Please set your exam date
Patient Assessment and Documentation
Study Questions
Introduction to Patient Assessment and Documentation
A nurse is assessing a client who has been admitted with chest pain.
Which of the following findings should the nurse report to the provider immediately?
Explanation
D) The client has an elevated troponin level in the blood.
Rationale: An elevated troponin level indicates myocardial damage and is a diagnostic marker for acute coronary syndrome (ACS), which includes unstable angina and myocardial infarction (MI). This is a life-threatening condition that requires immediate intervention.
A) The client has a history of hypertension and diabetes. - This is an important finding, as hypertension and diabetes are risk factors for cardiovascular disease, but it is not an urgent finding that requires immediate reporting.
B) The client rates the pain as 8 on a scale of 0 to 10. - This is a significant finding, as chest pain is a cardinal symptom of ACS, but it is not a definitive finding that confirms the diagnosis.
C) The client has crackles in the lower lobes of both lungs. - This is an abnormal finding, as crackles indicate fluid accumulation in the alveoli, which may be caused by heart failure, pneumonia, or pulmonary edema. However, it is not a specific finding for ACS and may be related to other conditions.
A nurse is documenting the findings of a head-to-toe assessment on a newly admitted client.
Which of the following information should the nurse include in the documentation?
Explanation
Rationale: The nurse should document all relevant and objective data obtained from the assessment, including vital signs, skin condition, bowel sounds, and any other findings that reflect the client's health status.
Incorrect options:
A) The client's vital signs are within normal limits. - This is a correct statement, but it is not the only information that should be documented.
B) The client's skin is warm, dry, and intact. - This is a correct statement, but it is not the only information that should be documented.
C) The client's bowel sounds are present in all four quadrants. - This is a correct statement, but it is not the only information that should be documented.
A nurse is performing a physical assessment on a client who has abdominal pain.
Which of the following techniques should the nurse use to assess the abdomen?
Explanation
Inspection, auscultation, percussion, palpation
Rationale: The correct order of techniques for abdominal assessment is inspection, auscultation, percussion, and palpation. This order prevents altering bowel sounds by manipulating the abdomen before listening to them.
Incorrect options:
A) Inspection, palpation, percussion, auscultation - This order may alter bowel sounds by palpating and percussing before auscultating them.
C) Auscultation, inspection, palpation, percussion - This order may miss visual cues by inspecting after auscultating.
D) Palpation, auscultation, inspection, percussion - This order may alter bowel sounds and miss visual cues by palpating before auscultating and inspecting.
A nurse is reviewing the medical record of a client who has been diagnosed with pneumonia.
Which of the following data should the nurse use to evaluate the effectiveness of the treatment plan?
Explanation
The client's chest x-ray shows clear lung fields.
Rationale: A chest x-ray is a diagnostic test that can confirm the presence or absence of pneumonia by showing areas of consolidation or infiltration in the lung tissue. A clear chest x-ray indicates resolution of pneumonia and effectiveness of treatment.
Incorrect options:
A) The client's temperature is 37.2°C (99°F). - This is a normal finding, but it does not rule out pneumonia as some clients may have low-grade fever or no fever at all with pneumonia.
B) The client's white blood cell count is 12.5 x 10^9/L. - This is an elevated finding, as the normal range for white blood cell count is 4.5 to 11 x 10^9/L. An elevated white blood cell count indicates inflammation or infection and does not reflect the effectiveness of treatment.
C) The client's oxygen saturation is 95% on room air. - This is a normal finding, as the normal range for oxygen saturation is 95% to 100%. However, it does not indicate the severity or resolution of pneumonia, as some clients may have normal oxygen saturation despite having pneumonia.
A nurse is preparing to perform a neurological assessment on a client who has a head injury.
Which of the following tools should the nurse use to assess the client's level of consciousness?
Explanation
The Glasgow Coma Scale (GCS) is a tool that measures the level of consciousness based on three parameters: eye opening, verbal response, and motor response. The GCS score ranges from 3 to 15, with lower scores indicating lower levels of consciousness.
Incorrect options:
B) Mini-Mental State Examination (MMSE) - This is a tool that measures cognitive function, such as orientation, memory, attention, and language. It is not used to assess level of consciousness.
C) Confusion Assessment Method (CAM) - This is a tool that screens for delirium, which is an acute and fluctuating disturbance of cognition and attention. It is not used to assess level of consciousness.
D) Morse Fall Scale (MFS) - This is a tool that assesses the risk of falling in hospitalized clients based on six factors: history of falling, secondary diagnosis, ambulatory aid, intravenous therapy, gait, and mental status. It is not used to assess level of consciousness.
A nurse is conducting a health history interview with a client who has a chronic cough.
Which of the following questions should the nurse ask to elicit relevant information about the cough?
Explanation
The nurse should ask open-ended questions that cover the characteristics, duration, frequency, severity, precipitating and relieving factors, associated symptoms, and impact of the cough on the client's health and quality of life.
Incorrect options:
A) "How long have you had this cough?" - This is a correct question, but it is not the only question that should be asked.
B) "What do you think is causing your cough?" - This is a correct question, but it is not the only question that should be asked.
C) "How does your cough affect your daily activities?" - This is a correct question, but it is not the only question that should be asked.
The Assessment Patient Process
A nurse is assessing a client who is in the first stage of labor.
Which finding should the nurse report to the provider immediately?
Explanation
The client's fetal heart rate is 180 beats per minute.
Rationale: A fetal heart rate of 180 beats per minute is above the normal range of 110 to 160 beats per minute and indicates fetal distress. The nurse should report this finding to the provider immediately and prepare for interventions to improve fetal oxygenation, such as changing the client's position, administering oxygen, or initiating a fluid bolus.
Incorrect options:
A) The client's cervix is dilated to 4 cm. - This is a normal finding for the first stage of labor, which lasts until the cervix is fully dilated to 10 cm.
