Please set your exam date
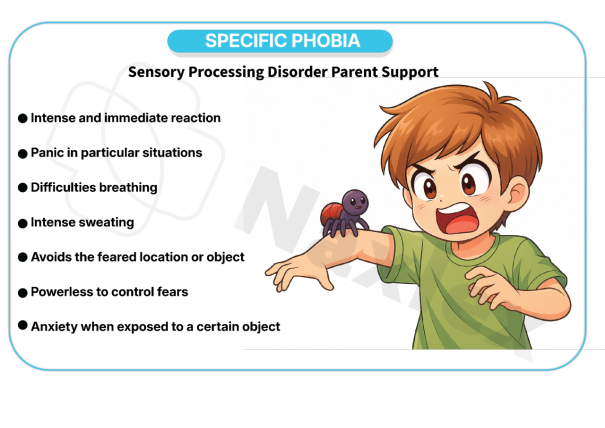
Specific Phobia
Study Questions
Practice Excercise 1
A nurse is assessing a client who reports an overwhelming fear of elevators. The client avoids visiting her doctor’s office on the 10th floor because she fears being trapped inside the elevator. The client states, “I know it's irrational, but I just can't help it.” Which of the following characteristics best supports a diagnosis of specific phobia?
Explanation
Specific phobiais a persistent fearof a particular object or situation that provokes immediate anxietyand leads to avoidance behavior. DSM-5 criteria require the fear to be excessive, last ≥6 months, and cause functional impairment. The individual may recognize the fear as irrational but still be unable to control the response. Physical symptoms include tachycardia, sweating, and shortness of breath. Common subtypes include animal, situational, and environmental phobias. Treatment involves exposure therapy and cognitive restructuring.
Rationale for correct answers
2.Persistent fear with insightinto its irrationality, coupled with avoidance, directly meets DSM-5 criteria for specific phobia. The client’s awareness and behavioral impact confirm the diagnosis.
Rationale for incorrect answers
1.Multiple unrelated fears suggest generalizedanxiety or another disorder, not specific phobia, which is tied to a distinct trigger.
3.Free-floating anxiety without a clear stimulus aligns with generalizedanxiety disorder, not the targeted fear seen in phobias.
4.Panic attacks without a trigger point to panicdisorder, which differs from phobia’s stimulus-bound anxiety response.
Take Home Points
- Specific phobia involves persistent, irrational fear of a distinct object or situation.
- DSM-5 requires immediate anxiety, avoidance, and functional impairment lasting ≥6 months.
- Insight into irrationality may be present but is not required for diagnosis.
A nurse is teaching a group of nursing students about the neurobiological mechanisms involved in specific phobias. Which of the following statements by a student indicates correct understanding?
Explanation
The amygdalais a central structure in the limbic systemresponsible for processing fear and emotional responses. Upon exposure to a phobic stimulus, it rapidly activates the sympathetic nervous system, triggering the fight-or-flight response. This includes increased heart rate, pupil dilation, and muscle tension. The amygdala communicates with the hypothalamus and brainstem to initiate autonomic and endocrine changes. It also stores emotional memories, contributing to conditioned fear responses. Dysfunctional amygdala circuits are implicated in persistent phobias and anxiety disorders.
Rationale for correct answers
3.The amygdala initiates sympathetic activationwhen exposed to a phobic stimulus, leading to physiological fear responses like tachycardia and hyperventilation.
Rationale for incorrect answers
1.Dopamine from the hypothalamus does not directly inhibit fear; instead, the hypothalamus coordinates stressresponses via the HPA axis.
2.The cerebellum regulates motor coordination, not emotional processing or fear recognition, making it irrelevant to phobic responses.
4.The pituitary gland facilitates hormonalstress responses (e.g., ACTH release), not suppression of the fight-or-flight reaction during phobia.
Take Home Points
- The amygdala is the primary brain structure involved in fear processing and phobic responses.
- Activation of the sympathetic nervous system is a hallmark of specific phobia episodes.
- The cerebellum and pituitary gland play indirect or unrelated roles in fear response.
- Differentiating neuroanatomical roles is essential in understanding anxiety and phobic disorders.
Systematic desensitization is the most suitable treatment for the treatment of:
Explanation
Phobiais a specific anxiety disordercharacterized by marked, persistent, and irrational fear of a particular object, situation, or place. Exposure to the feared stimulus provokes immediate anxiety, often leading to avoidance behavior. DSM-5 criteria require the fear to be disproportionate to actual danger, last ≥6 months, and cause functional impairment. Physical symptoms may include tachycardia, sweating, and trembling. Systematic desensitization is the most effective behavioral treatment, using graded exposure paired with relaxation.
Rationale for correct answers
1.Systematic desensitization is designed to treat phobiasby gradually exposing the client to the feared stimulus while inducing relaxation. It retrains the fear response through reciprocal inhibition, making it the most suitable and evidence-based intervention.
Rationale for incorrect answers
2.OCD involves intrusive thoughtsand compulsions, not stimulus-specific fear. Treatment focuses on exposure with response prevention, not desensitization.
3.Hysteria, now classified under conversion disorder, involves neurological symptoms without organic cause. Desensitization is not effective for motor or sensory deficits.
4.Hypochondriasis, now termed illness anxiety disorder, involves preoccupation with having a serious illness. Cognitive restructuring and reassurance techniques are preferred over exposure therapy.
Take Home Points
- Systematic desensitization is most effective for treating specific phobias.
- It uses graded exposure and relaxation to counter conditioned fear responses.
- Phobias differ from OCD, conversion disorder, and illness anxiety in symptom origin and treatment.
- DSM-5 requires phobic symptoms to be persistent, disproportionate, and impairing.
Practice Exercise 2
A client has been diagnosed with agoraphobia. Which behavior would be most characteristic of this disorder?
Explanation
Agoraphobiais a persistent anxiety disordermarked by intense fear of being in places or situations where escape might be difficult or help unavailable during panic-like symptoms. It typically involves avoidance of public spaces, crowds, or unfamiliar environments. The DSM-5 requires fear in at least two situations—such as public transport, open spaces, enclosed places, crowds, or being alone outside home—for ≥6 months. Individuals may become housebound, relying on others for basic needs, and often experience comorbid panic disorder.
Rationale for correct answers
4.The behavior of staying home due to fear of being in a place where escape is difficult is characteristicof agoraphobia. This reflects the core diagnostic criteria—marked avoidance of situations where panic or helplessness may occur, often leading to confinement indoors.
Rationale for incorrect answers
1.This reflects a specificphobia, not agoraphobia. Fear of snakes is situational and does not involve avoidance of public or escape-compromised environments.
2.Refusing to fly may indicate aviophobia, a specific phobia of flying. It lacks the broader avoidance pattern seen in agoraphobia and does not meet the DSM-5 criteria.
3.Avoiding public eating may suggest socialanxiety disorder, where fear centers on embarrassment or judgment, not escape difficulty or panic in open spaces.
5.Avoiding night driving due to fear of being far from help may resemble panicdisorder with anticipatory anxiety, but it lacks the pervasive avoidance of multiple public situations required for agoraphobia.
Take Home Points
- Agoraphobia involves fear of being in places where escape is difficult or help unavailable during panic symptoms.
- DSM-5 requires fear in at least two situations: open spaces, enclosed places, crowds, public transport, or being alone outside.
- It must persist for ≥6 months and cause significant distress or impairment in functioning.
- Differentiate agoraphobia from specific phobias and social anxiety disorder based on the breadth and nature of avoidance.
A 35-year-old male presents to the clinic reporting intense anxiety and a feeling of impending doom every time he must take an elevator to his 10th-floor office. He reports a racing heart, shortness of breath, and diaphoresis during these episodes. Which of the following is the most likely diagnosis?
Explanation
Claustrophobiais a specific phobiacharacterized by intense fear of enclosed spacessuch as elevators, tunnels, or small rooms. It is classified under situational-type phobias in DSM-5. Symptoms include panic attacks, shortness of breath, tachycardia, and a sense of impending doom. The fear is disproportionate to actual danger and leads to avoidance behaviors. It often begins in childhood or adolescence and may be triggered by traumatic confinement experiences. Diagnosis requires marked fear, avoidance, and functional impairment lasting ≥6 months.
Rationale for correct answers
3.The elevator scenario reflects situationalclaustrophobia, where enclosed spaces provoke panic symptoms like diaphoresis, tachycardia, and breathlessness. The fear is irrational and persistent, aligning with DSM-5 criteria for specific phobia.
