce key points, but the patient still usually needs a written summary to take home for later reference.
Take home points:
- Provide concise written instructions for same-day surgery.
- Include: NPO rules, meds, activity limits, warning signs, follow-up.
Which assessment questions should the nurse ask a preoperative patient preparing for surgery? Select all that apply
Explanation
The nurse’s role is to gather data that may influence anesthesia, surgical safety, and recovery. Priority questions target pain, medications, allergies, and lifestyle factors that alter healing and anesthesia response.
Rationale for correct answers:
1. “Are you experiencing any pain?”: Pain assessment is essential because uncontrolled preoperative pain can complicate stress responses, recovery, and overall comfort.
4. “Do you have any medication allergies?”: Allergies must always be assessed to prevent life-threatening anaphylaxis during surgery. This includes medications, latex, and anesthesia-related agents.
5. “Do you use drugs and/or tobacco products?”: Smoking and drug use impair wound healing, increase anesthesia risks, and compromise cardiovascular and respiratory stability.
Rationale for incorrect answers:
2. “Do you exercise on a daily basis?” While exercise habits reflect general health, they are not a priority in the immediate preoperative assessment. The nurse must focus on factors that directly impact anesthesia and surgical risks.
3. “When do you regularly take your medications?”: Although medication timing is useful, the standard preoperative question focuses more on what medications the patient is taking, not when.
Take home points:
- Preoperative assessment should focus on factors that affect anesthesia safety and healing (medications, allergies, drug/tobacco use, current pain).
- Effective pre-op questioning prevents complications and ensures safe surgical planning.
A 72-year-old woman is taking several medications on a regular basis. Which of the following categories of drugs would be most likely to increase her surgical risk?
Explanation
Preoperative assessment must include a careful medication history because some drugs markedly alter surgical risk. Anticoagulants are especially important because they increase bleeding and may need to be stopped days before surgery or managed with bridging. Other drug classes (sedatives, opioids, laxatives, herbal supplements) also affect anesthesia and recovery - they may cause respiratory depression, hemodynamic instability, electrolyte imbalance, or drug interactions.
Rationale for correct answer:
1. Anticoagulants (warfarin, DOACs, heparin) increase perioperative bleeding risk and often require careful stopping/timing and possible bridging- they are a major concern in preoperative medication review.
Rationale for incorrect answers:
2. Antacids generally do not increase surgical risk; they are sometimes used preop to reduce gastric acidity/aspiration risk. They are not a primary source of perioperative complications.
3. Laxatives can cause dehydration or electrolyte disturbances if overused, which may affect anesthesia tolerance, but they are usually less likely than anticoagulants to directly increase surgical risk.
4. Sedatives: Chronic sedative use poses risks- respiratory depression, interactions, tolerance/withdrawal.
Take home points:
- Anticoagulants are the highest concern preoperatively due to bleeding risk; always clarify timing of last dose and plan perioperative management.
- Do a full med reconciliation; manage sedatives, electrolytes, and interactions before surgery to reduce complications.
Practice Exercise 3
The nurse assesses a postoperative client who has a rapid, weak pulse; urine output of less than 30 mL/h; and decreased blood pressure. The client’s skin is cool and clammy. What complication should the nurse suspect?
Explanation
The hemodynamic signs of hypovolemic shock in a postoperative patient - tachycardia with a weak (thready) pulse, decreasing blood pressure, reduced urine output (oliguria), and cool, clammy skin from peripheral vasoconstriction.
Rationale for correct answer:
2. Hypovolemic shock: Classic features are compensatory tachycardia with a rapid, weak pulse, hypotension as volume loss progresses, oliguria, cool/clammy pale skin from peripheral vasoconstriction, and altered mental status.
Rationale for incorrect answers:
1. Thrombophlebitis: Usually produces localized signs in the affected limb- pain, redness, warmth, swelling, a tender, cord-like vein.
3. Pneumonia: Presents with respiratory symptoms (cough, sputum, dyspnea), fever, tachypnea and focal lung signs on auscultation; it may cause systemic signs if severe -sepsis.
4. Wound dehiscence: Manifests with separation of incision layers, increased drainage, visible sutures/staples disruption, possible evisceration and local pain.
Take home points:
- Differentiate localized complications from systemic shock by focusing on systemic perfusion signs.
- The combination of rapid, weak pulse + hypotension + low urine output + cool, clammy skin is a red flag for hypovolemic shock.
The client is most likely to require the greatest amount of analgesia for pain during which period?
Explanation
Acute surgical pain is typically most intense in the early postoperative period - commonly within the first 24 to 48 hours - because residual anesthesia and short-acting intraoperative analgesics wear off and inflammatory nociception increases. Nurses should anticipate and proactively manage pain using multimodal analgesia.
Rationale for correct answer:
3. 12 to 36 hours after surgery: For many procedures the analgesic requirement is highest once residual anesthesia and immediate intraoperative analgesia have worn off and inflammatory pain processes are peaking - which frequently falls in the 12-36 hour window.
Rationale for incorrect answers:
1. Immediately after surgery: Some pain exists immediately, but many patients have residual anesthesia and receive intraoperative/early postoperative IV analgesia (PCA or bolus) in PACU.
2. 4 hours after surgery: This may be a high-pain period for some procedures as anesthetics wear off, but many studies and clinical guidelines report that the worst pain is most often in the broader early postoperative window (first 24-48 hours).
4. 48 to 60 hours after surgery: By this time most patients’ acute surgical pain has begun to decline; while some moderate pain may persist.
Take home points:
- Anticipate highest analgesic needs during the first 24–48 hours post-op and plan multimodal pain control accordingly.
- Early, effective pain control- scheduled nonopioids, regional techniques and rescue opioids- reduces complications (poor cough/incentive spirometry, delayed mobilization).
A nurse is caring for an obese patient who has surgery. The nurse monitors this patient for which of the following postoperative complications?
Explanation
Obesity changes physiologic responses to surgery and increases certain postoperative risks. Fatty tissue has relatively poor blood supply and oxygenation, which predisposes to wound infection and delayed healing. Obese patients also have higher rates of respiratory complications, venous thromboembolism, and technical difficulties during the operation.
Rationale for correct answer:
2. Impaired wound healing: Obesity is associated with poorer wound healing and higher wound-infection rates because adipose tissue is less vascular, surgical wound tension is greater, and obesity is often accompanied by comorbidities (eg, diabetes) that impede healing.
Rationale for incorrect answers:
1. Hunger is not a complication specifically associated with obesity after surgery; postoperative appetite varies and is influenced more by anesthesia, analgesics, and ileus than by body weight alone.
3. Hemorrhage: Obesity by itself is not the primary predictor for postoperative bleeding; technical difficulty can increase operative time or risk.
4. Gas pains: Gas pains (postop abdominal gas/discomfort) are common after abdominal surgery but are not specifically more likely because of obesity; they relate more to bowel manipulation, anesthesia, and immobility.
Take home points:
- Obese surgical patients are at increased risk for impaired wound healing and wound infection.
- Nursing priorities include close wound assessment, infection prevention, and measures that support tissue healing.
While assessing a patient in the PACU, the nurse notes increased wound drainage, restlessness, a decreasing blood pressure, and an increase in the pulse rate. The nurse interprets these findings as most likely indicating which of the following?
Explanation
In the immediate postoperative period, sudden or increasing wound drainage together with tachycardia, hypotension, oliguria, and mental status changes (anxiety, restlessness) strongly suggest hemorrhage and hypovolemic shock.
Rationale for correct answer:
4. Hemorrhage: Restlessness is an early sign of decreased cerebral perfusion; tachycardia and hypotension reflect compensatory and then decompensatory circulatory failure.
Rationale for incorrect answers:
1. Thrombophlebitis typically causes localized limb pain, redness, warmth, and swelling - not generalized hypotension, tachycardia, and increased drainage from a surgical wound.
2. Atelectasis presents with tachypnea, dyspnea, decreased breath sounds, and low-grade fever - it does not explain a sudden drop in blood pressure with increased wound drainage.
3. Infection usually develops later and is associated with localized redness, warmth, purulent drainage, and sometimes fever; acute hypotension and tachycardia with increased surgical site drainage point toward active bleeding rather than established infection.
Take home points:
Immediate actions when suspecting acute hemorrhage:
- maintain airway/breathing
- control visible bleeding
- increase IV access
- begin fluid/blood resuscitation per protocol
- notify the surgical team/rapid response.
A patient tells the nurse she is having pain in her right lower leg. How does the nurse assess for the presence of thrombophlebitis?
Explanation
Thrombophlebitis and deep-vein thrombosis often presents with localized pain, tenderness, warmth, and unilateral swelling of the calf or thigh. Nurses should perform focused limb assessment: inspect for erythema and asymmetry, palpate for warmth and tenderness, and document objective measurements (calf circumference at a fixed point) daily to detect changes.
Rationale for correct answer:
2. By documenting daily calf circumference measurements: Serial calf measurements (taken at the same spot on both legs) objectively detect increasing unilateral swelling - an important sign of thrombophlebitis/DVT.
Rationale for incorrect answers:
1. By palpating the skin over the tibia and fibula: Palpating over the bones doesn’t assess the soft-tissue signs of venous inflammation or thrombus.
3. By recording vital signs obtained four times a day: Vitals may show fever or tachycardia with complications, but they aren’t sensitive or specific for detecting early thrombophlebitis.
4. By noting difficulty with ambulation: Difficulty walking is nonspecific and may reflect pain from many causes; it’s useful to note but is not a reliable primary assessment for thrombophlebitis.
Take home points:
- Use objective, serial calf circumference measurements and compare with the opposite leg to detect swelling early.
- Look also for localized tenderness, warmth, redness, and any sudden change in the limb - these findings warrant immediate reporting and further evaluation.
Which postoperative intervention best prevents atelectasis?
Explanation
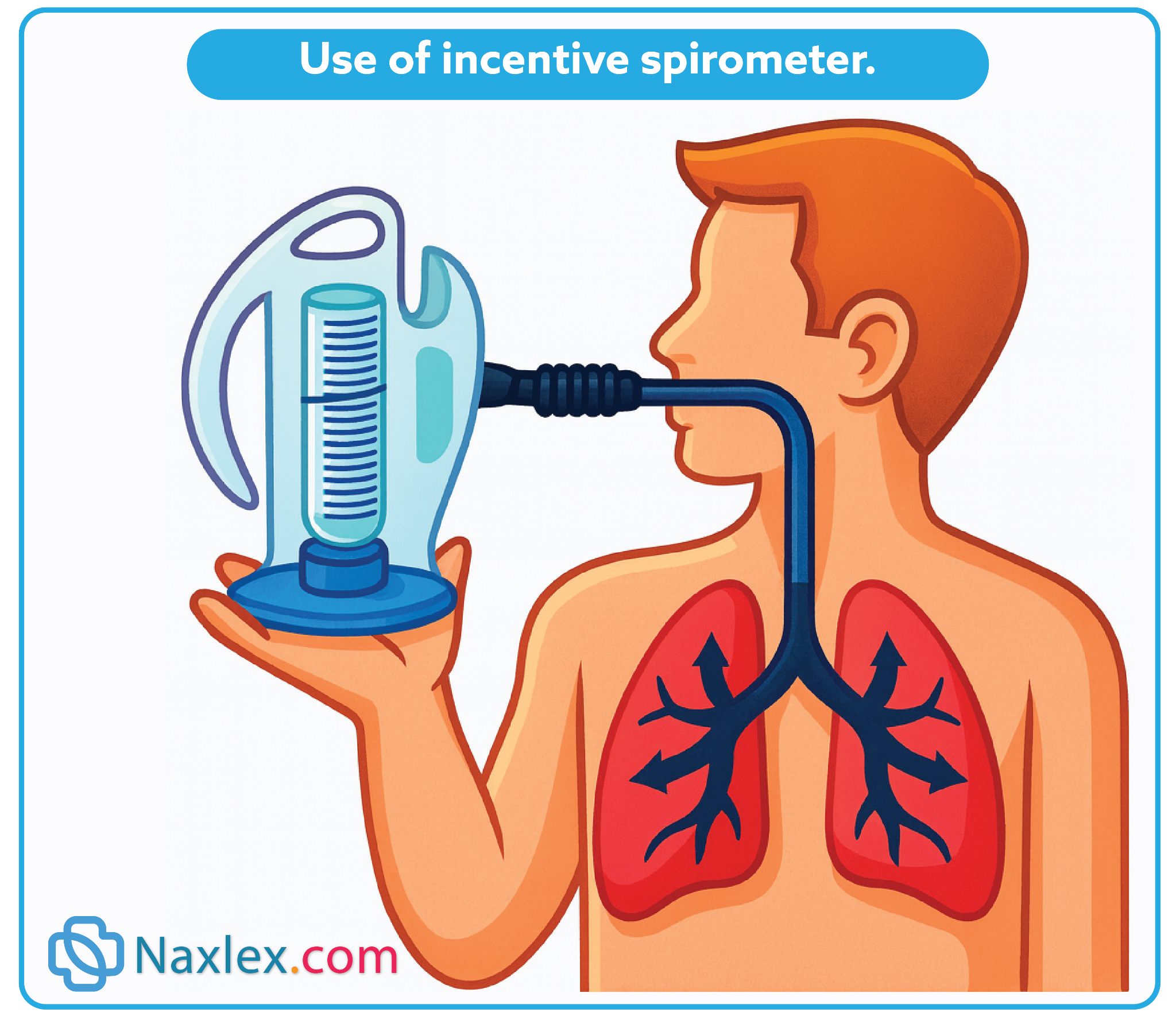
Atelectasis is a common postoperative complication caused by shallow breathing and immobility. Interventions such as incentive spirometry and deep breathing exercises are the most effective preventive measures.
