Please set your exam date
Documenting and Reporting
Study Questions
Documentation and Reporting
A nurse is reviewing the documentation and reporting policies of a healthcare facility.
The nurse understands that documentation serves as a permanent record of patient information, data, and care.
Which of the following is another purpose of documentation?
Explanation
To communicate with other healthcare providers about the patient’s needs and progress.
Documentation in nursing serves several purposes, including providing continuity of care for patients, determining clinical reimbursement, avoiding malpractice, and facilitating communication between rotating providers.It is also used to determine the severity of illness, the intensity of services, and the quality of care provided upon which payment or reimbursement of health care services is based.
Choice A is wrong because documentation is not meant to provide evidence of malpractice in case of a lawsuit, but rather to avoid it by following the guidelines and standards of nursing practice.
Choice C is wrong because documentation is not the only purpose of evaluating the quality and effectiveness of the care provided.There are other methods and tools for quality improvement, such as audits, surveys, feedback, etc.
Choice D is wrong because documentation is not the only purpose of justifying the reimbursement for the services rendered.There are other factors and criteria that determine the reimbursement rates, such as diagnosis-related groups, case mix index, etc.
Normal ranges for documentation vary depending on the type, format, and frequency of documentation.
However, some general principles for documentation are:.
• It should be clear, accurate, and accessible.
• It should reflect the nursing process (assessment, planning, implementation, and evaluation).
• It should use standardized terminologies and abbreviations.
• It should be completed in real time or as soon as possible after care delivery.
• It should include all relevant patient information and data.
• It should comply with the legal and ethical requirements of nursing practice.
A nurse is preparing to report the status of a patient to another nurse during a shift change.
The nurse should include which of the following information in the report?
(Select all that apply.).
Explanation
The nurse should include the patient’s name, age, and diagnosis, the patient’s current vital signs and pain level, the patient’s preferences and goals for care, and the patient’s plan of care and any pending interventions in the report.
These are the most relevant and important information that the oncoming nurse needs to know to provide safe and effective care for the patient.
Choice D is wrong because the patient’s family history and social support are not essential to include in the report.
They may be part of the patient’s medical record, but they are not likely to change during the shift or affect the patient’s immediate needs.
A nursing shift report is a document that a nurse writes about their patients at the end of their shift to give to the nurse tending to their patients on the next shift.
It helps the oncoming nurse understand the patient’s medical conditions, needs, and progress.It also helps ensure continuity of care and prevent errors or omissions.
Normal ranges for vital signs vary depending on age, gender, and health status, but generally they are:.
• Temperature: 36.5°C to 37.2°C (97.7°F to 99°F).
• Pulse: 60 to 100 beats per minute.
• Respiration: 12 to 20 breaths per minute.
• Blood pressure: less than 120/80 mmHg.
• Pain level: 0 to 10 on a numerical scale or using a visual analog scale.
A nurse is documenting the care provided to a patient who has a wound infection.
The nurse writes: “The wound was cleansed with normal saline and covered with a sterile dressing.
No signs of redness, swelling, or drainage were noted.” Which of the following statements reflects the nurse’s use of objective data?
Explanation
“The wound was cleansed with normal saline and covered with a sterile dressing.” This statement reflects the nurse’s use of objective data because it describes what the nurse did and observed using the five senses.Objective data is factual information that professionals gather through observation or measurement that is true regardless of the feelings or opinions of the person presenting or receiving the information.
Choice B is wrong because it also contains objective data.
The nurse observed the wound and did not see any signs of inflammation or infection.
Choice C is wrong because it contains subjective data.The patient stated how they felt about the wound, which is their perception, feeling, or concern.
Choice D is wrong because it also contains subjective data.The nurse inferred how the patient appeared, which is their opinion or interpretation.
Normal ranges for wound healing depend on various factors, such as the type, size, location, and severity of the wound, as well as the patient’s age, health status, nutrition, and infection risk.
Generally, wounds go through four phases of healing: hemostasis, inflammation, proliferation, and maturation.
Hemostasis occurs immediately after injury and involves blood clotting and vasoconstriction.
Inflammation lasts for 3 to 5 days and involves swelling, redness, pain, and immune response.
Proliferation lasts for 2 to 24 days and involves granulation tissue formation, wound contraction, and epithelialization.Maturation lasts for 21 days to 2 years and involves collagen remodeling and scar formation.
A nurse is caring for a patient who has a history of depression and is taking an antidepressant medication.
The nurse asks the patient how he is feeling today.
The patient responds: “I don’t know, I guess I’m okay.” Which of the following statements by the nurse is an appropriate response?
Explanation
Tell me more about how you are feeling.
This statement by the nurse is an appropriate response because it shows empathy, interest, and respect for the patient’s feelings.
It also encourages the patient to express his emotions and thoughts, which can help the nurse assess the severity of his depression and the effectiveness of his medication.Asking open-ended questions is a therapeutic communication technique that can facilitate rapport and trust between the nurse and the patient.
Choice A is wrong because it implies doubt and criticism of the patient’s response.
It may make the patient feel defensive or invalidated.
Choice B is wrong because it assumes that the patient is feeling better without verifying it.
It may also contradict the patient’s reality and discourage him from sharing his true feelings.
Choice D is wrong because it places unrealistic expectations on the patient and minimizes his struggle.
It may also imply that the patient is not trying hard enough or that his medication is not working.
Antidepressant medications are used to alter the concentration of neurotransmitters in the brain that are responsible for mood regulation, such as serotonin, norepinephrine, and dopamine.They can help relieve symptoms of depression, such as low mood, anhedonia, guilt, worthlessness, low energy, poor concentration, appetite changes, sleep disturbances, and suicidal thoughts.
However, antidepressant medications are not a cure for depression and they do not work immediately.They usually take several weeks to reach their full effect and they may cause side effects such as nausea, headache, weight gain, sexual dysfunction, and increased risk of bleeding.
Nursing care for patients taking antidepressant medications involves assessing and monitoring their depressive symptoms, suicidal thoughts, mental status, vital signs, weight, serum electrolytes, kidney and liver function, and pregnancy status.Nurses should also facilitate regular psychotherapy sessions, provide education on depression management, encourage adherence to medication regimen, teach coping skills and stress management techniques, promote healthy lifestyle habits such as exercise, nutrition, and sleep hygiene, and provide emotional support and encouragement.
A nurse is using a computer-based system to document the care provided to a patient who has diabetes mellitus.
The nurse enters the patient’s blood glucose level, insulin dose, dietary intake, and urine output.
The system automatically generates a graph that shows the trends and patterns of these data over time.
This type of documentation system is known as:.
Explanation
Flow sheet charting.
This type of documentation system uses graphs, tables, or checklists to record data that can be easily visualized and compared over time.Flow sheet charting is especially useful for documenting vital signs, blood glucose levels, intake and output, and other routine or repetitive measurements.
Choice A is wrong because narrative charting is a type of documentation system that uses descriptive sentences or paragraphs to record patient information.Narrative charting is often time-consuming and may include irrelevant or redundant details.
Choice B is wrong because problem-oriented charting is a type of documentation system that organizes patient information around specific problems or diagnoses.Problem-oriented charting typically uses the SOAP format (subjective, objective, assessment, plan) or its variations (SOAPIE, SOAPIER) to document the patient’s status and progress.
Choice C is wrong because charting by exception is a type of documentation system that only records abnormal or significant findings or deviations from pre-established standards or norms.Charting by exception assumes that everything is normal unless otherwise documented.
Normal ranges for blood glucose levels are 70 to 130 mg/dL before meals and less than 180 mg/dL two hours after meals.Normal ranges for urine output are 0.5 to 1 mL/kg/hour for adults and 1 to 2 mL/kg/hour for children.
Ethical and Legal Considerations in Documenting and Reporting
A nurse is reviewing the legal aspects of documentation and reporting.
Which of the following statements is true regarding the client’s record?
Explanation
The client’s record is a private and confidential document that is protected by law.This means that only authorized personnel who have a legitimate need to access the record can do so, and that the record cannot be disclosed to anyone without the client’s consent or a court order.The client’s record is also a legal document that serves as evidence of the care provided and the client’s condition and response.Therefore, it must be accurate, complete, objective, timely, and legible.
Choice A is wrong because the client’s record belongs to the health care facility or provider, not to the client.The client has the right to access and request copies of their record, but they cannot take it home or remove it from the facility.
Choice B is wrong because the client’s record cannot be accessed by anyone who works in the health care facility.
Only those who have a direct involvement in the client’s care or a valid reason to review the record can access it, such as nurses, physicians, therapists, quality improvement staff, etc.Accessing the record for personal or unauthorized reasons is a breach of confidentiality and can result in legal and disciplinary actions.
Choice D is wrong because the client’s record cannot be altered or destroyed by the nurse if it contains errors.
The nurse must follow the proper procedure for correcting errors in documentation, such as drawing a single line through the error, writing “error” above it, initialing and dating it, and writing the correct information.
The nurse must never erase, obliterate, or use correction fluid on the record.Destroying or tampering with the record can be considered fraud or negligence and can jeopardize the nurse’s license and credibility.
Normal ranges for documentation vary depending on the type of information recorded, such as vital signs, laboratory values, assessment findings, etc.
The nurse should follow the standards and policies of their facility and professional organizations when documenting.
A nurse is using a computerized system to document and report client information.
Which of the following actions should the nurse take to ensure confidentiality of computerized records?
(Select all that apply.).
Explanation
The nurse should use a personal password to log on and off the system and shred any unnecessary computer-generated worksheets.
These actions will help ensure confidentiality of computerized records by preventing unauthorized access and misuse of patient information.
Choice B is wrong because the nurse should not share the password with anyone, even a trusted colleague.This would violate the professional duty of maintaining a patient’s confidence and data security.
Choice C is wrong because the nurse should not leave the computer unattended while logged on.
This would create an opportunity for someone else to access or tamper with the records.
Choice E is wrong because installing a firewall on the personal computer is not enough to prevent unauthorized access.The nurse should also use encryption, antivirus software, and other security measures.
A nurse is caring for a client who has a diagnosis of AIDS.
The nurse needs to document and report sensitive information about the client’s condition.
What should the nurse say to the client before doing so?