Rationale for incorrect answers
1.Acrophobia involves fear of heights, not enclosed spaces. Elevators may be involved, but the trigger here is confinement, not elevation.
2.Agoraphobia centers on fear of open or publicspaces where escape may be difficult. Elevators are enclosed, not open, and the fear here is spatial confinement.
4.Social anxiety disorder involves fear of judgmentor embarrassment in social settings. The elevator scenario lacks social evaluation, making this diagnosis inappropriate.
Take Home Points
- Claustrophobia is a situational-specific phobia involving fear of enclosed spaces like elevators or tunnels.
- Symptoms include panic attacks, shortness of breath, and avoidance of confined environments.
- It differs from agoraphobia, which involves fear of open or escape-compromised public spaces.
- Social anxiety disorder involves fear of scrutiny, not spatial confinement.
The nurse is caring for a 45-year-old female with a history of hematophobia. The patient is scheduled for a blood draw. Which of the following is the most important physiological response for the nurse to anticipate and prepare for?
Explanation
Hematophobiais a blood-injection-injurytype of specific phobia characterized by an intense fear of blood or procedures involving blood. Unlike other phobias, it often triggers a vasovagal response, causing sudden bradycardiaand hypotension. This leads to fainting due to decreased cerebral perfusion. The physiological reaction is biphasic—initial sympathetic activation followed by abrupt parasympathetic overcompensation. This pattern is unique to BII phobias and must be anticipated during procedures like venipuncture.
Rationale for correct answers
3.The hallmark physiological response in hematophobia is vasovagal syncope, which presents as bradycardia and hypotension. This is due to parasympathetic overactivation triggered by blood-related stimuli, leading to fainting.
Rationale for incorrect answers
1.Tachycardia and hypertension reflect a sympatheticresponse typical of most phobias, but not blood-injection-injury types like hematophobia.
2.Diarrhea and abdominal cramps are gastrointestinalsymptoms more common in anxiety-related disorders, not specific to hematophobia’s vasovagal profile.
4.Hyperventilation and respiratory alkalosis are respiratorymanifestations seen in panic disorder or generalized anxiety, not in vasovagal reactions.
Take Home Points
- Hematophobia is a blood-injection-injury phobia with a unique vasovagal response: bradycardia and hypotension.
- Unlike other phobias, it may cause fainting due to parasympathetic overactivation.
- Nurses must anticipate syncope during procedures involving blood exposure.
- Differentiate hematophobia from panic disorder and generalized anxiety by its biphasic autonomic response.
A nurse is providing education to a group of nursing students on the etiology of specific phobias. The nurse explains that a phobia can develop when a neutral stimulus becomes associated with a traumatic event. This explanation is an example of which of the following psychological theories?
Explanation
Classical conditioningis a behavioral learningprocess where a neutral stimulus becomes associated with a reflexive responsethrough repeated pairing with an unconditioned stimulus. It was first described by Ivan Pavlov, who demonstrated that dogs could learn to salivate at the sound of a bell when it was consistently paired with food. In phobia development, a previously neutral stimulus (e.g., elevators) becomes linked to a traumatic experience (e.g., panic), resulting in a conditioned fearresponse. This mechanism explains how specific phobias can form even after a single distressing event.
Rationale for correct answers
3.Classical conditioningexplains how a neutral stimulus becomes a triggerfor fear after being paired with a traumatic event. The elevator becomes associated with panic symptoms, leading to a conditioned response of anxiety.
Rationale for incorrect answers
1.Observational learning involves acquiring behavior by watchingothers, not through direct pairing of stimuli and responses. It does not explain fear from personal traumatic experience.
2.Information transmission refers to acquiring fear through verbalor written communication, such as being told something is dangerous. It lacks the direct experiential pairing seen in classical conditioning.
4.Cognitive restructuring is a therapeutictechnique used to challenge and modify irrational beliefs. It is not a theory of how phobias develop but rather a method for treating them.
Take Home Points
- Classical conditioning explains how phobias form through pairing of neutral stimuli with traumatic events.
- It differs from observational learning, which involves modeling others’ behavior.
- Information transmission involves verbal acquisition of fear, not experiential conditioning.
- Cognitive restructuring is a treatment method, not a developmental theory of phobias.
A client has been diagnosed with agoraphobia. Should the therapist choose to use implosion therapy, the client would be:
Explanation
Implosion therapyis a behavioral exposuretechnique used to treat phobias by presenting the client with intense, prolonged exposure to feared stimuli. Unlike systematic desensitization, which uses gradual steps and relaxation, implosion therapy involves massive exposurewithout escape, often imaginal, until anxiety diminishes through habituation. It operates on extinction principles—repeated exposure without negative outcomes weakens the conditioned fear response. It is contraindicated in fragile clients due to its intensity and risk of overwhelming anxiety.
Rationale for correct answers
4.Implosion therapy involves massive exposureto feared stimuli, often in imagination, without allowing avoidance. This forces the client to confront anxiety until it extinguishes, aligning with the therapeutic goal of breaking avoidance patterns.
Rationale for incorrect answers
1.Relaxation exercises are part of systematicdesensitization, not implosion therapy. Implosion does not use calming techniques during exposure.
2.Graded intensities reflect gradualexposure used in systematic desensitization. Implosion therapy bypasses gradual steps and starts with high-intensity stimuli.
3.Stopping therapy upon anxiety contradicts the non-escapeprinciple of implosion therapy. Continued exposure is essential for extinction to occur.
Take Home Points
- Implosion therapy uses intense, prolonged exposure to feared stimuli to extinguish anxiety responses.
- It differs from systematic desensitization by avoiding relaxation and gradual steps.
- The therapy relies on extinction principles and prevents reinforcement of avoidance behaviors.
- It is contraindicated in clients with fragile coping or high risk of decompensation.
Practice Exercise 3
A nurse is preparing a patient with arachnophobia for exposure therapy. Which of the following is the first step in a systematic desensitization approach?
Explanation
Systematic desensitizationis a behavioral therapytechnique used to treat specific phobias by gradually exposing the individual to feared stimuliwhile pairing each exposure with relaxation techniques. It is based on classical conditioning and reciprocal inhibition—the idea that one cannot be anxious and relaxed simultaneously. The process involves constructing a fear hierarchy, teaching relaxation methods, and progressing through increasingly anxiety-provoking stimuli. This method is effective for phobias like arachnophobia, where exposure begins with mild triggers such as images or visualization before advancing to real-life encounters.
Rationale for correct answers
2.Visualizationof a spider from a distance while practicing relaxationis the first step in systematic desensitization. It introduces the least anxiety-provoking stimulus and pairs it with relaxation to inhibit fear.
Rationale for incorrect answers
1.Immediate placement of a live spider is too intenseand resembles flooding, not systematic desensitization. It bypasses the graded exposure hierarchy and risks overwhelming the patient.
3.A detailed photograph may be too provocativeearly in therapy. It represents a higher level in the fear hierarchy and is not appropriate as a starting point.
4.Describing worst fears is part of cognitivetherapy or fear hierarchy construction, not the initial exposure step. It precedes actual desensitization but is not itself exposure.
Take Home Points
- Systematic desensitization begins with mild exposure paired with relaxation to counter anxiety responses.
- It follows a structured fear hierarchy from least to most anxiety-provoking stimuli.
- The technique is grounded in classical conditioning and reciprocal inhibition principles.
- It differs from flooding, which uses immediate intense exposure without relaxation pairing.
A 28-year-old female with a severe fear of flying (aerophobia) is prescribed propranolol prior to a flight. The nurse understands that this medication is primarily intended to manage which of the following symptoms?
Explanation
Propranololis a non-selective beta-blockerused to manage cardiovascular and anxiety-related conditions. It works by blocking beta-adrenergic receptors, reducing the effects of adrenaline and noradrenaline. This leads to decreased heart rate, blood pressure, and tremors. In anxiety disorders, especially performance or situational anxiety, propranolol is used off-label to control physical symptoms like palpitations, sweating, and muscle tension. It does not affect cognitive or emotional aspects of anxiety. Contraindications include asthma, bradycardia, and uncompensated heart failure.
Rationale for correct answers
2.Propranolol targets physiological symptomsof anxiety such as palpitations and tremors by blocking beta-receptors. It reduces sympathetic nervous system activity, helping the patient remain physically calm during flight.
