Please set your exam date
Physiological And Physical Changes In Pregnancy
Study Questions
Introduction
A nurse is assessing a pregnant client who complains of lower back pain.
Which musculoskeletal change during pregnancy is primarily responsible for this symptom?
Explanation
This is because the growing uterus shifts the center of gravity and causes an increased strain on the back muscles and ligaments.
This can lead to lower back pain during pregnancy.
Choice A is wrong because increased joint laxity is caused by hormonal changes during pregnancy, not by musculoskeletal changes.
Joint laxity can affect the stability of the joints, but not necessarily cause lower back pain.
Choice C is wrong because increased muscle strain is a result of increased spinal curvature, not a cause of it.
Muscle strain can also contribute to lower back pain, but it is not the primary musculoskeletal change during pregnancy.
Choice D is wrong because decreased muscle strength is not a musculoskeletal change during pregnancy, but a possible consequence of reduced physical activity or poor posture.
Muscle strength can affect the support of the spine, but it is not the main factor for lower back pain.
Normal ranges for spinal curvature vary depending on age, sex, and posture, but generally the lumbar lordosis (the inward curve of the lower spine) should be between 20 and 45 degrees.
A nurse is providing dietary recommendations to a pregnant woman.
Which recommendation should the nurse prioritize?
Explanation
Alcohol can cross the placenta and cause fetal alcohol syndrome, which can result in physical and mental defects in the baby.
Alcohol should be avoided throughout pregnancy and breastfeeding.
Choice A is wrong because drinking 2-3 liters of water per day is a general recommendation for healthy adults, not specific to pregnant women.
However, hydration is important for pregnant women to prevent constipation and urinary tract infections.
Choice B is wrong because limiting caffeine intake to 300 milligrams per day is a moderate recommendation for pregnant women, not a priority.
High caffeine intake can increase the risk of miscarriage and low birth weight.
Choice D is wrong because consuming an extra 300-400 calories per day while breastfeeding is a recommendation for lactating women, not pregnant women.
Pregnant women need an extra 340-450 calories per day in the second and third trimesters.
A nurse is educating a pregnant client about sources of folic acid.
Which food group is a good source of folic acid that should be included in the client's diet?
Explanation
The correct answer is choice A. Green leafy vegetables are a good source of folate, which is also known as vitamin
B. Folate is important for healthy cell division and fetal growth and development.
It can also help prevent birth defects and lower homocysteine levels, which are associated with heart disease.
Choice B is wrong because lean meats and poultry are not rich in folate, although they do provide other B vitamins, such as B12 and B. Choice C is wrong because dairy products are not a significant source of folate, although they do provide other nutrients, such as calcium and protein.
Choice D is wrong because whole grains are not a natural source of folate, although they may be fortified with folic acid, which is a synthetic form of folate that is better absorbed by the body.
Normal ranges for folate in blood are 2.7–17.0 nanograms per milliliter (ng/mL) for adults and 5.0–21.0 ng/mL for children.
A nurse is discussing the importance of water intake with a pregnant client.
How many liters of water per day should the nurse recommend for the client?
Explanation
According to the American College of Obstetricians and Gynecologists (ACOG) and the Institute of Medicine, pregnant women should drink on average about 10 8-ounce cups of water or other beverages each day.
This is equivalent to about 2.4 liters of water per day.
However, this amount may vary depending on the individual’s body type, activity level, and weather conditions.
Choice A is wrong because 1-2 liters of water per day is not enough for pregnant women.
They need more water to support their increased metabolism, blood volume, and fetal development.
Choice C is wrong because 3-4 liters of water per day may be too much for some pregnant women.
Drinking too much water can cause hyponatremia, a condition where the sodium level in the blood becomes too low.
This can lead to symptoms such as nausea, headache, confusion, and seizures.
Choice D is wrong because 4-5 liters of water per day is definitely too much for most pregnant women.
This can cause overhydration and hyponatremia, as well as increase the risk of water intoxication, a potentially fatal condition where the brain swells due to excess fluid.
The best way to determine how much water to drink during pregnancy is to monitor the color and frequency of urine, as well as the level of thirst.
The urine should be pale yellow or colorless, and the thirst should be only occasional.
A nurse is educating a pregnant client about caffeine intake during pregnancy.
What is the recommended limit for caffeine intake per day?
Explanation
According to the American Pregnancy Organization and the American College of Obstetricians Gynecologists, pregnant women should limit their caffeine intake to no more than 200 mg per day.
This is because caffeine can cross the placenta and affect the baby’s health, such as increasing the risk of miscarriage or low birth weight.
Choice B is wrong because 300 milligrams of caffeine per day is above the recommended limit for pregnant women.
Choice C is wrong because 400 milligrams of caffeine per day is twice the recommended limit for pregnant women.
Choice D is wrong because 500 milligrams of caffeine per day is more than twice the recommended limit for pregnant women.
To stay within the safe limit of 200 mg of caffeine per day, pregnant women should be aware of the amount of caffeine in different foods and drinks.
For example, one cup of instant coffee has about 60 mg of caffeine, one mug of tea has about 75 mg of caffeine, one can of soft drink has about 40 mg of caffeine, and one can of energy drink has up to 80 mg of caffeine.
Chocolate and decaffeinated coffee also contain small amounts of caffeine.
A nurse is providing education to a pregnant client about alcohol consumption during pregnancy.
What is the recommended approach to alcohol intake?
Explanation
According to the CDC1, there is no known safe amount of alcohol use during pregnancy or while trying to get pregnant.
Alcohol can cause problems for the baby throughout pregnancy, including before a woman knows she is pregnant.
Alcohol use in the first three months of pregnancy can cause the baby to have abnormal facial features.
Growth and central nervous system problems (e.g., low birthweight, behavioral problems) can occur from alcohol use anytime during pregnancy.
Alcohol use during pregnancy can also cause fetal alcohol spectrum disorders (FASDs), which are lifelong physical, behavioral, and intellectual disabilities.
Choice B is wrong because limiting alcohol intake to one drink per day is not safe for the baby.
There is no known safe amount of alcohol use during pregnancy.
Choice C is wrong because limiting alcohol intake to two drinks per week is not safe for the baby.
There is no safe time for alcohol use during pregnancy.
Alcohol can cause problems for the baby throughout pregnancy, including before a woman knows she is pregnant.
Choice D is wrong because consuming alcohol only in moderation is not safe for the baby.
All types of alcohol are equally harmful, including all wines and beer.
Cardiovascular Changes in pregnancy
A nurse is reviewing the cardiovascular changes in pregnancy with a group of nursing students.
Which of the following statements by a student indicates a need for further teaching?
Explanation
The hemoglobin concentrationdecreasesby 15% to 25% during pregnancy due to hemodilution.
This is known as physiological anemia of pregnancy.
Choice A is wrong because the cardiac outputincreasesby 30% to 50% during pregnancy to meet the increased metabolic demands of the mother and fetus.
Choice B is wrong because the blood pressuredecreasesby 10 mmHg during pregnancy due to systemic vasodilation.
It returns to pre-pregnancy levels postpartum.
Choice D is wrong because the venous pressureincreasesduring pregnancy due to increased blood volume and compression of the inferior vena cava by the gravid uterus.
This can lead to lower extremity edema and varicose veins.
Answer and explanation..
The correct answer is choice C.The hemoglobin concentrationdecreasesby 15% to 20% during pregnancy due to the increase in plasma volume.This is known asphysiological anemiaof pregnancy.
Choice A is wrong because the cardiac outputincreasesby 30% to 50% during pregnancy to meet the increased metabolic demands of the mother and fetus.
Choice B is wrong because the blood pressuredecreasesby 10 mmHg during pregnancy due to the decrease in systemic vascular resistance.It gradually returns to pre-pregnancy levels by term.
Choice D is wrong because the venous pressureincreasesduring pregnancy due to the compression of the inferior vena cava by the gravid uterus.This can lead to lower extremity edema and varicose veins.
A nurse is caring for a pregnant client who has a hemoglobin level of 10 g/dL and a hematocrit level of 32%.
Which of the following explanations should the nurse give to the client?
Explanation
These levels are normal due to physiological anemia of pregnancy.Physiological anemia of pregnancy is a reduction in the concentration of hemoglobin or hematocrit in blood due to an increase in blood volume.The normal range of hemoglobin during pregnancy is11 to 16 g/dLand the normal range of hematocrit during pregnancy is32% to 42%.The minimum normal value of hemoglobin is11 g/dLin the first and third trimester and10.5 g/dLin the second trimester.
Choice B is wrong because these levels are not low enough to indicate iron deficiency anemia, which is the most common cause of anemia in pregnancy.Iron deficiency anemia is diagnosed when hemoglobin is below10.5 g/dLor hematocrit is below30%.
Choice C is wrong because these levels are not high enough to indicate polycythemia, which is a rare condition of increased red blood cell mass.Polycythemia is diagnosed when hemoglobin is above18 g/dLor hematocrit is above54%.
Choice D is wrong because these levels are not abnormal enough to indicate hemolysis, which is a destruction of red blood cells.Hemolysis can cause severe anemia and jaundice in pregnancy and may be associated with infections, autoimmune disorders, or blood transfusions.
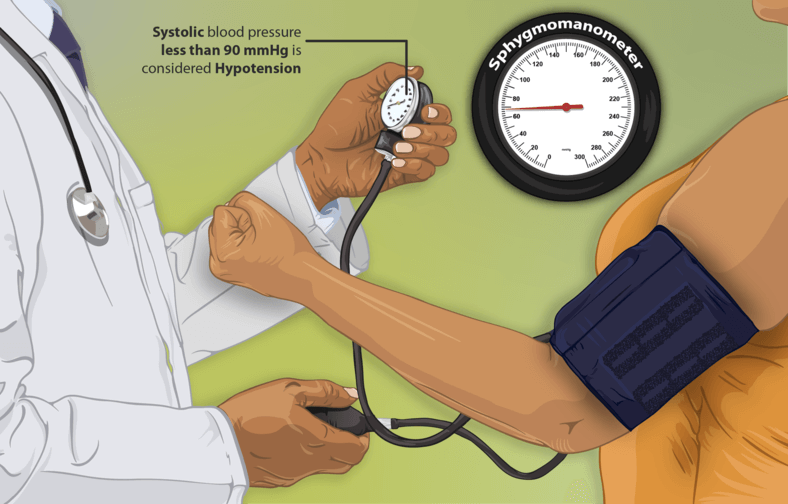
A nurse is caring for a client who is at her first prenatal visit and reports that she has been experiencing episodes of hypotension since becoming pregnant.
