Please set your exam date
Emergency Nursing Principles and Management
Study Questions
Practice Exericise 1
In a mass casualty incident (MCI), what are the primary goals of the triage process? Select all that apply
Explanation
In a mass casualty incident (MCI), the primary goals of triage are to allocate limited resources in a way that achieves the greatest good for the greatest number of people and to prioritize patients based on injury severity and likelihood of survival. Triage in an MCI is focused on rapid assessment to determine treatment priority rather than providing detailed diagnoses or definitive care at the scene.
Rationale for correct answers:
B. To allocate resources to do the greatest good for the greatest number of people: MCI triage balances resource limitations with the need to maximize overall survival.
D. To prioritize patients based on the severity of their injuries and their likelihood of survival: Patients most likely to survive with timely intervention are prioritized for care and transport.
Rationale for incorrect answers:
A. To identify all injuries for every patient: Detailed assessment is not the goal during initial MCI triage; rapid categorization is key.
B. To provide definitive care to the most critically ill first: In an MCI, patients with minimal survival chances may be assigned lower priority to conserve resources for those who can benefit most.
E. To transport all patients to the nearest hospital immediately: This can overwhelm facilities; transport is prioritized based on triage category and hospital capacity.
Take home points
- MCI triage aims for the greatest overall survival, not just saving the sickest individual.
- Rapid assessment and prioritization guide resource allocation and transport.
- Definitive care is typically deferred until patients reach an appropriate facility.
A trauma patient arrives at the emergency department. After ensuring a patent airway with cervical spine stabilization, the next step in the primary survey is to assess the patient's:
Explanation
After ensuring a patent airway with cervical spine stabilization, the next step in the primary survey is to assess breathing and ventilation. This involves checking for adequate chest rise, respiratory rate, oxygen saturation, and the presence of any injuries that could impair ventilation, such as pneumothorax or flail chest. Immediate interventions may be required to restore adequate oxygenation.
Rationale for correct answer:
B. Breathing and ventilation: In the ABCDE approach to trauma assessment, breathing follows airway management, ensuring oxygen delivery to the body once the airway is secure.
Rationale for incorrect answers:
A. Mental status and neurological function: This is evaluated later under "D" (Disability) in the primary survey.
B. Circulation, hemorrhage, and pulse: This comes after breathing assessment under "C" in the primary survey.
D. Full set of vital signs: Obtained after the primary survey is complete and life-threatening issues have been addressed.
Take home points
- The trauma primary survey follows the sequence: Airway, Breathing, Circulation, Disability, Exposure (ABCDE).
- Breathing assessment ensures oxygen is reaching the bloodstream after airway stabilization.
- Immediate, life-threatening issues are addressed before moving to the next step in the survey.
During a mass casualty incident, a triage nurse assesses a patient who is awake and able to walk. The patient has a laceration on their arm but no other apparent life-threatening injuries. According to the START triage system, what color tag should be assigned to this patient?
Explanation
In the START (Simple Triage and Rapid Treatment) triage system, a patient who is awake, able to walk, and has no life-threatening injuries is assigned a green tag, indicating the "minor" category. These patients can ambulate to a designated safe area and can wait for medical treatment until more urgent cases are addressed.
Rationale for correct answer:
B. Green: Represents minor injuries that are not life-threatening. Patients in this category are stable and can tolerate delayed treatment without risk of deterioration.
Rationale for incorrect answers:
A. Red: Indicates immediate care is needed for life-threatening conditions that are potentially reversible with prompt intervention.
B. Yellow: Indicates delayed treatment for serious but not immediately life-threatening injuries; patients are stable for now but require hospital care.
D. Black: Indicates the patient is deceased or injuries are incompatible with survival.
Take home points
- START triage quickly categorizes patients to maximize resource use in MCIs.
- Green-tagged patients can self-evacuate to a holding area for later evaluation.
- Immediate resources should be focused on red- and yellow-tagged patients.
Select all the components that are typically included in a secondary survey of a trauma patient. Select all that apply
Explanation
The secondary survey in trauma care is a comprehensive, head-to-toe assessment performed after life-threatening conditions have been identified and treated in the primary survey. It includes a full physical examination, obtaining a detailed patient history using the AMPLE mnemonic, and performing diagnostic studies such as X-rays, CT scans, and lab work to identify additional injuries.
Rationale for correct answers:
B. A head-to-toe physical examination: Ensures detection of injuries not apparent during the rapid primary survey.
B. A detailed patient history, including AMPLE: Provides critical background for diagnosis, treatment, and surgical planning.
E. Diagnostic studies such as X-rays and CT scans: Help confirm suspected injuries and guide further interventions.
Rationale for incorrect answers:
A. A focused assessment on the most obvious injury: This is more relevant to the primary survey when addressing immediate threats, not the full systematic secondary survey.
D. Insertion of a definitive airway, if needed: This is part of the primary survey under "A" (Airway), not the secondary survey.
Take home points
- Secondary survey occurs only after life-threatening issues are addressed.
- It involves a systematic exam, detailed history, and targeted diagnostics.
- The goal is to identify all injuries, not just the most obvious ones.
What is the fundamental difference in the purpose between a primary survey and a secondary survey?
Explanation
The fundamental difference between the primary and secondary survey is that the primary survey is a rapid, systematic assessment aimed at identifying and managing life-threatening conditions immediately, while the secondary survey is a thorough, head-to-toe evaluation to detect all other injuries or issues once the patient is stabilized.
Rationale for correct answer:
B. The primary survey is a rapid assessment to identify and manage life-threatening conditions, while the secondary survey is a more thorough head-to-toe evaluation: This distinction ensures critical issues are addressed first before moving on to less urgent findings.
Rationale for incorrect answers:
A. The primary survey is performed by paramedics, while the secondary survey is performed by physicians: Both can be performed by any trained healthcare provider; it is about purpose, not provider.
B. The primary survey is only for conscious patients, whereas the secondary survey is for unconscious patients: Both assessments apply to all patients, regardless of consciousness level.
D. The primary survey is completed in the field, and the secondary survey is completed at the hospital: Location does not define the surveys; they can occur in any setting where trauma care is provided.
Take home points
- Primary survey = rapid, life-saving assessment (ABCDE).
- Secondary survey = comprehensive exam after stabilization.
- This sequence prioritizes survival before full diagnostic evaluation.
Practice Exercise 2
A patient is experiencing crushing chest pain that radiates to their left arm and jaw. The EKG shows ST-segment elevation. Which of the following is the most likely diagnosis?
Explanation
Crushing chest pain radiating to the left arm and jaw, combined with ST-segment elevation on EKG, is most indicative of an acute myocardial infarction (STEMI). This condition results from complete occlusion of a coronary artery, leading to myocardial ischemia and injury. Immediate reperfusion therapy is critical to minimize heart muscle damage.
Rationale for correct answer:
C. Acute myocardial infarction (STEMI): Classic presentation includes severe, persistent chest pain, radiation to the arm or jaw, and ST-segment elevation on EKG, indicating full-thickness myocardial injury.