Rationale for correct answers:
3. Use of the incentive spirometer: The incentive spirometer encourages deep breathing, lung expansion, and mobilization of secretions, directly preventing atelectasis after surgery.
Rationale for incorrect answers:
1. Use of intermittent compression stockings: Compression stockings prevent venous stasis and DVT, not atelectasis.
2. Heel-toe flexion: Heel-toe flexion promotes circulation in the lower extremities but does not prevent pulmonary collapse.
4. Abdominal splinting when coughing: Splinting provides support and reduces pain while coughing, but by itself it does not ensure full lung expansion as effectively as incentive spirometry.
Take home points:
- Incentive spirometry is the primary intervention to prevent atelectasis.
- Circulatory-focused interventions (compression stockings, leg exercises) address DVT, not respiratory complications.
Comprehensive Questions
A semiconscious client in the post anesthesia care unit (PACU) is experiencing dyspnea (difficulty breathing). Which action should the nurse perform first?
Explanation
In the PACU the nurse’s first priority is airway (A in ABCs). Once the airway is patent, the nurse can suction if needed, insert or maintain an appropriate airway adjunct, and administer oxygen or escalate care.
Rationale for correct answer:
4. Reposition the client to keep the tongue forward: For a semiconscious patient the immediate priority is to open and maintain a patent airway (head-tilt–chin-lift or jaw-thrust as appropriate) so air can move. This maneuver is quick and noninvasive.
Rationale for incorrect answers:
1. Place a pillow under the client’s head: A pillow may flex the neck and worsen upper airway obstruction from the tongue falling back. It does not reliably open the airway.
2. Remove the oropharyngeal airway: Unless the airway is known to be causing obstruction or eliciting a gag/vomiting reflex, removing an airway when it is actually helping patency can make the problem worse.
3. Administer oxygen by mask: Important, but not first if the airway is obstructed. Oxygen will not relieve hypoxia if airway patency is not established.
Take home points:
- Always address airway patency first in a dyspneic, altered patient.
- Don’t remove airway adjuncts unless they are known to be causing gagging or obstruction.
- If dyspnea persists after positioning, proceed to suction, insert or adjust airway adjuncts, and give oxygen.
The client’s postoperative orders state “diet as tolerated.” The client has been NPO. The nurse will advance the client’s diet to clear liquids based on which assessment? Select all that apply
Explanation
When advancing a postoperative patient from NPO to clear liquids, the nurse checks for signs the GI tract and protective reflexes have returned: no nausea/vomiting, presence of bowel sounds or passage of flatus, intact gag reflex, and stable vital signs.
Rationale for correct answer:
1. Does not complain of nausea or vomiting: Absence of nausea or vomiting reduces aspiration risk and indicates the patient is more likely to tolerate oral intake.
3. States passing flatus: Passing flatus is an objective sign of returning bowel motility (ileus resolving) and supports advancing diet to clear liquids.
Rationale for incorrect answers:
2. Pain level is maintained at a rating of 2-3 out of 10: Good pain control is desirable, but a moderate pain score alone doesn’t guarantee GI tract readiness or safe swallowing.
4. Ambulates with minimal assistance: Ambulation shows overall stability and helps GI motility, but it is not by itself a direct indicator that the GI tract can tolerate oral intake.
5. Expresses feeling “hungry”: Subjective and not sufficient. Hunger does not confirm bowel function or absence of aspiration risk and should not be the sole reason to advance diet.
Take home points:
- Advance to clear liquids when objective signs of GI function and tolerance are present.
- Subjective cues (feeling hungry) and general stability (ambulating) are helpful context but do not replace primary clinical indicators of GI readiness.
The nurse plans to remove the client’s sutures. Which action demonstrates appropriate standards of care? Select all that apply
Explanation
The priority is to remove nonabsorbable sutures without injuring newly formed tissue or introducing contamination. That means assessing the wound first, using appropriate technique and instruments, lifting the knot, cutting the stitch close to the skin, and extracting the suture so contaminated external material is not pulled back through the wound.
Rationale for correct answers:
2. Grasp the suture at the knot with a pair of forceps: Lift the knot gently with forceps to expose the loop, stabilize the stitch, and allow safe placement of scissors beneath the suture for cutting. This minimizes trauma to the wound edges.
3. Place the curved tip of the suture scissors under the suture as close to the skin as possible: Cutting close to the skin limits contamination and eases atraumatic removal.
5. Remove alternate sutures first: Removing every other suture first helps maintain some wound support and lets you check approximation/healing as you go; if edges separate, you can stop and notify the provider. If the wound is well healed, sometimes all may be removed at once.
Rationale for incorrect answers:
1. Use clean technique: Suture removal is usually a sterile procedure.
4.Pull the suture material that is visible beneath the skin during removal: You must not pull the contaminated visible external portion of the suture through underlying tissue- that would drag external contaminants into the wound.
Take home points:
- Cut close, pull carefully.
- Always cut the suture as close to the skin as possible and remove the suture in a way that prevents dragging contaminated external material back through subcutaneous tissue.
Mr. Ying is scheduled for surgery. He says to the nurse, “I am so frightened-what if I don’t wake up?” What would be the best response?
Explanation
Preoperative anxiety is common; patients need empathy and a safe space to express fears. The nurse’s best immediate response acknowledges the feeling and opens a conversation so underlying concerns (fear of death, anesthesia, pain, loss of control) can be explored, corrected, and managed. Therapeutic communication (open-ended invitation, active listening) improves trust.
Rationale for correct answer:
2. “Let’s talk about how you are feeling.” Invites the patient to express concerns, shows empathy, and lets the nurse assess the intensity and content of the fear.
Rationale for incorrect answers:
1. “You have a wonderful doctor.” Diverts attention from the patient’s feelings and gives a vague reassurance rather than exploring fear.
3. “Everyone wakes up from surgery!” False reassurance; minimizes the patient’s worry and may undermine trust.
4. “Don’t worry, you will be just fine.” Dismissive; it shuts down emotional expression instead of addressing it.
Take home points:
- Use open-ended, empathetic statements that invite expression rather than offering premature reassurance.
- Exploring fears lets you assess need for teaching, more explanation from anesthesia, or anxiolytic interventions-don’t dismiss or minimize.
A patient asks a nurse what a PCA pump does. The nurse explains that a PCA pump allows postoperative patients to:
Explanation
Patient-controlled analgesia (PCA) gives the patient autonomy to push a button to receive a preset dose of analgesic, commonly IV opioid, with programmed lockouts and limits to prevent overdose.
Rationale for correct answer:
4. Administer their own analgesics: PCA lets the patient self-administer preset doses (usually opioid or other analgesic) when needed, within safety limits.
Rationale for incorrect answers:
1. Be totally pain free: PCA improves timely pain control but does not guarantee total absence of pain; goals are acceptable pain relief and function.
2. Take unlimited amounts of medication: PCA devices are programmed with fixed dose, lockout interval, and maximum limits to prevent overdose.
3. Choose the type of pain medication: The clinician prescribes the medication and PCA settings; the patient cannot change the drug.
Take home points:
- PCA - patient-initiated analgesia within clinician-set dose and safety parameters.
- PCA can improve pain control and patient satisfaction but requires monitoring for sedation and respiratory depression and teaching the patient proper use.
Mr. Moreno has had a surgical procedure that necessitated a thoracic incision. The nurse anticipates that he will have a higher risk for postoperative complications involving which body system?
Explanation
Thoracic incisions limit chest wall excursion and make coughing painful, so patients breathe more shallowly and cannot clear secretions effectively. This predisposes them to atelectasis and postoperative pneumonia.
Rationale for correct answer:
1. Respiratory system: A thoracic incision (thoracotomy, thoracic surgery) impairs chest wall movement, causes pain with deep breathing and coughing, and often leads to shallow respirations and ineffective cough - all of which increase risk for atelectasis and pneumonia.
Rationale for incorrect answers:
2. Circulatory system: Major thoracic surgery can affect hemodynamics in some cases, but the most immediate and common postoperative complications after a thoracic incision are pulmonary.
3. Digestive system: Digestive complications are more commonly related to abdominal surgery. A thoracic incision does not directly impair bowel motility the way abdominal manipulation does.
4. Nervous system: Neurologic complications are not the principal concern specifically from a thoracic incision; while pain and anesthesia affect the nervous system, the primary system at direct risk is respiratory.
Take home points:
- After thoracic surgery prioritize respiratory assessment and interventions- incentive spirometry, splinting, analgesia, early mobilization.
- Pain control that permits deep breathing and coughing is essential to prevent atelectasis and pneumonia.
Gas pains are a common postoperative discomfort. Which of the following nursing actions implemented in the plan of care would be most likely to relieve gas pains?
Explanation
Postoperative gas pain commonly results from anesthetic effects, decreased bowel motility, swallowed air, and manipulation of the bowel. Promoting early and frequent ambulation, position changes, and encouraging passing flatus are the most effective nonpharmacologic measures.
Rationale for correct answer:
3. Encourage frequent ambulation: Ambulation stimulates intestinal motility and helps move trapped gas, reducing distention and discomfort. It’s a first-line, low-risk intervention.
Rationale for incorrect answers:
1. Cough and deep breathe every 2 hours: Coughing and deep breathing primarily prevent pulmonary complications (atelectasis) and do not directly relieve intestinal gas.
2. Maintain NPO status for 48 hours: Prolonged NPO is unnecessary for routine gas pain and may delay return of bowel function; early oral intake as tolerated and activity often help.
4. Take vital signs every 4 hours: Monitoring vitals is important for overall postop care but will not directly relieve gas pain.
Take home points:
- Early ambulation is the single most effective nursing intervention to relieve postoperative gas pain by stimulating bowel motility.
- Use multimodal measures - positioning, ambulation, analgesia to allow activity, and ordered medications such as simethicone.
Which of the following surgical patients is at a greater risk for alterations in body image?