C) The client's contractions are 5 minutes apart. - This is a normal finding for the active phase of the first stage of labor, which occurs when the contractions are 3 to 5 minutes apart and last for 40 to 60 seconds.
D) The client's amniotic fluid is clear and odorless. - This is a normal finding that indicates the absence of infection or meconium staining in the amniotic fluid.
A nurse is caring for a client who has a chest tube connected to a water seal drainage system.
Which action should the nurse take to ensure proper functioning of the system?
Explanation
Keep the drainage system below the level of the client's chest.
Rationale: Keeping the drainage system below the level of the client's chest prevents backflow of fluid into the pleural space and maintains negative pressure in the system.
Incorrect options:
A) Clamp the chest tube periodically to check for air leaks. - This is an incorrect action, as clamping the chest tube can cause a tension pneumothorax or impair lung re-expansion. The nurse should only clamp the chest tube briefly when changing the drainage system or when ordered by the provider.
C) Empty the drainage chamber when it is half full. - This is an incorrect action, as emptying the drainage chamber can disrupt the water seal and allow air to enter the pleural space. The nurse should only empty the drainage chamber when it is full or when changing the system.
D) Add sterile water to the suction control chamber as needed. - This is an incorrect action, as adding sterile water to the suction control chamber can increase or decrease the amount of suction applied to the chest tube, depending on whether water is added or removed. The nurse should only add sterile water to the water seal chamber if it falls below the 2 cm mark.
A nurse is reviewing laboratory results for a client who has diabetic ketoacidosis (DKA).
Which finding should alert the nurse to a potential complication of DKA?
Explanation
Serum potassium level of 6.5 mEq/L
Rationale: A serum potassium level of 6.5 mEq/L indicates hyperkalemia, which is a potential complication of DKA due to insulin deficiency, acidosis, and dehydration. Hyperkalemia can cause cardiac dysrhythmias, muscle weakness, and paresthesia.
Incorrect options:
A) Blood glucose level of 350 mg/dL - This is an expected finding for a client who has DKA, as insulin deficiency leads to hyperglycemia and glycosuria. The goal of treatment for DKA is to lower blood glucose levels gradually to prevent cerebral edema.
C) Arterial blood pH of 7.25 - This is an expected finding for a client who has DKA, as insulin deficiency leads to increased breakdown of fatty acids and production of ketones, resulting in metabolic acidosis. The normal range for arterial blood pH is 7.35 to 7.45.
D) Serum bicarbonate level of 18 mEq/L - This is an expected finding for a client who has DKA, as metabolic acidosis causes a decrease in serum bicarbonate levels due to buffering mechanisms. The normal range for serum bicarbonate levels is 22 to 26 mEq/L.
A nurse is planning care for a client who has a new diagnosis of tuberculosis (TB).
Which intervention should the nurse include in the plan of care?
Explanation
Place the client in a negative pressure isolation room.
Rationale: Placing the client in a negative pressure isolation room is an intervention that prevents the transmission of TB to other clients and staff. Negative pressure rooms have ventilation systems that create a lower pressure inside the room than outside, causing air to flow into the room and preventing air from escaping.
Incorrect options:
B) Administer a single antitubercular medication daily. - This is an incorrect intervention, as TB requires combination therapy with multiple antitubercular medications to prevent drug resistance and ensure effective treatment. The standard regimen for TB consists of four drugs: isoniazid, rifampin, ethambutol, and pyrazinamide.
C) Obtain three consecutive sputum cultures for acid-fast bacilli (AFB). - This is an intervention that is done before the diagnosis of TB is confirmed, not after. Sputum cultures for AFB are used to identify the presence of Mycobacterium tuberculosis, the causative agent of TB. Three consecutive negative sputum cultures are required to declare the client noninfectious.
D) Instruct the client to wear a surgical mask when outside the room. - This is an incorrect intervention, as surgical masks do not provide adequate protection against TB. The client should wear a high-efficiency particulate air (HEPA) respirator when outside the room, which filters out 99.97% of airborne particles.
A nurse is evaluating a client who has chronic kidney disease (CKD) and is receiving hemodialysis.
Which finding indicates that the client's nutritional status is improving?
Explanation
The client's serum albumin level is 4.0 g/dL.
Rationale: A serum albumin level of 4.0 g/dL indicates that the client's nutritional status is improving, as albumin is a protein that reflects the client's protein intake and nutritional status. The normal range for serum albumin levels is 3.5 to 5.0 g/dL.
Incorrect options:
B) The client's blood urea nitrogen (BUN) level is 60 mg/dL. - This finding indicates that the client's nutritional status is worsening, as BUN is a waste product of protein metabolism that accumulates in the blood due to impaired renal function. A high BUN level can indicate excessive protein intake or inadequate dialysis. The normal range for BUN levels is 10 to 20 mg/dL.
C) The client's body weight is 2 kg higher than the dry weight. - This finding indicates that the client has fluid retention, not improved nutritional status. Dry weight is the weight of the client after dialysis, when all excess fluid has been removed. A weight gain of more than 1 kg above the dry weight can indicate inadequate fluid restriction or dialysis.
D) The client's serum creatinine level is 3.0 mg/dL. - This finding indicates that the client has impaired renal function, not improved nutritional status. Creatinine is a waste product of muscle metabolism that accumulates in the blood due to reduced glomerular filtration rate (GFR). A high creatinine level can indicate decreased muscle mass or inadequate dialysis. The normal range for serum creatinine levels is 0.6 to 1.2 mg/dL.
A nurse is teaching a client who has hypertension about lifestyle modifications to lower blood pressure.
Which statement by the client indicates an understanding of the teaching?
Explanation
"I will quit smoking as soon as possible."
Rationale: Quitting smoking is a lifestyle modification that can lower blood pressure, as smoking causes vasoconstriction and increases cardiac workload and oxygen demand.
Incorrect options:
A) "I will limit my sodium intake to 4 grams per day." - This statement indicates a need for further teaching, as limiting sodium intake to 4 grams per day is not sufficient for someone with hypertension. The recommended daily sodium intake for individuals with hypertension is generally lower, around 1,500-2,300 milligrams (mg).
