Please set your exam date
The Female Reproductive System
Study Questions
Comprehensive Questions
A nurse is teaching a community health class about conception. The nurse correctly identifies which of the following as the usual site of fertilization?
Explanation
Fertilization is the fusion of a spermatozoon and a secondary oocyte, forming a zygote. This typically occurs in the ampulla of the fallopian tube, the widest segment. It occurs within 12 to 24 hours post-ovulation. The oocyte remains viable for 12–24 hours, while sperm can survive in the female reproductive tract for up to 5 days. A surge in luteinizing hormone (LH) triggers ovulation. Successful fertilization requires capacitated sperm and an oocyte in the metaphase II stage.
Rationale for correct answer
C. The ampulla is the most common site of fertilization due to its anatomical structure and optimal environment for sperm-egg interaction. It provides enough space and favorable mucosal folds that support the meeting of sperm and oocyte post-ovulation. This segment accounts for over 90% of normal fertilizations.
Rationale for incorrect answers
A. The isthmus is the narrowest portion of the fallopian tube located near the uterine end. Although it plays a role in transporting the fertilized ovum to the uterus, its narrow lumen and muscular structure do not support fertilization. It is not conducive to sperm and egg interaction.
B. The infundibulum is the funnel-shaped, distal part of the fallopian tube with fimbriae that capture the oocyte post-ovulation. While it helps direct the oocyte into the tube, fertilization does not typically occur here due to its short length and insufficient time for sperm capacitation.
D. The interstitial (or intramural) portion traverses the myometrium of the uterus. It is very narrow and not structurally suited for fertilization. Fertilization in this region is rare and associated with interstitial ectopic pregnancies, which are high-risk due to late detection and significant vascularity.
Take home points
- Fertilization usually occurs in the ampulla, the widest and most spacious section of the fallopian tube.
- The isthmus and interstitial parts primarily function in transport, not fertilization.
- Ectopic pregnancies can result from fertilization outside the ampulla.
- The infundibulum helps capture the oocyte but is not the primary site of fertilization.
A nurse is counseling a client about maintaining vaginal health. The nurse instructs the client that the normal vaginal environment is characterized by which of the following pH levels?
Explanation
Vaginal pH is a critical marker of vaginal health, maintained by lactobacilli that produce lactic acid. This creates an acidic environment with a normal pH range of C.8–D.5 in reproductive-age individuals. The acidity protects against pathogens like Gardnerella vaginalis and Candida albicans. Estrogen promotes glycogen deposition in vaginal epithelial cells, which lactobacilli ferment into lactic acid. Disruption by antibiotics, semen, or douching can shift pH, predisposing to infection.
Rationale for correct answer
D. A vaginal pH of C.8–D.5 is considered normal due to the activity of lactobacilli converting glycogen into lactic acid. This acidic pH inhibits the growth of pathogenic organisms and supports a healthy vaginal microbiome in reproductive-age individuals.
Rationale for incorrect answers
A. A pH of 7.5–7.9 is alkaline and not characteristic of the normal vaginal environment. This level is often associated with infections like bacterial vaginosis, which result from a reduction in protective lactobacilli.
B. A neutral pH of approximately 7.0 is too high for normal vaginal flora maintenance. A pH near this value can support pathogenic overgrowth and is seen in postmenopausal women or those with infections.
C. A pH of F.0–F.5 is still higher than normal for healthy reproductive-age women. This range may be seen during menstruation or immediately after intercourse due to alkaline semen or blood, but it does not represent the baseline vaginal pH.
Take home points
- Normal vaginal pH ranges from C.8–D.5 and is maintained by lactobacilli.
- An elevated pH can indicate infection, especially bacterial vaginosis.
- Estrogen supports the acidic environment through glycogen metabolism.
- Disruption of pH balance increases risk for infections like candidiasis and trichomoniasis.
A nurse is reviewing the phases of the female reproductive cycle with a client. Which of the following describes the phase in which the corpus luteum degenerates?
Explanation
The menstrual cycle consists of the follicular, ovulatory, luteal, and menstrual phases, regulated by hormonal fluctuations. The luteal phase begins after ovulation, typically around day 14, and lasts approximately 14 days. The corpus luteum, formed from the ruptured follicle, secretes progesterone and estrogen. If fertilization does not occur, the corpus luteum degenerates into the corpus albicans, leading to a drop in hormone levels and onset of menstruation. Normal progesterone in the luteal phase ranges from 5 to 20 ng/mL.
Rationale for correct answer
A. The corpus luteum degenerates during the luteal phase if fertilization does not occur. This leads to decreased levels of progesterone and estrogen, initiating endometrial shedding.
Rationale for incorrect answers
B. The follicular phase precedes ovulation and involves the development of ovarian follicles under the influence of FSH. The corpus luteum has not yet formed in this phase, and degeneration does not occur here.
C. The proliferative phase corresponds to the endometrial changes during the follicular phase, where the endometrium thickens under the influence of estrogen. Corpus luteum degeneration is unrelated to this phase.
D. The ovulatory phase is marked by a surge in LH leading to ovulation, where the mature follicle ruptures to release an ovum. The corpus luteum forms after this event, so it does not degenerate during this phase.
Take home points
- The luteal phase involves corpus luteum activity and possible degeneration.
- Progesterone rises after ovulation due to corpus luteum secretion.
- Degeneration triggers menstruation by hormone withdrawal.
- Ovulatory and follicular phases precede luteal changes.
A nurse is teaching a client about hormonal regulation during the menstrual cycle. Which of the following hormones are directly involved in regulating the female reproductive cycle?
Explanation
The female reproductive cycle is tightly regulated by the hypothalamic-pituitary-ovarian axis involving the hormones gonadotropin-releasing hormone (GnRH), FSH, LH, estrogen, and progesterone. FSH stimulates follicle maturation, while LH triggers ovulation. Estrogen promotes endometrial proliferation, and progesterone maintains the endometrium. Normal ranges: FSH (D.7–2A.5 mIU/mL), LH (5–20 mIU/mL mid-cycle), estrogen (20–400 pg/mL), and progesterone (5–20 ng/mL in luteal phase).
Rationale for correct answer
A. Estrogen, progesterone, LH, and FSH are the key hormones that regulate follicular development, ovulation, endometrial changes, and menstrual shedding. FSH and LH come from the anterior pituitary and directly influence ovarian hormone secretion.
Rationale for incorrect answers
B. While estrogen, FSH, and LH are correct, androgens are not central regulators of the menstrual cycle. They are present in females in low levels and primarily serve as precursors for estrogen but do not directly regulate the cycle.
C. Testosterone and androgens play a minimal role in the female reproductive cycle. Estrogen and LH are involved, but this group omits progesterone and FSH, both of which are essential regulators of the menstrual cycle.
D. Although LH, estrogen, and progesterone are important, testosterone is not a major hormone in menstrual regulation. FSH, which is omitted, is essential for follicular development.
Take home points
- FSH and LH initiate and regulate follicular development and ovulation.
- Estrogen and progesterone regulate endometrial changes.
- Testosterone plays a minor role in female reproductive physiology.
- Androgens are not central to menstrual cycle regulation.
A nurse is preparing a client for vaginal delivery. Which of the following describes the role of the vagina during childbirth?
Explanation
The vagina forms the distensible muscular tube that connects the external genitalia to the uterus and serves as the lower part of the birth canal. During childbirth, the vaginal wall undergoes significant elastic stretching under hormonal influence, especially by estrogen and relaxin, to allow fetal passage. Vaginal pH ranges from C.8 to D.5, maintained by lactobacilli, which inhibit pathogenic growth but are not directly involved in labor mechanics.
Rationale for correct answers
B. The vagina functions as the lower portion of the birth canal, allowing the fetus to pass from the uterus to the outside during delivery. Its muscular and elastic walls accommodate fetal passage during the second stage of labor through distension and stretching.
Rationale for incorrect answers
A. The vagina does produce mucus, but this function is more relevant for sperm transport during ovulation, not for childbirth. The mucus originates primarily from the cervix, not the vaginal wall itself.