Which of the following responses by the nurse is appropriate?
Explanation
This is due to an increase in blood volume caused by pregnancy.According to Healthline, pregnancy causes many changes in a woman’s body, including expanding blood vessels to let blood flow to the uterus.
This can lower the blood pressure, especially in the first and second trimester of pregnancy.
Choice B is wrong because an increase in cardiac output would raise the blood pressure, not lower it.
Cardiac output is the amount of blood pumped by the heart per minute.
Choice C is wrong because an increase in body weight would also raise the blood pressure, not lower it.
Body weight affects the amount of resistance in the blood vessels.
Choice D is wrong because an increase in pressure on the diaphragm would not affect the blood pressure directly.
The diaphragm is a muscle that helps with breathing, not with circulation.
Normal blood pressure levels during pregnancy are less than 120/80 mmHg.Low blood pressure is usually diagnosed when the reading is around 90/60 mmHg or lower.Low blood pressure during pregnancy does not usually cause significant health issues, but it can cause symptoms such as dizziness, fainting, nausea, or fatigue.In some cases, very low blood pressure can be dangerous for the mother and the baby.
Therefore, it is important for pregnant women to have regular check-ups with their doctor and report any symptoms of low blood pressure.
A nurse is educating a pregnant client about the musculoskeletal changes during pregnancy.
Which hormone is primarily responsible for increasing joint laxity?
Explanation
Relaxin is primarily responsible for increasing joint laxity during pregnancy.
Relaxin is a hormone that is produced by the corpus luteum and the placenta, and it helps to soften and widen the cervix and the pubic symphysis for childbirth.Relaxin also affects other joints and ligaments throughout the body, making them more flexible and prone to injury.
Choice B is wrong because progesterone is not directly involved in joint laxity, although it does have other effects on the musculoskeletal system, such as increasing bone resorption and decreasing muscle strength.
Choice C is wrong because estrogen is not directly involved in joint laxity, although it does have other effects on the musculoskeletal system, such as increasing bone formation and modulating pain perception.
Choice D is wrong because human chorionic gonadotropin (hCG) is not directly involved in joint laxity, although it does have other effects on the musculoskeletal system, such as stimulating thyroid function and increasing fluid retention.
Normal ranges for these hormones vary depending on the stage of pregnancy, but generally they increase throughout gestation and peak near term.
Respiratory Changes in pregnancy
A nurse is teaching a pregnant client about the respiratory changes that occur during pregnancy.
The nurse should explain that the increased oxygen consumption is due to:.
Explanation
Increased progesterone levels and sensitivity to carbon dioxide.Progesterone is a hormone that increases during pregnancy and acts as a trigger of the primary respiratory center by increasing the sensitivity of the respiratory center to carbon dioxide.This leads to an increase in ventilation and oxygen consumption during pregnancy.
Choice A is wrong because increased metabolic rate and fetal oxygen demand are not the main causes of increased oxygen consumption during pregnancy.The maternal rate of oxygen consumption rises progressively during pregnancy, reaching a peak of 20% above nonpregnant levels.The fetal oxygen demand is only a small fraction of this increase.
Choice C is wrong because elevation of the diaphragm and increased chest wall compliance are mechanical effects of pregnancy that reduce the lung volumes and capacities, such as functional residual capacity and expiratory reserve volume.
These changes do not affect the oxygen consumption directly.
Choice D is wrong because increased tidal volume and respiratory rate are the consequences of increased oxygen consumption during pregnancy, not the causes.Tidal volume increases by 40% and respiratory rate increases by 15% during pregnancy.These changes result in an increase in minute ventilation by 50%.
A nurse is assessing a pregnant client who is in her third trimester.
The nurse notes that the client has a functional residual capacity of 1.8 L.
The nurse should recognize that this finding indicates:.
Explanation
A normal respiratory change in pregnancy caused by the gravid uterus.This is because the enlarging uterus increases the end-expiratory abdominal pressure and displaces the diaphragm upwards, leading to a reduction of functional residual capacity (FRC) and expiratory reserve volume (ERV).
FRC is the volume of air remaining in the lungs after a normal expiration.The normal FRC for an adult is about 2.4 L, so a value of 1.8 L indicates a decrease of about 25%.
Choice B is wrong because pulmonary edema is not a normal respiratory change in pregnancy, but a complication that can occur due to pre-eclampsia, heart failure, or fluid overload.
Pulmonary edema would cause symptoms such as dyspnea, cough, chest pain, and frothy sputum.
Choice C is wrong because increased alveolar ventilation is not caused by FRC reduction, but by increased levels of progesterone that stimulate the respiratory center and increase the sensitivity to carbon dioxide.
Alveolar ventilation is the amount of air that reaches the alveoli per minute.
Increased alveolar ventilation leads to increased oxygen consumption and decreased carbon dioxide levels in pregnancy.
Choice D is wrong because asthma is not a normal respiratory change in pregnancy, but a chronic inflammatory condition that affects the airways.
Asthma can cause symptoms such as wheezing, coughing, chest tightness, and shortness of breath.
Asthma can worsen or improve during pregnancy depending on various factors such as hormonal changes, allergen exposure, and stress.
A woman is in her seventh month of pregnancy.
She has been complaining of nasal congestion and occasional epistaxis.
The nurse suspects that:.
Explanation
This is a normal respiratory change in pregnancy caused by elevated levels of estrogen.Estrogen increases the blood volume and the vascularity of the nasal mucosa, making it more prone to congestion and bleeding.This condition is called pregnancy rhinitis and affects up to 39% of pregnant people.It usually resolves within 10 days after delivery.
Choice B is wrong because nasal congestion and epistaxis are not signs of cardiovascular problems in pregnancy.They are common and benign symptoms that do not indicate any complications.
Choice C is wrong because there is no evidence that the woman is a victim of domestic violence.
Domestic violence is a serious issue that should not be assumed without proper assessment and screening.
If there are any signs of physical or emotional abuse, the nurse should provide support and referral to appropriate resources.
Choice D is wrong because cocaine use is not a likely cause of nasal congestion and epistaxis in pregnancy.
Cocaine can cause damage to the nasal septum and mucosa, but it would also cause other symptoms such as agitation, tachycardia, hypertension, and fetal distress.Cocaine use in pregnancy is associated with increased risks of miscarriage, preterm labor, placental abruption, and fetal growth restriction.
The nurse should ask about substance use history and offer counseling and treatment if
A nurse is caring for a pregnant client who reports dyspnea and nasal congestion.
The nurse should inform the client that these symptoms are:.
Explanation
Normal and expected due to the respiratory changes in pregnancy.This is because pregnancy causes hormonal changes such as increased estrogen levels and high blood volume, which can lead to swelling of the blood vessels and mucus membranes in the nose, resulting in nasal congestion or pregnancy rhinitis.Pregnancy also increases the oxygen demand and carbon dioxide production, which can cause dyspnea or breathing discomfort.
These symptoms are usually physiologic and do not indicate any underlying disease.
Choice A is wrong because these symptoms are not dependent on the severity, duration, or frequency, but rather on the stage of pregnancy and the individual response to hormonal changes.
Choice C is wrong because these symptoms are not suggestive of a respiratory infection or allergy, unless there are other signs such as fever, cough, sneezing, or itching.
Choice D is wrong because these symptoms are not indicative of a cardiovascular complication, unless there are other signs such as chest pain, palpitations, edema, or cyanosis.
A nurse is reviewing the laboratory results of a pregnant client who has been ingesting white clay dirt from her backyard.
The nurse should expect to find:.
Explanation
A reduced iron level.This is because ingesting white clay dirt from the backyard, also known as calabash chalk or nzu, can bind iron and other minerals in the intestine and prevent their absorption.This can lead to iron deficiency anemia and other complications for the pregnant woman and the unborn child.
Choice A is wrong because an elevated hemoglobin level is not likely to result from clay ingestion.
Hemoglobin is the protein that carries oxygen in the blood and it requires iron for its synthesis.If iron levels are reduced due to clay ingestion, hemoglobin levels will also be reduced.
Choice B is wrong because a decreased platelet count is not directly related to clay ingestion.
Platelets are blood cells that help with clotting and they are not affected by the mineral content of clay.However, clay ingestion may increase the risk of bleeding due to iron deficiency anemia.
Choice C is wrong because an increased glucose level is not caused by clay ingestion.
Glucose is the main source of energy for the body and it is regulated by hormones such as insulin.
Clay ingestion does not affect glucose metabolism or insulin secretion.However, clay ingestion may interfere with the absorption of other nutrients that are important for glucose regulation, such as zinc.
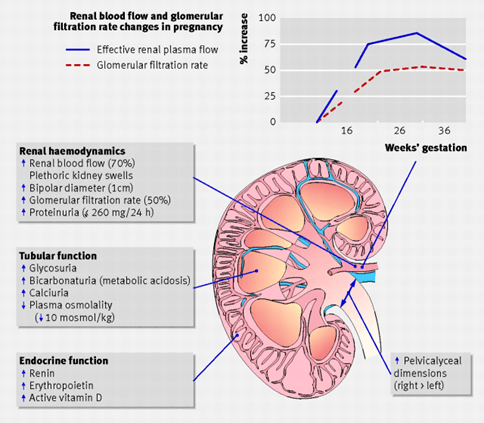
Renal Changes in pregnancy
A nurse is teaching a pregnant client about the renal changes that occur during pregnancy.
The nurse explains that the amount of urine produced per day increases by 25% to 50% during pregnancy due to:.
Explanation
This is because pregnancy leads to physiologic changes in renal and systemic hemodynamics that cause important alterations in acid-base, electrolyte, and kidney function.One of these changes is a decrease in renal vascular resistance due to hormonal and mechanical factors, which results in increased renal blood flow and glomerular filtration rate.Another change is an increase in plasma volume by 30% to 50% due to increased aldosterone and vasopressin secretion.
Choice A is wrong because increased renal blood flow and increased glomerular permeability are not the main causes of increased urine production during pregnancy.Increased glomerular permeability may occur in some pathological conditions, such as preeclampsia, but not in normal pregnancy.
