Please set your exam date
Dissociative Disorder
Study Questions
Practice Exercise 1
A nurse is caring for a client who has been diagnosed with psychogenic fugue. In reviewing the client’s medical record, which information in the client’s history should indicate to the nurse that the diagnosis is correct? SELECT ALL THAT APPLY.
Explanation
Psychogenic fugueis a rare dissociative disorder characterized by sudden, unexpected travel away from home with inability to recall one’s past and confusion about personal identity. It often follows severe psychological stress or trauma. The person may assume a new identity and is not aware of the memory loss. Unlike other dissociative or psychotic conditions, hallucinations or delusional thinking are not primary features. Amnesia, identity disturbance, and escape behavior are central diagnostic markers.
Rationale for correct answer
1.The presence of profound retrograde amnesiaafter a traumatic accident aligns with dissociative fugue. Inability to recall autobiographical details without evidence of neurological damage is consistent with the condition.
2.Assuming a new identityand leaving home following intense psychological trauma such as losing a child strongly indicates psychogenic fugue. The change occurs abruptly and serves as psychological escape.
Rationale for incorrect answers
3.Dissociative identitydisorder involves multiple distinct personalities, not a single episode of amnesia with travel and identity loss. This presentation is separate from psychogenic fugue.
4.Grandiose delusionssuch as superhero qualities are hallmarks of psychotic disorders like schizophrenia or mania, not dissociative fugue, which lacks psychosis as a central feature.
5.Residence in a homeless shelterafter spousal abuse suggests situational displacement due to trauma, but without identity loss or amnesia it does not meet the criteria for psychogenic fugue.
Take Home Points
- Psychogenic fugue involves sudden travel away from home, loss of autobiographical memory, and possible assumption of a new identity.
- It is triggered by overwhelming psychological trauma or stress rather than direct brain injury.
- Must be differentiated from dissociative identity disorder and psychotic conditions with delusions or hallucinations.
- Management includes psychotherapy, trauma processing, and ensuring patient safety when memory and identity are impaired.
A nurse is caring for a client diagnosed with dissociative amnesia. The client recently experienced a divorce. How should the nurse help the client deal with traumatic memories?
Explanation
Dissociative amnesiais a disorder marked by the inability to recall important autobiographical information, usually of a traumatic or stressful nature, that cannot be explained by normal forgetfulness. The condition often follows severe life stressors, and recovery involves gradual integration of memories through safe therapeutic exploration. Emotionalprocessing, patient safety, and supportive care are central in management.
Rationale for correct answer
4.Allowing the client to verbalize feelings provides a safe outlet for emotional expression. Encouraging discussion of distress promotes gradual processing of trauma, reducing dissociative defenses and aiding memory recovery without re-traumatization.
Rationale for incorrect answers
1.Discouraging verbalizationsuppresses coping mechanisms, increases internal tension, and prevents therapeutic progress. Avoidance maintains dissociation and hinders the client’s ability to integrate the traumatic event.
2.Forcing confrontationmay overwhelm the client, cause retraumatization, and worsen dissociation. Gradual supportive processing is the evidence-based approach, not aggressive exposure to painful memories.
3.Offering generic reassurancewithout addressing feelings invalidates the client’s experience. Such minimization prevents healing by ignoring the emotional complexity of the trauma and its psychological effects.
Take Home Points
- Dissociative amnesia involves memory loss linked to trauma without medical causes.
- Supportive therapy encourages safe verbalization and gradual processing of painful experiences.
- Confrontation and suppression can worsen symptoms and maintain dissociative defenses.
- Differentiation from other dissociative and psychotic disorders is essential for accurate management.
A nurse is caring for a client who has a dissociative disorder and is experiencing amnesia. What could have triggered the amnesia?
Explanation
Dissociative amnesiais a disorder characterized by an inability to recall important autobiographical information that is usually precipitated by extreme stress or trauma. The memory disturbance cannot be explained by substance use, neurological illness, or other medical conditions. Stressfulevents overwhelm normal coping, leading to psychological blocking of memory. Traumaexposure and unresolved conflict are most common triggers, with no direct physiological cause.
Rationale for correct answer
1.Severe psychosocial stressdisrupts cognitive integration of memory, producing dissociative amnesia. It functions as a protective mechanism that shields the individual from overwhelming trauma by preventing recall of distressing experiences.
Rationale for incorrect answers
2.Short-acting sedationcan cause temporary memory lapses due to pharmacologic effects, but this is drug-induced amnesia, not dissociative amnesia, and resolves as the drug wears off.
3.Conscious sedationmay impair immediate recall during medical procedures but is predictable, intentional, and medication-based. It does not meet the diagnostic framework of a dissociative disorder.
4.Syndrome of inappropriate antidiuretichormone leads to hyponatremia, confusion, or seizures due to electrolyte imbalance, but does not selectively produce dissociative-type amnesia or identity disturbance.
Take Home Points
- Dissociative amnesia arises from severe psychological trauma, not medication or metabolic disturbances.
- It is distinguished from drug-induced or organic causes of memory loss.
- Memory loss is protective, shielding the mind from overwhelming emotional stress.
- Accurate differentiation is essential for guiding therapy, which focuses on safe emotional expression and trauma processing.
Which client situation supports a potential diagnosis of a dissociative fugue?
Explanation
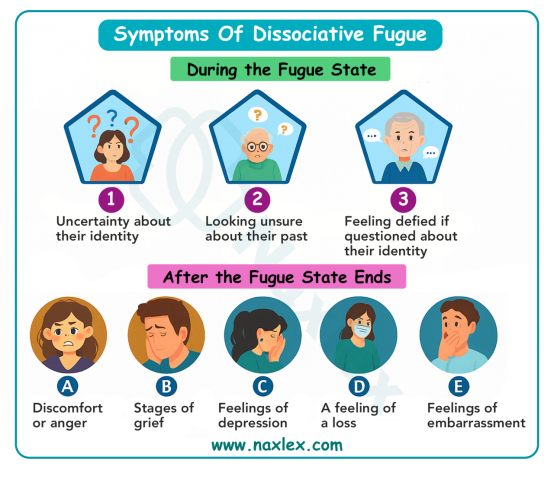
Dissociative fugueis a rare subtype of dissociative amnesia characterized by sudden, unexpected travel away from one’s usual environment, accompanied by amnesiafor personal identity and autobiographical information. Individuals may appear normal during the fugue but are unaware of their identity and how they arrived at the new location. The condition often follows severe psychological stressor trauma and may involve the creation of a new identity. Episodes can last hours to months and resolve spontaneously, often leaving the person confused or distressed.
Rationale for correct answer
1.The client’s presence in a distant location with no memory of identity or travel strongly supports amnesiaand disorientation, hallmark features of dissociative fugue. The sudden travel and identity confusion are diagnostic.
Rationale for incorrect answers
2.Sudden personality change such as aggression in a previously passive client may suggest a mood or personality disorder, but lacks the amnesiaand travel component essential for dissociative fugue.
3.Memory loss following trauma is more consistent with post-traumaticamnesia or concussion. The absence of travel and identity confusion excludes dissociative fugue.
4.Feelings of detachment are indicative of depersonalization, a separate dissociative disorder. There is no travel or identity loss, which are required for fugue diagnosis.
Take Home Points
- Dissociative fugue involves sudden travel and loss of personal identity without awareness of the journey.
- It must be differentiated from depersonalization, dissociative identity disorder, and post-traumatic amnesia.
- Clients may appear normal during the fugue, making diagnosis challenging until the episode ends.
- Fugue states often follow psychological trauma and may resolve spontaneously with memory restoration.
Practice Exercise 2
A nurse is treating a client diagnosed with dissociative identity disorder (DID). Which actions should the nurse take when working with this client? SELECT ALL THAT APPLY.
Explanation
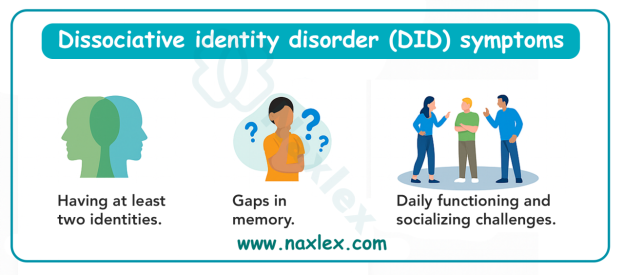
Dissociative identity disorderis a complex psychiatric condition marked by the presence of two or more distinct identity states that recurrently take control of behavior. It is associated with amnesia, severe trauma, and disruptions in memory, perception, and self-awareness. Each identity may have unique traits, preferences, and even physiological responses. Stress, environmental triggers, and interpersonal conflict can precipitate dissociative episodes. Management requires trauma-informed care, safety monitoring, and structured therapeutic engagement.
Rationale for correct answer
2.A calm environment reduces hyperarousaland minimizes dissociative triggers. It supports emotional regulation and promotes psychological safety for fragmented identity states.
3.Open communication fosters trustand therapeutic alliance. It allows the nurse to engage with different identities respectfully and helps the client feel validated and understood.
