Please set your exam date
Foundation of Pediatric Nursing
Study Questions
Practice Exercise 1
Because injuries are the most common cause of death and disability in children in the United States, which stage of development correctly determines the type of injury that may occur? Select all that apply
Explanation
Injury patterns in childrenvary by developmental stage, reflecting their motor skills, cognitive development, and social behaviors. Understanding these stages helps nurses and caregivers anticipate risks and implement prevention strategies.
Rationale for correct answers:
2.School-age and adolescent children are heavily influenced by peer pressure and the desire for social acceptance.This can lead them to take risky actions, such as accepting dares, engaging in dangerous stunts, or experimenting with unsafe behaviors.
3.Toddlers have increased mobility, they can run, climb, and explore, but have little understanding of safety. This combination makes them prone to burns, falls, and collisions with objects.
5.Infants at the crawling stageexplore their environment orally. This tendency to place objects in their mouths puts them at risk for aspiration and choking.
Rationale for incorrect answers:
1.Newborns cannot roll over intentionally, this skill usually develops around 4–6 months. Falls from rolling are more likely in older infants.
4.Preschoolers may ride tricycles or bikes with training wheels, but a two-wheel bike is usually ridden by older children with better balance and coordination. Reckless riding is more common in later childhood or adolescence.
Take home points
- Injury prevention strategies must be tailored to a child’s developmental stage.
- Mobility without awareness of danger is a major cause of injury in infants and toddlers.
- Peer influence becomes a key risk factor in later childhood and adolescence.
- Nurses and caregivers should educate families on age-specific safety measures to reduce preventable injuries.
The National Children’s Study is the largest prospective, long-term study of children’s health and development in the United States. Which of these options are the goals of this study? Select all that apply
Explanation
The National Children’s Studyaimed to track the effects of environmental, social, genetic, and behavioral factors on children’s health and development from before birth through adulthood. Its primary focus was on generating evidence to guide interventions that improve health outcomes and reduce preventable conditions among U.S. children.
Rationale for correct answers:
B.Improving diet, preventing dental caries, and reducing childhood obesitywere part of the study’s goals, as these issues are significant public health concerns with long-term impacts on physical and mental health.
D.Reducing violence, substance abuse, and mental health disorderswas a major focus, as these are leading contributors to morbidity, mortality, and impaired development among youth.
Rationale for incorrect answers:
A.While immunization is a public healthpriority, it was not a specific goal of the National Children’s Study. Immunization programs are typically addressed through other national initiatives like the CDC’s Vaccines for Children program.
C.School lunch program changeswere not part of the study’s direct goals. The study aimed to inform broad policy and community strategies, not prescribe specific food service requirements.
E.Attendance and graduation ratesare influenced by many social factors, but improving these metrics was not a stated goal of the study. The focus was on health outcomes rather than academic performance targets.
Take home points
- The National Children’s Study sought to understand how multiple factors influence child health over time.
- Diet, oral health, obesity prevention, and reducing behavioral health risks were key objectives.
- The findings were intended to guide evidence-based policies and interventions to improve children’s health nationwide.
A family you are caring for on the pediatric unit asks you about nutrition for their baby. What facts will you want to include in this nutritional information? Select all that apply
Explanation
Nutritional education for familiesshould address both the biological benefits of feeding choices and the social factors that influence children’s eating habits throughout development. Understanding these influences helps caregivers make informed decisions that promote lifelong healthy eating.
Rationale for correct answers:
A.Breastfeedingis the optimal source of nutrition for infants, providing essential micronutrients and immunologic properties that protect against infections and promote healthy growth.
B.Eating preferences and attitudes toward foodare shaped early by family habits, cultural practices, and mealtime patterns, influencing long-term dietary choices.
D.During adolescence, peer influence increases while parental control diminishes.Teens often choose foods based on social acceptance and convenience rather than nutritional value.
Rationale for incorrect answers:
C.Lifelong eating habitsare not firmly established by 18 months. While early experiences matter, preferences and habits continue to develop throughout childhood and adolescence.
E.While some mothers do stop breastfeeding upon returning to work, this is not a universal fact and should not be presented as such. Many continue breastfeeding by expressing milk or adjusting feeding schedules.
Take home points
- Breastfeeding supports infant health through nutrition and immune protection.
- Family and cultural influences are strong determinants of food preferences.
- Adolescence brings greater peer influence on food choices, often at the expense of nutrition.
- Nutritional counseling should address developmental stages and practical strategies for healthy eating at each stage.
A nurse is caring for a toddler in the pediatric unit. What is the overriding goal of atraumatic care?
Explanation
Atraumatic careis a foundational approach in pediatric nursing that aims to minimize or eliminate physical and psychological distress for children and their families during healthcare experiences. It incorporates strategies that reduce or eliminate distress and trauma during hospitalization or treatment, with a focus on preserving the child’s emotional and physical well-being.
Rationale for Correct Answer:
B. The overriding goal of atraumatic careis to do no harm, physically, psychologically, or emotionally, when providing healthcare to infants and children. This principle guides all nursing and medical interventions in pediatrics.
Rationale for Incorrect Answers:
A. Preventing or minimize the child’s separation from the familyis a key principle of atraumatic care, but it is a strategy, not the overriding goal. It helps reduce anxiety and trauma in hospitalized children but supports the broader goal of "do no harm."
C. Offering children and families choices and involvement in caresupports their emotional well-being. However, it is a componentof atraumatic care, not its primary goal.
D. Preventing or minimizing bodily injury and painis a major aspect of atraumatic care and contributes to the goal of doing no harm, but it is not the overarching aim itself.
Take home points
- The core goal of atraumatic care is to prevent or minimize physical and psychological harm to children during healthcare encounters.
- Key principles of atraumatic care include:
- Minimizing separation from caregivers.
- Reducing pain and invasive procedures.
- Supporting emotional and psychological comfort.
- Encouraging family involvement and a sense of control.
A nurse is educating a group of student nurses on childhood mortality. What is the number one cause for mortality among children?
Explanation
Childhood mortalityrefers to the death of children under the age of five, often measured as the under-five mortality rate, the number of deaths per 1,000 live births. It’s a critical indicator of a country’s overall health, development, and access to essential services.
Rationale for Correct Answer:
C. Unintentional injuries, particularly motor vehicle accidents, are the leading cause of death in children over the age of 1 year, especially in the U.S. and other high-income countries. These accidents may involve children as passengers, pedestrians, or cyclists. Despite improvements in vehicle safety and child restraint laws, motor vehicle crashes remain the primary cause of pediatric mortality.
Rationale for Incorrect Answers:
A. While Human immunodeficiency virus(HIV)can lead to child mortality, especially in areas with high prevalence and limited healthcare access, it is not the leading cause globally or in most developed countries. It ranks much lower than injury-related causes.
B. Congenital anomaliesare a leading cause of infant mortality, particularly in the first year of life, but among children over 1 year, they are less common causes of death compared to trauma and accidents.
D. Low birthweightis a major cause of neonatal and infant mortality, especially in preterm births. However, it does not account for most deaths in children beyond infancy.
Take home points
- Motor vehicle accidents are the leading cause of death in children, especially ages 1 and older.
- Prevention strategies include proper use of car seats, seat belts, helmet use, and parental supervision.
- For infants, low birthweight and congenital anomalies are more common causes of mortality.
- Pediatric mortality causes shift with age, from congenital and perinatal issues in infancy to unintentional injuries in later childhood.
A nurse is scheduling a home visit for a toddler with cystic fibrosis discharged 3-days ago. By doing this, the nurse demonstrates which of the following nursing roles?
Explanation
Pediatric nurses wear many hats, all centered around one goal: supporting the health and well-being of children from infancy through adolescence. Their roles are both clinical and emotional, blending technical skill with compassion and advocacy.
Rationale for Correct Answer:
C. The role of a case managerinvolves coordinating care and servicesto ensure that a client’s needs are met effectively and efficiently across different care settings. By scheduling a home visit post-discharge, the nurse is facilitating continuity of care, helping to manage resources, and supporting the family as they transition from hospital to home care.