Explanation
Body image refers to an individual’s perception of their physical self. Surgery that alters visible body parts (face, breasts, limbs) or sexual/reproductive organs carries the highest psychosocial impact. Nurses must anticipate these concerns, provide support, and involve counseling when needed.
Rationale for correct answer:
1. 19-year-old woman, facial laceration: Adolescents and young adults are particularly vulnerable to changes in body image because appearance and social acceptance are critical at this stage of psychosocial development.
Rationale for incorrect answers:
2. 42-year-old woman, gallbladder surgery: While scars may form, they are often small and hidden; adults in this age group generally have a more stable self-concept and body image compared to adolescents.
3. 14-year-old boy, fractured clavicle repair: Although body image is important in adolescence, clavicle repairs usually result in minimal visible long-term changes and full functional recovery.
4. 52-year-old man, inguinal hernia repair: Body image changes are minimal with this procedure, and psychosocial adaptation at this age tends to be less influenced by appearance.
Take home points:
- Visible surgical changes (especially on the face or reproductive areas) increase risk for disturbed body image.
- Age and developmental stage influence how strongly clients react to body image changes - adolescents and young adults are at greater risk.
Older adults often have reduced vital capacity as a result of normal physiologic changes. Which nursing intervention would be most important for the postoperative care of an older surgical patient specific to this change?
Explanation
Normal aging decreases lung elasticity, chest wall compliance, and vital capacity. These changes make older adults more prone to hypoventilation, atelectasis, and respiratory infections after anesthesia. Nursing care must focus on pulmonary hygiene: turning, coughing, deep breathing, and using incentive spirometry.
Rationale for correct answer:
2. Turn, cough, and deep breathe every 4 hours: Reduced vital capacity in older adults increases the risk of atelectasis and pneumonia postoperatively. Encouraging frequent deep breathing and coughing expands alveoli, promotes secretion clearance, and improves oxygenation.
Rationale for incorrect answers:
1. Take and record vital signs every shift: Vital signs help monitor overall stability but do not directly address the physiologic change of reduced vital capacity.
3. Encourage increased intake of oral fluids: Fluids are important for hydration and mucous membrane health, but they don’t directly improve vital capacity.
4. Assess bowel sounds daily: Monitoring bowel function is important after surgery, but it does not address the pulmonary risks related to decreased lung function.
Take home points:
- Older adults have decreased lung reserve, making pulmonary complications more likely after surgery.
- Frequent pulmonary exercises (turn, cough, deep breathe, incentive spirometry) are the most effective interventions to prevent atelectasis and pneumonia.
The nurse is explaining the rationale for performing leg exercises after surgery. Which reason would the nurse include in the explanation?
Explanation
After surgery, immobility increases the risk of venous stasis, leading to DVT and emboli. Preventive measures such as leg exercises, early ambulation, elastic stockings, and sequential compression devices are essential parts of postoperative nursing care.
Rationale for correct answer:
4. Increase venous return: Surgery and immobility increase the risk of venous stasis, which predisposes patients to deep vein thrombosis and pulmonary embolism. Leg exercises contract the muscles of the lower extremities, which act as a pump to improve circulation and venous return.
Rationale for incorrect answers:
1. Promote respiratory function: While respiratory function is an important concern postoperatively, leg exercises specifically target circulation in the lower extremities, not the lungs.
2. Maintain functional abilities: Early ambulation and mobility exercises are used to maintain muscle tone and prevent deconditioning.
3. Provide diversional activities: Leg exercises are not intended as recreation. While they may distract briefly, the primary purpose is physiological, not psychological.
Take home points:
- Leg exercises after surgery prevent venous stasis and thrombus formation by promoting blood flow and venous return.
- Patient education is critical - when patients understand why they need to do leg exercises, they are more likely to comply, reducing the risk of DVT and pulmonary embolism.
The nurse prepares a patient with type 2 diabetes for a surgical procedure. The patient weighs 112.7 kg (248 lb) and is 157.4 cm (5 feet, 2 inches) in height. Which factors increase this patient’s risk for surgical complications? Select all that apply
Explanation
Certain chronic conditions (diabetes, obesity, respiratory impairment) predispose clients to complications such as infection, poor healing, and respiratory compromise. Identifying these risks allows the nurse to implement preventive measures.
Rationale for correct answers:
1. Obesity increases surgical risk because excess adipose tissue reduces blood supply to tissues, impairs wound healing, and increases strain on the respiratory and cardiovascular systems. It also makes positioning and anesthesia management more difficult.
3. Delayed wound healing: Diabetes interferes with tissue perfusion and impairs immune response, increasing the risk of delayed wound healing and postoperative infections.
4. Ineffective vital capacity: Obesity can restrict chest expansion, reduce lung volume, and impair effective ventilation. This puts the client at higher risk for atelectasis and hypoxemia postoperatively.
Rationale for incorrect answers:
2. Prolonged bleeding time: There’s no evidence in the scenario that this client has a bleeding disorder. Prolonged bleeding time is a concern with anticoagulant therapy or platelet dysfunction, not specifically linked to this patient.
5. Immobility secondary to height: Height alone is not a risk factor for immobility or surgical complications. Immobility is more commonly associated with obesity, fractures, or neurologic impairment.
Take home points:
- Obesity and diabetes significantly increase surgical risks due to poor wound healing, infection risk, and respiratory limitations.
- Risk assessment guides pre- and post-op nursing care e.g., strict glucose control, pulmonary hygiene, infection prevention.
Communication between a nurse caring for a patient in the preoperative holding area and the circulating nurse in the operating room (OR) can best be enhanced by which of the following? Select all that apply
Explanation
Effective handoff communication reduces errors and ensures continuity of care. Tools like SBAR, active listening, and nonverbal cues are evidence-based methods to enhance safety in the perioperative setting.
Rationale for correct answers:
2.Using a standardized SBAR tool: SBAR (Situation, Background, Assessment, Recommendation) provides a structured, concise, and effective method for handoff communication, reducing errors.
3. Being responsive in using nonverbal communication techniques: Nonverbal cues such as nodding, eye contact, and attentiveness enhance understanding and ensure the receiver interprets the message accurately.
5. Listening to the OR nurse’s questions: Active listening ensures clarification, avoids misinterpretation, and allows for questions about critical client details.
Rationale for incorrect answers:
1.Documenting assessment findings in the medical record: Documentation is essential but does not ensure direct communication between nurses in different areas. Timely, verbal handoff is more effective for safe surgical care.
4. Giving specific information to a transport technician: Transport staff are not responsible for clinical handoff. Critical pre-op details must be directly communicated nurse-to-nurse.
Take home points:
- SBAR and active listening are gold standards for safe handoffs.
- Direct communication between responsible nurses is essential; documentation or delegation alone is not sufficient.
An 85-year-old patient returns to the inpatient surgical unit after leaving the PACU. Which of the following place the patient at risk during surgery? Select all that apply
Explanation
Older adults have predictable physiologic changes (pulmonary stiffness, reduced diaphragmatic movement, diminished airway reflexes, decreased renal perfusion, altered pharmacodynamics) that lower physiologic reserve and increase vulnerability to anesthesia and surgical stress.
Rationale for correct answers:
1. Stiffened lung tissue: Aging causes decreased lung elasticity and increased chest-wall stiffness, reducing pulmonary compliance and reserve. This increases the risk of hypoventilation, atelectasis, and postoperative pulmonary complications.
2. Reduced diaphragmatic excursion: Older adults often have weaker respiratory muscles and reduced chest-wall mobility, which limits diaphragmatic movement. This promotes shallow breathing and inability to clear secretions effectively.
4. Reduced blood flow to kidneys: Renal blood flow and glomerular filtration decline with age. Reduced renal perfusion decreases drug clearance and increases susceptibility to renal injury and fluid/electrolyte imbalances during and after surgery.
Rationale for incorrect answers:
3. Increased laryngeal reflexes: Aging typically reduces protective airway reflexes (gag/cough), which increases risk of aspiration.
5. Increased cholinergic transmission: Normal aging is associated with a decline in cholinergic neurons/transmission; increased cholinergic activity is not typical and would not explain common geriatric perioperative risks.
Take home points:
- Anticipate respiratory and renal vulnerabilities in elderly surgical patients.
- Many protective reflexes and neurotransmitter activities decline with age.
A nurse cares for a postoperative patient in the PACU. Upon assessment, the nurse finds the surgical dressing is saturated with serosanguineous drainage. Which two interventions are a priority? Select all that apply
Explanation
A saturated postoperative dressing with serosanguineous output and physiologic signs of compromise suggests active bleeding and evolving hypovolemia. Timely, systematic interventions can prevent progression to shock.
Rationale for correct answers:
1. Notify surgeon: Saturated dressing may indicate active bleeding; the surgeon must be informed immediately for orders (return to OR, exploratory measures) or further directives.
5. Reinforce the dressing: If a dressing is saturated, do not remove it (removing may disrupt clot); reinforce with additional sterile dressings and apply gentle pressure as ordered to help control external bleeding while arranging definitive care.
Rationale for incorrect answers:
2. Maintain the IV fluid infusion: Maintaining or increasing IV access/fluids preserves venous access for volume resuscitation or blood transfusion and helps stabilize hemodynamics while interventions are arranged.
4. Monitor the patient’s vital signs every 5 to 10 minutes: Frequent vital-sign monitoring detects hemodynamic deterioration early (tachycardia, hypotension, rising respiratory rate) and guides resuscitation decisions.
3. Provide 2 L/min oxygen via nasal cannula: Oxygen may be helpful if the patient shows hypoxia, but it does not stop bleeding or replace lost volume. It’s supportive care and not the highest-priority immediate action when active bleeding is suspected.
Take home points:
- Treat increasing wound drainage and hemodynamic changes as potential hemorrhage.
- Do not remove a saturated dressing unless specifically ordered.
- Reinforce over it and apply pressure; removing it may worsen bleeding and dislodge clots.
A patient who returned from surgery 3 hours ago following a kidney transplant is reporting pain at a 7 on a scale of 0 to 10. The nurse has tried repositioning with no improvement in the patient’s pain report. Unmanaged surgical pain can lead to which of the following problems? Select all that apply
Explanation
risk of complications. It reduces ventilation since the patient avoids deep breaths, leading to shallow breathing. Ineffective coughing due to pain results in retained pulmonary secretions, which predispose to atelectasis or pneumonia. Severe pain also reduces appetite by impairing gastrointestinal function.
Rationale for correct answers:
1. Delayed ambulation: Pain that is uncontrolled makes patients reluctant or unable to get out of bed. This can contribute to immobility complications such as deep vein thrombosis, pneumonia, or pressure injuries.
2. Reduced ventilation: Pain (especially abdominal or thoracic surgical pain) makes patients reluctant to take deep breaths. This can lead to shallow breathing, poor oxygen exchange, and hypoxemia. It increases the risk for respiratory complications.
4. Retained pulmonary secretions: Pain discourages effective coughing and deep breathing. As a result, secretions accumulate in the lungs, which can lead to atelectasis and secondary pneumonia.
5. Reduced appetite: Severe pain can activate stress responses and decrease gastrointestinal motility, leading to nausea, poor appetite, and delayed nutrition. Good pain control improves recovery by allowing earlier intake of food and fluids.
Rationale for incorrect answers:
3. Catheter-associated urinary tract infection: While UTIs are a postoperative risk, they are linked to indwelling catheter duration, not unmanaged pain. Pain control does not directly prevent or cause this complication.
Take home points:
- Poorly controlled pain impairs breathing, mobility, and nutrition.
- Effective pain management promotes faster recovery and prevents pulmonary and mobility complications.
Exams on Perioperative Nursing Care
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
To:
- Describe the surgical experience, including perioperative phases, classifications of surgery, types of anesthesia, informed consent and advance directives, and outpatient/same-day surgery.
