Please set your exam date
Musculoskeletal System
Study Questions
Skin Traction
Which statement best describes skin traction in nursing practice?
Explanation
Skin traction is a technique commonly used in orthopedic nursing to stabilize and align fractured bones without the need for invasive surgery. It involves attaching adhesive straps or wraps to the skin around the fractured area and applying a pulling force to maintain proper alignment.
a. Skin traction does not involve the application of a cast. It is a temporary and non-invasive method used to stabilize a fracture before further treatment is provided.
b. Skin traction is not used to reduce dislocated joints. It is specifically used for fractures.
d. Skin traction is not a surgical procedure but rather a non-surgical intervention used in conjunction with other treatments.
What is the primary goal of using skin traction for a patient with a fractured bone?
Explanation
The primary goal of using skin traction is to provide pain relief and reduce discomfort in patients with fractured bones. Traction helps to stabilize the fracture and alleviate pressure on the affected area, leading to pain relief.
a. While some immobilization is achieved with skin traction, the main focus is on pain relief and not complete immobilization.
c. Early ambulation is not the primary goal of skin traction. Ambulation is usually initiated once the fracture is stabilized and appropriate treatment is provided.
d. While skin traction may indirectly support bone healing by reducing pain and allowing proper alignment, it is not the primary goal of this intervention.
Which statement accurately explains how skin traction is applied?
Explanation
In skin traction, adhesive straps or wraps are applied to the skin near the fractured area, and weights are attached to create a pulling force. The pulling force helps to align and stabilize the fractured bone.
a. Skin traction does not involve surgically inserting metal pins into the bone. That technique is called skeletal traction.
b. Skin traction does not apply pressure directly on the fracture site; it uses a pulling force applied through the skin.
c. Adhesive straps or wraps are applied near the fractured area, not directly over it, to avoid pressure on the fracture site.
What is an important nursing consideration when caring for a patient with skin traction?
Explanation
Adjusting the weight used in skin traction without a healthcare provider's order can lead to complications or improper alignment of the fractured bone. Weight adjustments should only be made based on the healthcare provider's instructions.
a. Elevating the affected limb can help reduce edema but may not be specific to skin traction care.
c. Keeping the adhesive straps or wraps clean and dry is essential to prevent skin breakdown and infection, but it is not the primary nursing consideration related to traction.
d. Encouraging active range of motion exercises is not recommended while the patient is in skin traction, as it may disrupt the traction's stabilizing effect on the fractured bone. Passive range of motion exercises may be performed as appropriate, with the healthcare provider's approval.
Which statement is true regarding the use of skin traction?
Explanation
Skin traction is a temporary and short-term intervention used to stabilize a fractured bone and provide pain relief before more definitive treatments, such as casting or surgery, are implemented.
a. Skin traction is not a long-term treatment and is usually used as an interim measure while more definitive treatments are planned.
b. Skin traction is not intended to replace surgical interventions but rather to provide stabilization until surgery is performed, if necessary.
c. Skin traction can be used before surgery but is not typically applied only during surgery for immediate fracture stabilization.
What is the primary indication for using skin traction in nursing practice?
Explanation
The primary indication for skin traction is to provide short-term stabilization and pain relief for a fractured bone. It is a non-invasive method used to align and stabilize fractures before definitive treatment, such as casting or surgery.
a. Skin traction is not used to treat chronic orthopedic conditions; it is primarily used for acute fractures.
b. Skin traction is not typically used to immobilize a fractured bone during surgery; other surgical interventions are used for that purpose.
d. Skin traction does not replace the need for surgical interventions for joint dislocations; it is specifically used for fractures.
Which patient would benefit most from the use of skin traction?
Explanation
Skin traction is most beneficial for patients with fractures who are awaiting definitive treatment, such as surgical fixation. It provides temporary stabilization and pain relief for the fractured bone until further treatment is initiated.
a. Skin traction is not typically used for chronic joint inflammation; it is specific to fractures.
b. Skin traction is not used to treat dislocated joints; other interventions are employed for joint reductions.
d. Skin traction is not indicated for muscle strains; it is primarily used for fractures.
When is skin traction contraindicated in patient care?
Explanation
Skin traction is contraindicated in patients with open fractures where the skin is disrupted. The risk of infection and further complications is high in such cases.
a. Skin traction is not contraindicated in patients with a history of joint dislocations. It is primarily used for fractures.
c. Skin traction is not contraindicated in patients with muscle strains, as it is specific to fractures.
d. Skin traction is not contraindicated in patients with chronic orthopedic conditions; however, it may not be the appropriate intervention for their condition.
Which of the following fractures would benefit from the use of skin traction?
Explanation
Skin traction can be used for certain types of fractures, including hairline fractures, to provide temporary stabilization and pain relief.
b. Compound fractures involve broken bones that pierce the skin, which is a contraindication for skin traction.
c. Stress fractures are overuse injuries and may not require skin traction for management.
d. Greenstick fractures are incomplete fractures common in children, and their management may not necessitate skin traction.
How does skin traction compare to skeletal traction in nursing practice?
Explanation
Skin traction and skeletal traction are both used to stabilize and immobilize fractured bones, but they differ in the method of application. Skin traction uses weights attached to adhesive straps on the skin near the fractured area, while skeletal traction involves weights connected to metal pins inserted directly into the bone.
a. Skin traction is less invasive than skeletal traction because it does not require surgical insertion of metal pins.
c. Skin traction is not only used for chronic orthopedic conditions; it is commonly used for acute fractures as well.
d. Skin traction is not used to replace surgical interventions; it is an adjunctive intervention used in conjunction with other treatments for fractures.
Which type of skin traction is commonly used for patients with hip fractures?
Explanation
Buck's traction is commonly used for patients with hip fractures. It involves the application of skin traction to the lower extremity to stabilize the hip joint and provide pain relief before surgery.
b. Russell's traction is used for patients with lower leg fractures to reduce muscle spasms and align the bones. It is not the most common type of traction used for hip fractures.
c. Bryant's traction is specifically designed for pediatric patients with femur fractures. It is not typically used for hip fractures in adult patients.
d. Dunlop's traction is a type of head and neck traction used for cervical spine injuries. It is not used for hip fractures.
Which type of skin traction is often used for patients with lower leg fractures?
Explanation
Russell's traction is used for patients with lower leg fractures to reduce muscle spasms and align the bones. It involves the application of skin traction to the lower leg.
a. Buck's traction is commonly used for patients with hip fractures, not lower leg fractures.
c. Bryant's traction is specifically designed for pediatric patients with femur fractures, not lower leg fractures in adult patients.
d. Dunlop's traction is a type of head and neck traction used for cervical spine injuries, not lower leg fractures.
Which type of skin traction is specifically designed for pediatric patients with femur fractures?
Explanation
Bryant's traction is specifically designed for pediatric patients with femur fractures. It involves elevating the legs and applying skin traction to the lower extremities to stabilize the fracture.
a. Buck's traction is commonly used for patients with hip fractures, not pediatric patients with femur fractures.
b. Russell's traction is used for patients with lower leg fractures, not pediatric femur fractures.
d. Dunlop's traction is a type of head and neck traction used for cervical spine injuries, not pediatric femur fractures.
Which type of skin traction is applied to patients with fractures of the lower back and lower extremities?
Explanation
Buck's traction is often used for patients with fractures of the lower back and lower extremities. It helps stabilize the area and reduce pain before further treatment.
b. Russell's traction is used for lower leg fractures, not fractures of the lower back and lower extremities.
c. Bryant's traction is specifically designed for pediatric femur fractures, not fractures in the lower back or lower extremities.
d. Dunlop's traction is a type of head and neck traction, not used for fractures of the lower back or lower extremities.
The nurse is caring for a patient with skin traction. What action should the nurse take to prevent skin breakdown?
Explanation
The correct action to prevent skin breakdown in a patient with skin traction is to ensure that the traction weight is hanging freely and not resting on the bed. This prevents pressure on the skin and reduces the risk of skin breakdown.
a. Applying lotion to the skin under the traction can create a barrier that may interfere with proper skin assessment and could cause skin irritation. It is not recommended to apply lotion under the traction.
c. Loosening the traction bandages every 2 hours can compromise the effectiveness of the traction and may not be necessary if the skin is not showing signs of compromise.
d. Removing the traction periodically to assess the skin can disrupt the treatment plan and may not be necessary unless there are signs of skin compromise or other complications.
The nurse is assessing a patient with skin traction. What finding would be of concern and require immediate intervention?
Explanation
Swelling and discoloration of the affected limb can indicate neurovascular compromise and require immediate intervention. The nurse should assess circulation, sensation, and motion of the affected limb and notify the healthcare provider promptly.
a. Mild discomfort at the traction site is common and expected. The nurse can provide pain relief measures as prescribed.
c. Traction weights hanging freely off the edge of the bed is the correct way to set up skin traction. This finding does not raise concern.
d. Traction cords secured with tape to the bedrails is the appropriate way to secure the traction. This finding does not raise concern.
The nurse is preparing to reposition a patient with skin traction. What action should the nurse take to ensure proper alignment?
Explanation
To ensure proper alignment and prevent shearing forces on the skin, the nurse should use a lift sheet to slide the patient to the desired position. This reduces friction and minimizes the risk of skin breakdown.
a. Raising the head of the bed to a 30-degree angle does not address proper alignment for repositioning with skin traction.
b. Having the patient assist in turning to the side can place strain on the affected limb and is not recommended for patients with skin traction.
d. Applying a trochanter roll under the affected hip is not necessary for repositioning with skin traction.
The nurse is performing neurovascular checks on a patient with skin traction. Which assessment finding would be of concern and require immediate action?
Explanation
Absent pedal pulses in the affected foot could indicate compromised circulation and require immediate action. The nurse should notify the healthcare provider promptly to assess and address the issue.
a. Capillary refill of less than 3 seconds in the affected limb is a normal finding and indicates adequate peripheral circulation.
b. Warm and pink skin color in the affected limb is a normal finding and indicates good blood flow.
d. Mild tingling sensation in the affected limb can be a common sensation due to traction, and it does not indicate neurovascular compromise.
The nurse is providing discharge teaching to a patient with skin traction. What instruction should the nurse include to promote skin integrity?
Explanation
To promote skin integrity, the nurse should instruct the patient to inspect the skin under the traction daily for signs of redness, irritation, or breakdown. Early detection of skin issues can help prevent further complications.
a. Applying lotion to the skin under the traction is not recommended, as it can interfere with proper skin assessment and cause skin irritation.
b. Cleaning the skin under the traction with alcohol swabs daily can dry out the skin and increase the risk of skin breakdown.
c. Using a barrier cream on the skin under the traction is not necessary and may not be suitable for all patients. It can also interfere with skin assessment.
The nurse is caring for a patient with skin traction. What is a potential complication of skin traction?
Explanation
A potential complication of skin traction is pressure ulcer development due to constant pressure on the skin from the traction apparatus. The nurse should regularly assess the skin under the traction to prevent skin breakdown.
a. Increased risk of falls is not directly related to skin traction. However, the nurse should implement fall prevention measures for all patients as appropriate.
c. Hypertension is not directly related to skin traction. It is a condition characterized by elevated blood pressure.
d. Constipation is not directly related to skin traction. It can be caused by various factors, including medications and immobility, but it is not a specific complication of skin traction.
The nurse is providing care for a patient in skin traction. What intervention should the nurse implement to prevent contractures?
Explanation
Encouraging active range of motion exercises can help prevent contractures by promoting joint mobility and muscle flexibility. Contractures can occur if the patient remains immobile for an extended period.
b. Applying ice packs to the affected limb is not directly related to preventing contractures. Ice packs are typically used to reduce inflammation and swelling.
c. Limiting the patient's fluid intake is not necessary for preventing contractures. Adequate hydration is essential for overall health and well-being.
d. Maintaining the traction in a continuous position is a standard practice for skin traction. However, it does not specifically address the prevention of contractures.
The nurse is caring for a patient with skin traction. What is a potential complication of inadequate traction?
Explanation
Inadequate traction can lead to improper alignment, uneven pressure distribution, and increased risk of pressure ulcers. The nurse should ensure that the traction is appropriately applied to prevent complications.
a. Decreased muscle spasms may be a positive effect of adequate traction. However, inadequate traction does not necessarily lead to increased muscle spasms.
c. Improved circulation in the affected limb is a potential benefit of proper skin traction, not a complication of inadequate traction.
d. Faster healing of the injured limb is a desired outcome of effective traction. Inadequate traction may delay healing rather than promote it.
The nurse is caring for a patient with skin traction. What is an important nursing intervention to prevent complications?
Explanation
An important nursing intervention to prevent complications in a patient with skin traction is to monitor neurovascular status regularly. This includes assessing circulation, sensation, and motion of the affected limb to detect any signs of neurovascular compromise.
a. Elevating the foot of the bed for comfort is not directly related to preventing complications of skin traction.
b. Loosening the traction bandages every 8 hours can compromise the effectiveness of the traction and is not a recommended nursing intervention.
c. Assessing the patient's pain level once a day is important, but it is not the primary intervention for preventing complications of skin traction.
The nurse is caring for a patient in skin traction. What is a potential complication of skin traction if not properly secured?
Explanation
If the skin traction is not properly secured, there is a risk of traction weight displacement, leading to improper alignment and ineffective traction. Proper securing of the traction is essential to maintain its therapeutic effect.
a. Fracture of the affected limb is not a direct complication of improperly secured skin traction. Fractures are typically treated with other methods, such as casting or surgical interventions.
b. Infection at the traction site may occur if proper hygiene and wound care practices are not followed. It is not directly related to the security of the traction.
d. Excessive traction pressure can occur if the traction is not properly applied or adjusted. However, the primary concern is traction weight displacement, which affects the effectiveness of the treatment.
The nurse is caring for a patient in skin traction. Which action demonstrates effective nursing collaboration?
Explanation
Requesting physical therapy to assist with range of motion exercises demonstrates effective nursing collaboration. Physical therapists are experts in movement and can provide valuable input in promoting joint mobility for patients in traction.
a. Administering pain medication as prescribed is a standard nursing responsibility and does not involve collaboration with other healthcare providers.
b. Initiating skin traction without consulting the healthcare provider is not appropriate. Traction requires a healthcare provider's order, and nurses should not initiate any treatment without proper authorization.
c. Documenting the patient's neurovascular assessment in the chart is a part of the nurse's routine responsibilities and does not involve collaboration with other healthcare providers.
The nurse is caring for a patient in skin traction. When communicating with the healthcare provider about the patient's condition, which approach demonstrates effective nursing communication?
Explanation
Using a clear and concise verbal report is an effective approach to nursing communication. It allows for the efficient transfer of essential patient information to the healthcare provider.
a. Sending a text message to the healthcare provider may not be appropriate for discussing patient information as it may not be secure and may lack important details.
b. Speaking in medical jargon during the conversation can lead to miscommunication and misunderstandings between the nurse and the healthcare provider.
d. Providing the healthcare provider with outdated patient data is not effective in patient care and may lead to incorrect decision-making.
The nurse is collaborating with the physical therapist to assist a patient in skin traction with range of motion exercises. Which action demonstrates effective nursing collaboration?
Explanation
Asking the physical therapist for input on the patient's progress demonstrates effective nursing collaboration. The physical therapist's expertise is valuable in assessing the patient's response to range of motion exercises in traction.
a. Taking over the physical therapist's role in performing the exercises is not appropriate, as each healthcare professional has a specific scope of practice and should work collaboratively.
b. Informing the physical therapist that the exercises are unnecessary disregards the physical therapist's expertise and is not conducive to effective collaboration.
d. Disregarding the physical therapist's recommendations undermines the collaborative effort and diminishes the potential benefits of working together.
The nurse is collaborating with the healthcare team to provide care for a patient in skin traction. Which action demonstrates effective nursing collaboration?
Explanation
: Engaging in open communication and active listening demonstrates effective nursing collaboration. Collaboration involves actively participating in discussions, sharing information, and valuing the input of all team members.
a. Refusing to seek input from other team members is not conducive to collaboration and can hinder the effectiveness of patient care.
c. Failing to communicate changes in the patient's condition can lead to errors and compromises patient safety, which is contrary to effective collaboration.
d. Limiting collaboration to only certain team members can create barriers and may result in missed opportunities for valuable input from different perspectives.
The nurse is collaborating with the physical therapist to coordinate care for a patient in skin traction. Which action demonstrates effective nursing collaboration?
Explanation
Engaging in regular communication to discuss the patient's progress demonstrates effective nursing collaboration. This allows the nurse and physical therapist to coordinate care, make adjustments to the treatment plan, and ensure the best possible outcomes for the patient.
a. Taking over the physical therapist's treatment plan without discussion is not collaborative and can lead to misunderstandings and conflicts between the nurse and the physical therapist.
b. Providing the physical therapist with outdated patient information can compromise the patient's care and is not conducive to effective collaboration.
c. Scheduling therapy sessions at a convenient time for the nurse disregards the needs and progress of the patient, which is not a collaborative approach.
The nurse is evaluating the effectiveness of skin traction for a patient with a fractured femur. Which finding indicates successful traction?
Explanation
The patient's report of minimal discomfort indicates successful skin traction. Traction should alleviate pain and provide proper alignment of the fractured bone, leading to improved comfort for the patient.
b. The patient's pain being unchanged from before traction suggests that the traction may not be effectively relieving the pressure on the fractured bone.
c. The patient's leg appearing slightly misaligned indicates that the traction may not be adequately stabilizing the fracture, which is not a desirable outcome.
d. The patient's fractured femur showing signs of healing is not an immediate evaluation parameter for skin traction effectiveness. Skin traction is primarily aimed at reducing pain and realigning the bone.
The nurse is evaluating the skin condition of a patient in skeletal traction. Which finding requires immediate intervention?
Explanation
Deep tissue damage with visible blisters requires immediate intervention. It indicates that the skin is compromised, and the patient is at risk of developing pressure ulcers or skin breakdown. Prompt action is necessary to prevent further damage and ensure patient safety.
a. Slight redness at the site of the traction tape may be expected, and the nurse should monitor for any signs of worsening or discomfort. It does not require immediate intervention unless it progresses.
b. Minor irritation from the traction device can be managed by ensuring proper padding and positioning of the device. It is not a critical concern unless it worsens or leads to more severe skin issues.
c. Mild itching around the traction area may be common, but the nurse should assess for any signs of infection or allergic reaction. Immediate intervention is not typically required for mild itching.
The nurse is evaluating the patient's neurovascular status in skin traction. Which finding indicates a potential complication?
Explanation
Weak pedal pulses in the affected leg indicate a potential vascular compromise and are concerning in a patient with skin traction. It may indicate reduced blood flow, and immediate intervention is required to ensure proper circulation to the extremity.
a. Capillary refill time of less than 2 seconds is a normal finding and indicates adequate peripheral circulation. It is not indicative of a complication.
c. Symmetrical pedal pulses bilaterally are a positive finding and suggest good vascular status in both legs. It is not a potential complication.
d. Tingling sensation in the toes may be a normal sensation and does not necessarily indicate a complication unless it is accompanied by other neurovascular changes.
The nurse is evaluating the patient's pain level after applying skin traction. Which finding indicates the need for further intervention?
Explanation
The patient stating that the pain is worse with the traction off requires further intervention. Skin traction should relieve pain and discomfort; an increase in pain when the traction is off may indicate inadequate traction or an underlying issue.
a. The patient rating pain as a 3 on a scale of 0 to 10 suggests mild pain and may be expected with some level of discomfort related to the fracture and traction.
b. The patient's pain being well-controlled with prescribed analgesics is a positive finding and indicates that the current pain management plan is effective.
c. The patient reporting occasional sharp pain during movement may be expected with skin traction, but the nurse should assess for any signs of worsening or intolerable pain.
The nurse is evaluating the patient's range of motion in skin traction. Which finding requires further assessment?
Explanation
The patient being unable to move the affected limb in skin traction requires further assessment. Traction should allow some degree of movement, and the nurse should investigate the cause of the restricted motion and take appropriate action.
a. The patient being able to perform active range of motion exercises indicates that some mobility is possible with the traction, which is a positive finding.
b. The patient experiencing some discomfort during range of motion exercises is not unexpected, as traction may cause some discomfort due to realignment of the bone.
d. The patient having difficulty moving the affected limb may be expected with skin traction, and the nurse should continue to monitor the patient's progress.
The nurse is caring for a patient with a fractured femur in skin traction. Which action by the nurse is appropriate?
Explanation
Option A is appropriate because assessing the skin under the traction tape helps monitor for any signs of skin breakdown, irritation, or pressure ulcers. Regular skin assessments are essential to prevent complications related to skin traction.
b. Tightening the traction ropes to increase the traction force is incorrect. The traction force should be set by the healthcare provider, and altering it without proper authorization may lead to adverse effects or further injury.
c. Placing the traction weights on the bed instead of suspending them is incorrect. Traction weights should be suspended freely to provide the appropriate traction force and maintain proper alignment of the fractured bone.
The nurse is providing discharge education to a patient with skin traction. Which instruction should the nurse include?
Explanation
Option D is the correct instruction because the patient should be vigilant in monitoring for any signs of skin redness, irritation, or discomfort under the traction tape. Promptly reporting these symptoms to the healthcare provider allows for early intervention and prevention of skin complications.
a. "Avoid any weight-bearing activities for the duration of traction" is incorrect because weight-bearing activities are typically restricted only in certain types of traction, such as skeletal traction. The nurse should specify any activity restrictions based on the type of traction provided to the patient.
b. "You may remove the traction device at night for more comfort" is incorrect. Skin traction is a continuous intervention, and removing the device can compromise its effectiveness in providing traction and immobilizing the affected limb.
c. "Clean the skin under the traction tape with alcohol wipes daily" is incorrect. Alcohol wipes can cause skin dryness and irritation, which may exacerbate skin issues under the traction tape. The nurse should recommend gentle cleaning and moisturizing as needed.
The nurse is assessing a patient in skin traction. Which finding indicates the need for immediate intervention?
Explanation
While mild discomfort may seem minor, it could indicate skin breakdown, pressure injury, or neurovascular compromise. The nurse must immediately assess circulation, sensation, and motion (CSM) in the affected limb to rule out complications such as compartment syndrome, nerve compression, or improper traction alignment.
The nurse is providing care to a patient in skin traction. Which intervention is essential to maintain proper traction and alignment?
Explanation
Option D is essential in maintaining proper traction and alignment. Knots and kinks in the traction ropes can interfere with the traction force, leading to inadequate realignment of the fractured bone.
a. Reapplying the traction tape every 4 hours is not necessary and may cause skin irritation and complications. Traction tape is typically applied securely and remains in place for an extended period unless specifically indicated otherwise.
b. Keeping the patient's leg in a dependent position is incorrect. The affected leg should be elevated to reduce swelling and promote venous return to prevent further complications such as venous thromboembolism.
c. Elevating the foot of the bed to promote venous return is not a recommended practice for skin traction. The affected limb should be elevated to promote venous return, but the bed should remain flat to maintain the proper alignment and traction force.
The nurse is caring for a patient with a fractured femur who has been placed in skin traction. Which statement best describes the purpose of skin traction?
Explanation
Skin traction is a type of traction that involves applying force to the skin to reduce swelling and edema around the fractured bone. It helps to alleviate pain and promote proper alignment of the bone fragments.
a. Skin traction does not immobilize the fractured bone; rather, it provides continuous but controlled tension to reduce swelling and discomfort.
b. Skin traction is not applied directly to the fractured bone. Instead, it involves applying adhesive strips or bandages to the skin, followed by connecting weights to provide the desired tension.
d. While skin traction may promote some mobility, its primary purpose is to reduce swelling and discomfort rather than facilitating early ambulation.
The nurse is preparing to apply skin traction for a patient with a fractured hip. Which area is the most appropriate location to apply the traction?
Explanation
Skin traction is typically applied above the fractured area to provide a pulling force in the opposite direction to reduce swelling and discomfort. The traction should not be placed directly over the fractured bone to avoid further injury.
a. Placing traction directly over the fractured bone may exacerbate the fracture and cause additional harm.
b. Applying traction to the unaffected leg is not appropriate, as it will not address the fractured hip.
c. Applying traction to the bony prominence on the affected side can cause pressure sores and skin breakdown.
The nurse is assessing a patient with skin traction for any potential complications. Which finding requires immediate intervention?
Explanation
Purplish discoloration below the traction site may indicate impaired circulation, and it requires immediate intervention to prevent further complications like pressure ulcers or nerve damage.
a. Mild redness around the traction tape is common and may be expected, but it does not require immediate intervention unless it worsens or is accompanied by other signs of infection.
b. Slight discomfort at the traction site is expected as a result of the applied tension, and it can be managed with appropriate pain management techniques.
c. Skin irritation from the adhesive strips can be addressed by repositioning the strips or using appropriate skin protection measures.
The nurse is caring for a patient in skin traction and is monitoring the patient's neurovascular status. Which finding indicates a potential complication?
Explanation
Weakness in the unaffected leg may indicate nerve compression or impairment, which requires further assessment and intervention to prevent neurovascular complications.
a. Symmetrical pedal pulses bilaterally indicate adequate circulation to both legs and are a positive finding.
b. Capillary refill time less than 2 seconds indicates good peripheral perfusion and is a normal finding.
d. Tingling sensation in the toes may be expected with skin traction, but it does not necessarily indicate a complication unless it is accompanied by other neurovascular changes.
The nurse is educating a patient with skin traction about self-care measures. Which instruction should the nurse provide to the patient?
Explanation
Checking for signs of skin breakdown or pressure sores is essential to prevent complications associated with skin traction. The patient should inspect the skin around the traction site regularly and report any abnormalities to the healthcare provider.
a. Removing the traction weights without healthcare provider approval can lead to inadequate traction and compromise its effectiveness.
b. Avoiding movements that cause tension on the traction is essential to maintain proper alignment and prevent further injury.
c. Reapplying the traction tape daily is not necessary and may lead to skin irritation. Proper application by healthcare professionals is essential to maintain the appropriate tension.
The nurse is caring for a patient with a fractured femur who has been placed in skin traction. Which action should the nurse take to prevent skin breakdown?
Explanation
Checking the skin under the traction tape daily for redness is essential to monitor for signs of skin breakdown. This allows the nurse to identify early signs of pressure and adjust the traction as needed to prevent skin complications.
a. Applying lotion to the skin under the traction tape is not recommended, as it can create a barrier and interfere with the traction's effectiveness. It may also contribute to skin breakdown.
c. Keeping the traction device tightly secured at all times can lead to excessive pressure on the skin and increase the risk of skin breakdown. The traction should be secured firmly but not excessively tight.
d. Massaging the skin under the traction tape is not advisable, as it can cause friction and further damage the skin, increasing the risk of skin breakdown.
The nurse is preparing to apply skin traction to a patient's lower leg. What is the primary purpose of applying skin traction in this situation?
Explanation
The primary purpose of applying skin traction is to provide a pulling force on the fractured bone, which helps to reduce and realign the bone fragments. It allows for proper bone healing and minimizes pain and muscle spasms.
a. Skin traction does not completely immobilize the fractured bone; it provides some mobility while stabilizing the fracture.
b. Realignment of the fractured bone into its original position is the goal of closed reduction or surgical intervention, not skin traction.
d. While skin traction may promote some blood circulation in the affected limb, its primary purpose is to reduce the fracture and stabilize the bone, not to improve circulation.
The nurse is caring for a patient in skin traction. Which intervention is essential to prevent pressure ulcers?
Explanation
A. Applying petroleum jelly to the skin under the traction tape. Petroleum jelly should not be applied, as it can soften the skin and increase the risk of maceration or skin breakdown under the traction tape.
B. Keeping the traction device loose to allow for movement. The traction must remain properly secured to maintain alignment and prevent further injury. Loosening it defeats the purpose of traction and can lead to complications.
C. Repositioning the patient every 4 hours.Repositioning at least every 2- 4 hours helps relieve pressure, promote circulation, and prevent skin breakdown.Turning every 4 hours on a viscoelastic foam mattress/surface results in fewer pressure ulcers than turning every 2 hours on a standard mattress.
D. Applying direct pressure to the skin over bony prominences. Applying direct pressure to bony prominences increases the risk of skin breakdown and worsens pressure injuries. Instead, pressure should be relieved by using cushions or proper repositioning techniques.
The nurse is providing discharge instructions to a patient with skin traction. Which statement by the patient indicates a need for further teaching?
Explanation
The patient should not remove the traction device independently. Removing the traction can compromise the effectiveness of fracture reduction and delay healing. Only healthcare professionals should adjust or remove the traction as needed.
a. Cleaning the skin under the traction tape with mild soap and water daily helps to maintain skin integrity and reduce the risk of infection.
b. Reporting any signs of skin redness or irritation to the nurse is essential to monitor for potential skin breakdown and prevent complications.
d. Using the trapeze bar to reposition in bed is an appropriate method for the patient to move independently without compromising the traction's stability.
The nurse is assessing a patient with skin traction. Which finding requires immediate intervention?
Explanation
Visible signs of skin breakdown under the traction tape require immediate intervention. It indicates that the skin is compromised, and the patient is at risk of developing pressure ulcers or skin breakdown. Prompt action is necessary to prevent further damage and ensure patient safety.
a. Slight redness at the site of the traction tape may be expected, and the nurse should monitor for any signs of worsening or discomfort. It does not require immediate intervention unless it progresses.
b. Mild discomfort during movement of the affected limb is common with skin traction, and the nurse should assess for any signs of worsening or intolerable pain.
c. Pain rated as 6 out of 10 on the pain scale should be addressed, but it does not require immediate intervention unless it is associated with other concerning signs or symptoms
X-RAY Imaging
Question 1: X-ray imaging is commonly used in medical settings for various purposes. Which of the following statements best describes the principle behind X-ray imaging?
Explanation
X-ray imaging uses ionizing radiation, which has high energy and can penetrate tissues. When X-rays pass through the body, they are absorbed differently by various tissues, creating an image that allows visualization of bones and soft tissues.
a. X-rays do not produce sound waves; they use ionizing radiation to create images, as mentioned in the correct explanation.
b. X-rays do not use magnets; magnetic resonance imaging (MRI) uses magnets to create images of bones and soft tissues.
d. X-rays do not emit radio waves; magnetic resonance imaging (MRI) and computed tomography (CT) use radio waves to visualize organs and blood vessels.
What type of X-ray view is commonly used to visualize the bones of the spine?
Explanation
The lateral view is commonly used to visualize the bones of the spine. In this view, the X-ray beam enters from the side of the patient's body, providing a clear image of the vertebral column.
a. Anteroposterior (AP) view: The AP view is taken from the front to the back of the body and is commonly used to visualize the long bones of the extremities, such as the femur or humerus.
c. Oblique view: The oblique view is taken at an angle to visualize structures that are not well visualized in the standard views. It is not commonly used to visualize the bones of the spine.
d. Posteroanterior (PA) view: The PA view is taken from the back to the front of the body and is commonly used for chest X-rays to visualize the heart and lungs. It is not commonly used to visualize the bones of the spine.
What is the main advantage of X-ray imaging in medical practice?
Explanation
One of the main advantages of X-ray imaging is its cost-effectiveness and widespread availability in most healthcare settings. X-ray machines are relatively affordable and easy to operate, making them a common diagnostic tool.
a. X-ray imaging provides detailed images of bones and some soft tissues, but it is not as effective as other imaging modalities, such as magnetic resonance imaging (MRI), for detailed visualization of soft organs and tissues.
b. X-ray imaging uses ionizing radiation, which can pose some risk to patients. While the amount of radiation is generally considered safe, it is not entirely non-ionizing.
d. X-ray imaging requires some preparation, such as removing metal objects from the body, and may involve positioning the patient appropriately for optimal image capture.
Which safety measure is essential for the healthcare provider performing X-ray imaging on a pregnant patient?
Explanation
Wearing a lead apron during X-ray imaging is essential for the healthcare provider to minimize their exposure to ionizing radiation. This safety measure helps protect the provider from unnecessary radiation exposure, especially important when performing X-rays on pregnant patients to avoid potential harm to the developing fetus.
b. Administering a sedative to the patient is not a safety measure for the healthcare provider. Sedation may be used for patients who have difficulty remaining still during the procedure but does not address the provider's safety.
c. Increasing the X-ray exposure time is not a recommended practice, as it exposes both the patient and the provider to additional ionizing radiation without medical necessity.
d. Using a higher dose of ionizing radiation is not recommended, as it can increase the risk of radiation-related harm to the patient and provider.
Which type of X-ray imaging is commonly used for evaluating blood vessels and organs in the body?
Explanation
Fluoroscopy is a type of X-ray imaging that provides real-time moving images of blood vessels and organs in the body. It is commonly used for procedures such as angiography and barium studies.
a. Plain radiography, also known as X-ray radiography, is used to visualize bones and some soft tissues but does not provide real-time moving images like fluoroscopy.
c. Mammography is a specialized type of X-ray imaging used for breast examination, primarily for detecting breast cancer.
d. Magnetic resonance imaging (MRI) uses magnetic fields and radio waves to create detailed images of organs and tissues, but it does not use X-rays for imaging.
