Please set your exam date
Gestational Diabetes
Study Questions
Introduction
A nurse is providing education to a pregnant woman diagnosed with gestational diabetes.
The nurse explains that gestational diabetes primarily affects ?
Explanation
The correct answer is choice B.Gestational diabetes primarily affects the baby’s growth and development.Gestational diabetes is a condition in which women develop high blood sugar during pregnancy due to hormonal changes or insufficient insulin production.This can cause the baby to grow larger than usual, which can lead to difficulties during delivery and increase the risk of cesarean section.It can also cause other complications for the baby, such as low blood sugar, jaundice, respiratory distress syndrome, and future diabetes.
Choice A is wrong because gestational diabetes does not affect blood pressure levels during pregnancy.However, high blood pressure during pregnancy can be a sign of another condition called preeclampsia, which can also cause complications for the mother and the baby.
Choice C is wrong because gestational diabetes does not affect the woman’s ability to produce insulin.
Rather, it affects how the cells use insulin to control blood sugar levels.The woman may need to take insulin injections or oral medications to manage her blood sugar levels during pregnancy.
Choice D is wrong because gestational diabetes does not affect the woman’s blood sugar levels after giving birth.
In most cases, gestational diabetes goes away after the baby is born.However, the woman may have a higher risk of developing type 2 diabetes later in life.
Normal ranges for blood sugar levels during pregnancy are:
• Before meals: 95 mg/dL or less
• One hour after meals: 140 mg/dL or less
• Two hours after meals: 120 mg/dL or less
A client with gestational diabetes asks the nurse about the timing of when gestational diabetes typically occurs.
The nurse responds by saying that it usually develops:.
Explanation
The correct answer is choice C.Gestational diabetes usually develops in thesecond or third trimester of pregnancy, when the body’s cells become more resistant to insulin due to hormonal changes.
Insulin is a hormone that helps the body use glucose (sugar) for energy.
Choice A is wrong because gestational diabetes does not develop in thefirst trimester of pregnancy.In fact, some women may have undiagnosed diabetes or pre-diabetes before they get pregnant, which can be detected by early screening.
Choice B is wrong because gestational diabetes does not developafter the baby is born.
For most women with gestational diabetes, the diabetes goes away soon after delivery.However, some women may have persistent diabetes or pre-diabetes that requires further testing and management.
Choice D is wrong because gestational diabetes does not developbefore pregnancy.Gestational diabetes is a type of diabetes that can develop during pregnancy in women who don’t already have diabetes.However, some women may have risk factors for developing gestational diabetes, such as being overweight, having a family history of diabetes, or having a previous history of GDM or macrosomia.
A nurse is discussing the long-term implications of gestational diabetes with a client.
The nurse explains that gestational diabetes increases the risk of developing which type of diabetes in the future?
Explanation
The correct answer is choice B. Type 2 diabetes.
Gestational diabetes is a condition that occurs when the body is not able to use insulin properly during pregnancy, which can cause high blood sugar levels.Gestational diabetes usually goes away after the baby is born, but it increases the risk of developing type 2 diabetes later in life.Type 2 diabetes is a chronic condition that affects how the body processes glucose, and it can be caused by genetic or lifestyle factors, such as obesity or physical inactivity.
Choice A is wrong because type 1 diabetes is an autoimmune disease that destroys the insulin-producing cells in the pancreas, and it is not related to gestational diabetes.
Choice C is wrong because gestational diabetes is not a type of diabetes, but a temporary condition that only affects pregnant women.
Choice D is wrong because prediabetes is a state of impaired glucose tolerance that can precede type 2 diabetes, but it is not a type of diabetes itself.Prediabetes can also be reversed with lifestyle changes, unlike type 2 diabetes.
A client with gestational diabetes is concerned about the impact of the condition on the baby's health.
The nurse reassures the client by explaining that gestational diabetes primarily affects the baby's:.
Explanation
The correct answer is choice D. Growth and development.
Gestational diabetes is a condition in which women develop high blood sugar during pregnancy.
This can affect the baby’s growth and development, as the excess glucose from the mother crosses the placenta and causes the baby to produce more insulin.This can lead to macrosomia, or a “fat” baby, which can cause complications during birth and increase the risk of obesity and diabetes later in life.
Choice A is wrong because gestational diabetes does not affect the baby’s vision.
Choice B is wrong because gestational diabetes does not affect the baby’s hearing.
Choice C is wrong because gestational diabetes does not affect the baby’s heart directly, although it can increase the risk of high blood pressure and preeclampsia in the mother.
A nurse is teaching a pregnant woman with gestational diabetes about lifestyle modifications.
Which statement by the client indicates an understanding of the teaching?
Explanation
The correct answer is choice C. Regular exercise can help control blood sugar levels.This is because exercise can improve insulin sensitivity and lower blood glucose levels.Exercise is an important part of lifestyle modifications for women with gestational diabetes, along with dietary changes.
Choice A is wrong because carbohydrates are an essential macronutrient that provide energy and nutrients for the mother and the fetus.Women with gestational diabetes should not avoid all carbohydrates, but rather choose complex carbohydrates that have a low glycemic index and limit the portion size.
Choice B is wrong because a sedentary lifestyle can increase the risk of developing type 2 diabetes after gestational diabetes.Women with gestational diabetes should be encouraged to be physically active for at least 30 minutes a day, most days of the week.
Choice D is wrong because monitoring blood glucose levels regularly is essential for managing gestational diabetes and preventing complications.Women with gestational diabetes should check their blood glucose levels at least four times a day: before breakfast and one hour after each meal.
Causes
A nurse is teaching a pregnant woman about gestational diabetes.
Which of the following statements by the nurse is correct?
Explanation
The correct answer is choice C.Gestational diabetes is caused by a hormonal imbalance that reduces insulin sensitivity.
Insulin is a hormone that helps the body use glucose for energy and control blood glucose levels.During pregnancy, the body makes special hormones and goes through other changes that can make the cells less responsive to insulin, a condition called insulin resistance.Most pregnant women can produce enough insulin to overcome insulin resistance, but some cannot and develop gestational diabetes.
Choice A is wrong because gestational diabetes is not caused by an autoimmune destruction of the pancreatic beta cells.This is the cause of type 1 diabetes, which usually develops in childhood or adolescence.
Choice B is wrong because gestational diabetes is not caused by a genetic mutation that impairs insulin secretion.This is the cause of some rare forms of diabetes, such as maturity-onset diabetes of the young (MODY) or neonatal diabetes mellitus (NDM).
Choice D is wrong because gestational diabetes is not caused by a viral infection that damages the insulin receptors.This is not a known cause of any type of diabetes.
Normal ranges for blood glucose levels during pregnancy are 3.5 to 5.9 mmol/L before meals and less than 7.8 mmol/L one hour after meals.
A nurse is caring for a pregnant woman who has gestational diabetes.
The nurse knows that the woman’s placenta produces hormones that have which of the following effects on her cells?
Explanation
The correct answer is choice C. They increase the resistance to insulin by the cells.This is because the placenta produces hormones such ashuman placental lactogen,growth hormone,prolactin,corticotropin-releasing hormone, andprogesteronethat can have a blocking effect on insulin.This is calledinsulin resistanceand it causes glucose to build up in the blood instead of being absorbed by the cells.
Choice A is wrong because the placental hormones do not increase the uptake of glucose by the cells, but rather decrease it by interfering with insulin action.
Choice B is wrong because the placental hormones do not decrease the production of glucose by the cells, but rather increase it by stimulating gluconeogenesis and glycogenolysis in the liver.
Choice D is wrong because the placental hormones do not decrease the breakdown of glucose by the cells, but rather increase it by stimulating lipolysis and ketogenesis in adipose tissue.
A nurse is providing education to a pregnant woman diagnosed with gestational diabetes.
The nurse explains that gestational diabetes primarily occurs due to:.
Explanation
The correct answer is choice A.Gestational diabetes primarily occurs due to hormonal changes during pregnancy affecting insulin production and action.
Insulin is a hormone that helps your body use glucose for energy and control your blood glucose levels.
During pregnancy, your body makes special hormones and goes through other changes that cause insulin resistance, meaning your cells don’t use insulin well.
Most pregnant women can produce enough insulin to overcome insulin resistance, but some cannot.These women develop gestational diabetes.
Choice B is wrong because genetic factors are not the main cause of gestational diabetes, although having a family history of diabetes may increase the risk.
Choice C is wrong because inadequate dietary intake of glucose during pregnancy does not cause gestational diabetes.However, eating healthy foods and controlling weight gain are important for managing gestational diabetes.
Choice D is wrong because an autoimmune response targeting the pancreas is not the cause of gestational diabetes.
Autoimmune diseases occur when your immune system attacks your own cells.Type 1 diabetes is an example of an autoimmune disease that affects the pancreas and causes insulin deficiency.
Gestational diabetes is not an autoimmune disease and does not affect the pancreas.
A client with gestational diabetes asks the nurse about the role of insulin in managing the condition.
The nurse responds by explaining that insulin helps:.
Explanation
The correct answer is choice A.Insulin helps reduce insulin resistance in the cells.
Insulin resistance is a condition in which the cells do not respond well to insulin and cannot use glucose effectively.
This causes high blood sugar levels, which can harm the mother and the baby.
Insulin therapy can help lower blood sugar levels by increasing the uptake of glucose by the cells.
Choice B is wrong because insulin does not decrease the production of hormones by the placenta.The placenta produces hormones that can make insulin less effective, but insulin does not affect the placenta’s hormone production.
Choice C is wrong because insulin does not increase blood sugar levels for optimal fetal growth.
Insulin lowers blood sugar levels by delivering glucose to the cells.High blood sugar levels can cause problems for the baby, such as being very large, having low blood sugar after birth, or developing type 2 diabetes later in life.
Choice D is wrong because insulin does not prevent the development of type 1 diabetes.
Type 1 diabetes is an autoimmune disease in which the body’s immune system destroys the insulin-producing cells in the pancreas.Gestational diabetes is not caused by a lack of insulin, but by other hormones produced during pregnancy that can make insulin less effective.Gestational diabetes usually goes away after delivery, but it can increase the risk of developing type 2 diabetes later in life.
A nurse is discussing the causes of gestational diabetes with a pregnant client.
The nurse emphasizes that gestational diabetes develops when:.
Explanation
The correct answer is choice A. The pancreas fails to produce enough insulin during pregnancy.This is because gestational diabetes occurs when the body can’t make the extra insulin needed during pregnancy.Insulin is a hormone that helps the body use glucose for energy and control blood sugar levels.During pregnancy, the body makes more hormones and goes through other changes, such as weight gain, that cause insulin resistance.This means that the body’s cells don’t use insulin well and the blood sugar levels rise.
Choice B is wrong because consuming excessive amounts of sugary foods during pregnancy does not cause gestational diabetes.However, eating healthy foods and avoiding processed and baked foods can help prevent or manage gestational diabetes.
Choice C is wrong because hormones produced by the placenta decrease insulin sensitivity in the cells, not increase it.This makes it harder for the body to use insulin and lowers the amount of glucose that enters the cells.
Choice D is wrong because insulin production by the pancreas is not inhibited by certain medications.
However, some medications may affect blood sugar levels and should be used with caution during pregnancy.Always consult your doctor before taking any medication if you have gestational diabetes or are at risk of developing it.
A client diagnosed with gestational diabetes expresses confusion about why the condition occurs during pregnancy.
The nurse explains that gestational diabetes is primarily related to:.
Explanation
The correct answer is choice C.Gestational diabetes is primarily related to the production of hormones by the placenta affecting insulin action.
Insulin is a hormone that helps your body use glucose for energy and control your blood glucose levels.
During pregnancy, your body makes special hormones and goes through other changes that cause insulin resistance, meaning your body’s cells don’t use insulin well.
Most pregnant women can produce enough insulin to overcome insulin resistance, but some cannot.These women develop gestational diabetes.
Choice A is wrong because changes in the client’s metabolic rate during pregnancy are not the main cause of gestational diabetes.
Metabolic rate refers to how fast your body uses energy.
While pregnancy can affect your metabolic rate, it does not directly affect your insulin production or action.
Choice B is wrong because an autoimmune response triggered by the growing fetus is not the cause of gestational diabetes.
An autoimmune response is when your immune system attacks your own cells or tissues.
Gestational diabetes is not an autoimmune disease, but a condition related to hormonal changes.
Choice D is wrong because genetic mutations inherited from the client’s parents are not the primary cause of gestational diabetes.
Genetic factors may play a role in increasing the risk of developing gestational diabetes, but they are not the only factor.Other factors such as being overweight, having a family history of diabetes, or being older than 30 may also increase the risk.
Risk Factors
A nurse is conducting an assessment on a pregnant client.
Which factor increases the client's risk of developing gestational diabetes?
Explanation
The correct answer is choice A. Age younger than 30 years old is not a risk factor for gestational diabetes.According to the CDC, some of the risk factors for gestational diabetes are:
• Being overweight or obese before pregnancy
• Having a family history of diabetes
• Being older than 25 years
• Having a history of polycystic ovary syndrome (PCOS)
• Having a previous baby weighing more than 9 pounds or having gestational diabetes before
Choice B is wrong because body mass index (BMI) below 25 is considered normal and does not increase the risk of gestational diabetes.A BMI of 25 or higher is considered overweight or obese and increases the risk of gestational diabetes.
Choice C is wrong because having a previous baby weighing more than 4.5 kg (10 lb) at birth is a risk factor for gestational diabetes, not the opposite.A large baby can indicate that the mother had high blood sugar during pregnancy and can cause complications during delivery.
Choice D is wrong because having a family history of diabetes is a risk factor for gestational diabetes, not the opposite.This means that if someone in your close family has diabetes, you are more likely to develop gestational diabetes.
A client with a history of polycystic ovary syndrome (PCOS) asks the nurse about the potential impact on her pregnancy.
The nurse explains that PCOS is a risk factor for:.
Explanation
The correct answer is choice B. Gestational diabetes.Polycystic ovary syndrome (PCOS) is a condition that affects the ovaries and hormones, and is associated with increased risk of gestational diabetes mellitus (GDM), which is a type of diabetes that only pregnant women get.Women with PCOS are more likely to have insulin resistance, obesity, and metabolic syndrome, which are risk factors for GDM.GDM can cause complications for both the mother and the baby, such as preeclampsia, large for gestational age baby, cesarean delivery, low blood sugar, and breathing problems.
Choice A is wrong because PCOS is not a risk factor for gestational hypertension, which is a sudden increase in blood pressure after the 20th week of pregnancy.Gestational hypertension can lead to preeclampsia, which can affect the mother’s kidneys, liver, and brain.PCOS may increase the risk of preeclampsia, but not directly of gestational hypertension.
Choice C is wrong because PCOS is not a risk factor for preterm labor, which is the delivery of the baby before 37 weeks of pregnancy.Preterm labor can cause health problems for the baby, such as breathing difficulties, bleeding in the brain, and infections.PCOS may increase the risk of preterm delivery due to other complications, such as preeclampsia or GDM, but not directly of preterm labor.
Choice D is wrong because PCOS is not a risk factor for ectopic pregnancy, which is when the fertilized egg implants outside the uterus, usually in the fallopian tube.Ectopic pregnancy can cause severe pain and bleeding, and can be life-threatening if not treated promptly.PCOS may affect the ovulation and fertility of women, but it does not increase the risk of ectopic pregnancy.
Normal ranges for blood glucose levels during pregnancy are:
• Fasting: less than 95 mg/dL
• One hour after meal: less than 140 mg/dL
• Two hours after meal: less than 120 mg/dL
A nurse is providing education to a pregnant woman with a family history of diabetes.
The nurse explains that having a parent or sibling with diabetes increases the risk of developing:.
Explanation
The correct answer is choice B. Gestational diabetes.Having a parent or sibling with diabetes increases the risk of developing gestational diabetes mellitus (GDM), a condition that affects the way the body processes glucose during pregnancy.GDM can cause complications for both the mother and the baby, such as high blood pressure, preterm labor, macrosomia, hypoglycemia and increased risk of type 2 diabetes later in life.
Choice A is wrong because preeclampsia is not directly related to diabetes, but rather to high blood pressure and proteinuria that can occur during pregnancy.Preeclampsia can affect the placenta, kidneys, liver and brain of the mother and can lead to eclampsia, a life-threatening condition that causes seizures.
Choice C is wrong because ectopic pregnancy is not related to diabetes, but rather to a fertilized egg implanting outside the uterus, usually in the fallopian tube.
Ectopic pregnancy can cause severe bleeding and damage to the reproductive organs and can be fatal if not treated promptly.
Choice D is wrong because preterm labor is not caused by diabetes alone, but rather by a combination of factors that can trigger contractions before 37 weeks of gestation.
Some of these factors include infections, dehydration, multiple pregnancy, placental problems and stress.
A client is concerned about her increased risk of developing gestational diabetes due to her ethnic background.
The nurse explains that which ethnic origin is associated with a higher risk of gestational diabetes?
Explanation
The correct answer is choice C. Native American.According to UpToDate, Native American women have a higher risk of gestational diabetes than other ethnic groups.
Gestational diabetes is a condition that occurs when the body cannot produce enough insulin or use it effectively during pregnancy, leading to high blood sugar levels.
Choice A is wrong because Caucasian women have a lower risk of gestational diabetes than other ethnic groups.
Choice B is wrong because Hispanic women have an intermediate risk of gestational diabetes, lower than Native American but higher than Caucasian.
Choice D is wrong because Pacific Islander women have a similar risk of gestational diabetes as Hispanic women, lower than Native American but higher than Caucasian.
Normal ranges for fasting blood glucose are 60 to 99 mg/dL and for 1-hour glucose screening are less than 140 mg/dL.
Danielle’s fasting 1-hour glucose screening level of 164 mg/dL was above the normal range and indicated the need for further testing.
A nurse is reviewing the risk factors for gestational diabetes with a pregnant client.
Which factor increases the client's risk?
Explanation
The correct answer is choice A. Previous history of gestational diabetes.This is because having gestational diabetes (GDM) in a previous pregnancy increases the risk of developing it again in a subsequent pregnancy.GDM is a condition where the blood sugar (glucose) is higher than normal during pregnancy.
Choice B is wrong because normal body mass index (BMI) does not increase the risk of GDM.In fact, being overweight or obese is a risk factor for GDM.
Choice C is wrong because having a family history of diabetes is a risk factor for GDM.
This means that having relatives with diabetes increases the likelihood of developing GDM.
Choice D is wrong because being younger than 25 years old does not increase the risk of GDM.In fact, being older than 25 years old is a risk factor for GDM.
Normal ranges for blood glucose during pregnancy are 60-99 mg/dL before meals and less than 140 mg/dL one hour after meals.
Symptoms
A nurse is assessing a pregnant client who reports increased urination and excessive thirst.
These symptoms are most likely indicative of:.
Explanation
The correct answer is choice A. Gestational diabetes is a condition in which women develop high blood sugar during pregnancy.It may not cause any symptoms at first, but as it progresses, it may cause increased thirst, frequent urination, excessive sweating, fatigue and overweight.
These symptoms are most likely indicative of gestational diabetes because they are similar to the symptoms of type 2 diabetes, which is also caused by insulin resistance.
Choice B is wrong because urinary tract infection (UTI) is an infection of the urinary system that can cause pain or burning during urination, cloudy or bloody urine, fever, pelvic pain or pressure and lower back pain.
These symptoms are different from those of gestational diabetes.
Choice C is wrong because dehydration is a condition in which the body loses more water than it takes in.It can cause dry mouth, thirst, headache, dizziness, fatigue and decreased urine output.
These symptoms are not specific to gestational diabetes and can be caused by many other factors.
Choice D is wrong because preterm labor is a condition in which contractions start before the 37th week of pregnancy
A client presents to the healthcare clinic with complaints of fatigue and blurred vision during her pregnancy.
The nurse suspects these symptoms may be related to:.