Rationale for incorrect answers:
A. Pericarditis: Can cause chest pain and diffuse ST elevation, but the pain is usually sharp, pleuritic, and relieved by sitting forward, not crushing or radiating to the arm/jaw.
B. Aortic dissection: Causes sudden, tearing chest or back pain, often with pulse differences between limbs, not ST elevation from coronary occlusion.
D. Unstable angina: Presents with similar chest pain, but EKG changes do not show persistent ST elevation, and there is no complete coronary occlusion.
Take home points
- STEMI is characterized by chest pain, ST elevation, and requires immediate reperfusion.
- Prompt recognition and treatment reduce mortality and preserve cardiac function.
- Differentiating from other chest pain causes is critical for rapid intervention.
A nurse is assessing a patient with a suspected cardiac emergency. Which of the following are classic signs and symptoms of a myocardial infarction? Select all that apply
Explanation
Classic signs and symptoms of a myocardial infarction (MI) include cool, clammy skin due to sympathetic activation, shortness of breath from impaired cardiac output, palpitations from arrhythmias, and nausea/vomiting from vagal stimulation. MI pain is typically described as pressure, heaviness, or squeezing not sharp, stabbing pain that worsens with deep breathing.
Rationale for correct answers:
B. Cool, clammy skin: Caused by vasoconstriction and activation of the sympathetic nervous system.
C. Shortness of breath (dyspnea): Results from reduced cardiac output and possible pulmonary congestion.
D. Palpitations: May occur from arrhythmias triggered by ischemia.
E. Nausea and vomiting: Often due to vagal stimulation or inferior wall MI.
Rationale for incorrect answer:
A. Sudden, sharp, stabbing pain that worsens with deep breath: This type of pain is usually pleuritic or musculoskeletal, not typical of MI.
Take home points
- MI symptoms can include autonomic, respiratory, and gastrointestinal manifestations.
- Not all chest pain is cardiac—pain description and associated symptoms are key for differentiation.
- Early recognition and treatment improve survival and outcomes in MI patients.
A patient in the emergency department suddenly becomes unresponsive, apneic, and pulseless. A nurse should immediately initiate which of the following interventions?
Explanation
The immediate priority for a patient who is unresponsive, apneic, and pulseless is to begin high-quality chest compressions and call for the defibrillator, following the Basic Life Support (BLS) algorithm. This ensures circulation of oxygenated blood to vital organs and early defibrillation if a shockable rhythm is present.
Rationale for correct answer:
B. Beginning chest compressions and calling for the defibrillator: Early CPR and rapid defibrillation are the most critical interventions for cardiac arrest, significantly improving survival rates.
Rationale for incorrect answers:
A. Administering a bolus of intravenous fluids: Fluids may be helpful later depending on the cause, but circulation must be initiated first.
C. Obtaining a 12-lead EKG: This is performed after return of spontaneous circulation (ROSC), not during active arrest.
D. Preparing for endotracheal intubation: Airway management is important but should not delay initiation of chest compressions.
Take home points
- In cardiac arrest: Circulation → Airway → Breathing (CAB sequence) is the priority.
- High-quality CPR with minimal interruptions is essential.
- Early defibrillation for shockable rhythms greatly increases survival chances.
Which of the following are considered modifiable risk factors for coronary artery disease (CAD)? Select all that apply
Explanation
Modifiable risk factors are those that can be changed or controlled through lifestyle changes, medications, or both. Hypertension, hyperlipidemia, and smoking are major modifiable risk factors for coronary artery disease.
Rationale for correct answers:
C. Hypertension: Can be managed with medications, diet, exercise, and stress reduction.
D. Hyperlipidemia: Can be controlled with diet, exercise, and lipid-lowering drugs.
E. Smoking: Stopping smoking greatly reduces CAD risk.
Rationale for incorrect answers:
A. Family history of CAD: Non-modifiable; genetic predisposition cannot be changed.
B. Male gender: Non-modifiable; although men are at higher risk, gender itself cannot be altered as a risk factor.
Take home points
- Modifiable risk factors include hypertension, hyperlipidemia, smoking, diabetes, obesity, sedentary lifestyle, and poor diet.
- Non-modifiable risk factors include age, gender, and family history.
A patient presents with a rapid, irregular heart rate. The EKG shows no discernable P waves and a chaotic baseline with a variable ventricular response. This is a classic finding for which type of arrhythmia?
Explanation
Atrial fibrillation is characterized by the absence of distinct P waves, a chaotic (fibrillatory) baseline, and an irregularly irregular ventricular response on EKG.
Rationale for correct answer:
A. Atrial fibrillation: Results from disorganized atrial electrical activity, leading to fibrillatory waves instead of normal P waves, and an unpredictable ventricular rhythm.
Rationale for incorrect answers:
B. Ventricular tachycardia: Shows wide QRS complexes and a regular rhythm, often without visible P waves.
C. Supraventricular tachycardia: Usually presents with a rapid, regular rhythm, often with narrow QRS complexes, and sometimes hidden P waves.
D. Sinus tachycardia: Has a regular rhythm with identifiable P waves before each QRS complex.
Take home points
- AFib increases the risk of stroke due to atrial thrombus formation.
- Control of rate, rhythm, and anticoagulation are central to management.
Practice Exercise 3
A. Immediately following the return of spontaneous circulation (ROSC) in a patient, which of the following are primary goals of post-resuscitation care? Select all that apply
Explanation
After ROSC, the main objectives are to stabilize the patient, protect vital organs, and prevent recurrence of cardiac arrest. This includes maintaining adequate oxygenation and ventilation, identifying and correcting the cause of arrest, and evaluating neurological function to guide prognosis and further care. Hypotension should be avoided, and targeted temperature management is only indicated for specific patients.
Rationale for correct answers:
A. Optimizing ventilation and oxygenation: Adequate oxygen delivery is critical to prevent secondary brain injury and organ dysfunction after cardiac arrest. Oxygen saturation should be kept between 94–99% to avoid both hypoxia and hyperoxia, which can be harmful.
B. Identifying and treating the underlying cause of the cardiac arrest: Addressing reversible causes such as myocardial infarction, electrolyte imbalances, or pulmonary embolism prevents recurrence. This step is essential for long-term survival and improved patient outcomes.
E. Performing a detailed neurological assessment: Neurological status provides important information about the extent of brain recovery and guides further interventions. This includes assessing consciousness, pupil reaction, and motor responses.
Rationale for incorrect answers:
C. Maintaining a systolic blood pressure below 90 mmHg to prevent organ damage: Hypotension reduces perfusion to the brain and heart, worsening post-arrest injury. The target is to maintain systolic BP ≥ 90 mmHg or MAP ≥ 65 mmHg to support organ function.
D. Inducing therapeutic hypothermia in all patients: Targeted temperature management is not appropriate for every post-ROSC patient; it is mainly used in comatose patients to reduce neurological injury. Awake, responsive patients generally do not require this intervention.
Take home points:
- Post-ROSC care focuses on stabilizing airway, breathing, and circulation while preventing further injury.