C. Contractions that expel the fetus originate in the myometrium of the uterus, not the vagina. The vagina does not contract forcefully to aid in fetal expulsion; instead, it passively expands.
D. Hormones that initiate labor, such as oxytocin and prostaglandins, are secreted by the maternal hypothalamus, posterior pituitary, and fetal membranes. The vagina does not play a role in endocrine signaling for labor onset.
Take home points
- The vagina forms the terminal portion of the birth canal.
- Uterine myometrial contractions, not vaginal contractions, expel the fetus.
- Vaginal mucus secretion supports reproduction but not labor.
- Hormonal initiation of labor involves systemic sources, not the vagina.
A nurse is counseling a postpartum client about breastfeeding. Which of the following hormones is primarily responsible for milk production in the breasts?
Explanation
Lactation is the neuroendocrine process of milk synthesis and ejection that occurs in response to infant suckling and is regulated by hormonal control. The anterior pituitary secretes prolactin, which stimulates milk production, while the posterior pituitary releases oxytocin to induce milk ejection. Normal serum prolactin levels in non-lactating women are 4–23 ng/mL but rise to >100 ng/mL during lactation.
Rationale for correct answers
C. Prolactin is produced by the anterior pituitary and is responsible for stimulating the alveolar epithelial cells of the mammary glands to synthesize and secrete milk. Its levels increase significantly postpartum and are sustained by continued infant suckling.
Rationale for incorrect answers
A. Oxytocin, secreted by the posterior pituitary, is responsible for the milk ejection reflex, not milk production. It causes contraction of the myoepithelial cells surrounding the alveoli but does not initiate milk synthesis.
B. Estrogen promotes breast ductal growth during pregnancy but inhibits lactogenesis. After delivery, estrogen levels drop sharply, allowing prolactin to act unopposed. Estrogen does not directly contribute to milk synthesis postpartum.
D. Progesterone supports lobuloalveolar development during pregnancy and also inhibits milk production by blocking prolactin receptors. After childbirth, the decline in progesterone allows prolactin-mediated milk production to begin.
Take home points
- Prolactin is the principal hormone responsible for milk synthesis.
- Oxytocin is responsible for milk ejection, not production.
- Estrogen and progesterone suppress lactation during pregnancy.
- Prolactin levels rise with suckling and fall without breast stimulation.
A nurse is discussing hormonal changes with a client at 10 weeks gestation. Which of the following is the primary role of progesterone produced by the ovaries?
Explanation
Progesterone is a steroid hormone secreted by the corpus luteum during early pregnancy and later by the placenta. It is essential in maintaining uterine quiescence by inhibiting myometrial contractions, stabilizing the endometrial lining, and supporting immune tolerance of the fetus. Serum progesterone levels typically rise to >10 ng/mL in the first trimester to maintain pregnancy.
Rationale for correct answers
B. Progesterone inhibits uterine smooth muscle contractions, stabilizes the endometrium, and promotes decidualization to support embryo implantation. This prevents spontaneous miscarriage and maintains early pregnancy. It is crucial from conception through the first trimester until placental progesterone production takes over.
Rationale for incorrect answers
A. Follicle development is stimulated by follicle-stimulating hormone (FSH), not progesterone. Progesterone is secreted after ovulation and has no role in early follicular phase activities.
C. Ovulation is triggered by a surge in luteinizing hormone (LH), not progesterone. In fact, high levels of progesterone post-ovulation inhibit further ovulation through negative feedback on gonadotropins.
D. Milk ejection during breastfeeding is stimulated by oxytocin, not progesterone. Progesterone actually inhibits milk secretion during pregnancy by antagonizing prolactin's effects on the mammary glands.
Take home points
- Progesterone maintains pregnancy by inhibiting uterine contractions.
- It is produced by the corpus luteum and later by the placenta.
- It prevents miscarriage by stabilizing the endometrial lining.
- It suppresses ovulation and milk secretion during pregnancy.
A nurse is educating a group of women about lifestyle practices that support a healthy vaginal microbiome. Which of the following actions is most effective in promoting a balanced vaginal pH?
Explanation
The vaginal microbiome is dominated by Lactobacillus species which help maintain an acidic pH, typically ranging from C.8 to D.E. This low pH inhibits overgrowth of pathogenic organisms. Moisture retention, synthetic fabrics, and alkaline disruptions can shift the vaginal flora, increasing the risk for bacterial vaginosis, vulvovaginal candidiasis, and urinary tract infections. Lactobacilli also produce hydrogen peroxide and lactic acid, critical in maintaining the host defense barrier. Normal vaginal discharge is clear to white, pH C.8–D.5, and free from foul odor or itching. Disruption in this environment leads to increased colonization by Gardnerella vaginalis, Candida albicans, or Escherichia coli.
Rationale for correct answers
B. Wearing breathable cotton underwear prevents prolonged moisture retention, reduces heat accumulation, and allows air circulation, preserving the acidic environment. Avoiding moisture prevents maceration and supports Lactobacillus dominance, reducing the risk of pathogenic overgrowth and inflammation.
Rationale for incorrect answers
A. Scented vaginal wipes contain chemicals and preservatives that can disrupt the natural acidic pH. These products may eliminate beneficial Lactobacilli, causing a rise in pH above D.5, creating a favorable environment for Candida or Gardnerella proliferation.
C. High-sugar foods elevate systemic glucose levels and can increase vaginal glucose, feeding opportunistic pathogens like Candida albicans. This results in higher colonization and symptomatic yeast infections, disrupting microbial balance rather than promoting it.
D. Doubling menstrual pad use during light flow days retains moisture and heat, leading to a rise in pH and creating a breeding ground for bacteria. Occlusion of the perineal area impairs ventilation, suppresses Lactobacillus growth, and increases infection risk.
Take home points
- Vaginal pH of C.8–D.5 supports Lactobacillus dominance and prevents infection.
- Cotton underwear promotes air flow and reduces humidity, preserving vaginal microbiota.
- Scented hygiene products can disrupt vaginal flora by altering pH.
- High glucose intake promotes fungal overgrowth like Candida albicans.
A client asks the nurse, “What is the main function of the cervix?” Which of the following responses by the nurse is most accurate?
Explanation
The cervix is the lower narrow portion of the uterus that connects to the vagina, forming part of the birth canal. It is composed of fibrous and muscular tissue and contains the endocervical canal, which allows the passage of menstrual blood, sperm, and the fetus during labor. Cervical mucus changes throughout the cycle to facilitate or restrict sperm entry. During childbirth, the cervix dilates up to 10 cm to permit fetal expulsion. Normal cervical length in pregnancy is C.0–D.5 cm, and integrity of the cervix is vital to maintain pregnancy.
Rationale for correct answers
A. The cervix serves as a canal for menstrual blood to exit the uterus and expands during labor to allow passage of the fetus. Cervical dilation from 0 to 10 cm is a hallmark of labor progression, making this the most accurate description of its primary functions.
Rationale for incorrect answers
B. The cervix does not produce or regulate hormones. Hormonal control of the menstrual cycle is primarily mediated by the hypothalamus, anterior pituitary (FSH, LH), and ovaries (estrogen, progesterone).
C. Egg maturation and storage occur in the ovaries, not the cervix. The cervix plays no role in oocyte development or fertilization aside from allowing sperm entry into the uterus.
D. Milk production is stimulated by prolactin from the anterior pituitary and is unrelated to cervical function. The cervix has no involvement in lactation or postpartum hormone signaling.
Take home points
- The cervix allows passage of blood, sperm, and fetus.
- It dilates up to 10 cm during labor to enable childbirth.
- It does not produce hormones or eggs.
- Cervical mucus changes support fertility during ovulation.
A nurse is teaching a client about the function of the ovaries. Which of the following statements accurately describes the role of the ovaries?
Explanation
The ovaries are paired gonadal organs responsible for oogenesis and endocrine secretion. They produce ova (female gametes) through folliculogenesis and release them during ovulation, typically around day 14 of a 28-day menstrual cycle. Ovaries also secrete estrogen and progesterone, which regulate endometrial proliferation, ovulation, and pregnancy maintenance. Normal ovarian volume in reproductive-age women ranges from 5–15 cm³. Hormonal control involves the hypothalamic-pituitary-ovarian axis, with FSH stimulating follicle growth and LH triggering ovulation.