Explanation
“I will only share your information with those who are directly involved in your care.”
This is because the nurse has a legal and ethical obligation to protect the client’s confidentiality and privacy, especially when dealing with sensitive information such as HIV/AIDS diagnosis.
Choice B is wrong because the nurse does not need to ask for the client’s permission every time they need to disclose their information to someone who is part of the health care team.This would be impractical and unnecessary, as the client has already consented to share their information with those who need to know for their care.
Choice C is wrong because the nurse cannot keep the client’s information anonymous when they report it to others who are involved in their care.The client’s identity is important for accurate and safe care delivery, and anonymizing their information could compromise their quality of care or lead to errors.
Choice D is wrong because the nurse cannot withhold the client’s diagnosis from anyone who has a legitimate need to know, such as other health care providers, public health officials, or partner notification services.The nurse has a duty to warn those who are at risk of exposure to HIV from the client, and to comply with the legal requirements for reporting HIV cases to the state health department and CDC.
Normal ranges for HIV tests are negative or non-reactive for antibodies or antigens.A positive or reactive test indicates the presence of HIV infection and requires confirmation by a second test.
A nurse is using a computerized system to document and report client information.
The nurse realizes that an entry error has been made in the system.
What should the nurse do to correct the error?
Explanation
Follow the facility’s policy and procedure for correcting an entry error.This is because different computerized systems may have different methods for correcting errors, and the nurse should follow the guidelines of the specific system and facility to ensure accuracy, accountability and legal compliance.
Choice A is wrong because deleting the erroneous entry may not be possible or appropriate in some systems, and it may compromise the integrity and auditability of the documentation.
Choice B is wrong because drawing a line through the erroneous entry and initialing it is a method for correcting errors in paper documentation, not computerized documentation.
Choice D is wrong because ignoring the error and hoping that no one notices it is unprofessional, unethical and potentially dangerous for the patient’s care and safety.
The nurse should always document accurately, promptly and honestly, and report any errors or discrepancies in the documentation to the appropriate authority.
A nurse is reviewing the ethical and legal considerations of documentation and reporting.
The nurse understands that the client has the right to access their own record and to have a copy of it.
What is the rationale for this right?
Explanation
The client’s record is a reflection of the client’s health status and care.
The rationale for this right is that the client has the right to know and understand their own health condition and the care they receive from the health care providers.The client’s record is a source of information that can help the client make informed decisions about their health and well-being.
Choice A is wrong because the client’s record is not primarily a source of evidence for legal actions, although it may be used as such in some cases.The main purpose of the record is to document the care provided to the client and the client’s response to the care.
Choice B is wrong because the client’s record is not primarily a tool for quality improvement and research, although it may be used as such in some cases.The main purpose of the record is to document the care provided to the client and the client’s response to the care.
Choice C is wrong because the client’s record is not primarily a means of communication among health care providers, although it may be used as such in some cases.The main purpose of the record is to document the care provided to the client and the client’s response to the care.
Normal ranges for documentation vary depending on the type of data and the setting.
For example, vital signs, laboratory values, pain scales, and functional assessments may have different normal ranges in different contexts.Nurses should follow the policies and procedures of their organization and use standardized terminologies when documenting data.
Purposes/Reasons for Client Records
A nurse is reviewing the client records of a health care facility.
Which of the following purposes of client records is the nurse performing?
Explanation
The nurse is performing one of the main purposes of client records, which is to communicate with other health care providers about the client’s condition, needs, and interventions.Communication is essential for ensuring continuity and quality of care, as well as for preventing errors and misunderstandings.
Choice B is wrong because planning client care is not the purpose of reviewing client records, but rather the purpose of creating and updating them.Planning client care involves setting goals, choosing interventions, and evaluating outcomes based on the information in the client records.
Choice C is wrong because auditing health agencies is not the purpose of reviewing client records by a nurse, but rather the purpose of examining them by an external or internal agency.Auditing health agencies involves assessing the quality, efficiency, and effectiveness of health care services based on the client records.
Choice D is wrong because research is not the purpose of reviewing client records by a nurse, but rather the purpose of using them by researchers.Research involves collecting, analyzing, and interpreting data from client records to generate new knowledge, improve practice, or inform policy.
Normal ranges are not applicable in this question as it does not involve any physiological or laboratory measurements.
A nurse is documenting the care provided to a client in the electronic health record (EHR).
Which of the following actions should the nurse take?
(Select all that apply.).
Explanation
A. Use standardized terminology and abbreviations.This is correct because standardized terminology and abbreviations can improve communication, consistency and data collection among health care providers.
B. Include the date and time of each entry.This is correct because the date and time of each entry can provide accurate and timely information about the patient’s condition and care.
C. Delete any incorrect information with a single line.
This is wrong because deleting any incorrect information with a single line is not appropriate for electronic health records.Instead, the nurse should use the correction function of the EHR system to make any changes.
D. Sign each entry with the nurse’s name and credentials.This is correct because signing each entry with the nurse’s name and credentials can ensure accountability and responsibility for the documentation.
E. Share the password with other authorized staff.
E. Sharing passwords is unsafe and violates facility policy; each staff member must use their own login credentials.
A nurse is preparing a report for a client who is being transferred to another unit.
Which of the following statements should the nurse include in the report?
Explanation
“The client is alert and oriented to person, place, and time.”
This statement provides the most relevant and current information about the client’s mental status and level of consciousness, which are important for the receiving nurse to know.
The other statements are either too vague (C), too general (B), or not a priority (D) for a transfer report.
Choice B is wrong because it does not specify the current status of the client’s hypertension and diabetes, such as blood pressure, blood glucose, medications, or complications.
This information is more appropriate for a written summary or a discharge report.
Choice C is wrong because it does not provide the actual values of the client’s vital signs, which can vary depending on the client’s condition and baseline.
The receiving nurse should know the exact numbers to monitor for any changes or abnormalities.
Choice D is wrong because it does not indicate the reason why the client needs assistance with bathing and dressing, such as mobility issues, pain, or weakness.
This information is also less urgent than the client’s mental status and vital signs.
Normal ranges for vital signs are:.
• Temperature: 36.5°C to 37.2°C (97.7°F to 99°F).
• Pulse: 60 to 100 beats per minute.
• Respirations: 12 to 20 breaths per minute.
• Blood pressure: less than 120/80 mm Hg.
Sources:.
A client asks a nurse why it is necessary to document every aspect of care in the record.
Which of the following responses should the nurse give?
Explanation
“It helps us to communicate with other members of the health care team.”.
Nursing documentation is essential for clinical communication.Documentation provides an accurate reflection of nursing assessments, changes in clinical state, care provided and pertinent patient information to support the multidisciplinary team to deliver individualised care.
Choice B is wrong because reimbursement is not the primary purpose of nursing documentation, although it may be a secondary benefit.
Choice C is wrong because legal liability is not the main reason for documenting care, although it may provide evidence in case of litigation.
Choice D is wrong because quality improvement is not the direct result of nursing documentation, although it may be facilitated by it.
Nursing documentation should follow six essential principles: documentation characteristics, education and training, policies and procedures, protection systems, documentation entries and standardized terminologies.
These principles help nurses to create clear, accurate and accessible records that can improve patient outcomes and safety.
: ANA’s Principles for Nursing Documentation - ANA Enterprise: Clinical Guidelines (Nursing) : Nursing Documentation Principles.
A nurse is conducting a research study on the effectiveness of a new wound dressing.
Which of the following sources of data should the nurse use?
Explanation
Client records.
This is because client records contain objective and measurable data on the wound healing process, such as size, depth, drainage, infection, and pain.
Client records are also reliable and valid sources of data that can be easily accessed and compared.
Choice B is wrong because client interviews are subjective and may not reflect the actual effectiveness of the wound dressing.
Client interviews may also be influenced by factors such as mood, recall, and rapport.
Choice C is wrong because client surveys are also subjective and may not capture the relevant aspects of wound healing.
Client surveys may also have low response rates or biased responses.
Choice D is wrong because client observations are not enough to evaluate the effectiveness of a wound dressing.
Client observations may be affected by personal preferences, expectations, or beliefs.
Normal ranges for wound healing depend on various factors such as the type, location, and severity of the wound, the patient’s age, health status, and nutrition, and the type of dressing used.
However, some general guidelines are:.
• Acute wounds (such as surgical incisions) should heal within 2 to 4 weeks.
• Chronic wounds (such as pressure ulcers) may take longer than 6 weeks to heal.
• Wounds should show signs of improvement such as reduced size, decreased drainage, decreased inflammation, and increased granulation tissue within 2 weeks of treatment.
Sources:.
• Wound Healing - an overview | ScienceDirect Topics.
Documentation System
A nurse is reviewing the documentation system of a client’s chart.
Which of the following is an advantage of using a source-oriented record?
Explanation
It keeps data from each person or department in a separate section.A source-oriented record is a type of documentation system that organizes the data according to the source of information, such as the physician, nurse, laboratory, or physical therapy.This format has the advantage of making it easy to locate and trace the information from each person or department who provided care to the client.
Choice A is wrong because it does not encourage collaboration among health care providers.In fact, a source-oriented record may hinder communication and coordination of care because the data are fragmented and scattered throughout the chart.
Choice B is wrong because it does not organize the data according to the client’s problems.A problem-oriented medical record (POMR) is a different type of documentation system that arranges the data based on the problems identified by the health care team.The POMR has four components: database, problem list, plan of care, and progress notes.
Choice C is wrong because it does not track the status of each problem using a problem list.This is also a feature of the POMR, not the source-oriented record.A problem list is a numbered list of the client’s current and resolved problems that serves as an index to the progress notes.
A nurse is preparing to document the care plan for a client who has a problem-oriented medical record (POMR).
Which of the following actions should the nurse take?
(Select all that apply.).
Explanation
The nurse shouldnumber the care plan to correspond to the problem listandupdate the problem list as needed.These actions are consistent with the principles of the problem-oriented medical record (POMR), which is a method of organizing patient information by the health problems that require attention.The POMR includes a patient database, a problem list, a plan of care, and progress notes.
Choice A is wrong because the nurse should not generate the care plan from the database, but rather from the problem list.The problem list is the centerpiece of the POMR and reflects the patient’s current health status and needs.
