Please set your exam date
Disorders of Anxiety
Study Questions
Clinical Manifestations and Diagnostic Criteria
Explanation
Choice A rationale:
Presence of delusions. Delusions are false beliefs that are not based in reality and are more commonly associated with psychotic disorders such as schizophrenia. Anxiety disorders primarily involve excessive fear or worry, not delusional thinking.
Choice B rationale:
Excessive fear or worry. This is the primary characteristic of anxiety disorders. Individuals with anxiety disorders experience intense and persistent fear or worry that is out of proportion to the actual threat or situation. This heightened anxiety can significantly impact their daily functioning.
Choice C rationale:
Hallucinations. Hallucinations involve perceiving sensory experiences that are not actually present, such as hearing voices or seeing things that others cannot see. Hallucinations are more typical of psychotic disorders and are not a primary characteristic of anxiety disorders.
Choice D rationale:
Impaired social skills. While individuals with anxiety disorders might experience impaired social interactions due to their anxiety symptoms, impaired social skills are not the primary characteristic of anxiety disorders. The key feature is excessive fear or worry.
Explanation
Choice A rationale:
Elevated mood. Elevated mood refers to a heightened emotional state often associated with conditions like mania in bipolar disorder. It is not a typical sign of anxiety disorders.
Choice B rationale:
Avoidance of feared situations. Individuals with anxiety disorders often try to avoid situations or triggers that provoke their anxiety. This avoidance behavior is a coping mechanism aimed at reducing anxiety and is common in disorders like agoraphobia and social anxiety disorder.
Choice C rationale:
Decreased heart rate. Anxiety typically leads to an increased heart rate due to the body's fight-or-flight response. A decreased heart rate is not a common sign of anxiety disorders.
Choice D rationale:
Compulsive behaviors. Compulsions are repetitive behaviors performed in response to obsessive thoughts. They are characteristic of obsessive-compulsive disorder (OCD), which is an anxiety disorder.
Choice E rationale:
Increased appetite. While some individuals may experience a loss of appetite due to anxiety, others might have an increased appetite. Emotional eating as a response to anxiety can lead to overeating and weight gain.
Explanation
Choice A rationale:
"You're experiencing excessive and persistent worry that's hard to control, right?" This statement accurately reflects the nature of generalized anxiety disorder (GAD). GAD is characterized by excessive and uncontrollable worry about various aspects of life, even when there is no apparent reason for concern.
Choice B rationale:
"I understand that you're having panic attacks followed by persistent concern." This statement describes panic disorder, where panic attacks are followed by worry about having more panic attacks or their consequences.
Choice C rationale:
"Your fear of specific objects or situations is leading to avoidance behavior, correct?" This statement is more aligned with specific phobias, where individuals experience intense fear and go to great lengths to avoid the specific trigger.
Choice D rationale:
"It sounds like you're dealing with recurrent intrusive thoughts and behaviors." This description is characteristic of obsessive-compulsive disorder (OCD), not generalized anxiety disorder. OCD involves intrusive thoughts and the need to perform compulsive behaviors to alleviate distress.
Explanation
Choice A rationale:
"You're experiencing marked fear of specific objects, right?" This statement relates to specific phobias, where individuals have intense fear of particular objects or situations, which is not indicative of panic disorder.
Choice B rationale:
"Your fear of open spaces is leading to avoidance behavior, correct?" This choice reflects agoraphobia, where individuals fear and avoid places or situations where they might feel trapped or helpless, often due to fear of having a panic attack. However, panic disorder involves unexpected panic attacks without the specific trigger of open spaces.
Choice C rationale:
"You're having unexpected panic attacks followed by persistent fear, aren't you?" This statement accurately represents panic disorder. Individuals with panic disorder experience recurrent, unexpected panic attacks, often followed by apprehension about having more attacks or the consequences of the attacks. This persistent fear of future attacks is a key diagnostic criterion for panic disorder.
Choice D rationale:
"It sounds like you're dealing with obsessions and compulsions." This choice pertains to obsessive-compulsive disorder (OCD), which involves intrusive thoughts (obsessions) and repetitive behaviors or mental acts (compulsions). This is distinct from panic disorder.
Explanation
Choice A rationale:
"High self-esteem." High self-esteem is not a risk factor for anxiety disorders. In fact, low self-esteem may contribute to the development of anxiety disorders.
Choice B rationale:
"Absence of stressors." While chronic stressors can contribute to the development of anxiety disorders, the absence of stressors does not increase the risk. Genetic, environmental, and psychological factors play a more significant role.
Choice C rationale:
"Family history of anxiety disorders." This is the correct answer. Anxiety disorders have a clear genetic component, and individuals with a family history of anxiety disorders are at a higher risk of developing these disorders themselves.
Choice D rationale:
"Minimal life changes." This choice does not accurately reflect the risk factors for anxiety disorders. Major life changes, rather than minimal ones, can contribute to the development of anxiety disorders.
Explanation
Choice A rationale:
"Hyperventilation." Hyperventilation is a physiological symptom rather than a cognitive symptom. It can occur during anxiety or panic attacks but does not represent a cognitive aspect.
Choice B rationale:
"Restlessness." Restlessness is a behavioral symptom associated with anxiety disorders but does not specifically involve cognitive aspects.
Choice C rationale:
"Confusion." Confusion can be related to various conditions, but it is not a cognitive symptom commonly associated with anxiety disorders.
Choice D rationale:
"Compulsive behaviors." Compulsive behaviors are characteristic of OCD, not generalized anxiety disorder or other anxiety disorders.
Choice E rationale:
"Excessive fear or worry." This choice accurately represents a cognitive symptom commonly associated with anxiety disorders. Excessive fear or worry, often about various aspects of life, is a hallmark cognitive feature of generalized anxiety disorder and other anxiety disorders.
Explanation
Avoidance of stimuli related to the traumatic event.
Choice A rationale:
Elevated mood is not a characteristic symptom of PTSD. Individuals with PTSD often experience mood disturbances such as depression, irritability, and hypervigilance, but elevated mood is not a defining feature.
Choice B rationale:
Avoidance of stimuli related to the traumatic event is a hallmark symptom of PTSD. Individuals with PTSD actively avoid reminders, situations, or people that trigger memories of the traumatic event. This avoidance behavior helps them cope with distressing memories and emotions associated with the trauma.
Choice C rationale:
Reduced anxiety is not typically associated with PTSD. In fact, individuals with PTSD often experience heightened anxiety, hyperarousal, and exaggerated startle responses due to their trauma-related symptoms.
Choice D rationale:
Excessive energy is not a primary symptom of PTSD. Individuals with PTSD commonly experience symptoms of emotional numbing, fatigue, and difficulty concentrating, which are contrary to the idea of excessive energy.
Choice E rationale:
Compulsive behaviors are not a defining characteristic of PTSD. While individuals with PTSD may develop certain rituals or behaviors as a way to manage anxiety or distress, compulsions are more characteristic of obsessive-compulsive disorder (OCD) rather than PTSD.
Explanation
Cognitive-behavioral therapy (CBT).
Choice A rationale:
Relaxation techniques can be helpful in managing anxiety, but they do not involve exposing the client to feared situations. Relaxation techniques focus on calming the mind and body through methods like deep breathing and progressive muscle relaxation.
Choice B rationale:
Herbal remedies are not directly related to exposure-based anxiety treatment. They involve the use of natural substances to potentially alleviate symptoms but do not address the underlying fear response through controlled exposure.
Choice C rationale:
Cognitive-behavioral therapy (CBT) is the modality that involves reducing anxiety by exposing the client to the feared situation in a controlled manner. This process is called exposure therapy. CBT also incorporates cognitive restructuring to challenge and modify irrational thoughts and beliefs that contribute to anxiety.
Choice D rationale:
Medication therapy may include anti-anxiety medications, but it does not involve exposure to feared situations. Medications can help alleviate symptoms, but they do not target the underlying behavioral and cognitive responses that exposure-based therapies address.
Choice E rationale:
Complementary therapy is a broad category that includes various alternative treatments, but it doesn't specifically focus on exposure-based interventions for anxiety. Complementary therapies may include practices like acupuncture, massage, or meditation, which are not synonymous with exposure therapy.
Nursing Interventions and Pharmacological Treatments
Explanation
Assist the client in challenging irrational thoughts.
Choice A rationale:
While medication may be a part of the treatment plan, the primary goal of establishing a therapeutic relationship is not to immediately prescribe medication. Building trust, rapport, and understanding the client's needs are initial priorities.
Choice B rationale:
Educating the client about relaxation techniques can be helpful, but the primary goal is to address the cognitive and emotional aspects of anxiety. Challenging irrational thoughts is a more central focus.
Choice C rationale:
The primary goal of establishing a therapeutic relationship with a client with anxiety disorder is to assist the client in challenging irrational thoughts. This involves identifying distorted thought patterns and helping the client reframe or replace these thoughts with more realistic and balanced ones.
Choice D rationale:
Developing measurable and realistic outcomes is an important aspect of the therapeutic process, but it is not the primary goal of establishing the therapeutic relationship. Measurable outcomes come after working through various therapeutic interventions.
(Select all that apply):A nurse is providing education to a client with anxiety disorder. Which of the following are appropriate techniques for relaxation that the nurse might teach the client? Select all that apply.
Explanation
Choice A rationale:
Deep breathing is an appropriate relaxation technique for a client with anxiety disorder. It involves taking slow, deep breaths to activate the body's relaxation response. Deep breathing helps reduce the sympathetic nervous system's activity, leading to a calmer state. This technique is effective in lowering heart rate and blood pressure.
Choice D rationale:
Guided imagery is another suitable relaxation technique. It involves using mental visualization to create calming and peaceful images in the mind. Guided imagery can divert the client's attention away from stressors, promoting relaxation. This technique has been shown to reduce anxiety and promote a sense of well-being.
Choice B rationale:
Vigorous exercise is not typically recommended as a relaxation technique for individuals with anxiety disorder. While regular exercise has many benefits for mental health, intense exercise might actually increase physiological arousal and exacerbate anxiety symptoms.
Choice C rationale:
Hyperventilation is an inappropriate technique for relaxation. It involves rapid and shallow breathing, which can lead to an imbalance in oxygen and carbon dioxide levels, resulting in dizziness, tingling sensations, and increased anxiety. This technique is counterproductive and can trigger panic attacks.
Choice E rationale:
Critical thinking exercises are not commonly used as relaxation techniques. These exercises engage the mind in problem-solving activities, which might not be suitable for promoting immediate relaxation. Instead, the focus should be on techniques that calm the body and mind.
A nurse is assessing a client's level of anxiety and coping mechanisms. Which statement by the nurse is appropriate during the assessment?
Explanation
Choice A rationale:
Asking the client about their favorite hobbies is an appropriate statement during the assessment. This open-ended question encourages the client to talk about positive and enjoyable aspects of their life, providing insight into their interests and potential sources of relaxation. It also helps build rapport and trust between the nurse and the client.
Choice B rationale:
Advising the client to avoid anxiety-inducing situations oversimplifies anxiety management. Avoidance can reinforce anxiety and prevent the client from developing effective coping strategies. Encouraging gradual exposure to manageable stressors is often a more helpful approach.
Choice C rationale:
Asking "Why do you feel this way?" can be perceived as confrontational and may put the client on the defensive. It might hinder open communication and prevent the client from fully expressing their feelings. Instead, using more open-ended and nonjudgmental questions is recommended.
Choice D rationale:
Minimizing anxiety by stating that "Anxiety is not a big deal, everyone feels it sometimes" is dismissive of the client's emotions. It invalidates their experience and fails to acknowledge the impact anxiety may have on their well-being. Providing empathy and understanding is crucial in therapeutic communication.
Explanation
Choice C rationale:
Responding with empathy and validation, such as acknowledging the client's concerns about starting therapy, is appropriate communication. It demonstrates the nurse's understanding of the client's feelings and helps establish a supportive and trusting relationship. Many individuals with anxiety disorder have reservations about therapy, and addressing their concerns can alleviate some of their apprehensions.
Choice A rationale:
Suggesting that "Therapy won't really help, but you should try it anyway" is discouraging and undermines the potential benefits of therapy. It may lead to decreased motivation and engagement in the therapeutic process.
Choice B rationale:
Instructing the client to solely rely on medications oversimplifies treatment and disregards the potential effectiveness of therapy and other coping strategies. Medications can be a part of the treatment plan, but a comprehensive approach is usually recommended.
Choice D rationale:
Advising the client to rely on friends and family for support instead of seeking professional help minimizes the importance of therapeutic interventions. While social support is valuable, it is not a substitute for evidence-based treatments for anxiety disorder.
Explanation
Choice A rationale:
Blocking the effects of adrenaline is not the mechanism of action for anxiolytics. Anxiolytics primarily target neurotransmitter systems in the brain, not adrenaline (also known as epinephrine) pathways.
Choice B rationale:
Increasing the availability of neurotransmitters is not the primary mechanism of anxiolytics. While neurotransmitters are involved, anxiolytics like benzodiazepines and SSRIs focus on specific neurotransmitter systems, such as GABA (gamma-aminobutyric acid) and serotonin, rather than merely increasing neurotransmitter availability.
Choice C rationale:
Modulating the activity of glutamate is not the primary mechanism of anxiolytics. Glutamate is an excitatory neurotransmitter, and its modulation is more relevant to agents used in conditions like schizophrenia, rather than anxiety disorders.
Choice D rationale:
Enhancing the activity of serotonin and norepinephrine is the correct mechanism of anxiolytics. Medications like SSRIs (Selective Serotonin Reuptake Inhibitors) and SNRIs (Serotonin-Norepinephrine Reuptake Inhibitors) work by increasing the levels of these neurotransmitters in the brain. Serotonin and norepinephrine play critical roles in mood regulation and anxiety modulation.
Explanation
Choice A rationale:
Establishing a therapeutic relationship is essential for effective care, but it is not directly aimed at promoting coping skills and enhancing self-esteem. It's a foundational aspect of nursing care, focusing on building trust and rapport with the client.
Choice B rationale:
Teaching relaxation techniques is the correct intervention for promoting coping skills and enhancing self-esteem. Relaxation techniques, such as deep breathing, progressive muscle relaxation, and mindfulness, empower clients to manage their anxiety and build self-confidence.
Choice C rationale:
Providing a safe environment is important in a clinical setting, but it doesn't directly address promoting coping skills or enhancing self-esteem. This intervention contributes to the client's overall well-being and sense of security.
Choice D rationale:
Referring to support groups can be valuable for clients with anxiety disorders, but it doesn't directly involve teaching coping skills or enhancing self-esteem. Support groups provide social connections and a platform for shared experiences.
Explanation
Choice A rationale:
Fluoxetine is an example of an SSRI (Selective Serotonin Reuptake Inhibitor), which is commonly prescribed for anxiety disorders and depression. It increases serotonin levels in the brain, helping to alleviate anxiety symptoms.
Choice B rationale:
Alprazolam is a benzodiazepine that enhances the effects of GABA, a neurotransmitter that reduces brain activity, leading to sedative and anxiolytic effects. It's used to treat anxiety disorders, although it can be habit-forming and is usually prescribed for short-term use.
Choice C rationale:
Propranolol is a beta-blocker that primarily treats hypertension and certain cardiac conditions, but it can also be used to manage the physical symptoms of anxiety, such as rapid heart rate and tremors.
Choice D rationale:
Gabapentin is not a first-line treatment for anxiety disorders, but it's sometimes used off-label to manage anxiety symptoms. It modulates the release of certain neurotransmitters, which can have a calming effect.
Choice E rationale:
Diphenhydramine is an antihistamine commonly used for allergies and as a sleep aid. It's not a standard pharmacological treatment for anxiety disorders.
Explanation
"I understand your concerns. Let's discuss the potential side effects so you're prepared."
Choice A rationale:
This choice suggests a directive approach that disregards the client's apprehensions. Anxiety disorders often involve heightened sensitivity, and this response might exacerbate the client's distress.
Choice B rationale:
Choice B downplays the significance of side effects, which may undermine the client's worries. While some side effects might indeed be minimal, it's essential to address the client's concerns more empathetically.
Choice C rationale:
This is the appropriate response. Acknowledging the client's concerns and offering to discuss potential side effects in a supportive manner is a therapeutic approach. It promotes open communication, empowers the client, and helps them make informed decisions.
Choice D rationale:
Choice D dismisses the client's worries and could invalidate their feelings. It's important to avoid belittling the client's concerns, as it may hinder the development of a trusting nurse-client relationship.
Explanation
"Tell me about your favorite hobbies."
Choice A rationale:
Asking about hobbies is a non-threatening way to initiate the assessment while building rapport. This choice encourages the client to discuss positive aspects of their life, potentially lowering anxiety levels.
Choice B rationale:
Suggesting avoidance might not be suitable for assessment. While avoidance might reduce immediate anxiety, it's not a healthy long-term coping mechanism. This statement overlooks the opportunity to explore healthier strategies.
Choice C rationale:
This open-ended question might be too probing for an initial assessment. It could make the client defensive or overwhelmed and might not yield comprehensive information about their anxiety and coping mechanisms.
Choice D rationale:
This statement invalidates the client's feelings and suggests that anxiety is insignificant. It fails to acknowledge the client's experiences and discourages open expression.
Explanation
"Development of coping skills."
Choice A rationale:
Increased risk of depression is not a positive outcome of nursing interventions. The goal is to alleviate symptoms and improve the client's well-being, not to introduce new mental health challenges.
Choice B rationale:
Reduced adherence to medical treatment is a negative outcome. It suggests that the client's anxiety might be interfering with their ability to follow recommended treatments, which is undesirable.
Choice C rationale:
This is the correct choice. Developing coping skills is a positive outcome. It indicates that the client is learning effective ways to manage their anxiety, enhancing their overall quality of life.
Choice D rationale:
Impairment in personal domains is a negative outcome. Nursing interventions aim to improve functioning and minimize impairment, so this choice contradicts the therapeutic goals.
Generalized anxiety disorder (GAD)
Generalized anxiety disorder (GAD)
Explanation
Difficulty concentrating.
Choice A rationale:
Mood swings are not the primary characteristic of generalized anxiety disorder (GAD) GAD primarily involves excessive and persistent worry and anxiety, rather than mood swings.
Choice B rationale:
Difficulty concentrating is the primary characteristic of GAD. One of the core symptoms of GAD is the inability to focus or concentrate due to constant worry and anxiety. This cognitive impairment can significantly impact daily functioning.
Choice C rationale:
Muscle pain is not the primary characteristic of GAD. While muscle tension is a common symptom of GAD, it is not the main characteristic that distinguishes GAD from other disorders.
Choice D rationale:
Chest pain is not the primary characteristic of GAD. Chest pain might be associated with anxiety, but it's not the defining feature of GAD. GAD primarily involves excessive and uncontrollable worry.
Explanation
Choice A:
Fatigue,
Choice C:
Nausea,
Choice D:
Restlessness.
Choice A rationale:
Fatigue is commonly associated with GAD. The constant state of worry and the physical tension that accompanies anxiety can lead to fatigue and a feeling of being mentally and physically drained.
Choice B rationale:
Hypertension is not a commonly associated clinical manifestation of GAD. While anxiety can temporarily elevate blood pressure, it's not a defining feature of GAD.
Choice C rationale:
Nausea can be a common symptom of GAD. Anxiety and stress can lead to gastrointestinal distress, including nausea and even vomiting, in individuals with GAD.
Choice D rationale:
Restlessness is a common manifestation of GAD. Individuals with GAD often experience restlessness, an inability to sit still, and a constant feeling of being on edge.
Choice E rationale:
Hallucinations are not commonly associated with GAD. Hallucinations involve perceptual experiences that are not based in reality, and they are more characteristic of other mental health conditions such as schizophrenia, not GAD.
Explanation
"Excessive worry is a key feature of GAD."
Choice A rationale:
This statement is incorrect. GAD involves excessive worry about a wide range of situations, not just those that are likely to happen. The worry is often disproportionate to the actual circumstances.
