Please set your exam date
Contraception
Study Questions
Natural Methods of contraception
The method of contraception that involves monitoring a woman's menstrual cycle and avoiding intercourse during her fertile window is called ?
Explanation
The correct answer is choice A.Natural family planning is a method of contraception that involves monitoring a woman’s menstrual cycle and avoiding intercourse during her fertile window.This is based on the observation of the signs and symptoms of fertility, such as the length of the menstrual cycle, the body temperature, and the cervical secretions.
Choice B is wrong because hormonal methods are methods of contraception that use hormones to prevent ovulation, such as pills, patches, injections, implants, and rings.
Choice C is wrong because intrauterine methods are methods of contraception that involve inserting a device into the uterus to prevent implantation, such as copper IUDs and hormonal IUDs.
Choice D is wrong because barrier methods are methods of contraception that prevent sperm from reaching the egg, such as condoms, diaphragms, caps, and spermicides.
What is the term for surgical methods of contraception ?
Explanation
The correct answer is choice A. Permanent sterilization.This is because surgical methods of contraception involve procedures that block or cut the reproductive organs of men or women, preventing them from producing or releasing gametes.These methods are also known as sterilization and are considered permanent and irreversible.
Choice B is wrong because hormonal methods of contraception use synthetic hormones to prevent ovulation, thicken cervical mucus, or thin the uterine lining.These methods are not surgical and can be reversed by stopping the use of hormones.
Choice C is wrong because natural family planning methods rely on observing the signs of fertility and avoiding sexual intercourse during the fertile days of the menstrual cycle.These methods are not surgical and do not involve any devices or drugs.
Choice D is wrong because barrier methods of contraception use physical or chemical barriers to prevent sperm from reaching the egg.
These methods include condoms, diaphragms, cervical caps, spermicides, and sponge.These methods are not surgical and can be removed or discontinued at any time.
A nurse is teaching a client about natural family planning methods.
Which of the following statements by the client indicates a need for further teaching?
Explanation
The correct answer is choice A.“I will avoid intercourse during the days 8 to 19 of my menstrual cycle.” This statement indicates a need for further teaching because it is based on thestandard days methodof natural family planning, which assumes that ovulation happens near mid-cycle and that the fertile window is fixed.However, this method is not reliable for women who have irregular or variable menstrual cycles, or who ovulate at different times.A more accurate way to determine the fertile days is to monitor and record the changes incervical mucus,basal body temperature, and other signs of ovulation.
Choice B is wrong because checking the cervical mucus every day is one of the methods of natural family planning that can help a woman identify her fertile days.The cervical mucus becomes clear, stretchy, and wet when ovulation is approaching, indicating high fertility.
Choice C is wrong because measuring the basal body temperature every morning is another method of natural family planning that can help a woman identify her fertile days.The basal body temperature rises slightly after ovulation and stays elevated until the next period, indicating low fertility.
Choice D is wrong because using an ovulation predictor kit to confirm when ovulation is occurring is also a method of natural family planning that can help a woman identify her fertile days.
An ovulation predictor kit detects the surge of luteinizing hormone
A nurse is counseling a client who wants to use a barrier method of contraception.
Which of the following factors should the nurse consider when recommending a barrier method?
Explanation
The correct answer is choice D. All of the above factors should be considered when recommending a barrier method of contraception.
- Choice A is correct because the client’s preference and comfort level with the method are important for adherence and satisfaction.Different types of barrier methods have different advantages and disadvantages, such as ease of use, cost, availability, and side effects.
- The client should be informed about the options and choose the one that suits them best.
- Choice B is correct because the client’s history of STIs affects the choice of barrier method.Some barrier methods, such as condoms (male and female), can also protect against STIs by preventing contact with skin and fluids.However, other barrier methods, such as diaphragms and cervical caps, do not offer STI protection and may increase the risk of urinary tract infections (UTIs) or toxic shock syndrome (TSS) if not used correctly.
- Choice C is correct because the client’s frequency and regularity of sexual activity influences the convenience and effectiveness of barrier methods.Some barrier methods, such as spermicides, films, foams, creams, and gels, need to be inserted before each act of sex and have a limited duration of action.Other barrier methods, such as condoms, need to be used every time sex occurs and disposed of properly after use.Some barrier methods, such as diaphragms and cervical caps, can be inserted up to 6 hours before sex and need to be left in place for at least 6 hours after sex.
A nurse is providing education to a client who is prescribed a hormonal patch for contraception.
Which of the following instructions should the nurse include?
Explanation
The correct answer is choice C. The nurse should instruct the client to use a backup method of contraception for the first 7 days of patch use.This is because it takes about a week for the hormones in the patch to reach a level that prevents ovulation.The client should also apply a new patch every week for 3 weeks, and then have a patch-free week to allow for menstrual bleeding.
Choice A is wrong because the client should not apply the patch to the same site every week.This can cause skin irritation and reduce the effectiveness of the patch.The client should rotate the patch site among four areas: the upper arm, the abdomen, the buttock, or the back.
Choice B is wrong because the client should change the patch every week, not every 3 weeks.Changing the patch every 3 weeks would result in low hormone levels and increased risk of pregnancy.The client should have a patch-free week after 3 weeks of using the patch.
Choice D is correct but not complete.The nurse should instruct the client to report any signs of thromboembolism, such as leg pain or chest pain, as these can be serious complications of using hormonal contraception.
However, this instruction alone is not enough to ensure safe and effective use of the patch.The client also needs to know how to apply, change, and remove the patch correctly.
Barrier Methods
A nurse is caring for a client who has an intrauterine device (IUD) inserted for contraception.
Which of the following statements by the client indicates a potential complication of IUD use?
Explanation
The correct answer is choice C.A foul-smelling vaginal discharge indicates a potential complication of IUD use, such as a pelvic infection.Pelvic infections can cause serious problems, such as infertility, ectopic pregnancy, and chronic pain.
Therefore, a client who has an IUD and reports a foul-smelling vaginal discharge should be evaluated by a health care provider as soon as possible.
Choice A is wrong because spotting between periods is a common side effect of IUDs, especially during the first few months after insertion.
It is not a sign of a complication and usually goes away over time.
Choice B is wrong because cramping in the lower abdomen is also a common side effect of IUDs, especially during and after insertion.
It is not a sign of a complication and can be relieved with over-the-counter pain medication.
Choice D is wrong because feeling some strings in the vagina is normal for IUD users.The strings are attached to the end of the IUD and allow the user and the provider to check that the IUD is in place.
The strings are not harmful and do not interfere with sexual activity.
A nurse is discussing surgical methods of contraception with a client who is considering permanent sterilization.
Which of the following information should the nurse provide?
Explanation
The correct answer is choice C. Surgical methods do not protect against sexually transmitted infections (STIs).This is because surgical methods of contraception only prevent the sperm from reaching the egg or the egg from reaching the uterus, but they do not prevent the transmission of viruses or bacteria that cause STIs.
Choice A is wrong because surgical methods are not reversible and cannot be undone if the client changes their mind.Surgical methods are permanent and require a qualified healthcare provider to perform the procedure.
Choice B is wrong because surgical methods are not effective immediately and do require follow-up testing.
For example, after a vasectomy, a man needs to have semen analysis to confirm that there are no sperm in his semen.This may take several weeks or months after the surgery.Similarly, after a tubal ligation, a woman may need to have a hysterosalpingogram (HSG) to check that the fallopian tubes are completely blocked.
Choice D is wrong because surgical methods do not require general anesthesia and hospitalization.Most surgical methods can be done under local anesthesia and as outpatient procedures.However, some complications may arise that may require hospitalization, such as infection, bleeding, or injury to other organs.
A nurse is teaching a client about the calendar rhythm method of natural family planning.
The nurse should instruct the client to avoid sexual intercourse during which period?
Explanation
The correct answer is choice C.The calendar rhythm method of natural family planning is based on tracking the menstrual cycle and avoiding sexual intercourse during the fertile days, which are usually 14 days before the onset of the next menstrual cycle.
This is because ovulation typically occurs around day 14 of the cycle and the egg can survive for up to 24 hours after ovulation.
Sperm can survive for up to five days in the female reproductive tract, so having sex during this period can result in pregnancy.
Choice A is wrong because the first 7 days of the menstrual cycle are not necessarily safe for avoiding pregnancy.Some women may have shorter cycles or irregular ovulation, which can make them fertile during this time.
Choice B is wrong because the last 7 days of the menstrual cycle are also not necessarily safe for avoiding pregnancy.Some women may have longer cycles or irregular ovulation, which can make them fertile during this time.
Choice D is wrong because the 14 days after the onset of the previous menstrual cycle are not a reliable indicator of fertility.The length of the menstrual cycle can vary from month to month, so counting from the previous cycle may not accurately reflect when ovulation occurs
A nurse is reviewing the records of four clients who use the calendar rhythm method of contraception.
Which of the following clients has the highest risk of unintended pregnancy?
Explanation
The correct answer is choice C.A client who has an irregular menstrual cycle ranging from 25 to 35 days has the highest risk of unintended pregnancy because the calendar rhythm method requires a person to monitor their menstrual cycle and estimate their fertile days based on the length of their shortest and longest cycles.
If the cycle length varies widely, it is harder to predict the fertile days accurately and avoid unprotected sex during those days.
Choice A is wrong because a client who has a regular menstrual cycle of 28 days can easily calculate their fertile days by subtracting 18 from the shortest cycle and 11 from the longest cycle.
In this case, both numbers are 10, so the fertile days are from day 10 to day 10 of the cycle.
Choice B is wrong because a client who has a regular menstrual cycle of 30 days can also calculate their fertile days by subtracting 18 from the shortest cycle and 11 from the longest cycle.
In this case, both numbers are 12, so the fertile days are from day 12 to day 12 of the cycle.
Choice D is wrong because a client who has an irregular menstrual cycle ranging from 27 to 33 days has a lower risk of unintended pregnancy than choice C because the cycle length variation is smaller.The fertile days for this client are from day 9 to day 22 of the cycle, calculated by subtracting 18 from the shortest cycle and 11 from the longest cycle.
