Please set your exam date
Infection Control And Asepsis
Study Questions
Practice Exercise 1
A patient develops a urinary tract infection after an indwelling urinary catheter has been inserted. This would most accurately be termed as which type of infection?
Explanation
Healthcare-associated infections (HAIs), also known as nosocomial infections, are infections that patients acquire while receiving treatment for medical or surgical conditions.
Rationale for correct answer:
C. An iatrogenic infection includes infections from procedures, surgeries, or devices like urinary catheters. The UTI here is a direct consequence of catheter insertion, making it an iatrogenic infection.
Rationale for incorrect answers:
A. A viral infection describes infections caused by viruses (e.g., influenza, HIV, hepatitis). While UTIs can occasionally be viral, the majority-especially catheter-associated UTIs-are bacterial.
B. A chronic infection is one that persists over a long time (e.g., tuberculosis, hepatitis B). A catheter-associated UTI is typically acute and directly related to a procedure.
D. An opportunistic infection occurs when normal flora cause disease in immunocompromised hosts (e.g., HIV patients developing Pneumocystis pneumonia).
Take home points:
- A catheter-associated UTI is best classified as an iatrogenic infection because it results from a medical procedure.
- Proper aseptic technique and timely catheter removal are key nursing strategies to reduce the risk of iatrogenic infections.
Your patient has developed a low-grade fever and states that she has felt very tired lately. You interpret these findings as indicating which stage of infection?
Explanation
Infectious diseases typically follow a predictable course with defined stages. Understanding these stages-incubation, prodromal, illness, and convalescence-helps nurses anticipate signs and symptoms, implement timely interventions, and educate patients appropriately.
Rationale for correct answer:
B. Prodromal stage: This is the stage where nonspecific symptoms begin to appear-such as low-grade fever, fatigue, or general malaise. These symptoms signal that the body is starting to respond to the infection, but the illness has not yet fully developed.
Rationale for incorrect answers:
A. Incubation period: This is the time between exposure to the pathogen and the onset of symptoms. During this stage, the patient does not feel sick and shows no outward signs of illness. Pathogens are multiplying silently.
C. Full stage of illness: At this stage, the person experiences characteristic symptoms specific to the disease (e.g., high fever, rash, diarrhea). This does not match the vague, mild symptoms in the question.
D. Convalescent period: This is the recovery stage after the illness has peaked. Symptoms begin to resolve, and the body gradually returns to normal. Fatigue may linger, but fever typically subsides.
Take home points:
- The prodromal stage is marked by vague symptoms like fatigue and low-grade fever.
- Recognizing infection stages helps with early intervention and containment.
What type of transmission occurs when an intermediate carrier, such as a flea or mosquito, transfers an organism?
Explanation
Infectious agents can be transmitted through several routes, including direct contact, vehicles (like contaminated food or water), airborne particles, and living carriers known as vectors.
Rationale for correct answer:
A. Vector-borne transmission occurs when a living organism, usually an arthropod such as a mosquito, flea, or tick, carries and transmits pathogens to humans. The vector plays an essential role in the life cycle of the infectious agent.
Rationale for incorrect answers:
B. Vehicle-borne transmission refers to the indirect spread of infection through a non-living medium, such as contaminated food, water, blood, or surfaces (fomites).
C. Contact transmission involves the direct or indirect transfer of pathogens from one person to another. Direct contact includes touching an infected person, while indirect contact may involve touching contaminated surfaces.
D. Airborne transmission occurs when small respiratory particles (droplet nuclei) carrying pathogens remain suspended in the air and are inhaled by others.
Take home points:
- Vector-borne transmission involves living organisms (e.g., mosquitoes, fleas) that spread infectious agents between hosts.
- Knowing the mode of transmission guides proper infection control.
What’s the name for a laboratory-verified infection that causes no signs or symptoms?
Explanation
Terminology matters in infection control-knowing the difference between colonization, subclinical, latent, and active infection helps guide clinical and public health decisions.
Rationale for correct answer:
B. Subclinical: A subclinical infection is one that is confirmed by laboratory testing but does not produce noticeable signs or symptoms in the patient. These infections can still cause immune responses and may be transmissible to others.
Rationale for incorrect answers:
A. Colonized: Colonization refers to the presence of microorganisms (such as bacteria) on or in a host without tissue invasion or immune response. The person may act as a carrier but not necessarily have a laboratory-verified infection, and it's not synonymous with subclinical infection.
C. Latent: A latent infection is when the microorganism is present in the body in an inactive state and not currently causing symptoms or detectable by routine testing. However, it can reactivate.
D. Dormant: "Dormant" is more of a descriptive term than a clinical diagnosis. It implies inactivity of the pathogen but lacks the specificity of "latent" or "subclinical." It is not commonly used as a formal classification in infection terminology.
Take home points:
- A subclinical infection is lab-confirmed but asymptomatic, meaning the patient may unknowingly harbor and potentially spread the disease.
Which of these statements are true regarding disinfection and cleaning? Select all that apply
Explanation
Cleaning physically removes dirt and organic material, while disinfection kills many or all pathogenic microorganisms on inanimate objects.
Rationale for correct answer:
A. Proper cleaning requires mechanical removal of all soil from an object or area: Mechanical removal (e.g., scrubbing with friction) is crucial to eliminate organic material that can shield microorganisms and interfere with the effectiveness of disinfectants.
B. Routine environmental cleaning is an example of medical asepsis: Medical asepsis refers to procedures that reduce and prevent the spread of microorganisms, and routine cleaning of surfaces and equipment is a primary example. It reduces the risk of cross-contamination and infection.
D. Cleaning in a direction from the least to the most contaminated area helps reduce infections: This is a key principle in both wound care and general cleaning. By moving from clean to dirty areas, you minimize the risk of introducing contaminants into cleaner regions, reducing the chance of infection.
Rationale for incorrect answers:
C. When cleaning a wound, wipe around the wound edge first and then clean inward toward the center of the wound. The correct technique is to clean from the least contaminated area (usually the center of the wound) to the most contaminated area (the outer edge), to prevent dragging microorganisms from dirty areas into cleaner ones.
E. Disinfecting and sterilizing medical devices and equipment involve the same procedures: Disinfection eliminates many pathogenic microorganisms but not necessarily all spores, while sterilization destroys all forms of microbial life, including spores.
Take home points:
- Effective cleaning is the foundation of infection control- mechanical removal of dirt is essential before disinfection.
- Always clean from least contaminated to most contaminated areas.
Practice Exercise 2
Which of the following lists the recommended sequence for removing soiled personal protective equipment when the nurse prepares to leave the patient’s room?
Explanation
To minimize the risk of self-contamination, especially when dealing with infectious agents, PPE must be removed in a specific sequence that reflects the degree of contamination.
Rationale for correct answer:
C. Gloves, goggles, gown, mask, and wash hands: This is the recommended sequence: Gloves first (most contaminated); Goggles or face shield next (close to the face, may be contaminated); Gown (front and sleeves are contaminated); Mask/respirator last (least contaminated). Hand hygiene at the end is essential to remove any microorganisms transferred during PPE removal.
Rationale for incorrect answers:
A. Gown, goggles, mask, gloves, and exit the room: Gloves should be removed first because they are the most contaminated. Removing the gown first could expose the hands and arms to infectious material.
B. Gloves, wash hands, remove gown, mask, and goggles: Washing hands is important, but it should occur after all PPE is removed. Hand hygiene is the final step to ensure all contaminants are removed after contact with PPE.
D. Goggles, mask, gloves, gown, and wash hands: Removing goggles or the mask before the gloves is unsafe. Gloves should come off first to prevent contaminating other PPE while handling them.
Take home points:
- Always remove gloves first when taking off PPE, as they are the most contaminated item and pose the highest risk of spreading pathogens.
- Hand hygiene is the final step after removing all PPE to eliminate any pathogens that may have been transferred during the removal process.
In addition to standard precautions, the nurse caring for a patient with rubella would plan to implement what type of precautions?
Explanation
Transmission-based precautions are additional safety measures used when a patient is known or suspected to have an infectious disease that can be spread in specific ways-airborne, droplet, or contact.
Rationale for correct answer:
A. Droplet precautions: Rubella is transmitted through respiratory droplets produced when an infected person coughs, sneezes, or talks. Droplet precautions include wearing a surgical mask within 3 feet of the patient and placing the patient in a private room, if possible.
Rationale for incorrect answers:
B. Airborne precautions are used for pathogens that remain suspended in the air (e.g., tuberculosis, measles [rubeola], and varicella).
C. Contact precautions are for diseases spread through direct touch or contaminated surfaces (e.g., MRSA, C. difficile, RSV).
D. Universal precautions are outdated and were replaced by Standard Precautions in CDC guidelines.
Take-home points:
- Rubella requires droplet precautions in addition to standard precautions to prevent respiratory transmission.
- Understanding the mode of transmission for specific infectious diseases is essential for selecting the correct level of isolation and protecting both patients and healthcare staff.
The CDC standard precaution recommendations apply to which of the following?
Explanation
Standard Precautions are the foundational infection control practices that are used for all patients, regardless of their diagnosis or presumed infection status. The principles are based on the assumption that any person’s blood, body fluids (except sweat), non-intact skin, and mucous membranes may harbor infectious pathogens.
Rationale for correct answer:
D. All patients receiving care in hospitals: Standard Precautions are applied to all patients, in all settings, at all times. This universal approach is key to infection prevention, especially when a patient's infectious status is unknown.
Rationale for incorrect answers:
A. Only patients with diagnosed infections: Standard Precautions are not limited to patients with known infections. Because some infections may be undiagnosed or asymptomatic.
B. Only blood and body fluids with visible blood: Standard Precautions apply to all body fluids (except sweat), not just those visibly contaminated with blood. Even fluids that appear clear or clean may carry infectious agents.