Rationale for Incorrect Answers:
A. Educator: While education is a vital part of nursing care, especially in chronic illness management, simply scheduling a home visit does not in itself reflect the educator role. It’s a preparatory coordination action, not a teaching moment.
B. Advocacyinvolves supporting the client’s rights and needsby ensuring their voice is heard in care decisions. While case managers often advocate, this action is better classified as care coordination rather than direct advocacy.
D. Direct careimplies hands-on nursing activities, such as administering medications, performing assessments, or providing treatments. Scheduling a visit is an indirect care activity, making this option incorrect.
Take home points
- Case managers coordinate services to promote seamless care transitions, especially for clients with chronic conditions like cystic fibrosis.
- Nurses fulfill multiple roles, but correctly identifying the role depends on the specific activity being performed.
- Home visits play a crucial part in pediatric case management to ensure adherence to care plans, prevent complications, and support family education.
A nurse is caring for a group of pediatric clients. Which of the following actions by the nurse demonstrates their role as a client advocate?
Explanation
Pediatric nurses wear many hats, all centered around one goal: supporting the health and well-being of children from infancy through adolescence. Their roles are both clinical and emotional, blending technical skill with compassion and advocacy.
Rationale for Correct Answer:
D. Advocacyin nursing means acting on behalf of the client’s needs and best interests, especially when the client cannot speak for themselves, as is often the case with infants and children. In this scenario, the nurse identifies that an infant is in distressand takes action to relieve pain by requesting appropriate medical intervention, which is a clear demonstration of advocacy.
Rationale for Incorrect Answers:
A. Administering antibiotics to a child with bacterial meningitis: This reflects the role of a direct care provider, not advocacy. It involves following a provider’s prescription rather than speaking up for an unmet client need.
B. Teaching the caregiver of a child with cystic fibrosis on postural drainage technique: This action is an example of the nurse acting as an educator, not an advocate. The focus is on skill development and health teaching.
C. Using current evidence to choose the most effective vaccine for an infant: This reflects the evidence-based practitionerrole, using research and best practices to guide decisions. It does not involve speaking on behalf of the client.
Take home points
- Client advocacy involves identifying and responding to unmet client needs, especially when the client cannot do so themselves.
- Advocating for pain relief, safety, or equitable treatment is a central nursing responsibility, particularly in pediatrics.
- Nurses advocate by speaking up, requesting changes, or challenging decisions to protect and promote client well-being.
Practice Exercise 2
A 16-year-old patient tells the nurse that they have been sexually active and asks for a pregnancy test. The patient requests that their parents not be informed. What is the nurse's legal and ethical responsibility?
Explanation
Many states have laws that allow minors to consent to reproductive health services, including pregnancy testing, STI testing, and contraception, without parental involvement. Ethically, maintaining confidentiality encourages adolescents to seek timely and appropriate care.
Rationale for correct answer:
C.Providing the requested care while maintaining the patient’s confidentialityrespects the patient’s legal rights (in most states) and supports ethical obligations to maintain confidentiality in reproductive health matters. It also fosters trust, which is essential for ongoing healthcare engagement.
Rationale for incorrect answers:
A.Automatically telling the parentsviolates confidentiality laws in most states and could discourage adolescents from seeking care.
B.Requiring the patient to tell their parentsfirst undermines the patient’s legal right to confidential care where applicable.
D.Refusing the pregnancy test without parental consentis inappropriate if the state allows minors to consent to reproductive health services.
Take home points
- In many states, minors can access reproductive health services confidentially.
- Confidentiality is critical for encouraging adolescents to seek care for sensitive health issues.
- Nurses must know state-specific laws regarding minor consent to provide care that is both legal and ethical.
Which of the following is an example of an emancipated minor?
Explanation
An emancipated minoris a person under the age of majority (usually 18) who is legally recognized as independent from their parents or guardians. This status allows them to make healthcare and other legal decisions without parental consent.
Rationale for correct answer:
B.In most states, minors who are married, enlisted in the military, or have obtained a court order for emancipation are considered legally independent. A 17-year-old who is marriedmeets this legal definition.
Rationale for incorrect answers:
A.Being “mature”does not grant legal emancipation without formal legal status or qualifying conditions.
C.Having a part-time jobdoes not make a minor legally emancipated; parental consent is still required for most decisions.
D.At 18, the person is legally an adultand no longer considered a minor hence emancipation status is irrelevant.
Take home points
- Emancipated minors can make their own legal and healthcare decisions without parental involvement.
- Common pathways to emancipation include marriage, military service, parenthood, or a court order.
- Nurses must be aware of state laws to correctly determine a patient’s legal decision-making rights.
The parents of two school-age children state that they expect their children to adhere to their rules without question and that they make all the decisions. Which type of parenting style does this reflect?
Explanation
Parenting styles are psychological frameworksthat describe how parents interact with their children, especially in terms of discipline, communication, warmth, and expectations. These styles profoundly influence a child’s emotional development, behavior, and long-term outcomes.
Rationale for correct answer:
A. Authoritarian: Parents set rigid rules, expect unquestioned obedience, and often rely on punishment rather than positive reinforcement. Communication is typically one-way, from parent to child, with little regard for the child’s opinions or feelings.
Rationale for incorrect answers:
B. Democratic: Involves mutual respect, open communication, and joint decision-making between parent and child. This is not consistent with the “rules without question” approach.
C. Authoritative: Combines high expectations with warmth, responsiveness, and support. Parents set clear rules but also explain reasoning and encourage input.
D. Permissive: Parents are lenient, set few boundaries, and often avoid confrontation, allowing children significant freedom. This is the opposite of strict, unquestioned rule enforcement.
Take home points
- Authoritarian parenting is strict, rule-focused, and demands obedience without input from the child.
- Authoritative parenting, though sometimes confused with authoritarian, emphasizes structure with warmth and communication.
- Parenting style influences children’s self-esteem, social skills, and decision-making abilities well into adulthood.
A single mother asks the nurse for suggestions on disciplining her 2-year-old son. Which suggestion would be most appropriate?
Explanation
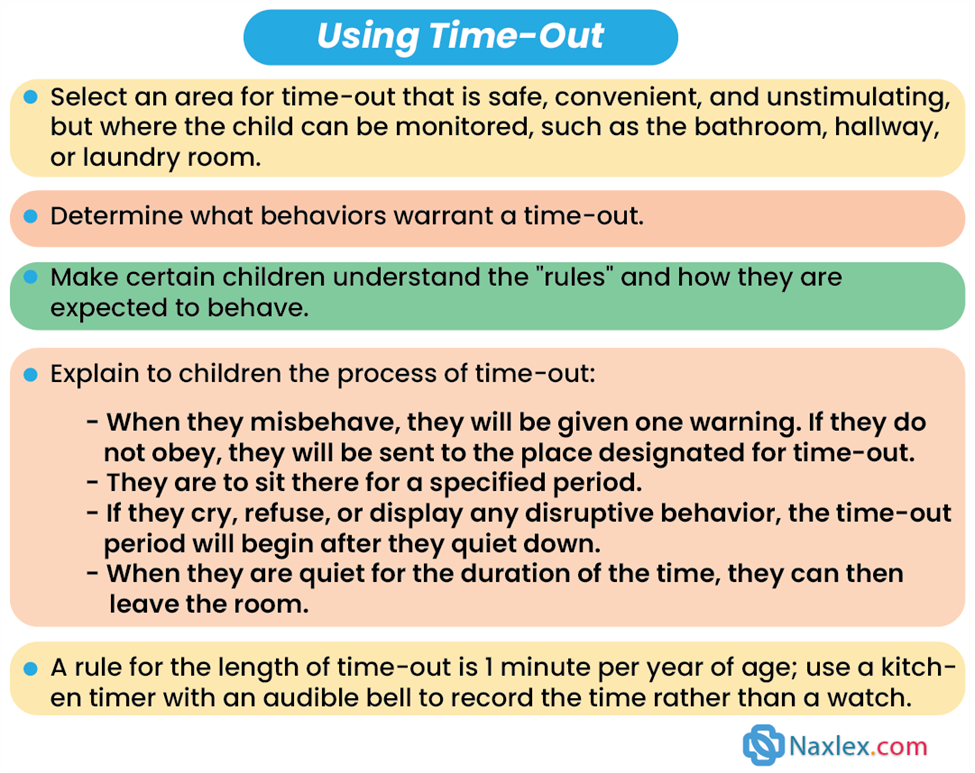
For toddlers, discipline should be immediate, consistent, and age-appropriate. Time-outs are effective when they are brief, about 1 minute per year of age, allowing the child to connect the consequence with the behavior.