X-ray imaging is based on the principle of:
Explanation
X-ray imaging uses ionizing radiation, which has high energy and can penetrate tissues. When X-rays pass through the body, they are absorbed differently by various tissues, creating an image that allows visualization of bones and soft tissues.
a. Using sound waves to create images of internal structures refers to ultrasound imaging, not X-ray imaging.
b. Utilizing magnetic fields to visualize bones and soft tissues describes magnetic resonance imaging (MRI), not X-ray imaging.
d. Emitting radio waves to visualize organs and blood vessels is a principle of MRI and not X-ray imaging.
What type of X-ray view is commonly used to visualize the bones of the chest and lungs?
Explanation
The PA view is taken from the back to the front of the body and is commonly used for chest X-rays to visualize the heart and lungs.
a. Anteroposterior (AP) view is taken from the front to the back of the body and is commonly used to visualize the long bones of the extremities, such as the femur or humerus.
b. Lateral view is commonly used to visualize the bones of the spine.
c. Oblique view is taken at an angle to visualize structures that are not well visualized in the standard views.
The main advantage of X-ray imaging in medical practice is:
Explanation
: One of the main advantages of X-ray imaging is its cost-effectiveness and widespread availability in most healthcare settings. X-ray machines are relatively affordable and easy to operate, making them a common diagnostic tool.
a. Providing detailed images of soft tissues and organs is an advantage of other imaging modalities, such as MRI, not X-ray imaging.
b. X-ray imaging uses ionizing radiation, which can pose some risk to patients. It is not non-ionizing.
d. X-ray imaging requires some preparation, such as removing metal objects from the body, and may involve positioning the patient appropriately for optimal image capture.
When obtaining an X-ray image, the healthcare provider must consider:
Explanation
Healthcare providers must take appropriate safety measures to minimize their exposure to ionizing radiation during X-ray imaging. This includes wearing lead aprons and using other protective measures to reduce radiation exposure.
a. The patient's comfort during the procedure is essential, but the provider's radiation safety takes precedence to avoid unnecessary exposure.
c. Using the highest X-ray dose is not recommended, as it can increase radiation exposure without medical necessity.
d. Keeping the X-ray machine unplugged when not in use is not a relevant safety measure for radiation exposure.
Which type of X-ray imaging is commonly used for evaluating the digestive system and the movement of contrast agents in real-time?
Explanation
Fluoroscopy is a type of X-ray imaging that provides real-time moving images of the digestive system and the movement of contrast agents in the body. It is commonly used for procedures such as barium studies and angiography.
b. Mammography is a specialized type of X-ray imaging used for breast examination, primarily for detecting breast cancer.
c. Magnetic resonance imaging (MRI) uses magnetic fields and radio waves to create detailed images of organs and tissues but does not use X-rays for imaging.
d. Computed Tomography (CT) uses X-rays and computer processing to create cross-sectional images of the body but does not provide real-time moving images like fluoroscopy.
Before obtaining X-ray images, the healthcare provider must ensure that the patient removes any:
Explanation
Before obtaining X-ray images, the patient should be instructed to remove any jewelry and metallic objects from the body, as they can interfere with the X-ray image and cause artifacts.
a. Personal identification documents are not required to be removed for X-ray imaging, as they do not interfere with the procedure or image quality.
c. Prescription medications taken on the day of the procedure do not need to be removed, as they are not related to the X-ray imaging process.
d. Clothing worn on the upper body may need to be adjusted or removed, depending on the area being imaged, but it is not necessary for the patient to completely remove all clothing.
A patient scheduled for an X-ray of the chest should be educated to:
Explanation
For an X-ray of the chest, the patient should wear loose-fitting clothing that does not contain any metal, such as zippers, buttons, or jewelry, to avoid interference with the X-ray image and ensure optimal visualization of the chest.
a. Refraining from eating or drinking for 24 hours before the procedure is not necessary for a chest X-ray, as it is a non-invasive procedure that does not require fasting.
c. While it is essential for the patient to lie still during the X-ray, this instruction is not specific to a chest X-ray; it applies to all X-ray procedures to prevent motion artifacts.
d. Emptying the bladder is not required for a chest X-ray, as the bladder is not in the field of view for this particular imaging procedure.
When preparing a patient for an X-ray of the lower extremities, the nurse should ask the patient to:
Explanation
Before an X-ray of the lower extremities, the patient should be instructed to remove any metal objects, such as jewelry, piercings, or metallic accessories, from the lower limbs to prevent artifacts on the X-ray image.
a. While the patient may be required to remove clothing covering the lower extremities, it is not necessary for them to wear a hospital gown for the procedure.
c. Applying a topical anesthetic is not routinely done for X-ray imaging, as X-rays are non-invasive and do not require anesthesia.
d. Refraining from bearing weight on the lower extremities is not a standard preparation for X-ray imaging of the lower limbs unless specifically instructed by the healthcare provider for certain conditions.
Before an X-ray of the abdomen, the nurse should inquire if the patient is:
Explanation
Before an X-ray of the abdomen, it is crucial to inquire if the patient is pregnant or potentially pregnant, as ionizing radiation used in X-rays can be harmful to the developing fetus.
b. Fasting for at least 12 hours is not required for an abdominal X-ray, as it is a non-invasive procedure that does not require fasting.
c. Allergic to iodine or shellfish is not directly relevant to an abdominal X-ray, as iodine-based contrast agents are not typically used for this imaging modality.
d. Taking pain medications is not a specific concern for an abdominal X-ray unless there are specific instructions from the healthcare provider regarding medication use before the procedure.
What should the nurse instruct the patient to do during the X-ray imaging procedure?
Explanation
The nurse should instruct the patient to remain as still as possible without movement during the X-ray imaging procedure to ensure clear and accurate images.
a. While taking slow and deep breaths may be helpful in reducing motion artifacts for some imaging procedures, it is not necessary for X-ray imaging as the procedure is typically brief.
c. Coughing or clearing the throat during the X-ray procedure is not recommended, as it can lead to motion artifacts and compromise the quality of the images.
d. Requesting to see the X-ray images immediately after the procedure is not a standard practice, as the X-ray images need to be reviewed and interpreted by a qualified radiologist or healthcare provider before sharing with the patient.
Which safety measure is essential to protect both the patient and the healthcare provider during X-ray imaging?
Explanation
Wearing a lead apron is essential to protect both the patient and the healthcare provider from unnecessary exposure to ionizing radiation during X-ray imaging. The lead apron serves as a barrier that absorbs and reduces the amount of radiation reaching the individual wearing it.
b. Using high doses of X-rays for better image quality is not a safe practice. X-ray imaging should be performed using the lowest dose of radiation necessary to obtain diagnostic images while still maintaining image quality.
c. Standing close to the X-ray machine during image capture can lead to increased radiation exposure for the healthcare provider. They should maintain a safe distance from the X-ray source during the procedure.
d. Taking X-ray images without any protective measures is unsafe and increases the risk of radiation exposure to both the patient and the healthcare provider.
Before performing an X-ray on a pediatric patient, what safety measure should the healthcare provider consider?
Explanation
When performing X-rays on pediatric patients, using pediatric-sized lead aprons or shields is crucial to protect sensitive tissues and organs from unnecessary radiation exposure.
a. Minimizing immobilization techniques may result in suboptimal image quality due to motion artifacts. The healthcare provider should use appropriate immobilization techniques to ensure clear images.
b. Adjusting the X-ray machine to deliver higher radiation doses is not safe for pediatric patients. The radiation dose should be minimized while maintaining image quality.
c. Having parents leave the room during the procedure is not necessary and may cause unnecessary distress for the child. However, the parents should also wear protective lead aprons if they are in close proximity to the X-ray source.
When performing an X-ray on a pregnant patient, what safety measure should be taken?
Explanation
When performing X-rays on pregnant patients, it is essential to use lead aprons to cover the abdomen and pelvic area to protect the developing fetus from unnecessary radiation exposure.
a. Setting the X-ray machine to maximum power is not safe for any patient, including pregnant individuals. The radiation dose should be minimized while maintaining image quality.
b. While X-rays during pregnancy should be used judiciously and only if medically necessary, avoiding X-rays during the entire first trimester is not practical in emergencies or urgent diagnostic situations.
d. Providing a lead apron only to the patient and not to the healthcare provider can result in increased radiation exposure to the provider, who should also wear protective equipment during the procedure.
How can the healthcare provider reduce the risk of radiation exposure during fluoroscopy procedures?
Explanation
Image intensifiers are used in fluoroscopy to enhance image brightness and quality. Limiting their use can help reduce X-ray scatter and unnecessary radiation exposure to the patient and healthcare provider.
b. Increasing the fluoroscopy time should be avoided to minimize radiation exposure to the patient and provider. The goal is to keep fluoroscopy time as short as possible while still obtaining necessary images.
c. Standing closer to the patient during the procedure increases the radiation exposure to the healthcare provider. Providers should maintain a safe distance from the X-ray source during fluoroscopy.
d. Using the highest possible radiation dose is not recommended, as the goal is to use the lowest radiation dose necessary to obtain diagnostic images while still maintaining image quality and reducing the risk of radiation exposure to the patient and provider.
During X-ray imaging, how can the healthcare provider reduce radiation exposure to other patients and staff in the vicinity?
Explanation
Requesting others in the room to wear protective lead aprons is an effective way to reduce radiation exposure to other patients and staff in the vicinity of the X-ray procedure.
a. Keeping the X-ray room door open during the procedure can lead to increased radiation exposure to people outside the room. The door should be closed during X-ray imaging to minimize radiation scatter.
b. Placing the X-ray machine at a higher elevation does not affect radiation exposure to other patients and staff in the room. The proper use of protective lead aprons is more effective.
d. Increasing the number of X-ray images taken at one time does not reduce radiation exposure to others in the room. The number of images taken should be limited to those necessary for diagnostic purposes while minimizing radiation dose to all individuals present.
Which safety measure is essential to protect both the patient and the healthcare provider during X-ray imaging?
Explanation
Wearing a lead apron is essential to protect both the patient and the healthcare provider from unnecessary exposure to ionizing radiation during X-ray imaging. The lead apron serves as a barrier that absorbs and reduces the amount of radiation reaching the individual wearing it.
b. Using high doses of X-rays for better image quality is not a safe practice. X-ray imaging should be performed using the lowest dose of radiation necessary to obtain diagnostic images while still maintaining image quality.
c. Standing close to the X-ray machine during image capture can lead to increased radiation exposure for the healthcare provider. They should maintain a safe distance from the X-ray source during the procedure.
d. Taking X-ray images without any protective measures is unsafe and increases the risk of radiation exposure to both the patient and the healthcare provider.
Before performing an X-ray on a pediatric patient, what safety measure should the healthcare provider consider?
Explanation
When performing X-rays on pediatric patients, using pediatric-sized lead aprons or shields is crucial to protect sensitive tissues and organs from unnecessary radiation exposure.
a. Minimizing immobilization techniques may result in suboptimal image quality due to motion artifacts. The healthcare provider should use appropriate immobilization techniques to ensure clear images.
b. Adjusting the X-ray machine to deliver higher radiation doses is not safe for pediatric patients. The radiation dose should be minimized while maintaining image quality.
c. Having parents leave the room during the procedure is not necessary and may cause unnecessary distress for the child. However, the parents should also wear protective lead aprons if they are in close proximity to the X-ray source.
When performing an X-ray on a pregnant patient, what safety measure should be taken?
Explanation
When performing X-rays on pregnant patients, it is essential to use lead aprons to cover the abdomen and pelvic area to protect the developing fetus from unnecessary radiation exposure.
a. Setting the X-ray machine to maximum power is not safe for any patient, including pregnant individuals. The radiation dose should be minimized while maintaining image quality.
b. While X-rays during pregnancy should be used judiciously and only if medically necessary, avoiding X-rays during the entire first trimester is not practical in emergencies or urgent diagnostic situations.
d. Providing a lead apron only to the patient and not to the healthcare provider can result in increased radiation exposure to the provider, who should also wear protective equipment during the procedure.
How can the healthcare provider reduce the risk of radiation exposure during fluoroscopy procedures?
Explanation
Image intensifiers are used in fluoroscopy to enhance image brightness and quality. Limiting their use can help reduce X-ray scatter and unnecessary radiation exposure to the patient and healthcare provider.
b. Increasing the fluoroscopy time should be avoided to minimize radiation exposure to the patient and provider. The goal is to keep fluoroscopy time as short as possible while still obtaining necessary images.
c. Standing closer to the patient during the procedure increases the radiation exposure to the healthcare provider. Providers should maintain a safe distance from the X-ray source during fluoroscopy.
d. Using the highest possible radiation dose is not recommended, as the goal is to use the lowest radiation dose necessary to obtain diagnostic images while still maintaining image quality and reducing the risk of radiation exposure to the patient and provider.
During X-ray imaging, how can the healthcare provider reduce radiation exposure to other patients and staff in the vicinity?
Explanation
Requesting others in the room to wear protective lead aprons is an effective way to reduce radiation exposure to other patients and staff in the vicinity of the X-ray procedure.
a. Keeping the X-ray room door open during the procedure can lead to increased radiation exposure to people outside the room. The door should be closed during X-ray imaging to minimize radiation scatter.
b. Placing the X-ray machine at a higher elevation does not affect radiation exposure to other patients and staff in the room. The proper use of protective lead aprons is more effective.
d. Increasing the number of X-ray images taken at one time does not reduce radiation exposure to others in the room. The number of images taken should be limited to those necessary for diagnostic purposes while minimizing radiation dose to all individuals present.
When performing X-ray imaging on pediatric patients, which consideration is essential to minimize radiation exposure?
Explanation
When performing X-ray imaging on pediatric patients, it is crucial to use pediatric-sized lead aprons or shields to protect sensitive tissues and organs from unnecessary radiation exposure.
a. Using lead aprons only for the healthcare providers is not sufficient to protect pediatric patients from radiation exposure. Both the patient and the healthcare providers should wear appropriate protective equipment.
b. Adjusting the X-ray machine to deliver higher radiation doses is not safe for pediatric patients. The radiation dose should be minimized while maintaining image quality.
c. Reducing the use of immobilization techniques can result in suboptimal image quality due to motion artifacts. Proper immobilization techniques should be used to ensure clear images.
Before performing X-ray imaging on a pediatric patient, what is the most important question to ask the parents or guardian?
Explanation
Asking about metal implants or devices is crucial before performing X-ray imaging on a pediatric patient as metal can cause artifacts on the X-ray image and affect diagnostic accuracy.
b. Asking about recent exposure to radiation is not directly relevant to X-ray imaging in the current situation. However, the healthcare provider should be aware of any previous medical imaging studies involving radiation.
c. Inquiring about the child's eating or drinking status is not specifically related to X-ray imaging preparation, as fasting is not typically required for X-ray procedures.
d. Asking about allergies to iodine is not directly relevant to X-ray imaging, as iodine-based contrast agents are not commonly used for routine X-rays.
How should the X-ray imaging procedure be modified for a pediatric patient who is unable to cooperate and hold still?
Explanation
When a pediatric patient is unable to cooperate and hold still during X-ray imaging, employing immobilization techniques and involving parents or caregivers to help keep the child still is essential for obtaining clear and accurate images.
a. Sedating a child solely for X-ray imaging is not ideal and should only be considered when medically necessary and under the guidance of a healthcare provider.
b. Using motion-blur reduction techniques during image processing can improve image quality to some extent, but it cannot compensate for significant motion artifacts caused by an uncooperative child.
d. Postponing the procedure may not be appropriate if the X-ray is urgently needed for diagnosis or medical management. Efforts should be made to use appropriate immobilization techniques to obtain necessary images.
What is the primary reason for using a lower radiation dose when performing X-ray imaging on pediatric patients?
Explanation
Pediatric patients are more sensitive to the effects of ionizing radiation compared to adults. Therefore, using a lower radiation dose is essential to minimize the potential long-term risks associated with radiation exposure in pediatric populations.
a. The thickness of bones is not the primary factor for using lower radiation doses in pediatric patients. The decision is based on their increased sensitivity to radiation.
c. Lowering the radiation dose in pediatric patients may compromise image quality to some extent, but the primary reason is to reduce radiation exposure to these vulnerable populations.
d. While the size of pediatric patients may influence radiation dose adjustments, the main concern is their increased radiation sensitivity rather than physical size.
What additional safety measure should be taken when performing X-ray imaging on a pediatric patient with suspected scoliosis?
Explanation
When performing X-ray imaging on a pediatric patient with suspected scoliosis, using gonad shields is essential to protect the child's reproductive organs from unnecessary radiation exposure.
a. Performing X-rays at a higher resolution may provide better visualization of the spine, but it is not directly related to the safety measure required for a pediatric patient with suspected scoliosis.
b. Applying lead aprons to protect the child's abdomen and chest only does not adequately protect the reproductive organs. Gonad shields are specifically designed for this purpose.
c. While limiting the number of X-ray images taken is a good practice to minimize radiation exposure, it may not be feasible for diagnostic purposes in cases of suspected scoliosis that require multiple images for evaluation and treatment planning.
What information should be included in the documentation after performing an X-ray imaging procedure?
Explanation
Documentation after an X-ray imaging procedure should include essential patient identifiers, such as the patient's name, date of birth, and medical history. This information helps ensure accurate record-keeping and patient identification.
b. The radiographer's personal observations and opinions should not be included in the documentation. Documentation should be objective and focus on factual information related to the procedure and patient's condition.
c. The specific dosage of radiation used during the procedure is an important detail for the radiographer to know but does not need to be included in the general patient documentation. Radiation dosage details are typically recorded in the radiographer's logbook or system.
d. The results and interpretation of the X-ray images should be documented by a radiologist or healthcare provider who reviews the images. The radiographer's documentation should focus on the technical aspects of the procedure and patient information.
After completing an X-ray imaging procedure, the radiographer notices an error in the patient's documentation. What is the appropriate action?
Explanation
If an error is noticed in the patient's documentation, the appropriate action is to correct the error by making a single line through the incorrect information, writing the correct information above or beside the error, and initialing the changes. This process ensures transparency and accountability for any modifications made.
b. Making a note in the documentation about the error is not sufficient. It is essential to correct the error directly in the documentation.
c. Removing the incorrect documentation and creating a new record may be seen as an attempt to hide the error and is not an appropriate course of action.
d. Informing the patient about the documentation error is not necessary in this context. The priority is to correct the documentation and ensure accuracy.
How should the radiographer ensure patient safety during post-procedure care following X-ray imaging?
Explanation
After X-ray imaging, it is essential to monitor the patient for any adverse reactions or symptoms that may arise. This helps ensure patient safety and early detection of any potential complications.
a. Providing the patient with a copy of the X-ray images to take home is not a safety measure for post-procedure care. It may be done as part of the patient's records, but monitoring for adverse reactions is more critical for immediate safety.
c. Allowing the patient to leave the facility immediately after the procedure may be appropriate in many cases, but monitoring for adverse reactions is still necessary before discharge.
d. Discontinuing the use of lead aprons and shields after the procedure is not safe. Proper protective equipment should be used until the patient leaves the radiology department to minimize radiation exposure.
What should the radiographer do if the patient experiences an allergic reaction to the contrast medium used in an X-ray procedure?
Explanation
If the patient experiences an allergic reaction to the contrast medium used in an X-ray procedure, the radiographer should document the reaction in the patient's record and notify the radiologist or healthcare provider immediately. This ensures that appropriate medical attention and follow-up can be provided to the patient.
b. Administering an antihistamine is not within the scope of practice for a radiographer. Only qualified healthcare providers can administer medications and manage allergic reactions.
c. Repeating the X-ray with a lower concentration of contrast medium is not appropriate if the patient has experienced an allergic reaction. The use of contrast should be carefully reconsidered, and alternative imaging modalities may be considered.
d. Discharging the patient without any further intervention is not appropriate if they have experienced an allergic reaction. The patient's condition should be assessed, and appropriate medical care should be provided as needed.
What documentation is essential in the patient's record after the removal of any protective lead aprons or shields post-X-ray imaging?
Explanation
After the removal of any protective lead aprons or shields post-X-ray imaging, the radiographer should note the time and date of removal in the patient's record. This documentation ensures that the appropriate radiation safety measures were followed during the procedure.
b. Indicating any radiation exposure the patient received is not relevant after the removal of lead aprons. The radiation exposure received during the procedure should be documented before the protective equipment is removed.
c. Writing down the patient's feedback about the procedure may be valuable for patient satisfaction and quality improvement but is not specifically related to the documentation of lead apron removal.
d. Documenting the radiographer's personal observations is not essential in the patient's record after lead apron removal. The focus should be on relevant patient information and safety measures taken during the procedure.
The nurse is preparing a client for an X-ray procedure. Which instruction should the nurse provide to the client before the procedure?
Explanation
Metal objects, including jewelry and accessories, can interfere with the X-ray image quality. Instructing the client to remove these items ensures accurate results.
b. "Consume a full meal before the procedure." This choice is incorrect because it is generally recommended to fast for a certain period before an X-ray, especially if contrast dye will be used. Eating a full meal could affect the accuracy of the images.
c. "Drink a large amount of water before the procedure." This choice is incorrect because drinking a large amount of water is not typically required for a standard X-ray procedure. However, specific instructions may be given if a contrast dye is used.
d. "Avoid taking any pain medications before the procedure." This choice is incorrect because taking pain medications is not typically contraindicated before an X-ray. Pain medications may be taken as needed and should not significantly affect the procedure.
The nurse is reviewing the laboratory results of a client who will undergo an X-ray with contrast dye. Which result is most important for the nurse to assess before the procedure?
Explanation
Contrast dye used in X-ray procedures can affect kidney function, and high blood glucose levels may increase the risk of kidney injury. Monitoring the blood glucose level is important before the procedure to ensure the client's safety.
a. Hemoglobin level. While monitoring the hemoglobin level is important for overall health assessment, it is not directly related to the use of contrast dye in an X-ray procedure.
c. Serum electrolyte levels. Electrolyte levels are important for assessing overall health and kidney function, but they are not specifically related to the administration of contrast dye.
d. White blood cell count. The white blood cell count is important for assessing immune function but is not directly related to the use of contrast dye for X-ray imaging.
The nurse is caring for a pediatric client who requires an X-ray. How should the nurse explain the procedure to the child?
Explanation
Explaining the procedure in simple and age-appropriate language is important when caring for pediatric clients. Describing the need to stay still for the X-ray helps reduce anxiety and fear.
a. "You will be put to sleep during the procedure." This choice is incorrect because sedation or anesthesia is not typically used for a routine X-ray procedure.
c. "You will need to drink a special liquid before the procedure." This choice is incorrect because drinking a special liquid is more commonly associated with other imaging procedures, such as CT scans.
d. "You will need to remove your clothing and put on a hospital gown." This choice is incorrect because it does not accurately describe the X-ray procedure, which typically requires the client to remain in their regular clothing.
The nurse is preparing a client for a chest X-ray. Which instruction should the nurse provide to the client before the procedure?
Explanation
Metal objects, including jewelry and accessories, can interfere with the X-ray image quality. Instructing the client to remove these items ensures accurate results.
b. "Consume a full meal before the procedure." This choice is incorrect because clients are usually instructed to fast for a specific period before an X-ray, especially if abdominal imaging is involved, to reduce interference with image quality due to food and gas.
c. "Drink a large amount of water before the procedure." This choice is incorrect because drinking water is typically not required before an X-ray procedure. Fasting or specific preparation instructions are more commonly given.
d. "Avoid taking any pain medications before the procedure." This choice is incorrect because the nurse does not typically instruct the client to avoid pain medications before an X-ray. Pain medications would not interfere with the X-ray procedure itself.
The nurse is caring for a pediatric client who requires an X-ray. How should the nurse explain the procedure to the child?
Explanation
Explaining the procedure in simple and age-appropriate language is important when caring for pediatric clients. Describing the need to stay still for the X-ray helps reduce anxiety and fear.
a. "You will be put to sleep during the procedure." This choice is incorrect because sedation or anesthesia is typically not required for a standard X-ray procedure.
c. "You will need to drink a special liquid before the procedure." This choice is incorrect because drinking a special liquid (contrast dye) before the procedure is more common for certain types of X-ray exams, such as those involving the digestive system.
d. "You will need to remove your clothing and put on a hospital gown." This choice is incorrect because wearing a hospital gown is not always necessary for an X-ray procedure. It depends on the area of the body being imaged and the specific instructions provided.
The nurse is assessing a client who recently had an X-ray procedure. Which information should the nurse prioritize when providing post-procedure care?
Explanation
After an X-ray procedure, the nurse should prioritize ensuring the client's mobility and safety. The client may have been immobilized during the procedure, and it is important to assess and promote circulation, sensation, and movement.
a. Administering pain medication. This choice is incorrect because routine administration of pain medication is not a standard post-procedure intervention after an X-ray. Pain medication may be administered if the client is experiencing pain, but it is not a priority for all clients.
b. Monitoring for allergic reactions. This choice is incorrect because allergic reactions are more relevant when contrast dye is used. Routine monitoring for allergic reactions is not typically required after a routine X-ray procedure.
c. Documenting the procedure time. This choice is incorrect because documenting the procedure time is important for record-keeping but is not a priority for immediate post-procedure care.
The nurse is reviewing the laboratory results of a client who will undergo an X-ray with contrast dye. Which result is most important for the nurse to assess before the procedure?
Explanation
Contrast dye used in X-ray procedures can affect kidney function, and high blood glucose levels may increase the risk of kidney injury. Monitoring the blood glucose level is important before the procedure to ensure the client's safety.
a. Hemoglobin level. This choice is incorrect because the hemoglobin level is not directly related to the administration of contrast dye for an X-ray procedure.
c. Serum electrolyte levels. This choice is incorrect because routine assessment of serum electrolyte levels is not a standard pre-procedure requirement for X-ray imaging with contrast dye.
d. White blood cell count. This choice is incorrect because the white blood cell count is not directly relevant to the administration of contrast dye for an X-ray procedure.
Bone Marrow Aspiration
The nurse is explaining the purpose of a bone marrow aspiration to a patient. Which statement accurately describes the primary goal of this procedure?
Explanation
Bone marrow aspiration is a procedure used to obtain a sample of the bone marrow for diagnostic purposes. It is commonly performed to assess and diagnose various blood disorders, such as leukemia, anemia, and other hematological conditions. It is also used to detect cancers that may originate in the bone marrow.
a. This statement is incorrect. Bone marrow aspiration is not used to assess lung function. Lung function is typically evaluated through respiratory tests, such as spirometry or arterial blood gas analysis.
b. This statement is incorrect. Bone marrow aspiration is not used to diagnose heart conditions. Heart function is usually assessed through cardiac tests, such as electrocardiography (ECG) or echocardiography.
d. This statement is incorrect. Bone marrow aspiration is not used to assess kidney function. Kidney function is typically evaluated through blood and urine tests, such as creatinine clearance or serum electrolytes.
The nurse is preparing a patient for a bone marrow aspiration. What is the most common site for bone marrow aspiration in adults?
Explanation
In adults, the most common site for bone marrow aspiration is the sternum (breastbone). Other sites that can be used for aspiration include the iliac crest (hip bone) and the posterior superior iliac spine (back of the hip bone).
a. This statement is incorrect. While the femur can be used for bone marrow aspiration in some cases, the sternum is the most common site in adults.
b. This statement is incorrect. The humerus is not a common site for bone marrow aspiration in adults.
d. This statement is incorrect. The tibia is not a common site for bone marrow aspiration in adults.
The nurse is explaining the bone marrow aspiration procedure to a patient. Which of the following statements is accurate?
Explanation
Bone marrow aspiration is usually performed using local anesthesia. This means that the area where the needle will be inserted is numbed, but the patient remains awake and alert during the procedure. General anesthesia is not typically used for bone marrow aspiration.
a. This statement is incorrect. Bone marrow aspiration requires some form of anesthesia to numb the area where the needle will be inserted.
b. This statement is incorrect. General anesthesia is not commonly used for bone marrow aspiration, as local anesthesia is sufficient for the procedure.
d. This statement is incorrect. Anesthesia is necessary for bone marrow aspiration to minimize pain and discomfort during the procedure.
The nurse is providing pre-procedure education to a patient scheduled for a bone marrow aspiration. Which of the following statements by the patient indicates a need for further teaching?
Explanation
Unlike some other procedures that require fasting, bone marrow aspiration does not usually require the patient to fast. Fasting is not necessary for this procedure.
a. This statement is correct. It is essential to inform the healthcare team if the patient is taking any blood-thinning medications, as they may need to be temporarily discontinued before the procedure to reduce the risk of bleeding.
c. This statement is correct. After a bone marrow aspiration, the patient should avoid strenuous activities for a day or two to minimize the risk of complications and allow the site to heal.
d. This statement is correct. During the bone marrow aspiration procedure, the patient will be asked to lie still to ensure accurate needle placement and reduce the risk of complications.
The nurse is caring for a patient after a bone marrow aspiration. Which of the following symptoms should the nurse monitor for as potential complications?
Explanation
After a bone marrow aspiration, the nurse should monitor for signs of infection or other complications, such as fever, chills, and an increased heart rate. These symptoms may indicate an infection or bleeding at the site.
b. This statement is incorrect. Elevated blood pressure and sweating are not typical symptoms of complications after a bone marrow aspiration.
c. This statement is incorrect. Excessive thirst and dry mouth are not typical symptoms of complications after a bone marrow aspiration.
d. This statement is incorrect. Muscle weakness and fatigue are not typical symptoms of complications after a bone marrow aspiration.
The healthcare provider orders a bone marrow aspiration for a patient with persistent anemia. What is the primary indication for this procedure in this patient?
Explanation
Bone marrow aspiration is commonly used to diagnose and evaluate the cause of various blood disorders, including anemia. By examining the bone marrow cells, healthcare providers can identify the underlying cause of the patient's anemia.
a. This choice is incorrect because bone marrow aspiration is not used to evaluate kidney function. Kidney function is typically assessed through blood and urine tests.
b. This choice is incorrect because bone marrow aspiration is not used to assess liver enzyme levels. Liver enzyme levels are usually measured through blood tests.
c. This choice is incorrect because bone marrow aspiration is not used to diagnose respiratory conditions. Respiratory conditions are typically diagnosed through various respiratory tests.
A patient is suspected of having leukemia. The healthcare provider orders a bone marrow aspiration to confirm the diagnosis. What is the primary indication for this procedure in this patient?
Explanation
Bone marrow aspiration is commonly used to diagnose various blood disorders, including leukemia, which is a cancer of the blood and bone marrow. By examining the bone marrow cells, healthcare providers can determine if cancerous cells are present and confirm the diagnosis of leukemia.
a. This choice is incorrect because bone marrow aspiration is not used to assess bone density. Bone density is typically evaluated through bone density scans or DEXA scans.
b. This choice is incorrect because bone marrow aspiration is not used to detect brain abnormalities. Brain abnormalities are typically diagnosed through imaging tests such as MRI or CT scans.
d. This choice is incorrect because bone marrow aspiration is not used to evaluate cardiac function. Cardiac function is typically assessed through various cardiac tests, such as electrocardiography (ECG) or echocardiography.
A patient with unexplained thrombocytopenia is scheduled for a bone marrow aspiration. What is the primary indication for this procedure in this patient?
Explanation
Bone marrow aspiration is commonly used to evaluate the production of blood cells, including platelets. In a patient with thrombocytopenia (low platelet count), bone marrow aspiration can help identify the cause of decreased platelet production.
a. This choice is incorrect because bone marrow aspiration is not used to assess lung function. Lung function is typically evaluated through respiratory tests, such as spirometry or arterial blood gas analysis.
b. This choice is incorrect because bone marrow aspiration is not used to diagnose gastrointestinal disorders. Gastrointestinal disorders are typically diagnosed through various gastrointestinal tests and imaging studies.
d. This choice is incorrect because bone marrow aspiration is not used to determine kidney health. Kidney health is typically assessed through blood and urine tests.
A patient with a history of multiple myeloma requires monitoring of disease progression. What is the primary indication for bone marrow aspiration in this patient?
Explanation
Bone marrow aspiration is commonly used to evaluate the extent of bone marrow involvement in conditions such as multiple myeloma, a cancer of the plasma cells in the bone marrow. By examining the bone marrow cells, healthcare providers can determine the progression of the disease and guide treatment decisions.
a. This choice is incorrect because bone marrow aspiration is not used to assess thyroid function. Thyroid function is typically assessed through blood tests, such as thyroid hormone levels.
b. This choice is incorrect because bone marrow aspiration is not used to diagnose liver cirrhosis. Liver cirrhosis is typically diagnosed through liver function tests and imaging studies.
d. This choice is incorrect because bone marrow aspiration is not used to determine lung health. Lung health is typically assessed through respiratory tests and imaging studies.
A patient with suspected iron-deficiency anemia is scheduled for a bone marrow aspiration. What is the primary indication for this procedure in this patient?
Explanation
Bone marrow aspiration can be used to assess the iron stores in the bone marrow, providing valuable information about iron metabolism and helping to confirm a diagnosis of iron-deficiency anemia.
a. This choice is incorrect because bone marrow aspiration is not used to evaluate pancreatic function. Pancreatic function is typically assessed through blood tests, such as pancreatic enzyme levels.
b. This choice is incorrect because bone marrow aspiration is not used to diagnose skin conditions. Skin conditions are typically diagnosed through visual examination and skin biopsies, if necessary.
d. This choice is incorrect because bone marrow aspiration is not used to determine muscle strength. Muscle strength is typically assessed through physical examination and strength testing.