C. All body fluids including sweat: While most body fluids are included (e.g., blood, urine, feces, saliva, sputum, vomit), sweat is specifically excluded because it is not considered a significant source of infectious pathogens in routine care.
Take home points:
- Standard Precautions must be followed for all patients.
- Sweat is the only body fluid excluded from Standard Precautions because it does not pose a significant risk of pathogen transmission.
When caring for a patient with latex allergy, the nurse creates a latex-safe environment by doing which of the following?
Explanation
Latex allergy is a serious concern in healthcare environments, as exposure to latex-containing products can cause reactions ranging from mild skin irritation to life-threatening anaphylaxis.
Rationale for correct answer:
C. Using a latex-free pharmacy protocol: Ensuring that medications, IV tubing, and syringes are latex-free is crucial for a truly safe environment. Many medication vial stoppers, IV ports, and delivery devices may contain latex. A latex-free pharmacy protocol addresses hidden sources of latex and reduces the risk of exposure.
Rationale for incorrect answers:
A. Carefully cleaning the wall-mounted blood pressure device before using it: While cleaning equipment is always important, simply cleaning a wall-mounted device is not enough to ensure it is latex-free.
B. Donning latex gloves outside the room to limit powder dispersal: Latex gloves should never be used in the care of latex-sensitive patients, regardless of where they are donned. Powdered latex gloves can aerosolize allergens, increasing the risk of a reaction.
D. Placing the patient in a semiprivate room: Patients with latex allergies should be placed in private rooms if possible to minimize accidental exposure. Room-sharing increases the risk of cross-contamination from latex-containing products used for another patient.
Take home points:
- A latex-free pharmacy protocol is essential in preventing systemic exposure to latex through medication administration.
- Only latex-free gloves should be used to ensure a truly safe care environment.
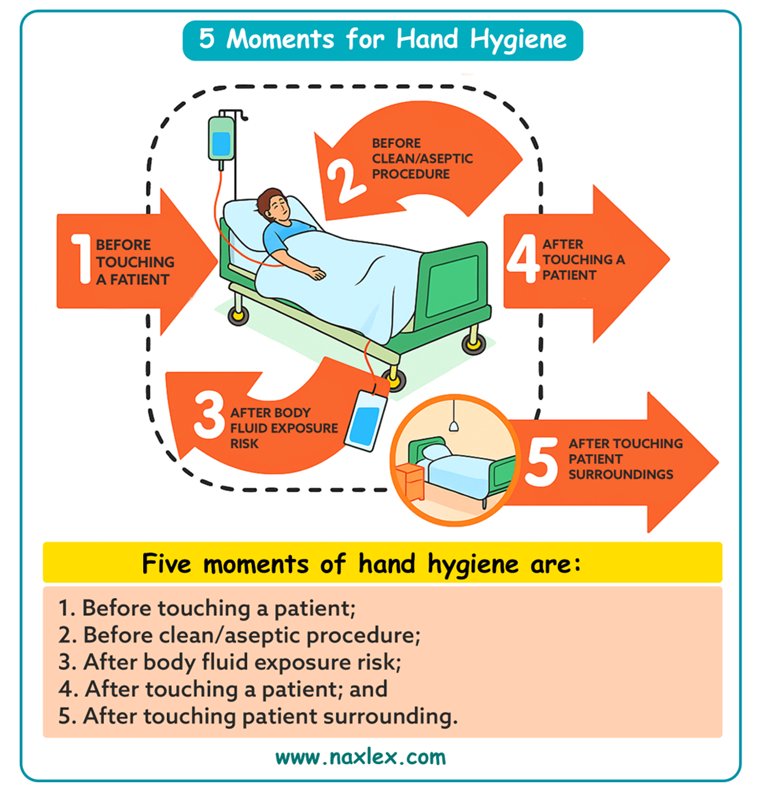
What’s the most effective method of infection control?
Explanation
Infection control is a critical component of safe nursing practice. Healthcare-associated infections (HAIs) significantly contribute to patient morbidity, mortality, and increased healthcare costs.
Rationale for correct answer:
B. Hand washing (or hand hygiene) is the most effective and evidence-based method of preventing the spread of infection. It reduces the transmission of pathogens from one patient or surface to another.
Rationale for incorrect answers:
A. Isolation precautions are used for patients with known or suspected infections to prevent spread. While highly effective in certain cases, they are not universally applicable and are only initiated after a pathogen is identified or suspected.
C. Neutropenic precautions are specialized measures used to protect immunocompromised patients (e.g., chemotherapy recipients) from infection.
D. Wearing sterile gloves: Sterile gloves are used during invasive procedures to protect patients from infection. However, they do not eliminate the need for hand hygiene, and misuse (e.g., touching surfaces with gloves) can still spread pathogens.
Take home points:
- Hand washing is the most effective and universal method of infection prevention.
- Other precautions are context-specific and important, but none replace the foundational role of proper hand hygiene.
Practice Exercise 3
Which organization(s) initially developed the guidelines for minimum protection standards for infection prevention and control?
Explanation
To ensure consistent and effective protective measures, national organizations develop guidelines that set minimum standards for infection control practices. Two key U.S. agencies-the CDC (Centers for Disease Control and Prevention) and OSHA (Occupational Safety and Health Administration)-play central roles in establishing and enforcing these guidelines.
Rationale for correct answer:
D. The CDC (Centers for Disease Control and Prevention): The CDC is the primary organization that developed the initial infection control guidelines, including standard precautions, transmission-based precautions, and hand hygiene in healthcare settings.
Rationale for incorrect answers:
A. OSHA (Occupational Safety and Health Administration): OSHA has issued and monitors regulations for use of infection control precautions in situations and settings in which exposure to blood and other infectious materials is possible.
B. Individual healthcare facilities: While hospitals and healthcare facilities develop internal policies and procedures, they do not initially develop national guidelines. They are required to follow and implement standards set by organizations such as the CDC and OSHA.
C. The state governing body: State health departments may enforce or adapt infection control standards based on federal guidelines, but they are not the originators of the core infection prevention guidelines.
Take home points:
- The CDC is the primary agency responsible for developing the initial evidence-based guidelines for infection prevention and control in healthcare settings.
- OSHA plays a complementary role by enforcing safety standards, particularly those that protect healthcare workers from occupational exposure to infectious agents.
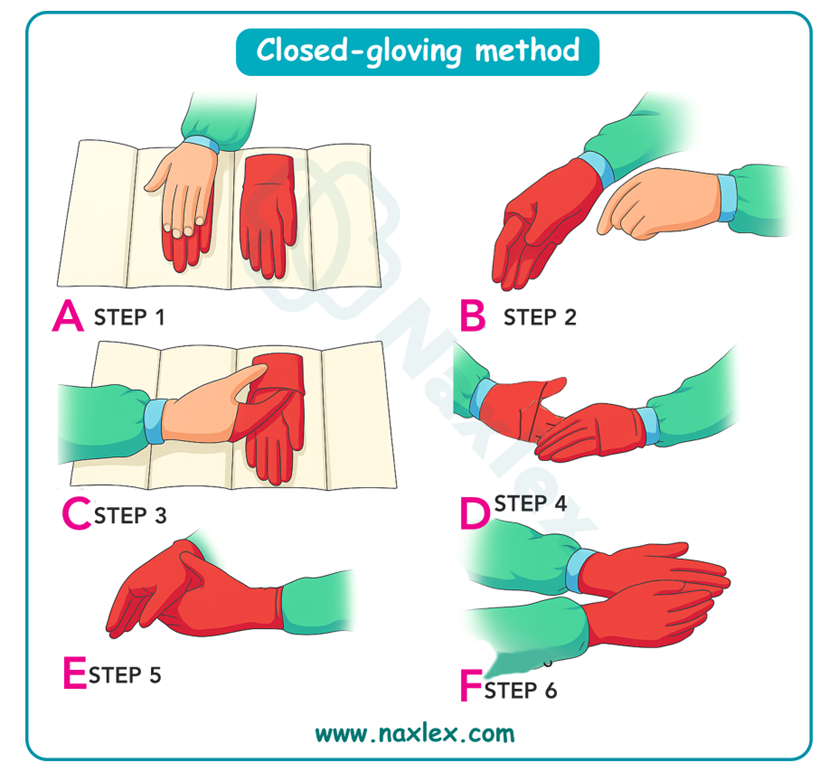
Which of the following actions by the nurse demonstrate the practice of core principles of surgical asepsis? Select all that apply
Explanation
Surgical asepsis, or sterile technique, is a fundamental principle in preventing infection during invasive procedures or when caring for clients with compromised immune systems.
Rationale for correct answer:
B. Keep the sterile field in view at all times: A sterile field must never be left unattended. If it is out of sight, sterility cannot be guaranteed, and the field is considered contaminated.
C. Consider the outer 2.5 cm (1 inch) of the sterile field as contaminated: The outer edge of a sterile drape or field is not considered sterile and is used for handling when positioning the field. This boundary helps prevent the accidental contamination of the true sterile zone.
Rationale for incorrect answer:
A. The front and sides of the sterile gown are considered sterile from the waist up: In surgical asepsis, the sterile area of a gown extends from the chest to the waist and from the sleeves (just above the elbow) to the cuff.
D. Only health care personnel within the sterile field must wear personal protective equipment: All health care personnel involved in sterile procedures must follow PPE protocols based on the situation, including masks, caps, and gowns, even if not within the sterile field.
E. After cleansing the hands with antiseptic rub, apply clean disposable gloves: For surgical asepsis, sterile gloves-not clean gloves-must be worn. After performing a surgical hand scrub or antiseptic rub, the nurse must don sterile gloves to maintain asepsis during sterile procedures.
Take home points:
- Maintaining visibility and boundaries of the sterile field is essential to surgical asepsis.