Choice B is wrong because increased glomerular filtration rate and decreased tubular reabsorption are not the main causes of increased urine production during pregnancy.Increased glomerular filtration rate is a consequence of decreased renal vascular resistance and increased plasma volume, not a cause.Decreased tubular reabsorption may occur in some pathological conditions, such as gestational diabetes, but not in normal pregnancy.
Choice D is wrong because decreased serum osmolality and increased renal clearance are not the main causes of increased urine production during pregnancy.Decreased serum osmolality is a consequence of increased plasma volume and decreased thirst threshold, not a cause.
Increased renal clearance may occur in some pathological conditions, such as urinary tract infection, but not in normal pregnancy
A nurse is reviewing the laboratory results of a client who is at 28 weeks of gestation and has mild preeclampsia (gestational hypertension with proteinuria).
Which of the following findings should the nurse report to the provider?
Explanation
This is because preeclampsia is a condition that causes high blood pressure and proteinuria (protein in the urine) after 20 weeks of gestation.Proteinuria is a sign of kidney damage and can lead to complications for the mother and the baby.The normal range of urinary protein is less than 300 mg/day.
Choice A is wrong because serum creatinine 0.6 mg/dL is within the normal range of 0.5 to 1.1 mg/dL for women.
Creatinine is a waste product that is filtered by the kidneys and excreted in the urine.A high level of creatinine indicates kidney impairment.
Choice C is wrong because serum uric acid 4 mg/dL is within the normal range of 2.4 to 6 mg/dL for women.
Uric acid is another waste product that is filtered by the kidneys and excreted in the urine.A high level of uric acid can cause gout or kidney stones.
Choice D is wrong because urinary specific gravity 1.015 is within the normal range of 1.005 to 1.030.
Specific gravity measures how concentrated the urine is.A high specific gravity indicates dehydration or kidney dysfunction.
A nurse is teaching a prenatal class about physiological changes during pregnancy and their effects on maternal nutrition and fluid intake requirements.
Which statement by one of the class participants indicates understanding?
Explanation
This statement indicates understanding of the physiological changes that occur during pregnancy and their effects on maternal nutrition and fluid intake requirements.Drinking more fluids helps to maintain adequate hydration and blood volume, which supports fetal growth and development.
Choice B is wrong because eating more protein does not directly relate to the increased workload of the kidneys during pregnancy.Protein intake should be adequate to meet the needs of the mother and the fetus, but not excessive.
Choice C is wrong because limiting sodium intake is not necessary for most pregnant women, unless they have hypertension or pre-eclampsia.Sodium is important for fluid balance and blood pressure regulation, and restricting it may impair placental perfusion.
Choice D is wrong because taking iron supplements does not compensate for the decreased red blood cell count during pregnancy.
Iron supplements are recommended to prevent or treat iron deficiency anemia, which is common in pregnancy due to increased maternal and fetal demands.However, the red blood cell count normally decreases during pregnancy due to hemodilution, which is a physiological adaptation that increases blood volume and cardiac output.
A nurse is collecting a urine sample from a pregnant client who is at 24 weeks of gestation.
The nurse performs a dipstick test and finds glucose in the urine.
The nurse knows that the normal range of urinary glucose in pregnancy is:.
Explanation
The normal range of urinary glucose in pregnancy is less than 100 mg/dL or negative on dipstick.
This means that there is no glucose or very little glucose in the urine of a healthy pregnant woman.
Choice B is wrong because less than 200 mg/dL or trace on dipstick indicates a mild glycosuria, which is when glucose is found in the urine.This can be normal during pregnancy as the kidneys allow more glucose to pass into urine during pregnancy, but it could also suggest the possibility of having undetected diabetes before this pregnancy.
Choice C is wrong because less than 300 mg/dL or 1+ on dipstick indicates a moderate glycosuria, which is more likely to be a sign of diabetes.A glucose tolerance test (GTT) is recommended to confirm or rule out diabetes.
Choice D is wrong because less than 400 mg/dL or 2+ on dipstick indicates a severe glycosuria, which is almost certainly a sign of diabetes.A GTT is also recommended to diagnose diabetes.
Gastrointestinal Changes in pregnancy
A nurse is teaching a pregnant client about the gastrointestinal changes that occur during pregnancy.
The nurse should explain that the increased progesterone levels cause which of the following effects?
Explanation
Decreased gastric motility.This is because the hormone progesterone, which causes smooth muscle relaxation, often causes relaxation and slowing of digestion in the stomach and the small and large intestines.
This can lead to constipation and delayed gastric emptying.
Choice B is wrong because progesterone does not increase gastric acid secretion.In fact, progesterone may decrease acid secretion by inhibiting histamine release.
Choice C is wrong because progesterone does decrease lower esophageal sphincter tone, but this is not a direct effect on the gastrointestinal system.Rather, it is a result of the growing uterus pushing the stomach upward and causing reflux.
Choice D is wrong because progesterone does not increase intestinal absorption.In fact, progesterone may decrease intestinal absorption by reducing intestinal blood flow and slowing down transit time.
A nurse is assessing a pregnant client who reports nausea and vomiting in the morning.
The nurse should recognize that this is most likely due to which of the following factors?
Explanation
Elevated human chorionic gonadotropin (hCG) levels.Nausea and vomiting in the morning are common symptoms of early pregnancy and are most likely due to the high levels of hCG hormone produced by the placenta.hCG levels peak around 8 to 10 weeks of gestation and then decline gradually.
Choice B is wrong because decreased gastric emptying time is not a cause of nausea and vomiting in pregnancy, but rather a consequence of hormonal changes and increased pressure on the stomach by the growing uterus.
Choice C is wrong because increased peristalsis of the colon is not related to nausea and vomiting in pregnancy, but rather to constipation, which is another common symptom of pregnancy due to hormonal changes and reduced physical activity.
Choice D is wrong because decreased bile production is not a factor in nausea and vomiting in pregnancy, but rather a possible cause of gallstones, which are more common in pregnant women due to hormonal changes and increased cholesterol levels.
A nurse is caring for a pregnant client who has constipation.
The nurse should recommend which of the following interventions to promote bowel elimination?
Explanation
Increasing fluid intake to at least 2 L per day can help prevent constipation by keeping stool soft and easy to pass.Fluids can include water, clear soups, teas, and fruit or vegetable juices.
Choice B is wrong because limiting intake of high-fiber foods can worsen constipation.High-fiber foods such as fruits, vegetables, whole grains, and beans can increase the number of stools and facilitate their passage through the intestines.Adults should eat between 28 and 34 grams of fiber each day.
Choice C is wrong because taking a daily iron supplement can cause constipation and hard, black stools.Iron can make it harder for bacteria in the bowel to break down food.
Prenatal vitamins that are high in iron may also contribute to constipation.If this is the case, a doctor may recommend trying a vitamin that contains less iron.
Choice D is wrong because avoiding physical activity can lead to constipation.Being active helps stool move through the intestines.
Getting regular exercise, with a doctor’s approval, can help relieve constipation.If exercising is not possible, try to fit in a gentle walk each day.
A nurse is providing dietary education to a pregnant client who has heartburn.
The nurse should instruct the client to avoid which of the following foods?
Explanation
Chocolate.Chocolate is one of the foods that can cause heartburn by increasing the acid production in your stomach.It also contains caffeine and theobromine, which can relax the valve between your esophagus and stomach and allow acid to escape up to your throat.
Choice A.Milk is wrong because milk can help neutralize stomach acid and ease heartburn symptoms.
Choice B.Bananas is wrong because bananas are low in acid and can act as a natural antacid.
Choice D.Rice is wrong because rice is a bland and starchy food that can help absorb excess stomach acid and prevent heartburn.
Some other foods to avoid for heartburn during pregnancy are citrus fruits, tomato-based foods, spicy foods, fried and fatty foods, carbonated beverages, and alcohol.
A nurse is reviewing the laboratory results of a pregnant client who has hyperemesis gravidarum.
The nurse should expect to find which of the following findings?
Explanation
Hypokalemia.Hyperemesis gravidarum (HG) is a severe form of nausea and vomiting during pregnancy that can lead to dehydration, electrolyte disturbances, ketosis, and weight loss.Hypokalemia is a common electrolyte abnormality in HG due to excessive vomiting and poor oral intake.Hypokalemia can cause cardiac arrhythmias, muscle weakness, and renal impairment.
Choice A is wrong because metabolic acidosis is not a typical finding in HG.Metabolic alkalosis is more likely due to loss of gastric acid from vomiting.
Choice C is wrong because hyperglycemia is not associated with HG.Hyperglycemia may occur in gestational diabetes or pregestational diabetes, which are risk factors for HG but not direct causes.
Choice D is wrong because hyponatremia is not a common complication of HG.Hyponatremia may occur in severe cases of dehydration or if excessive intravenous fluids are given without adequate sodium replacement.
Endocrine Changes in pregnancy
A nurse is caring for a pregnant client who is experiencing fatigue and mood swings.
These symptoms are primarily caused by:
A. Increased progesterone levels.
B. Increased estrogen levels.
C. Increased thyroid hormone levels.
D. Increased insulin resistance
Explanation
The correct answer is choice A.Progesterone levels significantly rise during pregnancy, especially during the first trimester. This hormone plays a key role in maintaining pregnancy, but it also has sedative effects on the body, which can contribute to fatigue. Additionally, progesterone can influence mood by affecting neurotransmitter levels, potentially leading to mood swings. As progesterone helps to maintain the uterine lining and prevent early contractions, it also has a relaxing effect on smooth muscles, leading to symptoms like fatigue and irritability.
Choice B is wrong because while estrogen levels also rise during pregnancy, estrogen is not primarily responsible for symptoms such as fatigue and mood swings. Estrogen is involved in the development of the placenta, fetal growth, and regulation of other pregnancy-related changes, but it is the increased progesterone that is more directly linked to the fatigue and mood changes often seen in early pregnancy.
Choice C is wrong because while thyroid hormone changes can occur during pregnancy, they are not typically the primary cause of fatigue and mood swings unless a thyroid disorder is present. In normal pregnancy, thyroid hormones may increase slightly due to the influence of human chorionic gonadotropin (hCG) but do not typically cause the fatigue and mood swings seen during pregnancy. Severe thyroid dysfunction, such as hyperthyroidism or hypothyroidism, may contribute to these symptoms, but in this case, the normal hormonal changes of pregnancy are more likely responsible.