Rationale for incorrect answers
1.Irrational thoughts are cognitive, not physiological. Propranolol does not alter thought patterns or beliefs; cognitive therapy is required for that.
3.Unconscious conflicts are psychodynamicin nature and require insight-oriented therapy. Propranolol does not address deep psychological roots of phobias.
4.Apathy and detachment are dissociativesymptoms, not typical of aerophobia. Propranolol does not treat emotional numbing or derealization.
Take Home Points
- Propranolol is used to manage physical symptoms of anxiety, not cognitive distortions or emotional conflicts.
- It is effective for situational anxiety like fear of flying, especially when symptoms include palpitations and tremors.
- It does not cause sedation, making it suitable for patients who need to remain alert.
- Differentiate propranolol’s role from therapies targeting cognitive or unconscious aspects of phobias.
A nurse is providing care for a patient with a specific phobia of needles (trypanophobia). The nurse observes the patient becoming pale and lightheaded as the phlebotomist prepares for the blood draw. Which of the following is the most appropriate initial nursing action?
Explanation
Trypanophobiais an intense, irrational fear of needles or injections, often leading to vasovagal syncope, characterized by hypotension, bradycardia, and fainting. This response is triggered by autonomic nervous system activation. Symptoms include pallor, dizziness, and nausea. Management involves positioning, reassurance, and preventing injury. Supine positioning with leg elevationimproves cerebral perfusion and stabilizes blood pressure. Benzodiazepines are not first-line unless anxiety is severe and persistent.
Rationale for correct answers
4.Supine positioning with elevated legs enhances venous returnand cerebral perfusion, counteracting vasovagal hypotension and preventing syncope. It’s the safest immediate intervention.
Rationale for incorrect answers
1.Benzodiazepines may reduce anxiety, but they are not appropriate for acute vasovagal symptoms and may cause sedation or hypotension.
2.Ambulation during presyncopal symptoms increases risk of fallingand injury due to compromised cerebral perfusion.
3.Stopping the procedure is premature; the priority is stabilization. Physician notification can follow once the patient is safe.
Take Home Points
- Trypanophobia can trigger vasovagal syncope requiring immediate physical stabilization.
- Supine positioning with leg elevation is the first-line response to presyncopal symptoms.
- Benzodiazepines are reserved for persistent anxiety, not acute vasovagal episodes.
- Differentiate vasovagal syncope from panic attacks and orthostatic hypotension based on autonomic signs.
A client tells a nurse about an intense fear of dogs that causes the client to avoid visiting others unless it is confirmed that there are no dogs on the premises. The client further explains that these fears seem unreasonable, but the fear continues in spite of this acknowledgment. Based on the client’s report, which conclusion by the nurse is accurate?
Explanation
Specific phobiais a marked and persistent fear of a clearly identifiable object or situation, which is excessive, irrational, and leads to avoidance behavior. The fear is recognized by the individual as unreasonable, yet remains distressing and impairing. Symptoms must persist for at least 6 monthsand cause significant functional interference. Common types include animal, situational, and blood-injection-injury phobias. Onset typically occurs in childhood or adolescence, and prevalence is higher in womenthan men.
Rationale for correct answers
2.The DSM-5 defines specific phobia as a persistent, excessive fearthat is recognized as irrational by the individual, yet still causes avoidance and distress. This aligns with the client’s self-awareness and behavior.
Rationale for incorrect answers
1.The presence of avoidance and distress indicates psychopathology, even if the fear is recognized. Recognition does not negate clinical significance.
3.Specific phobias are among the most commonanxiety disorders, with lifetime prevalence estimates around 12%, making them far from rare.
4.Although onset often occurs in childhood, phobias are more frequently diagnosed in females, not males. The gender distribution contradicts the statement.
Take Home Points
- Specific phobia involves excessive, irrational fear of a specific object or situation, recognized by the individual.
- Avoidance behavior and functional impairment are key diagnostic criteria.
- Phobias are common and more prevalent in females than males.
- Differentiate specific phobia from generalized anxiety and panic disorder based on stimulus specificity.
A nurse is caring for a client who was violently raped 3 months ago and has a diagnosis of rape-trauma syndrome. Which assessment findings associated with rape-trauma syndrome should a nurse anticipate? Select all that apply.
Explanation
Rape-trauma syndromeRape-trauma syndromeis a cluster of psychological and somatic responses following sexual assault, often resembling PTSD. It includes intrusive recollections, avoidance, hyperarousal, and somatic symptoms. Victims may develop phobias, eating disturbances, and chronic pain. Flashbacks and migraines are common due to heightened stress reactivity. The syndrome can persist for months or years and requires trauma-informed care. Sleep disturbances, sexual dysfunction, and emotional numbing are also prevalent.
Rationale for correct answers
1.Phobias often emerge post-trauma due to conditioned fearresponses, especially when the assault involved specific triggers like location or people.
2.Anorexia may result from emotional distress, loss of control, or body image disturbances following sexual trauma, affecting appetite and nutrition.
3.Flashbacks are hallmark features of PTSD, involving vivid re-experiencing of the traumatic event, often triggered by sensory or emotional cues.
6.Migraine headaches are linked to somatic stress, with increased muscle tension and neurovascular changes following trauma contributing to chronic pain.
Rationale for incorrect answers
4.Hypertension is not a consistent feature of rape-trauma syndrome; acute stressmay cause transient elevation, but not sustained blood pressure changes.
5.Sexual promiscuity is not a diagnostic or expected outcome; trauma often leads to avoidanceof sexual activity due to fear or emotional detachment.
Take Home Points
- Rape-trauma syndrome includes psychological and somatic symptoms resembling PTSD, such as flashbacks and phobias.
- Somatic symptoms like migraines and anorexia are common due to stress-related neuroendocrine dysregulation.
- Sexual trauma often leads to avoidance behaviors, not increased sexual activity.
- Differentiate rape-trauma syndrome from generalized anxiety and depression based on trauma-specific re-experiencing and avoidance.
Comprehensive Questions
A nurse is caring for a client who does not go outdoors due to agoraphobia and also has an inadequate milk intake. For which vitamin deficiency should the nurse specifically assess when caring for this client?
Explanation
Vitamin D deficiencyoccurs due to inadequate sunlight exposure, poor dietary intake, or malabsorption. It impairs calcium absorption, leading to bone demineralization, muscle weakness, and increased fracture risk. The skin synthesizes vitamin D when exposed to UVB rays; 15–30 minutes of midday sun several times a week is typically sufficient. Fortified dairy products are major dietary sources. Deficiency is common in individuals with limited outdoor activity, dark skin, or low intake of fortified foods.
Rationale for correct answers
3.Lack of sunlight and poor dairy intake directly reduce vitamin Dsynthesis and dietary absorption, increasing risk for deficiency and bone complications.
Rationale for incorrect answers
1.Vitamin B6 deficiency is linked to neuropathy, but it’s not primarily associated with reduced sunlight or dairy intake.
2.Vitamin A is mainly obtained from animal sourcesand vegetables; its deficiency is unrelated to outdoor activity or milk consumption.
4.Vitamin C deficiency results from low fruitand vegetable intake, not lack of sun exposure or dairy avoidance.
Take Home Points
- Vitamin D deficiency is common in individuals with limited sun exposure and low intake of fortified dairy products.
- Deficiency leads to impaired calcium absorption, bone pain, and increased fracture risk.
- Differentiate vitamin D deficiency from B6 and C deficiencies based on source and clinical presentation.
- Assess lifestyle factors such as agoraphobia or dietary restrictions when evaluating nutritional deficiencies.
A nurse is assessing a client who struggles with social phobia. Which assessment question does the nurse need to ask?
Explanation
Social phobia, also called social anxiety disorder, is a persistent fear of social situationswhere one may be scrutinized or judged. It often leads to avoidance, impaired functioning, and distress. Individuals may fear embarrassment, rejection, or humiliation. Substance use, especially alcohol, is common as a maladaptive coping strategy to reduce anxiety in social settings. Symptoms must persist for at least 6 months and interfere with occupational or interpersonal functioning.
Rationale for correct answers
1.Substance use is frequently associated with social phobia as individuals attempt to self-medicateanxiety symptoms, especially in social contexts.
Rationale for incorrect answers
2.Anger outlets are more relevant to impulsecontrol disorders or personality disorders, not typically associated with social phobia.
3.Impulse control issues are not characteristic of social phobia; the disorder involves inhibition, not impulsivity.