- Sterile gowns, gloves, and a clearly defined sterile field ensure patient safety during invasive procedures.
Which of the numbered areas is considered sterile on a person in the operating room? You may assume that all articles were sterile when applied.
Explanation
In surgical settings, maintaining a sterile field is essential to prevent surgical site infections and promote optimal outcomes. The sterile field includes areas and items that are free from microorganisms and must remain uncontaminated throughout the procedure.
Rationale for correct answer:
1. Sterile: This area includes the front of the surgeon's gown, from chest level to waist and from gloved hand to gloved hand (i.e., within the field of vision).
Rationale for incorrect answers:
2. Even though the mask is essential for infection control (to protect the surgical field from respiratory droplets), the mask itself is not considered a sterile part of the attire.
3. The part of the sleeve above the elbow is not considered sterile. Only the area of the sleeve from 2 inches above the elbow to the cuff is part of the sterile zone
4. This person is seated and charting, likely the circulating nurse or anesthetist, wearing only a mask and scrubs. They are not part of the sterile team and do not wear sterile gown/gloves.
5. Non-sterile: This part of the gown is the back of a sterile team member. The back of the gown is not visible to the wearer and is therefore not considered sterile.
Take home points:
- The sterile field is a visible, controlled space.
- Any area not in the wearer’s direct line of sight, or not specifically prepared for sterility (like masks or back of gowns), is considered non-sterile.
The nurse determines that a field remains sterile if which of the following conditions exist?
Explanation
Sterile technique, also known as surgical asepsis, is used to eliminate all microorganisms from an area or object to prevent infection during invasive procedures. A sterile field refers to a designated clean area where sterile supplies and instruments are placed and maintained during a procedure.
Rationale for correct answer:
C. Sterile items are 2 inches from the edge of the field: The outer 1-inch border of a sterile field is considered non-sterile. Placing sterile items at least 1 inch inward (in this case, 2 inches) ensures the items remain within the sterile zone.
Rationale for incorrect answers:
A. Tips of wet forceps are held upward when held in ungloved hands: Wet forceps should be held tips down, not up, to prevent contaminated fluid from running down the handle and then back to the sterile tip (via gravity).
B. The field was set up 1 hour before the procedure: A sterile field should never be left unattended or set up far in advance. Airborne contaminants can settle over time. Sterile fields are typically considered unsterile if left exposed for long periods, especially more than 30 minutes.
D. The nurse reaches over the field rather than around the edges: Reaching over a sterile field risks contaminating it through falling skin cells, droplets, or contact from sleeves. The nurse should always move around the sterile field to maintain its integrity.
Take home points:
- Reaching over, leaving the field unattended, or improper handling of sterile instruments can compromise the entire sterile setup and increase infection risk.
- Sterile items must be placed at least 1 inch inside the border of the sterile field to ensure they are not contaminated by the edges.
While applying sterile gloves (open method), the cuff of the first glove rolls under itself about 0.5 cm (1/4 in.). What is the best action for the nurse to take?
Explanation
The open method of sterile gloving is used during procedures requiring sterile technique, such as catheter insertion or sterile dressing changes. Maintaining sterility is crucial to prevent introducing pathogens into vulnerable areas, reducing the risk of infection.
Rationale for correct answer:
B. Wait until the second glove is in place and then unroll the cuff with the other sterile hand: Once both gloves are on, the nurse has two sterile hands and can gently adjust the rolled cuff without contaminating the sterile field. This maintains sterility while correcting the issue efficiently.
Rationale for incorrect answers:
A. Remove the glove and start over with a new pair: This action is necessary only if sterility has been compromised (e.g., glove touches a non-sterile surface). A minor roll at the cuff does not affect the sterility of the glove.
C. Ask a colleague to assist by unrolling the cuff: A non-sterile colleague touching the sterile glove would contaminate it. Even if gloved, unless the colleague is in sterile attire, this would break technique.
D. Leave the cuff rolled under: Leaving the cuff rolled can be uncomfortable and might hinder mobility or allow contamination if skin is exposed.
Take home points:
- Do not involve unsterile personnel or remove gloves unnecessarily unless sterility is compromised.
- Minor issues like rolled cuffs can be corrected safely with proper technique.
Comprehensive Questions
The client is a chronic carrier of infection. To prevent the spread of the infection to other clients or health care providers, the nurse emphasizes interventions that do which of the following?
Explanation
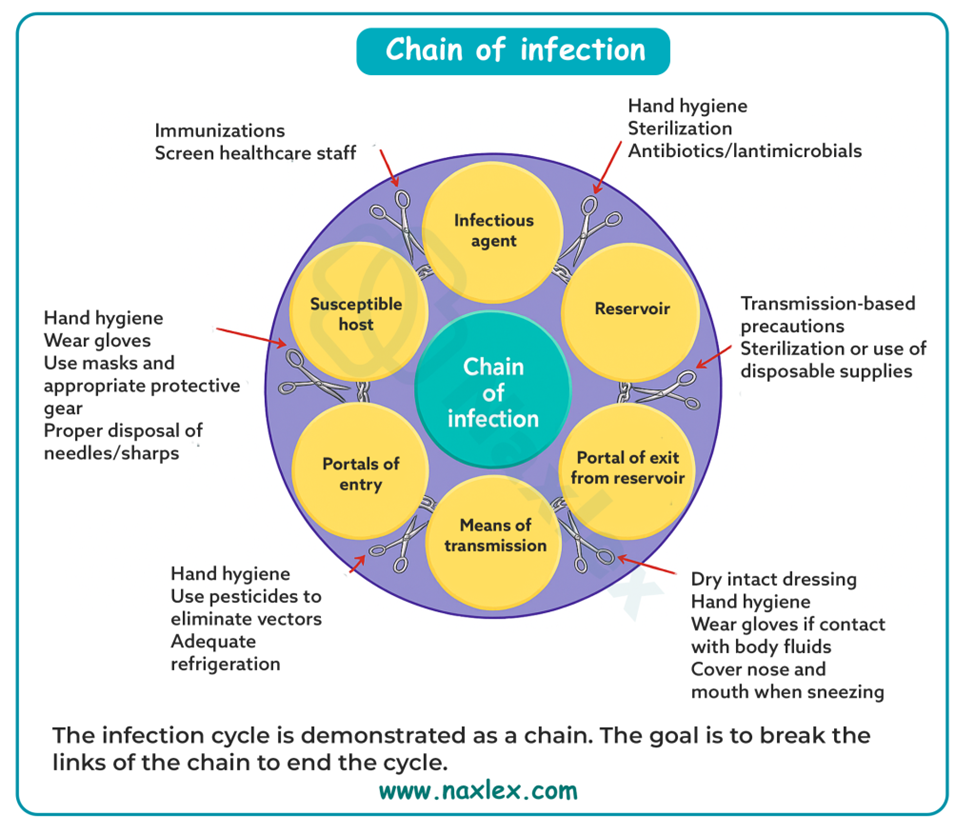
Preventing the spread of infection involves understanding and interrupting the chain of infection, which includes six links: the infectious agent, reservoir, portal of exit, mode of transmission, portal of entry, and susceptible host.
Rationale for correct answer:
B. Block the portal of exit from the reservoir: The most effective way to prevent transmission from a chronic carrier is by preventing the infectious agent from leaving the body. This includes using standard and transmission-based precautions.
Rationale for incorrect answers:
A. Eliminate the reservoir: While eliminating the reservoir (i.e., the source of infection) would be ideal, it is not always feasible in chronic carriers, as the host is the reservoir. Chronic carriers often cannot be cured completely, so this strategy is limited in practice.
C. Block the portal of entry into the host: This is a reactive measure focused on the next host, not the source, and does not address the spread from the chronic carrier.
D. Decrease the susceptibility of the host: Strengthening the immune system (e.g., through vaccination or proper nutrition) can help reduce a host’s risk of infection. However, this does not stop the chronic carrier from exposing others.
Take home points:
- Understanding the chain of infection helps nurses implement targeted interventions.
- When managing a client who is a chronic carrier, the most critical infection control strategy is to block the portal of exit to prevent the pathogen from reaching others.
Which is the most effective nursing action for preventing and controlling the spread of infection?
Explanation
Infection prevention and control are essential components of nursing practice that safeguard both clients and healthcare providers. In healthcare settings, infections can be transmitted through direct contact, droplets, airborne particles, or contaminated surfaces.
Rationale for correct answer:
A. Thorough hand hygiene: Hand hygiene removes or destroys transient microorganisms. It interrupts the chain of infection by removing transient microorganisms from the hands before they can be spread to others or enter the body through mucous membranes or broken skin.
Rationale for incorrect answers:
B. Wearing gloves and masks when providing direct client care: Gloves and masks provide a barrier to infectious agents. However, they are not substitutes for hand hygiene and may be misused or improperly removed, potentially increasing the risk of contamination.
C. Implementing appropriate isolation precautions: Isolation precautions (e.g., contact, droplet, airborne) help limit the transmission of specific pathogens. They are essential for infection control when a known pathogen exists.
D. Administering broad-spectrum prophylactic antibiotics: Antibiotics may be used in select cases (e.g., pre-op or immunocompromised clients), but overuse contributes to antimicrobial resistance and disrupts normal flora.
Take home points:
- Hand hygiene is the most effective and universally applicable infection control measure in nursing practice.
- It should be performed before and after client contact, after removing gloves, and after contact with bodily fluids or contaminated surfaces.
When caring for a single client during one shift, it is appropriate for the nurse to reuse only which of the following personal protective equipment?
Explanation
Correct use and reuse of PPE depends on the type of equipment, the level of contamination, and the nature of patient care. In some situations, certain PPE items may be reused for the same client during a single shift-but only if not visibly soiled, damaged, or contaminated.
Rationale for correct answer:
A. Goggles provide eye protection and are typically made of durable materials that can withstand cleaning and disinfection. When used for the same client, they may be reused during a shift as long as they are not visibly soiled or contaminated.