A nurse is counseling a client who wants to use the standard days method of natural family planning.
The nurse should inform the client that this method is most suitable for which of the following conditions?
Explanation
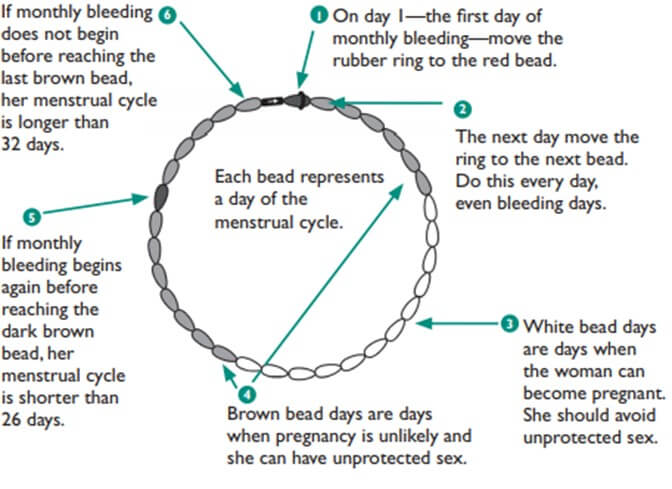
The correct answer is choice B.The Standard Days Method (SDM) is a natural family planning method that requires women to abstain from sex or use a barrier method during their fertile days, which are from day 8 to day 19 of their menstrual cycle.This method is most suitable for women who have regular cycles between 26 and 32 days.
Choice A is wrong because having a history of pelvic inflammatory disease does not affect the suitability of the SDM, as long as the woman has regular cycles.
Choice C is wrong because having a partner who travels frequently for work does not affect the suitability of the SDM, as long as the woman can track her cycle and avoid unprotected sex on her fertile days.
Choice D is wrong because having a history of endometriosis may cause irregular cycles, which makes the SDM less reliable.
Hormonal Methods
A nurse is explaining the use of cycle beads to a client who wants to use the standard days method of contraception.
The nurse should instruct the client to do which of the following actions?
Explanation
The correct answer is choice A. The client should move a rubber ring over one bead every day starting from the first day of menstruation.This is how theStandard Days Methodof contraception works, using a special string of beads calledCycleBeadsto track the days of the menstrual cycle and identify the fertile window.
Choice B is wrong because moving the ring from the last day of menstruation would not match the cycle days indicated by the beads.
Choice C is wrong because moving the ring over two beads every day would not accurately track the cycle days, and starting from the first day of ovulation would be too late to avoid pregnancy.
Choice D is wrong because moving the ring over two beads every day would not accurately track the cycle days, and starting from the last day of ovulation would not account for the fertile window before ovulation.
The Standard Days Method can only be used by women who have regular cycles between 26 and 32 days long.They should avoid unprotected sex or use another method of birth control on days 8 to 19 of their cycle.
A nurse is evaluating the understanding of a client who uses a smartphone app to track her fertility using the standard days method.
The nurse should ask the client which of the following questions?
Explanation
The correct answer is choice C.The standard days method is a calendar-based method that identifies a fixed fertile window in the woman’s cycle (days 8 to 19) when a couple should avoid sexual intercourse if they wish to prevent pregnancy.
All other days in a woman’s cycle are considered non-fertile.
The nurse should ask the client how she marks her fertile and non-fertile days on the app, as this is essential for using the method correctly.
Choice A is wrong because the standard days method does not require recording basal body temperature, which is another fertility awareness method that involves measuring and charting the daily changes in body temperature.
Choice B is wrong because the standard days method does not require identifying cervical mucus changes, which is another fertility awareness method that involves observing and tracking the changes in the quality and quantity of cervical mucus throughout the cycle.
Choice D is wrong because the standard days method does not require calculating ovulation date, which is another fertility awareness method that involves estimating the day of ovulation based on previous cycle lengths.
A nurse is providing education about spermicide to a patient.
Which of the following is a contraindication for the use of spermicide?
Explanation
The correct answer is choice C.Cervical infections are a contraindication for the use of spermicide because they can cause irritation and inflammation of the cervix, which can increase the risk of HIV and other STDs.Spermicide can also worsen existing infections by altering the vaginal flora and pH.
Choice A is wrong because history of cervical cancer is not a contraindication for the use of spermicide.However, women with cervical cancer should consult their doctor before using any form of contraception.
Choice B is wrong because allergy to latex condoms is not a contraindication for the use of spermicide.Spermicide can be used with non-latex condoms or other barrier methods, such as cervical caps or diaphragms.
Choice D is wrong because endometriosis is not a contraindication for the use of spermicide.Spermicide does not affect the growth of endometrial tissue outside the uterus.
A nurse is teaching a patient how to use a diaphragm.
Which of the following instructions should the nurse include?
Explanation
The correct answer is choice D.“You should empty your bladder before inserting the diaphragm.” This is because a full bladder can push the diaphragm out of place and reduce its effectiveness.
Emptying your bladder before inserting the diaphragm can help it stay in place and cover your cervix properly.
Choice A is wrong because “You should replace the diaphragm every year.” This is not true.You should replace the diaphragm every 1-2 years or if it has any holes, cracks, wrinkles, or weak spots.You can check your diaphragm for damage by holding it up to the light or filling it with water.
Choice B is wrong because “You should insert the diaphragm after intercourse.” This is not true.You should insert the diaphragm before intercourse, up to 2 hours in advance.If you have intercourse more than 2 hours after inserting the diaphragm, you should reapply spermicide without removing the diaphragm.
Choice C is wrong because “You should wash the diaphragm with hot water and strong soap.” This is not true.You should wash the diaphragm with soap and warm water, and let it air dry.Hot water and strong soap can damage the material of the diaphragm and make it less effective.
A nurse is assessing the effectiveness of a patient's contraceptive method.
The patient is using spermicide alone.
Which of the following statements is correct?
Explanation
The correct answer is choice B.Spermicide alone is 72% effective at preventing pregnancy when used correctly and consistently.
This means that out of 100 people who use spermicide as their only birth control method, about 28 will become pregnant in a year.
Choice A is wrong because spermicide alone is not 90% effective at preventing pregnancy.It is much less effective than other methods of birth control.
Choice C is wrong because spermicide alone is not 100% effective at preventing pregnancy.No method of birth control is 100% effective, except for abstinence.
Choice D is wrong because spermicide alone is not 50% effective at preventing pregnancy.It is slightly more effective than that, but still not very reliable.
Spermicide works by damaging the sperm and blocking the entrance to the cervix.
It needs to be inserted into the vagina before sex and reapplied every time.It does not protect against sexually transmitted infections (STIs) and may increase the risk of some STIs by irritating the vaginal lining.Spermicide is more effective when combined with another method of birth control, such as condoms or diaphragms.
More questions on this topic
A nurse is providing education about the diaphragm to a patient.
Which of the following is a contraindication for the use of a diaphragm?
Explanation
The correct answer is choice A.A history of toxic shock syndrome (TSS) is a contraindication for the use of a diaphragm.
TSS is a rare but serious condition caused by a bacterial infection that can occur when using a diaphragm for too long or not cleaning it properly.
Choice B is wrong because a history of uterine fibroids is not a contraindication for the use of a diaphragm.
Uterine fibroids are benign tumors that grow in the uterus and usually do not affect the cervix or the fit of the diaphragm.
Choice C is wrong because a history of irregular menstrual periods is not a contraindication for the use of a diaphragm.
Irregular periods may be caused by various factors such as stress, hormonal imbalance, or medical conditions, but they do not affect the effectiveness or safety of the diaphragm.
Choice D is wrong because a history of breast cancer is not a contraindication for the use of a diaphragm.
Breast cancer is not related to the use of barrier methods of contraception such as the diaphragm.
However, some hormonal methods of contraception may increase the risk of breast cancer or be contraindicated for women who have or had breast cancer.
A nurse is teaching a patient about the use of spermicide.
Which of the following is an adverse effect of some spermicides that contain nonoxynol-9 (N-9)?
Explanation
The correct answer is choice C. Increased risk of HIV transmission.According to some sources, spermicide that contains nonoxynol-9 (N-9) can irritate sensitive genital tissues, especially if used several times a day.
This irritation can increase the risk of HIV and other sexually transmitted infections by giving infections an easy pathway into the body.
Choice A is wrong because vaginal dryness is not a common side effect of spermicide.
Choice B is wrong because bacterial vaginosis is not directly linked to spermicide use.
Choice D is wrong because cervical cancer is not caused by spermicide use.
Spermicide is a type of contraceptive that works by stopping sperm from reaching an egg.
It comes in different forms such as gels, creams, foams, films or suppositories.It needs to be inserted into the vagina before sex and used correctly every time for it to be effective.
Which of the following is a contraindication for the use of a diaphragm as a contraceptive method?
Explanation
The correct answer is choice B.History of uterine prolapse is a contraindication for the use of a diaphragm as a contraceptive method.Uterine prolapse is a condition where the uterus descends into the vagina, which can interfere with the proper placement and seal of the diaphragm.
Choice A is wrong because history of cervical cancer is not a contraindication for diaphragm use.
Cervical cancer is a malignant tumor of the cervix, which can be treated with surgery, radiation, or chemotherapy.
Diaphragm use does not affect the risk or treatment of cervical cancer.
Choice C is wrong because history of ovarian cysts is not a contraindication for diaphragm use.
Ovarian cysts are fluid-filled sacs that develop in or on the ovaries, which can cause pain, bloating, or irregular periods.
Diaphragm use does not affect the formation or rupture of ovarian cysts.
Choice D is wrong because history of menopause is not a contraindication for diaphragm use.
Menopause is the natural cessation of menstrual cycles and fertility, which occurs around age 50 in most women.
Diaphragm use does not affect the hormonal changes or symptoms of menopause.
A nurse is teaching a client who is prescribed COCs about the mechanism of action of these pills.
The nurse should explain that COCs prevent pregnancy by?
Explanation
The correct answer is choice A.COCs prevent pregnancy byinhibiting the production of follicle-stimulating hormone (FSH) and luteinizing hormone (LH), which are responsible for ovulation.