4.Clients with DID have elevated risk for suicidalitydue to internal conflict between identities and unresolved trauma. Monitoring for suicidal ideation is essential for safety and crisis prevention.
5.Behavioral changes may reflect identity shiftsor dissociative episodes. Accurate documentation helps track patterns, supports diagnosis, and informs interdisciplinary care planning.
Rationale for incorrect answers
1.Long-term goals are inappropriate during acute care. The client’s immediate needs for stabilizationand safety take precedence over future-oriented planning.
Take Home Points
- DID involves identity fragmentation, amnesia, and behavioral shifts often linked to trauma.
- Acute care focuses on safety, stabilization, and therapeutic engagement—not long-term goal setting.
- Suicide risk is elevated in DID due to internal conflict and trauma history.
- Differentiation from schizophrenia, borderline personality disorder, and PTSD is essential for accurate diagnosis and care.
A nurse is caring for a client named Susan who has been diagnosed with dissociative identity disorder. Usually, the client arrives to therapy sessions dressed in a tasteful business suit. One day, the client comes to the clinic dressed in a gold lamé mini-dress and insists that her name is Ruby. How should the nurse respond?
Explanation
Dissociative identity disorderis a chronic psychiatric condition involving the presence of two or more distinct identity states that recurrently take control of behavior. These identities, often called alters, may differ in name, gender, affect, and even physiological responses. The disorder is strongly linked to early trauma, especially repeated abuse, and is characterized by disruptions in memory, identity, and perception. Each identity may emerge in response to specific stressors or triggers, and therapeutic engagement requires a nonjudgmentaland trauma-informed approach.
Rationale for correct answer
4.Exploring the characteristics of the newly emerged identity supports integrationand therapeutic insight. It allows the nurse to build rapport with the presenting identity and gather information about internal dynamics and triggers.
Rationale for incorrect answers
1.Labeling the outfit as ridiculous introduces judgment, which undermines therapeutic trust and may provoke shame or withdrawal from the client’s alter.
2.Refusing to acknowledge the presenting identity invalidates the client’s experienceand may escalate internal conflict or dissociation. Recognition of each identity is essential for therapeutic progress.
3.Ignoring the behavior disregards the emergence of a distinct identity state, missing an opportunity for assessmentand engagement. It may also signal disinterest or lack of support.
Take Home Points
- DID involves distinct identity states with unique behaviors, names, and emotional profiles.
- Therapeutic care requires validation of each identity without judgment or confrontation.
- Engagement with presenting alters supports integration and trauma processing.
- DID must be differentiated from schizophrenia, borderline personality disorder, and malingering.
A nurse is caring for a client who has a depersonalization disorder. Which clear and explicit outcomes should the nurse work toward?
Explanation
Depersonalization disorderis a dissociative condition characterized by persistent or recurrent experiences of feeling detached from one’s own body, thoughts, or surroundings. Clients often describe a sense of unreality, emotional numbing, or being an outside observer of themselves. It is frequently triggered by stress, trauma, or anxiety, and may co-occur with other psychiatric conditions. The disorder impairs self-perception and emotional integration, making active engagement in treatment and restoration of agency critical for recovery.
Rationale for correct answer
3.Promoting confidence and participation enhances self-efficacyand therapeutic engagement. It helps the client regain a sense of control and reality, which are often disrupted in depersonalization disorder.
Rationale for incorrect answers
1.While strengths-based approaches are valuable, they do not directly address the client’s detachmentor promote re-engagement with the self, which is central to depersonalization recovery.
2.Focusing on past accomplishments may reinforce avoidanceand disconnection from present reality. The goal is to re-anchor the client in current experiences and identity.
4.Eliciting empathetic responses from the client is not a therapeutic outcome. The focus should be on integration, not emotional output toward others, which may be blunted in depersonalization.
Take Home Points
- Depersonalization disorder involves persistent detachment from self or surroundings, often described as feeling unreal or emotionally numb.
- Treatment goals center on restoring self-awareness, emotional integration, and active participation in care.
- It must be differentiated from psychotic disorders, PTSD, and anxiety disorders.
- Nursing care should prioritize grounding techniques, reality orientation, and collaborative treatment planning.
Ellen has a history of childhood physical and sexual abuse. She was diagnosed with dissociative identity disorder (DID) 6 years ago. She has been admitted to the psychiatric unit following a suicide attempt. The primary nursing diagnosis for Ellen would be:
Explanation
Dissociative identity disorderis a trauma-related condition marked by the presence of two or more distinct identity states, often accompanied by amnesia, emotional instability, and identity fragmentation. It is strongly associated with early abuse, particularly sexual and physical trauma. Clients with DID are at elevated risk for self-harm and suicidal behavior due to internal conflict between identities, unresolved trauma, and impaired coping mechanisms. Acute psychiatric admissions often follow dissociative crises or suicide attempts, requiring immediate safety-focused interventions.
Rationale for correct answer
4.Suicide risk is the most urgent priorityin acute care. Ellen’s recent attempt and trauma history indicate unresolved psychological pain, necessitating focused interventions to ensure safetyand stabilization.
Rationale for incorrect answers
1.While identity disturbance is central to DID, it is not the most acuteconcern in this scenario. The suicide attempt demands prioritization of risk over long-term identity work.
2.Sensory perception disturbances are not core features of DID. The client’s presentation does not reflect hallucinationsor perceptual distortions typical of this diagnosis.
3.Memory impairment in DID is due to dissociation, not disturbed thought processes. This diagnosis misattributes the cause and overlooks the immediacyof the suicide risk.
Take Home Points
- Suicide risk is the highest priority in acute psychiatric care for clients with DID.
- DID involves identity fragmentation, amnesia, and trauma-related dissociation.
- Nursing diagnoses must reflect the most immediate threats to safety and functioning.
- DID should be differentiated from schizophrenia, PTSD, and borderline personality disorder.
In establishing trust with Ellen, a client with the diagnosis of DID, the nurse must:
Explanation
Dissociative identity disorderinvolves the presence of two or more distinct identity states that recurrently take control of behavior. Each identity, or alter, may have unique traits, memories, and emotional responses. These identities often emerge in response to trauma, serving as adaptive mechanisms to compartmentalize overwhelming experiences. Therapeutic care requires recognition of each identity as a valid part of the client’s psychological structure. Building trustwith each identity is essential for integration and stabilization.
Rationale for correct answer
2.Establishing relationships with each identity fosters rapportand therapeutic engagement. It validates the client’s internal experience and supports integrationby reducing conflict between alters and promoting cooperation.
Rationale for incorrect answers
1.Denying the presence of multiple identities invalidates the client’s reality and undermines trust, which is foundational in trauma-informed care for DID.
3.Ignoring behaviors attributed to other identities dismisses important clinical data. These behaviors reflect internal dynamicsand must be acknowledged to guide assessment and intervention.
4.Demanding that the client maintain a primary identity imposes controland disregards the fluid nature of DID. It may provoke resistance or exacerbate dissociation.
Take Home Points
- DID requires therapeutic engagement with each identity to foster trust and promote integration.
- Denial or invalidation of alters undermines rapport and may worsen dissociative symptoms.
- Nursing care must be trauma-informed, flexible, and respectful of the client’s internal experience.
- DID should be differentiated from schizophrenia, malingering, and borderline personality disorder.
Practice Exercise 3
A nurse is caring for a client who has a dissociative disorder. What should the nurse do to assist the client in goal achievement?
Explanation
Dissociative disorderrefers to a group of conditions involving disruptions in memory, identity, and perceptionof self or environment. These disorders often arise in response to severe trauma, particularly during early development, and serve as coping mechanisms to compartmentalize overwhelming experiences. Clients may struggle with fragmented self-concept, emotional regulation, and goal-directed behavior. Therapeutic strategies must reinforce stability, promote self-efficacy, and support reintegration of dissociated aspects of identity.
Rationale for correct answer
1.Facilitating success builds self-esteemand reinforces adaptive functioning. It helps the client reconnect with their capabilities, fostering confidenceand motivation toward recovery and goal achievement.
Rationale for incorrect answers
2.Excessive or unwarranted praise may appear insincere, undermining therapeutic trust. It can distort reality testing and hinder the development of authentic self-worth.
3.Evaluating self-concept is an assessment activity, not a direct intervention for goal achievement. It provides insight, but does not actively promote progress or behavioral change.
4.Discussing behavioral categories is educational, not therapeutic. It may overwhelm the client or reinforce pathologywithout offering actionable steps toward goal-directed outcomes.
Take Home Points
- Dissociative disorders impair identity, memory, and perception, often rooted in trauma.
- Goal achievement requires reinforcement of self-efficacy through structured success experiences.
- Interventions must be therapeutic, not merely educational or evaluative.
- Dissociative disorders should be differentiated from psychotic disorders, PTSD, and borderline personality disorder.