Choice C is wrong because the nurse should not repeat assessments and interventions that apply to more than one problem, but rather use cross-referencing to avoid duplication and confusion.
Choice E is wrong because the nurse should not use a standardized format for chart entries, but rather use a SOAP format (subjective, objective, assessment, plan) or a modified version of it (such as SOAPIE or SOAPIER) to document each problem and its progress.
The normal ranges for some common laboratory tests are:.
• CBC (complete blood count):.
➤ Hemoglobin: 13.5-17.5 g/dL (male), 12-16 g/dL (female).
➤ Hematocrit: 38.8-50% (male), 34.9-44.5% (female).
➤ White blood cell count: 4.5-11 x 10^9/L.
➤ Platelet count: 150-450 x 10^9/L.
• SMAC (sequential multiple analysis computer):.
➤ Sodium: 135-145 mEq/L.
➤ Potassium: 3.5-5 mEq/L.
➤ Chloride: 98-106 mEq/L.
➤ Bicarbonate: 22-29 mEq/L.
➤ Blood urea nitrogen: 7-20 mg/dL.
➤ Creatinine: 0.6-1.2 mg/dL (male), 0.5-1.1 mg/dL (female).
➤ Glucose: 70-110 mg/dL.
➤ Calcium: 8.5-10.2 mg/dL.
• EKG (electrocardiogram):.
➤ Heart rate: 60-100 beats per minute.
A nurse is using the SOAP format to write a progress note for a client who has impaired physical mobility.
Which of the following statements should the nurse include as the subjective data?
Explanation
“The client reports feeling less pain in his left leg.”
This is the subjective data because it is based on the client’s own perception and feelings.Subjective data is what the client tells the nurse or what the nurse observes from the client’s behavior.
Choice A is wrong because it is objective data, which is measurable and observable by the nurse or other healthcare providers.Objective data is what the nurse sees, hears, feels, or smells.
Choice C is wrong because it is also objective data, as it can be measured by the nurse using a goniometer or other tools.
Choice D is wrong because it is also objective data, as it can be observed by the nurse or documented in the care plan.
Normal ranges for vital signs are as follows:.
• Blood pressure: 90/60 mmHg to 120/80 mmHg.
• Pulse rate: 60 to 100 beats per minute.
• Respiratory rate: 12 to 20 breaths per minute.
• SpO2: 95% to 100%.
• Temperature: 36.5°C to 37.5°C.
A nurse is using the PIE format to write a progress note for a client who has constipation.
Which of the following statements should the nurse include as the intervention?
Explanation
“Administered bisacodyl suppository as prescribed.”.
The PIE format is a method of documentation that states theproblemor diagnosis (P), theinterventionor action the nurse takes (I), and theevaluationof the results (E).It eliminates the need for a traditional care plan by incorporating it into the progress notes.
The intervention is the action that the nurse takes to address the problem.
In this case, the problem is constipation, and the intervention is administering a bisacodyl suppository as prescribed by the physician.
This is a specific and measurable action that can be evaluated later.
Choice A is wrong because it is not an intervention, but a health promotion activity.
Encouraging the client to increase fluid and fiber intake is a good practice, but it is not directly related to the problem of constipation.
Choice B is wrong because it is not an intervention, but an assessment.
Assessing the client’s bowel sounds and abdominal distension is part of the data collection process, but it does not solve the problem of constipation.
Choice D is wrong because it is not an intervention, but an evaluation.
Evaluating the client’s response to the suppository is the last step of the PIE format, where the nurse determines if the intervention was effective or not.
It does not describe what the nurse did to address the problem of constipation.
The normal range for bowel movements varies from person to person, but generally, having less than three bowel movements per week is considered constipation.Constipation can be caused by various factors, such as medication side effects, dehydration, low-fiber diet, lack of physical activity, or underlying medical conditions.
A nurse is using the DAR format to write a progress note for a client who has a history of hypertension.
Which of the following statements should the nurse include as the action?
Explanation
“Instructed the client on low-sodium diet and exercise.”
This is the action that the nurse took to address the client’s problem of hypertension.
The action should describe the nursing intervention that was performed to help the client achieve the expected outcome.
Choice A is wrong because it is not an action, but a data.
Data is the information that the nurse collected about the client’s condition, such as vital signs, symptoms, or test results.
Data should be factual and objective.
Choice C is wrong because it is not an action, but a response.
Response is the outcome or result of the nursing intervention, such as the client’s reaction, behavior, or change in condition.
Response should be measurable and evaluative.
Choice D is wrong because it is not an action, but a focus.
Focus is the reason or purpose for writing the note, such as a nursing diagnosis, a change in condition, or a patient education need.
Focus should be concise and specific.
DAR format is a method of nursing documentation that stands for Data, Action, and Response.It is a form of focus charting that records significant events or changes in the client’s condition that require nursing care.DAR notes are organized, concise, and informative, and they help to communicate the nursing process and plan of care among health care providers.
Format of Progress Notes (DAR)
A nurse is documenting the progress notes of a client who has chronic pain.
The nurse uses the DAR format to record the data, action, and response.
Which of the following is an example of a data entry in the DAR format?
Explanation
Observed facial grimace and guarding of the abdomen.
This is an example of a data entry in the DAR format because it describes the objective and subjective information that the nurse collected from the client.Data entries can include vital signs, physical assessment findings, laboratory results, and client statements.
Choice A is wrong because it is an example of an action entry in the DAR format.Action entries describe the nursing interventions that the nurse performed to address the client’s problem or need.
For example, administering medication, providing education, or applying a dressing.
Choice B is wrong because it is an example of a response entry in the DAR format.Response entries describe the client’s reaction or outcome to the nursing interventions.
For example, reporting pain relief, expressing satisfaction, or showing improvement.
Choice D is wrong because it is also an example of an action entry in the DAR format.
It describes another nursing intervention that the nurse performed to help the client cope with pain.
The DAR format is a type of focus charting that helps nurses document problems identified in the client care plan.
It stands for data, action, and response.Some nurses may use the F-DAR format, which adds a focus component to provide a clearer context and prioritization of the client’s needs.The focus can be a nursing diagnosis, a change in condition, a symptom, or an event.
A nurse is using the SOAP format to document the progress notes of a client who has hypertension.
The nurse needs to select all that apply when writing the plan of care for this client.
Which of the following are appropriate components of the plan in the SOAP format?
Explanation
These are appropriate components of the plan in the SOAP format.SOAP stands forSubjective, Objective, Assessment, Planand it is a form of written documentation many healthcare professions use to record a patient or client interaction.
• Ais correct because monitoring blood pressure and pulse every 4 hours is an objective and measurable intervention that can help evaluate the patient’s condition and response to treatment.
• Bis correct because educating the client about dietary sodium restriction is an intervention that can help prevent or reduce hypertension and its complications.
• Dis correct because evaluating the effectiveness of antihypertensive medication is an intervention that can help assess the patient’s progress and adjust the treatment plan accordingly.
• Cis wrong because assessing for signs of orthostatic hypotension is not an intervention, but an observation that belongs to the objective section of the SOAP note.
• Eis wrong because identifying the risk factors for developing hypertension is not an intervention, but an assessment that belongs to the assessment section of the SOAP note.
Normal ranges for blood pressure are<120/80 mmHgfor normal,120-129/<80 mmHgfor elevated,130-139/80-89 mmHgfor stage 1 hypertension, and≥140/≥90 mmHgfor stage 2 hypertension.Normal ranges for pulse rate are60-100 beats per minutefor adults.
A nurse is using the SOAPIER format to document the progress notes of a client who has diabetes mellitus.
The nurse needs to write an intervention entry in the SOAPIER format.
Which of the following is an example of an intervention entry in the SOAPIER format?
Explanation
Instructed the client on how to use a glucometer at home.
This is an example of an intervention entry in the SOAPIER format, which stands for subjective, objective, assessment, plan, intervention, and evaluation.An intervention entry describes any actions that were taken to support the patient based on the assessment and plan.
In this case, the nurse provided patient education on how to monitor blood glucose levels at home using a glucometer.
Choice A is wrong because it is an example of a subjective entry, which includes anything related to what the patient has told the nurse.This should be recorded exactly as the patient reports and in quotation marks.
Choice B is wrong because it is an example of an objective entry, which consists of any measurable observations that the nurse makes during the patient assessment.This includes vital signs, laboratory results, physical findings, and other data that can be verified.
Choice D is wrong because it is an example of an assessment entry, which is the nurse’s interpretation of the subjective and objective information and conclusions regarding the patient’s condition.This may include nursing diagnoses, problem statements, or clinical impressions.
Choice E is wrong because it is an example of an evaluation entry, which describes the result of any interventions and whether they achieved the desired outcomes.This may include patient feedback, changes in condition, or need for further action.
Normal ranges for blood glucose levels vary depending on the type of test and the time of day.Generally, a normal fasting blood glucose level is between 70 and 100 mg/dL, while a normal postprandial (after meal) blood glucose level is less than 140 mg/dL.A blood glucose level of 250 mg/dL before lunch indicates hyperglycemia (high blood sugar), which is a common complication of diabetes mellitus.
A nurse is using the focus charting method to document the progress notes of a client who has anxiety.
The nurse needs to write an evaluation entry in the focus charting method.
Which of the following is an example of an evaluation entry in the focus charting method?
Explanation
“I feel more calm and relaxed after practicing the breathing exercises.”
This is an example of an evaluation entry in the focus charting method because it describes the client’s response to the nursing intervention of teaching relaxation techniques.Evaluation entries reflect theevaluation phaseof the nursing process and show whether the client’s goals and outcomes have been met or not.
Choice A is wrong because it is an example of an action entry, not an evaluation entry.Action entries reflect theplanning and implementation phaseof the nursing process and include immediate and future nursing actions.
Choice B is wrong because it is an example of a data entry, not an evaluation entry.Data entries reflect theassessment phaseof the nursing process and include subjective and objective information about the client’s health status.
Choice C is wrong because it is an example of a focus, not an evaluation entry.A focus is a key word or phrase that identifies the client’s concern, problem, or strength.It can be derived from a nursing diagnosis, a sign or symptom, an acute change in condition, a significant event, or a standard of care.