Choice B rationale:
This statement is incorrect. GAD can significantly impact daily life by causing distress, impairing concentration, and affecting decision-making and problem-solving abilities.
Choice C rationale:
This statement is incorrect. GAD involves uncontrollable worry that is difficult to manage, rather than easy to control whenever it arises.
Choice D rationale:
This statement is correct. Excessive worry is indeed a key feature of GAD. Individuals with GAD experience persistent and excessive worry about various aspects of their life, often accompanied by physical symptoms such as restlessness, muscle tension, and fatigue. This worry is difficult to control and can lead to significant distress and impairment in daily functioning.
Explanation
"Facing your fears gradually can be an effective strategy."
Choice A rationale:
Telling the client that avoiding triggers will help overcome anxiety might inadvertently reinforce avoidance behaviors, which can worsen anxiety over time. Avoidance prevents the client from developing coping skills and facing their fears, hindering their progress in managing anxiety.
Choice B rationale:
This response is appropriate because it supports the principle of exposure therapy, a widely recognized approach for anxiety disorders. Gradually confronting anxiety triggers in a controlled manner can help desensitize the client to those triggers and reduce anxiety over time. By facing fears, the client learns to manage their anxiety in real-life situations, leading to improved overall functioning.
Choice C rationale:
Indicating that avoidance is the best way to manage anxiety is incorrect. Avoidance perpetuates anxiety by preventing the client from learning how to cope with triggers and situations that provoke anxiety. Over time, avoidance can lead to greater distress and impairment in daily life.
Choice D rationale:
Stating that avoiding triggers is a permanent solution for GAD is inaccurate. Avoidance only offers temporary relief and does not address the underlying anxiety or provide long-term strategies for managing it. Without proper intervention, the client's anxiety is likely to persist and even worsen.
Explanation
"Extroverted personality traits."
Choice A rationale:
Having a family history of anxiety disorders can increase the risk of developing GAD due to genetic factors and shared environmental influences. Genetic predisposition contributes to the vulnerability to anxiety disorders.
Choice B rationale:
Chronic medical conditions can contribute to the development of GAD. Living with ongoing health concerns and uncertainties about one's health status can lead to chronic worry and anxiety.
Choice C rationale:
Extroverted personality traits are not typically associated with an increased risk of GAD. Instead, introverted traits and tendencies toward overthinking, perfectionism, and excessive worry are more closely linked to the development of GAD.
Choice D rationale:
A history of trauma or abuse is a well-established risk factor for GAD. Traumatic experiences can result in heightened anxiety responses and the development of anxiety disorders as a way of coping with the trauma.
Explanation
"Personal history of trauma and abuse."
Choice A rationale:
While family history of physical illnesses can contribute to a client's overall health profile, it is not a priority when assessing a client specifically for generalized anxiety disorder (GAD)
Choice B rationale:
Prioritizing obtaining information about a personal history of trauma and abuse is crucial because such experiences can significantly contribute to the development of GAD. Trauma and abuse can lead to chronic worry, hypervigilance, and increased anxiety responses.
Choice C rationale:
While the level of physical activity can impact a person's well-being, it is not a primary focus when assessing for GAD. The client's anxiety symptoms and triggers should take precedence during the assessment.
Choice D rationale:
Inquiring about the preferred type of relaxation technique is relevant but not as high a priority as understanding potential trauma and abuse history. Addressing trauma-related issues is fundamental to developing an effective treatment plan for GAD.
Explanation
Choice A rationale:
Encouraging participation in cognitive-behavioral therapy (CBT) is appropriate for a client with Generalized Anxiety Disorder (GAD) CBT is a well-established therapeutic approach for managing GAD. It helps the client identify and challenge their anxious thoughts, promoting healthier cognitive patterns. This intervention aids in reducing the excessive worry and anxiety associated with GAD.
Choice B rationale:
Advising against any form of physical activity is not appropriate for a client with GAD. Regular physical activity has been shown to have positive effects on mental health, including reducing anxiety symptoms. Engaging in exercise can help alleviate stress and tension, making this option counterproductive for managing GAD.
Choice C rationale:
Suggesting excessive consumption of caffeine is not appropriate for a client with GAD. Caffeine is a stimulant that can exacerbate anxiety symptoms. It can increase restlessness, heart palpitations, and contribute to racing thoughts – all of which are already heightened in individuals with GAD.
Choice D rationale:
Teaching deep breathing techniques is appropriate for a client with GAD. Deep breathing can help activate the body's relaxation response and decrease physiological symptoms of anxiety. It is a simple and effective coping strategy that the client can use to manage anxiety symptoms, especially during moments of heightened distress.
Choice E rationale:
Discouraging seeking social support is not appropriate for a client with GAD. Social support plays a crucial role in managing anxiety. Connecting with friends, family, or support groups can provide emotional reassurance, understanding, and an opportunity for the client to express their feelings. Isolation, on the other hand, can worsen anxiety.
A nurse observes a client with GAD exhibiting restlessness, difficulty concentrating, and irritability. The client says, "I can't sit still, and my mind is racing." How should the nurse respond?
Explanation
Choice D rationale:
Responding with "I understand you're having trouble focusing" is how the nurse should appropriately respond. This response acknowledges the client's experience and shows understanding of their symptoms. It encourages further communication and allows the client to express their feelings. It's important to address the client's restlessness, difficulty concentrating, and racing thoughts rather than attributing them to tiredness (Choice C) or suggesting keeping busy (Choice B), which may not address the underlying anxiety.
Choice A rationale:
Responding with "You seem to be experiencing a lot of physical symptoms" might overlook the underlying anxiety and focus solely on the physical aspects, missing the opportunity to explore the client's emotional state and provide appropriate support.
Explanation
Choice A rationale:
GAD is not a temporary condition that usually resolves on its own. Generalized Anxiety Disorder (GAD) is a chronic mental health condition characterized by persistent and excessive worry and anxiety that lasts for at least six months. It does not typically resolve spontaneously.
Choice B rationale:
GAD is not characterized by occasional episodes of extreme anxiety. Instead, it involves constant and chronic worry that is difficult to control and interferes with daily functioning.
Choice C rationale:
GAD is not more prevalent in men and individuals without a family history of mental illness. In fact, GAD is more commonly diagnosed in women and individuals with a family history of anxiety or mood disorders.
Choice D rationale:
This is the correct choice. GAD involves excessive and uncontrollable worry about various aspects of life, such as health, work, relationships, and everyday situations. This worry is often disproportionate to the actual situation and can cause significant distress and impairment in daily life.
Explanation
Choice A rationale:
This is the most pertinent information to obtain during the assessment of a client with GAD. Knowing the client's preferred relaxation technique can help tailor interventions to manage their anxiety effectively.
Choice B rationale:
While family history of physical illnesses can be relevant, it is not the priority when assessing a client with GAD. The focus should be on understanding the client's anxiety symptoms and coping mechanisms.
Choice C rationale:
The client's level of physical activity can be important, but it is not as directly related to managing GAD as understanding their preferred relaxation techniques.
Choice D rationale:
Recent social interactions may be relevant, but they are not as crucial as identifying the client's preferred methods of relaxation in order to address their anxiety symptoms.
Explanation
Choice A rationale:
Cognitive-behavioral therapy (CBT) is a well-established and effective intervention for GAD. It helps individuals recognize and change negative thought patterns and develop coping strategies to manage anxiety.
Choice B rationale:
Excessive consumption of caffeine is not appropriate for managing GAD. Caffeine can exacerbate anxiety symptoms and should be limited.
Choice C rationale:
Deep breathing techniques are helpful for managing anxiety symptoms in the moment. Teaching clients how to engage in deep, slow breathing can help them reduce their immediate feelings of anxiety.
Choice D rationale:
Encouraging social isolation is not appropriate for GAD management. Social support and interactions are important for overall mental well-being.
Choice E rationale:
Advising against any form of physical activity is not recommended. Regular physical activity can have a positive impact on mental health and can help alleviate anxiety symptoms.
Explanation
Choice A rationale:
"Try not to think about it too much." This response might invalidate the client's feelings and minimize their experience. It fails to address the client's concerns and could potentially increase their anxiety.
Choice B rationale:
"You're likely overthinking things; just relax." This response oversimplifies the client's experience and doesn't acknowledge the severity of their anxiety. It might come across as dismissive and unhelpful.
Choice C rationale:
"It seems like you're experiencing a lot of anxiety." This response validates the client's feelings and directly addresses their statement. It shows empathy and understanding, creating a supportive environment for further discussion about their anxiety.
Choice D rationale:
"Don't worry; these thoughts will pass soon." This response might be misleading and inaccurate. It doesn't provide any substantial help for managing the client's anxiety and could create false expectations.
Explanation
Choice A rationale:
"The client might have consumed excess caffeine." While excess caffeine intake can contribute to restlessness and a racing mind, the client's symptoms are more indicative of anxiety. This option ignores the possibility of an underlying mental health issue.
Choice B rationale:
Choice C rationale:
Choice D rationale:
"The client is probably feeling overwhelmed by anxiety." This response directly correlates the observed symptoms (restlessness, difficulty concentrating, racing thoughts) with anxiety, which is a common manifestation of Generalized Anxiety Disorder (GAD)
Explanation
Choice A rationale:
"GAD predominantly affects men." GAD actually affects both men and women, with a higher prevalence in women. This statement is inaccurate and gender-biased.
Choice B rationale:
"GAD symptoms are always temporary and go away on their own." GAD symptoms are persistent and chronic without intervention. This option provides misleading information that could lead to misunderstanding and lack of appropriate treatment.
Choice C rationale:
"GAD involves excessive and uncontrollable worry about various aspects of life." This statement accurately describes a core characteristic of Generalized Anxiety Disorder. People with GAD experience pervasive worry that is difficult to control and often extends beyond specific triggers.
Choice D rationale:
"GAD is primarily caused by physical health issues." While physical health issues can contribute to anxiety, GAD is a complex condition influenced by various factors including genetics, brain chemistry, and life experiences. This option oversimplifies the disorder's etiology.
Panic Disorder
A client with GAD states, "I'm always worried that something bad will happen. I can't control my thoughts." What is the nurse's appropriate response?
Explanation
Choice C rationale:
Responding with "It sounds like you're feeling overwhelmed by your thoughts" is the nurse's appropriate response. This response reflects therapeutic communication by acknowledging the client's feelings and demonstrating empathy. It validates the client's experience and opens the door for further exploration of their worries. It also avoids downplaying the client's concerns (Choice B) or giving false reassurance (Choice D), both of which are unhelpful in this situation.
Panic Disorder
Explanation
Choice A rationale:
The statement "I think my panic attacks are caused by a specific substance I'm using" suggests a possible link between substance use and panic attacks, which is not a typical characteristic of panic disorder. Panic disorder is primarily characterized by recurrent and unexpected panic attacks, not necessarily triggered by specific substances.
Choice B rationale:
The statement "I avoid situations that might trigger my panic attacks" reflects an understanding of the disorder. People with panic disorder often develop avoidance behaviors to prevent or minimize the occurrence of panic attacks. Avoidance of triggers is a common coping mechanism used to manage the fear associated with panic attacks.
Choice C rationale:
The statement "I don't worry about having more panic attacks" contradicts the typical experience of individuals with panic disorder. People with panic disorder often have heightened worry and fear about experiencing more panic attacks, which contributes to the cycle of anxiety.
Choice D rationale:
The statement "I believe my panic attacks are a result of a physical health problem" suggests a misunderstanding of panic disorder. While panic attacks can manifest with physical symptoms, they are primarily caused by psychological factors, such as anxiety and fear, rather than solely by physical health problems.
Explanation
Choice A rationale:
Palpitations, or a racing heart, are a common symptom of panic attacks. The body's "fight or flight" response during a panic attack can lead to rapid heart rate and sensations of palpitations.
Choice B rationale:
Numbness and tingling sensations, often referred to as paresthesias, can occur during a panic attack. These sensations are a result of the body's physiological response to stress, leading to altered sensory perceptions.
Choice D rationale:
Fear of losing control is a characteristic symptom of panic attacks. Individuals with panic disorder often describe feeling as though they are losing control over their thoughts, emotions, or even their physical actions during an attack.
Choice E rationale:
Muscle weakness can be experienced during a panic attack due to the release of stress hormones and the physiological changes that accompany the fight-or-flight response. This weakness can affect various muscle groups.
Choice C rationale:
Increased appetite is not typically associated with panic attacks. Panic attacks are more commonly associated with gastrointestinal symptoms such as nausea or stomach discomfort rather than an increased appetite.
Explanation
Choice A rationale:
The statement "I don't think I'll ever be able to control my panic attacks" indicates a negative and hopeless outlook. This perspective can contribute to increased anxiety and difficulty in managing panic attacks. Education is needed to address and challenge such negative beliefs.
Choice B rationale:
The statement "I'm worried about the consequences of having another panic attack" reflects a valid concern. People with panic disorder often worry about the impact of panic attacks on their daily lives and functioning.
Choice C rationale:
The statement "I feel confident that I can prevent future panic attacks" demonstrates an understanding of coping strategies and confidence in managing panic attacks. This is a positive sign that the client is actively engaged in their treatment and recovery.
Choice D rationale:
The statement "I've learned some relaxation techniques to help manage my anxiety" indicates that the client has acquired useful tools to manage anxiety. This suggests that the client is actively seeking ways to cope with panic attacks, which is a positive indicator.
A nurse is providing care to a client with panic disorder. Which of the following statements by the nurse is appropriate?
Explanation
The correct answer is Choice D.
Choice A rationale: Avoidance reinforces fear conditioning and impairs extinction learning; exposure-based strategies are more effective in reducing panic symptoms and restoring functional coping through cognitive-behavioral therapy.
Choice B rationale: Panic attacks are driven by autonomic dysregulation and cognitive misinterpretation, not physical pathology; suggesting physical illness increases somatic focus and health anxiety, worsening panic disorder outcomes.
Choice C rationale: Ignoring panic attacks delays cognitive restructuring and emotional processing; distraction may help short-term but does not address underlying maladaptive beliefs or autonomic hyperarousal.
Choice D rationale: Comorbidity between panic disorder and depression is well-documented; shared neurobiological pathways and chronic distress increase risk for mood disorders, requiring integrated assessment and treatment planning.
Explanation
Choice A rationale:
Substance abuse can be a significant complication of panic disorder. Individuals might turn to drugs or alcohol in attempts to self-medicate or alleviate symptoms.
Choice B rationale:
Hypertension isn't a primary complication of panic disorder. Panic attacks can lead to transient increases in blood pressure, but chronic hypertension isn't a well-documented outcome.
Choice C rationale:
Diabetes and panic disorder aren't directly linked. However, chronic stress and anxiety could potentially influence blood sugar levels in those predisposed to diabetes.
Choice D rationale:
Osteoporosis isn't a known complication of panic disorder. There's no physiological connection between panic attacks and bone health.
Explanation
Choice A rationale:
Family history of panic disorder is a recognized risk factor, suggesting a genetic predisposition. Anxiety disorders often have a hereditary component.
Choice B rationale:
High blood pressure might not directly lead to panic disorder. However, it could contribute to the overall stress burden on the individual.
Choice C rationale:
Recent weight loss isn't typically associated with an increased risk of panic disorder. Other factors are more relevant to its development.
Choice D rationale:
Allergies aren't linked to an increased risk of panic disorder. This choice lacks a plausible biological or psychological connection.
Explanation
Choice A rationale:
The statement "I'm not worried about having another panic attack" indicates a lack of understanding of anticipatory anxiety. Anticipatory anxiety is characterized by the fear of experiencing future panic attacks, so this statement contradicts that concept.
Choice B rationale:
This choice is correct because it reflects an accurate understanding of anticipatory anxiety. Anticipatory anxiety is the fear of being in situations or places where escape might be challenging or embarrassing in the event of a panic attack. This fear often leads to avoidance behavior and can worsen the overall anxiety.
Choice C rationale:
The statement "I don't think my panic attacks are related to my thought patterns" suggests a misunderstanding of the connection between thoughts and panic attacks. In reality, panic attacks are often triggered by anxious thoughts and thought patterns.
Choice D rationale:
The statement "I believe my panic attacks are caused by a substance I'm using" indicates a different perspective on the origin of panic attacks. While substance use can contribute to anxiety or trigger panic attacks in some cases, anticipatory anxiety specifically refers to the fear of future panic attacks, not their immediate causes.
Explanation
Choice A rationale:
Teaching relaxation techniques is a priority intervention for clients with panic disorder. Relaxation techniques, such as deep breathing, progressive muscle relaxation, and mindfulness, can help manage anxiety symptoms and reduce the frequency and intensity of panic attacks. These techniques empower clients to regain a sense of control over their anxiety.
Choice B rationale:
Administering antianxiety medication can be a helpful intervention, but it should not be prioritized over non-pharmacological approaches like teaching relaxation techniques. Medications may have side effects and are typically considered after other strategies have been explored.
Choice C rationale:
Encouraging socialization is important for overall mental health, but it may not directly address the immediate needs of a client experiencing panic disorder. Managing panic attacks and providing coping mechanisms should take precedence during the assessment.
Choice D rationale:
Monitoring vital signs regularly is important, but it is not the highest priority for a client with panic disorder. Addressing anxiety symptoms and providing appropriate interventions to manage panic attacks should come first.
Explanation
Choice A rationale:
Collecting vital signs, weight, height, and BMI is important for a general health assessment, but these measurements are not the primary focus when assessing a client with panic disorder.
Choice B rationale:
Gathering information about the client's support system, self-esteem, and coping strategies is relevant for understanding the client's overall well-being, but it may not provide as much insight into the specific factors contributing to panic disorder.
Choice C rationale:
This choice is correct because it addresses essential aspects of the assessment for a client with panic disorder. Understanding the client's medical history can reveal any underlying health conditions that might contribute to anxiety. Knowledge of medication use is crucial to identify potential interactions or side effects that could exacerbate anxiety. Family history provides insight into genetic predispositions and potential risk factors.
Choice D rationale:
Collecting laboratory tests and diagnostic tools might be necessary for ruling out other medical conditions that could mimic anxiety symptoms, but these should be secondary to gathering information about medical history, medication use, and family history when assessing a client with panic disorder.
Explanation
Choice A rationale:
Providing a safe and calm environment for the client during a panic attack is crucial to help minimize distress and prevent harm. Panic attacks can lead to heightened anxiety and fear, and creating a safe space can help the client feel secure. This intervention aids in reducing the overall intensity and duration of the panic attack.
Choice B rationale:
Using therapeutic communication skills to establish rapport and trust with the client is essential in managing panic disorder. By employing active listening, empathy, and non-judgmental responses, the nurse can create a supportive environment. Building a therapeutic relationship enhances the client's willingness to communicate, share their experiences, and adhere to the treatment plan.
Choice C rationale:
Educating the client about panic disorder and its treatment options is important, but it might be overwhelming during a panic attack. Providing education can be more effective when the client is relatively stable and receptive. The immediate focus during a panic attack should be on providing comfort and support.
Choice D rationale:
Encouraging the client to participate in cognitive-behavioral therapy (CBT) is a valuable intervention for panic disorder. However, suggesting this during a panic attack might not be appropriate, as the client's focus and ability to engage in a discussion could be compromised. It's better to introduce the idea of CBT when the client is in a more receptive state.
Choice E rationale:
Referring the client to self-help groups for peer support and education is also a beneficial intervention. However, during a panic attack, the client may not be open to the idea of group involvement. This recommendation is better suited for a calmer moment when the client can consider it more rationally.
Explanation
Choice A rationale:
Asking the client about coping strategies and support systems is an appropriate assessment question for a client with panic disorder. This question allows the nurse to understand how the client manages their panic attacks and identifies the resources available to them. The response can provide insights into the client's adaptive or maladaptive coping mechanisms.
Choice B rationale:
Inquiring about the frequency of panic attacks and their triggers is important, but this question may not be appropriate as the initial assessment question. It's better to first establish a rapport and gather broader information about the client's experiences before delving into specific details.