The ultimate goal of therapy for a client with DID is:
Explanation
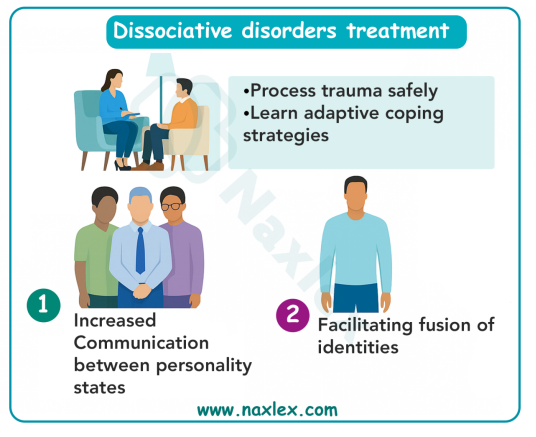
Dissociative identity disorderis a chronic trauma-related condition marked by the presence of two or more distinct identity states that recurrently take control of behavior. These identities, or alters, often have separate memories, emotions, and behavioral patterns. The disorder is rooted in severe childhood trauma, particularly abuse, and serves as a psychological defense mechanism to compartmentalize overwhelming experiences. Long-term therapy aims to reduce fragmentation, promote internal cooperation, and ultimately achieve identity integration.
Rationale for correct answer
1.Integration of personalities into one cohesive identity is the therapeutic endpoint. It allows the client to function with unified memory, emotional regulation, and self-awareness, eliminating dissociative switching and internal conflict.
Rationale for incorrect answers
2.Voluntary switching maintains fragmentation and does not resolve the underlying dissociation. It may offer temporary control but does not promote long-term psychological integration.
3.Selecting a dominant personality reinforces hierarchyamong alters and may increase internal conflict. Therapy focuses on merging identities, not choosing between them.
4.Recognition of personalities is an early therapeutic milestone, not the ultimategoal. It facilitates insight but does not address the need for full integration and resolution of trauma.
Take Home Points
- The final goal of DID therapy is full integration of all identity states into one cohesive self.
- DID arises from severe trauma and involves identity fragmentation, amnesia, and emotional dysregulation.
- Early therapy focuses on safety, stabilization, and recognition of alters; later phases aim for fusion.
- DID must be differentiated from schizophrenia, borderline personality disorder, and PTSD.
Which of the following interventions would be most helpful for a client with a dissociative disorder having difficulty expressing feelings?
Explanation
Dissociative disordersinvolve disruption of memory, identity, emotion, or perception, usually in response to trauma. They impair the ability to integrate experiences consciously. Groundingmethods help patients remain connected to the present moment. Safetyand emotional stabilization are first-line in management before trauma processing begins.
Rationale for correct answer
4.Grounding techniqueshelp reconnect the individual with reality when dissociation occurs. By focusing on sensory experiences or immediate surroundings, they reduce detachment and aid emotional regulation, allowing safe expression of feelings.
Rationale for incorrect answers
1.Distraction may shift attentionaway from painful thoughts temporarily, but it does not promote integration of dissociated feelings or help the client learn adaptive emotional expression.
2.Reality orientationis appropriate for cognitive disorders such as dementia, not dissociative conditions. The problem is emotional disconnection, not confusion about time or place.
3.Journaling encourages expressionbut may overwhelm clients with trauma if used before stabilization. Without grounding first, it can increase vulnerability and worsen dissociation rather than resolve it.
Take Home Points
- Dissociative disorders arise as protective responses to trauma, disrupting memory and identity.
- Grounding is the first-line technique to help stabilize patients and connect them to the present.
- Interventions like journaling can be helpful only after safety and stabilization are established.
- Differentiation from cognitive impairment is important, as treatment strategies differ significantly.
A newly admitted client is diagnosed with dissociative identity disorder. Which nursing intervention is a priority?
Explanation
Dissociative identity disorderis a complex dissociative condition characterized by the presence of two or more distinct personality states that recurrently take control of behavior. It is strongly associated with severe early trauma, often involving abuse. Management requires stabilization before trauma exploration. Establishing safety, building trust, and ensuring basic securityare essential before working on integration or coping skills. Without stability, interventions may worsen symptoms or retraumatize the client.
Rationale for correct answer
1.Creating safetyand securityis the priority intervention because clients with dissociative identity disorder often experience high vulnerability, self-harm risk, and fear. A safe environment allows stabilization before deeper therapeutic work.
Rationale for incorrect answers
2.Working with each subpersonalityequally and identifying relationships among them is important later in therapy, but it is not the immediate priority upon admission, when safety must come first.
3.Teaching coping skillsis a valuable long-term strategy to reduce dissociation, but these interventions require stability and readiness, which cannot be achieved without first ensuring safety.
4.Processing traumatic originstoo early can overwhelm the client and trigger further dissociation or crisis. Trauma exploration is a later therapeutic stage once safety and stabilization have been secured.
Take Home Points
- Dissociative identity disorder involves multiple distinct identities resulting from severe trauma, most often childhood abuse.
- Initial nursing priority is establishing safety and stabilization before therapeutic interventions.
- Coping skills and subpersonality work follow only after trust and stability are achieved.
- Trauma processing is delayed until later stages of therapy to prevent retraumatization.
Which of the following nursing evaluations for a hospitalized client diagnosed with dissociative identity disorder would lead the treatment team to consider discharge? SELECT ALL THAT APPLY.
Explanation
Dissociative identity disorderis a chronic trauma-related condition marked by the presence of two or more distinct identity states, often accompanied by amnesia, emotional dysregulation, and identity fragmentation. Hospitalization is indicated during acute crises such as suicidal behavior, severe dissociation, or inability to function safely. Discharge planning focuses on stabilization, insight, and the development of adaptive coping mechanisms. Indicators for discharge include improved emotional regulation, recognition of internal states, and reduced reliance on dissociative defenses.
Rationale for correct answer
1.Recalling traumatic events reflects improved integrationand emotional processing. It indicates that the client is beginning to confront and work through previously dissociated material.
2.Communicating anxiety before dissociation shows increased self-awarenessand emotional regulation. It allows for early intervention and reduces the likelihood of dissociative episodes.
3.Demonstrating adaptive coping strategies reflects behavioral stabilityand psychological resilience. It shows the client can manage stress without reverting to dissociative defenses.
4.Verbalizing the existence and function of alters indicates insightand internal cooperation. It supports therapeutic progress and readiness for outpatient continuation of care.
Rationale for incorrect answers
5.Continued use of alternate personalities to manage stress reflects persistent fragmentation. It suggests the client is still relying on dissociative mechanisms and is not yet ready for discharge.
Take Home Points
- Discharge readiness in DID requires emotional regulation, insight, and reduced reliance on dissociative defenses.
- Ability to recall trauma and communicate anxiety signals therapeutic progress.
- Adaptive coping and internal cooperation are essential for safe transition to outpatient care.
- Persistent use of alters for stress management indicates ongoing fragmentation and need for continued inpatient support.
Comprehensive questions
The ultimate goal of therapy for a client with DID is most likely achieved through:
Explanation
Dissociative identity disorderis a chronic trauma-related condition characterized by the presence of two or more distinct identity states that alternate in controlling behavior. It is associated with amnesia, identity fragmentation, and emotional dysregulation. The condition typically develops in response to severe childhood trauma, especially repeated abuse. Treatment focuses on stabilizing symptoms, processing traumatic memories, and integrating identities. Psychotherapeutic modalities, including trauma-focused approaches and adjunctive techniques like hypnosis, are central to long-term recovery.
Rationale for correct answer
2.Psychotherapy and hypnosis support integrationand trauma resolution. Psychotherapy facilitates emotional processing and identity stabilization, while hypnosis can access dissociated material and enhance recallof repressed memories.
Rationale for incorrect answers
1.Crisis intervention is short-term and focused on immediate safety, not long-term integration. Directed association lacks evidence-based support for treating identity fragmentation in DID.
3.Psychoanalysis and free association are less effective for DID due to their non-directivenature and limited focus on trauma stabilization. They may exacerbate dissociation without structured containment.
4.Dextroamphetamines are not indicated for DID and may worsen dissociationor anxiety. Insight psychotherapy alone is insufficient without trauma-focused strategies and stabilization techniques.
Take Home Points
- DID treatment requires long-term psychotherapy focused on trauma resolution and identity integration.
- Hypnosis may aid in accessing dissociated memories and enhancing therapeutic engagement.
- Pharmacologic agents like stimulants are not appropriate for core symptoms of DID.
- DID must be differentiated from schizophrenia, PTSD, and borderline personality disorder for accurate treatment planning.
You are caring for Susannah, a 29-year-old who has been diagnosed with dissociative identity disorder. She was recently hospitalized after coming to the emergency room with deep cuts on her arms with no memory of how this occurred. The priority nursing intervention for Susannah is:
Explanation
Dissociative identity disorderis a trauma-related psychiatric condition marked by the presence of two or more distinct identity states that alternate in controlling behavior. It is associated with amnesia, emotional instability, and identity fragmentation. Clients may experience dissociative episodes during which they are unaware of their actions, including self-harm. Acute presentations involving physical injury and memory loss require immediate safety-focusedinterventions before therapeutic exploration or long-term planning can begin.
