Please set your exam date
Postpartum Disorders: DVT, Pulmonary Embolism
Study Questions
Introduction
A nurse is caring for a postpartum client who had a cesarean birth.
Which of the following actions should the nurse take to prevent DVT in this client?
Explanation
The correct answer is choice B. Encourage early and frequent ambulation.This action helps to prevent DVT by keeping the blood flowing in the lower legs and reducing venous stasis.Early and frequent ambulation is also recommended by various clinical guidelines for postpartum VTE prevention.
Choice A is wrong because applying a heating pad to the lower legs does not prevent DVT and may increase the risk of bleeding or infection.
Choice C is wrong because placing a pillow under the knees when in bed does not prevent DVT and may worsen venous stasis by compressing the iliac veins.
Choice D is wrong because massaging the affected limb gently does not prevent DVT and may dislodge a clot or cause damage to the vein wall.
A nurse is assessing a postpartum client who reports leg pain and tenderness.
The nurse observes unilateral swelling, warmth, and redness of the lower extremity.
Which of the following conditions should the nurse suspect?
Explanation
The correct answer is choice B. Deep vein thrombosis (DVT) is a condition where a blood clot forms in a deep vein, usually in the leg.It can cause pain, swelling, redness and warmth in the affected area.DVT is more serious than superficial thrombophlebitis, which is inflammation of a vein near the skin due to a blood clot.DVT can lead to complications such as pulmonary embolism, which is a life-threatening condition where the blood clot travels to the lungs and blocks an artery.
Choice A is wrong because superficial thrombophlebitis is not as severe as DVT and does not usually cause swelling of the whole leg.
Choice C is wrong because pulmonary embolism is not a condition of the leg, but a complication of DVT that affects the lungs.
Choice D is wrong because idiopathic thrombocytopenic purpura (ITP) is a disorder that causes low platelet count and bleeding problems, not blood clots.
Normal ranges for platelet count are 150,000 to 450,000 platelets per microliter of blood.Normal ranges for D-dimer test are less than 0.5 micrograms per milliliter of blood.
A nurse is teaching a postpartum client who is at high risk for venous insufficiency about measures to prevent thrombophlebitis.
Which of the following instructions should the nurse include? (Select all that apply.)
Explanation
The correct answer is choice A, B, D and E. These are measures to prevent thrombophlebitis, which is a condition where a blood clot forms in a vein and causes inflammation and pain.
Thrombophlebitis can lead to serious complications such as pulmonary embolism, which is a life-threatening condition where a blood clot travels to the lungs and blocks the blood flow.
Choice A is correct because wearing fitted elastic thromboembolic hose can help compress the veins and improve the blood flow in the legs, reducing the risk of clot formation.
Choice B is correct because drinking 2 to 3 L of fluid per day can help prevent dehydration, which can make the blood thicker and more prone to clotting.
Choice D is correct because elevating your legs above your heart level can help reduce the pressure and swelling in the veins, improving the blood circulation and preventing stasis.
Choice E is correct because smoking can damage the lining of the blood vessels, increase the blood pressure and heart rate, and make the blood more sticky and likely to clot.
Choice C is wrong because crossing your legs when sitting can impair the blood flow in the legs and increase the risk of thrombophlebitis.
It is recommended to avoid prolonged sitting and to move your legs frequently.
Normal ranges for fluid intake are about 2 to 3 L per day for adults, depending on age, weight, activity level and health conditions.
Normal ranges for leg elevation are about 15 to 30 degrees above the heart level.
A nurse is reviewing the laboratory results of a postpartum client who has idiopathic thrombocytopenic purpura (ITP).
Which of the following findings should the nurse expect?
Explanation
The correct answer is choice A. Decreased platelet count.ITP is a disorder that causes low levels of platelets due to immune system malfunction or increased breakdown of platelets.
Platelets are blood cells that control bleeding and prevent bruising.Normal platelet count ranges from 150,000 to 450,000 per microliter of blood.
Choice B is wrong because increased prothrombin time means prolonged clotting time, which is not a feature of ITP.Prothrombin time measures how long it takes for the blood to clot and is affected by factors such as liver disease, vitamin K deficiency, or blood-thinning medications.
Choice C is wrong because decreased fibrinogen level means reduced ability to form blood clots, which is not a feature of ITP.Fibrinogen is a protein that helps the blood to clot and is affected by factors such as liver disease, inflammation, infection, or trauma.
Choice D is wrong because increased partial thromboplastin time means prolonged clotting time, which is not a feature of ITP.Partial thromboplastin time measures how long it takes for the blood to clot and is affected by factors such as hemophilia, lupus, or blood-thinning medications.
A nurse is monitoring a postpartum client who has disseminated intravascular coagulation (DIC).
Which of the following manifestations should the nurse report to the provider immediately?
Explanation
The correct answer is choice C. Tachycardia and hypotension.
These are signs of shock due to severe blood loss and should be reported to the provider immediately.DIC can cause both excessive clotting and bleeding, which can lead to organ damage and death.
Choice A is wrong because petechiae on the chest and abdomen are common manifestations of DIC due to low platelet count and increased fibrin degradation products.
They are not life-threatening by themselves and do not require immediate intervention.
Choice B is wrong because hematuria in the urinary catheter bag is another manifestation of DIC due to bleeding in the urinary tract.
It is not an emergency unless it is accompanied by other signs of shock or renal failure.