Rationale for incorrect answers:
B. Gowns, especially disposable ones, are single-use and should be removed after each client contact. Even with the same client, gowns can become contaminated with body fluids, increasing the risk of cross-contamination to the environment or nurse.
C. Surgical masks are single-use items. Prolonged use can lead to moisture buildup, reducing effectiveness. Masks should be discarded after removal or if they become damp or contaminated.
D. Clean gloves must be changed between tasks and after contact with potentially infectious material, even when caring for the same client. Reusing gloves increases the risk of spreading pathogens between clean and contaminated body sites.
Take home points:
- Goggles are the only PPE in this list that can be safely reused for the same client during a shift.
- Gloves, gowns, and surgical masks are considered single-use and should never be reused due to the high risk of cross-contamination.
In caring for a client on contact precautions for a draining infected foot ulcer, which action should the nurse perform?
Explanation
Contact precautions are used when caring for clients with infections that can be transmitted by direct or indirect contact with infectious material, such as wound drainage, feces, or contaminated surfaces.
Rationale for correct answer:
C. Follow standard precautions in all interactions with the client: Standard precautions (e.g., hand hygiene, glove use, avoiding contact with body fluids) are applied to all clients regardless of infection status, and they form the foundation of contact precautions.
Rationale for incorrect answers:
A. Wear a mask during dressing changes: Masks are not routinely required for contact precautions unless there is a risk of splashes or if the infection is also droplet or airborne in nature.
B. Provide disposable meal trays and silverware: This is unnecessary for contact precautions unless the client is also under enteric precautions (e.g., C. difficile) or severely immunocompromised.
D. Use surgical aseptic technique for all direct contact with the client: Surgical aseptic (sterile) technique is reserved for invasive procedures (e.g., catheter insertion, central line dressing changes), not general client interactions.
Take home points:
- Standard precautions are the baseline infection control practices applied to all clients and are always used.
- Contact precautions specifically focus on preventing transmission via direct or indirect contact.
The nurse evaluates the chart of a 65-year-old client with no apparent risk factors and concludes that which immunizations are current? Select all that apply
Explanation
Immunization in older adults is a key preventive strategy to reduce morbidity and mortality from vaccine-preventable diseases. For adults 65 years and older without specific risk factors, ensuring up-to-date status on influenza, tetanus, and zoster vaccines is crucial.
Rationale for correct answer:
B. Receives a flu shot every year: Annual influenza vaccination is strongly recommended for all individuals aged 6 months and older, and especially for adults over 65, due to higher risk of severe complications.
C. Has not received the hepatitis B vaccine: Hepatitis B vaccination is not routinely indicated for adults unless they are in a high-risk group (e.g., healthcare workers, IV drug users, diabetics under 60). This client has no risk factors, so it's not required.
D. Has not received the hepatitis A vaccine: Hepatitis A vaccine is given to those at increased risk (e.g., travelers to endemic areas, people with chronic liver disease, drug users). It's not a routine vaccine for healthy older adults with no risk.
Rationale for incorrect answers:
A. Last tetanus booster was at age 50: Tetanus boosters (Td or Tdap) are recommended every 10 years. Since the client received the last booster at age 50, another is due by age 60.
E. Has not received the herpes zoster vaccine: The Shingrix vaccine (2 doses, 2–6 months apart) is recommended for all adults aged 50 and above, regardless of prior shingles history. The absence of this vaccine means the client is not current.
Take home points:
Adults aged 65 and above should receive:
- the annual flu vaccine
- stay up-to-date on tetanus boosters (every 10 years)
- receive the shingles vaccine even if they’ve had shingles before.
After teaching a client and family strategies to prevent infection, which statement by the client would indicate effective learning has occurred?
Explanation
Preventing infection at home is a vital aspect of client and family education, especially for those recovering from illness, surgery, or living with compromised immune systems. Effective infection prevention involves proper hand hygiene, safe food handling, wound care, and avoiding the sharing of personal items.
Rationale for correct answer:
B. “We must wash or peel all raw fruits and vegetables before eating.” Raw fruits and vegetables can carry pathogens from soil, water, or handling. Washing or peeling them reduces the risk of foodborne illness, especially for those with weakened immunity.
Rationale for incorrect answers:
A. “We will use antimicrobial soap and hot water to wash our hands at least three times per day.” While hand hygiene is crucial, antimicrobial soap is not necessary and may contribute to skin irritation and antimicrobial resistance. Also, washing only three times per day is inadequate.
C. “A wound or sore is not infected unless we see it draining pus.” Infection may be present before pus appears. Early signs include redness, warmth, swelling, and pain. Waiting for pus means missing early intervention.
D. “We should not share toothbrushes but it is OK to share towels and washcloths.” While not sharing toothbrushes is correct, towels and washcloths can also harbor bacteria, viruses, and fungi. Sharing them increases the risk of skin infections or cross-contamination.
Take home points:
- Clients and families must understand that signs of infection can be subtle.
- Early preventive practices-like frequent handwashing and avoiding shared personal items-are more protective than reactive behaviors.
A patient who has been placed on contact precautions for Clostridium difficile (C. difficile) asks you to explain what he should know about this organism. Which statements made by the patient show an understanding of the patient teaching? Select all that apply
Explanation
Clostridium difficile (C. difficile) is a spore-forming, toxin-producing bacterium that causes severe diarrhea and colitis, often following antibiotic use. It is a major cause of healthcare-associated infections (HAIs) and is highly contagious through the fecal-oral route.
Rationale for correct answer:
A. “The organism is usually transmitted through the fecal-oral route.” C. difficile spreads when spores from feces are ingested, often via contaminated hands or surfaces. This statement shows an accurate understanding of the mode of transmission.
B. “Hands should always be cleaned with soap and water rather than the alcohol-based hand sanitizer.” Alcohol-based hand sanitizers are ineffective against C. difficile spores. Proper hand hygiene with soap and water is essential to physically remove the spores.
C. “Everyone coming into the room must wear a gown and gloves.” Contact Precautions for C. difficile require gloves and gowns to prevent contamination of clothing and skin with spores.
Rationale for incorrect answers:
D. “While I am in Contact Precautions, I cannot leave the room.” Patients on Contact precautions can leave the room for medically necessary procedures if they follow precautions (e.g., wearing a clean gown, hand hygiene).
E. “C. difficile dies quickly once outside the body.” C. difficile spores are very hardy and can survive on surfaces for weeks to months if not properly disinfected with sporicidal agents.
Take home points:
- C. difficile spreads through the fecal-oral route.
- C. difficile spores are resistant to alcohol-based hand sanitizers and many disinfectants.
- Thorough cleaning with sporicidal disinfectants is necessary.
A patient is diagnosed with meningitis. Which type of isolation precaution is most appropriate for this patient?
Explanation
Meningitis is an inflammation of the meninges that can be caused by various infectious agents, including bacteria and viruses. When caused by organisms like Neisseria meningitidis, it is highly contagious and can spread via respiratory droplets.
Rationale for correct answer:
B. Droplet Precautions: Bacterial meningitis (e.g., meningococcal) spreads through respiratory droplets, especially in the early stages of illness. Droplet precautions involve wearing a surgical mask when within 3 feet of the patient and isolating the patient in a private room.
Rationale for incorrect answers:
A. Reverse isolation (also known as protective isolation) is used to protect immunocompromised patients from external pathogens, not to prevent the spread of infection from the patient.
C. While standard precautions (e.g., hand hygiene, gloves) are always used, they are not sufficient alone for clients with droplet-spread infections like meningitis. Additional droplet precautions are required to reduce the risk of respiratory transmission.
D. Contact precautions are used for infections transmitted through direct or indirect contact with the patient or environment (e.g., C. difficile or MRSA). They are not appropriate for respiratory illnesses like meningitis.
Take home points:
- Clients with bacterial meningitis must be placed on droplet precautions.
- Understanding the transmission route of infections helps determine the right type of isolation precautions.
A patient is placed on airborne precautions for pulmonary tuberculosis. The nurse notes that the patient seems to be angry, but the nurse recognizes that this is a normal response to isolation. Which is the nurse’s best intervention?
Explanation
Patients placed under isolation precautions, such as for pulmonary tuberculosis (TB), may experience emotional distress, including anger, anxiety, loneliness, or depression. These feelings are often due to sensory deprivation, social isolation, and limited interaction with others.
Rationale for correct answer:
C. Explain the reasons for isolation procedures and provide meaningful stimulation: Helping the patient understand why isolation is necessary, reducing feelings of confusion and anger. Providing meaningful stimulation combats boredom and emotional distress while maintaining safety.
Rationale for incorrect answers:
A. Provide a dark, quiet room to calm the patient: While reducing environmental stimuli may help anxious patients, providing a dark, quiet room may actually worsen feelings of isolation, boredom, and depression.
B. Reduce the level of precautions to keep the patient from becoming angry: Reducing precautions due to the patient's emotional response puts others at risk of infection and is never an acceptable solution.
D. Limit family and other caregiver visits to reduce the risk of spreading the infection: While visitor precautions are important, completely limiting family and caregiver interactions can worsen the patient’s isolation.
Take home points:
- Maintaining engagement through meaningful activities can greatly improve cooperation and emotional well-being without compromising safety.
- These include: books, TV, music, virtual family contact.
Which type of personal protective equipment should the nurse wear when caring for a pediatric patient who is placed on airborne precautions for confirmed chickenpox/herpes zoster? Select all that apply
Explanation
Chickenpox is spread via airborne droplets and direct contact with vesicular fluid, which makes airborne and contact precautions necessary.
Rationale for correct answer:
A. Disposable gown is worn to prevent contact with lesions and contaminated surfaces. Though primarily used for contact precautions, varicella and disseminated herpes zoster require both airborne and contact precautions.
