Please set your exam date
Childhood And Family Assessment
Study Questions
Practice Exercise 1
Which statement indicates the best sequence for the nurse to conduct an assessment in a nonemergency situation?
Explanation
In a nonemergencypediatric assessment, the nurse should follow a sequence that builds rapport, identifies concerns, gathers relevant history, and then proceeds to the physical exam. This approach ensures the family feels heard and that the nurse has essential context before examining the child.
Rationale for correct answer:
A.Introducing yourselfestablishes trust. Asking about problems shows concern for immediate issues. Taking a history before the physical examprovides valuable background that can guide the assessment and focus attention on potential problem areas.
Rationale for incorrect answers:
B.Starting with the physical exambefore discussing problems may increase anxiety for the child and family and risks missing important background information.
C.Combining the physical exam with history-takingmay be efficient in some urgent situations but is less ideal for a relaxed, thorough nonemergency assessment.
D.While understanding health beliefsis important, taking an overly detailed family history before addressing immediate concerns or examining the child may delay care and rapport building.
Take home points
- In nonemergency pediatric care: build rapport → identify concerns → take history → perform physical exam.
- Sequencing the assessment properly improves cooperation and accuracy.
- Always tailor the approach to the child’s developmental stage and comfort level.
What approach by the nurse would most likely encourage a child to cooperate with an assessment of physical and developmental health?
Explanation
The most effective approach is to explain what is going to happen in words the child can understand. This builds trust, reduces fear, and fosters cooperation by ensuring the child knows what to expect in a way that matches their developmental level.
Rationale for correct answer:
B.Using age-appropriate languagehelps children feel respected, informed, and less anxious. It allows them to mentally prepare for the assessment and encourages active participation. This aligns with pediatric communication principles that emphasize honesty, clarity, and developmental sensitivity.
Rationale for incorrect answers:
A.Waiting to explain only when the child asks questionsis reactive and may leave the child uncertain or fearful. Proactive communication is more effective in reducing anxiety.
C.Forcing cooperationundermines trust, increases fear, and can cause long-term resistance to medical care. It should be avoided unless absolutely necessary for urgent safety reasons.
D.Offering a reward before startingmay create expectations of discomfort or coercion. While positive reinforcement is useful, it is most effective when given after the procedure as acknowledgment of cooperation.
Take home points
- Use clear, age-appropriate explanations before starting any assessment to build rapport and reduce anxiety.
- Establish trust by respecting the child’s developmental stage and involving them in the process where possible.
- Avoid coercive measures; instead, focus on communication, comfort, and post-procedure positive reinforcement.
A nurse in the pediatric clinic is examining a group of clients. These general approaches can be helpful when performing a physical examination. Select all that apply
Explanation
Therapeutic communicationduring pediatric physical exams involves adapting strategies based on developmental stages to minimize fear, encourage cooperation, and build trust. This includes using age-appropriate language, involving caregivers, and offering limited choicesto empower the child while maintaining control of the situation.
Rationale for correct answers:
A. Toddlers often resist examinations due to fear and lack of understanding. Gentle restraint, with parental support, helps keep the child safe while providing comfort. Involving parents reduces the toddler’s distress and strengthens the nurse–family alliance.
B. Preschoolers like to feel a sense of control. Offering limited choicessuch as, "Should I look in your ears or your mouth first?", encourages cooperation and helps reduce anxietywithout compromising the exam.
Rationale for incorrect answers:
C. School-age children, especially older ones may prefer privacy, particularly for sensitive topics or exams. Asking the child’s preference promotes respect and autonomy.
D. Adolescents benefit from clear explanationsand often want to understand what’s happening with their bodies. While they may be self-conscious, providing honest information builds trust and supports their need for autonomy.
E. Infant exams are typically foot to headto allow the nurse to assess the least invasive areas first, building trust before disturbing the infant with more uncomfortable procedures like inspecting the ears or mouth.
Take home points
- Involve parents in exams for infants and toddlers for comfort and safety.
- Respect privacy and decision-making in older children and adolescents.
- Modify your exam order and explanations based on the child’s developmental stage and comfort.
- The key to effective pediatric care is flexibility, respect, and developmentally appropriate communication.
A 4½-year-old child is being assessed after sustaining an injury. The child is reluctant to tell the nurse exactly how the injury occurred. Which of the following statements made to the child by the nurse would likely result in the child communicating with the nurse? Select all that apply
Explanation
Therapeutic communicationwith young children, especially after trauma, requires sensitivity to their developmental level. For preschool-age children (3–5 years), play, art, and indirect storytelling techniqueshelp them express thoughts and feelings when verbal expression may be limited or overwhelming.
Rationale for correct answers:
A. Drawingallows young children to express themselves nonverbally. It's a safe, developmentally appropriate method to explore thoughts and events, especially after distressing experiences.
C. Puppet playencourages communication through projection. A child may feel more comfortable attributing their experience to the puppet, reducing fear of judgment or retribution.
D. This technique uses third-person storytelling, allowing the child to describe their experience in a hypothetical, less direct way. It reduces anxiety and encourages narrativewithout direct confrontation.
Rationale for incorrect answers:
B. Most 4½-year-olds have not yet developed sufficient writing skills for storytelling. This request is developmentally inappropriate and may cause frustration or withdrawal.
E. This direct request can feel pressuring or guilt-inducing. It may cause the child to shut down, especially if fear or trauma is involved. Preschoolers respond better to indirect, play-based communication.
Take home points
- Use developmentally appropriate techniques like drawing, puppets, and storytelling to help young children express difficult experiences.
- Avoid direct, confrontational questions that may increase anxiety or lead to withdrawal.
- Create a safe, nonjudgmental space for expression, particularly in cases involving injury or suspected trauma.
Practice Exercise 2
A sleeping 5-month-old girl is being held by the mother when the nurse comes in to do a physical examination. What assessment should be done initially?
Explanation
A physical examination in childrenis a systematic evaluation of a child’s body systems to assess their health, growth, and development. It’s tailored to the child’s age, developmental stage, and presenting concerns, and it plays a vital role in early detection of illness and developmental delays.
Rationale for correct answer:
B.For infants, heart rate assessmentshould be performed first when they are calm or asleep because crying or activity can significantly elevate the rate. Accurate baseline readings are important for clinical evaluation, and the apical pulse should be counted for a full minute.
Rationale for incorrect answers:
A.Listening to bowel soundscan be done at any time, as bowel activity is not greatly affected by the infant’s state of alertness. It is not as time-sensitive as heart rate.
C.Checking temperaturerequires handling the infant more actively, which could wake her and cause distress before important calm-state measurements are taken.
D.Looking in the earsoften requires restraint and is uncomfortable for the infant, likely waking and upsetting her, making it harder to obtain accurate vital signs afterward.
Take home points
- In infants, assess least disruptive measures first while they are calm or asleep—especially heart rate and respiratory rate.
- More stimulating or invasive assessments should be saved for last to maintain cooperation and accurate readings.
- Prioritizing exam order helps ensure accuracy and reduces infant distress.
Which assessment finding is considered normal in children?
Explanation
A physical examination in childrenis a systematic evaluation of a child’s body systems to assess their health, growth, and development. It’s tailored to the child’s age, developmental stage, and presenting concerns, and it plays a vital role in early detection of illness and developmental delays.
Rationale for correct answer:
B.Sinus arrhythmiaresults from normal vagal tone variation with respiration. The heart rate increases with inspiration and decreases with expiration. A split S2 occurs because the aortic and pulmonic valves close at slightly different times during inspiration, which is normal in healthy children.
Rationale for incorrect answers:
A.An irregular respiratory rate and rhythmoutside the newborn period may indicate respiratory or neurologic issues; while periodic breathing can be normal in infants, it is not considered typical in older children.
C.Crying generally increases, not decreases, the heart ratedue to sympathetic stimulation; bradycardia with crying is abnormal and requires further evaluation.
D.Genu varum (bowlegs)is normal in toddlers but usually resolves by age 2–3; persistence beyond age 5 suggests underlying pathology such as rickets or Blount disease.
Take home points
- Sinus arrhythmia and split S2 are normal physiologic findings in healthy children.
- Assessment findings must be interpreted in the context of the child’s age and developmental stage.
- Persistent abnormal findings beyond expected age ranges should prompt further evaluation.
A nurse is attempting to get a 5-year-old child’s cooperation when auscultating heart sounds. Which of the following comments is most likely to elicit the child’s cooperation?
Explanation
A physical examination in childrenis a systematic evaluation of a child’s body systems to assess their health, growth, and development. It’s tailored to the child’s age, developmental stage, and presenting concerns, and it plays a vital role in early detection of illness and developmental delays.