Choice C rationale:
Asking about current medications is relevant, but it might be more suitable after building rapport and discussing the client's overall situation. Focusing solely on medication can overlook other important aspects of the client's condition and coping strategies.
Choice D rationale:
Inquiring about laboratory tests is not directly relevant to the assessment of panic disorder. Panic disorder is primarily diagnosed based on clinical criteria, and laboratory tests are not typically used for diagnosis.
Explanation
Choice A rationale:
The nursing diagnosis "Anxiety related to perceived threats or loss of control" is appropriate for a client with panic disorder. Panic disorder is characterized by recurrent and unexpected panic attacks, leading to heightened anxiety and apprehension. The client often perceives a loss of control during these attacks, making this diagnosis suitable.
Choice B rationale:
"Impaired social interaction related to avoidance behavior or low self-esteem" is not the most appropriate diagnosis for panic disorder. While social interaction might be affected, the core feature of panic disorder is the occurrence of panic attacks. The chosen diagnosis does not directly address this aspect.
Choice C rationale:
"Risk for self-directed violence related to hopelessness or depression" is not the most fitting diagnosis for panic disorder. Panic attacks typically involve intense anxiety and fear rather than depression or hopelessness, which are more associated with mood disorders.
Choice D rationale:
"Knowledge deficit related to panic disorder and its treatment" is not the best diagnosis for a client with panic disorder. While education about the disorder is important, panic disorder is primarily characterized by the presence of panic attacks and related symptoms, which should take precedence in the nursing diagnosis.
Explanation
Choice A rationale:
If the client reports a decrease in the frequency and severity of panic attacks, it indicates effective management of panic disorder. This outcome suggests that the treatment interventions are successfully reducing the occurrence and intensity of panic attacks, leading to improved overall well-being.
Choice B rationale:
While engaging in social activities and maintaining supportive relationships (choice B) is important for the client's mental health, it doesn't directly indicate the effectiveness of panic disorder management. The client might be socially active but still experiencing panic attacks.
Choice C rationale:
Demonstrating effective coping skills and positive self-talk (choice C) is certainly a positive outcome. However, this alone might not fully reflect the successful management of panic disorder. Effective coping skills are a part of the management plan, but the reduction in panic attack frequency is a more specific indicator of treatment effectiveness.
Choice D rationale:
Adhering to the prescribed treatment regimen and following up with appointments (choice D) is crucial for any medical condition, including panic disorder. However, this outcome doesn't directly measure the reduction in panic attacks, which is a more specific measure of successful management.
Explanation
Choice A rationale:
Monitoring vital signs, weight, height, and BMI (choice A) is relevant for a general health assessment, but it is not specific to evaluating a client with panic disorder.
Choice B rationale:
Assessing the client's support system, self-esteem, and coping strategies (choice B) is important for understanding the client's psychosocial well-being, but it doesn't directly provide information about their panic disorder and its management.
Choice C rationale:
Collecting the client's medical history, medication use, and family history (choice C) is crucial for assessing the context of the panic disorder. Medical history helps identify any contributing factors, medication use informs about the current treatment, and family history might reveal a genetic predisposition or relevant psychosocial factors.
Choice D rationale:
Requesting laboratory tests and diagnostic tools (choice D) can be useful in ruling out medical conditions that may mimic panic disorder symptoms, but they are not the primary focus of a panic disorder assessment.
Explanation
Choice A rationale:
Providing a safe and calm environment during a panic attack (choice A) is crucial to help the client feel secure and reduce the intensity of the attack.
Choice B rationale:
Using therapeutic communication skills (choice B) is essential to establish rapport and trust with the client, creating a foundation for effective therapeutic interventions.
Choice C rationale:
Educating the client about panic disorder and its treatment options (choice C) empowers them to actively participate in their treatment and make informed decisions.
Choice D rationale:
Encouraging the client to participate in cognitive-behavioral therapy (CBT) (choice D) is a evidence-based approach for managing panic disorder. CBT helps the client develop coping strategies and change maladaptive thought patterns.
Choice E rationale:
Referring the client to self-help groups for peer support and education (choice E) offers additional resources and insights from individuals who have experienced similar challenges, fostering a sense of community and reducing isolation.
Explanation
Choice A rationale:
Taking benzodiazepines as needed for panic attacks is an incorrect statement. Benzodiazepines are generally not intended for "as-needed" use due to the risk of dependence and withdrawal. They are typically prescribed on a scheduled basis to provide consistent anxiety relief.
Choice B rationale:
Avoiding alcohol while taking benzodiazepines is important due to potential interactions between alcohol and the medication. Both substances can have central nervous system depressant effects, which can lead to increased drowsiness, impaired coordination, and cognitive deficits.
Choice C rationale:
Experiencing drowsiness and dizziness are common side effects of benzodiazepines. Educating the client about these potential side effects is necessary to promote safety and to avoid engaging in activities that require alertness while taking the medication.
Choice D rationale:
This statement indicates a need for further education. Abruptly stopping benzodiazepines can lead to withdrawal symptoms, which may include increased anxiety, irritability, insomnia, and even seizures. Benzodiazepines should be tapered off gradually under medical supervision.
Explanation
Choice A rationale:
Cognitive-behavioral therapy (CBT) is a well-established non-pharmacological treatment for panic disorder. It focuses on identifying and challenging negative thought patterns and beliefs that contribute to anxiety. By addressing these cognitive distortions, clients can learn to manage their panic symptoms more effectively.
Choice B rationale:
Exposure therapy is another evidence-based approach for treating anxiety disorders. However, it involves gradual exposure to feared situations or stimuli to reduce anxiety over time. While it can benefit clients with panic disorder, it does not specifically address challenging negative thoughts as CBT does.
Choice C rationale:
Lifestyle modifications, such as regular exercise, a balanced diet, and stress reduction techniques, can indeed help reduce physical symptoms associated with panic attacks. However, they do not directly address the cognitive and emotional aspects of panic disorder like CBT does.
Choice D rationale:
Complementary therapies may have a role in managing anxiety, but they are unlikely to replace the need for medications or evidence-based psychotherapies. These therapies, such as acupuncture or herbal remedies, are typically used as adjuncts to conventional treatments rather than substitutes.
Explanation
Choice A rationale:
This statement accurately describes panic disorder. It is an anxiety disorder characterized by recurrent and unexpected panic attacks—sudden episodes of intense fear or discomfort accompanied by physical and cognitive symptoms. These attacks can lead to significant distress and avoidance behaviors.
Choice B rationale:
Panic disorder is not a type of depression; it is a separate anxiety disorder. While there can be co-occurrence of depression and anxiety disorders, they have distinct diagnostic criteria and features.
Choice C rationale:
Panic disorder is not related to substance abuse, nor is it influenced by biological factors that contribute to substance use disorders. It is primarily a psychological condition related to anxiety.
Choice D rationale:
The PDSS (Panic Disorder Severity Scale) is a tool used to assess the severity of panic disorder symptoms, not to diagnose the disorder itself. A diagnosis of panic disorder is based on clinical criteria outlined in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5)
Explanation
Choice A rationale:
Beta-blockers are not commonly used for the pharmacological treatment of panic disorder. While they are used for conditions like hypertension and certain heart conditions, they are not the primary choice for panic disorder. Panic disorder primarily involves disturbances in brain neurotransmitters, which beta-blockers do not directly target.
Choice B rationale:
Anticonvulsants are not the primary choice for treating panic disorder. While they may be used for other conditions such as epilepsy or bipolar disorder, their effectiveness in treating panic disorder is limited compared to other classes of medications like SSRIs.
Choice C rationale:
Selective serotonin reuptake inhibitors (SSRIs) are commonly used for the pharmacological treatment of panic disorder. Panic disorder often involves imbalances in serotonin, a neurotransmitter that plays a crucial role in mood regulation. SSRIs help increase serotonin levels in the brain by blocking its reuptake, thereby alleviating symptoms of panic and anxiety.
Choice D rationale:
Tricyclic antidepressants (TCAs) are sometimes used for panic disorder, but they are not the first-line treatment due to their potential side effects and safety concerns. SSRIs have largely replaced TCAs as the preferred choice due to their better tolerability and safety profile.
Explanation
Choice A rationale:
Cognitive-behavioral therapy (CBT) is a psychotherapy technique commonly used to help clients with panic disorder. It focuses on identifying and challenging negative thought patterns and behaviors that contribute to panic attacks. By changing these thought-behavior patterns, individuals can better manage their panic symptoms.
Choice B rationale:
Exposure therapy is another psychotherapy technique used for panic disorder. It involves gradually exposing clients to their feared situations or places in a controlled and supportive environment. Through repeated exposure, individuals can learn to tolerate and manage their anxiety, leading to a reduction in panic attacks.
Choice C rationale:
Relaxation techniques are not the primary psychotherapy technique for panic disorder. While relaxation techniques can help manage general anxiety, panic disorder often requires more targeted interventions like CBT and exposure therapy.
Choice D rationale:
Lifestyle modifications can be beneficial for managing anxiety in general, but they are not a psychotherapy technique specifically designed to help clients confront their feared situations. Psychotherapy techniques like CBT and exposure therapy are more effective in this context.
Explanation
Choice A rationale:
Assessing and diagnosing the client's physical health problems is important, but it does not accurately describe the nursing care for panic disorder. Panic disorder primarily involves psychological and emotional symptoms, so addressing the client's mental health needs takes precedence.
Choice B rationale:
Intervening and evaluating the client's social support and self-esteem accurately describe nursing care for panic disorder. Social support and self-esteem play significant roles in a client's ability to cope with and manage panic disorder. Nurses can provide interventions to enhance these factors, which can contribute to better outcomes.
Choice C rationale:
Monitoring for signs of serotonin syndrome is important when a client is taking certain medications, particularly serotonergic antidepressants. However, it is not a specific concern in panic disorder nursing care unless the client is on medication that could potentially lead to serotonin syndrome.
Choice D rationale:
Educating the client on the potential side effects of benzodiazepines is relevant, but it is not the most accurate description of nursing care for panic disorder. Nursing care goes beyond medication education and involves a comprehensive approach to addressing the client's emotional, psychological, and social needs.
Phobias
A nurse is providing education to a client with panic disorder about the pharmacological treatment options. Which statement by the client indicates understanding of the teaching?
Explanation
Choice A rationale:
"I should avoid medications that increase serotonin levels in the brain." While avoiding medications that increase serotonin levels is relevant in some cases, it's not a comprehensive understanding of pharmacological treatment for panic disorder. Serotonin-related medications like selective serotonin reuptake inhibitors (SSRIs) are commonly used for panic disorder treatment.
Choice B rationale:
"Antihypertensives can help reduce physical symptoms of panic attacks." This statement is not accurate. Antihypertensives are not commonly used to treat panic disorder. Medications like beta-blockers may be prescribed to manage some physical symptoms of anxiety, but they are not a primary treatment for panic disorder.
Choice C rationale:
"Antiepileptics can enhance the effects of gamma-aminobutyric acid (GABA) in the brain." This is the correct choice. Antiepileptic medications like pregabalin and gabapentin can indeed enhance the effects of GABA, an inhibitory neurotransmitter that helps reduce anxiety and panic. These medications are sometimes used to manage panic disorder symptoms.
Choice D rationale:
"Tricyclic antidepressants inhibit the reuptake of norepinephrine in the brain." While tricyclic antidepressants have been used historically to treat panic disorder, they are not considered first-line treatments due to their potential side effects and the availability of newer, safer options. The statement in Choice D is accurate but not as relevant to current treatment approaches.
A nurse is caring for a client with panic disorder who is prescribed pharmacological treatment. Which interventions should the nurse include in the plan of care? Select all that apply.
Explanation
Choice A rationale:
Encourage regular exercise and a healthy diet. Regular exercise and a healthy diet contribute to overall well-being and can have a positive impact on managing anxiety and panic disorder. Exercise releases endorphins, which are natural mood lifters, and a balanced diet supports physical and mental health.
Choice B rationale:
Teach deep breathing and progressive muscle relaxation techniques. Deep breathing and progressive muscle relaxation are evidence-based relaxation techniques that can help manage anxiety and panic symptoms. They promote relaxation and help clients cope with the physical sensations of panic.
Choice C rationale:
Assist with gradually confronting feared situations or places. This approach, known as exposure therapy, is a common component of cognitive-behavioral therapy for panic disorder. Gradual exposure to feared situations or places can help desensitize the client to triggers and reduce the intensity of panic reactions.
Choice D rationale:
Monitor for signs of serotonin syndrome. Serotonin syndrome is a potentially serious condition that can result from interactions between certain medications that affect serotonin levels. Monitoring for signs such as agitation, confusion, rapid heart rate, and high blood pressure is crucial when using medications that impact serotonin.
Choice E rationale:
Educate on the potential side effects of benzodiazepines. Benzodiazepines are sometimes prescribed for short-term relief of acute anxiety or panic symptoms, but they can be habit-forming and have potential side effects like sedation, dizziness, and cognitive impairment. Educating the client about these potential effects is important for informed decision-making.
A nurse is assessing a client with panic disorder. Which statement by the nurse would be appropriate during the assessment?
Explanation
Choice A rationale:
"Tell me about your coping strategies and support system." This choice may not be the most appropriate initial question because it focuses on coping strategies and support systems rather than gathering information about the frequency and triggers of panic attacks. While coping strategies and support systems are important, understanding the pattern of panic attacks is crucial for assessment and planning.
Choice B rationale:
"How often do you experience panic attacks and what triggers them?" This is the correct choice. It directly addresses the primary concerns related to panic disorder by inquiring about the frequency of panic attacks and their triggers. This information is essential for developing a comprehensive understanding of the client's condition and tailoring an effective treatment plan.
Choice C rationale:
"What medications are you currently taking for your panic disorder?" While inquiring about medication use is important, this question should come after understanding the frequency and triggers of panic attacks. Knowing about medications alone does not provide a holistic picture of the client's experience with panic disorder.
Choice D rationale:
"Have you ever had any laboratory tests done for your panic disorder?" This question is not directly relevant to the assessment of panic disorder. Panic disorder is primarily diagnosed based on clinical symptoms and criteria outlined in diagnostic manuals like the DSM-5. Laboratory tests are not routinely used for diagnosing panic disorder, so this question might not yield pertinent information for assessment.
Phobias
Explanation
Choice A rationale:
Specific phobias are fears of a particular stimulus that trigger an excessive and unreasonable response. In specific phobias, individuals experience intense fear and anxiety in response to specific objects or situations, such as heights, animals, or certain activities. The fear is often recognized as excessive or unreasonable, but the person feels powerless to control the anxiety. This is consistent with the definition of specific phobias, where the fear is focused on a specific trigger.
Choice B rationale:
This choice describes social anxiety disorder (social phobia), not specific phobias. Social phobia involves a fear of being judged, criticized, or embarrassed in social or performance situations. People with social phobia tend to avoid such situations or endure them with intense distress. It's a different type of anxiety disorder with a focus on social interactions rather than specific triggers.
Choice C rationale:
This choice refers to agoraphobia, not specific phobias. Agoraphobia involves a fear of being in places or situations from which escape might be difficult or embarrassing. People with agoraphobia often avoid situations like crowded places or open spaces due to fear of having a panic attack and not being able to escape.
Choice D rationale:
This choice incorrectly defines specific phobias. Specific phobias are characterized by an intense fear of a particular object, situation, or activity that may pose little or no actual danger. The fear is irrational and disproportionate to the threat posed by the trigger. This is why Choice A is the correct answer, as it accurately describes specific phobias.
Explanation
Choice A rationale:
This choice inaccurately describes specific phobias, not social phobia. Specific phobias are centered around specific triggers, while social phobia involves a fear of being negatively evaluated in social or performance situations.
Choice B rationale:
Social phobia, also known as social anxiety disorder, is indeed characterized by a fear of being judged, criticized, or embarrassed in social or performance situations. This fear often leads individuals to avoid social interactions or endure them with significant distress.
Choice C rationale:
This choice relates to agoraphobia, not social phobia. Agoraphobia involves the fear of being in situations from which escape might be difficult or embarrassing, such as crowded places or public transportation.
Choice D rationale:
This choice inaccurately characterizes specific phobias, not social phobia. Specific phobias are focused on particular triggers and are not related to a fear of a specific object, situation, or activity that poses little or no actual danger.
Explanation
Choice A rationale:
This response is appropriate as it aligns with the principles of exposure therapy. Exposure therapy involves gradually confronting feared situations to reduce anxiety over time. By encouraging the client to face their fears and expose themselves to anxiety-provoking situations in a controlled manner, they can learn that their anxiety decreases over time.
Choice B rationale:
This response is counterproductive and not recommended. Avoiding situations that trigger anxiety can actually reinforce the fear and make it more difficult for the client to cope with their agoraphobia. Avoidance prevents the client from learning that their fear is manageable.
Choice C rationale:
While distraction techniques can be helpful for managing anxiety in the moment, they do not address the underlying fear associated with agoraphobia. Encouraging distraction as the primary coping strategy might hinder the client's progress in overcoming their fear.
Choice D rationale:
This response promotes avoidance, which is not a recommended approach in treating anxiety disorders like agoraphobia. Avoiding situations altogether can worsen the fear and limit the client's ability to engage in normal activities.
Explanation
Choice A rationale:
This choice describes social anxiety disorder, where the individual fears being judged negatively by others in social situations. It doesn't reflect a specific phobia, which involves a marked and persistent fear of a specific object or situation.
Choice B rationale:
This statement indicates agoraphobia, which is the fear of being in places where escape might be difficult or help unavailable. It doesn't align with the criteria for a specific phobia, where the fear is directed at a specific object or situation.
Choice C rationale:
The correct answer. This choice represents a specific phobia. The fear of spiders is a classic example of a specific phobia, and the extreme anxiety triggered by the sight of a spider indicates an irrational and disproportionate fear response, which is characteristic of this condition.
Choice D rationale:
This statement describes aviophobia, the fear of flying. While it is a phobia, it doesn't cover the full spectrum of specific phobias, which can involve a wide range of objects or situations beyond just flying.
Explanation
Choice A rationale:
Neurochemical imbalances in the brain are more commonly associated with mood disorders like depression and anxiety disorders in general, rather than being a specific cause of the physiological symptoms seen in phobias.
Choice B rationale:
Negative self-beliefs and cognitive distortions are central to anxiety disorders like generalized anxiety disorder and social anxiety disorder, but they don't directly explain the acute physiological symptoms like palpitations and sweating seen in phobias.
Choice C rationale:
Traumatic experiences and learned associations are relevant to post-traumatic stress disorder (PTSD) and other anxiety disorders. However, they are not the primary cause of physiological symptoms in specific phobias.
Choice D rationale:
The correct answer. Specific phobias trigger a "fight or flight" response through the autonomic nervous system, leading to physiological symptoms like palpitations, sweating, and shortness of breath. This response is an evolutionary adaptation designed to prepare the body to respond to threats.
Explanation
Choice A rationale:
This description is more fitting for panic disorder or generalized anxiety disorder, which involve intense fear, anxiety, panic, and impaired functioning. Specific phobias can cause distress and impairment, but they are primarily characterized by the fear of a specific object or situation.
Choice B rationale:
Phobias are diagnosed based on the psychological and behavioral symptoms related to the fear of a specific object or situation, not solely on physiological symptoms.
Choice C rationale:
While duration and frequency of symptoms are important factors, they are not the central criteria for diagnosing specific phobias. These factors might be more relevant to other anxiety disorders.
Choice D rationale:
The correct answer. Phobias are diagnosed based on the specific type of fear-inducing object or situation and the associated features of the phobia. These features include the marked and persistent fear, avoidance behavior, and the irrationality of the fear response.
Explanation
Choice A rationale:
Genetic predisposition and neurochemical imbalances. While genetics and neurochemistry can contribute to the development of anxiety disorders, they are not the primary factors behind avoidance behaviors associated with specific phobias. Phobias are often learned responses.