- Conduct a preoperative nursing history and physical assessment to identify patient strengths as well as factors that increase risks for surgical and postoperative complications.
- Prepare a patient physically and psychologically for surgery.
- Identify assessments and interventions specific to the prevention of complications in the immediate and early postoperative phases.
- Use the nursing process to develop an individualized plan of care for the surgical patient during each phase of the perioperative period.
Introduction
Surgery may be done for a variety of reasons:
- to cure or minimize disease
- to diagnose the specific presence of a disease or condition
- to reconstruct or eliminate a defect
- to enhance form and function
- to prescribe appropriate postoperative treatment and prognosis
- to palliate, or offer comfort, when cure is not possible
- to follow up or monitor an incurable disease process
- to offer a preventative option when disease is inevitable, such as an elective, prophylactic mastectomy for a woman at high risk for breast cancer.
Surgery may be planned or unplanned, elective/optional or necessary, major or minor, and may involve any body part or system.
Nursing care provided for the patient before, during, and after surgery is called perioperative nursing.
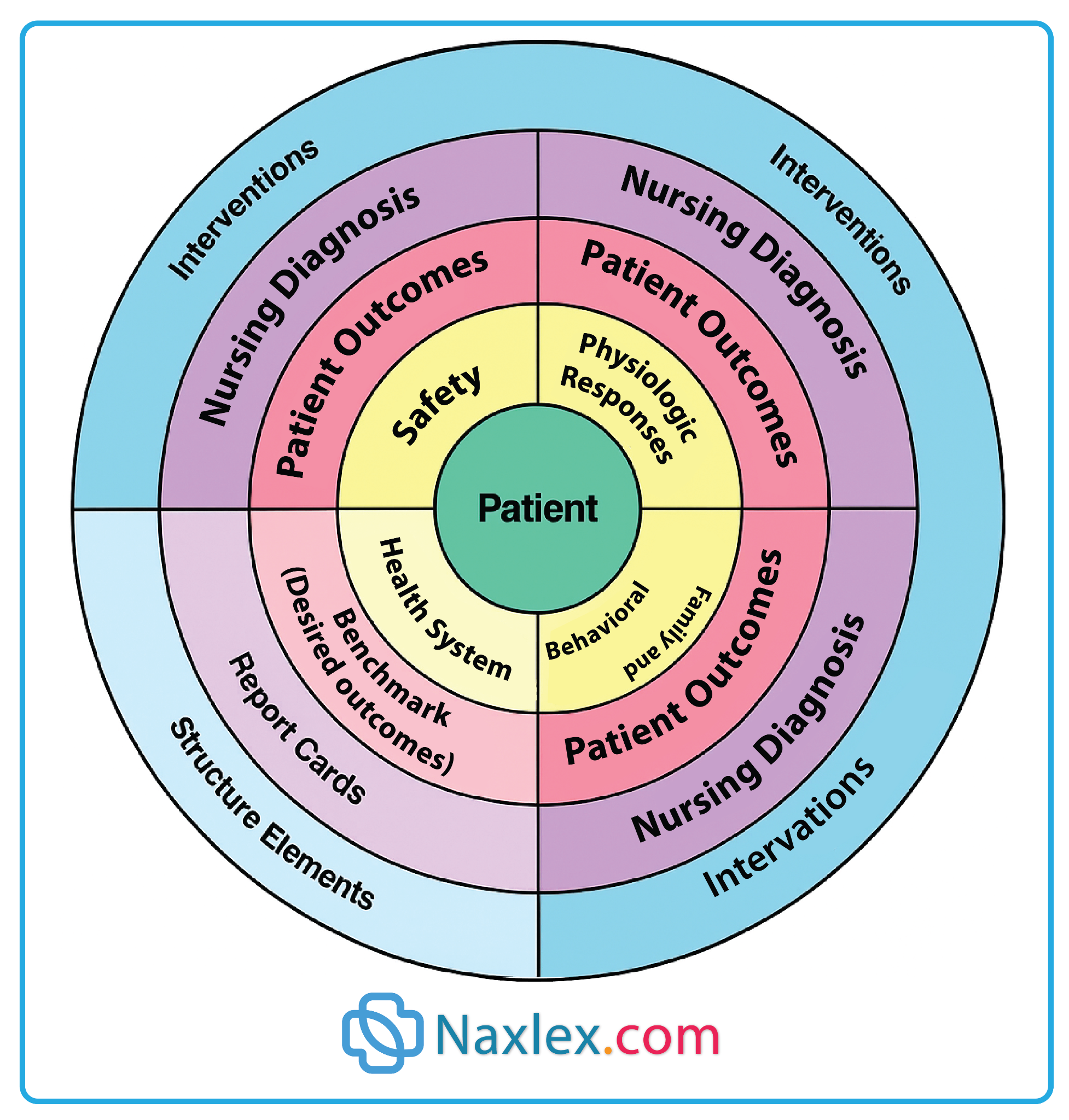
A conceptual model for perioperative nursing care is shown in the figure below. In this model, the patient is at the center of all care activities. Surrounding the patient are four domains. Three of these domains, safety, physiologic responses, and the patient and family behavioral responses, are critical for patient care. The fourth domain, health system, represents the structure elements and other system activities that must be present to support safe, effective, high-quality patient care.
The Surgical Experience
1.1 Phases of the Perioperative period
The patient who is having surgery progresses through several distinct phases, called the perioperative period. Include:
- The preoperative phase, beginning when the patient and surgeon mutually decide that surgery is necessary and will take place.
- The intraoperative phase, beginning when the patient is transferred to the OR bed, also called a table, until transfer to the postoperative recovery area.
- The postoperative phase, lasting from admission to the recovery area to complete recovery from surgery and the last follow-up physician visit. Further divided into:
- phase I - providing patient care from a totally anesthetized state to one requiring less acute nursing interventions
- phase II - preparing the patient for self or family care or for care in a phase III extended care environment
- phase III- providing ongoing care for patients requiring extended observation or intervention after transfer or discharge from phase I or II
1.2 Surgical procedure classification
Surgical procedures usually are classified according to urgency, risk, and purpose.
|
CLASSIFICATION OF SURGICAL PROCEDURES |
||
|
Classification |
Purpose |
Examples |
|
Based on Urgency Elective: Delay of surgery has no ill effects; can be scheduled in advance based on patient’s choice. Urgent: Usually done within 24-48 hours Emergency: Done immediately |
• To remove or repair a body part • To restore function • To improve health • To improve self-concept • To remove or repair a body part • To preserve or restore health • To prevent further tissue damage • To preserve life |
Elective: Tonsillectomy, hernia repair, cataract extraction and lens implantation
Urgent: Removal of gallbladder, coronary artery bypass, surgical removal of a malignant tumor
Emergency: Control of hemorrhage; repair of trauma, perforated ulcer, intestinal obstruction; tracheostomy |
|
Based on Degree of Risk Major: May be elective, urgent, or emergency Minor: Primarily elective |
To preserve life • To remove or repair a body part • To restore function • To improve or maintain health • To remove skin lesions • To correct deformities |
Major: Carotid endarterectomy, cholecystectomy, nephrectomy
Minor: Teeth extraction, removal of warts, skin biopsy, dilation and curettage, |
|
Based on Purpose
Diagnostic
Ablative
Palliative
Reconstructive
Transplantation
Constructive |
• To make or confirm a diagnosis
• To remove a diseased body part
• To relieve or reduce intensity of an illness; is not curative
• To restore function to traumatized or malfunctioning tissue • To improve self-concept
• To replace organs or structures that are diseased or malfunctioning
• To restore function in congenital anomalies |
Breast biopsy, laparoscopy, bronchoscopy, exploratory laparotomy Appendectomy, subtotal thyroidectomy, partial gastrectomy, colon resection, amputation
Colostomy, nerve root resection, debridement of necrotic tissue, balloon angioplasties, arthroscopy
Scar revision, plastic surgery, skin graft, internal fixation of a fracture, breast reconstruction
Kidney, liver, cornea, heart, joints
Cleft palate repair, closure of atrial–septal defect |
1.3 Anesthesia
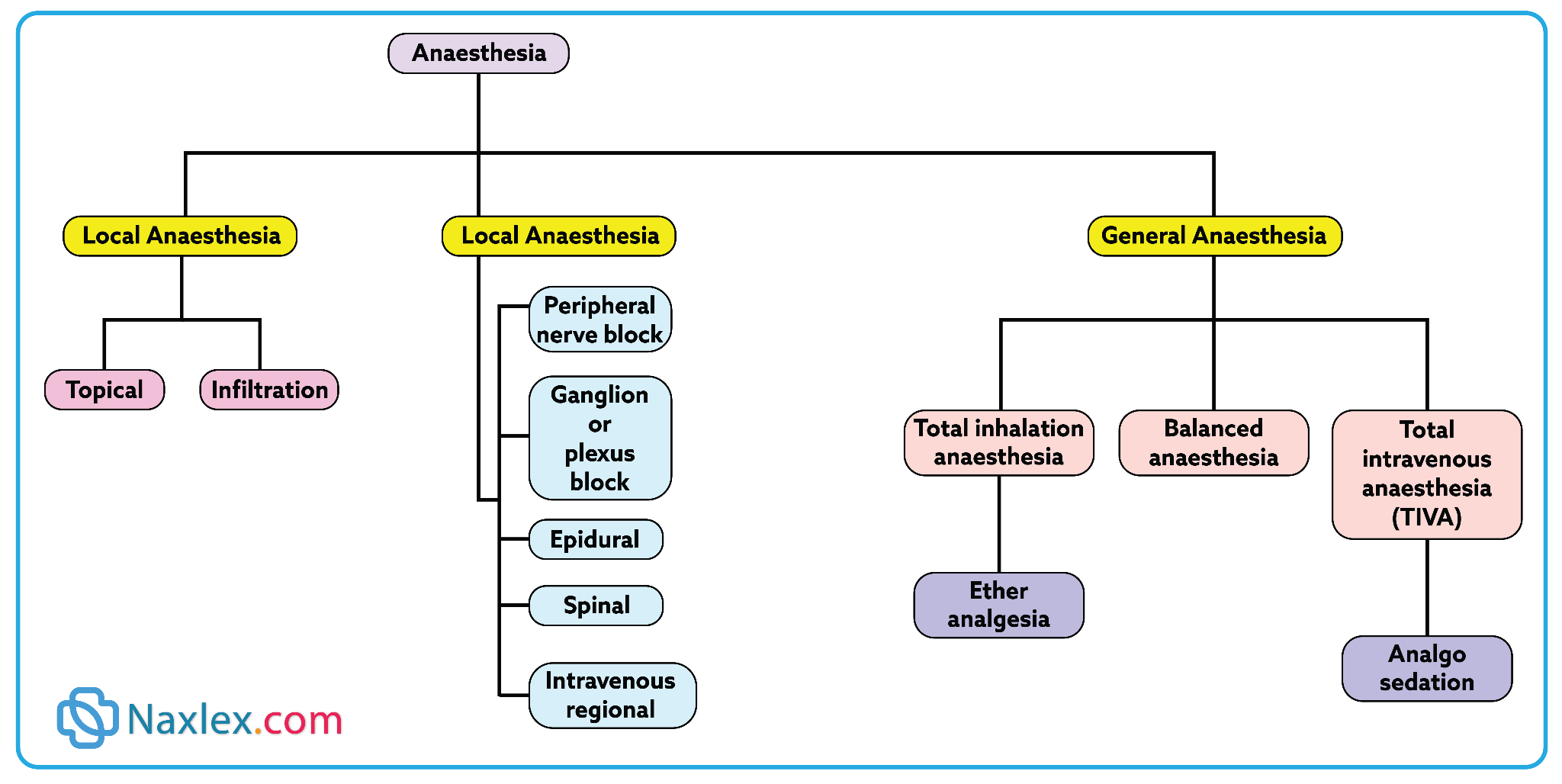
Anesthesia is a method and technique of making potentially uncomfortable interventions tolerable and safe. Anesthetic agents can be administered systemically, to the whole body, or regionally to block nerve conduction.