Rationale for correct answer:
C.Involving the child in the examinationturns the assessment into an interactive activity rather than a passive procedure. At age 5, children are naturally curious and enjoy hands-on participation, which can reduce anxiety and increase cooperation.
Rationale for incorrect answers:
A.While using playful language like “boom boom”may be friendly, it does not engage the child’s participation as effectively as offering them the chance to listen.
B.Providing information (“Did you know that your heart beats in your chest?”)may pique curiosity but is less likely to actively involve the child in the procedure.
D.Showing a pictureis educational but does not directly invite the child to engage in the examination.
Take home points
- Active participation and choice-giving help gain cooperation in preschool and school-age children.
- Interactive strategies reduce fear and build trust during physical assessments.
- Tailoring communication to the child’s developmental stage fosters a positive healthcare experience.
The nurse enters the examination room of a mother and her 8-month-old. The baby is asleep in the mother’s arms. Which of the following actions would be best for the nurse to perform at this time?
Explanation
A physical examination in childrenis a systematic evaluation of a child’s body systems to assess their health, growth, and development. It’s tailored to the child’s age, developmental stage, and presenting concerns, and it plays a vital role in early detection of illness and developmental delays.
Rationale for correct answer:
B.Heart, lung, and bowel sounds are best assessed when the infant is quiet or asleepto minimize interference from crying or movement. Starting with the least invasive and least disturbing assessments preserves cooperation and accuracy.
Rationale for incorrect answers:
A.While obtaining an updated historyis important, it can be done after completing quiet-state assessments. The priority is to take advantage of the infant’s current calm state.
C.Beginning a full head-to-toe examwould require more handling and could wake the baby, making it difficult to get accurate auscultation findings afterward.
D.Waking the baby unnecessarilydisrupts the opportunity for a calm, accurate examination and may make the rest of the assessment more challenging.
Take home points
- For infants, assess least disruptive measurements first when they are calm or asleep—especially heart rate, respiratory rate, and auscultation of heart/lungs/bowel sounds.
- More stimulating or invasive assessments should be left for last.
- Planning exam order around the child’s state maximizes accuracy and minimizes distress.
A clinic nurse assesses an infant diagnosed with thrush. Place an X on the photograph illustrating a thrush infection.
Explanation
Rationale:
Oral thrush, also called oral candidiasis, is a fungal infection in the mouth caused by Candida albicans, a type of yeast that normally lives in the body but can overgrow under certain conditions. They appear as creamy white patches on the tongue, inner cheeks, gums, or roof of the mouth. The patches resemble cottage cheese and don’t wipe off easily.
Take home points
- White patches in the mouth that resemble cottage cheese and don’t wipe off easily are a hallmark sign of oral thrush.
- Feeding difficulties or fussiness may indicate discomfort caused by the infection, especially in infants.
Practice Exercise 3
While performing a chest assessment on an 11-month-old child, the nurse palpates for the cardiac point of maximum intensity (PMI). The nurse would expect the PMI to be felt at the:
Explanation
A cardiac examination in childrenis a focused assessment of the heart and circulatory system, adapted to the child’s age, developmental stage, and clinical presentation. It’s essential for detecting congenital heart defects, acquired heart diseases, and circulatory abnormalities.
Rationale for correct answer:
B.In children under 7 years old, the heart lies higher and more horizontally in the thorax compared to adults. The PMI is found at the 4th intercostal space, slightly lateral to the midclavicular line. After age 7, the PMI moves to the adult position at the 5th intercostal space at the midclavicular line.
Rationale for incorrect answers:
A.The 3rd intercostal spaceis too high for a normal PMI location in infants or adults.
C.The 5th intercostal space at the midclavicular lineis the adult PMI location, typical after age 7, not at 11 months.
D.The 6th intercostal space near the axillais far too lateral and low for the PMI in any age group and would suggest pathology if palpated there.
Take home points
- PMI location changes with age:
- <7 years: 4th intercostal space, lateral to MCL
- ≥7 years: 5th intercostal space, at MCL
- The higher, more lateral PMI in infants is due to the anatomical position of the heart in the developing thorax.
- Deviation from expected PMI location for age may indicate cardiac enlargement or other pathology.
When taking an infant’s blood pressure, which points are important for a nurse to remember? Select all that apply
Explanation
Blood pressure (BP) monitoring in childrenis a vital part of pediatric care, used to assess cardiovascular health and detect early signs of hypertension or other systemic conditions. When taking an infant’s blood pressure, it is essential to use the correct cuff size, proper placement, and appropriate devices for accuracy.
Rationale for correct answers:
A.An infant cuffis designed to fit the smaller arm circumference and ensures accurate readings; an incorrect cuff size can lead to false high or low results.
B.The cuff bladder lengthshould be approximately two-thirdsthe length of the upper arm to obtain an accurate reading.
C.A Doppler ultrasound devicecan be used for infants because it allows detection of blood flow sounds even in low-pressure situations, improving accuracy in small or restless children.
Rationale for incorrect answers:
D.In infants and children, thigh systolic blood pressure is normally 10–40 mmHg higherthan arm systolic pressure due to greater distance from the heart and larger artery size; the reverse suggests possible pathology.
E.In coarctation of the aorta, the arm reading is higher than the thigh reading; equal readings are not diagnostic and are not a typical sign of coarctation.
Take home points
- Use correct cuff size and proper measurement technique for accurate pediatric BP readings.
- In healthy children, thigh BP > arm BP; reversed or significantly lower leg BP suggests possible coarctation of the aorta.
- Doppler devices are especially useful for obtaining reliable BP in infants and very young children.
A 22-month-old toddler is walking into the examination room independently in front of the toddler’s mother. Which method should the nurse plan to use to weigh the child?
Explanation
Weight assessment in childrenis the process of measuring and interpreting a child’s body weight in relation to age, height, and sex to evaluate growth, nutritional status, and overall health. It’s a key part of pediatric care and helps identify undernutrition, overweight, or obesity early on.
Rationale for correct answer:
A.If a toddler can stand alone, a standing scaleprovides an accurate weight and is more comfortable for the child. At 22 months, many children have the stability to stand still briefly for weighing.
Rationale for incorrect answers:
B.Infant scalesare generally used for babies and younger toddlers who cannot stand unsupported; by this age and developmental stage, a standing scale is suitable.
C.While involving the mother in care decisionsis important, the method of weighing is based on developmental capability, not caregiver preference.
D.The “subtracting method”is less accurate and is typically used only when the child cannot stand and an infant scale is unavailable.
Take home points
- Choose the weighing method based on developmental ability, not strictly on age.
- Standing scales are appropriate for toddlers who can stand still without assistance.
- Accurate anthropometric measurements are key for growth monitoring and detecting developmental or nutritional concerns.
A pediatric nurse is to perform a head-to-toe assessment on a toddler who is admitted to a hospital for nausea and vomiting. Which is most important for the nurse to consider before beginning the examination?
Explanation
A physical examination in childrenis a systematic evaluation of a child’s body systems to assess their health, growth, and development. It’s tailored to the child’s age, developmental stage, and presenting concerns, and it plays a vital role in early detection of illness and developmental delays.
Rationale for correct answer:
D.Developmental ageguides how the nurse communicates, sequences the exam, and engages the child. For toddlers, this means using simple language, allowing parental presence, and starting with least invasive assessments first.
Rationale for incorrect answers:
A.While parental presencecan provide comfort and reduce anxiety, it is not the primary consideration; the developmental approach to the exam comes first.
B.A firm tonemay increase fear and resistance in toddlers; calm, gentle, and encouraging communication is more effective.
C.Waiting until the child is “ready”may not be practical in a hospital setting, and some cooperation can be gained through distraction and play without unnecessary delays.
Take home points
- Pediatric assessments should always be tailored to developmental age for accuracy and cooperation.
- Toddlers respond best to gentle communication, parental presence, and strategic sequencing of the exam.
- Understanding developmental milestones helps nurses choose the right techniques for assessment and interaction.
A clinic nurse assesses an infant diagnosed with thrush. Place an X on the photograph illustrating a thrush infection.
Explanation
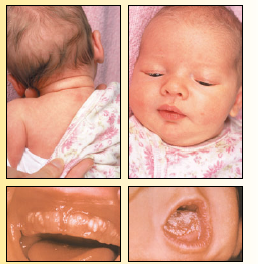
Oral thrush, also called oral candidiasis, is a fungal infectionin the mouth caused by Candida albicans, a type of yeast that normally lives in the body but can overgrow under certain conditions. They appear as creamy white patches on the tongue, inner cheeks, gums, or roof of the mouth. Thepatches resemble cottage cheese and don’t wipe off easily.