4.Underachievement may result from avoidance, but it is not a diagnostic or predictivefeature of social phobia.
Take Home Points
- Social phobia involves intense fear of social scrutiny and avoidance of social interactions.
- Substance use is a common maladaptive coping mechanism in individuals with social anxiety.
- Impulsivity and anger expression are not core features of social phobia.
- Differentiate social phobia from avoidant personality disorder and generalized anxiety based on situational specificity.
A client with the nursing diagnosis of fear related to being embarrassed in the presence of others exhibits symptoms of social phobia. What should be the goals for this client? Select all that apply.
Explanation
Social phobia, or social anxiety disorder, is a persistent fear of social interactionsinvolving scrutiny, judgment, or embarrassment. It leads to avoidance, emotional distress, and impaired functioning. Individuals often fear public speaking, meeting new people, or being observed. Treatment includes cognitive-behavioral therapy, exposure techniques, and sometimes pharmacologic support. Goals of care focus on emotional processing, behavioral adaptation, and developing coping strategies to manage anxiety in social contexts.
Rationale for correct answers
1.Managing fear in group settings promotes exposureand desensitization, which are central to behavioral therapy for social anxiety.
3.Verbalizing feelings helps with emotional regulationand insight, reducing internal distress and improving therapeutic engagement.
4.Developing a response plan enhances copingand self-efficacy, allowing the client to navigate anxiety-provoking situations with structured support.
Rationale for incorrect answers
2.Avoidance reinforces fearand impairs recovery; therapeutic goals aim to reduce avoidance through gradual exposure.
5.Denial prevents processingof emotions and obstructs therapeutic progress; acknowledgment is essential for healing.
6.Suppression delays emotional resolutionand may worsen anxiety symptoms; expression and reflection are more effective strategies.
Take Home Points
- Social phobia involves fear of embarrassment and judgment in social settings, leading to avoidance and distress.
- Therapeutic goals focus on exposure, emotional expression, and coping strategy development.
- Avoidance and suppression hinder recovery and reinforce anxiety.
- Differentiate social phobia from panic disorder and avoidant personality disorder based on situational triggers and behavioral patterns.
Which of the following is the most appropriate therapy for a client with agoraphobia?
Explanation
Agoraphobiais a marked fear or anxiety about situations where escape may be difficult or help unavailable, such as crowds, open spaces, or public transport. It often leads to avoidance and functional impairment. Treatment involves exposure therapy, where the client gradually confronts feared situations in a controlled, stepwise manner. This desensitizes the anxiety response and builds coping skills. Pharmacologic support may be used adjunctively but is not curative.
Rationale for correct answers
3.Gradual exposure is the most effective behavioral interventionfor agoraphobia, promoting desensitization and mastery over feared situations.
Rationale for incorrect answers
1.Valium (diazepam) may reduce acute anxiety, but long-term use risks dependence and does not address the underlying phobic avoidance.
2.Group therapy may increase distressin agoraphobic clients who fear social or public settings, making it less suitable initially.
4.Hypnosis lacks consistent evidencefor efficacy in treating agoraphobia and does not provide structured behavioral retraining.
Take Home Points
- Agoraphobia involves fear of situations where escape is difficult, leading to avoidance and isolation.
- Gradual exposure therapy is the most effective treatment for long-term improvement.
- Benzodiazepines may offer short-term relief but are not first-line due to dependence risk.
- Differentiate agoraphobia from panic disorder and social anxiety based on situational triggers and avoidance patterns.
A client was raped 6 months ago. Which symptom(s) should you anticipate for long-term successful outcomes? Select all that apply.
Explanation
Post-traumatic stress disorder (PTSD)PTSD is a psychiatric condition triggered by exposure to traumatic events such as sexual assault. It involves persistent hyperarousal, intrusive memories, and avoidance behaviors. Long-term recovery includes restoration of interpersonal trust, emotional regulation, and recognition of personal boundaries. Symptoms evolve over time, with acute responses like shock and fear often giving way to adaptive coping and reintegration. DSM-5 criteria emphasize functional impairment lasting over one month, with symptoms grouped into intrusion, avoidance, negative alterations in cognition/mood, and arousal/reactivity.
Rationale for correct answers
1.Interpersonal trustis a key marker of recovery. Comfort in relationships reflects emotional healing and reduced hypervigilance, indicating progress in trauma resolution.
3.Personal boundariesare often violated during trauma. Recognizing the right to protection shows restored self-worth and empowerment, essential for long-term recovery.
6.Emotional regulationimproves with therapy and time. Replacing anxiety with calmness reflects successful coping mechanisms and reduced physiological arousal.
Rationale for incorrect answers
2.Shock and numbness are acute phase reactions, typically seen immediately after trauma. Persistence at six months suggests unresolved PTSD, not recovery.
4.Fear of sexual encounters indicates ongoing avoidance and hyperarousal. It reflects continued trauma-related distress, not a successful outcome.
5.Dreams with violent content are intrusive symptoms. Their presence at six months suggests persistent re-experiencing, not resolution.
7.Phobia of being alone may not be present in all trauma survivors, but its absence alone doesn’t indicate recovery. It’s not a reliable marker of long-term outcome.
Take Home Points
- Long-term recovery from PTSD includes restored interpersonal trust and emotional regulation.
- Acute symptoms like shock and intrusive dreams should diminish over time with effective intervention.
- Recognition of personal rights and boundaries reflects psychological empowerment post-trauma.
- Persistent avoidance and hyperarousal symptoms indicate unresolved PTSD and require further intervention.
A client diagnosed with social phobia has an outcome that states, “Client will voluntarily participate in group activities with peers by day 3.” Which would be an appropriate intrapersonal intervention by the nurse to assist the client to achieve this outcome?
Explanation
Social anxiety disorderis a persistent, intense fearof social or performance situations where the person may be scrutinized by others. It often causes avoidance behavior, low self-esteem, and impaired functioning. Symptoms may include tachycardia, sweating, trembling, and intense worry before and during social interactions. Treatment includes cognitive-behavioral therapyand SSRIs, while benzodiazepines are generally short-term options. Behavioral strategies like exposureand role-play improve functioning by gradually increasing confidence and reducing anticipatory anxiety.
Rationale for correct answers
4. Role-playallows clients to mentally rehearse and emotionally prepare for the feared scenario, which reduces anticipatory anxietyand builds confidence for actual group participation. It is an effective intrapersonalcognitive-behavioral technique.
Rationale for incorrect answers
1.Although lorazepamreduces acute anxiety, it is not an intrapersonal intervention and does not support skill-building or long-term independence in social functioning.
2.Accompanying the client involves interpersonalsupport, not an intrapersonal approach. It may foster dependence and doesn’t build self-directed coping skills.
3.Discussing fearsis valuable but remains in the insight phase. It does not provide practical behavioral rehearsal needed for goal achievement within the time frame.
Take Home Points
- Social anxiety disorder requires structured behavioral interventions to reduce avoidance and enhance social skills.
- Intrapersonal interventions involve cognitive or behavioral techniques the client applies themselves.
- Role-play helps reduce anticipatory anxiety and build confidence before real-life exposure.
- Short-term pharmacologic interventions may help but are not substitutes for skill-building therapies.
In which situation would the nurse suspect a medical diagnosis of social phobia?
Explanation
Social phobiaSocial phobia, also known as social anxiety disorder, is marked by persistent fear of social situations where one may be judged, embarrassed, or humiliated. Symptoms include avoidance, intense anxiety, and physical signs like sweating or trembling. The DSM-5 requires symptoms to persist for at least 6 months, cause functional impairment, and not be attributable to substances or medical conditions. Performance-only specifier applies when anxiety is limited to public speaking or presentations.
Rationale for correct answers
4.The fear of being scrutinized during oral presentations aligns with performance-onlysocial anxiety. The DSM-5 recognizes this subtype when anxiety is limited to public speaking, and the avoidance behavior is disproportionate and persistent.
Rationale for incorrect answers
1.The avoidance here is secondary to substanceuse, which excludes a diagnosis of social phobia. DSM-5 criteria require that symptoms not be due to drugs or medications.
2.The child shows selective anxiety toward adults but maintains peerrelationships, which contradicts DSM-5 criteria requiring distress in peer settings for children.
3.Avoidance due to Parkinson’s-related tremors and drooling is linked to a medicalcondition. DSM-5 excludes social anxiety diagnosis when symptoms are better explained by physical illness.