Anesthesiologists (medical doctors) or certified registered nurse anesthetists (CRNA) administer anesthetic agents while monitoring the patient’s physiologic response and maintaining homeostasis
General anesthesia:
General anesthesia involves the administration of drugs by the inhalation or intravenous (IV) route to produce central nervous system depression.
The three phases of general anesthesia are induction, maintenance, and emergence.
- Induction begins with administration of the anesthetic agent and continues until the patient is ready for the incision.
- Maintenance continues from this point until near the completion of the procedure.
- Emergence starts as the patient begins to awaken from the altered state induced by the anesthesia and usually ends when the patient is ready to leave the operating room
Regional Anesthesia:
Regional anesthesia occurs when an anesthetic agent is injected near a nerve or nerve pathway in or around the operative site, inhibiting the transmission of sensory stimuli to central nervous system receptors. Accomplished through:
- Nerve blocks are accomplished by injecting a local anesthetic around a nerve trunk supplying the area of surgery such as the jaw, face, and extremities
- Spinal anesthesia is achieved by injecting a local anesthetic into the subarachnoid space through a lumbar puncture, causing sensory, motor, and autonomic blockage.
- Caudal anesthesia is the injection of the local anesthetic into the epidural space through the caudal canal in the sacrum.
- Epidural anesthesia involves the injection of the anesthetic through the intervertebral spaces, usually in the lumbar region.
Topical and Local Anesthesia
Topical anesthesia is used on mucous membranes, open skin surfaces, wounds, and burns. Topical anesthetics may be sprayed, spread, or applied with a compress of drug-saturated gauze or cotton tipped applicators.
Local anesthesia is the injection of an anesthetic agent such as lidocaine, bupivicaine, or tetracaine to a specific area of the body.
Moderate Sedation/Analgesia
Moderate sedation/analgesia, also called conscious or procedural sedation, is used for short-term and minimally invasive procedures.
1.4 Informed Consent and Advance Directives
Informed consent:
Informed consent is the patient’s voluntary agreement to undergo a particular procedure or treatment after having received the following information by the procedural physician:
- Description of the procedure or treatment along with potential alternative therapies.
- The underlying disease process and its natural course
- Name and qualifications of the person performing the procedure or treatment.
- Explanation of the risks involved, including risk for damage, disfigurement, or death, and how often they occur.
- Explanation that the patient has the right to refuse treatment and that consent can be withdrawn.
- Explanation of expected outcome, recovery, and rehabilitation plan and course.
The responsibility for securing informed consent from the patient lies with the person who will perform the procedure. This is usually the physician. The nurse may sign as a witness, signifying that the patient signed the consent form without coercion and was alert and aware of the act. The patient always has the right to refuse treatment.
Consent forms are not legal if the patient is confused, unconscious, sedated, mentally incompetent, or a minor (as determined by state laws). Consent may be given in those instances by a parent, spouse, next of kin, or legal guardian.
Note: In emergency situations, the physician may obtain consent over the telephone or by court order
Advanced directives:
Advance directives, also legal documents, allow the patient to specify instructions for healthcare treatment should he or she be unable to communicate these wishes postoperatively.
Two common forms of advance directive include living wills and durable power of attorney for healthcare.
It is important to discuss and document the exact wishes of the patient and family members before surgery, especially related to resuscitation (do-not-resuscitate [DNR]).
1.5 Outpatient/Same-day Surgery
Surgical procedures performed in outpatient or same-day (also referred to as ambulatory) surgical settings have become common.
Typically, patients are admitted to the healthcare setting the morning of surgery. Allowing the patient to spend the night before surgery at home and to return to his or her own home to recover, reduces much of the stress associated with surgery.
Preoperative information for outpatient/same-day surgery
Provide verbal and written instructions for patients having outpatient/same-day surgery as follows:
- List medications routinely taken, and ask the physician which should be taken or omitted the morning of surgery.
- Notify the surgeon’s office if a cold or infection develops before surgery.
- List allergies, and be sure the operating staff is aware of these.
- Remove nail polish and do not wear makeup for the procedure.
- Leave all jewelry and valuables at home.
- Wear clothing that buttons in front; short-sleeved garments are better for surgery on the hands.
- Have someone available for transportation home after recovery from anesthesia.
Inform patient of:
- Limitations on eating or drinking before surgery, with a specific time to begin the limitations.
- When and where to arrive for the procedure, as well as the estimated time when the procedure will be performed.
Preoperative Care: The Nursing Process
Surgical patients may be of any age and at any point on the health–illness continuum. It is the nurse’s responsibility to identify factors that affect the risk of a surgical procedure.
Some of the desired outcomes that frame the plan of care for the surgical patient, state that the patient will meet the following goals:
- Be free from injury and adverse effects related to positioning, retained foreign objects, or chemical, physical, or electrical hazards
- Be free from infection
- Maintain fluid and electrolyte balance and skin integrity
- Maintain normal body temperature
- Be free from deep vein thrombosis (DVT, formation of a blood clot [“thrombus”] in a deep vein)
- Have their pain managed
- Demonstrate an understanding of the physiologic and psychological responses to the planned surgery
- Participate in a rehabilitation process following surgery
1.1 Assessing
Assessment of the surgical patient includes:
- Obtaining a health history and performing a physical assessment to establish a baseline data base
- Identifying risk factors and allergies that could pose surgical complications
- Identifying medications and treatments the patient is currently receiving
- Determining the teaching and psychosocial needs of the patient and family
- Determining postsurgical support and referral needs for recovery
HEALTH HISTORY:
Developmental Level
- Infants: increased surgical risk due to small blood volume, immature liver/kidneys, unstable temperature, small airway, increased risk of hypoxia/bronchospasm. Surgery postponed if respiratory infection present.
- Older adults: Physiologic changes decreased stress response, affect meds/anesthesia, slow wound healing. Chronic illnesses (e.g., CHF, diabetes) increased risk.
Medical History
- Cardiovascular disease - risk of bleeding, shock, arrhythmias, venous stasis.
- Respiratory disorders - risk of anesthesia depression, pneumonia, atelectasis.
- Renal/Liver disease - impaired drug metabolism/excretion, wound healing issues.
- Endocrine (especially Diabetes) - hypoglycemia, acidosis, delayed healing, CV risk.
Medications
- Risks:
- Anticoagulants - bleeding.
- Diuretics - electrolyte imbalance, resp. depression.
- Tranquilizers - hypotension with anesthesia.
- Steroids - withdrawal - Cardiovascular collapse.
- Antibiotics (mycins) - resp. paralysis with muscle relaxants.
- Oral antidiabetics (e.g., metformin) - renal failure with contrast dyes.
- Some meds continued with sips of water (e.g., cardiac/diabetic drugs).
Previous Surgeries
- Complications (e.g., malignant hyperthermia, latex allergy, pneumonia, thrombophlebitis) increased current surgical risk.
- Past experiences (positive/negative) influence anxiety and teaching needs.
- Children: most stressful- admission, tests, transport, recovery.
Nutritional Status
- Malnutrition - delayed healing, infection, fluid/electrolyte imbalance.
- Obesity - risks: DVT, GI issues, respiratory compromise (OSA, GERD, aspiration), delayed wound healing, infection.
Substance Use
- Alcohol: increased anesthetic/analgesic needs, drug complications.
- Illicit drugs: unsafe anesthesia interactions, poor IV access.
- Smoking: increased mucus, decreased ciliary action - pneumonia, hypoxia, poor wound healing.
ADLs & Occupation
- Exercise: improves surgical recovery.
- Rest/Sleep: essential for recovery.
- Occupation: may affect rehab, return-to-work needs.
Coping Patterns & Support Systems
- Surgery is a major psychological stressor.
- Common fears: anesthesia, death, pain, disfigurement, finances.
- Anxiety may show as anger, withdrawal, apathy.
- Nursing role: therapeutic communication, teaching, involve family, encourage support, address spiritual needs.
Sociocultural Needs
- Influenced by family beliefs, culture, economics.
- May affect views on surgery, pain expression, response to teaching, ambulation, diet.
- Care must be culturally sensitive (e.g., language, family roles, rituals).
PHYSICAL ASSESSMENT
Assessing the patient’s current physical status provides data for interventions to decrease surgical risk and potential postoperative complications.
|
PREOPERATIVE PHYSICAL ASSESSMENT |
|
|
Factors to Assess |
Questions and Approaches |
|
General survey |
• Note general state of health. • Note body posture and stature. • Take and record vital signs. |
|
Skin |
• Inspect skin for color, characteristics, and location and appearance of lesions. • Assess skin over bony prominences. • Palpate skin turgor |
|
Chest and lungs |
• Observe chest excursion and diameter and shape of thorax. • Auscultate breath sounds. • Palpate for any pain or tenderness. |
|
Cardiovascular system |
• Inspect for jugular vein distention. • Auscultate apical rate, rhythm, and character. • Auscultate heart sounds. • Assess for peripheral edema. • Palpate character of peripheral pulses. |
|
Abdomen |
• Ask time of last bowel movement. • Inspect abdominal contour. • Auscultate bowel sounds |
|
Neurologic system |
• Note orientation, level of consciousness, awareness, and speech. • Assess reflexes. • Assess motor and sensory ability. • Assess visual and hearing ability. |
|
Musculoskeletal system |
• Inspect and note joint range of motion. • Palpate muscle strength. • Assess ability to ambulate. |
Usual presurgical screening tests include chest x-ray, electrocardiography, complete blood count, electrolyte levels, and urinalysis.
1.2 Diagnosing
Nursing diagnoses for patients in the preoperative phase may be identified for various actual or potential problems for which a patient is at risk.
Many diagnoses reflect assessment of risk and are made to guide interventions for patient needs in the intraoperative and postoperative phases.
Examples of NANDA Nursing Diagnoses:
- Grieving
- Anxiety
- Risk for Infection
1.3 Outcome Identification and Planning
Outcomes are standard for all patients having surgery, but nursing interventions are designed to meet the priority needs of individual patients and situations.
Specific appropriate outcomes include that the patient:
- Is physically and emotionally prepared for surgery
- Demonstrates turning, coughing, and deep-breathing exercises
- Verbalizes understanding of postoperative pain management
- Maintains fluid intake and nutritional balance to meet needs
1.4 Implementing
1. Preparing the Patient Psychologically
a. Communication
- Surgery - life crisis - evokes anxiety/fear.
- Use therapeutic communication to build trust and psychological safety.
- Avoid false reassurance - denies patient’s emotions & blocks trust.
b. Teaching
- Preoperative teaching - decreases complications, decreases length of stay, increases recovery outcomes.
- Should be individualized (depends on timing, type of surgery, support system).
- Teaching checklist helps ensure thorough education.
Key Teaching topics:
- Surgical events & sensations
- What to expect before/during/after surgery.
- Sensations: dry mouth, sore throat, cool environment, drowsiness, bright lights, incision pain.
- Emphasize: “You are the most important person in the room.”
- Pain management
- Pain - normal but treatable; uncontrolled pain delays recovery.
- Assess every 2 hours after major surgery.
- Teach use of pain scales, request meds before pain becomes severe.
- Techniques: relaxation (deep breathing, music, imagery), PCA, TENS, local anesthetic pumps, epidurals.
- Low risk of addiction in postoperative use.
- Physical activities
- Prevent respiratory & circulatory complications.
- Must be taught & practiced before surgery.
- Techniques:
- Deep breathing - expands lungs, clears anesthesia, prevents atelectasis.
- Coughing - clears mucus; splint incision with pillow/blanket.
- Incentive spirometry - improves lung inflation, encourages progress.