Rationale for correct answer
2.Maintaining 1:1 observation ensures safetyand allows for continuous monitoring of self-harm risk. It is the highest priority in acute care settings when the client presents with injuryand dissociation.
Rationale for incorrect answers
1.Assisting with memory recovery is not appropriate during acute crisis. It may increase distressand worsen dissociation. Trauma processing should only occur after stabilization.
3.Teaching coping skills is a long-term intervention. In the acute phase, the client may lack the capacityto absorb or apply these strategies due to dissociation and emotional dysregulation.
4.Referral for integrative therapy is future-oriented. It does not address the immediate riskof harm and cannot substitute for direct safety measures during hospitalization.
Take Home Points
- Acute care for DID prioritizes safety and stabilization before therapeutic interventions.
- 1:1 observation is essential when clients present with self-harm and dissociative amnesia.
- Trauma processing and coping skill development should follow once the client is stable.
Jamie, age 24, has been diagnosed with a dissociative disorder following a traumatic event. Jamie’s mother asks you, “Does this mean my daughter is now crazy?” Your best response would be:
Explanation
Dissociative disorderis a trauma-related psychiatric condition characterized by disruptions in consciousness, memory, and identity. It often arises as a psychological defense against overwhelming stressor trauma, allowing the individual to detach from painful experiences. Dissociation can range from mild detachment to severe fragmentation of identity and memory. These disorders are not indicative of psychosis or “craziness,” but rather represent adaptive mechanisms that become maladaptive over time. Recovery is possible with structured, trauma-informed care.
Rationale for correct answer
4.This response validates the client’s experience without stigmatizingthe condition. It explains dissociation as a trauma response and emphasizes hopethrough treatment and recovery, aligning with therapeutic communication principles.
Rationale for incorrect answers
1.Labeling the client as mentally ill and out of touch with reality reinforces stigmaand misrepresents dissociative disorders, which do not inherently involve psychosis or loss of reality testing.
2.Predicting long-term inpatient care and referencing delusions is inaccurate, as dissociative disorders do not typically involve delusional thinking. This response may increase fear and misunderstanding.
3.Suggesting the disorder may be fabricated undermines credibilityand invalidates the client’s suffering. It reflects bias and contradicts evidence-based understanding of trauma-related dissociation.
Take Home Points
- Dissociative disorders are trauma-related conditions involving detachment from memory, identity, or perception.
- They are not psychotic disorders and do not imply loss of reality testing or delusions.
- Therapeutic communication must validate the client’s experience and offer hope for recovery.
- Differentiation from schizophrenia, malingering, and borderline personality disorder is essential for accurate diagnosis and care.
Which statement supports a psychodynamic theory in the etiology of dissociative disorders?
Explanation
Psychodynamic theoryexplains dissociative disorders as unconscious defense mechanisms used to manage overwhelming emotional conflict. It emphasizes repression, internal conflict, and the role of early traumain shaping psychological responses. Dissociation is viewed as a protective strategy that allows the mind to avoid conscious awareness of painful experiences, preserving psychological stability at the cost of memory and identity continuity.
Rationale for correct answer
4.Repression aligns directly with psychodynamicprinciples. It reflects the unconscious blocking of distressing memories or emotions to protect the ego from emotional pain, a core concept in this theory.
Rationale for incorrect answers
1.Hippocampal dysfunction is a neurobiologicalexplanation, not psychodynamic. It relates to structural brain changes affecting memory, not unconscious defense mechanisms.
2.Cortical arousal is a physiologicalresponse linked to stress and anxiety. It does not reflect the symbolic or unconscious processes emphasized in psychodynamic models.
3.Overwhelmed coping capacity is a behavioralor trauma-based view. While relevant to dissociation, it lacks the emphasis on unconscious repression central to psychodynamic theory.
Take Home Points
- Psychodynamic theory attributes dissociation to unconscious repression of painful emotional experiences.
- It differs from neurobiological, behavioral, and trauma-based models by focusing on internal symbolic processes.
- Repression is a key defense mechanism in psychodynamic formulations of dissociative disorders.
- Differentiating theoretical models helps guide appropriate therapeutic approaches and communication strategies.
A frightened client diagnosed with dissociative fugue tells the nurse, “I don’t know where I am or how I got here. What is wrong with me?” Which nursing response reflects a neurobiological perspective?
Explanation
Dissociative fugueis a subtype of dissociative amnesia characterized by sudden, unexpected travel away from one’s usual environment, accompanied by amnesiafor personal identity and autobiographical information. Neurobiological models suggest that dissociative symptoms may arise from disruptions in brain function, particularly in regions responsible for memory and self-awareness. Abnormal activity in the temporal lobe, limbic system, and hippocampus has been implicated in dissociative phenomena, especially in individuals with seizure disorders or migraine-related neurological disturbances.
Rationale for correct answer
2.This response reflects a neurobiologicalunderstanding by linking dissociative symptoms to conditions like temporal lobe epilepsy and migraines, which involve altered cortical activityand can disrupt memory and spatial orientation.
Rationale for incorrect answers
1.Repression is a psychodynamicconcept, not neurobiological. It involves unconscious defense mechanisms rather than brain-based dysfunction.
3.Escaping from reality due to trauma aligns with trauma theory, emphasizing psychological adaptation rather than neurological etiology.
4.Familial patterns suggest a geneticor psychosocial influence, not a direct neurobiological mechanism. It lacks specificity regarding brain function or structure.
Take Home Points
- Neurobiological models of dissociation focus on brain regions like the temporal lobe and hippocampus.
- Dissociative fugue involves sudden travel and amnesia, often linked to neurological disruption.
- Differentiating theoretical models helps tailor nursing responses and guide interdisciplinary care.
- Dissociative symptoms may overlap with seizure disorders, migraines, and other neurological conditions.
A client admitted with dissociative fugue is being evaluated. Which assessment information would indicate that the client is ready for discharge?
Explanation
Dissociative fugueis a subtype of dissociative amnesia marked by sudden, unexpected travel away from one’s usual environment, accompanied by amnesiafor identity and autobiographical history. It often follows severe psychological stressand may involve the creation of a new identity. Clients may appear normal during the fugue but are unaware of their true identity or how they arrived at the new location. Discharge readiness is determined by the client’s ability to maintain reality orientation, manage stress without dissociative episodes, and demonstrate psychological stability.
Rationale for correct answer
1.The ability to maintain reality during stress reflects stabilizationand reduced vulnerability to dissociative episodes. It indicates the client can function safely and consistently in daily life, meeting criteria for dischargereadiness.
Rationale for incorrect answers
2.Verbalizing why personalities exist pertains to dissociative identity disorder, not dissociative fugue. This response misattributes diagnostic features and does not reflect discharge criteria for fugue.
3.Discussing depersonalization is relevant to depersonalization disorder, not fugue. While emotional insight is valuable, it does not confirm readiness for discharge in fugue cases.
4.Integration of subpersonalities is a therapeutic goal in dissociative identity disorder, not dissociative fugue. This choice confuses diagnostic boundaries and does not apply to the condition being evaluated.
Take Home Points
- Dissociative fugue involves sudden travel and identity amnesia, often triggered by psychological stress.
- Discharge readiness requires reality orientation and stress tolerance without dissociative symptoms.
- Differentiation from dissociative identity disorder and depersonalization disorder is essential for accurate assessment.
- Emotional insight and personality integration are not discharge criteria for fugue but may apply to other dissociative conditions.
A client diagnosed with depersonalization disorder has a short-term outcome that states, “The client will verbalize an alternate way of dealing with stress by day 4.” Which nursing diagnosis reflects the problem that this outcome addresses?
Explanation
Depersonalization disorderis a dissociative condition marked by persistent or recurrent experiences of feeling detached from one’s own body, thoughts, or surroundings. Clients often describe a sense of unreality, emotional numbing, or being an outside observer of themselves. These symptoms are typically triggered by stressor anxiety and may impair the ability to respond adaptively to emotional demands. The disorder does not involve psychosis but reflects a disruption in emotional integration and stress processing, making coping interventions central to care.
Rationale for correct answer
2.The outcome focuses on developing alternative stress responses, which directly addresses ineffective coping. The client’s inability to manage overwhelming anxietyleads to depersonalization, and improving coping strategies is the therapeutic goal.
Rationale for incorrect answers
1.Disturbed sensory perception refers to perceptual distortions like hallucinations, not the emotional detachmentseen in depersonalization. It misclassifies the nature of the symptoms.
3.Self-esteem disturbance involves negative self-evaluation, which is not the primary issue in depersonalization. The client’s challenge is with coping, not self-worth.
4.Anxiety related to repressed trauma may be present, but the outcome targets behavioral coping, not trauma processing. This diagnosis does not align with the stated goal.
Take Home Points
- Depersonalization disorder involves emotional detachment and altered self-perception triggered by stress.
- Ineffective coping is the most appropriate nursing diagnosis when the goal is to improve stress management.
- Symptoms are not psychotic but reflect maladaptive responses to anxiety and emotional overload.