Choice D is wrong because increased insulin resistance can occur in pregnancy, particularly during the second trimester, as the body adapts to increased glucose needs. However, while insulin resistance can contribute to gestational diabetes, it is not directly responsible for the fatigue and mood swings experienced early in pregnancy. Fatigue in early pregnancy is more commonly attributed to hormonal changes, particularly the rise in progesterone, rather than changes in insulin sensitivity.
A nurse is educating a pregnant client about the role of hCG in pregnancy.
Which of the following functions is primarily attributed to hCG?
Explanation
The correct answer is choice A. Maintaining the endometrium.HCG is a hormone produced by the placenta during pregnancy that helps thicken the uterine lining and tells the body to stop menstruating.
This supports the implantation and growth of the embryo.
Choice B is wrong because hCG does not stimulate milk production.
That is the role of another hormone called prolactin.
Choice C is wrong because hCG does not inhibit uterine contractions.
That is the role of another hormone called progesterone.
Choice D is wrong because hCG does not regulate the metabolic rate.
That is the role of another hormone called thyroid-stimulating hormone (TSH)
A nurse is assessing a pregnant client who is experiencing fatigue and increased urination.
These symptoms are primarily caused by:.
Explanation
. Increased insulin resistance.This is because during pregnancy, the placenta produces hormones such as human placental lactogen (hPL) and placental growth hormone that increase the mother’s blood glucose levels and decrease her sensitivity to insulin.This causes increased urination and fatigue as the body tries to eliminate excess glucose and cope with the higher energy demands of pregnancy.
Choice A is wrong because increased estrogen levels do not cause increased urination and fatigue.Estrogen is a hormone that helps develop the female sexual traits and maintain a healthy pregnancy.
It does not affect blood glucose levels or insulin sensitivity.
Choice C is wrong because decreased progesterone levels do not cause increased urination and fatigue.Progesterone is a hormone that stimulates the thickening of the uterine lining for implantation of a fertilized egg and prevents uterine contractions during pregnancy.
It does not affect blood glucose levels or insulin sensitivity.
Choice D is wrong because increased thyroid hormone levels do not cause increased urination and fatigue.Thyroid hormones are responsible for regulating the metabolism, growth and development of the body.
They do not affect blood glucose levels or insulin sensitivity.
A nurse is explaining the endocrine changes during pregnancy to a group of expectant mothers.
Which hormone is responsible for stimulating uterine growth and enhancing fetal organ development?
Explanation
Answer: C. Estrogen
Rationale:
A. hCG (Human Chorionic Gonadotropin):
hCG is responsible for maintaining the corpus luteum in early pregnancy, which produces progesterone until the placenta takes over. It does not directly stimulate uterine growth or enhance fetal organ development.
B. Progesterone:
Progesterone supports pregnancy by maintaining the uterine lining, relaxing uterine muscles to prevent contractions, and preventing preterm labor. However, it is not primarily responsible for uterine growth or fetal organ development.
C. Estrogen:
Estrogen plays a significant role in stimulating uterine growth by increasing the size and number of uterine muscle cells. It also enhances the development of fetal organs and promotes blood flow to the placenta. These effects make estrogen crucial during pregnancy.
D. Prolactin:
Prolactin prepares the mammary glands for lactation and stimulates milk production post-delivery. It does not contribute to uterine growth or fetal organ development during pregnancy.
Musculoskeletal Changes in pregnancy
A nurse is assessing a pregnant client who complains of back pain.
Which musculoskeletal change during pregnancy is primarily responsible for this symptom?
Explanation
During pregnancy, the center of gravity shifts forward as the uterus grows, causing an increased lordosis (inward curvature) of the lumbar spine.
This can lead to back pain and discomfort.
Choice A is wrong because increased joint laxity is due to hormonal changes that relax the ligaments and tendons, not the muscles.
Choice C is wrong because increased muscle strain is a result of increased spinal curvature, not a cause.
Choice D is wrong because decreased muscle strength is not a musculoskeletal change during pregnancy, but a possible consequence of reduced physical activity or poor nutrition.
A nurse is caring for a pregnant client who is in her third trimester.
Which musculoskeletal change is expected to be at its highest point during this stage?
Explanation
Spinal curvature is expected to be at its highest point during the third trimester of pregnancy because of the increased weight of the fetus and the relaxation of the ligaments in the pelvic area due to pregnancy hormones.
This can cause backaches and discomfort for the pregnant woman.
Choice A is wrong because joint laxity is not specific to the third trimester of pregnancy.Joint laxity occurs throughout pregnancy due to the effects of relaxin and other hormones on the connective tissue that holds the bones in place.
Choice C is wrong because muscle strain is not a musculoskeletal change, but a possible consequence of the changes in posture and balance that occur during pregnancy.Muscle strain can affect any trimester of pregnancy, depending on the physical activity and fitness level of the woman.
Choice D is wrong because muscle strength is not a musculoskeletal change, but a factor that can influence the ability to cope with the changes in weight and posture that occur during pregnancy.Muscle strength can vary depending on the exercise regimen and nutrition of the woman.
A nurse is caring for a pregnant client who is experiencing pelvic pain.
This symptom is primarily caused by:.
Explanation
This is because pelvic pain during pregnancy is typically caused by the release of a hormone calledrelaxin, which acts by relaxing the hip and pelvic ligaments and joints to make room for the growing baby.This hormone is released in higher quantities during labor to ease the passage of the baby, and it may cause pelvic pain, which resolves after labor.
Choice B is wrong because increased spinal curvature does not cause pelvic pain, but rather lower back pain.
Choice C is wrong because increased muscle strain does not cause pelvic pain, but rather round ligament pain, which is a sharp or crampy pain in the lower abdomen or groin area.
Choice D is wrong because decreased muscle strength does not cause pelvic pain, but rather increases the risk of urinary incontinence and pelvic organ prolapse after delivery.
Normal ranges for relaxin levels vary depending on the stage of pregnancy and the laboratory method used.
However, some general ranges are:
• First trimester: 6.3 to 110 ng/mL
• Second trimester: 19.5 to 155 ng/mL
• Third trimester: 55 to 210 ng/mL
A nurse is assessing a pregnant client who complains of numbness and tingling in her hands.
This symptom is most likely due to:
Explanation
This symptom is most likely due to carpal tunnel syndrome, which is a common condition in pregnancy caused by fluid retention and swelling in the wrists that compresses the median nerve, which controls feeling and movement in the hand.
Some possible explanations for the other choices are:
• Choice A is wrong because increased joint laxity is caused by the hormone relaxin, which loosens the ligaments and joints to prepare for childbirth.This can cause pain and instability in the pelvis, hips, and lower back, but not numbness and tingling in the hands.
• Choice B is wrong because increased spinal curvature is a result of the growing uterus and shifting center of gravity, which can cause back pain and posture changes, but not numbness and tingling in the hands.
• Choice D is wrong because decreased muscle strength is not a common symptom of pregnancy, unless it is due to an underlying condition such as anemia or thyroid problems.Numbness and tingling in the hands can affect grip strength and finger dexterity, but this is a consequence of carpal tunnel syndrome, not a cause.
Normal ranges for fluid retention and swelling in pregnancy vary depending on the individual, but some signs of excessive or abnormal swelling include sudden or severe swelling in the face, hands, or feet; swelling that does not go down after resting or elevating the limbs; or swelling that is accompanied by other symptoms such as headache, vision changes, or high blood pressure.These could indicate a serious condition such as preeclampsia, which requires immediate medical attention.
Weight Gain Guidelines in pregnancy
A nurse is providing education to a pregnant client about weight gain guidelines during pregnancy.
What is the recommended weight gain range for normal-weight women?
Explanation
This is the recommended weight gain range for normal-weight women with a BMI of 18.5-24.9 before pregnancy.Gaining the recommended amount of weight during pregnancy is important for the health of the baby and the mother.
Choice B is wrong because 15-25 pounds is the recommended weight gain range for overweight women with a BMI of 25.0-29.9 before pregnancy.
Choice C is wrong because 28-40 pounds is the recommended weight gain range for underweight women with a BMI of less than 18.5 before pregnancy.
Choice D is wrong because 10-20 pounds is the recommended weight gain range for obese women with a BMI of greater than or equal to 30.0 before pregnancy.
Normal ranges for BMI are 18.5-24.9 for normal weight, less than 18.5 for underweight, 25.0-29.9 for overweight, and greater than or equal to 30.0 for obese.
A nurse is assessing a pregnant client's understanding of trimester-specific weight gain.
Which statement by the client indicates a need for further education?
Explanation
This statement by the client indicates a need for further education because it is incorrect.
The recommended weight gain during the first trimester is 1-2 kilograms per month, not in total.
The other choices are correct and do not require further education.
Choice B states that after the first trimester, a weight gain of 1 pound per week is recommended for the remaining two trimesters, which is accurate.
Choice C states that during the second trimester, an extra 340 calories per day are needed, which is also true.
Choice D states that during the third trimester, an additional 450 calories per day are required, which is correct as well.
A nurse is discussing the importance of folic acid with a pregnant client.
What is the primary reason for recommending folic acid intake during pregnancy?
Explanation
Folic acid is a synthetic form of folate, a B vitamin that plays a role in the development of the neural tube, which becomes the brain and spinal cord of the fetus.
Neural tube defects are serious birth abnormalities that can cause disability or death.
Folic acid supplementation before and during pregnancy can significantly reduce the risk of neural tube defects.
Choice A is wrong because folic acid does not directly promote fetal brain development, although it is involved in the formation of the neural tube, which later develops into the brain.
Choice C is wrong because folic acid does not support healthy placental function.
The placenta is an organ that connects the mother and the fetus, and it does not depend on folic acid for its function.
Choice D is wrong because folic acid does not prevent maternal anemia.
Anemia is a condition in which the blood does not have enough red blood cells to carry oxygen.
Folic acid helps the body make new cells, including red blood cells, but it is not the only factor that affects anemia.
Iron deficiency is a more common cause of anemia during pregnancy.
The recommended daily intake of folic acid for pregnant women is 600 micrograms (mcg), which can be obtained from supplements and fortified foods.