Take Home Points
- Social phobia involves persistent fear of negative evaluation in social or performance settings.
- DSM-5 requires symptoms to last ≥6 months and cause functional impairment.
- Performance-only subtype includes fear limited to public speaking or presentations.
- Must differentiate from anxiety due to substances, medical conditions, or selective mutism in children.
A newly admitted client diagnosed with social phobia has a nursing diagnosis of social isolation related to fear of ridicule. Which outcome is appropriate for this client?
Explanation
Social isolation in social phobiaSocial isolation in social phobiastems from persistent fear of negative evaluation in social settings. Individuals may avoid interactions due to embarrassment, leading to impaired functioning. DSM-5 requires symptoms to last ≥6 months and cause distress. Treatment includes CBTand gradual exposure. Goals should target measurable social engagement, not just symptom relief or medication use.
Rationale for correct answers
1.Participation in group activities reflects behavioral activation, a core therapeutic goal in social phobia. It directly addresses isolation and fear of ridicule through exposure and social reinforcement.
Rationale for incorrect answers
2.While relaxation reduces physiologicalsymptoms, it does not directly address avoidance or social engagement, making it insufficient as a primary outcome.
3.Verbalizing a positive attribute supports self-esteem, but it lacks specificity in addressing social interaction or measurable engagement in group settings.
4.Requesting medication PRN reflects avoidancebehavior and reliance on pharmacologic coping, which does not align with therapeutic goals of independent social functioning.
Take Home Points
- Social phobia involves persistent fear of scrutiny and avoidance of social settings.
- Outcomes should focus on measurable social engagement, not just symptom relief.
- CBT and exposure therapy are first-line treatments for social anxiety disorder.
- Differentiate social phobia from generalized anxiety, selective mutism, and substance-induced anxiety.
A nurse is counseling the family of a child with school phobia. What should the parents be taught to do?
Explanation
School phobiais a form of specific phobiamarked by intense fear or anxiety about attending school. It often presents with somatic symptomslike nausea, headaches, or abdominal pain, and may be linked to separation anxiety or social fears. DSM-5 criteria require symptoms to persist for ≥6 months and cause functional impairment. Treatment focuses on gradual exposure, cognitive restructuring, and restoring school attendance as quickly as possible to prevent reinforcement of avoidance behavior.
Rationale for correct answers
2.Returning the child to school immediately interrupts avoidance patternsand reinforces normal routine. Early re-entry prevents reinforcement of fear and supports behavioral recovery.
Rationale for incorrect answers
1.Accompanying the child reinforces dependency, which can worsen separation anxiety and delay independent coping with school-related stress.
3.Instruction alone does not address emotionalresistance or anxiety. Rational explanations are ineffective during acute phobic responses.
4.Allowing early entry may reduce exposure, limiting the child’s ability to adapt to normal peer interactions and routine transitions.
Take Home Points
- School phobia involves intense fear of attending school, often with physical symptoms and avoidance behavior.
- Immediate return to school is essential to prevent reinforcement of avoidance and promote recovery.
- Parental overprotection and delayed re-entry can worsen symptoms and prolong school refusal.
- Differentiate school phobia from truancy, separation anxiety, and generalized anxiety disorder.
A nurse is interviewing a client with a phobia. Which treatment should the nurse inform the client has the highest success rate?
Explanation
Systematic desensitizationis a behavioral therapyused to treat phobias by gradually exposing individuals to feared stimuli while teaching relaxation techniques. It is based on reciprocal inhibition, where relaxation inhibits anxiety. The process involves creating an anxiety hierarchy and progressing from least to most distressing situations. Sessions typically range from 4 to 12 depending on severity. It has a success rate of 80–90%for specific phobias and is considered the most effective intervention for long-term resolution.
Rationale for correct answers
2.Systematic desensitization combines exposureand relaxation, directly targeting the conditioned fear response. It retrains the brain through gradual exposure, making it the most effective and evidence-based treatment for phobias.
Rationale for incorrect answers
1.Insight therapy focuses on origin, not symptom resolution. Understanding the cause does not reduce conditioned fear or avoidance behavior.
3.Psychotic thought processes are treated with antipsychotics, not relevant in phobia, which involves anxiety and conditioned avoidance, not delusions.
4.Psychoanalytic methods explore repression, which lacks empirical support for treating phobias. It is less structured and slower than behavioral approaches.
Take Home Points
- Systematic desensitization is the most effective treatment for specific phobias.
- It uses graded exposure and relaxation to counter conditioned fear responses.
- Insight and psychoanalytic therapies are less effective for phobia resolution.
- Differentiate phobias from psychotic disorders and generalized anxiety.
A client who has a phobia about dogs is about to begin systematic desensitization. The client asks what the treatment will involve. What is the nurse’s best response?
Explanation
Systematic desensitizationis a behavioral therapyused to treat specific phobias by gradually exposing the individual to the feared stimulus while practicing relaxation techniques. It is based on reciprocal inhibition, where relaxation inhibits anxiety. The process involves creating a fear hierarchy and progressing from least to most distressing stimuli. This method is highly effective for animal phobias like cynophobia, with success rates exceeding 80% when properly implemented.
Rationale for correct answers
3.This response describes the core mechanism of systematic desensitization, which involves gradual exposureto the feared object while using relaxation to counter anxiety. It reflects the structured therapeutic approach used in clinical settings.
Rationale for incorrect answers
1.Continuous exposure without relaxation can lead to flooding, which may worsen anxiety and cause emotional overwhelm rather than therapeutic progress.
2.Reward-based approaches reflect operant conditioning, not systematic desensitization. They do not address the conditioned fear response central to phobias.
4.In-depth discussion of origins aligns with psychoanalytictherapy, which lacks empirical support for treating specific phobias and does not involve exposure techniques.
Take Home Points
- Systematic desensitization treats phobias through gradual exposure paired with relaxation.
- It is based on classical conditioning and reciprocal inhibition principles.
- Flooding and psychoanalytic methods are less effective and may increase distress.
- Differentiate systematic desensitization from operant conditioning and insight-oriented therapies.
What childhood problem has legal as well as emotional aspects and cannot be ignored?
Explanation
School phobiais an emotional condition where a child refuses to attend school due to underlying anxietyor psychological distress. It may present with physical symptoms like headaches or nausea and often involves significant family dynamics. It is multifactorial, involving both emotional suffering and external consequences such as truancy laws, making it a matter with legalimplications. It can be mistaken for defiance but is rooted in fear, requiring early intervention. Left unaddressed, it can escalate to chronic absenteeism and impact social, academic, and legal outcomes.
Rationale for correct answers
1. School phobiahas both emotionaland legalimplications. The emotional aspect involves separation anxiety or social fears; the legal aspect arises when school absenteeism violates mandatory attendance laws, potentially leading to parental accountability.
Rationale for incorrect answers
2.Fear of animals is common in children and falls under normal developmental fears. It lacks legal consequence and typically resolves with reassurance or desensitization. It is not associated with educational neglect or systemic intervention.
3.Monsters are a typical fear in early childhood, especially around ages 3–6. They are developmentally appropriate and handled emotionally within the home environment without any legal dimension or mandatory reporting.
4.Sleep disturbances may stem from various causes like anxiety, trauma, or medical issues. While they affect well-being and may co-occur with emotional disorders, they do not have direct legal implications unless tied to neglect or abuse.
Take Home Points
- School phobia involves refusal to attend school due to anxiety, with both emotional and legal consequences.
- Developmental fears like fear of animals or monsters are common but typically do not require legal intervention.
- Chronic absenteeism from school due to emotional causes may lead to legal action against guardians.
- Early identification and support for school phobia prevent academic failure, social withdrawal, and systemic consequences.
In what situation should a nurse anticipate that a client will experience a phobic reaction?
Explanation
A phobic reaction is an immediate, intense fear responsetriggered by exposure to a specific object or situation. According to DSM-5, the reaction must be out of proportionto actual danger, provoke anxietyalmost instantly, and lead to avoidance or distress. Symptoms include tachycardia, sweating, trembling, and panic. The reaction occurs upon direct contact with the feared stimulus, not merely thinking about it or being in unfamiliar settings.
Rationale for correct answers
3.Contact with the feared object activates the amygdala, triggering a fight-or-flightresponse. This leads to acute anxiety symptoms such as palpitations, hyperventilation, and panic, consistent with DSM-5 diagnostic criteria.
