Please set your exam date
Medico-Surgical Procedures
Study Questions
Oxygen therapy
A nurse is caring for a patient who requires oxygen therapy due to hypoxia. What is the goal of oxygen therapy for this patient?
Explanation
Choice A rationale:
The goal of oxygen therapy is not to provide the highest fraction of inspired oxygen (FiO2) possible. This approach can be harmful because excessively high FiO2 levels can lead to oxygen toxicity and other side effects, especially in patients with certain conditions like chronic obstructive pulmonary disease (COPD).
Choice B rationale:
The goal of oxygen therapy is to use the lowest FiO2 that achieves an acceptable blood oxygen level without harmful side effects. This approach is known as titrating the oxygen therapy to the patient's needs and helps prevent potential complications associated with excessive oxygen administration.
Choice C rationale:
Maintaining a constant FiO2 regardless of the patient's breathing pattern is not the goal of oxygen therapy. In some cases, patients may require varying FiO2 levels based on their respiratory status, so it is essential to adjust the oxygen delivery accordingly.
Choice D rationale:
Delivering a fixed amount of oxygen that is independent of the patient's condition is not the goal of oxygen therapy. Oxygen therapy should be individualized and tailored to the patient's specific needs to optimize its effectiveness and safety.
(Select all that apply): A nurse is educating a group of patients about different oxygen delivery devices. Which of the following are examples of low-flow oxygen delivery systems?
Explanation
Choice A: Nasal cannula is a low-flow oxygen delivery system. It delivers a variable oxygen concentration depending on the patient's breathing pattern.
Choice B: Simple face mask is also a low-flow oxygen delivery system. It provides a variable oxygen concentration based on the patient's respiratory rate and tidal volume.
Choice C: Venturi mask is not a low-flow system. It is a high-flow oxygen delivery device that provides a fixed oxygen concentration by mixing oxygen with room air.
Choice D: Non-rebreather mask is considered a low-flow oxygen delivery system. It provides a high concentration of oxygen but does not ensure a precise oxygen concentration due to varying patient ventilation.
Explanation
Choice A rationale:
Switching to a simple face mask is not the appropriate intervention for nasal dryness and irritation. A simple face mask covers the nose and mouth, and it may not provide enough relief for nasal dryness as the oxygen flow is still directed towards the nose.
Choice B rationale:
Increasing the flow rate of oxygen will not directly improve humidity. Nasal dryness and irritation are often caused by the lack of moisture in the delivered oxygen. Increasing the flow rate may worsen the issue.
Choice C rationale:
Assessing the patient's nares for patency and skin integrity is the appropriate intervention. Nasal dryness and irritation can be caused by inadequate humidification of the oxygen. Checking the patency of the nares and the condition of the skin can help identify any issues that may be contributing to the discomfort.
Choice D rationale:
Reassuring the patient that nasal dryness is a normal side effect is not sufficient. While nasal dryness can be a common side effect of using a nasal cannula, it is essential to address the issue and provide appropriate interventions to alleviate the discomfort and prevent complications.
Explanation
Choice A rationale:
Increasing the flow rate of oxygen may not be the priority action because the patient's shortness of breath could be due to a problem with the mask itself, rather than the amount of oxygen being delivered. Before making any adjustments to the oxygen flow rate, it is essential to assess the equipment's integrity.
Choice B rationale:
This is the priority action because a partial rebreather mask relies on the patient's exhaled breath to partially fill the reservoir bag. If the mask bag does not remain inflated during both inspiration and expiration, the patient may not be receiving the appropriate oxygen concentration, leading to increased shortness of breath. Checking the mask bag ensures that the mask is functioning correctly and delivering the intended oxygen concentration.
Choice C rationale:
Switching the patient to a non-rebreather mask for higher oxygen delivery is not the priority action in this scenario. The non-rebreather mask is used when high oxygen concentrations are required, such as in emergencies or when a patient's condition requires immediate intervention. However, the priority at this moment is to assess the current equipment's effectiveness before considering a change in oxygen delivery method.
Choice D rationale:
Reassuring the patient that shortness of breath is common with this type of mask is not appropriate without first addressing the issue at hand. The nurse should first assess the mask's functionality to ensure it is working correctly and providing the appropriate oxygen concentration before addressing the patient's concerns.
Explanation
Choice A rationale:
Although a tracheostomy collar provides oxygen directly to the trachea, the advantage specified in the question is related to the ability to breathe room air when disconnected from the oxygen source.
Choice B rationale:
This is the correct answer because a tracheostomy collar has an opening that allows the patient to breathe room air when the oxygen source is disconnected. This feature enables the patient to participate in activities without continuous oxygen delivery, promoting mobility and reducing the feeling of being tethered to an oxygen supply.
Choice C rationale:
A tracheostomy collar does not provide the highest fraction of inspired oxygen (FiO2) among low-flow systems. High-flow systems, such as non-rebreather masks or venturi masks, typically provide the highest FiO2.
Choice D rationale:
A tracheostomy collar does not deliver a fixed amount of oxygen independent of the patient's breathing pattern. Instead, it provides supplemental oxygen in response to the patient's inspiratory effort, which is a characteristic of low-flow oxygen delivery systems.
Explanation
Choice A rationale:
Nasal cannula delivers low to moderate concentrations of oxygen and may not be effective for a client with thick secretions, dry mucous membranes, or upper airway edema. Additionally, the nasal cannula may not provide sufficient humidification to alleviate these conditions.
Choice B rationale:
The simple face mask is not ideal for a client with thick secretions, dry mucous membranes, or upper airway edema as it may not provide enough humidification and could be uncomfortable for the patient.
Choice C rationale:
A partial rebreather mask also may not be the most appropriate choice for this client as it has a reservoir bag that may not adequately humidify the oxygen, leading to discomfort and potential worsening of dry mucous membranes.
Choice D rationale:
The aerosol mask is the most appropriate choice because it delivers humidified oxygen in the form of small aerosol particles, which can help alleviate thick secretions, moisturize dry mucous membranes, and reduce upper airway edema. This mask is beneficial for patients who require higher humidity levels to maintain airway patency and comfort.
Explanation
Choice A rationale:
Nasal cannula delivers oxygen through two small prongs placed in the patient's nostrils. While it is a commonly used and well-tolerated device, the FiO2 delivered can vary significantly depending on the patient's breathing pattern and respiratory rate. Thus, it does not provide the most precise and consistent FiO2.
Choice B rationale:
Simple face masks cover the nose and mouth and can provide higher FiO2 levels compared to nasal cannulas. However, the FiO2 delivered still depends on the patient's breathing pattern and the mask's fit, making it less precise and consistent than other options.
Choice C rationale:
Venturi masks are designed to deliver a specific and accurate FiO2, regardless of the patient's breathing pattern. These masks have adjustable ports to control the mix of air and oxygen, providing precise oxygen concentrations.
Choice D rationale:
Non-rebreather masks have one-way valves and a reservoir bag to deliver higher concentrations of oxygen. Although they can provide high FiO2 levels, the delivered concentration can vary based on the patient's breathing pattern and the mask's fit.
Explanation
Choice A rationale:
Venturi masks are not typically used with tracheostomy patients, as they are more suitable for patients with intact upper airways.
Choice B rationale:
Tracheostomy collars are specifically designed for patients with tracheostomies. They provide oxygen directly to the tracheostomy tube, making them appropriate for weaning tracheostomized patients from mechanical ventilation.
Choice C rationale:
T-piece adapters are commonly used for patients with tracheostomies to deliver oxygen. They are simple devices that deliver oxygen directly to the tracheostomy tube.
Choice D rationale:
Aerosol masks are not specifically designed for tracheostomy patients and may not provide adequate oxygen delivery for them.
Choice E rationale:
Mechanical ventilators are not an oxygen delivery device; instead, they are used to provide mechanical ventilation support to the patient and can incorporate various oxygen delivery systems.
Explanation
Choice A rationale:
At a flow rate of 4 L/min, oxygen therapy through a nasal cannula can increase the risk of oxygen toxicity, especially if used for prolonged periods. Oxygen toxicity can cause damage to the lungs and other organs.
Choice B rationale:
Carbon dioxide retention is not a common complication at this flow rate. It may occur in patients with severe chronic obstructive pulmonary disease (COPD) at higher oxygen flow rates.
Choice C rationale:
Nasal dryness is a common but relatively minor complication of oxygen therapy via nasal cannula. It can cause discomfort but is not a severe concern.
Choice D rationale:
Fire hazard is not directly related to the use of a nasal cannula but rather to the use of oxygen in the presence of flammable materials or near open flames. It is a concern for all oxygen delivery devices, not specific to nasal cannulas.
(Select all that apply) A nurse is preparing to administer oxygen therapy to a client who has COPD and requires a precise concentration of oxygen. Which of the following devices should the nurse use for this client?
Explanation
The correct answers are choices A, C, and E.
Choice A rationale:
A Venturi mask is designed to deliver a precise concentration of oxygen and is often used in COPD, where it is important not to over-oxygenate the patient. It allows for the adjustment of oxygen concentration by changing the color-coded entrainment adapters.
Choice B rationale:
A non-rebreather mask is not typically used for clients who require a precise concentration of oxygen because it is designed to deliver high concentrations of oxygen, but without a way to precisely control the amount.
Choice C rationale:
An aerosol mask can be used with a nebulizer system to deliver specific concentrations of oxygen along with medication, which is beneficial for COPD patients who may need bronchodilators or steroids in addition to oxygen therapy.
Choice D rationale:
A simple face mask is not suitable for delivering a precise concentration of oxygen as it does not allow for the fine control needed for COPD patients. It is generally used for short-term oxygen therapy and for patients who require a moderate amount of oxygen.
Choice E rationale:
A tracheostomy collar can provide a specific concentration of oxygen when used with a tracheostomized patient and is suitable for long-term use in COPD patients who have a tracheostomy.
In summary, for a client with COPD who requires a precise concentration of oxygen, the Venturi mask, aerosol mask, and tracheostomy collar are appropriate choices as they allow for the delivery of a specific and controlled amount of oxygen.
Explanation
Choice A rationale:
Refilling the oxygen tank based on the client's perception of it feeling light and empty is not a reliable method, as it may lead to running out of oxygen unexpectedly.
Choice B rationale:
The nurse should instruct the client to refill the oxygen tank when the pressure gauge reads below 500 psi. This is a standardized method to ensure the client does not run out of oxygen, as the pressure gauge provides an accurate measure of the remaining oxygen in the tank.
Choice C rationale:
Refilling the tank when a hissing sound is heard from the valve is not a valid method for determining the need for a refill and may result in running out of oxygen.
Choice D rationale:
Waiting for an alarm sound from the regulator to refill the tank is not recommended, as the tank could run out of oxygen before the alarm activates.
A nurse is caring for a client who is dyspneic and slightly cyanotic, with a respiratory rate of 28/min. The nurse determines that the client has impaired gas exchange during which of the following phases of the nursing process?
Explanation
The correct answer is choice B: Diagnosis.
Choice A rationale:
Assessment is the first phase of the nursing process where the nurse collects comprehensive data pertinent to the patient’s health or the situation. In the scenario, the nurse has already gathered data about the client’s respiratory status, indicating that the assessment phase has been completed.
Choice B rationale:
Diagnosis is the phase where the nurse analyzes the assessment data to determine the issues, which in this case is ‘impaired gas exchange.’ This is the phase where the nurse identifies that the client’s symptoms (dyspnea and cyanosis) and elevated respiratory rate are indicative of impaired gas exchange.
Choice C rationale:
Planning is the phase where the nurse develops a plan that prescribes strategies and alternatives to attain expected outcomes. It follows the diagnosis and involves setting priorities, but in the given scenario, the nurse is still at the stage of identifying the problem rather than planning interventions.
Choice D rationale:
Evaluation is the final phase of the nursing process where the nurse assesses the client’s response to the nursing actions and plan’s effectiveness towards achieving the health care goals. Since the nurse is determining the issue, not evaluating the client’s response to interventions, this phase is not the correct answer.
A nurse is caring for a client who has been receiving oxygen via simple face mask for 6 hours. Which of the following assessment findings indicates that oxygen therapy has been effective?
Explanation
The correct answer is choice a. PaO2 80 mmHg.
Choice A rationale:
PaO2 (partial pressure of oxygen in arterial blood) of 80 mmHg indicates that the oxygen therapy has been effective. Normal PaO2 levels range from 75 to 100 mmHg, so a value of 80 mmHg suggests adequate oxygenation.
Choice B rationale:
SaO2 (arterial oxygen saturation) of 88% is below the normal range (typically 95-100%) and indicates hypoxemia, suggesting that the oxygen therapy has not been fully effective.
Choice C rationale:
A respiratory rate (RR) of 32 breaths per minute is significantly higher than the normal range (12-20 breaths per minute) and indicates respiratory distress, suggesting that the oxygen therapy has not been effective.
Choice D rationale:
Blood pressure (BP) of 160/90 mmHg is elevated and indicates hypertension, which is not a direct measure of the effectiveness of oxygen therapy. This finding does not provide information about the patient’s oxygenation status.
Explanation
A humidifier.
Choice A rationale:
A humidifier is necessary to prevent complications in a patient receiving oxygen therapy via a tracheostomy collar. Oxygen delivered through a tracheostomy can dry out the airways and cause discomfort and potential complications. Adding humidity helps maintain airway moisture and prevents drying of the mucous membranes, reducing the risk of mucus plugs and irritation.
Choice B rationale:
A water seal is not necessary for a patient receiving oxygen therapy via a tracheostomy collar. Water seals are used in chest drainage systems to prevent air from entering the pleural space, but they are not relevant in this scenario.
Choice C rationale:
A suction catheter is used to clear secretions from the airway but is not directly related to preventing complications with oxygen therapy via a tracheostomy collar.
Choice D rationale:
A chest tube is not needed for a patient receiving oxygen therapy via a tracheostomy collar. Chest tubes are inserted to drain fluid or air from the pleural space, which is not applicable to this situation.
Explanation
Keep the reservoir bag fully inflated at all times.
Choice A rationale:
In a partial rebreather mask, the reservoir bag should be kept fully inflated at all times to ensure the delivery of the highest possible oxygen concentration during inspiration. The bag collects oxygen during expiration, and the one-way valve prevents the exhaled gases from entering the bag. This way, the patient can inhale a mixture of oxygen from the reservoir and fresh oxygen flow.
Choice B rationale:
Breathing through the mouth and exhaling through the nose is not a necessary instruction for a patient using a partial rebreather mask. It doesn't directly impact the effectiveness of oxygen delivery.
Choice C rationale:
Adjusting the elastic strap to fit snugly around the face is not specific to ensuring effective oxygen delivery. It is a general guideline for mask fitting but doesn't directly affect oxygen administration.
Choice D rationale:
Removing the mask every 15 minutes to check the skin is not necessary and can disrupt the delivery of oxygen therapy. It's essential to maintain a consistent oxygen supply to the patient's lungs, and removing the mask frequently can compromise that. Checking the skin can be done periodically without removing the mask completely.
A nurse is caring for a patient who is receiving oxygen therapy via non-rebreather mask at 15 L/min. The nurse should recognize that this device has which of the following advantages?(Select all that apply)
Explanation

The correct answer is choice a, b, and e.
Choice A rationale:
A non-rebreather mask is designed to deliver a high concentration of oxygen, often deemed the highest among low-flow systems. It achieves this through a reservoir bag that is filled with pure oxygen, which the patient breathes in without the dilution of room air.
Choice B rationale:
This mask has one-way valves that prevent the patient from rebreathing exhaled carbon dioxide. The exhaled air exits through side ports, ensuring that only oxygen from the reservoir is inhaled.
Choice C rationale:
While a non-rebreather mask delivers a high concentration of oxygen, it does not provide a consistent and precise oxygen delivery compared to devices like a Venturi mask, which are designed to deliver a specific and constant oxygen concentration.
Choice D rationale:
The design of a non-rebreather mask does not allow room air to enter through the exhalation ports. The one-way valves are there to ensure that exhaled air does not enter the reservoir bag and that room air does not mix with the oxygen being inhaled.
Choice E rationale:
By delivering a high concentration of oxygen and preventing the rebreathing of exhaled gases, a non-rebreather mask minimizes the risk of carbon dioxide retention, which can be a concern with other oxygen delivery systems that allow for the rebreathing of a portion of exhaled air.
In summary, the non-rebreather mask is advantageous for its ability to deliver a high concentration of oxygen and prevent the rebreathing of exhaled air, which also minimizes the risk of carbon dioxide retention. It is not designed for precise oxygen delivery, nor does it allow the mixing of room air during inhalation.
Explanation
Choice D rationale:
The nurse should connect the nasal cannula to a humidifier first. Dry and irritated nares are common side effects of oxygen therapy via nasal cannula, and using a humidifier adds moisture to the oxygen, reducing irritation and discomfort for the patient.
Choice A rationale:
Applying petroleum jelly to the nares is not the first action to take. It might provide temporary relief, but it is essential to address the root cause of dryness, which is the lack of moisture in the oxygen delivered.
Choice B rationale:
Increasing the flow rate of oxygen is not the first step because it may not address the dryness issue. It can lead to a higher concentration of oxygen, but it won't solve the problem of dry and irritated nares.
Choice C rationale:
Changing the nasal cannula to a face mask is not necessary to address the dryness. Face masks may not be well-tolerated by some patients, and it's better to try less invasive interventions first.
Explanation
Choice A rationale:
The nurse should instruct the patient to avoid smoking or being near open flames while using oxygen. Oxygen supports combustion, and smoking or exposure to flames can lead to a fire hazard.
Choice C rationale:
Checking the position of the oxygen delivery device frequently is important to ensure proper oxygen delivery and avoid any displacement or obstruction that may compromise the therapy's effectiveness.
Choice D rationale:
Instructing the patient to report any signs of hypoxia (low oxygen levels) or hypercarbia (high carbon dioxide levels) to the provider is crucial for early detection of potential complications and appropriate management.
Choice E rationale:
Instructing the patient to adjust the flow rate of oxygen as needed allows them to respond to varying oxygen requirements, especially during activities or changes in their respiratory condition.
Choice B rationale:
Using cotton or wool clothing and bedding is not a recommended instruction for oxygen therapy. Synthetic materials are preferred as they are less likely to catch fire compared to cotton or wool.
Explanation
Choice A rationale:
The nurse should not immediately check the patient's oxygen level with a finger device because the priority is to address the hissing sound from the mask and the patient's pale skin color, which could indicate inadequate oxygen delivery.
Choice B rationale:
Instructing the patient to breathe more deeply and slowly won't address the issue of the hissing sound and the possible oxygen delivery problem. The nurse should address the equipment issue first.
Choice C rationale:
This is the correct choice. The nurse should inform the patient that there is a problem with the mask, and it needs to be fixed promptly to ensure adequate oxygen therapy.
Choice D rationale:
Lowering the flow rate may not be appropriate until the nurse has assessed and resolved the problem with the mask. It's essential to troubleshoot the equipment first.
Explanation
Choice A rationale:
The patient's PaO2 is 65 mmHg and SaO2 is 88%. PaO2 values below 80 mmHg and SaO2 below 90% are considered below normal ranges. Therefore, the patient's oxygen levels are not within the normal range for the condition.
Choice B rationale:
This is the correct choice. The patient's PaO2 and SaO2 levels indicate that they are not receiving enough oxygen, and additional oxygen therapy is needed.
Choice C rationale:
The patient's oxygen levels are low, not high. Providing less oxygen would worsen the situation.
Choice D rationale:
The patient's oxygen levels are affected by oxygen therapy, as they indicate that the current therapy is insufficient. Additional interventions are needed to improve oxygenation.
Explanation
Choice A rationale:
Monitoring the patient's respiratory rate, depth, rhythm, and effort is crucial for assessing the effectiveness of oxygen therapy and ensuring proper oxygenation through the tracheostomy collar.
Choice B rationale:
Educating the patient on how to use and care for the tracheostomy collar is essential to ensure the patient's safety and compliance with the therapy.
Choice C rationale:
Implementing safety measures to prevent fire hazards from the oxygen source is crucial, especially when oxygen is delivered via tracheostomy collar, which may have increased oxygen flow rates.
Choice D rationale:
This is the correct choice. All the provided interventions (monitoring respiratory parameters, patient education, and safety measures) are essential components of the plan of care for a patient with a tracheostomy who requires oxygen therapy.
Explanation
Choice A rationale:
Monitoring the patient's respiratory rate, depth, rhythm, and effort is crucial for assessing the effectiveness of oxygen therapy and ensuring proper oxygenation through the tracheostomy collar.
Choice B rationale:
Educating the patient on how to use and care for the tracheostomy collar is essential to ensure the patient's safety and compliance with the therapy.
Choice C rationale:
Implementing safety measures to prevent fire hazards from the oxygen source is crucial, especially when oxygen is delivered via tracheostomy collar, which may have increased oxygen flow rates.
Choice D rationale:
This is the correct choice. All the provided interventions (monitoring respiratory parameters, patient education, and safety measures) are essential components of the plan of care for a patient with a tracheostomy who requires oxygen therapy.
Sterile suctioning
Explanation
To assess lung sounds.
Choice A rationale:
Sterile suctioning is not performed to administer medications. Its primary purpose is to remove secretions and maintain a patent airway.
Choice B rationale:
Sterile suctioning is not done solely for promoting comfort. Its main goal is to clear the airway and prevent respiratory complications.
Choice C rationale:
The purpose of sterile suctioning is to assess lung sounds by removing excess secretions and mucus that may obstruct the airway. This helps in evaluating the patient's respiratory status and identifying any abnormal lung sounds.
Choice D rationale:
Sterile suctioning is not performed to monitor vital signs. Although vital signs may be monitored during the procedure, it is not the primary purpose of suctioning.
Explanation
Choice A:
Plastic,.
Choice B:
Metal,.
Choice C:
Silicone, and Choice D:
Rubber.
Choice A rationale:
Plastic suctioning catheters are commonly used for sterile suctioning as they are disposable and come in various sizes for different patient needs.
Choice B rationale:
Metal suctioning catheters are also used for sterile suctioning and are often reusable, making them cost-effective for healthcare facilities.
Choice C rationale:
Silicone suctioning catheters are commonly used in sensitive situations or patients with latex allergies, as silicone is a non-allergenic material.
Choice D rationale:
Rubber suctioning catheters were commonly used in the past, but they are less common now due to the availability of more suitable materials like plastic and silicone.
Choice E rationale:
Glass suctioning catheters are not used for sterile suctioning due to the risk of breakage, which can lead to serious injuries and complications.
Explanation
"I have been coughing up blood.”.
Choice A rationale:
Mild nasal congestion may be a common finding in many patients and does not necessarily contraindicate suctioning unless it significantly obstructs the airway.
Choice B rationale:
A sore throat may indicate local irritation, but it does not directly contraindicate suctioning unless there are other underlying complications.
Choice C rationale:
A history of coughing up blood (hemoptysis) suggests an ongoing bleeding disorder. Suctioning could exacerbate the bleeding, leading to further complications. The procedure should be avoided until the cause of hemoptysis is properly assessed and managed.
Choice D rationale:
Feeling lightheaded may be a common sensation during and after suctioning due to the stimulation of the gag reflex, but it does not necessarily contraindicate the procedure. It is essential to ensure adequate oxygenation and provide proper support during the procedure to minimize this discomfort.
Explanation
Choice A rationale:
Epiglottitis is an inflammation of the epiglottis, which is a crucial structure in protecting the airway during swallowing. Suctioning in patients with a history of epiglottitis can be dangerous because it can cause further irritation and swelling of the epiglottis, potentially leading to airway obstruction and respiratory distress. Therefore, sterile suctioning is contraindicated in patients with a history of epiglottitis.
Choice B rationale:
Laryngeal edema refers to swelling of the larynx, which can also compromise the airway. While it is essential to monitor and manage laryngeal edema carefully, it is not an absolute contraindication for sterile suctioning. In some cases, suctioning may be necessary to maintain a patent airway, but it should be performed with caution and by experienced personnel.