- Leg exercises - improve venous return, decreases DVT risk.
- Turning in bed - prevents skin breakdown, increases circulation & peristalsis; practice with splinting for comfort.
2. Preparing the Patient Physically
a. Hygiene & Skin Prep
- Clean skin reduces infection risk.
- Shower night before/morning of surgery (often with chlorhexidine).
- Hair removal: clippers preferred, not shaving.
- Document method & skin condition.
b. Nutrition & Fluids
- Good nutrition/hydration supports healing.
- Blood transfusion if Hgb < 10 g/dL or Hct < 33%.
- NPO guidelines:
- Clear fluids up to 2 hours before surgery (unless contraindicated).
- Examples: water, pulp-free juice, clear tea/coffee, soda.
- Explain purpose of NPO & enforce strictly.
c. Elimination
- Bowel prep not routine - depends on type of surgery.
- May require enema/cleansing for GI surgeries.
- Encourage voiding before pre-op meds; catheter may be inserted for pelvic surgery.
d. Rest & Sleep
- Rest reduces stress & aids healing.
- Support with teaching, quiet environment, relaxation measures, or sedatives.
3. Preparing the Patient on the Day of Surgery
- Pre-op checklist ensures completion of tasks: consent, teaching, NPO, skin prep, elimination, tests.
- Check that preoperative consent forms are signed, witnessed, and correct; that advance directives are in the medical record (as applicable); and that the patient’s chart is in order.
- Gather the needed equipment and supplies.
- Perform hand hygiene.
- Check vital signs. Notify physician of any pertinent changes (i.e., rise or drop in blood pressure, elevated temperature, cough, symptoms of infection).
- Provide hygiene and oral care. Assess for loose teeth. Remind patient of food and fluid restrictions before surgery.
- Instruct the patient to remove all personal clothing including underwear and put on a hospital gown.
- Ask patient to remove cosmetics, jewelry including body piercing, nail polish, and prostheses (e.g., contact lenses, false eyelashes, dentures). Some facilities allow a wedding band to be left in place, depending on the type of surgery, provided it is secured to the finger with tape.
- If possible, give valuables to a family member or place valuables in an appropriate area, such as the hospital safe if this is not possible.
- Have patient empty bladder before surgery.
- Attend to any special preoperative orders, such as starting an IV line.
- Complete preoperative checklist and record of patient’s preoperative preparation.
- Administer preoperative medication as prescribed by physician/anesthesia provider.
- Preoperative medications may include:
- Sedatives (e.g., diazepam, midazolam, lorazepam) -decreases anxiety, amnesia.
- Anticholinergics (e.g., atropine, glycopyrrolate) -decreases secretions, prevent laryngospasm.
- Narcotic analgesics (e.g., morphine, meperidine) - relaxation, decreases anesthetic needs.
- Neuroleptanalgesics (e.g., fentanyl + droperidol) - calmness/sleepiness.
- H2 receptor blockers (e.g., cimetidine, ranitidine) -decreases gastric acidity.
- Raise side rails of bed; place bed in lowest position. Instruct patient to remain in bed or on stretcher. If necessary, a safety belt may be used.
- Tell the family of the patient where the patient will be taken after surgery and the location of the waiting area where the surgeon will come to explain the outcome of the surgery.
1.5 Evaluating
Evaluating the plan of care for the preoperative phase is based on the expected outcomes. The plan is effective if the patient is physically and emotionally prepared for surgery, verbalizes expected events and sensations of the perioperative period, and demonstrates postoperative exercises and activities.
Nursing insights:
General Considerations
• Obese patients are at greater risk of surgical complications and death compared to optimal weight patients. In taking this patient’s history, the nurse needs to be alert for other medical conditions such as diabetes, hypertension, and sleep apnea.
Infant and Child Considerations
• Children have special needs related to their overall health, age, and size. Easing preoperative anxiety of the child is crucial and includes using simple and concrete terms when providing information.
• The nurse needs to be sensitive to the anxiety level of the parent and provide support, explanations, and patient teaching as needed.
• Accurate weights are essential for correct medication dosages.
• Developmentally appropriate pain assessment and therapy needs to be followed to ensure adequate pain management.
Older Adult Considerations
• Age-related changes and preexisting chronic conditions can affect the postoperative course of the older adult patient.
• It is important to present preoperative teaching information slowly with reinforcement, since processing of information can be slower.
• Pain assessment and therapy may be suboptimal due to communication barriers and comorbidities present in many older adult patients. These patients may respond differently to pain medication, therefore, careful and individualized attention is required in this more vulnerable age group.
Intraoperative Care: The Nursing Process
The intraoperative phase of surgery begins with admission of the patient to the surgical area and lasts until the patient is transferred to the PACU.
1.1 Assessing
Nurses in surgical scrub attire identify the surgical patient, assess the patient’s emotional and physical status, and verify the information on the preoperative checklist including assessment data, lab reports, and consents for surgery and blood transfusion.
They may also carry out required immediate preoperative care, including performing skin preparation, starting IV fluids, placing sequential compression devices to prevent deep vein thrombosis (DVT), determining pain level, assuring patient and family, providing comfort, and giving preoperative medications.
The patient’s response to the procedures is assessed, and the events of surgery are explained.
In the operating room, the patient is positioned on the operating bed, identified again with the operative team using at least two identifiers (such as name, birth date, medical record number), and then anesthetized and draped.
1.2 Diagnosing
Patient problems in the intraoperative period may occur as a result of the position of the patient during the procedure, the effects of the anesthesia, equipment used and potential hazards, disruption of tissues during surgery, and the incision.
Examples of NANDA Nursing Diagnoses:
- Risk for Imbalanced Fluid Volume
- Risk for Perioperative Positioning Injury
1.3 Outcome Identification and Planning
Some expected outcomes are that the patient will:
- Remain free of neuromuscular injury
- Remain free from wrong site, wrong side, wrong procedure surgery
- Maintain fluid and electrolyte balance
- Maintain skin integrity (other than for the incision)
- Have symmetric breathing patterns
- Be free of injury from burns, retained foreign objects (inaccurate count of supplies), and medication errors
- Remain free from surgical site infection
- Maintain normothermia
1.4 Implementing
The scrub nurse is a member of the sterile team who maintains surgical asepsis while draping and handling instruments and supplies.
The circulating nurse identifies and assesses the patient on admission to the operating room, collaborates in safely positioning the patient on the operating bed, assists with monitoring the patient during surgery, provides additional supplies, maintains environmental safety, and counts the number of instruments, needles, and sponges used during the surgery to prevent the accidental loss of an item in the open incision.
The RNFA (registered nurse first assistants) actively assists the surgeon by providing exposure of the operative area, hemostasis (blood clotting), and wound closure.
The APN (Advanced Practice Nurses) coordinates care activities, collaborates with physicians and nurses in all phases of perioperative and post anesthesia care, and integrates case management, critical paths, and research into care of the surgical patient.
Positioning:
The risk for skin injury is avoided by lifting, rather than rolling or pulling, the patient into the surgical position. Perioperative nurses need to know the position to be used and significant nursing considerations for that position. Examples:
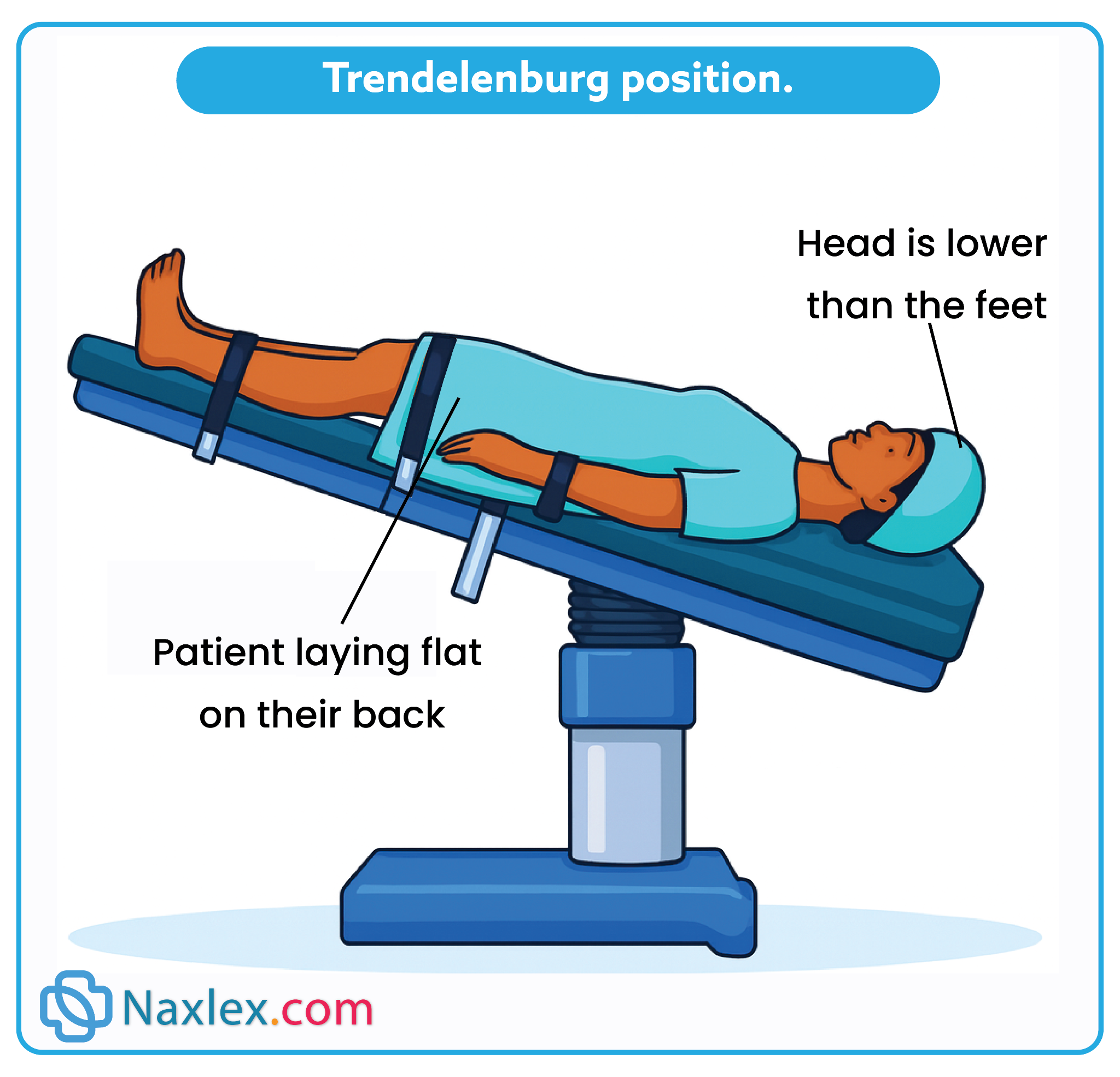
The Trendelenburg position requires lowering the upper torso and raising the feet.
- It is commonly used in minimally invasive surgery of the lower abdomen or pelvis.
- The displacement of the abdominal viscera toward the head decreases diaphragmatic movement and respiratory exchange; blood pools in the upper torso, and blood pressure increases; hypotension can result with return to the supine position.
