Please set your exam date
Critical Thinking and Nursing Process
Study Questions
Critical Thinking
A nurse is teaching a group of nursing students about the components of critical thinking. Which of the following statements by a student indicates a need for further teaching?
Explanation
Choice A:
This statement is correct and does not indicate a need for further teaching. Reflection is one of the key elements of critical thinking in nursing, as it allows nurses to examine their own actions and decisions and learn from them.
Choice B:
This statement is also correct and does not indicate a need for further teaching. Analysis is another key element of critical thinking in nursing, as it involves breaking down a complex situation into smaller parts that can be understood and evaluated.
Choice C:
This statement is incorrect and indicates a need for further teaching. Inference is not making assumptions based on one's experience, but rather drawing logical conclusions from the available evidence. Making assumptions can lead to errors in judgment and compromise patient safety. Nurses should use critical thinking to question their assumptions and biases and seek reliable and valid information.
Choice D:
This statement is correct and does not indicate a need for further teaching. Evaluation is another key element of critical thinking in nursing, as it involves checking the reliability and validity of information that is used to make decisions. Nurses should use critical thinking to assess the sources, methods, and outcomes of information they encounter in their practice.
A nurse is caring for a client who has a fever, cough, and shortness of breath. The nurse suspects that the client has pneumonia and orders a chest x-ray and blood cultures. Which of the following actions by the nurse demonstrate critical thinking?
Explanation
Choice A:
Comparing the client's vital signs with the normal ranges is a basic nursing skill that does not require critical thinking. It is part of the assessment process, but it does not involve analysis, interpretation, or evaluation of the data. Therefore, this choice is incorrect.
Choice B:
Asking the client about his medical history and allergies is also a basic nursing skill that does not require critical thinking. It is part of the assessment process, but it does not involve analysis, interpretation, or evaluation of the data. Therefore, this choice is incorrect.
Choice C :
Explaining to the client the purpose and procedure of the tests is an example of critical thinking because it involves applying knowledge, skills, and attitudes to provide patient-centered care. The nurse uses critical thinking to determine what information the client needs to know, how to communicate it effectively, and how to evaluate the client's understanding. Therefore, this choice is correct.
Choice D :
Administering an antipyretic medication to the client is a standard nursing intervention that does not require critical thinking. It is part of the implementation process, but it does not involve analysis, interpretation, or evaluation of the data. Therefore, this choice is incorrect.
Choice E:
Documenting the client's condition and interventions in the chart is a legal and ethical responsibility of the nurse that does not require critical thinking. It is part of the communication process, but it does not involve analysis, interpretation, or evaluation of the data. Therefore, this choice is incorrect. Source:.
A nurse is working in an emergency department and receives a call from a paramedic who is transporting a client who was involved in a motor vehicle crash. The paramedic reports that the client has multiple injuries, including a head trauma, chest trauma, and abdominal bleeding. The nurse prepares to receive the client and triage him accordingly. Which of the following statements by the nurse reflects critical thinking?
Explanation
Choice A :.
This statement reflects critical thinking because the nurse prioritizes the most important assessments for a client with multiple injuries and follows the ABC (airway, breathing, circulation) principle of trauma care. Assessing the level of consciousness, airway, breathing, and circulation is essential to determine the client's condition and plan appropriate interventions.
Choice B :.
This statement does not reflect critical thinking because the nurse expresses a hope rather than a fact or an action. Hoping for no internal injuries or organ damage does not help the nurse to provide effective care for the client. The nurse should focus on assessing the client's injuries and providing appropriate interventions based on the findings.
Choice C :.
This statement does not reflect critical thinking because the nurse wonders about irrelevant information that does not affect the client's care. The cause of the crash and the use of seat belt are not important for the nurse to know at this point. The nurse should focus on assessing the client's injuries and providing appropriate interventions based on the findings.
Choice D :.
This statement does not reflect critical thinking because the nurse jumps to a conclusion without assessing the client first. Calling the trauma surgeon and the neurologist right away may not be necessary or appropriate depending on the client's condition. The nurse should assess the client first and then consult with other health care professionals as needed.
A nurse is reviewing the laboratory results of a client who has diabetes mellitus and is receiving insulin therapy. The nurse notices that the client's blood glucose level is 250 mg/dL, which is higher than the target range. The nurse decides to increase the dose of insulin for the next administration. Which of the following statements by the nurse indicates a lack of critical thinking?
Explanation
Choice A:.
This statement does not indicate a lack of critical thinking because the nurse is planning to monitor the client's blood glucose level more frequently to evaluate the effectiveness of the insulin therapy. This is an appropriate nursing intervention for a client who has hyperglycemia.
Choice B :.
This statement does not indicate a lack of critical thinking because the nurse is checking the medication administration record to see if the client received his insulin as prescribed. This is an important step to identify any possible errors or omissions that could have contributed to the client's high blood glucose level.
Choice C:.
This statement indicates a lack of critical thinking because the nurse is increasing the insulin dose by 2 units as per the sliding scale protocol without considering other factors that could affect the client's blood glucose level, such as diet, exercise, stress, or infection. The nurse should not adjust the insulin dose without consulting the provider or following a specific protocol that takes into account the client's individual needs and goals.
Choice D:.
This statement does not indicate a lack of critical thinking because the nurse is asking the client if he ate anything that could have raised his blood sugar level. This is a relevant question to assess the client's dietary intake and adherence to the prescribed meal plan. The nurse should also educate the client about the importance of following a consistent carbohydrate diet and avoiding foods that can spike blood glucose levels.
A nurse is conducting a research project on the effectiveness of an educational intervention on improving critical thinking skills among nursing students. The nurse uses a pretest-posttest design with a control group and an experimental group. The experimental group receives the intervention, while the control group does not. The nurse administers a standardized test of critical thinking skills to both groups before and after the intervention. Which of the following steps in the nursing process does this research project illustrate?
Explanation
Choice A:
Assessment. This is the first step of the nursing process, where the nurse collects data about the patient's health status, needs, and problems. This step does not describe the research project, which already has data from the pretest and posttest.
Choice B:
Diagnosis. This is the second step of the nursing process, where the nurse analyzes the data and identifies the patient's actual or potential nursing diagnoses. This step does not describe the research project, which does not focus on individual patients or diagnoses.
Choice C:
Planning. This is the third step of the nursing process, where the nurse sets goals and outcomes for the patient and selects appropriate nursing interventions. This step does not describe the research project, which already has a plan for the intervention and the control group.
Choice D:
Implementation. This is the fourth step of the nursing process, where the nurse carries out the planned interventions and documents the care provided. This step partially describes the research project, which involves implementing the intervention for the experimental group. However, this is not the best answer because it does not capture the whole purpose of the project.
Choice E:
Evaluation. This is the fifth and final step of the nursing process, where the nurse evaluates the patient's progress toward the goals and outcomes and modifies the plan of care as needed. This step best describes the research project, which involves evaluating the effectiveness of the intervention by comparing the pretest and posttest scores of both groups. The nurse uses a standardized test of critical thinking skills as a measure of evaluation.
The Nursing Process
A nurse is performing an initial assessment on a client who was admitted for pneumonia. Which of the following actions should the nurse take?
Explanation
Choice A :
Comparing the client's vital signs with the previous ones is not the first action the nurse should take during an initial assessment. This is a part of an ongoing or focused assessment that monitors the client's response to treatment and identifies any changes in their condition.
Choice B :
Asking the client about their medical history and current medications is the correct action the nurse should take during an initial assessment. This is a part of collecting subjective data from the client that can provide valuable information about their health status, risk factors, allergies, preferences, and needs. This can help the nurse to identify any potential problems or complications related to the client's pneumonia and plan appropriate interventions.
Choice C :
Performing a head-to-toe physical examination of the client is not the first action the nurse should take during an initial assessment. This is a part of collecting objective data from the client that involves inspecting, palpating, percussing, and auscultating various body systems. However, before performing a physical examination, the nurse should obtain consent from the client, explain the purpose and procedure, and ensure privacy and comfort.
Choice D:
Evaluating the effectiveness of the prescribed antibiotics is not the first action the nurse should take during an initial assessment. This is a part of the evaluation phase of the nursing process that involves comparing the client's outcomes with the expected outcomes and modifying the plan of care as needed. However, before evaluating the effectiveness of any intervention, the nurse should first assess the client's baseline data and implement the intervention according to the plan of care.
A nurse is conducting a problem-focused assessment on a client who has a pressure ulcer on their sacrum. Which of the following data should the nurse collect? (Select all that apply.).
Explanation
Choice A :
The size, depth, and color of the wound are important indicators of the stage and severity of the pressure ulcer. Measuring these parameters can help monitor the healing process and guide the appropriate treatment.
Choice B:
The presence of drainage, odor, or infection can signal complications or poor healing of the pressure ulcer. Drainage can indicate excessive moisture or exudate that can impair wound healing. Odor can suggest bacterial colonization or necrotic tissue. Infection can cause systemic symptoms such as fever, malaise, or leukocytosis.
Choice C:
The type and frequency of dressing changes are essential components of pressure ulcer management. Dressings should be chosen based on the characteristics of the wound, such as the amount of exudate, the presence of necrotic tissue, or the need for debridement. Dressings should be changed as often as necessary to maintain a moist but not wet environment for wound healing.
Choice D :
The client's pain level and preferred analgesics are important data to collect because pressure ulcers can cause significant discomfort and affect the quality of life of the client. Pain can also interfere with wound healing by increasing stress and inflammation. Analgesics should be prescribed according to the client's needs and preferences, taking into account the potential side effects and interactions.
Choice E :
The client's nutritional status and fluid intake are not part of a problem-focused assessment on a client who has a pressure ulcer on their sacrum. These data are relevant for a comprehensive assessment that includes all aspects of the client's health and well-being. However, a problem-focused assessment is more narrow and specific to the presenting problem or issue. Therefore, choice E is not correct.
A nurse is caring for a client who is experiencing chest pain and shortness of breath. The nurse performs an emergency assessment and asks the client, "How would you rate your pain on a scale of 0 to 10?”. What is the nurse's rationale for asking this question?
Explanation
Choice A :
To determine the severity and location of the pain. This is not the best answer because the nurse already knows that the client is experiencing chest pain and shortness of breath, which are signs of a possible cardiac problem. The nurse should also ask about the quality, radiation, and aggravating or relieving factors of the pain, not just the severity and location.
Choice B:
To establish a baseline for evaluating interventions. This is the best answer because the nurse needs to know how severe the pain is before administering any medication or treatment, and then reassess the pain after the intervention to see if it was effective. The pain scale is a useful tool to measure the intensity of pain and compare it over time.
Choice C:
To assess the client's coping skills and anxiety level. This is not the best answer because the nurse should focus on relieving the pain first, as it is an emergency situation. The nurse can assess the client's coping skills and anxiety level later, when the pain is under control.
Choice D:
To identify any factors that aggravate or relieve the pain. This is not the best answer because the nurse should ask this question along with other questions about the pain characteristics, not as a single question. The nurse should also prioritize relieving the pain rather than identifying factors that may or may not affect it.
A nurse is documenting the data collected from an ongoing assessment of a client who has diabetes mellitus. The nurse writes, "The client reports feeling thirsty and hungry all the time.”. How should the nurse label this type of data?
Explanation
Choice A reason:.
Objective data is anything that you can observe through your sense of hearing, sight, smell, and touch while assessing the patient. For example, vital signs, physical examination findings, and laboratory results are objective data. The client's report of feeling thirsty and hungry is not something that the nurse can observe directly, so it is not objective data.
Choice B reason:.
Subjective data is information obtained from the patient and/or family members and offers important cues from their perspectives. For example, the patient's pain level, feelings, beliefs, and preferences are subjective data. The client's report of feeling thirsty and hungry is something that only the client can describe, so it is subjective data. This is the correct answer.
Choice C reason:.
Primary data is information provided directly by the patient. For example, the patient's history, symptoms, and concerns are primary data. The client's report of feeling thirsty and hungry is primary data, but this is not the best answer because it does not specify whether it is subjective or objective. Primary data can be either subjective or objective depending on the source.
Choice D reason:.
Secondary data is information collected from a family member, chart, or other sources. For example, the patient's previous records, family history, and test results are secondary data. The client's report of feeling thirsty and hungry is not secondary data because it comes from the client directly, not from another source.
A nurse is organizing the data collected from an assessment of a client who has chronic obstructive pulmonary disease (COPD). The nurse uses a framework that categorizes the data into functional health patterns, such as activity-exercise, nutrition-metabolism, and elimination. What is the name of this framework?