- Identifying and correcting the cause of arrest is key to preventing recurrence.
- Avoid hypotension and hyperoxia to improve outcomes after cardiac arrest.
What is the primary benefit of targeted temperature management in post-resuscitation care for comatose patients?
Explanation
Targeted temperature management (TTM) is used after ROSC in comatose patients to improve neurological outcomes. By lowering body temperature to a controlled range (typically 32–36°C), TTM slows metabolic processes in the brain, reducing ischemia-reperfusion injury and limiting secondary brain damage.
Rationale for correct answer:
B. It reduces cerebral metabolic rate and protects the brain from ischemic injury: Cooling slows neuronal metabolism, decreases oxygen demand, and reduces the cascade of chemical reactions that lead to further brain cell death after ischemia. This improves the likelihood of better neurological recovery.
Rationale for incorrect answers:
A. It prevents a secondary cardiac arrest: While TTM may stabilize some physiological processes, its primary purpose is neuroprotection, not direct prevention of another arrest.
C. It improves a patient's renal function: TTM does not directly improve kidney function; post-arrest renal issues are managed with supportive care and treatment of underlying causes.
D. It is a definitive treatment for the underlying cause of the arrest: TTM does not treat the cause of arrest; it is an adjunctive therapy alongside investigations and interventions to correct the cause.
Take home points:
- TTM is indicated for comatose patients after ROSC to protect brain function.
- The target temperature is typically maintained for 24 hours before controlled rewarming.
- TTM does not replace the need to identify and treat the underlying cause of cardiac arrest.
Which of the following are key components of hemodynamic support in the post-resuscitation period? Select all that apply
Explanation
Hemodynamic support after ROSC focuses on optimizing tissue perfusion and preventing secondary organ injury. Maintaining an adequate MAP (usually ≥65 mmHg) helps ensure cerebral and systemic perfusion, while close monitoring can detect complications such as cardiogenic shock or ischemia early. Continuous cardiac monitoring via EKG is essential for detecting arrhythmias and myocardial injury that are common after cardiac arrest.
Rationale for correct answers:
A. Titrating vasopressors to maintain a MAP greater than 65 mmHg: Adequate blood pressure supports oxygen delivery to vital organs, particularly the brain and heart. Vasopressors like norepinephrine are adjusted to meet individual patient needs.
C. Monitoring for signs of cardiogenic shock: Cardiac arrest survivors are at high risk for pump failure, so early identification of hypotension, low urine output, or poor perfusion is critical for timely intervention.
D. Using an EKG to monitor for myocardial ischemia and arrhythmias: Continuous monitoring helps detect rhythm disturbances or ischemic changes, guiding both acute management and prevention of re-arrest.
Rationale for incorrect answers:
B. Administering a large bolus of IV fluids to all patients: Fluid therapy should be individualized; excessive fluids can worsen outcomes, especially in patients with poor cardiac function.
E. Avoiding the use of inotropes to prevent an increase in myocardial oxygen demand: Inotropes may be necessary in cases of low cardiac output despite adequate preload and afterload; their use is guided by patient status, not avoided outright.
Take home points:
- Maintain MAP ≥65 mmHg using fluids and vasopressors as indicated.
- Monitor closely for shock, ischemia, and arrhythmias in the post-ROSC period.
- Fluid resuscitation and inotrope use should be individualized to prevent harm.
A nurse is performing a neurological assessment on a patient who remains unresponsive after ROSC. The nurse notes the absence of the gag reflex, and the pupils are fixed and dilated. These findings indicate:
Explanation
Fixed and dilated pupils along with the absence of the gag reflex in an unresponsive patient after ROSC are classic signs of severe neurological damage, most commonly due to prolonged cerebral hypoxia. These findings indicate that critical brainstem reflexes are absent, suggesting poor neurological prognosis.
Rationale for correct answer:
C. Significant anoxic brain injury has occurred: After cardiac arrest, prolonged lack of oxygen can cause widespread neuronal death, particularly affecting brainstem reflexes. Fixed, dilated pupils and absent gag reflex indicate severe brain injury, which often has a poor recovery outcome.
Rationale for incorrect answers:
A. The patient is likely to have a full neurological recovery: The absence of key brainstem reflexes strongly predicts poor neurological outcome, not recovery.
B. The patient is likely suffering from a mild concussion: A concussion does not cause fixed, dilated pupils or absent brainstem reflexes; these are signs of severe injury.
D. The patient is responding normally to sedation: Sedation may depress some reflexes, but fixed and dilated pupils with absent gag reflex generally indicate structural brain injury rather than drug effects, especially if sedation has worn off.
Take home points:
- Fixed, dilated pupils and absent gag reflex suggest severe brainstem damage.
- Anoxic brain injury is a major complication after cardiac arrest.
- Neurological assessment post-ROSC is essential for prognosis and care planning.
When managing ventilation for a post-resuscitation patient, what is the recommended target for a partial pressure of carbon dioxide (PCO2)?
Explanation
Maintaining normocarbia is essential in post-resuscitation care to prevent secondary brain injury. Both hypocarbia and hypercarbia can adversely affect cerebral blood flow, potentially worsening neurological outcomes.
Rationale for correct answer:
C. Maintaining normocarbia (PCO₂ between 35–45 mmHg) to avoid cerebral ischemia or edema: Normocarbia supports stable cerebral perfusion without causing excessive vasoconstriction or vasodilation. Tight control of ventilation helps protect the brain after ROSC.
Rationale for incorrect answers:
A. Hypocarbia (PCO₂ less than 35 mmHg) to cause cerebral vasoconstriction: While hypocarbia does cause vasoconstriction, it reduces cerebral blood flow and can worsen ischemia.
B. Hypercarbia (PCO₂ greater than 45 mmHg) to cause cerebral vasodilation: Hypercarbia increases intracranial pressure due to vasodilation, which can exacerbate cerebral edema.
D. There is no specific target for PCO₂ as it does not affect cerebral blood flow: This is incorrect because PCO₂ directly influences cerebral vessel diameter and blood flow.
Take home points:
- Aim for PCO₂ between 35–45 mmHg post-ROSC.
- Avoid both hypo- and hypercarbia to protect the brain.
- Ventilation management is a key part of post-resuscitation neuroprotection.
Comprehensive Questions
A nurse on a medical-surgical unit is caring for a group of clients. The nurse should notify the rapid response team for which of the following clients?
Explanation
The combination of right calf pain and shortness of breath raises concern for a deep vein thrombosis (DVT) that may have progressed to a pulmonary embolism (PE), a life-threatening emergency requiring immediate intervention. This scenario warrants activation of the rapid response team due to the risk of impaired gas exchange and sudden cardiac or respiratory decompensation.
Rationale for Correct Answer:
B. Calf pain suggests possible DVT, and shortness of breath indicates potential embolization to the lungs. A PE can cause hypoxia, hypotension, and cardiac arrest. Rapid recognition and escalation of care are critical to prevent deterioration.