Choice B rationale:
Traumatic experiences and learned associations. This choice is the correct answer. Avoidance behaviors seen in specific phobias are usually a result of traumatic experiences that lead to the formation of strong fear responses through learned associations. For instance, if someone had a traumatic experience with spiders, they might develop a phobia of spiders and actively avoid situations involving spiders to prevent the intense fear from reoccurring.
Choice C rationale:
Cultural influences and family dynamics. While cultural factors and family dynamics can impact a person's psychological development, they are not the primary drivers of avoidance behaviors in specific phobias. Phobias are more closely linked to personal experiences and learned responses.
Choice D rationale:
Negative self-beliefs and cognitive distortions. Negative self-beliefs and cognitive distortions are more characteristic of conditions like depression and anxiety disorders, but they are not the central factors driving avoidance behaviors in specific phobias. These behaviors are more strongly connected to learned fear responses.
Explanation
Choice A rationale:
Social phobia is a fear of a particular stimulus that triggers an excessive and unreasonable response. This description aligns more closely with the definition of a specific phobia rather than social phobia. Specific phobias involve a fear of specific objects or situations, not general social interactions.
Choice B rationale:
Social phobia is a fear of being judged, criticized, or embarrassed in social or performance situations. This is the correct answer. Social phobia, also known as social anxiety disorder, is characterized by an intense fear of negative evaluation in social settings. Individuals with social phobia are often excessively self-conscious and fear humiliation or embarrassment when interacting with others.
Choice C rationale:
Social phobia is a fear of being in places or situations from which escape might be difficult or embarrassing. This description aligns with agoraphobia, which involves a fear of situations from which escape may be challenging, rather than social phobia.
Choice D rationale:
Social phobia is a fear of a specific object, situation, or activity that poses little or no actual danger. This description aligns more with the definition of a specific phobia, where the fear is often triggered by a specific object or situation that poses limited real danger.
Explanation
Choice A rationale:
Specific Phobia. This is the correct answer. The client's symptoms of marked fear and anxiety about a specific object or situation that is out of proportion to the actual danger, along with resulting distress and impairment, are characteristic of a specific phobia. Specific phobias involve intense fear and avoidance behavior triggered by specific objects or situations, like heights, animals, or certain environments.
Choice B rationale:
Social Phobia. The client's symptoms do not align with social phobia, which centers around fears of social judgment and performance situations, not specific objects or situations.
Choice C rationale:
Agoraphobia. Agoraphobia involves fear of situations where escape may be difficult or embarrassing, such as crowded places. The client's fear does not seem related to this type of avoidance.
Choice D rationale:
Panic Disorder. While panic disorder involves recurrent panic attacks, it does not necessarily involve avoidance of specific objects or situations as the primary response. The client's avoidance behavior is more indicative of a specific phobia.
Explanation
Choice A rationale:
Exposure therapy is indeed a form of cognitive-behavioral therapy (CBT) It involves systematically exposing individuals to the feared object or situation in a controlled and gradual manner. The goal is to reduce their anxiety or fear response over time through repeated exposures. By confronting their fears, individuals can learn that their anxiety decreases over time, leading to behavioral changes.
Choice B rationale:
While cognitive-behavioral therapy (CBT) often includes challenging irrational thoughts and beliefs, exposure therapy primarily focuses on the behavioral aspect of fear reduction through systematic exposure. Cognitive restructuring, which addresses irrational beliefs, is a distinct component of CBT but not the primary emphasis of exposure therapy.
Choice C rationale:
Exposure therapy does not inherently involve teaching clients relaxation techniques. Instead, it centers on controlled exposure to the feared stimulus to weaken the fear response. Relaxation techniques might be used in some cases to help manage anxiety, but they are not a defining characteristic of exposure therapy.
Choice D rationale:
Although exposure therapy can be effective for various phobias, it is not exclusive to social phobias. It can be applied to specific phobias, agoraphobia, and other anxiety disorders as well.
Explanation
Choice A rationale:
The client's fear of flying in airplanes and the intense panic response when even thinking about it are indicative of a specific phobia. Specific phobias involve an intense and irrational fear of a specific object, situation, or activity. In this case, the fear of flying is specific and triggers a significant anxiety reaction.
Choice B rationale:
Social phobia (also known as social anxiety disorder) involves an excessive fear of social situations where the individual fears being scrutinized or judged by others. This fear extends beyond a specific object or situation, which is not the case in this scenario.
Choice C rationale:
Agoraphobia involves a fear of situations where escape might be difficult or help might not be available if a panic attack occurs. This fear often leads to avoidance of various places or situations, such as crowded spaces. The client's fear of flying is not characteristic of agoraphobia.
Choice D rationale:
Panic disorder is characterized by recurrent and unexpected panic attacks, often accompanied by a fear of having additional attacks. While the client does experience panic symptoms related to the fear of flying, the primary issue is the specific fear of flying itself, suggesting a specific phobia rather than panic disorder.
Explanation
Choice B rationale:
The client's intense fear of embarrassing themselves in front of others and the specific fear related to giving a presentation are indicative of social phobia (social anxiety disorder) Social phobia involves an excessive fear of social situations where the individual fears negative evaluation or judgment by others, leading to avoidance of such situations.
Choice A rationale:
While the client's fear is related to public speaking, the emphasis is on the fear of embarrassment and negative evaluation rather than a fear of a specific object or situation, which aligns more with social phobia.
Choice C rationale:
Agoraphobia does not align with the client's fear of public speaking. Agoraphobia involves the fear of situations where escape might be difficult or help might not be available if a panic attack occurs, often leading to avoidance of various places or situations.
Choice D rationale:
Panic disorder involves recurrent and unexpected panic attacks, which are not explicitly mentioned in the client's statement. The focus of the client's fear is on the social aspect of giving a presentation rather than on panic attacks.
Explanation
Choice A rationale:
Specific Phobia is characterized by the active avoidance of certain situations or objects accompanied by intense fear or anxiety. Individuals with specific phobias tend to go to great lengths to avoid the feared stimulus due to the overwhelming distress it causes. This aligns with the behavior described in the question.
Choice B rationale:
Social Phobia involves the fear or avoidance of social situations due to the perceived threat of negative evaluation by others. It doesn't necessarily involve specific situations or objects like the client's behavior in the question.
Choice C rationale:
Agoraphobia involves the fear of situations where escape might be difficult or help might not be available in the event of developing incapacitating symptoms. This doesn't fully match the behavior described, as the client is not expressing fear related to difficulty escaping or lack of available help.
Choice D rationale:
Panic Disorder is characterized by recurrent panic attacks and the persistent worry about future attacks. While panic attacks can be triggered by specific phobias, the avoidance behavior and the focus on certain situations are more indicative of a specific phobia rather than Panic Disorder.
Explanation
Choice A rationale:
While this characteristic is important, it doesn't distinguish specific phobia from other mental disorders. It's a common requirement for many mental disorders to ensure the symptoms are not transient.
Choice B rationale:
This characteristic is more aligned with Social Phobia, where individuals fear negative evaluation in social situations, rather than Specific Phobia, which involves fear of specific situations or objects.
Choice C rationale:
The persistence of fear or anxiety for at least 6 months is a defining feature of specific phobias. This chronic nature helps differentiate it from transient fears or anxieties.
Choice D rationale:
This characteristic is related to Agoraphobia, where individuals fear situations in which they might develop incapacitating symptoms and lack available help. It doesn't specifically describe the fear of certain situations or objects seen in specific phobias.
Explanation
Choice A rationale:
The client's statement reflects cognitive distortion, where their thoughts are irrational and exaggerated. The client's intense fear of bad things happening during a flight and their inability to imagine being on a plane without fear are examples of distorted thinking patterns.
Choice B rationale:
Maladaptive coping refers to using ineffective strategies to deal with stress or anxiety. While the client's fear of flying is indeed a maladaptive response, the statement doesn't directly describe coping mechanisms.
Choice C rationale:
Rational thinking involves logical and balanced thoughts. The client's statement does not reflect rational thinking, as their fear is intense and irrational.
Choice D rationale:
Effective self-management involves using appropriate strategies to manage one's fears or anxieties. The client's statement does not indicate effective self-management, as their fear seems to be controlling their emotions and thoughts rather than managing them.
Explanation
Choice A rationale:
Establishing a therapeutic relationship with the client based on trust, empathy, respect, and acceptance (Choice A) is a crucial nursing intervention for phobias. This helps create a foundation of trust and safety, allowing the client to feel understood and supported in addressing their phobic responses.
Choice B rationale:
Providing a safe and supportive environment for the client (Choice B) is another essential intervention. This environment enables the client to feel secure and encourages them to explore their fears gradually, knowing they are in a protected setting.
Choice C rationale:
Encouraging the client to avoid situations that trigger phobic responses (Choice C) is not a recommended intervention. Avoidance can reinforce the phobia and hinder progress in overcoming it. Encouraging gradual exposure to feared situations is a more effective strategy.
Choice D rationale:
Assisting the client to identify and challenge irrational thoughts and beliefs (Choice D) is an evidence-based intervention. This approach, known as cognitive-behavioral therapy, helps clients recognize and modify distorted thought patterns that contribute to their phobias.
Choice E rationale:
Implementing exposure therapy with the client (Choice E) is a valid intervention for phobias. Exposure therapy involves gradually exposing the client to the feared object or situation in a controlled manner, helping them desensitize and reduce their fear response.
Which of the following is a characteristic of agoraphobia?
Explanation
Choice D rationale:
The individual fears or avoids certain situations due to thoughts of difficulty escaping or lack of available help in case of developing incapacitating symptoms (Choice D) is a characteristic of agoraphobia. Individuals with agoraphobia often fear being in situations where escape might be challenging or help might not be readily available if they experience intense anxiety or panic symptoms.
Choice A rationale:
The fear or anxiety is not better explained by another mental disorder (Choice A) is a general criterion for diagnosing anxiety disorders, but it doesn't specifically relate to agoraphobia.
Choice B rationale:
The individual fears or avoids social situations due to the perceived threat of negative evaluation (Choice B) is more indicative of social anxiety disorder, not agoraphobia.
Choice C rationale:
The fear or anxiety is persistent, typically lasting for 6 months or more (Choice C) is a general criterion for diagnosing anxiety disorders, but it doesn't uniquely characterize agoraphobia.
What is one example of a nursing intervention for phobias?
Explanation
Choice C rationale:
Collaborating with the client to set realistic and achievable goals for overcoming phobias (Choice C) is an example of a nursing intervention for phobias. This empowers the client to actively participate in their treatment, fostering a sense of control and motivation to confront their fears.
Choice A rationale:
Providing a safe and supportive environment for the client (Choice A) is important, but it is a more general intervention that doesn't specifically address the process of overcoming phobias.
Choice B rationale:
Encouraging the client to avoid situations that trigger phobic responses (Choice B) is counterproductive, as mentioned earlier. It reinforces avoidance behaviors rather than helping the client confront their fears.
Choice D rationale:
Referring the client to other health care professionals as needed (Choice D) is a potential step in the treatment process, but it doesn't exemplify a direct nursing intervention for phobias. It's more about coordinating care if specialized help is required.
What is one example of an outcome for the nursing interventions aimed at reducing fear and anxiety in clients with phobias?
Explanation
Choice A rationale:
The client reporting decreased fear and anxiety related to phobias (Choice A) is a subjective outcome that might not accurately reflect the effectiveness of the nursing interventions. It relies solely on the client's self-report and might not provide an objective measure of improvement.
Choice B rationale:
The client demonstrating increased avoidance behavior (Choice B) is not an outcome aimed at reducing fear and anxiety. Increased avoidance behavior would actually indicate a worsening of the phobia-related symptoms, as the client is avoiding the feared stimulus more.
Choice C rationale:
The client engaging in exposure therapy without excessive distress (Choice C) is a desired outcome for interventions targeting phobias. Exposure therapy involves gradually exposing the client to the feared stimulus in a controlled manner. If the client can tolerate exposure without excessive distress, it indicates a positive response to the intervention and a reduction in fear and anxiety over time.
Choice D rationale:
The client applying cognitive-behavioral techniques ineffectively (Choice D) is not a desirable outcome. The goal of cognitive-behavioral techniques is to equip the client with effective coping strategies to manage their phobias. If the client is applying these techniques ineffectively, it indicates a need for further intervention or adjustment of the therapeutic approach.
A nurse is providing education to a client diagnosed with a specific phobia. Which medication class should the nurse include in the teaching plan?
Explanation
Choice A rationale:
Antidepressants (Choice A) are not typically the first-line medication class for treating specific phobias. While they may be used in some cases, they are not the primary choice for addressing the symptoms of phobias.
Choice B rationale:
Benzodiazepines (Choice B) are sometimes used to manage acute anxiety symptoms, but they are generally not recommended for long-term treatment of specific phobias due to the risk of dependence and potential side effects.
Choice C rationale:
Beta-blockers (Choice C) can be useful in managing the physical symptoms of anxiety, such as rapid heartbeat and trembling, which often accompany phobias. They work by blocking the effects of adrenaline, reducing the "fight or flight" response. This can help the client feel more physically at ease when confronting their phobic stimulus.
Choice D rationale:
Analgesics (Choice D) are pain-relieving medications and have no direct relevance to treating phobias. They do not address the underlying fear and anxiety associated with phobias.
A nurse is assessing a client with a phobia. Which non-pharmacological therapy should the nurse recommend to help the client cope with their fear?
Explanation
Choice A rationale:
Psychoeducation (Choice A) involves providing the client with information about their condition, treatment options, and coping strategies. It can help the client understand their phobia better and empower them to take an active role in managing their fear.
Choice B rationale:
Cognitive therapy (Choice B) focuses on identifying and challenging irrational thoughts and beliefs related to the phobia. By changing thought patterns, clients can learn to respond to their phobic triggers in a more rational and less anxiety-provoking manner.
Choice C rationale:
Behavioral therapy (Choice C), including exposure therapy, is a cornerstone of phobia treatment. It involves gradually exposing the client to the feared stimulus in a controlled manner, helping them learn that their anxiety decreases over time.
Choice D rationale:
Relaxation therapy (Choice D) teaches clients relaxation techniques such as deep breathing, progressive muscle relaxation, and meditation. These techniques can help reduce overall anxiety levels and provide a sense of control in anxiety-provoking situations.
Choice E rationale:
All of the above (Choice E) is the correct answer because each of the listed non-pharmacological therapies (psychoeducation, cognitive therapy, behavioral therapy, relaxation therapy) plays a valuable role in helping clients cope with their phobias. They can be used in combination to provide comprehensive support for the client's needs.
Explanation
Choice A rationale:
The statement "This medication will help regulate my mood and anxiety" is accurate. Antidepressants are commonly prescribed for mood and anxiety disorders, including phobias. They work by affecting neurotransmitters in the brain to improve mood and reduce anxiety.
Choice B rationale:
The statement "I should expect to see immediate results after taking this medication" is incorrect. This suggests a misunderstanding about the timeline for antidepressant effectiveness. Antidepressants typically take several weeks to show noticeable effects. It's important to educate the client that gradual improvement over time is expected.
Choice C rationale:
The statement "I may experience side effects such as nausea and drowsiness" is accurate. Many antidepressants can indeed cause side effects like nausea, drowsiness, and other gastrointestinal symptoms, especially when starting the medication. Educating the client about potential side effects promotes informed decision-making.
Choice D rationale:
The statement "It's important to take this medication consistently as prescribed" is accurate. Consistent adherence to the prescribed medication regimen is crucial for the effectiveness of antidepressants. Missing doses or stopping the medication abruptly can lead to discontinuation symptoms and a potential relapse of symptoms.
Explanation
Choice A rationale:
Encouraging the client to face their fear gradually is a cornerstone of exposure therapy, a proven psychological approach for treating phobias. Gradual exposure helps the client confront their fears in a controlled manner, allowing them to build tolerance and reduce anxiety over time.
Choice B rationale:
Administering benzodiazepines as needed for acute anxiety (choice B) is not the first-line intervention for treating phobias. While benzodiazepines can provide rapid relief from acute anxiety, they do not address the underlying phobia and can lead to dependence if used excessively.
Choice C rationale:
Providing psychoeducation about the causes and effects of phobias is valuable, but it alone might not be as effective as exposure therapy or other evidence-based treatments. Educating the client about the nature of phobias can complement their treatment plan.
Choice D rationale:
Teaching the client relaxation techniques to manage anxiety is beneficial but might not be as effective as exposure therapy for addressing phobias directly. Relaxation techniques can be useful in managing general anxiety, but specific phobias are best treated with exposure-based interventions.
Explanation
Choice A rationale:
This statement accurately captures the key features of phobias. Phobias involve intense, irrational fear reactions to specific objects or situations that persist over time. The fear is often excessive in relation to the actual threat posed by the phobic stimulus.
Choice B rationale:
The statement "Phobias can be caused by biological factors only" (choice B) is not accurate. While biological factors like genetics and brain chemistry can contribute to the development of phobias, they are not the sole cause. Psychological and environmental factors also play significant roles.
Choice C rationale:
The statement "Phobias can be diagnosed based on physical symptoms" (choice C) is incorrect. Phobias are diagnosed based on psychological symptoms, such as intense fear, avoidance behavior, and distress. Physical symptoms may accompany the fear response but are not the primary diagnostic criteria.
Choice D rationale:
The statement "Phobias can be managed with medication alone" (choice D) is not entirely accurate. While medication can help alleviate symptoms of anxiety associated with phobias, the most effective treatments often involve psychotherapy, particularly exposure therapy, to address the underlying fear response and promote lasting change.
Explanation
Choice A rationale:
Antipsychotics are not commonly prescribed to manage anxiety and fear associated with phobias. Antipsychotics are primarily used to treat psychotic disorders, such as schizophrenia, and are not the first-line treatment for anxiety-related disorders.
Choice B rationale:
Antihistamines are not commonly prescribed for managing anxiety and fear associated with phobias. While some sedating antihistamines might have a calming effect, they are not the primary choice for treating anxiety. Antihistamines are more commonly used for allergies and sleep disturbances.
Choice C rationale:
Anticonvulsants are not typically prescribed for managing anxiety and fear associated with phobias. Anticonvulsants are used to treat conditions such as epilepsy and mood disorders like bipolar disorder, but they are not the first-line treatment for specific phobias.
Choice D rationale:
Antidepressants are commonly prescribed to manage anxiety and fear associated with phobias. Selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs) are commonly used antidepressants that can effectively reduce the symptoms of anxiety and phobias by influencing neurotransmitter levels in the brain. These medications help regulate mood and reduce excessive anxiety associated with phobias.
Explanation
Choice A rationale:
Psychoeducation involves providing information about psychological conditions, symptoms, and treatment options to clients. However, it is not specifically aimed at helping clients identify and challenge irrational thoughts and beliefs associated with their phobias.
Choice B rationale:
Cognitive therapy aims to help clients identify and challenge irrational thoughts and beliefs associated with their phobias. By addressing cognitive distortions and negative thought patterns, individuals can learn to reframe their thinking, reduce anxiety, and manage their phobias more effectively.
Choice C rationale:
Behavioral therapy focuses on modifying behavior through techniques such as exposure therapy and desensitization. While behavioral therapy is often used in phobia treatment, it doesn't primarily target irrational thoughts and beliefs as cognitive therapy does.
Choice D rationale:
Relaxation therapy teaches individuals relaxation techniques to manage stress and anxiety. While relaxation techniques can be beneficial as a complementary approach, they are not specifically focused on addressing irrational thoughts associated with phobias.
Post-traumatic stress disorder (PTSD)
Post-traumatic stress disorder (PTSD)
Explanation
Choice A rationale:
Avoiding thoughts, feelings, people, places, or activities associated with the trauma is a symptom of post-traumatic stress disorder (PTSD), but it is not a re-experiencing symptom. This behavior is part of the avoidance and numbing cluster of symptoms in PTSD.