Rationale for correct answer:
C. Have the child spend 2 minutes in time-out: This approach is developmentally appropriate for a 2-year-old. The short duration matches their attention span and ensures the consequence is directly linked to the behavior, promoting learning without excessive frustration.
Rationale for incorrect answers:
A. Emphasizing the inappropriate behavior: This can unintentionally reinforce the behavior by giving it extra attention rather than redirecting the child toward acceptable actions.
B. Waiting an hour before enforcing discipline: Delaying discipline prevents the toddler from associating the consequence with the behavior, reducing its effectiveness.
D. Withholding a privilege for a week: This is too long for a toddler to understand or remember the connection between the behavior and the consequence.
Take home points
- Discipline for toddlers should be immediate, consistent, and brief.
- A good rule of thumb for time-outs is 1 minute per year of age.
- Positive reinforcement of desired behaviors should be used alongside discipline to encourage learning and cooperation.
The nurse is teaching a group of students about the possible effects of immigration on the health status of children. Which response by the group would indicate the need for additional teaching?
Explanation
Children of immigrantsare young individuals, typically under age 18, who live in families where at least one parent was born outside the country of residence. This group includes both foreign-born childrenwho immigrated themselves and U.S.-born children(or native-born in other countries) whose parents are immigrants.
Rationale for correct answer:
A.Children of immigrants are more likely to experience reduced access to preventive healthcare services compared to non-immigrant peers. Factors such as financial constraints, cultural differences, and systemic barrierslimit their healthcare utilization.
Rationale for incorrect answers:
B.Limited involvement in activities due to language barriersis accurate since difficulty communicating can prevent participation in school, sports, and community programs.
C.Lack of adequate support systemsis correct. Immigrant families may be separated from extended family and have limited local networks.
D.Increased stressors due to relocationis correct since adjustment to a new country can involve cultural adaptation stress, financial strain, and uncertainty about the future.
Take home points
- Immigrant children often face reduced access to preventive care, not improved access.
- Language, cultural, and financial barriers can affect healthcare, education, and social integration.
- Nurses should advocate for culturally competent care and connect families to community resources to bridge gaps in access.
When caring for an adolescent, in which case must the nurse share information with the parents no matter which state the care is provided in?
Explanation
Notifiable diseasesare specific communicable diseases that must be reported to public health authorities when diagnosed. This is usually mandated by law or regulation.
Rationale for correct answer:
D. Tuberculosisis a reportable infectious disease under public health laws nationwide. Notification ensures appropriate treatment, contact tracing, and prevention of community spread. This legal obligation overrides patient confidentiality for minors in this case.
Rationale for incorrect answers:
A. In many states, minors can receive pregnancy-related counselingand care without mandatory parental notification, depending on state laws.
B. Mental health treatment, for conditions such as depression, for minors can often occur confidentially, though laws vary by state. Parental involvement may be encouraged but is not universally required.
C. Many states allow minors to access contraceptionwithout parental consent, especially in federally funded clinics under Title X.
Take home points
- Reportable diseases like TB require disclosure to parents and public health officials, regardless of the patient’s age.
- Confidentiality laws for minors vary by state, but public health safety takes precedence for communicable diseases.
- Nurses must be familiar with both state-specific minor consent laws and federal public health reporting requirements
A nurse is caring for a 14-year-old client who was admitted for dehydration from nausea and vomiting.
The client is ready for discharge and says to the nurse, “I will tell you something, but you can’t tell anyone.” Which nursing action is most appropriate?
Explanation
When working with adolescents, nurses should encourage open communication while being honest about the limits of confidentiality.This builds trust while ensuring legal and ethical responsibilities are met, especially if the information involves potential harm to the client or others.
Rationale for correct answer:
B.This response maintains therapeutic rapportand clearly explains that confidentiality will be upheld unless the disclosure indicates harm to self or others, or involves situations requiring mandatory reporting such as abuse and certain communicable diseases.
Rationale for incorrect answers:
A.Promising unconditional confidentialityis inappropriate and unethical because nurses are legally obligated to report threats to safety.
C.Limiting disclosure to “only the physician”is misleading, as certain information may also need to be shared with other members of the healthcare team or authorities.
D.Referring the client directly to a social workerwithout first hearing the concern may damage trust and rapport, and it does not address the nurse’s duty to listen and assess the situation.
Take home points
- Nurses should always clarify the limits of confidentiality before a client shares sensitive information.
- Mandatory reporting laws override confidentiality in situations involving harm, abuse, or certain public health risks.
- Establishing trust with adolescents requires balancing openness with professional responsibility.
Comprehensive Questions
The new graduate nurse on the pediatric unit is concerned about maintaining a professional distance in her relationship with a client and the client’s family. Which comment indicates that she needs more mentoring regarding her patient-nurse relationship?
Explanation
The patient-nurse relationshipis a professional and therapeutic bond built on trust, communication, empathy, and mutual respect. It forms the foundation of effective nursing care and plays a vital role in promoting patient well-being, safety, and satisfaction.
Rationale for correct answer:
A. This reflects a boundary violationand indicates a lack of understanding about maintaining professional distance.While developing rapport and trust with pediatric patients and their families is essential, visiting patients outside of work hours blurs the professional boundaries and may lead to emotional overinvolvement.
Rationale for incorrect answers:
B. This response demonstrates professional boundary-setting. Explaining nurse-patient assignment processes maintains transparencyand avoids creating unrealistic expectations or dependency.
C. Offering polite but limited personal informationis an appropriate way to maintain professionalism and focus the relationship on the patient’s needs.
D. Participating in multidisciplinary rounds and listening to family concernsis a key component of holistic pediatric care. It reflects professional engagement without crossing boundaries.
Take home points
- Nurses must maintain professional boundaries even in emotionally charged settings like pediatrics.
- Overinvolvement, such as visiting patients outside of scheduled work hours, compromises professional judgment and objectivity.
- Effective nurses show empathy and support while keeping the relationship centered on the patient’s care, not personal attachment.
Mentoring new nurses about emotional boundaries is critical for preventing burnout and preserving therapeutic integrity.
The nurse is assessing the vital signs of a child who is being evaluated in an urgent care center. The child is to be seen by the pediatric nurse practitioner (PNP). The mother asks, “Why is my child seeing the PNP and not the doctor?” What is the best response by the nurse?
Explanation
Therapeutic communicationis a purposeful, goal-directed form of interaction used by healthcare professionals, especially nurses, to support a patient’s emotional, psychological, and physical well-being. It’s not just about exchanging information; it’s about building trust, understanding, and a healing connection.
Rationale for correct answer:
D. This provides an accurate, respectful, and informative explanationof the pediatric nurse practitioner (PNP) role. It reassures the parent while emphasizing the PNP’s specialized training and qualificationsin pediatric care. Nurse practitioners are advanced practice registered nurses (APRNs)who have completed graduate-level education and are licensed to assess, diagnose, treat, and manage health conditions.
Rationale for incorrect answers:
A. This statement is misleading. While both PNPs and PAs are advanced providers, they follow different educational and licensure pathways, and the comparison may not clarify the PNP’s unique role in pediatric care.
B. This response dismisses the parent's questionand undermines the PNP’s qualifications. It may also create unnecessary doubt about the provider’s competence.