Explanation
Choice A reason:.
Gordon's functional health patterns is a framework that categorizes the data into functional health patterns, such as activity-exercise, nutrition-metabolism, and elimination. This framework was developed by Marjory Gordon in 1987 and is widely used by nurses to assess the health status of individuals, families, and communities.
Choice B reason:.
Maslow's hierarchy of needs is a motivational theory in psychology that proposes a five-tier model of human needs, often depicted as a pyramid. The needs are physiological, safety, love and belonging, esteem, and self-actualization. This theory is not a framework for organizing data collected from an assessment of a client.
Choice C reason:.
Orem's self-care deficit theory is a nursing theory that states that people have an innate ability to perform self-care activities that maintain their health and well-being. The theory consists of three related theories: the theory of self-care, the theory of self-care deficit, and the theory of nursing system. This theory is not a framework for organizing data collected from an assessment of a client.
Choice D reason:.
Roy's adaptation model is a nursing theory that views the person as a bio-psycho-social being who is constantly interacting with a changing environment. The theory focuses on how the person adapts to stimuli through four adaptive modes: physiological-physical, self-concept-group identity, role function, and interdependence. This theory is not a framework for organizing data collected from.
Diagnosis
A nurse is reviewing the diagnostic statements of a client who has multiple health problems. Which of the following statements is an example of an actual diagnosis?
Explanation
Choice A reason:.
This is not an example of an actual diagnosis because it describes a potential problem that has not yet occurred. An actual diagnosis identifies a problem that is present at the time of the assessment and is based on signs and symptoms.
Choice B reason:.
This is an example of an actual diagnosis because it describes a problem that is present at the time of the assessment and is based on signs and symptoms. An actual diagnosis consists of three components: the problem, the etiology, and the defining characteristics. In this case, the problem is impaired skin integrity, the etiology is related to pressure ulcer, and the defining characteristics are evidenced by 4 cm x 3 cm wound on sacrum.
Choice C reason:.
This is not an example of an actual diagnosis because it does not include any defining characteristics that support the problem. An actual diagnosis requires evidence of signs and symptoms to validate the problem.
Choice D reason:.
This is not an example of an actual diagnosis because it describes a readiness to enhance a specific health behavior rather than a problem that is present at the time of the assessment. A readiness for enhanced diagnosis identifies a strength or potential for improvement in a client's health status.
A nurse is assessing a client who has a fever and reports feeling cold. The nurse observes that the client is shivering and has goosebumps on his skin. Which of the following terms should the nurse use to describe these findings in the diagnostic statement?
Explanation
Choice A reason:.
Problem is not the correct term to describe these findings because it is too vague and does not specify the human response to the health condition. A problem is a general label that can apply to many situations, but a nursing diagnosis should be more precise and descriptive.
Choice B reason:.
Etiology is not the correct term to describe these findings because it refers to the cause or contributing factors of the problem, not the problem itself. Etiology is usually preceded by the phrase "related to”. in a nursing diagnostic statement. For example, "Impaired skin integrity related to pressure ulcer”. is a nursing diagnosis where "pressure ulcer”. is the etiology.
Choice C reason:.
Defining characteristics is the correct term to describe these findings because it refers to the observable and verifiable signs and symptoms that indicate the presence of a problem or risk. Defining characteristics are usually preceded by the phrase "as evidenced by”. in a nursing diagnostic statement. For example, "Acute pain as evidenced by grimacing, guarding, and increased heart rate”. is a nursing diagnosis where "grimacing, guarding, and increased heart rate”. are the defining characteristics.
Choice D reason:.
Related factors is not the correct term to describe these findings because it refers to the conditions or circumstances that are associated with the problem or risk, but are not necessarily the cause. Related factors are usually preceded by the phrase "related to”. in a risk nursing diagnostic statement. For example, "Risk for falls related to impaired balance”. is a nursing diagnosis where "impaired balance”. is a related factor.
A nurse is caring for a client who has a history of substance abuse and is at risk for withdrawal. The nurse plans to monitor the client for signs of anxiety, agitation, and tremors. Which of the following types of diagnosis should the nurse use for this client?
Explanation
Choice A reason:
An actual diagnosis is based on the presence of associated signs and symptoms, not on the risk of developing them. The client in the question does not have any signs or symptoms of withdrawal yet, only a history of substance abuse. Therefore, an actual diagnosis is not appropriate for this client.
Choice B reason:
A risk diagnosis is based on the presence of risk factors that increase the likelihood of developing a problem or dysfunction. The client in the question has a history of substance abuse, which is a risk factor for withdrawal. The nurse plans to monitor the client for signs of anxiety, agitation, and tremors, which are potential indicators of withdrawal. Therefore, a risk diagnosis is appropriate for this client.
Choice C reason:
A health promotion diagnosis is based on the desire to enhance well-being and human potential. The client in the question does not express any desire to improve their health or well-being, nor does the nurse plan to implement any interventions to promote health. Therefore, a health promotion diagnosis is not appropriate for this client.
Choice D reason:
A wellness diagnosis is based on the presence of a transition from one level of wellness to a higher level of wellness. The client in the question does not show any evidence of a transition or a higher level of wellness, nor does the nurse plan to facilitate any wellness activities. Therefore, a wellness diagnosis is not appropriate for this client.
A nurse is evaluating a client who has expressed a desire to quit smoking. The client states that he has reduced his cigarette consumption by half and has joined a support group. Which of the following types of diagnosis should the nurse use for this client?
Explanation
Choice A reason:
An actual diagnosis is based on the presence of associated signs and symptoms of a health problem. The client does not have any signs or symptoms of a health problem related to smoking, but rather has expressed a desire to quit smoking and has taken some steps to do so.
Choice B reason:
A risk diagnosis is based on the presence of risk factors that increase the vulnerability of a person or group to develop a health problem. The client does not have any risk factors that increase his vulnerability to develop a health problem related to smoking, but rather has reduced his cigarette consumption by half and has joined a support group.
Choice C reason:
A health promotion diagnosis is based on the desire to enhance well-being and can be expressed by a readiness to enhance specific health behaviors. The client has expressed a desire to quit smoking, which is a specific health behavior that can enhance his well-being. Therefore, this is the correct type of diagnosis for this client.
Choice D reason:
A wellness diagnosis is based on the presence of potential or actual levels of wellness in an individual, family, or community that can be enhanced. The client does not have any potential or actual levels of wellness related to smoking, but rather has a desire to quit smoking and improve his health. Therefore, this is not the correct type of diagnosis for this client.
A nurse is formulating a diagnostic statement for a client who has diabetes mellitus and peripheral neuropathy. Which of the following components should the nurse include in the statement? (Select all that apply.).
Explanation
Choice A reason:
The problem is the first component of a diagnostic statement for a client who has diabetes mellitus and peripheral neuropathy. The problem is the nursing diagnosis that describes the client's health status in response to the actual or potential health problem. For example, the problem could be impaired skin integrity, risk for infection, or chronic pain.
Choice B reason:
The etiology is not a component of a diagnostic statement for a client who has diabetes mellitus and peripheral neuropathy. The etiology is the cause or contributing factor of the problem. For example, the etiology could be diabetes mellitus, peripheral neuropathy, or poor circulation.
Choice C reason:
The signs and symptoms are the third component of a diagnostic statement for a client who has diabetes mellitus and peripheral neuropathy. The signs and symptoms are the evidence or data that support the problem. For example, the signs and symptoms could be ulceration, numbness, or tingling.
Choice D reason:.
The medical diagnosis is not a component of a diagnostic statement for a client who has diabetes mellitus and peripheral neuropathy. The medical diagnosis is the identification of a disease or condition by a physician or other health care provider based on scientific criteria. For example, the medical diagnosis could be diabetes mellitus type 1 or type 2, or peripheral neuropathy.
Choice E reason:
The nursing interventions are not a component of a diagnostic statement for a client who has diabetes mellitus and peripheral neuropathy. The nursing interventions are the actions or treatments that the nurse plans and implements to address the problem. For example, the nursing interventions could be wound care, education, or medication administration
Planning
A nurse is performing initial planning for a client who has been admitted with pneumonia. Which of the following actions should the nurse take first?
Explanation
Choice A reason:
Assessing the client's vital signs, oxygen saturation, and respiratory status is the first action the nurse should take because it provides baseline data on the client's condition and helps to identify any urgent needs or complications. This is consistent with the principle of prioritizing assessment before intervention and following the ABCs (airway, breathing, circulation) of emergency care.
Choice B reason:
Educating the client about the disease process and preventive measures is an important action, but not the first one. The nurse should assess the client's learning needs, readiness, and preferences before providing education. Education is also a lower priority than addressing any immediate threats to the client's health or safety.
Choice C reason:
Collaborating with the physician to prescribe antibiotics and bronchodilators is an appropriate action for a client with pneumonia, but not the first one. The nurse should assess the client's condition and obtain relevant laboratory and diagnostic tests before initiating pharmacological interventions. The nurse should also follow the physician's orders and the facility's policies and protocols when administering medications.
Choice D reason:
Setting goals and outcomes for the client's recovery and discharge is a necessary step in the nursing process, but not the first one. The nurse should assess the client's current status, needs, preferences, and resources before planning care. The nurse should also involve the client and family in setting realistic and measurable goals and outcomes.
A nurse is updating the plan of care for a client who has a pressure ulcer on the sacrum. Which of the following outcomes are appropriate for this client?
Explanation
Choice A reason:
The client will have no signs of infection in the wound by day 7. This is an appropriate outcome because it indicates that the wound is healing properly and that the client is receiving adequate wound care and infection prevention measures. Infection can delay wound healing and increase the risk of complications.
Choice B reason:
The client will report pain level of 4/10 or less during dressing changes. This is not an appropriate outcome because it does not address the wound healing process or the prevention of further skin breakdown. Pain management is important for the client's comfort and quality of life, but it is not a specific goal for pressure ulcer care.
Choice C reason:
The client will consume at least 75% of meals and snacks daily. This is an appropriate outcome because it indicates that the client is receiving adequate nutrition to support wound healing. Nutrition plays a vital role in tissue integrity and repair, and the client should consume enough calories, protein, and micronutrients to meet their needs.
Choice D reason:
The client will reposition self in bed every 2 hours with assistance. This is not an appropriate outcome because it does not reflect the current evidence-based practice for pressure ulcer prevention and treatment. Repositioning should be done more frequently than every 2 hours, and the frequency should be individualized based on the client's risk factors, skin condition, comfort, and support surfaces.
Choice E reason:
The client will demonstrate proper wound care technique before discharge. This is an appropriate outcome because it indicates that the client has learned how to care for their wound at home and prevent further skin breakdown. Wound care education is essential for the client's self-management and adherence to the treatment plan.
A nurse is preparing to administer morphine sulfate 2 mg IV to a client who has acute pain. Which of the following statements by the nurse is an example of an independent intervention?
Explanation
Choice A reason:
Checking the pain level and location before and after giving the medication is an example of an independent intervention because it is within the nurse's scope of practice and does not require a provider's order. It is also part of the nursing process to assess the patient's pain and evaluate the effectiveness of the intervention.
Choice B reason:
Flushing the IV line with normal saline before and after giving the medication is not an independent intervention because it is a dependent intervention that requires a provider's order. It is also a standard procedure for administering IV medications to prevent occlusion and contamination of the IV line.
Choice C reason:
Monitoring the vital signs and level of consciousness every 15 minutes after giving the medication is not an independent intervention because it is a dependent intervention that requires a provider's order. It is also a safety measure to detect any adverse effects of the medication, such as respiratory depression, hypotension, or sedation.
Choice D reason:
Asking the physician to order naloxone in case of an adverse reaction to the medication is not an independent intervention because it is a collaborative intervention that involves consultation with another health care professional. It is also a precautionary measure to have an opioid antagonist available in case of overdose or severe respiratory depression.
A nurse is consulting with a physical therapist for a client who has chronic low back pain. Which of the following statements by the physical therapist is an example of a collaborative intervention?
Explanation
Choice A reason:
Teaching the client some exercises to strengthen the core muscles and improve posture is an example of an independent intervention, not a collaborative one. An independent intervention is one that the physical therapist can perform without consulting or coordinating with other members of the health care team.
Choice B reason:
Applying heat therapy to the client's back for 15 minutes before starting the exercises is also an example of an independent intervention, not a collaborative one. Heat therapy is a modality that the physical therapist can use to reduce pain and stiffness, and prepare the client for exercise.