B) "I will drink no more than two cups of coffee per day." - While limiting caffeine intake is generally recommended for individuals with hypertension, this statement does not address other lifestyle modifications specifically related to blood pressure.
C) "I will exercise for at least 30 minutes three times per week." - Regular exercise is beneficial for overall health, but the frequency and duration mentioned in this statement may not be sufficient for effectively lowering blood pressure. The American Heart Association recommends at least 150 minutes of moderate-intensity aerobic exercise or 75 minutes of vigorous-intensity exercise per week for individuals with hypertension.
Documentation and Reporting
A nurse is preparing to document a client's wound assessment in the electronic health record.
Which of the following actions should the nurse take?
Explanation
Include the date and time of the assessment.
Rationale: The nurse should include the date and time of the wound assessment in the documentation, as this provides a chronological and accurate record of the client's condition and response to treatment.
Incorrect options:
B) Use abbreviations that are approved by the facility. - This is a partially correct statement, as the nurse should use abbreviations that are approved by the facility to ensure clarity and consistency in the documentation. However, this is not the best answer, as some abbreviations may still be confusing or ambiguous, and should be avoided or spelled out.
C) Copy and paste the previous assessment as a template. - This is an incorrect statement, as copying and pasting the previous assessment as a template can result in errors, omissions, or duplication of information, compromising the quality and integrity of the documentation.
D) Delete any inaccurate entries made by other staff members. - This is an incorrect statement, as deleting any entries made by other staff members is unethical and illegal, as it alters the original record and may affect the client's care or legal outcomes. The nurse should follow the facility's policy on correcting errors in documentation, which usually involves drawing a single line through the error, writing "error" above it, and signing and dating it.
A client is admitted to the hospital with chest pain and shortness of breath. The nurse obtains a history and performs a physical examination.
Which of the following information should the nurse report to the provider immediately?
Explanation
The client's blood pressure is 180/100 mm Hg and heart rate is 110 beats/min.
Rationale: The nurse should report the client's blood pressure and heart rate to the provider immediately, as these are signs of hypertensive crisis and tachycardia, which can indicate a serious cardiovascular complication, such as myocardial infarction, stroke, or heart failure.
Incorrect options:
A) The client has a history of hypertension and diabetes mellitus. - This is an important information to obtain from the client, as it indicates risk factors for cardiovascular disease. However, this is not an urgent finding that requires immediate reporting to the provider, as it does not reflect the client's current condition or acuity.
B) The client takes aspirin 81 mg daily and metformin 500 mg twice daily. - This is an important information to obtain from the client, as it indicates the medications that the client is taking for their chronic conditions. However, this is not an urgent finding that requires immediate reporting to the provider, as it does not reflect any adverse effects or interactions of these medications.
D) The client's chest pain radiates to the left arm and is relieved by nitroglycerin. - This is an important information to obtain from the client, as it indicates that the client has angina pectoris, which is chest pain caused by reduced blood flow to the heart muscle. However, this is not an urgent finding that requires immediate reporting to the provider, as it shows that the chest pain is stable and responsive to nitroglycerin.
A nurse is reviewing a client's laboratory results before administering a blood transfusion.
Which of the following results should the nurse report to the provider before proceeding with the transfusion?
Explanation
Potassium 5.5 mEq/L
Rationale: The nurse should report the potassium level of 5.5 mEq/L to the provider before proceeding with
the blood transfusion, as this indicates hyperkalemia, which can cause cardiac arrhythmias or arrest. Blood transfusion can increase potassium levels further, especially if the blood has been stored for a long time or if it is administered rapidly.
Incorrect options:
A) Hemoglobin 8 g/dL - This is a low hemoglobin level, which indicates anemia, but it is not a contraindication for blood transfusion. In fact, blood transfusion may be indicated to treat severe anemia and improve oxygen delivery to the tissues.
B) Platelets 150,000/mm3 - This is a normal platelet count, which indicates adequate clotting function. It is not a reason to withhold or delay blood transfusion.
D) Blood type AB positive - This is the client's blood type, which is compatible with any blood type for transfusion, as AB positive is the universal recipient. It is not a reason to report to the provider or stop the transfusion.
A nurse is caring for a client who has a chest tube connected to a water seal drainage system. The nurse observes continuous bubbling in the water seal chamber.
Which of the following actions should the nurse take?
Explanation
Check the tubing for any leaks or kinks.
Rationale: The nurse should check the tubing for any leaks or kinks, as continuous bubbling in the water seal chamber indicates an air leak in the system, which can impair lung re-expansion and drainage. The nurse should locate and seal the leak, and notify the provider if necessary.
Incorrect options:
A) Clamp the chest tube near the insertion site. - This is an incorrect action, as clamping the chest tube can cause a tension pneumothorax, which is a life-threatening condition that occurs when air accumulates in the pleural space and compresses the lung and other structures. The nurse should only clamp the chest tube briefly when changing the drainage system or assessing for an air leak.
C) Increase the suction pressure to the drainage system. - This is an incorrect action, as increasing the suction pressure to the drainage system can cause damage to the lung tissue and increase the risk of infection. The nurse should follow
the provider's prescription and the manufacturer's guidelines for setting and adjusting the suction pressure.
D) Document the finding as an expected outcome. - This is an incorrect action, as documenting the finding as an expected outcome implies that continuous bubbling in the water seal chamber is normal, which it is not. The nurse should document
the finding as an abnormal finding and report it to the provider.
A nurse is teaching a client who has diabetes mellitus about self-monitoring of blood glucose levels at home.
Which of the following instructions should the nurse include in the teaching?
Explanation
"Wash your hands with warm water and soap before testing."
Rationale: The nurse should instruct the client to wash their hands with warm water and soap before testing, as this helps to prevent infection and remove any substances that may interfere with the accuracy of the test result.