C. This statement is vague and fails to explain the PNP’s role or qualifications, potentially causing more confusion or concern.
Take home points
- Pediatric Nurse Practitioners (PNPs) are highly trained in child health and capable of independently managing most pediatric conditions.
- When parents have questions about healthcare roles, clear and respectful education builds trust and understanding.
- Effective communication enhances family satisfaction and promotes confidence in the care team.
A 3-year-old Native American child is admitted to the pediatric unit for emergency surgery. Which of the following questions should the nurse include when taking the admission history from the child’s parents?
Explanation
Culturally-sensitive healthcareis an approach that recognizes, respects, and responds to the diverse cultural backgrounds, beliefs, values, and practices of patients. It’s about seeing each person as a unique individual, not just a diagnosis, and tailoring care in a way that honors their identity and lived experience.
Rationale for correct answer:
C. Asking whether the family has consulted a tribal healer demonstrates cultural sensitivity and acknowledges the importance of traditional healing practicesin many Native American communities. It encourages open dialogue about cultural beliefs and complementary health practices, which may be important in the child’s care planning and acceptance of medical interventions.
Rationale for incorrect answers:
A. “Does your Indian tribe believe in immunizing children?” This question is stereotypical and generalized, implying all Native American tribes think alike. It can be perceived as judgmental or culturally insensitive.
B. “Do you attend Native American powwows with the family?” While this may reflect cultural participation, it’s not relevant to the clinical context or the child’s current healthcare needs.
D. “What herbal remedies have you given your child today?” Although it's appropriate to ask about herbal remedies, the phrasing may feel accusatory or presumptive. A better approach would be: “Are there any traditional or herbal treatments you’ve used to help with your child’s symptoms?”
Take home points
- Cultural competence involves asking respectful, relevant, and open-ended questions about traditional beliefs and practices.
- Avoid assumptions and stereotypes about cultural groups.
- Including cultural practices in health assessments helps provide holistic and family-centered care.
The parents of an infant have just been informed by the infant’s primary health-care provider that their child has an aggressive form of cancer. The parents have previously communicated that they are Jewish. Which of the following statements would be appropriate for the nurse to make? “It is often comforting for parents of very sick children to:
Explanation
Therapeutic communicationis a purposeful, goal-directed form of interaction used by healthcare professionals, especially nurses, to support a patient’s emotional, psychological, and physical well-being. It’s not just about exchanging information; it’s about building trust, understanding, and a healing connection.
Rationale for correct answer:
A. This response reflects cultural and religious sensitivity. Since the parents have identified as Jewish, suggesting that they may find comfort in speaking with a rabbi, a recognized spiritual leader in Judaism, is appropriate and supportive. It acknowledges their faith and offers a relevant source of emotional and spiritual support without imposing beliefs or practices from other religions.
Rationale for incorrect answers:
B. This reflects Christian teachings, which may not align with the Jewish faith. Suggesting religious texts from another religion is inappropriate and potentially disrespectful in this context.
C. Refers to Christian worship practices. Jewish families typically worship in a synagogue, not a church, so this suggestion is inaccurate and culturally insensitive.
D. A mosqueis a place of worship in Islam, not Judaism. This suggestion is irrelevant to the family's stated beliefs and should be avoided.
Take home points
- Spiritual care should be based on the client’s or family’s stated religious or cultural background.
- Nurses should use respectful, inclusive language and avoid imposing or assuming religious practices.
- Offering to connect families with faith-specific support can provide meaningful comfort during crisis or grief.
Which would the nurse identify as a protective factor for youth violence?
Explanation
Youth violencerefers to harmful behaviors, ranging from bullying and physical fights to severe assaults and homicide, committed by individuals typically aged 10 to 29.
Rationale for correct answer:
D.Commitment to academic performanceis associated with positive self-esteem, goal setting, and involvement in constructive activities, all of which help shield youth from engaging in violence.
Rationale for incorrect answers:
A.Exposure to family violenceis a risk factor, not a protective factor. It increases the likelihood of behavioral problems and normalization of aggression.
B.Limited involvement in social activitiesreduces opportunities for positive peer connections and is linked to isolation, which can increase vulnerability to negative influences.
C.Inconsistency of parental supportis a risk factor, as stable, supportive parenting is essential for emotional regulation and resilience.
Take home points
- Protective factors for youth violence include academic engagement, positive peer relationships, strong family support, and involvement in pro-social activities.
- Risk factors often involve exposure to violence, poor social integration, and lack of supportive structures.
- Nurses play a role in identifying at-risk youth and promoting programs that strengthen protective factors.
In an effort to control health care costs, what is the best recommendation by the nurse?
Explanation
Primary preventionfocuses on avoiding disease or injury before it occurs, which is the most effective way to reduce long-term healthcare costs. Regular check-ups, screenings, immunizations, and health education help detect problems early and prevent costly complications.
Rationale for correct answer:
C.Encouraging primary preventionreduces the need for expensive emergency care or advanced treatment. It also promotes long-term wellness through early detection, health education, and risk reduction strategies.
Rationale for incorrect answers:
A.While comparing insurance planscan save money, it does not directly address controlling healthcare costs through improved health outcomes.
B.Obtaining employer-based insurancemay reduce personal costs but does not address the overall goal of reducing healthcare expenditures through prevention.
D.Avoiding care until illness occursoften leads to higher costs due to delayed diagnosis and more intensive treatments.
Take home points
- Primary prevention is the cornerstone of reducing healthcare costs and improving population health.
- Regular check-ups, immunizations, and health screenings prevent disease progression and complications.
- Nurses are key advocates for preventive care education and community health promotion.
The nurse notes in a toddler’s medical record that the child was adopted internationally at 1 week of age. The child has been diagnosed with a terminal autosomal dominant genetic disease. Which of the following statements would be appropriate for the nurse to make?
Explanation
Therapeutic communicationis a purposeful, goal-directed form of interaction used by healthcare professionals, especially nurses, to support a patient’s emotional, psychological, and physical well-being. It’s not just about exchanging information; it’s about building trust, understanding, and a healing connection.
Rationale for correct answer:
D. This response is respectful, supportive, and nonjudgmental. It provides the adoptive parents with access to important information and professional support, without making assumptions or implying blame. A genetic counselorcan help explain the disease, inheritance patterns, potential treatments, and prognosis in a way that empowers the parents.
Rationale for incorrect answers:
A. “I will provide you with a referral for a meeting with a genetic counselor regarding your pregnancy risks.”This is not relevant, as the parents did not give birth to the child and do not face pregnancy-related risksfrom an adopted child's genetic disease.
B. “It is very important that the mother be notified of the baby’s genetic condition.”This may be impractical or impossiblein international adoption cases. It is not the nurse’s roleto suggest contacting biological parents unless required by policy or law, and the child is already in the care of adoptive parents.
C. “What a shame that you adopted a sick child rather than a healthy child.”This statement is insensitive, inappropriate, and unethical. It implies regret or blame and fails to support the parents who are now caring for a child with a serious illness.
Take home points
- Genetic counseling is a valuable tool for adoptive parents to understand inherited conditions.
- Nurses should offer compassionate, unbiased support and avoid assumptions about biological ties or intentions.
- Communication should focus on available resources and family-centered care, not on judgment or blame.
A second grader enters the school nurse’s office crying and states, “I feel sick. My belly hurts.” The nurse replies, “I’ll call your mommy or daddy to pick you up.” The child replies, “I don’t have a mommy, I have 2 daddies.” Which of the following comments by the nurse is appropriate?
Explanation
Therapeutic communicationis a purposeful, goal-directed form of interaction used by healthcare professionals, especially nurses, to support a patient’s emotional, psychological, and physical well-being. It’s not just about exchanging information; it’s about building trust, understanding, and a healing connection.
Rationale for correct answer:
C. This statement is affirming, inclusive, and respectfulof the child’s family structure. It acknowledges and accepts the child's correction without judgment or assumptions. By using the child’s language, the nurse builds trust and communicates acceptance in a way that is supportive and age-appropriate.