Choice D is wrong because oozing of blood from IV site is also a manifestation of DIC due to impaired coagulation.
It can be managed by applying pressure and changing the dressing.
It is not a priority over signs of shock.
Normal ranges for platelet count are 150,000 to 450,000 per microliter of blood, for fibrinogen level are 200 to 400 mg/dL, for prothrombin time are 11 to 13.5 seconds, for partial thromboplastin time are 25 to 35 seconds, and for D-dimer level are less than 0.5 mcg/mL.
Clinical Manifestations of DVT
A nurse is assessing a client who has a history of deep vein thrombosis (DVT).
Which of the following findings should the nurse report to the provider?
Explanation
The correct answer is choice A.Warmth and erythema in the affected leg are signs of inflammation and possible infection caused by deep vein thrombosis (DVT), a condition in which blood clots form in veins located deep inside the body, usually in the thigh or lower legs.
The nurse should report this finding to the provider as it may indicate a serious complication.
Choice B is wrong because a negative Homans’ sign, which is the absence of pain in the calf when the foot is dorsiflexed, does not rule out DVT.This sign is unreliable and nonspecific for DVT diagnosis.
Choice C is wrong because decreased calf circumference is not a typical symptom of DVT.In fact, DVT may cause swelling of the affected leg due to impaired blood flow.
Choice D is wrong because pallor and coolness in the affected leg are more indicative of arterial occlusion, which is a blockage of blood flow in an artery, rather than venous occlusion, which is a blockage of blood flow in a vein.
Normal ranges for D-dimer blood test, which measures a substance in the blood that’s released when a blood clot dissolves, are less than 0.5 mcg/mL or 500 ng/mL.High levels of D-dimer may indicate DVT or other conditions that cause blood clots.
A nurse is caring for a client who is at risk for developing DVT after a total hip replacement surgery.
Which of the following interventions should the nurse include in the plan of care to prevent DVT? (Select all that apply.)
Explanation
The correct answer is choice C. Administer low molecular weight heparin.Low molecular weight heparin is an anticoagulant drug that prevents the formation and growth of blood clots in patients at risk for VTE.It is recommended for patients undergoing hip replacement surgery as a pharmacological prophylaxis.
Choice A is wrong because applying sequential compression devices (SCDs) is not enough to prevent VTE in patients undergoing hip replacement surgery.SCDs are mechanical devices that improve blood flow in the legs by inflating and deflating around them.However, they are not as effective as anticoagulant drugs in reducing the incidence of VTE.
Choice B is wrong because encouraging early ambulation is not enough to prevent VTE in patients undergoing hip replacement surgery.Early ambulation is the act of walking soon after surgery to improve circulation and prevent complications.However, it is not associated with a lower risk of VTE compared to bed rest.
It may also be contraindicated in some patients depending on their surgical and medical conditions.
Choice D is wrong because elevating the affected leg above the level of the heart is not enough to prevent VTE in patients undergoing hip replacement surgery.Elevating the leg may help reduce swelling and pain, but it does not prevent clot formation or propagation.
Choice E is wrong because massaging the affected leg gently is not only ineffective but also harmful for preventing VTE in patients undergoing hip replacement surgery.Massaging the leg may dislodge existing clots and cause them to travel to the lungs, resulting in a life-threatening pulmonary embolism.
A nurse is reviewing the laboratory results of a client who is receiving unfractionated heparin for DVT.
Which of the following values indicates a therapeutic effect of heparin?
Explanation
The correct answer is choice B. Activated partial thromboplastin time (aPTT) of 60 seconds.This value indicates a therapeutic effect of heparin because it is about two times the normal value of 25 to 35 seconds.Heparin produces its major anticoagulant effect by inactivating thrombin and factor Xa through an antithrombin-dependent mechanism.The APTT measures the intrinsic and common pathways of coagulation, which are affected by heparin.
Choice A is wrong because platelet count of 150,000/mm3 is within the normal range of 150,000 to 450,000/mm3.Heparin does not affect platelet count directly, but it can cause heparin-induced thrombocytopenia, a serious complication that reduces platelet count and increases the risk of thrombosis.
Choice C is wrong because prothrombin time (PT) of 12 seconds is within the normal range of 11 to 13.5 seconds.Heparin does not affect PT significantly because PT measures the extrinsic and common pathways of coagulation, which are not affected by heparin.
Choice D is wrong because international normalized ratio (INR) of 1.0 is within the normal range of 0.8 to 1.2.Heparin does not affect INR significantly because INR is a standardized measure of PT that reflects the activity of vitamin K-dependent factors, which are not affected by heparin.
A nurse is teaching a client who has DVT and is prescribed warfarin.
Which of the following instructions should the nurse include in the teaching?
Explanation
The correct answer is choice D. All of the above.
The nurse should include the following instructions in the teaching:
• Avoid foods that are high in vitamin K.Vitamin K can lower the effect of warfarin and increase the risk of blood clots.Foods rich in vitamin K are green vegetables, such as lettuce, spinach and broccoli.
• Use an electric razor for shaving.Warfarin can increase the risk of bleeding, so using a sharp blade can cause cuts and bruises.
• Monitor for signs of bleeding gums.Bleeding gums can be a sign of excessive anticoagulation and a potential side effect of warfarin.
Choice A is wrong because avoiding foods that are high in vitamin K is not enough to prevent bleeding complications.
The client should also follow other precautions, such as using an electric razor and monitoring for signs of bleeding gums.