Incorrect options:
B) "Use alcohol wipes to clean your finger before pricking it." - This is an incorrect instruction, as using alcohol wipes to clean the finger can dry out and irritate the skin, and may also affect the test result if the alcohol is not completely dry before pricking.
C) "Squeeze your finger firmly to obtain a drop of blood." - This is an incorrect instruction, as squeezing the finger firmly can cause hemolysis or dilution of the blood sample, leading to inaccurate readings. The client should apply gentle pressure to the finger after pricking it.
D) "Choose a different finger for each test throughout the day." - This is an incorrect instruction, as choosing a different finger for each test throughout the day can increase the risk of infection and pain. The client should rotate the testing sites within one finger or use alternate sites, such as the forearm or palm.
A nurse is receiving a report on a client who has just returned from the operating room after undergoing a total hip arthroplasty.
Which of the following information should the nurse obtain from the report?
Explanation
The presence and quality of pedal pulses on both legs.
Rationale: The nurse should obtain information on the presence and quality of pedal pulses on both legs from the report, as this indicates the adequacy of blood circulation and perfusion to the lower extremities, which can be compromised by surgery, positioning, or complications such as thromboembolism or compartment syndrome.
Incorrect options:
A) The type and size of the prosthesis used may be important information for the surgical team and the client's medical record, but it is not immediately relevant to the immediate post-operative care provided by the nurse.
B) The amount and color of urine output during surgery is not directly related to the client's condition after a total hip arthroplasty and is not the primary focus of the nurse's assessment at this time.
C) The type and dose of anesthesia administered is important information for the client's medical record and may have implications for post-operative care, but it is not the most critical information for the nurse to obtain immediately upon receiving the report.
Special Considerations in Patient Assessment and Documentation
A nurse is assessing a client who has a history of substance abuse.
Which of the following findings should the nurse report to the provider immediately?
Explanation
Respiratory depression
Rationale: Respiratory depression is a life-threatening complication of substance abuse, especially opioid overdose, that requires immediate intervention. The nurse should report this finding to the provider and prepare to administer naloxone, an opioid antagonist, as prescribed.
Incorrect options:
A) Dilated pupils - This is a common finding in clients who abuse stimulants, such as cocaine or methamphetamine, but it is not an emergency.
B) Slurred speech - This is a common finding in clients who abuse depressants, such as alcohol or benzodiazepines, but it is not an emergency.
C) Agitation and restlessness - This is a common finding in clients who abuse stimulants, such as cocaine or methamphetamine, but it is not an emergency.
A nurse is caring for a client who has a tracheostomy tube and requires suctioning.
Which of the following actions should the nurse take to prevent hypoxia during the procedure?
Explanation
All of the above
Rationale: The nurse should apply suction for no longer than 10 seconds at a time, preoxygenate the client with 100% oxygen before suctioning, and limit the number of suction passes to three per session to prevent hypoxia during tracheostomy suctioning. These actions help to minimize the interruption of oxygen delivery and reduce the risk of mucosal trauma and bleeding.
Incorrect options:
None
A nurse is performing a skin assessment on a client who has dark skin.
Which of the following techniques should the nurse use to detect cyanosis in this client?
Explanation
Inspect the nail beds and lips for a bluish hue.
Rationale: Cyanosis is a bluish discoloration of the skin and mucous membranes due to inadequate oxygenation of the blood. In clients who have dark skin, cyanosis may be difficult to detect by visual inspection of the skin alone. The nurse should inspect the nail beds and lips for a bluish hue, as these areas are more sensitive to changes in oxygen saturation.
Incorrect options:
B) Palpate the skin for warmth and moisture - This technique may help to assess for other skin conditions, such as dehydration or infection, but it does not indicate cyanosis.
C) Compare the skin color with a standardized color chart - This technique may help to assess for other skin conditions, such as jaundice or anemia, but it does not indicate cyanosis.
D) Observe the skin for pallor or ashiness - This technique may help to assess for other skin conditions, such as shock or hypovolemia, but it does not indicate cyanosis.
A nurse is documenting the findings of a physical examination on a client who has heart failure.
Which of the following terms should the nurse use to describe crackles heard in the lungs?
Explanation
Rales
Rationale: Rales are fine, high-pitched crackling sounds heard in the lungs due to fluid accumulation or inflammation. They are commonly heard in clients who have heart failure, pneumonia, or pulmonary edema.
Incorrect options:
A) Wheezes - Wheezes are high-pitched musical sounds heard in the lungs due to narrowed airways. They are commonly heard in clients who have asthma, chronic obstructive pulmonary disease (COPD), or bronchitis.
B) Rhonchi - Rhonchi are low-pitched snoring sounds heard in the lungs due to secretions or mucus in the large airways. They are commonly heard in clients who have bronchitis, cystic fibrosis, or pneumonia.
D) Stridor - Stridor is a high-pitched crowing sound heard in the upper airway due to obstruction or inflammation. It is commonly heard in clients who have croup, epiglottitis, or foreign body aspiration.
A nurse is reviewing the laboratory results of a client who has diabetes mellitus.
Which of the following values should the nurse report to the provider as a priority?
Explanation
Urine ketones 3+
Rationale: Urine ketones 3+ indicate a high level of ketones in the urine, which is a sign of diabetic ketoacidosis (DKA), a life-threatening complication of diabetes mellitus. DKA occurs when the body breaks down fat for energy due to insufficient insulin, resulting in the production of acidic ketones that cause metabolic acidosis. The nurse should report this value to the provider as a priority and prepare to administer intravenous fluids, insulin, and electrolytes as prescribed.
Incorrect options:
A) Hemoglobin A1c 8.5% - Hemoglobin A1c is a measure of the average blood glucose level over the past 2 to 3 months. A value of 8.5% indicates poor glycemic control and an increased risk of complications, but it is not an emergency.
B) Blood glucose 180 mg/dL - Blood glucose is a measure of the amount of glucose in the blood at a given time. A value of 180 mg/dL indicates hyperglycemia, which is common in clients who have diabetes mellitus, but it is not an emergency.