- Differentiation from anxiety disorders, PTSD, and psychotic conditions is essential for accurate care planning.
A client diagnosed with dissociative identity disorder has been hospitalized for 7 days. The client has a nursing diagnosis of ineffective coping R/T repressed severe anxiety. Which outcome would be appropriate?
Explanation
Dissociative identity disorderis a trauma-related psychiatric condition marked by the presence of two or more distinct identity states that alternate in controlling behavior. It is associated with amnesia, emotional dysregulation, and identity fragmentation. Clients often experience impaired coping due to unresolved trauma and internal conflict between alters. In early hospitalization, the focus is on stabilization and development of adaptive copingstrategies to reduce dissociative episodes and promote safety.
Rationale for correct answer
4.Demonstrating an adaptive way to manage stress reflects progress in copingand emotional regulation. It aligns directly with the nursing diagnosis and supports recovery by reducing reliance on dissociation as a defense.
Rationale for incorrect answers
1.Memory recovery is unpredictable and not a realistic short-term goal. It depends on integrationand trauma processing, which typically occur in later phases of treatment.
2.Verbalizing awareness of alters is a long-termtherapeutic milestone. It requires insight and internal cooperation, which are not expected within the first two weeks of hospitalization.
3.Perceiving stimuli accurately is more relevant to psychoticdisorders. DID does not inherently impair sensory perception, making this outcome diagnostically inappropriate.
Take Home Points
- Early outcomes in DID focus on coping, safety, and emotional regulation—not memory recovery or identity integration.
- Adaptive coping reduces dissociative defenses and supports stabilization.
- Insight into alters and memory restoration are long-term goals requiring extended therapy.
- Differentiation from psychotic disorders is essential for accurate outcome planning.
A client diagnosed with dissociative identity disorder attributed to childhood sexual abuse has an outcome that states, “The client will verbalize causative factors for the development of multiple personalities.” Which charting entry would support a successful evaluation of this outcome?
Explanation
Dissociative identity disorderis a trauma-related psychiatric condition marked by the presence of two or more distinct identity states that alternate in controlling behavior. It is strongly associated with childhood abuse, particularly sexual and physical trauma, and involves amnesia, identity fragmentation, and emotional dysregulation. The development of multiple personalities is understood as a defense mechanism to compartmentalize overwhelming experiences. Therapeutic outcomes often focus on helping the client recognize and verbalize the traumatic origins of their dissociation.
Rationale for correct answer
2.Discussing the history of childhood sexual abuse directly reflects causative factorsfor the development of multiple personalities. It shows the client is beginning to connect traumatic experiences with the emergence of dissociative states, fulfilling the stated outcome.
Rationale for incorrect answers
1.Stating the function of each personality reflects insightinto internal dynamics but does not address the origin or cause of their development. It’s relevant but not aligned with the outcome.
3.Being redirected during group therapy reflects engagement, not causative understanding. It indicates behavioral participation, not insight into trauma-related etiology.
4.Understanding that treatment may be lengthy reflects expectation management, not causative awareness. It shows readiness but does not fulfill the outcome’s focus on trauma origins.
Take Home Points
- DID is rooted in severe trauma, especially early childhood abuse, which leads to identity fragmentation.
- Verbalizing trauma history is a key milestone in recognizing the origins of dissociative states.
- Insight into personality function and treatment expectations are important but distinct from causative understanding.
- Differentiating between outcome types—insight, engagement, causation—is essential for accurate charting and evaluation.
The student nurse is learning about dissociative identity disorder. Which student statement indicates that learning has occurred?
Explanation
Dissociative identity disorderis a trauma-related psychiatric condition marked by the presence of two or more distinct identity states that alternate in controlling behavior. These identity states, or alters, often differ in name, affect, and behavior, and may hold separate memories or emotional responses. The switchingbetween identities is typically triggered by stress, and can be sudden or dramatic, reflecting the brain’s adaptive response to overwhelming psychological conflict. The condition is associated with amnesia, emotional dysregulation, and impaired continuity of self.
Rationale for correct answer
2.Sudden and dramatic transitions between identities are characteristic of DID. These switches are often precipitatedby stress or trauma-related triggers, reflecting the disorder’s core mechanismof psychological compartmentalization.
Rationale for incorrect answers
1.While some individuals with DID may experience functional impairment, many maintain occupationaland social roles. This statement overgeneralizes and misrepresents the variability in functioning.
3.DID is no longer classified under Axis II, as the multiaxial system was removed in DSM-5. It is now categorized under dissociative disorders, making this statement outdated.
4.Not all personalities are mutually aware. Amnesiabetween alters is common, and events experienced by one identity may not be accessible to others, contradicting this statement.
Take Home Points
- DID involves distinct identity states with separate memories, behaviors, and emotional responses.
- Switching between identities is often sudden and stress-induced.
- Functional capacity varies widely among individuals with DID.
- Mutual awareness between alters is not universal and memory gaps are common.
A newly admitted client diagnosed with depersonalization disorder has a nursing diagnosis of anxiety R/T family stressors. Which nursing intervention would be most helpful in building a trusting nurse-client relationship?
Explanation
Depersonalization disorderis a dissociative condition marked by persistent or recurrent experiences of feeling detached from one’s own body, thoughts, or surroundings. Clients often describe a sense of unreality, emotional numbing, or being an outside observer of themselves. These symptoms are typically triggered by stress, especially interpersonal or environmental, and may impair emotional regulation and trust in others. Establishing a therapeutic relationship requires consistent reassurance, emotional safety, and validation of the client’s experience.
Rationale for correct answer
4.Reassuring the client of safety and security during anxiety fosters trustand emotional containment. It helps the client feel groundedand supported, which is essential in depersonalization where reality feels distorted.
Rationale for incorrect answers
1.Identifying stressors is an assessmentactivity, not a relational intervention. While useful, it does not directly build trust or emotional safety.
2.Encouraging coping mechanisms is a teachingstrategy. It supports long-term management but does not address the immediate need for relational trust during acute anxiety.
3.Discussing depersonalization episodes may be prematureand overwhelming early in care. It risks retraumatization before trust and emotional safety are established.
Take Home Points
- Depersonalization disorder involves emotional detachment and altered self-perception triggered by stress.
- Building trust requires reassurance, emotional safety, and validation of the client’s experience.
- Assessment and teaching interventions are important but secondary to relational containment in early care.
- Differentiation from psychotic disorders and PTSD is essential for accurate therapeutic engagement.
The nursing student is learning about depersonalization disorder. Which student statement indicates that learning has occurred?
Explanation
Depersonalization disorderis a dissociative condition marked by persistent or recurrent episodes of feeling detached from one’s own thoughts, body, or actions. It involves self-awareness, perceptual distortion, and emotional numbing. Individuals often describe feeling like an outside observer of themselves, with intact reality testing. It typically begins in adolescence and may be triggered by trauma, stress, or substance use. Though transient episodes are common in the general population, the disorder is diagnosed only when symptoms are persistent and impair functioning.
Rationale for correct answer
3.Depersonalization disorder involves a temporary alterationin the sense of self-awareness, where individuals feel detached from their own thoughts or body. This reflects the core diagnostic feature of self-detachment.
Rationale for incorrect answers
1.The term “external environment” refers to derealization, not depersonalization. Depersonalization is centered on the self, not surroundings, making this statement inaccurate.
2.Transient depersonalization episodes are common, not rare. Up to 50–75% of adults report brief experiences, especially under stress, contradicting the claim of rarity.
4.Alterations in perception during depersonalization are typically distressing, not relaxing. They often provoke anxiety and fear of losing control or going insane, making this statement misleading.
Take Home Points
- Depersonalization disorder involves detachment from one’s own thoughts, body, or emotions, with preserved reality testing.
- It differs from derealization, which involves altered perception of the external environment.
- Transient depersonalization episodes are common and not necessarily pathological unless persistent and impairing.
- It must be differentiated from psychotic disorders, where reality testing is impaired, and from anxiety disorders where detachment may be episodic.
A nurse greets a client who had been experiencing delusions of persecution and auditory hallucinations by saying, “Good evening. How are you?” The client, who has been referring to himself as “man,” answers, “The man is bad.” Of what is this an example?
Explanation
Dissociationis a defense mechanism where an individual disconnects from aspects of reality, identity, memory, or consciousness to cope with overwhelming stress or trauma. It is common in psychotic disorders, especially schizophrenia, where identity fragmentationand altered perception of self may occur. Dissociation can manifest as depersonalization, derealization, or identity confusion. In severe cases, individuals may refer to themselves in the third person or adopt alternate identities, reflecting a breakdown in self-integration.
Rationale for correct answer
1.The client’s use of third-person self-reference (“The man is bad”) reflects a disconnectionfrom personal identity, consistent with dissociation. This is often seen in psychotic states where self-boundariesare impaired.
Rationale for incorrect answers
2.Transference involves projecting feelings from past relationships onto the caregiver. The client’s statement does not reflect projectionof past emotions onto the nurse, making this an inaccurate interpretation.