Rationale for Incorrect Answers:
A. A blood glucose level of 300 mg/dL in a client with a heel ulcer is concerning but not immediately life-threatening. It requires medical management, not emergency intervention.
C. Blood on a pressure dressing after cardiac catheterization suggests oozing or minor bleeding, but unless it’s active, pulsatile, or expanding, it does not yet meet criteria for a rapid response call.
D. Dark red toes and absent pedal pulse indicate possible critical limb ischemia but do not immediately threaten life. This requires urgent vascular evaluation, but not a rapid response unless systemic compromise occurs.
Key Takeaways:
• Sudden shortness of breath with DVT signs suggests a possible PE—this is a medical emergency.
• The rapid response team should be called for any signs of acute respiratory, cardiovascular, or neurological compromise.
• Other findings may require urgent or routine care but are not rapid response triggers without evidence of systemic instability.
A nurse is caring for a client who has ingested a toxic agent. Which of the following actions should the nurse plan to take? Select all that apply
Explanation
Management of toxic ingestion focuses on limiting absorption, enhancing elimination, and administering antidotes when available. The most appropriate interventions include activated charcoal, gastric lavage, and whole-bowel irrigation, depending on the substance, time since ingestion, and client condition.
Rationale for Correct Answers:
B. Instill activated charcoal: Effective in binding many toxic substances in the GI tract if administered within 1–2 hours of ingestion. It prevents systemic absorption.
C. Perform a gastric lavage with aspiration: May be considered if the ingestion is life-threatening and occurred within 1 hour. This procedure removes stomach contents before the toxin is absorbed.
E. Complete a whole-bowel irrigation: Used for sustained-release or enteric-coated drugs, or substances not adsorbed by charcoal (e.g., iron, lithium). It clears the entire GI tract using polyethylene glycol.
Rationale for Incorrect Answers:
A. Induce vomiting: No longer recommended due to risk of aspiration, especially in clients with altered consciousness or caustic ingestion.
D. Administer syrup of ipecac: Outdated and no longer used; it induces vomiting and can cause delays in definitive treatment or worsen outcomes.
Key Takeaways:
• Activated charcoal, gastric lavage, and whole-bowel irrigation are valid interventions depending on timing and substance.
• Induced vomiting and ipecac syrup are no longer recommended due to safety concerns.
• Always consider the type of toxin, time since ingestion, and client’s airway protection status when planning interventions.
A nurse in the emergency department is caring for a client who fell through the ice on a pond and is unresponsive and breathing slowly. Which of the following are appropriate actions by the nurse? Select all that apply
Explanation
This client is experiencing hypothermia due to prolonged cold-water exposure. Rewarming is essential to prevent further deterioration and complications such as bradycardia, arrhythmias, and decreased perfusion.
Rationale for Correct Answers:
A. Remove wet clothing: Wet garments accelerate heat loss through conduction and evaporation; removing them is essential to initiate rewarming.
C. Apply warm blankets: A standard passive external rewarming method that helps raise core temperature gradually and safely.
D. Apply a heat lamp: Provides external heat and assists in surface rewarming, especially in a controlled setting like the ED.
E. Infuse warmed IV fluids: Active internal rewarming that helps raise core body temperature and supports circulation.
Rationale for Incorrect Answer:
B. Maintain normal room temperature: Hypothermic clients need an elevated ambient temperature to assist rewarming. Keeping the room at normal temperature is inadequate and may hinder rewarming efforts.
Key Takeaways:
• Hypothermia management includes both external and internal rewarming techniques.
• Removing wet clothing is a critical first step.
• Warm blankets, heat lamps, and warmed IV fluids are all appropriate rewarming measures.
• The environment should be adjusted to support rewarming—normal room temperature is insufficient.
A nurse in the emergency department is assessing a client who is unresponsive. The client’s partner states, “He was pulling weeds in the yard and dropped to the ground.” Which of the following techniques should the nurse use to open the client’s airway?
Explanation
In an emergency setting where a client is unresponsive and the cause is unknown—such as sudden collapse during physical activity, cervical spine injury must be assumed until ruled out. The modified jaw thrust technique is the safest method to open the airway without compromising spinal alignment.
Rationale for Correct Answer:
A. Head-tilt, chin-lift: The nurse should open the client’s airway by the head-tilt, chin-lift because the client is
unresponsive without suspicion of trauma.
Rationale for Incorrect Answers:
B. Modified jaw thrust: This technique opens the airway by displacing the jaw forward without moving the neck and is for patients suspected to have cervical spine injury.
C. Hyperextension of the head: This position may further injure the cervical spine and does not follow trauma airway protocol.
D. Flexion of the head: This worsens airway obstruction by pushing the chin toward the chest and narrows the upper airway, making it inappropriate in any airway emergency.
Key Takeaways:
• Use the modified jaw thrust to open the airway in unresponsive clients with potential trauma.
• Spinal precautions are essential until injury is ruled out.
• Avoid techniques like head-tilt, hyperextension, or flexion if there is any suspicion of cervical injury.
A nurse is reviewing the common emergency management protocol for clients during a cardiac emergency. Which of the following is an appropriate action by the nurse?
Explanation
During a cardiac emergency, such as cardiac arrest or severe bradycardia with hemodynamic compromise, epinephrine is the first-line medication used in Advanced Cardiac Life Support (ACLS) protocols. It increases coronary and cerebral perfusion through vasoconstriction and enhances myocardial contractility.
Rationale for Correct Answer:
C. Administer IV epinephrine (Adrenaline): Epinephrine is a primary drug in cardiac arrest algorithms, including for asystole, pulseless electrical activity (PEA), ventricular fibrillation (VF), and pulseless ventricular tachycardia (VT). It promotes vasoconstriction and increases perfusion to vital organs during CPR.
Rationale for Incorrect Answers:
A. Dobutamine: Used in heart failure and cardiogenic shock to improve myocardial contractility, but not for cardiac arrest situations.
B. Dopamine: Used for symptomatic bradycardia or shock unresponsive to fluids, but not the first choice during active cardiac arrest.
D. Atropine: Used specifically for symptomatic bradycardia, not for pulseless rhythms or full cardiac arrest.
Key Takeaways:
• IV epinephrine is the drug of choice during cardiac arrest situations.
• Other medications like dobutamine, dopamine, and atropine have roles in specific cardiac conditions but not in initial emergency resuscitation.
• Familiarity with ACLS protocols ensures timely and effective interventions in cardiac emergencies.
An older client arrives in triage disoriented and tachypneic. His skin is hot and dry. His wife states that he was fine earlier today. The nurse’s next priority would be to:
Explanation
The client is showing signs of possible heat stroke, a life-threatening emergency in older adults. The priority is to obtain vital signs, especially a core temperature, which is best measured rectally to assess for hyperthermia. This guides immediate interventions.
Rationale for Correct Answer:
B. Assess his vital signs, including a rectal temperature: Disorientation, tachypnea, and hot, dry skin are hallmark signs of classic heat stroke. Core temperature measurement is essential for diagnosis and management. Prompt evaluation of vitals helps guide emergency treatment.