Choice C rationale:
Difficulty clearing secretions is a common indication for sterile suctioning. Patients who have difficulty clearing their secretions may need suctioning to prevent the accumulation of mucus and maintain a clear airway. Therefore, this statement does not indicate a contraindication for the procedure.
Choice D rationale:
Using an artificial airway at night, such as a tracheostomy tube, indicates that the patient may require suctioning to maintain airway patency. While having an artificial airway increases the risk of infection and other complications, it is not a contraindication for sterile suctioning if clinically indicated.
Explanation
Choice A rationale:
The most crucial measure to prevent cross-contamination during sterile suctioning is the use of personal protective equipment (PPE). PPE, including gloves, gown, mask, and eye protection, creates a barrier between the healthcare provider and the patient's respiratory secretions, reducing the risk of infection transmission.
Choice B rationale:
Proper disposal of waste materials is important for infection control, but it is not the most critical measure to prevent cross-contamination during sterile suctioning. While proper waste disposal is necessary to reduce the spread of infections, using PPE is more directly related to preventing cross-contamination during the procedure.
Choice C rationale:
Environmental cleaning of the suction device is essential for infection control, but it is not the most important measure to prevent cross-contamination during sterile suctioning. The immediate and direct protection provided by PPE is more effective in reducing the risk of transmission during the procedure.
Choice D rationale:
Performing hand hygiene before and after the procedure is vital for infection control, but it is not the most crucial measure to prevent cross-contamination during sterile suctioning. While hand hygiene is essential for reducing the spread of infections, using PPE provides an additional layer of protection during the procedure.
Explanation
Choice D rationale:
When suctioning patients with an artificial airway, using disposable plastic catheters is preferred to reduce the risk of infection. Disposable catheters are single-use and discarded after each procedure, minimizing the potential for contamination and cross-infection between patients.
Choice A rationale:
Glass suctioning catheters are not preferred because they cannot be effectively sterilized for reuse. Reusable materials carry a higher risk of infection transmission and should be avoided when possible.
Choice B rationale:
Metal suctioning catheters are also not the preferred choice for reducing the risk of infection. Like glass catheters, they can be difficult to clean and sterilize adequately for safe reuse. Using disposable materials, like plastic catheters, is a safer option.
Choice C rationale:
While reusable silicone catheters may be more flexible and gentler on the airway, they are not the preferred choice for infection control. Like other reusable materials, they carry a higher risk of contamination and are not as easily disposed of as disposable plastic catheters.
Explanation
Choice A rationale:
A closed catheter is the most appropriate choice for suctioning a patient with thick secretions. Closed catheters have a two-way valve that allows for continuous suction while minimizing the risk of introducing air into the patient's airway. This design prevents the loss of oxygen and maintains a closed system, reducing the risk of complications such as hypoxia and infection.
Choice B rationale:
Metal catheters are not suitable for suctioning thick secretions. They can be rigid and may cause trauma to the airway, leading to bleeding and discomfort for the patient.
Choice C rationale:
Large French scale catheters are not specifically designed for thick secretions and may not effectively aspirate them. These catheters are typically used for drainage of body cavities or larger organs.
Choice D rationale:
A catheter with a single opening is not ideal for suctioning thick secretions. It may not provide sufficient suctioning power and could lead to ineffective removal of secretions from the patient's airway.
Explanation
Choice A rationale:
Environmental cleaning before suctioning is crucial to maintain a clean and safe environment for the patient. This reduces the risk of introducing additional contaminants during the procedure.
Choice B rationale:
Using a reusable suctioning catheter is not appropriate for infection control measures. Reusable catheters can harbor microorganisms, even after proper cleaning and sterilization, increasing the risk of cross-contamination.
Choice C rationale:
Proper disposal of used catheters into a regular trash bin is not a suitable infection control measure. Used catheters should be disposed of in designated biohazard containers to prevent exposure to potential pathogens.
Choice D rationale:
Hand hygiene before and after the procedure is essential to reduce the transmission of microorganisms to and from the patient.
Choice E rationale:
Wearing gloves and a mask during suctioning helps protect the nurse from exposure to the patient's bodily fluids and potential infectious agents.
Repeat steps 7 to 9 until no more secretions are obtained or until three passes are completed. Do not suction more than three times in a row to prevent complications. Allow at least one minute of rest between each suction pass to prevent fatigue and distress .
Explanation
Choice A rationale:
Donning personal protective equipment (PPE) is the priority action before performing sterile suctioning. This helps prevent the transmission of infection from patient to nurse and vice versa.
Choice B rationale:
Preoxygenating the patient with 100% oxygen is essential before nasopharyngeal suctioning, but the priority action is to ensure the nurse's safety by using PPE.
Choice C rationale:
Obtaining baseline data on vital signs and secretions is an important step, but it can be done after the nurse has ensured their safety with appropriate PPE.
Choice D rationale:
Inserting the catheter into the artificial airway using sterile technique is part of the procedure but should be preceded by wearing proper PPE to maintain a sterile environment.
Explanation
Choice A rationale:
The nurse should not rotate the catheter between the thumb and forefinger during suctioning. This action could cause trauma to the airway.
Choice B rationale:
Limiting each suction pass to no more than 10 seconds is an essential practice during sterile suctioning. Prolonged suctioning can lead to hypoxia and potential complications.
Choice C rationale:
Rinsing the catheter and tubing with saline after each suction pass helps maintain patency and prevent the accumulation of secretions, ensuring effective suctioning during the procedure.
Choice D rationale:
Applying continuous suction while inserting the catheter is not recommended during sterile suctioning. Intermittent suction is preferred for safety and effectiveness.
Choice E rationale:
Providing encouragement and support to the client throughout the procedure is crucial for their comfort and cooperation. Suctioning can be uncomfortable, and the client may need reassurance during the process.
Explanation
Choice A rationale:
(Incorrect) Stating that it's common for oxygen saturation to drop during suctioning is not appropriate because a drop in oxygen saturation is an abnormal response that requires immediate intervention.
Choice B rationale:
(Incorrect) Telling the patient that a drop in oxygen levels is a normal response and will improve soon is incorrect and may lead to delay in addressing the potential respiratory distress.
Choice C rationale:
(Correct) This response is appropriate because the nurse should stop suctioning immediately if the patient's oxygen saturation drops below the normal range and provide supplemental oxygen to maintain adequate oxygenation.
Choice D rationale:
(Incorrect) Advising the patient to take slow deep breaths to increase oxygen levels may not be sufficient to address the oxygen saturation drop, which requires immediate intervention.
Explanation
Choice A rationale:
(Incorrect) Assuring the client that the procedure is entirely safe is not entirely accurate, as suctioning can carry some risks and discomfort.
Choice B rationale:
(Correct) This response acknowledges the client's concern about the suctioning procedure while providing a rationale for its importance, which is to maintain clear airways and prevent complications like airway blockage and respiratory distress.
Choice C rationale:
(Incorrect) Stating that there are no other options to remove secretions may not be true, and it does not address the client's concern effectively.
Choice D rationale:
(Incorrect) Promising to suction quickly may not address the client's worry and might compromise the effectiveness of the procedure, as thorough suctioning is necessary.
Explanation
Choice A rationale:
(Correct) After sterile suctioning, it is essential to reposition the patient to a comfortable and safe position, ensuring proper alignment and support to prevent complications.
Choice B rationale:
(Incorrect) While documentation is crucial, ensuring the patient's safety and comfort should be the immediate priority after the procedure.
Choice C rationale:
(Incorrect) The nurse should not remove the catheter and tubing from the artificial airway immediately after suctioning, as it may still be needed for subsequent interventions.
Choice D rationale:
(Incorrect) Assessing the patient's response to suctioning is essential, but ensuring safety and repositioning take precedence immediately after the procedure.
A nurse is preparing to perform sterile suctioning on a patient. What should the nurse do before suctioning?
Explanation
Choice A rationale:
The nurse should indeed provide reassurance and answer any questions before performing any procedure, as this helps to alleviate the patient's anxiety and ensure they are well-informed about the procedure.
Choice B rationale:
Gathering the necessary equipment and supplies is essential before starting sterile suctioning. This ensures that the nurse has everything needed for the procedure, promoting efficiency and safety.
Choice C rationale:
Connecting the suction tubing to the suction device is an important step in the suctioning process, but it should be done after gathering all the necessary equipment and supplies.
Choice D rationale:
Preoxygenating the patient with 100% oxygen is not a step required before suctioning. Preoxygenation may be necessary before some procedures, but it is not specifically indicated for sterile suctioning.
During sterile suctioning, the nurse observes the patient experiencing bronchospasm and increased intracranial pressure. What should be the nurse's immediate action?
Explanation
Choice A rationale:
Continuing suctioning when the patient is experiencing bronchospasm and increased intracranial pressure can worsen their condition and potentially lead to further complications. It is not appropriate to continue suctioning in this situation.
Choice B rationale:
Adjusting the pressure on the suction device may not be sufficient to address the patient's current condition. Stopping suctioning and providing appropriate interventions are more crucial in this situation.
Choice C rationale:
Stopping suctioning immediately is the most appropriate action when the patient experiences bronchospasm and increased intracranial pressure. The nurse should assess the patient's airway, administer bronchodilators or other prescribed treatments as needed, and seek medical assistance if necessary.
Choice D rationale:
Increasing the suction pass time is not recommended as it can exacerbate the patient's condition and lead to complications. The focus should be on stopping suctioning and providing appropriate interventions.
A client is undergoing sterile suctioning. Which interventions should the nurse implement to prevent complications? Select all that apply.
Explanation
Choice A rationale:
Rinsing the catheter and tubing with saline after each suction pass is not a standard practice and is not necessary for sterile suctioning.
Choice B rationale:
Inserting the catheter into the artificial airway using sterile technique is crucial to maintain the integrity of the procedure and prevent infections.
Choice C rationale:
Limiting each suction pass to no more than 10 seconds helps to prevent complications such as hypoxia and tissue damage.
Choice D rationale:
Providing oral or nasal care after suctioning helps maintain the patient's airway, promote comfort, and prevent infections.
Choice E rationale:
Applying continuous suction while withdrawing the catheter is not recommended as it can cause trauma to the airway and should be avoided during sterile suctioning.
A nurse is preparing to perform sterile suctioning for a patient with an endotracheal tube (ETT). What should the nurse do before suctioning?
Explanation
Choice D rationale:
Before performing sterile suctioning on a patient with an endotracheal tube (ETT), the nurse should preoxygenate the patient with 100% oxygen. Suctioning can temporarily decrease oxygen levels in the airway, and preoxygenation helps prevent hypoxia during the procedure.
Choice A rationale:
Checking the patient's blood pressure is not directly related to the preparation for sterile suctioning. However, the nurse should monitor vital signs during and after the procedure.
Choice B rationale:
Placing the patient in the supine position is not a specific requirement for sterile suctioning. The nurse should position the patient appropriately for the procedure to ensure optimal access to the airway.
Choice C rationale:
Inserting the catheter without resistance is not a recommended action. The nurse should assess the patient's airway and ensure proper placement of the suctioning catheter to avoid causing injury or damage.
(Select all that apply): A client requires sterile suctioning through a tracheostomy tube (TT). What steps should the nurse follow during the suctioning procedure? Select all that apply.
Explanation
Choice A rationale:
The nurse should limit each suction pass to no more than 10 seconds to minimize the risk of tissue damage and hypoxia. Prolonged suctioning can cause trauma to the mucosa and lead to inadequate oxygenation.
Choice B rationale:
The nurse should apply suction while inserting the catheter to prevent the catheter from touching the airway walls before suction is initiated. This helps avoid stimulating the gag reflex and causing discomfort to the client.
Choice C rationale:
Rotating the catheter between the thumb and forefinger helps to facilitate even suctioning and prevent the catheter from adhering to the airway walls. It allows for effective removal of secretions without causing harm to the delicate tissues.
Choice D rationale:
After each suction pass, the nurse should rinse the catheter and tubing with saline to maintain its patency and prevent the buildup of secretions. This practice ensures that subsequent suctions are effective in clearing the airway.
Choice E rationale:
Suctioning more than three times in a row is not recommended because it can lead to hypoxia and tissue trauma. Frequent suctioning can reduce the oxygen levels in the airway and cause damage to the delicate tissues.
A nurse is about to perform sterile suctioning and asks the patient if they are ready. The patient responds, "I am feeling very anxious about this.” What would be the appropriate response from the nurse?
Explanation
Choice C rationale:
The nurse should acknowledge the patient's anxiety and respond empathetically. Assuring the patient that the nurse will explain each step during the procedure can help alleviate anxiety. This approach promotes trust and helps the patient feel more in control, which is important for patient cooperation during the suctioning procedure.
Choice A rationale:
Telling the patient not to worry and that it won't take long may come across as dismissive and not address the patient's concerns adequately.
Choice B rationale:
Offering to postpone the procedure is an option, but the nurse should first attempt to address the patient's anxiety and provide reassurance. If the anxiety persists despite the explanation, postponing the procedure can be considered.
Choice D rationale:
Dismissing the patient's anxiety by stating that suctioning is routine may not effectively address the patient's feelings and may not be comforting.
A client has a nasopharyngeal tube (NPT) for oxygenation. During the suctioning procedure, the patient says, "I'm experiencing discomfort in my nose.” How should the nurse respond?
Explanation
Choice D rationale:
The nurse should respond by acknowledging the discomfort and pausing the procedure to reposition the nasopharyngeal tube. Repositioning can help alleviate the discomfort while ensuring the oxygenation needs are still met.
Choice A rationale:
Increasing the suction pressure may exacerbate the discomfort and cause further irritation to the nose and airway.
Choice B rationale:
Instructing the client to breathe through the mouth may not adequately address the discomfort and may not be feasible if the oxygenation is dependent on the nasopharyngeal tube.
Choice C rationale:
Although explaining the necessity of suctioning is important, it does not directly address the client's immediate discomfort. The priority is to address the client's comfort and safety during the procedure.
A nurse has completed sterile suctioning for a patient with an endotracheal tube (ETT). What should the nurse do next?
Explanation
Choice A rationale:
The nurse should not discard the used catheter and gloves into a regular trash bin because they were used in a sterile procedure, and improper disposal could lead to the risk of contamination and infection for both the patient and others.
Choice B rationale:
Although it is important to assess the patient's response to suctioning, including vital signs, this should not be the immediate next step after completing sterile suctioning. First, the nurse should ensure their own and the patient's safety by following proper infection control measures.
Choice C rationale:
After completing sterile suctioning, the nurse should perform hand hygiene to prevent the spread of infection and then don a new pair of sterile gloves before performing any other tasks or assessments. This step ensures that the nurse maintains a sterile field and minimizes the risk of introducing pathogens into the patient's airway.
Choice D rationale:
Increasing the suction pressure for one last pass is not necessary and may cause harm to the patient's airway. Proper suctioning technique involves limiting the suctioning time and pressure to avoid tissue damage and potential complications.
A nurse is performing tracheostomy care for a patient with a tracheostomy tube (TT). Which action should the nurse include in the procedure?
Explanation
Choice A rationale:
Cleaning the inner cannula once a week is insufficient to maintain proper hygiene for a patient with a tracheostomy tube. The inner cannula should be cleaned more frequently, as directed by the healthcare provider, to prevent the accumulation of secretions and potential respiratory complications.
Choice B rationale:
Deflating the cuff before cleaning the tracheostomy tube is not recommended because it may lead to aspiration of secretions or loss of the airway seal. The cuff should only be deflated when it is necessary to remove or change the tracheostomy tube.
Choice C rationale:
Using cotton-tipped applicators to clean the stoma is not the recommended method for tracheostomy care. Sterile tracheostomy care kits usually include specialized brushes or swabs designed for this purpose, ensuring effective and safe cleaning of the stoma without the risk of shedding fibers or causing injury.
Choice D rationale:
Changing the tracheostomy ties every 24 hours is the appropriate action. Regular changing of the ties helps prevent complications such as skin breakdown, ensures a secure fit of the tracheostomy tube, and reduces the risk of infection.
When suctioning a patient with an endotracheal tube (ETT), the nurse should limit the suctioning time to:
Explanation
Choice A rationale:
Limiting the suctioning time to 15 seconds may still be too long for some patients, increasing the risk of hypoxia and other complications related to prolonged suctioning. The optimal suctioning time should be shorter to minimize adverse effects.
Choice B rationale:
Limiting the suctioning time to 20 seconds is longer than the recommended duration. Prolonged suctioning can cause hypoxia, increased intracranial pressure, and other adverse effects, making it crucial to keep the time as short as possible.
Choice C rationale:
Suctioning time should generally be limited to 10 seconds to reduce the risk of complications while effectively clearing the patient's airway. This duration allows for adequate removal of secretions without causing significant disturbances to the patient's oxygenation and hemodynamic stability.
Choice D rationale:
Limiting the suctioning time to 5 seconds is too short to effectively clear secretions from the airway, especially in patients with excessive or tenacious secretions. Sufficient time is needed to ensure proper removal of respiratory secretions and maintain the patient's airway patency.
(Select all that apply): A nurse is preparing to perform nasopharyngeal suctioning for a patient with a nasopharyngeal tube (NPT). What actions should the nurse take during the procedure? Select all that apply.
Explanation
Choice A rationale:
The nurse should not insert the catheter until resistance is met during nasopharyngeal suctioning. This action could cause trauma to the nasal mucosa or other structures in the nasopharynx.
Choice B rationale:
Preoxygenating the patient with 100% oxygen is important before nasopharyngeal suctioning to prevent hypoxia during the procedure. Suctioning can temporarily decrease oxygen levels, so preoxygenation helps maintain adequate oxygenation.
Choice C rationale:
Applying intermittent suction while inserting the catheter is not recommended during nasopharyngeal suctioning. Continuous suction is preferred for effective removal of secretions.
Choice D rationale:
Limiting each suction pass to no more than 15 seconds is an essential practice during nasopharyngeal suctioning. Prolonged suctioning can cause hypoxia and discomfort for the patient.
Choice E rationale:
Rinsing the catheter and tubing with saline after each suction pass helps maintain patency and prevent the accumulation of secretions, ensuring effective suctioning during the procedure.
Tracheostomy care
Explanation
Choice A rationale:
A cuffed tracheostomy tube is most suitable for a patient who requires mechanical ventilation or has a high risk of aspiration. The cuff is inflated to create a seal between the trachea and the tube, preventing aspiration of oral secretions or gastric contents into the airway. This is crucial for patients on mechanical ventilation to ensure effective ventilation and prevent complications like ventilator-associated pneumonia.
Choice B rationale:
Uncuffed tracheostomy tubes do not have an inflatable cuff, making them unsuitable for patients who require mechanical ventilation or have a high risk of aspiration. They are more appropriate for patients who can protect their own airway and have minimal risk of aspiration.
Choice C rationale:
Fenestrated tracheostomy tubes have an opening or fenestration on the tube that allows airflow through the upper airway, bypassing the tracheostomy tube. These tubes are used for patients who are weaning off mechanical ventilation and require speech therapy. They are not the most suitable choice for patients who need mechanical ventilation or have a high aspiration risk.
Choice D rationale:
Double-lumen tracheostomy tubes have two separate tubes, which can be used for independent lung ventilation in certain situations. They are not specifically designed for patients requiring mechanical ventilation or with a high risk of aspiration.
Choice E rationale:
Metal tracheostomy tubes are not commonly used for patients requiring mechanical ventilation or with a high risk of aspiration. Metal tubes may be used in certain cases, but they are not the most suitable choice for this patient population.
Explanation
Choice C rationale:
A fenestrated tracheostomy tube would be the most appropriate choice for a client who is ready to wean from mechanical ventilation and also requires speech therapy. The fenestration in the tube allows the patient to breathe through the upper airway, facilitating the weaning process, and enabling speech by allowing air to pass over the vocal cords. This type of tube is commonly used for patients who have progressed in their recovery and are transitioning to breathing independently.
Choice A rationale:
A cuffed tracheostomy tube with an inflated cuff is more suitable for patients requiring mechanical ventilation or those at high risk of aspiration, rather than a patient who is ready to wean from ventilation.
Choice B rationale:
Uncuffed tracheostomy tubes may be appropriate for patients who can protect their airway and are weaning from mechanical ventilation. However, they would not be the most appropriate choice when speech therapy is also required.
Choice D rationale:
Double-lumen tracheostomy tubes are not typically used for weaning from mechanical ventilation or speech therapy needs. They are employed in specialized situations for independent lung ventilation.
Choice E rationale:
Plastic tracheostomy tubes are commonly used in clinical practice and may be suitable for a patient ready to wean from mechanical ventilation and requiring speech therapy. However, the fenestrated tube is a more specific choice for this scenario.
Explanation
Choice D rationale:
This statement is correct. A fenestrated tracheostomy tube is designed for patients with a low risk of aspiration and are weaning from mechanical ventilation. The fenestration allows the patient to breathe through the upper airway, promoting speech and facilitating the weaning process. The fenestration can be temporarily occluded to assess the patient's readiness for decannulation.
Choice A rationale:
Monitoring cuff pressure is essential, but the suggested range of 20 to 25 cm H2O is not universally applicable. The appropriate cuff pressure range may vary depending on the patient's condition, and it should be individualized based on the patient's needs.
Choice B rationale:
Keeping the fenestration open at all times is not accurate. The fenestration can be open to allow airflow during weaning and speech therapy, but it can be temporarily occluded when assessing the patient's ability to breathe without the tube.
Choice C rationale:
The inner cannula is not solely used during mechanical ventilation. It is also used for routine cleaning and maintenance of the tracheostomy tube, regardless of the patient's ventilation status.
Choice E rationale:
Metal tracheostomy tubes are not commonly used for long-term ventilation. They are mostly used in specific situations where a plastic tube may not be suitable, such as when there is a risk of tube distortion or damage. Plastic tubes are more commonly used for long-term ventilation due to their availability, flexibility, and ease of use.
Explanation
Choice A rationale:
A cuffed tracheostomy tube has an inflatable cuff that can create a seal in the trachea, but it also increases the risk of aspiration. In this case, the patient is at low risk of aspiration, so a cuffed tube is not the most suitable choice.
Choice B rationale:
An uncuffed tracheostomy tube lacks an inflatable cuff, which reduces the risk of aspiration. It allows air to flow freely around the tube and is appropriate for patients with a low risk of aspiration, making it the most suitable choice for this patient.
Choice C rationale:
A fenestrated tracheostomy tube has an opening in the posterior wall that allows airflow through the vocal cords, facilitating speech. However, since the patient is already speaking with a low risk of aspiration, a fenestrated tube may not be necessary or the best choice.
Choice D rationale:
A double-lumen tracheostomy tube is designed for independent lung ventilation during certain medical procedures and is not typically used for routine tracheostomy management. It would not be the most suitable choice in this scenario.
Choice E rationale:
Silicone tracheostomy tubes are made of a soft, flexible material that can reduce the risk of tissue damage and provide greater comfort. However, the material of the tracheostomy tube is not the primary consideration for a patient with a low risk of aspiration.
Explanation
Choice A rationale:
Performing tracheostomy care every 2 to 4 hours would be too frequent for most patients and may cause unnecessary disruption and discomfort. This interval is not the recommended standard of care.
Choice B rationale:
Tracheostomy care every 4 to 6 hours strikes a balance between maintaining airway hygiene and minimizing excessive handling of the tracheostomy site, reducing the risk of complications such as infection or irritation.
Choice C rationale:
Waiting to perform tracheostomy care every 6 to 8 hours may increase the risk of mucus buildup and potential complications, especially in patients with high secretions or respiratory issues.
Choice D rationale:
Extending the interval to every 8 to 12 hours may lead to inadequate airway clearance and increased risk of complications in patients who require more frequent care.
Choice E rationale:
Waiting to perform tracheostomy care every 12 to 24 hours is too infrequent for most patients and may not be sufficient to maintain a patent airway and prevent complications.
Explanation
Choice A rationale:
Administering antibiotics would be indicated if the patient develops a respiratory infection, but it would not directly address the issue of dry and crusted secretions.
Choice B rationale:
Increasing suction frequency may help remove secretions, but it may also lead to increased irritation and trauma to the tracheal lining. It is not the first-line intervention for dry and crusted secretions.