Take home points
- White patches in the mouth that resemble cottage cheese and don’t wipe off easily are a hallmark sign of oral thrush.
- Feeding difficulties or fussiness may indicate discomfort caused by the infection, especially in infants.
A nurse in the pediatric unit is preparing to take the blood pressure readings of several clients. When assessing blood pressure in a child:
Explanation
Effective pediatric assessmentincludes not only age-appropriate interaction but also a solid understanding of developmental physiology. Therapeutic communication complements accurate assessment by helping nurses explain procedures and results in ways appropriate to the child’s age and developmental stage.
Rationale for correct answer:
A. Accurate interpretation of BPin pediatric patients requires an understanding of age-specific norms. Blood pressure gradually increases with age, so a reading of 95/58 mm Hg may be normal for a toddler but hypotensive for a school-age child. Using correct reference values ensures appropriate identification of hypotension or hypertension.
Rationale for incorrect answers:
B. While cuff size is crucial, it should be based on limb circumference, not length. The cuff bladder width should be approximately 40% of the arm circumference, and the length should cover 80–100% of the arm. Using the wrong size can yield inaccurate readings.
C. A child is normotensiveif their BP is below the 90th percentilefor age, sex, and height. Readings between the 90th and 95th percentiles are considered prehypertensive, while readings above the 95th percentile suggest hypertension.
D. In conditions like coarctation of the aorta, upper-extremity BP is higherthan lower-extremity BP. A lower BP in the legscompared to the arms is a classic sign of this condition, not the reverse.
Take home points
- Know age-specific BP norms to detect abnormalities in pediatric clients.
- Use the correct cuff size, measured by arm circumference, for accurate readings.
- Interpret BP percentiles properly: Normal is below the 90th percentile.
- Compare upper and lower extremity BPs in suspected cardiac conditions like coarctation of the aorta, not aortic stenosis.
Comprehensive Questions
A nurse looks over her assignment for the day, which includes an infant, a preschool-age child, a third-grader, and a sophomore in high school. Which techniques take into consideration developmental stages when working with pediatric clients?
Explanation
Therapeutic communicationwith pediatric clients must be developmentally appropriate. It involves adjusting communication styles to match the child’s cognitive, emotional, and language abilities. This supports trust, reduces anxiety, and enhances cooperation during care.
Rationale for correct answer:
C. School-age children (ages 6–12)are in the concrete operational stage (Piaget), meaning they think logically about concrete events but still need reassurance. Demonstrating how equipment works helps reduce fear and encourages cooperation by satisfying their curiosity and building trust.
Rationale for incorrect answers:
A. Stranger anxietytypically starts around 6 to 8 months, not 4 months. Additionally, while recognizing developmental behavior is important, the statement doesn’t describe a communication technique.
B. Preschoolers (ages 3–5)are in the preoperational stageand rely on imagination more than logic. Detailed explanations can increase anxiety and confusion. Instead, simple, concrete termsand play-based explanations such as using a doll are more effective.
D. Adolescents need autonomy, respect, and honesty. A rigid, one-size-fits-all approach can increase resistance. Therapeutic communication with teens should be flexible, involve them in decision-making, and respect their growing independence.
Take home points
- Match your communication to the developmental level of the child.
- Use demonstrations and hands-on explanations with school-age children.
- For preschoolers, keep language simple and use familiar terms or play.
For adolescents, involve them in decisions and treat them with respect and autonomy
A nurse understands that growth measurement is a key element of health status in children. One measurement is linear growth. What should the nurse do to perfect this technique? Select all that apply
Explanation
Therapeutic communicationduring growth assessments involves not only speaking in a calm, reassuring manner to both the child and caregiver but also demonstrating procedural competence. Accurate and respectful handling during physical measurements builds caregiver trust and supports a child-friendly, developmentally appropriate experience.
Rationale for correct answers:
A. Accurate linear growth assessmentdepends on the child’s developmental stage. Children under 2 yearsshould be measured in the recumbentposition using a length board, while those older than 2and able to stand should be measured for stature using a stadiometer.
D. Measuring at least twice increases accuracy and reduces error. Averaging the measurements ensures a reliable estimate of true length or height, especially in wiggly infants or uncooperative toddlers.
E. Consistent traininghelps maintain accurate and standardized measurement techniques. Refresher trainingis essential when discrepancies or poor technique are observed, ensuring that measurements across providers are comparable and reliable.
Rationale for incorrect answers:
B. While a length boardis recommended, a tape measure is not accuratefor linear growth because it can follow body contours rather than straight lines, leading to inconsistent or inflated measurements. Tape measures should only be used for head circumferenceor limb girths, not length.
C. While two measurers improve accuracy, especially for infants who squirm, it is not always required for cooperative or sleeping infants. However, this is not a consistently correct approach in all cases.
Take home points
- Use recumbent length for children under 2 and standing height for those over 2.
- Avoid using tape measures for linear growth, always prefer length boards or stadiometers.
- Measure at least twice (preferably three times), and average the values for reliability.
- Maintain technical competency, and pursue refresher training when needed to prevent measurement errors.
The nurse is preparing to perform an examination of a 2-year-old boy. The child’s mother is present. At the start of the examination, which of the following actions by the nurse may help to prevent a negative response from the child?
Explanation
Therapeutic communicationwith toddlers (ages 1–3) emphasizes building trust gradually through observation, indirect interaction, and the use of familiar figures like caregivers. At this age, stranger anxietyand fear of unfamiliar situations are common. Gentle, non-threatening approaches are essential to reduce distress and encourage cooperation.
Rationale for correct answer:
A. Toddlers are cautious around unfamiliar people. By initially directing attention to the caregiver, the nurse allows the child to observe from a safe distancewithout feeling threatened. This indirect approach helps the child build trustat their own pace, reducing the likelihood of a negative reaction.
Rationale for incorrect answers:
B. Gently touching the child’s hair while looking directly into his eyes can be perceived as intrusive or threateningto a toddler, especially before trust is established. Direct eye contact and unsolicited touch often trigger anxiety or defensive behavior in young children.
C. While smiling is helpful, placing a stethoscope on the chest too sooncan alarm a child. The nurse should gradually approach and allow the child to exploreor observe instruments first.
D. A 2-year-old's language skills are limited, and many may not yet be capable of detailed verbal responses. This approach may cause frustration or confusion rather than cooperation.
Take home points
- Start by engaging with the caregiver, allowing the toddler to observe and feel secure before approaching.
- Avoid direct touch and eye contact early in the interaction, build trust first.
- Use non-threatening behavior and allow time for the child to warm up.
- Communicate at the child’s developmental level, and let them explore tools before the exam.
The nurse is obtaining a health history of a 6-year-old child who is being seen at the clinic for the first time. Which of the following questions should the nurse ask the child during the interview? Select all that apply
Explanation
When interviewing school-age children (ages 6–12), therapeutic communication involves using concrete, familiar topics, engaging them in ways that feel safe and approachable, and supporting their growing cognitive and social development. Children in this stage are capable of logical thinking, building friendships, and expressing preferences, especially when asked about familiar activities.
Rationale for correct answers:
A. “Do you have any pets at home?”Asking about pets is a neutral, familiar topicthat can help establish rapport and reduce anxiety. It also offers insight into the child’s environment and emotional attachments.
B. “Can you tell me how many 1 plus 1 makes?”This question checks cognitive developmentin a non-threatening way. Most 6-year-olds can do simple math, and answering gives them a sense of accomplishment and participation.
C. “Can you tell me the name of one of your school friends?”This allows assessment of social developmentand helps build conversation around the child’s interpersonal experiences in a familiar setting.
E. “What kinds of things do you like to play during recess at school?”Engaging the child in a conversation about play is age-appropriate and gives clues about physical activity, preferences, and peer interactions.
Rationale for incorrect answer:
D. “Can you tell me the names of any medicines that you take?”While important information, this is best addressed to the caregiver. A 6-year-old may not accurately recallmedication names, doses, or reasons for use. This question could also cause unnecessary confusion or anxiety if the child fears being “quizzed” on adult topics.
Take home points
- Use open-ended, concrete questions with school-age children to assess development and build rapport.
- Avoid questions that require abstract thinking or adult-level knowledge, such as medication names.
- Focus on familiar areas like school, friends, pets, and play to engage the child comfortably.
Allow the child to participate in the conversation at their developmental level, but verify critical medical information with the caregiver.
A 9-year-old child is being seen in the pediatrician’s office after experiencing a head injury. The nurse assesses the child’s vital signs as: TPR – 98.0°F, HR: 52 bpm, RR: 12 rpm, and BP: 88/50 mm Hg. The child’s capillary refill is 2 sec. Which of the following actions would be appropriate for the nurse to take?