B. The N95 respirator mask provides high-level filtration, protecting the nurse from inhaling airborne particles.
E. Gloves are necessary because of contact precautions-direct contact with vesicle fluid or contaminated surfaces can lead to transmission. Gloves protect both the nurse and other clients.
Rationale for incorrect answers:
C. Face shield or goggles: Eye protection is not routinely required for chickenpox or herpes zoster unless there’s a risk of splashes or sprays. These infections are not primarily transmitted via mucous membrane exposure.
D. Disposable mask: A regular surgical or disposable mask does not offer sufficient protection against airborne pathogens. For airborne precautions, a fit-tested N95 respirator is essential.
Take home points:
- Knowing the mode of transmission of infectious diseases is key to selecting appropriate PPE.
- Airborne precautions require an N95 respirator.
The infection control nurse has asked the staff to work on reducing the number of iatrogenic infections on the unit. Which of the following actions on the nurses’ part would contribute to reducing health care–acquired infections? Select all that apply
Explanation
Iatrogenic infections, also known as healthcare-associated infections (HAIs), are infections acquired during the course of receiving healthcare treatment. These infections can result from invasive procedures, improper hand hygiene, or contamination from the healthcare environment.
Rationale for correct answer:
A. Teaching correct handwashing to assigned patients: Hand hygiene is the most effective method to prevent the spread of infection. Educating patients on proper handwashing technique helps reduce transmission of pathogens.
B. Using correct procedures in starting and caring for an intravenous infusion: Proper aseptic technique when inserting and maintaining IV lines reduces the risk of bloodstream infections, a common type of HAI.
C. Providing perineal care to a patient with an indwelling urinary catheter: Perineal care prevents bacterial colonization around the catheter site and reduces the risk of catheter-associated urinary tract infections (CAUTIs), a common iatrogenic infection.
Rationale for incorrect answer:
D. Isolating a patient on antibiotics who has been having loose stool for 24 hours: While loose stool could suggest a Clostridioides difficile (C. diff) infection, isolation might not be warranted until there's confirmation-either through a positive lab result or continued symptoms with clinical suspicion. Premature isolation without evidence may not align with resource allocation or institutional policy.
E. Decreasing a patient’s environmental stimuli to decrease nausea: While comfort measures are important, reducing environmental stimuli for nausea does not contribute to the prevention of infections and is unrelated to infection control practices.
Take home points:
Preventing iatrogenic infections requires vigilance in patient care practices, including:
- proper catheter care
- IV-line maintenance
- patient education on hand hygiene among others
Put the following steps for removal of protective barriers after leaving an isolation room in order.
Explanation
Correct doffing (removal) of PPE is just as important as donning it. Most PPE surfaces are contaminated after client care; removing them in the wrong order greatly increases the risk of self-contamination and transmission to others. Move from clean to dirty.
Rationale for correct answer:
Step 1: Remove and dispose of gloves.
Gloves are typically the most contaminated item. Removing them first immediately lowers the bioburden on your hands (while using proper glove-removal technique to avoid touching the outside surface).
Step 2: Remove eyewear or goggles.
Eye protection may be contaminated by droplets/splashes. With gloves off, your (now cleaner) hands are less likely to contaminate your face when taking goggles off by the side arms/strap.
Step 3: Untie waist and neck strings of gown. Remove gown, rolling it onto itself without touching the contaminated side.
The gown’s front and sleeves are contaminated. Untie, then peel it away from the body, turning the contaminated surface inward to contain pathogens.
Step 4: Untie bottom and then top mask strings and remove from face.
Masks (or respirators) are removed last to maintain respiratory protection while you’re still handling other potentially contaminated PPE. Untying the bottom first, then top prevents the mask from falling forward against your face.
Step 5: Perform hand hygiene.
Always the final step to remove any microorganisms acquired during PPE removal.
Take home points:
- Doff the dirtiest first (gloves) and finish with hand hygiene.
- Never touch the contaminated fronts of gowns, masks, or goggles; handle by clean ties, straps, or inside surfaces only.
A patient is diagnosed with a multidrug-resistant organism (MDRO) in his surgical wound and asks the nurse what this means. What is the nurse’s best response? Select all that apply
Explanation
Multidrug-resistant organisms (MDROs) are strains of bacteria that have developed resistance to multiple antibiotics, particularly broad-spectrum agents that are typically used as first-line treatments. These organisms pose a significant public health threat because they are harder to treat, often require more toxic or expensive medications.
Rationale for correct answer:
B. The antibiotics the patient has received are not strong enough to kill the organism: MDROs have developed resistance to antibiotics that would normally be effective. This resistance means that the usual antibiotics are no longer strong enough to treat the infection.
D. The organism has developed a resistance to one or more broad-spectrum antibiotics, indicating that the organism will be hard to treat effectively: These organisms are difficult to treat precisely because they have adapted to survive exposure to multiple common antibiotics.
Rationale for incorrect answers:
A. There is more than one organism in the wound that is causing the infection: This describes a polymicrobial infection, not a multidrug-resistant organism. MDRO refers to a single organism that is resistant to several antibiotics.
E. There are no longer any antibiotic options available to treat the patient’s infection: While MDROs are difficult to treat, there are usually still some options available, though they may be more limited or have greater side effects.
Take home points:
- MDROs are single organisms resistant to multiple antibiotics, making infections harder to treat and control.
- Educating patients about antibiotic resistance and the importance of completing prescribed antibiotics helps prevent the emergence of MDROs.
The nurse assesses the following data from a patient with diabetes mellitus who is 4 days postoperative for repair of an abdominal aortic aneurysm. Which assessment finding is of greatest concern for the nurse?
Explanation
Postoperative clients with diabetes mellitus are at increased risk for infection, poor wound healing, and complications such as pneumonia or sepsis.
Rationale for correct answer:
B. Temperature 38.5°C (101.4°F): A postoperative fever (≥38.5°C) in a client with diabetes mellitus is a significant red flag for infection. Due to impaired immune response and delayed wound healing in diabetics, a fever can indicate a developing or ongoing infection.
Rationale for incorrect answers:
A. Vesicular breath sounds in the lung bases are normal findings in the peripheral lung fields. This is not concerning and indicates that the lung bases are clear and the client does not have adventitious sounds which could indicate fluid overload or pneumonia.
C. Incision pain rating of 6 out of 10: While a pain rating of 6/10 suggests moderate pain and should be managed appropriately, pain is expected after major abdominal surgery. Unless the pain is associated with signs of infection or dehiscence it is not the most concerning finding.
D. Blood glucose of 164 mg/dL is slightly elevated for a postoperative diabetic patient but is not critically high. Mild hyperglycemia can occur postoperatively due to stress and corticosteroid use.
Take home points:
- Postoperative fever in a diabetic patient is a potential sign of infection.
- Routine postoperative pain and slightly elevated glucose levels are expected findings.
Which type of mask or respirator is used for airborne precautions?
Explanation
Airborne precautions are infection control measures used to prevent the transmission of pathogens that remain suspended in the air for long periods and can travel over distances.
Rationale for correct answer:
C. An N95 mask (respirator) is specifically designed to filter at least 95% of airborne particles, making it the appropriate protection for airborne precautions.
Rationale for incorrect answers:
A. A standard surgical mask provides a barrier against large droplets but is not effective in protecting against small airborne particles. It is used for droplet precautions.
B. A face shield protects mucous membranes (eyes, nose, mouth) from splash or spray but does not provide respiratory protection. It should be used in addition to a mask or respirator.
D. None is needed: Airborne diseases are highly transmissible without proper PPE. Respiratory protection is essential when dealing with airborne infections. Without a respirator, both healthcare workers and other patients are at high risk of exposure.
Take home points:
- The N95 respirator is the standard protective equipment for airborne precautions.
- Surgical masks and face shields are useful for droplet and contact precautions.
Exams on Infection Control And Asepsis
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
- Describe the chain of infection.
- Explain the principles of medical and surgical asepsis.
- Contrast the various types of isolation precautions.
- Apply personal protective equipment properly in the correct order
- Implement recommended techniques for medical and surgical asepsis
- Explain the postexposure process for health care workers after exposure to hepatitis.
Introduction
Infection- results when a pathogen invades tissues and begins growing within a host.
Colonization is the presence and growth of microorganisms within a host but without tissue invasion or damage.
Communicable disease-If an infectious disease can be transmitted directly from one person to another.
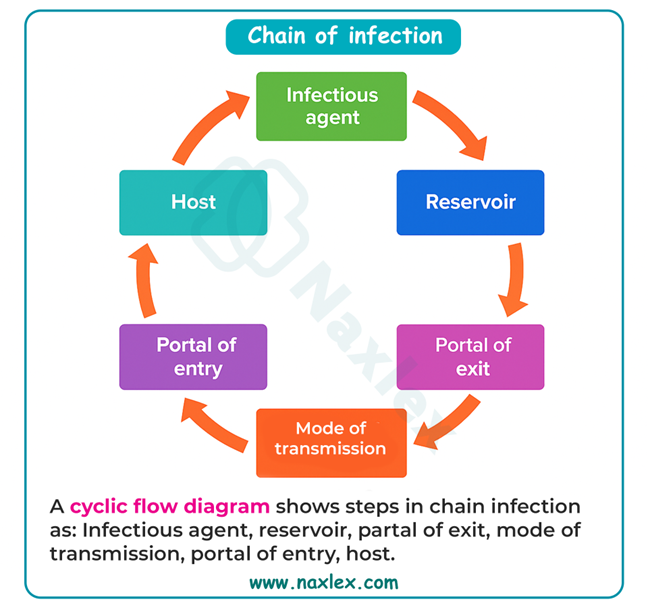
Infection Cycle
An infection is a disease state that results from the presence of pathogens (disease-producing microorganisms) in or on the body.