By suppressing ovulation, COCs prevent the release of a mature egg that can be fertilized by sperm.
Choice B is wrong because COCs do not increase the production of prostaglandins that cause uterine contractions.
Prostaglandins are involved in inflammation and pain, and are not directly related to contraception.
Choice C is wrong because COCs do not decrease the permeability of the fallopian tubes to sperm and egg.
The fallopian tubes are the site of fertilization, and COCs do not affect their function.
Choice D is partially correct but not the best answer.COCs do suppress ovulation, but they also have other mechanisms of action, such asthickening cervical mucusandaltering the uterine lining.
These effects make it harder for sperm to reach the egg and for a fertilized egg to implant in the uterus.
Therefore, choice D does not capture the full mechanism of action of COCs.
A nurse is caring for a client who is taking COCs and reports nausea.
The nurse should advise the client to
Explanation
The correct answer is choice B. The nurse should advise the client to take the pill at bedtime or with food.This can help reduce nausea, which is a common side effect of COCs.Nausea usually diminishes with continued use of the same method.
Choice A is wrong because taking the pill with a glass of water on an empty stomach may increase nausea.
Choice C is wrong because switching to a different brand of COCs is not effective in treating nausea.There are no significant differences among various COCs in terms of nausea.
Choice D is wrong because stopping the pill and using another method of contraception is not necessary unless the client prefers it.Nausea is not harmful and can be managed with simple measures.
A nurse is reviewing the medical history of a client who is considering using COCs as a method of contraception.
The nurse should identify that which of the following conditions is a contraindication for using COCs?
Explanation
The correct answer is choice A.History of migraine headaches with aura is a contraindication for using COCs because it increases the risk of stroke.
Some possible explanations for the other choices are:
- Choice B is wrong because history of dysmenorrhea and menorrhagia is not a contraindication for using COCs.In fact, COCs may help reduce menstrual pain and bleeding.
- Choice C is wrong because history of acne vulgaris and hirsutism is not a contraindication for using COCs.In fact, COCs may help improve acne and hirsutism by reducing androgen levels.
- Choice D is wrong because history of iron-deficiency anemia and fatigue is not a contraindication for using COCs.In fact, COCs may help prevent iron-deficiency anemia by reducing menstrual blood loss.
Normal ranges for relevant parameters are:
- Blood pressure: <140/90 mmHg
- Body mass index: 18.5–24.9 kg/m
- Hemoglobin: 12–16 g/dL for women
A nurse is instructing a client who is starting COCs for the first time.
The nurse should tell the client that if she misses one pill, she should ?
Explanation
The correct answer is choice A.The nurse should tell the client that if she misses one pill, she should take the missed pill as soon as possible and continue with the next pill at the usual time.This will ensure that she maintains a continuous hormonal exposure and does not extend the hormone-free interval beyond 7 days.She does not need to use extra contraception.
Choice B is wrong because taking two pills at once and skipping the next pill will disrupt the hormonal balance and may cause side effects such as nausea or breakthrough bleeding.Choice C is wrong because discarding the missed pill and taking the next pill at the usual time will shorten the duration of hormonal exposure and increase the risk of ovulation.Choice D is wrong because stopping taking the pills for the rest of the cycle and using a backup method of contraception will expose the client to an unnecessary hormone-free interval and may compromise her contraceptive efficacy.
COCs are combined oral contraceptives that contain synthetic estrogen and progestin hormones that prevent ovulation and thicken cervical mucus to inhibit sperm penetration.The normal range of COCs dosage is 20 to 35 micrograms of estrogen and 0.1 to 3 milligrams of progestin per pill.
A nurse is providing education to a client who is using COCs about some of the benefits of this method of contraception.
The nurse should inform the client that COCs can?
Explanation
The correct answer is choice A.COCs can reduce the risk of endometrial, ovarian and colon cancer.This is because COCs suppress ovulation and reduce inflammation in the genital tract, which may lower the exposure to carcinogens and mutagens.
Choice B is wrong because COCs do not increase bone density or prevent osteoporosis.In fact, some studies have suggested that COCs may have a negative effect on bone mineral density.
Choice C is wrong because COCs do not enhance fertility or improve menstrual regularity.
COCs prevent pregnancy by inhibiting ovulation, which means that they temporarily suppress fertility.COCs may also cause irregular bleeding or amenorrhea in some women.
Choice D is wrong because COCs do not lower blood pressure or cholesterol levels.On the contrary, COCs may increase the risk of hypertension and dyslipidemia in some women, especially those who smoke, are obese, or have a family history of cardiovascular disease.
A nurse in a clinic is caring for a client who has been taking oral contraceptives for several months and reports frequent breakthrough bleeding during her cycle.
Which of the following actions should the nurse take?
Explanation
The correct answer is choice D. The client should switch to a higher-dose formulation of oral contraceptives.Breakthrough bleeding is a common side effect of low-dose birth control pills, especially in the first months of use.It may indicate that the estrogen dose is too low to suppress the growth of the endometrium.
A higher-dose formulation may reduce or eliminate breakthrough bleeding by providing more estrogen.
Choice A is wrong because taking two pills daily until bleeding stops is not a recommended way to manage breakthrough bleeding.
It may cause side effects such as nausea, headache, or breast tenderness.It may also increase the risk of blood clots.
Choice B is wrong because stopping oral contraceptives immediately is not advisable unless there is a medical reason to do so.
Stopping oral contraceptives may cause irregular bleeding, ovulation, and pregnancy.
The client should consult with their provider before discontinuing any medication.
Choice C is wrong because smoking does not cause breakthrough bleeding, but it does increase the risk of serious complications from oral contraceptives, such as stroke, heart attack, or blood clots.The client should avoid smoking while taking any hormonal contraceptive, regardless of whether they experience breakthrough bleeding or not.
A nurse in a family planning clinic is teaching a group of clients about oral contraceptives (OCs).
Which of.
the following information should be included in this teaching?
Explanation
The correct answer is choice C. OCs can decrease menstrual blood loss and cramps.This is because OCs prevent ovulation and thin the lining of the uterus, which reduces the amount of bleeding and cramping during menstruation.
Choice A is wrong because OCs do not provide protection against STIs.The only contraceptive methods that can prevent STIs are barrier methods, such as condoms.
Choice B is wrong because OCs can have variable effects on libido and sexual satisfaction.
Some women may experience an increase, while others may experience a decrease or no change at all.This depends on individual factors, such as hormone levels, mood, and relationship quality.
Choice D is wrong because OCs can also have variable effects on mood and depression.
Some women may experience an improvement, while others may experience a worsening or no change at all.This also depends on individual factors, such as hormone sensitivity, stress, and history of mental health problems.
A nurse is providing teaching to a client who has a new prescription for oral contraceptives (OCs).
Which of the following statements by the client indicates an understanding of how to initiate OCs?
Explanation
The correct answer is choice B. The client should start taking oral contraceptives (OCs) on day one of their menstrual cycle, which is the first day of their period.This way, they will be protected from pregnancy right away and do not need to use a back-up contraceptive method.
Choice A is wrong because starting OCs on Sunday after the period begins may leave a gap of several days when the client is not protected from pregnancy.They would need to use a back-up method for the first seven days of taking OCs.
Choice C is wrong because starting OCs on day five of the menstrual cycle may also leave a gap of unprotected days.The client would need to use a back-up method for the first seven days of taking OCs.
Choice D is wrong because starting OCs on day fourteen of the menstrual cycle is too late and may not prevent ovulation.The client would need to use a back-up method for the first seven days of taking OCs.
A nurse is reviewing laboratory results for a female client who takes oral contraceptives (OCs).
Which of the following findings should indicate to the nurse that OCs are having an adverse effect on this client?
Explanation
The correct answer is choice B. Increased serum potassium level.Oral contraceptives can affect the levels of various electrolytes in the blood, such as sodium, potassium, calcium and magnesium.According to one study, oral contraceptives can increase the levels of serum copper, iron, calcium and cadmium, and decrease the levels of serum zinc, selenium, phosphorus and magnesium.
Therefore, a high serum potassium level can indicate an adverse effect of oral contraceptives on this client.
Choice A is wrong because oral contraceptives do not decrease serum glucose level.In fact, they can increase the plasma glucose level and insulin response, which can impair glucose tolerance and increase the risk of diabetes.
Choice C is wrong because oral contraceptives do not decrease serum triglyceride level.On the contrary, they can increase the fasting triglyceride level by 13 to 75 percent, which can elevate the risk of cardiovascular disease.
Choice D is wrong because oral contraceptives do not increase serum protein level.They can increase the levels of some apolipoproteins, such as A-I, A-II and B, but these are not the same as total protein.
A nurse is providing education to a patient about the benefits of injectable progestins.
Which of the following statements made by the patient indicates a need for further teaching?
Explanation
The correct answer is choice B.The patient should receive the injection withinsevendays after delivery if breastfeeding, not five.Injectable progestins are a type of hormonal contraception that prevent ovulation and thicken cervical mucus.They are given by a health professional every 12 weeks.
Choice A is wrong because injectable progestins may cause bone mineral loss with long-term use, so the patient should be aware of this risk.
Choice C is wrong because injectable progestins may cause decreased bleeding or amenorrhea in some women, which is not harmful but may be unexpected.
Choice D is wrong because injectable progestins are given every three months, not four times per year.
A nurse is caring for a patient who uses a contraceptive vaginal ring.
Which of the following symptoms should the nurse instruct the patient to report immediately?
No explanation
A nurse is providing education to a patient about implantable progestin.
Which of the following statements made by the patient indicates a need for further teaching?
Explanation
The correct answer is choice C. The patient needs further teaching if they think that the implant can be inserted immediately after childbirth.According to Mayo Clinic, the implant should not be inserted until at least 21 days after giving birth, or until the milk supply is well established if breastfeeding.
Inserting the implant too soon may increase the risk of blood clots or decrease milk production.
Choice A is correct because condoms are still needed to protect against STIs, even if using the implant as a birth control method.Choice B is correct because irregular and unpredictable menstruation is a common side effect of the implant.Choice D is correct because the implant can prevent pregnancy for up to three years.