Rationale for incorrect answers:
A. “That’s right. I forgot that your parents are gay.”This response is inappropriate and overly focused on the parents' sexual orientation, which is irrelevant to the current concern (the child feeling ill). It may also come across as labeling or stigmatizing.
B. “Of course you have a mommy. You just don’t live with your mommy.”This is invalidating and dismissive of the child’s statement. It imposes a heteronormative assumptionthat every child has a mother in their life, which may not be true or helpful in this situation.
D. “It must be interesting to live with two men and no women in the house.”This is intrusive and inappropriate, introducing a personal opinion or judgment. It is not relevant to the child’s health complaint and may make the child feel uncomfortable or judged.
Take home points
- Respect the family structure that a child identifies, without imposing assumptions.
- Use the child’s own language when referring to their family to promote trust and inclusivity.
- Nurses must ensure nonjudgmental, affirming communication that supports the emotional and physical well-being of all children, regardless of family background.
A 10-year-old Hindu child who has just been diagnosed with diabetes is admitted to the pediatric clinical unit. The nurse is counseling the parents and child regarding the child’s dietary needs. Which of the following statements by the nurse would be appropriate?
Explanation
Culturally-sensitive healthcareis an approach that recognizes, respects, and responds to the diverse cultural backgrounds, beliefs, values, and practices of patients. It’s about seeing each person as a unique individual, not just a diagnosis, and tailoring care in a way that honors their identity and lived experience.
Rationale for correct answer:
C. This statement is respectful, culturally sensitive, and patient-centered. It shows the nurse is seeking to understand the family's specific dietary practices before providing education. Many individuals of the Hindu faith may follow vegetarian or vegan diets, but dietary practices can vary widely.
Rationale for incorrect answers:
A. “It is very important for you to eat protein at each meal. Meat is an excellent source of protein.”This ignores the possibility that the family may be vegetarian or vegan, as is common in many Hindu households. Recommending meat without understanding cultural or dietary restrictions is culturally insensitive.
B. “I understand that you do not usually eat fruit, but because you are diabetic, it will be essential for you to eat fruit.”Diabetics must monitor carbohydrate intake, including fruit sugars. Assuming the child doesn't eat fruit and suggesting it is essential is inaccurate and dismissive of potential cultural or medical nuances.
D. “Diabetes is a very serious illness. It may be necessary for you to consume foods that you are unaccustomed to eating.”This statement is threatening and dismissiveof cultural practices. Effective diabetic care can be achieved within the boundaries of most dietary restrictionswith appropriate planning.
Take home points
- Cultural sensitivity is critical in dietary counseling, especially in chronic conditions like diabetes.
- Ask open, respectful questions to understand the client's beliefs and practices.
Adapt medical recommendations to the client’s lifestyle and preferences for better adherence and outcomes.
The nurse is preparing a class for a group of students about homeless children and families. Which of the following factors contribute to homelessness? Select all that apply
Explanation
Homelessness among children and familiesis often the result of economic hardship, lack of affordable housing, inadequate support systems, and family instability. Understanding these contributing factors helps guide prevention and intervention strategies.
Rationale for correct answers:
B. Job loss: Loss of employment reduces a family’s ability to pay for housing, utilities, and basic needs, making homelessness more likely.
C. Exposure to abuse or neglect: Children and families fleeing unsafe home environments, such as domestic violence or severe neglect, may have no stable housing options.
D. Cutbacks in public welfare programs: Reduced funding for housing assistance, mental health care, and income support increases vulnerability to homelessness.
Rationale for incorrect answers:
A. Increase in family income: This reduces, rather than increases, the risk of homelessness.
E. Development of community crisis centers: These provide temporary assistance, shelter, and resources, which help prevent or alleviate homelessness, not cause it.
Take home points
- Key drivers of homelessness include financial instability, unsafe home environments, and inadequate social safety nets.
- Prevention requires both economic supports and protection from abuse or neglect.
- Nurses can connect families to housing resources, social services, and community programs to reduce homelessness risk.
The school nurse is planning a screening program. What items should be included to address issues related to the “new morbidity”?
Explanation
The term “new morbidity”refers to the shift in pediatric health concerns from primarily infectious diseases to psychosocial, behavioral, and developmental issues that significantly affect children’s well-being and school performance.
Rationale for correct answer:
A.Academic problems, exposure to violence, and mental health concerns, such as anxiety, depression, and ADHD are central to the concept of the new morbidity. Screening for these issues allows for early identification and intervention to support overall health and development.
Rationale for incorrect answers:
B.While knowing the number of children with chronic illnessis important for school health planning, it does not specifically address the psychosocial and behavioral focus of the new morbidity.
C.Health insurance statisticsmay be relevant for resource allocation but are not a direct focus of the new morbidity concept.
D.HIV, asthma, and allergy testingaddress physical health conditions but not the behavioral, social, and emotional aspects central to new morbidity.
Take home points
- The “new morbidity” emphasizes psychosocial, behavioral, and developmental challenges as major determinants of child health.
- School screening programs should include mental health, academic performance, and violence exposure assessments.
Early detection and school-based interventions can reduce the long-term impact of these issues on children’s lives.
A nurse is caring for a 6-year-old client from a Jewish family. Which of the following practices are most likely observed in this community?
Explanation
Culturally-sensitive healthcareis an approach that recognizes, respects, and responds to the diverse cultural backgrounds, beliefs, values, and practices of patients. It’s about seeing each person as a unique individual, not just a diagnosis, and tailoring care in a way that honors their identity and lived experience.
Rationale for correct answer:
B. Jewish families typically observe religious and cultural practicessuch as Bris (Brit Milah), a religious circumcision ceremony performed on male infants on the 8th day of life. Kosher dietis food prepared according to Jewish dietary laws, including restrictions on certain animal products, the separation of meat and dairy, and specific methods of slaughter.
Rationale for incorrect answers:
A. Ramadhan fastingis an Islamic practice, observed by Muslims during the month of Ramadan. It is not a Jewish tradition.
C. While Jewish individuals may attend synagogue, the term "temple worship" is more often associated with Hindu practices.
D. Halal guidelinesgovern the permissible foods in Islam, not Judaism. Jewish dietary laws are referred to as kosher, not halal.
Take home points
- Always consider religious and cultural beliefs when planning care, especially in pediatrics where family customs heavily influence decisions.
- Jewish practices may include circumcision (bris), observing Sabbath rules, and adhering to kosher dietary laws.
- Providing culturally sensitive care means being accurate and respectful of the family's specific background and beliefs.
A nurse in the pediatric unit is caring for a child with pneumonia. Which of the following nursing actions demonstrate family-centered care? Select all that apply
Explanation
Family-centered careis a holistic approach to healthcare that emphasizes collaboration between healthcare providers, patients, and their families. It recognizes that families are essential partners in a child’s health and healing, not just visitors or bystanders.
Rationale for correct answers:
B. Asking the parents about their child’s usual bedtime routinerespects the family’s knowledge of their child and supports continuity of care, a key principle of family-centered care.
C. Educating the parents about the child’s conditionensures that the family is informed and empowers them to actively participate in the child’s care and make informed decisions.
E. Encouraging parents to participate in comfort measurespromotes parental involvement, strengthens bonding, and helps reduce the child's anxiety—core goals of family-centered care.
Rationale for incorrect answers:
A. Limiting parental visitation to reduce the risk of infectioncontradicts family-centered care, which emphasizes family presenceas essential for the child’s emotional and psychological well-being. Standard infection precautions should be used instead.
D. Ignoring or avoiding a child’s concernscan increase fear and anxiety. Age-appropriate, honest communication is important, even when discussing difficult topics.
Take home points
- Family-centered care involves including families in decision-making, routines, and comfort measures.
- Respecting family roles, empowering them with education, and maintaining open communication are essential.
- Partnership with families is a cornerstone of high-quality pediatric nursing care.