Choice C reason:
Documenting the client's progress and response to the exercises in the medical record is an example of a professional responsibility, not a collaborative intervention. Documentation is essential for communication, quality improvement, and legal purposes, but it does not involve working with other health care providers.
Choice D reason:
Coordinating with the nurse to schedule the exercises after the client receives analgesics is an example of a collaborative intervention. A collaborative intervention is one that requires consultation or coordination with other members of the health care team to achieve a common goal. In this case, the physical therapist and the nurse work together to ensure that the client has adequate pain relief before engaging in exercise, which can improve the client's comfort and compliance.
A nurse is performing discharge planning for a client who has diabetes mellitus. Which of the following actions should the nurse take as part of this process?
Explanation
Choice A reason:
Review the client’s medications and dosage instructions with them. This step is crucial to prevent medication errors and ensure the client understands their regimen. It helps in maintaining proper glycemic control and avoiding complications.
Choice B reason:
Evaluate the client’s blood glucose levels and insulin administration technique. This ensures the client can manage their diabetes effectively at home. Proper technique and understanding of blood glucose monitoring are essential for maintaining target glucose levels.
Choice C reason:
Refer the client to a home health nurse or a diabetes educator as needed. Ongoing support and education from healthcare professionals are vital for managing diabetes. This referral provides the client with resources and guidance to manage their condition effectively.
Choice D reason:
All of the above. Combining all these actions ensures a holistic approach to discharge planning, addressing medication management, self-monitoring, and continuous support, which are all critical for effective diabetes management.
Implementation
A nurse is preparing to perform a direct care intervention for a client who has a wound infection. What should the nurse do first?
Explanation
Choice A reason:
Reviewing the plan of care and the prescribed treatment is the first step in the nursing process for a direct care intervention. The nurse needs to know what the goals, outcomes, and interventions are for the client before performing any action. This ensures that the nurse is following the evidence-based practice and the client's preferences. Reviewing the plan of care also helps the nurse to identify any changes or updates that might be needed based on the client's current condition.
Choice B reason:
Applying sterile gloves and cleaning the wound with saline is an important intervention for a client who has a wound infection, but it is not the first step. The nurse needs to review the plan of care and the prescribed treatment before performing any procedure to ensure that it is appropriate, safe, and effective for the client. Cleaning the wound with saline is part of the implementation phase of the nursing process, which comes after assessment, diagnosis, and planning.
Choice C reason:
Teaching the client about wound care and infection prevention is another important intervention for a client who has a wound infection, but it is not the first step either. The nurse needs to review the plan of care and the prescribed treatment before providing any education to the client. Teaching the client is also part of the implementation phase of the nursing process, which comes after assessment, diagnosis, and planning.
Choice D reason:
Documenting the wound appearance and drainage is a vital component of nursing care, but it is not the first step in a direct care intervention. The nurse needs to review the plan of care and the prescribed treatment before documenting any findings or actions. Documenting the wound appearance and drainage is part of the evaluation phase of the nursing process, which comes after assessment, diagnosis, planning, and implementation.
A nurse is evaluating the effectiveness of indirect care interventions for a client who has diabetes mellitus. Which of the following are appropriate indicators of indirect care outcomes?
Explanation
Choice A reason:
The client's blood glucose level is within the target range. This is not an appropriate indicator of indirect care outcomes because it reflects the direct care provided by the nurse or the client to manage diabetes. Indirect care interventions are those that are performed away from or on behalf of a client, such as documentation, infection control, consultation, or coordination of care.
Choice B reason:
The client's medical record reflects accurate and timely documentation. This is an appropriate indicator of indirect care outcomes because documentation is an essential part of indirect care that ensures continuity and quality of care for the client.
Choice C reason:
The nurse adheres to infection control policies when handling glucose testing supplies. This is an appropriate indicator of indirect care outcomes because infection control is a vital aspect of indirect care that prevents the transmission of pathogens and protects the client and the health care team.
Choice D reason:
The nurse consults with a dietitian about the client's nutritional needs. This is an appropriate indicator of indirect care outcomes because consultation is a form of indirect care that involves seeking the expertise or advice of another health care professional to improve the client's care.
Choice E reason:
The client expresses satisfaction with the quality of care received. This is not an appropriate indicator of indirect care outcomes because it reflects the client's perception of the overall care provided by the nurse or the health care team, which may include both direct and indirect care interventions.
A nurse is providing emotional support to a client who is anxious about an upcoming surgery. Which of the following statements by the nurse demonstrates the use of evidence-based practice and clinical judgment?
Explanation
Choice A reason:
This statement by the nurse suggests a possible intervention for the client's anxiety, but it does not demonstrate the use of evidence-based practice or clinical judgment. Evidence-based practice involves using the best available research evidence, clinical expertise, and patient preferences to make decisions about care. Clinical judgment involves applying critical thinking, knowledge, skills, and experience to assess, plan, implement, and evaluate outcomes of care. The nurse should first assess the client's level of anxiety, sources of anxiety, and coping strategies before suggesting any relaxation techniques. The nurse should also consider the client's values and expectations when choosing an intervention.
Choice B reason:
This statement by the nurse is an example of false reassurance and self-disclosure, which are not appropriate or therapeutic communication techniques. The nurse should avoid saying "I know how you feel”. because it minimizes the client's feelings and assumes that the nurse's experience is similar to the client's. The nurse should also avoid sharing personal information unless it is relevant and beneficial for the client. The nurse should focus on the client's feelings and concerns rather than their own.
Choice C reason:
This statement by the nurse is another example of false reassurance, which is not helpful or evidence-based. The nurse should avoid saying "Don't worry”. or "Everything will be fine”. because it dismisses the client's feelings and implies that the client has no reason to be anxious. The nurse should also avoid giving opinions or guarantees about the outcome of the surgery, as they are not based on facts or evidence. The nurse should acknowledge the client's anxiety and provide factual information about the surgery and the care team.
Choice D reason:
This statement by the nurse demonstrates the use of evidence-based practice and clinical judgment. The nurse is using an open-ended question to elicit the client's main concerns about the surgery, which shows respect and empathy for the client's feelings. The nurse is also using clinical judgment to assess the client's level of anxiety and knowledge deficit. The nurse is planning to provide information that might help reduce the client's anxiety.
A nurse is applying knowledge, standards, and policies when performing an intervention for a client who has a urinary catheter. Which of the following statements by the nurse reflects this skill?
Explanation
Choice A reason:
This statement does not reflect the application of knowledge, standards, and policies when performing an intervention for a client who has a urinary catheter. Emptying the catheter bag every shift and measuring the output is a routine task that does not require any special skill or knowledge. This statement also does not specify the type of catheter or the reason for its use.
Choice B reason:
This statement reflects the application of knowledge, standards, and policies when performing an intervention for a client who has a urinary catheter. Using aseptic technique when inserting or manipulating the catheter is essential to prevent catheter-associated urinary tract infections (CAUTIs), which are a common and costly complication of indwelling catheters. The nurse demonstrates knowledge of infection prevention and control principles, as well as adherence to evidence-based guidelines and local policies for catheter care.
Choice C reason:
This statement does not reflect the application of knowledge, standards, and policies when performing an intervention for a client who has a urinary catheter. Removing the catheter as soon as possible to prevent infection is a general goal, but not a specific intervention. The nurse should also consider the indications for catheter use, the type of catheter, and the client's condition and preferences before deciding to remove the catheter. The nurse should follow the appropriate protocol for discontinuing the catheter.
Choice D reason:
This statement does not reflect the application of knowledge, standards, and policies when performing an intervention for a client who has a urinary catheter. Monitoring the urine for color, clarity, odor, and sediment is a basic assessment skill that does not require any special knowledge or policy. This statement also does not indicate what actions the nurse would take based on the findings or how they would document them.
A nurse is considering client preferences and values when implementing care for a client who has terminal cancer. Which of the following actions by the nurse demonstrates this skill?
Explanation
Choice A reason:
The nurse asks the client about their goals of care and end-of-life wishes. This action demonstrates the skill of considering client preferences and values because it involves respecting and responding to individual patient's care needs, preferences, and values in all clinical decisions. It also shows that the nurse acknowledges the patient's experiences, stories, and knowledge and engages the patient more in the care process. Asking the client about their goals of care and end-of-life wishes is an example of patient-centered communication, which is fundamental to ensuring optimal health outcomes.
Choice B reason:
The nurse provides palliative care and pain management for the client. This action does not necessarily demonstrate the skill of considering client preferences and values because it does not involve communicating with patients as partners or tailoring, adjusting and balancing overall care. Providing palliative care and pain management is a standard practice for clients who have terminal cancer, but it does not reflect the individualization of care that patient-centered care requires.
Choice C reason:
The nurse respects the client's cultural and spiritual beliefs and practices. This action partially demonstrates the skill of considering client preferences and values because it involves showing concern for the patient as a person and incorporating patient values and preferences in healthcare. However, respecting the client's cultural and spiritual beliefs and practices is not enough to achieve patient-centered care; the nurse also needs to involve the patient in the decision-making process and provide information and education that are relevant to the patient's needs.
Choice D reason:
The nurse involves the client's family and significant others in the care plan. This action partially demonstrates the skill of considering client preferences and values because it involves recognizing the role of family and caregivers in the patient's care. However, involving the client's family and significant others in the care plan is not sufficient to achieve patient-centered care; the nurse also needs to ensure that the patient's voice is heard and address any potential conflicts or disagreements that may arise between the patient and their family or significant others.
Evaluation
A nurse is evaluating the effectiveness of a plan of care for a client with hypertension. Which of the following actions should the nurse take first?
Explanation
Choice A reason:
The nurse should compare the client's blood pressure readings with the expected outcomes to evaluate the effectiveness of the plan of care. This is the first step in the evaluation process, according to the nursing process framework. Comparing the actual outcomes with the expected outcomes allows the nurse to determine if the plan of care was successful or if it needs to be modified.
Choice B reason:
The nurse should identify the factors that influenced the client's blood pressure control, such as medication adherence, lifestyle changes, stress levels, and comorbidities. This is an important step in the evaluation process, but it is not the first one. The nurse should first compare the outcomes before analyzing the factors that affected them.
Choice C reason:
The nurse should document the results of the evaluation in the client's chart to communicate the findings to other members of the health care team and to provide evidence of quality care. This is also an essential step in the evaluation process, but it is not the first one. The nurse should document after comparing and analyzing the outcomes.
Choice D reason:
The nurse should modify the plan of care based on the evaluation findings to improve the client's blood pressure control and prevent complications. This is the final step in the evaluation process, after comparing, analyzing, and documenting the outcomes. The nurse should revise the plan of care as needed to meet the client's changing needs and goals.
A nurse is interpreting and summarizing the findings of an evaluation for a client with chronic obstructive pulmonary disease (COPD). Which of the following statements should the nurse make?
Explanation
Choice A reason:
The client has achieved partial resolution of the problem. This statement is not accurate because it implies that the client's problem is no longer present or significant, which is not the case for COPD. COPD is a chronic and progressive disease that causes irreversible lung damage and airflow limitation. The client may have improved symptoms or reduced exacerbations, but the problem is still present and requires ongoing management.
Choice B reason:
The client has met all the goals and no longer needs nursing care. This statement is not correct because it suggests that the client has fully recovered from COPD, which is not possible. COPD is a lifelong condition that cannot be cured, only managed. The client will always need nursing care to monitor their condition, prevent complications, educate them on self-care, and provide emotional support.
Choice C reason:
The client has not made any progress and requires a different approach. This statement is not valid because it indicates that the client has failed to respond to the current plan of care, which may not be true. COPD is a variable disease that can have periods of stability and exacerbation. The client may have made some progress in achieving their goals, such as improving their gas exchange, airway clearance, breathing pattern, activity tolerance, or quality of life. A different approach may not be necessary unless the client's condition worsens or does not improve despite optimal treatment.
Choice D reason:
The client has shown improvement but needs more time to reach the goals. This statement is the best one to make because it reflects the realistic and positive outcome of the evaluation for a client with COPD. COPD is a complex and chronic disease that requires long-term and individualized care. The client may have shown improvement in some aspects of their condition, such as reducing their dyspnea, cough, or sputum production, increasing their oxygen saturation, or enhancing their exercise capacity. However, they may still need more time to reach their full potential or maintain their progress. The nurse should acknowledge the client's improvement but also encourage them to continue with their plan of care and follow-up. I hope this answer helps you with your question. If you need more information on COPD or nursing care plans, you can check out these.
A nurse is relating outcomes to interventions for a client with heart failure who was discharged from the hospital 2 weeks ago. Which of the following statements should the nurse make?