Choice B is wrong because using an electric razor for shaving is not enough to prevent bleeding complications.
The client should also avoid foods that are high in vitamin K and monitor for signs of bleeding gums.
Choice C is wrong because monitoring for signs of bleeding gums is not enough to prevent bleeding complications.
The client should also avoid foods that are high in vitamin K and use an electric razor for shaving.
A nurse is preparing to discharge a client who has DVT and is prescribed low molecular weight heparin (LMWH).
Which of the following information should the nurse include in the discharge teaching?
Explanation
The correct answer is A. How to administer LMWH subcutaneously.LMWH is a class of anticoagulant medications that are used to prevent and treat blood clots, such as DVT and PELMWH can be given subcutaneously and does not require frequent blood tests to monitor coagulation, unlike unfractionated heparinTherefore, the nurse should teach the client how to inject LMWH into the fatty tissue under the skin, usually in the abdomen or thigh, using a prefilled syringe.
B. The need for frequent blood tests to monitor coagulation.This statement is wrong because LMWH has more predictable pharmacokinetics and anticoagulant effect than unfractionated heparin, and does not require routine monitoring of APTT or anti-factor Xa levelsHowever, some patients may need monitoring in special situations, such as extremes of weight, renal impairment, or pregnancy.
C. The signs and symptoms of heparin-induced thrombocytopenia (HIT).This statement is wrong because HIT is a rare but serious complication of heparin therapy that causes a drop in platelet count and an increased risk of thrombosisHIT is more common with unfractionated heparin than with LMWH, but it can still occur with LMWH in some casesTherefore, the nurse should inform the client about the signs and symptoms of HIT, such as fever, chills, rash, bleeding, bruising, or new or worsening clots, and advise them to seek medical attention if they occur.
D. The antidote for LMWH in case of overdose.This statement is wrong because there is no specific antidote for LMWH in case of overdose or bleeding complicationsUnlike unfractionated heparin, which can be reversed with protamine sulfate, LMWH has only partial reversal with protamine sulfate and may require other measures such as transfusion of blood products or use of recombinant factor VIIaTherefore, the nurse should instruct the client to follow the prescribed dose and schedule of LMWH and to report any signs of bleeding or overdose, such as nosebleeds, gum bleeding, blood in urine or stool, or excessive bruising.
Clinical Manifestations of PE
A nurse is caring for a client who has a pulmonary embolism.
The client reports sudden onset of dyspnea and chest pain.
What is the priority action by the nurse?
Explanation
The correct answer is choice A. Administer oxygen therapy.The priority action by the nurse for a client who has a pulmonary embolism is to increase perfusion and oxygenation by providing oxygen therapy.
This can help reduce hypoxemia, dyspnea, and chest pain.
Oxygen therapy can also prevent further clotting and pulmonary vasoconstriction.
Choice B is wrong because obtaining a chest x-ray is not the immediate action for a client with a pulmonary embolism.A chest x-ray can help confirm the diagnosis, but it is not a priority over oxygen therapy.
Choice C is wrong because starting an IV line is not the first action for a client with a pulmonary embolism.An IV line can facilitate the administration of fluids and medications, such as anticoagulants and thrombolytics, but it is not as urgent as oxygen therapy.
Choice D is wrong because giving morphine for pain is not the most important action for a client with a pulmonary embolism.Morphine can help relieve pain and anxiety, but it can also depress respiration and lower blood pressure, which can worsen the condition of the client.
Normal ranges for oxygen saturation are 95% to 100%.
Normal ranges for blood pressure are 120/80 mmHg or lower.
Normal ranges for heart rate are 60 to 100 beats per minute.Normal ranges for respiratory rate are 12 to 20 breaths per minute.
A nurse is reviewing the laboratory results of a client who has a suspected pulmonary embolism.
Which of the following findings indicates an increased risk for clot formation?
Explanation
The correct answer is choice A. Elevated D-dimer level.
D-dimer is a fibrin degradation product that is released when a blood clot is dissolved.A high level of D-dimer indicates an increased likelihood of blood clots, such as pulmonary embolism.A normal D-dimer level (below 500 ng/mL) can rule out pulmonary embolism in patients with low or moderate clinical pretest probability.
Choice B is wrong because decreased platelet count is not associated with pulmonary embolism.Platelet count may decrease after pulmonary embolism due to platelet activation and consumption, but it is not a risk factor for clot formation.
Choice C is wrong because low hematocrit level is not associated with pulmonary embolism.
Hematocrit level may decrease due to blood loss, hemolysis, or dilution, but it does not affect the risk of clot formation.
Choice D is wrong because high prothrombin time is not associated with pulmonary embolism.
Prothrombin time measures the time it takes for blood to clot in the presence of vitamin K-dependent factors.
A high prothrombin time indicates a deficiency or inhibition of these factors, which may increase the risk of bleeding, not clotting.
Normal ranges for D-dimer, platelet count, hematocrit, and prothrombin time may vary depending on the laboratory and the method used, but generally they are:
• D-dimer: <500 ng/mL
• Platelet count: 150-450 x 10^9/L
• Hematocrit: 36-48% for females, 40-54% for males
• Prothrombin time: 11-13 seconds
A nurse is teaching a client who has a history of deep vein thrombosis about prevention of pulmonary embolism.
Which of the following statements by the client indicates understanding of the teaching?