3.Displacement refers to redirecting emotions from a threatening source to a safer one. There is no evidence of emotional redirectionhere; the client is speaking about himself, not shifting blame or emotion.
4.Identification involves adopting traits or behaviors of another person. The client is not mimicking or internalizing another’s identity or traits, so imitationis not evident in this scenario.
Take Home Points
- Dissociation in psychosis may present as third-person self-reference or fragmented identity.
- It differs from transference, which involves emotional projection onto caregivers.
- Displacement redirects emotions to safer targets, not evident in self-referential speech.
- Identification involves adopting traits of others, not merely speaking in third person.
A 35-year-old male was found by the police wandering in a city. He was unable to give information on his home address or other family members. He appeared to be well groomed and was able to converse with others. On examination, there was no medical illness or presence of psychotic symptoms. Urine screening revealed negative results for any psychoactive substances. What is the most likely diagnosis?
Explanation
Dissociative fugueis a rare subtype of dissociative amnesia characterized by sudden travel, identity confusion, and amnesiafor autobiographical information. Individuals may unexpectedly wander away from home or familiar surroundings and are unable to recall their past, including personal identity, family, or residence. Despite this, they often appear well-groomed and can interact socially. Fugue states are typically triggered by severe psychological stress or trauma and are not associated with psychosis, substance use, or neurological illness.
Rationale for correct answer
1.The client’s wandering behavior, inability to recall personal details, and intact grooming and social interaction strongly suggest dissociative fugue, which involves amnesia with traveland preserved general functioning.
Rationale for incorrect answers
2.Dissociative amnesia involves memory loss without travel. The presence of wanderingand disorientation to identity makes this diagnosis incomplete for the scenario.
3.Schizophrenia typically presents with psychoticfeatures such as hallucinations, delusions, or disorganized speech. The absence of these symptoms rules out schizophrenia.
4.Dementia involves progressive cognitive decline, often with poor grooming and impaired social interaction. The client’s intact functioning and age make dementia unlikely.
Take Home Points
- Dissociative fugue involves sudden travel and amnesia for personal identity, often triggered by psychological trauma.
- It differs from dissociative amnesia, which lacks travel or identity confusion.
- Schizophrenia requires psychotic symptoms such as hallucinations or delusions.
- Dementia presents with cognitive decline and impaired daily functioning, not sudden identity loss with preserved grooming.
A nurse is caring for a client who seems to lack spontaneity, has difficulty distinguishing himself from others, and has difficulty distinguishing between internal and external stimuli. The client describes a vague feeling of estrangement. Which statement would describe this client?
Explanation
Depersonalization disorderis a dissociative condition characterized by a persistent or recurrent feeling of detachment from one’s own body, thoughts, or surroundings while reality testing remains intact. It is often triggered by stress, trauma, or anxiety and differs from psychosis because insight is preserved. Clients describe experiences of being unreal, estranged, or outside their body, with symptoms causing marked distressand impairment. Treatment focuses on psychotherapy, stress management, and in some cases pharmacological support for comorbid conditions such as anxietyor depression.
Rationale for correct answer
2.The vague feeling of estrangement, inability to differentiate internal from external stimuli, and lack of spontaneityare consistent with depersonalization disorder. Unlike psychosis, the client recognizes the altered state, showing preserved insight, which confirms this diagnosis.
Rationale for incorrect answers
1.Depression involves low mood, anhedonia, and hopelessness, but the described estrangementand detachment from self point more toward a dissociative condition than primary mood disorder. Antidepressants may help comorbid depression but are not first-line.
3.Electroconvulsive therapy is reserved for severe depressionor treatment-resistant mood disorders, not depersonalization. This client’s presentation lacks vegetative depressive symptoms or severe suicidal risk, making ECT inappropriate.
4.Suicide precautions are necessary when there is evidence of suicidal ideationor intent. While dissociative symptoms can be distressing, the stem does not indicate suicidal risk, so constant precautions are not indicated.
Take Home Points
- Depersonalization disorder is a dissociative disorder marked by persistent detachment from self or environment with intact reality testing.
- It must be differentiated from psychosis, where reality testing is impaired, and from depression, where low mood predominates.
- Stress and trauma are common triggers, and comorbid anxiety or depression frequently coexist.
- Treatment focuses on psychotherapy, coping strategies, and management of associated psychiatric conditions rather than invasive treatments like ECT.
Exams on Dissociative Disorder
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
- Objectives
- Introduction
- Dissociative disorders
- Dissociative amnesia
- Practice Exercise 1
- Dissociative identity disorder
- Depersonalization/derealization disorder
- Practice Exercise 2
- Other specified dissociative disorder
- Nursing interventions across dissociative disorders
- Practice Exercise 3
- Summary
- Comprehensive questions
Notes Highlighting is available once you sign in. Login Here.
Objectives
- By the end of these notes, the learner will be able to define and classify the major dissociative disorders according to established diagnostic frameworks, including key features from the DSM-5.
- The learner will be able to explain the epidemiology, etiology, pathophysiology, and risk factors associated with dissociative disorders in a scientific manner.
- The learner will be able to describe the clinical presentations, diagnostic criteria, and differential diagnoses for each specific dissociative disorder.
- The learner will be able to outline evidence-based assessment techniques, nursing interventions, and treatment approaches tailored to patients with dissociative disorders.
- The learner will be able to identify high-yield nursing insights critical for patient safety, therapeutic communication, and multidisciplinary collaboration in mental health settings.
- The learner will be able to apply knowledge of dissociative disorders to hypothetical clinical scenarios through integrated practice and summaries.
Introduction
- Dissociative disorders represent a complex group of mental health conditions characterized by disruptions in the normal integration of consciousness, memory, identity, emotion, perception, body representation, motor control, and behavior.
- These disorders often emerge as a maladaptive response to overwhelming trauma or stress, leading to a disconnection from one's thoughts, feelings, or sense of self.
- In nursing practice, understanding dissociative disorders is essential because nurses frequently serve as the first point of contact in identifying symptoms, providing supportive care, and facilitating recovery in both inpatient and outpatient settings.
- Scientifically, these disorders are rooted in neurobiological alterations involving brain regions such as the amygdala, hippocampus, and prefrontal cortex, which regulate memory and emotional processing.
- The DSM-5 categorizes dissociative disorders based on the predominant symptoms, emphasizing the need for a thorough differential diagnosis to rule out medical or substance-related causes.
- This introduction sets the foundation for exploring each disorder in detail, highlighting the nurse's role in promoting patient-centered care through empathy, safety, and evidence-based interventions.
Dissociative disorders
- Dissociative disorders encompass a spectrum of conditions where individuals experience a profound disruption in the continuity of their psychological functioning.
- These disruptions can manifest as gaps in memory, altered sense of identity, or detachment from reality, often serving as a psychological defense mechanism against trauma.
- From a nursing perspective, recognizing these disorders early can prevent misdiagnosis and ensure appropriate therapeutic alliances.
1.1 Definition and Classification
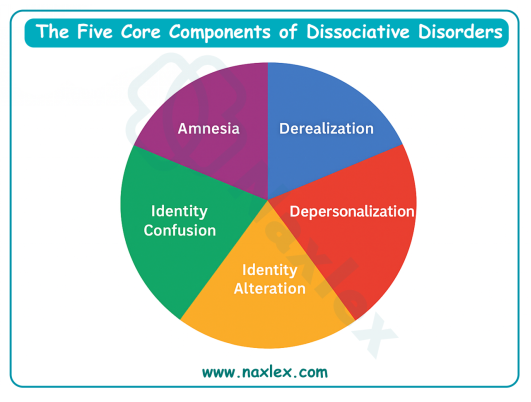
- The definition of dissociative disorders involves involuntary disruptions or discontinuities in the integrated functions of consciousness, memory, identity, or perception of the environment.
- According to diagnostic criteria, these disruptions must cause significant distress or impairment in social, occupational, or other important areas of functioning, and they are not better explained by another mental disorder, substance use, or a medical condition.
- Dissociative disorders are classified into several subtypes based on the primary manifestation of symptoms.
- Dissociative amnesia focuses on memory loss without identity confusion.
- Dissociative identity disorder involves the presence of multiple personality states.
- Depersonalization/derealization disorder centers on feelings of detachment from oneself or surroundings.
- Other specified dissociative disorder captures presentations that do not meet full criteria for the above but still cause clinical distress.
- Classification also considers cultural contexts, as some dissociative experiences may align with normative cultural or religious practices, which must be differentiated from pathological states.
Nursing Insights
- Nurses must recognize that dissociative symptoms can mimic neurological conditions like seizures or head injuries, necessitating a collaborative approach with physicians for comprehensive neuroimaging and laboratory evaluations to rule out organic causes.
1.2 Epidemiology
- Epidemiological data indicate that dissociative disorders are relatively rare in the general population but more prevalent in clinical settings, particularly among individuals with histories of trauma.
- Lifetime prevalence estimates for dissociative identity disorder range from 0.01% to 1%, while depersonalization/derealization disorder affects approximately 1-2% of the population.