A nurse is caring for a patient who is using an intrauterine device (IUD) for contraception.
Which of the following symptoms is a potential adverse effect of the copper IUD?
Explanation
The correct answer is choice B.Spotting and irregular bleeding are potential adverse effects of the copper IUD.The copper IUD works by creating a toxic environment for sperm and eggs in the uterus and cervix, but it does not affect the hormones that regulate the menstrual cycle.Therefore, it can cause changes in bleeding patterns, such as heavier, longer or more painful periods.
Choice A is wrong because decreased bone density is not a side effect of the copper IUD.It is a possible side effect of hormonal IUDs that contain progestin, which can lower estrogen levels and affect bone health.
Choice C is wrong because mood changes are not a side effect of the copper IUD.They are more likely to occur with hormonal methods of birth control that affect the levels of estrogen and progesterone in the body.
Choice D is wrong because headaches are not a side effect of the copper IUD.They are also more common with hormonal methods of birth control, especially those that contain estrogen.
A nurse is providing education to a patient about the use of intrauterine devices (IUDs).
Which of the following statements made by the patient indicates a need for further teaching?
Explanation
The correct answer is choice D. Choice D is wrong because it implies that the IUD affects fertility, which is not true.According to the NHS website, “Your fertility will return to normal as soon as the IUD is taken out.” The other choices are correct because:
- Choice A is correct because the copper IUD does not contain any hormones and can be used by people who cannot or do not want to use hormonal methods of contraception.
- Choice B is correct because a pregnancy test is needed before inserting an IUD to make sure that the person is not already pregnant.
- Choice C is correct because the hormonal IUD can reduce menstrual pain and heavy bleeding by thinning the lining of the uterus and thickening the cervical mucus.
Therefore, choice D indicates a need for further teaching.
A nurse is teaching a client who is starting medroxyprogesterone injections for contraception.
Which of the following statements by the client indicates a need for further teaching?
Explanation
The correct answer is choice C.“I can start the injections right after I give birth if I am not breastfeeding.” This statement indicates a need for further teaching because medroxyprogesterone injections should not be started until at leastsix weeksafter giving birth if the woman is not breastfeeding.Starting the injections earlier may increase the risk ofbleeding,blood clotsanddecreased milk production.
Choice A is correct because medroxyprogesterone injections are given every12 to 13 weeksfor contraception.
Choice B is correct because medroxyprogesterone injections may causebone lossover time, and calcium supplements may help prevent this.
Choice D is correct because medroxyprogesterone injections often reduce or stop menstrual bleeding by suppressing ovulation and thinning the lining of the uterus.
A nurse is caring for a client who has a history of breast cancer and cardiovascular disease and is seeking advice on contraception.
Which of the following contraceptive methods should the nurse recommend as the safest option for this client?
Explanation
The correct answer is choice C. Copper intrauterine device.This is because copper intrauterine devices do not contain hormones and are therefore safe for women with a history of breast cancer and cardiovascular disease.
Some possible explanations for the other choices are:
- Choice A. Injectable progestins.This is wrong because injectable progestins may increase the risk of breast cancer in women with the BRCA1 geneand may also worsen hypertension and dyslipidemia.
- Choice B. Contraceptive vaginal ring.This is wrong because contraceptive vaginal rings contain estrogen and progestin, which may increase the risk of thromboembolic events, stroke, and myocardial infarction in women with cardiovascular disease.
- Choice D. Combined oral contraceptives.This is wrong because combined oral contraceptives also contain estrogen and progestin, which have the same risks as contraceptive vaginal rings for women with cardiovascular disease.Additionally, combined oral contraceptives may interact with some medications used to treat chronic conditions and reduce their effectiveness.
A nurse is reviewing the laboratory results of a client who is taking medroxyprogesterone injections for contraception.
Which of the following findings should the nurse report to the provider?
Explanation
The correct answer is choice A. Elevated liver enzymes.Medroxyprogesterone injections can cause liver damage and impair its function.Elevated liver enzymes are a sign of liver injury and should be reported to the provider immediately.
Choice B is wrong because decreased hemoglobin is not a common side effect of medroxyprogesterone injections.
Decreased hemoglobin can indicate anemia, which can have many causes unrelated to medroxyprogesterone injections.
Choice C is wrong because increased platelets are not a common side effect of medroxyprogesterone injections.
Increased platelets can indicate inflammation, infection, or cancer, which can have many causes unrelated to medroxyprogesterone injections.
Choice D is wrong because decreased potassium is not a common side effect of medroxyprogesterone injections.
Decreased potassium can indicate dehydration, diarrhea, vomiting, or diuretic use, which can have many causes unrelated to medroxyprogesterone injections.
A nurse is providing discharge instructions to a client who has just received her first medroxyprogesterone injection for contraception.
Which of the following information should the nurse include in the teaching?
Explanation
The correct answer is choice A."You may experience weight gain as a side effect of the injection."
Choice B is wrong because you do not need to use a barrier method of contraception for the first week after the injection.Medroxyprogesterone injection provides contraception for three months and works mainly by stopping the release of an egg from the ovary (ovulation).
Choice C is wrong because you should not massage the injection site to promote absorption of the medication.
Massaging the injection site may cause irritation or pain.You should also avoid rubbing or scratching the injection site for a few days after receiving the injection.
Choice D is wrong because you may not resume fertility as soon as you stop the injections.
There may be a delay in your return to normal fertility after you finish using medroxyprogesterone injection.It might take 10 months or more before you begin ovulating again.
A nurse is counseling a client who is breastfeeding and wants to use medroxyprogesterone injections for contraception.
Which of the following statements should the nurse make?
Explanation
The correct answer is choice D.“You should wait until your baby is 6 weeks old before starting the injections.” This is because medroxyprogesterone may pass into breast milk and cause side effects in a child who is breastfed.The product labeling states that it should be started no sooner than 6 weeks postpartum, based on data submitted for product approval.
The World Health Organization also recommends that injectable depot medroxyprogesterone acetate should not be used before 6 weeks postpartum.
Choice A is wrong because starting the injections immediately after delivery could interfere with the exclusivity or duration of lactation, and could affect the newborn infant adversely because of slower metabolism of the drug than older infants.
Choice B is wrong because waiting until the baby is 6 months old is unnecessary and could expose the mother to a higher risk of unintended pregnancy.
Choice C is wrong because medroxyprogesterone has not been known to cause any decrease in milk supply while using the injections
Here are some possible ATI nursing school MCQ questions with a long stem of at least 15 words, from the text you provided:.
A nurse is caring for a client who has a copper IUD for contraception.
The nurse should instruct the client to report which of the following signs of a possible complication?
Explanation
The correct answer is choice C.Foul-smelling vaginal discharge is a sign of a possible infection, which can be a complication of using a copper IUD.
The nurse should instruct the client to report this symptom and seek medical attention.
Choice A is wrong because increased menstrual pain and bleeding are common side effects of copper IUDs, especially in the first 3-6 months after insertion.
They are not necessarily signs of a complication.
Choice B is wrong because irregular spotting or bleeding are also common side effects of copper IUDs.
They are not necessarily signs of a complication.
Choice D is wrong because a change in string length is not a sign of a complication.
The string length may vary depending on the position of the cervix and uterus.The client should check the string length regularly and report any missing or protruding strings, which could indicate displacement of the IUD.
A nurse is reinforcing teaching with a client who is considering a progestin-releasing IUD for contraception.
Which of the following benefits should the nurse include in the teaching?
Explanation
The correct answer is choice B. It can decrease menstrual loss and dysmenorrhea.According to, progestin IUDs can make your periods lighter and less painful.
This is a benefit for women who have heavy or painful periods.
Choice A is wrong because it can prevent Asherman’s syndrome.
Asherman’s syndrome is a condition where scar tissue forms in the uterus, which can cause infertility or miscarriage.
Progestin IUDs do not prevent this condition.
Choice C is wrong because it can remain in the uterus for up to 10 years.
Progestin IUDs have different durations of effectiveness depending on the type and brand.For example, Liletta can last up to 8 years, Mirena up to 7 years, and Skyla/Kyleena up to 5 years.
Choice D is wrong because it can protect against sexually transmitted infections.
Progestin IUDs do not protect against STIs.
You should use condoms with new partners to prevent STIs
A nurse is preparing to insert an IUD for a client who is nulliparous and has a negative pregnancy test.
Which of the following actions should the nurse take before the insertion?
Explanation
The correct answer is choiceD.
All of the above.
Here is why:
- Choice A is correct because obtaining informed consent from the client is a necessary step before any invasive procedure, including IUD insertion.
- Choice B is correct because performing a Pap smear and cervical culture can help screen for cervical cancer and sexually transmitted infections, which are contraindications for IUD use.
- Choice C is correct because administering an analgesic medication can help reduce the pain and discomfort associated with IUD insertion, especially in nulliparous women who have a smaller cervical diameter.
- Choice D is correct because it includes all of the above actions, which are recommended by the American College of Obstetricians and Gynecologists (ACOG) for IUD insertion in nulliparous women.
- Choice A is wrong if it is the only action taken, because it does not address the other aspects of IUD insertion such as screening and pain management.
- Choice B is wrong if it is the only action taken, because it does not ensure the client’s consent and comfort during the procedure.
- Choice C is wrong if it is the only action taken, because it does not verify the client’s eligibility and suitability for IUD use.
A nurse is reviewing the mechanism of action of IUDs with a group of nursing students.
Which of the following statements by a student indicates an understanding of the teaching?
Explanation
All of the above.
This is because IUDs have multiple mechanisms of action that prevent fertilization and implantation of the ovum.According to the search results, some of these mechanisms are:
- IUDs immobilize sperm and interfere with their migration from the vagina to the fallopian tubes.This is because copper ions released from copper IUDs are toxic for spermatozoa and impair their motility and viability.Hormonal IUDs also thicken the cervical mucus, which blocks sperm from entering the uterus.