Explanation
The correct answer is choice A. Gestational diabetes is a condition in which women develop high blood sugar during pregnancy.It may cause symptoms such as increased thirst, frequent urination, excessive sweating, overweight, and fatigue.Blurred vision can also be a sign of high blood sugar.
Choice B is wrong because iron deficiency anemia causes symptoms such as pale skin, weakness, shortness of breath, and fast heartbeat.
It does not cause blurred vision.
Choice C is wrong because hypertensive disorder of pregnancy causes symptoms such as high blood pressure, headache, swelling of the hands and feet, and protein in the urine.
It may cause blurred vision in severe cases, but it is not the most likely cause of the client’s symptoms.
Choice D is wrong because preterm labor causes symptoms such as regular contractions, lower back pain, pelvic pressure, and vaginal bleeding or discharge.
It does not cause blurred vision.
A nurse is providing education to a pregnant client who reports experiencing recurrent vaginal yeast infections.
The nurse explains that these infections may be associated with:.
Explanation
The correct answer is choice B.Hormonal changes during pregnancy can disrupt the normal balance of yeast and bacteria in the vagina and make it easier for yeast to grow and stick to the vaginal walls.Yeast infection during pregnancy can cause discomfort, itching, burning, and swelling in the vulva, as well as white, lumpy, and odorless discharge.
Choice A is wrong because gestational diabetes is not a direct cause of yeast infection, although it can increase the risk of getting one if the blood sugar levels are not well controlled.
Choice C is wrong because sexual activity is not a direct cause of yeast infection, although it can spread the infection from one partner to another or introduce new strains of yeast into the vagina.
Choice D is wrong because poor hygiene practices are not a direct cause of yeast infection, although they can worsen the symptoms or increase the risk of other infections.In fact, douching or using vaginal sprays can alter the vaginal pH and make yeast infection more likely.
A client presents with complaints of excessive sweating and genital itching during her pregnancy.
The nurse suspects these symptoms may be related to:.
Explanation
The correct answer is choice C. Hormonal changes during pregnancy.Hormonal changes can cause various symptoms during pregnancy, such as excessive sweating, vaginal dryness, and vaginal itching.
These symptoms are usually normal and common, but they can be uncomfortable and bothersome.
Choice A is wrong because gestational diabetes does not cause excessive sweating or genital itching.
Gestational diabetes is a type of diabetes that develops during pregnancy and affects how the body processes glucose (sugar).
Some of the symptoms of gestational diabetes are increased thirst, frequent urination, blurred vision, and fatigue.
Choice B is wrong because allergic reaction to medication does not cause excessive sweating or genital itching.
Allergic reaction to medication is a serious condition that can cause symptoms such as rash, hives, swelling, difficulty breathing, and anaphylaxis (a life-threatening reaction that affects the whole body).
Choice D is wrong because preterm labor does not cause excessive sweating or genital itching.
Preterm labor is a condition that occurs when the uterus contracts and the cervix opens before 37 weeks of pregnancy.
Some of the symptoms of preterm labor are regular contractions, lower back pain, pelvic pressure, abdominal cramps, and vaginal bleeding or discharge.
Normal ranges for excessive sweating and genital itching during pregnancy are not well-defined, as they may vary depending on individual factors such as body temperature, hygiene, clothing, and environment.
However, some general tips to cope with these symptoms are:
• Wear loose-fitting, breathable clothing made of natural fibers such as cotton
• Avoid synthetic fabrics, tight clothes, and underwear that trap heat and moisture
• Use mild soap and water to wash the genital area gently and pat it dry
• Avoid douching, perfumed products, and harsh chemicals that can irritate the skin
• Apply a moisturizer or lubricant to relieve vaginal dryness
• Use a cool compress or ice pack to soothe itching
• Keep hydrated by drinking plenty of fluids
• Consult your doctor if you have any signs of infection such as foul-smelling discharge, redness, swelling, pain, or fever
A pregnant client reports frequent episodes of urinary tract infections.
The nurse recognizes that this symptom may be associated with:.
Explanation
The correct answer is choice C.Hormonal changes during pregnancy can cause changes in the urinary tract, such as vesicoureteral reflux, which increases the risk of urinary tract infections (UTIs).UTIs are common during pregnancy and can lead to complications such as preterm labor and low birth weight if left untreated.
Choice A is wrong because gestational diabetes does not directly cause UTIs, although it may increase the risk of developing them due to high blood sugar levels.
Choice B is wrong because poor hygiene practices are not the main cause of UTIs during pregnancy, although they may contribute to the spread of bacteria from the rectum to the urethra.
Choice D is wrong because preterm labor is a possible consequence of UTIs, not a cause of them.
A nurse is screening a pregnant woman for gestational diabetes.
The nurse should ask the woman about which of the following symptoms that may indicate high blood sugar levels?
Explanation
The correct answer is choice C.Frequent urination and thirst are common symptoms of high blood sugar levels.Gestational diabetes is a condition in which women develop diabetes during pregnancy due to hormonal changes or other factors.It can affect the health of both the mother and the baby if not managed well.
Choice A is wrong because nausea and vomiting are not specific symptoms of gestational diabetes.They can occur in normal pregnancy or other conditions.
Choice B is wrong because headache and dizziness are also not specific symptoms of gestational diabetes.They can be caused by dehydration, low blood pressure, or other factors.
Choice D is wrong because abdominal pain and cramps are not typical symptoms of gestational diabetes.They can be signs of preterm labor, infection, or other problems.
Normal ranges for blood sugar levels during pregnancy are:
• Before meals: 60 to 90 mg/dL
• One hour after meals: 100 to 120 mg/dL
• Two hours after meals: 100 to 120 mg/dL
Screening and Diagnosis
A nurse is providing education to a pregnant client about the screening test for gestational diabetes.
The nurse explains that the test involves measuring blood sugar levels at different time points.
Which of the following blood sugar level readings would confirm a diagnosis of gestational diabetes?
Explanation
The correct answer is choice C. Fasting: 90 mg/dL, 1 hour: 185 mg/dL, 2 hours: 160 mg/dL.
This is because these blood sugar levels exceed the normal ranges for a pregnant woman undergoing a screening test for gestational diabetes.
The normal ranges are:
• Fasting: less than 95 mg/dL
• 1 hour: less than 180 mg/dL
• 2 hours: less than 155 mg/dL
Choice A is wrong because these blood sugar levels are within the normal ranges.
Choice B is wrong because only the fasting blood sugar level is slightly above the normal range, but not enough to confirm a diagnosis of gestational diabetes.
Choice D is wrong because only the 1 hour and 2 hours blood sugar levels are slightly above the normal ranges, but not enough to confirm a diagnosis of gestational diabetes.
A client undergoes the screening test for gestational diabetes.
The nurse reviews the client's blood sugar level results.
The fasting blood sugar level is 89 mg/dL, the 1-hour level is 178 mg/dL, and the 2-hour level is 150 mg/dL.
Based on these results, the nurse would interpret them as indicating:.
Explanation
The correct answer is choice B. Impaired glucose tolerance.
This means that the client’s blood sugar levels are higher than normal but not high enough to be diagnosed with diabetes.According to the Mayo Clinic, a normal blood glucose level two hours after drinking the glucose solution is lower than 140 mg/dL (7.8 mmol/L).
A level between 140 and 199 mg/dL (7.8 and 11 mmol/L) indicates impaired glucose tolerance, and a level of 200 mg/dL (11.1 mmol/L) or higher indicates diabetes.
Choice A is wrong because normal glucose tolerance means that the blood sugar levels are within the normal range after drinking the glucose solution.
The client’s 1-hour and 2-hour levels are above the normal range.
Choice C is wrong because gestational diabetes means that the blood sugar levels are too high during pregnancy and can cause complications for the mother and the baby.
The client’s fasting blood sugar level is within the normal range,
A nurse is preparing to perform the glucose tolerance test for a pregnant client.
Which of the following statements by the client indicates a need for further clarification?
Explanation
The correct answer is choice D.“I will be required to stay in the clinic for several hours during the test.” This statement indicates a need for further clarification because the glucose tolerance test for a pregnant client usually takes 1 hour, not several hours.The client should be informed that she will need to have blood drawn at fasting and 1 hour after drinking the sugary drink.
Choice A is wrong because it is correct that the client should not eat or drink anything after midnight before the test.
Choice B is wrong because it is correct that the client will need to have blood drawn at fasting and after drinking the sugary drink.
Choice C is wrong because it is correct that the sugary drink may taste sweet and cause some temporary discomfort.
The normal range for blood glucose level after a 1-hour glucose tolerance test is less than 140 mg/dL.A blood glucose level of 130 to 140 mg/dL is considered a positive screening and requires a 3-hour glucose tolerance test to confirm gestational diabetes mellitus.
A client is scheduled to undergo the glucose tolerance test for gestational diabetes screening.
The nurse provides instructions to the client.
Which statement by the client indicates an understanding of the procedure?
Explanation
The correct answer is choice B.“I can drink water during the test to stay hydrated.” This statement indicates an understanding of the procedure because water does not affect the blood glucose level and can help prevent dehydration during the test.
Choice A is wrong because “I should avoid any high-sugar foods for a week before the test.” This statement is incorrect because the client only needs to avoid eating or drinking anything except water for at least eight hours before the test.
Avoiding high-sugar foods for a week before the test is unnecessary and may alter the results.
Choice C is wrong because “I need to fast for 12 hours before the test.” This statement is incorrect because the client only needs to fast for eight hours before the test.
Fasting for longer than eight hours may cause hypoglycemia (low blood sugar) or ketosis (high levels of ketones in the blood).
Choice D is wrong because “I should avoid physical activity on the day of the test.” This statement is incorrect because moderate physical activity does not affect the blood glucose level and may help reduce stress during the test.
However, strenuous exercise should be avoided as it may lower the blood glucose level too much.
Normal ranges for blood glucose levels during the glucose tolerance test are:
• Fasting: less than 5.3 mmol/L (95 mg/dL)
• One hour: less than 10.0 mmol/L (180 mg/dL)
• Two hours: less than 8.6 mmol/L (155 mg/dL)
A pregnant client has just completed the glucose tolerance test for gestational diabetes.
The nurse reviews the client's blood sugar level results.
The fasting blood sugar level was 95 mg/dL, the 1-hour level was 175 mg/dL, and the 2-hour level was 145 mg/dL.
Based on these results, the nurse would interpret them as indicating:.
Explanation
The correct answer is choice B. Impaired glucose tolerance.This means that the blood sugar levels are higher than normal, but not high enough to diagnose gestational diabetes.The normal ranges for the glucose tolerance test for gestational diabetes are:
• Fasting blood sugar level: less than 95 mg/dL (5.3 mmol/L)
• 1-hour level: less than 180 mg/dL (10 mmol/L)
• 2-hour level: less than 155 mg/dL (8.6 mmol/L)
The client’s fasting blood sugar level was within the normal range, but the 1-hour and 2-hour levels were above the normal range, indicating impaired glucose tolerance.
Choice A is wrong because normal glucose tolerance means that the blood sugar levels are within the normal range for all three measurements.
Choice C is wrong because gestational diabetes means that the blood sugar levels are above the diagnostic threshold for all three measurements:
• Fasting blood sugar level: 92 mg/dL (5.1 mmol/L) or higher
• 1-hour level: 180 mg/dL (10 mmol/L) or higher
• 2-hour level: 153 mg/dL (8.5 mmol/L) or higher
Choice D is wrong because pre-existing diabetes means that the blood sugar levels are above the diagnostic threshold for diabetes before pregnancy:
• Fasting blood sugar level: 126 mg/dL (7 mmol/L) or higher
• Random blood sugar level: 200 mg/dL (11.1 mmol/L) or higher
A nurse is reviewing the antenatal care plan for a pregnant woman who has no risk factors for gestational diabetes.
The nurse should expect the woman to have which of the following tests to screen for gestational diabetes?
Explanation
The correct answer is choice C. Glucose tolerance test at 24 to 28 weeks of gestation.This is the recommended screening test for gestational diabetes mellitus (GDM) for women who have no risk factors.
The test involves measuring the blood glucose level one hour after ingesting a 50-gram glucose load.If the result is abnormal (greater than 140 mg/dL), a diagnostic three-hour oral glucose tolerance test (OGTT) is performed.
Choice A is wrong because fasting blood glucose test is not a screening test for GDM, but a diagnostic test that requires an overnight fast and measures the blood glucose level before eating.
It is usually done as part of the OGTT.
Choice B is wrong because random blood glucose test is not a reliable screening test for GDM, as it does not account for the timing and content of the last meal.
Choice D is wrong because hemoglobin A1c test is not a screening test for GDM, but a test that measures the average blood glucose level over the past two to three months.It is used to monitor the glycemic control of women with preexisting diabetes mellitus during pregnancy.
Complications
A nurse is providing education to a pregnant client with gestational diabetes.
The nurse explains that if the baby develops low blood sugar after birth due to excess insulin production, it can lead to which of the following complications if left untreated?
Explanation
The correct answer is choice B. Jaundice.
Jaundice is a condition where the skin and whites of the eyes turn yellow due to excess bilirubin in the blood.
Bilirubin is a byproduct of red blood cell breakdown.If the baby develops low blood sugar after birth due to excess insulin production, it can lead to increased red blood cell breakdown and jaundice.
Choice A is wrong because respiratory distress syndrome (RDS) is a condition where the baby has difficulty breathing due to immature lungs and lack of surfactant.RDS is more common in preterm babies and babies of diabetic mothers, but it is not caused by low blood sugar.
Choice C is wrong because preterm birth is a birth that occurs before 37 weeks of gestation.Preterm birth can be caused by many factors, such as infection, placental abruption, or multiple gestation, but it is not a complication of low blood sugar after birth.
Choice D is wrong because preeclampsia is a condition where the mother develops high blood pressure and proteinuria after 20 weeks of gestation.Preeclampsia can affect the placenta and the baby’s growth, but it is not a complication of low blood sugar after birth.
Normal ranges for blood sugar in newborns are 40 to 80 mg/dL (2.2 to 4.4 mmol/L).Normal ranges for bilirubin in newborns are 1 to 12 mg/dL (17 to 205 µmol/L).
A client with gestational diabetes asks the nurse about the risk of the baby growing larger than usual.
The nurse explains that this condition is known as macrosomia and it can result in which of the following difficulties during delivery?
Explanation
The correct answer is
B. Need for induced labor or cesarean section.
Gestational diabetes mellitus (GDM) is a condition where the mother has high blood sugar levels during pregnancy.
This can affect the growth and development of the baby.
One of the possible complications of GDM is fetal macrosomia, which means the baby is larger than normal for its gestational age.Macrosomia is usually defined as a birth weight above 4000 to 4500 grams (or 9 to 10 pounds).
Macrosomia can cause difficulties during delivery, such as shoulder dystocia, which is when the baby’s shoulder gets stuck behind the mother’s pelvic bone.This can lead to injuries to the baby’s nerves, bones, or muscles, or to the mother’s vagina, uterus, or bladder.To prevent these complications, doctors may recommend inducing labor or performing a cesarean section (C-section) to deliver the baby safely.
The other statements are wrong because:
A. Increased risk of jaundice.
Jaundice is a condition where the baby’s skin and eyes turn yellow due to high levels of bilirubin in the blood.
Bilirubin is a waste product that is normally removed by the liver.Jaundice can occur in any newborn, but it is more common in babies with GDM because they may have polycythemia (too many red blood cells) or hypoglycemia (low blood sugar levels) that can affect the liver function.
However, jaundice is not directly related to macrosomia and does not cause difficulties during delivery.
•
C. Development of preeclampsia.
Preeclampsia is a serious condition where the mother develops high blood pressure and protein in the urine after 20 weeks of pregnancy.
Preeclampsia can cause complications such as seizures, stroke, organ damage, or placental abruption (when the placenta separates from the uterus before delivery).Preeclampsia can increase the risk of fetal growth restriction (when the baby does not grow well in the womb), not macrosomia.
Preeclampsia can also cause difficulties during delivery, but it is not a result of macrosomia.
D. Higher risk of stillbirth.
Stillbirth is when the baby dies in the womb after 20 weeks of pregnancy.
Stillbirth can occur due to various causes, such as infections, genetic abnormalities, placental problems, or umbilical cord accidents.Stillbirth can also occur in babies with GDM because they may have hypoxia (low oxygen levels) or acidosis (high acid levels) in the blood due to poor placental function or uncontrolled blood sugar levels.
However, stillbirth is not directly related to macrosomia and does not cause difficulties during delivery.
A nurse is assessing a newborn for signs of hypoglycemia.
Which of the following blood glucose levels, taken 1 to 2 hours after birth, would indicate hypoglycemia in the newborn?
Explanation
The correct answer is choice D. 20 mg/dL.This is because a blood glucose level below 40 mg/dL is considered hypoglycemia in a newborn.Hypoglycemia can cause neurological damage and other complications in newborns.
Choice A.40 mg/dL is wrong because this is the lower limit of normal blood glucose level for a newborn.
Choice B.35 mg/dL is wrong because this is slightly below the normal range but not low enough to be hypoglycemic.
Choice C.30 mg/dL is wrong because this is also below the normal range but not as low as choice D. Normal blood glucose levels for newborns are between 40 and 150 mg/dL, depending on the time of measurement and the feeding status.Blood glucose levels are usually lowest 1 to 2 hours after birth and then gradually increase over the next few days.
A client with gestational diabetes asks the nurse about the risk of developing type 2 diabetes later in life.
The nurse explains that both the mother and the baby have an increased risk.
This is primarily due to:.
Explanation
The correct answer is choice D. Genetic factors.This is because having gestational diabetes increases the risk of developing type 2 diabetes later in life for both the mother and the baby, and this risk is influenced by genetic factors.
Some possible explanations for the other choices are:
• Choice A is wrong because the baby’s excessive insulin production is a result of high blood sugar levels in the mother, not a cause of gestational diabetes.
• Choice B is wrong because poor placental function is not a primary cause of gestational diabetes, although it may be affected by high blood sugar levels in the mother.
• Choice C is wrong because uncontrolled blood sugar levels during pregnancy are a consequence of gestational diabetes, not a primary cause of it.
A nurse is providing education to a pregnant client with gestational diabetes about the risk of preeclampsia.
The nurse explains that preeclampsia can lead to which of the following complications if left untreated?
Explanation
The correct answer is choice B. Increased risk of stillbirth.Preeclampsia is a condition that develops in pregnant women, marked by high blood pressure and presence of proteins in urine that indicate kidney damage.If left untreated, preeclampsia can lead to serious complications for both the mother and the baby.
Choice A is wrong because low blood sugar in the baby is not a direct complication of preeclampsia.Low blood sugar can occur in babies whose mothers have diabetes, but it can be prevented by proper management of blood glucose levels during pregnancy.
Choice C is wrong because brain damage due to jaundice is not a direct complication of preeclampsia.
Jaundice is a condition where the baby’s skin and eyes turn yellow due to high levels of bilirubin, a waste product of red blood cells.Jaundice can occur in babies whose mothers have liver problems, but it can be treated by phototherapy or blood transfusion.
Choice D is wrong because respiratory distress syndrome in the baby is not a direct complication of preeclampsia.
Respiratory distress syndrome is a condition where the baby’s lungs are not fully developed and cannot provide enough oxygen to the body.Respiratory distress syndrome can occur in premature babies, but it can be prevented by giving corticosteroids to the mother before delivery to help mature the baby’s lungs.
Normal ranges for blood pressure are 120/80 mmHg or lower for systolic (top number) and diastolic (bottom number) respectively.Normal ranges for protein in urine are less than 150 mg per day or less than 30 mg per liter.
Treatment
A client with gestational diabetes asks the nurse about the preferred medication for controlling blood sugar levels.
The nurse explains that the preferred medication is chosen because it does not cross the placenta and affect the baby.
Which medication is the nurse referring to?