Rationale for correct answers
B. The ovaries produce ova and secrete the hormones estrogen and progesterone, which are critical for menstrual cycle regulation, endometrial preparation, ovulation, and support of early pregnancy.
Rationale for incorrect answers
A. Ovaries do not regulate implantation or the precise timing of menstruation. Implantation occurs in the uterus, and timing of menstruation is hormonally controlled by the hypothalamic-pituitary-ovarian axis.
C. Prolactin and oxytocin are produced by the anterior and posterior pituitary glands, respectively—not the ovaries. These hormones are involved in milk production and let-down reflex, unrelated to ovarian function.
D. The ovaries do not serve as conduits for sperm. Sperm travel from the cervix into the uterus and then into the fallopian tubes, where fertilization typically occurs; the ovaries only release the ovum.
Take home points
- Ovaries produce ova and hormones regulating the menstrual cycle.
- Estrogen and progesterone originate from ovarian follicles and corpus luteum.
- Ovulation typically occurs around day 14 of a 28-day cycle.
- Ovaries are not involved in lactation or sperm transport.
A nurse is reviewing the functions of ovarian hormones. Which of the following are primary functions of estrogen? Select all that apply
Explanation
Estrogen is a steroid hormone primarily synthesized by granulosa cells in the ovaries under FSH stimulation. It regulates female reproductive physiology, including secondary sex characteristic development, endometrial proliferation, and bone metabolism. Serum estradiol (E2), the most active estrogen, typically ranges from 30–400 pg/mL during the menstrual cycle. Estrogen receptors α and β mediate its effects in reproductive tissues, bones, brain, and cardiovascular system.
Rationale for correct answers
B. Estrogen preserves bone density by inhibiting osteoclast activity and promoting osteoblast survival. It reduces bone resorption, and estrogen deficiency increases the risk for osteoporosis, particularly postmenopause.
C. Estrogen is essential for the development of secondary sexual characteristics, such as breast development, distribution of body fat to hips and breasts, and maturation of the female reproductive organs during puberty.
E. Estrogen regulates the menstrual cycle by stimulating endometrial proliferation during the follicular phase and modulating feedback on the hypothalamic-pituitary axis, which controls FSH and LH release.
Rationale for incorrect answers
A. Progesterone, not estrogen, primarily prepares the endometrium for implantation. After ovulation, the corpus luteum secretes progesterone, which stabilizes the endometrium and promotes secretory transformation necessary for blastocyst implantation.
D. Relaxin, not estrogen, is the hormone responsible for softening the pubic symphysis and pelvic ligaments in preparation for childbirth. It increases pelvic flexibility and reduces collagen synthesis in connective tissues during pregnancy.
Take home points
- Estrogen regulates endometrial proliferation, menstrual cycling, and bone metabolism.
- Progesterone prepares the endometrium for implantation post-ovulation.
- Relaxin, not estrogen, softens pelvic joints during pregnancy.
- Estrogen deficiency leads to osteoporosis due to increased bone resorption.
A nurse is educating a postpartum client about the physiology of breastfeeding. Which of the following hormones are directly involved in milk production and ejection? Select all that apply
Explanation
Lactation is regulated by neuroendocrine mechanisms involving prolactin and oxytocin, which coordinate milk synthesis and milk ejection. Prolactin, secreted by the anterior pituitary, stimulates alveolar epithelial cells to synthesize milk. Oxytocin, released from the posterior pituitary in response to suckling, induces contraction of myoepithelial cells. Normal prolactin levels in nonpregnant females are 4–23 ng/mL; levels rise significantly postpartum with suckling stimuli.
Rationale for correct answers
A. Oxytocin triggers the milk ejection reflex by stimulating contraction of myoepithelial cells surrounding alveoli, forcing milk into lactiferous ducts. It is released in response to nipple stimulation during breastfeeding and acts rapidly via neuroendocrine feedback.
C. Prolactin directly promotes milk production by stimulating alveolar epithelial cells to synthesize casein, lactose, and lipids. It is released in pulses with suckling, maintaining high concentrations postpartum to ensure sustained lactation.
Rationale for incorrect answers
B. FSH regulates the development of ovarian follicles and estradiol production during the follicular phase of the menstrual cycle. It has no physiological role in lactation or milk production.
D. LH triggers ovulation and luteinization of the follicle. Its primary function is in ovulation and corpus luteum maintenance, not in lactation. LH is suppressed during breastfeeding due to high prolactin levels.
E. Growth hormone stimulates tissue growth and metabolism but does not directly participate in milk synthesis or ejection. While it may influence mammary gland development, it is not involved in the lactational process postpartum.
Take home points
- Prolactin initiates and maintains milk synthesis postpartum.
- Oxytocin mediates the milk let-down reflex via myoepithelial contraction.
- FSH and LH are involved in ovarian function, not lactation.
- Growth hormone plays no direct role in postpartum milk production.
A nurse is explaining to a client the changes in cervical mucus throughout the menstrual cycle. Which of the following characteristics describe cervical mucus during the ovulation phase? Select all that apply
Explanation
Cervical mucus changes during ovulation
Cervical mucus undergoes cyclical changes in response to estrogen and progesterone. During ovulation, rising estrogen levels cause the mucus to become thin, alkaline, and stretchy to facilitate sperm transport and survival. Normal vaginal pH is C.8–D.5, but during ovulation, cervical mucus pH rises to 7.0–8.E. These changes optimize sperm motility and increase fertility. After ovulation, progesterone dominance causes mucus to become thick and impenetrable to sperm.
Rationale for correct answers
C. Thin and watery mucus appears during ovulation due to elevated estrogen levels, which reduce mucin content and increase water content. This texture supports sperm penetration.
D. Spinnbarkeit describes the mucus's ability to stretch between the fingers, characteristic of ovulatory mucus. This elasticity correlates with peak estrogen influence.
E. Alkaline pH (7.0–8.5) is seen in ovulatory mucus, neutralizing the normally acidic vaginal environment. This enhances sperm viability and motility for fertilization.
Rationale for incorrect answers
A. Thick and sticky mucus is characteristic of the luteal phase under progesterone influence. This mucus forms a barrier to sperm and pathogens post-ovulation.
B. Acidic pH is typical outside the fertile window, particularly in the follicular and luteal phases. Acidic mucus is hostile to sperm and prevents fertilization.
Take home points
- Estrogen makes cervical mucus thin, stretchy, and alkaline during ovulation.
- Spinnbarkeit and alkalinity signal peak fertility.
- Thick, acidic mucus after ovulation is progesterone-driven and sperm-inhibiting.
- Cervical mucus changes are essential fertility indicators.
A nurse is providing health education to a client about maintaining vaginal health. Which of the following instructions should the nurse include? Select all that apply
Explanation
Vaginal health maintenance
Vaginal health is preserved by a delicate balance of flora, pH, moisture, and hormonal regulation. The normal vaginal pH ranges from C.8 to D.5, maintained primarily by Lactobacillus species, which produce lactic acid and hydrogen peroxide, creating an environment hostile to pathogens. Disruption of this balance by douching, harsh chemicals, or non-breathable clothing increases the risk of infections like bacterial vaginosis or vulvovaginal candidiasis. Hormonal shifts, particularly post-menopause, can lead to atrophic vaginitis, which may be alleviated with localized estrogen or lubricants.
Rationale for correct answers
B. Cotton underwear is breathable and helps maintain dryness and ventilation in the genital area, reducing risk of yeast and bacterial overgrowth associated with moist, occlusive environments.
C. Lactobacillus species help sustain the vagina’s acidic pH (C.8–D.5) by metabolizing glycogen into lactic acid. This inhibits growth of pathogenic bacteria and fungi.
D. Harsh soaps and perfumed products can alter vaginal flora and pH, stripping protective oils and disrupting the mucosal barrier, leading to irritation or infection.