A nurse is caring for a 3-month-old infant newly diagnosed with hydrocephalus. The caregiver is concerned and states, “I'm afraid my baby will never be normal.” Which of the following is the most therapeutic response by the nurse?
Explanation
Therapeutic communicationis a purposeful, goal-directed form of interaction used by healthcare professionals, especially nurses, to support a patient’s emotional, psychological, and physical well-being. It’s not just about exchanging information; it’s about building trust, understanding, and a healing connection.
Rationale for correct answer:
C. This uses therapeutic communication by acknowledging the caregiver’s emotions without judgment and encouraging open expression. It reflects empathy, provides emotional support, and helps build trust between the nurse and caregiver.
Rationale for incorrect answers:
A. “Many children with hydrocephalus live completely normal lives, so don’t worry.”While reassuring, this dismisses the caregiver’s valid emotionsand may feel minimizing. It avoids addressing the caregiver’s actual fears and doesn’t invite further discussion.
B. “Why do you think your child will never be normal again.”This can feel confrontationaland may imply that the caregiver's feelings are irrational or need justification, which can shut down communication.
D. “You should trust the neurosurgeon since they are good at what they’re doing.”This redirects the concern to another professional and avoids providing emotional supportor addressing the caregiver’s feelings directly.
Take home points
- Use open-ended, empathetic communication when caregivers express fear or distress.
- Avoid reassurance without support, judgmental tones, or minimizing the caregiver’s concerns.
- Therapeutic communication helps caregivers feel heard, supported, and more confident in coping with their child’s condition.
A nurse is teaching a school-aged child newly diagnosed with type 1 diabetes mellitus about insulin administration. Which of the following therapeutic communication techniques would be most appropriate?
Explanation
Therapeutic communicationis a purposeful, goal-directed form of interaction used by healthcare professionals, especially nurses, to support a patient’s emotional, psychological, and physical well-being. It’s not just about exchanging information; it’s about building trust, understanding, and a healing connection.
Rationale for correct answer:
A. This employs developmentally appropriate communicationfor a school-aged child. Using visual and hands-on tools like a dollhelps the child understand the procedure in a non-threatening way. This approach encourages engagement, reduces anxiety, and enhances learning.
Rationale for incorrect answers:
B. Explaining insulin administration using detailed medical terminology is not appropriate for a child. School-aged children need simple, concrete language, not complex or abstract medical terms.
C. Avoiding the topic may increase fear or misunderstanding. Children benefit from preparation and reassurance using age-appropriate methods.
D. Telling the child not to be afraid since they will get used to the injections quicklydismisses the child's feelingsand does not validate their fear or promote discussion. Therapeutic communication should acknowledge and address emotions.
Take home points
- Use developmentally appropriate teaching tools, such as dolls, pictures, or role-play, with children.
- Validate and address feelings rather than dismissing them.
- Provide simple, clear explanations to support understanding and reduce anxiety.
- Effective therapeutic communication builds trust, understanding, and cooperation.
Exams on Foundation of Pediatric Nursing
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
- Describe the historical and contemporary perspectives of pediatric nursing.
- Identify key health concerns and challenges affecting children in the United States.
- Apply principles of family-centered and atraumatic care in clinical practice.
- Utilize the nursing process and clinical reasoning to develop comprehensive care plans for children.
- Analyze the impact of social, cultural, and family factors on a child's health and development.
- Discuss ethical and legal issues relevant to pediatric nursing practice, including informed consent and confidentiality.
- Demonstrate an understanding of evidence-based practices in pediatric care.
Introduction
- Pediatric nursing is a specialized field of nursing that focuses on the care of infants, children, and adolescents.
- It is a unique discipline that requires nurses to not only possess clinical expertise but also to understand the developmental, psychological, and social needs of their young patients.
- A pediatric nurse's role extends beyond the child to include the family, as they are a crucial component of the child's health and well-being.
- This module provides a comprehensive overview of the foundational principles that underpin pediatric nursing, from historical context to contemporary practice standards.
Perspectives Of Pediatric Nursing
Health Care for Children
The health of children is a national priority. The National Children’s Study (NCS) was a large-scale, long-term study designed to examine the effects of environmental influences on the health and development of children from before birth until age 21. While the original study was halted, its goals and findings have influenced subsequent research efforts aimed at understanding the complex factors impacting child health.
Health Promotion is a critical aspect of pediatric nursing. It involves empowering children and their families to increase control over and improve their health. Key areas of focus include:
- Development: Monitoring developmental milestones is essential. Nurses use standardized tools like the Denver Developmental Screening Test to assess a child’s progress in fine and gross motor skills, language, and social development.
- Nutrition: Proper nutrition is vital for growth and development. Nurses educate parents on breastfeeding, formula feeding, introduction of solid foods, and healthy eating habits to prevent malnutrition and obesity.
- Oral Health: Dental care should begin in infancy. Nurses advise parents on the importance of cleaning an infant's gums, the timing of the first dental visit, and the prevention of dental caries, which are a major childhood health problem.
Childhood Health Problems remain a significant concern in the United States:
- Obesity and Type 2 Diabetes: In 2018, the CDC reported that approximately 13.7 million children and adolescents aged 2-19 years were obese. The rate of childhood obesity has nearly tripled since the 1970s. This has led to a rise in Type 2 diabetes among children, a condition once almost exclusively seen in adults.
- Childhood Injuries: Injuries are the leading cause of death in children over the age of 1. These include unintentional injuries such as drowning, burns, falls, and motor vehicle accidents, as well as intentional injuries like abuse. Nurses play a key role in injury prevention education.
- Violence: Exposure to violence, whether in the home, community, or through media, can have a profound impact on a child's physical and mental health.
- Mental Health Problems: A 2018 study found that 1 in 5 children aged 3-17 had a mental, emotional, developmental, or behavioral disorder. Conditions like anxiety and depression are increasingly recognized in pediatric populations.
- Infant Mortality: The infant mortality rate is a key indicator of a nation's health. In 2019, the U.S. infant mortality rate was 5.6 deaths per 1,000 live births. It is higher than in many other developed countries, with significant racial and ethnic disparities.
- Childhood Mortality: After infancy, the leading causes of death are unintentional injuries, followed by homicide, suicide, and cancer.
- Childhood Morbidity: Illness and disability in childhood, such as asthma, poverty-related diseases, and chronic conditions, impact a child's quality of life and future health.
- In child health, "new morbidity" refers to the shift in major pediatric health concerns from mostly acute infectious diseases (which were the leading causes of illness and death decades ago) to a range of behavioral, developmental, psychosocial, and chronic health issues that now affect children’s functioning and well-being. It’s called new not because these problems never existed before, but because they have become more prominent as traditional childhood killers (like measles or polio) have been largely controlled through immunization, sanitation, and better medical care.
Examples of “new morbidity” in children include:
- Behavioral disorders (e.g., ADHD, conduct disorders)
- Developmental delays (speech, motor, learning disabilities)
- Mental health problems (childhood depression, anxiety, substance use)
- Psychosocial stressors (family breakdown, exposure to violence, bullying)
- Chronic illnesses with psychosocial impact (asthma, obesity, diabetes)
- School performance problems
- Risk-taking behaviors in adolescents
Nursing Insight: The new morbidity emphasizes that pediatric care must go beyond treating infections and injuries, it must also address emotional health, development, learning, and social functioning. Pediatricians and nurses are encouraged to screen for and intervene early in these areas to prevent long-term consequences.
Access to Healthcare is a major determinant of child health. Nurses must be aware of the Barriers to Healthcare that families face, including:
- Lack of health insurance or underinsurance.
- Geographic location (rural areas with limited access to specialists).
- Cultural and language differences.
- Financial constraints.
- Lack of transportation.
The Art of Pediatric Nursing
The "art" of pediatric nursing is the compassionate and humanistic side of care.
Philosophy of Care:
- Family-Centered Care: This philosophy recognizes the family as the constant in a child’s life. It involves a partnership between nurses, parents, and children, respecting the family’s values and expertise. Core principles include treating families with dignity and respect, sharing information in a timely and unbiased way, and encouraging family participation in decision-making.