Explanation
The correct answer is choice A. Insulin injections.Insulin is the preferred medication for controlling blood sugar levels in gestational diabetes because it does not cross the placenta and affect the baby.Insulin lowers blood glucose by stimulating glucose uptake in muscle and fat cells and inhibiting glucose production in the liver.
Choice B.Metformin is wrong because metformin is an oral antidiabetic drug that can cross the placenta and may have unknown effects on the baby.Metformin works by decreasing glucose production in the liver and increasing insulin sensitivity in muscle and fat cells.
Choice C.Glyburide is wrong because glyburide is another oral antidiabetic drug that can cross the placenta and may cause hypoglycemia or other adverse effects in the baby.Glyburide works by stimulating insulin secretion from the pancreas and increasing insulin sensitivity in peripheral tissues.
Choice D.Oral corticosteroids are wrong because oral corticosteroids are not used to treat gestational diabetes, but rather to accelerate fetal lung maturation in preterm labor.Oral corticosteroids can actually increase blood glucose levels by stimulating gluconeogenesis and decreasing insulin sensitivity.
A nurse is teaching a client with gestational diabetes about the importance of regular antenatal visits.
Which of the following is a primary reason for these visits?
Explanation
The correct answer is choice A. To monitor the progress of pregnancy and check for any complications.This is the primary reason for regular antenatal visits for women with gestational diabetes, as they are at increased risk of developing hypertension, preeclampsia, polyhydramnios, and fetal macrosomia.These visits also allow the health care provider to monitor the blood glucose levels and adjust the treatment plan accordingly.
Choice B is wrong because insulin injections are not always required for women with gestational diabetes.Some women can manage their blood sugar levels with dietary modifications and exercise alone.
Choice C is wrong because ultrasound scans are not the primary reason for antenatal visits, although they may be performed more frequently for women with gestational diabetes to assess the fetal growth and well-being.
Choice D is wrong because education on dietary modifications during pregnancy is not the primary reason for antenatal visits, although it is an important component of the management of gestational diabetes.Women with gestational diabetes should receive individualized nutrition counseling from a registered dietitian or a certified diabetes educator.
A client with gestational diabetes asks the nurse about the role of exercise in managing blood sugar levels.
The nurse explains that exercise can help lower blood sugar levels and improve insulin sensitivity.
How many minutes of moderate physical activity per day is recommended for this client, unless advised otherwise by a healthcare provider?
Explanation
The correct answer is choice C. 30 minutes.According to the CDC, the American Diabetes Association, and other sources, exercise can help lower blood sugar levels and improve insulin sensitivity for women with gestational diabetes.
It is recommended that they get at least30 minutesof moderate-intensity physical activity at leastfive days a week, unless advised otherwise by a healthcare provider.
Choice A is wrong because 10 minutes of exercise per day is too low to have a significant effect on blood sugar levels and insulin sensitivity.
Choice B is wrong because 20 minutes of exercise per day is also below the recommended amount for women with gestational diabetes.
Choice D is wrong because 60 minutes of exercise per day may be too much for some women with gestational diabetes, especially if they have other complications or risk factors.
They should consult their healthcare provider before engaging in such a high level of physical activity.
Normal ranges for blood sugar levels during pregnancy are:
• Fasting: less than 95 mg/dL
• One hour after a meal: less than 140 mg/dL
• Two hours after a meal: less than 120 mg/dL
A nurse is discussing the use of medication for gestational diabetes with a client.
Which statement accurately describes the use of oral antidiabetic drugs such as metformin or glyburide?
Explanation
The correct answer is choice C. They are used in cases where diet and exercise are not sufficient to control blood sugar levels.According to a study by Langer et al, oral antidiabetic drugs such as glyburide and metformin are equivalent to insulin in terms of pregnancy outcomes in gestational diabetes mellitus (GDM).These drugs can help lower blood sugar levels by stimulating the release of insulin from the pancreas, limiting the liver’s production of glucose, or improving the cells’ sensitivity to insulin.
Choice A is wrong because they are not the first-line treatment option for gestational diabetes.The first-line treatment is diet and exercise, which can help control blood sugar levels in most cases of GDM.
Choice B is wrong because they are not necessarily contraindicated during pregnancy.Although there are some potential risks to the baby, such as hypoglycemia or fetal growth restriction, these can be minimized by careful monitoring and dose adjustment.
Choice D is wrong because they are not preferred over insulin injections for their ease of use and convenience.Insulin injections are still the gold standard for treating GDM, especially in cases of severe hyperglycemia or when oral drugs fail to achieve adequate glycemic control.Insulin injections also have fewer side effects and interactions than oral drugs.
A nurse is providing dietary education to a pregnant woman who has gestational diabetes.
The nurse should advise the woman to consume how many calories per day during the third trimester of pregnancy?
Explanation
The correct answer is choice D. 2400 calories.A pregnant woman with gestational diabetes should consume about 2400 calories per day during the third trimester of pregnancy.This is based on the average energy requirement for a pregnant woman, which is about 2200 calories per day plus 200 calories for the baby’s growth.
A woman who is overweight before pregnancy may need fewer calories than this.
Choice A. 1800 calories is wrong because it is too low for a pregnant woman with gestational diabetes.Eating too few calories can cause ketones to build up in the blood, which can harm the baby.
Choice B. 2000 calories is wrong because it is also too low for a pregnant woman with gestational diabetes.It may not provide enough energy and nutrients for the mother and the baby.
Choice C. 2200 calories is wrong because it is the average energy requirement for a pregnant woman without gestational diabetes.A woman with gestational diabetes needs an extra 200 calories per day to support the baby’s growth and development.
A nurse is teaching a pregnant woman who has gestational diabetes about the benefits of exercise during pregnancy.
The nurse should explain that exercise can help the woman by doing which of the following?
Explanation
The correct answer is choice D.Exercise can help the woman by enhancing her insulin sensitivity and glucose utilization.
This means that her body can use the glucose in her blood more efficiently and lower her blood sugar levels.Exercise can also help prevent excess weight gain, which is a risk factor for gestational diabetes.
Choice A is wrong because exercise does not increase appetite and caloric intake, but rather helps regulate them.
Choice B is wrong because exercise does not lower blood pressure and heart rate, but rather increases them temporarily during physical activity.Choice C is wrong because exercise does not reduce the risk of preterm labor and delivery, but rather may increase it if done excessively or without proper supervision.
Nursing Interventions
A nurse is teaching a pregnant woman about gestational diabetes screening.
Which statement indicates understanding?
Explanation
The correct answer is choice A.“I should have the oral glucose tolerance test between 24 and 28 weeks of gestation.” This statement indicates understanding because it reflects the current recommendation for gestational diabetes screening for all pregnant women.The oral glucose tolerance test (OGTT) measures how the body handles glucose after a glucose load and can detect impaired glucose tolerance or diabetes.
Choice B is wrong because the woman does not need to eat a high-carbohydrate meal before the screening test.In fact, she should fast for at least 8 hours before the test.
Choice C is wrong because the screening process is necessary even if the woman has no family history of diabetes.Gestational diabetes can occur in any pregnant woman, especially if she has risk factors such as obesity, advanced maternal age, previous history of gestational diabetes, or a history of polycystic ovary syndrome.
Choice D is wrong because the screening test should not be done at any time during the pregnancy.The optimal time for screening is between 24 and 28 weeks of gestation, when insulin resistance peaks due to placental hormones.If the test is done too early or too late, it may miss some cases of gestational diabetes or give false-positive results.
A nurse is developing a meal plan for a pregnant woman with gestational diabetes.
Which instruction should the nurse include?
Explanation
The correct answer is choice A.“Consume regular meals and snacks to maintain stable blood glucose levels.” This is because eating at regular intervals helps prevent blood sugar spikes and drops, which can be harmful for both the mother and the baby.A healthy diet for gestational diabetes should include a variety of foods from different food groups, such as fruits, vegetables, whole grains, lean proteins, and low-fat dairy products.
Choice B is wrong because “Avoid fruits and vegetables to minimize carbohydrate intake.” Fruits and vegetables are rich in vitamins, minerals, antioxidants, and fiber, which are beneficial for both the mother and the baby.Carbohydrates are not bad for gestational diabetes, as long as they are complex carbohydrates that are digested slowly and do not cause rapid blood sugar spikes.Examples of complex carbohydrates are whole wheat bread, brown rice, oats, quinoa, beans, and lentils.
Choice C is wrong because “Focus on consuming high-fat foods to meet nutritional needs.” High-fat foods can increase the risk of weight gain, high cholesterol, high blood pressure, and heart disease, which can complicate gestational diabetes.
Moreover, not all fats are healthy.Saturated fats and trans fats should be avoided or limited, as they can raise bad cholesterol levels and increase inflammation.Examples of saturated fats are butter, cheese, cream, fatty meats, and coconut oil.Examples of trans fats are margarine, shortening, baked goods, fried foods, and processed snacks.Healthy fats are unsaturated fats that can lower bad cholesterol levels and provide essential fatty acids.
Examples of unsaturated fats
A nurse is educating a pregnant woman with gestational diabetes about physical activity.
Which statement by the client indicates understanding?
Explanation
The correct answer is choice A.“I should engage in moderate-intensity exercises like walking or swimming.” This statement indicates that the client understands the benefits of physical activity for gestational diabetes, such as improving glucose metabolism, reducing insulin resistance, and preventing excessive weight gain.Moderate-intensity exercises are recommended for pregnant women with gestational diabetes, as long as they are medically cleared and have no contraindications.
Choice B is wrong because physical activity does not cause complications for gestational diabetes, but rather helps to prevent them.Avoiding physical activity can lead to poor glycemic control, increased risk of hypertension, preeclampsia, and cesarean delivery.
Choice C is wrong because exercise should be done throughout pregnancy, not only in the third trimester.Starting exercise early in pregnancy can help to prevent or delay the onset of gestational diabetes, and continuing exercise until delivery can help to maintain glucose levels and prevent fetal macrosomia.
Choice D is wrong because high-intensity exercises are not recommended for pregnant women with gestational diabetes, as they can cause hypoglycemia, dehydration, and fetal distress.High-intensity exercises can also increase the production of stress hormones, which can impair glucose metabolism and increase insulin resistance.
A nurse is teaching a pregnant woman with gestational diabetes about blood glucose monitoring.
Which instruction should the nurse provide?
Explanation
The correct answer is choice A. “Perform self-monitoring of blood glucose using a glucometer.” This instruction will help the pregnant woman with gestational diabetes to monitor her blood glucose levels and adjust her insulin dosage accordingly.Self-monitoring of blood glucose is recommended at least four times a day for women with gestational diabetes.
Choice B is wrong because “Check blood glucose levels once a week.” is not frequent enough to ensure adequate glycemic control.Women with gestational diabetes need to check their blood glucose levels daily or more often.
Choice C is wrong because “Maintaining blood glucose levels within the recommended range is not necessary.” is false and dangerous.Maintaining blood glucose levels within the recommended range is essential to prevent maternal and fetal complications such as macrosomia, hypoglycemia, congenital anomalies, and preeclampsia.
Choice D is wrong because “Ignore symptoms of hypoglycemia and hyperglycemia.” is also false and dangerous.
Symptoms of hypoglycemia and hyperglycemia should not be ignored, but reported to the health care provider and treated promptly.
Hypoglycemia can cause maternal seizures, coma, and death.Hyperglycemia can cause fetal distress, stillbirth, and neonatal death.
The normal range for fasting blood glucose in pregnancy is 60 to 95 mg/dL.The normal range for postprandial blood glucose in pregnancy is 100 to 129 mg/dL.
A nurse is providing education to a pregnant woman who may require insulin therapy for gestational diabetes.
Which information should the nurse include?
Explanation
The correct answer is choice A. Insulin administration may be necessary if dietary modifications and physical activity alone are insufficient.
This is because gestational diabetes mellitus (GDM) is a condition that affects the way the body uses glucose during pregnancy, and it can cause high blood sugar levels that can affect the health of both the mother and the baby.Insulin is a hormone that helps the body use glucose for energy, and some women with GDM may need to take insulin injections to keep their blood sugar levels within normal range.
Choice B is wrong because skipping insulin doses can lead to dangerously high blood sugar levels that can cause complications such as ketoacidosis, fetal distress, preterm labor, or stillbirth.
Women with GDM should follow their prescribed insulin regimen and monitor their blood sugar levels regularly.
Choice C is wrong because insulin therapy is not the first-line treatment for GDM.The first-line treatment for GDM is lifestyle changes such as eating a balanced diet, limiting carbohydrates and sweets, increasing fiber intake, and exercising moderately for at least 30 minutes a day.
These measures can help lower blood sugar levels and reduce the need for insulin therapy.
However, if lifestyle changes are not enough to control blood sugar levels, insulin therapy may be added as a second-line treatment.
Choice D is wrong because insulin cannot be administered at any time during the day.
Insulin therapy for GDM requires careful timing and dosing to match the blood sugar patterns and needs of each woman.Insulin therapy for GDM usually involves a combination of short-acting and intermediate-acting insulin that are given before meals and at bedtime.
The timing and dosage of insulin depend on factors such as the woman’s weight, blood sugar levels, diet, activity level, and fetal growth.
Women with GDM should consult their health care provider or diabetes educator about their individualized insulin regimen.
A nurse is screening a pregnant woman for gestational diabetes using an oral glucose tolerance test (OGTT).
The nurse should instruct the woman to do which of the following before the test?
Explanation
The correct answer is choice B. Drink water only for 8 hours before the test.This is because the oral glucose tolerance test (OGTT) requires fasting for about 8 hours before the test to get accurate results.
The woman should not eat or drink anything except water during this time.
Choice A is wrong because eating a high-carbohydrate meal the night before can raise the blood glucose level and affect the test results.
Choice C is wrong because caffeine and smoking can also affect the blood glucose level and interfere with the test results.
Choice D is wrong because some medications can alter the blood glucose level and cause false-positive or false-negative results.The woman should consult her doctor about taking her usual medications before the test.
Normal ranges for OGTT vary depending on the laboratory and the type of glucose solution used.Generally, a normal fasting blood glucose level is less than 100 mg/dL, a normal 1-hour level is less than 180 mg/dL, a normal 2-hour level is less than 155 mg/dL, and a normal 3-hour level is less than 140 mg/dL.
More questions on this topic
In gestational diabetes, the condition primarily affects the?
Explanation
The correct answer is choice C. Pancreas.Gestational diabetes is a type of diabetes that develops during pregnancy and affects how the cells use sugar (glucose).Glucose is the main source of energy for the body and it is regulated by a hormone called insulin, which is produced by the pancreas.
In gestational diabetes, the placenta (the organ that connects the baby to the mother) produces hormones that can make insulin less effective, leading to high blood sugar levels.This condition is called insulin resistance
Choice A is wrong because the lungs are not directly involved in glucose metabolism or insulin production.
Choice B is wrong because the kidneys are not the primary site of insulin production, although they can be affected by high blood sugar levels over time.
Choice D is wrong because the liver is not the main source of insulin, although it can help regulate blood sugar levels by storing and releasing glucose as needed.
Gestational diabetes usually does not cause any symptoms, but it can increase the risk of complications for both the mother and the baby, such as high blood pressure, pre-eclampsia, large birth weight, premature delivery, low blood sugar, and future diabetesTherefore, it is important to screen for gestational diabetes during pregnancy and manage it with a healthy diet, exercise, and medication if needed
The primary risk factor for gestational diabetes is?
Explanation
The correct answer is choice D. Previous history of gestational diabetes.This is because having gestational diabetes in a previous pregnancy increases the risk of developing it again in a subsequent pregnancy.According to the CDC, about 50% of women with gestational diabetes go on to develop type 2 diabetes later in life.
Choice A is wrong because advanced maternal age is not a primary risk factor for gestational diabetes, although it may increase the risk slightly.
Choice B is wrong because family history of diabetes is not a primary risk factor for gestational diabetes, although it may indicate a genetic predisposition to insulin resistance.
Choice C is wrong because smoking during pregnancy is not a primary risk factor for gestational diabetes, although it may have other adverse effects on the mother and the baby.
Some of the other risk factors for gestational diabetes include obesity, hormonal changes, polycystic ovary syndrome, and pregnancy over 30 years of age.Gestational diabetes can cause complications such as high blood pressure, preeclampsia, large birth weight, premature delivery, respiratory distress syndrome, and low blood sugar in the baby.Gestational diabetes can be managed with a healthy diet, exercise, and medication if needed.
Gestational diabetes is most likely to develop during which trimester of pregnancy?
Explanation
The correct answer is choice B. Second trimester.
Gestational diabetes is high blood sugar that develops during pregnancy and usually disappears after giving birth.It can happen at any stage of pregnancy, but is more common in the second or third trimester.This is because hormonal changes that occur during pregnancy can affect the body’s ability to produce enough insulin, a hormone that helps control blood sugar levels.
Choice A is wrong because gestational diabetes is less likely to develop during the first trimester, when the hormonal changes are not as significant.
Choice C is wrong because gestational diabetes is usually diagnosed and treated before the third trimester, to prevent complications for the mother and the baby.
Choice D is wrong because gestational diabetes is not a postpartum condition, although some women may have a higher risk of developing type 2 diabetes later in life if they had gestational diabetes.
Normal ranges for blood sugar levels during pregnancy are:
• Before meals: 60 to 95 mg/dL
• One hour after meals: 100 to 129 mg/dL
• Two hours after meals: 70 to 119 mg/dL
Gestational diabetes increases the risk of which of the following complications during pregnancy?
Explanation
The correct answer is choice B. Preeclampsia.Gestational diabetes increases the risk of high blood pressure and preeclampsia, a serious complication of pregnancy that causes high blood pressure and other symptoms that can threaten both the mother’s and the baby’s life.
Choice A is wrong because preterm labor is not directly caused by gestational diabetes, although it may be done to prevent complications from preeclampsia or a large baby.
Choice C is wrong because ectopic pregnancy is not related to gestational diabetes.Ectopic pregnancy occurs when the fertilized egg implants outside the uterus, usually in the fallopian tube.
Choice D is wrong because placenta previa is not associated with gestational diabetes.Placenta previa occurs when the placenta covers part or all of the opening of the cervix.
The long-term implications of gestational diabetes primarily include an increased risk of developing
Explanation
The correct answer is
C. Type 2 diabetes.
Gestational diabetes (GDM) is a condition where the blood sugar levels are higher than normal during pregnancy.It usually goes away after giving birth, but it can increase the risk of developing type 2 diabetes later in life.
Type 2 diabetes is a chronic condition that affects how the body uses glucose (sugar) for energy.It can cause serious complications such as heart disease, kidney damage, nerve damage, eye problems and more.
A. Hypothyroidism is a condition where the thyroid gland does not produce enough thyroid hormones, which regulate the metabolism and other body functions.
It can cause symptoms such as fatigue, weight gain, depression, dry skin and hair loss.Hypothyroidism is not directly linked to gestational diabetes, but it can affect pregnancy outcomes and increase the risk of miscarriage, preterm birth and low birth weight.
B. Asthma is a condition where the airways become inflamed and narrow, making it hard to breathe.
It can cause symptoms such as wheezing, coughing, chest tightness and shortness of breath.Asthma is not directly linked to gestational diabetes, but it can affect pregnancy outcomes and increase the risk of preterm birth, low birth weight and preeclampsia.
D. Breast cancer is a type of cancer that starts in the breast tissue.
It can cause symptoms such as a lump in the breast, nipple discharge, skin changes and pain.Breast cancer is not directly linked to gestational diabetes, but it can be influenced by hormonal factors such as estrogen and progesterone levels, which may change during pregnancy and after menopause.
A nurse is reviewing the laboratory results of a pregnant woman who has gestational diabetes.
The nurse expects to find which of the following findings?
Explanation
The correct answer is
A. Elevated fasting blood glucose levels.
Gestational diabetes (GDM) is a condition where the blood sugar levels are higher than normal during pregnancy.