Explanation
The correct answer is choice A.“I should avoid smoking cigarettes.” Smoking cigarettes increases the risk of blood clots and deep vein thrombosis (DVT), which can lead to pulmonary embolism (PE) if the clot travels to the lungs.Smoking also damages the blood vessels and reduces oxygen levels in the blood.
Choice B is wrong because aspirin is not a recommended medication for preventing PE.Aspirin is a type of antiplatelet drug that prevents platelets from sticking together and forming clots, but it does not affect the clotting factors in the blood that are involved in DVT and PE.Anticoagulants, also known as blood thinners, are the preferred medications for preventing and treating DVT and PE, as they prevent further clot formation and decrease the chances of new clots.
Choice C is wrong because limiting fluid intake can increase the risk of dehydration, which can thicken the blood and make it more prone to clotting.Drinking plenty of water is important for preventing DVT and PE, especially when traveling or being immobile for long periods of time.
Choice D is wrong because wearing tight-fitting socks can restrict blood flow in the legs and increase the risk of DVT and PE.
A nurse is preparing to administer enoxaparin (Lovenox) to a client who has a pulmonary embolism.
Which of the following actions should the nurse take?
Explanation
Pinch the skin at the injection site.
This is because enoxaparin is a low molecular weight heparin that is administered subcutaneously, which means under the skin.Pinching the skin helps to create a fold of tissue that can be injected with the medication.Expelling the air bubble from the prefilled syringe is not necessary, as it helps to prevent leakage of the medication after injection.Injecting the medication into the deltoid muscle is wrong, as enoxaparin should not be given intramuscularly.Applying pressure to the injection site after administration is also wrong, as it can cause bruising or hematoma.
A nurse is monitoring a client who is receiving alteplase (Activase) for a pulmonary embolism.
Which of the following findings requires immediate intervention by the nurse?
Explanation
Hematuria.
Hematuria is the presence of blood in the urine and it indicates a bleeding complication from alteplase therapy.Alteplase is a thrombolytic drug that dissolves blood clots and restores blood flow, but it can also cause significant bleeding.
Hematuria requires immediate intervention by the nurse to stop the infusion and treat the bleeding.
Choice A is wrong because a blood pressure of 150/90 mmHg is not a contraindication for alteplase therapy.Alteplase should not be given to patients with severe uncontrolled hypertension, defined as systolic blood pressure >180 mmHg or diastolic blood pressure >110 mmHg.
Choice B is wrong because a heart rate of 100/min is not a sign of adverse reaction to alteplase therapy.Alteplase can cause cardiac arrhythmias, but they are usually transient and do not require treatment.
Choice C is wrong because a hemoglobin of 12 g/dL is within the normal range for adults (13.5-17.5 g/dL for males and 12-15.5 g/dL for females).
A low hemoglobin level may indicate bleeding or hemolysis from alteplase therapy and should be monitored closely.
Diagnostic Methods
A nurse is reviewing the results of a client’s D-dimer blood test.
The nurse knows that this test can help rule out which of the following conditions? (Select all that apply)
Explanation
The correct answer is choice A, B and E.A D-dimer test is a blood test that measures D-dimer, which is a protein fragment that your body makes when a blood clot dissolves in your body.A positive or elevated D-dimer test result may indicate that you have a blood clotting condition, such as:
• Deep vein thrombosis (DVT): a blood clot that develops in a vein deep in your body, usually in the legs.
• Pulmonary embolism (PE): a blockage in an artery in the lung caused by a blood clot that travels from another part of the body, such as the leg.
• Disseminated intravascular coagulation (DIC): a condition that prevents the blood from clotting normally and causes excessive bleeding or clotting throughout the body.
Choice C and D are wrong because:
• Myocardial infarction (MI): a heart attack caused by a blockage in one of the coronary arteries that supply blood to the heart muscle.A D-dimer test is not used to diagnose MI because other blood tests, such as troponin and CK-MB, are more specific and sensitive for detecting heart muscle damage.
• Stroke: a brain attack caused by a blockage or rupture of a blood vessel in the brain.A D-dimer test is not used to diagnose stroke because other imaging tests, such as CT scan or MRI, are more accurate and reliable for detecting brain damage.
The normal range of D-dimer levels varies depending on the laboratory and the method used, but it is usually less than 0.5 mg/L or 500 ng/mL.However, the normal range may also depend on other factors, such as age, pregnancy, inflammation, infection, trauma, surgery or cancer.
Therefore, a D-dimer test result should always be interpreted in the context of the clinical situation and other test results.
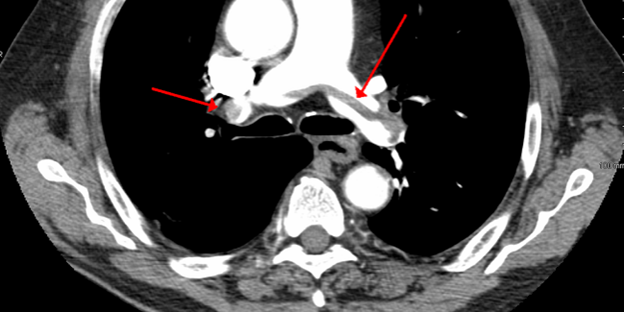
A nurse is caring for a client who has a suspected pulmonary embolism. The nurse anticipates that the physician will order which of the following diagnostic tests as the gold standard for confirming the diagnosis?
Explanation
CT pulmonary angiography (CTPA) is the new reference standard for the diagnosis of pulmonary embolism (PE).It is a non-invasive imaging test that uses contrast dye and X-rays to visualize the pulmonary arteries and detect blood clots.