Choice B rationale:
Having persistent negative beliefs and emotions is another symptom of PTSD, but it is not a re-experiencing symptom. This is related to the negative alterations in cognitions and mood that individuals with PTSD may experience.
Choice C rationale:
Experiencing intrusive and distressing memories of the trauma is a re-experiencing symptom of PTSD. Individuals with PTSD may have flashbacks, nightmares, or intrusive thoughts about the traumatic event, causing distress and emotional turmoil.
Choice D rationale:
Feeling detached or estranged from others is a symptom of PTSD but is not considered a re-experiencing symptom. It falls under the category of alterations in arousal and reactivity, affecting the individual's ability to connect with others emotionally.
sandia: question and answer choice is accurate
sandia: question and answer choice is accurate
sandia: question and answer choice is accurate
Explanation
Choice A rationale:
PTSD can indeed occur after experiencing or witnessing a traumatic event. Trauma can lead to a range of psychological and physiological responses that characterize PTSD.
Choice B rationale:
PTSD is characterized by four main types of symptoms: re-experiencing, avoidance, negative alterations in cognition and mood, and alterations in arousal and reactivity. Re-experiencing symptoms involve intrusive memories or flashbacks, avoidance symptoms involve efforts to avoid reminders of the trauma, negative alterations in cognition and mood encompass feelings of guilt, blame, and distorted thoughts, while alterations in arousal and reactivity can include irritability and exaggerated startle response.
Choice C rationale:
Cognitive-behavioral therapy (CBT) is indeed a recognized and effective treatment option for PTSD. CBT helps individuals identify and change negative thought patterns and behaviors associated with their trauma, aiming to reduce distress and improve coping mechanisms.
Choice D rationale:
PTSD is not limited to a specific duration for diagnosis. Symptoms must persist for more than a month and cause significant impairment in functioning, but there is no requirement for symptoms to last for more than one year.
Choice E rationale:
While it is true that individuals with a history of mental illness are generally more susceptible to developing various mental health conditions, this statement is not wholly accurate. PTSD can affect anyone exposed to traumatic events, regardless of their mental health history.
Explanation
Choice B rationale:
The statement "I try to avoid going to places that remind me of the trauma." indicates the presence of avoidance symptoms, which are a hallmark of PTSD. Avoidance symptoms involve efforts to stay away from situations, places, or people that trigger memories of the traumatic event.
Explanation
Choice D rationale:
The statement "I believe that the world is completely dangerous." indicates the presence of negative alterations in cognition and mood symptoms, which are another facet of PTSD. These symptoms often involve a distorted perception of the world, including beliefs about danger and an inability to trust others.
Explanation
Choice A rationale:
Encouraging the client to avoid talking about the traumatic event would not be a suitable intervention for a client with post-traumatic stress disorder (PTSD) Avoidance can exacerbate symptoms and hinder the healing process. Discussing the traumatic event in a safe and therapeutic environment is an essential part of PTSD treatment.
Choice B rationale:
Assisting the client in identifying and challenging negative thoughts is a crucial intervention for individuals with PTSD. Cognitive Behavioral Therapy (CBT) is a recommended approach for treating PTSD, and it involves addressing distorted or negative thought patterns that contribute to the distressing symptoms. By challenging and reframing these thoughts, clients can learn to manage their symptoms and regain a sense of control.
Choice C rationale:
Encouraging the client to engage in risky behaviors to cope with stress is not appropriate and can potentially worsen the client's condition. Engaging in risky behaviors could lead to harm and complicate the treatment process. Instead, promoting healthy coping mechanisms and stress-reduction strategies would be more beneficial.
Choice D rationale:
Referring the client to a support group for individuals with anxiety disorders might not be the most suitable intervention for PTSD. While anxiety disorders and PTSD share some similarities, they are distinct conditions with different treatment approaches. A support group specifically focused on PTSD would provide more tailored and effective assistance.
Explanation
Choice A rationale:
Being male is not a risk factor for developing PTSD. PTSD can affect individuals of any gender. While there may be differences in the prevalence and expression of symptoms between genders, being male alone is not a risk factor for developing the disorder.
Choice B rationale:
Having a family history of PTSD is a recognized risk factor for developing the disorder. Genetics and family environment can play a role in the predisposition to PTSD. Individuals with a family history of trauma-related disorders might have a higher vulnerability to developing PTSD after exposure to a traumatic event.
Choice C rationale:
Having exposure to media coverage of trauma can contribute to distress, anxiety, and even trigger symptoms in individuals with PTSD. However, it is not considered a primary risk factor for developing the disorder. Other factors, such as personal trauma history and individual vulnerability, play a more significant role.
Choice D rationale:
Having good social support is actually a protective factor against developing PTSD. Adequate social support can buffer the impact of trauma and contribute to better resilience and recovery. It is not a risk factor but rather a positive factor that can help mitigate the effects of trauma.
Explanation
Choice A rationale:
Assessing the client's physical health is a priority because physical health issues can significantly impact the overall well-being of an individual with PTSD. Trauma and chronic stress can lead to physical health problems, including sleep disturbances, cardiovascular issues, and gastrointestinal problems. Addressing these physical concerns is essential for a holistic approach to care.
Choice B rationale:
Assessing the client's coping skills is important, but it may not be the top priority. Coping skills assessment is essential for treatment planning, but addressing immediate physical health needs and safety concerns takes precedence, especially if the client is experiencing acute distress.
Choice C rationale:
Assessing the client's social support is important for long-term recovery, but it may not be the primary assessment in the initial stages of care. Social support can contribute to resilience, but addressing physical health and acute distress is more critical initially.
Choice D rationale:
Assessing the client's past trauma history is relevant for understanding the context of the disorder, but it might not be the priority in the moment. Trauma history can be explored in therapy sessions, but addressing immediate physical and emotional needs comes first.
A nurse is caring for a client with post-traumatic stress disorder (PTSD) Which of the following nursing interventions should the nurse implement? (Select all that apply.)
Explanation
The correct answer is Choice A, Choice B, Choice D.
Choice A rationale: Promoting self-care and healthy lifestyle habits is essential for clients with PTSD. It helps improve overall well-being, reduces stress, and enhances the effectiveness of other therapeutic interventions, contributing to a more comprehensive treatment approach.
Choice B rationale: Teaching the client relaxation techniques is crucial for managing PTSD symptoms. Techniques such as deep breathing, progressive muscle relaxation, and mindfulness can help reduce anxiety, improve emotional regulation, and provide coping mechanisms during stressful situations.
Choice C rationale: Assisting the client in avoiding triggers and symptoms is not typically recommended for PTSD management. Avoidance can reinforce fear and hinder the healing process. Instead, clients are encouraged to gradually face and process their triggers with appropriate support.
Choice D rationale: Facilitating exposure therapy is a key intervention for PTSD. It involves safely and gradually exposing the client to trauma-related stimuli, helping them process traumatic memories, reduce avoidance behaviors, and diminish the emotional impact of the trauma over time.
A nurse is educating a client about the pharmacological treatments for PTSD. Which of the following medications is an atypical antipsychotic commonly used in the management of PTSD?
Explanation
Choice A rationale:
Sertraline (Choice A) is a selective serotonin reuptake inhibitor (SSRI) commonly used to treat conditions such as depression and anxiety disorders. While it may be beneficial in managing certain symptoms of PTSD, it is not classified as an atypical antipsychotic.
Choice B rationale:
Risperidone (Choice B) is an atypical antipsychotic that can be used in the management of PTSD, particularly for reducing hyperarousal symptoms, aggression, and irritability. It helps regulate neurotransmitter activity and has shown efficacy in controlling certain PTSD-related symptoms.
Choice C rationale:
Venlafaxine (Choice C) is a serotonin-norepinephrine reuptake inhibitor (SNRI) used to treat various mood disorders. While it may have some benefits in treating anxiety symptoms associated with PTSD, it is not categorized as an atypical antipsychotic.
Choice D rationale:
Lamotrigine (Choice D) is an anticonvulsant primarily used in the treatment of epilepsy and bipolar disorder. It is not a typical medication for managing PTSD symptoms.
A nurse is providing teaching to a group of clients with PTSD. Which of the following non-pharmacological therapies is considered a trauma-focused psychotherapy?
Explanation
Choice A rationale:
Acupuncture (Choice A) is an alternative therapy that involves inserting thin needles into specific points on the body. While it may have benefits for pain management and relaxation, it is not considered a trauma-focused psychotherapy for PTSD.
Choice B rationale:
Yoga (Choice B) is a mind-body practice that can promote relaxation and stress reduction. While it can be a helpful component of a holistic approach to managing PTSD, it is not specifically classified as trauma-focused psychotherapy.
Choice C rationale:
Cognitive processing therapy (Choice C) is a well-established trauma-focused psychotherapy for PTSD. It involves helping clients process and reframe their traumatic experiences by challenging and modifying negative beliefs and thoughts associated with the trauma.
Choice D rationale:
Biofeedback (Choice D) is a technique that teaches individuals to control physiological functions, such as heart rate and muscle tension, through relaxation techniques. While it can aid in stress management, it is not a trauma-focused psychotherapy.
Choice E rationale:
Virtual reality therapy (Choice E) is a novel approach that uses virtual reality technology to expose individuals to controlled, virtual traumatic scenarios in a therapeutic setting. It can be effective in treating PTSD by allowing controlled exposure to triggers, but it's not a traditional trauma-focused psychotherapy method.
Explanation
Choice A rationale:
If the client states, "I am experiencing a reduction in PTSD symptoms," it reflects a positive change but not necessarily a comprehensive improvement. Reduction in symptoms could be due to various factors, and it might not indicate overall progress in managing PTSD.
Choice B rationale:
This choice indicates a positive outcome because improved coping skills and resilience are fundamental aspects of successful PTSD management. This suggests that the client has learned to deal with triggers and stressors more effectively, leading to better emotional regulation and adaptation.
Choice C rationale:
"I have restored self-esteem and identity" is important for psychological well-being, but it specifically focuses on self-esteem and identity rather than the broader range of symptoms associated with PTSD. While this could be a part of the recovery process, it's not as comprehensive as improved coping skills and resilience.
Choice D rationale:
"I have reintegration into society and relationships" also reflects progress, but it pertains to the social aspects of recovery rather than the individual's internal coping mechanisms. Social reintegration is crucial, but it may not directly correlate with better management of PTSD symptoms.
Explanation
Choice A rationale:
The severity of the trauma can influence the effectiveness of treatment since more severe traumas might require more intensive interventions. Higher severity could also lead to increased resistance to treatment.
Choice B rationale:
The availability of treatment options is significant because limited options might restrict the client's access to suitable interventions, potentially affecting the treatment's success.
Choice C rationale:
Adherence and compliance of the client play a vital role. If the client does not follow the treatment plan consistently, the effectiveness of any intervention can be compromised.
Choice D rationale:
This is the correct answer as all of the mentioned factors can impact the effectiveness of PTSD management. The severity of trauma, treatment availability, and client adherence are interrelated aspects that collectively influence the outcome.
Choice E rationale:
"None of the above" is not the correct answer since each of the factors mentioned can indeed impact the effectiveness of treatment in various ways.
Explanation
Choice A rationale:
Acupuncture is not one of the therapies that have substantial evidence for effectiveness in treating PTSD. While acupuncture has been explored for various conditions, including pain and anxiety, its evidence for treating PTSD specifically is limited and inconsistent.
Choice B rationale:
Yoga can be beneficial for individuals with PTSD as it combines physical postures, breathing exercises, and meditation, which can help manage stress and anxiety. However, the evidence for its effectiveness is not as strong as for meditation, which has shown more consistent results in reducing PTSD symptoms.
Choice C rationale:
Meditation, particularly mindfulness meditation, has demonstrated some evidence of effectiveness for PTSD. Mindfulness meditation involves focusing on the present moment and accepting thoughts and feelings without judgment. Studies have shown that it can reduce symptoms of hyperarousal, intrusive thoughts, and avoidance behaviors commonly associated with PTSD.
Choice D rationale:
Hypnosis is not considered a first-line therapy for PTSD. While some limited studies have explored its potential benefits, it lacks the robust evidence that other therapies like meditation and cognitive-behavioral therapies possess.
Explanation
Choice A rationale:
Sertraline is recommended as a first-line pharmacological treatment for PTSD by the National Institute for Health and Care Excellence (NICE) It is a selective serotonin reuptake inhibitor (SSRI) that has shown effectiveness in reducing PTSD symptoms, particularly in terms of intrusive thoughts and avoidance behaviors.
Choice B rationale:
Venlafaxine is also an antidepressant, but it is generally considered a second-line treatment option for PTSD. It might be considered if SSRIs are ineffective or not tolerated due to its different mechanism of action as a serotonin-norepinephrine reuptake inhibitor (SNRI)
Choice C rationale:
Amitriptyline is a tricyclic antidepressant that is not commonly recommended for the first-line treatment of PTSD. SSRIs like sertraline are preferred due to their generally more favorable side effect profiles.
Choice D rationale:
Mirtazapine is another antidepressant with different pharmacological properties compared to SSRIs. However, like venlafaxine, it is typically considered a second-line option for treating PTSD.
A nurse is providing teaching to a group of clients with PTSD. Which of the following non-pharmacological therapies has been shown to reduce PTSD symptoms by 50% to 80% in most clients after 8 to 16 sessions?
Explanation
Choice A rationale:
Prolonged exposure (PE) is a type of cognitive-behavioral therapy that involves confronting and processing traumatic memories. While it is effective for many individuals with PTSD, its effectiveness in reducing symptoms by 50% to 80% in most clients after 8 to 16 sessions is not as consistently reported as with EMDR.
Choice B rationale:
Cognitive processing therapy (CPT) focuses on addressing maladaptive beliefs related to the traumatic event. While it can be effective, its reported symptom reduction rates may vary, and it might not consistently achieve the 50% to 80% reduction mentioned.
Choice C rationale:
Eye movement desensitization and reprocessing (EMDR) is a well-established therapy specifically designed for trauma-related disorders like PTSD. Research indicates that many individuals experience significant symptom reduction within 8 to 16 sessions, with reported rates often falling within the 50% to 80% range.
Choice D rationale:
Acceptance and commitment therapy (ACT) and dialectical behavior therapy (DBT) are therapies often used for conditions like depression and anxiety but may not have as robust a body of evidence for PTSD treatment as EMDR or certain cognitive-behavioral therapies.
Pharmacological Management of Anxiety Disorders
Explanation
Choice A rationale:
Completely eliminate anxiety symptoms. While this might be an ideal goal, it's not always achievable due to the nature of anxiety disorders. Anxiety is a normal human emotion, and the goal of treatment is to manage it rather than eliminate it completely.
Choice B rationale:
Reduce the severity and frequency of anxiety symptoms. This is the correct goal of pharmacological treatment for anxiety disorders. Complete elimination of anxiety symptoms is often unrealistic, but reducing their severity and frequency can significantly improve the patient's quality of life.
Choice C rationale:
Treat the underlying cause of anxiety disorders. Anxiety disorders are multifactorial, involving genetic, environmental, and psychological factors. While addressing underlying causes is important, pharmacological treatment primarily aims to manage symptoms rather than target the complex underlying causes.
Choice D rationale:
Prevent comorbidities associated with anxiety disorders. While effective anxiety treatment can potentially prevent some comorbidities, such as depression, the primary focus of pharmacological treatment is directly on managing anxiety symptoms rather than solely preventing associated conditions.
Explanation
Choice A rationale:
Enhance the activity of gamma-aminobutyric acid (GABA) in the brain. Benzodiazepines are known to enhance the inhibitory effects of GABA, the major inhibitory neurotransmitter in the central nervous system. This results in reduced neuronal excitability, leading to the anxiolytic (anxiety-reducing) effects of benzodiazepines.
Choice B rationale:
Block beta-adrenergic receptors in the heart and blood vessels. This statement is incorrect. While beta-blockers can be used to manage certain physical symptoms of anxiety (such as rapid heartbeat), benzodiazepines do not directly block beta-adrenergic receptors.
Choice C rationale:
Partially agonize serotonin 5-HT1A receptors and antagonize dopamine D2 receptors. This statement is inaccurate. Benzodiazepines primarily interact with GABA receptors, not serotonin or dopamine receptors.
Choice D rationale:
Modulate the activity of various neurotransmitters and ion channels in the brain. This statement is overly broad and doesn't accurately describe the specific mechanism of benzodiazepines. Their primary mode of action is through enhancing GABAergic inhibition.
Explanation
Choice A rationale:
"I feel like something bad is going to happen." This statement is similar to the correct answer, but it lacks the specific phrase "impending doom," which is a hallmark description in anxiety-related disorders.
Choice B rationale:
"My heart is racing, and I can't catch my breath." This statement focuses on physiological symptoms and doesn't capture the broader sense of anxiety and apprehension that the patient is expressing.
Choice C rationale:
"I feel anxious and restless." While this choice captures the patient's emotional state, it doesn't include the crucial phrase "impending doom," which is a common and specific expression of anxiety.
Choice D rationale:
"I have a feeling of impending doom." This statement precisely captures the patient's description of their emotions and physical sensations, which is characteristic of anxiety and panic disorders. It reflects the patient's perception of a potential catastrophe about to occur.
Explanation
Choice A rationale:
Rapid onset of action - Antidepressant medications with rapid onset of action, such as selective serotonin reuptake inhibitors (SSRIs), can lead to quicker relief of symptoms. However, the nurse's statement mentions that it may take several weeks for the medication to start working fully, which contradicts the idea of rapid onset. Therefore, this choice is not applicable.
Choice B rationale:
Long duration of action - Antidepressants with long duration of action might provide sustained symptom relief once they take effect, but the nurse's statement focuses on the time it takes for the medication to start working fully rather than its duration of action. Thus, this choice is not relevant.
Choice C rationale:
Choice D rationale:
Slow onset of therapeutic effect - The nurse's statement, "It may take several weeks for the medication to start working fully," suggests that the medication has a slow onset of therapeutic effect. This is characteristic of many antidepressant medications, which often require several weeks of consistent use before significant symptom improvement is observed.
Explanation
Choice A rationale:
Enhance the activity of gamma-aminobutyric acid (GABA) in the brain - This choice is not accurate. Beta-blockers do not enhance GABA activity; instead, they affect adrenergic pathways in the body.
Choice B rationale:
Block beta-adrenergic receptors in the heart and blood vessels - This is correct. Beta-blockers primarily work by blocking beta-adrenergic receptors, leading to reduced heart rate, decreased blood pressure, and decreased cardiac output. In the context of social anxiety disorder, beta-blockers can help manage physical symptoms of anxiety, such as tremors and rapid heartbeat.
Choice C rationale:
Partially agonize serotonin 5-HT1A receptors and antagonize dopamine D2 receptors - This choice is not accurate. Beta-blockers do not significantly interact with serotonin or dopamine receptors in this manner.
Choice D rationale:
Modulate the activity of various neurotransmitters and ion channels in the brain - This is also correct. While beta-blockers are primarily known for their effects on adrenergic pathways, they can also have indirect effects on various neurotransmitters and ion channels in the brain, contributing to their anxiolytic properties.
Explanation
Choice A rationale:
Diazepam - Diazepam is a benzodiazepine commonly used to treat anxiety disorders, but it's not typically considered a first-line agent for panic disorder due to concerns about dependence and withdrawal.
Choice B rationale:
Buspirone - This is the correct answer. Buspirone is often used as a first-line agent for the treatment of panic disorder. It is a non-benzodiazepine anxiolytic that works by interacting with serotonin and dopamine receptors, providing anxiolytic effects without the risk of significant sedation or dependence.
Choice C rationale:
Fluoxetine - Fluoxetine is an SSRI commonly used to treat depression and some anxiety disorders, including panic disorder. However, it might not be the first-line choice due to its delayed onset of action compared to other treatments.
Choice D rationale:
Pregabalin - Pregabalin is an anticonvulsant used to treat various conditions, including neuropathic pain and generalized anxiety disorder. It may be used in the treatment of panic disorder in some cases, but it's not typically considered a first-line option.