Choice E is wrong because it is an example of an action entry, not an evaluation entry.Action entries reflect theplanning and implementation phaseof the nursing process and include immediate and future nursing actions.
Focus charting is a method for organizing health information in the client’s record using nursing terminology to describe the client’s health status and nursing actions.
It uses three columns: date and hour, focus, and progress notes.The progress notes are organized into data, action, and response (DAR).
Normal ranges for vital signs are:.
• Temperature: 36.5°C to 37.5°C (97.7°F to 99.5°F).
• Pulse: 60 to 100 beats per minute.
• Respirations: 12 to 20 breaths per minute.
• Blood pressure: 120/80 mmHg (systolic/diastolic).
A nurse is using the PIE documentation system to document the progress notes of a client who has pneumonia.
The nurse needs to write an evaluation entry in the PIE documentation system.
Which of the following is an example of an evaluation entry in the PIE documentation system?
Explanation
The client’s oxygen saturation level has improved from 88% to 95% after receiving oxygen therapy for 24 hours.
This is an example of an evaluation entry in the PIE documentation system because it describes the outcome of the intervention (oxygen therapy) for the problem (low oxygen saturation level) using objective data (percentage).
Other choices are wrong because:.
• Choice A: The client has been coughing less frequently and reports feeling less short of breath.
This is an example of an intervention entry because it describes the actions taken by the nurse to address the problem (coughing and shortness of breath).
• Choice B: The client has a productive cough with yellowish sputum and crackles in the lower lobes of both lungs.
This is an example of a problem entry because it identifies the signs and symptoms of the health condition (pneumonia).
• Choice D: The client will maintain a normal oxygen saturation level of at least 92% with supplemental oxygen as needed.
This is an example of a plan entry because it states the expected outcome or goal for the problem (low oxygen saturation level).
The PIE documentation system is a process-oriented system that uses the acronym PIE to document theProblem,Intervention, andEvaluation of the patient’s progress.It integrates care planning with progress notes and does not separate the patient from the environmental influences.The normal oxygen saturation level for healthy adults is between 95% and 100%.
Charting By Exception (CBE)
A nurse is using the CBE system to document the care of a client with pneumonia.
Which of the following actions should the nurse take?
Explanation
Record the client’s vital signs on a flow sheet every 4 hours.This is because charting by exception (CBE) documentation is a system that only requires the nurse to document deviations from predefined norms or standards of care.
Therefore, the nurse only needs to record routine data such as vital signs on a flow sheet and does not need to write a narrative note for every nursing intervention performed (B), document the client’s response to antibiotics in the progress notes ©, or refer to the agency’s standards of care for routine procedures (D).These actions are unnecessary and time-consuming in CBE documentation, as they would duplicate information that is already available in the electronic health record (EHR) or the agency’s policies.CBE documentation is designed to decrease the amount of time required to document care and to improve the quality and accuracy of patient records.
A nurse is reviewing the EHR of a client who is admitted for chest pain.
Which of the following information should the nurse expect to find in the EHR?
(Select all that apply.).
Explanation
The client’s medical history and current medications, and the results of the client’s electrocardiogram and cardiac enzymes are information that the nurse should expect to find in the EHR of a client who is admitted for chest pain.These are essential components of an EHR that provide comprehensive health information about the patient, such as their diagnosis, treatment, and progress.
Choice C is wrong because the discharge plan and teaching for the client and family are not part of the EHR until the client is ready to be discharged.They are not relevant for a client who is newly admitted for chest pain.
Choice D is wrong because the variances from the critical pathway for the client’s diagnosis are not part of the EHR, but rather a quality improvement tool that monitors the deviations from the expected outcomes and interventions for a specific diagnosis.
Choice E is wrong because the names and contact information of the case management team are not part of the EHR, but rather a communication tool that facilitates coordination of care among different providers and organizations.
A nurse is caring for a client who is on a critical pathway for a total hip arthroplasty.
The nurse notices that the client has developed a wound infection on postoperative day 3.
What should the nurse do next?
Explanation
Notify the surgeon and document the wound infection as a variance.A variance is a deviation from the expected course of care or outcome in a critical pathway.A wound infection is an example of a variance that can affect the patient’s recovery and length of stay after a total hip arthroplasty (THA).
The nurse should notify the surgeon to initiate appropriate treatment and document the infection as a variance in the patient’s record.
Choice B is wrong because changing the dressing alone is not sufficient to treat a wound infection.
The nurse should also notify the surgeon and document the infection as a variance.
Choice C is wrong because a wound infection is not an expected outcome of THA.It is a complication that can increase the risk of implant failure, sepsis, and revision surgery.
Choice D is wrong because discontinuing the critical pathway is not necessary or appropriate for a wound infection.The critical pathway is a guideline for optimal care that can be modified according to the patient’s condition and needs.
The nurse should follow the critical pathway as much as possible and document any variances.
Normal ranges for wound healing after THA are not well defined, but some signs of infection include increased pain, swelling, redness, drainage, fever, and elevated white blood cell count.
The nurse should monitor these signs and report any changes to the surgeon.
A nurse is preparing to discharge a client who has been on a case management model of care.
The nurse wants to evaluate the effectiveness of the care provided.
Which of the following statements should the nurse use?
Explanation
“Did you achieve your expected outcomes within the planned time frame?.”.
This statement is the best way to evaluate the effectiveness of the case management model of care, which is a plan that describes how to provide comprehensive and effective care to clients with different health needs and situations.It involves steps such as assessing, planning, implementing, coordinating, monitoring, and evaluating the care.By asking the client if they achieved their expected outcomes within the planned time frame, the nurse can measure the quality, satisfaction, and cost-efficiency of the care provided.
Choice A is wrong because it is too vague and subjective.
Asking the client if they received quality care during their stay does not specify what aspects of the care were satisfactory or not, or how they relate to the case management model.
Choice B is wrong because it is also too vague and subjective.
Asking the client how satisfied they are with their recovery process does not indicate what goals or outcomes were set or achieved, or how they were influenced by the case management model.
Choice D is wrong because it is too narrow and specific.
Asking the client how well they understood their discharge instructions does not reflect the whole process of the case management model, which involves more than just discharge planning.
It also does not measure the effectiveness of the care in terms of outcomes or cost-efficiency.
A nurse is using a computer terminal at the client’s bedside to document care immediately after it is given.
Which of the following advantages does this method of documentation have?
No explanation
Documenting Nursing Activities (Record System Used in an Agency)
A nurse is preparing to document the admission nursing assessment for a client who has pneumonia.
Which of the following information should the nurse include in this documentation?
Explanation
The client’s vital signs, oxygen saturation, and respiratory status.
This is because the admission nursing assessment is a comprehensive evaluation of the client’s physical, mental, emotional, and social status, as well as their current health problems and needs.
The admission assessment provides baseline data for comparison and planning of care.The client’s vital signs, oxygen saturation, and respiratory status are essential components of the admission assessment for a client who has pneumonia, as they reflect the severity of the infection and the risk of complications.
Choice B is wrong because the client’s medical history, allergies, and current medications are part of the health history interview, which is a component of the admission assessment but not the entire documentation.Choice C is wrong because the client’s nursing diagnosis, goals, and expected outcomes are part of the planning and implementation phases of the nursing process, which come after the assessment phase.Choice D is wrong because the client’s family contacts, insurance information, and advance directives are part of the administrative data collection, which is not directly related to the client’s health status or nursing care.
Normal ranges for vital signs vary depending on age, gender, and health conditions, but generally they are as follows:.
• Temperature: 36.5°C to 37.5°C (97.7°F to 99.5°F).
• Pulse: 60 to 100 beats per minute.
• Respirations: 12 to 20 breaths per minute.
• Blood pressure: less than 120/80 mm Hg.
• Oxygen saturation: 95% to 100%.
A nurse is reviewing the record system used in an agency.
Which of the following types of records are used for documenting concise data about a client and making information quickly accessible to all health professionals?
(Select all that apply.).
Explanation
Kardexes and flow sheets are types of records that are used for documenting concise data about a client and making information quickly accessible to all health professionals.Kardexes are a series of cards kept in a portable index file or on computer generated forms that contain a problem list, stated goals and list of nursing approaches to meet the goals.Flow sheets are forms that allow for recording routine aspects of care such as vital signs, intake and output, medications, etc.
Choice C is wrong because progress notes are not concise, but rather narrative descriptions of the client’s condition, interventions and outcomes.Choice D is wrong because nursing discharge summaries are not used for quick access, but rather for providing information about the client’s hospitalization, treatment and follow-up care.Choice E is wrong because care plan conferences are not records, but meetings where health professionals discuss the client’s needs, goals and progress.
Normal ranges for vital signs are as follows:.
• Temperature: 36.5°C to 37.5°C (97.7°F to 99.5°F).
• Pulse: 60 to 100 beats per minute.
• Respiration: 12 to 20 breaths per minute.
• Blood pressure: less than 120/80 mmHg.
A nurse is giving a change of shift report to the nurse on the next shift.
Which of the following statements by the nurse is appropriate for handoff communication?
Explanation
“The client in room 14 has a wound dressing that needs to be changed at 10 a.m.”
This statement is appropriate for handoff communication because it provides relevant and specific information about the patient’s care plan and any pending tasks that need to be completed by the next nurse.
It also allows for the opportunity for discussion and clarification between the nurses.
Choice A is wrong because it is subjective and disrespectful to the patient.
It does not convey any useful information about the patient’s condition, needs, or preferences.
It may also create a negative bias or impression on the next nurse, which could affect the quality of care.
Choice C is wrong because it is not timely or relevant for handoff communication.
The patient’s allergies should be documented in the electronic health record (EHR) and verified with the patient before administering any medications.
It is not necessary to repeat this information during every handoff, unless there is a change or concern.
Choice D is wrong because it is too vague and incomplete for handoff communication.
It does not provide any details about the patient’s current status, vital signs, medications, interventions, or goals.
It also does not indicate any anticipated changes or potential complications that the next nurse should be aware of.
Handoff communication is a critical element of patient safety and continuity of care.