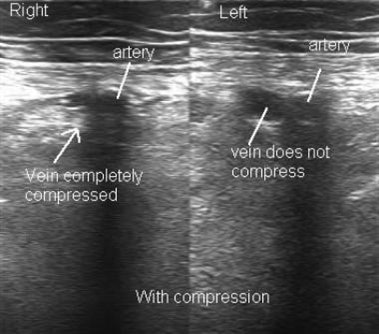
Choice A is wrong because compression ultrasound is used to diagnose deep vein thrombosis (DVT), not PE.However, if a DVT is found in a patient with clinical suspicion for PE, the diagnosis of PE can be accepted without further testing.
Choice C is wrong because ventilation-perfusion scan is an alternative test for PE when CTPA is contraindicated or unavailable.It uses radioactive tracers to measure the airflow and blood flow in the lungs and detect any mismatch that suggests a PE.
Choice D is wrong because chest X-ray cannot diagnose PE directly.
It can only show nonspecific signs of PE such as atelectasis, pleural effusion, or elevated hemidiaphragm.It can also help rule out other causes of chest pain or dyspnea.
A nurse is educating a client who is at high risk for developing deep vein thrombosis.
The nurse should instruct the client to avoid which of the following activities?
Explanation
Crossing the legs when sitting.
This is because crossing the legs can impair blood circulation and increase the risk of clot formation in the lower extremities.
Choice A is wrong because wearing compression stockings can help prevent deep vein thrombosis by applying pressure to the legs and improving blood flow.
Choice B is wrong because elevating the legs when sitting can also improve blood circulation and reduce swelling and pain in the legs.
Choice C is wrong because drinking plenty of fluids can prevent dehydration and blood viscosity, which are risk factors for deep vein thrombosis.
Normal ranges for blood clotting tests are:
• Prothrombin time (PT): 11 to 13.5 seconds
• International normalized ratio (INR): 0.8 to 1.2
• Activated partial thromboplastin time (aPTT): 25 to 35 seconds
• D-dimer: less than 0.5 mcg/mL
A nurse is assessing a client who has a pulmonary embolism.
The nurse should expect to find which of the following signs and symptoms? (Select all that apply)
Explanation
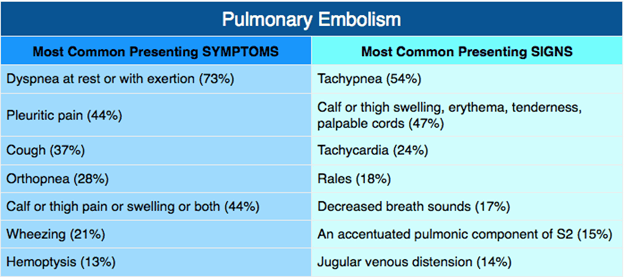
The correct answer is choice A, B and E. A pulmonary embolism (PE) is a blood clot that blocks an artery in the lung and reduces blood flow and oxygen levels.
The common symptoms of PE are:
• Dyspnea(sudden, unexplained shortness of breath)
• Pleuritic chest pain(dull pain that gets worse with deep breathing)
• Hemoptysis(coughing up blood)
Choice C is correct because hemoptysis is a possible symptom of PE, although it is less common than dyspnea and chest pain.Hemoptysis occurs when the blood clot damages the lung tissue and causes bleeding
Choice D is wrong because bradycardia (slow heart rate) is not a typical symptom of PE.In fact, most people with PE have tachycardia (fast heart rate) due to the increased strain on the heart and the reduced oxygen levels
Choice E is correct because hypoxemia (low oxygen levels in the blood) is a common complication of PE.
Hypoxemia can cause pale, clammy or bluish skin, excessive sweating, anxiety, lightheadedness or fainting.Hypoxemia can also worsen the heart strain and lead to heart failure or cardiac arrest
Normal ranges for oxygen saturation are 95% to 100%.Normal ranges for heart rate are 60 to 100 beats per minute
A nurse is administering heparin to a client who has a deep vein thrombosis.
The nurse should monitor which of the following laboratory values to evaluate the effectiveness of the therapy?
Explanation
Activated partial thromboplastin time (aPTT) is a test that measures how long it takes for blood to clot.It is used to monitor the effectiveness of heparin therapy, which is an anticoagulant (blood thinner) that prevents the formation of blood clots.Heparin affects one set of clotting factors that are measured by the aPTT test.The normal range of aPTT is 30-40 seconds, but in patients receiving heparin therapy, the range is 1.5-2.5 times the control value in seconds.
Choice A is wrong because prothrombin time (PT) is another test that measures how long it takes for blood to clot, but it is used to monitor the effectiveness of warfarin therapy, which is another anticoagulant that affects a different set of clotting factors than heparin.
Choice B is wrong because international normalized ratio (INR) is a standardized way of reporting the PT results, which are affected by warfarin therapy, not heparin therapy.
Choice D is wrong because platelet count is a test that measures the number of platelets in the blood, which are cells that help with clotting.Platelet count is not affected by heparin therapy and does not reflect its effectiveness.
Nursing Interventions for DVT and PE Prevention
A nurse is caring for a postpartum patient who is at risk for developing DVT.
Which of the following interventions should the nurse implement to prevent DVT? (Select all that apply.).
Explanation
These are the interventions that can help prevent DVT by keeping the blood flowing and preventing clot formation.