Explanation
In urgent or emergent pediatric scenarios, therapeutic communication includes clear, prompt reportingof abnormal findings to the healthcare team, while simultaneously maintaining calm, reassuring interactionswith the child and caregiver. The nurse's role includes timely recognition and escalation of critical changes.
Rationale for correct answer:
A. The child’s vital signs are concerning, particularly the bradycardia (HR: 52 bpm)and hypotension (BP: 88/50 mm Hg), which are not normal for a 9-year-old. These could be signs of increased intracranial pressure (ICP), especially following a head injury. Early intervention is crucial to prevent deterioration, making immediate notification the priority.
Rationale for incorrect answers:
B. While obtaining the historyis important, this is not the priority when abnormal vital signssuggest possible neurological compromise. Assessment and stabilization take precedence over gathering subjective data.
C. Rescue breaths are indicated for apnea or severe respiratory distress, neither of which is currently present (RR: 12 rpm is within normal range for age). Inappropriately providing rescue breaths could cause harm.
D. Although carefully examining the child’s head for signs of fracture is relevant in head trauma, it is not the immediate priority when life-threatening signs such as bradycardia and hypotensionare present. These findings require urgent escalation, not just local examination.
Take home points
- In pediatric clients with head injuries, bradycardia and hypotension may indicate increased intracranial pressure or impending deterioration.
- Vital signs in children should always be interpreted in age-specific context.
- The nurse’s first responsibility in an emergency is prompt recognition and notification of critical signs.
- Assessment of airway, breathing, and circulation (ABCs) remains the cornerstone of pediatric emergency care.
The nurse is assessing a 5-year-old child with a possible fractured leg following a bicycle accident. Which of the following actions would best determine the child’s pain level?
Explanation
Therapeutic communication in pain assessment involves using developmentally appropriate toolsthat empower the child to communicate their discomfort. For children around 5 years old, structured tools such as pictorial or numeric pain scalesprovide reliable, age-appropriate methods for self-reporting pain, which is considered the gold standard when possible.
Rationale for incorrect answer:
C. A 5-year-oldtypically has the cognitive ability to use a pictorial pain scalelike the Wong-Baker FACES Pain Rating Scale. This allows the child to match their pain to a facial expression that represents how they feel. Using a validated, child-friendly tool ensures a more accurate and reliable pain assessment.
Rationale for incorrect answers:
A. Behavioral cues such as grimacing and guarding are helpful, especially for non-verbal or very young children, but observation alone is subjectiveand may underestimate or misinterpret pain.
B. While asking directly can be useful, open-ended verbal questions may be too abstractfor a 5-year-old to answer accurately. Structured tools are more effective for this age.
D. Parental inputcan supplement pain assessment, especially in very young or nonverbal children, but in a verbal 5-year-old, the child’s self-report is preferred when possible. Relying solely on the parent may lead to inaccurate estimation.
Take home points
- Use age-appropriate pain rating scales like the Wong-Baker FACES for children aged 3 years and older.
- Self-report is the most reliable method of pain assessment in verbal children.
- Supplement with behavioral observations and parental input, but do not rely on them alone when the child can communicate.
- Tailor pain assessment tools to the child’s developmental stage and cognitive abilities.
The nurse is assessing the accommodation of a child’s eyes. Which of the following techniques would be appropriate for the nurse to perform?
Explanation
In pediatric assessments, therapeutic communication involves incorporating play and age-appropriate toolsto facilitate cooperation and accurate findings. Accommodation, which involves the eyes adjusting focus from a distant to a near object. When assessing eye accommodation in children, using engaging, familiar objectsreduces anxiety and promotes interaction, ensuring a smoother and more reliable assessment.
Rationale for correct answer:
D. In children, using a puppet or toy makes the exam developmentally appropriate and engaging, encouraging them to visually track the objectand enabling the nurse to observe pupil constriction and convergencewhich are key indicators of normal accommodation.
Rationale for incorrect answers:
A. Asking the child to follow the nurse’s fingers in all six quadrants assesses extraocular muscle movement (EOM), not accommodation. It's used to check for strabismus, cranial nerve function, and eye alignment, not lens focusing ability.
B. Having the child cover one eye and read from a vision chart tests visual acuity, not accommodation. While important in a full eye exam, this doesn’t assess how the eyes adjust focus from far to near.
C. Using an ophthalmoscope to assess for the red reflex screens for ocular opacity or abnormalities in the retina, such as cataracts or retinoblastoma, not accommodation.
Take home points
- Accommodation is assessed by observing how the eyes focus on a moving object approaching the face.
- In children, use playful, age-appropriate tools (e.g., puppets, toys) to gain cooperation and maintain attention.
- Don’t confuse accommodation with EOM testing, visual acuity, or ophthalmoscopic assessment—each evaluates different parts of eye function.
- Therapeutic play enhances the accuracy and ease of pediatric assessments.
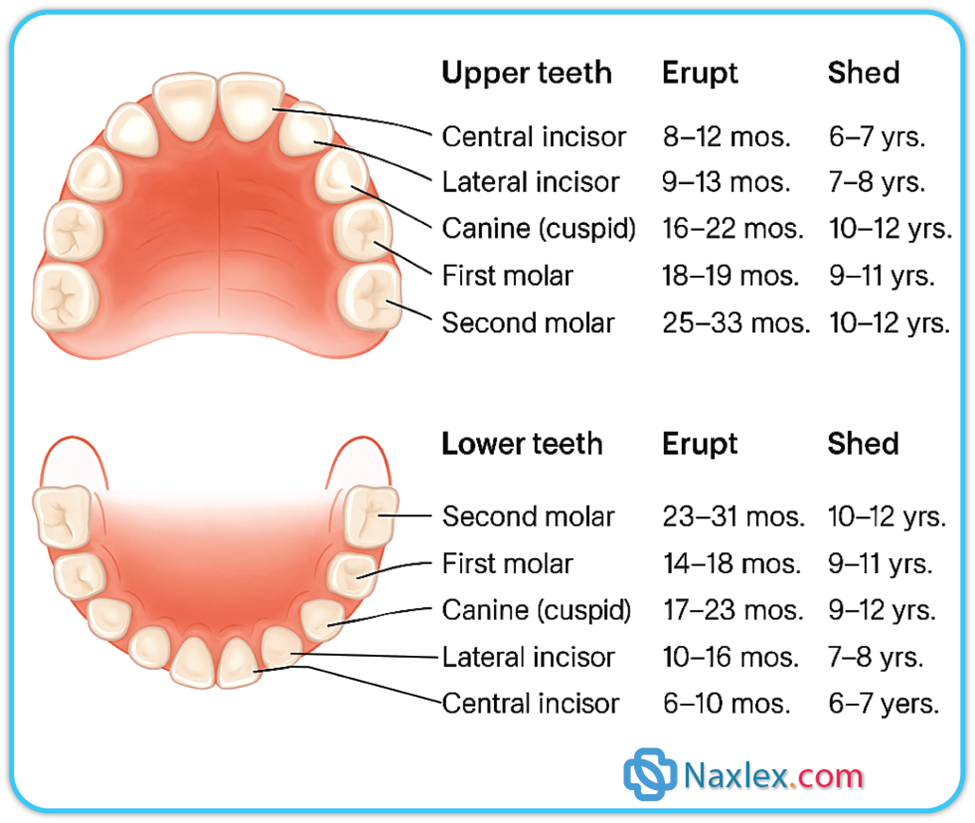
The nurse is assessing the dental development of a 7-month-old child. Which of the following findings would the nurse expect to see?
Explanation
Dental development in children, also known as odontogenesis, is the process by which a child’s teeth form, erupt, and mature, starting before birth and continuing into adolescence. It plays a critical role in nutrition, speech development, and overall facial structure.
Rationale for correct answer:
B. The first primary teethtypically erupt between 6–10 months, with the lower central incisorsmost commonly appearing first. At 7 months, it is developmentally appropriate to observe two lower central incisors. This is the expected milestone in dental development at this age.
Rationale for incorrect answers:
A. While drooling and chewing begin as early signs of teething, by 7 months, the first teeth have usually started to erupt. The complete absence of teeth could still be within normal limits, but is less typical than having two lower incisors.
C. Upper central incisorstypically erupt after the lower ones, usually around 8–12 months. At 7 months, it would be early for these to be the first and only teeth present.
D. Presence of both upper and lower incisorsgenerally occurs closer to 9–12 months. While some infants may develop teeth earlier, four incisors at 7 monthsis ahead of the typical developmental timeline.
Take home points
- Lower central incisors are usually the first teeth to erupt, around 6–10 months.
- Educate caregivers that drooling, chewing, and irritability may precede visible teeth.