- IUDs speed up the transport of the ovum through the fallopian tube.This is because IUDs induce a local inflammatory reaction in the endometrium, which affects the signaling between the uterus and the ovary and alters the tubal motility.This reduces the chances of fertilization by shortening the time window for sperm-egg interaction.
- IUDs inhibit fertilization and cause lysis of the blastocyst.This is because IUDs affect the function or viability of gametes, decreasing the rate of fertilization and lowering the chances of survival of any embryo that may be formed.IUDs also interfere with implantation of the fertilized ovum by creating a hostile environment in the uterine cavity.
Choice A is wrong because it only describes one mechanism of action of IUDs, not all of them.
Choice B is wrong because it only describes another mechanism of action of IUDs, not all of them.
Choice C is wrong because it only describes yet another mechanism of action of IUDs, not all of them.
A nurse is caring for a client who has an IUD and reports abdominal pain during sexual intercourse.
Which of the following actions should the nurse take first?
Explanation
The correct answer is choice A. The nurse should assess for signs of pelvic inflammatory disease (PID), which is an infection of the female reproductive organs that can be caused by sexually transmitted bacteria.PID can cause abdominal pain during sexual intercourse, as well as other symptoms such as fever, unusual vaginal discharge, and bleeding between periods.PID can lead to serious complications such as infertility and ectopic pregnancy if left untreated.
Choice B is wrong because checking the string length of the IUD is not a priority action.The string length may change due to normal variations in the position of the uterus and cervix, and does not indicate a problem with the IUD.However, if the string is missing or longer than usual, it may suggest that the IUD has moved or expelled, and the client should see a provider.
Choice C is wrong because advising the client to use a backup contraceptive method is not a priority action.The IUD is a highly effective form of birth control that does not require additional methods unless the client wants to prevent STIs.However, if the client has an STI that causes PID, using a condom may help prevent further infection and transmission.
Choice D is wrong because scheduling an appointment for IUD removal is not a priority action.The IUD does not cause PID, but it may increase the risk of infection shortly after insertion, especially if the client has an STI.The risk of PID from IUD use is very low (less than 1%) and usually disappears after 3 weeks of placement.Removing the IUD may not cure PID and may expose the client to unwanted pregnancy.
A nurse is caring for a client who desires an intrauterine device (IUD) for contraception.
Which of the following findings is a contraindication for the use of this device?
Explanation
The correct answer is choice A.Mennorhagia is a contraindication for the use of an intrauterine device (IUD) for contraception because it can cause heavy or prolonged menstrual bleeding.This can lead to anemia, infection, or expulsion of the device.
Choice B is wrong because ovarian cysts are not a contraindication for IUD use.They are usually benign and do not interfere with the placement or function of the device.
Choice C is wrong because fibrocystic breast disease is not a contraindication for IUD use.It is a common condition that causes benign lumps in the breast tissue and does not affect the hormonal balance or the risk of infection.
Choice D is wrong because endometriosis is not a contraindication for IUD use.In fact, some types of IUDs that release progestin can help reduce the symptoms of endometriosis by thinning the endometrial lining and suppressing ovulation.
A nurse is caring for a client who has an intrauterine device (IUD) in place and reports lower abdominal pain and fever for 2 days.
Which of the following actions should the nurse take?
Explanation
The correct answer is choice D. Refer the client to a provider for evaluation.Lower abdominal pain and fever for 2 days can indicate a serious complication of IUD use, such as pelvic inflammatory disease (PID) or perforation of the uterus.
These conditions require prompt medical attention and possible removal of the IUD.
Choice A is wrong because ibuprofen may not be enough to relieve the pain and may mask the signs of infection.
Choice B is wrong because avoiding sexual intercourse will not treat the underlying cause of the symptoms and may delay seeking medical help.
Choice C is wrong because a urine specimen may not be sufficient to diagnose the problem and may miss other possible causes of lower abdominal pain and fever, such as ectopic pregnancy or appendicitis.
A nurse is reinforcing teaching with a client who has an intrauterine device (IUD) in place and asks how it prevents pregnancy.
Which of the following responses should the nurse make?
Explanation
The correct answer is choice B. It creates a local inflammatory response that impairs implantation.This means that the IUD makes the lining of the uterus less suitable for a fertilized egg to attach to it.
Choice A is wrong because it describes how hormonal IUDs work, not copper IUDs.Hormonal IUDs release hormones that thicken cervical mucus and prevent ovulation.
Choice C is wrong because it describes how tubal ligation works, not IUDs.Tubal ligation is a surgical procedure that blocks or cuts the fallopian tubes, which prevents sperm from reaching an egg.
Choice D is wrong because it implies that all of the above choices are correct, which they are not.
Only choice B is correct for copper IUDs.
A nurse is caring for a client who has an intrauterine device (IUD) in place and reports missing her menstrual period this month.
Which of the following actions should the nurse take first?
Explanation
The correct answer is choice A. Perform a pregnancy test.An IUD is a form of birth control that is inserted into the uterus to prevent pregnancy, but it is not 100% effective.If a client with an IUD misses a menstrual period, the first action the nurse should take is to rule out pregnancy by performing a pregnancy test.This is because pregnancy with an IUD can have serious complications, such as ectopic pregnancy, infection, miscarriage or preterm labor.
Choice B is wrong because palpating for uterine enlargement is not a reliable way to diagnose pregnancy, especially in the early stages.It can also cause discomfort or bleeding for the client.
Choice C is wrong because assessing for signs of ectopic pregnancy is not the first action the nurse should take.
Ectopic pregnancy is a possible complication of pregnancy with an IUD, but it is not very common.The nurse should first confirm if the client is pregnant before looking for signs of ectopic pregnancy, such as abdominal pain, vaginal bleeding or shoulder pain.
Choice D is wrong because instructing the client to remove the IUD is not appropriate or safe.
The client should not attempt to remove the IUD by themselves, as this can cause injury or infection.The nurse should refer the client to an OB-GYN if they are pregnant with an IUD or if they want to remove the IUD for any reason.
A nurse is reinforcing teaching with a client who wants to use an intrauterine device (IUD) for contraception but has concerns about its safety and effectiveness.
Which of the following information should the nurse include in the teaching?
Explanation
The nurse should include all of the following information in the teaching:
- The typical failure rate for IUDs is 1% to 3% per year.
- This means that out of 100 women who use an IUD for a year, one to three may get pregnant.
- The risk of pelvic inflammatory disease (PID) is highest in the first 6 weeks after insertion.
- PID is an infection of the reproductive organs that can cause infertility, chronic pain, or ectopic pregnancy.
- The risk of PID is higher if the woman or her partner has multiple sexual partners or a sexually transmitted infection (STI).
- The IUD can be inserted at any time during the menstrual cycle.
- However, some doctors may prefer to insert it during or right after the period, when the cervix is more open and the chance of pregnancy is lower.
Choice A is wrong because it only states one piece of information that the nurse should include in the teaching.
Choice B is wrong because it only states one piece of information that the nurse should include in the teaching.
Choice C is wrong because it only statesone piece of information that the nurse should include in the teaching
A nurse is teaching a client who is considering female sterilization as a contraceptive method.
Which of the following statements by the nurse is appropriate?
Explanation
The correct answer is choice A.“You will need to use another form of birth control for 3 months after the procedure.” This is because it takes time for the remaining sperm in the reproductive tract to be cleared out after female sterilization.
Therefore, another contraceptive method is needed to prevent pregnancy during this period.
Choice B is wrong because female sterilization does not increase the risk of ovarian cancer.In fact, some studies have suggested that it may lower the risk of ovarian and endometrial cancers.
Choice C is wrong because female sterilization does not affect the menstrual cycle or sexual function.The ovaries still produce hormones and eggs as normal, but the eggs are absorbed by the body instead of travelling to the uterus.
Choice D is wrong because female sterilization is intended to be a permanent method of contraception and reversal is not guaranteed to be successful.Reversal surgery is also more complicated and expensive than the original procedure.Therefore, women who choose female sterilization should be sure that they do not want any more children in the future.
A nurse is caring for a client who had a vasectomy 2 days ago.
Which of the following instructions should the nurse include in the discharge teaching?
Explanation
The correct answer is choice B.The client should wear scrotal support for at least 48 hours after the procedure to decrease pain and swelling, and protect the wound.
Some possible explanations for the other choices are:
- Choice A is wrong because the client should avoid sexual activity for at least 1 week, not 4 weeks, after the procedure.The client will not be sterile right away and will need to use another form of birth control until the sperm count is zero.
- Choice C is wrong because the client should apply ice packs to the scrotum for at least 2 days, not 72 hours, after the procedure.Ice helps prevent tissue damage and decrease swelling and pain.
- Choice D is wrong because the client should not take aspirin for pain relief after the procedure, as it can increase the risk of bleeding.The client can take nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen or naproxen instead.
A nurse is reviewing the medical record of a client who is scheduled for a bilateral tubal ligation.
Which of the following findings is a contraindication for this procedure?
Explanation
The correct answer is choice B. The client has a positive pregnancy test result.
This is a contraindication for bilateral tubal ligation because the procedure is a permanent form of contraception and should not be performed on a pregnant woman.
The client should be counseled about other options for birth control or termination of pregnancy.
Choice A is wrong because a history of pelvic inflammatory disease is not a contraindication for bilateral tubal ligation.It may increase the risk of complications from the surgery, such as infection or adhesions, but it does not prevent the procedure from being performed.
Choice C is wrong because a family history of breast cancer is not a contraindication for bilateral tubal ligation.It may affect the client’s decision to undergo the procedure, as some studies have suggested that tubal ligation may reduce the risk of ovarian cancer, which is associated with breast cancer.
However, this is not a medical reason to avoid the surgery.
Choice D is wrong because a history of endometriosis is not a contraindication for bilateral tubal ligation.
It may cause pelvic pain or infertility, but it does not affect the effectiveness or safety of the procedure.In fact, some studies have shown that tubal ligation may improve the symptoms of endometriosis by reducing retrograde menstruation.
A nurse is providing preoperative teaching to a client who is undergoing a transcervical sterilization procedure.
Which of the following information should the nurse include?