The healthcare provider is explaining the bone marrow aspiration procedure to a patient. Which statement by the patient indicates an understanding of the procedure?
Explanation
Bone marrow aspiration involves the insertion of a needle into the bone marrow space to collect a small sample of bone marrow for examination. This statement accurately describes the procedure.
b. This choice is incorrect because bone marrow aspiration is not performed by inserting a needle into the joint. It is done by inserting a needle into the bone marrow cavity.
c. This choice is incorrect because bone marrow aspiration is not done to evaluate lung function. It is used to evaluate the production of blood cells and diagnose various blood disorders.
d. This choice is incorrect because bone marrow aspiration may cause discomfort or mild pain, so local anesthetics are often used to numb the area before the procedure.
The nurse is preparing a patient for a bone marrow aspiration. Which action is essential in the pre-procedure care?
Explanation
Obtaining informed consent from the patient is an essential pre-procedure action. It ensures that the patient is aware of the procedure, its risks, benefits, and alternatives, and gives their voluntary permission for the bone marrow aspiration.
a. Administering intravenous antibiotics is not typically part of the pre-procedure care for bone marrow aspiration. Antibiotics are usually administered if there is a risk of infection, but it is not a routine pre-procedure action.
c. Providing a high-calorie meal before the procedure is not necessary for bone marrow aspiration. In fact, patients may be advised to have a light meal or be NPO (nothing by mouth) for a certain period before the procedure.
d. Restricting fluid intake for 8 hours before the procedure is not recommended for bone marrow aspiration. Patients are usually advised to maintain adequate hydration before the procedure.
The patient asks the nurse about the potential complications of a bone marrow aspiration. What is the nurse's best response?
Explanation
Common side effects of bone marrow aspiration include temporary pain or discomfort at the needle insertion site and bruising. These are generally minor and resolve on their own.
a. The risk of developing blood clots after bone marrow aspiration is minimal and not a common complication.
b. Fever and chills are not typical side effects of bone marrow aspiration. If these symptoms occur, they may indicate an infection or other complication that needs medical attention.
c. Bone marrow aspiration is not associated with liver or kidney damage. It is a relatively safe procedure when performed by experienced healthcare providers.
During a bone marrow aspiration procedure, the patient reports severe pain at the site of the needle insertion. What should the nurse do first?
Explanation
Severe pain during a bone marrow aspiration may indicate complications or improper needle placement. The nurse should notify the healthcare provider immediately to assess the patient and take appropriate actions.
a. Applying a warm compress may not be appropriate for severe pain during a bone marrow aspiration. The cause of the pain needs to be addressed first.
b. Administering pain medication as ordered may not be sufficient for severe pain during the procedure. The healthcare provider needs to evaluate the patient's condition and decide on further interventions.
c. While documenting the patient's complaint is essential, it should not be the first action when the patient reports severe pain during a procedure. Addressing the patient's immediate needs and notifying the healthcare provider take priority.
The nurse is providing discharge instructions to a patient following a bone marrow aspiration. What should the nurse include in the instructions?
Explanation
After a bone marrow aspiration, the patient should be instructed to report any signs of infection at the needle insertion site, such as redness, swelling, drainage, or increased pain, to their healthcare provider for prompt evaluation and treatment.
a. Patients are usually advised to avoid strenuous activities and heavy lifting for a period after the procedure. Normal activities may need to be restricted based on the healthcare provider's instructions.
b. Encouraging the patient to avoid drinking fluids is not appropriate after a bone marrow aspiration. Adequate hydration is essential for recovery and healing.
c. It is important to provide guidance on wound care after the procedure, but instructing the patient to avoid pressure on the site for 24 hours may not be necessary. The healthcare provider's specific instructions regarding wound care should be followed.
The nurse is caring for a patient who underwent a bone marrow aspiration. What is the most common complication associated with this procedure?
Explanation
Infection at the needle insertion site is the most common complication associated with bone marrow aspiration. Patients are at risk of developing infections at the site where the needle was inserted into the bone marrow cavity.
b. Excessive bleeding during the procedure is a risk, but it is not the most common complication.
c. Formation of blood clots in the bone marrow is not a typical complication of bone marrow aspiration.
d. Development of bone fractures is not a common complication of the procedure. The needle used is usually very thin and does not cause fractures.
The healthcare provider is discussing the potential risks of bone marrow aspiration with a patient. Which statement by the patient indicates a need for further clarification?
Explanation
Bone marrow aspiration is a diagnostic procedure used to evaluate various blood disorders, including leukemia. However, the procedure itself does not lead to the development of leukemia. Leukemia is a separate medical condition that can be diagnosed through bone marrow aspiration.
a. Some discomfort at the needle insertion site is a common side effect of bone marrow aspiration.
b. Excessive bleeding during the procedure is a risk, especially if the patient has a bleeding disorder or is on blood-thinning medications.
d. Some patients may experience significant blood loss during the procedure, necessitating a blood transfusion to replace lost blood components.
The nurse is monitoring a patient who underwent a bone marrow aspiration. What is the most critical complication to assess for during the post-procedure period?
Explanation
The most critical complication to assess for after a bone marrow aspiration is the development of respiratory distress, shortness of breath, or chest pain, as these symptoms may indicate the occurrence of a pneumothorax, a serious condition that requires immediate medical attention.
a. Increased appetite and thirst are not typically associated with complications of bone marrow aspiration.
b. Mild fatigue and drowsiness are common post-procedure effects and do not require immediate concern.
d. Slight redness and swelling at the site are expected after the procedure and are not indicative of a critical complication.
A patient is scheduled to undergo a bone marrow aspiration. What pre-procedure intervention is essential to prevent excessive bleeding during the procedure?
Explanation
Platelets are essential for blood clotting, and a low platelet count can increase the risk of excessive bleeding during a bone marrow aspiration. Checking the patient's platelet count before the procedure allows the healthcare team to assess the risk of bleeding and take appropriate measures if needed.
a. Administering intravenous antibiotics is not a pre-procedure intervention to prevent excessive bleeding during a bone marrow aspiration.
b. Applying a tourniquet to the limb is not a recommended practice for bone marrow aspiration. Tourniquets can impede blood flow and cause complications.
d. Restricting the patient's fluid intake is not a necessary intervention before a bone marrow aspiration. Adequate hydration is essential for the patient's well-being.
The nurse is caring for a patient following a bone marrow aspiration. Which finding requires immediate intervention?
Explanation
Complaints of tingling and numbness in the extremities may indicate nerve injury during the procedure and require immediate intervention and assessment by the healthcare provider.
a. Mild tenderness at the needle insert
ion site is a common side effect and does not require immediate intervention.
b. Bruising and swelling around the aspiration site are expected after the procedure and should subside on their own.
c. A slight elevation in body temperature may be a normal post-procedure response and can be monitored without immediate intervention.
The nurse is providing discharge instructions to a patient who underwent a bone marrow aspiration. What post-procedure follow-up should the nurse recommend?
Explanation
Post-procedure follow-up for bone marrow aspiration includes instructing the patient to monitor the aspiration site for any signs of bleeding or infection. If bleeding occurs, the patient should contact the healthcare provider promptly for further evaluation and intervention.
a. A follow-up appointment in 3 months is not typically required for a routine bone marrow aspiration. Follow-up appointments are usually scheduled within a shorter timeframe after the procedure.
c. It is essential for the patient to rest and avoid vigorous physical activities immediately after the procedure to prevent complications and promote healing.
d. Pain management medications may be prescribed after the procedure to alleviate discomfort and should not be discontinued without consulting the healthcare provider.
The nurse is assessing a patient's post-procedure recovery following a bone marrow aspiration. Which finding would require further investigation?
Explanation
An elevation in body temperature to 100.4°F (38°C) or higher may indicate the development of an infection and requires further investigation and evaluation by the healthcare provider.
a. Mild bruising at the aspiration site is a common post-procedure finding and does not require further investigation unless accompanied by excessive bleeding or other complications.
b. Complaints of fatigue and drowsiness are typical post-procedure effects and do not require immediate concern.
c. Clear drainage at the aspiration site is expected during the healing process and is not indicative of a complication.
The nurse is reviewing the medical record of a patient who had a bone marrow aspiration. What information should the nurse seek in the medical record to plan appropriate post-procedure follow-up care?
Explanation
The patient's CBC results are essential for evaluating the patient's blood cell counts, especially platelet levels, which can help assess the risk of bleeding and guide post-procedure follow-up care.
a. Dietary preferences and restrictions are not directly related to post-procedure follow-up care for a bone marrow aspiration.
b. The date of the patient's last bone marrow aspiration is not relevant for the current post-procedure follow-up care.
d. The patient's family medical history is not directly related to post-procedure follow-up care for a bone marrow aspiration.
A patient underwent a bone marrow aspiration as part of a diagnostic evaluation. What post-procedure care should the nurse prioritize to prevent infection?
Explanation
To prevent infection, the nurse should prioritize keeping the aspiration site clean and dry with sterile dressings. This reduces the risk of contamination and promotes wound healing.
a. Administering intravenous antibiotics for 24 hours post-procedure is not a standard practice for routine bone marrow aspirations unless specifically indicated by the healthcare provider due to the patient's medical history or risk factors.
b. Strict isolation precautions are not necessary after a bone marrow aspiration, as the procedure is typically performed in a sterile environment and does not pose an infectious risk to others.
d. While proper nutrition is important for overall recovery, consuming a high-protein diet is not directly related to preventing infection after a bone marrow aspiration.
The nurse is providing discharge instructions to a patient after a bone marrow aspiration. What activity restriction should the nurse include in the instructions?
Explanation
After a bone marrow aspiration, patients may experience drowsiness or discomfort from the procedure, which can impair their ability to safely operate vehicles or machinery. It is essential to advise the patient to avoid such activities for 24 hours post-procedure.
a. Avoiding all physical activities for the next 2 weeks is not necessary after a bone marrow aspiration. Light activities are usually permitted after the initial recovery period.
b. Restricting movements of the affected limb for 48 hours is not typically required unless specified by the healthcare provider due to complications or the patient's specific condition.
d. Refraining from consuming solid foods for 12 hours post-procedure is not relevant to bone marrow aspiration care. Patients can resume their normal diet unless otherwise indicated by their healthcare provider.
A patient is scheduled to undergo a bone marrow aspiration. Which area is commonly used for the procedure?
Explanation
The sternum is a common site for bone marrow aspiration as it provides easy access to the bone marrow, and the risk of complications is relatively low.
a. The forearm is not typically used for bone marrow aspiration as the bone density is not suitable for the procedure.
c. The calf is not a common site for bone marrow aspiration as it may not provide sufficient access to the bone marrow.
d. The thigh is not a common site for bone marrow aspiration due to the thickness of the muscle and lack of direct access to the bone marrow.
A nurse is preparing a patient for a bone marrow aspiration procedure. What type of anesthesia is typically used for this procedure?
Explanation
Intravenous sedation is commonly used for bone marrow aspiration to provide pain relief and help the patient remain relaxed during the procedure.
a. General anesthesia is not typically used for bone marrow aspiration unless the patient has specific medical conditions that warrant it.
b. Regional anesthesia, such as spinal or epidural anesthesia, is not typically used for bone marrow aspiration.
d. Topical anesthesia is not sufficient for pain relief during a bone marrow aspiration procedure.
The nurse is explaining the purpose of a bone marrow aspiration to a patient. What is the primary purpose of this procedure?
Explanation
The primary purpose of a bone marrow aspiration is to collect a sample of bone marrow for examination and analysis. It helps diagnose various hematological and oncological conditions.
a. Bone marrow aspiration is not used to diagnose diabetes mellitus. Other tests, such as blood glucose levels, are used for diabetes diagnosis.
b. Bone marrow aspiration does not assess liver function. Liver function is typically assessed through blood tests and imaging studies.
c. While bone health may be indirectly evaluated through bone marrow examination, bone marrow aspiration is primarily used for diagnostic purposes rather than evaluating bone health.
A patient is undergoing a bone marrow aspiration procedure. What position is commonly used to perform this procedure?
Explanation
The lateral decubitus position is commonly used for bone marrow aspiration. The patient lies on their side with the knees and hips flexed to provide better access to the sternum or iliac crest.
a. The prone position (lying face down) is not typically used for bone marrow aspiration.
b. The supine position (lying face up) is not the optimal position for bone marrow aspiration as it may limit access to the bone marrow sites.
c. The Trendelenburg position (head down, feet up) is not commonly used for bone marrow aspiration.
The nurse is reviewing a patient's laboratory results before a bone marrow aspiration. Which laboratory parameter is essential to assess before the procedure?
Explanation
Before a bone marrow aspiration, it is essential to assess the patient's CBC results, including platelet count and coagulation factors. This helps determine the patient's ability to clot effectively and assess the risk of bleeding during and after the procedure.
a. Blood glucose levels are not directly related to bone marrow aspiration and are typically not assessed before the procedure.
b. Serum creatinine levels are not directly related to bone marrow aspiration and are typically not assessed before the procedure.
d. Liver function tests (LFTs) are not directly related to bone marrow aspiration and are typically not assessed before the procedure.
The nurse is educating a patient about bone marrow aspiration. Which statement by the patient indicates a need for further teaching?
Explanation
Bone marrow aspiration is typically performed with local anesthesia or intravenous sedation, not general anesthesia. General anesthesia is not commonly used for this procedure.
a. Bone marrow aspiration is used to diagnose various hematological conditions, including anemia, so this statement is accurate.
b. Fasting before the procedure is necessary to reduce the risk of aspiration during the procedure and is an appropriate instruction.
d. Bone marrow aspiration can be performed from various sites, including the sternum, iliac crest, or other bones, so this statement is accurate.
A nurse is preparing to assist with a bone marrow aspiration procedure. What equipment should the nurse ensure is readily available for the procedure?
Explanation
Specimen collection tubes are essential for collecting the bone marrow sample during the aspiration procedure.
a. A nebulizer and oxygen mask are not directly related to bone marrow aspiration and are not typically required for the procedure.
b. A suture removal kit is not needed for bone marrow aspiration.
d. A blood pressure cuff and stethoscope are not directly related to bone marrow aspiration and are not typically required for the procedure.
A patient is anxious about the upcoming bone marrow aspiration. What action by the nurse is most appropriate to help alleviate the patient's anxiety?
Explanation
Encouraging the patient to distract themselves can help alleviate anxiety before the procedure. It allows the patient to focus on something other than the procedure, reducing stress.
a. Administering a sedative medication may be appropriate if ordered by the healthcare provider, but it should not be the first option for addressing anxiety.
b. Providing too much detailed information about potential complications can increase the patient's anxiety. The nurse should offer information in a reassuring and concise manner.
d. Informing the patient that bone marrow aspirations are always painful is incorrect and may cause unnecessary anxiety. The nurse should explain that discomfort can vary among individuals, and pain management measures will be provided during the procedure.
A patient is post-procedure after a bone marrow aspiration. What position should the nurse instruct the patient to assume for at least 30 minutes after the procedure?
Explanation
After a bone marrow aspiration, the nurse should instruct the patient to assume the lateral decubitus position with the knees flexed to help minimize the risk of bleeding and promote clotting at the aspiration site.
a. The supine position with legs elevated is not typically recommended after a bone marrow aspiration as it does not promote clotting at the aspiration site.
b. Lying flat on the abdomen is not recommended after a bone marrow aspiration as it may put pressure on the aspiration site and increase the risk of bleeding.
c. The semi-Fowler's position with the head elevated may be used for comfort, but it does not specifically address clotting at the aspiration site.
The nurse is preparing to perform a bone marrow aspiration on a patient. What is the primary purpose of the bone marrow aspiration?
Explanation
The primary purpose of a bone marrow aspiration is to collect a sample of bone marrow for examination and analysis, aiding in the diagnosis of various hematological and oncological conditions.
a. Bone marrow aspiration is not used to assess liver function. Liver function is typically evaluated through blood tests and imaging studies.
b. Bone marrow aspiration is not used to diagnose diabetes mellitus. Diabetes diagnosis involves blood glucose level monitoring and other specific tests.
d. While bone health may be indirectly evaluated through bone marrow examination, the primary purpose of bone marrow aspiration is not to evaluate bone health.
Paget’s Disease
What is Paget's disease?
Explanation
Paget's disease is a metabolic bone disorder that involves abnormal bone remodeling, leading to areas of increased bone density and disorganized bone formation. It is not a genetic disorder, autoimmune disease, or neurological disorder.
a. A genetic disorder characterized by abnormal bone density: While Paget's disease has a genetic component, it is not solely a genetic disorder. The condition involves both genetic and environmental factors.
b. An autoimmune disease affecting the joints and connective tissues: Paget's disease is not an autoimmune disease. It primarily affects bone structures, not joints and connective tissues.
d. A degenerative neurological disorder causing muscle weakness: Paget's disease is not a neurological disorder. It does not directly affect the nervous system or cause muscle weakness.
What is the most common age group affected by Paget's disease?
Explanation
Paget's disease most commonly affects older adults, typically those over the age of 60. While it can occur at any age, the prevalence increases with age.
a. Children and adolescents: Paget's disease is rare in children and adolescents. It is more commonly seen in older individuals.
b. Young adults (ages 20-40): While Paget's disease can occur in young adults, it is less common in this age group compared to older adults.
c. Middle-aged adults (ages 40-60): While Paget's disease can occur in middle-aged adults, it is more commonly seen in older individuals.
Which of the following bones is often affected in Paget's disease?
Explanation
The femur, which is the thigh bone, is often affected in Paget's disease. The condition commonly involves the axial skeleton, such as the skull, spine, and pelvis, as well as the long bones like the femur.
a. Humerus (arm bone): The humerus can be affected in Paget's disease, but it is not as commonly involved as the femur.
b. Radius (forearm bone): The radius can be affected in Paget's disease, but it is not as commonly involved as the femur.
d. Fibula (lower leg bone): The fibula can be affected in Paget's disease, but it is not as commonly involved as the femur.
What are the typical clinical manifestations of Paget's disease?
Explanation
The typical clinical manifestations of Paget's disease include bone pain, bone deformities (e.g., enlarged skull, bowed legs), and an increased risk of fractures due to the weakened and structurally abnormal bones. Joint pain and gastrointestinal disturbances are not primary features of Paget's disease.
a. Joint pain and stiffness: Joint pain and stiffness are more characteristic of arthritis or other joint-related conditions, not the primary clinical manifestations of Paget's disease.
b. Muscle weakness and fatigue: While Paget's disease can cause discomfort and reduced mobility, it is not primarily associated with muscle weakness and fatigue.
d. Gastrointestinal disturbances and weight loss: Paget's disease primarily affects bone structures, and gastrointestinal disturbances and weight loss are not typical clinical manifestations of the condition.
What is the etiology of Paget's disease?
Explanation
The etiology of Paget's disease involves a combination of genetic factors and environmental triggers. There is evidence of a genetic predisposition, but environmental factors also play a role in the development of the condition. Viral and bacterial infections, as well as dietary deficiencies, are not considered primary causes of Paget's disease.
a. Viral infection: Paget's disease is not caused by a viral infection.
b. Bacterial infection: Paget's disease is not caused by a bacterial infection.
d. Dietary deficiencies: While nutrition is important for bone health, dietary deficiencies are not the primary cause of Paget's disease. Genetic and environmental factors are more influential in its development.
What is the underlying pathophysiology of Paget's disease?
Explanation
The underlying pathophysiology of Paget's disease involves increased bone turnover and disordered bone remodeling. Osteoclasts, the bone-resorbing cells, become overactive, leading to excessive bone resorption. Osteoblasts, the bone-forming cells, attempt to repair the resorbed bone, but their activity is disordered, resulting in the formation of structurally abnormal bone.
a. Decreased bone density due to calcium deficiency: This is the pathophysiology of osteoporosis, not Paget's disease. In Paget's disease, bone density can be normal or increased due to the disordered bone remodeling.
c. Excessive collagen production leading to bone deformities: Excessive collagen production is not a characteristic feature of Paget's disease. The condition primarily involves abnormal bone remodeling by osteoclasts and osteoblasts.
d. Autoimmune attack on osteoblasts causing bone destruction: Paget's disease is not an autoimmune disorder. The disease is characterized by increased bone resorption and disordered bone formation, not an immune-mediated attack on osteoblasts.
Which cell type is primarily responsible for the increased bone resorption seen in Paget's disease?
Explanation
Osteoclasts are the primary cell type responsible for bone resorption in Paget's disease. These cells become overactive, leading to excessive bone breakdown, which is a hallmark of the condition.
a. Osteocytes: Osteocytes are mature bone cells embedded in the bone matrix. While they play a role in maintaining bone health, they are not directly responsible for bone resorption.
b. Osteoblasts: Osteoblasts are bone-forming cells. In Paget's disease, they attempt to repair the resorbed bone but their activity is disordered, leading to structurally abnormal bone formation.
d. Osteoprogenitor cells: Osteoprogenitor cells are undifferentiated cells that can differentiate into osteoblasts. They are not directly involved in the increased bone resorption seen in Paget's disease.
What is the typical pattern of bone involvement in Paget's disease?
Explanation
The typical pattern of bone involvement in Paget's disease is characterized by patchy areas of increased bone density (osteosclerosis) and disorganized bone formation. These areas of abnormal bone remodeling result in structurally weak and misshapen bones.
a. Uniform increase in bone density throughout the skeleton: This pattern of bone density is not characteristic of Paget's disease. The condition involves localized areas of increased density rather than uniform changes.
b. Focal areas of bone demineralization scattered throughout the skeleton: This pattern of bone demineralization is more characteristic of osteoporosis, not Paget's disease.
c. Diffuse increase in bone density with areas of focal bone loss: This pattern is not typical of Paget's disease. The condition primarily involves areas of increased bone density and disordered bone remodeling.
Which bone structures are commonly affected by Paget's disease?
Explanation
Paget's disease commonly affects the axial skeleton, including the skull, spine, and pelvis. The bones in these areas are often involved in the patchy areas of increased bone density and disorganized bone remodeling seen in the condition.
a. Long bones of the extremities: While long bones can be affected by Paget's disease, the axial skeleton is more commonly involved.
c. Hands and feet: The hands and feet can be affected by Paget's disease, but the axial skeleton is more frequently involved.
d. Ribs and sternum: The ribs and sternum can be affected by Paget's disease, but the axial skeleton, including the skull, spine, and pelvis, is more commonly affected.
How does Paget's disease differ from osteoporosis?
Explanation
The main difference between Paget's disease and osteoporosis is in the underlying bone remodeling. Paget's disease is characterized by increased bone turnover and disordered bone formation, while osteoporosis involves decreased bone formation and increased bone resorption.
a. Paget's disease is characterized by decreased bone density, while osteoporosis is associated with increased bone density: This statement is incorrect. In Paget's disease, bone density can be normal or increased due to the disordered bone remodeling.
b. Paget's disease primarily affects trabecular bone, while osteoporosis affects cortical bone: This statement is incorrect. Both Paget's disease and osteoporosis can affect both trabecular and cortical bone.
d. Paget's disease is an autoimmune disorder, while osteoporosis is caused by hormonal imbalances: This statement is incorrect. Paget's disease is not an autoimmune disorder, and osteoporosis is not solely caused by hormonal imbalances. Both conditions have complex multifactorial etiologies.
A client with Paget's disease presents with bone pain. What other clinical manifestation should the nurse expect to find during the assessment?
Explanation
Bone pain is a common clinical manifestation of Paget's disease, but another hallmark of the condition is the development of bone deformities. The abnormal bone remodeling in Paget's disease can lead to enlarged, misshapen bones, particularly in weight-bearing areas such as the skull, pelvis, and long bones.
a. Muscle weakness: While bone pain can lead to discomfort and reduced mobility, muscle weakness is not a specific clinical manifestation of Paget's disease.
b. Hypercalcemia: Hypercalcemia (elevated blood calcium levels) is not typically associated with Paget's disease. Instead, the condition is characterized by disorganized bone remodeling.
c. Joint swelling: Joint swelling is not a primary clinical manifestation of Paget's disease. Bone deformities are more characteristic of the condition.
The nurse is assessing a client with suspected Paget's disease. Which skeletal finding should the nurse prioritize during the physical examination?
Explanation
Bowing of long bones is a characteristic skeletal finding in Paget's disease. The abnormal bone remodeling can lead to bone bowing and misalignment, particularly in the long bones of the arms and legs.
a. Scoliosis: Scoliosis is a lateral curvature of the spine and is not directly associated with Paget's disease. It may be related to other musculoskeletal conditions.
b. Kyphosis: Kyphosis is an excessive forward curvature of the spine, often seen in conditions like osteoporosis, but it is not a primary finding in Paget's disease.
c. Bone tenderness: Bone tenderness may be present due to the bone inflammation and pain associated with Paget's disease, but it is not a specific skeletal finding.
The nurse is performing a physical assessment on a client with Paget's disease. Which finding should the nurse attribute to the increased bone turnover and remodeling characteristic of this condition?
Explanation
The increased bone turnover and remodeling in Paget's disease can cause warmth and erythema (redness) over the affected bones. This is due to the increased blood flow and metabolic activity in the affected areas.
a. Cool, clammy skin: Cool, clammy skin is not directly related to the increased bone turnover and remodeling in Paget's disease. It may be related to other factors, such as circulation or environmental conditions.
b. Pulsating chest pain: Pulsating chest pain is not a typical finding in Paget's disease. It may be related to other cardiac or respiratory conditions.
d. Enlarged skull circumference: An enlarged skull circumference is a common manifestation of Paget's disease, but it is not directly related to the increased bone turnover and remodeling. It results from excessive bone growth in the skull bones.
A client with Paget's disease experiences frequent headaches. Which cranial finding should the nurse assess for during the neurological examination?
Explanation
Enlarged frontal bossing (prominent forehead) is a cranial finding often seen in clients with Paget's disease due to increased bone growth in the skull bones. This can cause pressure and contribute to headaches.
a. Nystagmus: Nystagmus is an involuntary, rhythmic movement of the eyes and is not directly associated with Paget's disease.
b. Diplopia: Diplopia, or double vision, is not a typical finding in Paget's disease. It may be related to other neurological or ocular conditions.
c. Papilledema: Papilledema is swelling of the optic disc due to increased intracranial pressure. While headaches can be associated with Paget's disease, papilledema is not a common manifestation of the condition.
A client with Paget's disease complains of bone pain that worsens with activity. What is the underlying cause of this pain?
Explanation
The bone pain experienced by clients with Paget's disease is often due to microfractures and inflammation in the affected bones. The increased bone turnover and remodeling lead to weaker bones, making them more susceptible to microfractures. The inflammation at the site of these microfractures contributes to the pain, which worsens with activity.
a. Decreased blood flow to bones: Paget's disease does not typically cause decreased blood flow to bones. Instead, the condition leads to increased vascularity in affected bones.
b. Bone infarction: Bone infarction (death of bone tissue due to inadequate blood supply) is not a characteristic feature of Paget's disease. Microfractures and inflammation are more common causes of bone pain in this condition.
d. Compression of nerve roots: While nerve compression can cause bone pain, it is not a primary mechanism of pain in Paget's disease. The pain is primarily related to bone remodeling and inflammation.
A client presents with bone pain, joint stiffness, and an enlarged skull. Which diagnostic test is most likely to confirm the diagnosis of Paget's disease?
Explanation
A bone scan is the most appropriate diagnostic test for confirming the diagnosis of Paget's disease. It can reveal increased bone turnover and abnormal bone remodeling patterns characteristic of the condition. The bone scan can show "hot spots" of increased uptake in affected bones.
a. Complete blood count (CBC): While a CBC can be useful in ruling out other conditions, it does not directly diagnose Paget's disease. Specific bone imaging is required for confirmation.
c. Liver function tests (LFTs): Liver function tests are not used to diagnose Paget's disease. The condition primarily affects bone structures, and liver involvement is not a primary concern.
d. Magnetic resonance imaging (MRI): While an MRI can provide detailed images of bones and soft tissues, it may not be the initial choice for diagnosing Paget's disease. A bone scan is more specific to evaluate bone turnover and remodeling.
The healthcare provider suspects a client may have Paget's disease based on clinical presentation. Which laboratory test should be ordered to aid in the diagnosis?
Explanation
An elevated alkaline phosphatase (ALP) level is a common finding in patients with Paget's disease. ALP is an enzyme present in bone cells, and its increased activity is indicative of increased bone turnover and remodeling seen in Paget's disease.
a. Serum calcium level: Serum calcium levels may be affected in Paget's disease due to abnormal bone remodeling, but they are not specific enough to confirm the diagnosis on their own.
b. Erythrocyte sedimentation rate (ESR): The ESR is a marker of inflammation and is not specific to Paget's disease. While it may be elevated due to bone inflammation, it does not confirm the diagnosis.
d. Serum creatinine level: Serum creatinine levels are not directly related to the diagnosis of Paget's disease. They are typically assessed to evaluate kidney function.
The healthcare provider orders an X-ray of a patient's bones due to suspicion of Paget's disease. What finding on the X-ray would support the diagnosis?
Explanation
The characteristic X-ray finding in Paget's disease is bony overgrowth and thickening of the affected bones. This is due to the increased bone turnover and abnormal remodeling associated with the condition.
a. Decreased bone density: Decreased bone density is associated with osteoporosis, not Paget's disease. In Paget's disease, bone density is often normal or increased due to the disorganized bone remodeling.
b. Erosions and bone cysts: Erosions and bone cysts are not specific to Paget's disease and may be seen in other bone conditions. Bony overgrowth is more characteristic of Paget's disease.
d. Presence of osteoporotic fractures: Osteoporotic fractures are not typically associated with Paget's disease. The increased bone density and thickening in Paget's disease can actually make bones more resistant to fractures.
The healthcare provider suspects Paget's disease in a patient. Which imaging modality is most useful for assessing the extent and severity of bone involvement?
Explanation
X-rays are the most useful imaging modality for assessing the extent and severity of bone involvement in Paget's disease. X-rays can reveal the characteristic bony overgrowth and thickening, as well as any bone deformities and fractures.
b. Computed tomography (CT) scan: CT scans can provide detailed images of bones and soft tissues, but they may not be the initial choice for evaluating Paget's disease. X-rays are more specific for the condition.
c. Magnetic resonance imaging (MRI): While an MRI can provide detailed images of bones and soft tissues, it may not be the first-line imaging choice for evaluating Paget's disease. X-rays are more specific for bone involvement.
d. Bone densitometry (DXA scan): Bone densitometry is used to assess bone mineral density and is commonly used for conditions like osteoporosis. It may not provide the necessary information for evaluating Paget's disease.
A patient with suspected Paget's disease undergoes a bone biopsy. What is the primary purpose of the bone biopsy in diagnosing this condition?
Explanation
The primary purpose of a bone biopsy in diagnosing Paget's disease is to examine bone tissue for characteristic changes that confirm the diagnosis. Microscopic examination of the bone tissue can reveal the disorganized bone remodeling and other characteristic features of the condition.
a. To assess calcium levels in the bone: Bone biopsies are not performed to assess calcium levels in the bone. Other diagnostic tests, such as blood tests, are used for that purpose.
b. To confirm the presence of bone tumors: Paget's disease is not a bone tumor, and the biopsy is not performed to confirm the presence of tumors. The biopsy confirms the specific bone changes associated with the condition.
c. To evaluate bone density and strength: Bone biopsies do not directly evaluate bone density and strength. Other imaging modalities, such as X-rays and DXA scans, are used for assessing bone density.
The nurse is providing education about medication management for a client with Paget's disease. Which medication is commonly used as the first-line treatment for this condition?
Explanation
Bisphosphonates are commonly used as the first-line treatment for Paget's disease. They work by slowing down bone resorption and promoting more balanced bone remodeling, helping to control the excessive bone turnover characteristic of the condition.
a. Calcium supplements: While calcium supplements are essential for overall bone health, they are not the first-line treatment for Paget's disease. Bisphosphonates specifically target the abnormal bone remodeling associated with the condition.
b. Nonsteroidal anti-inflammatory drugs (NSAIDs): NSAIDs may help manage pain and inflammation associated with Paget's disease, but they do not directly address the underlying bone remodeling abnormalities. Bisphosphonates are more effective in treating the condition.
d. Vitamin D supplements: Vitamin D is necessary for calcium absorption and bone health, but it is not the primary treatment for Paget's disease. Bisphosphonates are the mainstay of therapy.
The nurse is discussing dietary recommendations with a client diagnosed with Paget's disease. What dietary modification is important for this client?
Explanation
Increasing calcium intake is important for individuals with Paget's disease to support bone density and strength. Adequate calcium intake is essential for overall bone health and can help counteract the effects of abnormal bone remodeling seen in Paget's disease.
a. Increase sodium intake to promote bone health: High sodium intake can lead to calcium excretion, which may be detrimental to bone health. Reducing sodium intake is beneficial for overall bone health.
b. Limit caffeine consumption to reduce bone resorption: While excessive caffeine intake may affect calcium absorption, moderate caffeine consumption is not directly related to Paget's disease. Calcium intake is more critical for managing the condition.
c. Reduce protein intake to prevent bone deformities: Protein intake is essential for tissue repair and bone health. Restricting protein intake is not recommended for individuals with Paget's disease, as it can impact overall health.