Choice C rationale:
Providing humidification and hydration helps to moisten the secretions, making them easier to expectorate or suction. It is the most appropriate intervention to address dry and crusted secretions in a patient with a tracheostomy tube.
Choice D rationale:
Performing daily tracheostomy tube changes is not indicated solely to address dry and crusted secretions unless there is a specific problem with the current tube that requires changing.
Choice E rationale:
Recommending a fenestrated tracheostomy tube would not directly address the issue of dry and crusted secretions. Fenestrated tubes are more relevant for patients who need speech assistance, which is not the primary concern in this case.
Explanation
Choice A rationale:
Positioning the patient in semi-Fowler's position (Choice A) is an important step in tracheostomy care, but it is not the first step during the suctioning procedure. Semi-Fowler's position helps promote lung expansion and allows for better visualization during the procedure.
Choice B rationale:
Applying a new dressing around the stoma (Choice B) is essential after suctioning to maintain cleanliness and prevent infection. However, it is not the first step in the suctioning procedure. The nurse should first gather the necessary equipment.
Choice C rationale:
Cleaning the inner cannula with hydrogen peroxide (Choice C) is not the first step during suctioning. The nurse should gather equipment and supplies first before performing any cleaning or other procedures.
Choice E rationale:
Removing the old dressing and discarding it in a moisture-resistant bag (Choice E) is an important step, but it should come after the nurse gathers the necessary equipment for the suctioning procedure.
Explanation
Choice A rationale:
Cleaning the stoma with hydrogen peroxide (Choice A) is not recommended for tracheostomy care. Hydrogen peroxide can be irritating and damaging to the tissues. Normal saline solution should be used to clean the stoma.
Choice B rationale:
Changing the ties or straps every 4 hours (Choice B) is not necessary unless they are soiled or loose. Frequent changes may irritate the skin and increase the risk of infection. Straps should be changed only when needed.
Choice C rationale:
Inspecting the stoma for signs of infection (Choice C) is a crucial step in tracheostomy care. Signs of infection may include redness, swelling, discharge, or foul odor. Prompt identification and treatment of infection are essential to prevent complications.
Choice E rationale:
Applying a new dressing around the stoma and securing it with tape (Choice E) is essential after tracheostomy care to maintain cleanliness and protect the stoma. Proper dressing helps prevent infection and skin breakdown.
Suctioning a tracheostomy tube is a sterile, invasive technique that requires a nurse or a respiratory therapist. It is done to remove secretions from the tube and prevent obstruction, infection, or hypoxia. The steps of suctioning a tracheostomy tube are:
A nurse is preparing to suction a tracheostomy tube for a patient. What position should the nurse place the patient in?
Explanation
Choice A rationale:
Placing the patient in a prone position (Choice A) would not be suitable for suctioning a tracheostomy tube as it may impede breathing and proper access to the tracheostomy site.
Choice B rationale:
Placing the patient in a supine position (Choice B) is not the optimal position for tracheostomy suctioning. Semi-Fowler's position is preferred as it allows better lung expansion and facilitates the suctioning procedure.
Choice D rationale:
Placing the patient in Trendelenburg position (Choice D) is not appropriate for tracheostomy suctioning. Trendelenburg position is typically used for certain cardiovascular conditions and not for tracheostomy care.
(Select all that apply). A nurse is gathering equipment for suctioning a tracheostomy tube. Which of the following items should the nurse include in the setup?
Explanation
Choice A rationale:
Sterile gloves are essential for aseptic technique during tracheostomy suctioning to prevent the introduction of infection. However, they are not included in the setup, as they are worn by the nurse performing the procedure.
Choice B rationale:
Sterile water or saline is necessary for suctioning to moisten the suction catheter and facilitate the removal of secretions without causing trauma to the airway. Therefore, it should be included in the setup.
Choice C rationale:
A pulse oximeter is used to monitor the patient's oxygen saturation and is not directly related to tracheostomy suctioning. While continuous monitoring of oxygen saturation is essential during and after the procedure, it is not a part of the setup.
Choice D rationale:
A sphygmomanometer is used to measure blood pressure and is unrelated to tracheostomy suctioning. It is not required for this procedure.
Choice E rationale:
A non-sterile towel is used to protect the patient's clothing and bed linens from any secretions or spills during the suctioning procedure. It should be included in the setup to maintain cleanliness and prevent contamination.
A nurse is about to insert the suction catheter into the patient's tracheostomy tube. The patient says, "I'm feeling anxious about this.”What would be the nurse's appropriate response?
Explanation
Choice A rationale:
This response is dismissive of the patient's feelings and may increase their anxiety. It does not address the patient's concern appropriately.
Choice B rationale:
This response acknowledges the patient's anxiety and provides a clear explanation for the necessity of the procedure. It is empathetic and supportive while also emphasizing the importance of the intervention.
Choice C rationale:
This response is not entirely reassuring and may not be accurate. Simply asking the patient to trust the nurse without explaining the procedure further may not alleviate the patient's anxiety.
Choice D rationale:
Skipping the procedure without a valid reason may compromise the patient's airway and respiratory function. Postponing essential procedures is not appropriate unless there are specific clinical reasons for doing so.
Explanation
Choice A rationale:
This response acknowledges the patient's concern and provides a realistic expectation of potential discomfort during the procedure. It offers reassurance that any pain experienced will be brief.
Choice B rationale:
This response is not entirely accurate. While the procedure itself may not cause pain, some patients may experience discomfort during tracheostomy suctioning due to the sensation of suction in the airway.
Choice C rationale:
This response is not appropriate as it exaggerates the potential pain, causing unnecessary distress to the patient.
Choice D rationale:
Administering pain medication solely for the discomfort associated with tracheostomy suctioning is not standard practice. Pain medication should only be given for clinically significant pain or as part of a larger pain management plan.
Explanation
Choice A rationale:
Waiting for at least 10 seconds between each suctioning attempt may not provide sufficient time for the patient's oxygenation to stabilize. This short duration might not allow the patient's oxygen levels to return to an adequate baseline, leading to potential hypoxia during subsequent suctioning attempts.
Choice B rationale:
Waiting for at least 30 seconds between suctioning attempts allows more time for the patient's oxygen levels to recover. This duration strikes a balance between preventing hypoxia and removing secretions effectively. It also helps minimize the risk of complications associated with frequent or rapid suctioning.
Choice C rationale:
Waiting for at least 1 minute between suctioning attempts might be too long, especially if the patient is experiencing respiratory distress or has excessive secretions. Delaying suctioning for this duration could lead to an accumulation of secretions, potentially compromising the airway and causing distress for the patient.
Choice D rationale:
Waiting for at least 3 minutes between suctioning attempts is too long and not clinically appropriate. This extended time may lead to increased secretion buildup and potential airway obstruction, especially in patients with excessive secretions or those who are critically ill.
Explanation
Choice A rationale:
Proceeding with the suctioning as planned when signs of infection are present around the tracheostomy stoma can be detrimental to the patient's health. Suctioning in the presence of infection can exacerbate the infection, spread bacteria, and lead to more serious complications.
Choice B rationale:
Reporting the findings of infection to the healthcare provider is the correct action. The healthcare provider needs to assess the infection and determine the appropriate course of action, such as prescribing antibiotics or adjusting the suctioning regimen to prevent further complications.
Choice C rationale:
Cleaning the area with hydrogen peroxide before suctioning is not recommended. Hydrogen peroxide can be harsh on the skin, and using it around the stoma may cause irritation and delay healing. Moreover, cleaning the area without addressing the infection itself does not address the underlying issue.
Choice D rationale:
Using an antiseptic solution to cleanse the stoma is not the appropriate action in the presence of infection. Antiseptic solutions are designed to prevent infections, not treat existing ones. Using an antiseptic could further irritate the area and delay proper treatment for the infection.
Explanation
Choice A rationale:
A neonate with a tracheostomy tube would require lower suction pressure compared to an adult. Neonates have smaller and more delicate airways, making them more susceptible to damage from high suction pressures. Using lower suction pressures is essential to ensure the safety and well-being of the neonate.
Choice B rationale:
An adult with a tracheostomy tube may require higher suction pressure compared to other age groups. Adults generally have larger airways and more significant secretion production. Adequate suction pressure is necessary to effectively remove secretions and maintain airway patency.
Choice C rationale:
A child with a tracheostomy tube would typically require lower suction pressure than an adult. Children have smaller airways than adults, and using high suction pressures could cause harm and discomfort.
Choice D rationale:
An infant with a tracheostomy tube would require lower suction pressure compared to an adult. Infants have smaller airways and are more sensitive to changes in pressure. Using higher suction pressure could cause trauma to the delicate tissues in their airways.
(Select all that apply). A nurse is suctioning a tracheostomy tube for a patient. Which of the following actions are correct during the suctioning process?
Explanation
Choice A rationale:
Applying continuous suction while inserting the catheter can cause trauma to the tracheal mucosa and increase the risk of bleeding and infection.
Choice B rationale:
Rinsing the catheter with sterile saline between each suctioning attempt helps maintain aseptic technique, preventing the introduction of microorganisms into the airway.
Choice C rationale:
Limiting suctioning attempts to three per session reduces the risk of hypoxia and mucosal damage, ensuring adequate oxygenation and preventing complications.
Choice D rationale:
Withdrawing the catheter gently while applying suction prevents damage to the tracheal walls and minimizes the risk of bleeding.
Choice E rationale:
Hyperoxygenating the patient before and after suctioning helps prevent hypoxemia during the procedure, reducing the risk of complications and ensuring adequate oxygenation.
Explanation
Choice A rationale:
While notifying the healthcare provider is essential, the priority action in this situation is to stop the bleeding to prevent further complications.
Choice B rationale:
Applying direct pressure to the tracheostomy stoma is the first action the nurse should take to control the bleeding and stabilize the patient.
Choice C rationale:
Administering fluids and blood products may be necessary later, but it is not the first action to take when dealing with active bleeding.
Choice D rationale:
Ensuring proper positioning and alignment of the tracheostomy tube is important, but it is not the priority in this critical situation.
Explanation
Choice A rationale:
Maintaining proper cuff pressure prevents pressure-related injuries and potential tracheoesophageal fistula (TEF) formation.
Choice B rationale:
Progressing to a deflated cuff or cuffless tube reduces the risk of TEF by minimizing pressure on the tracheal tissues.
Choice C rationale:
Tracheal dilation or surgical intervention may be necessary if TEF has already developed but is not a preventive measure.
Choice D rationale:
Using a small soft feeding tube instead of a nasogastric tube for tube feedings reduces the risk of trauma to the tracheal tissues and lowers the risk of TEF formation.
Choice E rationale:
Administering oxygen by mask may be necessary for oxygenation, but it is not specifically related to preventing tracheoesophageal fistula formation.
Explanation
Choice A rationale:
This choice is not appropriate because increased coughing, difficulty breathing, and stridor suggest a mechanical issue rather than an infection. Monitoring for fever or increased secretions is not addressing the potential cause of the symptoms.
Choice B rationale:
This choice is not appropriate for the presented situation. Expectorating secretions may not directly address the narrowed tracheal lumen due to scar formation, and it is not the primary intervention needed.
Choice C rationale:
This is the correct choice. Ensuring the tracheostomy tube is securely positioned in the midline can help prevent further narrowing of the tracheal lumen. Proper alignment and securing of the tube can optimize airflow and reduce complications related to scar formation.
Choice D rationale:
Using a larger tracheostomy tube may not be the most appropriate action in this situation. Enlarging the tube may not be necessary and could potentially cause other complications. It's better to ensure proper positioning and consider other interventions before resorting to a larger tube.
Explanation
Choice A rationale:
This statement is correct. The client should inform the nurse if they notice any food particles in their tracheal secretions as it could indicate aspiration and require immediate attention.
Choice B rationale:
This statement indicates a need for further education. A larger tracheostomy tube to prevent an air leak at the stoma is not an appropriate intervention for tracheomalacia. Tracheomalacia is the weakening of the tracheal cartilage, and a larger tube would not address this underlying issue.
Choice C rationale:
This statement is also incorrect. Minimizing the time the cuff is inflated may be beneficial to prevent tracheal stenosis but would not prevent tracheomalacia, which is a different condition altogether.
Choice D rationale:
This statement is correct. Monitoring cuff pressure and air volumes closely is essential to prevent complications and ensure appropriate cuff inflation.
A nurse is educating a patient with a tracheostomy on communication methods. Which information should the nurse include?
Explanation
Choice A rationale:
This choice is not the most relevant information for the patient with a tracheostomy regarding communication methods. Effective oral communication with the tube in place may be challenging, and other options should be explored.
Choice B rationale:
While electronic devices can be helpful for communication, they may not be the most practical option for a patient with a tracheostomy, especially during emergencies when devices may not be readily available.
Choice C rationale:
This choice is somewhat relevant but not the most appropriate. While written communication is an option, it may not be the primary method used with a tracheostomy.
Choice D rationale:
This is the correct choice. Teaching the patient how to use speaking valves to facilitate speech with the tracheostomy tube in place can significantly improve communication. Speaking valves allow airflow during inhalation and redirect exhaled air through the vocal cords, enabling speech while maintaining a closed respiratory system during exhalation. This is a valuable communication method for patients with tracheostomies.
Chest tubes
Explanation
Choice A rationale:
Increased insulin production is not the primary cause of elevated blood sugar levels and excessive thirst in a client with diabetes. In fact, in type 1 diabetes, there is a lack of insulin production, while in type 2 diabetes, there is insulin resistance, both leading to inadequate cellular uptake of glucose.
Choice B rationale:
Decreased glucose production by the liver is also not the primary cause of the symptoms. In diabetes, the liver can overproduce glucose, especially in the fasting state, contributing to hyperglycemia.
Choice C rationale:
Inadequate cellular uptake of glucose is the correct choice. In diabetes, the body's cells do not effectively utilize glucose due to either insufficient insulin or insulin resistance, leading to high blood sugar levels in the blood.
Choice D rationale:
Overproduction of glucagon by the pancreas is not the primary cause of elevated blood sugar levels and excessive thirst. Glucagon, a hormone produced by the pancreas, raises blood sugar levels when necessary, but it is not the main culprit in diabetes.
Explanation
Choice A rationale:
Whole grains are generally recommended for individuals with diabetes as they provide a steady source of energy and contain fiber, which can help manage blood sugar levels.
Choice B rationale:
Fruits should be limited because they contain natural sugars, which can raise blood sugar levels. While fruits are a healthy choice, it's essential for people with diabetes to monitor their intake and choose lower-sugar options.
Choice C rationale:
Green leafy vegetables are generally encouraged for individuals with diabetes as they are low in calories and carbohydrates and have a positive impact on blood sugar levels.
Choice D rationale:
Saturated fats should be limited because they can contribute to insulin resistance and increase the risk of heart disease, which is already elevated in people with diabetes.
Choice E rationale:
Lean protein is a good choice for individuals with diabetes as it can help stabilize blood sugar levels and promote satiety without contributing to significant fluctuations in glucose.
Explanation
Choice A rationale:
Walking barefoot at home is not advisable for a client with diabetes. It can increase the risk of injury and foot complications, as individuals with diabetes may have reduced sensation in their feet, making it difficult to detect injuries promptly.
Choice B rationale:
"Inspect your feet daily, especially between the toes.”. This is the correct choice. Daily foot inspection is crucial for early detection of any signs of injury, infection, or changes in the skin. Early intervention can prevent more severe foot complications in individuals with diabetes.
Choice C rationale:
Applying heating pads to the feet for warmth in cold weather is not recommended for individuals with diabetes, as they may have reduced sensitivity to temperature changes and can accidentally burn their feet.
Choice D rationale:
Using adhesive tape to treat blisters or sores on the feet is not advised. Any wounds or foot issues should be assessed and treated by a healthcare professional to prevent infection and promote proper healing.
Explanation
Choice A rationale:
The client's statement, "I haven't been eating much lately,”. supports the suspicion of hypoglycemia. When a person with diabetes does not eat enough, especially if they are taking insulin or certain oral medications, their blood sugar levels can drop, leading to hypoglycemia. The symptoms reported by the client, including feeling shaky, weak, and dizzy, are typical manifestations of low blood sugar.
Choice B rationale:
"I've been drinking a lot of water recently”. does not support the suspicion of hypoglycemia. This statement could indicate hyperglycemia instead, as excessive thirst (polydipsia) is a common symptom of high blood sugar in diabetes.
Choice C rationale:
"I feel tired and lethargic all the time”. is a non-specific symptom and does not directly indicate hypoglycemia. Fatigue can be caused by various factors, and in this case, there is no clear link to low blood sugar.
Choice D rationale:
"My heart has been racing throughout the day”. is also not indicative of hypoglycemia. Rapid heart rate (tachycardia) can have multiple underlying causes, and it is not a primary symptom of low blood sugar.
Explanation
Choice B rationale:
The nurse should prioritize monitoring the client's blood glucose levels before administering insulin. It is essential to know the client's current blood sugar level to determine the appropriate dose of insulin to administer safely. Giving insulin without knowing the current blood glucose level can lead to hypoglycemia or hyperglycemia, both of which can be dangerous for the client.
Choice A rationale:
Assessing the client's blood pressure is important but not the priority before administering insulin. High or low blood pressure can be a concern in clients with diabetes, but checking blood glucose levels takes precedence when preparing to administer insulin.
Choice C rationale:
Asking the client about any allergies is a good practice before administering any medication, but it is not the priority in this situation. The immediate concern is to address the hyperglycemia with insulin while ensuring the client's safety.
Choice D rationale:
Checking the client's oxygen saturation is not directly related to insulin administration for diabetes. It may be relevant in certain medical conditions or emergencies, but it is not a priority action before giving insulin.
Explanation
Choice D rationale:
The nurse should administer regular insulin IV using an intravenous bolus injection in this scenario. When a client with diabetes is admitted to the hospital with hyperglycemia and requires immediate correction of blood sugar levels, intravenous insulin bolus is the most appropriate technique. Intravenous administration allows for rapid action and precise control over insulin dosing.
Choice A rationale:
Intramuscular injection is not the recommended route for insulin administration in this situation. It is a slower route, and the absorption may not be predictable, which could delay the desired effect of lowering blood glucose levels.
Choice B rationale:
Subcutaneous injection is the standard method for most routine insulin administration in clients with diabetes. However, in the case of hyperglycemia requiring rapid correction, intravenous bolus injection is preferred for faster action.
Choice C rationale:
Intradermal injection is not appropriate for insulin administration. This route is typically used for skin testing or allergen sensitivity assessments, not for delivering insulin.
Choice E rationale:
While an intravenous infusion pump can be used for insulin administration in some situations, it is not the best choice for rapidly correcting hyperglycemia. Intravenous bolus injection provides a more immediate and precise response. Infusion pumps are more commonly used for continuous insulin infusions, such as in critical care settings.
Explanation
Choice A rationale:
Increasing carbohydrate intake may lead to increased blood glucose levels, which is not recommended for a client experiencing frequent hypoglycemic episodes.
Choice B rationale:
Skipping meals when not hungry can lead to erratic blood glucose levels and may worsen the client's hypoglycemic episodes.
Choice C rationale:
Delaying insulin administration is not a safe strategy, as it can result in uncontrolled hyperglycemia and further complications.
Choice D rationale:
Engaging in intense physical activity can lower blood glucose levels, potentially exacerbating the hypoglycemic episodes.
Choice E rationale:
Monitoring blood glucose levels more frequently is essential for clients with diabetes experiencing hypoglycemic episodes. By regularly checking blood glucose levels, the client and healthcare team can identify trends and adjust insulin or medication dosages appropriately, helping to prevent future hypoglycemic episodes.
Explanation
Choice A rationale:
Obtaining cultures from the chest tube site before insertion is not a standard nursing action during chest tube preparation. Cultures are usually taken if there is an infection or concern after the insertion.
Choice B rationale:
Applying a pressure dressing to the wound site after chest tube insertion is not a recommended practice. Airtight dressing can lead to tension pneumothorax. Instead, a sterile occlusive dressing is typically applied.
Choice C rationale:
Administering antibiotics to the patient before the procedure is not a standard nursing action during chest tube preparation. Antibiotics are usually prescribed if there is an infection after the insertion.
Choice D rationale:
Monitoring vital signs and pain level after chest tube insertion is essential to assess the patient's response to the procedure and to identify any complications, such as pneumothorax, bleeding, or infection.
Choice E rationale:
Instructing the patient to take deep breaths during the insertion is not appropriate because chest tube insertion is a sterile procedure, and patients are usually not conscious during the process. The insertion site is anesthetized, and deep breaths could compromise sterile technique and increase the risk of infection.
Explanation
Choice A rationale:
Keeping the drainage system above the chest level is incorrect because the drainage system should be placed below the chest level to facilitate proper drainage of fluids and air.
Choice B rationale:
Clamping the tubing for an extended period to prevent leaks is incorrect. Chest tubes should never be clamped for an extended period as it can lead to a dangerous buildup of pressure within the pleural space and impair proper drainage.
Choice C rationale:
Ensuring adequate and stable water levels in the water-seal and suction-control chambers is correct. Maintaining appropriate water levels is essential for maintaining the proper functioning of the chest tube system, ensuring that it can effectively remove air and fluid from the pleural space.
Choice D rationale:
Milking or stripping the tubing regularly to enhance drainage is incorrect. This practice is outdated and can cause damage to the chest tube, leading to potential complications. The tubing should not be manipulated in this manner.
Choice E rationale:
Keeping the tubing free of kinks, loops, or dependent areas is correct. Any kinks, loops, or dependent areas can obstruct the flow of fluids and air within the chest tube system, impairing its functionality.
Explanation
Choice A rationale:
Stating that continuous bubbling in the water-seal chamber is a normal finding and does not require any intervention is incorrect. Continuous bubbling indicates an air leak, and it requires prompt evaluation and intervention.
Choice B rationale:
Clamping the tubing to see if the bubbling stops is incorrect. Clamping the tubing would only be done to assess if the air leak is from the patient or the system, but it does not address the underlying issue.
Choice C rationale:
Applying an occlusive dressing to seal the wound site is incorrect. While dressing changes may be necessary to maintain a sterile environment, it will not resolve the air leak causing continuous bubbling.
Choice D rationale:
Notifying the physician immediately about the air leak is the appropriate nursing action. Continuous bubbling in the water-seal chamber suggests an air leak, which could compromise the effectiveness of the chest tube and require immediate medical attention.
Explanation
Choice A rationale:
Administering diuretics to reduce fluid accumulation is incorrect. Severe dyspnea, absent breath sounds, and jugular venous distension indicate a potential tension pneumothorax or hemothorax, which requires prompt action, and diuretics would not address the underlying issue.
Choice B rationale:
Preparing for needle decompression or chest tube insertion is the appropriate nursing action. The client's symptoms of severe dyspnea, absent breath sounds, jugular venous distension, and increased intrathoracic pressure suggest a possible tension pneumothorax or hemothorax. Immediate decompression with a large-bore needle or insertion of a chest tube is necessary to relieve pressure and restore lung function.
Choice C rationale:
Positioning the client in a Trendelenburg position to facilitate breathing is incorrect. In the case of increased intrathoracic pressure, this position can further compromise respiratory function and is not recommended.
Choice D rationale:
Instructing the client to take slow, deep breaths to prevent further complications is incorrect. The client's condition requires urgent medical intervention, and slow, deep breaths would not address the acute issue of increased intrathoracic pressure and compromised lung function.
Explanation
Choice A rationale:
The nurse should instruct the patient and their family to keep the drainage system below the chest level at all times. This positioning helps ensure proper drainage of fluid or air from the chest, preventing any backflow or obstruction in the system. Gravity assists in maintaining the drainage flow, promoting the effectiveness of the chest tube.
Choice B rationale:
Deep breathing and coughing exercises are essential while the chest tube is in place. These exercises help prevent complications such as atelectasis and pneumonia by promoting lung expansion and clearing secretions. The patient should be encouraged to perform these exercises as directed by the healthcare provider.
Choice C rationale:
The nurse should educate the patient and their family to notify the physician immediately if they observe any subcutaneous emphysema around the chest tube site. Subcutaneous emphysema is a potential complication of chest tube placement, indicating air leakage into the tissues. Prompt notification allows for timely intervention to prevent further complications.