It involves the transfer of essential patient data from one caregiver to another during transitions of care across the continuum.It should be interactive, accurate, concise, and standardized.Some examples of handoff communication tools are SBAR (Situation, Background, Assessment, Recommendations), I PASS the BATON (Introduction, Patient, Assessment, Situation, Safety concerns, Background, Actions, Timing, Ownership, Next), ISHAPED (Introduction, Story, History, Assessment, Plan, Error prevention, Dialogue), and kardex.
These tools help to structure and organize the information exchange between providers and ensure that nothing is missed or misunderstood.
References:.
:12 patient handoff communication tools to know - Becker’s ASC.
:Handoff communication - standardizing nursing protocols.
:Communication Strategies for Patient Handoffs | ACOG.
:8 Tips for High-quality Hand-offs - The Joint Commission.
A nurse is taking a telephone order from a radiologist for a client who needs an urgent chest x-ray.
Which of the following statements by the nurse is correct for verifying the order?
Explanation
“I read back the order for a chest x-ray for Mr. Jones in room 20.”.
This is the best way to verify a telephone order from a radiologist, as it ensures that the nurse has accurately transcribed the order and that the radiologist has confirmed it.
Reading back the order also allows the nurse to clarify any doubts or questions about the order, such as the urgency, the reason, or the patient’s condition.
Choice A is wrong because it does not verify the order, but simply repeats it.
The nurse should not assume that the order is correct without confirmation from the radiologist.
Choice B is wrong because it asks the radiologist to repeat the order, which is inefficient and may cause confusion or errors.
The nurse should repeat the order to the radiologist, not the other way around.
Choice C is wrong because it uses a closed-ended question that can be answered with a yes or no, which may not reflect the radiologist’s true intention or understanding of the order.
The nurse should use an open-ended statement that requires the radiologist to acknowledge or correct the order.
According to federal regulations and accreditation standards, verbal and telephone orders should be authenticated by the prescriber within a specified time frame, usually 24 hours.Some states may have different or more stringent requirements, so nurses should be familiar with their state laws and regulations.Verbal and telephone orders should also be documented and signed by two nurses or one nurse and one enrolled endorsed nurse for verification and administration.
A nurse is participating in a care plan conference for a client who has multiple chronic conditions and complex care needs.
What is the main purpose of this meeting?
Explanation
To provide continuity of care.
A care plan conference is a meeting between the nursing home staff, the resident, and the resident’s family to set measurable, specific goals for the resident to meet during their stay, decide what needs to be done to meet those goals, and decide who in the nursing home is responsible for performing each job necessary to help the resident.The main purpose of this meeting is to provide continuity of care, which means ensuring that the resident receives consistent and coordinated care across different settings and providers.
Choice A is wrong becauseto discuss possible solutions to certain client problemsis not the main purpose of a care plan conference, although it may be one of the topics discussed.
A care plan conference is not meant to address only specific problems, but rather the overall plan of care for the resident.
Choice B is wrong becauseto evaluate the effectiveness of the care givenis not the main purpose of a care plan conference, although it may be one of the outcomes of the meeting.
A care plan conference is not meant to assess only the performance of the staff, but rather the progress of the resident.
Choice C is wrong becauseto gather information for the plan of careis not the main purpose of a care plan conference, although it may be one of the steps involved.
A care plan conference is not meant to collect only information, but rather to use it to develop and update the plan of care.
A client who has been hospitalized for two weeks tells the nurse that he wants to go home today because he feels fine now and does not need any more treatment or tests done on him at this time.
The nurse knows that this client is scheduled for a cardiac catheterization tomorrow morning and that his discharge date is not yet determined by his physician.
Which of the following actions should the nurse take first?
Explanation
Assess the client’s understanding and readiness for discharge.
This is the first action that the nurse should take because it allows the nurse to evaluate the client’s mental status, coping skills, and educational needs.
The nurse should also explore the reasons why the client wants to go home and address any concerns or fears that the client may have.
Choice A is wrong because it is not client-centered and may increase the client’s anxiety or anger.
The nurse should not threaten or coerce the client to stay in the hospital against his will.
Choice B is wrong because it is not the priority at this time.
The nurse should first assess the client’s knowledge and willingness to undergo the cardiac catheterization before providing information about it.
Choice D is wrong because it is not the first action that the nurse should take.
The nurse should notify the physician and the charge nurse after assessing the client and documenting the findings.
A cardiac catheterization is a procedure that uses a thin, flexible tube (catheter) to access the heart and blood vessels.It can help diagnose and treat various heart conditions, such as coronary artery disease, heart valve disease, congenital heart defects, or heart failure.
Some of the benefits of cardiac catheterization are:.
• It can provide detailed information about the structure and function of the heart and blood vessels that other tests may not show.
• It can help determine the best treatment plan for the client based on his or her specific condition and needs.
• It can deliver treatments such as angioplasty, stent placement, valve repair or replacement, or device implantation during the same procedure.
• It can reduce the need for more invasive surgery or repeated hospitalizations.
A nurse is caring for a client who has just undergone surgery for appendicitis.
The nurse documents in the client’s chart : “Client resting comfortably in bed with IV fluids infusing at 125 mL/hr.
Dressing clean , dry , and intact.
No complaints of pain or nausea.
Denies any problems or concerns.” This type of documentation is an example of :.
Explanation
Narrative charting.
This type of documentation is an example of narrative charting because it chronicles all of the patient’s assessment findings and nursing activities that occurred throughout the shift in a descriptive format.
Some other choices are:.
• Choice A is wrong because SOAP charting is a type of documentation that is organized by four categories: Subjective, Objective, Assessment, and Plan.
It is commonly used in problem-oriented medical records.
• Choice B is wrong because PIE charting is a type of documentation that uses three categories: Problem, Intervention, and Evaluation.
It is based on the nursing process and eliminates the need for a separate care plan.
• Choice C is wrong because Focus charting is a type of documentation that uses three categories: Data, Action, and Response.
It emphasizes the patient’s concerns, problems, or strengths rather than medical diagnoses.
Normal ranges for vital signs and laboratory values may vary depending on the facility and the patient’s condition.
However, some general ranges are:.
• Temperature: 36.5°C to 37.5°C (97.7°F to 99.5°F).
• Pulse: 60 to 100 beats per minute.
• Respirations: 12 to 20 breaths per minute.
• Blood pressure: 120/80 mmHg or lower.
• Oxygen saturation: 95% or higher.
• Hemoglobin: 12 to 18 g/dL for men, 11 to 16 g/dL for women.
• Hematocrit: 37% to 49% for men, 36% to 46% for women.
• White blood cell count: 4,000 to 11,000 cells/mm3.
• Platelet count: 150,000 to 400,000 cells/mm3.
• Blood glucose: 70 to 110 mg/dL.
A nurse is using an electronic health record (EHR) system to document the care provided to a client who has pneumonia.
The nurse should follow which of the following guidelines when using an EHR system ?
(Select all that apply.).
Explanation
Choice A is correct because using standardized terminology and abbreviations can improve the clarity, accuracy, and consistency of the documentation in an EHR system.
• Choice B is correct because entering data as soon as possible after providing care can ensure the timeliness, completeness, and validity of the information in an EHR system.
• Choice C is wrong because sharing login information with other authorized users can compromise the security, privacy, and integrity of the EHR system.HIPAA guidelines require that each user has a unique identifier and password to access the EHR system.
• Choice D is correct because reviewing and verifying data before saving or submitting can prevent errors, omissions, and discrepancies in the EHR system.
• Choice E is wrong because correcting errors by drawing a single line through them is a method used for paper records, not electronic records.Electronic records should have a mechanism to track changes and corrections without altering the original data.
:HIPAA Guidelines for Electronic Medical Records:Electronic Health Records - Health IT Playbook.
Which of these statements about documentation are true?
(Select all that apply.).
Explanation
Documentation should be done as soon as possible after an event has occurred, because this ensures accuracy, timeliness, and continuity of care.Documentation should include objective data (what the nurse observes or measures), subjective data (what the patient says or feels), and nursing interventions (what the nurse does or plans to do) to provide a clear picture of the patient’s condition and needs.Documentation should use abbreviations, symbols, and acronyms that are approved by the facility, because this promotes consistency, clarity, and compliance with legal and professional standards.
Choice D is wrong because documentation should not include opinions, judgments, or assumptions about the client’s condition, as these are not based on facts or evidence and may be biased or inaccurate.Documentation should be factual, accurate, and objective.
Choice E is wrong because documentation should reflect the nursing process and the standards of care, but this is not a complete statement.Documentation should also reflect the patient’s perspective, preferences, and goals.Documentation should be patient-centered, holistic, and individualized.
Normal ranges for clinical observations vary depending on the patient’s age, health status, and other factors.
However, some general ranges are:.
• Temperature: 36.5°C to 37.5°C.
• Pulse: 60 to 100 beats per minute.
• Respirations: 12 to 20 breaths per minute.
• Blood pressure: 120/80 mmHg or lower.
• Oxygen saturation: 95% or higher.
Sources:.
What is one advantage of using a computerized system for documentation and reporting?
Explanation
It allows access to client information from multiple locations.
This is an advantage of using a computerized system for documentation and reporting because it enables health care providers to access relevant and updated information about their clients from different locations, such as hospitals, clinics, or home care settings.This can improve the quality and continuity of care, as well as facilitate communication and collaboration among different members of the health care team.
Choice A is wrong because it is not true that a computerized system eliminates errors and inaccuracies in documentation.While a computerized system can reduce some types of errors, such as illegible handwriting or misplaced files, it can also introduce new types of errors, such as data entry mistakes, software glitches, or system failures.
Choice C is wrong because it is not true that a computerized system reduces the need for verbal or written communication among health care providers.On the contrary, a computerized system can enhance communication by allowing health care providers to share information more easily and quickly, but it does not replace the need for verbal or written communication to clarify, confirm, or discuss the information.
Choice D is wrong because it is not true that a computerized system protects client information from unauthorized disclosure or alteration.
While a computerized system can provide some security features, such as passwords, encryption, or audit trails, it can also pose some risks, such as hacking, phishing, or malware attacks.Therefore, health care providers need to follow ethical and legal guidelines to ensure the confidentiality and integrity of client information in a computerized system.