Choice D is wrong because massaging the affected limb can dislodge a clot and cause a PE.Choice E is wrong because elevating the affected limb can reduce blood flow and increase the risk of DVT.
Normal ranges for DVT prevention vary depending on the individual risk factors and clinical situation, but some general recommendations are:
• Encourage early and frequent ambulation as soon as possible after delivery.
• Apply anti-embolism stockings or intermittent pneumatic compression devices during hospital stay and until fully mobile.
• Administer prophylactic anticoagulant medication as prescribed, usually for 6 to 12 weeks postpartum or longer if high risk.The type and dose of anticoagulant may depend on the patient’s weight, renal function, breastfeeding status and preference.
A nurse is reviewing the laboratory results of a client who has DVT and is receiving unfractionated heparin IV.
Which of the following laboratory tests should the nurse monitor to evaluate the effectiveness of heparin therapy?
Explanation
Activated partial thromboplastin time (aPTT).The aPTT test is used to monitor the effectiveness of heparin therapy in clients with DVT.Heparin works by inhibiting the formation of blood clots by blocking the activity of clotting factors.The aPTT test measures the time it takes for a clot to form in a sample of blood after substances that cause clotting have been added.The normal range for aPTT is 30-40 seconds.
Prothrombin time (PT) is used to monitor warfarin therapy, not heparin therapy.
International normalized ratio (INR) is used to monitor warfarin therapy, not heparin therapy.
D-dimer is used to diagnose DVT, not monitor heparin therapy.
A nurse is teaching a client who has DVT and is prescribed warfarin.
The nurse should instruct the client to avoid fluctuations in the amount and frequency of consumption of which of the following foods?
Explanation
Spinach.The nurse should instruct the client to avoid fluctuations in the amount and frequency of consumption of foods that are rich in vitamin K, such as spinach, because they can make warfarin less effective.Vitamin K is involved in blood clotting and can counteract the anticoagulant effect of warfarin.
Grapefruit is wrong because grapefruit can increase the risk of bleeding by affecting warfarin metabolism or pharmacodynamics.Grapefruit can inhibit the enzyme CYP3A4 that metabolizes warfarin and increase its blood levels.
Cheese is wrong because cheese does not have a significant interaction with warfarin.However, some types of cheese, such as mature cheese and blue cheese, contain small amounts of vitamin K and should be consumed consistently.
Eggs is wrong because eggs do not have a significant interaction with warfarin.However, egg yolks contain some vitamin K and should be consumed consistently.
A nurse is assessing a client who has DVT and reports sudden onset of dyspnea and chest pain.
The nurse should suspect that the client has developed which of the following complications?
Explanation
Pulmonary embolism.A pulmonary embolism is a condition in which a blood clot blocks an artery in the lung, preventing blood flow to part of the lung.A pulmonary embolism can be a complication of deep vein thrombosis (DVT), which is a condition in which a blood clot forms in a deep vein, usually in the leg.If the clot breaks off and travels to the lung, it can cause a pulmonary embolism.The symptoms of a pulmonary embolism include sudden onset of dyspnea (difficulty breathing) and chest pain, which may worsen with coughing or deep breathing.
Heart failure is wrong because heart failure is a condition in which the heart cannot pump enough blood to meet the body’s needs.Heart failure can cause dyspnea and chest pain, but it is usually a chronic condition that worsens over time, not a sudden onset event.
Pneumonia is wrong because pneumonia is an infection that inflames the air sacs in the lungs, causing them to fill with fluid or pus.
Pneumonia can cause dyspnea and chest pain, but it also causes other symptoms such as fever, cough, and sputum production.Pneumonia usually develops gradually, not suddenly.
Pericarditis is wrong because pericarditis is an inflammation of the sac that surrounds the heart, called the pericardium.
Pericarditis can cause chest pain, but it is usually sharp and stabbing, and it changes with body position or breathing.
Pericarditis can also cause fever, fatigue, and palpitations.
Pericarditis does not cause dyspnea unless it leads to cardiac tamponade, which is a rare complication where fluid accumulates in the pericardial space
A nurse is preparing a client who has DVT for a venogram.
Which of the following actions should the nurse take?
Explanation
Assess for allergies to contrast material or iodine.This is because a venogram is a test that uses X-rays and a contrast dye to show blood flow in the veins.The contrast dye may contain iodine, which can cause an allergic reaction in some people.
Therefore, the nurse should check for any history of allergies to contrast material or iodine before the procedure.
Choice A is wrong because administering a sedative medication as prescribed is not necessary for a venogram.The procedure is minimally invasive and does not require sedation.
Choice C is wrong because applying a tourniquet to the affected limb is contraindicated for a venogram.A tourniquet would obstruct blood flow and interfere with the imaging of the veins.
Choice D is wrong because instructing the client to fast for 8 hours before the procedure is not required for a venogram.
The procedure does not affect the digestive system
Management of Postpartum Patients with DVT and PE
A nurse is caring for a postpartum client who has a deep vein thrombosis (DVT) in her right leg.
Which of the following actions should the nurse take?
Explanation
Elevate the affected leg above the level of the heart.This helps to reduce swelling and pain by improving venous blood flow and preventing stasis.
Choice A is wrong because applying a cold compress to the affected area can cause vasoconstriction and worsen blood flow.It can also increase the risk of skin damage and infection.