Explanation
Choice A reason:
This statement is incorrect because it does not relate an outcome to an intervention. The client's weight loss may be due to increased diuretic therapy, but it is not clear how this is an outcome of the nurse's actions. A better statement would be: "The client's weight has decreased by 2 kg since discharge as a result of the nurse's education on diuretic therapy and daily weight monitoring.".
Choice B reason:
This statement is incorrect because it does not relate an outcome to an intervention. The client's dyspnea may be due to noncompliance with fluid restriction, but it is not clear how this is an outcome of the nurse's actions. A better statement would be: "The client's dyspnea has worsened despite the nurse's education on fluid restriction and sodium intake.".
Choice C reason:
This statement is incorrect because it does not relate an outcome to an intervention. The client's edema may have improved due to elevation of the lower extremities, but it is not clear how this is an outcome of the nurse's actions. A better statement would be: "The client's edema has improved as a result of the nurse's instruction on elevating the lower extremities and wearing compression stockings.".
Choice D reason:
This statement is correct because it relates an outcome to an intervention. The client's fatigue may have decreased due to participation in a cardiac rehabilitation program, which is an intervention that the nurse can facilitate or recommend for a client with heart failure. This statement shows that the nurse is evaluating the effectiveness of the intervention and the client's progress.
A nurse is making judgments about problem status for a client with depression who has been receiving psychotherapy and antidepressant medication for 6 weeks. Which of the following statements should the nurse make?
Explanation
Choice A reason:
This choice is incorrect because the problem is not resolved by the client's self-report of feeling happier and more hopeful. The nurse should assess other indicators of improvement, such as mood, affect, cognition, behavior, and functioning. Feeling happier and more hopeful may be a sign of progress, but it does not mean that the problem is completely resolved.
Choice B reason:
This choice is incorrect because the problem is not ongoing if the client has been receiving psychotherapy and antidepressant medication for 6 weeks. The nurse should expect some degree of improvement in the client's symptoms and functioning after this period of treatment. Suicidal thoughts and low self-esteem are serious concerns, but they may not reflect the current problem status of the client.
Choice C reason:
This choice is correct because the problem is improved if the client shows increased interest in social activities and hobbies. These are positive signs of recovery from depression, as they indicate that the client is experiencing more pleasure, motivation, and engagement in life. The nurse should acknowledge and reinforce these improvements, as well as monitor the client's response to treatment.
Choice D reason:
This choice is incorrect because the problem is not potential if the client has already been diagnosed with depression and is receiving treatment. The client is at risk for relapse and adverse effects of medication, but these are not problems that need to be addressed at this stage. The nurse should focus on evaluating the effectiveness of the current treatment plan and providing education and support to the client
A nurse is using evaluative criteria and standards to measure the outcomes of a plan of care for a client with diabetes mellitus. Which of the following are examples of evaluative criteria and standards? (Select all that apply.)
Explanation
Choice A:
The client will demonstrate correct use of a glucometer by discharge. This is not an example of evaluative criteria or standards, but rather an expected outcome. Evaluative criteria or standards are the attributes or measures that are used to determine if the expected outcomes have been met. Expected outcomes are the specific, measurable, and realistic statements of goal attainment that are derived from the nursing diagnoses.
Choice B:
The client will maintain blood glucose levels between 70 and 130 mg/dL. This is an example of evaluative criteria or standards, because it specifies a measurable and objective indicator of the patient's progress toward the goal of managing diabetes mellitus. Blood glucose levels are a common evaluative measure for patients with diabetes mellitus.
Choice C:
The nurse will administer insulin as prescribed and monitor for adverse effects. This is not an example of evaluative criteria or standards, but rather a nursing intervention. Nursing interventions are the actions or treatments that nurses perform to help patients achieve the expected outcomes. Evaluative criteria or standards are not about what the nurse does, but about what the patient achieves.
Choice D:
The client will report increased energy and improved appetite after 2 weeks of treatment. This is an example of evaluative criteria or standards, because it specifies a measurable and subjective indicator of the patient's progress toward the goal of improving quality of life with diabetes mellitus. Patient-reported outcomes are a valid and reliable source of evaluative data.
Choice E:
The nurse will provide education on dietary modifications and physical activity. This is not an example of evaluative criteria or standards, but rather a nursing intervention. Nursing interventions are the actions or treatments that nurses perform to help patients achieve the expected outcomes. Evaluative criteria or standards are not about what the nurse does, but about what the patient achieves.
More questions on the topic
A nurse is conducting an initial assessment for a client who was admitted with pneumonia. Which of the following actions should the nurse take during this phase of the nursing process?
Explanation
Choice A reason:.
Establishing a baseline for planning care and evaluating outcomes is the main purpose of the assessment phase of the nursing process. The assessment phase involves collecting data about the client's health status and needs, which will help the nurse to identify any problems or potential problems that may need to be addressed. The assessment data will also serve as a reference point for comparing the client's progress and outcomes throughout the nursing process.
Choice B reason:.
Identifying the client's response to health concerns or illness is part of the diagnosis phase of the nursing process. The diagnosis phase involves analyzing the data collected during the assessment phase and identifying the client's problems and strengths. The nurse then formulates a nursing diagnosis, which is a statement of the client's actual or potential health problem that can be addressed by nursing interventions.
Choice C reason:.
Providing goal-directed, client-centered care is part of the planning and implementation phases of the nursing process. The planning phase involves setting goals and outcomes for the client and selecting appropriate interventions to achieve them. The goals and outcomes should be specific, measurable, attainable, realistic, and timely (SMART), and they should reflect the client's preferences and values. The implementation phase involves carrying out the interventions and documenting the actions and responses. The interventions should be evidence-based, safe, and effective, and they should involve the client as much as possible.
Choice D reason:.
Comparing the client's data with expected standards or reference ranges is part of the evaluation phase of the nursing process. The evaluation phase involves evaluating the effectiveness of the interventions and modifying the plan as needed. The nurse compares the client's actual outcomes with the expected outcomes and determines whether the goals have been met, partially met, or not met. The nurse also identifies any factors that may have influenced the outcomes, such as client compliance, environmental factors, or unexpected events.
A nurse is conducting a problem-focused assessment for a client who reports nausea and vomiting. Which of the following statements should the nurse make to gather more information about the problem?
Explanation
Choice A reason:
Asking the client when they first noticed the symptoms is a relevant and appropriate question for a problem-focused assessment. It helps the nurse to determine the onset, duration, and frequency of the nausea and vomiting, which can provide clues to the possible causes and severity of the problem.
Choice B reason:
Asking the client about allergies or food intolerances is not directly related to the problem of nausea and vomiting. It might be useful to ask this question later in the assessment, but it is not the priority at this point. This question is more suitable for a comprehensive or initial assessment.
Choice C reason:
Asking the client to rate their pain on a scale of 0 to 10 is not relevant to the problem of nausea and vomiting. Pain is a different symptom that might or might not be associated with nausea and vomiting. This question is more suitable for a pain assessment.
Choice D reason:
Asking the client about their health goals is not related to the problem of nausea and vomiting. This question is more suitable for a wellness assessment or a health promotion intervention.
A nurse is performing an emergency assessment for a client who is experiencing chest pain and shortness of breath. Which of the following questions should the nurse ask the client?
Explanation
Choice A reason:
Asking about family history of heart disease or stroke is not a priority question for a client who is experiencing chest pain and shortness of breath. This question may be relevant for assessing the client's risk factors, but it does not address the immediate problem or help to determine the cause of the symptoms. Therefore, this is not the best choice.
Choice B reason:
Asking how long the client has been feeling this way is a priority question for a client who is experiencing chest pain and shortness of breath. This question helps to determine the onset and duration of the symptoms, which are important factors for diagnosing and treating the client. For example, if the client has been feeling this way for more than 20 minutes, it may indicate a myocardial infarction (heart attack), which requires urgent intervention. Therefore, this is the best choice.
Choice C reason:
Asking about medications or supplements is not a priority question for a client who is experiencing chest pain and shortness of breath. This question may be relevant for assessing the client's medical history and possible drug interactions, but it does not address the immediate problem or help to determine the cause of the symptoms. Therefore, this is not the best choice.
Choice D reason:
Asking what the client was doing when the pain started is not a priority question for a client who is experiencing chest pain and shortness of breath. This question may be relevant for assessing the possible triggers or precipitating factors of the symptoms, but it does not address the immediate problem or help to determine the cause of the symptoms. Therefore, this is not the best choice.
A nurse is documenting the data collected from a comprehensive physical exam of a client. Which of the following data should the nurse identify as objective data?
Explanation
Choice A reason:
The client states that he has trouble sleeping at night. This is subjective data because it is information that the client shares with the nurse spontaneously or in response to a question. Subjective data is based on the client's perception and feelings.
Choice B reason:
The client has a blood pressure of 150/90 mm Hg. This is objective data because it is information that the nurse observes when conducting a physical assessment. Objective data is measurable and observable.
Choice C reason:
The client reports feeling anxious about his diagnosis. This is subjective data because it is information that the client shares with the nurse spontaneously or in response to a question. Subjective data is based on the client's perception and feelings.
Choice D reason:
The client prefers not to discuss his personal issues. This is subjective data because it is information that the client shares with the nurse spontaneously or in response to a question. Subjective data is based on the client's perception and feelings.
A nurse is reviewing the steps of the nursing process with a group of nursing students. Which of the following statements by one of the students indicates an understanding of the evaluation phase?
Explanation
Choice A reason:
It involves determining the effectiveness of nursing interventions. This is the correct definition of the evaluation phase of the nursing process, which is the final step where the nurse compares the actual outcomes with the expected outcomes and modifies the plan of care if needed.
Choice B reason:
It involves establishing priorities and measurable outcomes. This is not the correct definition of the evaluation phase, but rather the planning phase of the nursing process, which is the third step where the nurse identifies client goals and interventions based on the nursing diagnosis.
Choice C reason:
It involves identifying gaps between actual and expected findings. This is not the correct definition of the evaluation phase, but rather a component of it. Identifying gaps between actual and expected findings is one way to determine the effectiveness of nursing interventions, but it is not the only way. The evaluation phase also involves documenting and communicating the results of the evaluation.
Choice D reason:
It involves selecting appropriate evidence-based interventions. This is not the correct definition of the evaluation phase, but rather another component of the planning phase of the nursing process, which is the third step where the nurse identifies client goals and interventions based on the nursing diagnosis.
A nurse is developing a plan of care for a client who has diabetes mellitus. Which of the following actions should the nurse take first?
Explanation
Choice A reason:
Consulting with other members of the health care team is not the first action the nurse should take when developing a plan of care for a client who has diabetes mellitus. While collaboration is important, the nurse should first involve the client in decision making to ensure that the plan of care is individualized, realistic and acceptable to the client.
Choice B reason:
Involve the client in decision making is the correct answer. This is the first action the nurse should take when developing a plan of care for a client who has diabetes mellitus. Involving the client in decision making promotes self-management, adherence and empowerment. The client is the best source of information about their preferences, goals and needs.
Choice C reason:
Reviewing current literature on diabetes management is not the first action the nurse should take when developing a plan of care for a client who has diabetes mellitus. While evidence-based practice is essential, the nurse should first involve the client in decision making to ensure that the plan of care is based on the client's situation and values.
Choice D reason:
Identifying realistic and measurable outcomes is not the first action the nurse should take when developing a plan of care for a client who has diabetes mellitus. While outcome identification is a key step in the nursing process, the nurse should first involve the client in decision making to ensure that the outcomes are relevant and achievable for the client.
A nurse is caring for a patient who has just been admitted to the hospital with chest pain and shortness of breath. The patient has a history of coronary artery disease and hypertension. The nurse obtains vital signs, performs an electrocardiogram (ECG), and administers oxygen therapy as ordered by the physician. What is the next priority action for the nurse?
Explanation
Choice A reason:
Administering nitroglycerin sublingually as ordered is the next priority action for the nurse because nitroglycerin is a medication that relaxes the heart arteries and improves blood flow to the heart muscle, which can relieve chest pain and shortness of breath caused by coronary artery disease. Nitroglycerin can also lower blood pressure, which can help reduce the workload of the heart and prevent further damage to the heart muscle. Nitroglycerin is a fast-acting medication that should be given as soon as possible after chest pain occurs or is suspected.
Choice B reason:
Obtaining a complete health history from the patient is not the next priority action for the nurse because it is not an urgent intervention that can address the patient's immediate needs. A complete health history can provide valuable information about the patient's risk factors, past medical history, medications, allergies, and family history, but it can also take a long time to obtain and may not be feasible if the patient is in pain or distress. A complete health history can be obtained later after the patient's condition is stabilized and more urgent interventions are done.