Rationale for incorrect answers
A. Routine douching disrupts normal vaginal flora and pH, removing protective Lactobacillus and increasing susceptibility to bacterial vaginosis, pelvic inflammatory disease, and yeast infections. It is not medically recommended.
E. While vaginal dryness is common with aging due to estrogen decline, it is not considered a benign, untreatable issue. Management may include vaginal moisturizers, lubricants, or low-dose topical estrogen to alleviate discomfort and prevent atrophy.
Take home points
- Vaginal pH is maintained by Lactobacillus and should remain acidic to prevent infection.
- Cotton underwear promotes airflow and dryness, supporting vaginal health.
- Avoid douching and harsh products that disrupt the vaginal ecosystem.
- Vaginal dryness in aging is treatable and should not be ignored.
A nurse is teaching a group of clients about the role of the uterus in reproduction. Which of the following are true statements about the uterus? Select all that apply
Explanation
Uterine function in reproduction
The uterus is a muscular organ that plays a critical role in menstruation, implantation, fetal development, and labor. It consists of the endometrium, myometrium, and perimetrium layers. The endometrium undergoes cyclical changes under hormonal influence, shedding during menstruation if fertilization does not occur. In pregnancy, the uterus expands to accommodate the fetus, and its myometrial contractions are essential for expelling menstrual blood and delivering the newborn. It does not directly regulate ovarian hormones, but responds to them, particularly estrogen and progesterone, which drive the menstrual cycle.
Rationale for correct answers
A. The myometrium of the uterus contracts rhythmically during menstruation to expel endometrial tissue and blood through the cervix and vagina.
B. The endometrium provides a nutrient-rich environment necessary for the implantation and early nourishment of the embryo after fertilization.
D. The uterus expands significantly during pregnancy, from approximately 7.5 cm in length in the non-pregnant state to about 35 cm at term, accommodating fetal growth and amniotic fluid.
Rationale for incorrect answers
C. The uterus does not regulate hormone levels for ovulation. Ovulation is regulated by the hypothalamic-pituitary-ovarian axis, involving gonadotropin-releasing hormone (GnRH), luteinizing hormone (LH), and follicle-stimulating hormone (FSH), with the ovaries being the direct site of ovulation.
E. The uterus does not connect the fallopian tubes to the ovaries. The fallopian tubes extend from the uterine cornua toward the ovaries but are not physically connected; instead, the fimbriae help guide the released ovum into the tube during ovulation.
Take home points
- The uterus contracts during menstruation and labor to expel contents.
- The endometrium supports embryo implantation and early development.
- Uterine expansion accommodates fetal growth during pregnancy.
- The uterus responds to, but does not produce or regulate, ovulatory hormones.
Practice Exercise 1
Which ligament connects the ovary to the uterus?
Explanation
The ovarian ligament is a fibromuscular band that connects the medial pole of the ovary to the lateral aspect of the uterus, specifically at the uterine cornu. It is a remnant of the gubernaculum, which also gives rise to the round ligament. The ovarian ligament lies within the broad ligament, specifically in the mesovarium, and plays a role in stabilizing the ovary's position. It contains no major vessels, unlike the suspensory ligament, which houses the ovarian artery and vein. The ovarian ligament is not involved in lymphatic drainage or innervation.
Rationale for correct answers
B. The ovarian ligament directly connects the ovary to the uterus at the uterine cornu. This anatomical relationship is specific and distinguishes it from other pelvic ligaments. Its origin from the gubernaculum and its location within the mesovarium confirm its role in anchoring the ovary to the uterus.
Rationale for incorrect answers
A. The broad ligament is a double layer of peritoneum that supports the uterus, fallopian tubes, and ovaries. It does not directly connect the ovary to the uterus. Instead, it serves as a mesentery and contains the ovarian ligament, round ligament, and suspensory ligament within its subdivisions (mesovarium, mesosalpinx, mesometrium).
C. The suspensory ligament of the ovary connects the lateral pole of the ovary to the pelvic wall and contains the ovarian vessels. It is involved in vascular supply, not structural connection to the uterus. Its role is to suspend the ovary and facilitate blood flow, not to anchor it to the uterus.
D. The round ligament extends from the uterine cornu through the inguinal canal to the labia majora. It originates from the gubernaculum but does not connect to the ovary. Its function is to maintain anteversion of the uterus, not to stabilize the ovary.
Take home points
• The ovarian ligament connects the ovary to the uterus at the uterine cornu.
• The suspensory ligament contains ovarian vessels and connects the ovary to the pelvic wall.
• The broad ligament is a peritoneal fold that supports pelvic organs but does not directly connect them.
• The round ligament maintains uterine position and passes through the inguinal canal
Which are functions of progesterone? Select all that apply:
Explanation
Progesterone is a steroid hormone mainly produced by the corpus luteum and later by the placenta during pregnancy. It regulates the endometrium, prepares the uterus for implantation, and maintains pregnancy by inhibiting uterine contractions. It increases basal body temperature by about 0.3–0.5 °C post-ovulation. Normal serum progesterone is <1 ng/mL in the follicular phase and >3 ng/mL in the luteal phase.
Rationale for correct answers
A. Progesterone increases basal body temperature by acting on the hypothalamic thermoregulatory center, raising temperature by 0.3–0.5 °C after ovulation. This physiologic rise helps in ovulation detection.
B. Progesterone maintains the uterine lining by supporting secretory phase changes in the endometrium, preventing shedding during pregnancy. It suppresses myometrial contractility to allow embryo implantation and growth.
D. Progesterone softens pelvic ligaments, particularly during late pregnancy, by influencing connective tissue remodeling, aiding in birth canal flexibility.
Rationale for incorrect answers
C. Progesterone does not stimulate ovulation; instead, luteinizing hormone (LH) surge from the anterior pituitary triggers ovulation. Progesterone levels rise only after ovulation in the luteal phase.
E. Progesterone does not promote endometrial growth; estrogen is the main hormone driving proliferative phase endometrial growth. Progesterone acts after proliferation to convert the endometrium into a secretory form for implantation.
Take home points
• Progesterone prepares and maintains the endometrium for implantation.
• Estrogen drives endometrial proliferation, progesterone drives secretory changes.
• Progesterone inhibits uterine contractility to prevent miscarriage.
• LH, not progesterone, triggers ovulation.
At which stage of meiosis is the secondary oocyte arrested until fertilization occurs?
Explanation
Oogenesis is the process of haploid gamete formation in females, beginning before birth and completed only if fertilization occurs. Primary oocytes are arrested in prophase I from fetal life until ovulation. At ovulation, meiosis I completes, producing the secondary oocyte, which arrests in metaphase II until sperm penetration triggers completion of meiosis II. Normal female gametes have 23 chromosomes (n).
Rationale for correct answer
B. The secondary oocyte is arrested in metaphase II due to cytostatic factor, maintaining meiotic arrest until fertilization. Sperm entry activates calcium-dependent pathways that resume meiosis II, producing the ovum and second polar body.
Rationale for incorrect answers
A. Prophase I arrest occurs in primary oocytes from fetal life until puberty; this is before formation of the secondary oocyte.
C. Anaphase II is the stage where sister chromatids separate during completion of meiosis II; it occurs only after fertilization starts, not before.
D. Telophase I follows anaphase I when primary oocytes complete meiosis I; this produces the secondary oocyte but is not the arrest point before fertilization.
Which ovarian hormone primarily inhibits FSH secretion from the anterior pituitary?
Explanation
Inhibin is a peptide hormone secreted by granulosa cells in the ovary and by Sertoli cells in the testis. It selectively suppresses follicle-stimulating hormone (FSH) secretion from the anterior pituitary without significantly affecting luteinizing hormone (LH). Inhibin levels are highest in the luteal phase, helping prevent excessive follicular recruitment. Normal serum inhibin B levels in reproductive-age females are about 45–120 pg/mL during the follicular phase.
Rationale for correct answer
C. Inhibin directly inhibits FSH release by acting on the anterior pituitary gonadotrophs, providing negative feedback to regulate follicular development and prevent multiple dominant follicles in a cycle.