Some natural sources of folate include spinach, avocado, and banana.
A nurse is discussing weight gain guidelines with a pregnant client who is overweight.
What is the recommended weight gain range for overweight women during pregnancy?
Explanation
This is the recommended weight gain range for overweight women during pregnancy according to the CDC1 and ACOG.
Overweight women have a BMI of 25.0-29.9 before pregnancy.
Choice A is wrong because 25-35 pounds is the recommended weight gain range for normal weight women during pregnancy, who have a BMI of 18.5-24.9 before pregnancy.
Choice C is wrong because 28-40 pounds is the recommended weight gain range for underweight women during pregnancy, who have a BMI of less than 18.5 before pregnancy.
Choice D is wrong because 10-20 pounds is too low for any category of women during pregnancy, and may result in delivering a baby who is too small.
Gaining the recommended amount of weight during pregnancy is important for the health of the mother and the baby, as it can prevent complications such as gestational diabetes, preterm birth, and low birth weight.
A nurse is assessing a pregnant client's understanding of calorie intake during pregnancy.
What is the recommended additional calorie intake per day during the third trimester?
Explanation
According to the Academy of Nutrition and Dietetics, pregnant women need about an extra 450 calories per day during the third trimester.
This is to support the growth and development of the baby and the mother’s increased energy needs.
Choice A is wrong because 340 calories is the recommended additional intake for the second trimester.
Choice C is wrong because 250 calories is too low for the third trimester and may not provide enough nutrients for the baby.
Choice D is wrong because 550 calories is too high for the third trimester and may lead to excessive weight gain or gestational diabetes.
The normal range of calorie intake during pregnancy depends on the pre-pregnancy weight, activity level and age of the mother.
However, a general guideline is about 1,800 calories per day during the first trimester, 2,200 calories per day during the second trimester and 2,400 calories per day during the third trimester.
These calories should come from a balanced diet of protein, fruits, vegetables and whole grains.
Sweets and fats should be kept to a minimum.
Fluid intake is also important and pregnant women should drink several glasses of water each day.
Some foods and drinks should be avoided during pregnancy, such as unpasteurized milk and cheese, raw or undercooked meat and seafood, alcohol and caffeine.
Food safety practices such as washing, cooking and chilling food properly should also be followed.
More questions on this topic
A nurse is calculating the partial pressure of oxygen (PaO2) in the arterial blood of a pregnant client who is in her second trimester.
The nurse should use which of the following values as the normal range for PaO2 in pregnancy?
Explanation
95 to 105 mmHg.
This is the normal range for PaO2 in pregnancy according to several sources.
PaO2 is the partial pressure of oxygen in arterial blood and reflects the oxygenation of the blood.
It is influenced by factors such as ventilation, perfusion, diffusion, and hemoglobin affinity.
Choice A is wrong because 27 to 32 mmHg is too low for PaO2 and would indicate severe hypoxemia or low oxygen levels in the blood.
Choice C is wrong because 500 to 700 mL is a measure of tidal volume, not PaO.
Tidal volume is the amount of air that moves in and out of the lungs with each breath.
Choice D is wrong because 7 to 10 L/min is a measure of oxygen flow rate, not PaO.
Oxygen flow rate is the amount of oxygen delivered to a patient through a device such as a nasal cannula or a mask.
Which factors would change during pregnancy if the hormone progesterone were withdrawn or reduced?
Explanation
Peristalsis and uterine contractility would increase.
This is because progesterone is a hormone that relaxes the smooth muscles of the uterus and the gastrointestinal tract during pregnancy.
If progesterone were reduced or withdrawn, the uterus would contract more and peristalsis would increase, leading to possible preterm labor and digestive problems.
Choice A is wrong because insulin resistance would be decreased, not increased, by lower progesterone levels.
Progesterone increases insulin resistance during pregnancy to ensure adequate glucose supply for the fetus.
Choice B is wrong because sweat and sebaceous glands would decrease production, not increase, by lower progesterone levels.
Progesterone stimulates the activity of these glands during pregnancy to regulate body temperature and protect the skin from infections.
Choice C is wrong because pyrosis (heartburn) would decrease in frequency, not increase, by lower progesterone levels.
Progesterone relaxes the lower esophageal sphincter during pregnancy, allowing gastric acid to reflux into the esophagus and cause pyrosis.
A nurse is caring for a pregnant client who has hyperemesis gravidarum and is receiving IV fluids and antiemetics in an acute care facility.
Which of the following outcomes indicates that treatment has been effective?
Explanation
The correct answer is choice A. The client reports a decrease in nausea and vomiting.
This indicates that the treatment has been effective in reducing the symptoms of hyperemesis gravidarum and improving the quality of life of the client.
Choice B is wrong because weight gain alone is not a reliable indicator of treatment effectiveness.
Weight gain may be due to fluid retention or other factors unrelated to nausea and vomiting.
Choice C is wrong because urine specific gravity of 1.035 is high and indicates dehydration, which is a complication of hyperemesis gravidarum.
The normal range of urine specific gravity is 1.005 to 1.0302.
Choice D is wrong because hematocrit of 38% is within the normal range for pregnant women (33 to 39%) and does not reflect the severity or improvement of hyperemesis gravidarum.
A nurse is providing education to a pregnant client about the hormonal changes during pregnancy.
Which hormone is responsible for maintaining the corpus luteum and stimulating fetal growth ?
Explanation
Progesterone is responsible for maintaining the corpus luteum and stimulating fetal growth.
Progesterone also prevents miscarriage by relaxing the uterus and maintaining the endometrium.
Choice B is wrong because estrogen is not responsible for maintaining the corpus luteum or stimulating fetal growth.
Estrogen helps develop the female sexual traits and supports the growth of the uterus and placenta.
Choice C is wrong because thyroid hormones are not responsible for maintaining the corpus luteum or stimulating fetal growth.
Thyroid hormones regulate the metabolism and energy levels of the mother and the fetus.
Choice D is wrong because prolactin is not responsible for maintaining the corpus luteum or stimulating fetal growth.
Prolactin stimulates milk production in the breasts after delivery.
A nurse is caring for a pregnant client who is experiencing increased urinary protein levels.
What is the primary cause of this change?
Explanation
Increased glomerular filtration rate.
This is because during pregnancy, the renal blood flow and glomerular filtration rate increase to meet the increased metabolic demands of the mother and fetus.
This can result in increased urinary protein excretion, which is usually mild and does not indicate renal damage.
Choice A is wrong because decreased glomerular permeability would reduce the amount of protein that can pass through the glomerulus and into the urine.
Choice B is wrong because decreased protein intake would not affect the urinary protein levels, unless the intake is severely deficient.
Choice D is wrong because increased tubular reabsorption would decrease the amount of protein that is excreted in the urine, as the tubules would reabsorb more protein from the filtrate and return it to the blood.
A nurse is explaining the musculoskeletal changes during pregnancy to a group of expectant mothers.
Which change alters the center of gravity and posture of the body?
Explanation
This change alters the center of gravity and posture of the body because the uterus expands and shifts higher as the fetus grows during pregnancy.
This causes an increased strain on the muscles and ligaments supporting the vertebral column and leads to lower back pain.
Choice A is wrong because increased joint laxity does not alter the center of gravity and posture of the body.
It is caused by hormonal changes that loosen the ligaments throughout the body, resulting in decreased stability of the joints.
Choice C is wrong because increased muscle strain does not alter the center of gravity and posture of the body.
It is a consequence of the shift in the center of gravity and the weight gain during pregnancy, which put more pressure on the back muscles.
Choice D is wrong because decreased muscle strength does not alter the center of gravity and posture of the body.
It is not a common musculoskeletal change during pregnancy, although some women may experience fatigue or weakness due to hormonal changes or anemia.
A nurse is educating a pregnant client about the renal changes during pregnancy.
Which change is responsible for the increased urinary output?
Explanation
Increased renal blood flow is responsible for the increased urinary output during pregnancy.
This is because the renal plasma flow and glomerular filtration rate increase by 50% to 80% during pregnancy, resulting in more urine production.
Choice A is wrong because the glomerular filtration rate increases, not decreases, during pregnancy.
Choice B is wrong because the tubular reabsorption decreases, not increases, during pregnancy.
This is due to the increased levels of progesterone, which inhibit sodium reabsorption and cause diuresis.
Choice D is wrong because the increased plasma volume is a consequence, not a cause, of the increased renal blood flow.
The plasma volume expands by 30% to 50% during pregnancy to meet the increased metabolic demands of the mother and fetus.
A nurse is reviewing the laboratory results of a pregnant client.
Which finding is expected regarding serum creatinine and urea levels?
Explanation
Serum creatinine and urea are waste products of protein metabolism that are normally filtered by the kidneys and excreted in urine.
In pregnancy, the glomerular filtration rate (GFR) increases by about 50%, which means more creatinine and urea are cleared from the blood.Therefore, serum creatinine and urea levels decrease in pregnancy compared to nonpregnant women.
A. Increased serum creatinine and urea levels are wrong because they indicate impaired kidney function or dehydration, which are not normal in pregnancy.
C. Unchanged serum creatinine and urea levels are wrong because they do not reflect the increased GFR in pregnancy.
D. Increased glomerular filtration rate is correct but it is not a finding regarding serum creatinine and urea levels, which are the focus of the question.
Normal ranges for serum creatinine and urea vary depending on the laboratory and the units used, but based on a nonpregnant reference interval of 45-90 μmol/l (0.51-1.02 mg/dl) for creatinine and 2.5-6.4 mmol/l (7-18 mg/dl) for urea, a serum creatinine of >77 μmol/l (0.87 mg/dl) and a blood urea of >8.5 mmol/l (24 mg/dl) should be considered outside the normal range for pregnancy.
A nurse is providing education to a pregnant client about the symptoms associated with musculoskeletal changes.
Which symptom is commonly experienced due to increased muscle strain during pregnancy?
Explanation
Back pain is a common symptom experienced due to increased muscle strain during pregnancy.
As the uterus grows and the center of gravity shifts, there is more pressure on the lower back muscles and ligaments.
This can cause pain, difficulty with balance, and reduced activity.
Choice A is wrong because leg cramps are not caused by muscle strain, but by other factors such as dehydration, electrolyte imbalance, or compression of blood vessels.