The nurse is monitoring a client receiving bisphosphonate therapy for Paget's disease. Which laboratory parameter should the nurse prioritize monitoring during treatment?
Explanation
Monitoring serum calcium levels is important during bisphosphonate therapy for Paget's disease. Bisphosphonates can affect calcium metabolism, and monitoring calcium levels helps ensure appropriate dosing and prevent complications such as hypocalcemia or hypercalcemia.
a. Liver function tests (LFTs): Bisphosphonates generally do not have a significant impact on liver function. Monitoring LFTs is not a primary concern during bisphosphonate therapy.
c. Blood glucose levels: Bisphosphonate therapy is not known to affect blood glucose levels. Monitoring blood glucose is not directly related to Paget's disease treatment.
d. Complete blood count (CBC): Bisphosphonate therapy does not typically have a major effect on blood cell counts. Monitoring a CBC is not a primary concern during bisphosphonate treatment for Paget's disease.
The nurse is instructing a client with Paget's disease about self-care measures to manage bone pain. Which self-care measure should the nurse recommend?
Explanation
Engaging in gentle stretching exercises can help relieve bone pain and improve joint flexibility for individuals with Paget's disease. These exercises promote joint mobility and may help alleviate discomfort associated with bone deformities.
a. Applying cold compresses to affected areas: Applying cold compresses may provide some temporary relief for pain, but they do not address the underlying bone remodeling abnormalities in Paget's disease.
b. Limiting physical activity to reduce pain: While excessive physical activity may need to be moderated to prevent fractures, limiting all physical activity is not advisable for patients with Paget's disease. Gentle exercises can support bone health and overall well-being.
c. Taking hot baths to relieve discomfort: Hot baths may provide temporary relief for muscle discomfort, but they do not directly address bone pain associated with Paget's disease.
The nurse is assessing a client with Paget's disease for potential complications. Which complication should the nurse prioritize monitoring?
Explanation
A potential complication of Paget's disease is an increased risk of pathologic fractures. The abnormal bone remodeling weakens the bones, leading to an increased susceptibility to fractures.
a. Hypertension: Hypertension is not a direct complication of Paget's disease. The condition primarily affects bone structures.
c. Hyperthyroidism: Hyperthyroidism is not associated with Paget's disease. It is a separate condition related to thyroid gland dysfunction.
d. Type 2 diabetes mellitus: Type 2 diabetes mellitus is not a complication of Paget's disease. The conditions are unrelated and have different underlying causes.
The nurse is providing patient education to a client with Paget's disease. Which statement by the client indicates an understanding of the condition?
Explanation
Bisphosphonate medications are commonly prescribed for Paget's disease to slow down bone resorption and promote more balanced bone remodeling. Taking bisphosphonates with a full glass of water or milk helps ensure proper absorption and reduce the risk of gastrointestinal irritation.
a. "Paget's disease is a type of cancer that affects the bones." This statement is incorrect. Paget's disease is not a type of cancer but a chronic, non-cancerous condition characterized by abnormal bone remodeling.
b. "This condition is caused by a deficiency in vitamin D." This statement is incorrect. While vitamin D plays a role in bone health, Paget's disease is primarily a result of genetic factors that lead to abnormal bone remodeling.
c. "I should avoid weight-bearing exercises to prevent fractures." This statement is incorrect. Moderate weight-bearing exercises, under healthcare provider guidance, can help maintain bone strength and reduce the risk of fractures in individuals with Paget's disease.
The nurse is teaching a client with Paget's disease about potential complications. What complication should the nurse prioritize?
Explanation
A potential complication of Paget's disease is an increased risk of bone fractures. The abnormal bone remodeling in Paget's disease weakens the bones, leading to an increased susceptibility to fractures.
a. Hypertension: Hypertension is not a direct complication of Paget's disease. The condition primarily affects bone structures.
c. Hypothyroidism: Hypothyroidism is not associated with Paget's disease. It is a separate condition related to thyroid gland dysfunction.
d. Kidney stones: While kidney stones may be unrelated to Paget's disease, they can be a complication of other conditions or metabolic disorders.
The nurse is discussing self-care measures with a client newly diagnosed with Paget's disease. Which self-care measure is appropriate for the client to implement?
Explanation
Engaging in low-impact exercises is an appropriate self-care measure for individuals with Paget's disease. Low-impact exercises, such as walking and swimming, can help support bone health, joint mobility, and overall physical well-being.
a. Massaging affected areas to reduce swelling: Massaging affected areas may exacerbate bone deformities and lead to increased pain. It is not recommended for individuals with Paget's disease.
b. Taking over-the-counter anti-inflammatory medications: Over-the-counter anti-inflammatory medications may not be sufficient to manage the inflammation and pain associated with Paget's disease. Prescribed medications are more effective in managing the condition.
d. Applying heat to affected joints to relieve pain: Applying heat may provide temporary relief for some individuals, but it is not the primary method for managing bone pain in Paget's disease. Prescribed medications and exercises are more effective approaches.
The nurse is educating a client with Paget's disease about the importance of calcium and vitamin D intake. What is the rationale for this education?
Explanation
Calcium and vitamin D help reduce the risk of bone fractures in Paget's disease.
Explanation: Adequate calcium and vitamin D intake are essential for maintaining bone health and reducing the risk of bone fractures, especially in individuals with Paget's disease. While these nutrients do not cure Paget's disease, they play a crucial role in supporting bone strength and density.
a. Calcium and vitamin D can prevent the development of Paget's disease: This statement is incorrect. Paget's disease is primarily a result of genetic factors, and calcium and vitamin D intake do not prevent its development.
c. Calcium and vitamin D can cure Paget's disease: This statement is incorrect. While calcium and vitamin D are important for bone health, they do not cure Paget's disease. Treatment usually involves medications to manage the condition.
d. Calcium and vitamin D decrease bone turnover in Paget's disease: This statement is not entirely accurate. Calcium and vitamin D do not directly decrease bone turnover in Paget's disease. Medications like bisphosphonates are prescribed to address bone remodeling.
The nurse is teaching a client with Paget's disease about the importance of regular follow-up appointments with the healthcare provider. What is the rationale for this education?
Explanation
Regular follow-up appointments with the healthcare provider are essential for clients with Paget's disease to monitor for potential complications and disease progression. Periodic evaluations help assess bone health, check for bone deformities, and adjust the treatment plan if necessary.
b. To obtain prescriptions for pain medications: While pain management may be addressed during follow-up appointments, it is not the primary reason for regular visits. Pain medications can be prescribed as needed.
c. To receive physical therapy for bone pain: Physical therapy may be part of the treatment plan for managing bone pain, but it does not solely warrant regular follow-up appointments.
d. To assess calcium and vitamin D levels: Calcium and vitamin D levels may be assessed, but they are not the main focus of regular follow-up appointments. The primary purpose is to monitor the condition's progression and assess for potential complications.
When caring for a patient with Paget's disease, the nurse should prioritize which intervention?
Explanation
A. Encouraging high-impact exercises to strengthen bones:
High-impact exercises are contraindicated in patients with Paget's disease due to the risk of fractures and bone injury. Low-impact and weight-bearing exercises are safer to maintain bone health and improve mobility.
B. Monitoring serum calcium levels regularly: Paget's disease often requires treatment with bisphosphonates or calcitonin to regulate bone remodeling. These treatments can affect calcium levels, potentially leading to hypocalcemia. Regular monitoring is crucial to detect and manage these imbalances.
C. Assisting with range-of-motion exercises to maintain joint mobility: While maintaining joint mobility is important, this is not the priority intervention. ROM exercises can be part of the overall care plan but do not address the critical metabolic imbalances associated with Paget's disease.
D. Administering corticosteroids to reduce inflammation: Corticosteroids are not a standard treatment for Paget's disease. Instead, the focus is on medications like bisphosphonates or calcitonin to regulate bone turnover.
Which precaution is essential when caring for a patient with Paget's disease?
Explanation
Contact precautions are essential when caring for a patient with Paget's disease. The disease involves abnormal bone remodeling, leading to bone deformities and increased bone turnover. Close contact with the patient's body or potentially contaminated objects should be minimized to prevent transmission of the disease.
a. Airborne precautions: Paget's disease is not transmitted through the airborne route. Airborne precautions are used for diseases that spread through respiratory droplets.
b. Droplet precautions: Paget's disease is not transmitted through droplets. Droplet precautions are used for diseases spread through respiratory droplets.
c. Standard precautions: While standard precautions are essential for all patients to prevent transmission of infections, specific precautions for Paget's disease involve contact precautions.
The nurse should encourage patients with Paget's disease to maintain which dietary intake?
Explanation
Patients with Paget's disease should be encouraged to maintain a high-calcium diet to support bone health. Adequate calcium intake is essential for bone strength and density, and it can help counteract the effects of abnormal bone remodeling seen in Paget's disease.
b. High-phosphorus diet: While phosphorus is also important for bone health, a high-phosphorus diet is not specific to Paget's disease. It is more relevant for patients with renal disorders.
c. High-vitamin D diet: Vitamin D is necessary for calcium absorption and bone health. However, a high-vitamin D diet is not specific to Paget's disease. Vitamin D supplements may be recommended if a deficiency is present.
d. Low-potassium diet: Potassium intake is not directly related to Paget's disease. Potassium is an essential mineral for various bodily functions, but it is not a focus in the management of the condition.
Which symptom should the nurse closely monitor for in patients with Paget's disease?
Explanation
Joint stiffness is a common symptom in patients with Paget's disease, especially when bone deformities are present. The nurse should closely monitor for any changes in joint mobility and range of motion, as joint stiffness can impact the patient's ability to perform daily activities.
a. Weight gain: Weight gain is not a specific symptom of Paget's disease. It is not directly related to the condition.
c. Hyperactivity: Hyperactivity is not a characteristic symptom of Paget's disease. The condition primarily affects bone structures.
d. Blurred vision: Blurred vision is not associated with Paget's disease. It is not a symptom commonly observed in individuals with the condition.
Which nursing intervention is essential when caring for a patient with Paget's disease experiencing bone pain?
Explanation
Administering nonsteroidal anti-inflammatory drugs (NSAIDs) is an essential nursing intervention for managing bone pain in patients with Paget's disease. NSAIDs can help reduce inflammation and alleviate pain associated with bone deformities.
a. Applying cold compresses to the affected area: Applying cold compresses may provide some temporary relief, but it is not the primary intervention for managing bone pain in Paget's disease. NSAIDs are more effective for managing inflammation and pain.
c. Elevating the affected extremity: Elevating the affected extremity is not a specific intervention for managing bone pain in Paget's disease. It may be useful for managing other conditions, such as edema, but not for addressing bone pain.
d. Encouraging bed rest: While rest is important for managing pain, encouraging prolonged bed rest is not advisable for patients with Paget's disease. Moderate physical activity is essential for overall bone health and joint mobility.
Paget's disease is a disorder primarily affecting which part of the body?
Explanation
Paget's disease is a bone disorder that causes abnormal bone remodeling, leading to enlarged, weak, and deformed bones.
a. Muscles: Paget's disease primarily affects bones, not muscles. While muscles surrounding affected bones may be impacted indirectly, they are not the primary target of the disease.
c. Skin: Paget's disease does not affect the skin. It is a bone disorder and does not involve the skin.
d. Lungs: Paget's disease does not directly affect the lungs. The disease primarily involves bone remodeling, not lung function.
Which of the following is a common clinical manifestation of Paget's disease?
Explanation
The most common clinical manifestation of Paget's disease is bone pain and deformities due to abnormal bone remodeling and increased bone turnover.
a. Severe joint pain: While joint pain can occur in Paget's disease due to bone involvement, it is not the most common manifestation. Bone pain and deformities are more characteristic.
b. Unexplained weight loss: Unexplained weight loss is not a typical symptom of Paget's disease. It is not directly related to the bone disorder.
c. Visual disturbances: Visual disturbances are not associated with Paget's disease. This condition primarily affects bones, not the eyes or vision.
Which diagnostic test is commonly used to confirm the diagnosis of Paget's disease?
Explanation
X-ray imaging is commonly used to confirm the diagnosis of Paget's disease. X-rays can show characteristic bone changes, such as bone enlargement, thickening, and deformities, which are indicative of Paget's disease.
a. Bone density scan: While bone density scans may be useful to assess bone health in other conditions, they are not the primary diagnostic tool for Paget's disease. X-rays are preferred.
b. Magnetic resonance imaging (MRI): MRI may provide detailed images of bones and surrounding soft tissues, but it is not the first-line diagnostic test for Paget's disease. X-rays are more commonly used.
d. Blood glucose test: A blood glucose test is used to diagnose and monitor diabetes, not Paget's disease. These conditions are unrelated.
Paget's disease can lead to an increased risk of which complication?
Explanation
Paget's disease can weaken bones, leading to an increased risk of bone fractures. The abnormal bone remodeling and increased bone turnover can result in bones that are more susceptible to breaking.
a. Heart attack: Paget's disease primarily affects bones, not the cardiovascular system. There is no direct association between Paget's disease and an increased risk of heart attacks.
b. Stroke: Paget's disease does not increase the risk of stroke. Stroke is a condition primarily related to the brain and blood vessels, not bones.
c. Osteoporosis: While both Paget's disease and osteoporosis involve changes in bone density, they are distinct conditions. Paget's disease leads to enlarged and weakened bones, while osteoporosis leads to decreased bone density and increased fracture risk.
Which of the following is the goal of treatment for Paget's disease?
Explanation
The goal of treatment for Paget's disease is to relieve pain and prevent complications associated with bone deformities and fractures. There is no cure for Paget's disease, but treatment aims to manage symptoms and reduce the risk of complications.
a. Cure the disease completely: Paget's disease is a chronic condition with no known cure. Treatment focuses on symptom management and preventing complications.
c. Restore normal bone density: While treatment may aim to reduce abnormal bone remodeling, restoring normal bone density is not typically achievable. The focus is on pain relief and preventing complications.
d. Regenerate damaged bones: While treatment may improve bone health and reduce deformities, regenerating damaged bones to their original state is not feasible. Treatment aims to manage the disease and its consequences effectively.
Which nursing intervention is important when caring for a patient with Paget's disease?
Explanation
Assisting with range-of-motion exercises is important when caring for a patient with Paget's disease. Range-of-motion exercises can help maintain joint mobility and prevent joint contractures, which may occur due to bone changes in the disease.
a. Encouraging bed rest to prevent fractures: Bed rest is not recommended for individuals with Paget's disease, as it can lead to muscle weakness and joint stiffness.
c. Administering corticosteroids to reduce inflammation: Corticosteroids are not typically used to treat Paget's disease, as they do not address the underlying bone changes.
d. Providing a high-calcium diet: While adequate calcium intake is important for bone health, a high-calcium diet is not a specific nursing intervention for Paget's disease. Bisphosphonates are typically prescribed to address bone changes.
What is a potential complication of Paget's disease?
Explanation
A potential complication of Paget's disease is an increased risk of fractures. The abnormal bone remodeling and weakening of bone structures in Paget's disease can lead to an increased susceptibility to fractures.
a. Hypertension: Hypertension is not a direct complication of Paget's disease. The condition primarily affects bone structures.
b. Osteoporosis: Paget's disease is not a form of osteoporosis. While both conditions involve bone changes, they have distinct pathophysiological mechanisms.
d. Type 2 diabetes mellitus: Type 2 diabetes mellitus is not a complication of Paget's disease. The conditions are unrelated and have different underlying causes.
Paget's disease is most commonly observed in which age group?
Explanation
Paget's disease is most commonly observed in older adults, typically over the age of 40. It is more prevalent in the elderly population.
a. Children and adolescents: While Paget's disease can occur in younger individuals, it is much more common in older adults.
b. Young adults: Paget's disease is not commonly observed in young adults. It typically develops later in life.
c. Middle-aged adults: While Paget's disease can occur in middle-aged adults, it is more commonly seen in older adults.
Which of the following statements about Paget's disease is true?
Explanation
Paget's disease has a genetic component, and there is evidence of familial inheritance. Individuals with a family history of Paget's disease are at a higher risk of developing the condition.
b. It is caused by vitamin D deficiency: Paget's disease is not caused by vitamin D deficiency. It is primarily a result of genetic factors leading to abnormal bone remodeling.
c. It primarily affects the hands and feet: Paget's disease can affect various bones in the body, not just the hands and feet. It commonly involves the pelvis, vertebrae, and ribs.
d. It is a rare condition with a prevalence of less than 1%: Paget's disease is not considered rare. It is relatively common, particularly in older adults, with a prevalence estimated to be around 1-3% in individuals over the age of 40.
Which of the following activities should individuals with Paget's disease be encouraged to perform to promote bone health?
Explanation
Individuals with Paget's disease should be encouraged to engage in walking and low-impact exercises to promote bone health. These activities are less likely to cause fractures or stress on the bones while still supporting bone strength and density.
a. Participating in high-impact sports: High-impact sports can put excessive stress on the bones and increase the risk of fractures in individuals with Paget's disease. It is not recommended.
b. Limiting physical activity to avoid fractures: While excessive physical activity may need to be moderated to prevent fractures, limiting all physical activity is not advisable. Moderate exercise is essential for overall health and bone strength.
d. Heavy weightlifting: Heavy weightlifting can increase the risk of fractures in individuals with Paget's disease. It is not recommended, as it can put excessive stress on the bones.
Fractures
What is the definition of a fracture?
Explanation
A fracture is a break in the continuity of a bone, resulting from excessive force or stress applied to the bone. It is different from a dislocation, which involves the displacement of bone from its normal position at a joint.
a. A dislocation of a joint: A dislocation involves the displacement of bone from its normal position at a joint and is not the same as a fracture.
c. A stretching or tearing of ligaments: A stretching or tearing of ligaments is known as a sprain, not a fracture.
d. A separation of bone fragments at a joint: This description is more in line with a dislocation, where the bone separates from its normal position at a joint.
Which of the following types of fractures involves the bone breaking into multiple pieces?
Explanation
In a comminuted fracture, the bone is broken into multiple pieces, which may require more complex treatment and longer healing time.
a. Greenstick fracture: A greenstick fracture involves the bone bending and partially breaking, commonly seen in children. It does not result in multiple pieces.
b. Transverse fracture: A transverse fracture occurs when the bone breaks straight across its long axis, but it does not involve multiple pieces.
d. Spiral fracture: A spiral fracture is characterized by a twisting or spiraling break along the bone, but it does not result in multiple pieces.
Which type of fracture occurs when the bone bends and partially breaks, commonly seen in children?
Explanation
In a greenstick fracture, the bone bends and partially breaks, usually occurring in children due to the flexibility of their bones.
a. Transverse fracture: A transverse fracture occurs when the bone breaks straight across its long axis, not bending.
b. Oblique fracture: An oblique fracture involves a diagonal break, not bending and partial breaking.
d. Avulsion fracture: An avulsion fracture occurs when a piece of bone is torn away by a ligament or tendon, not bending and partial breaking.
Which factor is NOT a common cause of fractures in older adults?
Explanation
High-impact sports are not a common cause of fractures in older adults. Fractures in this age group are more often associated with conditions such as osteoporosis and falls.
a. Osteoporosis: Osteoporosis is a common cause of fractures in older adults, as it leads to weakened bones.
b. Falls: Falls are a leading cause of fractures in older adults, as they may have decreased balance and mobility.
d. Decreased bone density: Decreased bone density, often seen in osteoporosis, contributes to fractures in older adults.
What is a closed fracture?
Explanation
A closed fracture is a fracture where the skin remains intact over the fractured bone, and there is no open wound at the site of the fracture.
a. A fracture where the bone breaks through the skin: This type of fracture is known as an open or compound fracture, where the bone pierces through the skin.
b. A fracture where the bone is out of alignment: This type of fracture is known as a displaced fracture, where the bone fragments are not aligned properly.
c. A fracture where the bone is completely broken in two: A complete fracture refers to a fracture that results in two separate bone fragments, but it does not necessarily involve the skin.
What is a closed fracture?
Explanation
A closed fracture is a fracture where the skin remains intact over the fractured bone, and there is no open wound at the site of the fracture.
a. A fracture where the bone breaks through the skin: This type of fracture is known as an open or compound fracture, where the bone pierces through the skin.
b. A fracture where the bone is out of alignment: This type of fracture is known as a displaced fracture, where the bone fragments are not aligned properly.
c. A fracture where the bone is completely broken in two: A complete fracture refers to a fracture that results in two separate bone fragments, but it does not necessarily involve the skin.
Which type of fracture occurs when the bone breaks straight across its long axis?
Explanation
A transverse fracture occurs when the bone breaks straight across its long axis, perpendicular to the bone's length.
a. Greenstick fracture: A greenstick fracture involves the bone bending and partially breaking, usually seen in children. It does not break straight across the bone.
c. Oblique fracture: An oblique fracture involves a diagonal break, not straight across the bone's long axis.
d. Comminuted fracture: In a comminuted fracture, the bone breaks into multiple pieces, which is different from breaking straight across the bone.
Which type of fracture occurs due to twisting or rotational forces on the bone?
Explanation
A spiral fracture occurs due to twisting or rotational forces on the bone, resulting in a twisting break along the bone's length.
a. Greenstick fracture: A greenstick fracture involves the bone bending and partially breaking, usually seen in children. It is not caused by twisting forces.
b. Transverse fracture: A transverse fracture occurs when the bone breaks straight across its long axis, not due to twisting.
d. Comminuted fracture: In a comminuted fracture, the bone breaks into multiple pieces, which is not associated with twisting forces.
Which type of fracture occurs when a piece of bone is torn away by a ligament or tendon?
Explanation
An avulsion fracture occurs when a piece of bone is torn away by a ligament or tendon, often due to a sudden and forceful contraction of the muscle.
a. Greenstick fracture: A greenstick fracture involves the bone bending and partially breaking, not being torn away by a ligament or tendon.
b. Transverse fracture: A transverse fracture occurs when the bone breaks straight across its long axis, not due to ligament or tendon forces.
d. Impacted fracture: An impacted fracture occurs when the bone fragments are driven into each other, often seen in a fall or compression injury, not involving ligament or tendon tears.
What type of fracture occurs when one side of the bone is broken, and the other side is bent?
Explanation
A greenstick fracture involves the bone bending and partially breaking, with one side of the bone being broken and the other side bent.
b. Transverse fracture: A transverse fracture occurs when the bone breaks straight across its long axis, not involving bending.
c. Oblique fracture: An oblique fracture involves a diagonal break, not breaking on one side and bending on the other.
d. Stress fracture: A stress fracture occurs due to repetitive stress on the bone, not involving one side breaking and the other side bending.
Which of the following factors is NOT considered a risk factor for fractures?
Explanation
Regular exercise is not considered a risk factor for fractures. In fact, regular exercise, especially weight-bearing activities, can help improve bone density and reduce the risk of fractures.
a. Advanced age: Advanced age is a significant risk factor for fractures, as bone density tends to decrease with age, making bones more susceptible to fractures.
c. Osteoporosis: Osteoporosis is a condition characterized by low bone density and increased risk of fractures, particularly in postmenopausal women and older adults.
d. History of previous fractures: Having a history of previous fractures is considered a risk factor, as it may indicate underlying bone fragility and susceptibility to future fractures.
Which condition is characterized by weakened and porous bones, increasing the risk of fractures?
Explanation
Osteoporosis is a condition characterized by weakened and porous bones, leading to an increased risk of fractures, especially in the hip, spine, and wrist.
a. Arthritis: Arthritis is a condition that involves joint inflammation and may cause joint pain and stiffness but does not directly weaken bones.
b. Osteoarthritis: Osteoarthritis is a degenerative joint disease that affects the cartilage and joints, but it does not specifically increase the risk of fractures.
c. Osteomyelitis: Osteomyelitis is a bone infection that can lead to bone destruction and inflammation but does not directly weaken bones to the same extent as osteoporosis.
Which population is at a higher risk of stress fractures?
Explanation
Adolescents, especially those involved in high-impact sports or activities, are at a higher risk of stress fractures due to their bones still growing and being more susceptible to repetitive stress injuries.
b. Young adults: Young adults may also be at risk of stress fractures, but adolescents are more vulnerable due to their ongoing bone growth and development.
c. Older adults: While older adults are at risk of fractures, stress fractures are more commonly seen in younger individuals engaged in high-impact activities.
d. Middle-aged adults: Middle-aged adults may experience fractures related to osteoporosis, trauma, or other factors, but they are not the primary population at risk for stress fractures.
Which lifestyle factor is associated with an increased risk of fractures?
Explanation
Smoking is associated with an increased risk of fractures because it can negatively impact bone health, reduce bone density, and impair bone healing.
a. Adequate calcium intake: Adequate calcium intake is essential for maintaining strong bones and reducing the risk of fractures, so it is not associated with an increased risk.
b. Regular weight-bearing exercise: Regular weight-bearing exercise helps improve bone density and reduces fracture risk, so it is not associated with an increased risk.
d. Maintaining a healthy body weight: Maintaining a healthy body weight is beneficial for overall health, but it is not specifically associated with an increased risk of fractures.
Which medical condition is a risk factor for pathological fractures?
Explanation
Cancer is a risk factor for pathological fractures because cancer cells can weaken bones and cause fractures, even with minimal trauma.
a. Hypertension: Hypertension is a condition characterized by high blood pressure and is not directly associated with an increased risk of fractures.
b. Diabetes mellitus: Diabetes mellitus is a metabolic disorder that affects blood sugar levels and does not directly increase the risk of fractures.
d. Asthma: Asthma is a respiratory condition that affects the airways and lungs and is not linked to an increased risk of fractures.
Which clinical manifestation is common in a closed fracture?
Explanation
In a closed fracture, where the skin remains intact over the fractured bone, intense localized pain and tenderness at the fracture site are common symptoms. The skin acts as a barrier, preventing bone fragments from protruding through the skin.
a. Bone fragments protruding through the skin: This symptom is associated with an open or compound fracture, where the bone pierces through the skin.
b. Visible deformity at the fracture site: Visible deformity may occur in both closed and open fractures, but it is not specific to closed fractures.
d. Open wound with bleeding at the fracture site: An open wound with bleeding is characteristic of an open or compound fracture, not a closed fracture.
Which clinical manifestation is most concerning in a patient with a fracture?
Explanation
Numbness and tingling distal to the fracture, along with loss of pulses or capillary refill, may indicate compromised blood flow or nerve injury. It is a concerning sign that requires immediate medical attention.
a. Swelling and bruising at the fracture site: Swelling and bruising are common signs of inflammation and injury at the fracture site, but they are not as concerning as neurovascular compromise.
c. Mild localized pain with movement: Mild localized pain with movement is expected with a fracture, and it does not raise immediate concerns.
d. Warmth and redness at the fracture site: Warmth and redness are signs of inflammation and increased blood flow to the injured area, which is normal during the healing process.
Which clinical manifestation is often present in a stress fracture?
Explanation
: Stress fractures are small, hairline cracks in the bone that occur due to repetitive stress or overuse. They typically present with a gradual onset of localized pain that worsens with activity.
a. Severe pain and deformity: Severe pain and deformity are more commonly seen in acute fractures resulting from trauma or high-impact injuries, not stress fractures.
b. Sudden onset of swelling and bruising: Sudden onset of swelling and bruising is more indicative of acute fractures, not stress fractures.
d. Inability to bear weight on the affected limb: Inability to bear weight may be present in some fractures, but it is not a specific characteristic of stress fractures.
Which clinical manifestation is commonly seen in a Colles' fracture?
Explanation
Colles' fracture is a type of distal radius fracture that results in angulation and swelling of the distal forearm near the wrist joint.
a. Pain and swelling of the ankle: Pain and swelling of the ankle are not related to a Colles' fracture, which occurs in the distal forearm, not the ankle.
b. Deformity and shortening of the affected limb: Deformity and shortening of the limb may occur in some fractures but are not specific to a Colles' fracture.
c. Loss of sensation and motor function distal to the fracture: Loss of sensation and motor function may occur in nerve injuries associated with fractures, but it is not a characteristic of Colles' fracture.
Which clinical manifestation is concerning for compartment syndrome in a patient with a fracture?
Explanation
Severe pain, pallor (pale skin color), and loss of pulses distal to the fracture are concerning signs of compartment syndrome, a serious complication that requires immediate medical intervention.
a. Bruising and discoloration at the fracture site: Bruising and discoloration are common signs of inflammation and injury at the fracture site but are not specific to compartment syndrome.
b. Mild pain and swelling in the affected limb: Mild pain and swelling are expected with a fracture but do not raise immediate concerns for compartment syndrome.
c. Prolonged capillary refill distal to the fracture: Prolonged capillary refill time may indicate reduced blood flow but is not as concerning as the combination of severe pain, pallor, and loss of pulses seen in compartment syndrome.
Which assessment finding is indicative of a possible fracture?
Explanation
Localized swelling and bruising are common signs of inflammation and injury at the fracture site. They may indicate the presence of a fracture, especially if the patient experienced trauma or a fall.
b. Warmth and redness at the site: Warmth and redness are signs of inflammation, but they are not specific to fractures and can occur in various musculoskeletal conditions.
c. Absence of pain with movement: Absence of pain with movement is not a typical finding in fractures. Fractures usually cause pain, especially with movement.
d. Increased range of motion at the joint: Increased range of motion may occur in some injuries, but it is not a reliable indicator of a fracture, especially if there is swelling and bruising present.
What is the most appropriate initial diagnostic study for suspected fractures?
Explanation
X-ray is the most appropriate initial diagnostic study for suspected fractures. It provides clear images of bones and can help identify the presence, location, and extent of the fracture.
b. MRI: MRI is useful for soft tissue imaging, but it may not be the first choice for initial evaluation of fractures. X-rays are more commonly used for immediate assessment.
c. CT scan: CT scan can provide detailed images of bones and soft tissues, but it is not typically the first-line imaging study for fractures. X-rays are more commonly performed first.
d. Ultrasound: Ultrasound is primarily used for imaging soft tissues and may not provide sufficient detail for evaluating fractures. X-rays are more appropriate for initial assessment.
Which clinical manifestation may indicate a possible stress fracture?
Explanation
Stress fractures are small, hairline cracks in the bone that occur due to repetitive stress or overuse. They typically present with a gradual onset of localized pain that worsens with activity.
a. Severe pain and visible deformity: Severe pain and visible deformity are more commonly seen in acute fractures resulting from trauma or high-impact injuries, not stress fractures.
b. Sudden onset of swelling and bruising: Sudden onset of swelling and bruising is more indicative of acute fractures, not stress fractures.
d. Inability to bear weight on the affected limb: Inability to bear weight may be present in some fractures, but it is not a specific characteristic of stress fractures.
What is an essential part of the nursing assessment for a patient with a suspected fracture?
Explanation
Checking peripheral pulses is an essential part of the nursing assessment for a patient with a suspected fracture, especially in the extremity near the fracture site. It helps monitor circulation and ensures adequate blood flow to the injured area.
a. Assessing cognitive function: Assessing cognitive function is important for patients' overall health, but it is not directly related to a suspected fracture assessment.
b. Measuring blood pressure: Measuring blood pressure is part of the routine nursing assessment but is not specific to a suspected fracture.
d. Evaluating liver function: Evaluating liver function is not directly related to the assessment of a suspected fracture.
Which treatment option is commonly used for a stable closed fracture?
Explanation
For a stable closed fracture, cast immobilization is a common treatment option. A cast helps support and protect the fractured bone, allowing it to heal properly.
a. Open reduction and internal fixation (ORIF): ORIF is a surgical procedure used for complex or unstable fractures that cannot be treated with a cast alone.
b. Traction: Traction is applied to realign and stabilize fractures, but it is not typically the first-line treatment for stable closed fractures.
d. External fixation: External fixation involves using pins and an external frame to stabilize fractures, and it is typically used for complex or open fractures.
What is the primary goal of closed reduction in the treatment of fractures?
Explanation
Closed reduction is a non-surgical procedure used to manually realign the fractured bone to its normal position without making an incision. It is often followed by cast immobilization or other forms of stabilization.
a. To surgically realign the fractured bone: Surgical realignment is typically performed through open reduction and internal fixation (ORIF), not closed reduction.
b. To stabilize the fracture with internal fixation: Internal fixation involves the use of screws, plates, or rods to stabilize fractures, and it is not part of the closed reduction procedure.
c. To immobilize the fractured bone with a cast: Immobilization with a cast may follow closed reduction, but it is not the primary goal of the reduction procedure itself.
Which intervention is important for preventing complications in a patient with a lower extremity fracture?
Explanation
Early ambulation (walking) is important for preventing complications such as deep vein thrombosis (DVT) and muscle atrophy in patients with lower extremity fractures.
b. Bed rest for 24 hours: Prolonged bed rest can lead to complications such as muscle weakness, DVT, and pressure ulcers. Early ambulation is preferred to prevent these issues.
c. Avoidance of pain medication: Pain management is essential for patient comfort and mobility. Avoiding pain medication may hinder early ambulation and delay recovery.
d. Delayed wound dressing changes: Appropriate wound care is crucial for preventing infection and ensuring proper healing. Delayed wound dressing changes may increase the risk of infection.
Which medication is commonly prescribed to promote bone healing in patients with fractures?