Rationale for incorrect answers
A. Estrogen can exert both negative and positive feedback on gonadotropin release, but its negative feedback affects both LH and FSH; selective inhibition of FSH is mainly by inhibin.
B. Progesterone primarily inhibits GnRH pulse frequency and has stronger effects on LH suppression; it is not the main selective inhibitor of FSH.
D. Relaxin is produced by the corpus luteum and placenta, mainly to soften pelvic ligaments and prepare the cervix for labor, with no significant role in FSH suppression.
Take home points
- Inhibin is the main selective suppressor of FSH.
- Granulosa cells secrete inhibin in females; Sertoli cells do so in males.
- Estrogen and progesterone provide broader gonadotropin feedback, not selective FSH inhibition.
- Inhibin levels are highest in the luteal phase.
Approximately how many oocytes will mature and be ovulated during a woman’s reproductive lifespan?
Explanation
Ovarian follicular reserve refers to the finite number of oocytes a female is born with. At birth, ovaries contain about 1–2 million primary oocytes, decreasing to about 300,000–400,000 by puberty due to atresia. Only about 400–500 of these will fully mature and be ovulated during the reproductive lifespan, while the remainder degenerate. Normal reproductive lifespan averages 35–40 years from menarche to menopause.
Rationale for correct answer
C. Over an average reproductive lifespan, with approximately 1 ovulation per menstrual cycle and about 12 cycles per year, only around 400–500 oocytes are released; the rest undergo atresia.
Rationale for incorrect answers
A. 50–100 is too low, as this would account for fewer than 10 years of ovulatory cycles, which is far shorter than the normal reproductive span.
B. 100–200 is still below the expected number, corresponding to fewer than 20 years of ovulations.
D. 1,000–2,000 is too high, as this would require more than double the number of ovulatory cycles that normally occur in a woman’s reproductive life.
Take home points
- Females are born with a finite, non-renewable oocyte reserve.
- Only 400–500 oocytes are ovulated in a lifetime.
- The majority of oocytes undergo atresia before ovulation.
- Menstrual cycles average 12 per year over 35–40 reproductive years.
Practice Exercise 2
Which part of the fallopian tube is the most common site for fertilization?
Explanation
Ampulla of the fallopian tube is the most frequent site of fertilization due to its wider lumen, mucosal folds, and slower flow, allowing prolonged contact between the oocyte and sperm. The tube’s epithelial cells secrete nutrients for gamete survival. The normal fallopian tube length is 10–12 cm, with the ampulla comprising the longest segment.
Rationale for correct answer
B. The ampulla provides the optimal environment for fertilization because its expanded lumen and ciliated epithelium facilitate sperm transBport and oocyte retention, maximizing contact time for fertilization.
Rationale for incorrect answers
A. The infundibulum, with fimbriae, captures the ovulated oocyte but is not the main fertilization site due to rapid passage into the ampulla.
C. The isthmus is a narrow muscular segment leading to the uterus; it is involved in embryo transport but is less favorable for fertilization.
D. The interstitial part passes through the uterine wall and is primarily for embryo passage into the uterine cavity, not for fertilization.
Take home points
- Fertilization most often occurs in the ampulla.
- The ampulla’s anatomy supports prolonged sperm–oocyte interaction.
- Infundibulum captures the oocyte; isthmus aids embryo transport.
- Interstitial part lies within the uterine wall.
Which are functions of the uterus during pregnancy? Select all that apply:
Explanation
Uterus is a hollow muscular organ in the female pelvis that supports embryonic and fetal development. Its endometrium undergoes cyclic changes to facilitate implantation, and the myometrium provides contractile force for delivery. During pregnancy, the uterus expands from about 7.5 cm to over 30 cm in length, with increased blood flow reaching 500–700 mL/min at term.
Rationale for correct answers
A. The uterus provides a protective, vascular, and nutrient-rich environment that supports fetal development throughout pregnancy.
C. The endometrium undergoes secretory changes under progesterone, creating optimal conditions for blastocyst implantation.
E. The myometrium contracts powerfully during labor, coordinated by oxytocin and prostaglandins, to expel the fetus.
Rationale for incorrect answers
B. The uterus does not produce sperm; spermatogenesis occurs in the seminiferous tubules of the testes.
D. The uterus does not store menstrual blood; menstrual bleeding results from shedding of the functional endometrium when implantation does not occur.
Take home points
- The uterus facilitates implantation and fetal development.
- Myometrial contractions expel the fetus during labor.
- It is hormonally responsive to estrogen and progesterone.
- It does not produce gametes or store menstrual blood.
Which uterine layer regenerates the endometrium after menstruation?
Explanation
Stratum basalis is the permanent basal layer of the endometrium that remains intact after menstruation. It contains stem cells, glands, and blood vessels that regenerate the stratum functionalis during each menstrual cycle under estrogen influence. The endometrium is normally 1–5 mm thick in the proliferative phase and can reach 5–7 mm in the secretory phase.
Rationale for correct answer
B. The stratum basalis is not shed during menstruation and serves as the source for regrowth of the stratum functionalis during the proliferative phase, driven mainly by estrogen.
Rationale for incorrect answers
A. The stratum functionalis is the superficial functional layer that thickens under estrogen and progesterone and is shed during menstruation; it does not regenerate itself.
C. The myometrium is the thick smooth muscle layer responsible for uterine contractions; it does not participate in endometrial regeneration.
D. The perimetrium is the outer serosal layer covering the uterus; it provides structural covering but has no role in regenerating endometrium.
Take home points
- Stratum basalis is the permanent regenerative layer of the endometrium.
- Stratum functionalis is shed during menstruation.
- Estrogen stimulates proliferation of endometrium post-menstruation.
- Myometrium and perimetrium are structural, not regenerative, layers.
A patient with a boggy uterus and heavy postpartum bleeding is most likely experiencing:
Explanation
Uterine atony is the failure of the myometrium to contract effectively after delivery, leading to postpartum hemorrhage (PPH). Effective myometrial contraction compresses spiral arteries to prevent excessive blood loss. Normal blood loss after vaginal delivery is ≤500 mL; in PPH, blood loss exceeds this amount, often >1,000 mL in severe cases. Risk factors include prolonged labor, overdistended uterus, multiple gestations, and chorioamnionitis.
Rationale for correct answer
B. A boggy uterus on palpation with heavy postpartum bleeding indicates inadequate myometrial contraction, the hallmark of uterine atony, which is the most common cause of early postpartum hemorrhage.
Rationale for incorrect answers
A. Endometriosis involves ectopic endometrial tissue causing pelvic pain and infertility; it is unrelated to acute postpartum bleeding.
C. Fibroids (leiomyomas) are benign smooth muscle tumors that may cause menorrhagia and infertility but do not present acutely with boggy uterus and massive postpartum bleeding.
D. Uterine prolapse is descent of the uterus into or beyond the vaginal canal due to pelvic floor weakness, presenting with pelvic pressure, not acute postpartum hemorrhage.
Take home points
- Uterine atony is the leading cause of early postpartum hemorrhage.
- A boggy uterus post-delivery indicates poor myometrial contraction.
- Risk factors include uterine overdistension, prolonged labor, and infection.
- Immediate uterotonic therapy and uterine massage are key interventions.
Which ligament contains the ovarian artery and vein?
Explanation
Suspensory ligament of the ovary (infundibulopelvic ligament) is a fold of peritoneum that extends from the ovary to the lateral pelvic wall and contains the ovarian artery, ovarian vein, lymphatics, and nerves. The ovarian artery normally arises from the abdominal aorta at the level of L2 and supplies the ovary and part of the fallopian tube.
Rationale for correct answer
B. The suspensory ligament transmits the ovarian vessels, making it clinically significant in oophorectomy where it must be ligated to control bleeding.
Rationale for incorrect answers
A. The broad ligament is a double layer of peritoneum supporting the uterus, fallopian tubes, and ovaries, but it does not enclose the ovarian vessels within its main structure.
C. The round ligament extends from the uterine fundus through the inguinal canal to the labia majora, containing mainly connective tissue, arteries of the round ligament, and nerves, not the ovarian vessels.