D) Serum creatinine 1.2 mg/dL - Serum creatinine is a measure of the amount of creatinine, a waste product of muscle metabolism, in the blood. A value of 1.2 mg/dL is within the normal range for adults and does not indicate any problem.
A nurse is obtaining informed consent from a client who is scheduled for a colonoscopy.
Which of the following statements by the client indicates a need for further clarification?
Explanation
"I think that I can drive myself home after the procedure."
Rationale: The client should be informed that they cannot drive themselves home after the procedure, as they will be under the influence of sedation and may experience drowsiness, impaired judgment, and delayed reaction time. The client should arrange for a responsible adult to accompany them home and stay with them until the effects of sedation wear off.
Incorrect options:
A) "I understand that I will be sedated during the procedure." - This is a correct statement, as sedation is usually administered during a colonoscopy to reduce discomfort and anxiety.
B) "I know that I have to drink a lot of clear liquids before the procedure." - This is a correct statement, as drinking clear liquids before the procedure helps to cleanse the bowel and improve visualization.
C) "I expect that I will have some abdominal cramps and gas after the procedure." - This is a correct statement, as abdominal cramps and gas are common after a colonoscopy due to air insufflation during the procedure. The client should be advised to ambulate and pass gas as tolerated to relieve these symptoms.
Nursing roles in Patient assessment and documentation
A nurse is assessing a client who has been admitted with suspected sepsis.
Which finding should the nurse report to the provider immediately?
Explanation
Blood pressure of 90/60 mmHg
Rationale: A blood pressure of 90/60 mmHg indicates hypotension, which is a sign of septic shock and requires immediate intervention. Hypotension results from vasodilation and fluid loss due to the systemic inflammatory response to infection.
Incorrect options:
A) Temperature of 38.5°C (101.3°F) - This is a sign of fever, which is a common symptom of sepsis, but not as urgent as hypotension.
B) Heart rate of 110 beats per minute - This is a sign of tachycardia, which is a compensatory mechanism to maintain cardiac output in sepsis, but not as urgent as hypotension.
D) Respiratory rate of 22 breaths per minute - This is within the normal range for adults and does not indicate respiratory distress.
A nurse is documenting the findings of a head-to-toe assessment on a client who has been hospitalized for pneumonia.
Which statement by the nurse reflects the appropriate use of objective data?
Explanation
"The client has crackles in the lower lobes bilaterally."
Rationale: Objective data are observable and measurable facts that can be verified by the nurse or another health care provider. Crackles are an abnormal lung sound that can be heard with a stethoscope and indicate fluid accumulation in the alveoli.
Incorrect options:
A) "The client reports feeling short of breath and fatigued." - This is an example of subjective data, which are information that only the client can perceive and describe, such as feelings, sensations, and beliefs.
C) "The client states that he has been coughing up green sputum." - This is also an example of subjective data, as it is based on the client's verbal report.
D) "The client rates his pain as 4 out of 10 on a numeric scale." - This is another example of subjective data, as pain is a personal experience that cannot be directly measured by the nurse.
A nurse is performing a skin assessment on a client who has a history of melanoma.
Which finding should alert the nurse to a possible malignant lesion?
Explanation
A black nodule with an irregular border and asymmetrical shape
Rationale: A black nodule with an irregular border and asymmetrical shape is consistent with the ABCDE criteria for melanoma, which are: Asymmetry, Border irregularity, Color variation, Diameter greater than 6 mm, and Evolving or changing appearance.
Incorrect options:
A) A brown mole with a smooth border and symmetrical shape - This is a normal finding that does not indicate malignancy.
B) A red macule with a flat surface and well-defined edges - This is likely a benign vascular lesion, such as a cherry angioma or petechiae.
D) A yellow papule with a raised surface and round edges - This is likely a benign sebaceous lesion, such as a sebaceous cyst or milia.
A nurse is reviewing the laboratory results of a client who has been diagnosed with diabetes mellitus.
Which value should the nurse recognize as an indicator of poor glycemic control?
Explanation
Glycosylated hemoglobin (HbA1c) of 8%
Rationale: Glycosylated hemoglobin (HbA1c) reflects the average blood glucose level over the past two to three months. A normal HbA1c level is less than 5.7%, while a level above 6.5% indicates diabetes. A level of 8% or higher indicates poor glycemic control and increased risk of complications.
Incorrect options:
A) Fasting blood glucose of 126 mg/dL - This is a borderline value that may indicate prediabetes, but not necessarily poor glycemic control. A fasting blood glucose of 126 mg/dL or higher on two separate occasions is diagnostic of diabetes.
C) Random blood glucose of 180 mg/dL - This is an elevated value that may indicate hyperglycemia, but not necessarily poor glycemic control. A random blood glucose of 200 mg/dL or higher with symptoms of diabetes is diagnostic of diabetes.
D) Urine ketones of negative - This is a normal finding that indicates the absence of ketones in the urine. Ketones are produced when the body breaks down fat for energy due to insufficient insulin. The presence of ketones in the urine indicates diabetic ketoacidosis, a life-threatening complication of diabetes.
A nurse is conducting a mental status examination on a client who has been admitted for psychiatric evaluation.
Which question should the nurse ask to assess the client's orientation?
Explanation
"What day of the week and month of the year is it?"
Rationale: Orientation is the awareness of one's personal identity, location, and time. Asking the client what day of the week and month of the year it is can help to assess the client's orientation to time.
Incorrect options:
A) "What is your name and date of birth?" - This question can help to assess the client's orientation to person, but not to location or time.
B) "Do you know where you are and why you are here?" - This question can help to assess the client's orientation to place, but not to person or time.
D) "Do you have any thoughts of harming yourself or others?" - This question can help to assess the client's suicidal or homicidal ideation, but not their orientation.
A nurse is preparing to administer an intramuscular injection to a client who has a latex allergy.