- Shearing with resultant tissue damage is also a significant risk in this position
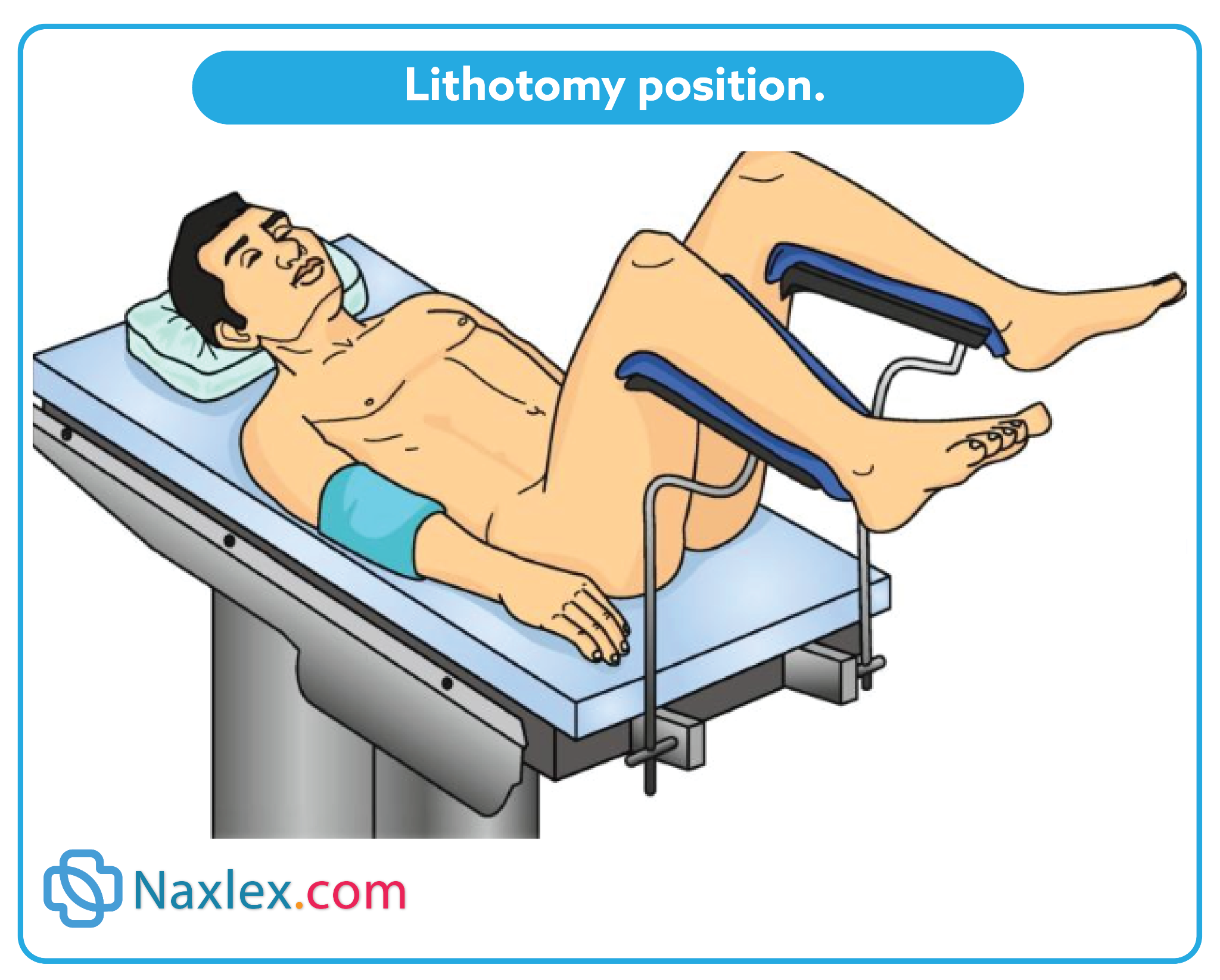
The lithotomy position is used for gynecologic, rectal, and urologic procedures.
- The placement of legs in stirrups causes pooling of blood in the legs increasing the risk of thrombophlebitis.
- Pressure can also damage the peroneal nerve, with resultant foot drop.
Draping:
Drapes are used to create and maintain a sterile field around the operative site, preventing the passage of microorganisms, particulate matter, and fluids between sterile and nonsterile areas.
Documenting:
Throughout surgery, the perioperative nurse documents ongoing patient assessment, item counts (sponges, sharps, instruments), monitoring data (e.g., vital signs, urine output, blood loss, pulse oximetry results), positioning, medications, dressings and drains, specimens, and responses to care on the intraoperative record.
Transferring to the Post anesthesia Care Unit:
This is a critical time: Sudden or rough handling can cause severe hypotension or potentially lethal cardiac or respiratory arrest.
The primary objective of the hand-off report from OR nurse to PACU nurse is to provide accurate information about the patient’s care, procedure, presenting condition, and any important events that occurred during the procedure.
1.5 Evaluating
Evaluation of the effectiveness of the plan of care for the intraoperative phase is based on the expected outcomes. If met, the plan was effective.
Postoperative Nursing Care
The postoperative phase can be divided into two stages:
- immediate care (usually provided in the PACU in both in hospital and outpatient/same-day surgery centers)
- ongoing postoperative care (lasting from return to the unit through convalescence).
1.1 Immediate Postoperative Assessment and Care
Purpose of PACU Care
- Continuous monitoring to prevent complications from anesthesia/surgery.
- Assessments compared with preoperative & intraoperative data.
- Frequency: every 10–15 minutes initially.
- Children: high risk for airway loss; emergence delirium common.
- Average PACU stay: ~1 hour (varies by surgery, anesthesia, patient response).
- PACU nurse role: vigilant monitoring, pain control, fluid/electrolyte balance, physiologic stabilization, prepare for next level of care.
Key Assessment Areas
1. Respiratory Status
- Monitor: rate, rhythm, depth, breath sounds, O₂ saturation, skin color, cardiovascular & mental status.
- Airway: patent, humidified O₂, pulse oximetry. Remove ET tube only after reflexes return.
- Signs of ineffective breathing: restlessness, anxiety, unequal chest expansion, noisy/shallow respirations, cyanosis, tachycardia.
- Common emergency: respiratory obstruction (from tongue, secretions, laryngospasm, or edema).
- Management: positioning, suctioning, O₂, encourage deep breaths.
2. Cardiovascular Status
- Monitor: vital signs, ECG, skin color/condition, compare BP with baseline.
- Hypertension causes: anesthetics, respiratory issues, surgical stress, recovery excitement.
- Hypotension causes: anesthesia, blood loss, positioning, pooling, meds.
- Interventions: O₂, deep breathing, leg exercises, verbal stimulation, accurate IV rates.
- Temperature regulation:
- Risk for inadvertent hypothermia (<35.5°C / 96°F).
- Complications: poor healing, cardiac disturbances, coagulopathy, delayed emergence.
- Interventions: warmed blankets, forced-air warming.
- Shock signs: tachycardia, decreased BP, cyanosis, cool skin, decreased urine output.
3. Central Nervous System Status
- Monitor return of consciousness:
- Unconscious
- Response to touch/sound
- Drowsy
- Awake, not oriented
- Awake, oriented
- Provide reorientation (touch, name, reassurance).
4. Fluid Status
- Risks: restriction, intraoperative loss, wound drainage, stress response (Na⁺/H₂O retention).
- High risk: children, older adults.
- Assess: skin turgor, vitals, urine output, wound drainage, IV intake.
- IV care: check type, rate, insertion site, tubing patency.
5. Wound Status
- Assess incision dressing for amount, color, consistency of drainage.
- Check drains/tubes output.
- Warning signs: large bright-red drainage and restlessness, pallor, cool moist skin, decreased BP, increased pulse/RR - possible hemorrhage/hypovolemic shock (report immediately).
6. Pain Management
- Use pain scales (verbal, numeric 0–10, or faces).
- Administer analgesia early: NSAIDs, opioids (PCA possible).
- Nonpharmacologic: positioning, reassurance, touch.
- Use preoperative pain-preference info for individualized care.
7. General Condition & Safety
- Maintain psychological comfort with reorientation and reassurance.
- Ensure physical safety: proper positioning, side rails.
- Discharge criteria: stable vitals & consciousness.
- PACU nurse communicates a handoff report to unit nurse upon transfer.
1.2 Ongoing Postoperative Care
Ongoing postoperative care is planned to facilitate recovery from surgery and coping with alterations.
THE NURSING PROCESS FOR ONGOING POSTOPERATIVE CARE
Assessing:
The nurse on the unit assists PACU personnel in transferring the patient to the bed in the unit and makes an initial assessment using data from the preoperative and intraoperative phases. A postoperative checklist or flow sheet may be used.
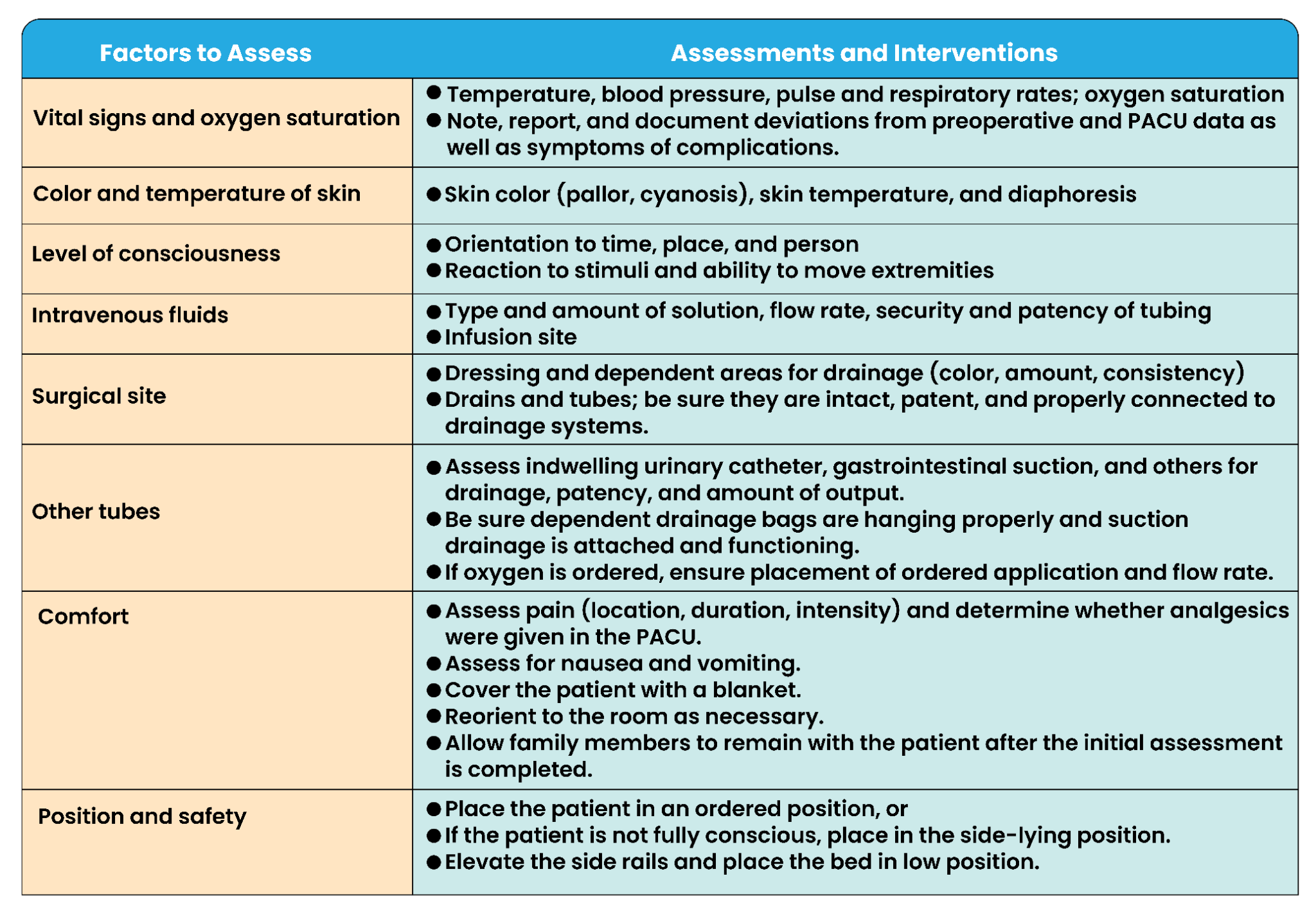
Common time frames are every 15 minutes until stable, changing to every 1 to 2 hours for the first 24 hours, and every 4 hours thereafter.