Explanation
The correct answer is choice A.The procedure involves inserting flexible agents into your fallopian tubes.These agents cause tissue to grow around them and block the tubes, preventing pregnancy.
Choice B is wrong because the procedure does not require general anesthesia or an operating room.It can be done in an outpatient facility with local anesthesia.
Choice C is wrong because the procedure does not make you sterile immediately after it is done.
It takes about 3 months for the tissue to grow and occlude the tubes.You need to use another form of contraception during this time and have a test to confirm the tubal blockage.
Choice D is wrong because the procedure does not affect your hormone levels or menstrual cycle.It only blocks the fallopian tubes, not the ovaries or uterus.
A nurse is counseling a client who had a vasectomy 6 weeks ago and wants to know if he is sterile yet.
Which of the following responses should the nurse make?
Explanation
The correct answer is choice A.“You need to have a sperm count test to confirm your sterility.”
A sperm count test is a semen analysis that measures the number of sperm in the ejaculate.
It is the only way to verify that a vasectomy has been successful and that the man is sterile.A man is considered sterile when his sperm count is zero or below 100,000 non-motile sperm per sample.
Choice B is wrong because the number of ejaculations does not guarantee sterility.Some sperm may still be present in the severed vas deferens for months after a vasectomy.
Choice C is wrong because the duration of contraception use after a vasectomy depends on the sperm count test results, not on a fixed time period.It may take more or less than 3 months for a man to become sterile after a vasectomy.
Choice D is wrong because a repeat vasectomy is unnecessary and ineffective to ensure sterility.A vasectomy is a permanent birth control method that rarely fails or reverses.
A nurse is caring for a client who requests information about female sterilization (bilateral tubal ligation).
Which of the following statements by the nurse is appropriate? (Select all that apply.).
Explanation
The correct answer is choice B and E.Bilateral tubal ligation (BTL) is a permanent form of contraception that involves cutting, tying or blocking the fallopian tubes to prevent pregnancy.It can be performed within 24 hours following childbirthand it is immediately effective.
Choice A is wrong because BTL does not provide protection against sexually transmitted infections (STIs).
People who have BTL should still use condoms to prevent STIs.
Choice C is wrong because BTL does not increase the risk for an ectopic pregnancy.
An ectopic pregnancy is when a fertilized egg implants outside the uterus, usually in the fallopian tube.
BTL prevents fertilization by blocking the passage of eggs and sperm.
Choice D is wrong because BTL does not require abdominal surgery with general anesthesia.
BTL can be done using different methods, such as laparoscopy, minilaparotomy, or hysteroscopy.
These methods use small incisions or no incisions at all and can be done with local or regional anesthesia.
A nurse in an outpatient clinic is providing teaching to a male client who is scheduled for vasectomy with local anesthesia in 1 week and states that he plans on going hunting with his friends on day 2 following his surgery and asks if this will be okay? Which of the following responses should the nurse make?
Explanation
The correct answer is choice C) “No, you should avoid activities that could cause straining or trauma until healing occurs.” This is because a vasectomy is a surgical procedure that involves cutting and sealing the tubes that carry sperm from the testicles to the semen.It requires some time for recovery and healing, and strenuous activities like hunting could increase the risk of bleeding, infection, or reopening the incisions.
Choice A) “Yes, this activity level will be fine.” is wrong because it contradicts the medical advice to rest and avoid heavy lifting or exercise for at least a week after a vasectomy.
Choice B) “No, you should avoid sexual intercourse until your follow-up visit.” is wrong because it is too restrictive.Sexual intercourse can be resumed after a few days or when the pain and swelling subside, as long as contraception is used until the semen is confirmed to be sperm-free.
Choice D) “Yes, but you should wear tight-fitting underwear.” is wrong because it is not enough to prevent complications.Tight-fitting underwear can help support the scrotum and reduce discomfort, but it does not eliminate the need to avoid activities that could cause straining or trauma.
Exams on Contraception
Custom Exams
Login to Create a Quiz
Click here to loginContraception - 1
Lessons
 Naxlex
Just Now
Naxlex
Just Now
Login to View Contraception Study Video
Notes Highlighting is available once you sign in. Login Here.
Objectives
- Understand what contraception is and be able to identify the various methods.
- Explain the importance of regular refitting for diaphragm use.
- Discuss the necessity of using spermicide with a diaphragm and its duration of use.
- Identify the potential side effects of hormonal contraception and their implications.
- List the contraindications for oral contraceptive pill use.
- Explain the need for adequate calcium and vitamin D intake while using Depo-Provera.
- Discuss the potential risks associated with the use of an intrauterine device (IUD).
- Attempt over 50 Practice Questions on the topic to reinforce learning
Introduction
Contraception refers to the methods used to prevent pregnancy by blocking the fertilization of a female egg by male sperm.
The use of contraception is crucial in family planning, as it allows individuals to control their reproductive choices and avoid unintended pregnancies.
Timing is critical when it comes to contraception.
The human ovum can be fertilized within 24 hours after ovulation, while motile sperm can survive in the female reproductive system for an average of 48-72 hours.
Therefore, the use of contraception can be an effective way to prevent pregnancy.
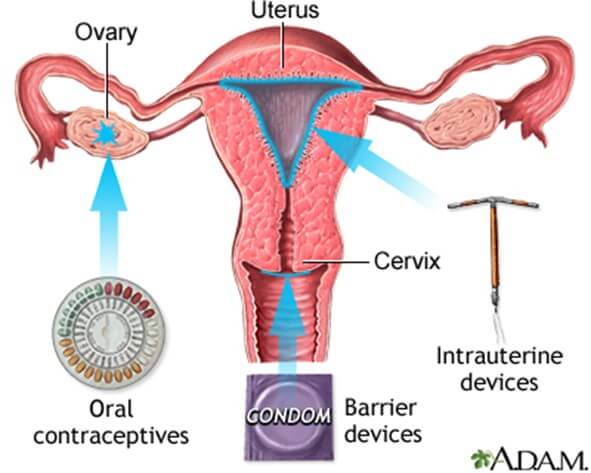
There are various methods of contraception, which can be broadly categorized into natural family planning, barrier, hormonal, intrauterine, and surgical methods.
- Natural Family Planning: This method involves monitoring a woman's menstrual cycle and avoiding intercourse during her fertile window, which is the period when she is most likely to get pregnant.
- Barrier Methods: These methods prevent the sperm from reaching the egg by creating a physical barrier. Examples include condoms, diaphragms, and cervical caps.
- Hormonal Methods: These methods use hormones to prevent pregnancy by inhibiting ovulation or thickening the cervical mucus to prevent sperm from entering the uterus. Examples include birth control pills, patches, and injections.
- Intrauterine Methods: These methods involve placing a device inside the uterus to prevent pregnancy. Examples include intrauterine devices (IUDs) and hormonal implants.
- Surgical Methods: These methods involve permanent sterilization to prevent pregnancy. Examples include tubal ligation (for females) and vasectomy (for males).
Natural Methods of contraception
A. Abstinence
o This method involves avoiding sexual intercourse during the fertile period of a woman's menstrual cycle.
o It is also known as the rhythm method and requires an understanding of the menstrual cycle and fertility awareness.
o Abstinence during this period can greatly reduce the chances of pregnancy.
o However, it is important to note that abstinence is not 100% effective and there is still a risk of pregnancy if sexual intercourse occurs.
B. Coitus Interruptus
o This method involves withdrawing the penis before ejaculation to prevent the release of sperm into the woman's body.
o However, it is important to be aware of pre-ejaculatory fluid which can contain sperm and increase the risk of pregnancy.
o Coitus interruptus is one of the least effective methods of birth control, with a failure rate of around 22%.
C. Calendar Rhythm Method
o This method involves keeping track of your menstrual cycle to determine when are the fertile days and when are the non-fertile days.
o To use this method, maintain a diary of at least 6 menstrual cycles, then calculate the fertile days.
o Fertile days can be approximately calculated by subtracting 18 days from the number of days in the shortest menstrual cycle for the start of the fertile period and subtracting 11 days from the number of days in the longest cycle for the end of the fertile period.
o The window of fertility is typically the 14 days prior to the onset of the next menstrual cycle.
o Therefore, sexual intercourse should be avoided during the fertile period to prevent pregnancy.
o Conversely, sexual intercourse during the fertile period can facilitate conception.
o The effectiveness of this method heavily relies on the individual being able to accurately track their menstrual cycle.
o This method has an estimated failure rate of 24% in the first year of use according to a study by The American College of Obstetricians and Gynecologists.
D. Standard Days Method
o This method is a modification of the Calendar Rhythm Method and is typically aided by cycle beads or smartphone apps.
o Red beads represent the first day of the menstrual cycle, brown beads represent non-fertile days, and white beads represent the fertile period.
o This method can be useful for people with regular menstrual cycles, with intervals between 26 and 32 days.
o However, this method is less accurate if the menstrual cycle is not regular or falls outside the appropriate duration.
o According to a trial published by the World Health Organization, the Standard Days Method has a typical use failure rate of 5.3%
E. Basal Body Temperature (BBT) Method
o This is a symptom-based method that measures the temperature of the body at rest to determine the fertile window for facilitating or avoiding conception.
o Before ovulation, the body temperature decreases slightly, and then rises during ovulation due to hormonal changes.
o To use this method, take your temperature immediately after waking up and before getting out of bed. If you work nights, take your temperature after waking up from your longest sleep cycle.
o The first day that your temperature drops or elevates is considered the first fertile day and it extends through three consecutive days of temperature elevations. You can use this method with the calendar method to increase its effectiveness.
o The normal range of BBT is between 36.1°C to 36.4°C (97°F to 97.6°F) before ovulation and 36.4°C to 37°C (97.6°F to 98.6°F) after ovulation.
F. Cervical Mucus Ovulation Detection Method
o This is a symptom-based method that involves analyzing the cervical mucus to identify the fertile period.
o After ovulation, the mucus becomes thin and flexible due to estrogen and progesterone, allowing for sperm viability and motility. The mucus stretching between fingers is greatest during ovulation (spinnbarkeit sign).
o The fertile period begins when the mucus is thin, slippery, and clear, and lasts until four days after the last day of cervical mucus having this appearance.
o To use this method, begin examining your mucus from the last day of your menstrual cycle, using your fingers and tissue paper. A stretchy consistency of egg whites is a good example of how cervical mucus will look during ovulation.