Rationale for incorrect answers
1.Seeking attention is a behavioralmotive, not a diagnostic trigger. Phobic reactions are involuntary and rooted in anxiety, not social reinforcement.
2.Thinking about the object may cause anticipatoryanxiety, but it does not consistently provoke the immediate physiological response required for a phobic reaction.
4.Unfamiliar environments may cause generalizedanxiety, not specific phobic responses. Phobias are tied to distinct stimuli, not novelty or unfamiliarity.
Take Home Points
- Phobic reactions occur upon direct exposure to the feared object or situation.
- DSM-5 requires immediate anxiety, avoidance, and disproportionate fear lasting ≥6 months.
- Anticipatory anxiety is not sufficient for diagnosis without physical symptoms during exposure.
- Differentiate phobic reactions from attention-seeking, generalized anxiety, and novelty-related stress.
A client with the nursing diagnosis of fear related to being embarrassed in the presence of others exhibits symptoms of social phobia. What should be the goals for this client? Select all that apply.
Explanation
Social phobia, also called social anxiety disorder, is marked by persistent fear of social situations where one may be judgedor humiliated. Symptoms include avoidance, intense anxiety, and physical signs like sweating or trembling. DSM-5 requires symptoms to persist for ≥6 months and cause functional impairment. Treatment goals focus on improving coping, reducing avoidance, and enhancing social functioning through CBT, exposure therapy, and emotional processing.
Rationale for correct answers
1.Managing fear in group settings promotes exposureand behavioral activation, which are central to CBT-based treatment for social phobia.
3.Verbalizing feelings supports emotional processing, helping the client identify and challenge irrational beliefs that fuel anxiety.
4.Developing a response plan enhances copingand self-efficacy, allowing the client to navigate feared situations with reduced distress.
Rationale for incorrect answers
2.Avoidance reinforces the phobia, worsening symptoms over time and contradicting therapeutic goals focused on exposure and engagement.
5.Denial prevents insight, limiting emotional awareness and blocking progress in therapy by suppressing key cognitive distortions.
6.Suppression leads to internalization, increasing anxiety and distress rather than resolving the underlying fear through therapeutic techniques.
Take Home Points
- Social phobia involves persistent fear of scrutiny and avoidance of social situations.
- Treatment goals should focus on exposure, emotional expression, and coping strategy development.
- Avoidance and suppression worsen symptoms and hinder therapeutic progress.
- Differentiate social phobia from generalized anxiety, selective mutism, and personality disorders.
Fear restricted to a particular object, situation, or place is known as:
Explanation
Phobiais a type of anxiety disordercharacterized by intense, irrational fear of a specific object, situation, or place. The fear response is immediateand disproportionate to actual danger, leading to avoidance behavior. DSM-5 criteria require symptoms to persist for ≥6 months and cause significant distress or impairment. Common physical symptoms include tachycardia, sweating, and shortness of breath. Treatment includes exposure therapy and cognitive restructuring.
Rationale for correct answers
3.The fear is tied to a specific stimulus, and exposure provokes immediate anxiety. This fits the DSM-5 definition of a phobia, which is restricted to particular triggers and leads to avoidance.
Rationale for incorrect answers
1.Attention-seeking is a behavioralmotive, not a diagnostic feature. Phobias are involuntary and rooted in anxiety, not social gain.
2.Thinking about the object may cause anticipatoryanxiety, but it does not consistently provoke the acute response required for diagnosis.
4.Unfamiliar environments may trigger generalizedanxiety, not phobic reactions. Phobias are linked to specific, identifiable stimuli.
Take Home Points
- Phobia involves intense fear of a specific object, situation, or place.
- DSM-5 requires immediate anxiety, avoidance, and disproportionate fear lasting ≥6 months.
- Phobias differ from generalized anxiety and attention-seeking behaviors.
- Treatment includes exposure therapy and cognitive behavioral techniques.
Exams on Specific Phobia
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
Upon completion of this module, the student nurse will be able to:
- Define specific phobia in a scientific and medically accurate manner.
- Differentiate between various types of specific phobias, including their characteristic presentations.
- Identify the etiological factors and pathophysiological mechanisms implicated in the development of specific phobias.
- Formulate a comprehensive nursing care plan for a patient experiencing specific phobia.
- Articulate the evidence-based therapeutic interventions for specific phobia, including cognitive-behavioral therapy (CBT) and pharmacological modalities.
- Apply nursing insights to ensure the provision of safe, effective, and patient-centered care.
Introduction
- Specific phobia is an anxiety disorder characterized by a persistent, irrational, and excessive fear of a specific object or situation.
- This fear is disproportionate to the actual danger posed by the stimulus and often leads to avoidance behaviors that significantly impair the individual's occupational, social, and academic functioning.
- The American Psychiatric Association's Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), categorizes specific phobia within the anxiety disorders spectrum.
- The prevalence of specific phobias is estimated to be approximately 7-9% of the population, with onset typically occurring in childhood or early adolescence.
- The condition is more common in females than in males.
- The primary clinical manifestation is an immediate and intense anxiety response, often escalating to a panic attack, upon exposure to the feared object or situation.
- This response can include a constellation of physiological symptoms such as palpitations, diaphoresis, shortness of breath, and dizziness.
Description
- Specific phobia is an anxiety disorder defined by an intense and unreasonable fear of a specific object or situation.
- The fear is persistent, lasting for six months or more, and is not merely a transient feeling of anxiety.
- This fear is a marked and immediate response, and it is almost invariably triggered by the presence or anticipation of the specific phobic stimulus.
- The individual with a specific phobia recognizes that their fear is irrational and excessive, but they are unable to control their emotional and physiological reactions.
- This awareness of the irrationality of the fear is a key diagnostic criterion, though it may be absent in young children.
- The phobic object or situation is actively avoided or is endured with significant distress and anxiety.
- This avoidance behavior is a primary feature of the disorder and is often the reason for the individual seeking professional help.
- The avoidance can lead to significant functional impairment, disrupting daily routines, relationships, and professional responsibilities.
- The fear and avoidance are not better explained by another mental disorder, such as obsessive-compulsive disorder or post-traumatic stress disorder.
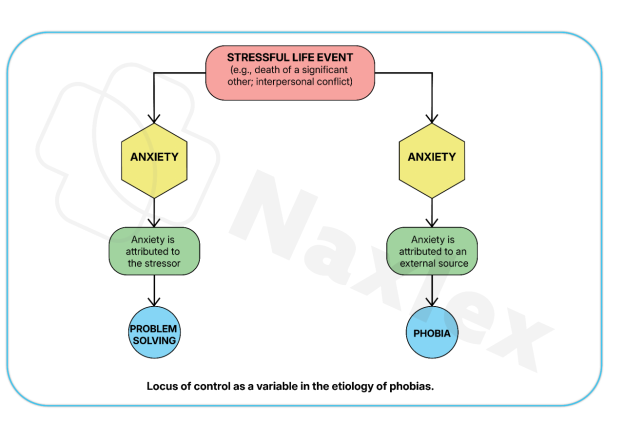
- Etiological Factors: The etiology of specific phobias is multifactorial and involves a complex interplay of genetic, neurobiological, and psychological factors.
- Genetic Predisposition: There is a strong familial component, with a higher prevalence of anxiety disorders among first-degree relatives of individuals with specific phobias. Twin studies have indicated a significant heritability for these conditions.
- Neurobiological Mechanisms: The amygdala, a brain region crucial for processing fear and emotional responses, plays a central role. The phobic stimulus activates the amygdala, triggering a cascade of physiological responses mediated by the hypothalamic-pituitary-adrenal (HPA) axis and the sympathetic nervous system. This results in the "fight-or-flight" response. Neurotransmitter systems, particularly those involving serotonin and gamma-aminobutyric acid (GABA), are also implicated.
- Psychological Theories:
- Classical Conditioning: The development of a phobia can be explained by classical conditioning, where a neutral stimulus becomes associated with a traumatic or frightening event. For example, a dog bite (unconditioned stimulus) leads to fear (unconditioned response). A dog (previously neutral stimulus) becomes a conditioned stimulus, and the sight of a dog elicits a conditioned fear response.
- Observational Learning: Individuals may acquire a phobia by observing the fearful reactions of others, such as a parent's intense fear of spiders.
- Information Transmission: A person can develop a phobia after being repeatedly warned about the dangers of a specific object or situation, even without direct personal experience.