Which action should the nurse take to prevent an allergic reaction?
Explanation
Use a non-latex glove to palpate the injection site
Rationale: The nurse should use a non-latex glove to palpate the injection site, as latex gloves can cause skin irritation, rash, or anaphylaxis in clients who have a latex allergy.
Incorrect options:
A) Use a filter needle to draw up the medication from the vial - This action is not related to preventing an allergic reaction, but rather to preventing contamination or injury from glass particles that may be present in some vials.
C) Use an alcohol swab to cleanse the injection site - This action is not related to preventing an allergic reaction, but rather to preventing infection by reducing the number of microorganisms on the skin.
D) Use a Z-track technique to inject the medication - This action is not related to preventing an allergic reaction, but rather to preventing leakage or irritation of the medication into the subcutaneous tissue by creating a zigzag path with the needle.
Summary
A nurse is assessing a client who has a history of chronic obstructive pulmonary disease (COPD).
Which finding should the nurse report to the provider immediately?
Explanation
Cyanosis of the lips and nail beds
Rationale: Cyanosis of the lips and nail beds indicates severe hypoxia and requires immediate intervention. The nurse should report this finding to the provider and administer oxygen as prescribed.
Incorrect options:
A) Barrel-shaped chest - This is a common finding in clients with COPD, due to the increased anteroposterior diameter of the chest caused by air trapping and hyperinflation of the lungs. It does not require immediate intervention.
B) Clubbing of the fingers - This is a sign of chronic hypoxia and is often seen in clients with COPD. It results from the proliferation of connective tissue at the base of the nails due to chronic low oxygen levels. It does not require immediate intervention.
D) Wheezes on auscultation - This is an expected finding in clients with COPD, due to the narrowing of the airways caused by inflammation, mucus production, and bronchospasm. It does not require immediate intervention.
A client is admitted to the hospital with suspected meningitis.
Which assessment finding should alert the nurse to perform a Kernig's sign test?
Explanation
Nuchal rigidity
Rationale: Nuchal rigidity, or stiffness of the neck, is a classic sign of meningitis and indicates inflammation of the meninges, the membranes that cover the brain and spinal cord. Kernig's sign is a test that involves flexing the client's hip and knee at 90 degrees and then attempting to straighten the leg. A positive Kernig's sign is when the client experiences pain or resistance in the hamstring muscles, indicating meningeal irritation.
Incorrect options:
A) Fever - This is a nonspecific sign of infection and inflammation and does not indicate meningitis specifically.
B) Headache - This is a common symptom of meningitis, due to the increased intracranial pressure caused by inflammation of the meninges. However, it is not a specific sign that warrants performing a Kernig's sign test.
D) Photophobia - This is a common symptom of meningitis, due to the sensitivity of the optic nerve to light caused by inflammation of the meninges. However, it is not a specific sign that warrants performing a Kernig's sign test.
A nurse is documenting the wound care provided to a client who has a pressure ulcer on the sacrum.
Which information should the nurse include in the documentation?
Explanation
All of the above
Rationale: The nurse should document all aspects of wound care, including the type and amount of dressing used, the location and size of the wound, and the appearance and odor of the wound. This information helps to monitor the healing process, evaluate the effectiveness of interventions, and identify any signs of infection or complications.
Incorrect options:
A) The type and amount of dressing used - This is an important information to document, but not the only one.
B) The location and size of the wound - This is an important information to document, but not the only one.
C) The appearance and odor of the wound - This is an important information to document, but not the only one.
A client who has diabetes mellitus is scheduled for a colonoscopy. The nurse instructs the client to stop taking metformin 48 hours before and after the procedure.
What is the rationale for this instruction?
Explanation
To prevent lactic acidosis due to contrast dye
Rationale: Metformin is an oral antidiabetic agent that lowers blood glucose levels by decreasing hepatic glucose production and increasing peripheral glucose uptake. However, metformin can cause lactic acidosis, a rare but serious condition that occurs when lactate accumulates in the blood faster than it can be metabolized. Lactic acidosis can be triggered by contrast dye used for radiographic procedures, such as colonoscopy, especially in clients who have renal impairment or dehydration. Therefore, metformin should be discontinued 48 hours before and after any procedure that involves contrast dye.
Incorrect options:
A) To prevent hypoglycemia during fasting - This is not the rationale for discontinuing metformin, as metformin does not cause hypoglycemia by itself. However, the client may need to adjust the dose of other antidiabetic medications or insulin to prevent hypoglycemia during fasting.
C) To prevent hyperglycemia due to stress response - This is not the rationale for discontinuing metformin, as metformin does not cause hyperglycemia by itself. However, the client may need to monitor blood glucose levels more frequently and report any signs of hyperglycemia to the provider.
D) To prevent nephrotoxicity due to dehydration - This is not the rationale for discontinuing metformin, as metformin does not cause nephrotoxicity by itself. However, the client should be advised to maintain adequate hydration before and after the procedure to prevent dehydration and renal impairment.
A nurse is assessing a client who has a chest tube connected to a water seal drainage system. The nurse observes continuous bubbling in the water seal chamber.
What does this finding indicate?
Explanation
An air leak in the system
Rationale: Continuous bubbling in the water seal chamber indicates an air leak in the system, which can compromise the negative pressure needed for effective drainage of air and fluid from the pleural space. The nurse should locate the source of the air leak and take appropriate measures to correct it. Possible sources of air leak include loose connections, cracks or holes in the tubing or drainage container, or a leak in the lung tissue.
Incorrect options:
B) A normal functioning of the system - Intermittent bubbling in the water seal chamber during inspiration, expiration, or coughing is a normal finding that indicates that air is being removed from the pleural space. Continuous bubbling is abnormal and indicates an air leak.
C) A need to empty the collection chamber - The collection chamber is where fluid drained from the pleural space accumulates. The nurse should empty the collection chamber when it is full or according to facility policy. Bubbling in the collection chamber is not a normal finding and does not indicate a need to empty it.