G. Two-day Method
o This is a symptom-based method that checks for vaginal secretions daily to determine the end of the fertile window.
o If vaginal secretions are present for two days in a row, you should avoid unprotected intercourse to prevent pregnancy.
o If you have no vaginal secretions for two consecutive days, the fertile period has passed and you can have unprotected intercourse without risk of pregnancy.
o This method has a typical use failure rate of 14% per year.
o The window of fertility is typically the 14 days prior to the onset of the next menstrual cycle.
o Therefore, sexual intercourse should be avoided during the fertile period to prevent pregnancy.
o Conversely, sexual intercourse during the fertile period can facilitate conception.
o The effectiveness of this method heavily relies on the individual being able to accurately track their menstrual cycle.
Barrier Methods
A. Male condom
o This is a thin sheath that covers the penis during sexual intercourse.
o It can be made of latex, polyurethane, or natural membrane (such as lambskin).

o Only water-soluble lubricants should be used with latex condoms to avoid breakage.
o Male condoms are 98% effective at preventing pregnancy when used correctly and consistently.
B. Female condom
o This is a pouch that lines the inside of the vagina and partially covers the external genitalia.
o It is made of nitrile (a nonlatex synthetic rubber) with flexible rings on both ends that hold it in place.
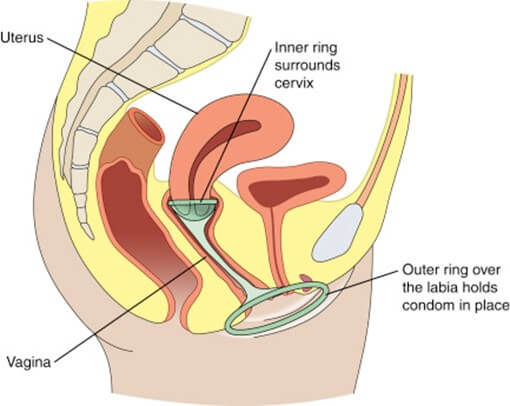
o It is pre-lubricated with a spermicide (a substance that kills sperm).
o Female condoms are 95% effective at preventing pregnancy when used correctly and consistently.
C. Spermicide
o This is a chemical barrier that destroys sperm before they enter the cervix (the opening of the uterus).
o It also makes the vaginal flora more acidic, which inhibits sperm motility.
o Spermicide should be inserted into the vagina 15 minutes before sexual intercourse and is only effective for one hour.
o It should not be removed until six hours after intercourse, but no more than 24 hours later.
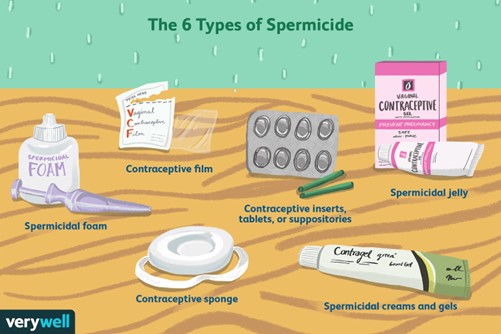
o Spermicide can come in different preparations, such as suppositories, foams, creams, gels, or films.
o Spermicide alone is 72% effective at preventing pregnancy when used correctly and consistently.
o Spermicide is contraindicated (not recommended) in people with cervical infections or allergies to its ingredients.
o Some spermicides contain nonoxynol-9 (N-9), which can cause lesions (sores) in the vaginal or rectal lining and increase the risk of HIV transmission if used more than twice a day.
D. Diaphragm
o A diaphragm is a dome-shaped cup that fits snugly over the cervix.
o It acts as a physical barrier to prevent sperm from entering the uterus.
o Its effectiveness is increased with the use of a spermicide or gel that is placed in the dome and around the rim of the diaphragm.
o A diaphragm needs to be properly fitted by a healthcare provider and replaced every two years.
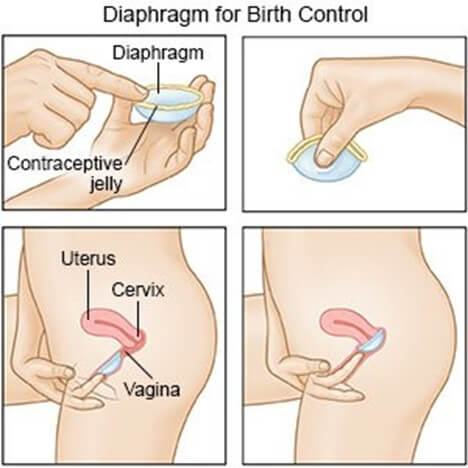
o It also requires proper insertion and removal techniques.
o A woman should empty her bladder prior to insertion and wash the diaphragm with warm water and mild soap after each use.
o A diaphragm is not recommended for people who have a history of toxic shock syndrome (TSS), cystocele, uterine prolapse, or urinary tract infection (UTI).
o Clinical findings of TSS include high fever, faint feeling, drop in blood pressure, watery diarrhea, headache, macular rash, and muscle aches.
E. Cervical Cap
o A cervical cap is a silicone rubber cap that fits tightly around the base of the cervix.
o It also acts as a physical barrier to prevent sperm from entering the uterus.
o It comes in three sizes and needs to be fitted by a health care provider.
o It should be inserted at least 6 hours before intercourse and left in place for at least 6 hours after intercourse, but no more than 48 hours.
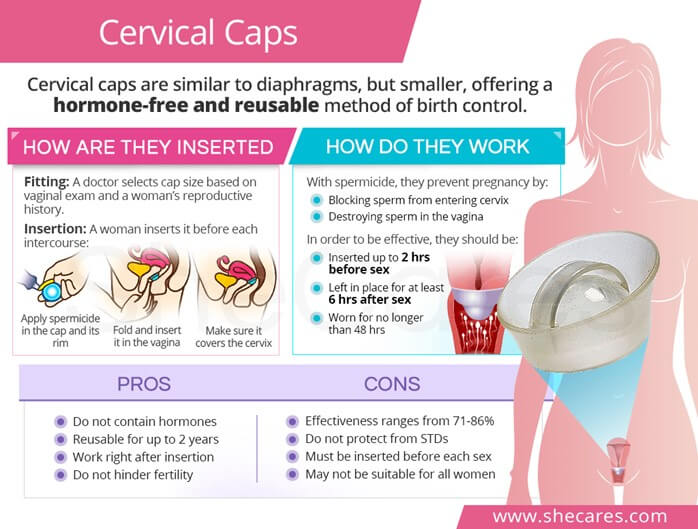 o It should be replaced every two years.
o It should be replaced every two years.
o A cervical cap is not suitable for clients who have abnormal Pap test results or a history of TSS.
F. Contraceptive Sponge
o A contraceptive sponge is a small, round, concave-shaped, polyurethane sponge that contains spermicide.
o It acts as both a physical and a chemical barrier to prevent sperm from entering the uterus.
o It is one-size fits all and does not require fitting by a health care provider.
o It should be moistened with water before insertion and left in place for 6 hours after the last act of intercourse.
o It provides protection for up to 24 hours and can be used for repeated acts of intercourse within that time frame.
Hormonal Methods
A. Combined Oral Contraceptives (COCs) These pills contain estrogen and progestin, which work by:
1. Suppressing ovulation, which prevents the release of an egg from the ovaries.
2. Thickening cervical mucus, which blocks the entry of semen into the uterus.
3. Altering the uterine lining (decidua), which prevents the implantation of a fertilized egg.
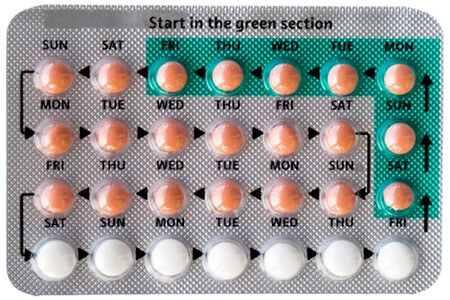
Some important points to remember when using COCs are:
• Routine Pap smears and breast examinations may be needed to check for any abnormalities.
• Consistent and proper use is essential for effectiveness. Follow the instructions on the package and do not skip any pills.
• Report any complications such as chest pain, shortness of breath (SOB), leg pain, headache, vision changes or high blood pressure (HTN) to your health care provider. These could be signs of serious side effects.
• If nausea occurs, take the pill at bedtime or with food.
Some benefits of using COCs are:
• They offer protection against endometrial, ovarian and colon cancer by reducing the exposure of these tissues to hormones.
• They reduce the incidence of benign breast disease, such as fibrocystic changes or lumps.
• They improve acne by lowering the levels of androgens (male hormones) in the body.
• They protect against the development of functional ovarian cysts, which are fluid-filled sacs that form on the ovaries.
Some risks of using COCs are:
• They increase the risk of blood clots (thromboembolism), stroke, heart attack and high blood pressure (HTN) by affecting the blood vessels and clotting factors.
• They increase the risk of gallbladder disease and liver tumors by stimulating the production and secretion of bile and liver enzymes.
• They exacerbate certain conditions such as migraine, epilepsy, asthma, kidney or heart disease by altering the levels of neurotransmitters and electrolytes in the body.
• Their effectiveness decreases when taking medications that affect liver enzymes, such as anticonvulsants (for seizures), antifungals (for fungal infections) or antibiotics (for bacterial infections). These drugs can increase the metabolism and clearance of COCs from the body.
B. Progestin-only Pills (minipill) These pills contain only progestin, which provides the same action as COCs by:
1. Decreasing the chances of fertilization by suppressing ovulation or altering cervical mucus.
2. Decreasing the chances of implantation by thinning or disrupting the uterine lining.
Some important points to remember when using minipills are:
• Another form of birth control may be needed during the first month of use to prevent pregnancy. This is because minipills take longer to become effective than COCs.
• Fewer adverse effects are associated with minipills than with COCs. This is because minipills do not contain estrogen, which is responsible for most of the side effects of COCs.