It can affect the health of the mother and the baby if not well controlled.GDM usually goes away after delivery, but it can increase the risk of developing type 2 diabetes later in life.
A. Elevated fasting blood glucose levels.
This statement is true.
Fasting blood glucose levels are the levels of glucose in the blood after not eating or drinking anything except water for at least 8 hours.
Normal fasting blood glucose levels are between 70 and 100 mg/dL (3.9 and 5.6 mmol/L).
In GDM, the fasting blood glucose levels are higher than normal, usually above 95 mg/dL (5.3 mmol/L).This indicates that the body is not able to use insulin effectively to lower the blood sugar levels.
B. Decreased postprandial blood glucose levels.
This statement is false.
Postprandial blood glucose levels are the levels of glucose in the blood after eating a meal or a snack.
Normal postprandial blood glucose levels are below 140 mg/dL (7.8 mmol/L) within 2 hours of eating.
In GDM, the postprandial blood glucose levels are higher than normal, usually above 140 mg/dL (7.8 mmol/L) within 1 hour or above 120 mg/dL (6.7 mmol/L) within 2 hours of eating.This indicates that the body is not able to use insulin effectively to lower the blood sugar levels after a meal.
C. Elevated serum insulin levels.
This statement is false.
Serum insulin levels are the levels of insulin in the blood.
Insulin is a hormone that helps the cells to take up glucose from the blood for energy or storage.
Normal serum insulin levels vary depending on the time of day, the type of food eaten, and other factors.
In GDM, the serum insulin levels are not necessarily elevated, but they may be insufficient to overcome the insulin resistance caused by hormonal changes during pregnancy.Insulin resistance is a condition where the cells do not respond well to insulin and require more insulin to lower the blood sugar levels.
D. Decreased glycosylated hemoglobin levels.
This statement is false.
Glycosylated hemoglobin (HbA1c) is a measure of how much glucose is attached to hemoglobin, a protein in red blood cells that carries oxygen.
HbA1c reflects the average blood sugar levels over the past 2 to 3 months.
Normal HbA1c levels are below 5.7%.
In GDM, the HbA1c levels are not necessarily decreased, but they may be within or slightly above the normal range, depending on how well the blood sugar levels are controlled during pregnancy.HbA1c is not a reliable test for diagnosing GDM, as it may not reflect the recent changes in blood sugar levels caused by pregnancy.
A nurse is explaining the role of insulin in glucose metabolism to a pregnant woman who has gestational diabetes.
The nurse should tell the woman that insulin is a hormone that does which of the following?
Explanation
The correct answer is
C. It transports glucose from the bloodstream into the cells for energy production.
Insulin is a hormone that regulates the metabolism of carbohydrates, fats, and proteins.It promotes the absorption of glucose from the blood into cells, where it can be used for energy or stored as glycogen or fat.It also inhibits glucose production and secretion by the liver and stimulates lipogenesis and protein synthesis.Insulin is essential for cell metabolism and low insulin levels can cause catabolism of body fat.
A. It converts glucose into glycogen for storage in the liver and muscles.
This statement is partially true, but not the main role of insulin.
Insulin does stimulate the formation of glycogen from glucose in the liver and muscles, but this is not its primary function.Glycogen is a form of stored glucose that can be mobilized when blood glucose levels are low.Insulin also inhibits the breakdown of glycogen (glycogenolysis) and the synthesis of glucose from amino acids and fatty acids (gluconeogenesis) in the liver.
B. It breaks down glucose into carbon dioxide and water for excretion in the urine and lungs.
This statement is false.
Insulin does not break down glucose, but rather facilitates its uptake by cells.
Glucose is broken down by a process called glycolysis, which produces pyruvate and ATP (energy).
Pyruvate can then enter the Krebs cycle and the electron transport chain to produce more ATP, carbon dioxide and water.Carbon dioxide is exhaled by the lungs and water is excreted by the kidneys.
Insulin has no direct role in these processes.
D. It stimulates glucose synthesis from amino acids and fatty acids in the liver.
This statement is false.
Insulin does not stimulate glucose synthesis, but rather inhibits it.
Glucose synthesis from non-carbohydrate sources, such as amino acids and fatty acids, is called gluconeogenesis.
This process occurs mainly in the liver and is stimulated by glucagon, a hormone that opposes insulin.Gluconeogenesis helps to maintain blood glucose levels when dietary intake or glycogen stores are low.Insulin suppresses gluconeogenesis by inhibiting the enzymes involved in this pathway.
A nurse is assessing a pregnant woman who has gestational diabetes for possible complications.
The nurse should monitor the woman for which of the following signs and symptoms?
Explanation
The correct answer is
A. Polyuria, polydipsia, and polyphagia.
These are the classic signs and symptoms of diabetes, which occur due to high blood sugar levels.Gestational diabetes is a type of diabetes that develops during pregnancy and can affect the health of the mother and the baby.
B. Hypotension, bradycardia, and bradypnea.
Statement is wrong because these are signs of low blood pressure, low heart rate, and low breathing rate, which are not related to gestational diabetes.
C. Nausea, vomiting, and abdominal pain.
Statement is wrong because these are signs of ketoacidosis, a serious complication of diabetes that occurs when the body breaks down fat for energy and produces ketones.Ketoacidosis is rare in gestational diabetes and usually affects people with type 1 diabetes.
D. Headache, blurred vision, and drowsiness.
Statement is wrong because these are signs of hyperglycemia (high blood sugar) or hypertensive disorders (high blood pressure), which can occur in gestational diabetes but are not specific to it.They can also be caused by other conditions such as dehydration, infection, or preeclampsia.
Normal ranges for blood sugar levels during pregnancy are:
• Before meals: 3.5 to 5.9 mmol/L (63 to 106 mg/dL)
• One hour after meals: 7.8 mmol/L (140 mg/dL) or less
• Two hours after meals: 6.4 mmol/L (115 mg/dL) or less
A nurse is providing dietary education to a pregnant woman who has gestational diabetes.
Which of the following instructions should the nurse include?
Explanation
The correct answer is choice C. Choose foods that are high in fiber and low in fat.
This instruction will help the client control blood glucose levels and prevent constipation, which is common in pregnancy.
Foods high in fiber include fruits, vegetables, whole grains, beans, nuts, and seeds.
Foods low in fat include lean meats, poultry, fish, low-fat dairy products, and vegetable oils.
Choice A is wrong because eating three large meals per day with snacks in between can cause spikes and drops in blood glucose levels.
The client should eat smaller, more frequent meals throughout the day to maintain a steady blood glucose level.
Choice B is wrong because limiting carbohydrate intake to less than 40% of total calories can lead to ketosis, which is harmful for the fetus.
The client should consume about 45% to 65% of total calories from carbohydrates, preferably from complex sources such as whole grains, fruits, and vegetables.
Choice D is wrong because avoiding foods that contain artificial sweeteners is not necessary for gestational diabetes.
Artificial sweeteners do not affect blood glucose levels and can be used in moderation as part of a balanced diet.
However, the client should limit foods and beverages that are high in sugar and calories, such as soda, candy, cake, and ice cream.
A nurse is preparing to administer insulin to a pregnant woman who has gestational diabetes.
Which of the following types of insulin should the nurse use?
Explanation
The correct answer is choice D. Lispro insulin.
Lispro insulin is a rapid-acting insulin that can be injected 15 minutes before a meal to lower blood sugar.It is safe and effective for pregnant women with gestational diabetes.
Choice A is wrong because regular insulin is a short-acting insulin that needs to be injected 30 minutes before a meal.It may not provide enough control over blood sugar levels during pregnancy.
Choice B is wrong because NPH insulin is an intermediate-acting insulin that has a peak effect several hours after injection.It may cause low blood sugar (hypoglycemia) or high blood sugar (hyperglycemia) if not timed correctly with meals and snacks.
Choice C is wrong because glargine insulin is a long-acting insulin that provides a steady level of insulin throughout the day.
It cannot be mixed with other types of insulin
A nurse is evaluating the blood glucose levels of a pregnant woman who has gestational diabetes after a glucose tolerance test.
Which of the following results indicates that the woman has impaired glucose tolerance?
Explanation
The correct answer is choice B. One-hour blood glucose level of 185 mg/dL.
This indicates that the woman has impaired glucose tolerance, which is a risk factor for gestational diabetes.According to Mayo Clinic, a normal blood glucose level is lower than 140 mg/dL (7.8 mmol/L) after a glucose tolerance test.
A blood glucose level between 140 and 199 mg/dL (7.8 and 11 mmol/L) is considered impaired glucose tolerance,
A nurse is caring for a newborn whose mother has gestational diabetes.
The nurse should monitor the newborn for which of the following complications?
Explanation
Polycythemia is a condition where the baby has too many red blood cells, which can cause blood clots and other problems.It can occur in newborns whose mothers have gestational diabetes because of the high blood sugar levels in the mother’s blood.
Choice A is wrong because macrosomia is not a complication, but a risk factor for gestational diabetes.Macrosomia means having a large baby, which can cause difficulties during delivery and increase the need for a C-section.
Choice B is wrong because hypothermia is not a common complication of gestational diabetes.
Hypothermia means having a low body temperature, which can occur in newborns for various reasons, such as infection, prematurity, or exposure to cold.
Choice D is wrong because hyperglycemia is not a complication of gestational diabetes, but a cause of it.
Hyperglycemia means having high
A nurse is teaching a pregnant woman who has gestational diabetes about how to prevent type 2 diabetes in the future.
Which of the following statements by the woman indicates an understanding of the teaching?
Explanation
A nurse is teaching a pregnant woman who has gestational diabetes about how to prevent type 2 diabetes in the future.
Which of the following statements by the woman indicates an understanding of the teaching?.
A. “I should have my blood glucose levels checked every year.”.
B. “I should avoid breastfeeding my baby.”.
C. “I should gain weight gradually after delivery.”.
D. “I should take oral antidiabetic drugs as prescribed.
Answer and explanation..
The correct answer is choice A.“I should have my blood glucose levels checked every year.” This statement indicates that the woman understands that she is at high risk of developing type 2 diabetes after having gestational diabetes and that regular screening can help detect it early and prevent complications.
Choice B is wrong because breastfeeding can actually lower the risk of type 2 diabetes in women who had gestational diabetes.Breastfeeding can also benefit the baby by reducing the risk of obesity and diabetes later in life.
Choice C is wrong because gaining weight gradually after delivery can increase the risk of type 2 diabetes in women who had gestational diabetes.
Losing excess weight and
A nurse is providing education to a pregnant client who is 42 years old.
The nurse explains that advanced maternal age increases the risk of which condition during pregnancy?
Explanation
The correct answer is
B. Preeclampsia.
Preeclampsia is a condition that causes high blood pressure and protein in the urine during pregnancy.It can lead to serious complications for the mother and the baby, such as seizures, organ damage, growth restriction, and placental abruption.
Advanced maternal age (35 years or older) is one of the risk factors for preeclampsia.Other risk factors include chronic hypertension, kidney disease, diabetes, obesity, multiple gestation, and history of preeclampsia.
A. Gestational diabetes.
Statement is wrong because gestational diabetes is a condition that causes high blood sugar levels during pregnancy.
It can affect the health of the mother and the baby, such as increasing the risk of macrosomia, cesarean delivery, hypoglycemia, and future diabetes.
However, advanced maternal age is not a major risk factor for gestational diabetes.
The main risk factors are obesity, family history of diabetes, previous gestational diabetes, and certain ethnicities.
C. Preterm labor.
Statement is wrong because preterm labor is when contractions start before 37 weeks of pregnancy and lead to cervical changes.
It can result in premature birth, which can cause health problems for the baby, such as breathing difficulties, bleeding in the brain, and infections.
Advanced maternal age is not a direct risk factor for preterm labor.
The main risk factors are multiple gestation, history of preterm birth, cervical insufficiency, infection, placental problems, and certain medical conditions.
D. Placenta previa.
Statement is wrong because placenta previa is when the placenta covers part or all of the cervix.
It can cause painless vaginal bleeding during pregnancy and delivery complications, such as hemorrhage and cesarean delivery.
Advanced maternal age is not a strong risk factor for placenta previa.
The main risk factors are previous cesarean delivery, multiple gestation, smoking, and previous uterine surgery.
A client with a body mass index (BMI) of 32 asks the nurse about the potential risks during pregnancy.
The nurse explains that an elevated BMI increases the risk of developing:.
Explanation
The correct answer is choice D. Gestational diabetes.
Gestational diabetes is a condition in which a woman without diabetes develops high blood sugar levels during pregnancy.
It can cause complications for both the mother and the baby, such as preeclampsia, macrosomia, and neonatal hypoglycemia.An elevated BMI increases the risk of developing gestational diabetes because excess body fat can impair insulin sensitivity and secretion.
Choice A is wrong because preterm labor is not directly related to BMI, but rather to other factors such as infections, cervical insufficiency, or multiple gestation.
Choice B is wrong because ectopic pregnancy is not associated with BMI, but rather with pelvic inflammatory disease, tubal surgery, or previous ectopic pregnancy.
Choice C is wrong because gestational hypertension is not caused by BMI alone, but rather by genetic factors, chronic hypertension, or renal disease.
Normal ranges for BMI are 18.5-24.9 kg/m2 for normal weight, 25.0-29.9 kg/m2 for overweight, and 30.0 kg/m2 or higher for obesity.
A nurse is assessing a pregnant client's medical history.
Which factor increases the client's risk of developing gestational diabetes?
Explanation
The correct answer is choiceD.
No history of endocrine disorders.This factor increases the client’s risk of developing gestational diabetes because endocrine disorders such as thyroid disease or polycystic ovary syndrome can affect insulin resistance and glucose metabolism.
Choice A is wrong because having a previous baby withlow birth weightis not a risk factor for gestational diabetes.In fact, having a previous baby withhigh birth weight(> 9 pounds) is a risk factor.
Choice B is wrong because being ofCaucasian originis not a risk factor for gestational diabetes.In fact, being ofnon-Caucasian originsuch as African American, Hispanic, Native American, Asian American, or Pacific Islander is a risk factor.
Choice C is wrong because havingno family history of diabetesis not a risk factor for gestational diabetes.In fact, having afamily history of diabetes(especially type 2 diabetes) in a first-degree relative (parent or sibling) is a risk factor.
Some other risk factors for gestational diabetes include being older than 25 years, being overweight or obese, having prediabetes or impaired glucose tolerance, having a history of gestational diabetes in a previous pregnancy, having hypertension or preeclampsia, or having polycystic ovary syndrome.
Normal ranges for fasting plasma glucose are 60 to 99 mg/dL for nonpregnant women and 70 to 95 mg/dL for pregnant women.Normal ranges for oral glucose tolerance test are less than 140 mg/dL at 1 hour and less than 120 mg/dL at 2 hours for nonpregnant women and less than 180 mg/dL at 1 hour and less than 155 mg/dL at 2 hours for pregnant women.
A client with a history of impaired glucose tolerance asks the nurse about the potential impact on her current pregnancy.
The nurse explains that impaired glucose tolerance increases the risk of developing:.
Explanation
The correct answer is choice C. Gestational diabetes.Impaired glucose tolerance in pregnancy means that the blood sugar levels are elevated, but not high enough to be diagnosed with diabetes.However, this condition increases the risk of developing gestational diabetes, which is a type of diabetes that occurs only during pregnancy and affects both the mother and the baby.
Choice A is wrong because preterm labor is not directly caused by impaired glucose tolerance, although gestational diabetes may increase the risk of preterm labor.
Choice B is wrong because ectopic pregnancy is not related to impaired glucose tolerance or gestational diabetes.Ectopic pregnancy occurs when a fertilized egg implants outside the uterus, usually in the fallopian tube.
Choice D is wrong because gestational hypertension is not caused by impaired glucose tolerance, although gestational diabetes may increase the risk of gestational hypertension.Gestational hypertension is high blood pressure that develops after 20 weeks of pregnancy and goes away after delivery.
A nurse is providing education to a pregnant client of Middle Eastern origin.
The nurse explains that which factor increases the client's risk of developing gestational diabetes?
Explanation
The correct answer is choice D. No history of endocrine disorder.This is because having a history of endocrine disorder, such as thyroid disease or polycystic ovary syndrome, can increase the risk of developing gestational diabetes.
Choice A is wrong because being of African-Caribbean origin is not a risk factor for gestational diabetes.The ethnic groups that have higher risk include Asian, Hispanic, Native American, and Pacific Islander.
Choice B is wrong because normal body mass index (BMI) is not a risk factor for gestational diabetes.On the contrary, having a high BMI (over 30) before pregnancy or gaining too much weight during pregnancy can increase the risk of gestational diabetes.
Choice C is wrong because no family history of diabetes is not a risk factor for gestational diabetes.Having a family history of diabetes, especially in a first-degree relative (such as a parent or sibling), can increase the risk of gestational diabetes.
Normal ranges for blood glucose levels during pregnancy are:
• Fasting: less than 95 mg/dL
• One hour after meal: less than 140 mg/dL
• Two hours after meal: less than 120 mg/dL
A nurse is assessing a pregnant woman for risk factors for gestational diabetes.
Which of the following factors should the nurse identify as increasing the woman's risk?
Explanation
The correct answer is choice A.Being 35 years old is a risk factor for gestational diabetes because the risk increases with age.
Choice B is wrong because having a BMI of 28 is not considered obese, which is a risk factor for gestational diabetes.Obesity is usually defined as having a BMI of 30 or higher.
Choice C is wrong because having a previous baby who weighed 3.5 kg (7.7 lb) at birth is not a risk factor for gestational diabetes.A risk factor is having a previous baby who weighed more than 4 kg (9 lb) at birth.
Choice D is wrong because having a history of PCOS (polycystic ovary syndrome) is not a risk factor for gestational diabetes.PCOS is a condition that affects the ovaries and hormones, but it does not directly cause gestational diabetes.
A nurse is providing education to a pregnant woman who has gestational diabetes.
The nurse should explain that the woman has a higher risk of developing which of the following conditions in the future?
Explanation
The correct answer is choice C. Type 2 diabetes.The nurse should explain that the woman has a higher risk of developing type 2 diabetes later in life because gestational diabetes is a condition where the body cannot use insulin properly during pregnancy.This can lead to high blood sugar levels and affect the health of both the mother and the baby.Gestational diabetes usually goes away after the baby is born, but it increases the chance of getting type 2 diabetes in the future.According to the CDC, up to 50% of women with gestational diabetes will develop type 2 diabetes within 5 to 10 years after delivery.
Choice A is wrong because hypertension is not directly related to gestational diabetes.However, high blood pressure can be a complication of pregnancy and can increase the risk of preeclampsia, a serious condition that can affect both the mother and the baby.
Choice B is wrong because osteoporosis is not directly related to gestational diabetes.
Osteoporosis is a condition where the bones become weak and brittle due to loss of bone density.It can be influenced by factors such as age, genetics, diet, lifestyle, and hormonal changes.
Choice D is wrong because thyroid disease is not directly related to gestational diabetes.
Thyroid disease is a condition where the thyroid gland produces too much or too little thyroid hormone, which regulates the metabolism and other body functions.It can be caused by autoimmune disorders, infections, tumors, medications, or iodine deficiency.
A nurse is reviewing the laboratory results of a pregnant woman who is being screened for gestational diabetes.
The nurse notes that the woman has a fasting blood glucose level of 100 mg/dL.
Which of the following actions should the nurse take?
Explanation
The correct answer is choice C. Perform a glucose tolerance test.
A fasting blood glucose level of 100 mg/dL is considered borderline for gestational diabetes and indicates the need for further testing.
A glucose tolerance test measures how the body responds to a glucose load and can diagnose gestational diabetes.
Choice A is wrong because a fasting blood glucose level of 100 mg/dL is not normal for a pregnant woman and does not rule out gestational diabetes.
Choice B is wrong because repeating the test in one week will not provide any additional information and may delay the diagnosis and treatment of gestational diabetes.