D) A need to clamp the chest tube - Clamping the chest tube is not recommended unless ordered by the provider or necessary for changing the drainage system. Clamping the chest tube can cause a buildup of pressure in the pleural space and lead to complications such as tension pneumothorax.
A client who has hypertension is prescribed hydrochlorothiazide, a thiazide diuretic. The nurse teaches the client about dietary modifications while taking this medication.
Which statement by the client indicates a need for further teaching?
Explanation
"I will avoid foods that are high in calcium."
Rationale: Hydrochlorothiazide is a thiazide diuretic that lowers blood pressure by increasing urine output and reducing fluid volume. However, it also causes increased excretion of potassium and magnesium, and decreased excretion of calcium and uric acid. Therefore, clients taking hydrochlorothiazide should eat more foods that are rich in potassium and magnesium, such as bananas, oranges, potatoes, spinach, nuts, and seeds; limit their intake of sodium and fluids to prevent fluid retention and edema; avoid foods that are high in uric acid, such as organ meats, shellfish, and alcohol; and monitor their serum calcium levels regularly. There is no need to avoid foods that are high in calcium, as hydrochlorothiazide does not increase calcium excretion.
Incorrect options:
A) "I will eat more foods that are rich in potassium." - This is a correct statement, as hydrochlorothiazide causes increased potassium excretion and can lead to hypokalemia if not supplemented.
B) "I will limit my intake of sodium and fluids." - This is a correct statement, as sodium and fluids can cause fluid retention and edema, which can increase blood pressure and counteract the effects of hydrochlorothiazide.
D) "I will drink alcohol in moderation." - This is a correct statement, as alcohol can increase uric acid levels and cause gout attacks in clients taking hydrochlorothiazide. Alcohol can also lower blood pressure and increase the risk of orthostatic hypotension.
A nurse is preparing to report a medication error to the nurse manager.
What is the most appropriate action for the nurse to take?
Explanation
Document the error in the client's medical record and the incident report.
Rationale: The nurse should document the error in both the client's medical record and the incident report, as this is part of the legal and ethical responsibility of the nurse. The documentation should include the facts of what happened, what actions were taken, and the client's response.
Incorrect options:
B) Notify the client's physician and the risk management department. - This is not the most appropriate action, as the nurse should first report the error to the nurse manager, who will then decide who else needs to be notified and how to proceed with further investigation and follow-up.
C) Explain the error to the client and apologize sincerely. - This is not the most appropriate action, as the nurse should first ensure that the client is safe and stable, and then consult with the nurse manager and the legal department before disclosing the error to the client. The nurse should also avoid admitting fault or liability, as this could have legal implications.
D) Wait until the end of the shift to report the error. - This is not an appropriate action, as the nurse should report the error as soon as possible, preferably within an hour of its occurrence. Delaying reporting could compromise client safety and quality of care, as well as increase the risk of legal action.
A client who had a stroke is being transferred from the intensive care unit (ICU) to a rehabilitation unit. The ICU nurse is giving a handoff report to the rehabilitation nurse.
Which information should be included in the report?
Explanation
The client's functional status, goals, and discharge plan.
Rationale: The client's functional status, goals, and discharge plan are relevant information for the rehabilitation nurse, as they provide a baseline for assessing progress and planning interventions. The rehabilitation nurse will focus on helping the client regain function and independence, as well as preparing for discharge.
Incorrect options:
A) The client's vital signs, laboratory results, and medications. - This is not relevant information for the rehabilitation nurse, as these are routine data that can be obtained from other sources, such as electronic records or charts. The rehabilitation nurse will monitor these parameters as needed, but they are not essential for planning care.
B) The client's medical history, diagnosis, and prognosis. - This is not relevant information for the rehabilitation nurse, as these are general data that can be obtained from other sources, such as electronic records or charts. The rehabilitation nurse will be aware of these factors, but they are not specific for planning care.
D) The client's preferences, family involvement, and psychosocial needs. - This is not relevant information for the rehabilitation nurse, as these are subjective data that can be obtained from direct communication with the client and family. The rehabilitation nurse will address these aspects as part of holistic care, but they are not critical for planning care.
A nurse is receiving a telephone order from a physician for a new medication for a client.
Which action should the nurse take to ensure accuracy and safety?
Explanation
Repeat back the order to the physician verbatim.
Rationale: The nurse should repeat back the order to the physician verbatim, as this is a standard practice to verify the accuracy and completeness of the order. Repeating back the order allows the nurse and the physician to check for any errors, omissions, or ambiguities, and to clarify any questions or concerns.
Incorrect options:
B) Ask another nurse to listen to the order on speakerphone. - This is not an appropriate action, as it violates the confidentiality and privacy of the client and the physician. Moreover, it does not ensure that the order is correctly understood and recorded by the nurse who will enter it into the computer.
C) Writing down the order on a piece of paper before entering it into the computer is not an appropriate action as it increases the risk of transcription errors, lost or misplaced orders, or delayed entry. The nurse should enter the order directly into the computer as soon as possible and discard any paper notes after verification.
D) Confirming the order with a pharmacist before administering it to the client is not an appropriate action as it adds an unnecessary step and delays the implementation of the order. The nurse should confirm the order with the physician, not the pharmacist, and administer it to the client according to the prescribed schedule. The pharmacist will review the order for any potential interactions, allergies, or contraindications and alert the nurse if any issues arise.
Exams on Patient Assessment and Documentation
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
-
Define patient assessment and documentation and explain their importance in nursing practice.
-
Describe the steps of the assessment patient process and the types of data to collect.
-
Identify the principles and methods of documentation and reporting in nursing.
-
Discuss the special considerations in patient assessment and documentation for different patient populations and settings.
-
Explain the nursing roles and responsibilities in patient assessment and documentation.
Introduction to Patient Assessment and Documentation
-
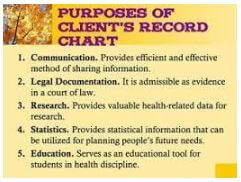
Patient assessment is the systematic collection, analysis, and interpretation of data about a patient's health status, needs, preferences, and goals.