- Teething timelines vary slightly, but major deviations should prompt monitoring.
- Use gentle techniques and offer anticipatory guidance about teething care and oral hygiene.
The nurse is preparing to palpate a 2-year-old girl’s tongue during a physical examination. Which of the following actions would help to prevent the nurse from being bitten?
Explanation
During physical assessments in toddlers, safety and trust-buildingare top priorities. Therapeutic communication involves explaining procedures to caregivers, using age-appropriate reassurance, and ensuring that examinations are performed efficiently and safely, especially when a child may become defensive or frightened.
Rationale for correct answer:
C. Holding the toddler’s cheeks with the fingers of one hand helps prevent the child from closing their mouth forcefully and biting, which is a common reflex in toddlers when their mouths are manipulated. By gently securing the cheeks, the nurse creates a controlled and safer environmentto palpate the tongue while reducing the risk of injury.
Rationale for incorrect answers:
A. While parents can assist in calming the child, the nurse must maintain controlduring an oral assessment to ensure safety and proper technique. Relying on the parent may not offer adequate control or bite prevention.
B. A 2-year-old may not consistently follow verbal instructions, especially during unfamiliar or uncomfortable procedures. Cooperation at this age is unpredictable, and this method doesn’t provide physical safety against sudden closure of the jaw.
D. Inserting a tongue blade without stabilizing the mouth may provoke bitingand result in injury to the nurse or discomfort to the child. It should be done only after securing the cheeks or using proper restrainttechniques.
Take home points
- Toddlers may bite reflexively during oral exams, preventive positioning is essential.
- Gently holding the cheeks helps keep the mouth open and protects the examiner's fingers.
- Use developmentally appropriate strategies—toddlers often resist unfamiliar touch or instructions.
- Involve caregivers for comfort, but nurses must maintain control of the assessment process for safety and accuracy.
- Approach oral assessments calmly, quickly, and with gentle physical support to minimize stress and risk.
The nurse is performing a whisper test when assessing the hearing of a 10-year-old child. Which of the following actions would be appropriate for the nurse to perform?
Explanation
The whisper test is a simple, non-invasive screening toolfor assessing hearing in older children and should be conducted in a way that is both accurate and engaging for the child. It is a quick and simple screening tool used to assess hearing acuity, especially in clinical or bedside settings.
Rationale for correct answer:
D. This method is an appropriate and standard techniquefor performing the whisper test. It checks for hearing acuityby assessing whether the child can hear and comprehend whispered instructionswithout visual cues. Whispering a simple command from behind the child helps evaluate hearing in each ear separately if done appropriately.
Rationale for incorrect answers:
A. Asking the child to whisper the wordswhile assessing the tympanic membrane is incorrect because the whisper test assesses the child’s ability to hear, not speak. Also, tympanic membrane inspection and hearing evaluation are separate components of an ear exam.
B. Asking the child to whisper into the nurse’s ear evaluates the child’s speaking volume, not their hearing ability, and does not provide information about auditory perception.
C. Asking the child whether or not he hears his friends when they whisper to him is subjectiveand may not accurately reflect the child's hearing ability. A proper assessment requires objective observation, not just self-reporting.
Take-Home Points
- The whisper test is a quick, effective way to assess hearing in school-age children.
- Conduct it by standing behind the child, whispering a simple command, and observing if the child responds appropriately.
- Avoid relying solely on subjective questions or unrelated behaviors to assess hearing.
- Tailor your explanation and tone to the child's developmental level to reduce anxiety and ensure cooperation.
The nurse is assessing the posture of a 13-month-old child who has been walking for 1 month. Which of the following findings should the nurse determine are within normal limits? Select all that apply
Explanation
During developmental assessments, therapeutic communication includes reassuring caregiversabout what is developmentally appropriate and explaining normal variations in physical appearance and movement. Providing this context helps reduce anxiety and fosters trustbetween the caregiver and nurse.
Rationale for correct answers:
A. Flat feetare common and normal in toddlers due to the fat padthat obscures the arch. The arch typically becomes more apparent as the child grows older.
C. Toddlers frequently exhibit lumbar lordosis, a forward curve in the lower back, to balance their large heads and weak abdominal muscles. This is a normal postural adaptation during early walking.
D. A wide base of supportand waddling gait are typical for new walkers. These features provide balance and stabilityas they develop coordination and muscle strength.
E. Genu varum (bowlegs)is normal in toddlers, especially in early walkers. It usually corrects itself as the child grows and the legs straighten with weight-bearing and muscle development.
Rationale for incorrect answer:
B. Thoracic kyphosis, excessive forward curvature of the upper back, is not a normal finding in toddlers. It may indicate muscular or structural abnormalitiesand warrants further evaluation if observed.
Take-Home Points
- Many postural characteristics seen in early walkers such as flat feet, bowlegs, lordosis, and wide gaits, are normal and self-limiting.
- These features reflect immature musculoskeletal development and will typically resolve by age 2–3.
- Kyphosis is not a normal developmental posture in toddlers and should be evaluated if present.
- Educate caregivers that transitional gait patterns are expected and not a sign of pathology unless accompanied by pain or asymmetry.
A 5-year-old boy visits the physician’s office with an upper respiratory infection. Which approach would give the nurse the most information about the child’s developmental level?
Explanation
Playis the most effective way to assess developmental level in young children because it allows the nurse to observe physical, cognitive, social, and language skills in a natural and engaging way.
Rationale for correct answer:
A.Play is the “work” of childhoodsince it reflects the child’s developmental abilities, problem-solving skills, and interactions with others. Observing how a child plays can reveal fine and gross motor skills, language development, and social behaviors.
Rationale for incorrect answers:
B.Talking about a teddy bearmay engage the child but provides limited and less comprehensive developmental information compared to active play observation.
C.Screening toolsare helpful but often rely on structured questions or parental input; they don’t provide as much real-time, holistic information as play observation.
D.Asking the siblingmight offer anecdotal insight but is not a reliable or objective method for developmental assessment.
Take home points
- Play is a powerful assessment tool for understanding a child’s developmental stage.
- Observing play offers insight into motor skills, language, cognition, and social interaction.
- Developmental assessment should be both age-appropriate and engaging to ensure accurate observations.
The abdomen of a 7-year-old child, whose percentile weight is slightly lower than percentile height, is being assessed. Which of the following findings would the nurse expect to see?
Explanation
Growth in childrenrefers to the increase in physical size, including height, weight, and organ development, as they mature from infancy through adolescence. It’s a key indicator of health and development, and is influenced by genetics, nutrition, environment, and overall well-being.
Rationale for correct answer:
C.Visible aortic pulsationsare common in slender children because there is less subcutaneous tissue to obscure the aorta’s movement. This is a benign finding as long as there are no signs of abdominal mass, bruit, or other abnormal features.
Rationale for incorrect answers:
A.Umbilical herniasare common in infants and toddlers but usually resolve by age 3–5; persistence at age 7 is abnormal and would require evaluation.
B.The liver may be palpable 1–2 cm below the right costal marginin infants and toddlers, but in older children, it should generally not be felt below the costal margin unless enlarged.
D.The spleen is not normally palpable in healthy children; palpation below the left costal margin suggests splenomegaly and requires further investigation.
Take home points
- Visible aortic pulsations can be normal in lean children due to a thin abdominal wall.
- Umbilical hernias, hepatomegaly, or splenomegaly in a 7-year-old warrant further evaluation.
- Always interpret abdominal findings in the context of age, body habitus, and associated symptoms.
The nurse has performed physical assessments on 4 preschool children who have been referred for potential genitourinary problems. It would be appropriate for the nurse to report to the primary health-care provider that which of the children’s findings is actually within normal limits?
Explanation
A physical examination in childrenis a systematic evaluation of a child’s body systems to assess their health, growth, and development. It’s tailored to the child’s age, developmental stage, and presenting concerns, and it plays a vital role in early detection of illness and developmental delays.
Rationale for correct answer:
C.In young boys, the foreskin is often still adherent to the glans and not fully retractable.Forcing retraction can cause pain, tearing, and scarring. This is a normal developmental stage and not considered pathological unless accompanied by pain, swelling, or infection.
Rationale for incorrect answers:
A.While a soft scrotal sac without massesmay seem benign, the absence of palpable testes could indicate cryptorchidism, which should be reported for further evaluation.
B.Wide-spread labia majora in a preschool girlmay suggest hormonal influence (e.g., from androgen exposure) or an anatomical variation requiring assessment.
D.Vaginal discharge with afishy odoris abnormal and often associated with infection such as bacterial vaginosis or a foreign body, both of which require prompt evaluation.
Take home points
- Physiologic phimosis is normal in preschool boys; do not force retraction.