Choice D is wrong because insulin is not prescribed unless the woman has confirmed gestational diabetes and fails to control her blood glucose levels with diet and exercise.
The normal range for fasting blood glucose in pregnancy is 70 to 95 mg/dL.
A nurse is caring for a pregnant woman who has gestational diabetes and is of African-Caribbean origin.
The nurse should recognize that the woman's ethnicity is associated with which of the following characteristics?
Explanation
The correct answer is choice A. Higher insulin resistance.According to a systematic review of gestational diabetes mellitus (GDM) in Africa, African-Caribbean women have higher insulin resistance than other ethnic groups, which increases their risk of developing GDM.
Insulin resistance is a condition where the body does not respond well to the hormone insulin, which regulates blood sugar levels.
Choice B is wrong because lower birth weight is not associated with GDM in African-Caribbean women.In fact, some studies have found that GDM increases the risk of macrosomia (large for gestational age infants) and higher mean birth weight.
Choice C is wrong because earlier onset of diabetes is not a characteristic of African-Caribbean women with GDM.
GDM is usually diagnosed in the second or third trimester of pregnancy, regardless of ethnicity.However, women with GDM have a higher risk of developing type 2 diabetes later in life.
Choice D is wrong because faster resolution of diabetes is not a characteristic of African-Caribbean women with GDM.Most women with GDM revert to normal glucose metabolism after delivery, but some may have persistent glucose intolerance or diabetes.The risk of developing type 2 diabetes after GDM is also higher for African-Caribbean women than other ethnic groups.
A nurse is planning care for a pregnant woman who has gestational diabetes and a history of prediabetes.
Which of the following interventions should the nurse include in the plan?
Explanation
The correct answer is choice D. Teach the woman how to check her blood glucose levels at home.This is because gestational diabetes is a condition where the blood glucose levels are higher than normal during pregnancy, and it can affect the health of the mother and the baby.By checking her blood glucose levels at home, the woman can monitor her condition and adjust her treatment accordingly.
Choice A is wrong because increasing the intake of complex carbohydrates can raise the blood glucose levels and worsen gestational diabetes.Instead, the woman should follow a healthy eating plan that balances carbohydrates with protein and fat.
Choice B is wrong because blood pressure and urine protein levels are not directly related to gestational diabetes.They are more relevant for preeclampsia, a different complication of pregnancy that involves high blood pressure and kidney damage.
Choice C is wrong because limiting physical activity during pregnancy can increase the risk of gestational diabetes and other problems.Physical activity can help lower blood glucose levels, improve blood pressure and cholesterol levels, relieve stress, and prevent excessive weight gain.The woman should aim for 30 minutes of moderate activity at least 5 days a week, unless her doctor advises otherwise.
A nurse is teaching a group of pregnant women about risk factors for gestational diabetes.
Which of the following statements by one of the women indicates a need for further teaching?
Explanation
The correct answer is choice D. “I should have my baby weighed at every prenatal visit.” This statement indicates a need for further teaching because having the baby weighed at every prenatal visit is not a way to prevent or detect gestational diabetes.Gestational diabetes is a condition in which women develop high blood sugar during pregnancy due to hormonal changes and insufficient insulin production.It can cause complications for the mother and the baby, such as high blood pressure, heavy birth weight, premature delivery, low blood sugar and future diabetes.
Choice A is wrong because losing weight before getting pregnant if one has a high BMI is a good way to reduce the risk of gestational diabetes.Obesity is one of the biggest risk factors for developing gestational diabetes, as it affects the body’s ability to use insulin effectively.
Choice B is wrong because telling the doctor if one has a family history of diabetes is also a good way to reduce the risk of gestational diabetes.Having a parent or sibling with diabetes increases the likelihood of developing gestational diabetes, as it may indicate a genetic predisposition to insulin resistance.
Choice C is wrong because avoiding getting pregnant after 40 years old is another good way to reduce the risk of gestational diabetes.Maternal age is one of the most important independent risk factors for gestational diabetes, as older women tend to have more insulin resistance and less beta-cell function than younger women.
A nurse is conducting a prenatal class for women who have gestational diabetes.
The nurse should inform the women that having gestational diabetes increases their risk of having which of the following complications during pregnancy?
Explanation
The correct answer is choice B. Preeclampsia.Gestational diabetes increases the risk of developing preeclampsia, a condition characterized by high blood pressure and protein in the urine that can lead to serious complications for the mother and the baby.
Choice A is wrong because anemia is not a common complication of gestational diabetes.
Anemia is a condition where the red blood cells are low or abnormal, causing fatigue, weakness and pale skin.
Choice C is wrong because placenta previa is not related to gestational diabetes.
Placenta previa is a condition where the placenta covers part or all of the opening of the cervix, causing bleeding and possible premature delivery.
Choice D is wrong because preterm labor is not directly caused by gestational diabetes.
Preterm labor is when contractions start before 37 weeks of pregnancy, which can result in a premature birth.However, gestational diabetes can increase the risk of other conditions that can lead to preterm labor, such as polyhydramnios (excess amniotic fluid) or macrosomia (large baby).
A nurse is reviewing the medical records of four pregnant women who are being screened for gestational diabetes.
Which of the following women has the highest risk factor for developing gestational diabetes?
Explanation
The correct answer is choice A. A 32-year-old woman who is obese and has PCOS.
This woman has two major risk factors for developing gestational diabetes: obesity and polycystic ovary syndrome (PCOS).Obesity increases insulin resistance and PCOS is associated with hormonal imbalances that affect glucose metabolism.
Choice B is wrong because being Asian and having a previous baby who weighed 4 kg (8.8 lb) at birth are not as strong risk factors as obesity and PCOS.However, they do increase the risk slightly.
Choice C is wrong because being Caucasian and having impaired glucose tolerance are also not as strong risk factors as obesity and PCOS.Impaired glucose tolerance means that the blood sugar level is higher than normal but not high enough to be diagnosed as diabetes.
Choice D is wrong because being Hispanic and having a parent with type 2 diabetes are also not as strong risk factors as obesity and PCOS.However, they do increase the risk slightly.
Normal ranges for blood glucose levels during pregnancy are:
• Fasting: less than 95 mg/dL
• One hour after meal: less than 140 mg/dL
• Two hours after meal: less than 120 mg/dL
A nurse is counseling a pregnant woman who has gestational diabetes and wants to know how to prevent type 2 diabetes after delivery.
Which of the following recommendations should the nurse give?
Explanation
The correct answer is choice A. Breastfeed your baby for at least six months.According to the CDC, breastfeeding can lower the risk of type 2 diabetes for both mothers and babies.
Breastfeeding can also help mothers lose weight after delivery and improve blood sugar control.
Choice B is wrong because oral antidiabetic drugs are not recommended for women with gestational diabetes.
Instead, they should monitor their blood glucose levels and follow a healthy eating plan and physical activity routine.If these measures are not enough, they may need insulin injections.
Choice C is wrong because having blood glucose levels checked every six months is not enough to prevent type 2 diabetes after delivery.Women with gestational diabetes should have their blood glucose tested 6 to 12 weeks after their baby is born and then every 1 to 3 years to make sure their levels are on target.
Choice D is wrong because following a low-protein, high-fat diet is not a good way to prevent type 2 diabetes after delivery.
A high-fat diet can increase the risk of obesity, heart disease, and insulin resistance.Women with gestational diabetes should follow a balanced diet that includes lean protein, healthy fats, whole grains, fruits, and vegetables.
A nurse is evaluating the outcomes of care for a pregnant woman who has gestational diabetes and received insulin therapy during pregnancy.
Which of the following findings indicates that the insulin therapy was effective?
Explanation
The correct answer is choice B. The woman delivered a healthy baby who weighed 3 kg (6.6 lb) at birth.This indicates that the insulin therapy was effective in preventing macrosomia, which is a common complication of gestational diabetes mellitus (GDM).Macrosomia is defined as a birth weight above the 90th percentile for gestational age or above 4 kg (8.8 lb).Macrosomia increases the risk of birth trauma, shoulder dystocia, cesarean section, and neonatal hypoglycemia.
Choice A is wrong because normal blood pressure and urine protein levels throughout pregnancy are not specific indicators of insulin therapy effectiveness.They are more related to the prevention of pre-eclampsia, which is a separate complication of pregnancy that can affect women with or without GDM.
Choice C is wrong because having no episodes of hypoglycemia or hyperglycemia during pregnancy is not sufficient to indicate insulin therapy
A nurse is teaching a pregnant woman who has gestational diabetes about the possible complications of uncontrolled blood sugar levels.
The nurse should explain that high blood sugar levels can increase the risk of which of the following infections?
Explanation
The correct answer is choice D. Thrush.
Thrush is a fungal infection that can affect the mouth, skin, or genitals.
It is more common in people with diabetes, especially if their blood sugar levels are not well controlled.High blood sugar levels can weaken the immune system and make it harder to fight off infections.
Choice A is wrong because pneumonia is a bacterial or viral infection of the lungs.It is not directly related to gestational diabetes, although having diabetes may increase the risk of respiratory infections in general.
Choice B is wrong because meningitis is an inflammation of the membranes that cover the brain and spinal cord.
It can be caused by bacteria, viruses, fungi, or other organisms.Gestational diabetes does not increase the risk of meningitis.
Choice C is wrong because cholecystitis is an inflammation of the gallbladder.
It can be caused by gallstones, infections, or other factors.Gestational diabetes does not increase the risk of cholecystitis.
Normal ranges for blood sugar levels during pregnancy are:
• Before meals: 3.5 to 5.9 mmol/L
• One hour after meals: 7.8 mmol/L or lower
• Two hours after meals: 6.4 mmol/L or lower
A nurse is assessing a pregnant woman who has gestational diabetes for signs of hyperglycemia.
The nurse should monitor the woman for which of the following findings?
Explanation
The correct answer is choice C. Blurred vision.
Blurred vision is a sign of hyperglycemia, which means high blood sugar.Hyperglycemia can occur in pregnant women who have gestational diabetes, a condition that develops during pregnancy and usually disappears after giving birth.Hyperglycemia can cause problems for the mother and the baby if not treated properly.
Choice A is wrong because hypotension means low blood pressure, which is not a sign of hyperglycemia.Hypotension can have other causes, such as dehydration, bleeding, or infection.
Choice B is wrong because bradycardia means slow heart rate, which is not a sign of hyperglycemia.Bradycardia can have other causes, such as heart disease, medication, or hypothyroidism.
Choice D is wrong because pallor means pale skin, which is not a sign of hyperglycemia.Pallor can have other causes, such as anemia, shock, or low blood flow.
Some other signs of hyperglycemia include increased thirst, frequent urination, excessive sweating, fatigue, and genital itching or thrush.Normal blood sugar ranges for pregnant women are 60 to 99 mg/dL before meals and less than 120 mg/dL one hour after meals.
A nurse is caring for a pregnant woman who has gestational diabetes and reports excessive sweating.
The nurse should recognize that this symptom is most likely caused by which of the following factors?
Explanation
The correct answer is choice B. Hypoglycemia.Excessive sweating is a common symptom of low blood sugar (glucose) levels, which can occur in gestational diabetes if the woman takes too much insulin or does not eat enough carbohydrates.Hypoglycemia can also cause other symptoms such as shakiness, dizziness, hunger, headache, and confusion.
Choice A is wrong because dehydration does not cause excessive sweating, but rather the opposite.Dehydration can occur if the woman has high blood sugar levels, which can cause increased thirst and urination.
Choice C is wrong because ketoacidosis is a serious complication of diabetes that occurs when the body breaks down fat for energy due to lack of insulin.Ketoacidosis can cause symptoms such as nausea, vomiting, abdominal pain, fruity breath odor, and rapid breathing.
Excessive sweating is not a typical sign of ketoacidosis.
Choice D is wrong because anemia is a condition in which the blood does not have enough red blood cells or hemoglobin to carry oxygen to the tissues.Anemia can cause symptoms such as fatigue, weakness, pale skin, shortness of breath, and chest pain.
Excessive sweating is not a common symptom of anemia.
Normal ranges for blood glucose levels during pregnancy are:
• Fasting: 60 to 95 mg/dL
• One hour after a meal: 100 to 129 mg/dL
• Two hours after a meal: 70 to 119 mg/dL
A nurse is evaluating the blood glucose levels of a pregnant woman who has gestational diabetes after a meal.
The nurse notes that the woman has a blood glucose level of 200 mg/dL.
Which of the following actions should the nurse take?
Explanation
The correct answer is choice D. Notify the provider.
A blood glucose level of 200 mg/dL (11.1 mmol/L) after a meal is too high for a pregnant woman with gestational diabetes and indicates poor glycemic control.
The provider should be informed of this result and may adjust the woman’s treatment plan accordingly.
Choice A is wrong because insulin is not always prescribed for gestational diabetes.
Some women can manage their blood sugar levels with diet and exercise alone.
Insulin should only be administered as prescribed by the provider and not based on a single test result.
Choice B is wrong because drinking water will not lower the blood glucose level significantly.
Water can help prevent dehydration and constipation, which are common problems in pregnancy, but it does not affect insulin sensitivity or glucose metabolism.
Choice C is wrong because repeating the test in 15 minutes will not change the outcome.
A blood glucose level of 200 mg/dL (11.1 mmol/L) after a meal is clearly abnormal and needs immediate attention.
Delaying the notification of the provider may increase the risk of complications for the woman and her baby.
According to Diabetic.org, the normal blood glucose levels for gestational diabetes are:
• Fasting: less than 95 mg/dL (5.3 mmol/L)
• One hour after a meal: less than 140 mg/dL (7.8 mmol/L)
• Two hours after a meal: less than 120 mg/dL (6.7 mmol/L)
These levels may vary slightly depending on the clinic or lab, but
A nurse is providing education to a pregnant woman who has gestational diabetes and wants to know how to prevent symptoms of hyperglycemia.
Which of the following instructions should the nurse include?
Explanation
The correct answer is choice A. Eat smaller meals more frequently throughout the day.
This can help prevent symptoms of hyperglycemia (high blood sugar) by keeping the blood sugar level more stable and avoiding spikes and dips.Eating smaller meals can also help prevent overeating and weight gain, which can worsen insulin resistance and gestational diabetes.
Choice B is wrong because foods that are high in fiber and low in fat can actually help control blood sugar levels by slowing down the digestion and absorption of carbohydrates.Fiber can also help lower cholesterol levels and prevent constipation.
Choice C is wrong because simple carbohydrates and sugars can raise blood sugar levels quickly and cause hyperglycemia.Women with gestational diabetes should limit their intake of these foods and choose complex carbohydrates that are rich in fiber, such as whole grains, fruits, and vegetables.
Choice D is wrong because skipping breakfast can lead to low blood sugar levels in the morning and high blood sugar levels later in the day.
It can also increase hunger and cravings, which can result in overeating at lunch and dinner.Women with gestational diabetes should eat a balanced breakfast that includes protein, carbohydrates, and healthy fats.
A nurse is reviewing the laboratory results of a pregnant woman who has gestational diabetes and is experiencing symptoms of hyperglycemia.
The nurse expects to find which of the following findings?
Explanation
The correct answer is choice C. Elevated urine specific gravity.
This is because hyperglycemia causes osmotic diuresis, which increases the concentration of solutes in the urine.
Urine specific gravity is a measure of the density of urine compared to water and reflects the amount of solutes in the urine.A normal range for urine specific gravity is 1.005 to 1.030.
Choice A is wrong because elevated serum ketones are a sign of ketoacidosis, which is a complication of diabetes mellitus type 1, not gestational diabetes.Ketoacidosis occurs when the body breaks down fat for energy due to insufficient insulin and produces ketones, which are acidic byproducts that can lower the blood pH.
Choice B is wrong because decreased serum osmolality indicates dilution of the blood, which can be caused by excessive fluid intake, diuretic use, or syndrome of inappropriate antidiuretic hormone (SIADH).
Serum osmolality is a measure of the concentration of solutes in the blood and reflects the balance between water and electrolytes.A normal range for serum osmolality is 275 to 295 mOsm/kg.
Choice D is wrong because decreased blood pH indicates acidosis, which can be caused by ketoacidosis, lactic acidosis, renal failure, or respiratory failure.
Blood pH is a measure of the acidity or alkalinity of the blood and reflects the balance between carbon dioxide and bicarbonate.A normal range for blood pH is 7.35 to 7.45.
A nurse is preparing to administer oral glucose to a pregnant woman who has gestational diabetes and is experiencing symptoms of hyperglycemia.
The nurse should use which of the following routes to administer the glucose?
Explanation
The correct answer is choice A. Sublingual.
The nurse should use the sublingual route to administer the glucose, which means placing the glucose under the tongue of the woman.This route allows for faster absorption of glucose into the bloodstream than the oral route, which involves swallowing the glucose.This is especially important for a pregnant woman with gestational diabetes and hyperglycemia, who needs to lower her blood sugar levels quickly to avoid complications for herself and her baby.
Choice B. Buccal is wrong because it means placing the glucose inside the cheek against the buccal mucosa.This route has been shown to result in a lower plasma glucose concentration than the oral route, which is not desirable for a woman with hyperglycemia.
Choice C. Oropharyngeal is wrong because it means placing the glucose in the back of the mouth near the throat.This route is not recommended for glucose administration because it can cause choking or aspiration.
Choice D. Nasogastric is wrong because it means inserting a tube through the nose into the stomach and delivering the glucose through the tube.This route is invasive and unnecessary for glucose administration, unless the woman is unable to take glucose by mouth.
Normal ranges for blood glucose levels during pregnancy are 3.5 to 5.9 mmol/l before meals and less than 7.8 mmol/l one hour after meals.
A nurse is assessing a pregnant woman who has gestational diabetes for complications of hyperglycemia during labor and delivery.
The nurse should monitor the woman for which of the following signs and symptoms?
Explanation
The correct answer is choice A. Fetal distress.According to the search results, maternal hyperglycemia during labor is highly associated with macrosomia in neonates, which can lead to fetal distress due to shoulder dystocia, birth trauma, or hypoxia.
Fetal distress can be detected by abnormal fetal heart rate patterns or meconium-stained amniotic fluid.
Choice B. Uterine atony is wrong because it is not a direct complication of hyperglycemia during labor.
Uterine atony is a failure of the uterus to contract after delivery, which can cause postpartum hemorrhage.
It can be caused by multiple factors such as prolonged labor, overdistension of the uterus, infection, or medications.
Choice C. Maternal hypothermia is wrong because it is not a common complication of hyperglycemia during labor.
Maternal hypothermia can occur due to exposure to cold environment, anesthesia, or infection.
It can affect the maternal and fetal metabolism and oxygenation.
Choice D. Placental abruption is wrong because it is not a direct complication of hyperglycemia during labor.
Placental abruption is a premature separation of the placenta from the uterine wall, which can cause fetal and maternal hemorrhage, hypoxia, and shock.
It can be caused by trauma, hypertension, smoking, or cocaine use.
A nurse is teaching a pregnant woman who has gestational diabetes about how to recognize and manage symptoms of hyperglycemia after delivery.
Which of the following statements by the woman indicates an understanding of the teaching?
Explanation
The correct answer is choice A.“I should check my blood glucose levels four times a day.” This statement indicates that the woman understands the importance of monitoring her blood sugar levels regularly to manage gestational diabetes and prevent complications for herself and her baby.
Choice B is wrong because drinking juice or soda can increase blood sugar levels and worsen hyperglycemia.Instead, the woman should drink water or sugar-free beverages if she feels thirsty.
Choice C is wrong because vaginal discharge or itching are not symptoms of hyperglycemia, but of a possible yeast infection, which can be more common in women with diabetes.The woman should report any signs of infection to her doctor, but this is not related to managing hyperglycemia.
Choice D is wrong because stopping insulin or oral medication after delivery can cause blood sugar levels to rise and increase the risk of developing type 2 diabetes in the future.The woman should follow her doctor’s advice on when and how to stop taking medication for gestational diabetes.