Choice E rationale:
Propranolol - Propranolol is a beta-blocker that can help manage physical symptoms of anxiety, such as rapid heartbeat and tremors. While it may be used adjunctively in panic disorder treatment, it's not a first-line choice for addressing the core symptoms of panic disorder.
A nurse is providing education to a patient with generalized anxiety disorder who has been prescribed a benzodiazepine medication. The nurse instructs the patient to avoid consuming alcohol while taking the medication.
Which of the following is the rationale for this instruction?
Explanation
Choice A rationale:
Benzodiazepines are central nervous system (CNS) depressants, and alcohol also has a depressant effect on the CNS. When combined, they can potentiate each other's effects, leading to excessive sedation, dizziness, and impaired coordination. This can result in increased risks of accidents and injuries.
Choice B rationale:
While alcohol can indeed enhance the sedative effects of benzodiazepines, this is not the primary reason for instructing the patient to avoid alcohol. The main concern is the potential for adverse interactions, as mentioned in choice C.
Choice C rationale:
(Correct Choice) Alcohol can cause adverse interactions with benzodiazepines. Both substances act as depressants on the CNS, and their combined use can lead to severe sedation, respiratory depression, and even coma or death. In addition, the combination can impair cognitive and motor functions, making it unsafe to engage in activities such as driving.
Choice D rationale:
Alcohol's potential to increase the risk of dependence on benzodiazepines is a valid concern, but it is not the primary reason for advising the patient to avoid alcohol. The immediate risk of adverse interactions takes precedence.
Choice E rationale:
While alcohol can worsen the symptoms of anxiety disorder, this is not the primary reason for instructing the patient to avoid alcohol. The focus here is on the potential dangerous interactions between alcohol and benzodiazepine medications.
A nurse is caring for a patient with obsessive-compulsive disorder (OCD). The nurse understands that the pharmacological treatment for OCD often involves the use of which of the following medications? (Select all that apply.)
Explanation
Choice A rationale:
(Correct Choice) Fluoxetine is a selective serotonin reuptake inhibitor (SSRI) commonly used in the treatment of obsessive-compulsive disorder (OCD). It helps to increase serotonin levels in the brain, which can alleviate the symptoms of OCD. SSRIs are considered first-line treatments for OCD due to their efficacy and relatively favorable side effect profile.
Choice B rationale:
Clonazepam is not typically used as a first-line treatment for OCD. It is a benzodiazepine that can be helpful for anxiety-related conditions but is not among the primary medications prescribed specifically for OCD.
Choice C rationale:
Venlafaxine is an antidepressant that primarily affects serotonin and norepinephrine levels. While it can be used for conditions like generalized anxiety disorder and major depressive disorder, it is not a first-line treatment for OCD.
Choice D rationale:
Buspirone is used to treat generalized anxiety disorder but is not one of the preferred medications for treating OCD. It works differently from SSRIs and does not have the same established evidence base for managing OCD symptoms.
Choice E rationale:
(Correct Choice) Sertraline is another SSRI commonly used in the treatment of OCD. Similar to fluoxetine, sertraline increases serotonin levels, which can help reduce the obsessions and compulsions associated with OCD. Its efficacy and tolerability make it a suitable choice for OCD treatment.
Exams on Disorders of Anxiety
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
- Objectives
- Introduction
- Risk Factors and Causes
- Clinical Manifestations and Diagnostic Criteria
- Nursing Interventions and Pharmacological Treatments
- Generalized anxiety disorder (GAD)
- Panic Disorder
- Phobias
- Post-traumatic stress disorder (PTSD)
- Pharmacological Management of Anxiety Disorders
- Objectives
Notes Highlighting is available once you sign in. Login Here.
Objectives
- Define anxiety and its types, causes, and symptoms.
- Explain the pathophysiology and epidemiology of anxiety disorders.
- Identify the assessment and diagnostic tools for anxiety disorders.
- Describe the pharmacological and non-pharmacological management of anxiety disorders.
- Discuss the nursing interventions and education for patients with anxiety disorders.
- Evaluate the outcomes and complications of anxiety disorders.
Introduction
- Anxiety is a normal and adaptive response to stress, threat, or danger that helps us cope and survive.

- Anxiety disorders are a group of mental health conditions characterized by excessive, persistent, and irrational fear or worry that interferes with daily functioning and quality of life.
- Anxiety disorders are the most common psychiatric disorders, affecting about 18% of adults and 25% of children and adolescents in the US
- Anxiety disorders can be classified into several types, such as generalized anxiety disorder (GAD), panic disorder (PD), phobias, social anxiety disorder (SAD), obsessive-compulsive disorder (OCD), and post-traumatic stress disorder (PTSD).
- Anxiety disorders can have various causes, such as genetic factors, environmental factors, neurobiological factors, psychological factors, and medical conditions or substance use.
- Anxiety disorders can have various signs and symptoms, such as physical symptoms (e.g., palpitations, sweating, trembling, chest pain, shortness of breath, nausea, dizziness), cognitive symptoms (e.g., negative thoughts, fear of losing control, fear of dying, fear of embarrassment or rejection), and behavioral symptoms (e.g., avoidance, escape, compulsions, rituals).
- Anxiety disorders can be diagnosed using standardized criteria from the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), clinical interviews, psychological tests, and medical tests to rule out other causes.
- Anxiety disorders can be treated using various modalities, such as psychotherapy (e.g., cognitive-behavioral therapy [CBT], exposure therapy, relaxation techniques), pharmacotherapy (e.g., antidepressants, benzodiazepines, beta-blockers), complementary and alternative therapies (e.g., herbal remedies, acupuncture, yoga), and self-help strategies (e.g., education, support groups, lifestyle changes).
Risk Factors and Causes
- The exact etiology of anxiety disorders is unknown, but it is likely influenced by a combination of biological, psychological, environmental, and genetic factors
- Some of the risk factors and causes of anxiety disorders include
- Family history of anxiety or other mental disorders
- History of trauma, abuse, or violence
- Personality traits such as neuroticism, perfectionism, or low self-esteem
- Stressful life events or transitions
- Medical conditions such as thyroid disorders, cardiac arrhythmias, asthma, or chronic pain
- Substance use or withdrawal from alcohol, caffeine, nicotine, or drugs
- Medications such as corticosteroids, antihypertensives, or bronchodilators
Clinical Manifestations and Diagnostic Criteria
- The clinical manifestations of anxiety disorders vary depending on the type, severity, and duration of the disorder.
- However, some common signs and symptoms include
- Cognitive: irrational or excessive fear, worry, or nervousness; difficulty concentrating or remembering; negative or catastrophic thinking; confusion or disorientation
- Behavioral: avoidance of feared situations or objects; restlessness or agitation; compulsive or repetitive behaviors; impaired social or occupational functioning; increased use of coping mechanisms such as smoking, drinking, or overeating
- Physical: palpitations, chest pain, dyspnea, hyperventilation, sweating, trembling, nausea, diarrhea, dizziness, headache, insomnia, fatigue, muscle tension
- The diagnostic criteria for anxiety disorders are based on the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), which provides specific features and duration for each type of disorder
- For example:
- Generalized anxiety disorder (GAD): excessive and persistent worry about various aspects of life for at least 6 months that is difficult to control and causes significant distress or impairment
- Panic disorder (PD): recurrent and unexpected panic attacks that are followed by at least 1 month of persistent concern or fear about having another attack or its consequences
- A panic attack is a sudden surge of intense fear or discomfort that reaches a peak within minutes and is accompanied by at least four physical or cognitive symptoms
- Phobias: marked and persistent fear of a specific object or situation that provokes immediate anxiety and avoidance behavior that is out of proportion to the actual danger posed by the object or situation
- .
- Phobias can be classified into three types: specific phobia (e.g., fear of animals), social phobia (e.g., fear of public speaking), and agoraphobia (e.g., fear of open spaces)
- Obsessive-compulsive disorder (OCD): presence of obsessions and/or compulsions that are time-consuming (more than 1 hour per day) and cause significant distress or impairment
- . Obsessions are recurrent and intrusive thoughts, images, or impulses that cause anxiety.
- Compulsions are repetitive behaviors or mental acts that are performed to reduce anxiety caused by obsessions.
- Post-traumatic stress disorder (PTSD): exposure to a traumatic event that involved actual or threatened death, serious injury, or sexual violence that causes persistent re-experiencing of the event (e.g., flashbacks), avoidance of stimuli associated with the event (e.g., places), negative alterations in cognition and mood (e.g., guilt), and increased arousal and reactivity (e.g., hypervigilance) for more than 1 month after the event
- Acute stress disorder (ASD): similar to PTSD, but the symptoms last from 3 days to 1 month after the traumatic event
Nursing Interventions and Pharmacological Treatments

- The nursing interventions for anxiety disorders are aimed at reducing anxiety, promoting coping skills, enhancing self-esteem, and improving quality of life
- Some of the nursing interventions include:
- Establishing a therapeutic relationship with the client based on trust, empathy, and respect
- Assessing the client’s level of anxiety, triggers, coping mechanisms, and support system
- Providing a safe and calm environment for the client
- Encouraging the client to express feelings and concerns without judgment or criticism
- Educating the client about the nature, causes, and treatment of anxiety disorders
- Teaching the client relaxation techniques such as deep breathing, progressive muscle relaxation, guided imagery, or meditation
- Assisting the client to identify and challenge negative or irrational thoughts and replace them with positive or realistic ones
- Helping the client to set realistic and achievable goals and reinforce small steps of progress
- Referring the client to other resources such as psychotherapy, support groups, or community services
- The pharmacological treatments for anxiety disorders are aimed at reducing the symptoms and enhancing the effects of psychotherapy. Some of the pharmacological treatments include:
- Antidepressants: such as selective serotonin reuptake inhibitors (SSRIs), serotonin-norepinephrine reuptake inhibitors (SNRIs), tricyclic antidepressants (TCAs), or monoamine oxidase inhibitors (MAOIs) that increase the availability of neurotransmitters such as serotonin and norepinephrine in the brain that regulate mood and anxiety . Examples are fluoxetine, sertraline, venlafaxine, imipramine, or phenelzine .
- Anxiolytics: such as benzodiazepines or buspirone that enhance the activity of gamma-aminobutyric acid (GABA), a neurotransmitter that inhibits anxiety and induces relaxation . Examples are diazepam, alprazolam, or buspirone .
- Beta-blockers: such as propranolol or atenolol block the effects of adrenaline and reduce the physical symptoms of anxiety such as palpitations, tremors, or sweating.
- Anticonvulsants: such as gabapentin or pregabalin modulate the activity of glutamate, a neurotransmitter that mediates excitatory signals in the brain that may contribute to anxiety.
- Antihistamines: such as hydroxyzine or diphenhydramine have sedative effects and reduce anxiety by blocking histamine receptors in the brain .
Outcomes and Complications
- The outcomes of anxiety disorders depend on several factors such as the type, severity, duration, comorbidity, treatment adherence, and response of the disorder. Some of the possible outcomes include:
- Improvement or remission of symptoms with appropriate treatment
- Maintenance or enhancement of functioning and quality of life
- Development of coping skills and resilience
- Prevention or reduction of relapse or recurrence
- The complications of anxiety disorders include:
- Impairment in social, occupational, academic, or personal domains
- Increased risk of depression, substance abuse, suicide, or other mental disorders
- Decreased physical health due to chronic stress or somatic complaints
- Reduced adherence to medical treatment or self-care
Nursing Process and Critical Thinking
- The nursing process is a systematic and dynamic method of providing holistic and individualized care to clients with anxiety disorders. It involves five steps: assessment, diagnosis, planning, implementation, and evaluation.
- The nursing process and critical thinking skills are interrelated and essential for providing safe and effective care to clients with anxiety disorders. They enable the nurse to:
- Collect relevant data from various sources to identify actual or potential problems
- Interpret and prioritize data to formulate accurate and appropriate nursing diagnoses
- Establish measurable and realistic outcomes and interventions based on evidence-based practice and client preferences
- Implement interventions using clinical judgment and technical skills to achieve the desired outcomes
- Evaluate the effectiveness of interventions and outcomes and modify the plan of care as needed
Generalized anxiety disorder (GAD)
- Generalized anxiety disorder (GAD) is a chronic and persistent condition characterized by excessive and uncontrollable worry about various aspects of life, such as health, work, family, or social situations.
- The worry is disproportionate to the actual likelihood or impact of the feared events, causes significant distress or impairment in daily functioning, and lasts for at least 6 months.
- GAD affects about 3.1% of the U.S. adult population in any given year, and is more common in women than in men.
- GAD can coexist with other mental disorders, such as depression, panic disorder, phobias, or substance use disorders.
Risk Factors and Causes:
- The exact cause of GAD is unknown, but it is likely influenced by a combination of biological, psychological, and environmental factors.
- Some of the risk factors for developing GAD include:
- Family history of anxiety disorders or other mental illnesses
- History of trauma, abuse, or stressful life events
- Personality traits such as neuroticism, perfectionism, or low self-esteem
- Chronic medical conditions such as cardiovascular disease, diabetes, or chronic pain
- Substance use or withdrawal from alcohol, nicotine, caffeine, or illicit drugs
Clinical Manifestations and Complications
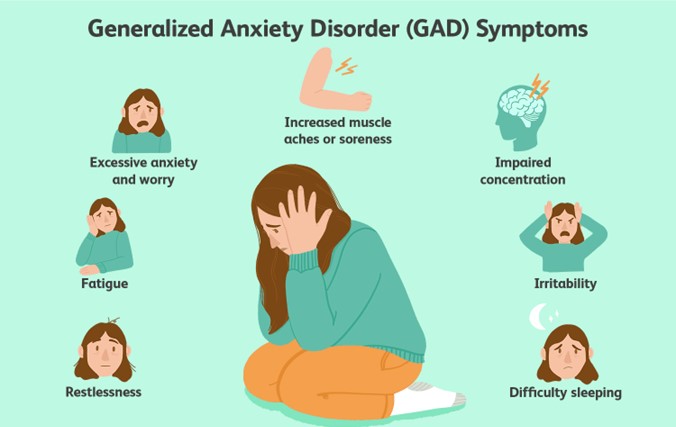
- The main symptom of GAD is excessive and persistent worry that interferes with daily activities and causes significant distress.
- The worry may focus on various domains, such as health, finances, relationships, work performance, or future events.
- The worry is difficult to control and often leads to avoidance of situations that may trigger anxiety.
- In addition to worry, people with GAD may experience a variety of physical and psychological symptoms, such as:
- Restlessness or feeling on edge
- Fatigue or difficulty sleeping
- Irritability or mood swings
- Muscle tension or pain
- Headaches or gastrointestinal problems
- Difficulty concentrating or remembering
- Nervousness or trembling
- Palpitations or chest pain
- Shortness of breath or hyperventilation
- Sweating or hot flashes
- Nausea or dizziness
- The symptoms of GAD may vary in intensity and frequency depending on the level of stress, coping skills, and treatment adherence.
- If left untreated, GAD can lead to serious complications, such as:
- Impaired social and occupational functioning
- Reduced quality of life and well-being
- Increased risk of depression, suicide, or substance abuse
- Increased risk of cardiovascular disease, hypertension, diabetes, or obesity
Nursing Assessment and Diagnosis:
- The nursing assessment for a client with GAD involves collecting data from various sources, such as the client’s history, physical examination, mental status examination, screening tools, laboratory tests, and diagnostic criteria.
- Some of the data that the nurse should obtain include:
- The onset, duration, frequency, severity, and triggers of worry and anxiety symptoms
- The impact of worry and anxiety on daily functioning and quality of life
- The coping strategies and resources that the client uses to manage worry and anxiety
- The presence of any coexisting mental or physical disorders that may affect worry and anxiety
- The client’s medication history, including any prescribed or over-the-counter drugs, herbal supplements, or substances that may affect worry and anxiety
- The client’s family history of anxiety disorders or other mental illnesses
- The client’s personal history of trauma, abuse, or stressful life events that may contribute to worry and anxiety
- The client’s level of insight, motivation, readiness for change, and expectations for treatment outcomes
- The nurse should also perform a physical examination to assess for any signs of anxiety-related symptoms or complications, such as vital signs, cardiovascular system, respiratory system, musculoskeletal system, neurological system, gastrointestinal system, and skin.
- The nurse should also conduct a mental status examination to evaluate the client’s cognitive, emotional, and behavioral aspects, such as orientation, attention, memory, judgment, mood, affect, thought process, thought content, perception, insight, and impulse control.
- The nurse should also use screening tools to measure the severity and impact of worry and anxiety, such as the Generalized Anxiety Disorder 7-item (GAD-7) scale, the Hamilton Anxiety Rating Scale (HAM-A), or the Penn State Worry Questionnaire (PSWQ).
- The nurse should also order laboratory tests to rule out any medical conditions that may cause or mimic anxiety symptoms, such as thyroid function tests, blood glucose levels, electrolyte levels, complete blood count, urine drug screen, or toxicology screen.
- The nurse should also compare the data collected with the diagnostic criteria for GAD according to the Diagnostic and Statistical Manual of Mental Disorders, 5th edition (DSM-5), which are:
- Excessive anxiety and worry about a number of events or activities, occurring more days than not for at least 6 months
- Difficulty controlling the worry
- Anxiety and worry associated with at least three of the following six symptoms: restlessness, fatigue, difficulty concentrating, irritability, muscle tension, sleep disturbance
- Anxiety and worry causing clinically significant distress or impairment in social, occupational, or other important areas of functioning
- Anxiety and worry not attributable to the physiological effects of a substance or another medical condition
- Anxiety and worry not better explained by another mental disorder
- Based on the assessment data, the nurse can formulate nursing diagnoses for the client with GAD. Some of the possible nursing diagnoses are:
- Anxiety related to perceived threats or uncertainties
- Ineffective coping related to inadequate or maladaptive coping skills
- Disturbed sleep pattern related to anxiety symptoms
- Impaired social interaction related to anxiety symptoms
- Chronic pain related to muscle tension
- Risk for self-directed violence related to hopelessness or depression
Nursing Interventions and Rationales:
- The nursing interventions for a client with GAD are aimed at reducing anxiety and worry, enhancing coping skills and resources, promoting physical and mental health, and preventing complications.
- Some of the nursing interventions and rationales are :
- Establish a therapeutic relationship with the client based on trust, respect, empathy, and genuineness. This helps to create a safe and supportive environment for the client to express feelings, concerns, and needs.
- Provide education and information to the client about GAD, its causes, symptoms, treatment options, and prognosis. This helps to increase the client’s knowledge, insight, motivation, and adherence to treatment.
- Encourage the client to participate in cognitive-behavioral therapy (CBT), which is an evidence-based psychotherapy that focuses on identifying and challenging negative thoughts and beliefs that contribute to worry and anxiety. This helps to modify the client’s cognitive distortions, reduce anxiety symptoms, and improve coping skills.
- Encourage the client to practice relaxation techniques, such as deep breathing, progressive muscle relaxation, guided imagery, meditation, or yoga. This helps to reduce physiological arousal, muscle tension, and stress levels.
- Encourage the client to engage in physical activity, such as walking, jogging, swimming, or cycling. This helps to release endorphins, improve mood, and distract from worry.
- Encourage the client to maintain a healthy lifestyle, such as eating a balanced diet, drinking enough water, avoiding caffeine, alcohol, nicotine, and illicit drugs, and following a regular sleep schedule. This helps to enhance physical and mental well-being and prevent complications.
- Encourage the client to use positive coping strategies, such as problem-solving, goal-setting, time management, assertiveness, humor, or hobbies. This helps to increase the client’s sense of control, self-efficacy, and satisfaction.
- Encourage the client to seek social support from family, friends, or support groups. This helps to reduce isolation, loneliness, and stigma.