- Gender differences show a higher incidence in females for dissociative identity disorder, with a female-to-male ratio of about 9:1, potentially linked to higher rates of reported childhood sexual abuse.
- Age of onset typically occurs in childhood or adolescence, but diagnosis often happens in adulthood due to delayed presentation or misattribution of symptoms.
- Cultural variations exist, with higher reported rates in populations exposed to war, natural disasters, or systemic violence, underscoring the role of environmental stressors.
Comorbidity is common, with up to 80% of individuals with dissociative disorders also meeting criteria for posttraumatic stress disorder (PTSD), major depressive disorder, or substance use disorders.
Nursing Insights
- In nursing assessments, it's crucial to screen for comorbid conditions, as untreated dissociation can exacerbate substance abuse or suicidal ideation.
- Nurses should use validated tools like the Dissociative Experiences Scale (DES) to quantify symptom severity and guide referrals.
1.3 Etiology and Risk Factors
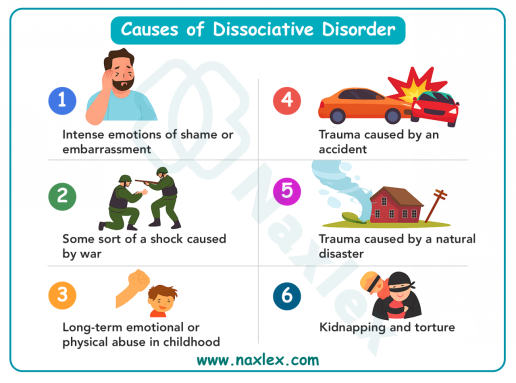
- Etiologically, dissociative disorders are multifactorial, involving an interplay of genetic, neurobiological, psychological, and environmental factors.
- Trauma, especially severe and repeated childhood abuse, is a primary risk factor, with studies showing that 90% of individuals with dissociative identity disorder report histories of physical or sexual abuse.
- Genetic predispositions may involve polymorphisms in genes regulating stress response systems, such as the hypothalamic-pituitary-adrenal (HPA) axis.
- Environmental risk factors include attachment disruptions in early life, leading to insecure attachment styles that impair emotional regulation.
- Psychological models, such as the betrayal trauma theory, posit that dissociation develops as a survival mechanism to preserve relationships with abusive caregivers by compartmentalizing traumatic memories.
- Neuroimaging studies reveal altered connectivity in the default mode network, which is responsible for self-referential processing, in individuals with dissociative disorders.
-
Nursing Insights
- Nurses should prioritize trauma-informed care, avoiding re-traumatization during assessments by using gentle, non-confrontational questioning techniques to build trust and elicit accurate histories.
1.4 Pathophysiology
- Pathophysiologically, dissociative disorders involve dysregulation in brain circuits that integrate sensory, emotional, and cognitive information.
- Hyperactivation of the amygdala during stress can lead to hippocampal atrophy, impairing memory consolidation and retrieval.
- Neurotransmitter imbalances, particularly in serotonin and glutamate systems, contribute to altered states of consciousness.
- Functional MRI studies demonstrate reduced activity in the prefrontal cortex, which normally inhibits emotional responses, resulting in detachment or identity fragmentation.
- Autonomic nervous system dysregulation, including sympathetic overdrive, manifests as physiological symptoms like tachycardia during dissociative episodes.
- Epigenetic changes from chronic stress may alter gene expression in stress-related pathways, perpetuating dissociative vulnerability.
Nursing Insights
Understanding the neurobiological basis empowers nurses to educate patients on how trauma affects the brain, reducing stigma and encouraging adherence to therapies like cognitive behavioral therapy (CBT) that target these pathways.
Dissociative amnesia
- Dissociative amnesia is characterized by an inability to recall important autobiographical information, usually of a traumatic or stressful nature, that is inconsistent with ordinary forgetting.
- This disorder highlights the brain's capacity to selectively block access to memories as a protective mechanism, often resolving spontaneously but requiring nursing support for safety and recovery.
1.1 Definition and Diagnostic Criteria
- Dissociative amnesia is defined as a disruption in memory function where individuals cannot recall episodic memories, typically related to trauma, without evidence of brain injury or substance effects.
- Diagnostic criteria require that the amnesia causes clinically significant distress or impairment and is not attributable to another disorder.
- The memory loss must be retrograde, affecting past events, and not anterograde, which would suggest organic amnesia.
- Specifiers include with or without dissociative fugue, where sudden, unexpected travel occurs with identity confusion.
- Dissociative Fugue: This is a specifier of dissociative amnesia characterized by purposeful travel or bewildered wandering that is associated with amnesia for identity or other important autobiographical information.
The individual may assume a new identity, either partially or completely, and may be unaware of their memory loss until they are "found" or the fugue state ends.
1.2 Subtypes
- Subtypes of dissociative amnesia are delineated based on the extent and nature of memory loss, allowing for tailored nursing interventions.
- Localized amnesia involves failure to recall events from a specific time period, often surrounding a traumatic incident.
- Selective amnesia permits recall of some but not all events from a period, such as remembering a car accident but not the emotional aftermath.
- Generalized amnesia encompasses loss of all personal identity and life history, which is rare and often presents in emergency settings.
- Systematized amnesia targets specific categories of information, like memories of a particular person.
- Continuous amnesia involves ongoing forgetting of new events as they occur, blending with other dissociative features.
1.3 Clinical Features and Presentation
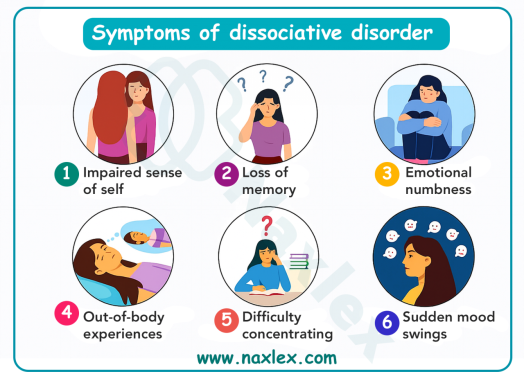
- Clinical features of dissociative amnesia include sudden onset of memory gaps, confusion, and emotional numbness, with patients often appearing bewildered or detached.
- Presentation may involve wandering behaviors in fugue states, where individuals assume new identities temporarily.
- Associated symptoms can include depression, anxiety, or suicidal thoughts due to the distress of lost memories.
- Physical examinations are typically normal, but patients may report headaches or sleep disturbances secondary to underlying stress.
- In chronic cases, interpersonal relationships suffer from repeated episodes, leading to social isolation.
1.4 Differential Diagnosis
- Differential diagnosis for dissociative amnesia requires ruling out neurological conditions such as transient global amnesia, epilepsy, or head trauma through CT scans or EEGs.
- Substance-induced amnesia from alcohol blackouts or benzodiazepines must also be excluded via toxicology screens.
- Psychiatric differentials include PTSD, where flashbacks coexist with amnesia, or somatic symptom disorder if physical complaints predominate.
- Malingering is considered in contexts of legal or financial gain, assessed via inconsistency in self-reports.
Table: Key Differentials for Dissociative Amnesia
|
Condition |
Key Distinguishing Features |
Diagnostic Tools |
|
Transient Global Amnesia |
Sudden onset, resolves within 24 hours, anterograde focus |
MRI to rule out stroke |
|
PTSD |
Intrusive memories and hypervigilance present |
Trauma history and PCL-5 scale |
|
Substance-Induced |
Positive toxicology, history of use |
Urine/blood screens |
|
Malingering |
Inconsistent symptoms, external incentives |
Structured interviews like SIRS |
1.5 Assessment and Nursing Role
- Assessment involves a detailed psychiatric history, focusing on trauma triggers, using tools like the Structured Clinical Interview for DSM-5 Dissociative Disorders (SCID-D).
- The nursing role includes establishing a safe environment, validating patient experiences, and coordinating multidisciplinary evaluations.
- Nurses conduct mental status examinations to assess orientation, memory, and affect.
- Cultural sensitivity is key, as dissociative states may be interpreted differently across cultures.
1.6 Treatment Approaches
- Treatment for dissociative amnesia emphasizes psychotherapy to gently retrieve memories, such as hypnosis or cognitive processing therapy, combined with supportive care.
- Pharmacotherapy is adjunctive, using SSRIs for comorbid anxiety or depression.
- Hospitalization may be needed for fugue states to prevent harm.
- Long-term therapy focuses on building coping skills to prevent recurrence.
Nursing Insights
- Always assess for suicide risk using scales like the Columbia-Suicide Severity Rating Scale (C-SSRS), as amnesia can uncover suppressed traumatic memories leading to acute distress.
- During acute presentations, nurses should ensure patient safety by monitoring for disorientation that could lead to accidents, and document behaviors meticulously to aid in longitudinal care planning.
- Nurses must differentiate dissociative amnesia from malingering or factitious disorder, especially in forensic settings, by observing for inconsistencies in presentation and collaborating with psychologists for structured interviews.