A nurse is preparing to report a change in a client’s condition to another health care provider.
What should the nurse include in the report?
Explanation
A statement of facts, changes, trends, and responses to treatment.This is the best way to report a change in a client’s condition to another health care provider because it provides clear, concise, and relevant information that can help with decision making and continuity of care.
Choice A is wrong because a summary of all the interventions performed since admission is too broad and may not reflect the current situation of the client.
Choice B is wrong because a description of how the nurse feels about the client’s situation is subjective and may not be helpful for the other health care provider.Choice C is wrong because a comparison of the client’s condition with other similar cases is not specific to the individual client and may not account for differences in factors such as age, comorbidities, or preferences.
Normal ranges for vital signs, laboratory values, and other parameters may vary depending on the source and the context, but some common examples are:.
• Temperature: 36.5°C to 37.5°C (97.7°F to 99.5°F).
• Pulse: 60 to 100 beats per minute.
• Respirations: 12 to 20 breaths per minute.
• Blood pressure: less than 120/80 mm Hg.
• Oxygen saturation: greater than 95%.
• Blood glucose: 4.0 to 7.8 mmol/L (72 to 140 mg/dL).
• Hemoglobin: 13.5 to 17.5 g/dL for males, 12.0 to 15.5 g/dL for females.
• White blood cell count: 4.0 to 11.0 x 10^9/L.
• Platelet count: 150 to 400 x 10^9/L.
A nurse is using SOAP format to document a client’s progress note.
What does SOAP stand for?
Explanation
Subjective, Objective, Assessment, Plan.This is the meaning of SOAP format, which is a documentation method used by nurses and other healthcare providers to write out notes in the patient’s chart.
Choice B is wrong becauseSituation, Observation, Action, Problemis not a documentation method, but a communication tool used in handovers and briefings.
Choice C is wrong becauseSummary, Outcome, Analysis, Processis not a documentation method, but a framework for writing reflective essays.
Choice D is wrong becauseSource, Opinion, Accuracy, Purposeis not a documentation method, but a criteria for evaluating information sources.
SOAP format helps to organize the information collected from the patient in a clear and consistent manner.
It consists of four components:.
• Subjective: This includes how the patient is feeling and how they have been since the last review in their own words.
• Objective: This includes the objective observations that can be measured, seen, heard, felt or smelled, such as vital signs, fluid balance, clinical examination findings and investigation results.
• Assessment: This includes the thoughts on the salient issues and the diagnosis (or differential diagnosis) based on the subjective and objective data.
• Plan: This includes the actions that will be taken to address the patient’s problems, such as medications, investigations, referrals and follow-ups.
A nurse is teaching a newly hired nurse about the legal aspects of documentation.
Which of the following statements by the newly hired nurse indicates an understanding of the teaching?
Explanation
“I should document any incident that occurs during my shift and notify the provider.” This statement indicates an understanding of the legal aspects of documentation, which include:.
• Documenting accurately, objectively, and completely to provide evidence of care delivery and support the nurse’s moral and legal responsibilities.
• Documenting any change in the patient’s condition, treatments, medications, interventions, client responses, and complaints.
• Documenting any incident that occurs during the shift and notifying the provider to ensure appropriate follow-up and prevent further harm.
• Documenting in a timely manner to minimize errors and omissions.
The other choices are wrong because:.
• Choice A is wrong because documenting only normal findings can mislead the client and other health professionals about the actual status of the client.It can also impede patient care and hinder the nurse’s legal defense in the event of a malpractice lawsuit.
• Choice C is wrong because documenting in advance can compromise the accuracy and integrity of the documentation.It can also lead to legal action if the documented events do not match the actual events.
• Choice D is wrong because documenting personal opinions about the client’s condition and care can be considered unprofessional, biased, and disrespectful.It can also damage the nurse-client relationship and expose the nurse to legal liability.
Normal ranges for documentation depend on the type of information being documented, such as vital signs, laboratory values, assessment findings, etc.
They may vary according to different sources and standards.
Nurses should follow the policies and procedures of their institution and use their clinical judgment when documenting abnormal findings.
A nurse is teaching a newly hired nurse about the legal aspects of documentation.
Which of the following statements by the newly hired nurse indicates an understanding of the teaching?
Explanation
“I should document any incident that occurs during my shift and notify the provider.” This statement indicates an understanding of the legal aspects of documentation, which include:.
• Documenting accurately, objectively, and completely to provide evidence of care delivery and support the nurse’s moral and legal responsibilities.
• Documenting any change in the patient’s condition, treatments, medications, interventions, client responses, and complaints.
• Documenting any incident that occurs during the shift and notifying the provider to ensure appropriate follow-up and prevent further harm.
• Documenting in a timely manner to minimize errors and omissions.
The other choices are wrong because:.
• Choice A is wrong because documenting only normal findings can mislead the client and other health professionals about the actual status of the client.It can also impede patient care and hinder the nurse’s legal defense in the event of a malpractice lawsuit.
• Choice C is wrong because documenting in advance can compromise the accuracy and integrity of the documentation.It can also lead to legal action if the documented events do not match the actual events.
• Choice D is wrong because documenting personal opinions about the client’s condition and care can be considered unprofessional, biased, and disrespectful.It can also damage the nurse-client relationship and expose the nurse to legal liability.
Normal ranges for documentation depend on the type of information being documented, such as vital signs, laboratory values, assessment findings, etc.
They may vary according to different sources and standards.
Nurses should follow the policies and procedures of their institution and use their clinical judgment when documenting abnormal findings.
A nurse is using a computerized documentation system in a health care facility.
Which of the following actions should the nurse take to ensure confidentiality and security?
(Select all that apply.).
Explanation
A. Log off the system when leaving the workstation.
This is a correct action to ensure confidentiality and security of electronic health records (EHRs).
Logging off prevents unauthorized access to client information by other users who may use the same workstation.It also protects the system from malware or cyberattacks that may compromise the data integrity or availability.
B. Shred any printouts before discarding them.
This is also a correct action to ensure confidentiality and security of EHRs.
Shredding any printouts that contain client information prevents them from being accessed by unauthorized persons who may find them in the trash or recycling bins.It also complies with the legal and ethical obligations to protect the privacy of clients.
C. Use a personal digital assistant (PDA) to access client information.
This is an incorrect action to ensure confidentiality and security of EHRs.
Using a PDA to access client information may expose the data to unauthorized access, loss, theft, or damage.
PDAs are typically not encrypted or password-protected, and may not have adequate security features or software updates to prevent cyberattacks or malware infections.PDAs may also not be compatible with the EHR system or follow the data standards and interoperability requirements.
D. Change the password at regular intervals.
This is another correct action to ensure confidentiality and security of EHRs.
Changing the password at regular intervals reduces the risk of password cracking, guessing, or phishing by unauthorized users or hackers.It also helps to maintain the accountability and authentication of authorized users who access the EHR system.
E. Report any breaches or attempted breaches to the appropriate authority.
This is also a correct action to ensure confidentiality and security of EHRs.
Reporting any breaches or attempted breaches to the appropriate authority helps to identify and mitigate the impact of any data loss, corruption, or disclosure.It also helps to comply with the legal and regulatory obligations to notify the affected clients and stakeholders, and to prevent further breaches or incidents.
A nurse is using the focus charting method to document care for a client who has diabetes mellitus.
Which of the following terms should the nurse use to begin each entry?
Explanation
Focus.
Focus charting is a method of organizing health information in an individual’s record using nursing terminology to describe the individual’s health status and nursing actions.The focus of each entry can be a nursing diagnosis, a sign or symptom, an acute change in condition, a significant event, or a key word indicating compliance with a standard of care.
The focus charting method uses three columns: date and hour, focus, and progress notes.The progress notes are organized into data, action, and response, referred to as DAR.
Choice A is wrong because data is not the term used to begin each entry, but rather the category that describes the subjective and/or objective information supporting the stated focus.Choice B is wrong because problem is not the term used to begin each entry, but rather the nursing diagnosis or collaborative problem on the plan of care.Choice D is wrong because assessment is not the term used to begin each entry, but rather the phase of the nursing process that involves collecting data.
A nurse is using an electronic health record (EHR) system to document care for a client who has pneumonia.
Which of the following is an advantage of using an EHR system?
Explanation
It reduces duplication of documentation among caregivers.
This is an advantage of using an EHR system because it allows different healthcare providers to access and update the same record, avoiding unnecessary repetition and inconsistency.An EHR system also improves the quality and safety of care by providing clinical decision support, reducing medication errors, and facilitating communication among caregivers.
Choice A is wrong because it is not the only advantage of using an EHR system.While it is true that an EHR system eliminates errors due to illegible handwriting, it may also introduce new types of errors such as data entry mistakes, system failures, or unauthorized access.
Choice B is wrong because it is not an advantage of using an EHR system.
In fact, it may be a disadvantage because it poses a risk to the confidentiality and security of the clients’ records.An EHR system should have built-in safeguards to protect the privacy and integrity of the data, such as encryption, passwords, and audit trails.
Choice D is wrong because it is not an advantage of using an EHR system.It is a requirement of any health record system, whether electronic or paper-based, to comply with the ethical and legal standards of confidentiality.
An EHR system does not provide any additional safeguards that are not already present in a paper-based system.
Normal ranges for vital signs are as follows:.
• Temperature: 36.5°C to 37.5°C (97.7°F to 99.5°F).
• Pulse: 60 to 100 beats per minute.
• Respirations: 12 to 20 breaths per minute.
• Blood pressure: less than 120/80 mm Hg.
A nurse is documenting an incident report for a medication error that occurred on her unit.
Which of the following actions should the nurse take?
(Select all that apply.).
Explanation
The nurse should include factual information about what happened and notify the risk management department.These actions are part of the steps of reporting medication errorsand the good practice guide on recording, coding, reporting and assessment of medication errors.
Choice B is wrong because the nurse should not state opinions about who was responsible for the error.
This could be seen as biased, unprofessional or accusatory.
The nurse should focus on the facts and the causes of the error, not on blaming individuals.
Choice C is wrong because the nurse should not file the report in the client’s medical record.
This could violate the client’s privacy and confidentiality.
The report should be filed in a separate system that is accessible only to authorized personnel.