- Administer prescribed anti-anxiety medications as ordered by the provider. Some of the common medications used for GAD include selective serotonin reuptake inhibitors (SSRIs), such as fluoxetine or sertraline; serotonin-norepinephrine reuptake inhibitors (SNRIs), such as venlafaxine or duloxetine; buspirone; or benzodiazepines, such as alprazolam or lorazepam. These medications help to reduce anxiety symptoms by modulating neurotransmitter activity in the brain.
- Monitor for adverse effects of anti-anxiety medications, such as nausea, drowsiness, dizziness, headache, weight gain or loss, sexual dysfunction, or dependence. Report any abnormal
- Report any abnormal findings or reactions to the provider and adjust the medication dosage or regimen as needed. This helps to ensure the safety and effectiveness of pharmacological treatment.
- Evaluate the outcomes and effectiveness of nursing care for the client with GAD by using outcome criteria, such as:
- Reduced frequency, intensity, and duration of worry and anxiety symptoms
- Improved coping skills and resources
- Enhanced physical and mental health and well-being
- Increased social and occupational functioning and quality of life
- Absence of complications or adverse effects
- Document the nursing care process, including assessment, diagnosis, interventions, outcomes, and evaluation. This helps to provide evidence-based and quality care, communicate with other healthcare professionals, and facilitate continuity of care.
Conclusion
- Generalized anxiety disorder (GAD) is a common and chronic mental disorder that causes excessive and uncontrollable worry about various aspects of life.
- GAD can affect anyone, but it is more prevalent in women and people with a family history of anxiety disorders or other mental illnesses.
- GAD can cause various physical and psychological symptoms that interfere with daily functioning and quality of life, such as restlessness, fatigue, irritability, muscle tension, sleep disturbance, difficulty concentrating, nervousness, palpitations, shortness of breath, sweating, nausea, or dizziness.
- GAD can also lead to serious complications if left untreated, such as depression, suicide, substance abuse, cardiovascular disease, hypertension, diabetes, or obesity.
- The nursing care for a client with GAD involves assessing the client’s history, physical examination, mental status examination, screening tools, laboratory tests, and diagnostic criteria; formulating nursing diagnoses based on the assessment data; implementing nursing interventions based on the client’s needs and preferences; and evaluating the outcomes and effectiveness of nursing care using outcome criteria.
- The nursing interventions for a client with GAD include establishing a therapeutic relationship; providing education and information; encouraging cognitive-behavioral therapy; encouraging relaxation techniques; encouraging physical activity; encouraging a healthy lifestyle; encouraging positive coping strategies; encouraging social support; administering anti-anxiety medications; monitoring for adverse effects; and documenting the nursing care process.
- The goal of nursing care for a client with GAD is to reduce anxiety and worry, enhance coping skills and resources, promote physical and mental health, and prevent complications.
Panic Disorder
- Panic disorder is a type of anxiety disorder characterized by recurrent, unexpected panic attacks that cause intense fear and discomfort, and are accompanied by physical and cognitive symptoms.
- A panic attack is a sudden surge of overwhelming anxiety that reaches a peak within minutes and can last from a few minutes to an hour.
- To be diagnosed with panic disorder, a person must have at least one of the following criteria:
- Persistent concern or worry about having more panic attacks or their consequences
- Significant maladaptive change in behavior related to the attacks, such as avoiding situations that might trigger them
- The disturbance is not attributable to the physiological effects of a substance or another medical condition
- The disturbance is not better explained by another mental disorder
Risk Factors and Causes:
- The exact cause of panic disorder is unknown, but it is likely influenced by a combination of biological, psychological, and environmental factors.
- Some of the possible risk factors and causes of panic disorder are:
- Genetic predisposition: Panic disorder tends to run in families and may have a hereditary component
- Neurobiological factors: Panic disorder may be associated with abnormalities in the brain structures and neurotransmitters that regulate fear and anxiety
- Cognitive factors: Panic disorder may be related to distorted thinking patterns that exaggerate perceived threats and negative outcomes
- Behavioral factors: Panic disorder may be influenced by learned responses to stressful situations or cues that trigger fear
- Life events: Panic disorder may be triggered or worsened by traumatic or stressful life events, such as abuse, loss, illness, or major changes
Clinical Manifestations and Complications
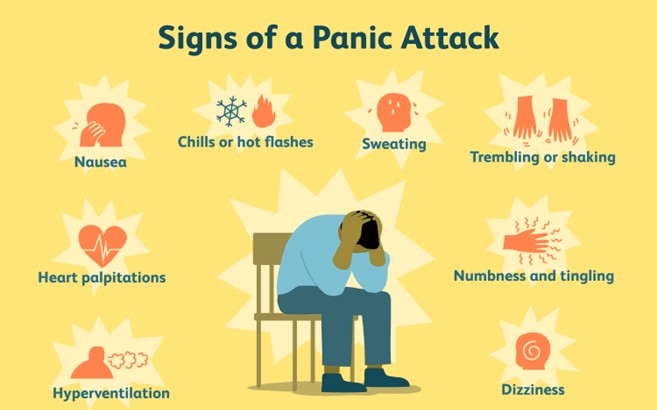
- The main clinical manifestation of panic disorder is the occurrence of recurrent, unexpected panic attacks that cause significant distress and impairment in daily functioning.
- The frequency and severity of panic attacks can vary from person to person, and some people may experience anticipatory anxiety or agoraphobia between attacks.
- Anticipatory anxiety is the fear of having another panic attack or its consequences.
- Agoraphobia is the fear of being in situations or places where escape might be difficult or help might not be available in case of a panic attack. People with agoraphobia may avoid public places, crowds, traveling, or being alone.
- Some of the possible complications of panic disorder are:
- Depression: Panic disorder can increase the risk of developing depression or suicidal thoughts or behaviors
- Substance abuse: Panic disorder can increase the likelihood of using alcohol or drugs to cope with anxiety or reduce symptoms
- Physical health problems: Panic disorder can affect the cardiovascular, respiratory, gastrointestinal, and musculoskeletal systems due to chronic stress and activation of the sympathetic nervous system
- Social isolation: Panic disorder can interfere with social relationships, work performance, education, and quality of life due to avoidance behavior and stigma
Nursing Assessment and Diagnosis:
- The nursing assessment for panic disorder involves collecting data from various sources, such as the client’s history, physical examination, mental status examination, laboratory tests, and diagnostic tools.
- Some of the data that should be obtained during the nursing assessment are:
- The onset, frequency, duration, severity, triggers, and symptoms of panic attacks
- The client’s coping strategies, support system, self-esteem, and self-efficacy
- The client’s medical history, medication use, substance use, family history, and personal history
- The client’s vital signs, weight, height, body mass index (BMI), cardiac rhythm (ECG), blood pressure (BP), pulse oximetry (SpO2), respiratory rate (RR), temperature (T), pain level (PL), and other physical findings
- The client’s mental status examination (MSE), which includes appearance, behavior, mood, affect, speech, thought process, thought content, perception, cognition, insight, and judgment
- The client’s laboratory tests, such as complete blood count (CBC), blood glucose, electrolytes, thyroid function tests (TFT), liver function tests (LFT), renal function tests (RFT), urine drug screen (UDS), and toxicology screen (TS)
- The client’s diagnostic tools, such as the Panic Disorder Severity Scale (PDSS), which is a 7-item questionnaire that measures the severity of panic disorder symptoms in the past week
- The nursing diagnosis for panic disorder is based on the analysis of the data collected during the nursing assessment.
- Some of the possible nursing diagnoses for panic disorder are:
- Anxiety related to perceived threats or loss of control
- Ineffective coping related to maladaptive responses to stress or anxiety
- Social isolation related to fear of embarrassment or rejection
- Impaired social interaction related to avoidance behavior or low self-esteem
- Risk for self-directed violence related to hopelessness or depression
- Knowledge deficit related to panic disorder and its treatment
Nursing Interventions and Evaluation
- The nursing interventions for panic disorder are aimed at reducing anxiety, promoting coping skills, enhancing social support, increasing self-esteem, preventing complications, and facilitating treatment adherence.
- Some of the nursing interventions for panic disorder are:
- Provide a safe and calm environment for the client and stay with them during a panic attack
- Use therapeutic communication skills, such as active listening, empathy, reflection, and validation, to establish rapport and trust with the client
- Assess the client’s level of anxiety and use appropriate interventions, such as deep breathing, relaxation techniques, distraction, or positive self-talk, to help them cope
- Educate the client about panic disorder and its treatment options, including the benefits, risks, side effects, and interactions of medications
- Encourage the client to participate in cognitive-behavioral therapy (CBT), which is a type of psychotherapy that helps the client identify and challenge negative thoughts and beliefs that contribute to anxiety
- Assist the client in developing a plan for managing panic attacks, such as identifying triggers, using coping strategies, seeking help when needed, and rewarding themselves for their efforts
- Support the client in gradually exposing themselves to feared situations or places with the guidance of a therapist or a trusted person
- Refer the client to self-help groups or community resources that can provide peer support and education
- Collaborate with other health care professionals, such as psychiatrists, pharmacists, social workers, or counselors, to provide holistic care for the client
- The evaluation for panic disorder is based on the outcomes that are established during the planning phase of the nursing process.
- Some of the outcomes that can be used to evaluate panic disorder are:
- The client reports a decrease in the frequency and severity of panic attacks
- The client demonstrates effective coping skills and positive self-talk during stressful situations
- The client engages in social activities and maintains supportive relationships
- The client expresses satisfaction with their self-image and achievements
- The client adheres to the prescribed treatment regimen and follows up with appointments
- The client has no signs of depression, substance abuse, or suicidal ideation
Pharmacological and Non-Pharmacological Treatments:
- The pharmacological treatment for panic disorder involves the use of medications that can reduce anxiety and prevent panic attacks.
- Some of the medications that can be used for panic disorder are:
- Selective serotonin reuptake inhibitors (SSRIs), such as fluoxetine, sertraline, paroxetine, or escitalopram, which are antidepressants that increase serotonin levels in the brain and improve mood and anxiety
- Serotonin-norepinephrine reuptake inhibitors (SNRIs), such as venlafaxine or duloxetine, which are antidepressants that increase serotonin and norepinephrine levels in the brain and enhance mood and anxiety
- Benzodiazepines, such as alprazolam, lorazepam, clonazepam, or diazepam, which are sedatives that enhance the effects of gamma-aminobutyric acid (GABA) in the brain and induce relaxation and calmness
- Beta-blockers, such as propranolol, atenolol, or metoprolol, which are antihypertensives that block the effects of adrenaline in the body and reduce heart rate, blood pressure, and physical symptoms of panic attacks, such as palpitations, chest pain, or dyspnea
- Anticonvulsants, such as gabapentin or pregabalin, which are antiepileptics that modulate calcium channels in the brain and reduce anxiety and neuropathic pain
- Tricyclic antidepressants (TCAs), such as imipramine or clomipramine, are antidepressants that inhibit the reuptake of serotonin and norepinephrine in the brain and improve mood and anxiety
- The non-pharmacological treatment for panic disorder involves the use of psychotherapy, lifestyle modifications, and complementary therapies that can help the client cope with anxiety and prevent panic attacks.
- Some of the non-pharmacological treatments for panic disorder are :
- Cognitive-behavioral therapy (CBT), which is a type of psychotherapy that helps the client identify and challenge negative thoughts and beliefs that contribute to anxiety and panic attacks, and replace them with more realistic and positive ones
- Exposure therapy, which is a type of psychotherapy that helps the client gradually confront their feared situations or places with the guidance of a therapist or a trusted person, and learn to tolerate anxiety and reduce avoidance behavior
- Relaxation techniques, such as deep breathing, progressive muscle relaxation, meditation, yoga, or biofeedback, which can help the client calm their mind and body and reduce stress and anxiety
- Lifestyle modifications, such as regular exercise, healthy diet, adequate sleep, smoking cessation, alcohol moderation, caffeine reduction, and stress management, which can improve the client’s physical and mental health and well-being
- Complementary therapies, such as acupuncture, aromatherapy, massage therapy, herbal remedies, or supplements, which can provide additional benefits for the client’s anxiety and mood
Conclusion
- Panic disorder is a type of anxiety disorder characterized by recurrent, unexpected panic attacks that cause intense fear and discomfort, and are accompanied by physical and cognitive symptoms
- Panic disorder can be influenced by a combination of biological, psychological, and environmental factors, and can lead to various complications, such as depression, substance abuse, physical health problems, or social isolation
- Panic disorder can be diagnosed by using the DSM-5 criteria, the PDSS, or other tools, and can be treated by using pharmacological and non-pharmacological interventions
- The nursing care for panic disorder involves assessing, diagnosing, intervening, and evaluating the client’s anxiety, coping skills, social support, self-esteem, complications, and treatment adherence
Phobias
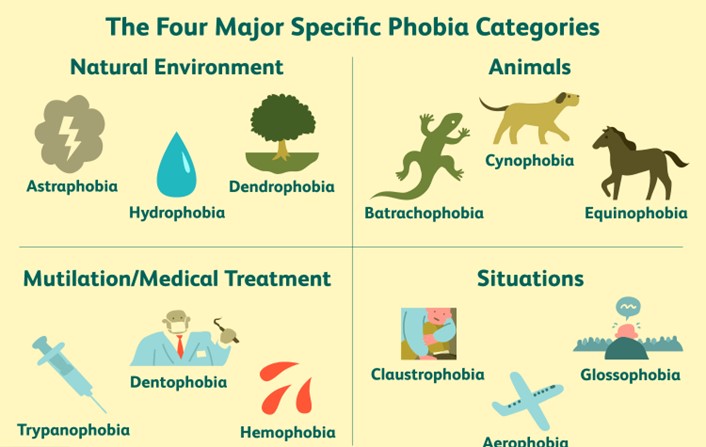
- Phobias are a type of anxiety disorder characterized by a persistent and irrational fear of a specific object, situation, or activity that poses little or no actual danger.
- Phobias can interfere with daily functioning, social relationships, and quality of life.
- Phobias can be classified into three main categories: specific phobias, social phobia, and agoraphobia.
Specific Phobias:
- Specific phobias are fears of a particular stimulus that trigger an excessive and unreasonable response.
- Specific phobias can be further divided into five subtypes: animal, natural environment, blood-injection-injury, situational, and other.
- Examples of specific phobias include fear of spiders (arachnophobia), fear of heights (acrophobia), fear of needles (trypanophobia), fear of flying (aerophobia), and fear of clowns (coulrophobia).
Agoraphobia:
- Agoraphobia is a fear of being in places or situations from which escape might be difficult or embarrassing, or where help might not be available in the event of a panic attack or other incapacitating symptoms.
- Agoraphobia can cause avoidance of a wide range of situations, such as crowds, public transportation, open spaces, enclosed spaces, or being alone outside the home.
- Agoraphobia can occur with or without a history of panic disorder.
Pathophysiology and Etiology:
- The exact pathophysiology and etiology of phobias are not fully understood, but several factors may contribute to their development and maintenance.
- Biological factors may include genetic predisposition, neurochemical imbalances, brain structure and function abnormalities, and autonomic nervous system hyperactivity.
- Psychological factors may include cognitive distortions, negative self-beliefs, learned associations, traumatic experiences, and modeling or vicarious learning.
- Environmental factors may include stressful life events, cultural influences, family dynamics, and peer pressure.
Clinical Manifestations and Diagnostic Criteria
- The clinical manifestations of phobias vary depending on the type and severity of the phobia, but they generally include both psychological and physiological symptoms.
- Psychological symptoms may include intense fear, anxiety, panic, dread, nervousness, embarrassment, shame, guilt, avoidance behavior, anticipatory anxiety, impaired concentration, and impaired functioning.
- Physiological symptoms may include palpitations, sweating, trembling, shortness of breath, chest pain, nausea, dizziness, fainting, chills or hot flashes, numbness or tingling sensations, and derealization or depersonalization.
- The diagnostic criteria for phobias are based on the Diagnostic and Statistical Manual of Mental Disorders (DSM-V), which requires the following features for each type of phobia:
Social Phobia:
- Social phobia, also known as social anxiety disorder, is a fear of being judged, criticized, or embarrassed in social or performance situations.
- Social phobia can cause significant distress and impairment in social, occupational, or academic functioning.
- Examples of social phobia include fear of public speaking (glossophobia), fear of eating in public (sitophobia), fear of meeting new people (anthropophobia), and fear of using public restrooms (paruresis).
Nursing Assessment and Diagnosis:
- The nursing assessment of phobias involves collecting subjective and objective data from the client and other sources, such as family members, friends, or healthcare providers.
- Subjective data may include the client’s history of phobias, triggers, symptoms, coping strategies, impact on functioning, and treatment preferences.
- Objective data may include the client’s appearance, behavior, mood, affect, speech, thought process, insight, judgment, and vital signs.
- The nursing diagnosis of phobias is based on the analysis and interpretation of the data collected during the assessment. Some examples of nursing diagnoses for phobias are:
- Anxiety related to an irrational fear of a specific object or situation
- Fear related to the perceived threat of social evaluation or humiliation
- Ineffective coping related to maladaptive avoidance behavior
- Impaired social interaction related to excessive self-consciousness or isolation
- Powerlessness related to perceived loss of control over phobic response
Nursing Interventions and Evaluation
- The nursing interventions for phobias are aimed at reducing the client’s fear and anxiety, enhancing the client’s coping skills, improving the client’s social functioning, and promoting the client’s self-efficacy and well-being.
- Some examples of nursing interventions for phobias are:
- Establishing a therapeutic relationship with the client based on trust, empathy, respect, and acceptance
- Providing a safe and supportive environment for the client
- Educating the client about phobias and their treatment options
- Encouraging the client to express feelings and concerns about phobias and their impact on life
- Assisting the client to identify and challenge irrational thoughts and beliefs that contribute to phobias
- Collaborating with the client to set realistic and achievable goals for overcoming phobias
- Implementing exposure therapy with the client, which involves gradual and repeated exposure to the feared object or situation in a controlled manner until the fear diminishes
- Implementing cognitive-behavioral therapy with the client, which involves teaching the client cognitive and behavioral techniques to cope with phobias, such as relaxation training, breathing exercises, positive self-talk, assertiveness training, and problem-solving skills
- Implementing group therapy with the client, which involves providing the client with opportunities to interact with others who have similar phobias and share experiences, feedback, and support
- Referring the client to other health care professionals as needed, such as psychiatrists, psychologists, social workers, or counselors
- The nursing evaluation of phobias involves measuring the outcomes of the nursing interventions and determining whether the goals have been met. Some examples of outcomes for phobias are:
- The client reports decreased fear and anxiety related to phobias
- The client demonstrates increased confidence and self-esteem related to phobias
- The client engages in exposure therapy without excessive distress or avoidance
- The client applies cognitive-behavioral techniques effectively to cope with phobias
- The client participates in social activities without excessive fear or embarrassment
Pharmacological and Non-pharmacological Management
- The pharmacological management of phobias involves prescribing medications that can help reduce the symptoms of fear and anxiety associated with phobias. Some examples of medications for phobias are:
- Antidepressants: These medications can help regulate mood and anxiety by affecting neurotransmitters such as serotonin, norepinephrine, and dopamine. Examples include selective serotonin reuptake inhibitors (SSRIs) such as fluoxetine (Prozac), sertraline (Zoloft), and paroxetine (Paxil); serotonin-norepinephrine reuptake inhibitors (SNRIs) such as venlafaxine (Effexor) and duloxetine (Cymbalta); and tricyclic antidepressants (TCAs) such as imipramine (Tofranil) and clomipramine (Anafranil).
- Benzodiazepines: These medications can help reduce acute anxiety and panic by enhancing the effects of gamma-aminobutyric acid (GABA), a neurotransmitter that inhibits brain activity. Examples include alprazolam (Xanax), diazepam (Valium), lorazepam (Ativan), and clonazepam (Klonopin).
- Beta-blockers: These medications can help reduce the physical symptoms of anxiety, such as palpitations, sweating, and trembling, by blocking the effects of adrenaline on the heart and blood vessels. Examples include propranolol (Inderal), atenolol (Tenormin), and metoprolol (Lopressor).