An infection occurs as a result of a cyclic process, consisting of six components. These components are:
• Infectious agent
• Reservoir
• Portal of exit
• Means of transmission
• Portals of entry
• Susceptible host
Modes of transmission.
Each disease has a specific mode of transmission.
Often, you are able to do little about the infectious agent or the susceptible host, but by practicing infection prevention and control techniques such as hand hygiene and use of PPE, you interrupt the mode of transmission.
They include:
- Contact:
- Direct: Person-to-person physical contact.
- Indirect: Personal contact of susceptible host with contaminated inanimate object
- Droplet: infected person coughs or sneezes.
- Airborne: Organisms are carried in droplet nuclei or residue or evaporated droplets suspended in air during coughing or sneezing
- Vehicles: Contaminated items, Water, Drugs, solutions, Blood, Food
- Vector: External mechanical transfer e.g. flies. Internal transmission e.g. mosquito, louse.
Course of Infection by Stage:
Incubation period:
Interval between entrance of pathogen into body and appearance of first symptoms.
Prodromal stage:
Interval from onset of nonspecific signs and symptoms (malaise, low-grade fever, fatigue) to more specific symptoms.
Illness stage:
Interval when a patient manifests signs and symptoms specific to type of infection.
Convalescence:
Interval when acute symptoms of infection disappear.
Factors Affecting the Risk for Infection
The susceptibility of the host depends on various factors:
• Integrity of skin and mucous membranes, which protect the body against microbial invasion
• pH levels of the gastrointestinal and genitourinary tracts, as well as the skin, which help to ward off microbial invasion
• Integrity and number of the body’s white blood cells, which provide resistance to certain pathogens
• Age, sex, race, and hereditary, which influence susceptibility. Neonates and older adults appear to be more vulnerable to infection. (See the accompanying box, Focus on the Older Adult.)
• Immunizations, natural or acquired, which act to resist infection
• Level of fatigue, nutritional and general health status, the presence of preexisting illnesses, previous or current treatments, and certain medications, which play a part in the susceptibility of a potential host
• Stress level, which if increased, may adversely affect the body’s normal defense mechanisms
• Use of invasive or indwelling medical devices, which provide exposure to and entry for more potential sources of disease-producing organisms, particularly in a patient whose defenses are already weakened by disease
Health care–associated infections:
They occur as the result of invasive procedures, antibiotic administration, the presence of multidrug-resistant organisms (MDROs), and breaks in infection prevention and control activities.
Examples of Sites for and Causes of Health Care–Associated Infections:
- Improperly performing hand hygiene increases patient risk for all types of healthcare–associated infections.
- Urinary tract- Unsterile insertion of urinary catheter, Improper positioning of the drainage tubing, Repeated catheter irrigations, Improper perineal hygiene
- Surgical or traumatic wounds- Improper skin preparation before surgery, Failure to use aseptic technique during operative procedures and dressing changes, Use of contaminated antiseptic solutions.
- Respiratory tract-Contaminated respiratory therapy equipment, Failure to use aseptic technique while suctioning airway, Improper disposal of secretions.
- Bloodstream- Improper care of needle insertion site, Contaminated needles or catheters, Improper technique during administration of multiple blood products, Improper care of peritoneal or hemodialysis shunts, improperly accessing an IV port.
Categories for Sterilization, Disinfection, and Cleaning:
Critical items
Items that enter sterile tissue or the vascular system present a high risk of infection if they are contaminated with microorganisms, especially bacterial spores. Critical items must be sterile.
Semi-critical items
Items that come in contact with mucous membranes or nonintact skin also present a risk. These objects must be free of all microorganisms (except bacterial spores). Semi-critical items must be high-level disinfected (HLD) or sterilized.
Noncritical items
Items that come in contact with intact skin but not mucous membranes must be clean. Noncritical items must be disinfected.
Nursing insights:
- Transmission of infection can occur if the six elements of the infection chain are present and uninterrupted.
- Normal body flora and body system defenses help the body resist infection by reducing the number of pathogenic organisms.
- Health care-associated infections lead to adverse patient events and significantly higher health care costs that are often not reimbursed.
Centers For Disease Control And Prevention Isolation Guidelines
By 1970, the CDC was actively involved in developing and recommending infection-control practices and procedures for hospitals.
OSHA, a government agency that administers the Occupational Safety and Health Act of 1970, establishes minimum health and safety standards for workers.
The revised guidelines continue the designation of two tiers of precautions:
- Standard precautions- for use with all patients.
- Transmission-based precautions- for use with specific types of patients.
Standard Precautions:
These precautions apply to blood, all body fluids (whether or not they contain blood), secretions and excretions, nonintact skin, and mucous membranes.
They include:
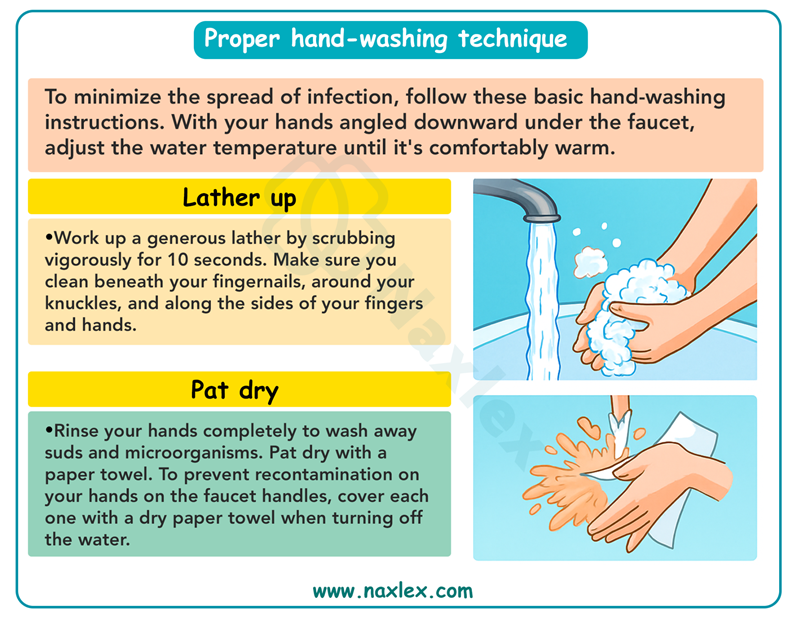
- Perform hand hygiene before direct contact with patients; between patient contacts; after contact with blood, body fluids, secretions, and excretions and with equipment or articles contaminated by them; and immediately after gloves are removed.
- When hands are visibly soiled or contaminated with blood or body fluids, wash them with either a nonantimicrobial soap or antimicrobial soap and water.
- When hands are not visibly soiled or contaminated with blood or body fluids, use an alcohol-based hand rub to perform hand hygiene.
- Wash hands with nonantimicrobial or antimicrobial soap and water if contact with spores (e.g., Clostridium difficile) is likely to have occurred.
- Do not wear artificial fingernails or extenders if duties include direct contact with patients at high risk for infection and associated adverse outcomes.
- Wear gloves when touching blood, body fluids, secretions, excretions, nonintact skin, mucous membranes, or contaminated items or surfaces. Remove and dispose of gloves and perform hand hygiene between patient care encounters and when going from a contaminated to a clean body site.
- Wear PPE when your anticipated patient interaction is likely to involve contact with blood or body fluids.
- Discard all contaminated sharp instruments and needles in a puncture-resistant container.
Transmission based precautions:
1.Airborne precautions:
Airborne precautions apply to patients known or suspected to be infected with microorganisms transmitted by airborne droplet nuclei.
Use these for patients who have infections that spread through the air such as tuberculosis, varicella (chicken pox), rubeola (measles), and possibly SARS.
- Place the patient in a private room that has monitored negative air pressure in relation to surrounding areas, 6 to 12 air changes per hour, and appropriate discharge of air outside or monitored filtration if air is recirculated.
- Keep the door closed and patient in the room.
- Wear a mask or respirator when entering the room of a patient with known or suspected tuberculosis.
- If a patient has known or suspected rubeola (measles) or varicella (chicken pox), respiratory protection should be worn unless the person entering the room is immune to these diseases.
- Transport patients out of the room only when necessary and place a surgical mask on the patient if possible.
2. Droplet precautions:
Are used for clients known to have or suspected of having serious illnesses transmitted by particle droplets larger than 5 microns.
- Place the client in a private room.
- If a private room is not available, place the client with another client who is infected with the same microorganism.
- Wear a mask if working within 1 m (3 ft) of the client.
- Limit movement of client outside the room to essential purposes.
- Place a surgical mask on the client while outside the room.
3. Contact precautions:
Are used for clients known to have or suspected of having serious illnesses easily transmitted by direct client contact or by contact with items in the client’s environment. According to the CDC, such illnesses include GI, respiratory, skin, or wound infections or colonization with multidrug-resistant bacteria.
- Place the client in a private room.
- If a private room is not available, place the client with another client who is infected with the same microorganism.
- Wear gloves as described in standard precautions.
- Change gloves after contact with infectious material.
- Remove gloves before leaving the client's room.
- Cleanse hands immediately after removing gloves. Use an antimicrobial agent.
Note: If the client is infected with C. difficile, do not use an alcohol-based hand rub because it is not effective on these spores. Use soap and water.
-
- After hand hygiene, do not touch possibly contaminated surfaces or items in the room.
- Wear a gown when entering a room if there is a possibility of contact with infected surfaces or items, or if the client is incontinent, or has diarrhea, a colostomy, or wound drainage not contained by a dressing.
- Remove the gown in the client’s room.
- Make sure the uniform does not contact possible contaminated surfaces.
- Limit movement of clients outside the room.
- Dedicate the use of noncritical client care equipment to a single client or to clients with the same infecting microorganisms.