D. The uterosacral ligament extends from the uterus to the sacrum and contains connective tissue and autonomic nerves; it has no ovarian vessels.
Take home points
- The suspensory ligament contains the ovarian artery and vein.
- It must be ligated carefully in oophorectomy to prevent bleeding.
- The ovarian artery branches from the abdominal aorta at LB.
- The broad, round, and uterosacral ligaments have different structural and vascular roles.
Practice Exercise 3
Which cervical structure is the primary site for precancerous changes?
Explanation
Transformation zone is the area of the cervix where columnar epithelium of the endocervix meets the stratified squamous epithelium of the ectocervix. This region undergoes squamous metaplasia, making it particularly vulnerable to oncogenic human papillomavirus (HPV) infection, especially types 16 and 18. Normal cervical epithelium thickness varies, with the squamous epithelium being 0.2–0.5 mm thick.
Rationale for correct answer
C. The transformation zone is the most common site for cervical intraepithelial neoplasia (CIN) due to active cell turnover and susceptibility to HPV-induced dysplasia.
Rationale for incorrect answers
A. The ectocervix is the outer portion of the cervix lined by squamous epithelium, but precancerous changes typically begin at the transformation zone rather than the entire ectocervix.
B. The endocervix is lined with columnar epithelium and produces cervical mucus, but it is less commonly the site of CIN compared to the transformation zone.
D. The internal os is the anatomical junction between the cervical canal and the uterine cavity, not a common site for precancerous changes.
The acidic vaginal pH is primarily maintained by:
Explanation
Lactobacillus species are normal vaginal flora that metabolize glycogen from exfoliated epithelial cells into lactic acid, maintaining an acidic vaginal pH of C.8–D.E. This acidic environment inhibits pathogenic bacterial and yeast overgrowth. Estrogen indirectly supports this process by increasing epithelial glycogen content, especially during reproductive years.
Rationale for correct answer
B. Lactobacillus bacteria produce lactic acid from glycogen metabolism, directly lowering vaginal pH and providing antimicrobial defense.
Rationale for incorrect answers
A. Estrogen promotes glycogen-rich epithelium but does not directly acidify the vagina; its effect is mediated through lactobacilli.
C. Cervical mucus lubricates and protects the cervix but does not maintain vaginal pH.
D. Progesterone modulates cervical mucus and uterine environment but has no direct role in maintaining acidic vaginal pH.
Take home points
- Lactobacillus maintains vaginal pH at C.8–D.5 via lactic acid production.
- Estrogen indirectly supports acidity by increasing epithelial glycogen.
- Acidic pH inhibits pathogenic bacteria and yeast.
- Disruption of flora can lead to bacterial vaginosis with elevated pH.
Which hormones are directly involved in lactation? Select all that apply:
Explanation
Lactation is the process of milk synthesis and milk ejection from the mammary glands, regulated by hormonal control. Prolactin, secreted by the anterior pituitary, stimulates milk production in alveolar epithelial cells, while oxytocin, from the posterior pituitary, triggers contraction of myoepithelial cells for milk let-down. Normal prolactin levels in non-pregnant women are <25 ng/mL; during lactation, they may exceed 200 ng/mL.
Rationale for correct answers
C. Prolactin directly stimulates milk synthesis in mammary alveoli by promoting transcription of milk protein genes and lactose production.
D. Oxytocin causes myoepithelial cell contraction around alveoli and ducts, ejecting milk into the nipple during suckling.
Rationale for incorrect answers
A. Estrogen promotes ductal growth during breast development but inhibits milk secretion during pregnancy; it is not directly involved in milk production or ejection postpartum.
B. Progesterone stimulates lobuloalveolar development but, like estrogen, inhibits lactation during pregnancy; its drop after delivery allows prolactin action.
E. Relaxin softens pelvic ligaments and cervical connective tissue for labor; it plays no role in milk production or ejection.
Take home points
- Prolactin stimulates milk production; oxytocin triggers milk let-down.
- Estrogen and progesterone inhibit lactation during pregnancy despite breast development.
- Lactation requires both secretory and ejection phases.
- Suckling stimulates prolactin and oxytocin release via neuroendocrine reflexes.
What is the maximum cervical dilation during labor?
Explanation
Cervical dilation refers to the widening of the cervical opening during labor to allow passage of the fetus. Maximum dilation at complete labor is 10 cm, which permits fetal head delivery. Normal active labor progresses from 6 cm to 10 cm, with average dilation rates of about A.2 cm/hr in nulliparas and A.5 cm/hr in multiparas.
Rationale for correct answer
D. Complete cervical dilation of 10 cm is required to allow the fetal head to pass through the birth canal without cervical injury.
Rationale for incorrect answers
A. 5 cm represents early active labor, not maximum dilation.
B. 7 cm occurs in mid-active labor but is still incomplete dilation.
C. 9 cm is near-complete dilation, but delivery usually requires the full 10 cm to avoid cervical trauma.
Take home points
- Maximum cervical dilation in labor is 10 cm.
- Active labor begins at 6 cm dilation.
- Nulliparas dilate slower than multiparas on average.
- Full dilation prevents cervical tearing during fetal passage.
Montgomery glands are located in which structure?
Explanation
Montgomery glands are sebaceous glands located in the areola surrounding the nipple. They secrete an oily substance that lubricates and protects the nipple and areolar skin during breastfeeding, and may have antimicrobial properties. The average areola diameter is 15–45 mm, and Montgomery tubercles become more prominent during pregnancy and lactation.
Rationale for correct answer
B. Montgomery glands are embedded in the areola’s dermis and open onto the skin surface as Montgomery tubercles, aiding nipple protection during lactation.
Rationale for incorrect answers
A. The nipple contains openings of lactiferous ducts but not the sebaceous Montgomery glands.
C. Lactiferous ducts transport milk from mammary alveoli to the nipple; they do not contain sebaceous glands.
D. Suspensory ligaments (Cooper’s ligaments) are connective tissue structures supporting breast shape; they have no secretory or protective gland function.
Take home points
- Montgomery glands are sebaceous glands in the areola.
- They secrete lubricating and protective substances for breastfeeding.
- Prominent during pregnancy and lactation.
- Different from milk-producing and milk-transporting structures.
Exams on The Female Reproductive System
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
Upon completion of these notes, the nursing student will be able to:
• Identify and describe the key anatomical structures of the female reproductive system.
• Explain the primary physiological functions of each reproductive organ, including their roles in menstruation, conception, pregnancy, and lactation.
• Recognize important nursing implications and common conditions associated with each structure, vital for patient assessment and care.
• Differentiate between normal and abnormal findings related to the female reproductive system.
• Apply scientific principles to understand the hormonal regulation of reproductive processes.
• Identify high-yield information crucial for success in nursing examinations.