Choice C reason:
Educating the patient about lifestyle modifications is not the next priority action for the nurse because it is not an acute intervention that can relieve the patient's symptoms or prevent further complications. Lifestyle modifications such as quitting smoking, eating a healthy diet, exercising regularly, managing stress, and controlling blood pressure and cholesterol levels are important for preventing or managing coronary artery disease in the long term, but they do not have an immediate effect on the patient's condition. Educating the patient about lifestyle modifications can be done later after the patient's condition is improved and the patient is ready to learn.
Choice D reason:
Preparing the patient for cardiac catheterization is not the next priority action for the nurse because it is not a definitive intervention that can confirm or rule out coronary artery disease or other causes of chest pain and shortness of breath. Cardiac catheterization is a diagnostic procedure that involves inserting a thin tube into an artery in the groin or arm and advancing it to the heart to inject contrast dye and take X-ray images of the heart and blood vessels. Cardiac catheterization can help identify blockages or narrowing in the coronary arteries that may cause chest pain and shortness of breath, but it also carries some risks such as bleeding, infection, allergic reaction, kidney damage, or heart attack. Cardiac catheterization may be ordered by the physician after other tests such as ECG, blood tests, or.
A nurse is evaluating a patient's response to pain medication after surgery. The patient reports that his pain level is 8 out of 10 on a numeric rating scale, despite receiving morphine 10 mg intravenously 30 minutes ago. What should the nurse do first?
Explanation
Choice A reason:
Assessing the patient's vital signs and oxygen saturation is the first step in evaluating the patient's response to pain medication. This is because vital signs and oxygen saturation can indicate the severity of pain, the effectiveness of the medication, and the presence of any adverse effects such as respiratory depression or hypotension. Assessing vital signs and oxygen saturation is also consistent with the nursing process of assessment, which guides the nurse's subsequent actions.
Choice B reason:
Notifying the physician and requesting a different medication is not the first action that the nurse should take. The nurse should first assess the patient's condition and determine the cause of inadequate pain relief. The physician may not be available or may not agree to change the medication without further information. Changing the medication may also not be necessary or appropriate, depending on the patient's pain level, type of pain, allergies, contraindications, and preferences.
Choice C reason:
Reassessing the patient's pain level in another 15 minutes is not the first action that the nurse should take. The patient is reporting a high level of pain (8 out of 10) despite receiving morphine 10 mg intravenously 30 minutes ago. This indicates that the patient is experiencing breakthrough pain, which is a sudden increase in pain intensity that occurs despite adequate analgesia. Breakthrough pain requires immediate attention and intervention, not delayed reassessment.
Choice D reason:
Providing nonpharmacological interventions such as massage or distraction is not the first action that the nurse should take. Nonpharmacological interventions are complementary methods that can enhance the effect of pharmacological interventions, but they are not sufficient to treat severe acute pain by themselves. The nurse should first assess the patient's condition and administer additional analgesia if indicated and prescribed before implementing nonpharmacological interventions.
A nurse is validating the data collected from an assessment of a client who has hypertension. Which of the following actions should the nurse take?
Explanation
Choice A:
Compare the data with normal standards and ranges. This is a valid action for the nurse to take, because it helps to identify any abnormal findings or deviations from the expected values. For example, the nurse can compare the client's blood pressure, pulse, and temperature with the normal ranges for adults.
Choice B:
Use open-ended questions to clarify the data. This is also a valid action for the nurse to take, because it allows the client to provide more information and elaborate on their responses. Open-ended questions are those that cannot be answered with a simple yes or no, such as "How do you feel about your condition?.”. or "What are your main concerns?.".
Choice C:
Repeat the assessment using a different method or source. This is another valid action for the nurse to take, because it helps to confirm the accuracy and reliability of the data. For example, the nurse can use a different device to measure the blood pressure, ask another health care professional to verify the findings, or check the client's medical records for previous data.
Choice D:
All of the above. This is the correct answer, because all of the actions listed above are appropriate ways for the nurse to validate the data collected from an assessment of a client who has hypertension. Validation is an important step in the assessment process, because it ensures that the data are complete, accurate, and consistent.
A nurse is documenting the data collected from an assessment of a client who has a urinary tract infection (UTI). Which of the following statements should the nurse use to record objective data?
Explanation
Choice A reason:
This statement is not objective data because it is based on what the client states, not what the nurse observes or measures. This is an example of subjective data, which is information that depends on personal feelings.
Choice B reason:
This statement is objective data because it is based on what the nurse observes or measures using a thermometer and a pulse oximeter. This is an example of objective data, which is information that is factual and can be verified.
Choice C reason:
This statement is not objective data because it is based on the nurse's interpretation of the client's appearance and behavior, not on direct observation or measurement. This is an example of subjective data, which is information that represents the patient's perceptions, feelings, or concerns.
Choice D reason:
This statement is not objective data because it is based on what the client reports, not what the nurse observes or measures. This is an example of subjective data, which is information that the patient tells the nurse that cannot be measured or observed.
A nurse is developing a care plan for a client who has impaired mobility due to a stroke. Which of the following actions should the nurse take first when formulating a diagnostic statement?
Explanation
Choice A reason:
Identifying the client's health problems is not the first step in formulating a diagnostic statement. The nurse needs to gather and analyze the assessment data before identifying the health problems.
Choice B reason:
Clustering the assessment data is the first step in formulating a diagnostic statement. The nurse groups related data together to identify patterns and relationships that indicate a human response to health conditions or life processes.
Choice C reason:
Validating the data with the client is not the first step in formulating a diagnostic statement. The nurse needs to cluster the data first and then validate it with the client to ensure accuracy and completeness.
Choice D reason:
Prioritizing the health problems is not the first step in formulating a diagnostic statement. The nurse needs to cluster the data first and then identify the health problems before prioritizing them.
A nurse is preparing a diagnostic statement for a client who has chronic obstructive pulmonary disease (COPD) and reports shortness of breath and fatigue with minimal exertion. Which of the following formats should the nurse use to write the statement?
Explanation
Choice A reason:
The PES format (problem, etiology, signs and symptoms) is the most comprehensive and accurate way to write a nursing diagnostic statement. It identifies the nursing problem, the cause or contributing factors, and the evidence or manifestations of the problem. For example, a possible PES statement for the client with COPD and shortness of breath and fatigue with minimal exertion is: Ineffective breathing pattern related to chronic airway obstruction as evidenced by dyspnea, tachypnea, and use of accessory muscles.
Choice B reason:
The PE format (problem, etiology) is a two-part diagnostic statement that omits the signs and symptoms of the problem. It is less specific and does not provide enough information to guide the nursing interventions and outcomes. For example, a possible PE statement for the client with COPD and shortness of breath and fatigue with minimal exertion is: Ineffective breathing pattern related to chronic airway obstruction. This statement does not indicate how the problem is manifested or measured.
Choice C reason:
The PS format (problem, signs and symptoms) is a two-part diagnostic statement that omits the etiology or cause of the problem. It is less precise and does not identify the factors that contribute to or influence the problem. For example, a possible PS statement for the client with COPD and shortness of breath and fatigue with minimal exertion is: Ineffective breathing pattern as evidenced by dyspnea, tachypnea, and use of accessory muscles. This statement does not indicate why the problem exists or what can be done to address it.
Choice D reason:
The ES format (etiology, signs and symptoms) is a two-part diagnostic statement that omits the problem or nursing diagnosis. It is incomplete and does not state what the actual or potential health issue is. For example, a possible ES statement for the client with COPD and shortness of breath and fatigue with minimal exertion is: Chronic airway obstruction as evidenced by dyspnea, tachypnea, and use of accessory muscles. This statement does not indicate what the nursing problem is or what the desired outcome is.
Which of these is an example of a goal rather than an outcome?
Explanation
Choice A reason:
The client will ambulate 50 feet with a walker by day 3. This is an example of a goal rather than an outcome because it is a specific action that the client intends to achieve within a certain time frame. It is also a process goal because it is a step or sub-goal towards a more significant and overarching goal, such as improving mobility or preventing complications. Process goals are more controllable and measurable than outcome goals.
Choice B reason:
The client will maintain fluid balance as evidenced by stable weight and urine output. This is an example of an outcome rather than a goal because it is the overarching result that the client intends to achieve. It is also an outcome goal because it enables the client to assess their present and intended performance results while developing an outline that guides the steps to realize it. Outcome goals are more general and less controllable than process goals.
Choice C reason:
The client will have improved gas exchange as indicated by oxygen saturation above 92%. This is an example of an outcome rather than a goal because it is the overarching result that the client intends to achieve. It is also an outcome goal because it enables the client to assess their present and intended performance results while developing an outline that guides the steps to realize it. Outcome goals are more general and less controllable than process goals.
Choice D reason:
The client will have normal bowel function. This is an example of an outcome rather than a goal because it is the overarching result that the client intends to achieve. It is also an outcome goal because it enables the client to assess their present and intended performance results while developing an outline that guides the steps to realize it. Outcome goals are more general and less controllable than process goals.
Which type of intervention requires a health care provider's order?
Explanation
Choice A reason:
Independent nursing interventions are actions that nurses can perform by themselves, without any management from a doctor or another discipline. For example, checking vital signs, repositioning a patient, or providing patient education are independent nursing interventions. These interventions do not require a health care provider's order.
Choice B reason:
Dependent nursing interventions are actions that nurses perform under the direction of a physician or as part of a care plan. For example, administering medications, performing diagnostic tests, or inserting an intravenous line are dependent nursing interventions. These interventions require a health care provider's order.
Choice C reason:
Collaborative nursing interventions are actions that nurses perform in coordination with other health care professionals, such as physicians, pharmacists, dietitians, or physical therapists. For example, developing a discharge plan, implementing a wound care protocol, or providing nutritional counseling are collaborative nursing interventions. These interventions may or may not require a health care provider's order, depending on the situation and the scope of practice of the nurse.
Choice D reason:
Evaluative nursing interventions are not a type of intervention, but rather a step in the nursing process. Evaluative nursing interventions are actions that nurses take to assess the outcomes of their care and the effectiveness of their interventions. For example, measuring pain levels, monitoring wound healing, or evaluating patient satisfaction are evaluative nursing interventions. These interventions do not require a health care provider's order.
A nurse is using appropriate resources and equipment when implementing care for a client who has impaired mobility due to a stroke. Which of the following actions by the nurse demonstrates this skill?
Explanation
Choice A reason:
The nurse uses a mechanical lift to transfer the client from bed to chair. This is the correct answer because it demonstrates the use of appropriate resources and equipment to prevent injury to the client and the nurse, and to facilitate safe mobility for the client who has impaired mobility due to a stroke. A mechanical lift is a device that helps lift and move a person who cannot move on their own or with minimal assistance.
Choice B reason:
The nurse performs passive range of motion exercises for the affected limbs. This is not the correct answer because it does not demonstrate the use of appropriate resources and equipment, but rather a nursing intervention that helps maintain joint mobility, prevent contractures, and improve circulation for the client who has impaired mobility due to a stroke. Passive range of motion exercises are movements that are done by someone else for a person who cannot move their own limbs.
Choice C reason:.
The nurse encourages the client to participate in physical therapy sessions. This is not the correct answer because it does not demonstrate the use of appropriate resources and equipment, but rather a nursing intervention that helps promote recovery, prevent complications, and improve function for the client who has impaired mobility due to a stroke. Physical therapy is a type of rehabilitation that involves exercises and activities that help improve strength, balance, coordination, and mobility.
Choice D reason:
The nurse applies antiembolic stockings and sequential compression devices to the lower extremities. This is not the correct answer because it does not demonstrate the use of appropriate resources and equipment, but rather a nursing intervention that helps prevent deep vein thrombosis (DVT), a potential complication of stroke that occurs when a blood clot forms in a vein deep in the body. Antiembolic stockings are tight-fitting elastic socks that apply pressure to the legs and feet to improve blood flow and prevent clotting. Sequential compression devices are inflatable sleeves that wrap around the legs and inflate and deflate periodically to squeeze the veins and improve blood flow.
A nurse is collaborating and communicating with other health care providers when implementing care for a client who has chronic heart failure. Which of the following actions by the nurse demonstrates this skill?