Rationale for Incorrect Answers:
A. Obtain a detailed medical history: While important, this is not the immediate priority when the client shows signs of acute physiological compromise.
C. Determine the kind of insurance: Administrative concerns do not take precedence over emergency care. Treatment should never be delayed for financial or coverage issues.
D. Start supplemental oxygen and have the ED physician see him: While oxygen may be supportive, initiating care without first assessing vitals and core temperature misses the most critical diagnostic step in this situation.
Key Takeaways:
• Disorientation, hot dry skin, and tachypnea in an older adult suggest heat stroke, requiring immediate action.
• Core temperature (via rectal route) is the most reliable method for identifying hyperthermia.
• In emergencies, vital signs assessment precedes other interventions to guide life-saving treatment.
The first responders at a chemical explosion report that victims are being decontaminated at the scene and approximately 125 workers will need medical evaluation and care. The nurse receiving this report should know that this will first require activation of:
Explanation
A mass casualty incident, such as a chemical explosion involving a large number of victims, requires immediate implementation of the hospital’s emergency response plan to coordinate triage, staffing, communication, and resource management.
Rationale for Correct Answer:
D. The hospital’s emergency response plan: This is the comprehensive, pre-established protocol that guides hospitals during large-scale emergencies. It ensures proper mobilization of staff, equipment, decontamination procedures, and coordination with external agencies. Activation is essential to manage an influx of 125 victims safely and effectively.
Rationale for Incorrect Answers:
- Code blue alert: This is used for individual in-hospital cardiopulmonary arrests, not for external mass casualty situations.
- Disaster medical assistance team (DMAT): While helpful, DMATs are federal response teams and require time to deploy. The hospital must first activate its internal response.
- Local police and fire departments: These agencies are likely already involved at the scene and do not control hospital-based response operations.
Key Takeaways:
• Hospital emergency response plans are essential during mass casualty incidents.
• Early activation ensures coordinated triage, care, and communication.
• Internal response is the first step before relying on external disaster teams or agencies.
A nurse is teaching a group of students about activities during the secondary survey of a trauma patient in the ED. Why is it important that the nurse obtain details of the incident?
Explanation
In trauma care, understanding the mechanism of injury (MOI) is essential because it helps the healthcare team anticipate specific types of injuries that may not be immediately visible during the primary assessment. This information is critical during the secondary survey, where a more detailed head-to-toe examination is conducted.
Rationale for Correct Answer:
- The mechanism of injury can indicate specific injuries: Knowing how the injury occurred (e.g., fall from height, high-speed collision, blunt trauma) allows the nurse and trauma team to predict internal or occult injuries, prioritize diagnostics, and initiate appropriate interventions early.
Rationale for Incorrect Answers:
B. Important facts may be forgotten when needed later for legal actions: While legal documentation is important, the priority in a secondary survey is clinical decision-making based on the patient’s condition, not legal preparation.
C. Alcohol use associated with many accidents can affect treatment of injuries: Though true, alcohol screening is part of routine trauma assessment and labs, but it is not the primary reason for asking about the incident itself.
D. Many types of accidents or trauma must be reported to government agencies: This is a regulatory requirement, not a priority during clinical assessment in the secondary survey phase.
Key Takeaways:
• Understanding the mechanism of injury is central to anticipating trauma-related complications.
• The secondary survey builds on this information to guide diagnostic and therapeutic decisions.
• While legal and regulatory concerns are relevant, clinical priorities come first in emergency trauma care.
A nurse is reviewing an emergency client’s health history, what information is obtained with the use of the mnemonic AMPLE?
Explanation
The AMPLE mnemonic is a standardized tool used during the secondary survey in emergency care to gather a focused and essential health history. It helps clinicians obtain key background information that can influence diagnosis, treatment, and safety.
Rationale for Correct Answer:
C. Allergies, medications, past health history, last meal, and events/environment leading to the illness or injury: This is the correct breakdown of the AMPLE mnemonic. It ensures the nurse collects critical information quickly to support safe and efficient emergency care.
Rationale for Incorrect Answers:
A. Anatomy of injuries, mucous membranes, peripheral edema, leukocytosis, eczema location: This is not a standard or clinically useful framework for trauma assessment.
B. Approximate weight, motor function, palpable swelling, labored breathing, edema severity: These are not part of the AMPLE components and do not reflect a structured emergency history.
D. Abdominal sounds, memory loss, people exposed to, last medication, earliest availability of past medical records: These elements are not relevant to the AMPLE acronym and do not follow established emergency protocols.
Key Takeaways:
• The AMPLE mnemonic supports rapid, focused data collection in emergencies.
• It stands for Allergies, Medications, Past health history, Last meal, and Events/Environment.
• This tool helps identify potential complications and tailor emergency interventions.
A nurse is educating a group of nursing students about primary survey in the emergency department. Which of the following assessments are done during this survey?
Explanation
The primary survey in emergency care focuses on rapidly identifying and managing life-threatening conditions using the ABCDE approach: Airway, Breathing, Circulation, Disability, and Exposure/Environmental control. This systematic assessment ensures that vital functions are stabilized before continuing with a more detailed evaluation.
Rationale for Correct Answer:
D. The status of airway, breathing, circulation, disability, and exposure/environmental control: This structured approach allows healthcare providers to immediately detect and treat life-threatening issues. It prioritizes stabilization over diagnostic details or history-taking.
Rationale for Incorrect Answers:
A. Whether the resources of the ED are adequate: This is part of administrative triage planning, not the clinical assessment performed during the primary survey.
B. The acuity of the patient’s condition to determine priority of care: This refers to triage, which typically occurs before or alongside the primary survey but is not the same as the clinical ABCDE assessment.
C. Whether the patient is responsive enough to provide information: This might influence the history-taking process but is not a component of the primary survey, which focuses on physical and physiological assessment.
Key Takeaways:
• The primary survey uses the ABCDE framework to address immediate threats to life.
• It ensures prompt intervention in airway, breathing, circulation, neurological status, and exposure.
• It differs from triage and history-taking, which occur before or after the primary survey.
A nurse is performing a primary survey on a client involved in a road traffic accident and identifies asymmetric chest wall movement. Which intervention should the nurse do first?
Explanation
Asymmetric chest wall movement indicates a potential life-threatening respiratory issue such as a flail chest, pneumothorax, or severe pulmonary contusion. In the primary survey, after ensuring airway patency, the priority is to ensure effective breathing. Immediate bag-mask ventilation with 100% oxygen supports oxygenation and ventilation while definitive interventions are arranged.
Rationale for Correct Answer:
D. Administer bag-mask ventilation with 100% oxygen: Asymmetric chest rise suggests impaired ventilation, which requires prompt respiratory support. Administering high-flow oxygen with a bag-mask device addresses the breathing component of the ABCDE approach.
Rationale for Incorrect Answers:
- Check a central pulse: While circulation assessment is important, it is not the priority when breathing is compromised.
- Stabilize the cervical spine: This is performed at the start of the primary survey, typically simultaneously with airway management, but it is not the next immediate action after identifying compromised breathing.