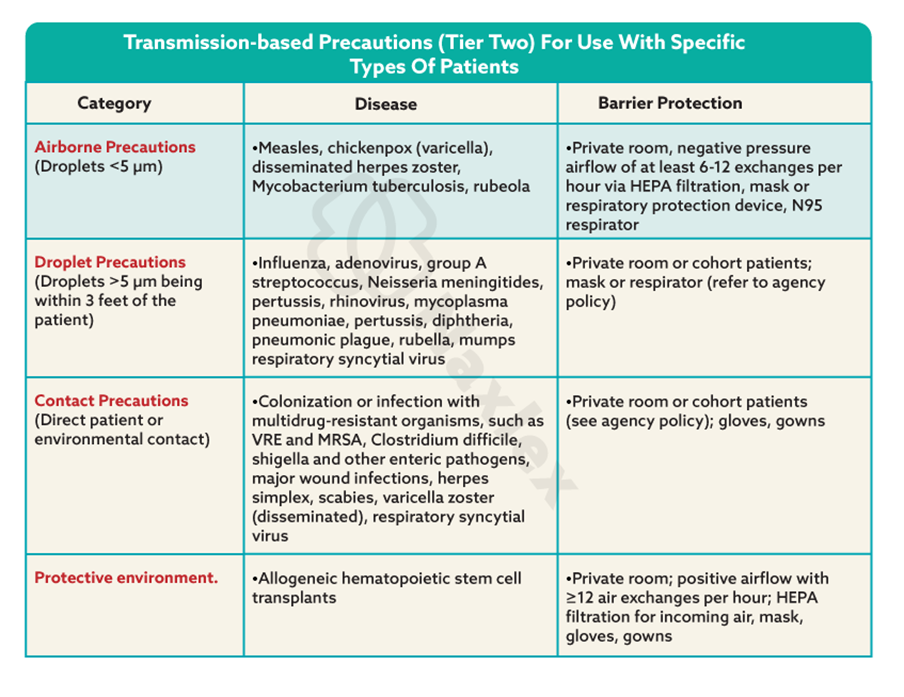
Immunocompromised patients:
Include those who:
- Have diseases, such as leukemia, or treatments such as chemotherapy, that depress the client’s resistance to infectious organisms.
- Have extensive skin impairments, such as severe dermatitis or major burns, which cannot be effectively covered with dressings
The protective environment category is designed for patients who have undergone transplants and gene therapy, making them highly vulnerable to infection.
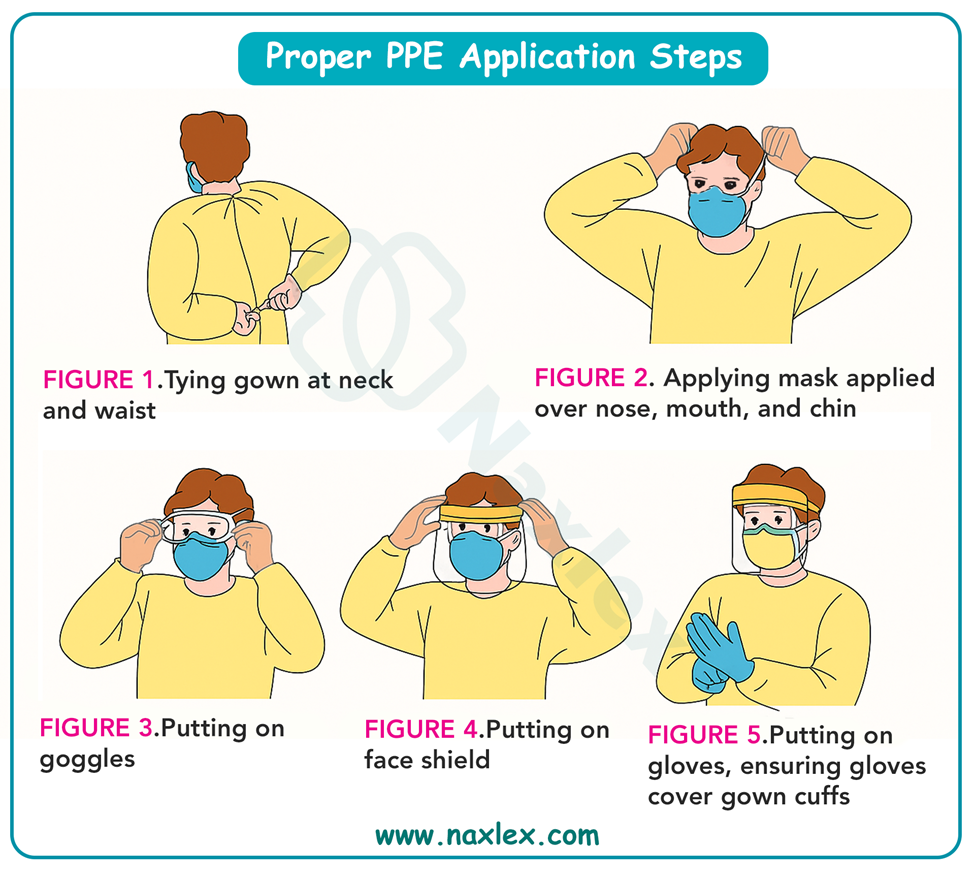
Personal protective equipment (PPE)
The PPE, specialized clothing or equipment (e.g., gowns, masks or respirators, protective eyewear, and gloves) that you wear for protection against exposure to infectious materials, should be readily available in a patient care area.
Donning PPE:
- Check medical record and nursing plan of care for type of precautions and review precautions in infection-control manual- Mode of transmission of organism determines type of precautions required.
- Plan nursing activities before entering the patient's room.
- Perform hand hygiene.
- Put on the gown, with the opening in the back. Tie gown securely at neck and waist.
- Put on the mask or respirator over your nose, mouth, and chin. Secure ties or elastic bands at the middle of the head and neck. If a respirator is used, perform a fit check. Inhale; the respirator should collapse. Exhale; air should not leak out.
- Put on goggles. Place over eyes and adjust to fit. Alternatively, a face shield could be used to take the place of the goggles.
- Put on clean disposable gloves. Extend gloves to cover the cuffs of the gown
Doffing PPE:
- Except for the respirator, remove PPE at the doorway or in the anteroom. Remove the respirator after leaving the patient room and closing the door.
- If an impervious gown has been tied in front of the body at the waistline, untie waist strings before removing gloves.
- Grasp the outside of one glove with the opposite gloved hand and peel off, turning the glove inside out as you pull it off. Hold the removed glove in the remaining gloved hand.
- Slide fingers of ungloved hand under the remaining glove at the wrist, taking care not to touch the outer surface of the glove.
- Peel off the glove over the first glove, containing the one glove inside the other. Discard in the appropriate container.
- To remove the goggles or face shield: Handle by the headband or ear pieces. Lift away from the face. Place in designated receptacle for reprocessing or in an appropriate waste container.
- To remove gown: Unfasten ties, if at the neck and back. Allow the gown to fall away from shoulders. Touching only the inside of the gown, pull away from the torso. Keeping hands on the inner surface of the gown, pull from arms. Turn the gown inside out. Fold or roll into a bundle and discard.
- To remove mask or respirator: Grasp the neck ties or elastic, then top ties or elastic and remove. Take care to avoid touching the front of the mask or respirator. Discard in the waste container. If using a respirator, save for future use in the designated area.
- Perform hand hygiene immediately after removing all PPE.
Latex allergy
Risk Factors
• Healthcare workers who wear latex gloves
• People with allergic tendencies
• People with food allergies, specifically banana, papaya, avocado, potatoes, kiwi fruit, chestnuts, and pineapples
• Latex-industry workers
• People with asthma, spina bifida, or a history of multiple surgical procedures or exposures to latex
Frequently Used Products That Contain Latex
- Blood pressure cuffs
- Stethoscopes
- Electrode pads
- IV tubing
- Foley catheters
- Baby bottle nipples
- Tourniquets
- Syringes
- Surgical masks
- Pacifiers
Types of Reactions
• Irritant contact dermatitis: nonallergic dermatitis, restricted to areas that have made contact with the latex. Gloves may cause erythematous and pruritic hands. This is not a true allergy.
• Chemical sensitivity dermatitis or delayed hypersensitivity: allergic contact dermatitis, displayed as dry, crusty bumps, erythema, pruritus, scaling vesicles, papular lesions at site of contact, including the palms; not a life-threatening reaction, however, person should be aware of latex contact.
• Latex allergy or Type I hypersensitivity: systemic reactions, displayed as rhinitis, conjunctivitis, angioedema, bronchospasm, shock, and/or systemic anaphylactic reactions; this is a life-threatening sensitivity.
Diagnosis
-
- RAST: blood test for IgE antibodies to latex
- Skin prick: small amount of serum derived from latex placed on small prick in skin
- Glove challenge: patient wearing a latex glove for a period of time, with periodic checking for any signs of latex reactions listed above.
Treatment
• Avoidance of latex-containing products
• Localized reaction treated with oral diphenhydramine, cool compresses, and hydrocortisone 1% cream
• Systemic reaction possibly treated with epinephrine subcutaneously, systemic steroids, antihistamines, with transport to the emergency department
Protocols for patients with latex allergies
-
- Assess patients for allergy to latex products.
- Place an allergy sticker on a chart, a Caution sign on the door, and an allergy band on the patient’s wrist.
- Remove all latex-containing articles from the room.
- Place three-way stopcocks in IV lines for medication administration. Place tape over any injection ports on IV tubing.
- Remove rubber stoppers from vials before drawing up medications.
- If available, place a cart containing all latex-free supplies in or outside of the patient's room.
- Use glass syringes if no latex-free alternative is available.
- Cover the latex portion of the blood pressure cuff or stethoscope before using on the patient.
- Wear vinyl or synthetic gloves when caring for patients.