- Genitourinary findings should always be interpreted in the context of age and developmental norms.
- Abnormal odors, absent testes, or unusual anatomical changes in children warrant prompt reporting and further investigation.
The nurse is assessing the reflex development of a 5-month-old child. Which of the following rudimentary reflexes would the nurse expect still to be present?
Explanation
Primitive reflexes, are automatic, involuntary movements present at birth that help infants survive and interact with their environment. These reflexes are controlled by the brainstem and spinal cord and typically fade as the child’s nervous system matures and voluntary motor control develops.
Rationale for correct answer:
C.The Babinski reflex is a normal finding in infants and young toddlers due to incomplete myelination of the corticospinal tracts. It gradually disappears as voluntary motor control develops. In a 5-month-old child, the Babinski reflexis still normally present. This primitive reflex, extension and fanning of the toes when the sole of the foot is stroked, typically disappears by 12–24 monthsas the nervous system matures.
Rationale for incorrect answers:
A.The Moro reflex (startle reflex)usually disappears by 4–6 months; persistence beyond this age may indicate neurological issues.
B.The trunk incurvation (Galant) reflextypically disappears by 4–6 monthsof age.
D.The palmar grasp reflexusually fades by 5–6 monthsas voluntary grasping replaces the reflexive action.
Take home points
- Primitive reflexes have specific disappearance timelines; persistence beyond these can signal neurological problems.
- Babinski is the last major primitive reflex to disappear, remaining normal through the first year or longer.
- Reflex assessment in infants is a key part of evaluating neurological development.
Exams on Childhood And Family Assessment
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
- Understand the critical components of a comprehensive childhood and family assessment.
- Master effective communication techniques for interviewing children and their parents.
- Learn how to conduct a thorough health history and physical examination tailored to a pediatric population.
- Identify key developmental milestones and nutritional considerations for children.
- Learn how to perform systematic head-to-toe physical examinations.
Introduction
- A comprehensive childhood and family assessment is the cornerstone of pediatric nursing.
- It's not just about a single physical exam but about creating a complete picture of the child's health within their family and environmental context.
- This includes evaluating their physical, emotional, social, and cognitive development.
- The assessment is a dynamic process that begins the moment you meet the child and family and continues throughout every interaction.
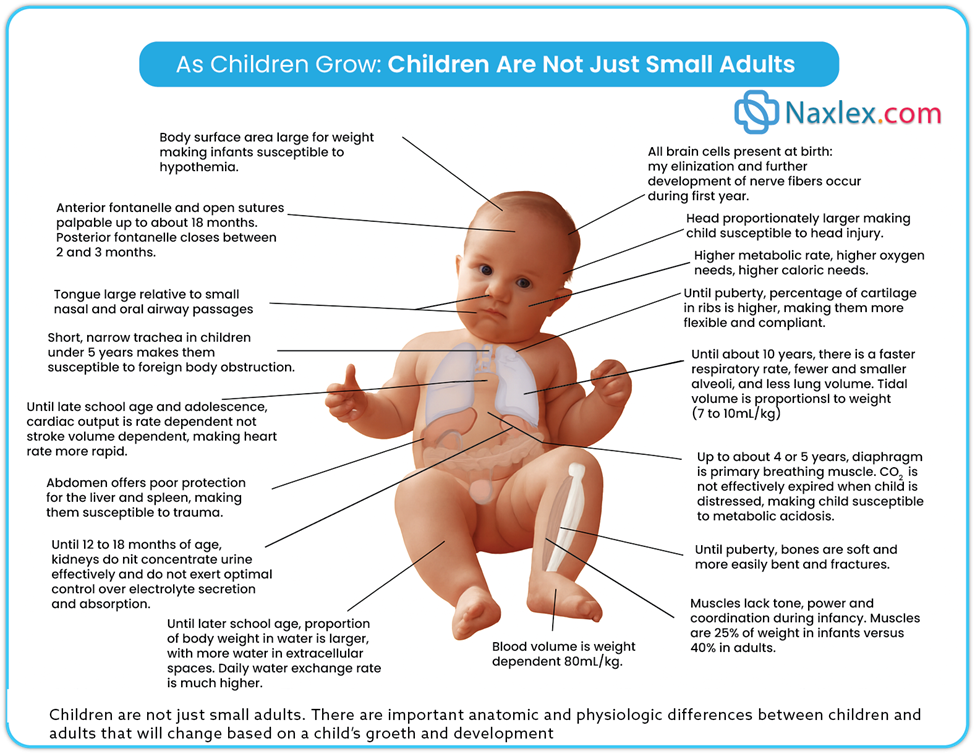
Key Differences Between Children and Adults
System / Characteristic
Pediatric Differences
Body Surface Area
Larger for weight → susceptible to hypothermia
Head Size
Proportionately larger → increased risk of head injury
Metabolism & Needs
Higher metabolic rate, oxygen needs, and caloric demands
Rib Cage
More cartilage → ribs more flexible and compliant
Respiratory
Faster rate, fewer/smaller alveoli, lower lung volume; primary breathing muscle is diaphragm (up to 4–5 years)
Acid-Base Balance
CO₂ not effectively expired when in distress → risk for metabolic acidosis
Skeletal System
Bones softer and more prone to bending/fracture
Muscular System
Less tone, power, coordination; muscles make up 25% of weight in infants vs. 40% in adults
Fontanelles
Anterior: palpable up to ~18 months; Posterior: closes between 2–3 months
Airway Anatomy
Tongue large relative to oral cavity; short, narrow trachea (↑ risk of obstruction)
Abdominal Organs
Liver and spleen poorly protected → vulnerable to trauma
Renal Function
Kidneys immature until ~12–18 months → limited urine concentration and electrolyte control
Water Balance
Larger proportion of total body weight is water (especially extracellular); rapid daily water exchange
Blood Volume
Weight dependent: ~80 mL/kg
Neurologic System
All brain cells present at birth; myelination continues during the first year
Cardiac Output
Rate-dependent (not stroke volume) until late school age/adolescence → HR crucial for perfusion
Communication And Interviewing A Child
- Effective communication is the most powerful tool a pediatric nurse has. It's essential to establish trust and rapport with both the child and their parents to obtain accurate information and ensure a positive healthcare experience.
Establishing a Setting for Communication
Create a safe, private, and comfortable environment. This might involve:
- Ensuring the room is quiet and free from distractions.
- Positioning yourself at the child's eye level.
- Using a warm, calm tone of voice.
- Having age-appropriate toys or books available.
Computer Privacy and Applications in Nursing
Nurses must adhere to strict privacy regulations (like HIPAA in the U.S.). This means:
- Never leaving a computer screen with patient information visible.
- Logging out of electronic health records (EHRs) when not in use.
- Using secure, encrypted systems for any electronic communication.
EHRs are invaluable for documenting assessments, tracking growth, and sharing information securely with other providers.
Telephone Triage and Counseling
When providing care over the phone, nurses must use a structured approach to:
- Assess the severity of the child's symptoms.
- Provide clear, concise instructions.
- Document every conversation meticulously.
- Recognize when a child needs immediate medical attention versus at-home care.
Communicating with Parents
Parents are the primary source of information and a crucial partner in care. The key is to:
- Listen actively and show empathy.
- Acknowledge their concerns and feelings.
- Use clear, simple language, avoiding medical jargon.
- Encourage them to ask questions and participate in decision-making.
Communicating with Children
Communication must be tailored to the child's developmental stage.
- Infants: Respond to touch, sound, and a calm tone. The assessment is often done with the parent holding the infant.
- Toddlers (1-3 years): Use simple words and short sentences. Give them choices when possible (e.g., "Do you want me to listen to your tummy first or your back?"). Fear of separation is common.
- Preschoolers (3-5 years): They have magical thinking. Explain procedures in a simple, non-threatening way (e.g., "I'm going to put a sticker on your finger to see how much air is in your blood.").
- School-age children (6-12 years): They can understand cause and effect. Give them more detailed explanations and allow them to participate in the exam.
- Adolescents (13-18 years): Treat them with respect. Ensure privacy and confidentiality. Address them directly and allow them to speak without interruption from parents.
Communication Techniques
- Therapeutic play: Use dolls, puppets, or drawings to explain procedures and assess the child's understanding and feelings.
- Clarification: "Can you tell me more about that?"
- Reflection: Repeating a word or phrase to encourage them to elaborate.
- Open-ended questions: "How have you been feeling?" vs. "Do you feel sick?"
History Taking
A comprehensive history provides context for the physical examination. Key components include:
- Demographics: Name, age, gender, ethnicity.
- Chief Complaint: The reason for the visit in the parent's and/or child's own words.