- Apply direct pressure to the wound: This addresses external bleeding under the circulation step (C), which is secondary to airway and breathing in the ABCDE hierarchy.
Key Takeaways:
• Breathing difficulties identified during the primary survey must be addressed immediately.
• Bag-mask ventilation with 100% oxygen is the first-line intervention for asymmetric chest movement and suspected respiratory compromise.
• Follow the ABCs of trauma care to guide priorities: Airway → Breathing → Circulation.
A nurse is preparing to insert a nasogastric (NG) tube for a client in the emergency department. In which of the following situations would NG tube placement be contraindicated? Select all that apply
Explanation
Nasogastric (NG) tube placement is contraindicated in conditions where insertion poses a risk of worsening injury or causing life-threatening complications. These include airway burns, craniofacial trauma, and unstable cervical spine injury. In such cases, the risks of misplacement or further trauma outweigh the benefits of tube insertion.
Rationale for Correct Answers:
A. Inhalation injury: Placement of an NG tube is contraindicated due to potential airway edema and friability. Inserting a tube could worsen airway obstruction or provoke laryngospasm.
B. Head or facial trauma: NG insertion is contraindicated when facial fractures or basilar skull fractures are suspected. The tube could inadvertently enter the cranial vault, leading to severe brain injury.
D. Cervical spine fracture: Neck manipulation during NG placement may exacerbate a spinal cord injury unless the cervical spine has been cleared or stabilized. NG tube insertion should be deferred until spine precautions are ensured.
Rationale for Incorrect Answers:
C. Intestinal obstruction: NG tubes are often indicated in intestinal obstruction to decompress the bowel and relieve symptoms like vomiting and distension.
E. History of upper gastrointestinal bleeding: While caution is necessary, NG tubes may be used in active GI bleeding to assess the amount and nature of the bleed or for gastric lavage. It is not an absolute contraindication.
Key Takeaways:
• Facial/head trauma, inhalation injury, and cervical spine instability are major contraindications to NG tube placement.
• Always assess for airway protection and anatomic disruption before inserting an NG tube.
• Some gastrointestinal conditions like obstruction may actually require NG tube use for management.
A nursing is reviewing emergency management of poisoning. For which of the following ingested poisons may gastric lavage be considered? Select all that apply
Explanation
Gastric lavage may be considered in life-threatening ingestions of substances that do not have effective antidotes and when the procedure can be performed within 1 hour of ingestion. It is not recommended for caustic or corrosive substances due to risk of esophageal or gastric perforation.
Rationale for Correct Answers:
A. Bleach: Bleach is not classified as caustic hence lavage can be done.
B. Aspirin: A salicylate overdose may cause metabolic acidosis and other severe effects. Gastric lavage may be used early after ingestion when the dose is potentially lethal.
D. Iron supplements: Iron toxicity is serious and can be fatal. Gastric lavage may be beneficial in severe overdoses when initiated early.
E. Amitriptyline (Elavil): A tricyclic antidepressant overdose can lead to life-threatening cardiac and neurological effects. Gastric lavage may be performed early, especially if ingestion is recent and the patient is not at risk for aspiration.
Rationale for Incorrect Answers:
C. Drain cleaner: Also a caustic agent (usually alkaline), which poses high risk for esophageal burns and perforation. Gastric lavage is contraindicated in these cases.
Key Takeaways:
• Gastric lavage is reserved for life-threatening poisonings with substances that are not corrosive and when done within a 1-hour window.
• Caustic substances like bleach or drain cleaner should never be lavaged due to high risk of GI tract damage.
• Aspirin, iron, and tricyclic antidepressants may be considered for lavage depending on timing, dose, and clinical status.
The emergency department nurse is triaging four clients. Which client should the nurse see first?
Explanation
Prioritization is a principle that is central in nursing. Nurses learn prioritization to optimize the limited resources while saving lives. Prioritization is based on the principles of ABC, Maslow’s hierarchy of needs and acute vs chronic conditions.
Rationale for Correct Answer:
B. A 22-year-old woman with asthma in acute respiratory distress: This is a life-threatening airway emergency. Respiratory distress may lead to hypoxia, respiratory arrest, or cardiac arrest if not managed urgently. According to the ABC (Airway, Breathing, Circulation) prioritization, breathing issues are critical and must be addressed first.
Rationale for Incorrect Answers:
- A 6-year-old child with a temperature of 10C.2°F (39.6°C): While concerning, a high fever alone without signs of respiratory distress, seizure, or altered consciousness is not an immediate life-threatening emergency and can be triaged after stabilizing airway/breathing concerns.
- An infant who has been vomiting for 2 days: Risk of dehydration is high in infants, but unless the infant shows signs of shock, altered mental status, or severe electrolyte disturbance, this is not as emergent as active respiratory compromise.
- A 50-year-old man with low back pain and spasms: This is a painful but non-emergent condition without signs of neurologic deficit, infection, or trauma-related spinal injury.
Key Takeaways:
• Airway and breathing emergencies are top triage priorities.
• Respiratory distress in asthma can become fatal if not promptly treated.
• High fever and vomiting are concerning but generally triaged after airway or breathing issues are stabilized.
A client is brought to the emergency department after a near-drowning incident. Which of the following interventions is the priority in the management of this client?
Explanation
Correction of hypoxia is the immediate and most critical priority in the management of a near-drowning client. Oxygen deprivation is the primary cause of morbidity and mortality in these cases, and rapid restoration of adequate oxygenation is essential.
Rationale for Correct Answer:
- Correction of hypoxia: Hypoxia is the central and most urgent issue in near-drowning. Submersion leads to impaired gas exchange, resulting in hypoxemia. Immediate airway management and oxygen supplementation or mechanical ventilation are necessary to prevent irreversible organ damage, especially to the brain and heart.
Rationale for Incorrect Answers:
B. Correction of acidosis: Acidosis (metabolic and/or respiratory) is a consequence of hypoxia and can be resolved by restoring oxygenation and perfusion. It is important, but not the first priority.
C. Maintenance of fluid balance: Fluid shifts and aspiration can cause pulmonary edema, but this is addressed after securing the airway and correcting hypoxia.
D. Prevention of cerebral edema: While cerebral edema is a potential complication due to prolonged hypoxia, the immediate threat is oxygen deprivation, which must be corrected first to prevent cerebral hypoxia and subsequent edema.
Key Takeaways:
• Hypoxia is the most life-threatening consequence of near-drowning and must be corrected immediately.
• Management should always follow the ABCs (Airway, Breathing, Circulation) of emergency care.
• Secondary complications like acidosis, fluid imbalance, and cerebral edema are addressed after stabilization of oxygenation.
Exams on Emergency Nursing Principles and Management
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
- Define the principles and categories of emergency triage.
- Apply the ABCDE approach in emergency assessments.
- Identify interventions for common poisonings and overdoses.
- Explain the function of the Rapid Response Team.
- Recognize and respond to life-threatening arrhythmias.
- Implement key components of post-resuscitation care.
- Evaluate outcomes of emergency nursing interventions.