Nursing insights:
- Standard Precautions are applied in all patient care activities to prevent patients and health care workers from transmitting infection even in the absence of disease.
- Transmission-based precautions, including airborne, droplet, contact, and protective environment, are used in addition to Standard Precautions for patients with highly transmissible pathogens.
Surgical Asepsis
Surgical asepsis or sterile technique prevents contamination of an open wound, serves to isolate an operative or procedural area from an unsterile environment, and maintains a sterile field for surgery or procedural intervention.
In surgical asepsis an area or object is considered contaminated if touched by any object that is not sterile.
Use surgical asepsis in the following situations:
- During procedures that require intentional perforation of the patient’s skin, such as insertion of peripheral IV catheters or a central IV line.
- When the integrity of the skin is broken as a result of trauma, surgical incision, or burns.
- During invasive procedures, such as the insertion of a urinary catheter or the insertion of surgical instruments into sterile body cavities (e.g., placement of a wound drain)
Principles of surgical asepsis:
- A sterile object remains sterile only when touched by another sterile object.
- Only sterile objects may be placed on a sterile field.
- A sterile object or field out of the range of vision or an object held below a person’s waist is contaminated.
- A sterile object or field becomes contaminated by prolonged exposure to air.
- When a sterile surface comes in contact with a wet, contaminated surface, the sterile object or field becomes contaminated by capillary action.
- Fluid flows in the direction of gravity- during a surgical hand scrub, hold your hands above your elbows.
- The edges of a sterile field or container are considered contaminated- a 2.5-cm (1inch) border around the drape is considered contaminated.
Preparing a sterile field:
A sterile field is an area free of microorganisms that is prepared to receive sterile items.
- Use the inner surface of a sterile wrapper as the work surface or by using a sterile drape or dressing tray.
- After creating the surface for the sterile field, add sterile items by placing them directly on the field or transferring them with sterile forceps.
- Discard an object that comes in contact with the 2.5-cm (1-inch) border.
- Sometimes you will wear sterile gloves while preparing items on a sterile field- the gloves cannot touch the wrappers of sterile items.
- Pouring sterile solutions:
- Hold the bottle with its label in the palm of the hand to prevent the possibility of the solution wetting and fading the label.
- Keep the edge of the bottle away from the edge or inside of the receiving container.
- Pour the solution slowly to avoid splashing the underlying drape or field.
- Hold the bottle outside the edge of the sterile field.
Surgical hand scrub:
Nurses working in operating rooms perform surgical hand antisepsis to decrease and suppress the growth of skin microorganisms under gloved hands in case of glove tears.
A surgical hand scrub must eliminate the transient flora and reduce the resident flora on the hands.
Chlorhexidine gluconate has been found to be more effective than povidone-iodine as a cleansing agent, although both can be found in health care agencies.
The traditional scrub time in the United States for both the initial and the subsequent scrub is 5 minutes, but research has shown effectiveness can be gained when scrubs are performed for 2, 3, and 6 minutes.
Applying sterile gloves:
Sterile gloves are an additional barrier to bacterial transfer.
There are two gloving methods: open and closed.
In the open glove technique, your hands slide all the way through the sleeves out beyond the cuffs of the gown (if worn).

The closed-gloving method, performed after applying a sterile gown, is practiced in operating rooms and special procedure areas.
Donning a sterile gown:
- Nurses wear sterile gowns when assisting at the sterile field in the operating room, delivery room, and special procedure areas.
- It allows a nurse to handle sterile objects and also be comfortable with less risk of contamination.
- Nurses caring for patients with large open wounds or assisting health care providers during major invasive procedures (e.g., inserting an arterial catheter) also wear sterile gowns.
- Only a certain portion of the gown (i.e., the area from the anterior waist to, but not including, the collar and the anterior surface of the sleeves) is considered sterile.
- The back of the gown, the area under the arms, the collar, the area below the waist, and the underside of the sleeves are not sterile because you cannot keep these areas in constant view and ensure their sterility.
Post Exposure Prophylaxis
HBV and HCV are the infections most commonly transmitted by contaminated needles. Report any contaminated needlestick immediately.
Additional criteria for exposure reporting include blood or other potentially infectious materials (OPIMs) that come into direct contact with an open area of the skin, blood or OPIM that is splashed into a health care worker’s eye or mouth or up the nose, and cuts with a sharp object that is covered with blood or OPIM.
Exposure to human immunodeficiency virus
- If the patient is positive for human immunodeficiency virus (HIV) infection, a viral load study should be performed to determine the amount of virus present in the blood.
- If the exposure meets the CDC criteria for HIV PEP, it should be started as soon as possible, preferably within 24 hours after the exposure.
Exposure to hepatitis C virus
- If the source patient is positive for hepatitis C virus (HCV), the employee receives a baseline test.
- At 4 weeks after exposure the employee should be offered an HCV-RNA test to determine whether the employee contracted HCV.
- If positive, the employee starts treatment.
- There is no prophylactic treatment for HCV after exposure.
- Early treatment for infection can prevent chronic infection.
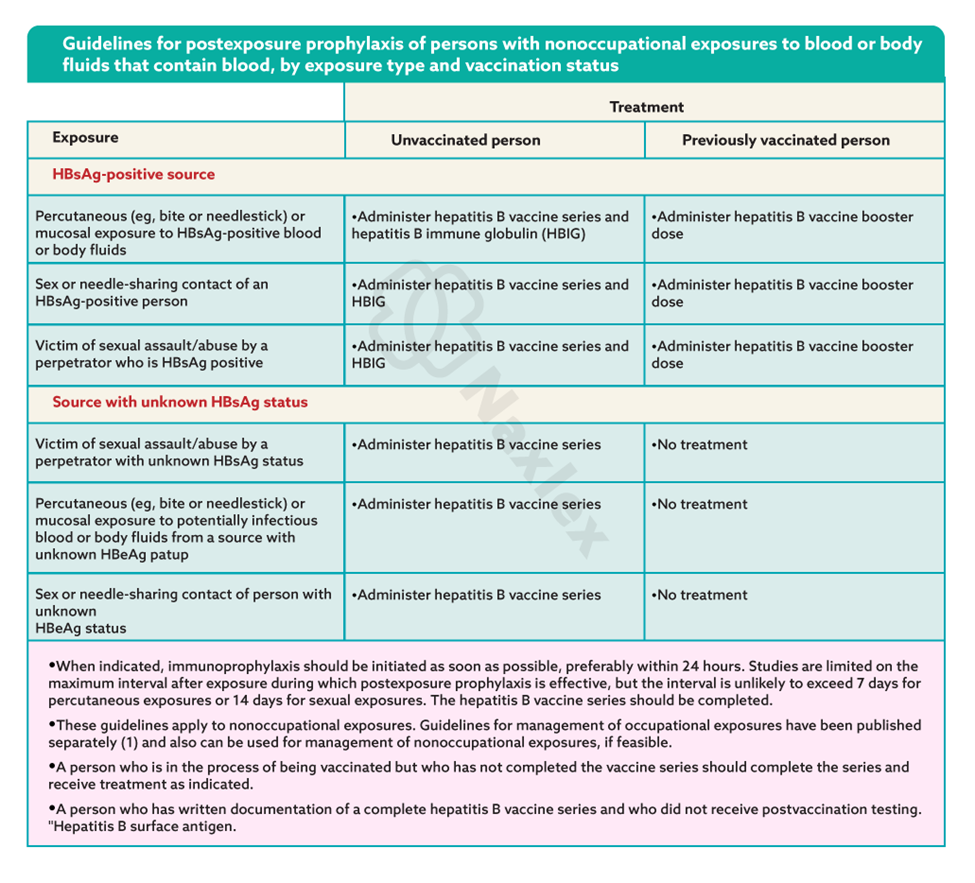
Exposure to hepatitis B virus
- After exposure, no treatment is needed if there is a positive blood titer on file.
- If no positive titer is on file, follow CDC guidelines if positive exposure source:
- Persons who have written documentation of a complete hepatitis B vaccine series and who did not receive postvaccination testing should receive a single vaccine booster dose.
- Persons who are in the process of being vaccinated but who have not completed the vaccine series should receive the appropriate dose of hepatitis B immune globulin (HBIG) and should complete the vaccine series.
- Unvaccinated persons should receive both HBIG and hepatitis B vaccine as soon as possible after exposure (preferably within 24 hours). Hepatitis B vaccine may be administered simultaneously with HBIG in a separate injection site. The hepatitis B vaccine series should be completed in accordance with the age-appropriate vaccine dose and schedule.
Follow up risk:
Follow-up for risk of acquiring infection begins with source patient testing.
Access to testing the source patient is stated in the testing law for each state.
- Some states have deemed consent, which means that the state has granted the patient’s consent to be tested.
- Other states require that the patient consent to testing for the presence of bloodborne pathogens.
Health care agencies and workers’ compensation require exposed employees to complete an injury report and seek appropriate treatment if needed.
If positive for HIV or HCV, testing for syphilis may be indicated because of the incidence of coinfection.
Nursing insights:
- Surgical asepsis, such as sterile gloving, is a more stringent technique than medical asepsis.
- Health care workers believed to have been exposed to hepatitis B will receive the vaccine and vaccination series.
Summary
- Effective prevention and control of infectious disease is an international, national, community, and individual responsibility.
- Asepsis is the freedom from disease-causing microorganisms.
- Surgical aseptic practices keep an area or objects free of all microorganisms.
- An infection can develop if the links in the chain of infection-etiologic agent, reservoir, portal of exit, mode of transmission, portal of entry, and susceptible host-are not interrupted.
- Preventing infections in healthy or ill persons and preventing the transmission of microorganisms from infected clients to others are major nursing functions.
- All health care providers must apply clean or sterile gloves, gowns, masks, and protective eyewear according to the risk of exposure to potentially infective materials.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Infection Control And Asepsis
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