Explanation
Calcium supplements are commonly prescribed to promote bone healing in patients with fractures. Adequate calcium intake is essential for bone repair and regeneration.
a. Nonsteroidal anti-inflammatory drugs (NSAIDs): NSAIDs may help manage pain and inflammation, but they do not directly promote bone healing and may even inhibit it in some cases.
b. Antibiotics: Antibiotics are prescribed to treat or prevent infection, but they do not play a direct role in bone healing unless an infection is present.
d. Bisphosphonates: Bisphosphonates are used to treat osteoporosis and other bone disorders but are not typically prescribed specifically for fracture healing.
Which nursing intervention is essential for patients with external fixation for fracture management?
Explanation
Patients with external fixation require close monitoring of the pin sites for signs of infection, as they are at risk of developing pin site infections.
a. Providing passive range of motion exercises: Passive range of motion exercises may be appropriate in some cases, but they are not specific to external fixation management.
b. Changing the dressing daily: Dressing changes for external fixation are typically done as instructed by the healthcare provider, which may not necessarily be daily.
c. Loosening the fixation screws every 4 hours: Fixation screws should not be loosened without proper medical guidance, as this can compromise the stability of the external fixation device.
Which complication of fractures requires immediate medical attention?
Explanation
Numbness and tingling distal to the fracture, along with loss of pulses or capillary refill, may indicate neurovascular compromise. This is a serious complication that requires immediate medical attention to prevent potential tissue damage and complications.
a. Swelling and bruising at the fracture site: Swelling and bruising are common signs of inflammation and injury at the fracture site but do not require immediate medical attention unless accompanied by other concerning symptoms.
b. Mild localized pain with movement: Mild localized pain with movement is expected with a fracture and is not as concerning as neurovascular compromise.
d. Stiffness and limited range of motion in nearby joints: Stiffness and limited range of motion may occur after a fracture but are not as urgent as neurovascular compromise.
Which complication of fractures is characterized by pain, warmth, redness, and swelling at the site?
Explanation
Infection is a complication of fractures that can occur when bacteria enter the body through an open wound or during surgery. It presents with pain, warmth, redness, and swelling at the site.
b. Compartment syndrome: Compartment syndrome is characterized by severe pain, pallor, and loss of pulses distal to the fracture site, not warmth and redness.
c. Delayed union: Delayed union refers to a fracture that takes longer than usual to heal, and it does not typically present with warmth and redness.
d. Osteomyelitis: Osteomyelitis is a bone infection that can develop as a complication of fractures, but it does not typically present with warmth and redness at the site.
Which complication of fractures is a result of excessive callus formation at the fracture site?
Explanation
Hypertrophic nonunion occurs when there is excessive callus formation at the fracture site, but the bone ends fail to unite. This can lead to persistent pain and limited function.
a. Nonunion: Nonunion occurs when the fractured bone fails to heal and fuse together, but it does not involve excessive callus formation.
b. Malunion: Malunion refers to a fracture that heals in an incorrect position or alignment, and it is not directly related to excessive callus formation.
c. Delayed union: Delayed union refers to a fracture that takes longer than usual to heal, and it is not specifically characterized by excessive callus formation.
Which complication of fractures is a severe condition that results from increased pressure within a closed space?
Explanation
Compartment syndrome is a severe condition that results from increased pressure within a closed space (compartment) in the body, such as the muscle compartment near the fracture site. It can lead to decreased blood flow, nerve compression, and tissue damage.
a. Infection: Infection is a complication of fractures caused by the introduction of bacteria into the body, and it does not involve increased pressure within a closed space.
c. Delayed union: Delayed union refers to a fracture that takes longer than usual to heal and is not related to increased pressure within a closed space.
d. Osteomyelitis: Osteomyelitis is a bone infection that can occur as a complication of fractures and is not specifically related to increased pressure within a closed space.
Which complication of fractures is associated with persistent pain and limited function despite appropriate treatment?
Explanation
Nonunion occurs when the fractured bone fails to heal and fuse together despite appropriate treatment. It is associated with persistent pain and limited function.
b. Malunion: Malunion refers to a fracture that heals in an incorrect position or alignment, but it may or may not cause persistent pain and limited function.
c. Delayed union: Delayed union refers to a fracture that takes longer than usual to heal but eventually heals properly. It is not specifically associated with persistent pain and limited function.
d. Osteomyelitis: Osteomyelitis is a bone infection that can develop as a complication of fractures, but it may or may not cause persistent pain and limited function, depending on its severity and treatment response.
What should the nurse include in the patient education about cast care?
Explanation
It is essential for the patient to avoid moving the cast to relieve itching as this can lead to skin breakdown, discomfort, and improper healing. The nurse should instruct the patient to use cool air or apply ice packs on the outside of the cast to alleviate itching without disturbing the cast's positioning.
b. Using a hairdryer on a warm setting to dry the inside of the cast is not recommended. The heat can cause discomfort and may not effectively dry the interior of the cast, leading to skin irritation and potential infection.
c. Sticking objects under the cast to scratch the skin can damage the skin and introduce bacteria, increasing the risk of infection. The patient should be instructed not to insert any objects under the cast.
d. Removing the cast if it becomes loose is not within the patient's scope of practice. If the cast becomes loose or uncomfortable, the patient should seek immediate medical attention for evaluation and adjustment by a healthcare professional.
What is a crucial aspect of patient education about weight-bearing status after a fracture?
Explanation
It is crucial for the patient to understand the importance of partial weight-bearing on the affected limb during the healing process. Partial weight-bearing helps promote bone healing and prevents excessive stress on the fracture site, reducing the risk of complications.
a. Encouraging immediate full weight-bearing on the affected limb can lead to further damage to the healing bone and may delay the healing process.
c. Advising the patient to avoid putting any weight on the affected limb can result in muscle atrophy, decreased circulation, and joint stiffness. Some weight-bearing is necessary for proper bone healing.
d. Instructing the patient to use assistive devices only during walking is not enough to ensure appropriate weight-bearing. The patient should follow specific weight-bearing restrictions as advised by the healthcare provider, even when using assistive devices.
What should the nurse include in the patient education about cast drying?
Explanation
The patient should be instructed not to cover the cast with plastic when bathing or swimming, as moisture can weaken the cast and increase the risk of skin irritation and infection. The cast should be kept dry to maintain its structural integrity.
b. Applying heat directly to the cast to speed up drying is not recommended, as excessive heat can lead to discomfort and skin irritation. The cast should be air-dried or gently patted dry with a towel.
c. Using cotton swabs to clean the skin under the cast can introduce fibers into the cast and potentially irritate the skin. The nurse should advise the patient not to insert anything under the cast.
d. Keeping the cast exposed to air for long periods may lead to dirt and debris getting trapped in the cast and increasing the risk of infection. The patient should be cautious and avoid exposing the cast to dirt and contaminants.
What is a critical aspect of patient education regarding cast maintenance?
Explanation
It is crucial for the patient to regularly check for signs of skin irritation and redness around the cast edges. Skin irritation and redness can indicate pressure points or infection, and early identification can prevent complications.
a. Breaking off rough edges of the cast with scissors can damage the cast and compromise its structural integrity. The patient should not alter the cast in any way.
c. Using lotion to moisturize the skin under the cast is not recommended, as it can lead to skin irritation and may compromise the cast's fit and function. The skin under the cast should be kept dry and clean.
d. Using a heating pad to alleviate discomfort is not recommended, as excessive heat can lead to skin irritation and may weaken the cast. The patient should use ice packs or follow the healthcare provider's instructions for pain management.
When assessing a patient with a fracture, what is the priority nursing consideration?
Explanation
Assessing the neurovascular status of the affected limb is the priority nursing consideration in a patient with a fracture. Checking for pulses, capillary refill, sensation, and motor function helps identify neurovascular compromise, which requires immediate intervention to prevent potential tissue damage and complications.
a. Monitoring the patient's pain level is essential, but it is not the priority over assessing neurovascular status. Pain management can be addressed after ensuring the limb's vascular and neurological integrity.
c. Evaluating the range of motion in nearby joints is important for overall assessment, but it is not as critical as assessing neurovascular status in a patient with a fracture.
d. Instructing the patient about cast care is necessary, but it is not the priority consideration when the patient's neurovascular status is at risk.
What nursing intervention is essential to prevent skin breakdown and pressure ulcers in a patient with a long-term immobilization due to a fracture?
Explanation
Using a lift sheet to reposition the patient is essential to prevent skin breakdown and pressure ulcers in a patient with long-term immobilization. This helps redistribute pressure on bony prominences and reduces the risk of skin damage.
a. Performing passive range of motion exercises regularly is important for preventing joint stiffness and muscle atrophy but may not directly prevent skin breakdown and pressure ulcers.
b. Applying petroleum jelly to the skin under the immobilization device is not recommended, as it can cause skin maceration and compromise the device's fit and function.
d. Providing a soft foam mattress overlay can enhance patient comfort but may not be sufficient to prevent skin breakdown and pressure ulcers in patients with prolonged immobilization.
What should the nurse include in the discharge teaching for a patient with a newly applied cast?
Explanation
: Educating the patient about signs of neurovascular compromise, such as changes in sensation, color, or temperature of the limb, is essential to ensure early detection of potential complications and timely intervention.
a. Encouraging the patient to bear full weight on the cast immediately is not recommended, as weight-bearing should follow the healthcare provider's instructions, which may involve partial weight-bearing initially.
b. Instructing the patient to elevate the casted limb above the heart can help reduce swelling but may not be the primary focus of discharge teaching for a newly applied cast.
c. Advising the patient to use a heating pad on the cast to relieve discomfort is not recommended, as excessive heat can damage the cast and increase the risk of skin irritation.
What should the nurse assess for in a patient with an open fracture?
Explanation
In a patient with an open fracture (compound fracture), there is a risk of infection due to the exposure of the bone to the external environment. The nurse should assess for signs of infection, such as redness, warmth, swelling, drainage, and increased pain at the fracture site.
a. Assessing joint range of motion is important, but it is not the priority in a patient with an open fracture, where preventing infection is the main concern.
b. Assessing neurological function in the unaffected limb is not directly related to the open fracture and may not be the priority at this time.
d. Assessing the quality of pain experienced by the patient is important for pain management but is not the priority over assessing for signs of infection in an open fracture.
What nursing intervention should be implemented for a patient with a fractured extremity before applying a cast?
Explanation
Before applying a cast, the nurse should obtain a baseline neurovascular assessment of the extremity to establish normal function. This assessment will serve as a reference for comparison throughout the cast's application and during the healing process.
a. Elevating the extremity to reduce swelling is a valuable intervention but is not directly related to applying a cast. It can be performed later as part of post-cast application care.
b. Applying ice packs to the fracture site can help reduce swelling and pain but is not a step in preparing for the cast application.
c. Administering analgesics to manage pain is important, but obtaining a baseline neurovascular assessment is the priority before applying a cast.
Which type of fracture occurs when the bone is crushed and shattered into multiple fragments?
Explanation
A comminuted fracture occurs when the bone is crushed and shattered into multiple fragments, resulting in significant bone displacement and increased difficulty in alignment during the healing process.
a. Greenstick fracture: A greenstick fracture is an incomplete fracture where the bone bends and partially breaks, commonly seen in pediatric patients. It does not involve bone crushing or fragmentation.
c. Avulsion fracture: An avulsion fracture occurs when a small fragment of bone is pulled away from the main bone due to the forceful attachment of a tendon or ligament. It is not characterized by bone crushing or fragmentation.
d. Stress fracture: A stress fracture is a tiny crack in the bone caused by repetitive stress and overuse. It does not involve bone crushing or fragmentation.
Which type of fracture occurs when the bone breaks incompletely, with one side bending and the other side breaking?
Explanation
A greenstick fracture is an incomplete fracture where the bone breaks incompletely, with one side bending and the other side breaking. It is commonly seen in children due to their more flexible bones.
b. Comminuted fracture: A comminuted fracture occurs when the bone is crushed and shattered into multiple fragments, but it does not involve one side bending and the other side breaking.
c. Spiral fracture: A spiral fracture occurs when the bone is twisted, resulting in a spiral-shaped fracture line. It does not involve one side bending and the other side breaking.
d. Oblique fracture: An oblique fracture occurs when the bone breaks at an angle, but it does not involve one side bending and the other side breaking.
What type of fracture occurs when the bone is completely broken into two separate pieces?
Explanation
A transverse fracture occurs when the bone is completely broken into two separate pieces at a right angle to the bone's long axis.
a. Greenstick fracture: A greenstick fracture is an incomplete fracture where the bone bends and partially breaks, but it does not result in two separate pieces of bone.
c. Impacted fracture: An impacted fracture occurs when the bone ends are forced into each other, commonly seen in long bones such as the femur. It does not involve the bone breaking into two separate pieces.
d. Spiral fracture: A spiral fracture occurs when the bone is twisted, resulting in a spiral-shaped fracture line. It does not involve the bone breaking into two separate pieces.
Which term describes a fracture where the bone penetrates the skin and is exposed to the external environment?
Explanation
An open fracture, also known as a compound fracture, occurs when the bone penetrates the skin and is exposed to the external environment. It carries a higher risk of infection due to the exposure of the bone to external contaminants.
b. Closed fracture: A closed fracture, also known as a simple fracture, does not break the skin, and the bone remains enclosed within the body.
c. Impacted fracture: An impacted fracture occurs when the bone ends are forced into each other, commonly seen in long bones such as the femur. It does not involve the bone penetrating the skin.
d. Stress fracture: A stress fracture is a tiny crack in the bone caused by repetitive stress and overuse. It does not involve the bone penetrating the skin.
Which factor is essential in assessing the patient's readiness for weight-bearing after a fracture?
Explanation
The type of fracture is essential in assessing the patient's readiness for weight-bearing. Some fractures require non-weight-bearing, partial weight-bearing, or full weight-bearing, depending on the bone's location, severity of the fracture, and treatment plan.
a. Age of the patient: The patient's age can influence fracture healing but is not the primary factor in determining weight-bearing status.
c. Pain level: Pain assessment is important for managing discomfort, but it is not the sole factor in determining weight-bearing status.
d. Patient's occupation: The patient's occupation may be considered in the treatment plan, but it is not the primary factor in determining weight-bearing status after a fracture.
Which imaging modality is commonly used to diagnose fractures in the emergency department?
Explanation
X-ray (radiography) is the most common imaging modality used to diagnose fractures in the emergency department. X-rays can visualize the bone's structure and detect fractures, bone displacement, or other abnormalities.
a. Magnetic Resonance Imaging (MRI): MRI is useful for soft tissue evaluation but is not routinely used for initial fracture diagnosis in the emergency department.
b. Computed Tomography (CT): CT scans provide detailed cross-sectional images of bones and soft tissues, but they are not typically the first-line imaging for initial fracture assessment in the emergency department.
d. Ultrasound: Ultrasound is useful for certain soft tissue evaluations but is not commonly used for diagnosing fractures.
What nursing intervention is essential for the prevention of compartment syndrome in a patient with a fracture?
Explanation
Regularly monitoring neurovascular status, including assessing pulses, capillary refill, sensation, and motor function, is essential for early detection of compartment syndrome, which can occur after a fracture. Compartment syndrome is a serious condition where increased pressure within the muscle compartment can compromise blood flow and nerve function.
a. Administering analgesics for pain relief is important, but it does not directly prevent compartment syndrome.
b. Elevating the affected limb above the heart can help reduce swelling but does not specifically prevent compartment syndrome.
c. Applying ice packs to the fracture site can help reduce pain and swelling but is not a preventive measure for compartment syndrome.
What is the primary goal of fracture reduction and immobilization?
Explanation
The primary goal of fracture reduction and immobilization is to promote bone realignment and healing. By aligning the fractured bone properly and immobilizing it with casts or splints, the healing process is facilitated, and bone stability is ensured.
a. Reducing pain and discomfort is an important aspect of fracture management but is not the primary goal of fracture reduction and immobilization.
c. Restoring full range of motion is an essential goal of fracture rehabilitation, but it comes after the bone has healed and the immobilization is removed.
d. Minimizing the risk of infection is crucial, particularly in open fractures, but it is not the primary goal of fracture reduction and immobilization.
What is an essential nursing consideration for a patient with a suspected fracture before moving or handling the affected limb?
Explanation
Before moving or handling the affected limb, the nurse must assess for any signs of neurovascular compromise, such as changes in pulses, capillary refill, sensation, and motor function. This assessment helps identify potential vascular or nerve injuries and guides appropriate care to prevent complications.
a. Explaining the importance of immobilization to the patient is important but is not directly related to assessing for neurovascular compromise before moving the limb.
b. Applying a splint or cast to the affected limb is typically done after the initial assessment and diagnosis of the fracture, not before handling the limb.
d. Administering analgesics for pain relief is important, but it does not directly relate to assessing for neurovascular compromise before moving the limb.
What patient education should the nurse provide to a patient with a newly applied cast?
Explanation
The nurse should instruct the patient to avoid placing any objects under the cast to prevent skin irritation, damage to the cast, and potential introduction of bacteria or contaminants.
a. Encouraging the patient to frequently remove the cast for skin care is not recommended, as it can compromise the cast's fit and function and increase the risk of complications.
b. Advising the patient to use a hairdryer on the cast to relieve itching is not recommended, as it can cause skin maceration and damage the cast.
d. Educating the patient to keep the cast exposed to air for prolonged periods is not recommended, as dirt and debris can get trapped inside the cast, increasing the risk of infection. The patient should follow the healthcare provider's instructions for cast care.
Which type of fracture involves the bone breaking into multiple fragments?
Explanation
A comminuted fracture is a type of fracture where the bone breaks into multiple fragments. This can occur due to a high-impact injury or significant force applied to the bone.
b. Greenstick fracture: A greenstick fracture is an incomplete fracture seen in children, where the bone bends and partially breaks on one side but remains intact on the other side.
c. Spiral fracture: A spiral fracture occurs when the bone is twisted, causing a spiral-shaped fracture line. It often results from a twisting force applied to the bone.
d. Transverse fracture: A transverse fracture is a type of fracture where the fracture line is perpendicular to the long axis of the bone.
Which type of fracture occurs when the bone penetrates the skin?
Explanation
An open fracture, also known as a compound fracture, occurs when the bone breaks and penetrates the skin, exposing the fracture site to the external environment. It carries an increased risk of infection and requires immediate medical attention.
a. Closed fracture: A closed fracture is a type of fracture where the bone breaks but does not penetrate the skin, keeping the fracture site enclosed.
b. Greenstick fracture: A greenstick fracture is an incomplete fracture seen in children, where the bone bends and partially breaks on one side but remains intact on the other side.
d. Stress fracture: A stress fracture is a small crack or incomplete break in the bone, often caused by repetitive stress and overuse.
Which type of fracture occurs in children due to their bones being more pliable?
Explanation
A greenstick fracture is an incomplete fracture that commonly occurs in children due to their bones being more pliable and flexible than adult bones. In a greenstick fracture, one side of the bone bends and partially breaks, while the other side remains intact.
a. Spiral fracture: A spiral fracture occurs when the bone is twisted, causing a spiral-shaped fracture line. It often results from a twisting force applied to the bone and can occur in both children and adults.
c. Transverse fracture: A transverse fracture is a type of fracture where the fracture line is perpendicular to the long axis of the bone and can occur in both children and adults.
d. Oblique fracture: An oblique fracture is a type of fracture where the fracture line is diagonal to the long axis of the bone and can occur in both children and adults.
Which fracture type is commonly seen in osteoporotic bones, especially in older adults?
Explanation
A compression fracture is commonly seen in osteoporotic bones, especially in older adults, due to decreased bone density and strength. It occurs when the bone is compressed and collapses, often resulting from a fall or minor trauma.
b. Avulsion fracture: An avulsion fracture occurs when a small piece of bone is torn away from the main bone due to the pull of a ligament or tendon. It can happen in individuals of all ages.
c. Greenstick fracture: A greenstick fracture is an incomplete fracture seen in children, where the bone bends and partially breaks on one side but remains intact on the other side.
d. Impacted fracture: An impacted fracture occurs when the broken ends of the bone are driven into each other, often seen in long bones like the femur or humerus. It can occur in individuals of all ages.
Which fracture type involves a break in the bone that is at an angle to the long axis of the bone?
Explanation
An oblique fracture involves a break in the bone that is at an angle to the long axis of the bone. It is often the result of a diagonal force applied to the bone.
b. Spiral fracture: A spiral fracture occurs when the bone is twisted, causing a spiral-shaped fracture line. It often results from a twisting force applied to the bone and is not specifically at an angle to the long axis of the bone.
c. Transverse fracture: A transverse fracture is a type of fracture where the fracture line is perpendicular to the long axis of the bone and is not at an angle.
d. Greenstick fracture: A greenstick fracture is an incomplete fracture seen in children, where the bone bends and partially breaks on one side but remains intact on the other side. It is not specifically at an angle to the long axis of the bone.
Osteoarthritis
Which of the following statements best describes the introduction of osteoarthritis?
Explanation
Osteoarthritis is a degenerative joint disease characterized by the gradual breakdown of joint cartilage over time. It is not an autoimmune disease, and it does not involve inflammation like rheumatoid arthritis. While it can affect people of all ages, it is more commonly seen in older adults.
a. Osteoarthritis is not a systemic autoimmune disease. It is primarily a non-inflammatory condition, and the immune system is not involved in its pathogenesis.
b. Osteoarthritis is not a condition that primarily affects young adults. While it can occur at any age, it is more commonly seen in older individuals.
d. Osteoarthritis is not caused by the deposition of urate crystals. Urate crystal deposition is associated with gout, a different form of arthritis.
What is the main characteristic of osteoarthritis?
Explanation
The main characteristic of osteoarthritis is the gradual breakdown of joint cartilage, which leads to joint pain, stiffness, and loss of function. This breakdown occurs over time due to various factors such as aging, joint overuse, and mechanical stress.
a. Osteoarthritis is primarily a non-inflammatory condition. While some inflammation may occur in later stages, it is not the main characteristic of the disease. Inflammation of the synovial membrane is more characteristic of other types of arthritis, such as rheumatoid arthritis.
b. Formation of bony nodules in the joints is not a primary characteristic of osteoarthritis. It is more commonly seen in conditions like osteophytes, which are small, bony outgrowths that can develop around the joints in response to cartilage degeneration.
d. Overproduction of synovial fluid is not a characteristic of osteoarthritis. Osteoarthritis is not primarily a disease of the synovial membrane, and excessive synovial fluid production is more characteristic of inflammatory joint conditions.
Which of the following statements accurately describes the pathophysiology of osteoarthritis?
Explanation
Osteoarthritis is a degenerative joint disease characterized by the breakdown of joint cartilage, leading to joint pain and stiffness. As the cartilage wears away, the bones may develop small, bony outgrowths called osteophytes.
a. Osteoarthritis is not an autoimmune disease. It is primarily a non-inflammatory condition, and the immune system is not involved in its pathogenesis.
b. Osteoarthritis is not primarily a disease of the synovial membrane. While changes in the synovium can occur in osteoarthritis, the primary pathology is in the articular cartilage.
d. Osteoarthritis is not caused by the deposition of urate crystals. Urate crystal deposition is associated with gout, a different form of arthritis.
Which of the following factors contributes to the development of osteoarthritis?
Explanation
Excessive physical activity and joint overuse can contribute to the development of osteoarthritis. Repetitive use and mechanical stress on the joints can lead to cartilage degeneration over time.
a. Osteoarthritis is primarily a non-inflammatory condition. Chronic inflammation of the synovial membrane is more characteristic of other types of arthritis, such as rheumatoid arthritis.
b. Osteoarthritis is not related to hyperactivity of the immune system. It is not an autoimmune disease, and the immune system is not involved in its pathogenesis.
c. Collagen is an essential component of joint cartilage. A deficiency of collagen would weaken the cartilage and contribute to joint degeneration. However, osteoarthritis is not primarily caused by collagen deficiency.
Which of the following is a modifiable risk factor for osteoarthritis?
Explanation
Obesity is a modifiable risk factor for osteoarthritis. Excess body weight puts increased stress on weight-bearing joints, such as the knees and hips, leading to accelerated wear and tear of the joint cartilage.
a. Age over 60 years is a non-modifiable risk factor for osteoarthritis. While the risk of osteoarthritis increases with age, the age itself cannot be modified.
b. Female gender is a non-modifiable risk factor for osteoarthritis. Women have a higher risk of developing osteoarthritis compared to men, but gender cannot be modified.
c. Family history of osteoarthritis is a non-modifiable risk factor. Having a family history of the condition increases the risk, but it cannot be modified.
A client has a sedentary lifestyle, primarily involving sitting for prolonged periods. Which of the following risk factors for osteoarthritis is described in this scenario?
Explanation
Lack of physical activity and a sedentary lifestyle are risk factors for osteoarthritis. Regular physical activity helps maintain joint health and reduces the risk of joint degeneration.
a. Female gender is a non-modifiable risk factor for osteoarthritis.
b. Joint injury is a risk factor, especially in individuals with a history of joint trauma or repetitive use injuries. However, the scenario does not mention any joint injury.
d. Age over 60 years is a non-modifiable risk factor for osteoarthritis.
A client has a family history of osteoarthritis and engages in regular physical activity. Which of the following risk factors for osteoarthritis is NOT present in this client?
Explanation
Lack of physical activity is not present in this client, as they engage in regular physical activity. However, the other risk factors are present. Age over 60 years and family history of osteoarthritis are non-modifiable risk factors, while joint injury is a risk factor associated with joint trauma or repetitive use injuries.
a. Age over 60 years is a non-modifiable risk factor for osteoarthritis.
b. Family history of osteoarthritis is a risk factor for the condition.
d. Joint injury is a risk factor associated with joint trauma or repetitive use injuries. The scenario does not provide information about any joint injury in this client.
Which of the following clinical manifestations is commonly seen in osteoarthritis?
Explanation
Crepitus, a crackling or grating sensation during joint movement, is a common clinical manifestation of osteoarthritis. It occurs due to the irregular surfaces of the joint caused by cartilage degeneration.
a. Warm and swollen joints are characteristic of inflammatory arthritis conditions like rheumatoid arthritis, not osteoarthritis.
b. Morning joint stiffness lasting for several hours is typical of inflammatory arthritis conditions like rheumatoid arthritis, not osteoarthritis.
c. Red, hot, and tender joints are signs of inflammation and are more commonly seen in inflammatory arthritis conditions, not osteoarthritis.
A client with osteoarthritis presents with joint pain that worsens with weight-bearing activities and improves with rest. Which of the following clinical manifestations is described?
Explanation
Pain that worsens with weight-bearing activities and improves with rest is a classic clinical manifestation of osteoarthritis. Activity-related pain is due to the increased stress on the affected joint during movement, while rest allows for decreased pressure and relief of pain.
a. Nocturnal joint pain is more typical of inflammatory arthritis conditions like rheumatoid arthritis, not osteoarthritis.
b. Morning joint stiffness lasting for 1 hour is characteristic of inflammatory arthritis conditions like rheumatoid arthritis, not osteoarthritis.
d. Joint pain that is constant throughout the day may be seen in various joint disorders, but the pattern of pain relief with activity is more indicative of osteoarthritis.
A client presents with joint pain, tenderness, and swelling in the hands and knees. The healthcare provider notes the presence of Heberden's nodes on physical examination. Which of the following clinical manifestations is most consistent with these findings?
Explanation
The presence of Heberden's nodes, which are bony enlargements at the distal interphalangeal (DIP) joints, is a characteristic clinical manifestation of osteoarthritis. These nodes are a result of cartilage degeneration in the affected joints.
a. Joint pain that worsens with rest is more indicative of inflammatory arthritis conditions like rheumatoid arthritis, not osteoarthritis.
b. Joint pain that improves with activity is not typical of osteoarthritis, which tends to worsen with weight-bearing activities.
d. Warm and erythematous joints are signs of inflammation and are more commonly seen in inflammatory arthritis conditions, not osteoarthritis.
The healthcare provider is assessing a client with suspected osteoarthritis. Which of the following diagnostic tests is most appropriate to confirm the diagnosis?
Explanation
MRI is the most appropriate diagnostic test to confirm the diagnosis of osteoarthritis. It can provide detailed images of the affected joints, allowing the healthcare provider to assess the joint structures, cartilage, and bone for signs of osteoarthritis. Rheumatoid factor (RF) blood test and C-reactive protein (CRP) blood test are used to diagnose inflammatory arthritis conditions like rheumatoid arthritis, not osteoarthritis. Synovial fluid analysis is usually performed to assess for infection or inflammation in the joint, not to diagnose osteoarthritis.
a. Rheumatoid factor (RF) blood test is used to diagnose inflammatory arthritis conditions like rheumatoid arthritis, not osteoarthritis.
c. C-reactive protein (CRP) blood test is used to diagnose inflammatory conditions, but it is not specific to osteoarthritis.
d. Synovial fluid analysis is usually performed to assess for infection or inflammation in the joint, not to diagnose osteoarthritis.
The healthcare provider is evaluating a client with joint pain and stiffness for possible osteoarthritis. Which of the following physical examination findings is most consistent with osteoarthritis?
Explanation
Heberden's nodes are bony enlargements that occur at the distal interphalangeal (DIP) joints of the fingers and are a characteristic finding in osteoarthritis. Warm, swollen, and tender joints are typical of inflammatory arthritis conditions like rheumatoid arthritis, not osteoarthritis. Symmetrical joint involvement is more common in systemic autoimmune disorders such as rheumatoid arthritis, not osteoarthritis. A positive Babinski reflex is a neurological finding and is not related to the diagnosis of osteoarthritis.
a. Warm, swollen, and tender joints are typical of inflammatory arthritis conditions like rheumatoid arthritis, not osteoarthritis.
b. Symmetrical joint involvement is more common in systemic autoimmune disorders such as rheumatoid arthritis, not osteoarthritis.
d. A positive Babinski reflex is a neurological finding and is not related to the diagnosis of osteoarthritis.
A client presents with joint pain and stiffness. The healthcare provider performs a physical examination and finds tenderness over the affected joint, as well as crepitus during joint movement. Which of the following diagnostic tests is most appropriate to evaluate the joint for osteoarthritis?
Explanation
X-ray of the joint is the most appropriate diagnostic test to evaluate for osteoarthritis. X-ray can show joint space narrowing, osteophyte formation, and changes in bone density, which are typical findings in osteoarthritis. A complete blood count (CBC) and rheumatoid factor (RF) blood test are used to assess for inflammation and autoimmune markers, respectively, which are more indicative of inflammatory arthritis conditions like rheumatoid arthritis, not osteoarthritis. Synovial fluid analysis is usually performed to assess for infection or inflammation in the joint and may not be as helpful in diagnosing osteoarthritis.
a. A complete blood count (CBC) is used to assess for general health and detect various conditions, but it is not specific to osteoarthritis.
b. A rheumatoid factor (RF) blood test is used to diagnose inflammatory arthritis conditions like rheumatoid arthritis, not osteoarthritis.
d. Synovial fluid analysis is usually performed to assess for infection or inflammation in the joint, but it may not provide definitive evidence of osteoarthritis.
A client with osteoarthritis reports joint pain and stiffness in the knees. Which of the following medications should the nurse expect the healthcare provider to prescribe initially?
Explanation
Ibuprofen is a nonsteroidal anti-inflammatory drug (NSAID) commonly prescribed for the initial management of osteoarthritis. It helps reduce pain and inflammation in the affected joints. Methotrexate, prednisone, and infliximab are medications used to manage inflammatory arthritis conditions, such as rheumatoid arthritis, and are not typically prescribed for osteoarthritis.
a. Methotrexate is used in the management of inflammatory arthritis conditions, such as rheumatoid arthritis, and is not typically prescribed for osteoarthritis.
c. Prednisone is a corticosteroid used to manage inflammatory arthritis conditions, such as rheumatoid arthritis, and is not typically prescribed for osteoarthritis.
d. Infliximab is a biologic medication used in the management of inflammatory arthritis conditions, such as rheumatoid arthritis, and is not typically prescribed for osteoarthritis.
The nurse is providing education to a client with osteoarthritis about the use of assistive devices. Which of the following statements by the client indicates understanding of the instructions?
Explanation
Using a walker is an appropriate choice for a client with osteoarthritis who needs support and stability while moving around the house. It helps distribute weight evenly and reduces stress on the affected joints. Using a cane on the same side as the affected knee can provide some support but may not be as effective as a walker. Placing the crutches under the arms is not a correct technique for using crutches, as they should be positioned in the hand grips for proper support. Using a wheelchair for all daily activities may not be necessary for a client with osteoarthritis, as it may lead to decreased mobility and muscle weakness.
a. "I will use a cane on the same side as my affected knee." Using a cane on the same side as the affected knee may not provide sufficient support and stability for the client.
c. "I will place the crutches under my arms for support." Placing the crutches under the arms is not a correct technique for using crutches, as they should be positioned in the hand grips for proper support.
d. "I will use a wheelchair for all my daily activities." Using a wheelchair for all daily activities may not be necessary for a client with osteoarthritis, as it may lead to decreased mobility and muscle weakness.
A client with osteoarthritis is experiencing severe joint pain and limited mobility. The nurse should recommend which of the following non-pharmacological interventions for pain management?