Choice C is wrong because pelvic pain is not a typical symptom of musculoskeletal changes during pregnancy.
Pelvic pain can be caused by other conditions such as urinary tract infection, preterm labor, or pelvic girdle pain.
Choice D is wrong because carpal tunnel syndrome is not a result of muscle strain, but of fluid retention and swelling that compresses the median nerve in the wrist.
This can cause numbness, tingling, or pain in the hand and fingers.
A pregnant client reports experiencing frequent urination at night.
The nurse explains that this symptom is primarily caused by:.
Explanation
This is because a pregnant client may experience frequent urination at night due to increased urinary output caused by the increased blood volume and renal function during pregnancy.
This symptom is more common in the first and third trimesters.
Choice A is wrong because increased glomerular permeability does not cause nocturia, but it may cause proteinuria, which is the presence of protein in the urine.
Choice B is wrong because decreased renal blood flow does not cause nocturia, but it may cause renal ischemia, which is a condition where the kidneys do not receive enough blood supply.
Choice C is wrong because increased tubular reabsorption does not cause nocturia, but it may cause water retention and edema, which are swelling of the body tissues due to fluid accumulation.
A nurse is educating a pregnant client about the endocrine changes during pregnancy.
Which hormone is responsible for inhibiting ovulation and stimulating milk production?
Explanation
Prolactin is a hormone that is responsible for inhibiting ovulation and stimulating milk production during pregnancy.
It is produced by the anterior pituitary gland and increases throughout pregnancy.
Choice A is wrong because hCG (human chorionic gonadotropin) is a hormone that is produced by the placenta and maintains the corpus luteum, which secretes progesterone and estrogen.
hCG does not inhibit ovulation or stimulate milk production.
Choice B is wrong because progesterone is a hormone that is produced by the corpus luteum and the placenta and supports the endometrium, prevents uterine contractions, and prepares the breasts for lactation.
Progesterone does not inhibit ovulation or stimulate milk production.
Choice C is wrong because estrogen is a hormone that is produced by the corpus luteum and the placenta and stimulates uterine growth, blood flow, and breast duct development.
Estrogen does not inhibit ovulation or stimulate milk production.
A nurse is educating a pregnant client about the changes in her posture during pregnancy.
Which factor contributes to increased spinal curvature?
Explanation
The correct answer is choice A. Increased joint laxity contributes to increased spinal curvature in pregnant women.
Joint laxity is caused by the hormone relaxin, which loosens the ligaments and joints of the pelvis and spine to prepare for childbirth.
This can result in increased lordosis (inward curvature) of the lumbar spine and increased kyphosis (outward curvature) of the thoracic spine.
Choice B is wrong because increased weight gain does not directly affect spinal curvature, but it can cause postural changes such as anterior pelvic tilt and forward trunk lean.
Choice C is wrong because increased muscle strain is a consequence, not a cause, of spinal curvature changes.
Muscle strain can occur due to the altered biomechanics and balance of the spine and pelvis during pregnancy.
Choice D is wrong because decreased muscle strength is also a consequence, not a cause, of spinal curvature changes.
Muscle strength can decrease due to reduced physical activity, hormonal changes, or pain during pregnancy.
Normal ranges for spinal curvature vary depending on age, sex, and measurement method, but generally they are:
Sacral inclination: 30-50 degrees
Lumbar curvature: 20-45 degrees
Thoracic curvature: 20-40 degrees
Cervical curvature: 20-35 degrees
A nurse is caring for a pregnant client who is experiencing leg cramps.
These cramps are primarily caused by:.
Explanation
Leg cramps are painful muscle contractions that typically affect the calf, foot or both.
They are common during pregnancy, often happening at night during the second and third trimesters.
While the exact cause of leg cramps during pregnancy isn’t clear, various theories point to the following causes of leg cramps during pregnancy: 2
Pregnancy fatigue from carrying the extra baby weight
Compression of the blood vessels in the legs
Diet (an excess of phosphorus and a shortage of calcium or magnesium)
Pregnancy hormones since they seem to cause so many pregnancy aches and pains
Choice A is wrong because increased joint laxity is not a cause of leg cramps, but rather a result of hormonal changes that relax the ligaments and joints in preparation for childbirth.
Choice B is wrong because increased spinal curvature is not a cause of leg cramps, but rather a result of the changing center of gravity and posture during pregnancy.
Choice D is wrong because decreased muscle strength is not a cause of leg cramps, but rather a consequence of muscle fatigue and weight gain during pregnancy.
Normal ranges for calcium are 8.5 to 10.2 mg/dL, for magnesium are 1.7 to 2.2 mg/dL, and for phosphorus are 2.5 to 4.5 mg/dL.
A nurse is caring for a patient who had an amniocentesis performed at 16 weeks gestation and reports cramping and vaginal bleeding 24 hours later.
Which action should be taken first?
Explanation
This is because cramping and vaginal bleeding 24 hours after amniocentesis are signs of possible complications, such as injury to the baby or mother, leaking of amniotic fluid, infection, Rh sensitization, preterm labor, or miscarriage.
These complications are rare, but they can be serious and require immediate medical attention.
Choice B is wrong because administering pain medication to the patient does not address the underlying cause of the cramping and bleeding, and may delay seeking help.
Choice C is wrong because encouraging the patient to rest and elevate her legs may not prevent further complications, and may also delay seeking help.
Choice D is wrong because offering emotional support and reassurance to the patient is not enough to ensure the safety of the baby and the mother, and may give a false sense of security.
Normal ranges for amniocentesis are:
No chromosomal defects detected in the fetus and no abnormal proteins present in amniotic fluid
No signs of infection or other illness in the baby
Fetal lungs mature enough for birth if delivery is planned sooner than 39 weeks
Exams on Physiological And Physical Changes In Pregnancy
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
- Objectives
- Introduction
- Cardiovascular Changes in pregnancy
- Respiratory Changes in pregnancy
- Renal Changes in pregnancy
- Gastrointestinal Changes in pregnancy
- Endocrine Changes in pregnancy
- Musculoskeletal Changes in pregnancy
- Weight Gain Guidelines in pregnancy
- Conclusion
- Summary
- More questions on this topic
Notes Highlighting is available once you sign in. Login Here.
Objectives
- To identify the physiological and physical changes that occur in pregnancy
- To explain the mechanisms and functions of these changes
- To describe the effects of these changes on the maternal and fetal health
- To recognize the normal ranges and variations of these changes
- To provide nursing care and education for pregnant women experiencing these changes
- To differentiate between normal and abnormal changes that may indicate complications or risks
- Attempt 60+ questions on the topic Physiological and physical changes in pregnancy.
Introduction
- Pregnancy is a period of profound physiological and physical changes that affect every system of the body
- These changes are influenced by hormonal, mechanical, metabolic, immunological, and psychological factors
- These changes are adaptive and essential for the survival and development of the fetus and the preparation for labor and lactation
- These changes begin from conception and continue until the postpartum period
- These changes may cause discomfort, symptoms, or signs that are normal or abnormal depending on the severity, duration, and frequency
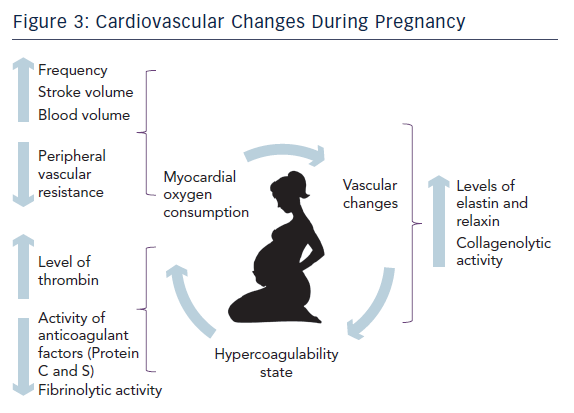
Cardiovascular Changes in pregnancy
- The cardiovascular system undergoes significant changes to meet the increased metabolic demands of pregnancy and to ensure adequate blood supply to the uterus and placenta
- The main cardiovascular changes include:
- Increased cardiac output: The amount of blood pumped by the heart per minute increases by 30% to 50% during pregnancy. This is due to increased stroke volume (the amount of blood pumped by the heart per beat) and increased heart rate (the number of beats per minute). The cardiac output peaks at 24 to 28 weeks of gestation and then declines slightly until term. The normal range of cardiac output in pregnancy is 4.5 to 6.5 L/min.
- Increased blood volume: The total amount of blood in the body increases by 40% to 50% during pregnancy. This is due to increased plasma volume (the liquid part of the blood) and increased red blood cell mass (the solid part of the blood). The plasma volume increases more than the red blood cell mass, resulting in a physiological anemia or hemodilution (a decrease in the concentration of hemoglobin and hematocrit). The normal range of hemoglobin in pregnancy is 11 to 14 g/dL and the normal range of hematocrit is 33% to 39%.
- Decreased blood pressure: The average blood pressure decreases by 10 mmHg during pregnancy. This is due to decreased peripheral vascular resistance (the resistance of the blood vessels to the flow of blood) caused by hormonal relaxation of smooth muscle and vasodilation (widening of blood vessels). The blood pressure reaches its lowest point at mid-pregnancy and then returns to pre-pregnancy levels by term. The normal range of blood pressure in pregnancy is less than 140/90 mmHg.
-
- Increased venous pressure: The pressure in the veins increases during pregnancy due to compression of the inferior vena cava (the large vein that carries blood from the lower body to the heart) by the gravid uterus (the enlarged uterus containing the fetus) and decreased venous tone (the elasticity of the veins). This leads to venous stasis (slowing or pooling of blood in the veins) and edema (swelling) of the lower extremities, vulva, and hemorrhoids. The risk of venous thromboembolism (blood clot formation in the veins) also increases during pregnancy due to hypercoagulability (increased tendency of blood to clot) caused by hormonal and fibrinolytic (clot-dissolving) changes.