Choice D rationale:
The nurse should inform the patient that the drainage color may change from serosanguineous (pale, pink, or slightly bloody) to bright red during the recovery process. Initially, the drainage may be bloody, but as healing progresses, it should become clearer. However, if the drainage suddenly becomes bright red, it could indicate active bleeding, and the healthcare provider should be notified immediately.
Explanation
Choice A rationale:
Applying a pressure dressing to the wound site is not the priority intervention for a chest tube with signs of infection. The primary concern is to address the infection and prevent its spread.
Choice B rationale:
The nurse should prioritize obtaining cultures from the chest tube site to identify the causative organism responsible for the infection. This information will guide the selection of appropriate antibiotics to treat the infection effectively.
Choice C rationale:
Administering oxygen to improve ventilation may be beneficial for some patients, but it does not address the underlying infection. Oxygen therapy can support respiratory function but is not the priority intervention in this situation.
Choice D rationale:
Monitoring vital signs and oxygen saturation is essential but does not address the infection directly. Vital sign monitoring is ongoing, while obtaining cultures is a specific intervention targeted at the suspected infection.
Explanation
Choice A rationale:
The nurse should suspect tension pneumothorax in the patient with a chest tube who shows sudden decreased drainage, pink frothy sputum, and crackles on auscultation. Tension pneumothorax is a life-threatening condition where air accumulates in the pleural space, leading to increased pressure on the affected lung and heart. Immediate intervention, such as chest tube insertion on the affected side, is crucial to relieve the pressure and improve ventilation.
Choice B rationale:
Subcutaneous emphysema does not present with decreased drainage or pink frothy sputum. It is characterized by air trapped under the skin, causing a crackling sensation on palpation. Monitoring respiratory status and elevating the head of the bed are appropriate interventions for subcutaneous emphysema but not in this scenario.
Choice C rationale:
Re-expansion pulmonary edema is a rare complication that occurs after rapid lung re-expansion. It does not typically manifest with pink frothy sputum and crackles. Administering diuretics may be appropriate, but it is not the primary intervention in this situation.
Choice D rationale:
Infection does not explain the sudden decrease in drainage and pink frothy sputum. Although obtaining cultures from the chest tube site is important to assess for infection, it is not the most appropriate intervention at this moment. The priority is to address the potential tension pneumothorax.
A nurse is preparing to remove a chest tube from a patient. Which of the following actions should the nurse take during the removal procedure? Select all that apply:
Explanation
Choice A rationale: Physician’s order and informed consent are required because chest tube removal is an invasive procedure; legal and ethical standards ensure patient safety and autonomy in care decisions.
Choice B rationale: The patient should perform the Valsalva maneuver or hold breath during removal to prevent air entry; forceful exhalation increases risk of pneumothorax, making this incorrect.
Choice C rationale: Monitoring respiratory status and vital signs after removal detects complications such as pneumothorax, hypoxia, or bleeding, ensuring prompt intervention and patient safety following the procedure.
Choice D rationale: Applying an occlusive dressing with petroleum gauze seals the wound, preventing air entry into the pleural space and reducing risk of recurrent pneumothorax after chest tube removal.
Exams on Medico-Surgical Procedures
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
Notes Highlighting is available once you sign in. Login Here.
Oxygen therapy
Types of Oxygen Delivery Devices
- Oxygen delivery devices are classified into low-flow and high-flow systems, depending on whether they provide a fixed or variable amount of oxygen to the patient.
- Low-flow systems deliver a variable amount of oxygen that depends on the patient’s breathing pattern and rate. They include a nasal cannula, simple face mask, partial rebreather mask, and non-rebreather mask.
- High-flow systems deliver a fixed amount of oxygen that is independent of the patient’s breathing pattern and rate. They include a venturi mask, aerosol mask, face tent, tracheostomy collar, T-piece, and mechanical ventilator.
- The table below summarizes the characteristics, advantages, disadvantages, and nursing implications of each type of oxygen delivery device.
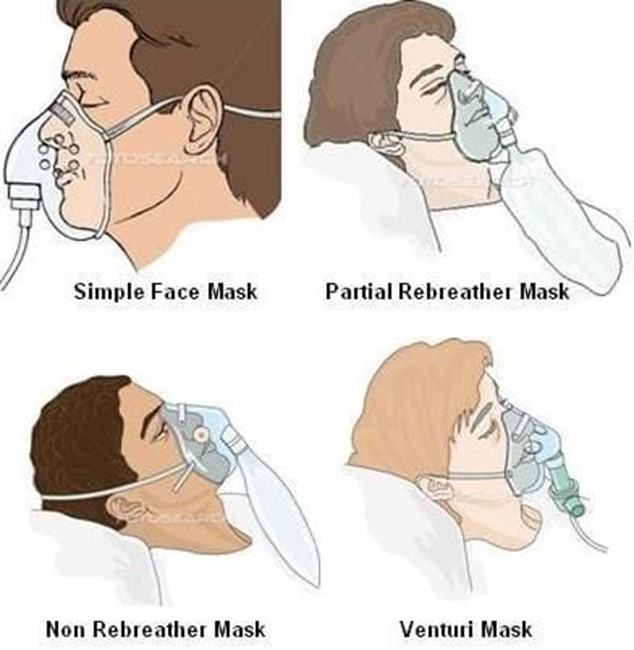
|
Device
|
FiO2 range
|
Flow rate
|
Characteristics
|
Advantages
|
Disadvantages
|
Nursing implications |
|
Nasal cannula
|
24%-44%
|
1-6 L/min
|
A plastic tubing with two prongs that fit into the nostrils.
|
Comfortable, easy to apply, well-tolerated by most patients.
|
Can cause nasal dryness, irritation, or bleeding. Can be dislodged by movement or mouth breathing. FiO2 can vary with breathing pattern.
|
Assess nares for patency and skin integrity. Humidify oxygen if flow rate is higher than 4 L/min. Ensure proper fit and secure tubing. Monitor for signs of hypoxia or hypercarbia. |
|
Simple face mask
|
40%-60%
|
5-8 L/min
|
A plastic mask that covers the nose and mouth. Has holes on the sides to allow exhaled air to escape.
|
Easy to apply and remove. Provides higher FiO2 than nasal cannula. Humidifies oxygen.
|
Can cause skin irritation, pressure ulcers, or claustrophobia. Can interfere with eating, drinking, or talking. FiO2 can vary with breathing pattern. Risk of aspiration if vomiting occurs.
|
Assess skin integrity and comfort. Ensure proper fit and secure straps. Monitor for signs of hypoxia or hypercarbia. Provide oral care every 2-4 hours. Remove mask for eating or drinking. |
|
Partial rebreather mask
|
60%-75%
|
6-11 L/min
|
A plastic mask that covers the nose and mouth. Has a reservoir bag attached to store oxygen-enriched air. Has holes on the sides to allow some exhaled air to escape and some to be rebreathed.
|
Provides higher FiO2 than simple face mask. Allows conservation of oxygen by rebreathing some exhaled air. Humidifies oxygen.
|
Same as simple face mask plus risk of suffocation if bag deflates or collapses. FiO2 can vary with breathing pattern and bag inflation. Requires close monitoring.
|
Same as simple face mask plus ensure bag remains inflated during inspiration and expiration. Adjust flow rate to prevent bag collapse. Monitor for signs of hypoxia or hypercarbia. |
|
Non-rebreather mask
|
80%-95%
|
10-15 L/min
|
A plastic mask that covers the nose and mouth. Has a reservoir bag attached to store 100% oxygen. Has one-way valves on the mask and bag to prevent exhaled air from entering the bag or being rebreathed. Has holes on the sides to allow exhaled air to escape completely.
|
Provides highest FiO2 among low-flow systems. Prevents rebreathing of exhaled air and carbon dioxide. Humidifies oxygen.
|
Same as partial rebreather mask plus risk of carbon dioxide retention if valves malfunction. Requires close monitoring.
|
Same as partial rebreather mask plus ensure valves are patent and functional. Monitor for signs of hypoxia or hypercarbia. |
|
Venturi mask
|
24%-50%
|
4-12 L/min
|
A plastic mask that covers the nose and mouth. Has a cone-shaped adapter (venturi) attached to the oxygen source. Has holes on the sides to allow room air to mix with oxygen. The FiO2 is determined by the size and color of the adapter.
|
Provides precise and consistent FiO2 regardless of breathing pattern. Allows control of oxygen concentration and humidity.
|
Can cause skin irritation, pressure ulcers, or claustrophobia. Can interfere with eating, drinking, or talking. Risk of aspiration if vomiting occurs. Requires careful monitoring and maintenance.
|
Assess skin integrity and comfort. Ensure proper fit and secure straps. Monitor for signs of hypoxia or hypercarbia. Provide oral care every 2-4 hours. Remove mask for eating or drinking. Check adapter size and color and flow rate according to prescription. Ensure adequate water level in humidifier. |
|
Aerosol mask
|
24%-100%
|
8-15 L/min
|
A plastic mask that covers the nose and mouth or the entire face. Has a large-bore tubing connected to an aerosol generator that produces a mist of oxygen and water particles. The FiO2 is determined by the flow rate and the amount of mist generated.
|
Provides high FiO2 and humidity for patients with thick secretions, dry mucous membranes, or upper airway edema. Can be used for patients who cannot tolerate masks or nasal cannula.
|
Can cause skin irritation, pressure ulcers, or claustrophobia. Can interfere with eating, drinking, or talking. Risk of aspiration if vomiting occurs. Requires careful monitoring and maintenance. Can be noisy and messy.
|
Same as venturi mask plus ensure adequate water level in aerosol generator. Check tubing for condensation and drainage. Monitor for signs of infection or fluid overload. |
|
Face tent
|
24%-100%
|
8-15 L/min
|
A soft plastic cone that fits loosely around the face and neck. Has a large-bore tubing connected to an aerosol generator that produces a mist of oxygen and water particles. The FiO2 is determined by the flow rate and the amount of mist generated.
|
Same as aerosol mask plus more comfortable and less confining than masks.
|
Same as aerosol mask plus less precise and consistent FiO2 than masks.
|
Same as aerosol mask plus ensure proper fit and secure straps. |
|
Device
|
FiO2
|
Flow rate
|
Description
|
Advantages
|
Disadvantages
|
Nursing considerations |
|
Tracheostomy collar
|
24%-100%
|
8-15 L/min
|
A plastic collar that fits around the neck and covers the tracheostomy opening. Has a large-bore tubing connected to an aerosol generator that produces a mist of oxygen and water particles. The FiO2 is determined by the flow rate and the amount of mist generated.
|
Same as aerosol mask plus provides direct oxygen delivery to the trachea. Can be used for patients who have a tracheostomy or laryngectomy.
|
Same as aerosol mask plus risk of infection, bleeding, or obstruction of the tracheostomy site. Requires careful monitoring and maintenance. Can be noisy and messy.
|
Same as aerosol mask plus assess tracheostomy site for patency, cleanliness, and signs of infection. Provide tracheostomy care every 8 hours or as needed. Suction secretions as needed. Monitor for signs of hypoxia or hypercarbia. |
|
T-piece
|
24%-100%
|
8-15 L/min
|
A plastic adapter that connects to the end of a tracheostomy tube, endotracheal tube, or laryngectomy tube. Has a large-bore tubing connected to an aerosol generator that produces a mist of oxygen and water particles. The FiO2 is determined by the flow rate and the amount of mist generated.
|
Same as tracheostomy collar plus allows the patient to breathe room air when disconnected from the oxygen source. Can be used for patients who are being weaned from mechanical ventilation or have intermittent suctioning needs.
|
Same as tracheostomy collar plus risk of accidental disconnection or loss of oxygen supply. Requires careful monitoring and maintenance. Can be noisy and messy.
|
Same as tracheostomy collar plus ensure proper fit and secure connection. Monitor for signs of hypoxia or hypercarbia. Disconnect from oxygen source only when ordered or indicated. |
|
Mechanical ventilator
|
21%-100%
|
Variable
|
A machine that delivers oxygen and air to the lungs through a tracheostomy tube or an endotracheal tube. The FiO2, tidal volume, respiratory rate, inspiratory pressure, positive end-expiratory pressure (PEEP), and other parameters are set by the health care provider according to the patient’s condition and needs.
|
Provides precise and consistent FiO2 and ventilation for patients who cannot breathe adequately on their own. Allows control of oxygen concentration, humidity, temperature, and pressure. Can provide various modes of ventilation, such as assist-control, synchronized intermittent mandatory ventilation (SIMV), pressure support ventilation (PSV), etc.
|
Can cause complications such as barotrauma, volutrauma, atelectrauma, ventilator-associated pneumonia (VAP), ventilator-induced lung injury (VILI), etc. Requires invasive intubation or tracheostomy and sedation or paralysis for some patients. Requires careful monitoring and maintenance by trained personnel. Can be noisy and complex.
|
Assess respiratory status and ventilator settings frequently. Monitor ABG results and pulse oximetry readings. Ensure proper placement and securement of the artificial airway. Provide oral care every 2-4 hours or as needed. Suction secretions as needed. Prevent accidental extubation or disconnection. Monitor for signs of infection, bleeding, or obstruction of the artificial airway. Monitor for signs of hypoxia, hypercarbia, or ventilator complications. |
Nursing Interventions for Patients Receiving Oxygen Therapy
- Assess the patient’s need for oxygen therapy based on their history, physical examination, vital signs, ABG results, pulse oximetry readings, and clinical manifestations.
- Obtain a prescription for oxygen therapy that specifies the type of device, FiO2 or flow rate, duration, frequency, and indications for changing or discontinuing the therapy.
- Explain the purpose, benefits, risks, and procedure of oxygen therapy to the patient and their family members.
- Select the appropriate oxygen delivery device according to the prescription and the patient’s condition, preference, comfort, and tolerance.
- Apply the device correctly and securely to ensure adequate oxygen delivery and prevent dislodgement or leakage.
- Adjust the flow meter to deliver the prescribed FiO2 or flow rate.
- Connect the device to a humidifier if indicated to prevent mucosal dryness and irritation.
- Monitor the patient’s response to oxygen therapy by observing their respiratory rate, depth, rhythm, effort, breath sounds, skin color, level of consciousness, mental status, etc.
- Evaluate the effectiveness of oxygen therapy by measuring their PaO2 or SaO2 using ABG analysis or pulse oximetry.
- Document the type of device, FiO2 or flow rate, duration, frequency, response, effectiveness, complications, and education provided for oxygen therapy.
- Educate the patient and their family members on how to use and care for the oxygen delivery device, how to recognize and report signs of hypoxia or hypercarbia, how to prevent complications, and when to seek medical attention.
- Implement safety measures to prevent fire hazards, such as avoiding smoking, open flames, sparks, or flammable materials near the oxygen source, using cotton or wool clothing and bedding, and grounding electrical equipment.
Complications of Oxygen Therapy
- Oxygen toxicity: A condition caused by exposure to high concentrations of oxygen for prolonged periods of time. It can damage the lungs and other organs by producing free radicals that injure the cells. Signs and symptoms include dyspnea, cough, chest pain, substernal discomfort, crackles, decreased lung compliance, pulmonary edema, and respiratory failure.
- Carbon dioxide retention: A condition caused by increased levels of carbon dioxide in the blood due to hypoventilation or impaired gas exchange. It can occur in patients with chronic obstructive pulmonary disease (COPD) who rely on hypoxic drive to stimulate breathing. High concentrations of oxygen can suppress this drive and reduce the respiratory rate and depth. Signs and symptoms include headache, confusion, drowsiness, coma, and respiratory acidosis.
- Absorption atelectasis: A condition caused by the collapse of the alveoli due to nitrogen washout. Nitrogen is normally present in the alveoli and helps maintain their patency. High concentrations of oxygen can displace nitrogen and reduce the alveolar volume. Signs and symptoms include dyspnea, hypoxemia, decreased breath sounds, and increased respiratory rate.
- Fire hazard: A condition caused by ignition of oxygen-enriched air or materials near the oxygen source. Oxygen supports combustion and can cause rapid and intense burning. Sources of ignition include smoking, open flames, sparks, or flammable materials. Signs and symptoms include smoke, flames, heat, burns, and injuries.
Conclusion
- Oxygen therapy is a common and important intervention for patients with hypoxemia or hypoxia.
- Oxygen therapy requires careful assessment, prescription, application, monitoring, evaluation, documentation, education, and safety measures.
- Oxygen therapy can cause complications such as oxygen toxicity, carbon dioxide retention, absorption atelectasis, and fire hazard.
Summary
- Oxygen therapy is the administration of supplemental oxygen to increase the amount of oxygen available to the tissues and organs.
- Oxygen therapy is prescribed when the patient’s oxygen needs cannot be met by atmospheric or room air alone.
- The goal of oxygen therapy is to use the lowest fraction of inspired oxygen (FiO2) to achieve an acceptable blood oxygen level without causing harmful side effects.
- The effectiveness of oxygen therapy is evaluated by measuring the partial pressure of arterial oxygen (PaO2) or the arterial oxygen saturation (SaO2) using arterial blood gas (ABG) analysis or pulse oximetry.
- Oxygen delivery devices are classified into low-flow and high-flow systems. Low-flow systems deliver a variable amount of oxygen that depends on the patient’s breathing pattern and rate. High-flow systems deliver a fixed amount of oxygen that is independent of the patient’s breathing pattern and rate.
- The types of oxygen delivery devices include a nasal cannula, simple face mask, partial rebreather mask, non-rebreather mask, venturi mask, aerosol mask, face tent, tracheostomy collar, T-piece, and mechanical ventilator. Each device has its own characteristics, advantages, disadvantages, and nursing implications.
- Nursing interventions for patients receiving oxygen therapy include assessing the need for oxygen therapy; obtaining a prescription for oxygen therapy; explaining the purpose, benefits, risks, and procedure of oxygen therapy; selecting the appropriate device; applying the device correctly and securely; adjusting the flow meter; connecting the device to a humidifier if indicated; monitoring the response to oxygen therapy; evaluating the effectiveness of oxygen therapy; documenting the oxygen therapy; educating the patient and family members on how to use and care for the device; recognizing and reporting signs of hypoxia or hypercarbia; preventing complications; and seeking medical attention; implementing safety measures to prevent fire hazards.
- Complications of oxygen therapy include oxygen toxicity, carbon dioxide retention, absorption atelectasis, and fire hazard.
Sterile suctioning
- Sterile suctioning is a procedure that involves applying negative pressure to remove secretions from the airway of a patient who has an artificial airway or impaired cough reflex.
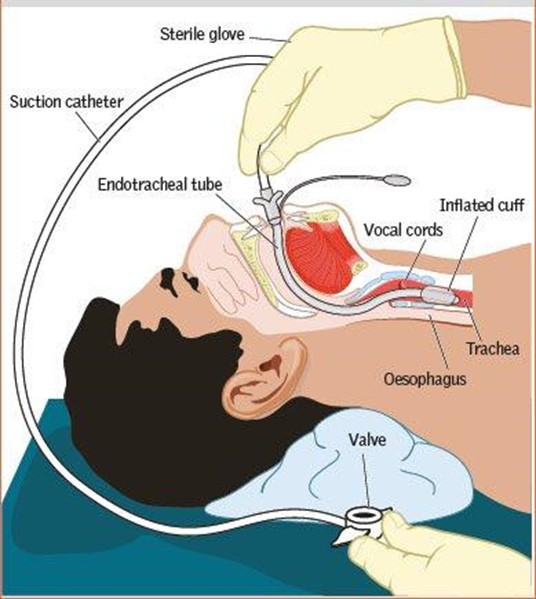
- The purpose of sterile suctioning is to maintain airway patency, prevent infection, improve gas exchange, and promote comfort.
- Sterile suctioning is indicated for patients who have excessive or thick secretions that obstruct the airway, or who are unable to clear their own secretions due to decreased level of consciousness, neuromuscular weakness, or respiratory distress.
- Sterile suctioning is contraindicated for patients who have bleeding disorders, nasal or oral trauma, epiglottitis, croup, or laryngeal edema.
- Sterile suctioning can cause complications such as hypoxia, hypotension, bradycardia, arrhythmias, bleeding, infection, mucosal damage, bronchospasm, atelectasis, and increased intracranial pressure.
Types of Suctioning Devices and Catheters
- Suctioning devices are machines that generate negative pressure to aspirate secretions from the airway. They can be wall-mounted or portable.
- Suctioning devices have a collection container for secretions, a pressure gauge to adjust the level of suction, a tubing system to connect the device to the catheter, and a control valve to regulate the suction.
- Suctioning catheters are flexible tubes that are inserted into the airway through the artificial airway or the nose or mouth. They have a tip with one or more openings to collect secretions, and a vent that allows intermittent suction by covering and releasing it with the thumb.
- Suctioning catheters come in different sizes and materials. The size is measured by the French scale (Fr), which indicates the external diameter of the catheter. The appropriate size of the catheter depends on the type and size of the artificial airway. Generally, the catheter should not exceed half of the internal diameter of the artificial airway.
- Suctioning catheters can be made of plastic, rubber, or silicone. They can be disposable or reusable. Disposable catheters are preferred for infection control purposes. Reusable catheters should be cleaned and sterilized after each use.
- Suctioning catheters can be open or closed. Open catheters are single-use catheters that are attached to the suction tubing directly. Closed catheters are multi-use catheters that are enclosed in a plastic sleeve that connects to the suction tubing. Closed catheters reduce the risk of infection and contamination, but they are more expensive than open catheters.
Principles of Infection Control and Aseptic Technique in Sterile Suctioning
- Sterile suctioning is an invasive procedure that can introduce microorganisms into the lower respiratory tract and cause infection. Therefore, infection control measures are essential to prevent nosocomial pneumonia and other complications.
- Infection control measures include hand hygiene, personal protective equipment (PPE), sterile equipment and supplies, proper disposal of waste materials, and environmental cleaning.
- Hand hygiene is the most important measure to prevent cross-contamination. It involves washing hands with soap and water or using alcohol-based hand rub before and after contact with the patient or any potentially contaminated items.
- PPE consists of gloves, gown, mask, eye protection, and hair cover. It protects the health care worker from exposure to bloodborne pathogens and other infectious agents. It also prevents transmission of microorganisms from the health care worker to the patient or vice versa.
- Sterile equipment and supplies include suction device, tubing system, collection container, catheter, saline solution, gloves, and sterile drape. They should be opened and handled using aseptic technique, which involves avoiding contact with any non-sterile surfaces or items.
- Proper disposal of waste materials involves discarding used catheters, gloves, and other contaminated items into appropriate biohazard bags or containers. The collection container should be emptied and cleaned after each use or when it is full.
- Environmental cleaning involves wiping the suction device, tubing system, and other surfaces with disinfectant solution after each use or at least once a day. The suction device should be checked for proper functioning and maintenance regularly.
Steps of Performing Sterile Suctioning for Different Types of Artificial Airways
- The steps of performing sterile suctioning vary depending on the type of artificial airway that the patient has. The most common types of artificial airways are endotracheal tube (ETT), tracheostomy tube (TT), and nasopharyngeal tube (NPT).
- Endotracheal tube (ETT) is a plastic tube that is inserted through the mouth or nose into the trachea to provide mechanical ventilation or oxygenation. It is secured with tape or a cuff that is inflated to seal the airway.
- Tracheostomy tube (TT) is a metal or plastic tube that is inserted through a surgical opening in the neck into the trachea to bypass the upper airway obstruction or facilitate long-term ventilation. It can have an inner cannula that can be removed for cleaning and a cuff that can be inflated or deflated depending on the patient’s condition.
- Nasopharyngeal tube (NPT) is a soft rubber or plastic tube that is inserted through the nose into the pharynx to provide oxygenation or humidification. It is used for patients who have difficulty breathing through the mouth or who need frequent suctioning.
- The general steps of performing sterile suctioning for any type of artificial airway are as follows:
- Assess the patient’s need for suctioning by observing for signs and symptoms of airway obstruction, such as increased respiratory rate, decreased oxygen saturation, adventitious breath sounds, restlessness, agitation, cyanosis, or coughing.