A nurse is preparing a pregnant woman for a glucose tolerance test to screen for gestational diabetes.
The nurse should instruct the woman to do which of the following before the test?
Explanation
The correct answer is choice B. Drink water only for 8 hours before the test.This is because the test measures how your body responds to sugar (glucose) and drinking water will not affect your blood sugar levels.The test involves drinking a sugary drink and having your blood drawn before and after to check how your body handles the glucose.
Choice A is wrong because eating a high-carbohydrate meal the night before will raise your blood sugar levels and may interfere with the test results.
Choice C is wrong because caffeine and smoking can also affect your blood sugar levels and should be avoided before the test.
Choice D is wrong because some medications can affect your blood sugar levels and should be discussed with your doctor before the test.
The normal range for blood sugar levels during the glucose tolerance test is below 140 mg/dL (7.8 mmol/L) at one hour after drinking the sugary drink.If your level is higher than that, you may have gestational diabetes and need further testing.Gestational diabetes is a condition that develops during pregnancy and can cause problems for you and your baby if not well managed.
A nurse is interpreting the results of a glucose tolerance test for a pregnant woman who was screened for gestational diabetes.
The nurse should recognize that the woman has gestational diabetes if her blood glucose level is which of the following at 1 hour after drinking the sugary drink?
Explanation
The correct answer is choice C. 185 mg/dL.According to the Mayo Clinic, a blood sugar level of 190 mg/dL or higher indicates gestational diabetes.A blood sugar level below 140 mg/dL is usually considered normal.
Therefore, a blood sugar level of 185 mg/dL is above the normal range and below the diagnostic threshold for gestational diabetes.
Choice A is wrong because 160 mg/dL is within the normal range for the glucose tolerance test.
Choice B is wrong because 175 mg/dL is also within the normal range for the glucose tolerance test.
Choice D is wrong because 200 mg/dL is above the diagnostic threshold for gestational diabetes.
A nurse is teaching a pregnant woman who has gestational diabetes about the importance of diagnosing and treating the condition.
The nurse should explain that untreated gestational diabetes can lead to which of the following complications for the baby?
Explanation
The correct answer is choice D. Macrosomia.Macrosomia is a condition where the baby grows larger than normal due to excess sugar from the mother’s blood.This can lead to complications such as injuries during delivery, low blood sugar and mineral levels, jaundice, pre-term birth, and breathing problems for the baby.It can also increase the risk of obesity and diabetes later in life for the baby.
Choice A is wrong because intrauterine growth restriction (IUGR) is a condition where the baby grows smaller than normal due to poor nutrition or oxygen supply from the placenta.
Gestational diabetes does not cause IUGR, but other factors such as high blood pressure, smoking, infections, or chromosomal abnormalities can.
Choice B is wrong because respiratory distress syndrome (RDS) is a condition where the baby has difficulty breathing due to immature lungs that lack surfactant, a substance that helps keep the air sacs open.
Gestational diabetes does not directly cause RDS, but it can increase the risk of pre-term birth, which is a major risk factor for RDS.
Choice C is wrong because congenital anomalies are structural or functional defects that are present at birth due to genetic or environmental factors.
Gestational diabetes does not cause congenital anomalies, but it can increase the risk of them if it is present before or during early pregnancy, when the baby’s organs are forming.
A nurse is caring for a pregnant woman who has gestational diabetes and is scheduled for a follow-up glucose tolerance test six weeks after delivery.
The nurse should inform the woman that this test is done to check for which of the following conditions?
Explanation
The correct answer is choice B. Type 2 diabetes.This test is done to check if the woman has developed type 2 diabetes after having gestational diabetes during pregnancy.Gestational diabetes is a condition in which women develop high blood sugar during pregnancy.It usually goes away after delivery, but it increases the risk of developing type 2 diabetes later in life.Type 2 diabetes is a chronic condition that affects how the body uses glucose, a type of sugar that is the main source of energy for the cells.
Choice A is wrong because type 1 diabetes is an autoimmune condition that usually develops in childhood or young adulthood and requires insulin injections for life.
It is not caused by gestational diabetes.
Choice C is wrong because prediabetes is a condition in which blood sugar levels are higher than normal but not high enough to be diagnosed as diabetes.
It is a risk factor for developing type 2 diabetes, but it is not the same as having diabetes.
Choice D is wrong because metabolic syndrome is a cluster of conditions that increase the risk of heart disease, stroke and type 2 diabetes.These conditions include high blood pressure, high blood sugar, excess body fat around the waist and abnormal cholesterol levels.
Metabolic syndrome can be diagnosed by measuring these factors, not by a glucose tolerance test.
A nurse is providing dietary education to a pregnant woman who has gestational diabetes and a BMI of 30.
The nurse should advise the woman to consume how many calories per day during the third trimester of pregnancy.?
Explanation
The correct answer is choice D. 2400 calories.
A pregnant woman with gestational diabetes and a BMI of 30 needs to consume enough calories to support her pregnancy and maintain a healthy weight.The calorie level recommended for gestational diabetes varies widely depending on the individual’s needs, activity level, and weight gain goals.However, a general guideline is to consume 30 kcal/kg of ideal body weight (pre-pregnant weight) in the first trimester, 36 kcal/kg in the second trimester, and 38 kcal/kg in the third trimester.
Assuming that the woman’s ideal body weight is 65 kg (based on a BMI of 25), her calorie intake would be:
• First trimester: 30 x 65 = 1950 calories
• Second trimester: 36 x 65 = 2340 calories
• Third trimester: 38 x 65 = 2470 calories
Therefore, the closest answer is 2400 calories per day during the third trimester of pregnancy.
A. 1800 calories.
Statement is wrong because this is too low for a pregnant woman with gestational diabetes and a BMI of 30.Eating too few calories can lead to ketosis, which is harmful for the baby.
It can also cause low blood sugar, hunger, fatigue, and poor nutrition.
B. 2000 calories.
Statement is wrong because this is also too low for a pregnant woman with gestational diabetes and a BMI of 30.
It may not provide enough energy and nutrients for the mother and the baby.
C. 2200 calories.
Statement is wrong because this is still below the recommended range for a pregnant woman with gestational diabetes and a BMI of 30.
It may not meet the increased needs of the third trimester of pregnancy.
A nurse is administering insulin to a pregnant woman who has gestational diabetes and is in labor.
The nurse should monitor the woman’s blood glucose levels every how often during labor?
Explanation
The correct answer is choice A. The nurse should monitor the woman’s blood glucose levels every hour during labor.This is because the goal of intrapartum insulin therapy is maternal and fetal euglycemia with a maternal glucose less than 90 mg/dL.Hourly blood glucose monitoring can help adjust the insulin infusion rate and prevent hypoglycemia or hyperglycemia.
Choice B is wrong because every two hours is not frequent enough to maintain optimal glucose control during labor.
Choice C is wrong because every four hours is too long to wait between blood glucose checks and could lead to complications.
Choice D is wrong because every six hours is even longer and more risky than choice C. Normal ranges for blood glucose levels during labor are between 4.0 and 6.0-7.0 mmol/L (72-108 mg/dL).Women with gestational diabetes who require less than 1.0 units/kg/d of insulin may not need intravenous insulin, but they still need to be monitored regularly.
A nurse is assessing a newborn whose mother has gestational diabetes for signs of hypoglycemia.
The nurse should check the newborn’s blood glucose level within how many hours after birth?
Explanation
The correct answer is choice A. The nurse should check the newborn’s blood glucose level within one hour after birth.This is because infants born to mothers with gestational diabetes are at risk of developing hypoglycemia due to increased insulin secretion in response to maternal-fetal hyperglycemia.Hypoglycemia can cause neurological damage and other complications in newborns, so early detection and treatment are essential.
Choice B is wrong because two hours after birth may be too late to prevent or treat hypoglycemia in some infants.
Choice C is wrong because three hours after birth is even later and may increase the risk of adverse outcomes.
Choice D is wrong because four hours after birth is the latest time to check the blood glucose level and may miss some cases of hypoglycemia that occur earlier.
A nurse is evaluating the effectiveness of nursing interventions for a pregnant woman who has gestational diabetes and received nutritional therapy and exercise counseling during pregnancy.
Which of the following outcomes indicates that the interventions were successful?
Explanation
The correct answer is choice C. The woman had no episodes of hypoglycemia or hyperglycemia during pregnancy.This indicates that the interventions were successful in maintaining normal blood glucose levels and preventing complications for the mother and the baby.
Choice A is wrong because the woman gained less than 10 kg (22 lb) during pregnancy.
This is below the recommended weight gain range for women with gestational diabetes, which depends on their pre-pregnancy body mass index (BMI).According to a study based on over 12 thousand participants, the ideal weight gain range for women with gestational diabetes was 10–15.9 kg for underweight, 8–11.9 kg for normal weight, 6–7.9 kg for overweight, and -5–3.9 kg for obesity.
Choice B is wrong because the woman delivered a baby who weighed 3 kg (6.6 lb) at birth.
This is within the normal range for birth weight, but it does not necessarily reflect the effectiveness of the interventions for gestational diabetes.A baby born to a mother with gestational diabetes may be at risk of being large for gestational age (LGA), which is defined as a birth weight above the 90th percentile for gestational age.LGA babies may have complications such as shoulder dystocia, hypoglycemia, and respiratory distress syndrome.
Choice D is wrong because the woman’s blood glucose levels returned to normal within six weeks after delivery.
This is a desirable outcome, but it does not indicate that the interventions were successful during pregnancy.
Gestational diabetes usually
A nurse is reviewing the risk factors for developing gestational diabetes with a group of pregnant women during a prenatal class.
The nurse should include which of the following factors in the teaching?
Explanation
The correct answer is choice C.Being older than 25 years at the time of pregnancy is a risk factor for developing gestational diabetes.Gestational diabetes is a type of diabetes that can develop during pregnancy in women who don’t already have diabetes.It occurs when the body can’t make enough insulin during pregnancy.
Choice A is wrong because being underweight before pregnancy is not a risk factor for gestational diabetes.In fact, obesity is one of the biggest risk factors for this condition.
Choice B is wrong because having a history of infertility or miscarriage is not a risk factor for gestational diabetes.However, having a family history of diabetes is a risk factor.
Choice D is wrong because having a family history of autoimmune disease is not a risk factor for gestational diabetes.
Autoimmune diseases are conditions where the immune system attacks the body’s own tissues, such as type 1 diabetes or rheumatoid arthritis.Gestational diabetes is not an autoimmune disease, but rather a disorder of insulin resistance.
Normal ranges for blood glucose levels during pregnancy are:
• Fasting: less
A nurse is caring for a pregnant woman who has gestational diabetes and is in labor.
The nurse should monitor the woman for which of the following complications that can result from uncontrolled blood sugar levels?
Explanation
The correct answer is choice B. Preeclampsia.
Preeclampsia is a complication of pregnancy that is characterized by high blood pressure, proteinuria, and edema.It can result from uncontrolled blood sugar levels, as well as other risk factors such as obesity, hypertension, and previous large for gestational age (LGA) infant.
Preeclampsia can lead to serious complications for both the mother and the baby, such as eclampsia, HELLP syndrome, placental abruption, and intrauterine growth restriction.
Choice A. Placenta previa is wrong because it is a condition where the placenta covers the cervix partially or completely.It is not caused by uncontrolled blood sugar levels, but by factors such as previous cesarean section, multiple gestation, advanced maternal age, and smoking.
Choice C. Chorioamnionitis is wrong because it is an infection of the amniotic fluid and membranes that surround the fetus.
It is not caused by uncontrolled blood sugar levels, but by bacteria that ascend from the vagina or cervix into the uterus.It can cause fever, uterine tenderness, foul-smelling amniotic fluid, and fetal tachycardia.
Choice D. Abruptio placentae is wrong because it is a condition where the placenta separates from the uterine wall before delivery.It is not caused by uncontrolled blood sugar levels, but by factors such as trauma, hypertension, smoking, cocaine use, and previous history of abruption.
A nurse is assessing a newborn whose mother has gestational diabetes for signs of macrosomia.
The nurse should measure which of the following parameters to determine if the newborn has macrosomia?
Explanation
The correct answer is choice D. Birth weight.
The nurse should measure the birth weight of the newborn to determine if the newborn has macrosomia.Macrosomia is a condition in which a baby has a weight of more than 8 pounds, 13 ounces at birth.It is commonly caused by medical conditions, such as obesity or diabetes, of the mother during pregnancy.
Choice A is wrong because head circumference is not a reliable indicator of macrosomia.Some babies may have a large head circumference due to genetic factors or hydrocephalus, but not necessarily due to macrosomia.
Choice B is wrong because chest circumference is not a reliable indicator of macrosomia.Some babies may have a large chest circumference due to genetic factors or congenital heart defects, but not necessarily due to macrosomia.
Choice C is wrong because abdominal circumference is not a reliable indicator of macrosomia.Some babies may have a large abdominal circumference due to genetic factors or abdominal wall defects, but not necessarily due to macrosomia.
A nurse is teaching a pregnant woman who has gestational diabetes about how to prevent preterm birth.
The nurse should instruct the woman to do which of the following?
Explanation
The correct answer is choice A. Monitor her blood glucose levels regularly and keep them within the target range.This is because gestational diabetes can cause high blood sugar that can affect the pregnancy and the baby’s health.High blood sugar can increase the risk of premature birth and other complications.
By monitoring and controlling blood glucose levels, the woman can reduce these risks and have a healthier pregnancy.
Choice B is wrong because drinking plenty of fluids and avoiding caffeine and alcohol are general recommendations for pregnant women, but they do not specifically prevent preterm birth due to gestational diabetes.
Choice C is wrong because progesterone supplements are used to prevent preterm birth in women who have a history of spontaneous preterm birth or a short cervix, but they are not indicated for women with gestational diabetes.
Choice D is wrong because pelvic floor exercises and avoiding lifting heavy objects are also general recommendations for pregnant women, but they do not directly prevent preterm birth due to gestational diabetes.Pelvic floor exercises can help with urinary incontinence and pelvic organ prolapse, while avoiding lifting heavy objects can prevent back pain and injury.
A nurse is preparing to administer intravenous glucose to a newborn whose mother has gestational diabetes and who has hypoglycemia.
The nurse should recognize that this intervention is necessary to prevent which of the following complications?
Explanation
The correct answer is choice D. Seizures.This intervention is necessary to prevent seizures because hypoglycemia can cause brain injury and neurologic impairment in newborns.Seizures are one of the most common signs of hypoglycemia in newborns.
Choice A is wrong because respiratory distress syndrome is caused by a lack of surfactant in the lungs, not by hypoglycemia.
Choice B is wrong because necrotizing enterocolitis is an inflammatory condition of the intestines that affects premature or sick infants, not by hypoglycemia.
Choice C is wrong because intraventricular hemorrhage is a bleeding into the brain ventricles that occurs mainly in very low birth weight infants, not by hypoglycemia.
A nurse is providing discharge education to a pregnant woman who has gestational diabetes and delivered a healthy baby.
The nurse should inform the woman that she has an increased risk of developing which of the following conditions in the future?
Explanation
The correct answer is choice C. Type 2 diabetes.Women with gestational diabetes have a very high risk of developing type 2 diabetes later in life.Gestational diabetes is a condition where the body cannot use insulin properly during pregnancy, leading to high blood sugar levels.
This can affect the health of both the mother and the baby.
Choice A is wrong because hypothyroidism is a condition where the thyroid gland does not produce enough thyroid hormones, which regulate metabolism and growth.
Gestational diabetes does not increase the risk of hypothyroidism.
Choice B is wrong because osteoporosis is a condition where the bones become weak and brittle, increasing the risk of fractures.
Gestational diabetes does not increase the risk of osteoporosis.
Choice D is wrong because cardiovascular disease is a term that refers to various conditions that affect the heart and blood vessels, such as heart attack and stroke.Gestational diabetes may increase the risk of cardiovascular disease, but not as much as type 2 diabetes.
A nurse is reviewing the risk factors for developing gestational diabetes with a group of pregnant women during a prenatal class.
The nurse should include which of the following factors in the teaching?
Explanation
The correct answer is choice C.Being older than 25 years at the time of pregnancy is a risk factor for developing gestational diabetes.Gestational diabetes is a type of diabetes that can develop during pregnancy in women who don’t already have diabetes.It occurs when the body can’t make enough insulin during pregnancy.
Choice A is wrong because being underweight before pregnancy is not a risk factor for gestational diabetes.In fact, obesity is one of the biggest risk factors for gestational diabetes.
Choice B is wrong because having a history of infertility or miscarriage is not a risk factor for gestational diabetes.However, having a family history of diabetes is a risk factor for gestational diabetes.
Choice D is wrong because having a family history of autoimmune diseases is not a risk factor for gestational diabetes.
Autoimmune diseases are conditions where the immune system attacks the body’s own tissues, such as type 1 diabetes or rheumatoid arthritis.Gestational diabetes is not an autoimmune disease, but rather a disorder of insulin resistance and secretion.
A nurse is administering insulin to a pregnant woman who has gestational diabetes and is in labor.
The nurse should monitor the woman's blood glucose levels every how often during labor?
Explanation
The correct answer is choice A. The nurse should monitor the woman’s blood glucose levels every hour during labor.This is because labor is a stressful event that can increase the blood glucose levels and the risk of complications for both the mother and the baby.The goal is to maintain the maternal glucose between 4.0 and 6.0-7.0 mmol/L during labor.
Choice B is wrong because every two hours is too infrequent to detect and correct any fluctuations in blood glucose levels during labor.
Choice C is wrong because every four hours is even more infrequent and could lead to poor glucose control and adverse outcomes.
Choice D is wrong because every six hours is the least frequent and the most dangerous option for monitoring blood glucose levels during labor.
Normal ranges for blood glucose levels are 3.9 to 5.5 mmol/L for fasting or preprandial values, and less than 7.8 mmol/L for postprandial values.
A nurse is assessing a newborn whose mother has gestational diabetes for signs of hypoglycemia.
The nurse should check the newborn's blood glucose level within how many hours after birth?
Explanation
The correct answer is choice A. One hour.The nurse should check the newborn’s blood glucose level within one hour after birth because infants born to mothers with gestational diabetes are at risk of hypoglycemia due to hyperinsulinemia.Hypoglycemia can cause neurologic damage or death if left untreated.
Choice B is wrong because two hours is too long to wait for checking the blood glucose level of a newborn at risk of hypoglycemia.
Choice C is wrong because three hours is too long to wait for checking the blood glucose level of a newborn at risk of hypoglycemia.
Choice D is wrong because four hours is too long to wait for checking the blood glucose level of a newborn at risk of hypoglycemia.
Normal blood glucose levels for newborns are between 47 and 70 mg/dL.Mild hypoglycemia is defined as less than 47 mg/dL and severe hypoglycemia is defined as less than 36 mg/dL.
A nurse is evaluating the effectiveness of nursing interventions for a pregnant woman who has gestational diabetes and received nutritional therapy and exercise counseling during pregnancy.
Which of the following outcomes indicates that the interventions were successful?
Explanation
The correct answer is choice C. The woman had no episodes of hypoglycemia or hyperglycemia during pregnancy.This indicates that the interventions were successful in maintaining normal blood glucose levels and preventing complications for the mother and the baby.
Choice A is wrong because the woman gained less than 10 kg (22 lb) during pregnancy.This is not a reliable outcome of gestational diabetes interventions, as weight gain depends on many factors such as pre-pregnancy weight, body mass index, diet, and physical activity.
Choice B is wrong because the woman delivered a baby who weighed 3 kg (6.6 lb) at birth.This is not a specific outcome of gestational diabetes interventions, as birth weight can be influenced by other factors such as genetics, gestational age, maternal nutrition, and fetal growth.