Introduction
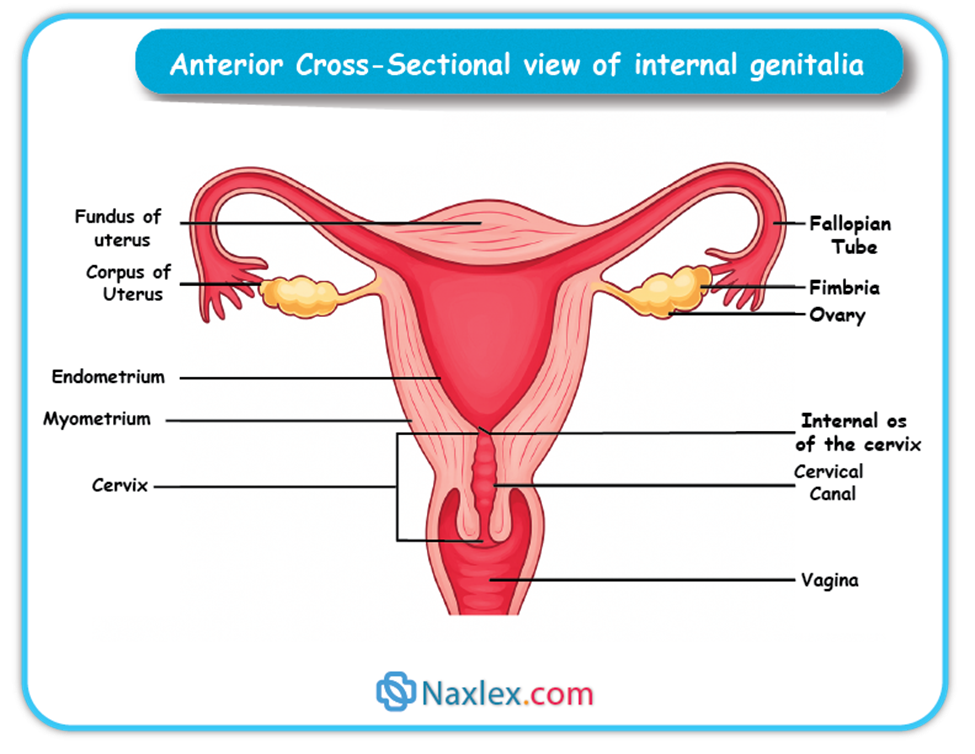
The female reproductive system is a complex biological system responsible for producing female gametes (ova), facilitating fertilization, supporting fetal development during pregnancy, and providing nourishment to the newborn through lactation. It consists of internal genitalia (ovaries, fallopian tubes, uterus, cervix, and vagina) and external genitalia, with accessory structures such as the breasts.
A detailed understanding of its anatomy, physiology, and hormonal control is essential for maternal-newborn nursing practice, especially in the areas of contraception, infertility, prenatal care, labor and delivery, postpartum recovery, and breastfeeding.
Ovaries
Anatomy and Location:
• Paired, almond-shaped organs, 2–4 cm in length, located on either side of the uterus in the pelvic cavity.
• Ligament Attachments:
➤ Ovarian ligament: Connects ovary to uterus.
➤ Suspensory ligament: Contains ovarian artery, vein, and nerves.
➤ Broad ligament (mesovarium): Fold of peritoneum providing partial support.
• Structure:
➤ Cortex: Contains ovarian follicles at various stages.
➤ Medulla: Connective tissue, blood vessels, lymphatics, nerves.
Physiology:
• Oogenesis:
➤ Begins before birth — females are born with ~1–2 million primary oocytes arrested in Prophase I.
➤ Puberty triggers resumption; one oocyte typically matures monthly.
➤ Ovulation releases a secondary oocyte arrested in Metaphase II (completes meiosis only if fertilized).
• Hormone Production:
➤ Estrogen: Endometrial growth, secondary sexual characteristics, bone health.
➤ Progesterone: Prepares/maintains endometrium for pregnancy, increases basal body temp.
➤ Relaxin: Softens pelvic ligaments, prevents premature uterine contractions.
➤ Inhibin: Inhibits FSH release.
Nursing Implications and Common Conditions:
• Ovarian cysts, PCOS, ovarian cancer.
• Early detection and patient education are critical.
Nursing Insight:
In exam scenarios, remember:
• E = Estrogen → Establishes endometrial lining.
• P = Progesterone → Prepares & Preserves pregnancy.
Fallopian Tubes
Anatomy:
• Length: Approximately 10–12 cm long.
• Parts:
➤ Infundibulum: Funnel-shaped lateral end opening into the peritoneal cavity, fringed by fimbriae that sweep the ovum into the tube.
➤ Ampulla: Widest, longest part — most common site of fertilization.
➤ Isthmus: Narrow, medial portion connecting ampulla to uterus.
➤ Interstitial (Intramural) Part: Passes through uterine wall into uterine cavity.
• Wall Layers:
➤ Serosa: Outer covering.
➤ Muscularis: Smooth muscle layer responsible for peristalsis.
➤ Mucosa: Ciliated epithelium for ovum movement; non-ciliated cells secrete nutritive fluid.
Physiology:
• Ovum Transport: Coordinated ciliary movement and muscular peristalsis move the ovum toward the uterus.
• Fertilization Site: Ampulla — optimal due to ciliary action, fluid environment, and sperm capacitation.
• Sperm Capacitation: Functional changes in sperm enabling penetration of ovum.
Nursing Implications and Common Conditions:
• Ectopic Pregnancy: Fertilized ovum implants in tube — life-threatening if ruptured.
• Pelvic Inflammatory Disease (PID): Common cause of tubal scarring → infertility.
• Tubal Ligation: Permanent contraception by blocking/cutting tubes.
Clinical Alert – Ectopic Pregnancy:
• Symptoms: Unilateral abdominal pain, vaginal bleeding, shoulder pain (referred from diaphragm irritation).
• Risk factors: PID, prior ectopic pregnancy, IUD use.
• Requires immediate medical intervention.
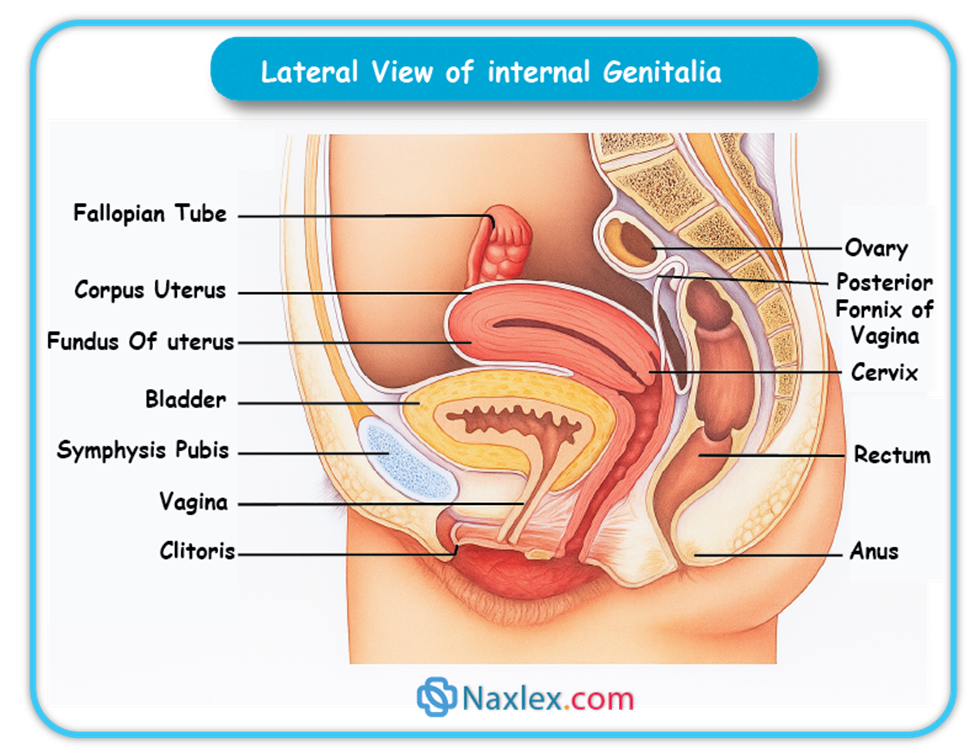
Uterus
Anatomy:
• Size (nulliparous): ~7.5 cm long, 5 cm wide, 2.5 cm thick.
• Divisions:
➤ Fundus: Dome-shaped top, above fallopian tube openings.
➤ Corpus (Body): Main central portion for implantation & fetal development.
➤ Isthmus: Narrow segment between corpus and cervix — forms lower uterine segment during labor.
• Layers:
➤ Perimetrium: Outer serous layer.
➤ Myometrium: Middle muscular layer with three fiber orientations for strong contractions.
➤ Endometrium: Inner mucosal lining with:
◆ Stratum functionalis: Proliferates and sheds each cycle.
◆ Stratum basalis: Regenerates the functional layer after menstruation.
Physiology:
• Menstruation: Shedding of stratum functionalis if no implantation occurs.
• Implantation: Blastocyst embeds in prepared endometrium.
• Fetal Development: Protective, nutritive environment for fetus.
• Labor: Myometrial contractions expel fetus; oxytocin amplifies contractions.
• Postpartum Involution: Gradual return to pre-pregnancy size; fundal height assessed by nurses.