- Pathophysiology: Exposure to the phobic stimulus activates the sympathetic nervous system, leading to the release of catecholamines, such as epinephrine and norepinephrine. This results in a cascade of physiological changes:
- Increased heart rate and blood pressure (tachycardia and hypertension).
- Rapid, shallow breathing (tachypnea).
- Diaphoresis (sweating).
- Pupil dilation (mydriasis).
- Peripheral vasoconstriction, leading to a feeling of coldness or tingling.
- Gastrointestinal distress, such as nausea or abdominal pain.
- Dizziness, lightheadedness, and feelings of unreality (derealization or depersonalization).
Nursing Insights:
- The nurse must be able to differentiate between a specific phobia and a generalized anxiety disorder.
- While both involve anxiety, a specific phobia is tied to a specific, identifiable trigger, whereas generalized anxiety disorder is characterized by a pervasive, free-floating anxiety that is not limited to a specific situation or object.
- Recognizing the specific trigger is crucial for developing a targeted nursing care plan that focuses on gradual exposure and desensitization.
-
The nurse should also be aware that individuals with specific phobias may be at increased risk for developing other anxiety disorders, depression, and substance use disorders.
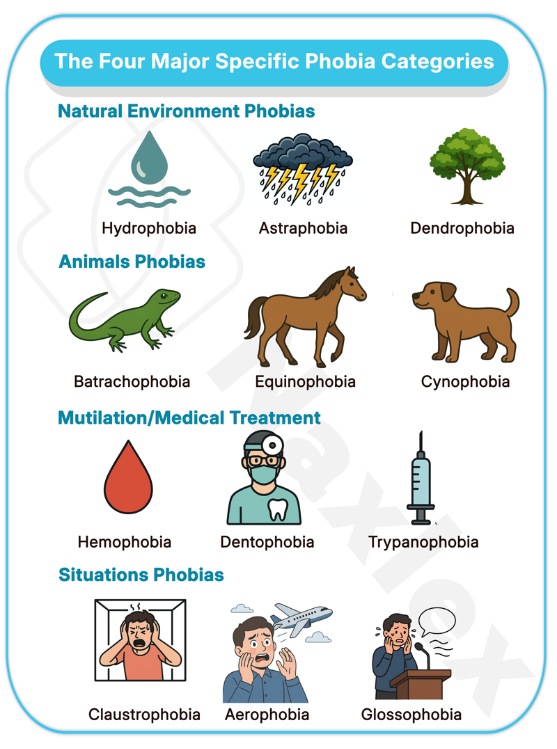
Types
- Specific phobias are categorized into five subtypes in the DSM-5 based on the phobic stimulus: animal, natural environment, blood-injection-injury, situational, and other.
- The following are common examples of specific phobias, some of which fall under these subtypes.
- Specific Phobia Categories: Specific phobias are classified into distinct categories based on the nature of the feared object or situation. Below is an organized summary of these categories.
- Natural Environmental Phobias
- Involve fears of natural phenomena such as storms, water, or heights.
- Blood-Injection Phobias
- Characterized by fear of seeing one’s own or others’ blood, traumatic injuries, or invasive medical procedures like injections.
- Situational Phobias
- Involve fear of specific situations, such as being on a bridge, in a tunnel, elevator, small room, hospital, or airplane.
- Animal Phobias
- Involve fear of specific animals or insects, often developing in childhood and persisting into adulthood for both men and women.
- Common phobic objects include cats and dogs.
- Other Types of Specific Phobias
- Include unique fears, such as the fear of getting lost while driving if unable to make all right turns (and no left turns) to reach a destination.
- Include unique fears, such as the fear of getting lost while driving if unable to make all right turns (and no left turns) to reach a destination.
1.1 Acrophobia: Fear of heights
- Acrophobia is a profound and irrational fear of heights.
- Individuals with acrophobia experience severe anxiety or panic when in high places, such as on a tall building, a bridge, or a mountain.
- This fear often leads to a physical sensation of vertigo or dizziness, which is distinct from actual vertigo.
- Avoidance behaviors include refusing to use elevators with glass walls, avoiding balconies, and declining invitations to activities that involve being at an elevated location.
1.2 Agoraphobia: Fear of open spaces
- Agoraphobia is a fear of situations where escape might be difficult or help might not be available if panic-like symptoms or other incapacitating or embarrassing symptoms occur.
- This fear often centers on being in open spaces, public transportation, large crowds, or being outside the home alone.
- The fear is typically of the situation itself, rather than a specific object.
- Agoraphobia is a separate diagnosis in the DSM-5 and is not a subtype of specific phobia.
- It is often a complication of panic disorder.
-
Nursing Insights:
- It is imperative for the nursing student to understand the distinction between agoraphobia and specific phobia.
- While agoraphobia may involve fear of open spaces, it is fundamentally a fear of experiencing a panic attack or other incapacitating symptoms in a situation where escape is difficult.
- A specific phobia of heights (acrophobia), in contrast, is a fear of the height itself.
- This distinction is critical for accurate diagnosis and the selection of appropriate therapeutic interventions.
1.3 Astraphobia: Fear of electrical storms
- Astraphobia is an intense and irrational fear of thunder and lightning.
- Individuals with astraphobia may experience extreme anxiety, panic, and avoidance behaviors during electrical storms.
- They may seek shelter, hide under beds, or engage in compulsive behaviors to avoid the perceived threat.
- This phobia is particularly common in children and can be debilitating.
1.4 Claustrophobia: Fear of closed spaces
- Claustrophobia is the intense fear of being in enclosed or confined spaces.
- This phobia can be triggered by situations such as being in an elevator, a small room, or an MRI machine.
- The individual may experience a feeling of suffocation or being trapped, leading to a panic attack.
- Avoidance of these situations is a hallmark of the disorder.
1.5 Hematophobia: Fear of blood
- Hematophobia is a specific phobia of blood, injuries, or injections.
- This phobia is unique in that it often elicits a vasovagal response, leading to a drop in heart rate and blood pressure, which can result in fainting (syncope).
- This is in contrast to most other phobias, which cause an increase in heart rate and blood pressure.
- The fear is not only of seeing blood but also of the sight of injuries, injections, or medical procedures.
-
Nursing Insights:
- When caring for a patient with hematophobia, the nurse must be aware of the vasovagal response.
- Unlike other phobias that trigger a sympathetic "fight-or-flight" response, hematophobia can trigger a parasympathetic response.
- The nurse must be prepared to manage potential syncope by ensuring the patient is in a supine position before any procedure involving needles or blood.
- Reassuring the patient and using distraction techniques are essential components of care.
1.6 Hydrophobia: Fear of water
- Hydrophobia is the irrational fear of water.
- This phobia can be triggered by various situations, such as being near a body of water, swimming, or even thinking about water.
- It can significantly impact an individual's life, as they may avoid bathing, drinking water, or going to the beach.
- The term hydrophobia is also used to describe a symptom of rabies, which is a different clinical entity.
1.7 Monophobia: Fear of being alone
- Monophobia is the persistent and irrational fear of being alone.
- This fear can lead to significant distress and impairment, as the individual may avoid living alone, staying in a room by themselves, or even being left for a short period.
- This phobia is often associated with a fear of a lack of help if an emergency were to occur.
1.8 Mysophobia: Fear of dirt or germs
- Mysophobia is an excessive and irrational fear of dirt, germs, or contamination.
- This phobia can lead to compulsive behaviors such as excessive handwashing, cleaning, or avoidance of public places.
- It is often a key feature of obsessive-compulsive disorder (OCD), but it can also exist as a standalone specific phobia.
- The distinction lies in whether the fear is a single, isolated symptom or part of a broader pattern of obsessions and compulsions.
1.9 Nyctophobia: Fear of darkness
- Nyctophobia is an extreme and irrational fear of the dark.
- This phobia is most common in children but can persist into adulthood.
- The fear is not of the darkness itself, but of the imagined dangers or events that might occur in the dark.
- It can lead to significant sleep disturbances and avoidance of activities that take place at night.
2.0 Pyrophobia: Fear of fires
- Pyrophobia is the irrational and excessive fear of fire.
- This phobia can be triggered by the sight or smell of smoke, the sound of a fire alarm, or even a picture of fire.
- Individuals with pyrophobia may avoid fireplaces, campfires, and cooking with an open flame.
2.1 Social Phobia (Social Anxiety Disorder): Fear of social situations
- Social phobia, now termed social anxiety disorder in the DSM-5, is a distinct anxiety disorder characterized by a persistent fear of social or performance situations in which one might be scrutinized, judged, or embarrassed.