Overview of Emergency Nursing
- Emergency nursing involves rapid assessment and immediate intervention during life-threatening conditions.
- Core principles include:
- Triage (usual & mass casualty)
- Primary survey using ABCDE
- Poisoning management
- Rapid Response Team (RRT) activation
- Cardiac emergencies
- Post-resuscitation care
Triage
Under Usual Conditions
- Purpose: Prioritize care based on acuity.
- Categories:
- Emergent: Immediate threat to life or limb.
- Urgent: Requires prompt care but not life-threatening.
- Nonurgent: Can wait safely for care.
- Five-Level System includes:
- Resuscitation: Requires immediate treatment.
- Minor: Requires minimal intervention.
Mass Casualty Triage (Military System)
- Goal: Greatest good for the greatest number.
- Tag Classifications:
- Class I (Red): Immediate/life-threatening.
- Class II (Yellow): Major injuries, delayed treatment.
- Class III (Green): Minor injuries, can wait.
- Class IV (Black): Expectant; not likely to survive.

A – Airway & Cervical Spine
- First priority. No airway = no survival.
- Use:
- Head-tilt/chin-lift (no spinal injury).
- Jaw-thrust (with spinal injury).
- Clear obstructions: suction/finger sweep.
- Maintain airway: oropharyngeal/nasopharyngeal airway, BVM, or nonrebreather mask.
B – Breathing
- Assess:
- Breath sounds
- Respiratory effort and rate
- Chest movement
- Trachea position and JVD
- Support:
- Manual ventilation (BVM)
- Supplemental oxygen
C – Circulation
- Assess HR, BP, perfusion.
- Intervene:
- CPR if needed
- Control bleeding
- IV access with large-bore catheters
- Fluid resuscitation: LR or NS
- Monitor for shock: ↑HR, ↓BP
- Treat shock:
- Oxygen, fluids, blood
- Elevate feet
- Reassure client
D – Disability (Neuro Check)
- Use AVPU scale:
- Alert
- Voice-responsive
- Pain-responsive
- Unresponsive
- Glasgow Coma Scale (3–15):
- Eye, verbal, motor responses
E – Exposure/Environmental Control
- Remove clothes for full assessment.
- Prevent hypothermia:
- Warm blankets, heat lamps, room temp
- Warmed IV fluids
- Preserve evidence (clothing, bullets)

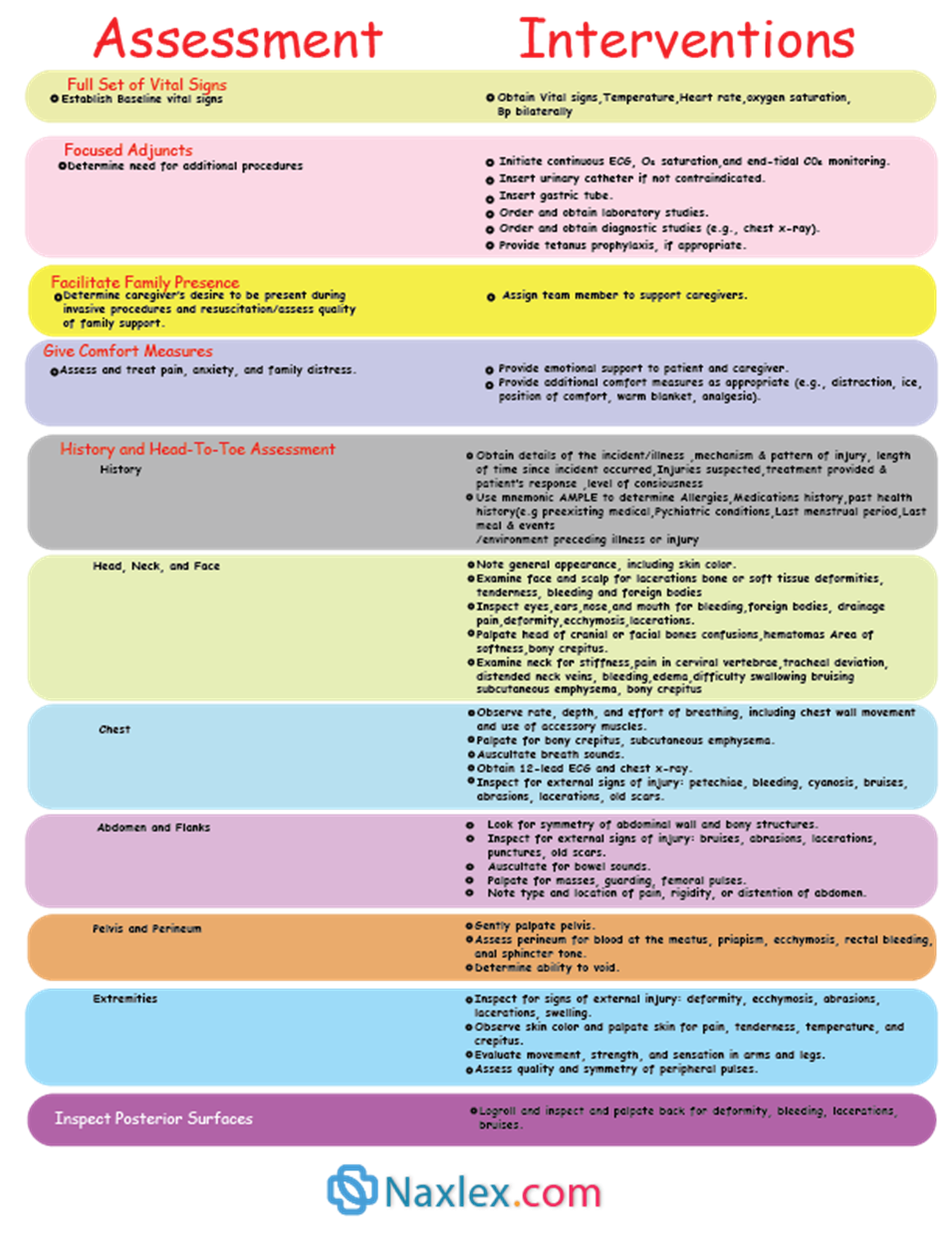
Secondary Survey
Poisoning
- Definition: Exposure to toxic agents (drugs, bites, pollutants).
- Steps:
- Identify substance
- Provide supportive care
- Prevent absorption
- Remove agent
- Administer antidotes (e.g., naloxone, antivenin)
- Interventions:
- Airway and respiratory support
- IV fluids for circulation
- Monitor: BP, ECG, glucose, ABGs, coagulation
- Pain management for bites
- Seizure management (IV diazepam)
- Dialysis or blood exchange if needed
Rapid Response Team (RRT)
- Members: ICU nurse, RT, provider/hospitalist.
- Purpose: Intervene before arrest/stroke.
- Communication: Use SBAR.
- Outcomes:
- Identify systemic issues
- Educate staff
- Encourage story-sharing post-event
Cardiac Emergencies
Types
- Cardiac Arrest: Sudden loss of cardiac function.