Explanation
Using a TENS unit on the affected joint can help alleviate pain by delivering electrical impulses that interfere with pain signals to the brain. Applying a heating pad may provide temporary relief, but it is not as effective as using a TENS unit for pain management in osteoarthritis. High-impact exercises are not recommended, as they can exacerbate joint pain and damage. Massaging the affected joint with essential oils may offer some relief, but it is not as effective as using a TENS unit for pain management.
a. Applying a heating pad to the affected joint for 30 minutes daily. While applying a heating pad may provide some temporary relief, using a TENS unit is a more effective non-pharmacological intervention for pain management in osteoarthritis.
c. Performing high-impact exercises to strengthen the affected joint. High-impact exercises can exacerbate joint pain and damage in clients with osteoarthritis. Low-impact exercises are recommended instead.
d. Massaging the affected joint with essential oils. While massaging the affected joint may offer some relief, using a TENS unit is a more effective non-pharmacological intervention for pain management in osteoarthritis.
Which of the following statements by a client with osteoarthritis indicates a need for further education?
Explanation
High-impact exercises can exacerbate joint pain and damage in clients with osteoarthritis. Low-impact exercises are recommended to improve joint flexibility and reduce pain. The other options demonstrate appropriate understanding of osteoarthritis self-management.
a. "I will try to avoid activities that put stress on my affected joints." This statement shows appropriate understanding, as avoiding stress on affected joints is beneficial for clients with osteoarthritis.
b. "I should take my prescribed medications even if my symptoms improve." This statement demonstrates adherence to the prescribed treatment plan, which is important for managing osteoarthritis symptoms.
c. "I will use a heating pad to relieve pain and inflammation in my joints." This statement indicates a correct understanding of using heat therapy to alleviate pain and inflammation in osteoarthritis.
Which of the following is an essential component of patient education for clients with osteoarthritis?
Explanation
Joint protection techniques are an essential component of patient education for clients with osteoarthritis. These techniques help clients reduce stress on their affected joints and manage pain during daily activities. Encouraging frequent high-impact exercises can worsen joint pain and damage in osteoarthritis. Advising the client to avoid all physical activity is not recommended, as regular low-impact exercises are beneficial for joint health. Using a cold pack daily can provide temporary relief from pain and inflammation, but it is not the primary focus of patient education for osteoarthritis.
a. Encouraging frequent high-impact exercises can exacerbate joint pain and damage in clients with osteoarthritis. Low-impact exercises are recommended instead.
b. Advising the client to avoid all physical activity is not recommended. Regular low-impact exercises, such as swimming or walking, are beneficial for joint health in osteoarthritis.
c. Using a cold pack daily can provide temporary relief from pain and inflammation, but it is not the primary focus of patient education for osteoarthritis.
Which of the following instructions should the nurse include in the education of a client with osteoarthritis?
Explanation
Instructing the client to take frequent breaks during activities to rest the affected joints helps reduce stress and prevent worsening of symptoms. Avoiding the use of assistive devices can lead to increased joint strain and pain, so it is essential to encourage their appropriate use. Performing high-impact exercises is not recommended, as they can worsen joint pain and damage. Applying a heating pad for an extended period is not advisable, as it can cause burns and skin irritation.
b. "Avoid using assistive devices to prevent dependency on them." Encouraging the appropriate use of assistive devices is important for clients with osteoarthritis to reduce joint stress during daily activities.
c. "Perform high-impact exercises regularly to strengthen your joints." High-impact exercises can exacerbate joint pain and damage in clients with osteoarthritis. Low-impact exercises are recommended instead.
d. "Apply a heating pad for at least 1 hour to alleviate joint pain." Applying a heating pad for an extended period can cause burns and skin irritation. Using a heating pad for short intervals is appropriate for pain relief.
Which of the following nursing considerations is essential for a client with osteoarthritis?
Explanation
One of the main nursing considerations for a client with osteoarthritis is pain management. Nonsteroidal anti-inflammatory drugs (NSAIDs) are commonly used to provide pain relief and reduce inflammation in individuals with osteoarthritis.
Incorrect responses:
a. Encouraging high-impact exercises is not recommended for clients with osteoarthritis. High-impact activities can cause additional stress on the affected joints and worsen the symptoms.
c. Promoting weight loss is important for overweight or obese clients with osteoarthritis to reduce joint stress. However, it is not applicable for clients with a BMI within the normal range.
d. Advising the client to avoid any form of physical activity is not recommended. Regular low-impact exercises, such as swimming or cycling, are beneficial for individuals with osteoarthritis.
What nursing intervention is crucial to preventing skin breakdown in a client with osteoarthritis?
Explanation
Regularly inspecting the client's skin for signs of redness or irritation is crucial to prevent skin breakdown in individuals with osteoarthritis. Since they may have difficulty changing positions frequently due to joint pain, it is essential to identify early signs of pressure sores or skin breakdown and implement appropriate interventions. Providing a firm mattress and using pressure-relieving devices (such as cushions and heel protectors) are recommended to prevent skin breakdown. Encouraging the client to sit or lie in one position for extended periods can lead to pressure ulcers. Applying lotion with a high alcohol content can dry out the skin and increase the risk of skin irritation and breakdown.
a. Providing a firm mattress and using pressure-relieving devices are essential interventions to prevent skin breakdown in clients with osteoarthritis.
b. Encouraging the client to sit or lie in one position for extended periods can lead to pressure ulcers and skin breakdown. Frequent position changes are important for preventing pressure sores.
When caring for a client with osteoarthritis, which nursing intervention is essential to promote joint mobility and reduce stiffness?
Explanation
Assisting the client with range-of-motion exercises regularly is an essential nursing intervention to promote joint mobility and reduce stiffness in individuals with osteoarthritis. These exercises help maintain joint flexibility and prevent further joint contractures. Encouraging the client to avoid physical activity can lead to joint stiffness and worsen the symptoms of osteoarthritis. Applying cold packs can provide temporary relief from pain and inflammation, but it is not a primary intervention to promote joint mobility. Administering muscle relaxants may not be the best approach to address joint stiffness in osteoarthritis.
a. Encouraging the client to avoid physical activity is not recommended. Regular low-impact exercises, such as swimming or walking, are beneficial for joint health and mobility in clients with osteoarthritis.
b. Applying cold packs can provide temporary relief from pain and inflammation but is not a primary intervention for promoting joint mobility in osteoarthritis.
d. Administering muscle relaxants may not be the best approach for addressing joint stiffness in osteoarthritis. Range-of-motion exercises and physical therapy are more effective interventions for improving joint mobility.
Osteoarthritis is a chronic degenerative joint disease primarily affecting which structures?
Explanation
Osteoarthritis is characterized by the breakdown of articular cartilage and changes in the underlying bone. It primarily affects the joint structures, leading to pain, stiffness, and loss of joint function.
a. The synovial membrane and tendons are involved in other joint diseases such as rheumatoid arthritis and tendinitis, not osteoarthritis.
c. Ligaments and bursae are important for joint stability and movement, but they are not primarily affected in osteoarthritis.
d. Muscles and nerves can be affected indirectly due to joint changes in osteoarthritis, but they are not the primary structures involved in the disease process.
Which of the following risk factors is associated with the development of osteoarthritis?
Explanation
Obesity is a significant risk factor for the development of osteoarthritis, especially in weight-bearing joints such as knees and hips. Excess body weight increases stress on the joints, leading to cartilage damage and joint degeneration.
a. Regular physical activity is generally beneficial for joint health and may help prevent osteoarthritis.
b. Young age is not a risk factor for osteoarthritis; it is more common in older adults.
c. Family history of osteoporosis is not directly linked to osteoarthritis; however, a family history of osteoarthritis itself may increase the risk.
Which of the following statements about osteoarthritis is correct?
Explanation
Osteoarthritis commonly affects the distal finger joints, such as the DIP (distal interphalangeal) and PIP (proximal interphalangeal) joints. This form of osteoarthritis is known as Heberden's and Bouchard's nodes, respectively.
a. Osteoarthritis is not an autoimmune disorder; it is a degenerative joint disease.
b. Unlike rheumatoid arthritis, osteoarthritis is not characterized by joint inflammation and swelling.
d. While osteoarthritis primarily involves synovial joints, it is not limited to these joints.
Which of the following imaging modalities is commonly used to diagnose osteoarthritis?
Explanation
X-ray imaging is commonly used to diagnose osteoarthritis. It can visualize joint space narrowing, bone spurs, and other changes associated with the disease.
a. MRI is more commonly used to assess soft tissue structures and is not the first-line imaging modality for osteoarthritis.
b. CT scan is not typically used for diagnosing osteoarthritis due to its higher radiation exposure compared to X-ray.
d. Ultrasound is not commonly used for diagnosing osteoarthritis; it is more useful for soft tissue assessment.
Which of the following symptoms is often experienced by individuals with osteoarthritis?
Explanation
Early morning joint stiffness lasting for around 1 hour is a common symptom of osteoarthritis. It is caused by the accumulation of synovial fluid in the affected joint during periods of inactivity.
a. Joint redness and warmth are characteristic of inflammatory joint conditions like rheumatoid arthritis, not osteoarthritis.
c. Symmetrical joint involvement is more typical of systemic autoimmune disorders such as rheumatoid arthritis, not osteoarthritis.
d. Rheumatoid nodules are a specific feature of rheumatoid arthritis, not osteoarthritis.
Which of the following is the primary risk factor for the development of osteoarthritis?
Explanation
Obesity is a primary risk factor for the development of osteoarthritis, particularly in weight-bearing joints such as the knees and hips. Excess weight puts increased stress on the joints, leading to cartilage breakdown and the development of osteoarthritis. While age, family history, and a sedentary lifestyle can also contribute to the development of osteoarthritis, obesity is the most significant risk factor.
a. While age over 65 years is a risk factor for osteoarthritis, it is not the primary risk factor. Osteoarthritis can occur at any age, especially if other risk factors are present.
b. Family history of osteoporosis is not a primary risk factor for osteoarthritis. Osteoarthritis and osteoporosis are separate conditions with different risk factors.
c. While a sedentary lifestyle can contribute to the development of osteoarthritis, it is not the primary risk factor. Obesity is a more significant risk factor in this context.
Which of the following diagnostic tests is most commonly used to confirm the diagnosis of osteoarthritis?
Explanation
X-ray is the most commonly used diagnostic test to confirm the diagnosis of osteoarthritis. It can show joint space narrowing, osteophyte formation (bony overgrowths), and other changes characteristic of osteoarthritis. Rheumatoid factor (RF) and antinuclear antibody (ANA) blood tests are used to diagnose autoimmune conditions like rheumatoid arthritis, not osteoarthritis. Magnetic resonance imaging (MRI) can provide more detailed images of joint structures, but X-ray is typically the initial diagnostic test for osteoarthritis.
a. Rheumatoid factor (RF) blood test is used to diagnose rheumatoid arthritis, not osteoarthritis.
b. Antinuclear antibody (ANA) blood test is used to diagnose autoimmune disorders such as systemic lupus erythematosus (SLE), not osteoarthritis.
c. Magnetic resonance imaging (MRI) can be helpful in assessing joint structures in more detail, but X-ray is the primary diagnostic test for osteoarthritis.
Which of the following lifestyle modifications is recommended for individuals with osteoarthritis to manage their condition effectively?
Explanation
Regular low-impact exercises, such as swimming, cycling, and walking, are recommended for individuals with osteoarthritis to improve joint flexibility and strength without causing excessive stress on the affected joints. Avoiding all forms of exercise and physical activity can lead to joint stiffness and worsen the symptoms of osteoarthritis. Maintaining a sedentary lifestyle is not beneficial for managing osteoarthritis. High-impact sports and activities can cause additional stress on the joints and are generally not recommended for individuals with osteoarthritis.
a. Avoiding all forms of exercise and physical activity is not recommended for individuals with osteoarthritis. Regular exercise is essential for managing the condition effectively.
b. Maintaining a sedentary lifestyle is not beneficial for individuals with osteoarthritis. Engaging in regular physical activity is important for joint health and overall well-being.
d. Participating in high-impact sports and activities can exacerbate the symptoms of osteoarthritis and cause further joint damage. Low-impact exercises are a safer option for individuals with this condition.
Amputation
Which of the following statements best describes amputation?
Explanation
: Amputation is the surgical removal of a limb or body part due to injury, disease, or medical necessity. It involves cutting through bones, muscles, and other tissues to remove the affected limb or body part.
a. A surgical procedure to repair damaged bones and tissues: This statement is incorrect. Amputation involves the removal of a limb or body part rather than repairing damaged bones and tissues.
c. A procedure to treat joint diseases and improve mobility: While amputation may improve mobility in certain cases, it is not primarily used to treat joint diseases. Joint diseases are usually managed through other treatment modalities.
d. The transplantation of a healthy limb from one person to another: This statement is incorrect. Amputation does not involve the transplantation of a healthy limb from one person to another. It is the removal of an affected limb or body part from the same individual.
Which of the following is a common indication for amputation?
Explanation
Peripheral vascular disease, which involves decreased blood flow to the extremities, is a common indication for amputation. In severe cases, where blood flow cannot be restored, amputation may be necessary to prevent further complications.
a. Chronic low back pain: Chronic low back pain is not an indication for amputation. It is usually managed through conservative treatments such as physical therapy, medications, or injections.
b. Osteoarthritis of the knee: Osteoarthritis of the knee may cause pain and mobility issues, but it does not typically lead to amputation. Treatment for osteoarthritis includes pain management, physical therapy, and, in some cases, joint replacement surgery.
d. Minor soft tissue injury: Minor soft tissue injuries do not require amputation. They are usually treated with wound care, rest, and possibly antibiotics if there is an infection.
What is an essential consideration in the decision-making process for amputation?
Explanation
The decision for amputation is complex and takes into account the patient's overall health status, goals, and preferences. Factors such as the extent of the disease or injury, the potential for rehabilitation, and the impact on the patient's quality of life are considered when determining the most appropriate treatment plan.
a. Patient's age and gender: While age and gender may be factors in the decision-making process, they are not the primary consideration for amputation. Each patient's case is evaluated individually based on their specific circumstances.
b. Healthcare provider's preference: The healthcare provider's preference alone does not dictate the decision for amputation. The decision should be made collaboratively between the patient, the healthcare team, and other specialists as needed.
d. Availability of advanced medical technology: While medical technology can play a role in the treatment and rehabilitation of amputees, it is not the primary consideration in the decision for amputation. The decision is primarily based on the patient's health and overall well-being.
What is the primary goal of rehabilitation after amputation?
Explanation
The primary goal of rehabilitation after amputation is to help the patient achieve the highest level of mobility and independence possible with the use of assistive devices and prosthetics. While rehabilitation can improve function and quality of life, it may not fully restore the limb to its pre-amputation function.
a. To restore the limb to its pre-amputation function: While rehabilitation aims to improve function, restoring the limb to its pre-amputation function is not always feasible. Amputation involves the permanent removal of a limb or body part, and some limitations may persist.
b. To minimize the use of assistive devices: While rehabilitation may help the patient adapt to using assistive devices, the goal is not necessarily to minimize their use. Assistive devices can greatly improve mobility and independence for amputees.
d. To eliminate all residual pain and discomfort: While rehabilitation can help manage pain and discomfort, eliminating all residual pain is not always achievable. The goal is to optimize the patient's function and well-being while addressing pain and discomfort as effectively as possible.
Which healthcare team member plays a critical role in the post-operative rehabilitation process for a patient who has undergone amputation?
Explanation
A physical therapist plays a critical role in the post-operative rehabilitation process for a patient who has undergone amputation. They work closely with the patient to help improve strength, mobility, and function, and assist them in adapting to the use of assistive devices and prosthetics.
a. Surgeon: The surgeon performs the amputation surgery but is not directly involved in post-operative rehabilitation. Their role is to ensure a safe and successful surgical procedure.
b. Anesthesiologist: The anesthesiologist is responsible for administering anesthesia during the surgery and ensuring the patient's comfort and safety. They are not directly involved in post-operative rehabilitation.
d. Radiologic technologist: Radiologic technologists perform medical imaging procedures but are not involved in the rehabilitation process for patients who have undergone amputation.
Which of the following is a common indication for amputation?
Explanation
Peripheral vascular disease, which involves decreased blood flow to the extremities, is a common indication for amputation. In severe cases, where blood flow cannot be restored, amputation may be necessary to prevent further complications. It is important to address the underlying vascular issues to avoid the risk of gangrene and potential spread of infection.
a. Chronic low back pain: Chronic low back pain is not an indication for amputation. It is usually managed through conservative treatments such as physical therapy, medications, or injections.
b. Osteoarthritis of the knee: Osteoarthritis of the knee may cause pain and mobility issues, but it does not typically lead to amputation. Treatment for osteoarthritis includes pain management, physical therapy, and, in some cases, joint replacement surgery.
d. Minor soft tissue injury: Minor soft tissue injuries do not require amputation. They are usually treated with wound care, rest, and possibly antibiotics if there is an infection.
Which of the following conditions may require amputation to prevent the spread of infection and tissue damage?
Explanation
Acute osteomyelitis is a severe bacterial infection of the bone that can lead to tissue damage and the spread of infection if not promptly treated. In some cases, when antibiotic therapy is not effective or the infection is severe, amputation may be considered to remove the infected bone and prevent further complications.
a. Severe joint pain: Severe joint pain may be caused by various conditions, but it is not an indication for amputation. Treatment for joint pain involves identifying and managing the underlying cause.
b. Chronic osteoporosis: Osteoporosis is a condition characterized by weakened bones, but it does not typically lead to amputation. Treatment for osteoporosis focuses on preventing fractures and improving bone density through medication and lifestyle modifications.
d. Muscle strain: Muscle strains are common injuries that do not require amputation. They can usually be managed with rest, ice, compression, and elevation (RICE) and physical therapy.
In which situation would amputation be considered as a lifesaving measure?
Explanation
In severe cases of diabetic neuropathy, where peripheral nerve damage leads to non-healing ulcers, infections, and gangrene, amputation may be considered as a lifesaving measure. Removing the affected limb can prevent the spread of infection and potentially save the patient's life.
b. Chronic obstructive pulmonary disease (COPD): COPD is a chronic respiratory condition that primarily affects the lungs. It is not an indication for amputation.
c. Bone fracture with non-union: A bone fracture with non-union refers to a fracture that fails to heal properly. While it may require surgical intervention, it does not typically lead to amputation unless there are severe complications.
d. Malignant bone tumor: Malignant bone tumors may require surgical resection, but amputation is usually a last resort and only considered when the tumor cannot be safely removed through other means.
What condition might lead to the need for an emergency amputation to save a patient's life?
Explanation
Acute compartment syndrome is a medical emergency where increased pressure within a muscle compartment compromises blood flow and can lead to tissue damage and permanent disability. In severe cases, where the condition is not relieved promptly, emergency amputation may be necessary to prevent further tissue damage and save the patient's life.
a. Acute appendicitis: Acute appendicitis is a condition involving inflammation of the appendix and typically requires surgical removal of the appendix (appendectomy) but not amputation.
c. Urinary tract infection: A urinary tract infection is a common infection that is not an indication for amputation. It is usually treated with antibiotics.
d. Minor laceration: A minor laceration does not require amputation. It can typically be treated with wound care and, if needed, sutures or adhesive strips.
What is a potential pre-operative complication that may occur in a patient scheduled for amputation?
Explanation
Infection at the amputation site is a potential pre-operative complication that may occur before the actual surgery. The presence of infection at the surgical site can increase the risk of post-operative complications, delay the surgery, and affect wound healing. Proper pre-operative assessment and management of infections are crucial to ensure a successful amputation procedure.
b. Post-operative pain management: Post-operative pain management is a consideration after the surgery, not a pre-operative complication. It involves planning for pain relief strategies to provide comfort and promote healing after the amputation.
c. Surgical wound dehiscence: Surgical wound dehiscence refers to the separation or opening of the surgical wound, which can occur after the surgery, not before. Proper wound care and surgical techniques are essential to prevent wound dehiscence.
d. Prosthetic fitting and training: Prosthetic fitting and training are part of the post-operative care, not pre-operative complications. After the amputation, the patient will be evaluated for the appropriate prosthetic device, and training will be provided to adapt to using it effectively.
Which pre-operative intervention is essential to prevent potential complications in a patient scheduled for amputation?
Explanation
Assessing the patient's psychological readiness for surgery is essential to prevent potential complications in a patient scheduled for amputation. Pre-operative anxiety, fear, or emotional distress can impact the patient's overall well-being and affect their post-operative recovery. Identifying and addressing these concerns before the surgery is crucial to promote a positive surgical experience and improve outcomes.
a. Performing active range of motion exercises on the affected limb: While range of motion exercises may be beneficial in certain cases, this intervention is not specific to preventing pre-operative complications. Pre-operative exercises may be recommended in some cases to improve overall limb function, but they are not directly related to preventing complications.
b. Administering post-operative pain medications: Administering post-operative pain medications is a consideration after the surgery, not a pre-operative intervention. Pain management strategies are planned and implemented to address pain after the amputation.
d. Educating the patient about post-operative care and rehabilitation: Patient education about post-operative care and rehabilitation is vital, but it is not a pre-operative intervention to prevent complications. This education takes place before and after the surgery to prepare the patient for the recovery process.
Which of the following pre-operative assessments is essential for a patient scheduled for amputation?
Explanation
Circulation assessment of the affected limb is essential for a patient scheduled for amputation. This assessment helps identify any vascular issues or compromised blood flow to the limb, which can impact wound healing and increase the risk of post-operative complications. It is crucial to assess circulation to ensure the patient's safety during and after the amputation procedure.
a. Blood pressure measurement: While blood pressure measurement is a routine assessment, it is not specific to amputation and not directly related to preventing pre-operative complications.
b. Assessment of respiratory rate: Respiratory rate assessment is important for general health assessment, but it is not directly related to preventing complications specifically related to amputation.
d. Height and weight measurement: Height and weight measurement are important for general health assessment, but they are not directly related to preventing complications specifically related to amputation.
What pre-operative intervention is essential to prevent post-operative infection in a patient undergoing amputation?
Explanation
Administering pre-operative antibiotics is essential to prevent post-operative infection in a patient undergoing amputation. Prophylactic antibiotics are often given before the surgical procedure to reduce the risk of infection at the surgical site and promote successful wound healing.
b. Providing pre-operative analgesia: Providing pre-operative analgesia is important for pain management, but it is not directly related to preventing post-operative infection.
c. Ensuring proper patient positioning: Ensuring proper patient positioning is crucial for the surgical procedure's success and patient safety, but it is not directly related to preventing post-operative infection.
d. Educating the patient about post-operative exercises: Patient education about post-operative exercises is important for rehabilitation, but it does not directly prevent post-operative infection. Proper wound care and infection prevention protocols are more relevant to reducing the risk of infection.
Why is it important to identify pre-existing medical conditions and allergies in a patient scheduled for amputation?
Explanation
Identifying pre-existing medical conditions and allergies is essential to assess the risk of post-operative infection and complications in a patient scheduled for amputation. Certain medical conditions and allergies can impact wound healing and increase the risk of surgical complications. By knowing the patient's medical history and allergies, the healthcare team can take appropriate measures to prevent potential problems and improve the patient's overall surgical outcome.
a. To determine the patient's ability to perform post-operative exercises: While identifying pre-existing conditions may provide some insight into the patient's functional abilities, it is not the primary reason for identifying medical conditions and allergies in this context.
b. To identify potential complications during the surgical procedure: Identifying pre-existing conditions is not primarily for identifying potential complications during the surgery itself. Pre-operative assessments and evaluations are conducted to ensure the patient's safety during the surgical procedure.
c. To tailor the prosthetic fitting and training: Identifying pre-existing conditions and allergies can be relevant for prosthetic fitting and training, but it is not the primary reason for identifying them.
Which surgical technique is commonly used for below-the-knee amputations?
Explanation
Transmetatarsal amputation involves the surgical removal of the forefoot and toes while preserving the heel and ankle joint. It is commonly used for below-the-knee amputations, specifically for conditions that affect the toes and forefoot but spare the ankle joint.
a. Hip disarticulation: Hip disarticulation is a higher-level amputation that involves the removal of the entire lower limb at the hip joint. It is not commonly used for below-the-knee amputations.
c. Above-the-knee amputation: Above-the-knee amputation involves the removal of the entire lower limb above the knee joint. It is not used for below-the-knee amputations.
d. Syme amputation: Syme amputation involves the removal of the foot at the ankle joint while preserving the heel pad. It is used for specific conditions affecting the foot and ankle joint but is not a common choice for below-the-knee amputations.
What is the primary goal of surgical amputation?
Explanation
The primary goal of surgical amputation is to remove the diseased or damaged tissue to promote healing and prevent the spread of infection. While pain relief and restoration of function are important considerations, the main purpose of amputation is to address the underlying condition and improve the patient's overall health and well-being.
a. To eliminate all pain and discomfort in the affected limb: While pain relief is a desired outcome of amputation, it is not always possible to eliminate all pain and discomfort. The goal is to manage pain effectively and improve the patient's quality of life.
b. To restore full function and mobility of the limb: Restoring full function and mobility may not always be achievable after amputation. The extent of functional restoration depends on various factors, including the level of amputation and the patient's overall health.
c. To achieve the most cosmetically appealing result: While achieving a cosmetically appealing result may be important for some patients, it is not the primary goal of amputation. The focus is on medical necessity and addressing the underlying condition.
During an amputation procedure, which structure is typically left intact to facilitate prosthetic fitting?
Explanation
During an amputation procedure, the bone stump is typically left intact to provide a stable base for prosthetic fitting. The muscles, nerves, and tendons are carefully dissected and secured to prevent complications and facilitate healing.
a. Muscles: While muscles are involved in the surgical procedure, they are typically resected to the appropriate level to accommodate the prosthetic device.
b. Nerves: Nerves are carefully dissected and secured during the amputation procedure to prevent neuromas and phantom limb pain but are not left intact for prosthetic fitting.
c. Tendons: Tendons are typically resected during the amputation procedure, and their positioning and attachment are crucial for proper wound closure and healing, but they are not left intact for prosthetic fitting.
Which surgical technique involves the removal of a limb at the joint level?
Explanation
Hip disarticulation involves the removal of the entire lower limb at the hip joint. This surgical technique is indicated for severe disease or trauma affecting the entire lower limb, where preservation of the knee joint is not feasible or beneficial.
b. Knee disarticulation: Knee disarticulation involves the removal of the lower limb at the knee joint. It is a different level of amputation compared to hip disarticulation.
c. Transfemoral amputation: Transfemoral amputation is the removal of the lower limb above the knee joint, preserving the femur. It is a different level of amputation compared to hip disarticulation.
d. Transtibial amputation: Transtibial amputation involves the removal of the lower limb below the knee joint, preserving the tibia. It is a different level of amputation compared to hip disarticulation.
During a below-the-knee amputation, what is the primary focus of the surgical technique?
Explanation
During a below-the-knee amputation, the primary focus of the surgical technique is to preserve the ankle joint whenever possible. This allows for better functional outcomes and facilitates the use of a prosthetic device.
b. Removing all muscles from the affected limb: While some muscle tissue is removed during amputation, the goal is not to remove all muscles. Some muscles are retained to provide coverage over the bone stump and to facilitate prosthetic fitting.
c. Creating a cosmetic incision line: While cosmetic considerations may be taken into account, the primary focus of the surgical technique is not solely on creating a cosmetic incision line. The incision is made to ensure appropriate tissue healing and to prevent complications.
d. Resecting the tibia and fibula bones: In a below-the-knee amputation, the tibia and fibula bones are typically resected to the appropriate level to accommodate the prosthetic device, but the primary focus is on preserving the ankle joint when possible.
What is the priority nursing intervention in the immediate post-operative period for a patient who has undergone amputation?
Explanation
The priority nursing intervention in the immediate post-operative period for a patient who has undergone amputation is to assess the surgical incision for signs of infection. Infection is a common concern after surgery, and early detection and intervention are crucial to prevent complications and promote healing.
a. Administering pain medications as prescribed: Pain management is important for the patient's comfort and well-being, but it is not the priority nursing intervention immediately after amputation. Assessing the surgical incision for signs of infection takes precedence to prevent potential complications.
c. Applying a compression bandage to the residual limb: While compression bandages may be used as part of the post-operative care, they are not the priority intervention immediately after amputation. Ensuring the surgical site's integrity and preventing infection are more critical in the early post-operative period.
d. Providing emotional support and counseling: Emotional support and counseling are essential for the patient's overall well-being, but they are not the priority nursing intervention in the immediate post-operative period. The focus at this time is on physical assessment and early detection of any complications.
What is the purpose of elevation in the post-operative care of a patient with a lower extremity amputation?
Explanation
The purpose of elevation in the post-operative care of a patient with a lower extremity amputation is to promote venous return and reduce swelling. Elevating the residual limb helps to decrease edema and improve blood flow, which can enhance healing and prevent complications such as deep vein thrombosis.
b. To improve the patient's comfort and relaxation: While elevation may improve the patient's comfort, the primary purpose is to address physiological concerns related to venous return and swelling.
c. To encourage early ambulation and mobility: Ambulation and mobility are essential components of post-operative care, but the specific purpose of elevation is not related to encouraging early ambulation.
d. To protect the surgical incision from contamination: While protecting the surgical incision is important, elevation is not the primary method for this purpose. Dressings and wound care techniques are used to protect the surgical site from contamination.
What is the appropriate method of positioning the residual limb in the post-operative period for a patient who underwent a below-the-knee amputation?
Explanation
The appropriate method of positioning the residual limb in the post-operative period for a patient who underwent a below-the-knee amputation is to elevate the residual limb on a pillow. Elevating the limb helps reduce swelling and promotes venous return, which can enhance healing and prevent complications.
a. Keep the residual limb in a dependent position: Keeping the residual limb in a dependent position (hanging down) can impede venous return and increase swelling. It is not the recommended position for post-operative care.
b. Maintain the residual limb in a flexed position: Keeping the residual limb in a flexed position may increase pressure on the surgical site and hinder proper wound healing. A flexed position is not the recommended post-operative positioning for the residual limb.
d. Keep the residual limb in a neutral, flat position: While keeping the residual limb in a neutral, flat position is generally recommended for some post-operative care, elevating the limb on a pillow is preferred in the immediate post-operative period for below-the-knee amputation to reduce swelling and promote healing.
What is the primary goal of wound care in the post-operative period for a patient who underwent amputation?
Explanation
The primary goal of wound care in the post-operative period for a patient who underwent amputation is to promote tissue regeneration and wound healing. Proper wound care techniques, including dressing changes, are essential to create an optimal environment for healing and prevent infection.
a. Preventing pressure ulcers and skin breakdown: While pressure ulcers and skin breakdown are important considerations in post-operative care, they are not the primary goal of wound care specifically for amputation.
c. Removing all dressings to allow for air exposure: Dressings are typically used to protect the surgical site and promote healing by creating a moist wound environment. Removing all dressings for air exposure is not recommended as it can impede wound healing.
d. Applying topical antibiotics to the surgical site: While topical antibiotics may be used if there is an infection or as directed by the healthcare provider, applying them to the surgical site without proper indication can lead to antibiotic resistance and is not the primary goal of wound care for amputation.
Why is meticulous monitoring of wound drainage important in the post-operative care of a patient who underwent amputation?
Explanation
Meticulous monitoring of wound drainage is important in the post-operative care of a patient who underwent amputation to assess for signs of infection. Excessive drainage, changes in color or odor, or the presence of pus may indicate an infection at the surgical site, and prompt intervention is essential to prevent complications.
b. To determine the need for wound irrigation: While wound irrigation may be part of wound care, monitoring wound drainage is primarily to assess for signs of infection, not to determine the need for wound irrigation.
c. To prevent pressure ulcers and skin breakdown: Monitoring wound drainage is not directly related to preventing pressure ulcers and skin breakdown. Preventing pressure ulcers involves measures such as repositioning and proper support surfaces.
d. To evaluate the effectiveness of pain management: Monitoring wound drainage does not directly evaluate the effectiveness of pain management. Pain management is assessed separately through communication with the patient and observation of their pain levels and response to interventions.
What is a potential complication of amputation that may occur in the immediate post-operative period?
Explanation
Delayed wound healing is a potential complication that may occur in the immediate post-operative period following amputation. Factors such as poor circulation, infection, or underlying health conditions can contribute to delayed healing of the surgical wound.
a. Phantom limb pain: Phantom limb pain is a sensation of pain, discomfort, or other sensations in the absent limb, but it is not typically an immediate post-operative complication. It may develop later as the nerve endings undergo reorganization.
c. Hypertrophic scarring: Hypertrophic scarring refers to excessive and raised scar tissue formation at the surgical site. While it can occur after amputation, it is not typically an immediate post-operative complication.
d. Contractures: Contractures are abnormal shortening and tightening of muscles and tendons, leading to restricted joint movement. While contractures can develop in the post-operative period, they are not usually immediate complications.
What is the primary purpose of a follow-up visit for a patient who underwent amputation?
Explanation
The primary purpose of a follow-up visit for a patient who underwent amputation is to adjust the prosthetic fitting and alignment. Prosthetic devices need to be customized and aligned correctly to ensure the patient's optimal mobility and function.
a. To assess for surgical wound dehiscence: While wound assessment is essential, it is not the primary purpose of a follow-up visit. Wound dehiscence, if present, would typically be detected earlier and addressed during the immediate post-operative period.
b. To provide emotional support and counseling: Emotional support and counseling are essential aspects of care for a patient who underwent amputation, but they are not the primary purpose of a follow-up visit, which focuses on the prosthetic fitting and functional outcomes.
d. To initiate post-operative physical therapy: Post-operative physical therapy may be initiated during the rehabilitation process, but it is not typically the primary purpose of a follow-up visit. Initial physical therapy sessions may begin earlier, often shortly after the amputation surgery.