Nursing Implications and Common Conditions:
• Fibroids (Leiomyomas): Benign myometrial tumors causing bleeding/pain.
• Endometriosis: Ectopic endometrial tissue → pain, infertility.
• Uterine Prolapse: Descent into vaginal canal due to pelvic floor weakness.
• Postpartum Hemorrhage (PPH): Often from uterine atony — massage fundus to promote contraction.
Nursing Insight:
• Myometrium function: Interwoven muscle fibers compress blood vessels after birth to prevent hemorrhage.
• Fundal checks postpartum are vital — a boggy uterus indicates atony and high PPH risk.
Cervix
Anatomy:
• External os: Opens into vagina.
• Internal os: Opens into uterine cavity.
• Cervical canal: Passage between os openings.
• Ectocervix: Squamous epithelium.
• Endocervix: Columnar epithelium.
• Transformation zone: Squamocolumnar junction — primary site of dysplasia & cancer.
Physiology:
• Mucus production: Cyclical changes — thin/stretchy at ovulation (spinnbarkeit), thick/acidic in luteal phase & pregnancy.
• Barrier role: Protects uterus from infection.
• Labor role: Effaces (thins) & dilates for fetal passage.
Nursing Insight:
• Effacement: % thinning (100% = paper-thin).
• Dilation: cm opening (10 cm = fully dilated).
• These parameters guide labor progress assessment.
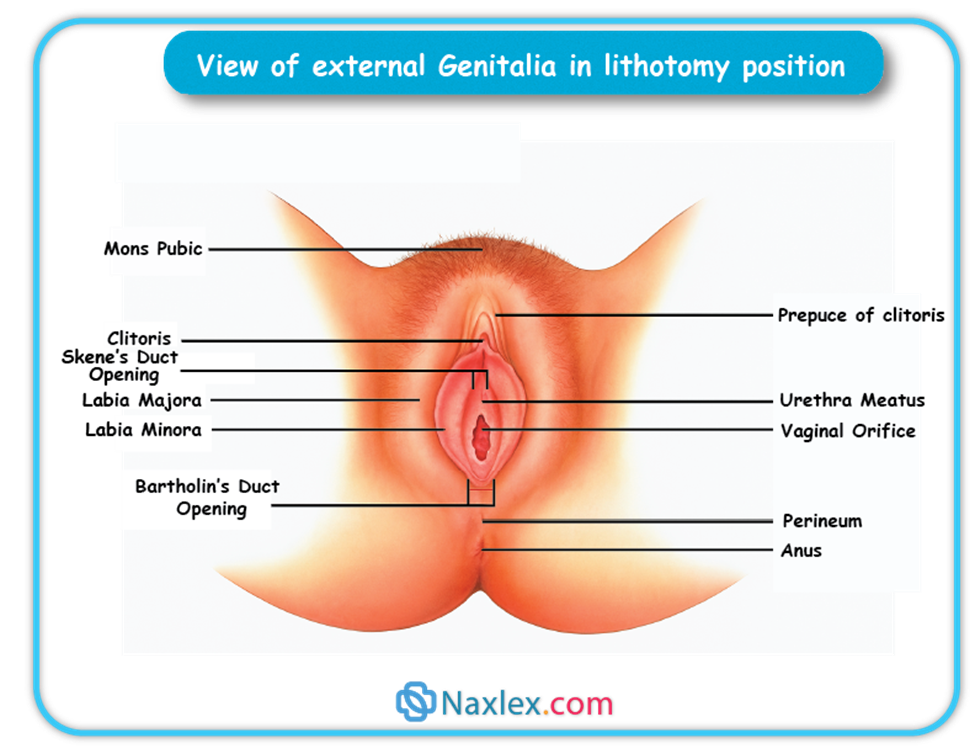
Vagina
Anatomy:
• Length: 8–10 cm.
• Lining: Stratified squamous epithelium with rugae for distention.
• pH: 3.8–4.5, maintained by lactobacilli.
• Fornices: Anterior, posterior, lateral recesses around cervix.
Physiology:
• Receives sperm, acts as birth canal, allows menstrual flow exit.
• Acidic pH + normal flora prevent infection.
Nursing Implications:
• Educate on hygiene, avoid pH disruption.
• Pelvic floor exercises for incontinence prevention.
• Manage vaginal dryness in menopause with lubricants/HRT.
Breasts (mammary Glands)
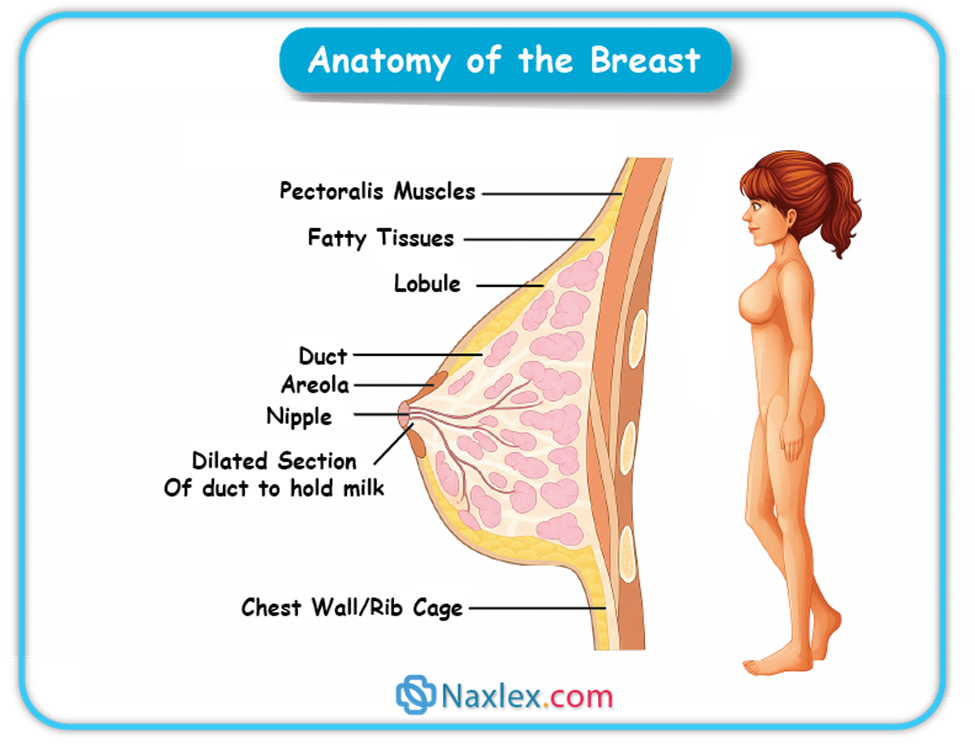
Anatomy:
• Overlie pectoralis major; extend from 2nd–6th ribs.
• Lobes & Lobules: 15–20 lobes containing milk-producing alveoli.
• Lactiferous ducts: Drain to nipple.
• Areola & Montgomery glands: Lubrication during feeding.
• Suspensory ligaments: Support structure.
Physiology:
• Mammogenesis: Breast development (estrogen, progesterone, prolactin).
• Lactogenesis: Prolactin stimulates milk production post-delivery.
• Milk ejection: Oxytocin-induced myoepithelial contraction.
• Supply-demand regulation: Frequent feeding increases production.
Nursing Implications:
• Teach latch, feeding cues, breast care.
• Monitor for mastitis, engorgement.
• Promote breast self-awareness & mammography screening.
Nursing Insight:
• Prolactin = Production
• Oxytocin = Ejection and postpartum uterine contraction.
Summary Of Concepts
• Ovaries produce ova and key reproductive hormones.
• Fallopian tubes transport ova and are the site of fertilization.
• Uterus supports fetal development, contracts during labor, and returns to pre-pregnancy state postpartum.
• Cervix serves as a gateway, changing in mucus consistency and structure during cycle and labor.
• Vagina functions in reproduction, menstruation, and childbirth, maintaining protective pH.
• Breasts produce and deliver milk, hormonally regulated by prolactin and oxytocin.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on The Female Reproductive System
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