Choice E is wrong because the nurse should not discuss possible solutions to prevent future errors.
This could be premature, unrealistic or inappropriate.
The nurse should leave this task to the investigation team or the risk management department, who will analyse the incident and make recommendations based on evidence and best practice.
A nurse is documenting a client’s admission assessment using a flow sheet.
Which of the following information should be included in a flow sheet?
(Select all that apply.).
Explanation
A flow sheet is a type of document that recordsroutineandfrequentdata in agraphicalortabularform.It is used tomonitorandevaluatethe patient’s condition and response to treatment over time.A flow sheet should include information that isrelevant,conciseandeasy to read.
• Choice A is correct because vital signs are one of the most common and important data that need to be recorded and monitored regularly for any patient.
• Choice B is correct because allergies are essential information that can affect the patient’s treatment plan and prevent adverse reactions.
• Choice C is correct because medication administration is another crucial data that shows what drugs, doses, routes and times the patient has received or will receive.
• Choice D is wrong because medical history is not a routine or frequent data that needs to be recorded in a flow sheet.Medical history is usually documented in a separate form that provides more details and background information about the patient’s past and present health conditions.
• Choice E is correct because intake and output are important data that indicate the patient’s fluid balance and renal function.
They need to be recorded and monitored regularly, especially for patients who have fluid restrictions.
A nurse is using focus charting to document a client’s progress notes.
What are the advantages of using focus charting?
(Select all that apply.).
Explanation
Focus charting is a method of organizing health information in an individual’s record that centers on the patient’s concerns and strengths.It uses a three-column format to document the data, action and response (DAR) of each focus.
The advantages of using focus charting are:.
• It highlights the client’s concerns and strengths, which makes the care more patient-centered and holistic.
• It reduces redundancy and duplication of data, as it avoids repeating information that is already recorded in other forms or flow sheets.
• It facilitates communication among health care team members, as it promotes interdisciplinary documentation and helps organize the information in a concise and precise way.
Choice D is wrong because focus charting does not incorporate nursing diagnoses and care plans, although it is based on the nursing process.Nursing diagnoses and care plans are documented separately or as part of the action category.
Choice E is wrong because focus charting does not provide a chronological record of events, but rather organizes the data by the focus.A chronological record of events can be found in other forms of documentation, such as narrative or SOAP notes.
A nurse is using SOAP documentation to write a progress note for a client who has cellulitis of the lower leg.
The nurse needs to select all that apply when writing an assessment entry in SOAP documentation.
Explanation
These are the only options that describe thesubjectiveandobjectivedata of the patient, which are part of theSOAPdocumentation method.SOAP stands forSubjective, Objective, Assessment, and Plan, and it is a way of recording patient data in a clear and consistent manner.
ChoiceCis wrong because wound culture results are not part of the assessment entry in SOAP documentation.They are part of the investigation results, which are usually documented in the objective section.
ChoiceDis wrong because risk for infection related to impaired skin integrity is a nursing diagnosis, not an assessment.Nursing diagnoses are usually documented in the plan section of SOAP documentation.
ChoiceEis wrong because applied moist heat compresses to the wound site is an intervention, not an assessment.Interventions are also documented in the plan section of SOAP documentation.
Normal ranges for vital signs are as follows:.
• Blood pressure: 90/60 mmHg to 120/80 mmHg.
• Pulse rate: 60 to 100 beats per minute.
• Respiratory rate: 12 to 20 breaths per minute.
• SpO2: 95% to 100%.
• Temperature: 36.5°C to 37.5°C.
A nurse is using CBE documentation for a client who has diabetes mellitus.
The nurse administers insulin to the client and documents this on a:.
Explanation
Medication administration record.
A medication administration record (MAR) is a document that records the medications that have been given to a patient, including the dose, route, time, and nurse’s initials.
A MAR is an essential part of nursing documentation and ensures safe and accurate medication administration.
Choice A is wrong because a graphic record is a document that shows the trends of vital signs, intake and output, weight, and other measurements over time.
A graphic record does not include information about medications.
Choice B is wrong because a daily care record is a document that records the routine care activities that have been performed for a patient, such as hygiene, nutrition, elimination, mobility, and comfort measures.
A daily care record does not include information about medications.
Choice D is wrong because a client teaching record is a document that records the education that has been provided to a patient or family, such as disease process, medications, diet, exercise, self-care, and discharge planning.
A client teaching record does not include information about medication administration.
CBE documentation is a method of charting by exception that allows the nurse to document only those findings that fall outside the standard of care or norms defined by a specific institution.
CBE documentation reduces the amount of time required to document care and eliminates unnecessary or redundant information.
However, CBE documentation does not apply to medication administration, which must be documented accurately and completely for every patient.
A nurse is reviewing a critical pathway for a client who has chronic obstructive pulmonary disease (COPD).
The nurse should understand that a critical pathway:.
Explanation
A critical pathway provides guidelines for managing clients with similar health problems.According to the definition from Wikipedia, a critical pathway is one of the main tools used to manage the quality in healthcare concerning the standardisation of care processes.It has been shown that their implementation reduces the variability in clinical practice and improves outcomes.
Choice A is wrong because a critical pathway does not specify the plan of care for clients with different diagnoses, but rather for a specific group of patients with a predictable clinical course.Choice C is wrong because a critical pathway does not describe the roles and responsibilities of each member of the health care team, but rather defines, optimizes and sequences the different tasks (interventions) by the professionals involved in the patient care.Choice D is wrong because a critical pathway does not evaluate the quality and cost-effectiveness of care delivered to clients, but rather aims to promote organised and efficient patient care based on evidence-based medicine.
Normal ranges for COPD are: FEV1/FVC ratio < 0.7; FEV1 < 80% predicted; FVC normal or reduced; TLC > 80% predicted; RV > 120% predicted; DLCO < 80% predicted.
A nurse is working in an agency that uses EHR for documentation.
Which of the following actions should the nurse take to ensure confidentiality and security of the client’s information?
(Select all that apply.).
Explanation
The nurse should use a personal password to access the system and log off when finished, and report any breaches or attempted breaches of security to the appropriate personnel.
These actions ensure confidentiality and security of the client’s information by preventing unauthorized access and disclosing any violations.
Choice B is wrong because sharing the password with other nurses who need to access the system violates the principle ofminimum necessary access, which means that only those who need the information for a specific purpose should have access to it.
Choice C is wrong because printing out a copy of the client’s record and storing it in a locked cabinet creates a risk ofloss, theft, or unauthorized disclosureof the paper record.The nurse should avoid printing out electronic health records unless absolutely necessary, and should follow the proper disposal procedures if they do.
Choice E is wrong because deleting any information that is incorrect or outdated from the system may compromise theintegrity and availabilityof the client’s information.The nurse should follow the established policies and procedures for correcting or updating electronic health records, which may include adding an addendum or annotation to the original entry, but not deleting it.
A nurse is documenting the care provided to a client who receives home health services.
Which of the following records should the nurse use to certify that the client meets Medicare eligibility criteria and to outline the services to be provided?
Explanation
Home health certification and plan of treatment.This is the record that the nurse uses to certify that the client meets Medicare eligibility criteria and to outline the services to be provided.A home health certification and plan of treatment is a document that contains the physician’s or allowed practitioner’s orders for home health services, the patient’s diagnosis, the patient’s functional limitations, the type and amount of services needed, and the expected duration of care.
Choice B is wrong becauseOutcome and Assessment Information Set (OASIS)is a standardized assessment tool that HHAs use to collect data on adult patients receiving skilled services.
OASIS is not used to certify eligibility or plan treatment.
Choice C is wrong becauseHome care flow sheetis a form that HHAs use to document the daily care provided by nurses and home health aides.
A home care flow sheet does not certify eligibility or plan treatment.
Choice D is wrong becauseHome care progress noteis a form that HHAs use to document the patient’s progress toward the goals of care, any changes in the plan of care, and any communication with other health care providers.
A home care progress note does not certify eligibility or plan treatment.
A nurse is using a flow sheet to document the care of a client who has heart disease and is admitted to a long-term care facility.
Which of the following data should the nurse record on this type of document?
Explanation
Daily weight, blood pressure, and pulse.
A flow sheet is a type of document that records specific information in a structured and concise way, such as vital signs, fluid intake and output, pain level, etc.A flow sheet is useful for clinical communication and tracking the patient’s condition over time.A medication administration record (MAR) is a separate document that records the medications given to the patient, the dosage, the route, and the time.A nursing diagnosis and care plan is a document that identifies the patient’s problems and goals, and the interventions to achieve them.A discharge planning and referral summary is a document that outlines the patient’s needs and resources after leaving the facility, such as follow-up appointments, home care services, etc.
These documents are not part of a flow sheet.
Choice B is wrong because a MAR is not a flow sheet.
Choice C is wrong because a nursing diagnosis and care plan is not a flow sheet.
Choice D is wrong because a discharge planning and referral summary is not a flow sheet.
Normal ranges for daily weight vary depending on the patient’s age, height, gender, and medical condition.However, a general guideline is that a weight gain or loss of more than 2 kg (4.4 lbs) in a week or 0.9 kg (2 lbs) in a day may indicate fluid retention or dehydration.Normal ranges for blood pressure are less than 120/80 mmHg for adults, and less than 95/65 mmHg for children.Normal ranges for pulse are 60 to 100 beats per minute for adults, and 70 to 120 beats per minute for children.
A nurse is using accepted terminology and abbreviations when documenting the care of a client who has pneumonia and is receiving oxygen therapy via nasal cannula at 2 L/min.
Which of the following abbreviations should the nurse use?
(Select all that apply.).
Explanation
The nurse should use the following abbreviations when documenting the care of a client who has pneumonia and is receiving oxygen therapy via nasal cannula at 2 L/min:.
• O2: This stands for oxygen and indicates the type of gas being delivered to the patient.
• NC: This stands for nasal cannula and indicates the device used to deliver oxygen to the patient.
• SpO2: This stands for peripheral oxygen saturation and indicates the percentage of hemoglobin that is saturated with oxygen in the blood.
It is measured by a pulse oximeter attached to the patient’s finger or earlobe.
• RR: This stands for respiratory rate and indicates the number of breaths per minute that the patient takes.