- Check the prescriber’s order for suctioning, including the frequency, duration, pressure, and type of catheter.
- Gather the equipment and supplies needed for suctioning, such as suction device, tubing system, collection container, catheter, saline solution, gloves, sterile drape, PPE, oxygen source, and stethoscope.
- Explain the procedure to the patient and obtain consent if possible. Provide privacy and ensure comfort. Position the patient in semi-Fowler’s or Fowler’s position to facilitate breathing and drainage.
- Perform hand hygiene and don PPE. Open the sterile equipment and supplies using aseptic technique. Connect the suction tubing to the suction device and adjust the pressure according to the prescriber’s order. Test the suction by occluding the vent with the thumb.
- Preoxygenate the patient with 100% oxygen for 30 seconds to 3 minutes before suctioning to prevent hypoxia. Monitor the patient’s vital signs and oxygen saturation during this step.
- Insert the catheter into the artificial airway using sterile technique. For ETT and TT, insert the catheter until resistance is met or until the patient coughs. For NPT, insert the catheter until it reaches the pharynx. Do not apply suction while inserting the catheter.
- Apply intermittent suction by placing and releasing the thumb over the vent while withdrawing the catheter slowly. Rotate the catheter between the thumb and forefinger to remove secretions from all sides of the airway. Limit each suction pass to no more than 10 seconds to prevent hypoxia and mucosal damage.
- Rinse the catheter and tubing with saline solution or water after each suction pass to clear secretions and prevent infection. Reoxygenate the patient with 100% oxygen for 30 seconds to 3 minutes after each suction pass to restore oxygenation.
- Repeat steps 7 to 9 until no more secretions are obtained or until three passes are completed. Do not suction more than three times in a row to prevent complications. Allow at least one minute of rest between each suction pass to prevent fatigue and distress.
- Remove the catheter and tubing from the artificial airway and disconnect them from the suction device. Discard the used catheter and gloves into a biohazard bag or container. Clean the collection container and tubing with disinfectant solution. Turn off the suction device.
- Assess the patient’s response to suctioning by monitoring vital signs, oxygen saturation, breath sounds, secretions, and comfort level. Provide oral or nasal care as needed. Reposition the patient and ensure safety .
- Perform hand hygiene and remove PPE. Dispose of waste materials according to facility policy. Clean the environment and equipment as needed .
- Document the procedure and findings, including the date, time, type, size, and frequency of suctioning, the amount, color, consistency, and odor of secretions, the patient’s tolerance and response, any complications or interventions, and any teaching or evaluation done.
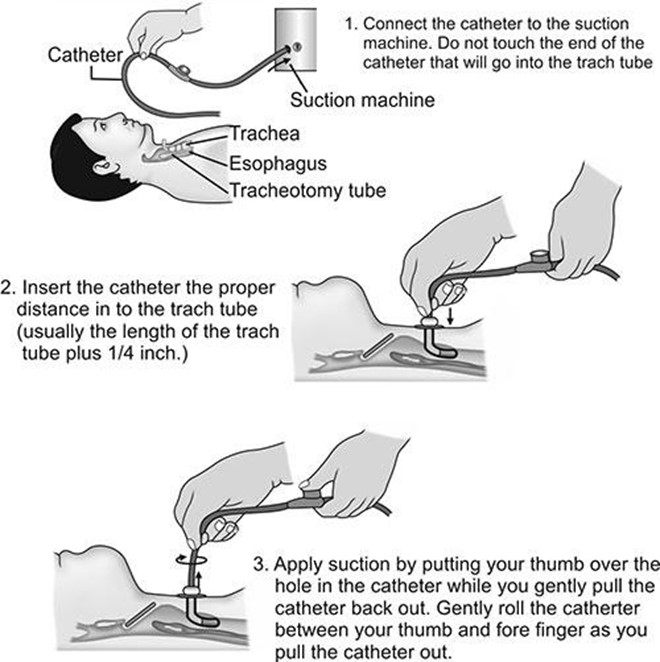
Nursing Interventions and Assessments Before, During, and After Sterile Suctioning
- Nursing interventions and assessments before, during, and after sterile suctioning are aimed at ensuring patient safety, comfort, and optimal outcomes. They include the following :
- Before suctioning:
- Obtain baseline data on vital signs, oxygen saturation, breath sounds, secretions, and comfort level.
- Verify the prescriber’s order for suctioning and check for any contraindications or precautions.
- Explain the procedure to the patient and provide reassurance. Answer any questions or concerns.
- Gather the necessary equipment and supplies and check their expiration dates and functionality.
- Perform hand hygiene and don PPE. Prepare a sterile field and open the sterile equipment and supplies using aseptic technique.
- Connect the suction tubing to the suction device and adjust the pressure according to the prescriber’s order. Test the suction by occluding the vent with the thumb.
- Preoxygenate the patient with 100% oxygen for 30 seconds to 3 minutes before suctioning to prevent hypoxia.
- During suctioning:
- Insert the catheter into the artificial airway using sterile technique. Do not apply suction while inserting the catheter.
- Apply intermittent suction by placing and releasing the thumb over the vent while withdrawing the catheter slowly. Rotate the catheter between the thumb and forefinger to remove secretions from all sides of the airway. Limit each suction pass to no more than 10 seconds to prevent hypoxia and mucosal damage.
- Rinse the catheter and tubing with saline solution or water after each suction pass to clear secretions and prevent infection. Reoxygenate the patient with 100% oxygen for 30 seconds to 3 minutes after each suction pass to restore oxygenation.
- Observe the patient’s vital signs, oxygen saturation, breath sounds, secretions, comfort level, and tolerance during suctioning. Watch for any signs of complications or adverse reactions, such as hypoxia, hypotension, bradycardia, arrhythmias, bleeding, infection, mucosal damage, bronchospasm, atelectasis, or increased intracranial pressure. Stop suctioning immediately if any of these occur and provide appropriate interventions.
- Communicate with the patient throughout suctioning and provide encouragement and support.
- After suctioning:
- Remove the catheter and tubing from the artificial airway and disconnect them from the suction device. Discard the used catheter and gloves into a biohazard bag or container. Clean the collection container and tubing with disinfectant solution. Turn off the suction device.
- Assess the patient’s response to suctioning by monitoring vital signs, oxygen saturation, breath sounds, secretions, and comfort level. Provide oral or nasal care as needed. Reposition the patient and ensure safety.
- Perform hand hygiene and remove PPE. Dispose of waste materials according to facility policy. Clean the environment and equipment as needed.
- Document the procedure and findings, including the date, time, type, size, and frequency of suctioning, the amount, color, consistency, and odor of secretions, the patient’s tolerance and response, any complications or interventions, and any teaching or evaluation done.
Outcomes and Effectiveness of Sterile Suctioning
- The outcomes and effectiveness of sterile suctioning are evaluated by comparing the patient’s condition before and after suctioning, and by monitoring for any changes or improvements in the following indicators :
- Airway patency: The airway should be clear of secretions and obstruction after suctioning. The patient should have normal or improved breath sounds, respiratory rate, oxygen saturation, and chest expansion.
- Infection prevention: The patient should have no signs or symptoms of infection after suctioning, such as fever, chills, purulent or foul-smelling secretions, increased white blood cell count, or positive culture results.
- Gas exchange: The patient should have adequate oxygenation and ventilation after suctioning. The patient should have normal or improved arterial blood gas values, such as pH, PaO2, PaCO2, HCO3, and SaO2.
- Comfort: The patient should have minimal or no pain or discomfort after suctioning. The patient should have normal or decreased anxiety, agitation, restlessness, or dyspnea.
- Complications: The patient should have no complications or adverse reactions after suctioning, such as hypoxia, hypotension, bradycardia, arrhythmias, bleeding, infection, mucosal damage, bronchospasm, atelectasis, or increased intracranial pressure.
Conclusion
- Sterile suctioning is a medico-surgical procedure that involves applying negative pressure to remove secretions from the airway of a patient who has an artificial airway or impaired cough reflex.
- Sterile suctioning is indicated for patients who have excessive or thick secretions that obstruct the airway, or who are unable to clear their own secretions due to decreased level of consciousness, neuromuscular weakness, or respiratory distress.
- Sterile suctioning requires sterile equipment and supplies, such as a suction device, tubing system, collection container, catheter, saline solution, gloves, sterile drape, PPE, oxygen source, and stethoscope.
- Sterile suctioning involves inserting the catheter into the artificial airway using sterile technique, applying intermittent suction by placing and releasing the thumb over the vent while withdrawing the catheter slowly, rotating the catheter between the thumb and forefinger to remove secretions from all sides of the airway, rinsing the catheter and tubing with saline solution or water after each suction pass, reoxygenating the patient with 100% oxygen for 30 seconds to 3 minutes after each suction pass, and repeating these steps until no more secretions are obtained or until three passes are completed.
- Sterile suctioning can cause complications such as hypoxia, hypotension, bradycardia, arrhythmias, bleeding, infection, mucosal damage, bronchospasm, atelectasis, and increased intracranial pressure.
- Sterile suctioning requires nursing interventions and assessments before, during, and after the procedure to ensure patient safety, comfort, and optimal outcomes.
- Sterile suctioning is evaluated by comparing the patient’s condition before and after suctioning, and by monitoring for any changes or improvements in airway patency, infection prevention, gas exchange, comfort, and complications.
Tracheostomy care

- A tracheostomy is an opening (stoma) created in the anterior wall of the trachea to provide a stable and secure airway. It is usually performed when the upper airway is obstructed or compromised by trauma, tumor, infection, or edema. It can also be done for patients who require long-term mechanical ventilation or frequent suctioning to prevent aspiration of secretions. A tracheostomy tube is inserted into the stoma to maintain its patency and facilitate ventilation.
Types and Components of Tracheostomy Tubes
- Tracheostomy tubes come in various sizes and angles to fit different patients’ anatomy and needs. They are made of metal, plastic, or silicone. Some common types of tracheostomy tubes are:
- Cuffed: A cuff is a balloon-like device that inflates around the tube to seal the trachea and prevent air leakage or aspiration. It is used for patients who need mechanical ventilation or have a high risk of aspiration. The cuff pressure should be monitored regularly and kept between 20 to 25 cm H2O to prevent tracheal damage.
- Uncuffed: An uncuffed tube has no cuff and allows air to flow around the tube. It is used for patients who can breathe spontaneously and have a low risk of aspiration. It also allows the patient to speak and cough more easily.
- Fenestrated: A fenestrated tube has one or more holes on the outer cannula that allow air to pass through the vocal cords when the inner cannula is removed. It is used for patients who are ready to wean from mechanical ventilation or need speech therapy. The fenestration should be covered by a cap or plug when suctioning or ventilating.
- Double-lumen: A double-lumen tube has two cannulas: an outer cannula that stays in place and an inner cannula that can be removed for cleaning or changing. The inner cannula provides a clear passage for air and secretions and reduces the risk of tube occlusion.
The components of a tracheostomy tube are:
- Flange: A flat plate that rests on the neck and holds the tube in place. It has holes for securing the tube with ties or straps.
- Obturator: A cone-shaped device that is inserted into the tube to guide its insertion and prevent injury to the tracheal wall. It is removed after the tube is in place.
- Pilot balloon: A small balloon that indicates the status of the cuff. It is connected to a valve that allows inflation or deflation of the cuff.
- Suction port: An opening on the tube that allows connection to a suction catheter for removing secretions.
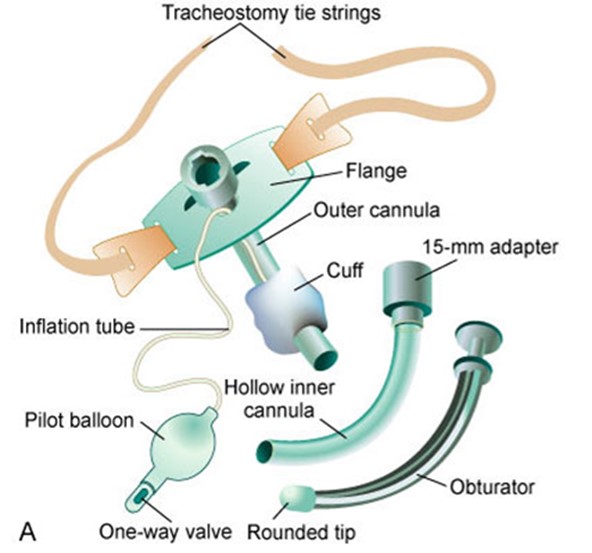
Nursing Interventions for Tracheostomy Care
- The nursing interventions for tracheostomy care include:
- Assessing the patient’s respiratory status, vital signs, oxygen saturation, and level of consciousness frequently.
- Monitoring the position, patency, and security of the tube and ensuring that it is not displaced or dislodged.
- Changing the dressing around the stoma daily or as needed using a sterile technique and observing for signs of infection, bleeding, or skin breakdown.
- Cleaning the stoma and the flange with normal saline or sterile water using cotton swabs or gauze pads.
- Changing the ties or straps when they are soiled, wet, or loose using a square knot and leaving enough space for one finger between the tie and the neck.
- Providing humidification and hydration to prevent drying and crusting of secretions.
- Performing tracheostomy care every 8 to 12 hours or as needed using a sterile technique and following these steps:
- Gather equipment and supplies such as gloves, goggles, mask, gown, sterile towel, sterile gloves, sterile water or saline, hydrogen peroxide, suction catheter, suction machine, tracheostomy cleaning kit, new dressing, new ties or straps, and bag-valve-mask (BVM) ventilator system connected to an oxygen source.
- Explain the procedure to the patient and obtain consent if possible.
- Position the patient in semi-Fowler’s position with the head slightly hyperextended.
- Put on gloves, goggles, mask, and gown if necessary.
- Remove the old dressing and discard it in a moisture-resistant bag.
- Inspect the stoma for signs of infection, bleeding, or skin breakdown and report any abnormal findings to the health care provider.
- Remove the inner cannula if present and place it in a container with sterile water or saline.
- Clean the inner cannula with a brush or pipe cleaner soaked in hydrogen peroxide and rinse it with sterile water or saline.
- Reinsert the inner cannula and lock it in place.
- Clean the outer cannula and the flange with cotton swabs or gauze pads soaked in hydrogen peroxide and rinse them with sterile water or saline.
- Apply a new dressing around the stoma and secure it with tape or clips.
- Change the ties or straps if needed using a square knot and leaving enough space for one finger between the tie and the neck.
- Remove gloves and perform hand hygiene.
- Put on sterile gloves and prepare to suction the tube.
Steps of Suctioning a Tracheostomy Tube
- Suctioning a tracheostomy tube is a sterile, invasive technique that requires a nurse or a respiratory therapist. It is done to remove secretions from the tube and prevent obstruction, infection, or hypoxia. The steps of suctioning a tracheostomy tube are:
- Review the health care provider’s orders and the patient’s nursing plan of care.
- Gather equipment and supplies such as gloves, goggles, mask, gown, sterile towel, sterile gloves, sterile water or saline, hydrogen peroxide, suction catheter, suction machine, pulse oximeter, oxygen source, and bag-valve-mask (BVM) ventilator system.
- Explain the procedure to the patient and obtain consent if possible.
- Position the patient in semi-Fowler’s position with the head slightly hyperextended.
- Perform hand hygiene and don gloves, goggles, mask, and gown if necessary.
- Remove the old dressing and discard it in a moisture-resistant bag.
- Inspect the stoma for signs of infection, bleeding, or skin breakdown and report any abnormal findings to the health care provider.
- Assess the patient’s respiratory status, vital signs, oxygen saturation, and level of consciousness before suctioning.
- Provide humidification and hydration to the patient to prevent drying and crusting of secretions.
- Hyperoxygenate the patient before and after suctioning using a BVM ventilator system connected to an oxygen source.
- Lower the side rail and place a sterile towel or a waterproof pad across the patient’s chest.
- Turn on the suction machine and set the pressure to the appropriate level according to the patient’s age:
|
Age |
Pressure (mm Hg) |
|
Adult |
100-160 |
|
Child |
100-120 |
|
Infant |
80-100 |
|
Neonate |
60-80 |
- Check the pressure by occluding the end of the connecting tube with a gloved hand.
- Pour sterile saline into a container and open a suction catheter kit.
- Don sterile gloves and pick up the sterile catheter with the dominant hand.
- With the non-dominant hand, pick up the connecting tubing and connect it to the suction catheter.
- Moisten the tip of the catheter in the sterile saline and occlude the Y-port to check suction.
- Remove the inner cannula if present and place it in a container with sterile water or saline.
- With the dominant hand, gently insert the catheter into the tracheostomy tube until resistance is met. Do not occlude the Y-port or apply suction when inserting the catheter.
- Apply suction by intermittently occluding the Y-port on the catheter with the thumb of your non-dominant hand, and gently rotate and withdraw the catheter. Do not apply suction for more than 10 seconds at a time.
- Rinse the catheter with sterile saline between each suctioning attempt. Limit suctioning attempts to three per session. Allow at least one minute between each attempt for oxygenation. Monitor oxygen saturation throughout suctioning.
Potential Complications and Emergency Situations Related to Tracheostomy
- Tracheostomy is a life-saving procedure, but it also carries some risks and complications that require prompt recognition and management. Some of the potential complications and emergency situations related to tracheostomy are:
- Bleeding: Bleeding can occur during or after the tracheostomy procedure due to injury to the blood vessels, erosion of the tracheal wall, or infection. Bleeding can be minor or massive and can cause airway obstruction, hypovolemia, or shock. To manage bleeding, apply direct pressure to the site, elevate the head of the bed, notify the health care provider, and prepare for possible transfusion or surgical intervention.
- Infection: Infection can occur at the stoma site or in the lower respiratory tract due to contamination of the tube or secretions. Infection can cause inflammation, edema, pus formation, fever, increased secretions, or foul odor. To prevent and treat infection, use sterile technique for tracheostomy care and suctioning, change the tube and dressing as ordered, administer antibiotics as prescribed, and monitor for signs and symptoms of infection.
- Tracheomalacia: Tracheomalacia is a condition where the tracheal wall becomes soft and weak due to constant pressure exerted by the cuff. It causes tracheal dilation and erosion of cartilage, leading to loss of tissue integrity. Tracheomalacia can manifest as an increased amount of air required in the cuff to maintain the seal, a larger tracheostomy tube required to prevent an air leak at the stoma, food particles seen in tracheal secretions, or reduced tidal volume on the ventilator. To prevent and manage tracheomalacia, use an uncuffed tube as soon as possible, monitor cuff pressure and air volumes closely, and detect changes.
- Tracheal stenosis: Tracheal stenosis is a narrowing of the tracheal lumen due to scar formation from irritation of the tracheal mucosa by the cuff. It impairs tissue integrity and airflow. Tracheal stenosis is usually seen after the cuff is deflated or the tracheostomy tube is removed. It can present as increased coughing, inability to expectorate secretions, difficulty breathing or talking, stridor, or cyanosis. To prevent and manage tracheal stenosis, prevent pulling or traction on the tracheostomy tube, properly secure the tube in the midline position, maintain proper cuff pressure, minimize oronasal intubation time, and perform tracheal dilation or surgical intervention if needed.
- Tracheoesophageal fistula (TEF): TEF is a hole created between the trachea and the anterior esophagus due to excessive cuff pressure that causes erosion of the posterior wall of the trachea. It allows communication between the respiratory and digestive systems. The patient at highest risk also has a nasogastric tube present. TEF can cause similar manifestations as tracheomalacia, such as increased air in cuff needed to achieve a seal, food particles seen in tracheal secretions, reduced tidal volume on the ventilator, as well as increased coughing and choking while eating. To prevent and manage TEF, maintain cuff pressure, monitor the amount of air needed for inflation and detect changes, progress to a deflated cuff or cuffless tube as soon as possible, manually administer oxygen by mask to prevent hypoxemia, use a small soft feeding tube instead of a nasogastric tube for tube feedings, perform a gastrostomy or jejunostomy if indicated, monitor for TEF and aspiration signs.
- Trachea-innominate artery fistula: Trachea-innominate artery fistula is a rare but life-threatening complication where a malpositioned tube causes its distal tip to push against the lateral wall of the tracheostomy. Continued pressure causes necrosis and erosion of the innominate artery (a large artery that branches from the aortic arch). It can result in massive hemorrhage into the trachea that can be fatal within minutes. Trachea-innominate artery fistula can manifest as pulsation of the tracheostomy tube in synchrony with the heartbeat, sudden bright red bleeding from the tube or stoma, hypotension, tachycardia, or shock. To prevent and manage trachea-innominate artery fistula, ensure proper positioning and alignment of the tube, monitor for signs of bleeding, apply direct pressure to stop bleeding, notify health care provider immediately, prepare for emergency surgery, and administer fluids and blood products as ordered.
Patient Education and Support for Tracheostomy
- Patients with a tracheostomy need education and support to cope with their condition and promote their recovery. Some of the patient education and support topics for tracheostomy are:
- Anatomy and physiology of the respiratory system and the purpose and function of the tracheostomy tube
- Care and maintenance of the tracheostomy tube, stoma, dressing, and ties or straps
- Suctioning technique, frequency, and indications
- Humidification and hydration methods and importance
- Signs and symptoms of infection, bleeding, or other complications and when to seek medical attention
- Communication methods such as speaking valves, electronic devices, or writing tools
- Swallowing assessment and evaluation and dietary modifications if needed
- Medication administration and management
- Activity level and exercise recommendations
- Emotional and psychological support and coping strategies
- Resources and referrals for home care, rehabilitation, or support groups
Conclusion
- Tracheostomy is a surgical procedure that creates an opening in the trachea to provide a stable and secure airway. It is indicated for patients who have upper airway obstruction, require long-term mechanical ventilation, or need frequent suctioning. Tracheostomy tubes come in various types and components to suit different patients’ needs. Nursing interventions for tracheostomy care include assessing, monitoring, cleaning, changing, humidifying, and suctioning the tube and stoma. Potential complications and emergency situations related to tracheostomy include bleeding, infection, tracheomalacia, tracheal stenosis, tracheoesophageal fistula, and trachea-innominate artery fistula. Patient education and support for tracheostomy include anatomy and physiology, care and maintenance, suctioning, humidification, hydration, infection prevention, complication recognition, communication, swallowing, medication administration, activity level, exercise, emotional support, coping strategies, resources, and referrals.
Summary
- A tracheostomy is an opening in the trachea to provide a stable and secure airway.
- Tracheostomy tubes come in various types and components such as cuffed, uncuffed, fenestrated, double-lumen, flange, obturator, pilot balloon, suction port.
- Nursing interventions for tracheostomy care include assessing, monitoring, cleaning, changing, humidifying, and suctioning the tube and stoma using sterile technique.
- Suctioning a tracheostomy tube is a sterile invasive technique that requires a nurse or a respiratory therapist. It is done to remove secretions from the tube and prevent obstruction, infection, or hypoxia. The steps of suctioning a tracheostomy tube are: review orders, gather equipment, explain procedure, position patient, perform hand hygiene, don PPE, remove old dressing, inspect stoma, assess respiratory status, provide humidification, hyperoxygenate patient, lower side rail, place towel or pad, turn on suction machine, set pressure, check pressure, pour saline, open catheter kit, don sterile gloves, pick up catheter, connect tubing, moisten catheter, occlude Y-port, remove inner cannula, insert catheter until resistance, apply suction by occluding Y-port intermittently while rotating and withdrawing catheter, rinse catheter between attempts, limit attempts to three per session with one minute between each attempt for oxygenation.
- Potential complications and emergency situations related to tracheostomy include bleeding (apply direct pressure), infection (use sterile technique), tracheomalacia (use uncuffed tube), tracheal stenosis (prevent pulling or traction), tracheoesophageal fistula (maintain cuff pressure), trachea-innominate artery fistula (ensure proper positioning).
- Patient education and support for tracheostomy include anatomy and physiology, care and maintenance, suctioning, humidification, hydration, infection prevention, complication recognition, communication, swallowing, medication administration, activity level, exercise, emotional support, coping strategies, resources,and referrals.