Choice D is wrong because the woman’s blood glucose levels returned to normal within six weeks after delivery.This is not a direct outcome of gestational diabetes interventions during pregnancy, as blood glucose levels usually return to normal after delivery regardless of the interventions.However, women with gestational diabetes have a higher risk of developing type 2 diabetes later in life and should be screened regularly.
A nurse is teaching a pregnant woman who has gestational diabetes about how to recognize and manage symptoms of hyperglycemia after delivery.
Which of the following statements by the woman indicates an understanding of the teaching?
Explanation
The correct answer is choice C. The woman should report any vaginal discharge or itching to her doctor, as these could be signs of a yeast infection, which is more common in women with diabetes.Yeast infections can cause irritation and discomfort, and may increase the risk of preterm labor or urinary tract infections
Choice A is wrong because checking blood glucose levels four times a day is recommended during pregnancy, not after delivery.After delivery, the woman may need to check her blood glucose levels less often, depending on her doctor’s advice
Choice B is wrong because drinking juice or soda can raise blood glucose levels and worsen hyperglycemia.The woman should drink water or sugar-free beverages if she feels thirsty
Choice D is wrong because stopping insulin or oral medication after delivery can lead to uncontrolled blood glucose levels and complications.
The woman should follow her doctor’s instructions on how to adjust her medication after delivery.Some women may need to continue taking insulin or oral medication for a while, while others may be able to stop or switch to a different type of medication
A nurse is instructing a pregnant woman who has gestational diabetes on how to use a glucose meter to monitor her blood sugar levels at home.
The nurse should tell the woman to do which of the following?
Explanation
The nurse should tell the woman to wash her hands with soap and water before testing, prick the side of her fingertip with a lancet, and apply gentle pressure to the puncture site until a drop of blood forms.These steps are necessary to ensure a clean and adequate blood sample for the glucose meter.
Choice A is wrong because washing hands with soap and water is not enough.The woman should also dry her hands thoroughly to avoid diluting the blood sample.
Choice B is wrong because pricking the side of the fingertip with a lancet is not enough.The woman should also avoid squeezing the finger too hard, as this can affect the accuracy of the result.
Choice C is wrong because applying gentle pressure to the puncture site until a drop of blood forms is not enough.The woman should also wipe away the first drop of blood with a clean tissue and use the second drop for testing.
Normal ranges for blood glucose levels during pregnancy are 60 to 105 mg/dL before meals and less than 120 mg/dL one hour after meals.
The woman should report any abnormal readings to her health care provider.
A nurse is administering insulin to a pregnant woman who has gestational diabetes and is experiencing symptoms of hyperglycemia.
The nurse should use which of the following types of insulin to provide rapid-acting blood glucose control?
Explanation
Lispro insulin is a rapid-acting insulin that starts to work within 15 minutes and lasts for 2 to 4 hours.It is used to provide blood glucose control before meals for people with diabetes.A pregnant woman with gestational diabetes who is experiencing symptoms of hyperglycemia needs rapid-acting blood glucose control to prevent complications for herself and her baby.
Choice A is wrong because regular insulin is a short-acting insulin that starts to work within 30 minutes and lasts for 5 to 8 hours.It is not as fast as lispro insulin and may not provide adequate blood glucose control for a pregnant woman with hyperglycemia.
Choice B is wrong because NPH insulin is an intermediate-acting insulin that starts to work within 2 to 4 hours and lasts for 10 to 18 hours.It is used to provide background insulin throughout the day and night, but it is not suitable for rapid-acting blood glucose control.
Choice C is wrong because glargine insulin is a long-acting insulin that starts to work within 1 to 2 hours and lasts for 24 hours.It is used to provide steady insulin levels between meals and overnight, but it is not appropriate for rapid-acting blood glucose control.
A nurse is reviewing the antenatal care plan for a pregnant woman who has gestational diabetes and is taking oral antidiabetic drugs.
The nurse should expect the woman to have which of the following tests to monitor the effects of the medication on the baby?
Explanation
The correct answer is choice B. Biophysical profile.
A biophysical profile is a test that combines a nonstress test with an ultrasound to assess the well-being of the fetus.
It measures five parameters: fetal heart rate, fetal breathing movements, fetal body movements, fetal tone, and amniotic fluid volume.A biophysical profile is indicated for pregnant women with gestational diabetes who are taking oral antidiabetic drugs because these medications can cross the placenta and affect the fetal blood glucose levels.
Choice A is wrong because a nonstress test is a test that measures the fetal heart rate response to fetal movements.It is a screening test for fetal well-being, but it does not provide information about the fetal blood glucose levels or the amniotic fluid volume.
Choice C is wrong because an amniocentesis is a test that involves inserting a needle into the uterus to obtain a sample of amniotic fluid for genetic or biochemical analysis.It is not routinely performed for pregnant women with gestational diabetes unless there is a suspicion of a chromosomal abnormality or a fetal infection.
Choice D is wrong because chorionic villus sampling is a test that involves obtaining a sample of placental tissue for genetic or biochemical analysis.
It is usually performed between 10 and 13 weeks of gestation for women who are at high risk of having a baby with a chromosomal abnormality or a genetic disorder.It is not indicated for pregnant women with gestational diabetes who are taking oral antidiabetic drugs.
A nurse is caring for a pregnant woman who has gestational diabetes and is in labor.
The nurse should monitor the woman’s blood glucose levels every how often during labor?
Explanation
The correct answer is choice A. The nurse should monitor the woman’s blood glucose levels every hour during labor.This is because the maternal glucose level should be maintained between 4.0 and 6.0-7.0 mmol/L during labor to prevent neonatal hypoglycemia.
Choice B is wrong because monitoring every two hours may not be frequent enough to detect and correct any fluctuations in blood glucose levels.
Choice C is wrong because monitoring every four hours is too infrequent and may increase the risk of complications for the mother and the baby.
Choice D is wrong because monitoring every six hours is even more infrequent and may lead to poor outcomes.
Normal ranges for blood glucose levels during pregnancy are:
• Fasting or preprandial: < 95 mg/dL
• Postprandial (1 hour): < 140 mg/dL
• Postprandial (2 hours): < 120 mg/dL
A nurse is assessing a newborn whose mother has gestational diabetes for signs of hypoglycemia.
The nurse should check the newborn’s blood glucose level within how many hours after birth?
Explanation
The correct answer is choice A. One hour.The nurse should check the newborn’s blood glucose level within one hour after birth because infants born to mothers with gestational diabetes are at risk of hypoglycemia due to increased insulin secretion in response to maternal-fetal hyperglycemia.Hypoglycemia can cause symptoms such as jitteriness, lethargy, poor feeding, cyanosis and apnea.
Checking the blood glucose level within one hour can help identify and treat hypoglycemia promptly.
Choice B. Two hours is wrong because it may delay the detection and treatment of hypoglycemia, which can have adverse effects on the newborn’s brain development.
Choice C. Three hours is wrong for the same reason as choice B. Choice D. Four hours is wrong for the same reason as choice B and C. Normal ranges for blood glucose levels in newborns vary depending on the method of measurement, but generally they are above 47 mg/dL.Some sources suggest a lower cutoff of 40 mg/dL.
A nurse is evaluating the effectiveness of nursing interventions for a pregnant woman who has gestational diabetes and received nutritional therapy and exercise counseling during pregnancy.
Which of the following outcomes indicates that the interventions were successful?
Explanation
The correct answer is choice C. The woman had no episodes of hypoglycemia or hyperglycemia during pregnancy.
This outcome indicates that the interventions were successful in maintaining a normal blood glucose level for the woman and preventing complications for her and her baby.
Choice A is wrong because the recommended weight gain for a pregnant woman with gestational diabetes is 11.5 to 16 kg (25 to 35 lb).
Gaining less than 10 kg (22 lb) may indicate inadequate nutrition or poor glycemic control.
Choice B is wrong because the ideal birth weight for a baby of a woman with gestational diabetes is between 2.5 and 4 kg (5.5 and 8.8 lb).
A baby who weighs 3 kg (6.6 lb) at birth is within the normal range, but it does not necessarily reflect the effectiveness of the interventions.
Choice D is wrong because the woman’s blood glucose levels may or may not return to normal within six weeks after delivery.
Gestational diabetes usually resolves after giving birth, but some women may develop type 2 diabetes later in life.
Therefore, a postpartum glucose test is recommended to check the woman’s status.
Normal ranges for blood glucose levels during pregnancy are:
• Fasting: less than 95 mg/dL
• One hour after meals: less than 140 mg/dL
• Two hours after meals: less than 120 mg/dL
A nurse is teaching a pregnant woman who has gestational diabetes about how to recognize and manage symptoms of hyperglycemia after delivery.
Which of the following statements by the woman indicates an understanding of the teaching?
Explanation
The correct answer is choice A. “I should check my blood glucose levels four times a day.” This statement indicates that the woman understands the importance of monitoring her blood glucose levels after delivery to detect any changes or abnormalities.Most women with gestational diabetes will not have severe hyperglycemia after delivery, but they should be followed for at least 6–12 weeks to determine their glucose status.
Normal blood glucose levels are between 70 and 130 mg/dL before meals and less than 180 mg/dL two hours after meals.
Choice B is wrong because “I should drink juice or soda if I feel thirsty.” This statement indicates that the woman does not understand how to manage symptoms of hyperglycemia after delivery.
Drinking juice or soda can raise blood glucose levels and worsen hyperglycemia.
The woman should drink water or sugar-free beverages if she feels thirsty.
Choice C is wrong because “I should report any vaginal discharge or itching to my doctor.” This statement indicates that the woman does not understand how to recognize symptoms of hyperglycemia after delivery.
Vaginal discharge or itching can be signs of a yeast infection, which can occur more frequently in women with diabetes, but they are not specific to hyperglycemia.
Symptoms of hyperglycemia include increased thirst, frequent urination, blurred vision, fatigue, and headache.
Choice D is wrong because “I should stop taking my insulin or oral medication after delivery.” This statement indicates that the woman does not understand how to manage her blood glucose levels after delivery.Although most women with gestational diabetes will have normal blood glucose levels after delivery, some may have persisting hyperglycemia that requires medical management.The woman should consult with her doctor before stopping any medication and follow the guidelines of the American Diabetes Association and other relevant organizations.
A nurse is reviewing the risk factors for developing gestational diabetes with a group of pregnant women during a prenatal class.
The nurse should include which of the following factors in the teaching?
Explanation
The correct answer is choice C.Being older than 25 years at the time of pregnancy is a risk factor for developing gestational diabetes.Gestational diabetes is a type of diabetes that can develop during pregnancy in women who don’t already have diabetes.It occurs when the body can’t make enough insulin during pregnancy.
Choice A is wrong because being underweight before pregnancy is not a risk factor for gestational diabetes.In fact, obesity is one of the biggest risk factors for this condition.
Choice B is wrong because having a history of infertility or miscarriage is not a risk factor for gestational diabetes.However, having a family history of diabetes is a risk factor.
Choice D is wrong because having a family history of autoimmune disease is not a risk factor for gestational diabetes.Autoimmune diseases are conditions where the immune system attacks the body’s own tissues, such as type 1 diabetes or rheumatoid arthritis.Gestational diabetes is not an autoimmune disease, but rather a disorder of insulin resistance and secretion.
A nurse is providing dietary education to a pregnant woman who has gestational diabetes.
The nurse should advise the woman to consume which of the following types of carbohydrates to help control her blood glucose levels?
Explanation
The correct answer is choice C. Complex carbohydrates.
Complex carbohydrates are composed of long chains of glucose molecules that take longer to digest and provide a steady source of energy for the body.
They also help regulate blood glucose levels by preventing rapid spikes and drops.Complex carbohydrates are found in foods such as whole grains, beans, fruits, and vegetables.
Choice A is wrong because simple carbohydrates are composed of one or two sugar units that are quickly absorbed and metabolized by the body.
They can cause rapid fluctuations in blood glucose levels and should be limited by people who have gestational diabetes.Simple carbohydrates are found in foods such as candy, soda, honey, and white bread.
Choice B is wrong because refined carbohydrates are processed foods that have had most of their fiber and nutrients removed.
They are also quickly digested and can cause blood glucose levels to rise rapidly.Refined carbohydrates are found in foods such as white rice, pasta, pastries, and cereals.
Choice D is wrong because sugar alcohols are a type of sweetener that have fewer calories
A nurse is instructing a pregnant woman who has gestational diabetes on how to use a glucose meter to monitor her blood sugar levels at home.
The nurse should tell the woman to do which of the following?
Explanation
The correct answer is choice D. All of the above.
The nurse should tell the woman to wash her hands with soap and water before testing, prick the side of her fingertip with a lancet, and apply gentle pressure to the puncture site until a drop of blood forms.These steps are necessary to ensure accurate and safe blood glucose monitoring at home.
Choice A is wrong because washing hands with soap and water is not enough.The woman should also dry her hands thoroughly before testing.
Choice B is wrong because pricking the side of the fingertip is not enough.The woman should also rotate the puncture sites to avoid soreness and infection.
Choice C is wrong because applying gentle pressure to the puncture site is not enough.The woman should also dispose of the lancet and the test strip properly and record the blood glucose result.
Normal blood glucose ranges for pregnant women with gestational diabetes are 95 mg/dL or less before meals, 140 mg/dL or less 1 hour after meals, and 120 mg/dL or less 2 hours after meals.
A nurse is administering insulin to a pregnant woman who has gestational diabetes and is experiencing symptoms of hyperglycemia.
The nurse should use which of the following types of insulin to provide rapid-acting blood glucose control?
Explanation
The correct answer is choice D. Lispro insulin.
Lispro insulin is a type of rapid-acting insulin that can provide blood glucose control within 15 minutes of injection.It is suitable for pregnant women with gestational diabetes who need to lower their blood sugar quickly after meals.
Choice A is wrong because regular insulin is a type of short-acting insulin that takes about 30 minutes to start working and lasts for 3 to 6 hours.It is not as fast as lispro insulin and may cause low blood sugar if taken too early before meals.
Choice B is wrong because NPH insulin is a type of intermediate-acting insulin that takes about 2 to 4 hours to start working and lasts for 12 to 18 hours.It is not suitable for rapid-acting blood glucose control and may cause low blood sugar if taken too often or at the wrong time.
Choice C is wrong because glargine insulin is a type of long-acting insulin that takes about 1 to 2 hours to start working and lasts for 24 hours.It is not suitable for rapid-acting blood glucose control and may cause low blood sugar if taken with other types of insulin.
Gestational diabetes is a condition in which a hormone made by the placenta prevents the body from using insulin effectively.
Glucose builds up in the blood instead of being absorbed by the cells.It can cause complications for the mother and the baby, such as high blood pressure, large birth weight, premature delivery, low blood sugar, and future diabetes.Gestational diabetes can be managed with a healthy diet, exercise, and medication if needed.
Insulin is a hormone that helps regulate blood glucose levels.There are different types of insulin that vary in how quickly they start working, how long they last, and how they are taken.
A nurse is reviewing the antenatal care plan for a pregnant woman who has gestational diabetes and is taking oral antidiabetic drugs.
The nurse should expect the woman to have which of the following tests to monitor the effects of the medication on the baby?
Explanation
The correct answer is choice A. Nonstress test.A nonstress test is a screening tool that uses fetal heart rate patterns and accelerations as an indicator of fetal well-being.It is commonly performed for pregnant women who have gestational diabetes and are taking oral antidiabetic drugs to monitor the effects of the medication on the baby.
Choice B. Biophysical profile is wrong because it is an ultrasound assessment of the fetal status with an NST.It utilizes ultrasound with EFM to assess five variables: fetal breathing movements, fetal movement, fetal tone, amniotic fluid volume, and fetal heart rate.
Choice C.Amniocentesis is wrong because it is a diagnostic procedure where a needle is inserted through the abdominal wall into the uterine cavity to obtain amniotic fluid and commonly performed for genetic testing, neural tube defects, fetal lung maturity, and hemolytic disease in the fetus or intrauterine infection.
Choice D. Chorionic villus sampling (CVS) is wrong because it is a diagnostic procedure where a needle is inserted through the abdominal wall into the uterine cavity to obtain chorionic villi (placental tissue) and commonly performed for chromosomal, metabolic and DNA testing.It does not test for neural tube defects.
A nurse is caring for a pregnant woman who has gestational diabetes and is in labor.
The nurse should monitor the woman’s blood glucose levels every how often during labor?
Explanation
The correct answer is choice A. The nurse should monitor the woman’s blood glucose levels every hour during labor.This is because maternal blood glucose levels around the time of delivery are directly related to the risk of neonatal hypoglycemia.Therefore, achieving maternal euglycemia in women with gestational diabetes mellitus is critical to decreasing the risk of neonatal complications.
Choice B is wrong because every two hours is not frequent enough to ensure optimal glucose control during labor.
Choice C is wrong because every four hours is even less frequent and may miss significant fluctuations in blood glucose levels.
Choice D is wrong because every six hours is too infrequent and may put the mother and the baby at risk of adverse outcomes.
The maternal glucose should be maintained between 4.0 and 6.0-7.0 mmol/L during labor.Most women with gestational diabetes, especially if they require less than 1.0 units/kg/d of insulin, can simply be monitored without intravenous insulin.However, women who are taking medication for gestational diabetes require more frequent glucose monitoring, typically with hourly evaluations.
A nurse is assessing a newborn whose mother has gestational diabetes for signs of hypoglycemia.
The nurse should check the newborn’s blood glucose level within how many hours after birth?
Explanation
The correct answer is choice A. The nurse should check the newborn’s blood glucose level within one hour after birth.This is because newborns of mothers with gestational diabetes are at risk of developing hypoglycemia due to hyperinsulinemia.Hypoglycemia can cause neurological damage or death if not treated promptly.
Choice B is wrong because two hours may be too late to detect and treat hypoglycemia in a newborn at risk.
Choice C is wrong because three hours is definitely too late to check the blood glucose level of a newborn at risk of hypoglycemia.
Choice D is wrong because four hours is way too late to check the blood glucose level of a newborn at risk of hypoglycemia.
The normal blood glucose level for a newborn is between 70 and 150 mg/dL.However, some infants may have transient low blood glucose levels as low as 25 mg/dL within the first two hours of life, which is physiologic and self-limited.Infants with risk factors for hypoglycemia, such as maternal diabetes, should be screened at 2 hours of age and then before each feeding for the first and second days of life.A blood glucose level of less than 45 mg/dL in an asymptomatic infant or less than 36 mg/dL in a symptomatic infant is considered hypoglycemic and requires treatment.
A nurse is evaluating the effectiveness of nursing interventions for a pregnant woman who has gestational diabetes and received nutritional therapy and exercise counseling during pregnancy.
Which of the following outcomes indicates that the interventions were successful?
Explanation
The correct answer is choice B. The woman delivered a baby who weighed 3 kg (6.6 lb) at birth.
This indicates that the interventions were successful because the baby’s weight is within the normal range and not affected by gestational diabetes mellitus (GDM).According to one study, an ideal gestational weight gain (GWG) range for women with GDM is 8-11.9 kg for normal weight, 6-7.9 kg for overweight, and -5-3.9 kg for obesity.
Choice A is wrong because the woman gained less than 10 kg (22 lb) during pregnancy.This may be too low for a normal weight woman and may increase the risk of small for gestational age (SGA) or preterm birth.
Choice C is wrong because the woman had no episodes of hypoglycemia or hyperglycemia during pregnancy.
This may be a result of good blood glucose control, but it does not reflect the outcome of the interventions on the baby’s health.
Choice D is wrong because the woman’s blood glucose levels returned to normal within six weeks after delivery.This may happen in most women with GDM, but it does not indicate the effectiveness of the interventions during pregnancy.
A nurse is teaching a pregnant woman who has gestational diabetes about how to recognize and manage symptoms of hyperglycemia after delivery.
Which of the following statements by the woman indicates an understanding of the teaching?
Explanation
The correct answer is choice A. The woman should check her blood glucose levels four times a day to monitor and manage her condition.This will help her avoid complications such as ketoacidosis, hypoglycemia, or fetal macrosomia.