It is an important vital sign to monitor in patients with respiratory conditions.
Choice C is wrong because LPM is not an accepted abbreviation for oxygen therapy.LPM stands for liters per minute and indicates the flow rate of oxygen being delivered to the patient.However, it should not be abbreviated as LPM, but written out in full or as L/min.This is to avoid confusion with other abbreviations such as lpm (lowercase L) which stands for light per minute, a unit of luminous flux.
Normal ranges for SpO2 and RR vary depending on the age, health status and activity level of the patient, but generally they are:.
• SpO2: 95% to 100% for healthy adults.
Lower values may indicate hypoxemia (low blood oxygen level) or other conditions affecting oxygen delivery or uptake in the body.
• RR: 12 to 20 breaths per minute for healthy adults.
Higher or lower values may indicate respiratory distress, infection, pain, anxiety or other conditions affecting breathing.
Exams on Documenting and Reporting
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
-
List the measures used to maintain confidentiality and security of computer client records.
-
Discuss the purposes of client records.
-
Explain how various forms in the client records are used to document steps in nursing process.
-
Compare and contrast different documentation needed for clients in acute care, home care, and long-term care settings.
-
Identify and discuss the guidelines for effective recording that meet legal and ethical standards.
-
Identify essential guidelines for reporting client data.
Documentation and Reporting
- Documentation and reporting are the major communication techniques used by all healthcare providers.
-
Serves as a permanent record of patient information, data, and care.
-
Takes place when two or more people share information and data about patients in written or oral form.
-
An informal oral consideration of a subject by two or more healthcare personnel, to identify a problem or establish strategies to resolve a problem.
-
Oral, written, or computer-based communication intended to convey information to others.
-
A formal legal document that provides evidence of a client's care and can be written or computer-based.
-
Recording
-
Charting or Documenting
Documentation:
Reporting:
Communication Among Health Personnel
Discussion:
Report:
Record (Chart or Client Record):
The Process of Making an Entry on a Client
Ethical and Legal Considerations in Documenting and Reporting
-
Maintain the confidentiality of all patient information.
-
The client's record is also protected legally as a private record of the client's care.
-
Access to the record is restricted to health professionals involved in giving care to the client.
-
The institution or agency is the rightful owner of the client's record.
-
The client has the right to access all information contained within their own record and to have a copy of the original record.

-
Ensuring Confidentiality of Computerized Records
-
A personal password is needed to enter and sign off computer files.
-
Do not share the password with anyone, including other members of the health team.
-
After logging on, never leave a computer unattended.
-
Do not leave client information displayed on the monitor where others may see it.
-
The Information Technology team must install a firewall to protect the server from unauthorized access.
-
Shed all that is NOT needed in computer-generated worksheets.
-
Know the facility's policy and procedure for correcting an entry error.
-
Follow the agency's procedures for documenting sensitive material such as a diagnosis of AIDS.
Purposes/Reasons for Client Records
Purposes/Reasons for Client Records
-
Communication.
-
Planning client care.
-
Auditing health agencies.
-
Research.
-
Education.
-
Reimbursement/payment.
-
Legal documentation.
-
Health care analysis.
Communication:
-
Prevents repetition and delays in client care.
Planning client care:
-
Client records may be used to plan for care.
Auditing health agencies:
-
Review client records for quality assurance to determine if the hospital is meeting its stated standards.
Research:
-
Data in the record can be used for nursing research.
Education:
-
Client records may use data as educational tools.
Reimbursement/payment:
-
Records help facilities receive refunds from the government or get payment through Medicare.
Legal documentation:
-
Client's records serve as evidence in court.
Health care analysis:
-
Records may help health care planners identify agency needs, such as overuse or underuse of hospital services.
Documentation System
Source-Oriented Record: (Traditional)
-
Each person or department makes a separate section or sections of the client's chart (admission sheet, doctor order sheet, nursing assessment, diagnostic report, discharge plan, nurses' notes).
Problem-Oriented Medical Record (POMR):
-
The data is arranged according to the problems the client has rather than the source of the information.
Advantages of POMR
1. It encourages collaboration.
2. The problem list in the front of the chart alerts caregivers to the client's needs and makes it easier to track the status of each problem.
Disadvantages of POMR
1. Caregivers differ in their ability to use the required charting format.
2. It requires constant attention to maintain an up-to-date problem list.
Somewhat inefficient because assessments and interventions that apply to more than one problem must be repeated.
4 Basic Components of POMR
1. Database: Consists of all information when the client first enters the healthcare agency. It includes:
-
Nursing assessment
-
Physician history
-
Social and family data
-
Results of physical examination
-
Baseline diagnostic tests
2. Problem list: Derived from the database.
-
Impaired physical mobility
-
History of hypertension
-
Constipation
3. Plan of care: Care plans are generated by the person who lists the problems.
4. Progress notes:
-
Chart entries made by all health professionals involved in the client's care.
-
Numbered to correspond to the problems on the problem list.
Format of Progress Notes (DAR)
D: DATA (assessment phase): e.g., facial grimace, rates pain at 4/10.
A: ACTION (planning and implementing): Reflects planning and implementation, e.g., Administer paracetamol 500 mg every 4 hrs.
R: RESPONSE (evaluation phase): e.g., Rates pain at "2". States willingness to ambulate.
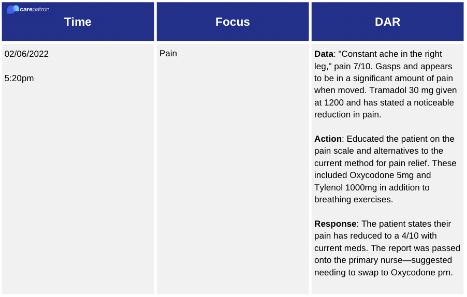
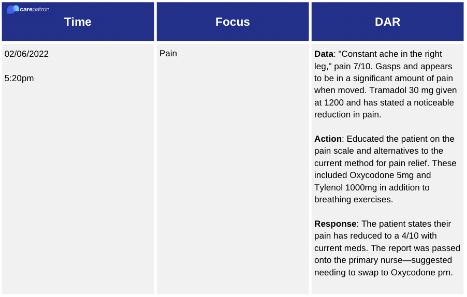
Format of Nursing Progress Notes
SOAP: An acronym for subjective, objective, assessment, and planning.
S: Subjective data consists of information obtained from what the client says.
O: Objective data consists of information that is measured or observed using the senses.
A: Assessment is the interpretation or conclusions drawn about the subjective and objective data.
P: Plan of care designed to resolve the stated problem, the initial plan is written by the person who enters the problem into the record.
Examples of Nursing Progress Notes
SOAPIER: add intervention, evaluation, revision.
I: Intervention refers to the specific interventions that have actually been performed by the caregiver.
E: Evaluation includes client responses to nursing interventions and medical treatment.
R: Revision reflects care plan modifications suggested by the evaluation.
Documentation System
-
Problems, Interventions, and Evaluation Documentation (PIE)
-
PIE is an acronym for problems, interventions, and evaluation of nursing care. This system consists of a client care assessment flow sheet and progress notes.
Flow Sheet
-
Use specific assessment criteria in a particular format. The time parameters for a flow sheet can vary from minutes to months. Examples include a graphic record and fluid balance.
Focus Charting
Focus Charting is intended to make the client and client concerns and strengths the focus of care. It has three columns for recording:
1. Date & Time
2. Focus: May be a condition, a nursing diagnosis, behavior, signs and symptoms, or an acute change in client condition or client strength.
3. Progress note (data, action, and response)
Charting By Exception (CBE)
CBE is a documentation system in which only abnormal or significant findings or exceptions to norms are recorded.
Key Elements of Charting By Exception (CBE)
- Flow sheet: Examples include a graphic record, fluid balance record, daily care record, client teaching record, client discharge, and skin assessment record.
- Standards of nursing care: Documentation by reference to the agency's printed standards of nursing practice eliminates much of the repetitive charting of routine care.
Bedside Access to Chart Forms
-
In the CBE system, all flow sheets are kept at the client's bedside to allow immediate recording.
-
Computerized Documentation: Electronic Health Record (EHR)
-
EHR was developed to manage the huge volume of information required in contemporary healthcare. It stores the client's database, new data, revised care plans, and documents client progress. Some institutions have a computer terminal at each client's bedside to enable the nurse to document care immediately after it is given.
Case Management
Case Management is a model that emphasizes quality, cost-effective care delivered within an established length of stay. It uses a multidisciplinary approach to planning and documenting client care. Using critical pathways helps identify the expected outcomes for each day of care. Variances are deviations from what was planned on the critical pathways, such as elevated temperature or impaired skin integrity.
Documenting Nursing Activities (Record System Used in an Agency)
- Admission Nursing Assessment: Referred to as the initial database, nursing history, completed when the client is admitted to the nursing unit. It includes the nursing diagnosis, client goals, and outcomes.
- Kardexes: A widely used concise method of organizing and recording data about a client, making information quickly accessible to all health professionals.
Flow Sheets, Progress Notes, and Nursing Discharge/Referral Summaries are also used for documenting nursing activities.
General Guidelines for Recording
1. Date and time must be specific.
2. Timing should be done after providing care.
3. Legibility is important to prevent errors.
4. Use accepted terminology and abbreviations.
5. Correct spelling is essential.
6. Signatures should include the nurse's name and credentials.
7. Accuracy is crucial, including the correct client name and identification.
Reporting
- Change of shift reports: Handoff communication given to the nurse on the next shift to provide continuity of care.
- Telephone reports: Nurses must be concise and accurate when reporting results from radiologists or taking telephone orders.
- Care plan conference: A meeting of a group of nurses to discuss possible solutions to certain client problems.
- Nursing rounds: Procedures in which two or more nurses visit selected clients at each client's bedside to gather information for the plan of care, discuss care, and evaluate care given.
Documentation of Clients' Care
1. Long-Term Care Documentation: Based on professional standards and policies of the healthcare agency, for adults with chronic conditions such as pneumonia or heart disease.
2. Home Care Documentation: Must standardize their documentation methods. Two types of records are used: home health certification and a plan of treatment form, as well as medical update and client information forms.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Documenting and Reporting
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now