Explanation
Choice A reason:
The nurse reports any changes in the client's vital signs, weight, or fluid status to the primary provider. This action demonstrates the skill of collaborating and communicating with other health care providers because it involves sharing relevant and timely information about the client's condition and needs with the primary provider, who can then make appropriate decisions or adjustments to the plan of care. Reporting changes in vital signs, weight, or fluid status is especially important for a client who has chronic heart failure, as these indicators can reflect worsening or improving cardiac function. Reporting changes also follows the ISBARR format of communication, which is a standardized method of exchanging patient information between health care team members.
Choice B reason:
The nurse administers prescribed medications, such as diuretics, beta blockers, and ACE inhibitors. This action does not demonstrate the skill of collaborating and communicating with other health care providers because it is a routine nursing task that does not involve direct interaction or exchange of information with other health care team members. Administering medications is part of the nurse's scope of practice and responsibility, and does not require collaboration or communication with other providers, unless there are questions, concerns, or issues regarding the medication orders.
Choice C reason:
The nurse educates the client about lifestyle modifications, such as sodium restriction, exercise, and smoking cessation. This action does not demonstrate the skill of collaborating and communicating with other health care providers because it is a nursing intervention that focuses on the client's education and self-management, not on the interaction or exchange of information with other health care team members. Educating the client about lifestyle modifications is part of the nurse's role in promoting health and preventing complications, and does not require collaboration or communication with other providers, unless there are discrepancies or inconsistencies in the education materials or messages.
Choice D reason:.
The nurse assesses the client's cardiac function, such as heart sounds, rhythm, and peripheral pulses. This action does not demonstrate the skill of collaborating and communicating with other health care providers because it is a nursing assessment that does not involve direct interaction or exchange of information with other health care team members. Assessing the client's cardiac function is part of the nurse's role in monitoring and evaluating the client's response to treatment, and does not require collaboration or communication with other providers, unless there are abnormal findings that need to be reported or documented.
A nurse is recognizing errors or omissions in a plan of care for a client with chronic kidney disease who is on hemodialysis. Which of the following actions should the nurse take?
Explanation
Choice A reason:
Reporting the errors or omissions to the quality improvement committee is not the best action to take because it does not address the immediate needs of the client or correct the plan of care. Quality improvement committees are responsible for monitoring and evaluating the quality of care and services provided by the health care organization, but they are not directly involved in the care of individual clients. Reporting the errors or omissions to the committee may be appropriate after discussing and revising the plan of care with the health care team, but it is not the first or most important action to take.
Choice B reason:
Discussing the errors or omissions with the health care team and revising the plan of care accordingly is the best action to take because it ensures that the client receives safe and effective care that meets their needs and preferences. Errors or omissions in a plan of care are failures to do the right thing that may cause harm or poor outcomes for the client Examples of errors or omissions in a plan of care include failing to order necessary tests, procedures, medications, or consultations; failing to document or communicate important information; failing to monitor or evaluate the client's condition or response to treatment; or failing to follow evidence-based guidelines or standards of care Discussing the errors or omissions with the health care team allows for identifying and correcting the causes of the errors or omissions, such as lack of knowledge, skills, resources, communication, coordination, or supervision. Revising the plan of care accordingly allows for updating and modifying the goals, interventions, and outcomes based on the client's current status and needs.
Choice C reason:
Ignoring the errors or omissions as they are not significant enough to affect outcomes is not a good action to take because it violates the ethical principles of beneficence and nonmaleficence, which require nurses to do good and avoid harm for their clients Ignoring the errors or omissions may also lead to legal consequences, such as negligence or malpractice claims, if the client suffers harm or injury as a result of the errors or omissions Furthermore, ignoring the errors or omissions does not contribute to improving the quality and safety of care or preventing future errors or omissions from occurring.
Choice D reason:
Documenting the errors or omissions in an incident report and filing it in the client's chart is not a good action to take because it does not correct the errors or omissions or revise the plan of care. Incident reports are tools for documenting and analyzing adverse events or near misses that occur in health care settings, such as medication errors, falls, infections, or equipment failures Incident reports are not part of the client's medical record and should not be filed in their chart. They are confidential documents that are used for quality improvement purposes, such as identifying system failures, implementing corrective actions,.
A nurse is performing an ongoing assessment for a client who has a pressure ulcer. Which of the following data should the nurse collect? (Select all that apply).
Explanation
Choice A reason:
The size and depth of the ulcer are important indicators of the severity and healing progress of the wound. The nurse should measure the length, width, and depth of the ulcer using a ruler or a probe and document the findings. The nurse should also note the presence of any undermining or tunneling in the wound bed.
Choice B reason:
The presence of drainage or odor can signal infection or necrosis in the wound. The nurse should assess the amount, color, consistency, and odor of the drainage and document the findings. The nurse should also culture the wound if indicated and initiate appropriate wound care interventions.
Choice C reason:
The type and amount of pain medication administered are not directly related to the assessment of the pressure ulcer. Pain is a subjective experience that varies among individuals and situations. The nurse should assess the client's pain level using a valid pain scale and administer analgesics as prescribed, but this is not part of the ongoing assessment of the wound itself.
Choice D reason:
The client's nutritional status and intake are vital factors that affect wound healing. The nurse should assess the client's weight, body mass index, serum albumin, prealbumin, and transferrin levels, and dietary intake of protein, calories, vitamins, minerals, and fluids. The nurse should also provide nutritional supplements or consult a dietitian as needed to optimize the client's nutritional status.
Choice E reason:
The client's level of mobility and activity are also important factors that influence wound healing. The nurse should assess the client's ability to move, reposition, and ambulate independently or with assistance. The nurse should also implement measures to reduce pressure, shear, and friction on the wound site, such as using pressure-relieving devices, turning and repositioning the client frequently, and providing skin care.
A nurse is using critical thinking skills to analyze data during the assessment phase of the nursing process. Which of the following actions should the nurse take?(Select all that apply).
Explanation
Choice A reason:
Comparing data with normal values and standards is an important action for the nurse to take during the assessment phase of the nursing process. This helps the nurse to identify any deviations from normal and potential problems that need further investigation or intervention.
Choice B reason:
Organizing data into clusters that have similar underlying causes is another action that the nurse should take during the assessment phase. This helps the nurse to recognize patterns and relationships among the data and to formulate nursing diagnoses.
Choice C reason:
Validating data by using multiple sources of information is also an action that the nurse should take during the assessment phase. This helps the nurse to ensure that the data are accurate, complete, and factual, and to avoid making assumptions or errors.
Choice D reason:
Documenting data using standardized terminology and abbreviations is not an action that the nurse should take during the assessment phase of the nursing process. Although documentation is an essential part of nursing practice, it is not specific to the assessment phase. Moreover, standardized terminology and abbreviations are not always appropriate or clear for documenting data.
Choice E reason:
Prioritizing data according to urgency and importance is another action that the nurse should take during the assessment phase of the nursing process. This helps the nurse to focus on the most relevant and significant data and to plan for further assessment or intervention based on the patient's needs and priorities.
A nurse is planning care for a patient who has chronic obstructive pulmonary disease (COPD) and is experiencing dyspnea at rest. Which of the following interventions should be included in the plan of care?(Select all that apply.).
Explanation
Choice A:
Positioning the patient in high Fowler's position. This is a correct intervention because it allows for optimal chest expansion and lung ventilation, reducing dyspnea and work of breathing.
Choice B:
Encouraging deep breathing and coughing exercises. This is an incorrect intervention because it may increase dyspnea and fatigue in a patient with COPD who already has difficulty breathing. Instead, the nurse should teach pursed-lip breathing and diaphragmatic breathing techniques to improve gas exchange and reduce air trapping.
Choice C:
Administering bronchodilators and corticosteroids as ordered. This is a correct intervention because these medications help to relax the smooth muscles of the airways, reduce inflammation, and improve airflow in a patient with COPD.
Choice D:
Providing supplemental oxygen via nasal cannula as ordered. This is a correct intervention because oxygen therapy helps to correct hypoxemia, reduce pulmonary hypertension, and improve exercise tolerance and quality of life in a patient with COPD. The nurse should monitor the oxygen saturation and adjust the flow rate according to the prescription and the patient's response.
Choice E:
Restricting fluid intake to prevent fluid overload. This is an incorrect intervention because fluid restriction is not indicated for a patient with COPD unless there is evidence of heart failure or renal impairment. Adequate hydration helps to thin the secretions and facilitate expectoration in a patient with COPD. The nurse should encourage oral fluids unless contraindicated and monitor the fluid balance and electrolytes of the patient.
A nurse is conducting an assessment on a client who has multiple sclerosis (MS). Which of the following data should the nurse collect? (Select all that apply.).
Explanation
Choice A reason:
The client's level of fatigue and weakness is an important data to collect because fatigue is one of the most common and disabling symptoms of MS, affecting about 80% of people with the condition. Fatigue can interfere with the client's daily activities, quality of life, and ability to cope with other symptoms. Weakness is also a common symptom of MS, caused by damage to the nerve fibers that control muscle movements. Weakness can affect the client's mobility, balance, and coordination.
Choice B reason:
The client's cognitive and emotional status is another important data to collect because MS can affect the brain and spinal cord, leading to cognitive impairment in about 50% of people with MS. Cognitive impairment can affect the client's memory, attention, concentration, problem-solving, and decision-making skills. MS can also cause emotional changes, such as depression, anxiety, mood swings, irritability, and euphoria. Emotional changes can affect the client's coping skills, social relationships, and self-esteem.
Choice C reason:
The client's family history and genetic risk factors is not an important data to collect because MS is not a hereditary disease. Although genetic factors may play a role in increasing the susceptibility to MS, they are not sufficient to cause the disease by themselves. MS is thought to be caused by a combination of genetic and environmental factors that trigger an autoimmune response in the central nervous system. Therefore, knowing the client's family history and genetic risk factors will not help in diagnosing or managing MS.
Choice D reason:
The client's vision and hearing acuity is an important data to collect because MS can affect the optic nerve and cause visual disturbances, such as blurred vision, double vision, loss of color vision, pain in the eye, or temporary blindness. Visual disturbances are often the first symptom of MS and can recur or worsen over time. MS can also affect the auditory nerve and cause hearing problems, such as hearing loss, tinnitus, or vertigo. Hearing problems are less common than visual problems in MS but can still affect the client's communication and quality of life.
Choice E reason:
The client's mobility and coordination skills is an important data to collect because MS can damage the nerve fibers that control muscle movements and cause spasticity, tremors, ataxia, dysmetria, or dysdiadochokinesia. These symptoms can affect the client's mobility and coordination skills and increase the risk of falls, injuries, or disability. Assessing the client's mobility and coordination skills can help in planning interventions to improve function, safety, and independence.
A nurse is conducting a health promotion workshop for a group of clients who want to improve their physical activity levels. Which of the following questions should the nurse ask to assess their readiness for enhanced fitness?(Select all that apply.).
Explanation
Choice A reason:
Asking about the clients' current exercise habits helps the nurse to assess their baseline physical activity levels, their preferences, their strengths, and their areas for improvement. This information can help the nurse to tailor the health promotion interventions to the clients' needs and goals.
Choice B reason:
Asking about the benefits of regular physical activity helps the nurse to evaluate the clients' knowledge and awareness of the positive effects of exercise on their health and well-being. This information can help the nurse to reinforce the clients' motivation and provide education as needed.
Choice C reason:
Asking about the barriers to increasing physical activity helps the nurse to identify the factors that may prevent or hinder the clients from engaging in exercise. These factors may include lack of time, resources, support, or confidence. This information can help the nurse to address the clients' concerns and challenges and help them find solutions.
Choice D reason:
Asking about the strategies to overcome the barriers helps the nurse to empower the clients to take action and make changes in their behavior. The nurse can help the clients to develop realistic and specific plans that suit their abilities and preferences. The nurse can also provide support and encouragement along the way.
Choice E reason:
Asking about the potential complications of physical inactivity is not a relevant question to assess the clients' readiness for enhanced fitness. This question may be appropriate for secondary or tertiary prevention, but not for primary prevention. Primary prevention focuses on promoting health and preventing disease or injury, not on treating or rehabilitating existing problems.
Which of these are characteristics of a well-written outcome?(Select all that apply.)
Explanation
Choice A reason:
A well-written outcome should be specific, meaning it should clearly state what is expected to be achieved, by whom, and under what conditions. A specific outcome helps to focus the actions and resources needed to accomplish it. For example, an outcome that states "Students will improve their writing skills”. is too vague and does not specify how the improvement will be measured or what level of improvement is expected. A more specific outcome would be "Students will demonstrate an increase in their average writing score by 10% on the final exam.".