Chest tubes
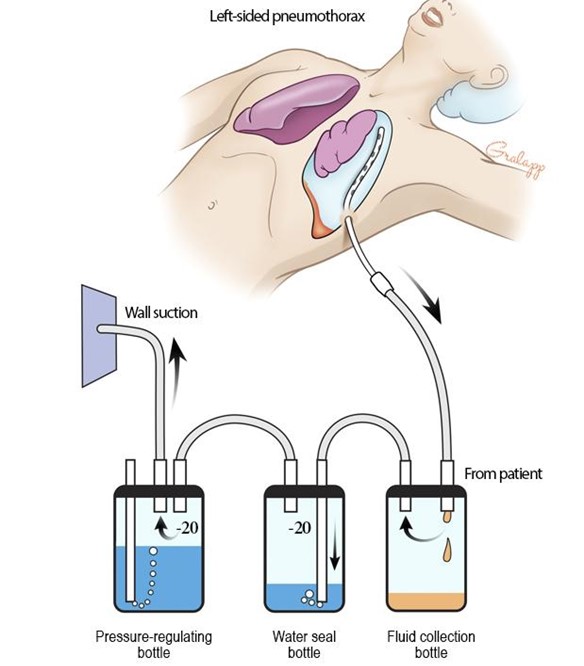
- Chest tubes are hollow, flexible tubes that are inserted into the pleural space (the space between the lungs and the chest wall) or the mediastinum (the space between the lungs that contains the heart, great vessels, and other structures) to drain air, blood, pus, or fluid and restore normal intrathoracic pressure.
- Chest tubes are connected to a drainage system that collects the drainage and prevents air or fluid from re-entering the chest cavity.
- Chest tube insertion is a sterile, invasive procedure that requires a physician’s order and informed consent from the patient.
- Chest tube care and management are essential nursing skills that involve monitoring, assessing, documenting, and troubleshooting the chest tube and drainage system.
Indications and Contraindications
- The main indications for chest tube insertion are:
- Pneumothorax: a collection of air in the pleural space that causes lung collapse
- Hemothorax: a collection of blood in the pleural space that compresses the lung
- Pleural effusion: an accumulation of fluid in the pleural space that impairs gas exchange
- Empyema: an infection of the pleural space that produces pus
- Chylothorax: a leakage of lymphatic fluid into the pleural space
- Postoperative thoracic surgery: to prevent or treat complications such as atelectasis, pneumothorax, or bleeding
- The main contraindications for chest tube insertion are:
- Coagulopathy: a bleeding disorder that increases the risk of hemorrhage
- Skin infection: a source of contamination that increases the risk of infection
- Lung adhesion: a condition where the lung is attached to the chest wall, making it difficult to insert the chest tube
Types and Components of Chest Tube Drainage Systems
- There are four main types of chest tube drainage systems:
- Wet suction: a system that uses water to create suction and a water seal
- Dry suction: a system that uses a mechanical regulator to create suction and a water seal
- Dry-Wet suction: a system that uses a mechanical regulator to create suction and water to create a water seal
- Mediastinal: a system that drains air or fluid from the mediastinum without suction or water seal
- The common components of chest tube drainage systems are:
- Collection chamber: a chamber that collects the drainage from the chest tube and has a calibrated scale to measure the amount and rate of drainage
- Water-seal chamber: a chamber that contains water (usually 2 cm) and acts as a one-way valve to prevent air or fluid from returning to the chest cavity. It also allows for monitoring of intrapleural pressure changes by observing fluctuations (tidaling) or bubbling in the water column.
- Suction-control chamber: a chamber that regulates the amount of suction applied to the chest cavity by using either water (usually 20 cm) or a mechanical regulator. It also indicates the presence and level of suction by observing gentle bubbling in the water column or an orange bellows in the regulator.
- Tubing: a set of tubing that connects the chest tube to the drainage system and has clamps, stopcocks, or caps to control or occlude the flow of air or fluid. The tubing should be patent, secured, and free of kinks, loops, or dependent areas.
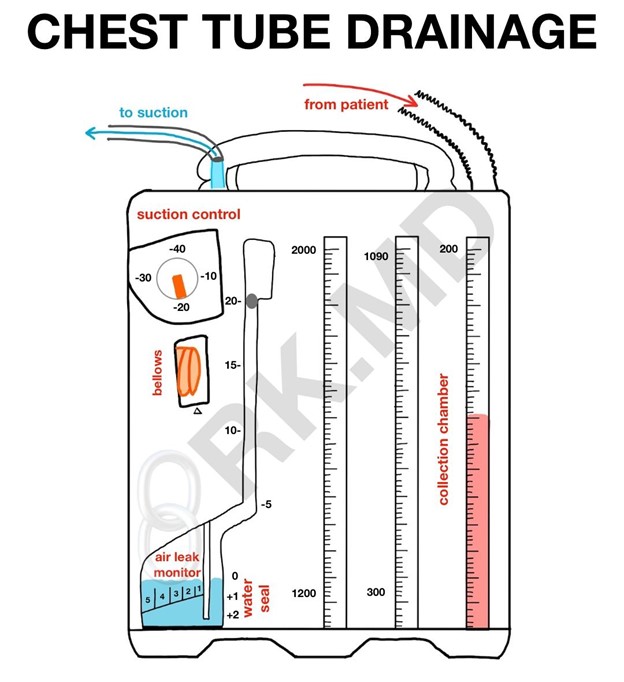
Nursing Responsibilities for Chest Tube Care and Management
- The nursing responsibilities for chest tube care and management include:
- Preparing the patient for chest tube insertion by explaining the procedure, obtaining informed consent, administering analgesia or sedation, positioning the patient, monitoring vital signs, oxygen saturation, and pain level, assisting with sterile technique, applying dressing and securing tubing, and obtaining a chest x-ray to confirm placement.
- Monitoring and assessing the patient’s respiratory status, vital signs, pain level, wound site, chest tube function, drainage system function, drainage amount, color, and consistency, and documenting findings at least every four hours or as ordered.
- Maintaining the chest tube patency by avoiding kinks, loops, or dependent areas in the tubing, keeping the drainage system below the chest level, and milking or stripping the tubing only if ordered and with caution to prevent increased intrathoracic pressure or damage to the lung tissue.
- Maintaining the chest tube function by ensuring that the water levels are adequate and stable in the water-seal and suction-control chambers, that the suction source is connected and working properly, that the tubing is clamped only when necessary and for a short time, and that the drainage system is intact and upright.
- Preventing complications by observing for signs of infection, bleeding, air leak, tension pneumothorax, subcutaneous emphysema, or re-expansion pulmonary edema, and intervening accordingly by administering antibiotics, applying pressure dressing, locating and sealing the air leak source, notifying the physician, releasing the clamp, administering oxygen, or diuretics as ordered.
- Educating the patient and family about the purpose and function of the chest tube and drainage system, the expected outcomes and potential complications, the importance of deep breathing, coughing, incentive spirometry, pain management, mobility, and nutrition, and the discharge instructions and follow-up care.
Potential Complications and Interventions for Chest Tube Malfunction or Removal
- The potential complications and interventions for chest tube malfunction or removal are: Open in browser
|
Complication |
Description |
Intervention |
|
Infection |
A bacterial invasion of the pleural space or wound site that causes fever, chills, increased white blood cell count, purulent drainage, redness, swelling, or pain. |
Administer antibiotics as ordered. Monitor vital signs and wound site. Change dressing using sterile technique. Obtain cultures as ordered. |
|
Bleeding |
A hemorrhage from the chest tube insertion site or from the lung or pleural vessels that causes increased drainage (>100 mL/hour), bright red drainage, hypotension, tachycardia, pallor, or decreased hemoglobin. |
Apply pressure dressing to the wound site. Monitor vital signs and drainage. Notify the physician. Administer fluids and blood products as ordered. Prepare for surgery if needed. |
|
Air leak |
A leakage of air from the chest tube system that causes continuous bubbling in the water-seal chamber or a loss of tidaling. |
Locate the source of air leak by clamping the tubing at different segments (starting from the chest) until bubbling stops. If leak is in the tubing or drainage system, replace or repair it. If leak is in the chest tube or wound site, notify the physician. Apply occlusive dressing to seal wound site. |
|
Tension pneumothorax |
A life-threatening condition where air accumulates in the pleural space and causes increased intrathoracic pressure that compresses the lung and shifts the mediastinum to the opposite side. It causes severe dyspnea, hypoxia, hypotension, tachycardia, tracheal deviation, jugular venous distension, absent breath sounds on affected side. |
Release any clamps on the tubing. Assess for kinks or obstructions in the tubing. Notify the physician immediately. Prepare for needle decompression or chest tube insertion on affected side. Administer oxygen as ordered. Monitor vital signs and oxygen saturation. |
|
Subcutaneous emphysema |
A condition where air escapes into the subcutaneous tissue around the chest tube insertion site or wound site. It causes crepitus (crackling sensation) on palpation. |
Notify the physician. Monitor respiratory status and oxygen saturation. Administer oxygen as ordered. Elevate head of bed to facilitate breathing. |
|
Re-expansion pulmonary edema |
A rare but serious complication where fluid accumulates in the lung tissue after rapid re-expansion of a collapsed lung. It causes dyspnea, hypoxia, coughing up pink frothy sputum, crackles on auscultation. |
Notify the physician immediately. Administer oxygen as ordered. Monitor vital signs and oxygen saturation. Administer diuretics as ordered. Prepare for intubation or mechanical ventilation if needed. |
- The procedure for chest tube removal involves:
- Obtaining a physician’s order and informed consent from the patient
- Administering analgesia or sedation as ordered
- Preparing sterile supplies such as dressing, suture removal kit, petroleum gauze
- Positioning the patient in semi-Fowler’s position with affected arm raised above head
- Instructing the patient to perform Valsalva maneuver (exhale forcefully with mouth closed) or hold breath at end expiration
- Cutting sutures and removing chest tube quickly with one motion
- Applying occlusive dressing with petroleum gauze over wound site
- Instructing patient to resume normal breathing
- Obtaining a
- Obtaining a chest x-ray to confirm chest tube removal and absence of pneumothorax
- Monitoring and assessing the patient’s respiratory status, vital signs, pain level, wound site, and dressing for any signs of complications such as infection, bleeding, air leak, or pneumothorax
- Educating the patient and family about the wound care, activity restrictions, signs and symptoms to report, and follow-up care

Conclusion
- Chest tubes are lifesaving devices that are used to drain air, blood, pus, or fluid from the pleural space or the mediastinum and restore normal intrathoracic pressure
- Chest tube care and management require knowledge and skills in preparing the patient for chest tube insertion, monitoring and assessing the patient and the drainage system, maintaining the chest tube patency and function, preventing and managing complications, and removing the chest tube safely
- Chest tube care and management are collaborative efforts that involve the physician, nurse, patient, and family
Summary
- Chest tubes are inserted into the pleural space or the mediastinum to drain air, blood, pus, or fluid
- Chest tubes are connected to a drainage system that collects the drainage and prevents air or fluid from re-entering the chest cavity
- Chest tube drainage systems have four main types: wet suction, dry suction, dry-wet suction, and mediastinal
- Chest tube drainage systems have common components: collection chamber, water-seal chamber, suction-control chamber, and tubing
- Chest tube care and management involve preparing the patient for chest tube insertion, monitoring and assessing the patient and the drainage system, maintaining the chest tube patency and function, preventing and managing complications, and removing the chest tube safely
- Chest tube complications include infection, bleeding, air leak, tension pneumothorax, subcutaneous emphysema, and re-expansion pulmonary edema
Nasogastric (NG) tube Insertion
- A nasogastric (NG) tube is a flexible plastic tube that is inserted through the nose, down the esophagus, and into the stomach. It can be used for various purposes, such as:
- Decompressing the stomach by removing gas and fluids.
- Feeding the patient with liquid nutrition or medications.
- Lavaging the stomach to remove toxins or blood.
- Obtaining gastric samples for diagnostic tests.
- There are different types of NG tubes, depending on their size, shape, and function. Some common ones are:
- Levin tube: a single-lumen tube with holes near the tip that is used for decompression or feeding. It requires intermittent suction.
- Salem sump tube: a double-lumen tube with one lumen for decompression or feeding and another lumen for air venting. It allows continuous suction without collapsing the stomach wall.
- Dobhoff tube: a small-bore tube with a weighted tip that is used for feeding. It has a stylet (wire) inside that helps guide the tube into the stomach or duodenum. It requires radiographic confirmation of placement.
- The insertion of an NG tube is a sterile or clean procedure that requires a medical order and informed consent from the patient or their representative. It also requires careful assessment of the patient’s condition, anatomy, and ability to cooperate. Some indications for NG tube insertion are:
- Gastric obstruction, ileus, or bowel perforation.
- Gastric bleeding or poisoning.
- Malnutrition or dysphagia.
- Gastric analysis or pH monitoring.
- Some contraindications or cautions for NG tube insertion are:
- Facial trauma, nasal surgery, or deviated septum.
- Esophageal varices, stricture, or diverticulum.
- Coagulopathy or anticoagulant therapy.
- Increased intracranial pressure or skull fracture.
- Some potential complications or risks of NG tube insertion are:
- Nasal irritation, bleeding, or ulceration.
- Esophageal perforation, bleeding, or spasm.
- Aspiration pneumonia or pulmonary edema.
- Gastric erosion, ulceration, or perforation.
Equipment
- The equipment needed for NG tube insertion may vary depending on the type of tube and the purpose of insertion. However, some common items are:
- NG tube of appropriate size and type (usually 14 to 18 French for adults).
- Water-soluble lubricant (or mannequin lube).
- Topical anesthetic spray or gel (optional).
- Tape measure and marker or tape to mark the insertion distance.
- Clean gloves and protective eyewear.
Procedure
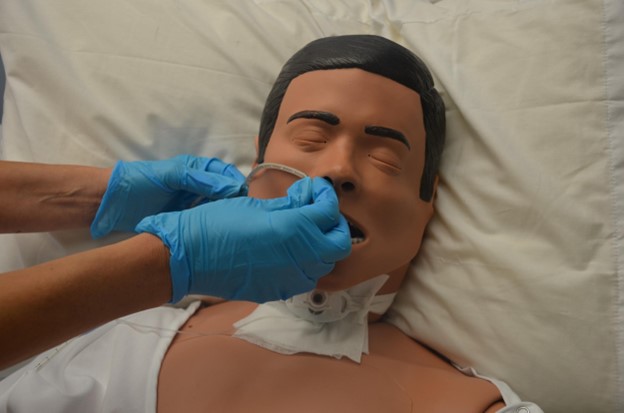
- The procedure for NG tube insertion may vary depending on the type of tube and the purpose of insertion. However, some common steps are:
- Explain the procedure to the patient and obtain informed consent. Assess the patient’s condition, anatomy, and ability to cooperate. Check for any contraindications or cautions. Gather the necessary equipment and supplies.
- Choose the side for tube insertion and spray topical anesthetic in this nostril and the pharynx at least 5 minutes before tube insertion. If time permits, give 4 mL of 10% lidocaine via a nebulizer or insert 5 mL of 2% lidocaine gel into the nares.
- Measure the insertion distance by placing the tip of the tube at the tip of the nose, then extending it to the earlobe and then to the xiphoid process. Mark this distance with a marker or tape.
- Lubricate the tip of the tube with water-soluble lubricant. Position the patient in a high-Fowler’s position with the head tilted forward. If the patient is unconscious or intubated, position them in a supine position with the head of the bed elevated to 30 degrees.
- Insert the tube through the nostril with gentle pressure and a slight twisting motion. Ask the patient to swallow water or saliva as the tube advances. If resistance is felt, withdraw the tube slightly and try another direction. Do not force the tube or insert it deeper than the marked distance.
- Verify the placement of the tube by using one or more of the following methods:
- Aspirate gastric contents with a syringe and check the pH. A pH of 5.5 or less indicates gastric placement.
- Inject air through the tube while auscultating over the stomach. A whooshing sound indicates gastric placement. However, this method is not reliable and should be used with caution.
- Obtain a chest x-ray and confirm that the tip of the tube is below the diaphragm and in the stomach. This is the most accurate method and should be used for small-bore tubes or when other methods are inconclusive.
- Secure the tube to the nose with tape or a commercial device. Make sure there is no tension on the tube and that it does not interfere with breathing or swallowing. Label the tube with the date, time, type, and length of insertion.
- Connect the tube to a feeding bag, syringe, or suction device as ordered. Adjust the flow rate, volume, and frequency of feeding or suctioning as prescribed. Monitor for any signs of complications such as aspiration, bleeding, infection, or displacement.
- Document the procedure, including:
- The type, size, and length of the tube.
- The method and result of placement verification.
- The patient’s tolerance and response to the procedure.
- The type, rate, volume, and frequency of feeding or suctioning.
- The appearance, amount, and pH of gastric aspirate.
- The condition of the nose, mouth, and skin around the tube.
- Any teaching done or referrals made.
Nursing Care
- The nursing care for patients with NG tubes involves the following aspects:
- Assessing the patient’s condition, vital signs, fluid and electrolyte balance, nutritional status, and comfort level at least every 4 hours or as ordered.
- Checking the tube placement, patency, and security at least every 4 to 8 hours or as ordered. If the tube is dislodged, kinked, or clogged, do not attempt to reinsert or flush it. Notify the physician and obtain a new order for tube insertion.
- Providing oral and nasal hygiene at least every 4 hours or as needed. Use a soft toothbrush, mouthwash, and lip balm to clean the mouth and teeth. Use a moist cotton swab or gauze to clean the nostrils and apply a thin layer of petroleum jelly to prevent dryness and irritation.
- Monitoring for any signs of complications such as aspiration, bleeding, infection, or displacement. Some signs are:
- Coughing, choking, wheezing, or dyspnea.
- Hematemesis, melena, or hemoptysis.
- Fever, purulent drainage, or erythema around the tube site.
- Nausea, vomiting, abdominal distension, or pain.
- Educating the patient and family about the purpose, procedure, and care of the NG tube. Teach them how to:
- Recognize and report any signs of complications.
- Maintain proper positioning and head elevation during and after feeding or suctioning.
- Perform oral and nasal hygiene and tube care as instructed.
- Measure and record the intake and output of fluids.
- Administer medications through the tube as prescribed .
Conclusion
- NG tube insertion is a common procedure that can be used for various purposes such as decompression, feeding, lavage, or diagnosis. It requires a medical order and informed consent from the patient or their representative. It also requires careful assessment of the patient’s condition, anatomy, and ability to cooperate. It involves measuring the insertion distance, lubricating the tube tip, inserting the tube through the nostril, verifying the placement of the tube, securing the tube to the nose, connecting the tube to a feeding bag, syringe, or suction device as ordered, and documenting the procedure. The nursing care for patients with NG tubes involves assessing the patient’s condition and comfort level, checking the tube placement and patency, providing oral and nasal hygiene, monitoring for any signs of complications, and educating the patient and family about the purpose, procedure, and care of the NG tube.
Summary
- NG tube is a flexible plastic tube that is inserted through the nose into the stomach for various purposes.
- NG tube insertion requires a medical order and informed consent from the patient or their representative.
- NG tube insertion involves measuring the insertion distance, lubricating the tube tip, inserting the tube through the nostril, verifying the placement of the tube, securing the tube to the nose, connecting the tube to a feeding bag, syringe, or suction device as ordered, and documenting the procedure.
- Nursing care for patients with NG tubes involves assessing the patient’s condition and comfort level, checking the tube placement and patency, providing oral and nasal hygiene, monitoring for any signs of complications, and educating the patient and family about the purpose, procedure, and care of the NG tube.
Continuous Passive ROM Machine

- A continuous passive ROM machine is a device that moves a joint through a prescribed range of motion without active muscle contraction by the patient. It is used by patients who have stiffness, swelling, pain, or limited mobility in a joint due to surgery, injury, or disease. It can also prevent complications such as contractures, adhesions, or thrombosis. The most common joints that are treated with a continuous passive ROM machine are the knee and the shoulder.
The nurse should set up and operate a continuous passive ROM machine by following these steps:
- Obtain a physician’s order for using a continuous passive ROM machine that specifies the joint, speed, duration, frequency, and range of motion.
- Explain the procedure and its benefits to the patient and obtain informed consent.
- Position the patient comfortably on a bed or a chair and secure the device to the affected joint according to the manufacturer’s instructions.
- Adjust the settings of the device according to the physician’s order and start the machine.
- Monitor the patient’s vital signs, pain level, comfort, and response to the device throughout the session.
- Stop the machine and remove it from the patient after completing the session or as ordered by the physician.
- The nurse should monitor for complications such as bleeding, infection, nerve damage, or mechanical failure from using a continuous passive ROM machine. The nurse should also inspect the device regularly for cleanliness and functionality and report any problems to the appropriate personnel.

Enteral nutrition
- Enteral nutrition (EN) is the delivery of nutrients directly into the gastrointestinal (GI) tract through a tube, catheter, or stoma.
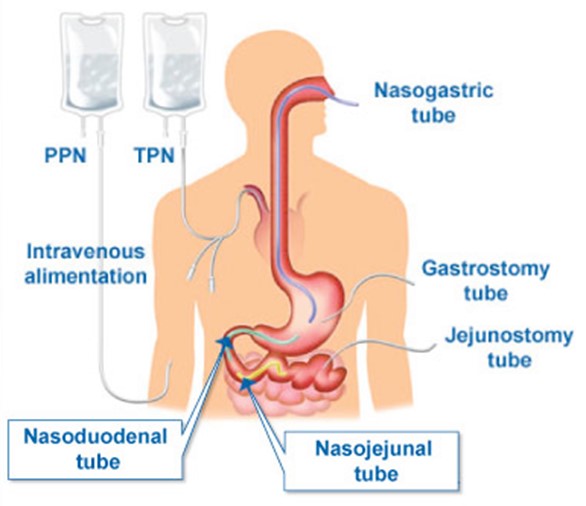
- EN is indicated for patients who have a functional GI tract but are unable to meet their nutritional needs orally due to impaired swallowing, anorexia, facial trauma, oral cancer, etc.
- EN is contraindicated for patients who have a nonfunctional or inaccessible GI tract due to obstruction, ileus, peritonitis, severe diarrhea, vomiting, etc.
- EN has several advantages over parenteral nutrition (PN), such as lower cost, lower risk of infection, fewer metabolic complications, and preservation of gut integrity and immunity.
- EN also has some potential complications, such as aspiration, tube displacement or occlusion, diarrhea, nausea, vomiting, abdominal distension or cramping, electrolyte imbalance, dehydration, etc.
Types of Enteral Nutrition
- EN formulas vary in their composition, osmolality, caloric density, fiber content, and protein quality.
- EN formulas can be classified into four main types:
- Standard or polymeric formulas: These contain intact proteins, carbohydrates, and fats that require normal digestion and absorption. They provide 1 to 1.5 kcal/mL and are suitable for most patients with normal or mildly impaired GI function. Examples include Ensure, Isocal, and Osmolite.
- Hydrolyzed or elemental formulas: These contain predigested proteins (peptides or amino acids), carbohydrates (glucose or maltodextrin), and fats (medium-chain triglycerides) that require minimal digestion and absorption. They provide 1 to 1.5 kcal/mL and are suitable for patients with impaired GI function or malabsorption. Examples include Peptamen, Vivonex, and NutriHep.
- Disease-specific formulas: These are designed to meet the special nutritional needs of patients with specific diseases or conditions. They may have modified amounts of protein, carbohydrates, fats, vitamins, minerals, electrolytes, or other nutrients. Examples include Nepro (for renal disease), Glucerna (for diabetes), Pulmocare (for respiratory disease), and Impact (for trauma or surgery).
- Modular formulas: These are single-nutrient preparations that can be added to other formulas or foods to increase the caloric or protein content. They may contain protein (ProMod), carbohydrates (Polycose), fats (Microlipid), or fiber (Benefiber).
Routes of Enteral Nutrition
- EN can be delivered through different routes depending on the patient’s condition, anatomy, and expected duration of therapy.