Which complication of amputation may result in the need for revision surgery?
Explanation
A non-healing surgical wound is a significant complication of amputation that may require revision surgery. Revision surgery involves re-intervention on the surgical site to address wound healing issues and promote better outcomes.
a. Phantom limb sensation: Phantom limb sensation is a common experience after amputation but does not typically require revision surgery. It is a neurological phenomenon related to the brain's perception of the missing limb.
b. Skin breakdown and pressure ulcers: Skin breakdown and pressure ulcers can occur around the residual limb due to pressure and friction from the prosthetic device. While they require attention and management, they may not always necessitate revision surgery.
c. Infection at the surgical site: Infection at the surgical site is a serious complication, but it is typically managed with appropriate antimicrobial therapy and wound care. In some cases, infection may lead to revision surgery, but it is not an automatic indication.
Which assessment finding indicates a possible complication of a below-the-knee amputation?
Explanation
Increased swelling and bruising of the residual limb after a below-the-knee amputation may indicate a possible complication such as hematoma formation or poor wound healing. It requires further assessment and intervention by the healthcare team.
b. Mild tenderness and discomfort at the surgical site: Mild tenderness and discomfort are common after surgery and may be expected in the post-operative period. As long as the pain is manageable and not worsening, it is not necessarily an indication of a significant complication.
c. Gradual decrease in phantom limb pain over time: Phantom limb pain may gradually decrease over time as the nerve endings adapt to the amputation, and the brain's perception of the missing limb changes. This finding is a normal part of the post-amputation process and is not typically a complication.
d. Resumption of normal daily activities with a prosthetic limb: Resuming normal daily activities with a prosthetic limb is a positive outcome and a sign of successful rehabilitation and adaptation to the prosthesis. It is not indicative of a complication.
The nurse is caring for a patient who underwent a below-the-knee amputation. What is the primary purpose of positioning the residual limb in a flexed position?
Explanation
The primary purpose of positioning the residual limb in a flexed position after a below-the-knee amputation is to prevent contractures. Contractures are abnormal shortening and tightening of muscles and tendons, leading to restricted joint movement. Maintaining the limb in a flexed position helps prevent contractures and ensures optimal prosthetic fitting and functional outcomes.
b. To promote venous return: While positioning the limb in a flexed position may have some impact on venous return, it is not the primary purpose of this positioning. Elevating the limb on a pillow is more effective for promoting venous return.
c. To reduce edema: Keeping the residual limb elevated on a pillow is the preferred method for reducing edema in the immediate post-operative period, not positioning it in a flexed position.
d. To facilitate wound healing: Facilitating wound healing is not the primary purpose of positioning the residual limb in a flexed position. Proper wound care, dressing changes, and monitoring for signs of infection are essential for wound healing.
The nurse is providing education to a patient who will undergo an upper extremity amputation. What should the nurse emphasize as the priority nursing intervention in the immediate post-operative period?
Explanation
The priority nursing intervention in the immediate post-operative period after an upper extremity amputation is to assess the surgical incision for infection. Early detection of signs of infection, such as redness, swelling, warmth, or drainage, is crucial to prevent complications and promote healing.
a. Managing phantom limb pain: While managing phantom limb pain is important, it may not be the priority nursing intervention immediately after the surgery. Assessing the surgical incision for infection and monitoring for any complications take precedence.
b. Ensuring proper prosthetic fitting: Prosthetic fitting is essential for functional outcomes, but it may not be the priority in the immediate post-operative period. It is addressed during the rehabilitation phase.
c. Elevating the residual limb on a pillow: Elevating the residual limb on a pillow is typically recommended for lower extremity amputations to reduce edema and promote venous return, not for upper extremity amputations.
Which nursing intervention is essential to prevent skin breakdown in a patient with a lower extremity amputation who is using a prosthetic device?
Explanation
Inspecting the skin under the prosthetic device daily is essential to prevent skin breakdown and pressure ulcers. Continuous pressure and friction from the prosthetic device can cause skin irritation and breakdown, and early detection allows for timely intervention and prevention of complications.
a. Applying a topical antibiotic to the residual limb daily: Applying a topical antibiotic daily is not recommended unless specifically prescribed by the healthcare provider for a wound or infection. Routine use of topical antibiotics can lead to antibiotic resistance.
b. Massaging the residual limb with lotion to improve circulation: Massaging the residual limb with lotion may be beneficial for comfort, but it is not a preventive measure for skin breakdown. Excessive massage can cause skin irritation.
d. Wearing a compression bandage over the prosthetic device: While compression bandages may be used as part of post-operative care, wearing a compression bandage over the prosthetic device is not a standard preventive measure for skin breakdown.
The nurse is caring for a patient who underwent an above-the-knee amputation. What is the priority nursing intervention to prevent hip flexion contractures?
Explanation
The priority nursing intervention to prevent hip flexion contractures after an above-the-knee amputation is performing passive range of motion exercises to the hip joint. Contractures are abnormal shortening and tightening of muscles and tendons, leading to restricted joint movement. Passive range of motion exercises help maintain joint flexibility and prevent contractures.
b. Elevating the residual limb on a pillow: Elevating the residual limb on a pillow is more applicable for preventing swelling and edema, not specifically for preventing hip flexion contractures.
c. Administering analgesics as prescribed: While pain management is essential for the patient's comfort, it is not directly related to preventing hip flexion contractures.
d. Providing emotional support and counseling: Emotional support and counseling are important aspects of care but are not directly related to preventing hip flexion contractures.
The nurse is caring for a patient who had a below-the-elbow amputation. Which activity should the nurse encourage the patient to perform during the post-operative period to promote muscle strength and flexibility in the residual limb?
Explanation
Encouraging the patient to perform active range of motion exercises is important to promote muscle strength and flexibility in the residual limb after a below-the-elbow amputation. Active exercises engage the muscles and joints, preventing stiffness and maintaining function.
a. Lifting heavy weights with the residual limb: Lifting heavy weights with the residual limb may be contraindicated, especially in the immediate post-operative period, as it can strain the healing tissues and lead to injury.
c. Keeping the residual limb immobile: Keeping the residual limb immobile can lead to stiffness, weakness, and contractures. Active range of motion exercises are essential to maintain mobility and function.
d. Applying cold packs to the residual limb: Cold packs may be used for pain relief or to reduce swelling in the immediate post-operative period, but they are not specifically aimed at promoting muscle strength and flexibility in the residual limb. Active exercises are more appropriate for this purpose.
Which nursing intervention is essential for preventing complications in the immediate post-operative period after amputation?
Explanation
Assessing the surgical incision for signs of infection is essential in the immediate post-operative period after amputation to detect any early signs of complications such as infection. Prompt identification and intervention can prevent further complications and promote healing.
a. Administering opioid pain medications regularly: While pain management is important after amputation, administering opioid pain medications regularly may lead to potential side effects and dependency. Pain medications should be given as needed and in response to the patient's pain level.
c. Encouraging the patient to perform active range of motion exercises: Active range of motion exercises may not be appropriate immediately after amputation due to wound healing and surgical site considerations. The focus in the immediate post-operative period is on wound care and monitoring.
d. Providing emotional support and counseling: Emotional support and counseling are essential for a patient who underwent amputation, but in the immediate post-operative period, the priority is on physical assessment and wound care.
What is the primary goal of positioning the residual limb in the post-operative period after amputation?
Explanation
The primary goal of positioning the residual limb in the post-operative period after amputation is to promote venous return and reduce swelling. Elevating the limb helps improve blood flow and reduce edema, which can enhance healing and prevent complications.
b. To improve the patient's comfort and relaxation: While positioning may improve the patient's comfort, the primary goal is related to physiological considerations such as venous return and swelling reduction.
c. To encourage early ambulation and mobility: Early ambulation and mobility are important components of post-operative care, but the primary goal of positioning is not directly related to encouraging ambulation.
d. To protect the surgical incision from contamination: Positioning the residual limb is not primarily intended to protect the surgical incision from contamination. Dressings and wound care techniques are used for this purpose.
What is the primary purpose of wound care in the post-operative period after amputation?
Explanation
The primary purpose of wound care in the post-operative period after amputation is to promote tissue regeneration and wound healing. Proper wound care techniques, including dressing changes, are essential to create an optimal environment for healing and prevent infection.
a. To prevent pressure ulcers and skin breakdown: While pressure ulcers and skin breakdown are important considerations in post-operative care, they are not the primary purpose of wound care specifically for amputation.
c. To remove all dressings to allow for air exposure: Dressings are typically used to protect the surgical site and promote healing by creating a moist wound environment. Removing all dressings for air exposure is not recommended as it can impede wound healing.
d. To apply topical antibiotics to the surgical site: While topical antibiotics may be used if there is an infection or as directed by the healthcare provider, applying them to the surgical site without proper indication can lead to antibiotic resistance and is not the primary purpose of wound care for amputation.
What is a common complication that may occur in the immediate post-operative period after amputation?
Explanation
Delayed wound healing is a common complication that may occur in the immediate post-operative period after amputation. Factors such as poor circulation, infection, or underlying health conditions can contribute to delayed healing of the surgical wound.
a. Phantom limb pain: Phantom limb pain is a sensation of pain, discomfort, or other sensations in the absent limb, but it is not typically an immediate post-operative complication. It may develop later as the nerve endings undergo reorganization.
c. Hypertrophic scarring: Hypertrophic scarring refers to excessive and raised scar tissue formation at the surgical site. While it can occur after amputation, it is not typically an immediate post-operative complication.
d. Contractures: Contractures are abnormal shortening and tightening of muscles and tendons, leading to restricted joint movement. While contractures can develop in the post-operative period, they are not usually immediate complications.
Which nursing intervention is important to prevent infection in a patient who underwent amputation?
Explanation
Using sterile technique during wound dressing changes is important to prevent infection in a patient who underwent amputation. Sterile technique helps reduce the risk of introducing microorganisms into the wound, promoting healing and reducing the risk of complications.
a. Performing passive range of motion exercises regularly: Passive range of motion exercises may be appropriate at the appropriate time during the rehabilitation process but are not directly related to preventing infection.
b. Applying a compression bandage to the residual limb: Compression bandages may be used as part of post-operative care, but they are not the primary intervention to prevent infection.
d. Encouraging the patient to bear weight on the residual limb: Encouraging weight-bearing on the residual limb is part of the rehabilitation process but may not be appropriate immediately after amputation. It is not a direct measure to prevent infection.
Exams on Musculoskeletal System
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
Notes Highlighting is available once you sign in. Login Here.
Skin Traction
Skin traction is a common orthopedic intervention used to stabilize and align fractures or dislocations.
As a healthcare professional, understanding the principles, indications, application, and nursing care associated with skin traction is crucial for providing safe and effective care for patients undergoing this treatment.
Objectives
- Describe the purpose and principles of skin traction, including its role in reducing and stabilizing fractures.
- Identify the appropriate indications and contraindications for the use of skin traction in patient care.
- Demonstrate the correct application and removal of skin traction devices, ensuring proper placement and alignment to achieve therapeutic outcomes.
- Evaluate the patient's skin integrity regularly, recognize early signs of pressure ulcers or skin breakdown associated with skin traction, and implement appropriate interventions to prevent complications.
- Develop a comprehensive nursing care plan for a patient in skin traction, incorporating strategies to promote patient comfort, mobility, and safety while minimizing potential complications.
Definition and Background
- Skin traction is a non-invasive method of applying external force to a fractured or dislocated limb to stabilize bone alignment and provide pain relief.
- It involves the application of a pulling force through the patient's skin using adhesive strapping or elastic bandages, rather than through pins or wires inserted directly into the bone.
- Skin traction is typically used as a temporary measure until definitive treatment, such as surgery or skeletal traction, can be initiated.
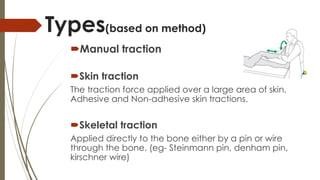
Indications for Skin Traction
1. Fractures:
- Skin traction may be indicated for certain types of fractures, particularly those involving long bones or bones of the lower extremities.
- It can be used to stabilize fractures of the femur, tibia, fibula, humerus, and other long bones, providing temporary immobilization until definitive treatment can be initiated.
2. Dislocations:
- Skin traction is beneficial in reducing and stabilizing dislocated joints, particularly in the hip and knee.
- By exerting a pulling force on the affected joint, skin traction can help realign the joint components, reducing pain and preventing further damage until further management is possible.
3. Preoperative Stabilization:
- Skin traction may be utilized as a preparatory measure before surgical intervention, particularly in cases where surgery may be delayed or when the patient's condition requires stabilization before the procedure.
- By aligning bones and reducing pain, skin traction can optimize the surgical procedure's safety and effectiveness.
4. Pain Relief:
- Skin traction is often used to provide pain relief in patients with fractures or dislocations.
- The traction force helps to reduce pressure on injured tissues and nerves, alleviating pain and promoting patient comfort.
5. Temporarily Unfit for Surgery:
- In some cases, a patient's overall health or other medical conditions may temporarily preclude them from undergoing surgery.
- Skin traction can be employed as a temporary measure to stabilize the injury and manage pain until the patient is fit for the surgical procedure.
6. Pediatric Patients:
- Skin traction is commonly used in pediatric patients with certain types of fractures, especially those involving the femur.
- It can provide effective stabilization and alignment in children, who may not be suitable candidates for other forms of traction due to their age and size.
7. Non-Surgical Approach:
- Skin traction is a non-invasive treatment option, making it suitable for patients who are not candidates for more invasive traction methods, such as skeletal traction.
8. Skeletal Immaturity:
- In pediatric patients with open growth plates, skin traction may be preferred over other forms of traction to minimize the risk of growth plate damage or complications.
Types of Skin Traction
Buck's Traction:
- Buck's traction is commonly used for lower extremity fractures, such as fractures of the femur, tibia, or fibula.
- The traction force is applied through a boot-like device placed on the lower leg, with the patient's knee in slight flexion.
- Adhesive straps or bandages are used to secure the traction to the leg, and weights are applied to the end of the bed to provide the pulling force.
Russell's Traction:
- Russell's traction is utilized for fractures of the femur or dislocated hips, where greater traction force is required.
- The patient's affected leg is placed in a sling-like device that extends from the hip to just above the ankle.
- Weights are attached to the traction apparatus, and the patient's hip and knee joints are maintained in a slightly flexed position.
Bryant's Traction:
- Bryant's traction is primarily used for pediatric patients with femur fractures.
- Both lower extremities are elevated and suspended off the bed, and traction is applied to both legs using adhesive strapping or bandages.
- The patient is positioned in a supine position, and weights are attached to the traction to provide the necessary force.
Pelvic Skin Traction:
- Pelvic skin traction is applied to stabilize and align fractures or dislocations involving the pelvis.
- Traction is exerted on the pelvis through pelvic belts or adhesive strapping, which are secured to the patient's body.
- This type of traction requires careful assessment and monitoring due to the proximity to vital structures and potential complications.
Cervical Skin Traction:
- Cervical skin traction is applied to the cervical spine to stabilize and reduce fractures or dislocations in this region.
- Traction is exerted through the use of a cervical collar or head halter that is secured around the patient's neck and attached to a weight system.
Upper Extremity Skin Traction:
- Skin traction can also be applied to fractures or dislocations involving the upper extremities, such as the humerus or radius/ulna.
- The affected arm is usually placed in a sling-like device or splint, and traction is applied through adhesive strapping or bandages with weights.
Modified Skin Traction:
- In some cases, healthcare providers may use a modified approach to skin traction based on the patient's unique condition and needs.
- This may involve adaptations to the type of traction device used or the amount of traction force applied.
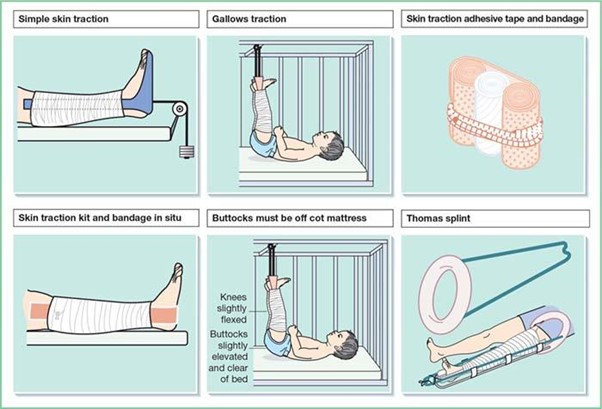
Nursing Care of Patient with Skin Traction
- Assessment: Perform a thorough assessment of the patient's limb, including neurovascular status, skin integrity, and pain level, before and after traction application.
- Traction Setup: Ensure the correct setup of the traction apparatus, including proper positioning of the weights and ensuring they hang freely without touching the floor.
- Skin Assessment: Regularly assess the skin under the traction apparatus for signs of pressure, irritation, or breakdown, and provide appropriate skin care.
- Neurovascular Checks: Perform frequent neurovascular checks to assess circulation, sensation, and motor function of the affected limb to detect any signs of compromised perfusion or nerve function.
- Pain Management: Monitor the patient's pain level and administer prescribed pain medications as needed to ensure comfort and optimal traction tolerance.
- Positioning: Assist the patient in maintaining the prescribed position, as movement outside of the specified parameters may affect the effectiveness of traction.
- Mobility: Encourage active and passive range-of-motion exercises for the unaffected limbs to prevent complications related to immobility.
- Hygiene and Comfort: Provide measures to maintain hygiene and comfort, such as ensuring a clean and dry environment and using pillows or foam padding to alleviate pressure on bony prominences.
- Education: Educate the patient and family about the purpose and care of the skin traction, including the importance of maintaining proper body alignment and avoiding excessive weight-bearing on the affected limb.
Complications and Interventions
Complications of Skin Traction:
- Skin Breakdown: Prolonged application of skin traction can lead to pressure and friction on the skin, resulting in skin breakdown, pressure ulcers, or open sores.
- Circulatory Compromise: Improperly applied or excessively tight traction may impede blood flow, leading to circulatory compromise, ischemia, and tissue damage.
- Nerve Compression: Traction forces may compress nerves, leading to neuropathy, numbness, tingling, or loss of sensation in the affected limb.
- Joint Stiffness: Extended immobilization in traction can contribute to joint stiffness, contractures, and decreased range of motion.
- Muscle Atrophy: Prolonged immobility and reduced weight-bearing can cause muscle wasting and weakness in the affected limb.
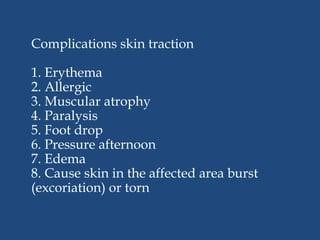
Interventions to Prevent Complications:
- Regular Repositioning: Reposition the patient regularly to relieve pressure on bony prominences and distribute weight evenly on the skin.
- Skin Assessment: Perform frequent skin assessments to identify areas of pressure or early signs of skin breakdown. Provide appropriate skin care and ensure the skin is clean and dry.
- Padding and Pressure-Relieving Devices: Use foam padding or pressure-relieving devices under bony prominences to minimize pressure and protect the skin.
- Adequate Traction Setup: Ensure that the traction apparatus is correctly set up, and weights hang freely without touching the floor, reducing the risk of traction-related complications.
- Neurovascular Checks: Perform regular neurovascular checks to assess circulation, sensation, and motor function of the affected limb. Report any changes in neurovascular status promptly.
- Encourage Mobility: Encourage active and passive range-of-motion exercises for unaffected limbs to maintain joint mobility and prevent muscle atrophy.
- Educate Patients and Families: Educate the patient and family about the importance of maintaining proper body alignment, adhering to prescribed traction parameters, and promptly reporting any concerns or complications.
Collaboration and Communication
Collaboration: Work collaboratively with the healthcare team, including physicians, physical therapists, and occupational therapists, to ensure proper management and monitoring of the patient's traction.
Communication: Effectively communicate with the patient and family, providing clear explanations of the treatment plan, potential complications, and expectations for recovery and mobilization.
Evaluation
Neurovascular Status:
- Monitor the patient's neurovascular status regularly, especially in the affected limb undergoing traction.
- Assess for signs of impaired circulation, such as pallor, cyanosis, coolness, or diminished pulses.
- Evaluate sensory and motor function in the affected limb to detect any signs of nerve compression or compromise.
Pain Assessment:
- Assess the patient's pain level regularly, considering both the intensity and location of pain.
- Document any changes in pain intensity and the effectiveness of pain management interventions.
- Evaluate the patient's response to traction in terms of pain relief and comfort.
Alignment of Fracture or Dislocation:
- Evaluate the alignment of the fractured or dislocated bone to determine the effectiveness of the traction in stabilizing and reducing the injury.
- Collaborate with the healthcare provider to ensure proper positioning and adjustments if needed to achieve optimal alignment.
Skin Integrity:
- Regularly assess the skin under the traction apparatus for signs of pressure, irritation, or breakdown.
- Look for areas of redness, blistering, or skin breakdown, especially around bony prominences or areas in direct contact with the traction.
- Implement appropriate skin care measures and provide padding or pressure-relieving devices as needed.
Traction Setup:
- Ensure that the traction apparatus is correctly set up, and the weights hang freely without touching the floor.
- Check that the traction force is maintained at the prescribed level and adjusted as needed based on the healthcare provider's orders.
Mobility and Range of Motion:
- Assess the patient's mobility and range of motion, particularly in unaffected limbs.
- Encourage the patient to perform active and passive range-of-motion exercises to prevent complications related to immobility.
Patient Comfort and Satisfaction:
- Engage in communication with the patient to assess their comfort level, understanding of the traction process, and satisfaction with the care provided.
- Address any concerns or questions the patient may have and provide emotional support as needed.
Complications and Adverse Effects:
- Monitor for potential complications related to skin traction, such as skin breakdown, pressure ulcers, circulatory compromise, nerve compression, joint stiffness, or muscle atrophy.
- Report any adverse effects to the healthcare provider promptly for appropriate intervention.
Treatment Outcomes:
- Evaluate the overall treatment outcomes, including pain relief, improvement in fracture alignment or dislocation reduction, and patient's progress toward recovery.
- Collaborate with the healthcare team to assess the need for ongoing traction, transition to other treatment modalities, or preparation for surgical intervention if indicated.
Conclusion
In conclusion, skin traction is a valuable orthopedic intervention used to stabilize fractures or dislocations and provide pain relief.
As a healthcare professional, your role in the nursing care of a patient with skin traction is crucial in ensuring safe and effective treatment.
By conducting thorough assessments, monitoring for complications, providing adequate skin care, promoting mobility, and educating the patient and family, you can contribute to the patient's successful recovery and overall well-being.
X-RAY Imaging
Objectives
- Describe the principles of X-ray imaging: Upon completion of this topic, learners will be able to explain the basic principles of X-ray imaging, including the production of X-rays, their interaction with tissues, and the formation of X-ray images.
- Identify indications and contraindications for X-ray imaging: After studying this topic, learners will be able to recognize common clinical indications for X-ray imaging in various medical conditions, as well as identify contraindications for X-ray procedures, such as pregnancy or potential risks in certain patient populations.
- Demonstrate radiation safety measures in X-ray imaging: By the end of this topic, learners will be able to apply radiation safety principles, including the ALARA (As Low As Reasonably Achievable) concept, to minimize radiation exposure to both patients and healthcare providers during X-ray procedures.
- Explain patient preparation and positioning for X-ray imaging: Upon completion of this topic, learners will be able to describe the essential steps of patient preparation for X-ray imaging, including obtaining informed consent, removing metal objects, and providing proper patient positioning to ensure accurate imaging results.
- Analyze and interpret X-ray images: After studying this topic, learners will be able to interpret basic X-ray images, identify normal anatomical structures, and recognize common abnormalities, such as fractures, dislocations, and foreign bodies, to support clinical decision-making and patient care planning.
Introduction
X-ray imaging, also known as radiography, is a common diagnostic imaging technique used to visualize internal structures of the body, such as bones, soft tissues, and organs.
X-rays are produced by passing a controlled amount of radiation through the body, and the resulting images provide valuable information for diagnosing various medical conditions.
As a healthcare professional, understanding the principles of X-ray care, safety measures, and patient preparation is essential to ensure accurate imaging results and the well-being of patients.

Principles of X-ray Imaging
- Ionizing Radiation: X-rays are a form of ionizing radiation that can penetrate body tissues and interact with atoms, producing images on X-ray film or digital detectors.
- Absorption: Different tissues in the body absorb X-rays to varying degrees. Dense tissues, such as bones, absorb more X-rays and appear white on X-ray images, while less dense tissues appear darker.
- X-ray Views: X-rays can be taken from different angles (e.g., anteroposterior, lateral, oblique) to visualize specific structures or identify abnormalities from multiple perspectives.
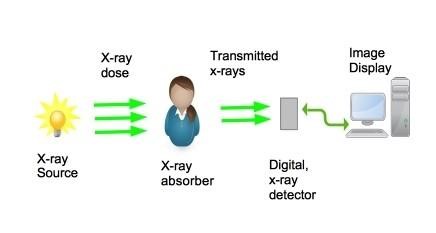
Patient Preparation
- Informed Consent: Before performing an X-ray, healthcare providers must obtain informed consent from the patient or their legal guardian, explaining the procedure, its purpose, and any potential risks.
- Remove Metal Objects: Patients should remove all metal objects, including jewelry, watches, and clothing with metal zippers or fasteners, to prevent artifacts on the X-ray image.
- Protective Aprons: Lead aprons or shields should be provided to patients, especially pregnant women, to protect them from unnecessary radiation exposure.
- Pregnancy Assessment: Female patients of childbearing age should be asked about the possibility of pregnancy, and X-rays should be deferred if not medically urgent or performed only with additional shielding.
- Patient Comfort and Positioning: Ensure the patient is comfortable and properly positioned to achieve optimal imaging results.
Safety Measures
- Radiation Protection: X-ray technologists and other healthcare personnel should wear lead aprons, thyroid collars, and protective gloves to minimize radiation exposure during the procedure.
- Distance: Whenever possible, healthcare providers should maintain a safe distance from the X-ray tube and the patient during exposure to reduce radiation exposure.
- Time: Limit the time of exposure to X-rays by using the shortest exposure time necessary to obtain diagnostic images.
- Collimation: Use collimators to restrict the X-ray beam to the specific area of interest and minimize unnecessary radiation exposure to surrounding tissues.
- Shielding: Employ appropriate shielding techniques to protect sensitive areas, such as the reproductive organs, from radiation exposure.
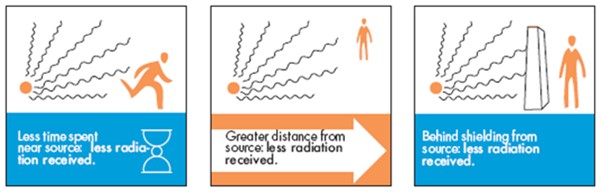
Patient Safety and Communication
- Patient Identification: Verify the patient's identity using two patient identifiers (e.g., name and date of birth) before performing an X-ray to ensure correct patient identification.
- Communication: Inform the patient about the procedure, explain any necessary instructions or breath-holding techniques, and answer any questions or concerns they may have.
- Immobilization: Instruct the patient to remain still during the X-ray exposure to avoid blurring the images and ensure accurate diagnosis.
Pediatric Considerations
- Special Precautions: Minimize the number of X-rays performed on pediatric patients and use lead shielding appropriately to reduce radiation exposure.
- Parental Presence: Encourage parents or caregivers to be present during the X-ray to provide comfort and reassurance to the child.
Documentation and Post-Procedure Care
- Accurate Documentation: Thoroughly document the X-ray procedure, including the type of X-ray performed, patient positioning, and any relevant observations or patient responses.
- Post-Procedure Care: Provide appropriate post-procedure care, including addressing any immediate concerns or discomfort experienced by the patient.
Conclusion
X-ray imaging is a valuable diagnostic tool used to visualize the internal structures of the body.
As healthcare professionals, adhering to principles of X-ray imaging, following safety measures, and ensuring proper patient preparation and communication are crucial for obtaining accurate and useful X-ray images while safeguarding the well-being of patients and healthcare providers.
By incorporating best practices in X-ray care, healthcare professionals can optimize patient care and diagnostic outcomes, leading to improved clinical decision-making and patient management.
Bone Marrow Aspiration
Objectives
- Describe the purpose and indications for bone marrow aspiration.
- Identify the appropriate anatomical sites commonly used for bone marrow aspiration.
- Demonstrate the steps of the bone marrow aspiration procedure, including patient positioning and sterile technique.
- Recognize potential complications and risks associated with bone marrow aspiration and implement appropriate nursing interventions to address them.
- Discuss the nursing responsibilities in caring for a patient before, during, and after a bone marrow aspiration procedure, including patient education and post-procedure follow-up.
- Evaluate the patient's understanding of the bone marrow aspiration procedure and their ability to provide informed consent.
- Develop a plan of care for patients undergoing bone marrow aspiration, addressing their physical and emotional needs during the procedure.
- Identify the appropriate equipment and supplies needed for a bone marrow aspiration procedure and ensure their readiness.
- Discuss the significance and interpretation of laboratory results obtained from bone marrow aspirates.
- Collaborate effectively with the interprofessional healthcare team to provide comprehensive care for patients undergoing bone marrow aspiration.
Introduction
Bone marrow aspiration is a diagnostic and therapeutic procedure performed to obtain a sample of bone marrow from the patient's body.
The bone marrow is a soft, spongy tissue found inside certain bones, and it is responsible for the production of blood cells, including red blood cells, white blood cells, and platelets.
Bone marrow aspiration provides valuable information about the health and functioning of the bone marrow and is often used to diagnose various hematological disorders and to assess treatment responses in certain conditions.
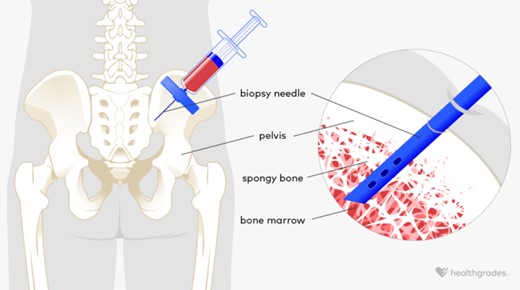
Indications for Bone Marrow Aspiration
Bone marrow aspiration is indicated for various medical reasons, including:
- Diagnosis of Hematological Disorders: It is used to diagnose and differentiate between different types of anemia, leukemia, lymphoma, and other blood-related diseases.
- Staging and Prognostication: In patients with known hematologic malignancies, bone marrow aspiration helps determine the disease stage and predict the prognosis.
- Monitoring Treatment Responses: It is used to assess the response to chemotherapy or other treatments in patients with hematologic cancers.
- Unexplained Cytopenias: Bone marrow aspiration helps investigate unexplained low blood cell counts, such as anemia, leukopenia, or thrombocytopenia.
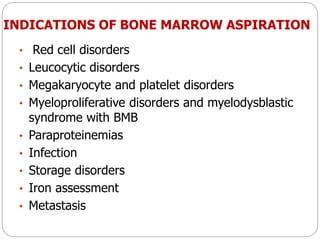
- Fever of Unknown Origin: In cases of prolonged fever with no apparent cause, bone marrow aspiration may help identify an underlying infection or malignancy.
- Donor Assessment for Transplant: Before hematopoietic stem cell transplantation, bone marrow aspiration is performed to evaluate potential donors.
Procedure Overview
Bone marrow aspiration is typically performed by a hematologist, oncologist, or other trained healthcare provider. The procedure involves the following steps:
- Patient Preparation: The patient is positioned comfortably, usually lying on their side or abdomen. Local anesthesia is administered to numb the skin and the bone marrow site.
- Site Selection: The most common sites for bone marrow aspiration are the posterior iliac crest (hipbone) and the sternum (breastbone). The specific site is chosen based on the patient's age, medical condition, and provider preference.
- Aspiration Process: Using a specialized needle, the healthcare provider carefully inserts the needle into the bone marrow space, puncturing the bone's hard outer surface to reach the spongy marrow.
- Aspiration and Biopsy: Once the needle is correctly positioned within the bone marrow space, a syringe is used to aspirate a small amount of liquid bone marrow, which contains blood and stem cells. A bone marrow biopsy may also be performed by removing a small core of bone and marrow tissue for further examination.
- Post-Procedure Care: After the procedure, pressure is applied to the site to control bleeding, and a dressing is applied. The patient is observed for any immediate complications or adverse reactions.
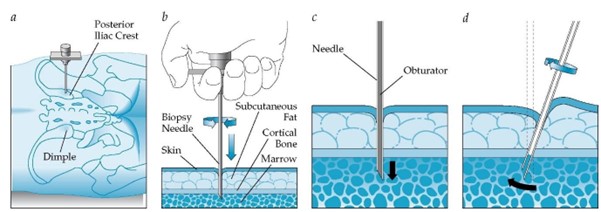
Potential Complications and Risks
Bone marrow aspiration is generally considered safe, but like any medical procedure, it carries some risks and potential complications, including:
- Pain or Discomfort: The procedure may cause temporary pain or discomfort at the aspiration site.