Choice B reason:
A well-written outcome should also be measurable, meaning it should have a quantifiable indicator that can be used to assess the progress and achievement of the outcome. A measurable outcome helps to determine whether the outcome has been met or not, and to what extent. For example, an outcome that states "Students will enjoy the course”. is not measurable because it does not have a clear criterion for evaluating the students' satisfaction. A more measurable outcome would be "At least 80% of the students will rate the course as satisfactory or higher on the course evaluation survey.".
Choice C reason:
Another characteristic of a well-written outcome is that it should be realistic, meaning it should be achievable within the given time frame, resources, and constraints. A realistic outcome helps to set reasonable expectations and avoid frustration or disappointment. For example, an outcome that states "Students will master all the topics covered in the course”. is not realistic because it is too ambitious and unrealistic for a single course. A more realistic outcome would be "Students will demonstrate proficiency in at least 75% of the topics covered in the course.".
Choice D reason:
Finally, a well-written outcome should be time-bound, meaning it should have a specific deadline or target date for completion. A time-bound outcome helps to create a sense of urgency and motivation, and to monitor the progress and results of the outcome. For example, an outcome that states "Students will apply their knowledge to real-world problems”. is not time-bound because it does not indicate when or how often the students will do so. A more time-bound outcome would be "By the end of the semester, students will complete at least two projects that require them to apply their knowledge to real-world problems.".
Choice E reason:
A well-written outcome should not be broad, meaning it should not be too general or vague that it does not provide any guidance or direction for action. A broad outcome makes it difficult to plan, implement, and evaluate the outcome. For example,.
A nurse is reassessing a client before performing an intervention for a client who has hypertension. Which of the following are essential components of this skill? (Select all that apply.).
Explanation
Choice A reason:
The nurse checks the client's identification bracelet and verifies allergies. This is an essential component of this skill because it ensures that the nurse is performing the intervention for the right client and avoids any potential adverse reactions or interactions due to allergies.
Choice B reason:
The nurse measures the client's blood pressure in both arms and compares with previous readings. This is not an essential component of this skill because it is not directly related to the intervention for hypertension. It is a part of the assessment process that should be done before planning the intervention.
Choice C reason:
The nurse asks the client if they have taken any over-the-counter medications or herbal supplements. This is an essential component of this skill because it helps the nurse to identify any possible factors that may affect the client's blood pressure or the effectiveness of the intervention. Some medications or supplements may interact with the prescribed drugs or alter the blood pressure level.
Choice D reason:
The nurse reviews the most current evidence and guidelines for hypertension management. This is not an essential component of this skill because it is not specific to the client's situation or needs. It is a part of the planning process that should be done before implementing the intervention.
Choice E reason:
The nurse explains the purpose, procedure, and potential side effects of the intervention to the client. This is an essential component of this skill because it respects the client's autonomy and informed consent. It also helps the client to understand what to expect and how to cope with any possible complications or discomforts.
A nurse is documenting the results of an evaluation in a client's chart. Which of the following information should the nurse include? (Select all that apply.).
Explanation
Choice A reason:
The date and time of the evaluation are essential to document because they provide a reference point for the progress of the patient and the effectiveness of the nursing interventions. They also help to establish a timeline of events and facilitate communication among the health care team.
Choice B reason:
The methods used to measure outcomes are important to document because they show how the nurse assessed the patient's condition and whether the expected outcomes were met, partially met, or not met. They also provide evidence of the quality and consistency of care provided by the nurse.
Choice C reason:
The revisions made to the plan of care are necessary to document because they reflect the changes in the patient's status and needs, as well as the nurse's clinical judgment and decision making. They also demonstrate the ongoing evaluation and adaptation of the nursing care plan to achieve optimal outcomes for the patient.
Choice D reason:
The rationale for choosing interventions is not required to document because it is part of the planning phase of the nursing process, not the evaluation phase. The rationale for choosing interventions should be based on evidence-based practice, standards of care, and clinical guidelines, which are already established and available for reference.
Choice E reason:
The comparison of outcomes with goals is essential to document because it shows whether the nursing care plan was effective in addressing the patient's problems and improving the patient's condition. It also helps to identify areas of improvement, gaps in care, and opportunities for learning and feedback.
A nurse is identifying factors that contribute to success or failure of a plan of care for a client with anxiety disorder who is undergoing cognitive behavioral therapy (CBT). Which of the following factors should the nurse consider? (Select all that apply.).
Explanation
Choice A reason:
The client's readiness and motivation to change are crucial factors for the success of CBT, as it requires active participation and homework assignments from the client. CBT is based on the premise that changing maladaptive thoughts and behaviors can improve emotional well-being. Therefore, the client needs to be willing and able to engage in this process and apply the learned skills to their daily life.
Choice B reason:
The availability and accessibility of CBT services are also important factors for the success of CBT, as they determine how often and how easily the client can receive the therapy. CBT is typically delivered in a time-limited and structured manner, with sessions ranging from 8 to 20 weeks. The client needs to have regular access to a qualified CBT therapist who can provide consistent and evidence-based treatment.
Choice C reason:
The cost and duration of CBT sessions are not relevant factors for the success of CBT, as they do not directly affect the quality or effectiveness of the therapy. CBT is generally considered to be a cost-effective and efficient intervention for anxiety disorders, as it can produce lasting benefits in a relatively short period of time. The cost and duration of CBT sessions may affect the client's preference or adherence to the therapy, but they are not essential for its outcome.
Choice D reason:
The compatibility and rapport between the client and therapist are vital factors for the success of CBT, as they influence the therapeutic alliance and the client's trust in the therapist. CBT is a collaborative and goal-oriented therapy that requires a strong working relationship between the client and therapist. The client needs to feel comfortable and supported by the therapist, who can provide empathy, feedback, guidance, and encouragement.
Choice E reason:
The evidence base and efficacy of CBT for anxiety disorders are significant factors for the success of CBT, as they demonstrate the validity and reliability of the therapy. CBT is one of the most researched and empirically supported psychological interventions for anxiety disorders, with numerous studies showing its superiority over other treatments or placebo. The client can benefit from knowing that CBT is based on sound scientific principles and proven techniques.
Exams on Critical Thinking and Nursing Process
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
- Define critical thinking and its components
- Explain the importance of critical thinking for nurses
- Identify the different kinds of nursing knowledge
- Describe the phases of the nursing process and their activities
- Apply critical thinking skills to nursing practice
Introduction
Critical thinking is a combination of reasoned thinking, openness to alternatives, the ability to reflect, and a desire to seek truth.
It is the art of thinking about what you are doing, while you are doing it. Critical thinking is essential for nurses because they face complex situations, unique clients, and the need to provide holistic care.
Critical thinking helps nurses to use a systematic problem-solving process that guides all nursing actions. This process is called the nursing process.
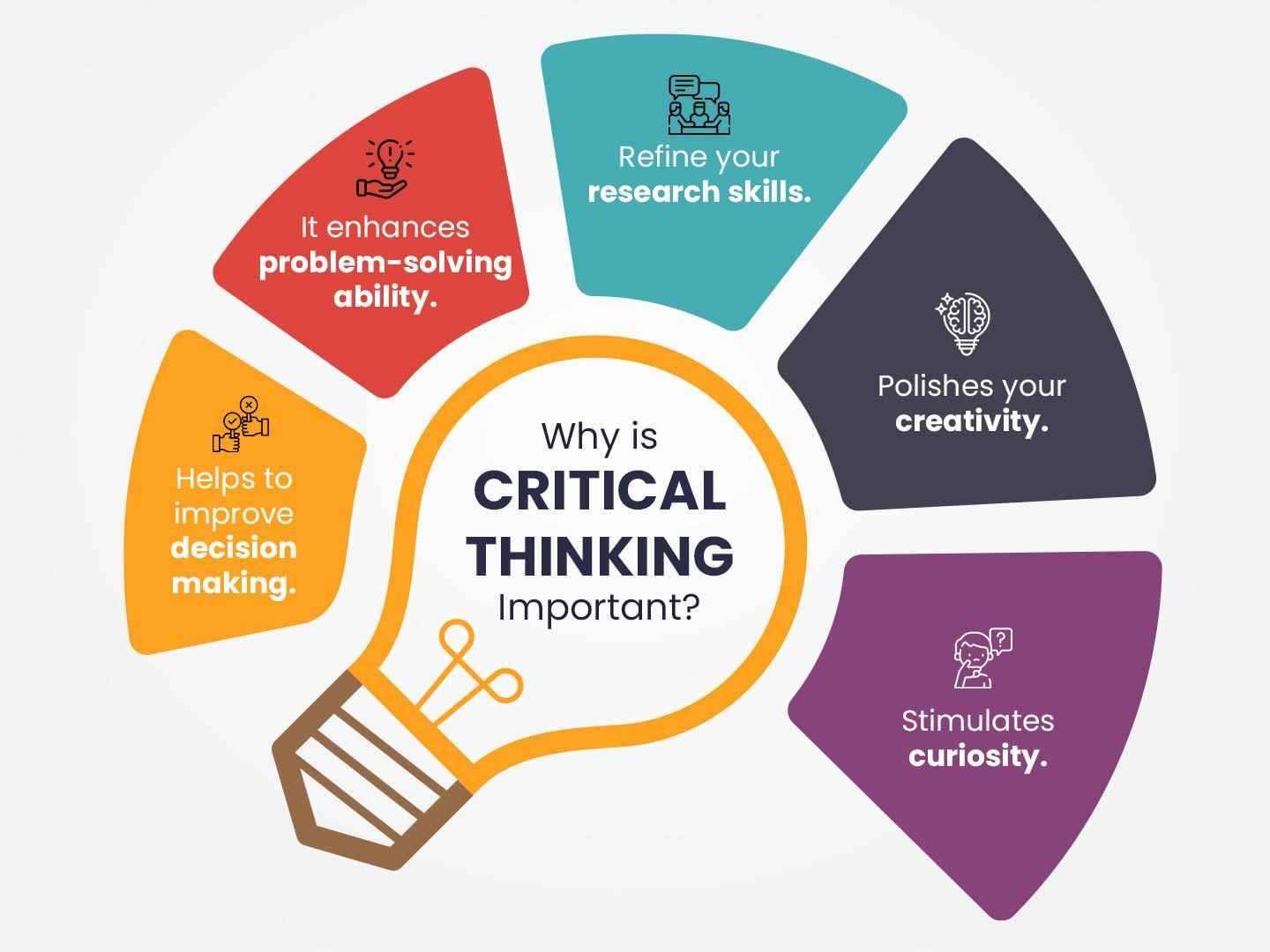
Critical Thinking
Critical thinking is essential for nurses because it helps them make sound clinical judgments, solve problems, and provide safe and effective care to patients.
Critical thinking is the ability to actively and skillfully conceptualize, analyze, synthesize, and evaluate information. It involves a combination of knowledge, experience, and intuition. The components of critical thinking include:
-
Reflection: Deliberate thinking about one's own actions and experiences.
-
Analysis: Breaking down complex situations into smaller parts to understand their relationships.
-
Inference: Drawing logical conclusions based on available evidence.
-
Evaluation: Assessing the credibility and relevance of information.
-
Explanation: Clearly communicating one's thoughts and reasoning.
-
Self-regulation: Monitoring and adjusting one's thinking process to improve outcomes.