- Ventricular Fibrillation (VF):
- Chaotic rhythm, no pulse.
- Needs immediate defibrillation.
- Pulseless Ventricular Tachycardia (VT):
- Rapid rhythm → unconsciousness → VF.
- Ventricular Asystole:
- No electrical activity.
- Requires BLS + ACLS.
- Pulseless Electrical Activity (PEA):
- Electrical rhythm without pulse.
- Treat reversible causes + CPR.
Emergency Nurse Certifications
Emergency nurses in the United States are typically required to hold certifications in the following:
-
Focuses on hands-on assessment and management of airway, breathing, and circulation.
- Emphasizes high-quality CPR and early defibrillation for cardiac arrest.
2. Advanced Cardiac Life Support (ACLS)
- Builds on BLS with advanced interventions for adult cardiac emergencies, including:
- Cardiac rhythm recognition and monitoring
- Invasive airway management
- Electrical therapies (defibrillation, synchronized cardioversion)
- Intravenous (IV) access and medication administration
- Post-resuscitation care and stabilization
ACLS Protocols (American Heart Association – AHA)
- Ventricular Fibrillation (VF) / Pulseless Ventricular Tachycardia (VT):
- Begin BLS with immediate CPR and defibrillation
- Establish IV access
- Administer:
- Epinephrine 1 mg IV every 3–5 minutes
- Consider vasopressin 40 units IV once (alternative to first or second dose of epinephrine)
- Antidysrhythmic medications:
- Amiodarone
- Lidocaine
- Magnesium sulfate
- Procainamide
- Pulseless Electrical Activity (PEA):
- Begin CPR and establish IV access
- Identify and treat reversible causes:
- 5 H’s: Hypovolemia, Hypoxia, Hydrogen ion (acidosis), Hypo-/Hyperkalemia, Hypothermia
- 5 T’s: Toxins, Cardiac tamponade, Tension pneumothorax, Coronary thrombosis, Pulmonary thrombosis
- Administer epinephrine 1 mg IV every 3–5 minutes
- Asystole:
- Begin CPR and IV access
- Administer epinephrine 1 mg IV every 3–5 minutes
- Consider transcutaneous pacing
- Terminate efforts if rhythm remains unresponsive
3. Pediatric Advanced Life Support (PALS)
- Based on BLS principles, tailored to infant and child resuscitation
- Includes:
- Pediatric-specific assessment and airway management
- Fluid and medication dosing by weight
- Recognition and treatment of pediatric cardiac arrest and shock
Emergency Nurse Certifications
Emergency nurses in the United States are typically required to hold certifications in the following:
- Focuses on hands-on assessment and management of airway, breathing, and circulation.
- Emphasizes high-quality CPR and early defibrillation for cardiac arrest.
2. Advanced Cardiac Life Support (ACLS)
- Builds on BLS with advanced interventions for adult cardiac emergencies, including:
- Cardiac rhythm recognition and monitoring
- Invasive airway management
- Electrical therapies (defibrillation, synchronized cardioversion)
- Intravenous (IV) access and medication administration
- Post-resuscitation care and stabilization
ACLS Protocols (American Heart Association – AHA)
- Ventricular Fibrillation (VF) / Pulseless Ventricular Tachycardia (VT):
- Begin BLS with immediate CPR and defibrillation
- Establish IV access
- Administer:
- Epinephrine 1 mg IV every 3–5 minutes
- Consider vasopressin 40 units IV once (alternative to first or second dose of epinephrine)
- Antidysrhythmic medications:
- Amiodarone
- Lidocaine
- Magnesium sulfate
- Procainamide
- Pulseless Electrical Activity (PEA):
- Begin CPR and establish IV access
- Identify and treat reversible causes:
- 5 H’s: Hypovolemia, Hypoxia, Hydrogen ion (acidosis), Hypo-/Hyperkalemia, Hypothermia
- 5 T’s: Toxins, Cardiac tamponade, Tension pneumothorax, Coronary thrombosis, Pulmonary thrombosis
- Administer epinephrine 1 mg IV every 3–5 minutes
- Asystole:
- Begin CPR and IV access
- Administer epinephrine 1 mg IV every 3–5 minutes
- Consider transcutaneous pacing
- Terminate efforts if rhythm remains unresponsive
3. Pediatric Advanced Life Support (PALS)
- Based on BLS principles, tailored to infant and child resuscitation
- Includes:
- Pediatric-specific assessment and airway management
- Fluid and medication dosing by weight
- Recognition and treatment of pediatric cardiac arrest and shock
Postresuscitation Care
-
Maintain perfusion and prevent organ failure.
-
Monitor vital signs, oxygenation, neurologic function.
-
Provide emotional support for family.
-
Document thoroughly.
AVPU Neurological Scale
|
Letter |
Meaning |
|
A |
Alert |
|
V |
Responds to Voice |
|
P |
Responds to Pain |
|
U |
Unresponsive |
Mass Casualty Triage Tags
|
Tag Color |
Class |
Priority |
|
Red |
Class I |
Immediate |
|
Yellow |
Class II |
Delayed |
|
Green |
Class III |
Minimal |
|
Black |
Class IV |
Expectant (deceased) |
Post-Resuscitation Care
Goals
-
Optimize perfusion, prevent further injury, and support recovery of organ systems.
Airway and Breathing
-
Maintain advanced airway and ventilation.
-
Use oxygen to keep SpO₂ >94%.
-
Monitor for pulmonary edema, aspiration, and respiratory failure.
Circulation
-
Maintain MAP ≥65 mmHg and adequate urine output.
-
Use fluids and vasopressors if hypotensive.
-
Monitor ECG for dysrhythmias.
-
Treat underlying cause of arrest (e.g., hypoxia, electrolyte imbalance).
-
Assess for return of consciousness.
-
Initiate targeted temperature management (32–36°C) for unconscious clients.
-
Frequent Glasgow Coma Scale and pupillary response checks.
-
ABGs, lactate, electrolytes, troponin, glucose.
-
12-lead ECG.
-
Head CT if trauma or neurologic concerns.
Infection Prevention
-
Aseptic technique for all lines and airways.
-
Monitor WBCs, cultures, temperature.
Family Support
-
Provide updates and psychological support.
-
Allow family presence during care if appropriate.
Summary
- Emergency nurses rapidly prioritize patients based on the severity of their condition to ensure the most critical are treated first.
- This is a systematic and rapid assessment to identify and manage immediate, life-threatening conditions.
- After stabilizing life-threatening issues, a thorough head-to-toe assessment and patient history (AMPLE) is conducted.
- Nurses are responsible for initiating resuscitation efforts and stabilizing patients, including administering medications and preparing for advanced procedures.
- A key principle is the timely and effective assessment and management of pain to improve patient comfort.
- Emergency nurses must communicate clearly and provide support to both patients and families in a high-stress environment.
- Adhering to strict infection control practices, such as hand hygiene and standard precautions, is essential to protect everyone.
- Providing emotional and psychological support is a critical part of care for patients and families facing sudden illness or trauma.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Emergency Nursing Principles and Management
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