- EN routes can be classified into two main categories:
- Gastric routes: These involve placing a tube into the stomach through the nose (nasogastric tube) or the abdominal wall (gastrostomy tube). Gastric routes are preferred for short-term (<4 weeks) or long-term (>4 weeks) EN in patients with normal gastric emptying and low risk of aspiration. Gastric routes allow for larger volumes and bolus feedings. Examples of gastric tubes include Levin tube (single-lumen), Salem sump tube (double-lumen), percutaneous endoscopic gastrostomy (PEG) tube, and surgical gastrostomy tube.
- Intestinal routes: These involve placing a tube into the duodenum or jejunum through the nose (nasoduodenal or nasojejunal tube) or the abdominal wall (jejunostomy tube). Intestinal routes are preferred for short-term (<4 weeks) or long-term (>4 weeks) EN in patients with impaired gastric emptying or high risk of aspiration. Intestinal routes require smaller volumes and continuous feedings. Examples of intestinal tubes include Dobbhoff tube (small-bore), percutaneous endoscopic jejunostomy (PEJ) tube, and surgical jejunostomy tube.
Methods of Enteral Nutrition
- EN can be administered by different methods depending on the patient’s tolerance, nutritional needs, and type and location of the tube.
- EN methods can be classified into four main types:
- Bolus method: This involves rapidly delivering 250 to 400 mL of formula through a syringe or funnel into the tube four to six times a day. This method takes about 10 minutes per feeding and mimics normal meal patterns. This method is suitable for gastric tubes only and may cause nausea, vomiting, aspiration, abdominal cramping, or diarrhea in some patients.
- Intermittent method: This involves delivering 300 to 400 mL of formula over 30 to 60 minutes by gravity drip or pump infusion every 3 to 6 hours. This method uses a feeding bag and allows for more flexibility and mobility. This method is suitable for gastric or intestinal tubes and may cause similar complications as the bolus method in some patients.
- Continuous method: This involves delivering a constant rate of formula over 8 to 24 hours by pump infusion. This method uses a feeding bag and requires close monitoring and frequent flushing of the tube. This method is suitable for intestinal tubes or patients with poor tolerance to other methods and may cause fewer complications than the bolus or intermittent methods in some patients.
- Cyclic method: This involves delivering a higher rate of formula over 8 to 16 hours, usually at night, by pump infusion. This method uses a feeding bag and allows for more freedom and oral intake during the day. This method is suitable for gastric or intestinal tubes or patients who are transitioning from EN to oral nutrition and may cause similar complications as the continuous method in some patients.
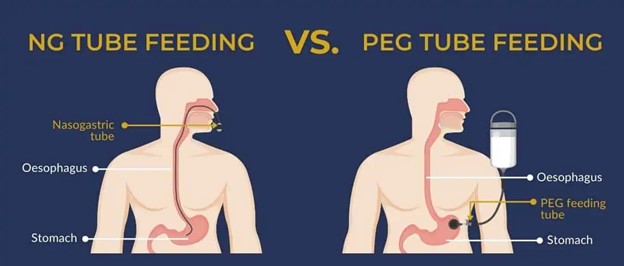
Nursing Interventions
- EN requires careful nursing interventions to ensure safe and effective delivery of nutrition and prevention of complications.
- Nursing interventions for EN can be divided into three phases:
- Initiation phase: This involves preparing the patient, verifying the tube placement, checking the residual volume, and starting the feeding. The nurse should:
- Obtain a baseline assessment of the patient’s weight, height, body mass index (BMI), nutritional status, laboratory values, fluid balance, and bowel function.
- Educate the patient and family about the purpose, procedure, benefits, and risks of EN.
- Confirm the type, route, method, rate, volume, frequency, and duration of EN ordered by the physician.
- Ensure that the tube is correctly placed in the desired location by checking the external markings, aspirating gastric contents and testing their pH (should be <5), or obtaining an x-ray confirmation.
- Check the residual volume (the amount of formula left in the stomach) before each feeding or every 4 to 6 hours for continuous feedings by aspirating with a syringe. The residual volume should be less than 200 mL or 10% of the previous feeding volume. If the residual volume is higher, the nurse should stop the feeding, return the aspirate to the stomach, and notify the physician.
- Start the feeding at a low rate (25 to 50 mL/hour) and gradually increase it by 10 to 20 mL/hour every 8 to 12 hours until the desired rate is reached. Monitor the patient’s tolerance and response to EN.
- Maintenance phase: This involves monitoring the patient’s condition, maintaining the tube patency and integrity, preventing infection and aspiration, and providing oral hygiene and comfort measures. The nurse should:
- Assess the patient’s vital signs, weight, fluid balance, nutritional status, laboratory values, bowel function, and skin integrity at least daily.
- Adjust the rate, volume, frequency, and duration of EN according to the patient’s needs and tolerance. Record the intake and output of EN.
- Flush the tube with at least 30 mL of water before and after each feeding or medication administration or every 4 hours for continuous feedings to prevent clogging. Use sterile water for immunocompromised patients.
- Change the feeding bag and tubing every 24 hours or according to the manufacturer’s instructions to prevent bacterial growth. Label the bag and tubing with date and time of initiation.
- Elevate the head of the bed at least 30 degrees during and for at least one hour after each feeding to prevent aspiration. Do not position the patient flat or on the right side unless ordered by the physician.
- Provide oral hygiene every 4 hours or as needed to prevent dryness, cracking, infection, or halitosis. Apply lip balm or moisturizer as needed.
- Rotate and secure the tube every day to prevent pressure ulcers or erosion at the insertion site. Cleanse the site with soap and water or saline solution and cover it with a sterile dressing as needed.
- Termination phase: This involves discontinuing EN when the patient’s nutritional needs can be met orally or when EN is no longer indicated or tolerated. The nurse should:
- Collaborate with the physician, dietitian, and speech therapist to determine the readiness and plan for oral nutrition. Assess the patient’s ability to swallow, chew, and digest food.
- Gradually decrease the rate, volume, frequency, and duration of EN while increasing the oral intake. Monitor the patient’s tolerance and response to oral nutrition.
- Flush the tube with at least 30 mL of water and clamp it before removing it. Gently withdraw the tube while the patient takes deep breaths or coughs. Discard the tube and dressing appropriately.
- Observe the patient for any signs of bleeding, infection, or perforation at the insertion site. Apply pressure and a sterile dressing as needed.
- Document the date, time, reason, and method of termination of EN. Record the patient’s condition and response to oral nutrition.
Evaluation and Outcomes
- EN requires regular evaluation and monitoring of the patient’s condition, response, and outcomes to determine the effectiveness and appropriateness of the therapy. The nurse should :
- Compare the patient’s actual intake with the prescribed intake and calculate the percentage of goal attainment. The patient should receive at least 75% of the prescribed intake to meet the nutritional needs.
- Compare the patient’s weight, BMI, nutritional status, laboratory values, fluid balance, and bowel function with the baseline and expected values. The patient should maintain or improve these parameters within normal ranges.
- Compare the patient’s tolerance and complications with the expected outcomes. The patient should have minimal or no adverse effects from EN.
- Compare the patient’s oral intake and readiness for oral nutrition with the expected outcomes. The patient should progress to oral nutrition as soon as possible and discontinue EN when no longer needed.
Summary
- EN is the delivery of nutrients directly into the GI tract through a tube, catheter, or stoma.
- EN is indicated for patients who have a functional GI tract but are unable to meet their nutritional needs orally.
- EN is contraindicated for patients who have a nonfunctional or inaccessible GI tract.
- EN has several advantages over PN, such as lower cost, lower risk of infection, fewer metabolic complications, and preservation of gut integrity and immunity.
- EN also has some potential complications, such as aspiration, tube displacement or occlusion, diarrhea, nausea, vomiting, abdominal distension or cramping, electrolyte imbalance, dehydration, etc.
- EN formulas vary in their composition, osmolality, caloric density, fiber content, and protein quality. They can be classified into standard or polymeric formulas, hydrolyzed or elemental formulas, disease-specific formulas, and modular formulas.
- EN can be delivered through different routes depending on the patient’s condition, anatomy, and expected duration of therapy. They can be classified into gastric routes and intestinal routes.
- EN can be administered by different methods depending on the patient’s tolerance, nutritional needs, and type and location of the tube. They can be classified into bolus method, intermittent method, continuous method, and cyclic method.
- EN requires careful nursing interventions to ensure safe and effective delivery of nutrition and prevention of complications. Nursing interventions for EN can be divided into initiation phase, maintenance phase, and termination phase.
- EN may encounter some problems that require prompt identification and intervention to prevent serious complications. Some of the common problems and solutions are aspiration, tube displacement or occlusion, and diarrhea.
- EN requires regular evaluation and monitoring of the patient’s condition, response, and outcomes to determine the effectiveness and appropriateness of the therapy.
Mobility devices: crutches, canes, continuous passive ROM machine
- Mobility devices are assistive devices that help patients with impaired mobility to move around independently or with minimal assistance. They include crutches, canes, walkers, wheelchairs, scooters, and continuous passive ROM (range of motion) machines. Mobility devices can improve the quality of life, functional status, and psychological well-being of patients with mobility impairments. They can also prevent complications such as pressure ulcers, contractures, muscle atrophy, venous stasis, and respiratory infections.
- Mobility devices are prescribed by a physician or a physical therapist based on the patient’s condition, needs, goals, and preferences. The type and size of the device should be appropriate for the patient’s height, weight, strength, balance, coordination, and comfort. The device should also be compatible with the patient’s environment and lifestyle.
- The nurse plays an important role in assessing the patient’s mobility status, teaching the patient how to use the device correctly and safely, monitoring the patient’s progress and response to the device, and preventing or managing any complications or problems related to the device.
Crutches

- Crutches are devices that transfer weight from the legs to the upper body. They are used by patients who have weakness, injury, or surgery on one or both lower extremities. Crutches can be made of wood or metal and have three parts: a handgrip, an axillary bar, and a tip. There are different types of crutches such as axillary crutches, forearm crutches, platform crutches, and strutter crutches.
- The nurse should measure the patient for crutches by following these steps:
- Have the patient stand upright with shoes on and arms at the sides.
- Place two fingers horizontally under the axilla and measure from this point to a point 6 inches lateral to the heel of the foot. This is the length of the crutch.
- Adjust the handgrip so that it is level with the patient’s wrist when the elbow is flexed at 30 degrees.
- Check that there is a 2-inch space between the top of the crutch and the axilla when the patient stands upright with shoulders relaxed.
- The nurse should teach the patient how to use crutches by following these steps:
- Instruct the patient to hold the crutches firmly by the handgrips and place them 6 inches in front and to the side of each foot.
- Teach the patient different gaits depending on their weight-bearing status. The most common gaits are:
- Four-point gait: The patient moves each leg alternately with each opposing crutch. This gait is used for partial weight-bearing on both legs.
- Three-point gait: The patient moves both crutches and then moves both legs simultaneously. This gait is used for non-weight-bearing on one leg.
- Two-point gait: The patient moves one crutch simultaneously with the opposite leg. This gait is used for partial weight-bearing on both legs.
- Swing-through gait: The patient moves both crutches forward together and then swings both legs forward past them. This gait is used for non-weight-bearing on both legs.
- Teach the patient how to sit down and stand up with crutches by following these steps:
- To sit down: Back up to a sturdy chair until it touches the back of your legs. Hold both crutches in one hand by their handgrips. Reach back with your other hand and grasp the armrest or seat of the chair. Lower yourself slowly into the chair while keeping your injured leg extended.
- To stand up: Move to the edge of your seat. Hold both crutches in one hand by their handgrips. Push yourself up with your other hand on the armrest or seat of your chair while keeping your injured leg extended. Balance yourself before putting your weight on your crutches.
- The nurse should monitor for complications such as nerve damage, skin breakdown, falls, or infection from using crutches. The nurse should also inspect the crutches regularly for wear and tear and replace them if needed.
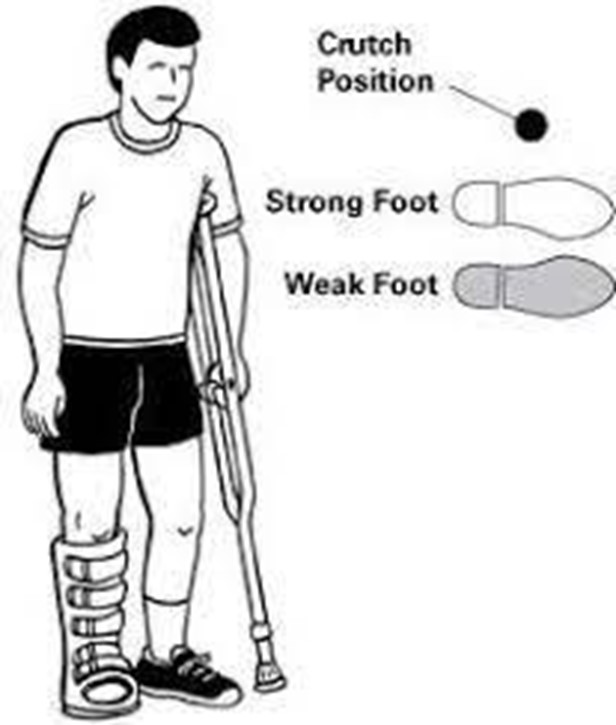
Canes

- Canes are devices that provide partial support to patients who have weakness or instability on one side of the body. They are used by patients who have arthritis, stroke, or injury on one lower extremity. Canes can be made of wood or metal and have a single tip, a tripod tip, or a quad tip. The most common type of cane is the single-tip cane.
- The nurse should measure the patient for a cane by following these steps:
- Have the patient stand upright with shoes on and arms at the sides.
- Adjust the height of the cane so that it is level with the patient’s wrist when the elbow is flexed at 30 degrees.
- Check that the patient can grip the handle comfortably and securely.
- The nurse should teach the patient how to use a cane by following these steps:
- Instruct the patient to hold the cane in the hand opposite to the affected leg.
- Teach the patient to move the cane forward about 6 inches and then move the affected leg forward to the level of the cane. Then move the unaffected leg past them.
- Teach the patient to use stairs with a cane by following these steps:
- To go up: Hold the cane in one hand and the handrail in the other. Step up with your unaffected leg first, then bring your affected leg and your cane up to the same step.
- To go down: Hold the cane in one hand and the handrail in the other. Step down with your affected leg and your cane first, then bring your unaffected leg down to the same step.
- The nurse should monitor for complications such as falls, muscle strain, joint pain, or infection from using a cane. The nurse should also inspect the cane regularly for wear and tear and replace it if needed.
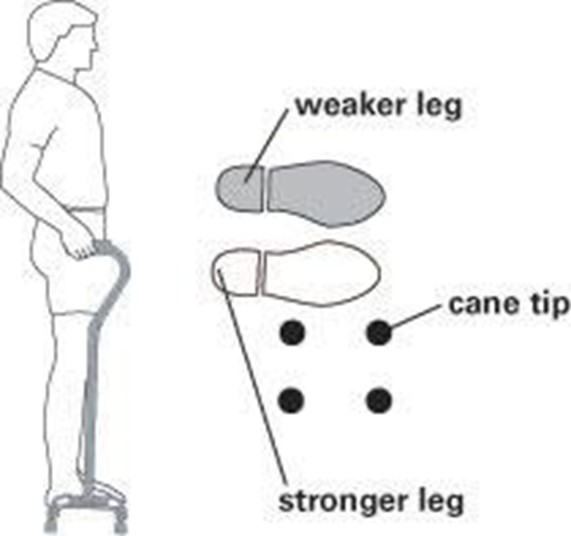
Conclusion
Mobility devices are important tools that can help patients with impaired mobility to improve their function, independence, and quality of life. The nurse has a key role in assessing, teaching, monitoring, and preventing complications related to mobility devices. The nurse should also collaborate with other health care professionals such as physicians, physical therapists, occupational therapists, and social workers to provide holistic care for patients who use mobility devices.
Bandaging

- Bandaging is the process of applying a material or device to a wound or injured body part to protect it from further damage, promote healing, prevent infection, control bleeding, reduce swelling, provide support, or immobilize the area.
- Bandages can be classified into two main categories: dressings and binders.
- Dressings are materials that are applied directly to the wound surface to absorb drainage, prevent contamination, and facilitate healing. They can be dry, moist, wet-to-dry, nonadherent, occlusive, or impregnated with substances such as antiseptics, antibiotics, or silver.
- Binders are materials that are wrapped around a body part to hold a dressing in place, provide compression, support a weak or injured area, or shape a body contour. They can be elastic, inelastic, tubular, triangular, or circular.
- Bandaging is an essential skill for nurses who care for patients with wounds or injuries. It requires knowledge of wound assessment, bandage selection, application techniques, monitoring methods, and patient education.
Types of Bandages
 - There are many types of bandages available for different purposes and situations. Some of the common ones are:
- There are many types of bandages available for different purposes and situations. Some of the common ones are:
- Gauze: A thin, woven fabric that is used to cover wounds or hold dressings in place. It can be sterile or nonsterile, plain or impregnated with substances such as petrolatum or zinc oxide. It can also be used to pack wounds or apply pressure to bleeding areas.
- Elastic: A stretchable fabric that is used to provide compression or support to a body part. It can be adhesive or nonadhesive, cohesive or noncohesive. It can also be used to reduce edema or prevent venous stasis.
- Muslin: A cotton fabric that is used to make straps or slings for traction or immobilization. It can also be used to shape body contours such as breasts or abdomen.
- Outing flannel: A soft fabric that is used to provide warmth and comfort to a body part. It can also be used to prevent skin irritation from other bandages.
- Tubular: A cylindrical fabric that is used to cover fingers, toes, arms, legs, or other tubular structures. It can be elastic or inelastic, knitted or woven. It can also be used to hold dressings in place or provide mild compression.
- Triangular: A triangular-shaped fabric that is used to make slings for arm injuries or splints for finger injuries. It can also be used to cover head wounds or apply pressure to bleeding areas.
- Circular: A circular-shaped fabric that is used to cover circular structures such as eyes, ears, nose, mouth, or anus. It can also be used to hold dressings in place or provide mild compression.
Indications
- Bandages are indicated for various reasons depending on the type of wound or injury and the desired outcome. Some of the common indications are:
- To protect the wound from contamination, trauma, or friction.
- To promote wound healing by creating a moist environment, removing necrotic tissue, delivering medications, or stimulating granulation tissue formation.
- To prevent wound infection by reducing bacterial load, preventing foreign bodies from entering the wound, or enhancing immune response.
- To control wound bleeding by applying direct pressure, elevating the injured area, or constricting blood vessels.
- To reduce wound edema by applying compression, elevating the injured area, or improving venous return.
- To provide wound support by stabilizing the wound edges, reducing tension on the wound, or preventing wound dehiscence or evisceration.
- To immobilize the injured area by restricting movement, maintaining alignment, or preventing further damage.
- To shape the body contour by applying pressure, molding the tissue, or correcting deformities.
Contraindications
- Bandages are contraindicated for some situations where they may cause harm or interfere with healing. Some of the common contraindications are:
- To cover wounds that are infected, gangrenous, or malodorous, as they may trap bacteria, toxins, or odors and worsen the condition.
- To apply compression to wounds that are ischemic, necrotic, or have impaired circulation, as they may compromise blood flow and oxygen delivery and increase tissue damage.
- To immobilize joints that are inflamed, infected, or have limited range of motion, as they may aggravate the inflammation, impair drainage, or cause joint stiffness.
- To shape body contours that are distorted by tumors, cysts, or masses, as they may compress the underlying structures and cause pain, obstruction, or rupture.
Complications
- Bandages can cause complications if they are applied incorrectly, inappropriately, or excessively. Some of the common complications are:
- Skin irritation or breakdown due to friction, pressure, moisture, or allergic reaction to the bandage material or substance.
- Wound infection due to contamination, poor aseptic technique, inadequate wound cleansing, or prolonged use of occlusive bandages.
- Wound dehiscence or evisceration due to excessive tension on the wound edges, inadequate wound support, or sudden movement or coughing.
- Circulation impairment due to tight bandaging, edema formation, arterial occlusion, or venous thrombosis. This can lead to pain, numbness, tingling, cyanosis, pallor, coldness, or pulselessness of the affected area.
- Nerve damage due to compression, stretching, or entrapment of the nerve by the bandage. This can lead to sensory loss, motor weakness, paralysis, or neuropathic pain of the affected area.
- Muscle atrophy or contracture due to prolonged immobilization, disuse, or lack of exercise of the affected area. This can lead to muscle wasting, weakness, stiffness, or deformity of the affected area.
Principles and Techniques
- Bandaging requires following some general principles and techniques to ensure its effectiveness and safety. Some of the general principles and techniques are:
- Assess the wound and the surrounding skin before applying a bandage. Check for signs of infection, bleeding, drainage, odor, pain, edema, color, temperature, sensation, and pulses of the affected area.
- Prepare the wound and the surrounding skin before applying a bandage. Cleanse the wound with normal saline or an appropriate solution. Debride any necrotic tissue if indicated. Apply an appropriate dressing to the wound surface. Protect the surrounding skin with a barrier cream or film if needed.
- Choose an appropriate bandage for the wound and the desired outcome. Consider the type, size, shape, location, depth, and condition of the wound. Consider the purpose, function, and duration of the bandage. Consider the patient’s preference, comfort, mobility, and ability to care for the bandage.
- Apply the bandage using proper techniques and precautions. Use aseptic technique if the wound is open or sterile. Use clean gloves and equipment if the wound is closed or clean. Start from the distal end of the body part and work proximally. Wrap the bandage evenly and smoothly without wrinkles or creases. Overlap each layer by one-half to two-thirds of its width. Secure the bandage with tape, clips, pins, ties, or velcro. Avoid applying too much pressure or tension on the bandage. Avoid covering bony prominences or joints with tape or adhesive. Avoid constricting blood vessels or nerves with tight bandaging. Leave some space for swelling or dressing changes if needed.
- Remove the bandage using proper techniques and precautions. Loosen and unwrap the bandage gently and slowly from proximal to distal end of the body part. Avoid pulling or tearing the bandage from the wound surface. Use scissors or a bandage remover to cut the bandage if it is stuck or adhered to the wound surface. Dispose of the used bandage in a biohazard bag or container.
- Document the bandaging process in the patient’s record. Include the date, time, type, size, and location of the bandage. Include the wound assessment, dressing type, and bandage application technique. Include the patient’s response, tolerance, and education. Include any problems, complications, or interventions related to the bandage.
- Monitor the bandage and the wound regularly and as ordered. Check for signs of infection, bleeding, drainage, odor, pain, edema, color, temperature, sensation, and pulses of the affected area. Check for signs of skin irritation or breakdown, wound dehiscence or evisceration, circulation impairment, nerve damage, muscle atrophy or contracture related to the bandage. Compare the findings with the baseline and previous assessments.
- Change the bandage and the dressing as needed and as ordered. Follow the same principles and techniques as for applying a new bandage. Consider the wound condition, healing stage, drainage amount, infection risk, and patient preference when changing the bandage and dressing. Use aseptic technique if the wound is open or sterile. Use clean technique if the wound is closed or clean.
- Educate the patient and family about bandage care. Teach them how to recognize and report signs of infection, bleeding, drainage, odor, pain, edema, color change, temperature change, sensation loss, pulse loss, skin irritation or breakdown, wound dehiscence or evisceration, circulation impairment, nerve damage, muscle atrophy or contracture related to the bandage. Teach them how to check and maintain the bandage and dressing. Teach them how to change the bandage and dressing if indicated. Teach them how to prevent complications related to the bandage. Teach them how to promote wound healing and prevent wound recurrence.
Demonstration
- The following are some examples of how to apply various bandages for different body parts and wound types :
- Gauze bandage for a hand wound: Wash your hands and put on gloves. Cleanse the wound with normal saline or an appropriate solution. Apply a nonadherent dressing to the wound surface. Cut a piece of gauze bandage about 2 inches longer than the hand. Wrap it around the hand starting from the wrist and moving toward the fingers. Overlap each layer by one-half to two-thirds of its width. Secure the end with tape or a clip. Check for circulation and sensation of the fingers.