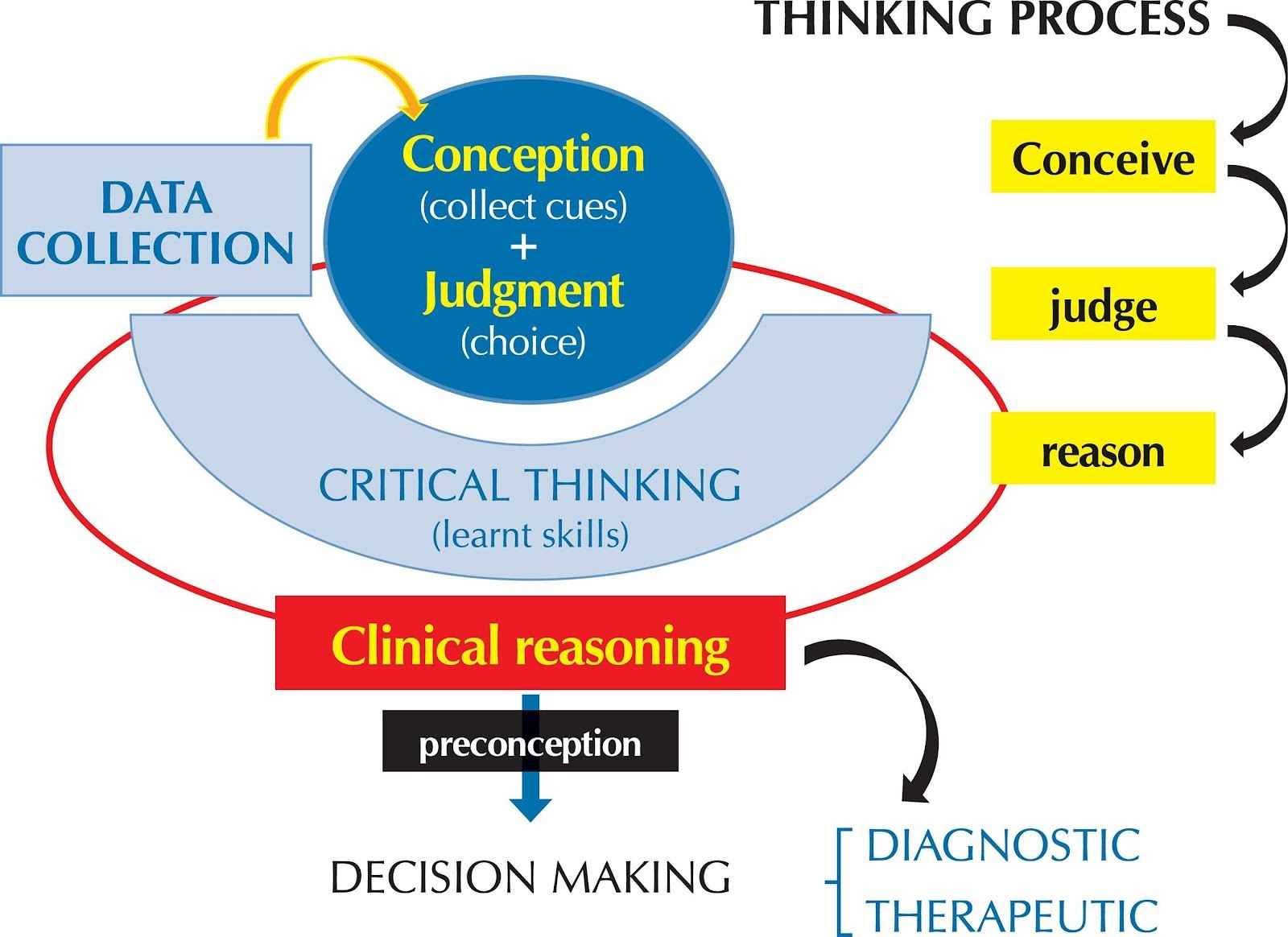
Importance of Critical Thinking for Nurses
Critical thinking is crucial for nurses as it allows them to:
-
Make accurate clinical judgments and decisions.
-
Identify potential complications and take preventive measures.
-
Prioritize patient care based on individual needs and acuity.
-
Collaborate effectively with the healthcare team.
-
Continuously improve the quality of care provided.
-
Adapt to changing situations and handle emergencies efficiently.
The Nursing Process
The nursing process is a cyclical and dynamic process that consists of five phases: assessment, diagnosis, planning, implementation, and evaluation.
The purpose of the nursing process is to help the nurse provide goal-directed, client-centered care.
The nursing process is guided by the ANA scope of practice.
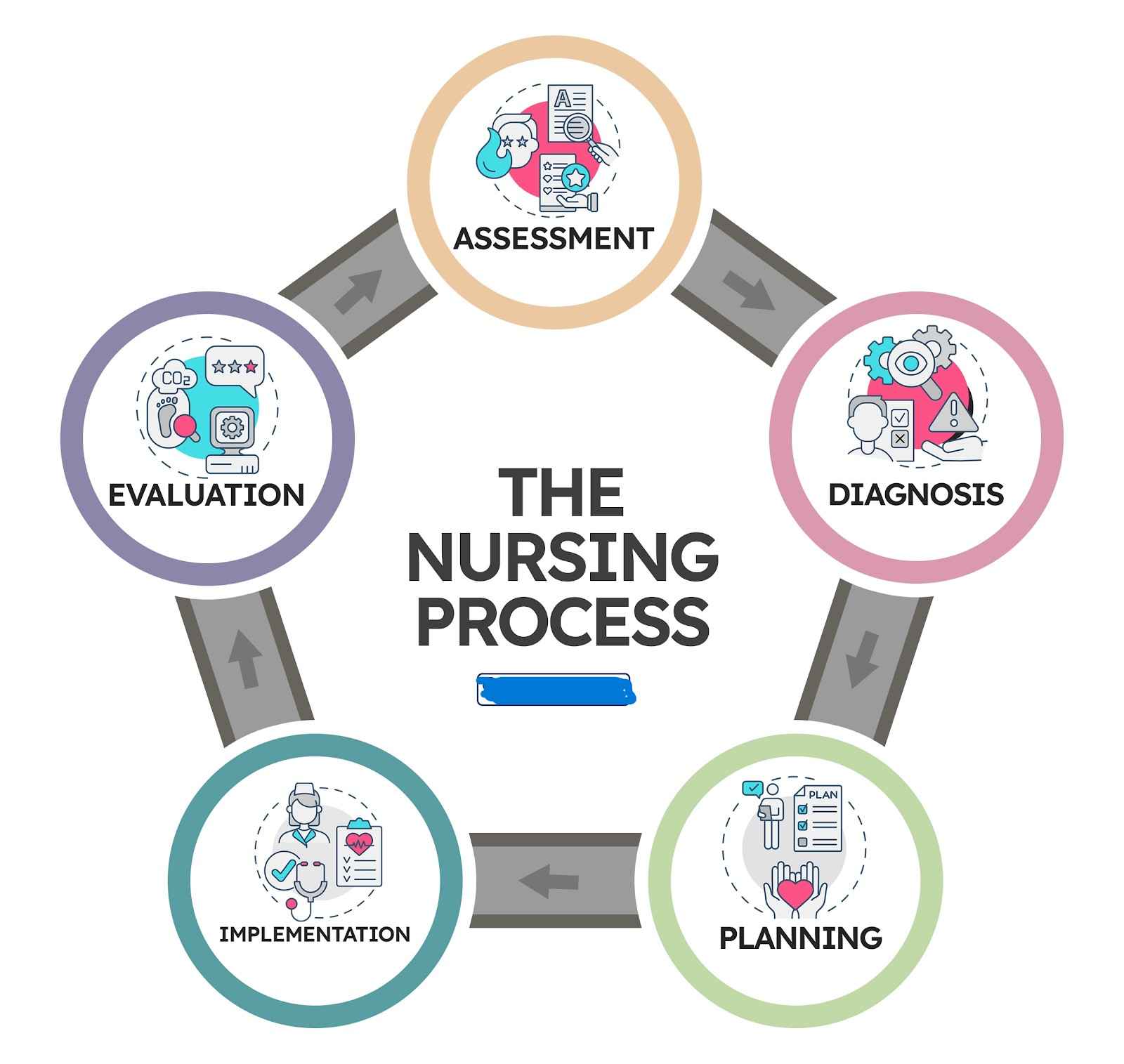
Assessment
Assessment is the first phase of the nursing process. It involves collecting data, organizing data, validating data, and documenting data about the client’s response to health concerns or illness. The goal of assessment is to establish a baseline for planning care and evaluating outcomes.
There are different types of assessments, such as:
-
Initial assessment: performed within 24 hours of admission to collect comprehensive information to complete the database.
-
Ongoing assessment: performed every shift to compare with the initial assessment and identify changes.
-
Problem-focused assessment: performed when a specific problem is identified to gather more information about it.
-
Emergency assessment: performed during a crisis to identify life-threatening problems.
Assessment can be systematic (head-to-toe) or continuous (every time the nurse comes into contact with the client).
Diagnosis
Diagnosis is the second phase of the nursing process. It involves analyzing data, identifying health problems, risks, and strengths, and formulating diagnostic statements.
The goal of diagnosis is to identify the client’s actual or potential health needs that can be addressed by nursing interventions.
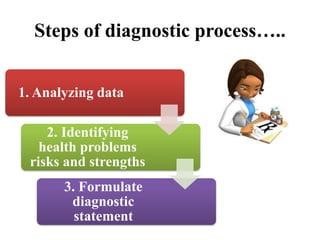
There are different types of diagnoses, such as:
-
Actual diagnosis: describes a problem that is present at the time of assessment.
-
Risk diagnosis: describes a problem that is likely to develop if interventions are not implemented.
-
Health promotion diagnosis: describes a desire or readiness to enhance well-being.
A diagnostic statement consists of three parts: the problem (nursing diagnosis), the etiology (related factors), and the signs and symptoms (defining characteristics). For example:
-
Acute pain related to tissue injury as evidenced by verbal report of 8/10 pain, grimacing, guarding, and elevated blood pressure.
-
Risk for infection related to surgical incision.
-
Readiness for enhanced nutrition as evidenced by verbalization of interest in healthy eating.
Planning
Planning is the third phase of the nursing process. It involves prioritizing problems, formulating goals and outcomes, selecting interventions, and documenting the plan of care. The goal of planning is to develop an individualized plan that will achieve the desired outcomes for the client.
There are different types of planning, such as:
-
Initial planning: performed by the nurse who performs the admission assessment and develops the initial comprehensive plan of care.
-
Ongoing planning: performed by all nurses who work with the client to update and modify the plan as needed.
-
Discharge planning: performed by all nurses who work with the client to anticipate and plan for the client’s needs after discharge.
A goal is a broad statement that describes a desired change in the client’s condition or behavior. An outcome is a specific, measurable, realistic, and time-bound statement that describes how the goal will be achieved. For example:
-
Goal: The client will have adequate pain relief.
-
Outcome: The client will report pain level of 3/10 or less within 30 minutes after receiving analgesics.
An intervention is an action performed by the nurse or delegated to another health care provider that helps the client achieve a specific outcome. Interventions can be independent (nurse-initiated), dependent (physician-initiated), or collaborative (interprofessional). For example:
-
Independent intervention: Assess pain level and location every 2 hours.
-
Dependent intervention: Administer morphine sulfate 2 mg IV as ordered for pain level of 7/10 or higher.
-
Collaborative intervention: Consult with physical therapist for pain management techniques.
Implementation
Implementation is the fourth phase of the nursing process. It involves performing interventions, recording actions and client responses, and reporting and documenting relevant information. The goal of implementation is to assist the client to meet desired outcomes and promote wellness.
There are different types of implementation, such as:
-
Direct care: involves interaction with the client, such as physical care, emotional support, patient teaching, etc.
-
Indirect care: involves activities performed away from the client, such as communication, documentation, infection control, etc.
Implementation requires critical thinking skills, such as:
-
Reassessing the client before performing an intervention
-
Reviewing the plan of care and modifying it if needed
-
Applying knowledge, standards, and policies
-
Using evidence-based practices and clinical judgment
-
Collaborating and communicating with other health care providers
-
Considering client preferences and values
-
Using appropriate resources and equipment
Evaluation
Evaluation is the fifth and final phase of the nursing process. It involves measuring outcomes, comparing outcomes with goals, drawing conclusions, modifying the plan of care, and documenting results. The goal of evaluation is to determine whether the plan of care was effective or needs revision.
Evaluation requires critical thinking skills, such as:
-
Identifying evaluative criteria and standards
-
Collecting data to determine whether criteria and standards are met
-
Interpreting and summarizing findings
-
Relating outcomes to interventions
-
Making judgments about problem status
-
Recognizing errors or omissions
-
Identifying factors that contribute to success or failure
Summary
- Critical thinking is a combination of reasoned thinking, openness to alternatives, ability to reflect, and a desire to seek truth.
- Critical thinking is important for nurses because they face complex situations, unique clients, and the need to provide holistic care.
-Nursing knowledge can be theoretical, practical, self, or ethical.
- The nursing process is a systematic problem-solving process that guides all nursing actions. It consists of five phases: assessment, diagnosis, planning, implementation, and evaluation.
- Assessment involves collecting data, organizing data, validating data, and documenting data about the client’s response to health concerns or illness.
- Diagnosis involves analyzing data, identifying health problems, risks, and strengths, and formulating diagnostic statements.
- Planning involves prioritizing problems, formulating goals and outcomes, selecting interventions, and documenting the plan of care.
- Implementation involves performing interventions, recording actions and client responses, and reporting and documenting relevant information.
- Evaluation involves measuring outcomes, comparing outcomes with goals, drawing conclusions, modifying the plan of care, and documenting results.
Nursing Assessment of Wounds and Pressure Ulcers
wetewarya54whj
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Critical Thinking and Nursing Process
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