- Atraumatic Care: This approach aims to eliminate or minimize the psychological and physical distress experienced by children and their families in the healthcare system. Strategies include preparing the child for procedures, providing choices when possible, using distraction techniques, and minimizing physical restraints. This approach not only improves the child's hospital experience but can also prevent the development of long-term medical fears and anxieties.
Role of the Pediatric Nurse: The pediatric nurse's role is multifaceted and includes:
- Caregiver: Providing direct, hands-on care.
- Advocate: Speaking up for the child's and family's needs and rights.
- Educator: Teaching families about health, illness, and care.
- Manager: Coordinating care and resources.
- Collaborator: Working with other healthcare professionals.
- Researcher: Participating in or using research to improve practice.
Research and Evidence-Based Practice (EBP) are crucial for providing high-quality care. EBP involves integrating the best available research evidence with clinical expertise and patient values to make informed decisions about patient care.
Nursing Insight: The nurse's role extends beyond providing direct care to becoming a family-centered advocate and educator. This means the nurse must prioritize listening to and collaborating with families, respecting their values and cultural beliefs, and providing education that empowers them to make informed healthcare decisions. The nurse's success is measured by the entire family unit's well-being, not just the child's physical recovery.
Clinical Reasoning and the Process of Providing Nursing Care to Children and Families
Clinical reasoning is the cognitive process that nurses use to analyze patient data and make judgments about patient care. In pediatrics, this process is adapted to the child's developmental stage and family context.
The Nursing Process is a systematic, five-step framework for providing care:
- Assessment: Gathering subjective and objective data about the child and family. This includes a health history, physical examination, and psychosocial assessment.
- Diagnosis: Analyzing the assessment data to formulate nursing diagnoses.
- Planning: Developing an individualized plan of care with goals and interventions.
- Implementation: Carrying out the planned interventions.
- Evaluation: Determining the effectiveness of the interventions and modifying the plan as needed.
Quality Outcome Measures are used to evaluate the effectiveness of nursing care and improve patient safety. Examples include hospital-acquired infection rates, readmission rates, and patient satisfaction scores.
Social, Cultural, Religious, And Family Influences On Child Health Promotion
General Concepts
- Definition of Family: The concept of "family" has evolved beyond the traditional nuclear family. A family can be defined as two or more individuals who are joined together by marriage, blood, adoption, or mutual commitment and who assume responsibility for each other.
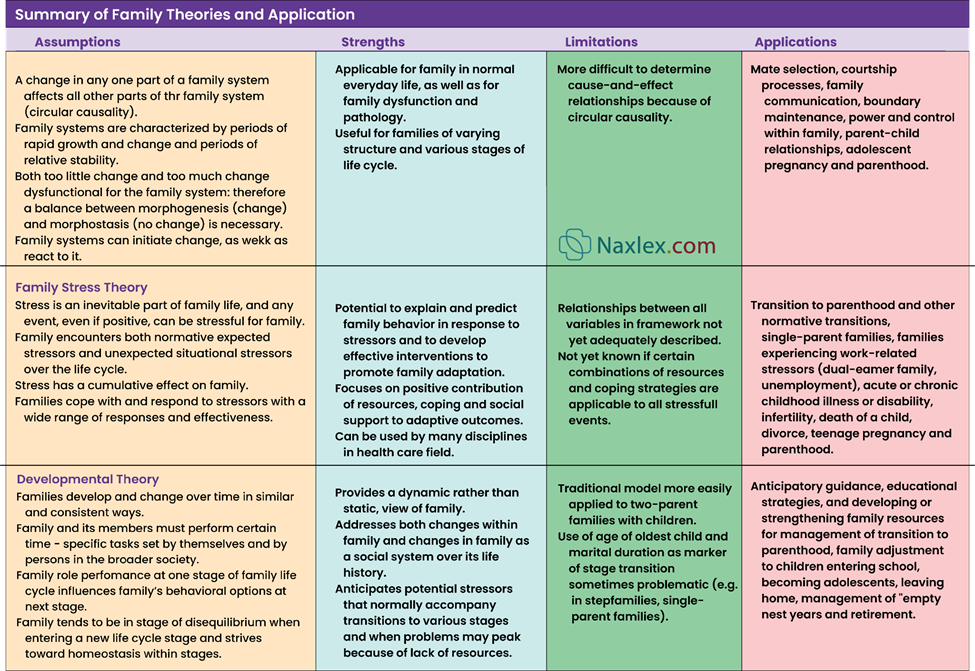
- Family Theories: Family systems theory views the family as a whole system where each member's actions affect the others. Developmental theory focuses on the developmental stages a family goes through over its life cycle.
Family Structure and Function
- Family Structure: Can include nuclear, extended, single-parent, blended, and same-sex parent families. The structure of the family impacts the resources and support available to the child.
- Family Strengths and Functioning Style: Strong families often demonstrate clear communication, mutual respect, adaptability, and resilience.
Family Roles and Relationship
- Parental Roles: Include nurturing, disciplining, and providing for the child. These roles can be shared or divided.
- Role Learning: Children learn social roles and behaviors by observing and imitating their parents and other family members.
Parenting
- Parenting Styles:
- Authoritarian: High control, low warmth. Parents expect obedience and provide little explanation.
- Authoritative: High control, high warmth. Parents set clear limits but are also responsive and provide explanations. This style is often associated with the most positive child outcomes.
- Permissive: Low control, high warmth. Parents are nurturing but provide few rules or limits.
- Neglectful: Low control, low warmth. Parents are uninvolved and provide little emotional support.
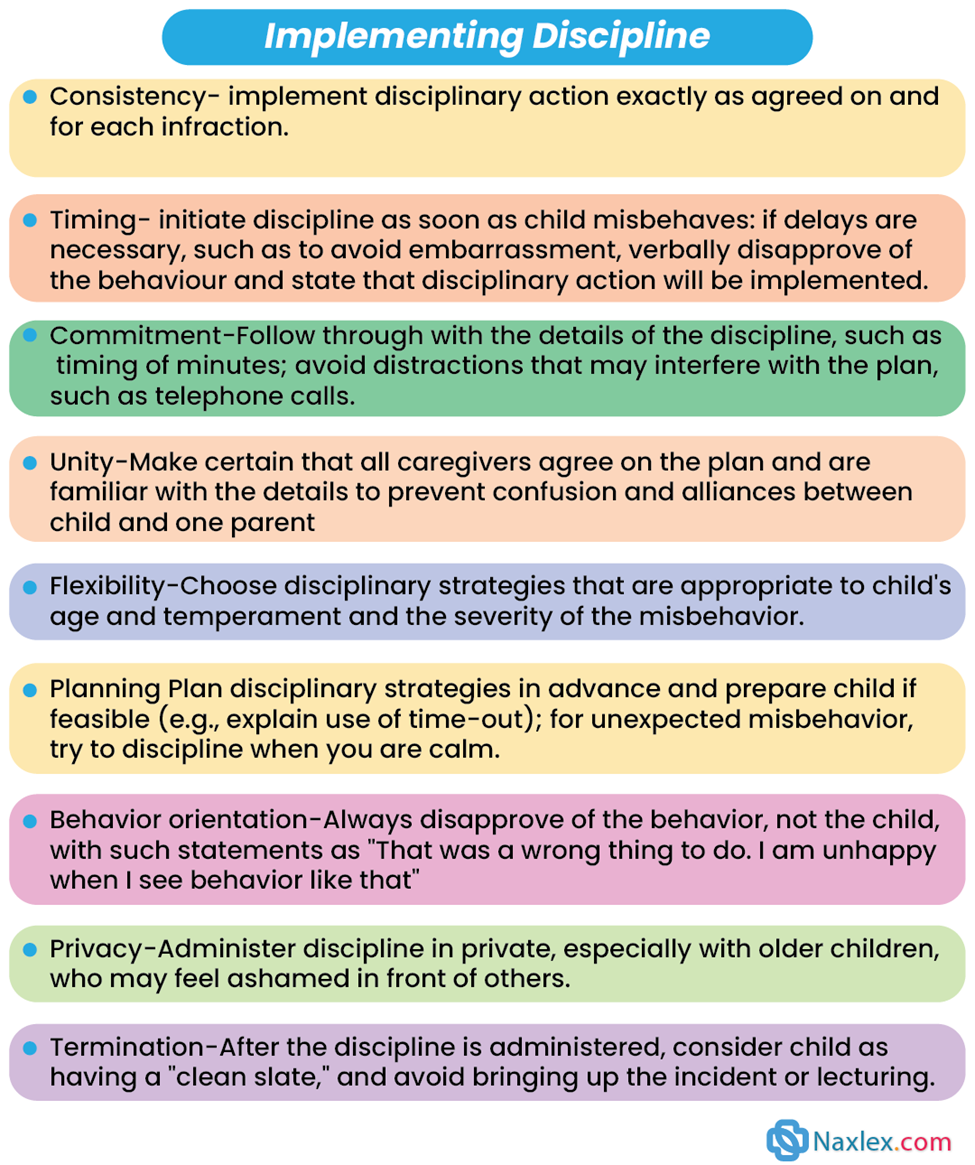
- Limit Setting and Discipline: Discipline involves teaching children self-control and responsibility. Limit setting is about establishing clear boundaries. Nurses can educate parents on age-appropriate discipline techniques.