- History of Present Illness (HPI): Use the mnemonic "OLD CARTS" or "PQRST" to get a detailed description of the symptoms (Onset, Location, Duration, Character, Aggravating/Alleviating factors, Radiation, Timing, Severity).
- Past Medical History: Birth history, previous illnesses, hospitalizations, surgeries, injuries, and allergies.
- Family History: Genetic conditions, chronic diseases, and mental health issues within the family.
- Social History: Home environment, school performance, peer relationships, and exposure to tobacco or other substances.
- Review of Systems (ROS): A head-to-toe questioning about each body system to uncover any missed symptoms.
Nutritional Assessment
Nutrition is vital for growth and development. A proper nutritional assessment includes:
Dietary Intake
- 24-hour dietary recall: Ask the parent or child to describe everything the child ate and drank in the past 24 hours.
- Food frequency questionnaire: Ask about how often the child consumes certain foods or food groups.
- Observation: Note the child's appetite, feeding behaviors, and any feeding difficulties.
- Breastfeeding/Formula: For infants, document the type, amount, and frequency of feeding.
Clinical Examination and Nutrition
- General appearance: Note if the child appears well-nourished, underweight, or overweight.
- Skin: Check for signs of vitamin deficiencies, such as dry, flaky skin or petechiae.
- Hair: Note if the hair is dry, brittle, or sparse (can indicate protein deficiency).
- Mouth: Check for cracked lips, swollen tongue, or bleeding gums.
Evaluation of Nutritional Assessment
- Growth charts: Plot the child's weight, height/length, and head circumference on growth charts to see if they are following a consistent growth curve.
- BMI: Calculate and plot BMI for children over 2 years of age to screen for overweight or obesity.
- Laboratory values: Check for anemia (iron deficiency), vitamin D levels, or other micronutrient deficiencies if indicated.
General Approaches Toward Examining The Child
The pediatric physical exam is not a rigid, head-to-toe procedure. It must be flexible and opportunistic.
Sequence of Examination
- "Least invasive to most invasive" is the golden rule.
- Observation: Start by simply observing the child's general appearance, activity level, and interactions with parents.
- Auscultation: Listen to the heart, lungs, and abdomen while the child is quiet. This is best done early.
- Palpation/Percussion: Perform these on the abdomen and chest.
- Otoscopic/Oropharyngeal Exam: Save this for last, as it's often the most invasive and can cause the child to cry, making the rest of the exam difficult.
Preparation of the Child
- Infants: Keep them warm and close to their parent.
- Toddlers: Let them sit on the parent's lap. Use a toy or distraction.
- Preschoolers: Use simple, concrete explanations and let them touch the equipment.
- School-age: Give them choices and explain what you're doing.
- Adolescents: Provide privacy and explain the purpose of each part of the exam.
Nursing Insight: A key difference between a pediatric and adult physical exam is the order. You must adapt the exam to the child's mood and developmental stage. Crying can significantly alter vital signs, especially heart rate and respiratory rate.
Age-Based Examination Approaches
A. Newborns and Infants Under 6 Months
- Easiest to examine: Less resistance and less stranger anxiety.
- Keep the parent present for comfort.
- Soothing techniques: Feeding, pacifier, rocking, diaper change.
- Begin with auscultation when infant is quiet or sleeping.
- Proceed head-to-toe, saving disturbing procedures (e.g., hips) for last.
- Observe activity level, mood, responsiveness.
B. Infants Over 6 Months
- Separation/stranger anxiety emerges.
- Examine while sitting on parent’s lap; some steps (e.g., ears) may require child held against parent's chest.
- Keep room warm and child comfortable.
- Use soothing voice, toys, pacifier, bottle to calm.
- Begin exam with hands and feet, saving more invasive steps for later.
C. Toddlers
- Strong stranger anxiety; prefer to stay on parent’s lap.
- Allow child to observe instruments.
- Avoid yes/no questions (expect "No"). Instead, state actions confidently.
- Offer choices when possible (e.g., “Which ear first?”).
- Assess neurologic/musculoskeletal system by observing play.
- Perform ear, eye, and mouth exams last.
D. Preschoolers
- May be examined on parent’s lap or alone depending on age.
- Most cooperate and are willing to undress; keep underpants until genital exam.
- Let them handle equipment; use distraction and simple explanations.
- Offer praise and encouragement throughout.
E. School-Age Children
- Willing to cooperate; modesty begins to develop.
- Offer a gown to preserve modesty.
- Let child decide on privacy (parent present or not).
- Use a head-to-toe sequence.
- Teach using opportunities (e.g., let child listen to heart sounds).
F. Adolescents
- Protect modesty: Provide privacy for dressing, gowning, and during exam.
- Use head-to-toe sequence.
- Unless requested, perform exam without parents; chaperone required for genital/breast exams.
Nursing insight: Professionalism in Practice/Using Chaperones
Use a same-gender chaperone (nurse or technician) for breast/genital/anorectal exams. Family members are not substitutes. Follow institutional policies for documentation.
Physical Assessment
A detailed physical exam provides objective data to confirm or refute findings from the history.
Growth Measurements
- Head Circumference: Measured at the widest part of the head, from the supraorbital ridges to the occipital prominence. Monitored until age 2 to screen for microcephaly or macrocephaly.
- Length or Height: Length is measured while the child is lying down until age 2. Height is measured standing.
- Weight: Measured on a pediatric scale.
- Weight for Length: Used for infants and toddlers up to 24 months to assess for failure to thrive or obesity.
- Body Mass Index (BMI): Calculated for children 2 years and older as weight (kg)/height (m²). Plotted on a growth chart to assess for overweight or underweight.
Physiologic Measurements
- Temperature: Can be rectal (most accurate for infants), axillary, or tympanic depending on the age and situation.
- Pulse: Apical pulse is taken for 1 full minute in infants and young children. Radial pulse is used in older children.
- Respiratory Rate: Count for 1 full minute, noting any signs of respiratory distress.
- Oxygen Saturation: Measured with a pulse oximeter.
- Blood Pressure: Use an appropriate-sized cuff. The bladder should cover 80% of the arm's circumference.
General Appearance
- Appearance: Grooming, hygiene, and clothing appropriate for the weather.
- Posture and Position: Note any abnormal posturing or limp.
- Behavior: Note alertness, mood, and activity level.
- Nutrition: Note if the child appears well-nourished.
- Facial Expressions: Note for symmetry and any signs of pain or distress.
Skin
- Color: Note pallor, cyanosis, jaundice, or erythema.
- Temperature and Texture: Assess for warmth, dryness, or diaphoresis.
- Turgor: Assesses hydration by gently pinching the skin on the abdomen.
- Lesions: Document any rashes, bruises, or birthmarks.
Hyperpigmented patches (Mongolian spots)—bluish patches on sacral/buttock area in dark-skinned infants. Normal; fade by puberty.

- Nursing Insight: Bruises in non-mobile infants or in uncommon locations (e.g., trunk) may indicate abuse.
Lymph Nodes
- Palpate for enlarged nodes in the cervical, occipital, and axillary areas. Normal nodes are small, non-tender, and mobile.
Head and Neck, Eyes, Ears, and Nose
Head: Skull and Facial Features
|
Assessment Focus |
Normal Findings |
Abnormal Findings |
|
Skull shape & size |
Symmetrical, rounded; fontanels soft and flat in infants |
Bulging fontanel (↑ ICP), sunken fontanel (dehydration), asymmetry (craniosynostosis) |
|
Sutures |
Palpable in newborns, gradually fuse with age |
Wide sutures (↑ ICP), early closure |
|
Facial features |
Symmetrical, appropriate for age |
Dysmorphic features (e.g., low-set ears, slanted eyes, wide-spaced eyes—may indicate syndromes) |
Nursing Insight: The anterior fontanelle typically closes between 12 and 18 months of age, while the posterior fontanelle closes much earlier, usually by 2 to 3 months. A bulging fontanelle can indicate increased intracranial pressure, and a sunken fontanelle can indicate dehydration.
Eyes: Structures, Function, and Vision
|
Assessment Focus |
Normal Findings |
Abnormal Findings |
|
Eyelids, sclera, conjunctiva |
Symmetrical, white sclera, pink conjunctiva |
Redness, discharge, ptosis, jaundice |
|
Pupils (PERRLA) |
Equal, round, reactive to light and accommodation |
Unequal size, sluggish or non-reactive pupils |
|
Extraocular movements |
Eyes move together in 6 directions |
Strabismus, nystagmus |
|
Vision screening |
Age-appropriate acuity (Snellen chart from age 3–4) |
Inattention, squinting, poor school performance |
Ears: Structure and Hearing
|
Assessment Focus |
Normal Findings |
Abnormal Findings |
|
External ear |
Aligned with outer canthus of eye |
Low-set ears (may indicate genetic conditions) |
|
Ear canal & tympanic membrane |
Clear canal, pearly-gray TM with light reflex |
Redness, bulging TM (otitis media), discharge |
|
Hearing (age-appropriate) |
Startle to loud sound (infants), responds to name |
Lack of response, inattentiveness |
Hearing tests:
- Newborns: Otoacoustic emissions (OAE)
- Older infants/children: Response to sound, audiometry
Nursing Insight: When performing an otoscopic exam on a child under 3, pull the pinna down and back. For a child over 3, pull the pinna up and back, just like in adults.