Respiratory Changes in pregnancy
- The respiratory system undergoes significant changes to meet the increased oxygen requirements of pregnancy and to facilitate gas exchange between the maternal and fetal blood
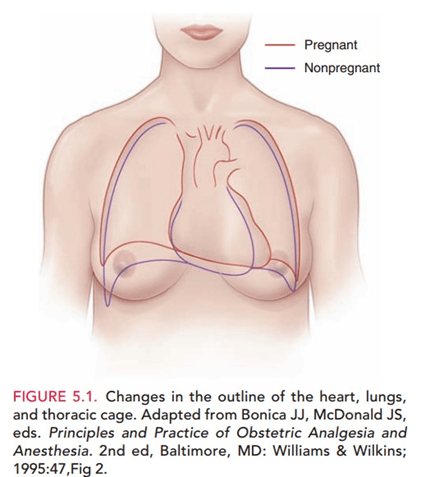
- The main respiratory changes include:
- Increased oxygen consumption: The amount of oxygen used by the body per minute increases by 15% to 20% during pregnancy. This is due to increased metabolic rate (the rate at which chemical reactions occur in the body) and increased fetal oxygen demand. The oxygen consumption peaks at 32 weeks of gestation and then remains stable until term. The normal range of oxygen consumption in pregnancy is 250 to 300 mL/min.
- Increased tidal volume: The amount of air breathed in or out per breath increases by 30% to 40% during pregnancy. This is due to increased progesterone levels that stimulate the respiratory center in the brain and increase the sensitivity to carbon dioxide. The tidal volume peaks at 28 weeks of gestation and then remains stable until term. The normal range of tidal volume in pregnancy is 500 to 700 mL.
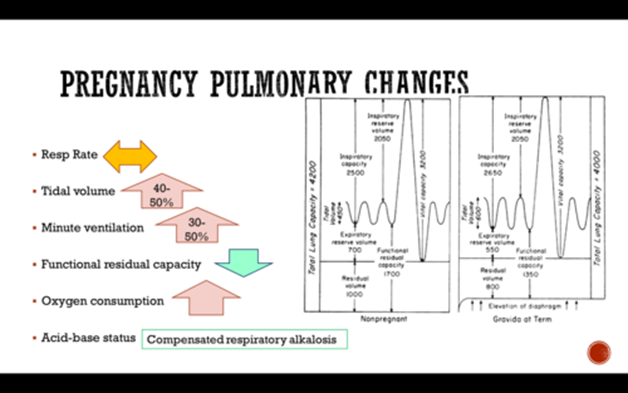
-
- Decreased functional residual capacity: The amount of air remaining in the lungs after a normal expiration decreases by 20% during pregnancy. This is due to elevation of the diaphragm (the muscle that separates the chest and abdomen) by the gravid uterus and increased chest wall compliance (the ease of expansion of the chest). The functional residual capacity decreases progressively throughout pregnancy and reaches its lowest point at term. The normal range of functional residual capacity in pregnancy is 1.5 to 2 L.
- Increased minute ventilation: The amount of air breathed in or out per minute increases by 40% to 50% during pregnancy. This is due to increased tidal volume and increased respiratory rate (the number of breaths per minute). The minute ventilation peaks at 28 weeks of gestation and then remains stable until term. The normal range of minute ventilation in pregnancy is 7 to 10 L/min.
- Decreased partial pressure of carbon dioxide: The pressure exerted by carbon dioxide in the arterial blood decreases by 15% during pregnancy. This is due to increased minute ventilation that removes more carbon dioxide from the body. The partial pressure of carbon dioxide reaches its lowest point at mid-pregnancy and then remains stable until term. The normal range of partial pressure of carbon dioxide in pregnancy is 27 to 32 mmHg.
- Increased partial pressure of oxygen: The pressure exerted by oxygen in the arterial blood increases by 5% during pregnancy. This is due to increased minute ventilation that brings more oxygen into the body. The partial pressure of oxygen reaches its highest point at mid-pregnancy and then remains stable until term. The normal range of partial pressure of oxygen in pregnancy is 95 to 105 mmHg.
- The respiratory changes result in increased alveolar ventilation (the amount of air reaching the alveoli or air sacs in the lungs) and decreased physiological dead space (the amount of air that does not participate in gas exchange) that enhance gas exchange between the maternal and fetal blood
- The respiratory changes may cause symptoms such as dyspnea (difficulty breathing), nasal congestion, epistaxis (nosebleed), or voice changes that are normal or abnormal depending on the severity, duration, and frequency
Renal Changes in pregnancy
- The renal system undergoes significant changes to maintain fluid and electrolyte balance, excrete metabolic wastes, and regulate blood pressure during pregnancy
- The main renal changes include:
- Increased renal blood flow: The amount of blood flowing through the kidneys per minute increases by 50% to 80% during pregnancy. This is due to increased cardiac output and decreased renal vascular resistance. The renal blood flow peaks at mid-pregnancy and then declines slightly until term. The normal range of renal blood flow in pregnancy is 1200 to 1500 mL/min.
- Increased glomerular filtration rate: The rate at which the kidneys filter blood and produce urine increases by 40% to 60% during pregnancy. This is due to increased renal blood flow and increased glomerular permeability (the ability of the glomeruli or clusters of capillaries in the kidneys to allow substances to pass through). The glomerular filtration rate peaks at mid-pregnancy and then declines slightly until term. The normal range of glomerular filtration rate in pregnancy is 120 to 150 mL/min.
- Increased urinary output: The amount of urine produced per day increases by 25% to 50% during pregnancy. This is due to increased glomerular filtration rate and decreased tubular reabsorption (the process by which the kidneys return substances from the urine back to the blood). The urinary output peaks at mid-pregnancy and then declines slightly until term. The normal range of urinary output in pregnancy is 1200 to 1500 mL/day.
- Decreased serum creatinine and urea: The concentration of creatinine and urea in the blood decreases by 25% to 50% during pregnancy. This is due to increased glomerular filtration rate and increased plasma volume. The serum creatinine and urea reach their lowest point at mid-pregnancy and then remain stable until term. The normal range of serum creatinine in pregnancy is 0.4 to 0.8 mg/dL and the normal range of serum urea in pregnancy is 9 to 21 mg/dL.
- Increased urinary protein: The amount of protein excreted in the urine increases by 50% to 100% during pregnancy. This is due to increased glomerular permeability and increased protein intake. The urinary protein reaches its highest point at term and then returns to pre-pregnancy levels by the postpartum period. The normal range of urinary protein in pregnancy is less than 300 mg/day or less than 1+ on dipstick.
- Increased urinary glucose: The amount of glucose excreted in the urine increases by 100% to 200% during pregnancy. This is due to decreased tubular reabsorption and increased insulin resistance (the reduced ability of the body to respond to insulin). The urinary glucose reaches its highest point at mid-pregnancy and then declines slightly until term. The normal range of urinary glucose in pregnancy is less than 100 mg/dL or negative on dipstick.
- The renal changes result in increased renal clearance (the rate at which the kidneys remove substances from the blood) and decreased serum osmolality (the concentration of solutes in the blood) that maintain fluid and electrolyte balance, excrete metabolic wastes, and regulate blood pressure during pregnancy
- The renal changes may cause symptoms such as frequency, urgency, nocturia (urination at night), or glycosuria (glucose in the urine) that are normal or abnormal depending on the severity, duration, and frequency
Gastrointestinal Changes in pregnancy
- The gastrointestinal system undergoes significant changes to meet the increased nutritional needs of pregnancy and to accommodate the growing uterus.
- The main gastrointestinal changes include:
- Decreased gastric motility: The movement of food through the stomach and intestines slows down during pregnancy. This is due to increased progesterone levels that relax the smooth muscle of the gastrointestinal tract and decrease the tone of the lower esophageal sphincter (the valve that prevents reflux of stomach contents into the esophagus). The gastric motility decreases progressively throughout pregnancy and reaches its lowest point at term.
- Decreased gastric acid secretion: The amount of acid produced by the stomach decreases during pregnancy. This is due to increased progesterone levels that inhibit the secretion of gastrin (the hormone that stimulates acid production) and increase the secretion of bicarbonate (the substance that neutralizes acid). The gastric acid secretion decreases progressively throughout pregnancy and reaches its lowest point at term.
- Increased nausea and vomiting: The sensation of nausea and the act of vomiting increase during pregnancy. This is due to increased human chorionic gonadotropin (hCG) levels that stimulate the vomiting center in the brain and increase the sensitivity to smells, tastes, or sights. The nausea and vomiting peak at 8 to 12 weeks of gestation and then subside by 16 to 20 weeks of gestation. The normal range of nausea and vomiting in pregnancy is less than five episodes per day or less than 5% weight loss.
- Increased appetite and food cravings: The desire to eat and the preference for certain foods increase during pregnancy. This is due to increased metabolic rate, increased nutritional needs, and hormonal fluctuations that affect the taste buds and olfactory receptors. The appetite and food cravings vary throughout pregnancy and may differ among individuals. The normal range of appetite and food cravings in pregnancy is based on the individual’s pre-pregnancy weight, height, and activity level.
- Increased constipation and hemorrhoids: The difficulty in passing stool and the swelling of the veins in the anus increase during pregnancy. This is due to decreased gastric motility, increased progesterone levels, increased pressure of the gravid uterus on the rectum, and increased iron intake. The constipation and hemorrhoids peak at late pregnancy and then improve by the postpartum period. The normal range of constipation and hemorrhoids in pregnancy is less than three bowel movements per week or less than 2+ on grading scale.
- Increased gallbladder dysfunction: The function of the gallbladder (the organ that stores and releases bile) decreases during pregnancy. This is due to increased progesterone levels that decrease the contractility of the gallbladder and increase the cholesterol content of the bile. The gallbladder dysfunction peaks at late pregnancy and then resolves by the postpartum period. The normal range of gallbladder dysfunction in pregnancy is asymptomatic or mild symptoms such as bloating, indigestion, or right upper quadrant pain.