- The non-pharmacological management of phobias involves using psychological therapies that can help the client cope with and overcome their fears. Some examples of psychological therapies for phobias are:
- Psychoeducation: This therapy involves providing the client with information about phobias, their causes, their effects, and their treatment options. Psychoeducation can help the client understand their condition, reduce stigma, increase motivation, and enhance adherence to treatment.
- Cognitive therapy: This therapy involves helping the client identify and challenge irrational thoughts and beliefs that contribute to their phobias. Cognitive therapy can help the client replace negative thoughts with more realistic and positive ones, reduce cognitive distortions, and increase self-confidence.
- Behavioral therapy: This therapy involves helping the client modify their behavior in response to their phobias. Behavioral therapy can help the client learn new skills, practice exposure techniques, reinforce positive behaviors, and extinguish negative ones.
- Relaxation therapy: This therapy involves teaching the client various methods to relax their mind and body in the face of their phobias. Relaxation therapy can help the client reduce stress, tension, anxiety, and physiological arousal. Some examples of relaxation methods are deep breathing, progressive muscle relaxation, guided imagery, meditation, yoga, and biofeedback.
Conclusion
- Phobias are a type of anxiety disorder characterized by a persistent and irrational fear of a specific object, situation, or activity that poses little or no actual danger.
- Phobias can be classified into three main categories: specific phobias, social phobia, and agoraphobia.
- Phobias can be caused by a combination of biological, psychological, and environmental factors.
- Phobias can be diagnosed based on the DSM-V criteria for each type of phobia.
- Phobias can be treated with a combination of pharmacological and non-pharmacological interventions.
- Phobias can be managed with the help of nursing care that involves assessment, diagnosis, intervention, and evaluation.
Post-traumatic stress disorder (PTSD)
- Post-traumatic stress disorder (PTSD) is a psychiatric disorder that occurs in some people who have experienced or witnessed a traumatic event, such as war, violence, abuse, accident, disaster, or death of a loved one.
- PTSD is characterized by four types of symptoms: re-experiencing, avoidance, negative alterations in cognition and mood, and alterations in arousal and reactivity.
- Re-experiencing symptoms include intrusive and distressing memories, nightmares, flashbacks, or emotional and physical reactions to reminders of the trauma.
- Avoidance symptoms include avoiding thoughts, feelings, people, places, or activities that are associated with the trauma.
- Negative alterations in cognition and mood include persistent negative beliefs and emotions, diminished interest or participation in activities, detachment or estrangement from others, or inability to experience positive emotions.
- Alterations in arousal and reactivity include hypervigilance, exaggerated startle response, irritability, anger, aggression, difficulty concentrating or sleeping, or reckless or self-destructive behavior.
- To be diagnosed with PTSD, a person must have experienced or witnessed a traumatic event that involved actual or threatened death, serious injury, or sexual violence; have at least one re-experiencing symptom, one avoidance symptom, two negative alterations in cognition and mood symptoms, and two alterations in arousal and reactivity symptoms; have symptoms that last for more than one month; and have symptoms that cause significant distress or impairment in social, occupational, or other areas of functioning.
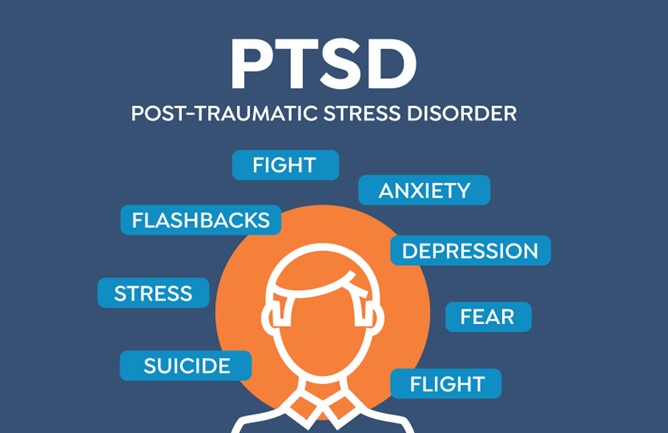
Risk Factors and Causes:
- The development of PTSD depends on various factors, such as the type, severity, duration, and proximity of the trauma; the individual’s biological, psychological, and social characteristics; and the availability of social support and coping resources.
- Some of the risk factors for PTSD include: being female; having a history of mental illness; having a family history of PTSD; having a history of childhood abuse or neglect; having a history of substance abuse; having poor social support; having exposure to multiple traumas; having exposure to interpersonal violence; having exposure to intentional harm; having exposure to human suffering or death; having exposure to perceived life threat; having exposure to perceived loss of control; having exposure to betrayal or injustice; having exposure to media coverage of trauma.
- The causes of PTSD are not fully understood, but some of the possible mechanisms include abnormal activation of the amygdala (the brain region involved in fear and emotion); impaired functioning of the hippocampus (the brain region involved in memory and learning); altered levels of neurotransmitters (such as serotonin, norepinephrine, dopamine) and hormones (such as cortisol); genetic variations that affect the response to stress; epigenetic changes that affect gene expression; environmental factors that influence gene-environment interactions.
Clinical Manifestations and Complications:
- The clinical manifestations of PTSD vary depending on the individual’s age, developmental stage, personality, culture, and coping style. Some of the common signs and symptoms include:
- Re-experiencing symptoms: recurrent and intrusive memories of the trauma; recurrent distressing dreams related to the trauma; dissociative reactions (such as flashbacks) that make the person feel or act as if the trauma is happening again; intense or prolonged psychological distress or physiological reactions to internal or external cues that resemble or symbolize an aspect of the trauma.
- Avoidance symptoms: efforts to avoid distressing memories, thoughts, or feelings about or closely associated with the trauma; efforts to avoid external reminders (such as people, places, conversations, activities) that arouse distressing memories, thoughts, or feelings about or closely associated with the trauma.
- Negative alterations in cognition and mood symptoms: inability to remember an important aspect of the trauma (due to dissociative amnesia); persistent and exaggerated negative beliefs or expectations about oneself, others, or the world (such as “I am bad,” “No one can be trusted,” “The world is completely dangerous”); persistent distorted cognitions about the cause or consequences of the trauma that lead to self-blame or blame of others; persistent negative emotional state (such as fear, anger, guilt, shame); markedly diminished interest or participation in significant activities; feelings of detachment or estrangement from others; persistent inability to experience positive emotions (such as happiness, satisfaction, love).
- Alterations in arousal and reactivity symptoms: irritable behavior and angry outbursts (with little or no provocation) typically expressed as verbal or physical aggression toward people or objects; reckless or self-destructive behavior (such as substance abuse, driving too fast, engaging in unsafe sex); hypervigilance (being constantly on guard or alert for potential threats); exaggerated startle response (being easily startled by sudden noises or movements); problems with concentration (having difficulty focusing or paying attention); sleep disturbance (having difficulty falling or staying asleep, having nightmares).
- The complications of PTSD include impaired social, occupational, and interpersonal functioning; increased risk of physical and mental health problems (such as cardiovascular disease, chronic pain, depression, anxiety, substance abuse, and suicide); increased risk of re-traumatization and revictimization; increased risk of violence and aggression; decreased quality of life and well-being.
Nursing Assessment and Interventions
- The nursing assessment for PTSD includes: obtaining a comprehensive history of the trauma and its impact on the client’s life; screening for PTSD symptoms using standardized tools (such as the PTSD Checklist for DSM-5 or the Primary Care PTSD Screen for DSM-5); assessing for co-occurring conditions (such as depression, anxiety, substance abuse, suicidal ideation); evaluating the client’s coping skills, social support, and resources; performing a physical examination to identify any signs of injury, illness, or neglect.
- The nursing interventions for PTSD include: establishing a therapeutic relationship with the client based on trust, empathy, respect, and safety; providing psychoeducation about PTSD and its treatment options; promoting self-care and healthy lifestyle habits (such as nutrition, exercise, sleep hygiene); encouraging the client to express and process emotions related to the trauma; teaching the client relaxation techniques (such as deep breathing, progressive muscle relaxation, guided imagery) to reduce stress and anxiety; assisting the client to identify and challenge negative or distorted thoughts and beliefs; helping the client to develop and implement coping strategies (such as problem-solving, assertiveness, distraction) to manage triggers and symptoms; facilitating exposure therapy (such as prolonged exposure or eye movement desensitization and reprocessing) to help the client confront and desensitize to traumatic memories and stimuli; providing cognitive-behavioral therapy (CBT) to help the client modify maladaptive thoughts and behaviors; supporting the client to participate in group therapy or support groups to share experiences and receive feedback from others with similar problems; referring the client to other health care professionals or community resources as needed (such as psychiatrists, psychologists, social workers, counselors, peer specialists).
Pharmacological and Non-pharmacological Treatments:
- The pharmacological treatments for PTSD include selective serotonin reuptake inhibitors (SSRIs) such as sertraline or paroxetine; serotonin-norepinephrine reuptake inhibitors (SNRIs) such as venlafaxine or duloxetine; tricyclic antidepressants (TCAs) such as amitriptyline or imipramine; monoamine oxidase inhibitors (MAOIs) such as phenelzine or tranylcypromine; atypical antipsychotics such as risperidone or quetiapine; antiadrenergic agents such as prazosin or clonidine; mood stabilizers such as lamotrigine or valproate; benzodiazepines such as alprazolam or lorazepam.
- The non-pharmacological treatments for PTSD include psychotherapy modalities such as CBT, exposure therapy, EMDR, acceptance and commitment therapy, dialectical behavior therapy, interpersonal therapy, psychodynamic therapy, family therapy, or couples therapy; complementary and alternative therapies such as acupuncture, yoga, meditation, hypnosis, biofeedback, art therapy, music therapy, animal-assisted therapy, or virtual reality therapy.
Outcomes and Effectiveness:
- The outcomes of PTSD management include reduction or remission of PTSD symptoms; improvement in functioning and quality of life; enhancement of coping skills and resilience; restoration of self-esteem and identity; resolution of grief and loss; reintegration into society and relationships; prevention of relapse and chronicity.
- The effectiveness of PTSD management depends on various factors, such as the type, severity, duration, and frequency of the trauma; the individual’s characteristics, preferences, and readiness for change; the availability and accessibility of treatment options; the quality and consistency of treatment delivery; the adherence and compliance of the client; and the monitoring and evaluation of treatment outcomes.
- The evidence for the effectiveness of PTSD management is based on various sources, such as randomized controlled trials, meta-analyses, systematic reviews, clinical guidelines, expert opinions, and client feedback.
- According to the American Psychiatric Association (APA), the most effective treatments for PTSD are trauma-focused psychotherapies, such as prolonged exposure (PE), cognitive processing therapy (CPT), and eye movement desensitization and reprocessing (EMDR). These therapies have been shown to reduce PTSD symptoms by 50% to 80% in most clients after 8 to 16 sessions.
- According to the National Institute for Health and Care Excellence (NICE), the first-line pharmacological treatments for PTSD are SSRIs or SNRIs, such as sertraline, paroxetine, venlafaxine, or mirtazapine. These medications have been shown to reduce PTSD symptoms by 30% to 50% in most clients after 8 to 12 weeks.
- According to the Cochrane Database of Systematic Reviews, some of the complementary and alternative therapies that have some evidence of effectiveness for PTSD are acupuncture, yoga, meditation, hypnosis, biofeedback, and virtual reality therapy. However, these therapies have not been studied as extensively as psychotherapy or pharmacotherapy, and their effects are often small or moderate.
Conclusion
- PTSD is a complex and debilitating disorder that affects millions of people worldwide who have experienced or witnessed a traumatic event.
- PTSD can cause various symptoms that interfere with the person’s functioning and well-being, such as re-experiencing, avoidance, negative alterations in cognition and mood, and alterations in arousal and reactivity.
- PTSD can also increase the risk of developing other physical and mental health problems, such as cardiovascular disease, chronic pain, depression, anxiety, substance abuse, suicide, violence, and aggression.
PTSD can be effectively managed with a combination of pharmacological and non-pharmacological treatments that are tailored to the individual’s needs and preferences.
- The most effective treatments for PTSD are trauma-focused psychotherapies that help the person confront and process their traumatic memories and stimuli.
- The first-line medications for PTSD are antidepressants that help regulate the person’s mood and anxiety.
- Some complementary and alternative therapies may also provide some benefits for PTSD, such as relaxation, distraction, or stimulation.
Pharmacological Management of Anxiety Disorders
- Anxiety disorders are the most common psychiatric disorders and include panic disorder, generalized anxiety disorder, social anxiety disorder, specific phobias, obsessive-compulsive disorder, and post-traumatic stress disorder.
- Anxiety disorders are characterized by excessive fear, nervousness, or worry that interferes with daily functioning and causes significant distress or impairment.
- The exact causes of anxiety disorders are not fully understood, but they may involve genetic, biological, psychological, and environmental factors.
- The goal of pharmacological treatment for anxiety disorders is to reduce the severity and frequency of anxiety symptoms, improve the quality of life, and prevent complications or comorbidities.
- The choice of medication depends on the type and severity of the anxiety disorder, the patient’s preference and response, the side effect profile, the potential for drug interactions, and the cost and availability of the medication.
Classes of Medications for Anxiety Disorders
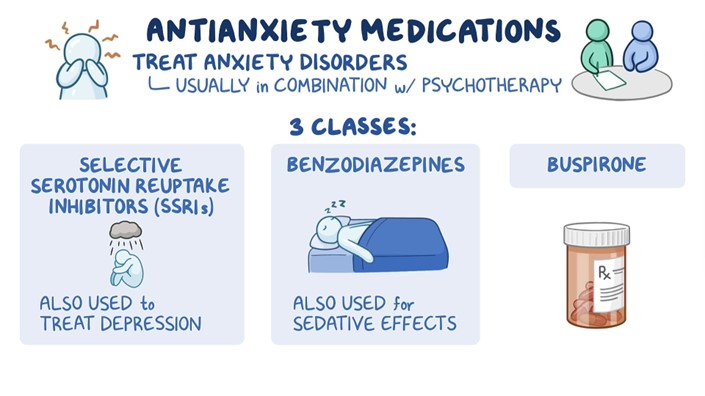
- The main classes of medications used to treat anxiety disorders are antidepressants, benzodiazepines, buspirone, beta-blockers, antihistamines, and anticonvulsants. Each class has its own advantages and disadvantages, and some may be more effective or appropriate for certain types of anxiety disorders than others.
- The following table summarizes the main features of each class of medication for anxiety disorders:
- I will continue the table for you with the information from the web search results. Here is the updated table:
|
Class |
Examples |
Mechanism of Action |
Indications |
Advantages |
Disadvantages |
|
Antidepressants |
Selective serotonin reuptake inhibitors (SSRIs): fluoxetine, sertraline, paroxetine, citalopram, escitalopram Serotonin-norepinephrine reuptake inhibitors (SNRIs): venlafaxine, duloxetine Tricyclic antidepressants (TCAs): imipramine, clomipramine Monoamine oxidase inhibitors (MAOIs): phenelzine, tranylcypromine |
Increase the availability of serotonin and/or norepinephrine in the brain by inhibiting their reuptake by presynaptic neurons. MAOIs also inhibit the enzyme that breaks down these neurotransmitters. |
All types of anxiety disorders, especially panic disorder, generalized anxiety disorder, social anxiety disorder, obsessive-compulsive disorder, and post-traumatic stress disorder. Often used as first-line agents. |
Effective for both anxiety and depression symptoms. Have a low potential for abuse or dependence. Have a long duration of action. |
May take several weeks to achieve full therapeutic effect. May cause initial worsening of anxiety symptoms. May cause sexual dysfunction, weight gain, nausea, insomnia, headache, dry mouth, and other side effects. May interact with other medications or foods containing tyramine (MAOIs). Require careful monitoring for suicidal ideation or behavior in children and adolescents. |
|
Benzodiazepines |
Diazepam, lorazepam, alprazolam, clonazepam |
Enhance the activity of gamma-aminobutyric acid (GABA), an inhibitory neurotransmitter in the brain that reduces neuronal excitability and induces relaxation. |
All types of anxiety disorders, especially panic disorder and generalized anxiety disorder. Often used as second-line agents or as adjuncts to antidepressants. Also used for acute management of severe anxiety or agitation. |
Rapid onset of action. Effective for reducing acute anxiety symptoms. Have sedative-hypnotic, anticonvulsant, and muscle relaxant properties. |
May cause drowsiness, dizziness, confusion, impaired memory and coordination, dependence, tolerance, withdrawal symptoms, rebound anxiety, and respiratory depression. May interact with alcohol and other CNS depressants. May worsen depression or increase suicidal risk in some patients. |
|
Buspirone |
Buspirone |
Partially agonizes serotonin 5-HT1A receptors and antagonizes dopamine D2 receptors in the brain. Modulates neuronal activity in the limbic system and prefrontal cortex. |
Generalized anxiety disorder and social anxiety disorder. May also be used as an adjunct to antidepressants for other types of anxiety disorders. |
Does not cause sedation, cognitive impairment, dependence, tolerance, or withdrawal symptoms. Has a low potential for abuse or interaction with other substances. Does not worsen depression or increase suicidal risk. |
May take several weeks to achieve full therapeutic effect. May cause nausea, headache, dizziness, restlessness, nervousness, and insomnia. May interact with grapefruit juice or other medications that affect liver enzymes (CYP3A4). |
|
Beta-blockers |
Propranolol, atenolol |
Block beta-adrenergic receptors in the heart and blood vessels and reduce the effects of adrenaline and noradrenaline on the cardiovascular system. Decrease heart rate, blood pressure, cardiac output, and oxygen consumption. |
Social anxiety disorder and specific phobias (especially performance-related). May also be used as an adjunct to antidepressants for other types of anxiety disorders or for physical symptoms of anxiety (such as palpitations or tremors). |
Rapid onset of action. Effective for reducing somatic symptoms of anxiety (such as sweating or blushing). Have anti-arrhythmic and anti-anginal properties. |
May cause fatigue, drowsiness, insomnia, nightmares, depression, bradycardia, hypotension, bronchospasm, and sexual dysfunction. May interact with other medications that affect blood pressure or heart rate (such as calcium channel blockers or digoxin). May mask signs of hypoglycemia in diabetic patients. |
|
Antihistamines |
Hydroxyzine |
Block histamine H1 receptors in the brain and periphery and exert sedative-hypnotic effects. |
Generalized anxiety disorder and social anxiety disorder. May also be used as an adjunct to antidepressants for other types of anxiety disorders or for insomnia caused by anxiety or other medical conditions. |
Rapid onset of action. Effective for reducing mild to moderate anxiety symptoms. Have anti-nausea and anti-pruritic properties. Have a low potential for abuse or dependence. |
May cause drowsiness, dry mouth, blurred vision, constipation, urinary retention, and weight gain. May interact with alcohol and other CNS depressants. May worsen depression or increase suicidal risk in some patients. |
|
Anticonvulsants |
Pregabalin, gabapentin, carbamazepine, oxcarbazepine, lamotrigine, valproate |
Modulate the activity of various neurotransmitters and ion channels in the brain that are involved in neuronal excitability and synaptic transmission. May affect GABA, glutamate, calcium, or sodium. |
Generalized anxiety disorder and social anxiety disorder. May also be used as an adjunct to antidepressants for other types of anxiety disorders or for treatment-resistant anxiety. |
Effective for reducing both somatic and psychic symptoms of anxiety. Have antiepileptic and mood-stabilizing properties. Have a low potential for abuse or dependence. |
May take several weeks to achieve full therapeutic effect. May cause dizziness, drowsiness, weight gain, edema, rash, nausea, headache, and cognitive impairment. May interact with other medications that affect liver enzymes or blood levels (such as oral contraceptives or warfarin). May cause serious adverse effects such as Stevens-Johnson syndrome, agranulocytosis, hepatotoxicity, or pancreatitis. |
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Disorders of Anxiety
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