- This fear is not of a specific object but of a social context.
- It is a separate diagnosis from specific phobia.
- Diagnostic Criteria for Social Phobia (Social Anxiety Disorder)
- There is a marked and persistent fear of one or more social or performance situations in which the individual is exposed to:
• Unfamiliar people
• Possible scrutiny by others
- There is a marked and persistent fear of one or more social or performance situations in which the individual is exposed to:
-
The individual fears that they will:
• Act in a way that will be humiliating or embarrassing
• Show anxiety symptoms that will be humiliating or embarrassingNote (Children):
• There must be evidence of the capacity for age-appropriate social relationships with familiar people.
• Anxiety must occur in peer settings, not just in interactions with adults. -
- Exposure to the feared social situation almost invariably provokes anxiety. This anxiety may take the form of:
• A situationally bound panic attack
• A situationally predisposed panic attack
- Exposure to the feared social situation almost invariably provokes anxiety. This anxiety may take the form of:
-
Note (Children):
• Anxiety may be expressed as crying, tantrums, freezing, or shrinking from social situations with unfamiliar people. -
- The individual recognizes that the fear is excessive or unreasonable.
-
Note (Children): This insight may be absent.
-
- The feared social or performance situations are either:
• Avoided entirely
• Endured with intense anxiety or distress - The avoidance, anxious anticipation, or distress in the feared social or performance situation(s) results in:
• Significant interference with normal routine
• Impairment in occupational or academic functioning
• Disruption of social activities or relationships
• Marked distress about having the phobia
- The feared social or performance situations are either:
-
Nursing Insights:
- The nurse must differentiate between a specific phobia and social anxiety disorder.
- Social anxiety disorder is a fear of social situations due to the fear of being judged, whereas a specific phobia is a fear of a specific object or situation.
- A person with a specific phobia of dogs may fear a dog in any setting, while a person with social anxiety disorder fears being judged in a public setting.
- The interventions for these two conditions are similar but have different focuses.
2.2 Xenophobia: Fear of strangers
- Xenophobia is the intense and irrational fear or dislike of people from other countries or cultures.
- This is not a specific phobia in the traditional sense as defined by the DSM-5, which focuses on discrete objects or situations.
- Instead, it is a social phenomenon rooted in prejudice and is often discussed in the context of sociology and political science.
- While it can be associated with anxiety, it does not typically meet the criteria for a diagnosable specific phobia.
2.3 Zoophobia: Fear of animals
- Zoophobia is a general term for the fear of animals.
- This is not a specific diagnosis but is often used as a broad category that encompasses specific animal phobias, such as cynophobia (fear of dogs), arachnophobia (fear of spiders), and ophidiophobia (fear of snakes).
- The fear is often rooted in a traumatic experience or a learned response.
2.4 Additional Types of Specific Phobias The list of specific phobias is extensive and can include nearly any object or situation. Some other examples include:
- Aerophobia: Fear of flying.
- Trypanophobia: Fear of injections or needles.
- Emetophobia: Fear of vomiting.
- Koulrophobia: Fear of clowns.
- Cynophobia: Fear of dogs.
Interventions
- The management of specific phobias involves a multidisciplinary approach, with the nurse playing a crucial role in the assessment, planning, and implementation of care.
- The primary goal of intervention is to reduce the patient's anxiety and help them confront the feared object or situation without a panic response.
1.1 Cognitive-Behavioral Therapy (CBT)
- CBT is the first-line treatment for specific phobias and is highly effective.
- The central tenet of CBT is that thoughts, feelings, and behaviors are interconnected, and by changing one, the others can be influenced.
- Exposure Therapy: This is the most effective component of CBT for phobias. It involves systematically and gradually exposing the individual to the feared object or situation in a safe and controlled environment.
- Systematic Desensitization:
- This technique involves pairing a relaxation technique with a gradual exposure to the feared stimulus.
- The patient first learns deep breathing and progressive muscle relaxation. Then, a hierarchy of feared situations is created, starting with the least anxiety-provoking and progressing to the most.
- The patient is exposed to each item on the hierarchy while maintaining a state of relaxation.
- Flooding:
- This involves exposing the patient to the most feared stimulus for a prolonged period, preventing them from engaging in avoidance behaviors.
- While potentially more rapid, it can be very distressing for the patient and is not always the preferred method.
- Systematic Desensitization:
- Cognitive Restructuring: This technique involves helping the patient identify and challenge the irrational and distorted thoughts associated with their phobia. The nurse helps the patient reframe their thinking from catastrophic thoughts (e.g., "The spider will kill me") to more realistic ones (e.g., "The spider is small and harmless").
1.2 Pharmacological Interventions
- Medications are generally not the first-line treatment for specific phobias, as psychotherapy is more effective.
- However, they can be used in certain situations, particularly as an adjunct to therapy or for short-term use in managing severe anxiety.
- Beta-Blockers: Medications such as propranolol can be used to manage the physical symptoms of anxiety, such as tachycardia, tremors, and palpitations, especially in a performance-related phobia (e.g., stage fright). They work by blocking the effects of epinephrine.
- Benzodiazepines: Medications like alprazolam or lorazepam can be used for short-term relief of severe anxiety, but their use is limited due to the risk of dependence and tolerance. They are not recommended for long-term management.
- Selective Serotonin Reuptake Inhibitors (SSRIs): While not typically used as a primary treatment for specific phobias, they may be prescribed if the patient also has co-occurring depression or another anxiety disorder.
1.3 Nursing Interventions
- The nurse's role in the care of a patient with a specific phobia is multifaceted and includes assessment, education, and direct therapeutic interventions.
- Assessment:
- Conduct a comprehensive mental health assessment, including a detailed history of the phobia, its triggers, and its impact on the patient's life.
- Assess for co-occurring conditions such as depression, other anxiety disorders, or substance use.
- Evaluate the patient's current coping mechanisms and support systems.
- Assess the patient’s willingness and motivation to engage in therapeutic interventions.
- Planning and Implementation:
- Establish a trusting and therapeutic nurse-patient relationship.
- Provide psychoeducation on the nature of specific phobias, explaining the physiological basis of their anxiety response. This helps demystify the experience and reduces the patient's sense of powerlessness.
- Teach and reinforce relaxation techniques, such as deep breathing exercises, mindfulness, and progressive muscle relaxation, which the patient can use to manage their anxiety during exposure to the phobic stimulus.
- Collaborate with the patient and the interdisciplinary team (e.g., psychologist, psychiatrist) to develop a personalized exposure plan. The nurse can play a direct role in guiding the patient through the exposure hierarchy.
- Monitor the patient's response to both pharmacological and non-pharmacological interventions.
- Address safety concerns. For example, for a patient with hematophobia, ensure they are seated or lying down to prevent injury from fainting.
Nursing Insights:
- When implementing exposure therapy, it is crucial for the nurse to ensure that the process is gradual and controlled.
- Pushing the patient too quickly can lead to re-traumatization and a worsening of the phobia.
- The nurse must provide continuous support and positive reinforcement, celebrating small victories as the patient progresses through the exposure hierarchy.
- It is also important to educate the patient that anxiety is a normal physiological response and that the goal is not to eliminate anxiety entirely, but to learn to tolerate it and manage it effectively.
Summary
- Specific phobia is an anxiety disorder characterized by a persistent and irrational fear of a specific object or situation.
- This fear is disproportionate to the actual danger and leads to significant avoidance behaviors that impair daily functioning.
- The etiology is multifactorial, involving genetic predispositions, neurobiological mechanisms centered on the amygdala, and psychological factors such as classical conditioning and observational learning.
- The nurse must be adept at recognizing the diverse types of specific phobias, from acrophobia to hematophobia, and understanding their unique clinical presentations.
- The primary evidence-based intervention for specific phobias is cognitive-behavioral therapy (CBT), particularly exposure-based techniques like systematic desensitization.
- The nurse's role is pivotal in assessing the patient, providing psychoeducation, teaching relaxation techniques, and collaborating with the interdisciplinary team to implement a safe and effective exposure plan.
- Pharmacological agents, such as beta-blockers, can be used to manage acute physical symptoms, but they are not a substitute for therapy.
- The nurse must also be vigilant for specific physiological responses, such as the vasovagal response in hematophobia, and take appropriate actions to ensure patient safety.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Specific Phobia
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