Special Parenting Situations
- Parenting the Adopted Child: Requires sensitivity to the child's feelings about their birth family and a focus on building a secure attachment.
- Parenting and Divorce: Children may experience feelings of loss and instability. Nurses can provide support and resources to help families navigate this transition.
- Single Parenting: Single parents may face unique challenges, including financial strain and balancing work and childcare.
- Parenting in Reconstituted Families (stepfamilies): Requires time and patience for all members to adjust to new roles and relationships.
- Parenting in Dual-Earner Families: Balancing work and family life can be a source of stress.
- Foster Parenting: These parents care for children who have been removed from their biological homes. They require special training and support to address the child's emotional and developmental needs.
Sociocultural Influences on Children and Families
Culture, race, and ethnicity profoundly impact a child’s health beliefs and practices. Nurses must understand these influences to provide culturally sensitive care. The major religions practiced in the U.S. include:
- Christianity: The largest religious group. Practices vary widely but may include beliefs about prayer, healing, and end-of-life care.
- Judaism: Observant Jews may have dietary laws (kosher), observe the Sabbath, and have specific beliefs about birth and death rituals.
- Islam: Muslims may have specific dietary practices (halal), observe prayer times, and have specific beliefs about modesty and gender roles in healthcare.
- Hinduism: Believers may be vegetarian, have beliefs about reincarnation, and have specific rituals related to birth and death.
Influences in the Surrounding Environment
- School Communities: School health programs provide immunizations, screenings, and health education. School connectedness, a feeling of belonging at school, has been linked to positive health outcomes.
- Schools: The school environment is a primary setting for a child's socialization and learning.
- Peer Cultures: Peer relationships become increasingly important during childhood and adolescence, influencing behaviors and attitudes.
- Community: The community provides resources such as parks, libraries, and healthcare facilities that support child health.
Broader Influences on Child Health
- Social Media and Mass Media: Can influence body image, social relationships, and exposure to misinformation.
- Race and Ethnicity: There are significant health disparities among racial and ethnic groups. For example, a 2019 report by the CDC found that Black women had an infant mortality rate of 10.8 deaths per 1,000 live births, more than double the rate for white women (4.6 per 1,000).
- Social Class: Poverty is a significant risk factor for poor health outcomes. Children in poverty are more likely to experience chronic diseases, malnutrition, and limited access to care. In 2021, the U.S. Census Bureau reported that 15.3% of children under 18 lived in poverty.
- Land of Origin and Immigration Status: Immigrant children may face unique health challenges, including language barriers, cultural adjustment issues, and a lack of familiarity with the U.S. healthcare system.
- Religion/Spiritual Identity: A child’s spiritual beliefs can provide a source of comfort and resilience.
- Cultural Humility and Health Care Providers’ Contribution: Nurses must practice cultural humility, a commitment to a lifelong process of self-reflection and self-critique. This involves acknowledging one's own biases and actively learning from patients from different cultural backgrounds.
Ethical And Legal Issues Related To Caring For Children
Ethical Issues Related to Working with Children and Their Families
Ethical dilemmas in pediatrics often involve balancing the child’s best interests with the parents’ rights and beliefs. Examples include:
- Informed Consent: The ethical duty to ensure a person understands the risks and benefits of a procedure before agreeing to it.
- Parental Refusal of Medical Treatment: When parents refuse a life-saving treatment for their child based on religious or personal beliefs. This can lead to court intervention.
- Confidentiality: Maintaining patient privacy, especially with adolescents.
- Allocation of Scarce Resources: Deciding which child receives a limited resource like an organ transplant.
Legal Issues Related to Working with Children and Their Families
- Informed Consent: Legally, parents or legal guardians must provide informed consent for their child’s medical care.
- Special Situations to Informed Consent:
- Mature Minor Doctrine: In some states, adolescents who can demonstrate the capacity to understand and make a decision may be considered "mature minors" and can consent to their own care.
- Emancipated Minor: A minor who is legally recognized as an adult and can consent to their own care. Conditions for emancipation include marriage, joining the armed forces, or court order.
- Exceptions to Parental Consent Requirement: In emergencies, treatment can be provided without parental consent if delaying care would endanger the child's life or health. Laws also allow minors to seek care for certain conditions (e.g., STIs, pregnancy, substance abuse) without parental consent.
- Parental Refusal of Medical Treatment: If a parent's refusal of treatment is deemed a form of neglect and could lead to significant harm or death, the hospital can seek a court order to override the parental decision.
- Assent: Assent is the ethical principle of involving a child in the decision-making process, even if they cannot legally consent. It means the child agrees to a procedure or treatment. Nurses must ensure the child’s assent is obtained in a way that is developmentally appropriate.
- Advance Directives: Legal documents like a living will or a durable power of attorney for healthcare can be used for adolescents to state their wishes for end-of-life care.
- Confidentiality Issues in Caring for Children: While parents have a right to know about their child's health, adolescents also have a right to confidentiality, especially regarding sensitive issues.
- Exceptions to Confidential Treatment in Children: Nurses are mandated reporters. If a child discloses abuse, neglect, or harm to self or others, the nurse is legally and ethically obligated to report it to the appropriate authorities, which overrides confidentiality.
- Nursing Insight: The nurse must have a deep understanding of concepts like informed consent, assent, and the exceptions to parental consent (e.g., mature minor doctrine, emancipated minor, emergency situations). The ethical and legal duty to report suspected abuse or neglect (mandated reporting) is also paramount and overrides confidentiality. This requires the nurse to be not only a skilled caregiver but also a knowledgeable professional who can navigate these challenging situations while always protecting the child's safety and well-being.
Summary
- Pediatric nursing is a specialized and rewarding field that requires a unique blend of clinical skill, developmental knowledge, and compassionate care.
- The foundation of this practice is a deep respect for the child and their family, emphasizing family-centered and atraumatic care.
- Pediatric nurses must be adept at using the nursing process and clinical reasoning to address the myriad health challenges facing children today, including obesity, injuries, and mental health issues.
- A comprehensive understanding of social, cultural, and family influences is paramount to providing culturally sensitive care and addressing health disparities.
- Nurses must be aware of various parenting styles, family structures, and cultural beliefs to effectively advocate for their patients.
- Navigating the ethical and legal landscape of pediatric care, from informed consent and assent to confidentiality and mandated reporting, is a core competency for all pediatric nurses.
- By integrating these foundational principles, nurses can ensure they provide the highest quality of care to the youngest and most vulnerable members of society.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Foundation of Pediatric Nursing
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