- Bleeding: There is a risk of bleeding at the aspiration site, which can usually be managed with direct pressure.
- Infection: Although rare, there is a small risk of infection at the aspiration site.
- Vasovagal Reaction: Some patients may experience a temporary drop in blood pressure or fainting due to anxiety or discomfort during the procedure.
- Damage to Surrounding Structures: In rare cases, the needle may cause injury to nearby blood vessels, nerves, or organs.
Post-Procedure Follow-Up
Following bone marrow aspiration, the collected samples are sent to the laboratory for analysis.
Results from the bone marrow examination are used to make or confirm a diagnosis, monitor treatment responses, or plan further medical management.
Patients may experience mild soreness or discomfort at the aspiration site for a few days, and they are advised to avoid strenuous activities for a short period.
Conclusion
Bone marrow aspiration is a valuable procedure used for diagnostic and therapeutic purposes in patients with various hematological disorders.
It provides crucial information about the health and functioning of the bone marrow, and it is an essential tool for hematologists, oncologists, and other healthcare professionals in the diagnosis and management of hematologic conditions.
By understanding the indications, procedure, potential risks, and post-procedure care, healthcare providers can ensure the safe and effective use of bone marrow aspiration in patient care.
Paget’s Disease
Objectives
- Identify the pathophysiology and etiology of Paget's disease, including the role of genetic factors and environmental influences.
- Recognize the clinical manifestations of Paget's disease, such as bone pain, deformities, and neurological symptoms, to facilitate early detection and appropriate management.
- Differentiate Paget's disease from other bone disorders through radiological and laboratory assessments, enhancing diagnostic accuracy.
- Describe the pharmacological and non-pharmacological treatment options for Paget's disease, outlining their mechanisms of action and potential side effects.
- Develop nursing care plans that address the physical, psychosocial, and educational needs of patients with Paget's disease, promoting optimal quality of life and adherence to treatment regimens.
Introduction
Paget's disease, also known as osteitis deformans, is a chronic and progressive bone disorder that primarily affects older adults.
It is characterized by abnormal bone remodeling, leading to enlarged and weakened bones.
Although the exact cause of Paget's disease remains unclear, it is believed to result from a combination of genetic and environmental factors.
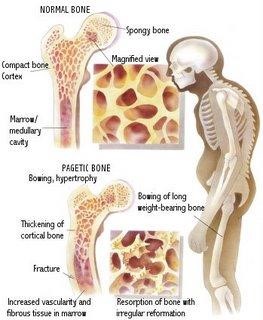
Pathophysiology
- Paget's disease involves a dysregulation in bone remodeling, leading to an imbalance between bone resorption and bone formation.
- Initially, there is excessive bone resorption, during which osteoclasts become overactive, leading to the destruction of bone tissue.
- In response to the increased bone resorption, the body attempts to repair the bone by laying down new bone tissue through osteoblasts.
- However, the new bone formed is disorganized and structurally weak, leading to enlarged, misshapen, and brittle bones.
- The affected bones may be prone to fractures and may cause symptoms such as bone pain, deformities, and neurological complications if bones compress surrounding nerves.
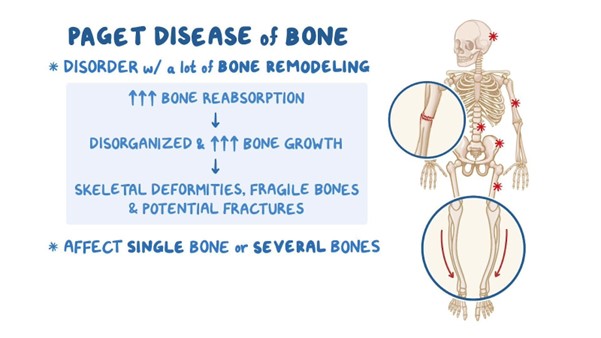
Clinical Manifestations
Paget's disease often starts asymptomatically, and the condition may be incidentally discovered on routine imaging or blood tests.
As the disease progresses, common clinical manifestations may include:
- Bone Pain: Patients may experience deep, aching bone pain, which is commonly localized in the pelvis, spine, and legs.
- Bone Deformities: Enlargement and deformities of bones may lead to changes in posture and gait.
- Fractures: Weakened bones are more susceptible to fractures, especially in weight-bearing bones like the hips and legs.
- Neurological Complications: In some cases, enlarged bones can compress adjacent nerves, leading to neurological symptoms such as tingling, numbness, or weakness.
- Hearing Loss: Paget's disease can affect the bones of the skull, including those surrounding the ear, potentially leading to hearing loss.
- Cardiovascular Complications: Rarely, Paget's disease may affect the heart, leading to heart failure in severe cases.
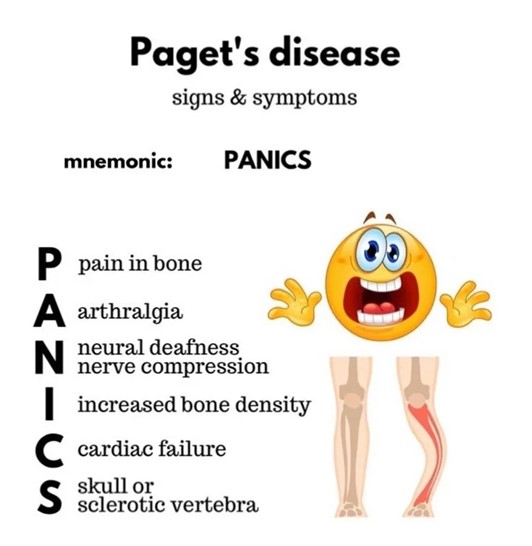
Diagnosis
- The diagnosis of Paget's disease is made through a combination of clinical evaluation, imaging studies, and laboratory tests.
- X-rays and bone scans may show characteristic changes in affected bones, such as enlarged and deformed bone structures.
- Blood tests, specifically measuring serum alkaline phosphatase (ALP) and urinary hydroxyproline levels, can help assess the extent of bone turnover.
- In some cases, a bone biopsy may be performed to confirm the diagnosis and rule out other bone disorders.

Treatment
- The management of Paget's disease aims to alleviate symptoms, prevent complications, and improve bone health.
- Bisphosphonates are the mainstay of treatment, as they inhibit bone resorption and promote more normal bone remodeling.
- Pain management with analgesics and anti-inflammatory medications may be necessary to address bone pain.
- In cases of severe bone deformities, fractures, or neurological complications, surgical intervention may be considered.
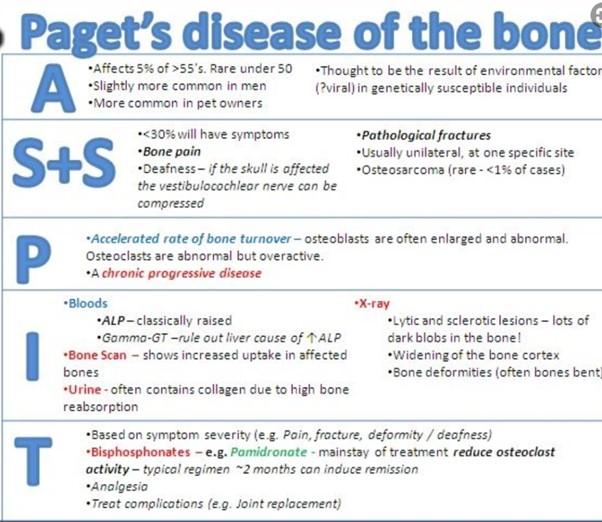
Patient Education
- Patients with Paget's disease should receive education on the nature of the condition, its treatment options, and the importance of adherence to prescribed medications.
- Encourage weight-bearing exercises and physical therapy to maintain bone strength and improve mobility.
- Advise patients to report any new or worsening bone pain, fractures, or neurological symptoms promptly.
Nursing Considerations
- Provide supportive care and pain management for patients experiencing bone pain and fractures.
- Monitor for signs of complications such as neurological deficits, hearing impairment, and cardiovascular issues.
- Educate patients and their families on the importance of medication compliance and regular follow-up visits.
- Collaborate with a multidisciplinary healthcare team, including physicians, physical therapists, and social workers, to optimize patient care and quality of life.
Conclusion
In conclusion, Paget's disease is a chronic bone disorder characterized by abnormal bone remodeling, leading to enlarged and weakened bones.
Clinical manifestations include bone pain, deformities, fractures, and potential neurological or hearing complications.
Diagnosis is based on clinical evaluation, imaging studies, and laboratory tests.
Treatment involves bisphosphonates and supportive care, while patient education and nursing considerations are essential in optimizing patient outcomes and quality of life.
Fractures
Objectives
- Identify the different types of fractures and their characteristics, such as open, closed, displaced, and non-displaced fractures.
- Describe the process of fracture healing, including the stages of inflammation, repair, and remodeling.
- Recognize the signs and symptoms of a fracture, including pain, swelling, deformity, and loss of function.
- Explain the appropriate nursing interventions for a patient with a fracture, including immobilization, pain management, and wound care.
- Discuss the potential complications associated with fractures and their prevention strategies, such as infection, compartment syndrome, and delayed union.
Introduction
Fractures, also known as broken bones, are common injuries that occur when the structural integrity of a bone is disrupted due to excessive force, trauma, or repetitive stress.
Fractures can vary in severity, ranging from minor cracks or hairline fractures to complete bone breaks with displacement.
Understanding fractures is essential for healthcare professionals as they are prevalent in clinical practice, and comprehensive knowledge enables proper assessment, treatment, and management of patients with these injuries.
Classification of Fractures
Fractures can be classified based on various criteria, including the mechanism of injury, location, pattern of the break, and whether the bone is displaced or not. Common types of fractures include:
- Closed (Simple) Fracture: The bone breaks but does not penetrate the skin.
- Open (Compound) Fracture: The broken bone penetrates through the skin, increasing the risk of infection.
- Greenstick Fracture: Common in children, the bone bends and partially breaks, similar to a green twig.
- Comminuted Fracture: The bone shatters into multiple fragments.
- Transverse Fracture: The break occurs in a straight line across the bone.
- Oblique Fracture: The break is at an angle to the bone's long axis.
- Spiral Fracture: The fracture spirals around the bone due to torsional forces.
- Impacted Fracture: The bone fragments are driven into each other.
- Pathological Fracture: Occurs in weakened bones due to underlying conditions like osteoporosis or cancer.
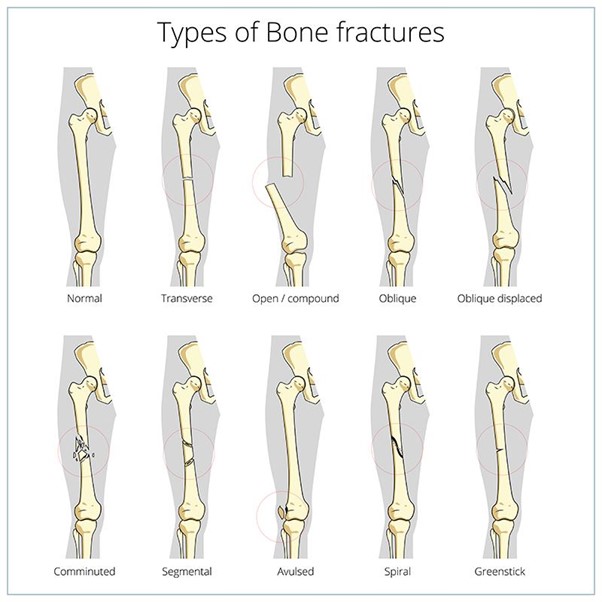
Etiology and Risk Factors
Fractures can result from various causes, including:
- Traumatic Injury: Falls, motor vehicle accidents, sports-related injuries, and direct blows are common traumatic causes of fractures.
- Overuse or Repetitive Stress: Repeated stress on bones, as seen in stress fractures, can cause small cracks to develop.
- Osteoporosis: Decreased bone density and strength in osteoporosis increase the risk of fractures, especially in older adults.
- Pathological Conditions: Certain medical conditions weaken bones, making them more susceptible to fractures.
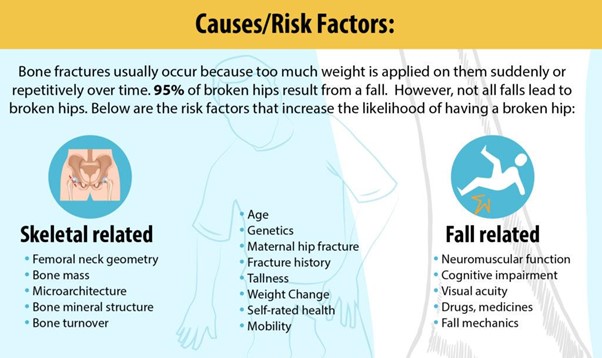
Clinical Manifestations
The signs and symptoms of fractures depend on the type and location of the injury but may include:
- Pain: Intense pain at the site of the fracture, aggravated by movement or pressure.
- Swelling: Localized swelling and bruising due to tissue damage and bleeding.
- Deformity: Visible deformity, angulation, or abnormal alignment of the affected limb.
- Loss of Function: Inability to move or bear weight on the injured limb.
- Crepitus: A grating or crackling sensation or sound at the fracture site caused by bone fragments rubbing against each other.
- Open Wound (in Open Fractures): In cases of open fractures, the bone may protrude through the skin, increasing the risk of infection.
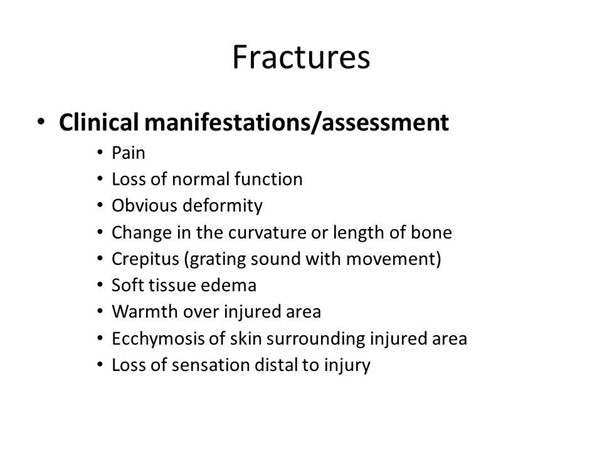
Assessment and Diagnosis
A thorough assessment of a suspected fracture includes:
- History-Taking: Gathering information about the mechanism of injury and any associated symptoms.
- Physical Examination: Assessing for swelling, deformities, crepitus, range of motion, and neurovascular status.
- Radiographic Imaging: X-rays are the primary diagnostic tool to confirm the presence, type, and extent of the fracture.
Treatment and Management
The management of fractures aims to promote healing and restore function, and it may include:
- Immobilization: Splints, casts, or braces are used to stabilize the fracture and prevent further displacement during the initial healing phase.
- Reduction: Closed or open reduction is performed to realign displaced bones before immobilization.
- Surgical Intervention: Internal fixation, such as using plates, screws, or rods, may be necessary for complex or unstable fractures.
- Pain Management: Analgesics are prescribed to control pain, while non-pharmacological methods may also be utilized.
- Rehabilitation: Physical therapy helps improve mobility and strength during the recovery phase.
Classification of Fractures
Complications associated with fractures may include:
- Delayed Union or Nonunion: Prolonged healing or failure of bone ends to heal together.
- Malunion: Healing with incorrect alignment, leading to functional impairment or deformity.
- Infection: Open fractures carry a risk of infection at the injury site.
- Compartment Syndrome: Swelling and increased pressure within the muscles or soft tissues surrounding the fracture site, potentially leading to nerve and blood vessel compression.
- Deep Vein Thrombosis (DVT) or Pulmonary Embolism (PE): Immobilization and reduced mobility increase the risk of blood clots.
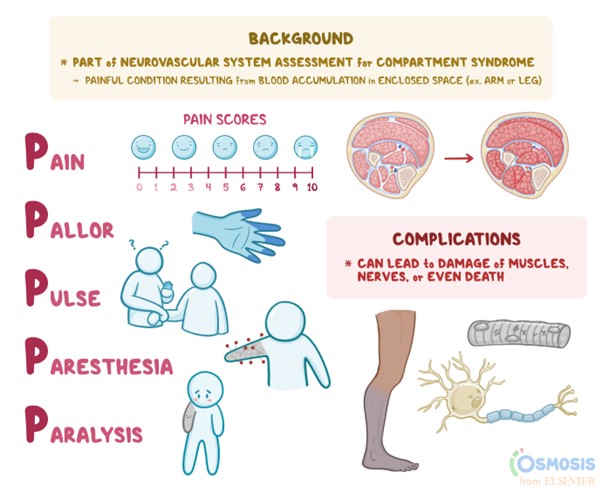
Patient Education
Patients with fractures require comprehensive education on:
- Home Care: Proper cast or brace care, keeping the limb elevated, and recognizing signs of complications.
- Mobility: Gradually resuming activity as directed by healthcare providers.
- Medication: Understanding pain management and any prescribed medications.
- Follow-Up Care: Scheduling and attending follow-up appointments to monitor healing progress.
Nursing Considerations
Nurses play a vital role in caring for patients with fractures by:
- Performing a thorough assessment and documenting findings accurately.
- Monitoring for signs of complications, such as neurovascular compromise or infection.
- Administering prescribed medications and pain management as needed.
- Assisting with reduction procedures and providing emotional support during the process.
- Educating patients and families about fracture care, follow-up appointments, and home care instructions.
Conclusion
Fractures are common injuries that result from various causes and can vary in severity and type.
Timely assessment, appropriate management, and patient education are essential in promoting optimal healing and restoring functionality.
Nurses play a crucial role in providing comprehensive care, monitoring for complications, and supporting patients and their families throughout the healing process.
Understanding the different types of fractures, their clinical manifestations, and the management approaches allows healthcare professionals to deliver high-quality care to patients with fractures and facilitate their recovery and rehabilitation.
Osteoarthritis
Objectives
- Understand the pathophysiology of osteoarthritis, including the breakdown of articular cartilage and joint space narrowing.
- Identify the risk factors for osteoarthritis, such as obesity, aging, joint injury, and genetic predisposition.
- Recognize the clinical manifestations of osteoarthritis, including joint pain, stiffness, and limited range of motion.
- Differentiate between osteoarthritis and other types of arthritis based on clinical presentation and diagnostic criteria.
- Describe the nursing management for patients with osteoarthritis, including pain management, exercise recommendations, and patient education on joint protection techniques.
- Discuss the pharmacological interventions commonly used for osteoarthritis, such as nonsteroidal anti-inflammatory drugs (NSAIDs) and acetaminophen.
- Understand the importance of interdisciplinary collaboration in managing osteoarthritis, involving physical therapists, occupational therapists, and rheumatologists.
- Evaluate the effectiveness of nursing interventions and medical treatments in improving the quality of life for patients with osteoarthritis.
- Educate patients and their families about lifestyle modifications, weight management, and self-care strategies to manage osteoarthritis symptoms.
- Identify potential complications of osteoarthritis and implement preventive measures to reduce their occurrence, such as falls and joint deformities
Introduction
Osteoarthritis (OA) is a chronic and degenerative joint disease that affects millions of people worldwide. It is the most common form of arthritis and primarily affects the joints, leading to pain, stiffness, and reduced joint function.
OA typically develops slowly over time, and its prevalence increases with age.
Understanding the pathophysiology, clinical manifestations, diagnosis, and management of OA is essential for healthcare professionals to provide comprehensive care to individuals affected by this condition.
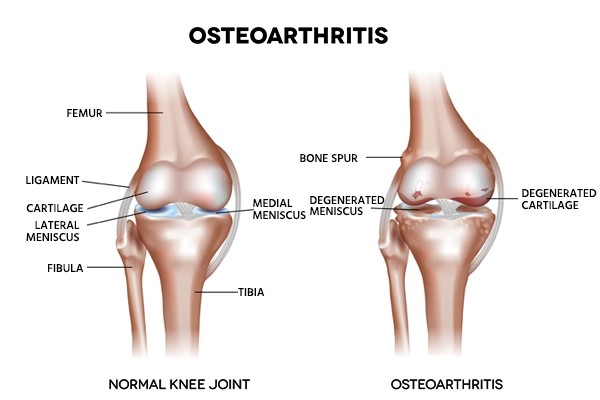
Pathophysiology
- OA is characterized by the gradual deterioration of joint cartilage, which serves as a cushion between bones, leading to joint space narrowing and increased friction between bones during movement.
- Over time, the repetitive mechanical stress on the joint can cause the cartilage to break down and wear away, resulting in the formation of bone spurs (osteophytes) at the joint edges.
- In response to cartilage damage, the synovial membrane that lines the joint capsule may become inflamed, further contributing to pain and swelling.
- As OA progresses, the joint may lose its ability to absorb shock, leading to increased pain, stiffness, and reduced joint flexibility and mobility.
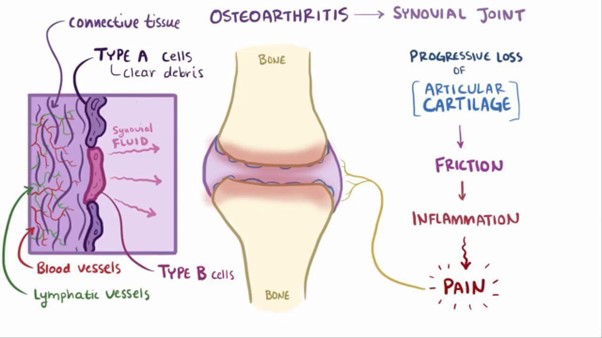
Risk Factors
Several factors increase the risk of developing OA, including:
- Age: The incidence of OA increases with advancing age, particularly in individuals over 65.
- Obesity: Excess body weight places additional stress on weight-bearing joints, such as the knees and hips.
- Joint Injury: Traumatic injuries or repetitive stress on joints, especially in physically demanding occupations or sports, can contribute to OA development.
- Genetics: Family history may play a role in the likelihood of developing OA.
- Joint Abnormalities: Congenital joint abnormalities or malalignment can lead to uneven pressure distribution on cartilage, accelerating its degeneration.
- Other Medical Conditions: Certain medical conditions, such as rheumatoid arthritis or metabolic disorders, can increase the risk of OA.

Clinical Manifestations
The clinical presentation of OA varies depending on the affected joints, but common signs and symptoms include:
- Joint Pain: Pain is the hallmark symptom of OA and is typically worse with movement or weight-bearing activities.
- Joint Stiffness: Stiffness and limited range of motion in the affected joint, particularly after periods of inactivity or rest.
- Joint Swelling: Inflammation may cause mild to moderate joint swelling.
- Crepitus: A crunching or cracking sensation during joint movement due to roughened joint surfaces rubbing against each other.
- Joint Instability: The affected joint may feel less stable and may give way or feel weak during movement.
- Functional Impairment: OA can limit daily activities, such as walking, climbing stairs, and grasping objects.

Diagnosis
Diagnosis of OA is primarily based on a combination of clinical assessment and imaging studies, including:
- Patient History: Evaluating the patient's symptoms, medical history, and risk factors.
- Physical Examination: Assessing joint tenderness, range of motion, stability, and signs of inflammation.
- X-rays: Imaging studies can reveal joint space narrowing, osteophyte formation, and other characteristic changes in affected joints.
- Joint Aspiration: In certain cases, joint fluid analysis may be performed to rule out other inflammatory joint conditions.
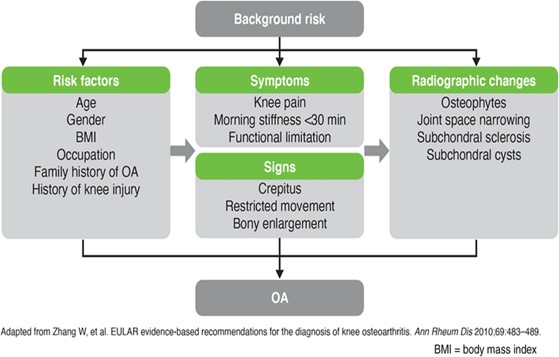
Management
The management of OA aims to relieve pain, improve joint function, and enhance the patient's quality of life. It includes:
- Non-Pharmacological Interventions: Weight management, physical therapy, and joint protection techniques can help reduce stress on affected joints.
- Pharmacological Therapies: Over-the-counter pain relievers (e.g., acetaminophen, nonsteroidal anti-inflammatory drugs) and topical agents (e.g., capsaicin) may be used to manage pain and inflammation.
- Intra-Articular Injections: Corticosteroids or hyaluronic acid injections may provide temporary relief for painful joints.
- Assistive Devices: The use of canes, walkers, or braces can help support and stabilize affected joints.
- Surgical Interventions: In severe cases, joint replacement surgery (e.g., hip or knee replacement) may be considered for pain relief and improved joint function.
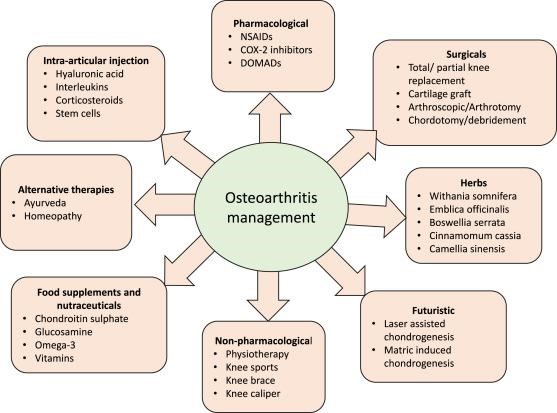
Patient Education
Educating patients with OA is crucial to help them manage their condition effectively, and key educational points include:
- Lifestyle Modifications: Encourage weight management, regular exercise, and joint-friendly activities to maintain joint health.
- Pain Management: Educate patients about the appropriate use of pain medications and non-pharmacological pain relief strategies.
- Joint Protection: Teach techniques for reducing stress on affected joints during daily activities.
- Disease Progression: Inform patients about the chronic nature of OA and the importance of regular follow-up with healthcare providers.
Nursing Considerations
Nurses play a vital role in caring for patients with OA by:
- Assessing pain levels and functional status regularly to monitor disease progression and treatment effectiveness.
- Administering prescribed medications and monitoring for potential side effects.
- Providing patient education on OA management, including lifestyle modifications and proper use of assistive devices.
- Collaborating with the interdisciplinary team, including physical therapists and occupational therapists, to optimize patient care.
Conclusion
Osteoarthritis is a prevalent chronic joint disease characterized by the degeneration of cartilage and subsequent joint changes, leading to pain, stiffness, and functional impairment.
Understanding the pathophysiology, risk factors, clinical manifestations, and management strategies of OA allows healthcare professionals to deliver comprehensive care to patients with this condition.
By providing appropriate education, promoting lifestyle modifications, and using a multidisciplinary approach, healthcare providers can help patients manage OA effectively and improve their overall quality of life.
Amputation
Objectives
- Identify the indications for amputation based on specific medical conditions and patient-related factors.
- Differentiate between the various types of amputations (e.g., above-the-knee, below-the-knee, upper extremity) and their implications for rehabilitation and mobility.
- Describe the pre-operative assessment and preparation for a patient undergoing amputation surgery.
- Analyze the psychosocial and cultural implications of amputation for the patient and their family and provide culturally competent care and support.
- Develop a comprehensive post-operative care plan for a patient who underwent amputation, including pain management, early mobilization, and prosthetic assessment and fitting.
Introduction
Amputation is a surgical procedure in which a part of or an entire limb or digit is removed from the body due to various medical conditions or traumatic injuries.
The decision to undergo amputation is carefully considered by the healthcare team and the patient, taking into account the potential benefits and risks associated with the procedure.
The primary goals of amputation are to improve the patient's overall health, functionality, and quality of life, either by removing a diseased or damaged limb or by preventing the spread of infection or injury to other parts of the body.
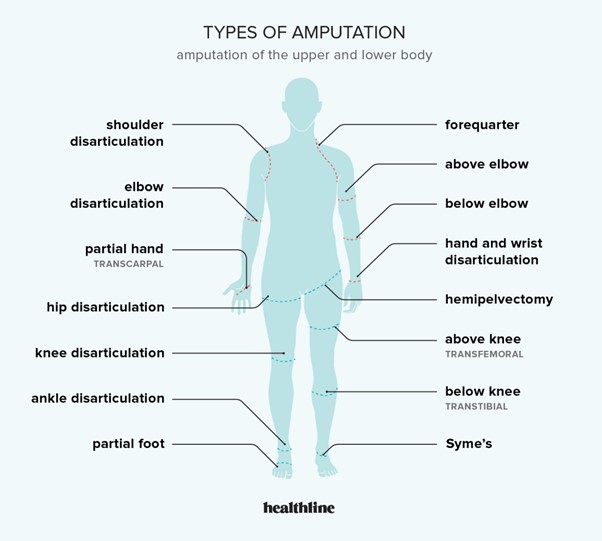
Indications for Amputation
The decision for amputation is based on the patient's specific medical condition and the extent of limb damage or disease. Some common indications include:
- Peripheral Vascular Disease: Severe peripheral arterial disease or ischemia that compromises blood flow to the extremities, leading to tissue necrosis and non-healing wounds.
- Traumatic Injuries: Irreparable injuries resulting from severe crush injuries, burns, or extensive soft tissue damage, where limb salvage is not feasible.
- Cancer: Advanced malignancies in bones or soft tissues that cannot be adequately managed by other treatment modalities, such as surgery, chemotherapy, or radiation therapy.
- Infections: Untreatable or life-threatening infections, such as gangrene or necrotizing fasciitis, that necessitate the removal of affected limbs to prevent further spread.
- Congenital Conditions: Certain congenital anomalies or malformations may require surgical amputation for functional and cosmetic reasons.
- Peripheral Neuropathy: Neuropathic complications related to conditions like diabetes, leading to chronic non-healing foot ulcers or infections.
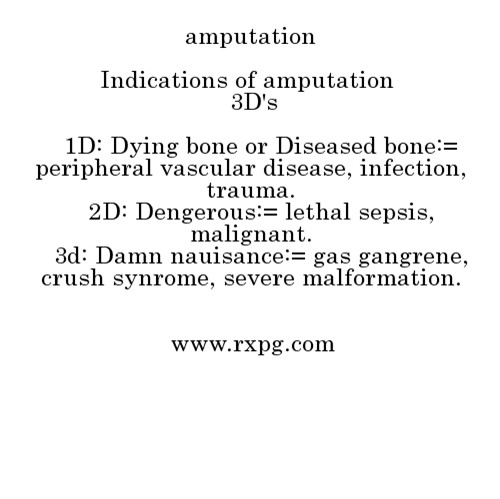
Preoperative Considerations
Prior to amputation, a comprehensive evaluation is performed, including:
- Medical History: Assessing the patient's medical history, including the underlying condition requiring amputation and any relevant comorbidities.
- Diagnostic Tests: Conducting imaging studies and vascular assessments to determine the extent of limb damage and perfusion status.
- Psychological Evaluation: Addressing the patient's emotional well-being and coping mechanisms to prepare them for the physical and psychological impact of amputation.
- Consent: Obtaining informed consent from the patient or their legal representative after discussing the procedure, potential risks, and expected outcomes.
Surgical Procedure
The surgical amputation is performed by an experienced surgical team, and the procedure involves:
- Anesthesia: Administering general or regional anesthesia to ensure the patient's comfort and prevent pain during the operation.
- Tissue Removal: Skillfully removing the affected limb or digit through a precise incision, taking care to preserve as much healthy tissue as possible.
- Hemostasis: Ensuring proper hemostasis to prevent excessive bleeding during the procedure.
- Closure: Closing the wound using sutures or staples, and dressing the surgical site appropriately to promote healing.
Postoperative Care
Following amputation, the patient's postoperative care includes:
- Wound Care: Meticulous wound care and monitoring for signs of infection or wound healing complications.
- Pain Management: Administering pain medications and providing non-pharmacological pain relief techniques to manage postoperative pain effectively.
- Early Mobilization: Encouraging early mobilization and physical therapy to prevent complications such as joint contractures and promote functional independence.
- Psychological Support: Offering emotional support and counseling to help the patient adjust to their new physical state and cope with body image issues.
- Prosthetic Evaluation: Assessing the patient's suitability for prosthetic devices and providing education and training on their use, when applicable.
- Rehabilitation: Collaborating with physical and occupational therapists to develop a rehabilitation plan that focuses on achieving functional goals and maximizing independence.
- Patient Education: Providing comprehensive patient education on post-amputation care, including self-care techniques, wound management, and lifestyle adjustments.
Complications and Follow-Up
Despite appropriate care, amputation can be associated with potential complications, such as infection, delayed wound healing, phantom limb sensation, and psychosocial issues.
Regular follow-up appointments are essential to monitor wound healing, address complications promptly, and provide ongoing support to the patient during their recovery and rehabilitation journey.
Conclusion
In conclusion, amputation is a surgical procedure undertaken for various medical conditions or traumatic injuries that necessitate the removal of all or part of a limb or digit. Preoperative evaluations, meticulous surgical techniques, and comprehensive postoperative care are critical to achieving successful outcomes and facilitating the patient's adaptation to their new physical state. By providing holistic care, addressing physical and emotional needs, and fostering rehabilitation, healthcare professionals can empower patients to optimize their functional abilities and overall quality of life post-amputation.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Musculoskeletal System
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now