- Elastic bandage for an ankle sprain: Wash your hands and put on gloves. Elevate the injured ankle above the heart level. Apply an ice pack to reduce swelling and pain. Cut a piece of elastic bandage about 4 inches longer than the ankle circumference. Wrap it around the ankle starting from the foot and moving toward the calf. Overlap each layer by one-half to two-thirds of its width. Secure the end with tape, a clip, or velcro. Check for circulation and sensation of the foot.
- Muslin bandage for a shoulder sling: Wash your hands and put on gloves. Fold a triangular-shaped muslin bandage in half along its longest side to form a right angle. Place it over the injured shoulder with one end hanging over the chest and the other end hanging over the back. Tie the ends together at the side of the neck opposite to the injured shoulder. Adjust the sling to support the arm at a right angle to the body. Check for circulation and sensation of the hand.
- Outing flannel bandage for an abdominal incision: Wash your hands and put on gloves. Cleanse the incision site with normal saline or an appropriate solution. Apply a nonadherent dressing to cover the incision site. Cut a piece of outing flannel bandage about 6 inches longer than the abdomen circumference. Wrap it around the abdomen starting from below the navel and moving upward. Overlap each layer by one-half to two-thirds of its width. Secure the end with tape, a clip, or velcro. Check for breathing comfort and incision integrity.
Conclusion
- Bandaging is an important skill for nurses who care for patients with wounds or injuries. It involves applying a material or device to a wound or injured body part to protect it from further damage, promote healing, prevent infection, control bleeding, reduce swelling, provide support, or immobilize the area.
- Bandages can be classified into two main categories: dressings and binders. Dressings are materials that are applied directly to the wound surface to absorb drainage, prevent contamination, and facilitate healing. Binders are materials that are wrapped around a body part to hold a dressing in place, provide compression, support a weak or injured area, or shape a body contour.
- Bandages are indicated for various reasons depending on the type of wound or injury and the desired outcome. Bandages are contraindicated for some situations where they may cause harm or interfere with healing. Bandages can cause complications if they are applied incorrectly, inappropriately, or excessively.
- Bandaging requires following some general principles and techniques to ensure its effectiveness and safety. Bandaging also requires regular monitoring, changing, and documenting of the bandage and the wound. Bandaging also requires educating the patient and family about bandage care.
Summary
- Bandaging is the process of applying a material or device to a wound or injured body part for various purposes.
Bandages can be dressings or binders depending on their function and location.
- Bandages have indications, contraindications, and complications that need to be considered before applying them.
- Bandaging involves assessing, preparing, choosing, applying, removing, documenting, monitoring, changing, and educating about the bandage and the wound.
- Bandaging requires proper techniques and precautions to ensure its effectiveness and safety.
IV insertion

- Intravenous (IV) therapy is the delivery of liquid substances directly into a vein.
- IV therapy may be used for various purposes, such as:
- Correcting electrolyte abnormalities
- Delivering medications
- Administering blood products
- Fluid replacement
- Specialized medication such as chemotherapy
- Nutrition
- Dialysis
- Hemodynamic monitoring
- IV therapy requires surgical asepsis, which is the elimination of all microorganisms from an object or area.
- IV therapy involves various types of IV access, materials, sites, complications, and nursing interventions.
Types of IV Access
- There are two main types of IV access: peripheral and central.
Peripheral IV Access
- Peripheral IV access involves inserting a catheter into a vein in the hand or arm.
- Peripheral IV access is suitable for short-term therapy (less than a week) and low-risk fluids or medications.
- Peripheral IV access may also be used for specialized placement in the external jugular vein or the dorsal foot vein.
- Peripheral IV access requires a tourniquet to constrict the vein and make it more visible and palpable.
- Peripheral IV access uses angiocatheters that range from 14 to 24 gauge in size. The gauge refers to the diameter of the catheter; the larger the gauge, the smaller the diameter. The choice of gauge depends on the type and viscosity of the fluid or medication, the size and condition of the vein, and the duration of therapy.
- Peripheral IV access may cause complications such as infiltration, phlebitis, infection, hematoma, nerve damage, or extravasation.
Central IV Access
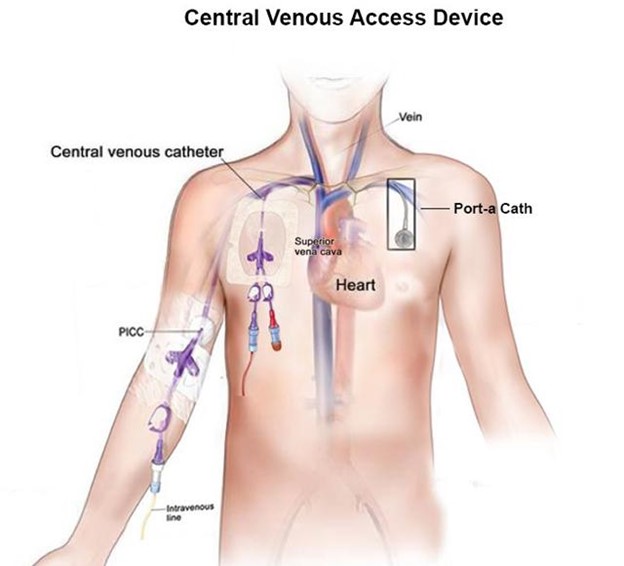
- Central IV access involves inserting a catheter into a large vein that leads directly to the heart.
- Central IV access is suitable for long-term therapy (more than a week) and high-risk fluids or medications that require rapid dilution or precise infusion rates.
- Central IV access may be achieved through percutaneous central lines, peripherally inserted central catheters (PICCs), tunneled catheters, or implanted ports.
- Central IV access does not require a tourniquet but may require ultrasound guidance or fluoroscopy to locate the vein and confirm placement.
- Central IV access uses catheters that range from 16 to 24 gauge in size. The choice of gauge depends on the type and volume of fluid or medication, the number of lumens (channels) needed, and the patient’s condition.
- Central IV access may cause complications such as pneumothorax, hemothorax, air embolism, infection, thrombosis, or catheter malposition.
Vein Anatomy
- Veins are blood vessels that carry blood back to the heart. Veins are unlike arteries in that they are:
- Superficial: they lie close to the skin surface and can be seen as dark red lines
- Non-pulsatile: they do not have a rhythmic contraction that can be felt
- Valved: they have one-way valves that prevent backflow of blood
- Veins have three layers of tissue:
- Tunica adventitia: the outermost layer that provides support and protection
- Tunica media: the middle layer that contains smooth muscle and elastic fibers
- Tunica intima: the innermost layer that lines the lumen (space) of the vein and prevents clotting
IV Materials
- The materials needed for starting a peripheral IV include:
- Absorbent disposable sheet (chuck or towel) to protect the bed or surface from spills
- Aseptic cleansers such as chlorhexidine, alcohol, or betadine to disinfect the skin
- Tourniquet to apply pressure and constrict the vein
- Angiocatheter of appropriate size and gauge to insert into the vein
- IV fluid or saline lock to connect to the catheter and maintain patency
- Saline-filled syringe to flush the catheter and check for blood return
- OpSite or prepared tape strips to secure and cover the catheter and site
- Gloves to protect the nurse and the patient from contamination
- Gauze (several pieces of 4x4 or 2x2) to apply pressure and stop bleeding
IV Sites
- The choice of IV site depends on several factors, such as:
- The type and duration of therapy
- The size and condition of the vein
- The patient’s preference and comfort
- The patient’s medical history and current status
- The potential for complications or interference
- Some general guidelines for choosing an IV site are:
- Go by “feel”, not by sight. Palpate the vein for “bounce” or resilience.
- Use warm compresses and allow the arm to hang dependently to fill the veins.
- Apply the tourniquet 10 mmHg below the known systolic pressure. Arterial flow continues with maximum venous constriction.
- Avoid areas of joint flexion, such as the wrist or antecubital fossa, as they may cause kinking or dislodgement of the catheter.
- Start distally and use the shortest length/smallest gauge access device that will properly administer the prescribed therapy.
- Rotate sites every 72 to 96 hours or as needed to prevent complications.
- Avoid veins that are sclerosed, thrombosed, inflamed, infected, or injured.
- Some common peripheral IV sites are:
- Cephalic vein: located on the lateral side of the arm, near the thumb. It is large and easy to access but may be more painful.
- Basilic vein: located on the medial side of the arm, near the pinky finger. It is large and easy to access but may be more prone to infiltration or nerve damage.
- Median cubital vein: located in the antecubital fossa, between the cephalic and basilic veins. It is large and easy to access but may be more affected by joint flexion or movement.
- Dorsal metacarpal veins: located on the back of the hand, between the knuckles. They are small and superficial but may be more comfortable and less likely to interfere with activities.
Steps for Peripheral IV Catheter Insertion
- The steps for inserting a peripheral IV catheter are:
- Verify the order for IV therapy and gather all the necessary materials.
- Identify the patient using two identifiers and explain the procedure, purpose, and potential risks. Obtain informed consent if required.
- Perform hand hygiene and don gloves.
- Select an appropriate IV site and apply a tourniquet about 4 inches above it. Assess for a suitable vein by palpating for bounce and observing for color and size.
- Cleanse the site with an aseptic cleanser using a circular motion from the center outward. Allow it to dry completely.
- Remove the cap from the angiocatheter and hold it like a pencil with your dominant hand. Stabilize the vein with your non-dominant hand by pulling the skin taut below the site.
- Insert the needle into the vein at a 10 to 30 degree angle, with the bevel up. Advance it until you see a flash of blood in the chamber.
- Lower the angle of the needle and advance it slightly further into the vein. Slide the catheter off the needle and into the vein until only the hub is visible.
- Release the tourniquet and activate the safety mechanism on the needle. Dispose of it in a sharps container.
- Attach the IV fluid or saline lock to the hub of the catheter. Flush it with saline using a syringe and check for blood return and signs of infiltration or phlebitis.
- Stabilize and secure the catheter with Opsite or tape strips. Cover it with an occlusive dressing that allows visualization of the site.
- Label the dressing with your initials, date, time, gauge, and lot number of the catheter.
- 13. Adjust the infusion rate according to the order and monitor the patient for any adverse reactions or complications.
- Document the procedure, the site, the type and amount of fluid or medication, the infusion rate, the patient’s response, and any interventions or outcomes.
Nursing Interventions for IV Therapy
- Nursing interventions for IV therapy are the actions that nurses take to ensure the safety and effectiveness of IV therapy. Some of the nursing interventions for IV therapy are:
- Pre-IV Therapy Interventions
- Verify the order for IV therapy and gather all the necessary materials.
- Identify the patient using two identifiers and explain the procedure, purpose, and potential risks. Obtain informed consent if required.
- Perform hand hygiene and don gloves.
- Select an appropriate IV site and apply a tourniquet about 4 inches above it. Assess for a suitable vein by palpating for bounce and observing for color and size.
- Cleanse the site with an aseptic cleanser using a circular motion from the center outward. Allow it to dry completely.
- Intra-IV Therapy Interventions
- Insert the needle into the vein at a 10 to 30-degree angle, with the bevel up. Advance it until you see a flash of blood in the chamber.
- Lower the angle of the needle and advance it slightly further into the vein. Slide the catheter off the needle and into the vein until only the hub is visible.
- Release the tourniquet and activate the safety mechanism on the needle. Dispose of it in a sharps container.
- Attach the IV fluid or saline lock to the hub of the catheter. Flush it with saline using a syringe and check for blood return and signs of infiltration or phlebitis.
- Stabilize and secure the catheter with Opsite or tape strips. Cover it with an occlusive dressing that allows visualization of the site.
Label the dressing with your initials, date, time, gauge, and lot number of the catheter.
Adjust the infusion rate according to the order and monitor the patient for any adverse reactions or complications.
- Post-IV Therapy Interventions
Discontinue the IV when ordered or indicated by removing the dressing, the catheter, and applying pressure to the site with gauze.
Inspect the catheter tip for intactness and report any missing fragments.
Apply a sterile dressing to the site and observe for bleeding or hematoma.
Document the procedure, the site, the type and amount of fluid or medication, the infusion rate, the patient’s response, and any interventions or outcomes.
Complications of IV Therapy and Nursing Management
- Complications of IV therapy are problems that may arise from inserting, maintaining, or removing an IV catheter or administering IV fluids or medications. Some of the possible complications of IV therapy and their nursing management are:
Infiltration
- Infiltration is the leakage of fluid or medication into the surrounding tissue due to dislodgement or puncture of the vein by the catheter. Signs and symptoms of infiltration include:
- Swelling, pallor, coolness, or pain at or near the insertion site
- Decreased or stopped flow rate
- Absence of blood return
- Edema or tightness of skin
- Blanching or blisters
- Nursing management for infiltration includes:
- Stop the infusion immediately and disconnect the tubing from the catheter.
- Remove the catheter gently and apply pressure to the site with gauze until the bleeding stops.
- Elevate the affected extremity above heart level to reduce swelling.
- Apply a warm or cold compress depending on the type of fluid infiltrated.
- Start a new IV line in another site, preferably on another extremity.
- Document the incident, the actions taken, and the patient’s response.
Phlebitis

- Phlebitis is the inflammation of a vein due to mechanical, chemical, or bacterial irritation from the catheter or fluid. Signs and symptoms of phlebitis include:
- Redness, warmth, tenderness, or pain along the course of the vein
- Swelling or induration at or near the insertion site
- Palpable cord along the vein
- Fever or chills
- Purulent drainage from the site
- Nursing management for phlebitis includes:
- Stop the infusion immediately and disconnect the tubing from the catheter.
- Remove the catheter gently and apply pressure to the site with gauze until bleeding stops.
- Apply a warm compress to the affected area to relieve pain and inflammation.
- Start a new IV line in another site, preferably on another extremity.
- Culture the catheter tip and the site if infection is suspected.
- Administer antibiotics, analgesics, or anti-inflammatory agents as ordered.
- Document the incident, the actions taken, and the patient’s response.
Infection
- Infection is the invasion of microorganisms into the bloodstream or the insertion site due to poor aseptic technique, prolonged use of the same catheter, or contamination of the fluid or equipment. Signs and symptoms of infection include:
- Fever, chills, malaise, or headache
- Redness, warmth, tenderness, or pain at or near the insertion site
- Purulent drainage from the site
- Swelling or induration at or near the insertion site
- Positive blood culture
- Nursing management for infection includes:
- Stop the infusion immediately and disconnect the tubing from the catheter.
- Remove the catheter gently and apply pressure to the site with gauze until bleeding stops.
- Culture the catheter tip and the site to identify the causative organism.
- Start a new IV line in another site, preferably on another extremity.
- Administer antibiotics, antipyretics, or analgesics as ordered.
- Monitor the patient’s vital signs, white blood cell count, and temperature.
- Document the incident, the actions taken, and the patient’s response.
Hematoma
- Hematoma is the collection of blood in the tissue due to puncture of an artery or a vein by the needle or catheter. Signs and symptoms of hematoma include:
- Ecchymosis or bruising at or near the insertion site
- Swelling or bulging at or near the insertion site
- Pain or discomfort at or near the insertion site
- Difficulty advancing the catheter into the vein
- Arterial blood return instead of venous blood return
Nursing management for hematoma includes:
Stop the infusion immediately and disconnect the tubing from the catheter.
Remove the catheter gently and apply pressure to the site with gauze until bleeding stops.
Apply a cold compress to the affected area to reduce swelling and pain.
Elevate the affected extremity above heart level to reduce bleeding.
Start a new IV line in another site, preferably on another extremity.
Document the incident, the actions taken, and the patient’s response.
Nerve Damage
- Nerve damage is the injury to a nerve due to compression, stretching, or puncture by the needle or catheter. Signs and symptoms of nerve damage include:
- Numbness, tingling, or burning sensation at or near the insertion site
- Sharp pain radiating along the nerve pathway
- Weakness or paralysis of the affected extremity
- Difficulty moving or flexing the affected extremity
- Loss of sensation or function of the affected extremity
- Nursing management for nerve damage includes:
- Stop the infusion immediately and disconnect the tubing from the catheter.
- Remove the catheter gently and apply pressure to the site with gauze until bleeding stops.
- Assess the neurovascular status of the affected extremity by checking the pulse, the capillary refill, the sensation, and the movement.
- Notify the physician and report the findings and the incident.
- Administer analgesics, anti-inflammatory agents, or steroids as ordered.
- Refer the patient to a neurologist or a physical therapist as needed.
- Document the incident, the actions taken, and the patient’s response.
Extravasation
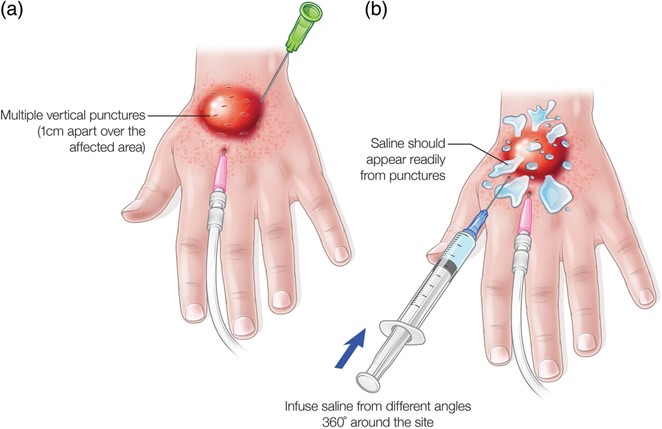
- Extravasation is the leakage of vesicant fluid or medication into the surrounding tissue due to dislodgement or puncture of the vein by the catheter. Vesicants are fluids or medications that can cause severe tissue damage such as necrosis, ulceration, or blistering if they escape from the vein. Examples of vesicants include chemotherapy agents, potassium chloride, calcium chloride, sodium bicarbonate, and phenytoin. Signs and symptoms of extravasation include:
- Swelling, redness, pain, burning, or stinging at or near the insertion site
- Decreased or stopped flow rate
- Absence of blood return
- Blistering, ulceration, necrosis, or sloughing of skin
- Tissue damage that may extend to tendons, nerves, muscles, or bones
- Nursing management for extravasation includes:
- Stop the infusion immediately and disconnect the tubing from the catheter.
- Remove the catheter gently and apply pressure to the site with gauze until the bleeding stops.
- Identify the type and amount of vesicant that extravasated.
- Notify the physician and report the findings and the incident.
Administer an antidote or a neutralizing agent as ordered. Some examples of antidotes or neutralizing agents are:
- Hyaluronidase: for phenytoin, norepinephrine, dopamine, or vinca alkaloids
- Sodium thiosulfate: for cisplatin
- Dimethyl sulfoxide (DMSO): for anthracyclines
- Nitroglycerin paste: for vasopressors
- Cold compress: for vinca alkaloids, etoposide, or mitomycin C
- Warm compress: for anthracyclines, mannitol, or calcium gluconate
Apply a sterile dressing to the site and monitor for signs of tissue damage.
Document the incident, the actions taken, and the patient’s response.
In summary, these are some of the main points from these notes:
- IV therapy is the delivery of liquid substances directly into a vein for various purposes.
- IV therapy requires surgical asepsis, which is the elimination of all microorganisms from an object or area.
- IV therapy involves various types of IV access, materials, sites, complications, and nursing interventions.
- Peripheral IV access involves inserting a catheter into a vein in the hand or arm. It is suitable for short-term therapy and low-risk fluids or medications.
- Central IV access involves inserting a catheter into a large vein that leads directly to the heart. It is suitable for long-term therapy and high-risk fluids or medications that require rapid dilution or precise infusion rates.
- Veins are blood vessels that carry blood back to the heart. They are superficial, non-pulsatile, and valved. They have three layers of tissue: tunica adventitia, tunica media, and tunica intima.
- The materials needed for starting a peripheral IV include an absorbent disposable sheet, an aseptic cleanser, a tourniquet, an angiocatheter, an IV fluid or saline lock, a saline-filled syringe, Opsite or tape strips, gloves, and gauze.
- The choice of IV site depends on several factors, such as the type and duration of therapy, the size and condition of the vein, the patient’s preference and comfort, the patient’s medical history and current status, and the potential for complications or interference.
- Some common peripheral IV sites are the cephalic vein, the basilic vein, the median cubital vein, and the dorsal metacarpal veins.
The steps for inserting a peripheral IV catheter are: verify the order; identify the patient; perform hand hygiene; select an appropriate site; apply a tourniquet; cleanse the site; insert the needle; advance the catheter; release the tourniquet; dispose of the needle; attach the fluid or saline lock; flush the catheter; stabilize and secure the catheter; label the dressing; adjust the infusion rate; and document the procedure.
- Nursing interventions for IV therapy are pre-, intra-, and post-IV therapy interventions that ensure the safety and effectiveness of IV therapy.
Some possible complications of IV therapy are infiltration, phlebitis, infection, hematoma, nerve damage, and extravasation .
Nursing management for each complication involves stopping the infusion; removing the catheter; applying pressure, a compress, or an antidote to the site; starting a new IV line; notifying the physician; administering medications; monitoring the patient; and documenting the incident .
- Documentation of IV therapy is the recording of all the relevant information about the IV therapy in the patient’s medical record. It is important for communication, evaluation, legal evidence, and quality and safety standards.
Documentation of IV Therapy
- Documentation of IV therapy is the recording of all the relevant information about the IV therapy in the patient’s medical record. Documentation of IV therapy is important for:
- Communicating with other healthcare providers
- Evaluating the effectiveness and outcomes of IV therapy
- Providing legal evidence of care
- Ensuring quality and safety standards
- Some of the information that should be documented for IV therapy are:
- The date and time of IV insertion, maintenance, or discontinuation
- The type, size, and lot number of the catheter
- The location and condition of the insertion site
- The type, amount, and rate of fluid or medication infused
- The patient’s response to IV therapy, including vital signs, pain level, and comfort level
- Any complications or adverse reactions that occurred and how they were managed
- Any patient education or instructions given about IV therapy
Summary
- In summary, these are some of the main points from these notes:
- IV therapy is the delivery of liquid substances directly into a vein for various purposes.
- IV therapy requires surgical asepsis, which is the elimination of all microorganisms from an object or area.
- IV therapy involves various types of IV access, materials, sites, complications, and nursing interventions.
- Peripheral IV access involves inserting a catheter into a vein in the hand or arm. It is suitable for short-term therapy and low-risk fluids or medications.
- Central IV access involves inserting a catheter into a large vein that leads directly to the heart. It is suitable for long-term therapy and high-risk fluids or medications that require rapid dilution or precise infusion rates.
- Veins are blood vessels that carry blood back to the heart. They are superficial, non-pulsatile, and valved. They have three layers of tissue: tunica adventitia, tunica media, and tunica intima.
- The materials needed for starting a peripheral IV include an absorbent disposable sheet, an aseptic cleanser, a tourniquet, an angiocatheter, an IV fluid or saline lock, a saline-filled syringe, Opsite or tape strips, gloves, and gauze.
- The choice of IV site depends on several factors, such as the type and duration of therapy, the size and condition of the vein, the patient’s preference and comfort, the patient’s medical history and current status, and the potential for complications or interference.
- Some common peripheral IV sites are the cephalic vein, the basilic vein, the median cubital vein, and the dorsal metacarpal veins.
- The steps for inserting a peripheral IV catheter are: verify the order; identify the patient; perform hand hygiene; select an appropriate site; apply a tourniquet; cleanse the site; insert the needle; advance the catheter; release the tourniquet; dispose of the needle; attach the fluid or saline lock; flush the catheter; stabilize and secure the catheter; label the dressing; adjust the infusion rate; and document the procedure.
- Nursing interventions for IV therapy are pre-, intra-, and post-IV therapy interventions that ensure the safety and effectiveness of IV therapy.
- Some possible complications of IV therapy are infiltration, phlebitis, infection, hematoma, nerve damage, and extravasation .
- Nursing management for each complication involves stopping the infusion; removing the catheter; applying pressure, a compress, or an antidote to the site; starting a new IV line; notifying the physician; administering medications; monitoring the patient; and documenting the incident .
- Documentation of IV therapy is the recording of all the relevant information about the IV therapy in the patient’s medical record. It is important for communication, evaluation, legal evidence, and quality and safety standards.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Medico-Surgical Procedures
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now