- In administering treatments, nurses monitor for adverse effects of anxiolytics, which can paradoxically worsen dissociation, and educate on grounding techniques like sensory awareness exercises to manage episodes.
Dissociative identity disorder
- Dissociative identity disorder, formerly known as multiple personality disorder, involves the presence of two or more distinct personality states or "alters" that recurrently take control of the individual's behavior, accompanied by amnesia between states.
- This disorder exemplifies extreme fragmentation of identity as a response to severe trauma, requiring long-term nursing involvement for integration and stability.
1.1 Definition and Diagnostic Criteria
- Dissociative identity disorder is defined by the disruption of identity characterized by multiple personality states, each with its own pattern of perceiving, relating to, and thinking about the environment and self.
- Diagnostic criteria include recurrent gaps in recall of everyday events, personal information, or traumatic events, inconsistent with ordinary forgetting.
- The symptoms must cause distress or impairment and not be part of a broadly accepted cultural or religious practice.
- Exclusion of substance use or medical conditions is mandatory.
1.2 Clinical Features and Presentation
- Clinical features include the emergence of alters, which may differ in age, gender, or temperament, leading to inconsistent behaviors.
- Presentation often involves headaches, mood swings, or self-harm attributed to internal conflicts between alters.
- Amnesic barriers prevent awareness of other alters' actions, resulting in "lost time."
- Comorbid symptoms like auditory hallucinations (internal voices of alters) or somatic complaints are common.
Childhood onset is typical, with diagnosis delayed until adulthood.
1.3 Etiology and Development
- Etiology centers on chronic childhood trauma, with the iatrogenic model suggesting that alters develop as fragmented aspects of the self to compartmentalize abuse.
- Development involves failure to integrate personality facets due to overwhelming stress.
- Biological factors include heightened HPA axis sensitivity.
- Psychosocial models highlight disorganized attachment and modeling from suggestive therapies, though trauma remains the core.
1.4 Assessment and Nursing Role
- Assessment utilizes the Dissociative Disorders Interview Schedule (DDIS) to identify alters and amnesic episodes.
- The nursing role encompasses safety planning, therapeutic alliance with all alters, and collaboration with therapists for integration.
- Nurses facilitate group therapy sessions where alters can communicate.
- Monitoring for exploitation or abuse in vulnerable states is critical.
1.5 Treatment Approaches
- Treatment is phased: stabilization to build safety, trauma processing to confront memories, and integration to merge alters.
- Psychotherapy like dialectical behavior therapy (DBT) or eye movement desensitization and reprocessing (EMDR) is primary.
- Medications target comorbidities, such as antipsychotics for hallucinations or mood stabilizers.
Hospitalization during crises prevents self-harm.
1.6 Complications and Prognosis
- Complications include chronic suicidality, substance abuse, and relational instability.
- Prognosis varies; with therapy, many achieve functional integration, though full fusion of alters may take years.
- Poor prognosis factors include untreated comorbidities or ongoing trauma.
Table: Phases of Treatment for Dissociative Identity Disorder
|
Phase |
Goals |
Nursing Interventions |
|
Stabilization |
Safety, coping skills |
Crisis intervention, grounding |
|
Trauma Work |
Process memories |
Support during sessions, monitor distress |
|
Integration |
Merge alters |
Encourage communication, track progress |
Nursing Insights
- When taking histories, nurses should use trauma-sensitive language to avoid triggering switches, focusing on building rapport with the "host" personality first.
- Nurses must be vigilant for subtle switches between alters during interactions, documenting changes in voice, posture, or demeanor to inform therapeutic strategies.
- Nurses administering care must avoid reinforcing alters as separate entities.
- Instead, promote unity by addressing the patient as a whole, which supports integration goals.
Depersonalization/derealization disorder
- Depersonalization/derealization disorder features persistent or recurrent experiences of detachment from one's mental processes or body (depersonalization) or from surroundings (derealization), while reality testing remains intact.
- This disorder underscores the perceptual distortions in dissociation, often chronic and debilitating.
1.1 Definition and Diagnostic Criteria
- The disorder is defined by experiences of unreality, detachment, or being an outside observer of one's thoughts, feelings, sensations, body, or actions.
- Diagnostic criteria require that these experiences are persistent, cause distress, and are not explained by another disorder, substance, or medical condition.
- Reality testing must be preserved, distinguishing it from psychotic disorders.
1.2 Clinical Features and Presentation
- Clinical features include feeling like an automaton, emotional numbing, or viewing the world as foggy or dreamlike.
- Presentation may involve anxiety, depression, or functional impairment in daily activities.
- Episodes can be transient or chronic, lasting months to years.
- Sensory alterations, like distorted time perception, are common.
1.3 Etiology and Risk Factors
- Etiology involves stress or trauma precipitating neurochemical changes, with risk factors including anxiety disorders or cannabis use.
- Brain imaging shows altered insula activity, involved in self-awareness.
- Genetic factors may predispose, with familial patterns in anxiety-related traits.
1.4 Assessment and Nursing Role
- Assessment uses the Cambridge Depersonalization Scale to quantify severity.
- Nursing role includes reassurance that symptoms are not indicative of "going crazy" and promoting grounding techniques.
- Collaborate for ruling out temporal lobe epilepsy via EEG.
1.5 Treatment Approaches
- Treatment includes CBT to challenge distorted perceptions and mindfulness-based therapies.
- Medications like lamotrigine or SSRIs may reduce symptoms.
- Lifestyle interventions focus on stress reduction.
Nursing Insights
- Nurses should assess for the subjective nature of symptoms, as patients remain aware of the unreality, which can help differentiate from delirium.
- In history-taking, nurses should explore precipitating events like panic attacks, as these often trigger onset, guiding preventive education.
- Nurses monitoring treatment should watch for medication side effects that mimic depersonalization, adjusting doses accordingly.
Other specified dissociative disorder
- Other specified dissociative disorder applies to presentations with dissociative symptoms causing distress but not meeting full criteria for other disorders.
- This category ensures clinical attention to atypical cases, emphasizing flexibility in nursing care.
1.1 Definition and Examples
- Defined as dissociative symptoms not fitting elsewhere, examples include chronic mixed dissociative symptoms without identity disruption or acute dissociative reactions to stress lasting less than a month.
- Brainwashing or cult involvement scenarios may fall here.
1.2 Clinical Features
- Features vary but include identity confusion without full alters, trance-like states, or possession experiences in cultural contexts.
- Distress is key, often with impaired functioning.
1.3 Assessment and Nursing Role
- Assessment involves comprehensive interviews to capture nuances.
- Nursing role focuses on validation and referral to specialists.
1.4 Treatment Approaches
- Treatment mirrors other dissociative therapies, adapted to specifics, like brief interventions for acute reactions.
Nursing interventions across dissociative disorders
- Nursing interventions for dissociative disorders are holistic, integrating biological, psychological, and social elements to foster recovery.
- These strategies emphasize patient empowerment and multidisciplinary teamwork.
1.1 Therapeutic Communication Strategies
- Therapeutic communication builds trust through active listening, empathy, and non-judgmental attitudes.
- Use open-ended questions to explore experiences without pressure.
- Avoid challenging dissociative realities abruptly to prevent fragmentation.
- Validate feelings: "It sounds frightening to feel disconnected."
1.2 Safety and Crisis Management
- Safety planning includes environmental modifications to prevent harm during dissociative states.
- Assess for self-harm risks routinely.
- Implement crisis protocols, like one-to-one observation in inpatient settings.
1.3 Pharmacological Considerations
- Pharmacology is supportive, targeting symptoms like anxiety with benzodiazepines cautiously due to dependency risks.
- Monitor for interactions with comorbidities.
Nursing Insights
- Mastering therapeutic communication is vital for de-escalating dissociative episodes.
- Nurses should practice reflective statements to mirror patient emotions accurately.
- Nurses administering psychotropics must educate on adherence and side effects, as non-compliance can exacerbate dissociation.
1.4 Psychotherapeutic Modalities
- Support psychotherapies like trauma-focused CBT or art therapy for expression.
- Group therapy for peer support.
1.5 Patient Education and Family Involvement
- Educate on disorder mechanics using simple analogies, like "dissociation as a mental escape hatch."
- Involve families in therapy to reduce enabling behaviors.
Nursing Insights
- Family education reduces stigma.
- Nurses should facilitate sessions explaining how to respond to episodes without overprotecting.
Summary
- In summary, dissociative disorders encompass a range of conditions involving disruptions in identity, memory, and perception, primarily linked to trauma.
- Key disorders include dissociative amnesia, with its memory gaps; dissociative identity disorder, featuring multiple alters; depersonalization/derealization disorder, marked by detachment; and other specified types for atypical presentations.
- Epidemiologically, they are trauma-associated, with neurobiological underpinnings in stress-response systems.
- Nursing care emphasizes safety, therapeutic communication, and evidence-based interventions like psychotherapy and adjunctive medications.
- High-yield insights highlight trauma-informed approaches, differential diagnosis, and patient empowerment to achieve integration and improved functioning.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Dissociative Disorder
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