Choice B is wrong because massaging the affected leg gently can dislodge the thrombus and cause a pulmonary embolism, which is a life-threatening complication of DVT.
Choice D is wrong because removing the antiembolism stockings periodically can increase the risk of thrombus formation and extension.Antiembolism stockings provide graduated compression that improves venous return and prevents edema.
Normal ranges for D-dimer, a marker of fibrin degradation and thrombosis, are less than 0.5 mcg/mL or 500 ng/mL.Elevated levels indicate a high probability of DVT or PE.
A nurse is teaching a postpartum client who is at high risk for developing a pulmonary embolism (PE) due to a history of thromboembolism.
Which of the following instructions should the nurse include in the teaching?
Explanation
All of the above.
The nurse should include all of these instructions in the teaching to prevent pulmonary embolism (PE) in a postpartum client who is at high risk due to a history of thromboembolism.
Choice A is correct because crossing the legs can impair venous return and increase the risk of deep vein thrombosis (DVT), which can lead to PE.
Choice B is correct because drinking enough fluids can prevent dehydration and blood viscosity, which are risk factors for DVT and PE.
Choice C is correct because chest pain and shortness of breath are common signs of PE and should be reported immediately for prompt diagnosis and treatment.
Normal ranges for fluid intake are about 2 to 3 liters per day for healthy adults, but may vary depending on individual factors such as activity level, climate, and medical conditions.Normal ranges for leg crossing are not well defined, but it is generally advised to avoid prolonged periods of sitting or lying down with crossed legs.
A nurse is reviewing the laboratory results of a postpartum client who has idiopathic thrombocytopenic purpura (ITP).
Which of the following findings should the nurse expect?
Explanation
Decreased platelet count.This is because idiopathic thrombocytopenic purpura (ITP) is a disorder that causes the immune system to destroy the platelets, which are blood cells that help control bleeding.
Therefore, a person with ITP will have a low number of platelets in their blood.
Increased prothrombin time (PT) is wrong because PT measures how long it takes for the blood to clot.
A high PT means that the blood clots too slowly, which can be caused by liver disease, vitamin K deficiency, or blood-thinning medications.ITP does not affect the PT.
Decreased fibrinogen level is wrong because fibrinogen is a protein that helps form blood clots.
A low fibrinogen level can be caused by excessive bleeding, liver disease, or inherited disorders.ITP does not affect the fibrinogen level.
Increased partial thromboplastin time (PTT) is wrong because PTT measures how long it takes for the blood to clot.
A high PTT means that the blood clots too slowly, which can be caused by hemophilia, lupus, or blood-thinning medications.ITP does not affect the PTT.
Normal ranges for platelet count are 150,000 to 450,000 per microliter of blood.Normal ranges for PT are 11 to 13.5 seconds.Normal ranges for fibrinogen are 200 to 400 milligrams per deciliter of blood.Normal ranges for PTT are 25 to 35 seconds.
A nurse is administering heparin IV to a postpartum client who has a pulmonary embolism (PE).
Which of the following assessments should the nurse monitor to evaluate the effectiveness of the therapy?
Explanation
Activated partial thromboplastin time (aPTT) is a test that measures how long it takes for the blood to clot.
Heparin is a drug that prevents blood clots by inhibiting certain clotting factors.The effectiveness of heparin therapy is monitored by measuring the aPTT, which should be 1.5 to 2.5 times the normal value.
If the aPTT is too low, it means that heparin is not working well and the risk of clotting is high.
If the aPTT is too high, it means that heparin is working too well and the risk of bleeding is high.
Choice A is wrong because haemoglobin and hematocrit levels are not affected by heparin therapy.
They measure the amount and concentration of red blood cells in the blood, which are not involved in clotting.
Choice C is wrong because the international normalized ratio (INR) is a test that measures how long it takes for the blood to clot when taking another anticoagulant drug called warfarin.
Warfarin works by inhibiting the synthesis of vitamin K-dependent clotting factors.The effectiveness of warfarin therapy is monitored by measuring the INR, which should be 2 to 3 for most conditions.
Heparin does not affect the INR.
Choice D is wrong because platelet count is not affected by heparin therapy.
Platelets are small cell fragments that help form clots by sticking together and activating clotting factors.
Heparin does not affect the number of platelets in the blood, but it reduces their ability to aggregate and activate clotting factors.
A nurse is providing discharge teaching to a postpartum client who will be taking warfarin for 3 months following a deep vein thrombosis (DVT).
Which of the following statements by the client indicates an understanding of the teaching
Explanation
“I will have my blood tested once a week to check my medication level.” Warfarin is an anticoagulant that prevents blood clots from forming or growing larger.
It works by inhibiting the synthesis of vitamin K-dependent clotting factors in the liver.
The effect of warfarin varies from person to person and can be influenced by many factors, such as diet, other medications, and health conditions.
Therefore, it is important to monitor the blood level of warfarin regularly using a test called the international normalized ratio (INR), which measures how long it takes for the blood to clot.
The INR should be within a certain range, usually between 2 and 3, to prevent bleeding or clotting complications.
The client should have their INR checked at least once a week and adjust their warfarin dose accordingly.
Choice A is wrong because using a soft-bristled toothbrush is not enough to prevent bleeding gums.
Warfarin can increase the risk of bleeding from any injury or trauma, such as brushing the teeth, shaving, or cutting the skin.
The client should avoid activities that can cause bleeding and report any signs of bleeding, such as bruising, nosebleeds, blood in the urine or stool, or heavy menstrual bleeding.