Diagnosing:
Nursing diagnoses in the postoperative phase may represent actual problems or those for which the patient is at risk.
Examples:
- Risk for Infection
- Disturbed Body Image
- Acute Pain
- Urinary Retention
Outcome Identification and Planning
Examples of desired postoperative outcomes for a patient after major surgery are as follows: The patient will:
- Carry out leg exercises every 2 to 4 hours.
- Deep breathe and cough effectively every 2 hours.
- Verbalize decreasing levels of pain.
- Have a balanced intake and output.
- Regain normal bowel and bladder elimination.
- Exhibit a healing surgical incision.
- Remain free of infection.
- Verbalize any concerns about appearance of wound.
- Verbalize and demonstrate wound self-care
Implementing:
Nursing care is discussed to prevent complications, promote a return to health, and facilitate coping with alterations.
1. Preventing Cardiovascular Complications
Hemorrhage
- Cause: slipped suture, dislodged clot, stress on site, meds, conditions
- Signs: restlessness, anxiety, frank bleeding, hypotension, cold/clammy skin, weak rapid pulse, mottled extremities, decreased urine, thirst
- Care: stop bleeding, replace blood volume, apply pressure dressing, notify surgeon, prepare for OR if uncontrolled.
Shock (usually hypovolemic)
- Cause: blood/fluid loss, circulatory failure
- Signs: same as hemorrhage
- Care: airway, flat with legs elevated 30–45°, O₂, cover for warmth, monitor vitals/Hct/ABGs, start IV lines, fluids/blood, meds, notify surgeon.
Thrombophlebitis
- Cause: venous stasis, clot in leg vein
- Signs: calf/thigh pain & cramping, redness, swelling, increased temperature, increased limb diameter
- Care: prevent embolus, give meds (anticoagulants, anti-inflammatory, analgesics), bed rest, apply heat, compression devices, measure calf/thigh circumference, do not massage legs.
2. Preventing Respiratory Complications
- General measures: monitor vitals, deep breathing, coughing, incentive spirometry, turning q2h, ambulation, hydration, semi-Fowler’s position, monitor narcotic response.
Pulmonary Embolus
- Cause: clot lodges in pulmonary vessels
- Signs: dyspnea, chest pain, cough, cyanosis, tachypnea, tachycardia, anxiety
- Care: emergency! Notify physician, semi-Fowler’s, O₂, bed rest, meds (anticoagulants, analgesics), avoid Valsalva.
Pneumonia
- Cause: aspiration, infection, weak cough, anesthesia secretions, dehydration, immobility
- Signs: fever, chills, cough with or without purulent or rusty sputum, crackles, wheezes, dyspnea, chest pain
- Care: semi-Fowler’s/Fowler’s, O₂, antibiotics, expectorants, analgesics, oral hygiene, rest.
Atelectasis
- Cause: alveoli collapse from mucus retention leading to poor gas exchange
- Signs: decreased breath sounds, dyspnea, cyanosis, crackles, restlessness, apprehension
- Care: O₂, semi-Fowler’s, pain relief, lung expansion interventions.
3. Preventing Surgical Site Complications
- Risks: infection, dehiscence (separation), evisceration (organ protrusion)
- Care: monitor vitals (fever), hydration, nutrition (protein, carbs, calories, vitamins), aseptic dressing changes, hand hygiene, proper disposal of soiled materials.
4. Promoting a Return to Health
Elimination Needs
- May be altered by anesthesia, surgery, inactivity, altered intake.
- Assess urine and bowel function, encourage mobility and fluids.
Fluid & Nutrition Needs
- Monitor I&O, IV rates, skin turgor, mucous membranes.
- Nutrition: advance diet as tolerated (clear then full liquids then soft then regular), monitor weight, oral hygiene, clean environment, upright position for meals, involve family.
Comfort & Rest
- Address nausea, vomiting, thirst, hiccups, pain.
- Provide hygiene, clean linens, quiet rest periods, allow family presence.
|
NURSING INSIGHTS: PROMOTING POSTOPERATIVE REST AND COMFORT Nausea and Vomiting Avoid giving the patient a large amount of fluids or food at one time, especially after being NPO. Administer prescribed medications. Provide oral hygiene, as needed. Maintain clean environment. Avoid use of a straw. Avoid strong-smelling food. Assess for possible allergy to medications, such as antibiotics or analgesics. Maintain bowel elimination
Thirst Offer sips of water or ice chips when NPO (if permitted). Maintain oral hygiene.
Hiccups Have the patient do the following: Take several swallows of water while holding the breath (if not NPO). Rebreathe into a paper bag. Eat a teaspoon of granulated sugar
Surgical Pain Assess pain frequently; administer prescribed analgesics every 2 to 4 hours on a regular schedule during the first 24 to 36 hours after surgery. Reinforce preoperative teaching for pain management. Offer nonpharmacologic measures to supplement medications: massage, position changes, relaxation, guided imagery, meditation, music. |
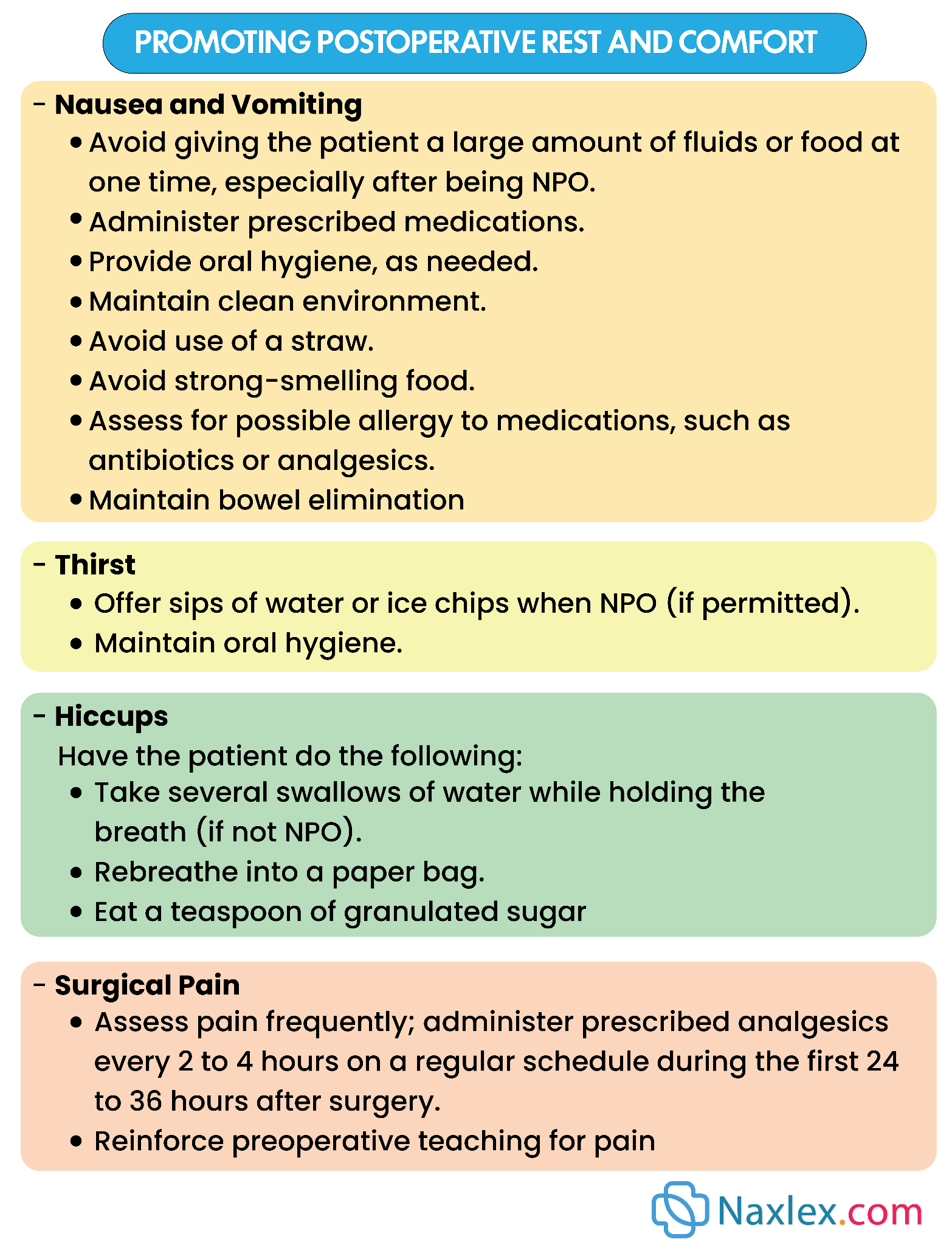
5. Helping the Patient Cope
- Surgery can affect body image and self-concept.
- Reactions may resemble grief; coping depends on age, culture, visibility of change, support system.
- Nurses provide emotional support, facilitate adaptation, respect cultural values, and acknowledge grief as normal.
6. Outpatient/Same-Day Surgery Care
- Discharge criteria: awake, alert, stable vitals, voided, tolerated oral fluids, not dizzy/drowsy.
- Must leave with responsible adult (no driving or solo public transport).
- Discharge usually 1-3 hours after surgery.
- Provide written and verbal home care instructions.
UNEXPECTED SITUATIONS AND ASSOCIATED INTERVENTIONS
• Vital signs are progressively increasing or decreasing from baseline: Notify primary care provider. A continued decrease in blood pressure or an increase in heart rate could indicate internal bleeding.
• Dressing was clean before but now has large amount of fresh blood: Do not remove dressing. Reinforce dressing with more bandages. Removing the bandage could dislodge any clot that is forming and lead to further blood loss. Notify primary care provider.
• Patient reports pain that is not relieved by ordered medication: After fully assessing pain (location, description, alleviating factors, causal factors), notify primary care provider. Pain can be a clue to other problems, such as hemorrhage.
• Patient is febrile within 12 hours of surgery: Assist patient with coughing and deep breathing. If ordered, begin incentive spirometry. Continue to monitor vital signs and laboratory values, such as complete blood count (CBC).
Nursing insights:
Older Adult Considerations:
In the older adult patient, postoperative pneumonia can be a very serious complication resulting in death. Therefore, it is especially important to encourage and assist the patient in using the incentive spirometer and with deep-breathing exercises.
Older patients may take longer to return to their level of orientation before surgery. Drugs and anesthetics will delay this return.
Infant and Child Considerations:
Postoperative complications are related to the respiratory system in this age group. After receiving general anesthesia, premature infants are at greater risk for apnea.
Infants and children are at great risk for temperature-related complications since their body temperature can change rapidly. It is essential to have warmed blankets and other warming equipment available to avoid this complication.
Summary
- Perioperative nursing includes the preoperative, intraoperative, and postoperative phases. Each phase focuses on different aspects of a patient’s surgical experience.
- The assessment of risk factors such as history of smoking, obesity, and obstructive sleep apnea allows a nurse to anticipate patient needs and the types of preparation required preoperatively to prevent intraoperative and postoperative complications.
- Malnutrition, diabetes, obesity, smoking, age, obstructive sleep apnea, and cardiac disorders increase patients’ risks for perioperative complications.
- A nurse assesses a patient’s potential psychological response by identifying the patient’s previous experiences with surgery to anticipate needs, providing teaching, addressing fears, and clarifying concerns.
- Postoperative patient education should be relevant and specific, culturally appropriate, and accurate to enhance the ability of patients to care for themselves at home.
- When caring for patients who are undergoing ambulatory surgery, prioritize education because of the limited time available, and involve the patient’s family or support system.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Perioperative Nursing Care
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