Nose and Sinuses
|
Assessment Focus |
Normal Findings |
Abnormal Findings |
|
Patency |
Bilateral air movement |
Nasal flaring (respiratory distress), obstruction |
|
Nasal mucosa |
Moist, pink |
Pale (allergies), red/swollen (infection) |
|
Discharge |
None or clear |
Purulent (infection), unilateral foul odor (foreign body) |
|
Sinus palpation |
Nontender (older children) |
Tenderness (sinusitis) |
Mouth and Throat
|
Assessment Focus |
Normal Findings |
Abnormal Findings |
|
Lips/mucosa/tongue |
Pink, moist, intact |
Dry/cracked (dehydration), lesions, thrush |
|
Teeth |
Appropriate for age, no caries |
Cavities, delayed eruption |
|
Tonsils |
Small to moderate size, pink |
Enlarged, exudate (pharyngitis, tonsillitis) |
|
Uvula |
Midline, rises with phonation |
Deviation (cranial nerve palsy) |
Primary and Secondary Tooth Eruption
Chest and Lungs
|
Assessment Focus |
Normal Findings |
Abnormal Findings |
|
Chest shape |
Symmetrical, rounded in infants; more adult-like with age |
Pectus excavatum/carinatum, barrel chest (asthma) |
|
Respiratory effort |
Quiet, even, no retractions |
Nasal flaring, retractions, grunting, tachypnea |
|
Breath sounds |
Clear bilaterally |
Crackles (pneumonia), wheezes (asthma), absent sounds |
9.9. Heart
|
Assessment Focus |
Normal Findings |
Abnormal Findings |
|
Heart sounds |
S1 & S2 distinct, regular rhythm |
Murmurs, gallops, irregular rhythms |
|
Apical pulse |
Counted for 1 full minute |
Tachycardia or bradycardia for age |
|
Capillary refill |
< 2 seconds |
Delayed refill (poor perfusion) |
|
Pulses (central/peripheral) |
Equal bilaterally |
Bounding or weak pulses (cardiac issues) |
Abdomen
- Inspection: Note contour, symmetry, and visible pulsations.
- Auscultation: Listen for bowel sounds.
- Palpation: Palpate for tenderness, masses, or organomegaly (e.g., enlarged liver or spleen).
|
Assessment Focus |
Normal Findings |
Abnormal Findings |
|
Contour |
Round in infants, flat in older children |
Distension, visible peristalsis |
|
Bowel sounds |
Present in all quadrants |
Absent (ileus), hyperactive (diarrhea) |
|
Palpation |
Soft, non-tender, organs not enlarged |
Masses, guarding, tenderness |
|
Liver & spleen |
May be palpable in young children |
Enlargement (hepatosplenomegaly) |
Genitalia
|
Assessment Focus |
Normal Findings |
Abnormal Findings |
|
External genitalia (male/female) |
Normal anatomy, no lesions or swelling |
Hypospadias, labial fusion, masses, discharge |
|
Testes (males) |
Descended, no masses |
Undescended testes, hydrocele, hernia |
|
Hygiene |
Clean, no odor or rash |
Signs of infection or abuse |
Anus
- Inspection: Check for rashes, fissures, or hemorrhoids.
Musculoskeletal System
|
Assessment Focus |
Normal Findings |
Abnormal Findings |
|
Posture & gait |
Symmetrical, age-appropriate |
Limping, scoliosis, toe-walking |
|
Joints |
Full range of motion, no swelling |
Limited movement, swelling, redness |
|
Muscle strength |
Equal bilaterally |
Weakness, asymmetry |
|
Spine |
Straight alignment |
Scoliosis (screen from age 10 onward) |
Neurologic Assessment
|
Assessment Focus |
Normal Findings |
Abnormal Findings |
|
Behavior & alertness |
Alert, appropriate for age |
Lethargy, irritability, altered LOC |
|
Cranial nerves |
Intact (e.g., suck/swallow, facial expression) |
Facial asymmetry, drooling, ptosis |
|
Motor coordination |
Smooth, purposeful movements |
Tremors, clumsiness, abnormal reflexes |
|
Reflexes |
Age-appropriate (e.g., Moro in infants) |
Persistence of primitive reflexes |
|
Sensory |
Responsive to touch/pain |
Absent or exaggerated responses |
Developmental Assessment
- Use standardized screening tools (e.g., Denver II) to assess gross motor, fine motor, language, and personal-social skills.
- Compare the child's skills to expected milestones for their age.
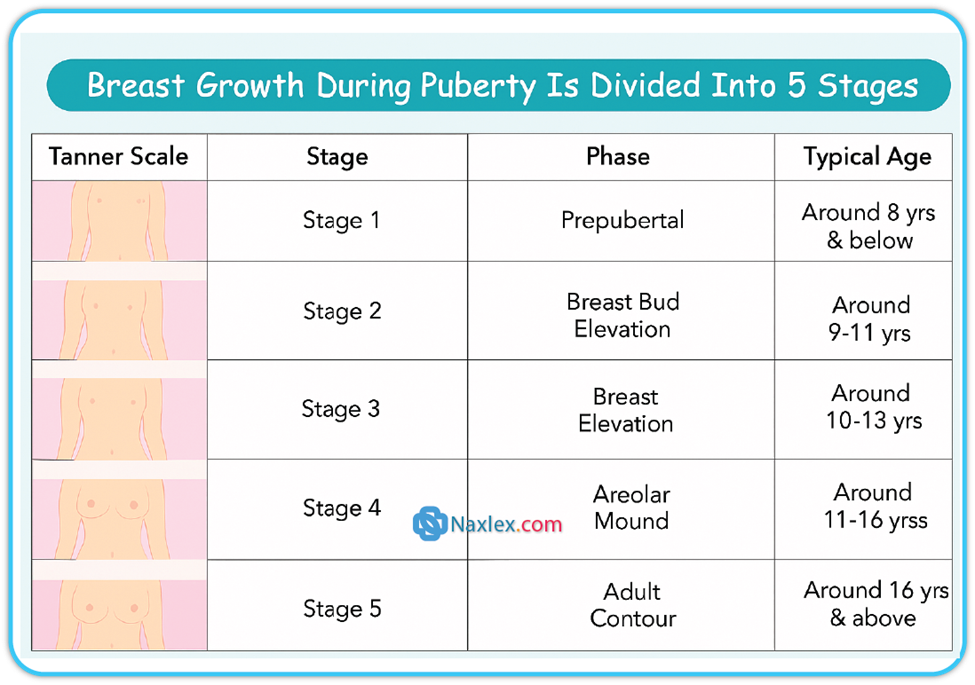
Pubertal Development and Sexual Maturation
Use Tanner Staging to assess:
|
Stage |
Girls (Breasts/Pubic Hair) |
Boys (Genitalia/Pubic Hair) |
|
I |
Prepubertal |
Prepubertal |
|
II |
Breast budding, sparse hair |
Testes enlarge, sparse hair |
|
III |
Enlargement, dark curlier hair |
Penis enlarges, darker hair |
|
IV |
Areola forms mound, coarse hair |
Scrotum darkens, coarse hair |
|
V |
Adult maturity |
Adult maturity |
Summary
- A comprehensive childhood and family assessment is a dynamic, multifaceted process. It combines effective communication, a detailed health history, a thorough physical examination, and an evaluation of a child's nutritional status and development.
- Pediatric history-taking involves both the caregiver and child, emphasizing rapport, open-ended questions, empathy, and cultural sensitivity. Communication should be age-appropriate and respectful of family dynamics and traditions. Nurses must listen carefully to verbal and nonverbal cues and address sensitive topics gently.
- The key to a successful assessment is to be flexible, patient, and to always put the child and family at the center of your care. By mastering these skills, you can provide the best possible care for your pediatric patients.
- Systematic review of all body systems, growth measurements, and observation of developmental milestones guide holistic evaluation. Cultural competence, privacy, and age-appropriate communication are essential to ensure accurate, respectful, and effective pediatric care.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Childhood And Family Assessment
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