• Minipills are safer to take while breastfeeding than COCs. This is because minipills do not affect the quantity or quality of breast milk, unlike estrogen.
• Minipills are less effective than COCs. This is because minipills have a lower dose of progestin and a narrower window of time for taking them. If a pill is missed by more than three hours, backup contraception is needed for 48 hours.
• Increased occurrence of ovarian cysts may occur with minipills. This is because minipills do not suppress ovulation as effectively as COCs, which can lead to cyst formation on the ovaries.
• Breakthrough or irregular vaginal bleeding is the most common adverse effect of minipills. This is because minipills cause unpredictable changes in the uterine lining, which can result in spotting or bleeding between periods.
Some factors that decrease the effectiveness of minipills are:
• Taking medications that decrease liver function, such as rifampin (for tuberculosis) or ritonavir (for HIV). These drugs can reduce the absorption and efficacy of progestin in the body.
• Having certain medical conditions that contraindicate minipill use, such as bariatric surgery (weight loss surgery), lupus (an autoimmune disease), severe cirrhosis (liver damage), liver tumors or current or past breast cancer. These conditions can increase the risk of complications or interactions with progestin.
C. Emergency Contraceptive
o Emergency oral contraceptives should be taken within 72 hours after sex to prevent fertilization from taking place.
o They work by inhibiting ovulation and the transportation of sperm.
o An OTC antiemetic should be taken one hour before use, and if menstruation does not begin within 21 days, medical attention is required.
o A copper IUD can be used up to five days after sex for emergency contraception with a prescription.
o Emergency oral contraceptives and IUDs don't terminate an established pregnancy, and contraindicated for those who are already pregnant or have undiagnosed vaginal bleeding.
o The side effects of emergency oral contraception are nausea, heavier menstrual bleeding, lower abdomen pain, fatigue, and headache.
D. Transdermal Contraceptive Patch
o The transdermal contraceptive patch delivers estrogen and progesterone/progestin through the skin, inhibiting ovulation by thickening cervical mucus.
o It should be applied to dry skin on the butt, tummy, upper arm, or torso (except breast area).
o The patch should be replaced once a week and applied on the same day each week for three weeks, with no application on the fourth week.
o The contraceptive patch maintains consistent blood levels of hormones, avoids liver issues, and allows for swimming.
o However, it has the same adverse effects as oral contraceptives and increases the risk of Deep Vein Thrombosis (DVT) and venous thromboembolism slightly higher.
o Skin reactions and breast discomfort are also possible side effects.
o The contraceptive patch is contraindicated in the same cases as oral contraceptives and, it is less effective for people over 198lbs.
E. Injectable Progestins (Medroxyprogesterone)
Medroxyprogesterone is an intramuscular or subcutaneous injection given every 11-13 weeks. It inhibits ovulation and thickens cervical mucus. The injection should be started during the first five days of the menstrual cycle and repeated every 11-13 weeks thereafter. For postpartum non-breastfeeding, it should be administered within five days after delivery, and for breastfeeding mothers, it should be given in the sixth week postpartum.

Benefits of Injectable Progestins:
• Requires only four injections per year; Does not impair lactation; Possible absence of period and decreased bleeding; Decrease in uterine cancer risk (long-term use)
Adverse Effects of Injectable Progestins:
• Decreased bone mineral density; Weight gain; Depression; Irregular vaginal spotting; Return to fertility can be delayed for up to 18 months after discontinuation
Contraindications of Injectable Progestins:
• Breast cancer; Cardiovascular disease; Abnormal liver function; Liver tumors; Unexplained vaginal bleeding
• Can impair glucose tolerance for patients with Diabetes Mellitus (DM) and increase diabetes risk
Additional Information on Injectable Progestins:
• Calcium intake and weight-bearing exercise are recommended to prevent osteoporosis
• Do not massage the injection site.
F. Contraceptive Vaginal Ring (Etonogestrel and Ethinyl Estradiol)
The contraceptive vaginal ring is a flexible silicone ring containing etonogestrel and ethinyl estradiol. It should be replaced after three weeks, and a new ring should be inserted within seven days. It should be inserted on the same day of the week each month. If removed for more than four hours, a new ring should be inserted, and a barrier method should be used for seven days.
Benefits:
• Doesn't have to be fitted
• Route increases bioavailability of hormones (lower dose, reducing adverse effects)
Adverse Effects:
• Blood clots; Hypertension (HTN); Stroke; Myocardial Infarction (MI); Vaginal irritation/discomfort; Increased vaginal secretions; Same adverse effects as oral contraceptives; Some users report discomfort during sex (the ring can be removed for up to three hours without compromising effectiveness)
• Prescription required
G. Implantable Progestin
The implantable progestin consists of thin rods of progestin implanted under the skin of the inner upper arm. It suppresses the ovulatory cycle and thickens cervical mucus. Patients should avoid trauma to the area and use condoms for protection from sexually transmitted infections (STIs).
Benefits:
• Continuous for three years
• Reversible
• Inserted immediately after spontaneous/elective abortion, childbirth, while breastfeeding
Adverse Effects:
• Irregular unpredictable menstruation; Mood changes; Headache; Acne; Depression; Decreased bone density; Weight gain; Scarring at the site warrants the need for removal
Contraindications:
• Unexplained vaginal bleeding
• Infection at the site
Additional Information:
• Increased risk for ectopic pregnancy
Intrauterine Methods
A. Intrauterine Device (IUD)
The Intrauterine Device (IUD) releases a chemical that damages sperm, making it one of the most effective Long-Acting Reversible Contraceptive (LARC) methods along with the implant.
It is used by nulliparous and multiparous females and should be monitored monthly after menstruation to check placement.
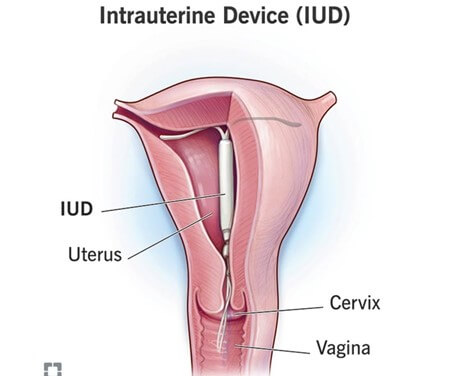
Consent is required, and a pregnancy test, Pap smear, and cervical culture should be negative before usage.
IUD Types There are two types of IUDs: the 3-5 year hormonal IUD (which can decrease menstrual pain and heavy bleeding but may cause spotting, irregular bleeding, headaches, nausea, depression, and breast tenderness) and the 10-year copper IUD (which contains no hormones and is therefore safe for patients cautioned against hormonal birth control methods but may increase menstrual pain and bleeding).
Contraception can be reversed with immediate return to fertility, and it does not interfere with spontaneity.
It is important to report late or abnormal spotting/bleeding, tummy pain during sex, abnormal/foul-smelling vaginal discharge, fever, chills, change in string length, or questioned location.
Usage Recommendations IUDs are best used by clients in monogamous relationships to decrease the risk of sexually transmitted infections.
However, they can cause irregular menstrual bleeding and increase the risk of bacterial vaginosis, pelvic inflammatory disease (PID), uterine perforation, and uterine expulsion.
If pregnancy occurs, the IUD must be removed.
IUDs are contraindicated in patients with an active pelvic infection, abnormal uterine bleeding, or severe uterine distortion.
Surgical Methods
A. Female Sterilization (BTL)
Female sterilization, also known as Bilateral Tubal Ligation (BTL), is the severance and/or blocking of the fallopian tubes, leading to permanent and immediate contraception.
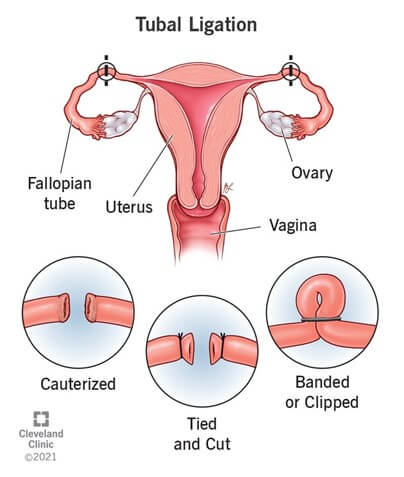
It is normally done within 24-48 hours of birthing and does not affect sex.
Research shows that BTL can decrease the incidence of ovarian cancer.
However, surgical complications can occur, and the procedure is irreversible, leading to the risk of ectopic pregnancy.
B. Male Sterilization (Vasectomy)
Male sterilization, also known as vasectomy, involves the ligation and severance of the vas deferens, leading to a permanent and immediate reduction in fertility.
Scrotal support and moderate activities for a couple of days are recommended after the procedure, and sterility is delayed for approximately 20 ejaculations.
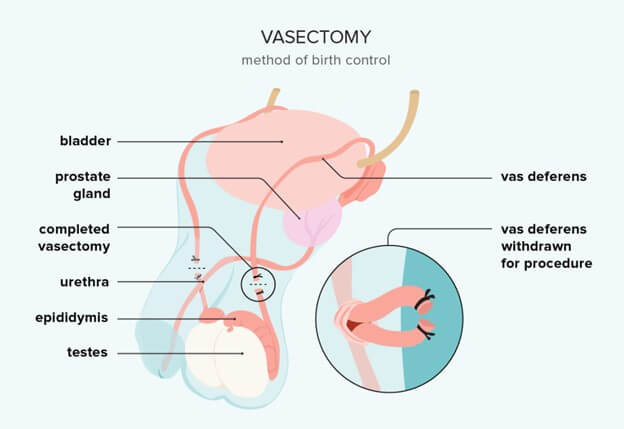
Follow-up for sperm count is required to confirm sterility.
It is possible to reverse vasectomy, but it is a complicated, expensive, and not always successful procedure.
Vasectomy is a safe and simple procedure with rare complications such as bleeding, infection, anesthesia reaction, hematoma at the site, kidney stones, or chronic pain.
Accumulated sperm can cause granulomas, but a vasectomy does not affect sex.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Contraception
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