Choice B is wrong because eating more green leafy vegetables can interfere with the effect of warfarin.
Green leafy vegetables are rich in vitamin K, which is needed for the production of clotting factors.
Eating more vitamin K can reduce the effectiveness of warfarin and increase the risk of clotting.
The client should maintain a consistent intake of vitamin K and avoid sudden changes in their diet.
Choice C is wrong because taking ibuprofen can increase the risk of bleeding.
Ibuprofen is a nonsteroidal anti-inflammatory drug (NSAID) that can inhibit platelet function and cause stomach ulcers.
Both of these effects can worsen the bleeding tendency of warfarin.
The client should avoid NSAIDs and use other pain relievers, such as acetaminophen, if needed.
Exams on Postpartum Disorders: DVT, Pulmonary Embolism
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
-
Understand the pathophysiology of deep vein thrombosis (DVT) and pulmonary embolism (PE) in the postpartum period.
-
Recognize the risk factors associated with the development of DVT and PE.
-
Identify the clinical manifestations of DVT and PE.
-
Explain the diagnostic methods used to confirm the presence of DVT and PE.
-
Describe the nursing interventions for preventing DVT and PE in postpartum patients.
-
Discuss the management strategies for postpartum patients with DVT and PE.
Introduction
-
Postpartum period is a time of increased risk for the development of DVT and PE.
-
Changes in the coagulation system, decreased mobility, and other factors contribute to the increased risk.
-
DVT occurs when a blood clot forms in a deep vein, typically in the lower extremities.
-
PE occurs when a blood clot from a DVT travels to the lungs, causing a blockage.
Clinical Manifestations of DVT
-
Unilateral leg pain, warmth, swelling, and erythema.
-
Positive Homans' sign (pain in the calf with dorsiflexion of the foot).
-
Positive Pratt's sign (pain in the calf with compression of the calf muscle).
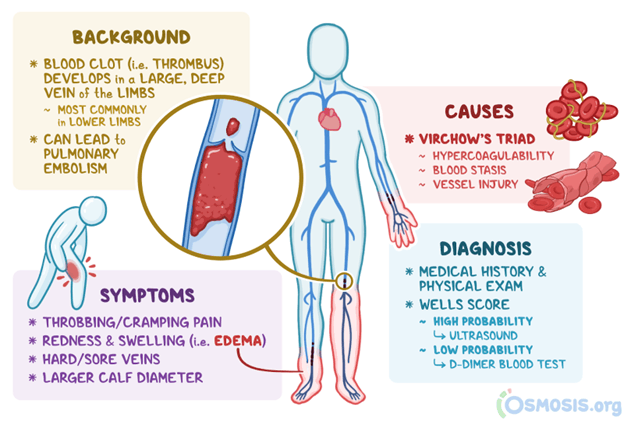
Clinical Manifestations of PE
-
Sudden onset of dyspnea, tachypnea, and chest pain.
-
Hemoptysis, cough, and pleuritic pain may be present.
-
Tachycardia and hypoxemia may be observed.
Diagnostic Methods
Compression ultrasound is the primary diagnostic tool for DVT.
D-dimer blood test can help rule out DVT or PE if the result is negative.
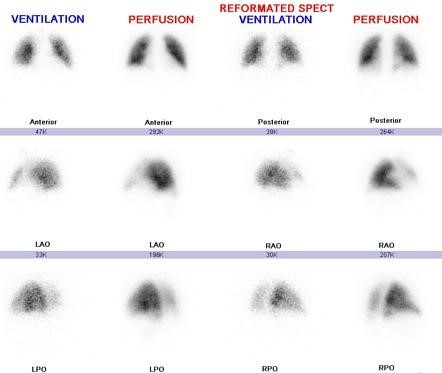
CT pulmonary angiography is the gold standard for diagnosing PE.
Ventilation-perfusion (V/Q) scan can be used if CT is contraindicated
Nursing Interventions for DVT and PE Prevention
Encourage early and frequent ambulation.
Teach postpartum patients about the importance of leg exercises.
Apply anti-embolism stockings or intermittent pneumatic compression devices.

Administer prophylactic anticoagulant medication as prescribed.
Assess for risk factors and provide education on prevention strategies.
Management of Postpartum Patients with DVT and PE
- Administer anticoagulant therapy based on the severity of the condition.
- Monitor for bleeding complications and adjust the dosage accordingly.
- Provide emotional support and encourage open communication.
- Promote rest and adequate hydration.
- Collaborate with the healthcare team to ensure appropriate follow-up care.
Conclusion
In the postpartum period, the risk of DVT and PE is heightened.
Nurses play a crucial role in the prevention, early detection, and management of these potentially life-threatening conditions. By understanding the pathophysiology, recognizing risk factors, and implementing appropriate interventions, nurses can effectively contribute to the well-being and safety of postpartum patients.
Summary
- DVT: Unilateral leg pain, swelling, positive Homans' and Pratt's signs.
- PE: Sudden dyspnea, chest pain, tachypnea, hemoptysis.
- Diagnostic methods: Compression ultrasound, D-dimer blood test, CT pulmonary angiography.
-
Nursing interventions: Early ambulation, leg exercises, anti-embolism stockings, anticoagulant medication.
-
Management: Anticoagulant therapy, monitoring for bleeding complications, emotional support, rest and hydration.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Postpartum Disorders: DVT, Pulmonary Embolism
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