-
Documentation is the recording of the patient assessment data and the nursing interventions, outcomes, and evaluations in a clear, accurate, timely, and legal manner.
-
Patient assessment and documentation are essential for providing safe, effective, and individualized nursing care, as well as for communicating with other health care providers, ensuring continuity of care, evaluating the quality of care, and meeting legal and ethical standards.
-
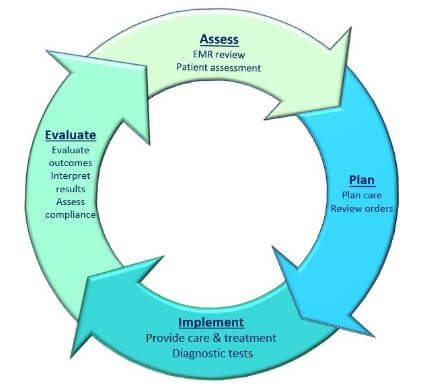
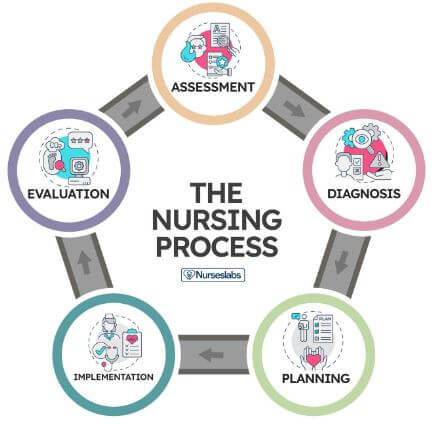
The Assessment Patient Process
-
The assessment patient process consists of four steps: preparation, data collection, data analysis, and data validation.
-
Preparation involves reviewing the patient's medical history, previous assessments, and current orders; setting the purpose and scope of the assessment; and establishing rapport with the patient.
-
Data collection involves gathering subjective data (what the patient says) and objective data (what the nurse observes or measures) using various sources (e.g., patient interview, physical examination, diagnostic tests) and techniques (e.g., inspection, palpation, auscultation, percussion).
-
Data analysis involves organizing, comparing, and interpreting the data to identify the patient's actual or potential health problems, strengths, risks, and needs.
-
Data validation involves verifying the accuracy and completeness of the data by comparing it with other sources (e.g., other health care providers, family members, medical records) and resolving any discrepancies or gaps.
-
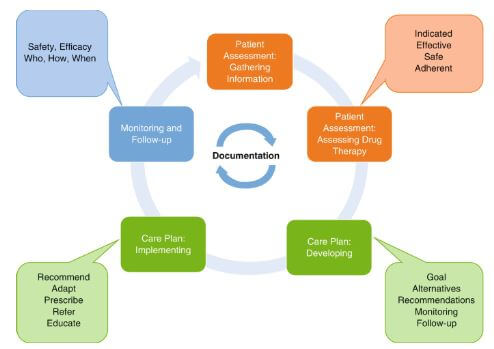
Documentation and Reporting
-
Documentation is the process of recording the patient assessment data and the nursing care plan in a standardized format using appropriate terminology, abbreviations, symbols, and charts.
-
Reporting is the process of communicating the patient assessment data and the nursing care plan to other health care providers verbally or in writing.
-
The principles of documentation and reporting include accuracy, completeness, clarity, conciseness, timeliness, confidentiality, and accountability.
-
The methods of documentation and reporting include narrative notes, flow sheets, checklists, graphic records, care plans, incident reports, hand-off reports, progress notes, discharge summaries.
-
Special Considerations in Patient Assessment and Documentation
-
Patient assessment and documentation should be adapted to the specific characteristics of the patient population (e.g., age group, cultural background, health literacy level) and the setting (e.g., acute care, home care, community health).
-
Some examples of special considerations are:
-
Using developmentally appropriate language and techniques for pediatric patients
-
Assessing cognitive function and mental status for geriatric patients
-
Incorporating cultural beliefs and practices into the assessment process for diverse patients
-
Using standardized tools and scales for pain assessment for patients with communication barriers
-
Documenting relevant environmental factors for patients in home care or community health settings
Nursing roles in Patient assessment and documentation
-
The nursing roles in patient assessment and documentation include:
-
Initiating and conducting comprehensive or focused assessments based on the patient's condition, needs, and situation
-
Collaborating with other health care providers in conducting interdisciplinary assessments
-
Documenting the assessment data and the nursing care plan using electronic or paper-based systems
-
Reporting the assessment data and the nursing care plan to other health care providers using oral or written methods
-
Updating and revising the assessment data and the nursing care plan as needed based on changes in the patient's status or response to interventions
-
Evaluating the effectiveness of the assessment process and the documentation system
-
Conclusion
-
Patient assessment and documentation are vital components of nursing practice that enable nurses to provide quality care to their patients.
-
Nurses should follow a systematic process of preparation, data collection, data analysis, and data validation when conducting patient assessments.
-
Nurses should adhere to the principles and methods of documentation and reporting when recording and communicating patient assessments.
-
Nurses should consider the special needs of different patient populations and settings when performing patient assessments and documentation.
-
Nurses should assume various roles and responsibilities in patient assessment and documentation as part of their professional practice.
Summary
-
Patient assessment and documentation are essential for safe and effective nursing care.
-
The assessment patient process includes preparation, data collection, data analysis, and data validation.
-
Documentation and reporting should be accurate, complete, clear, concise, timely, confidential, and accountable.
-
Special considerations include adapting to patient population and setting characteristics.
-
Nursing roles in patient assessment and documentation involve initiating assessments, collaborating with other providers, documenting and reporting, and evaluating effectiveness.
-
Patient assessment and documentation support quality care, and nurses should follow systematic processes and consider individual needs.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Patient Assessment and Documentation
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