Choice B is wrong because drinking juice or soda can increase blood glucose levels and worsen hyperglycemia.The woman should drink water or sugar-free beverages if she feels thirsty.
Choice C is wrong because vaginal discharge or itching may indicate a yeast infection, which is more common in women with diabetes, but not a sign of hyperglycemia.The woman should report any signs of infection to her doctor, but also check her blood glucose levels regularly.
Choice D is wrong because stopping insulin or oral medication after delivery can cause blood glucose levels to rise and lead to diabetic ketoacidosis, a life-threatening condition.The woman should consult with her doctor before making any changes to her medication regimen.
Normal ranges for blood glucose levels during pregnancy are:
• Before meals: 60-99 mg/dL
• One hour after meals: 100-129 mg/dL
• Two hours after meals: <120 mg/dL
A nurse is teaching a client with gestational diabetes about the importance of attending regular prenatal appointments.
Which of the following statements accurately reflects the rationale behind this recommendation?
Explanation
The correct answer is choice A. Regular appointments allow for insulin therapy initiation if needed.This is because gestational diabetes is a condition in which women develop high blood sugar during pregnancy, which can cause complications for both the mother and the baby.Insulin is a hormone that helps lower blood sugar levels, and some women with gestational diabetes may need to take insulin injections to control their blood sugar.
Choice B is wrong because prenatal appointments do not help in diagnosing gestational diabetes.Gestational diabetes is usually diagnosed by a blood test that measures the glucose levels before and after meals.This test is typically done between 24 and 28 weeks of pregnancy.
Choice C is wrong because attending appointments does not ensure access to emotional support.Emotional support is important for pregnant women, especially those with gestational diabetes, but it can be provided by other sources such as family, friends, counselors or support groups.
Choice D is wrong because regular appointments do not allow for adjustment of insulin dosage.Insulin dosage is determined by the blood sugar levels of the woman, which she can monitor at home using a glucose meter.The doctor or midwife may adjust the insulin dosage based on the results of the blood tests and the feedback from the woman.
A client with gestational diabetes asks the nurse about the recommended types of exercise during pregnancy.
Which of the following responses by the nurse is correct?
Explanation
The correct answer is choice B. Walking, swimming, or prenatal yoga are moderate-intensity exercises that can improve insulin sensitivity.
This means that the body can use insulin more effectively to lower blood glucose levels.Exercise also has other benefits for pregnant women with gestational diabetes, such as reducing the risk of hypertension, preeclampsia, and macrosomia.
Choice A is wrong because engaging in high-intensity exercises such as weightlifting is not recommended for pregnant women with gestational diabetes.High-intensity exercises can increase blood pressure and stress hormones, which can raise blood glucose levels and cause complications.
Choice C is wrong because avoiding physical activity altogether is not recommended for pregnant women with gestational diabetes.Physical activity can help control blood glucose levels and prevent excessive weight gain, which can lead to adverse outcomes for both the mother and the baby.
Choice D is wrong because only strenuous exercises such as running are not effective in managing blood sugar levels.Strenuous exercises can also increase blood pressure and stress hormones, which can have negative effects on blood glucose levels and fetal well-being.Moderate-intensity exercises are preferred over strenuous exercises for pregnant women with gestational diabetes.
Normal ranges for blood glucose levels during pregnancy are 60 to 100 mg/dL before meals and bedtime snacks, and less than 140 mg/dL one hour after meals.
A nurse is instructing a client with gestational diabetes on carbohydrate counting.
Which of the following statements by the client indicates understanding of the teaching?
Explanation
The correct answer is choice C. “I will monitor my portion sizes and calculate the number of carbohydrates I consume.” This statement indicates that the client understands the concept of carbohydrate counting, which is a method of planning meals based on the amount and type of carbohydrates in foods.
Carbohydrate counting helps to control blood glucose levels by matching insulin or medication doses to carbohydrate intake.
Choice A is wrong because protein intake does not directly affect blood glucose levels, although it is important to consume adequate protein for overall health and fetal development.
Choice B is wrong because fruits and vegetables are good sources of carbohydrates, vitamins, minerals, and fiber, and should not be avoided.
However, they should be counted as part of the total carbohydrate intake.
Choice D is wrong because consuming unlimited amounts of carbohydrates, even from whole grains, can cause hyperglycemia and complications for the mother and the fetus.
Whole grains are preferable to refined grains because they have more fiber and nutrients, but they still need to be measured and counted as carbohydrates.
A client with gestational diabetes is prescribed insulin therapy.
The nurse is educating the client on proper insulin administration techniques.
Which of the following instructions should the nurse provide?
Explanation
The correct answer is choice C. The nurse should instruct the client to rotate injection sites to ensure consistent insulin absorption.Rotating injection sites helps prevent lipodystrophy, which is a condition that affects the subcutaneous fat tissue and can impair insulin absorption.
Choice A is wrong because injecting insulin directly into the umbilical area is not recommended for pregnant clients, as it may cause irritation or infection of the umbilical cord.
Choice B is wrong because needles should be disposed of in a puncture-resistant container, not in a regular trash bin, to prevent needlestick injuries.
Choice D is wrong because insulin vials should be stored in the refrigerator, not in the freezer, to maintain potency.Freezing can damage the insulin molecules and reduce their effectiveness.
A nurse is discussing dietary modifications with a client with gestational diabetes.
Which of the following food choices should the nurse recommend as part of a balanced meal plan?
Explanation
The correct answer is choice C. Grilled salmon and quinoa.
This food choice provides a good balance of protein, healthy fats, and complex carbohydrates that can help regulate blood glucose levels for a client with gestational diabetes.
Choice A is wrong because fried chicken and French fries are high in saturated fat and simple carbohydrates that can raise blood glucose levels and increase the risk of cardiovascular complications.
Choice B is wrong because processed deli meats and white bread are high in sodium, nitrates, and refined flour that can also increase blood glucose levels and blood pressure.
Choice D is wrong because sugary cereal and whole milk are high in sugar and lactose that can spike blood glucose levels and cause digestive issues.
A client with gestational diabetes should follow a balanced meal plan that includes lean protein, healthy fats, fiber, and complex carbohydrates that are low on the glycemic index.
The client should also limit intake of simple sugars, refined grains, fried foods, and processed meats.The client should monitor blood glucose levels regularly and consult with a dietitian for individualized recommendations.
Exams on Gestational Diabetes
Custom Exams
Login to Create a Quiz
Click here to loginGestational Diabetes
Lessons
 Naxlex
Just Now
Naxlex
Just Now
Login to View Gestational Diabetes Study Video
Notes Highlighting is available once you sign in. Login Here.
Objectives
- Define gestational diabetes and its causes
- Identify the risk factors and symptoms of gestational diabetes
- Explain the screening and diagnosis methods for gestational diabetes
- Describe the complications and treatment options for gestational diabetes
- Discuss the nursing interventions and patient education for gestational diabetes
- Summarize the main points of gestational diabetes
Antepartum Management: For HELLP syndrome
efwefqw23es
Introduction
Gestational diabetes is a type of diabetes that develops during pregnancy in women who do not already have diabetes.
Prevalence: It affects approximately 2-10% of pregnancies.
It affects how the cells use sugar (glucose), resulting in high blood sugar levels that can affect the pregnancy and the baby’s health.
It usually occurs in the second or third trimester of pregnancy and often goes away after giving birth.
However, it increases the risk of developing type 2 diabetes in the future for both the mother and the baby.
Causes
- The exact cause of gestational diabetes is not known, but it is related to hormonal changes during pregnancy that affect insulin production and action.
- Insulin is a hormone that helps the cells use glucose for energy. During pregnancy, the placenta produces hormones that make the cells more resistant to insulin, requiring more insulin to keep the blood sugar levels normal.
- If the pancreas cannot produce enough insulin to overcome the insulin resistance, the blood sugar levels rise and gestational diabetes develops.
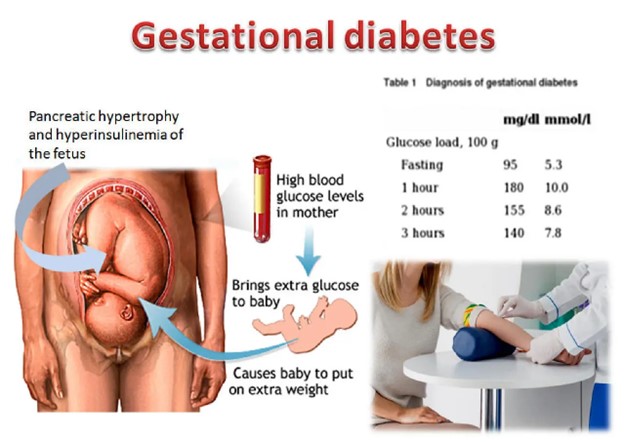
Risk Factors
- Any woman can develop gestational diabetes during pregnancy, but some factors increase the risk, such as:
- Being over 40 years old
- Having a body mass index (BMI) above 30
- Having a previous baby who weighed more than 4.5 kg (10 lb) at birth
- Having gestational diabetes in a previous pregnancy
- Having a parent or sibling with diabetes
- Being of south Asian, Black, African-Caribbean or Middle Eastern origin
- Having a history of polycystic ovary syndrome (PCOS) or other endocrine disorders
- Having a history of prediabetes or impaired glucose tolerance
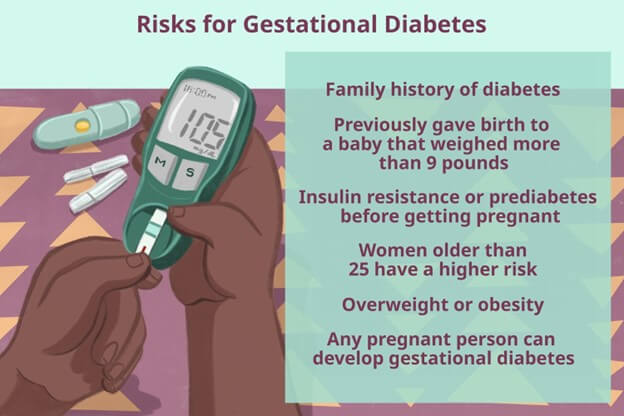
Symptoms
- Gestational diabetes does not usually cause any symptoms, and most cases are detected by routine screening tests during pregnancy.
- Some women may experience symptoms of high blood sugar (hyperglycemia), such as:
- Polyuria (increased urination) due to elevated blood glucose levels.
- Polydipsia (increased thirst) caused by dehydration secondary to polyuria.
- Excessive sweating
- Fatigue due to inadequate glucose utilization.
- Blurred vision
- Recurrent infections (e.g., urinary tract infections, vaginal yeast infections) due to increased glucose levels in body fluids.
- Genital itching or thrush

Screening and Diagnosis
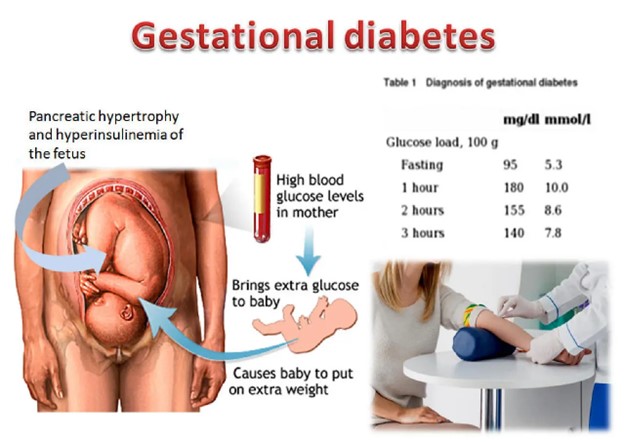
- Screening for gestational diabetes is part of the antenatal care for pregnant women. It is usually done between 24 and 28 weeks of gestation, or earlier if there are risk factors.
- The screening test involves measuring the blood sugar levels before and after drinking a sugary drink (glucose tolerance test). If the results are abnormal, a diagnosis of gestational diabetes is confirmed.
- The diagnosis criteria are based on the blood sugar levels at different time points after drinking the sugary drink:
|
Time |
Normal |
Gestational Diabetes |
|
Fasting (before drinking) |
Less than 92 mg/dL |
92 mg/dL or higher |
|
1 hour after drinking |
Less than 180 mg/dL |
180 mg/dL or higher |
|
2 hours after drinking |
Less than 153 mg/dL |
153 mg/dL or higher |
Complications
- Gestational diabetes can cause problems for both the mother and the baby if it is not well managed. Some of the possible complications are:
- Macrosomia: The baby grows larger than usual, which can lead to difficulties during delivery and increase the need for induced labor or cesarean section. (A birth weight of 4 kilograms (8.8 pounds) or higher is considered indicative of macrosomia.)
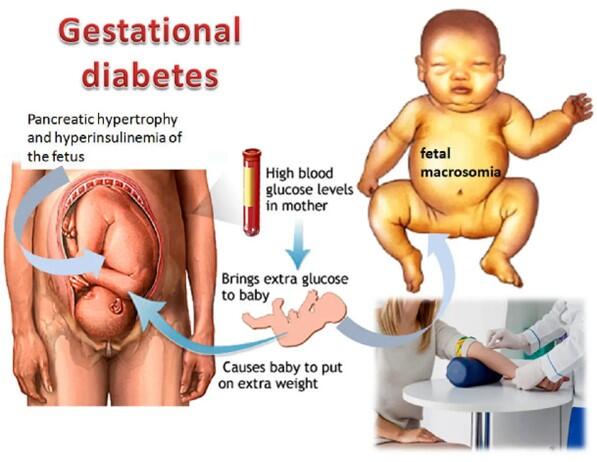
- Preterm birth: The baby is born before 37 weeks of gestation, which can increase the risk of respiratory distress syndrome, jaundice, low blood sugar, and other health problems.
- Preeclampsia: The mother develops high blood pressure and protein in the urine during pregnancy, which can lead to serious complications such as seizures, stroke, organ damage, or death if not treated.
- Hypoglycemia: The baby develops low blood sugar after birth due to excess insulin production, which can cause seizures, brain damage, or death if not treated. (Newborn hypoglycemia = 1 to 2 hours after birth: blood glucose less than 25 to 30 mg/dL)
- Jaundice: The baby develops yellowing of the skin and eyes due to high bilirubin levels in the blood, which can cause brain damage if not treated.
- Congenital anomalies – birth defects e.g sacral agenesis
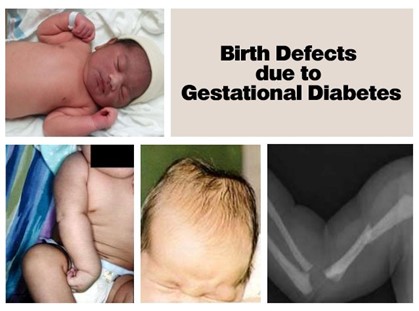
- Stillbirth: The baby dies in the womb after 20 weeks of gestation, which can be caused by poor placental function or uncontrolled blood sugar levels.
- Future diabetes: The mother and the baby have an increased risk of developing type 2 diabetes later in life.
Treatment
- The main goal of treatment for gestational diabetes is to keep the blood sugar levels within a normal range throughout pregnancy. This can be achieved by:
- Diet: Eating a balanced diet that provides adequate calories, protein, carbohydrates, fats, vitamins, and minerals for pregnancy. Avoiding foods that are high in sugar, fat, or salt. Eating smaller meals more frequently and limiting snacks between meals.
- Exercise: Engaging in moderate physical activity for at least 30 minutes a day, unless advised otherwise by a health care provider. Exercise can help lower blood sugar levels and improve insulin sensitivity.

- Monitoring: Checking blood sugar levels at home several times a day using a glucose meter. Keeping a record of the results and reporting any abnormal values to a health care provider.
- Medication: Taking insulin injections or oral antidiabetic drugs if diet and exercise are not enough to control blood sugar levels. Insulin is the preferred medication for gestational diabetes because it does not cross the placenta and affect the baby. Oral antidiabetic drugs such as metformin or glyburide may be used in some cases under close supervision by a health care provider.

- Follow-up: Having regular antenatal visits to monitor the progress of pregnancy and check for any complications. Having frequent ultrasound scans to assess the growth and development of the baby. Having a delivery plan that considers the best timing and mode of delivery for both mother and baby.
Nursing Interventions
- Screening:
- All pregnant women should be screened for gestational diabetes between 24 and 28 weeks of gestation using an oral glucose tolerance test (OGTT).
- Encourage compliance with the screening process and explain its importance in identifying and managing gestational diabetes.
- Provide instructions regarding fasting requirements and the procedure for the OGTT.
- Dietary Modifications:
- Collaborate with a registered dietitian to develop an individualized meal plan based on the woman's nutritional needs, blood glucose levels, and weight gain goals.
- Educate the woman about carbohydrate counting, meal timing, and portion control.
- Encourage regular meals and snacks to maintain stable blood glucose levels.
- Emphasize the importance of consuming a balanced diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats.
- Provide examples of appropriate food choices and meal combinations.
- Physical Activity:
- Encourage regular physical activity according to the woman's healthcare provider's recommendations.
- Advise the woman to engage in moderate-intensity exercises such as walking, swimming, or prenatal yoga.
- Explain that regular physical activity helps improve insulin sensitivity and glucose metabolism.
- Emphasize the importance of discussing exercise plans with the healthcare provider to ensure safety for both the woman and the fetus.
- Blood Glucose Monitoring:
- Teach the woman how to perform self-monitoring of blood glucose levels using a glucometer.
- Instruct her on the appropriate timing of blood glucose checks, target ranges, and recording the results.
- Discuss the significance of maintaining blood glucose levels within the recommended range to prevent complications.
- Review the symptoms of hypoglycemia and hyperglycemia and instruct the woman on appropriate actions to take if these occur.
- Insulin Administration (if needed):
- If dietary modifications and physical activity alone are insufficient to control blood glucose levels, insulin therapy may be initiated.
- Provide education on insulin administration techniques, including proper injection sites, needle disposal, and rotation of injection sites.
- Teach the woman about insulin storage, handling, and the importance of adhering to the prescribed dosage and schedule.
- Emphasize the need for regular follow-up appointments to assess glycemic control and adjust insulin therapy if necessary.
- Education and Support:
- Provide comprehensive education on gestational diabetes, its management, and potential complications.
- Discuss the importance of attending regular prenatal appointments and collaborating with the healthcare team.
- Offer emotional support and address any concerns or fears the woman may have regarding her diagnosis and its impact on her pregnancy.
- Connect the woman with support groups or resources that specialize in gestational diabetes for additional guidance and encouragement.
Patient Education
- Patient education is an essential component of nursing care for gestational diabetes. It helps pregnant women understand their condition and how to manage it effectively. Some of the topics that should be covered are:
- What is gestational diabetes and what causes it?
- What are the risks and complications of gestational diabetes for both mother and baby?
- How is gestational diabetes diagnosed and monitored?
- How can gestational diabetes be treated with diet, exercise, medication, etc.?
- How can gestational diabetes affect labor and delivery?
- How can gestational diabetes affect breastfeeding?
- How can gestational diabetes affect future health for both mother and baby?
- What are some resources and support groups available for women with gestational diabetes?
Summary
- Gestational diabetes is a type of diabetes that develops during pregnancy in women who do not already have diabetes.
- It is caused by hormonal changes during pregnancy that affect insulin production and action.
- It can cause problems for both mother and baby if not well managed such as macrosomia; preterm birth; preeclampsia; hypoglycemia; jaundice; stillbirth; future diabetes; etc.
- It is diagnosed by screening tests that measure blood sugar levels before and after drinking a sugary drink between 24 and 28 weeks of gestation.
- It is treated by keeping blood sugar levels within a normal range throughout pregnancy with diet; exercise; monitoring; medication; follow-up; etc.
- Nursing interventions include assessing; planning; implementing; evaluating; patient education; etc
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Gestational Diabetes
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