- The gastrointestinal changes result in increased nutrient absorption (the process by which nutrients are taken up from the food into the blood) and decreased gastric emptying (the time it takes for food to leave the stomach) that meet the increased nutritional needs of pregnancy and accommodate the growing uterus
- The gastrointestinal changes may cause symptoms such as heartburn, flatulence, belching, or diarrhea that are normal or abnormal depending on the severity, duration, and frequency
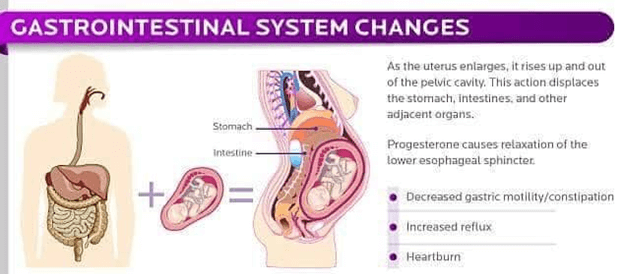
Endocrine Changes in pregnancy
- The endocrine system undergoes significant changes to regulate the metabolic, reproductive, and immunological functions of pregnancy
- The main endocrine changes include:
- Increased human chorionic gonadotropin (hCG): The hormone produced by the placenta that maintains the corpus luteum (the structure that produces progesterone) and stimulates fetal growth increases during pregnancy. The hCG levels peak at 8 to 10 weeks of gestation and then decline until term. The normal range of hCG in pregnancy is based on the gestational age and varies widely among individuals.
- Increased progesterone: The hormone produced by the corpus luteum and then by the placenta that maintains the endometrium (the lining of the uterus), inhibits uterine contractions, and prepares the breasts for lactation increases during pregnancy. The progesterone levels rise steadily throughout pregnancy and reach their highest point at term. The normal range of progesterone in pregnancy is based on the gestational age and varies widely among individuals.
- Increased estrogen: The hormone produced by the ovaries and then by the placenta that stimulates uterine growth, increases blood flow to the uterus and breasts, and enhances fetal organ development increases during pregnancy. The estrogen levels rise steadily throughout pregnancy and reach their highest point at term. The normal range of estrogen in pregnancy is based on the gestational age and varies widely among individuals.
- Increased thyroid hormones: The hormones produced by the thyroid gland that regulates the metabolic rate, protein synthesis, and fetal brain development increase during pregnancy. The thyroid hormones increase by 50% to 100% during pregnancy due to increased hCG levels, increased estrogen levels, and increased thyroid-binding globulin (the protein that carries thyroid hormones in the blood). The normal range of thyroid hormones in pregnancy is based on the gestational age and varies widely among individuals.
- Increased insulin resistance: The reduced ability of the body to respond to insulin (the hormone that lowers blood glucose levels) increases during pregnancy. This is due to increased placental hormones such as human placental lactogen (hPL), cortisol, and progesterone that antagonize the action of insulin. The insulin resistance increases progressively throughout pregnancy and reaches its highest point at term. The normal range of insulin resistance in pregnancy is based on the individual’s pre-pregnancy glucose tolerance and varies widely among individuals.
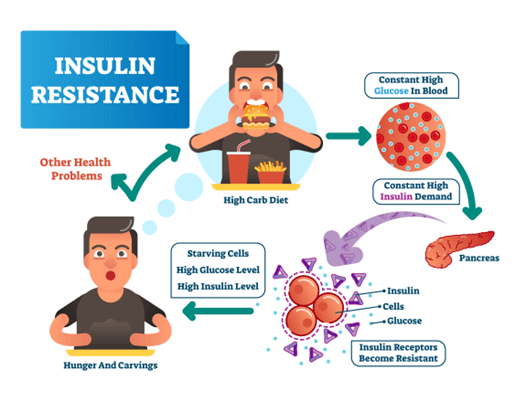
- Increased prolactin: The hormone produced by the pituitary gland that stimulates milk production and inhibits ovulation increases during pregnancy. The prolactin levels increase by 10-fold to 20-fold during pregnancy due to increased estrogen levels and suckling stimulation. The normal range of prolactin in pregnancy is based on the gestational age and varies widely among individuals.
- The endocrine changes may cause symptoms such as fatigue, mood swings, breast tenderness, or polyuria (increased urination) that are normal or abnormal depending on the severity, duration, and frequency
- The endocrine changes result in increased hormonal feedback (the process by which hormones regulate their own secretion or the secretion of other hormones) and decreased hypothalamic-pituitary-ovarian axis (the system that controls the reproductive function) that regulate the metabolic, reproductive, and immunological functions of pregnancy
- The endocrine changes may cause symptoms such as fatigue, mood swings, breast tenderness, or polyuria (increased urination) that are normal or abnormal depending on the severity, duration, and frequency
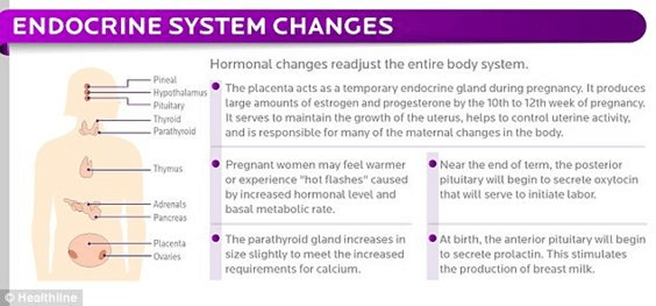
Musculoskeletal Changes in pregnancy
- The musculoskeletal system undergoes significant changes to support weight gain, posture change, and fetal growth during pregnancy
- The main musculoskeletal changes include:
- Increased joint laxity: The looseness of the joints increases during pregnancy. This is due to increased relaxin levels that relax the ligaments (the bands of tissue that connect bones) and increase the range of motion of the joints. The joint laxity increases progressively throughout pregnancy and reaches its highest point at term.
- Increased spinal curvature: The shape of the spine changes during pregnancy. This is due to increased weight gain, breast size, abdominal protrusion, and decreased abdominal muscle tone that alters the center of gravity and posture of the body. The spinal curvature increases progressively throughout pregnancy and reaches its highest point at term.
-
- Increased muscle strain: The stress on the muscles increases during pregnancy. This is due to increased weight gain, joint laxity, spinal curvature, and decreased muscle strength that affect the balance and stability of the body. The muscle strain increases progressively throughout pregnancy and reaches its highest point at term.
- The musculoskeletal changes result in increased mobility (the ability to move freely) and decreased stability (the ability to maintain balance) that support weight gain, posture change, and fetal growth during pregnancy
- The musculoskeletal changes may cause symptoms such as back pain, pelvic pain, leg cramps, or carpal tunnel syndrome (numbness or tingling in the hand) that are normal or abnormal depending on the severity, duration, and frequency
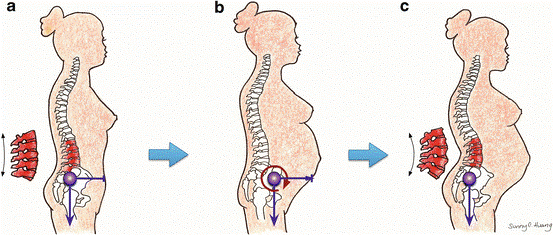
Weight Gain Guidelines in pregnancy
- Normal weight gain during pregnancy ranges from 25-35 pounds.
- Overweight women should aim to gain 15-25 pounds.
- Underweight women may need to gain 28-40 pounds.
- During the first trimester, weight gain should not exceed 1-2 kilograms.
- After the first trimester, a weight gain of 1 pound per week is recommended for the remaining two trimesters.
- In the second trimester, an extra 340 calories per day are needed.
- During the third trimester, an additional 450 calories per day are required.
- Breastfeeding mothers should consume an extra 300-400 calories per day.
- Folic acid is vital for preventing neural tube defects in the fetus.
- Good sources of folic acid include green leafy vegetables.
- Pregnant women should aim to drink 2-3 liters of water per day.
- Caffeine intake should be limited to 300 milligrams per day.
- Alcohol consumption must be avoided entirely.
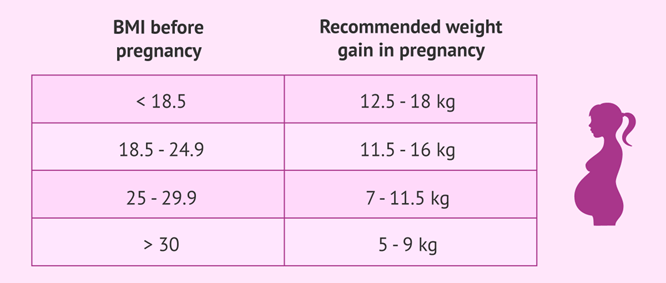
Trimester-specific Weight Gain:
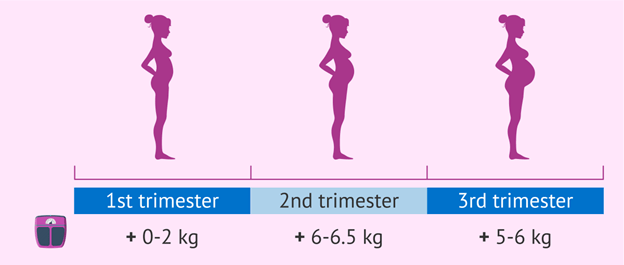
Additional Caloric Intake:
Importance of Folic Acid:
Dietary Recommendations:
Conclusion
- Pregnancy is a period of profound physiological and physical changes that affect every system of the body
- These changes are influenced by hormonal, mechanical, metabolic, immunological, and psychological factors
- These changes are adaptive and essential for the survival and development of the fetus and the preparation for labor and lactation
- These changes begin from conception and continue until the postpartum period
- These changes may cause discomfort, symptoms, or signs that are normal or abnormal depending on the severity,
- These changes may cause discomfort, symptoms, or signs that are normal or abnormal depending on the severity, duration, and frequency
- The normal ranges and variations of these changes are based on the gestational age and individual factors and vary widely among individuals
- Following appropriate weight gain guidelines, meeting increased calorie requirements, consuming folic acid-rich foods, and adhering to dietary recommendations are essential for a successful pregnancy.
- The nursing care and education for pregnant women experiencing these changes are based on the assessment, diagnosis, planning, intervention, and evaluation of the individual needs and preferences of the women and their families
Summary
- Physiological and physical changes in pregnancy affect every system of the body
- These changes are influenced by hormonal, mechanical, metabolic, immunological, and psychological factors
- These changes are adaptive and essential for the survival and development of the fetus and the preparation for labor and lactation
- These changes begin from conception and continue until the postpartum period
- These changes may cause discomfort, symptoms, or signs that are normal or abnormal depending on the severity, duration, and frequency
- The normal ranges and variations of these changes are based on the gestational age and individual factors and vary widely among individuals
- The nursing care and education for pregnant women experiencing these changes are based on the assessment, diagnosis, planning, intervention, and evaluation of the individual needs and preferences of the women and their families
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Physiological And Physical Changes In Pregnancy
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


