Please set your exam date
The Menstrual Cycle
Study Questions
Practice Exercise 1
What is the average duration of a typical menstrual cycle?
Explanation
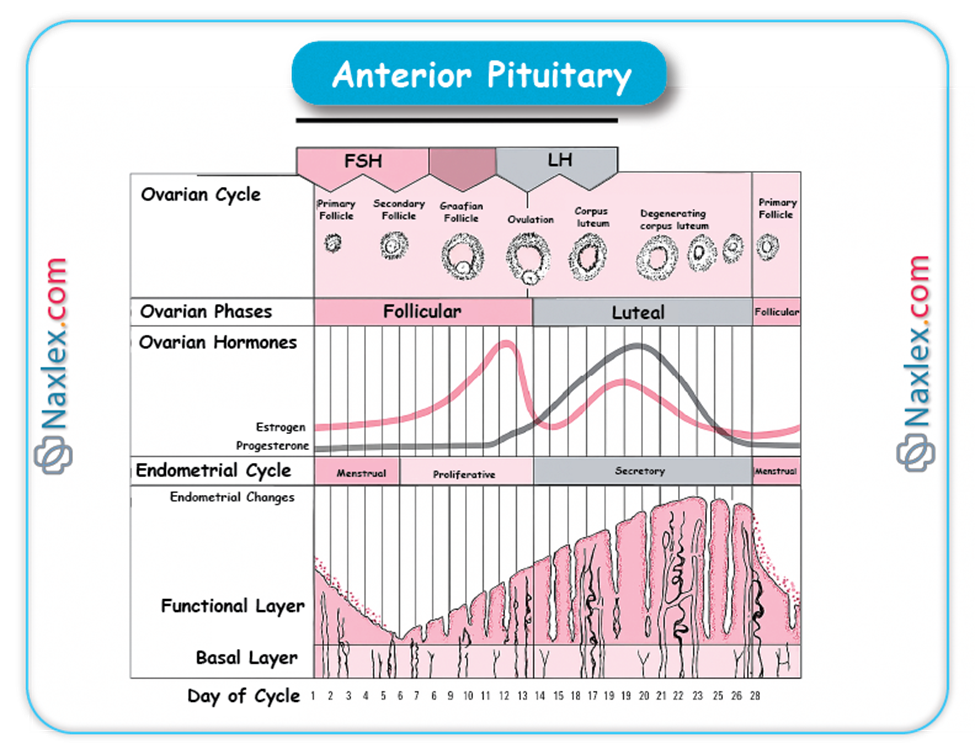
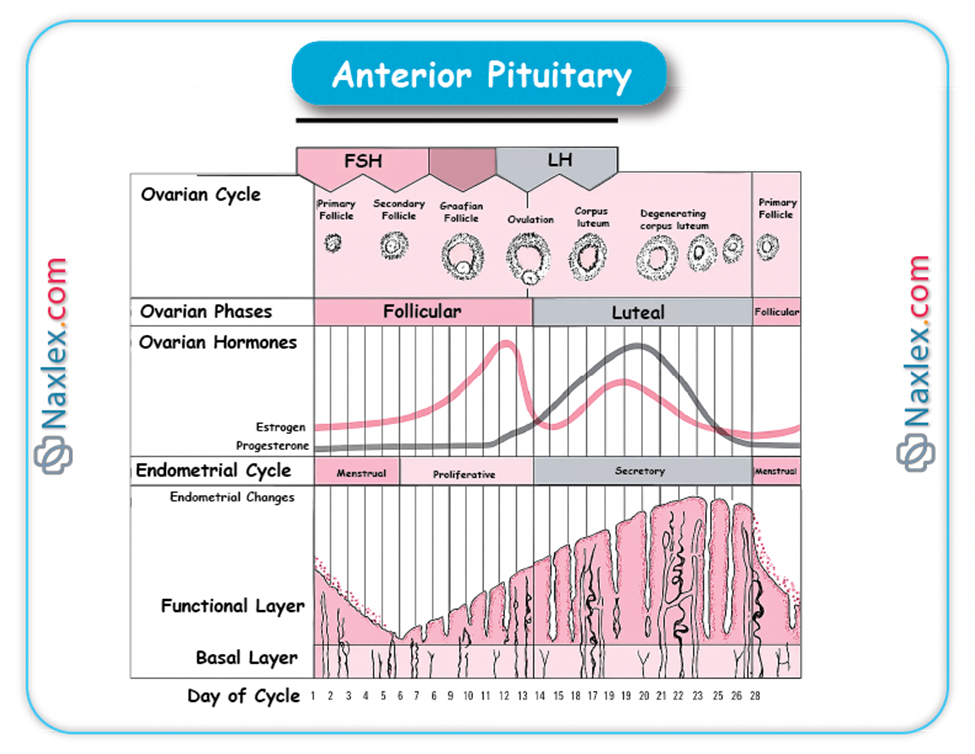
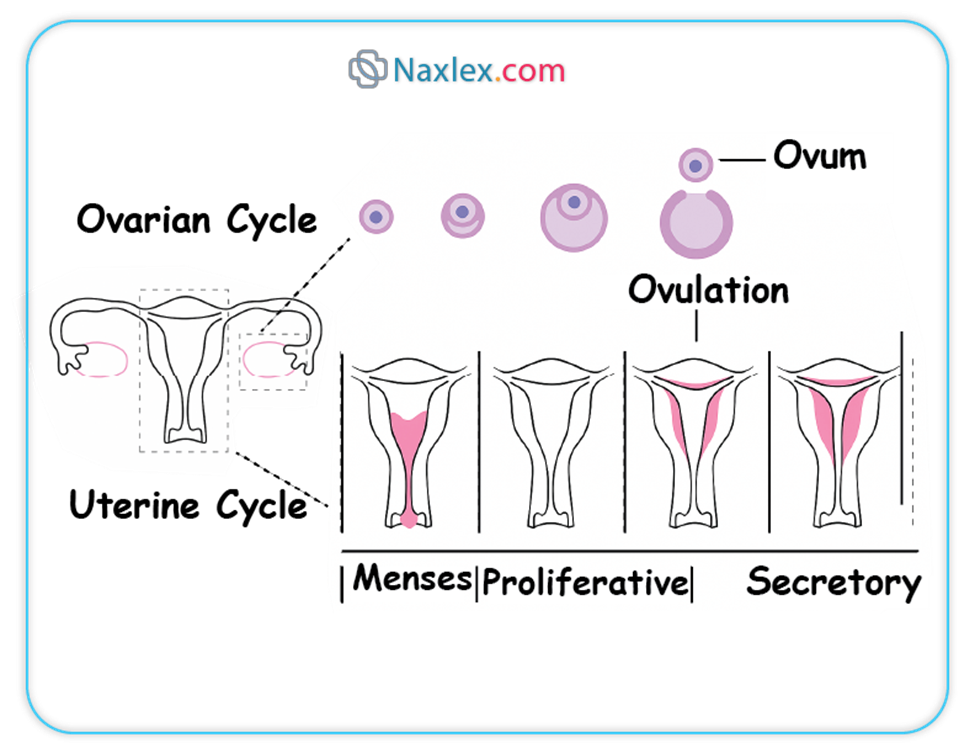
Menstrual cycle is a recurring cycle of physiological changes in females of reproductive age, driven by hormonal fluctuations. The cycle prepares the uterus for the possibility of pregnancy. The average length is 28 days, with a normal range of 21–35 days. Key phases include the follicular phase, leading to ovulation around day 14, and the luteal phase, where the corpus luteum forms. Hormones like estrogen and progesterone regulate this process, ensuring a receptive uterine lining, the endometrium, for implantation.
Rationale for correct answers
B. The normal duration of a typical menstrual cycle is between 21 and 35 days. This range accounts for individual variations and is considered physiologically normal. A cycle lasting less than 21 days is termed polymenorrhea, while one lasting longer than 35 days is oligomenorrhea.
Rationale for incorrect answers
A. A menstrual cycle of 14–21 days is shorter than the typical average and falls outside the normal range for most women. This condition is known as polymenorrhea and can be caused by various factors, including hormonal imbalances, stress, or underlying medical conditions. While it occurs, it is not considered the average duration.
C. A cycle of 35–45 days is longer than the normal range. This is known as oligomenorrhea and can be caused by hormonal disturbances, such as polycystic ovary syndrome (PCOS), or other endocrine disorders. While it can occur in some individuals, it is not representative of the average cycle duration.
D. A menstrual cycle lasting 45–60 days is significantly longer than the normal range and is indicative of oligomenorrhea or amenorrhea. This prolonged cycle length often suggests significant hormonal dysfunction or anovulation. It is not a typical duration for a healthy, regular menstrual cycle.
Take home points
- The normal menstrual cycle duration is 21 to 35 days.
- Polymenorrhea is a cycle lasting less than 21 days.
- Oligomenorrhea is a cycle lasting longer than 35 days.
- The menstrual cycle is regulated by hormones like estrogen and progesterone.
Which hormone stimulates the growth of ovarian follicles during the follicular phase?
Explanation
Follicular phase is the first phase of the menstrual cycle, characterized by the growth of ovarian follicles. This phase begins on the first day of menses and ends with ovulation. The duration is approximately 14 days, though it can vary. The pituitary gland releases follicle-stimulating hormone and luteinizing hormone, with FSH being dominant early on, promoting the development of several follicles. One dominant follicle is selected to mature fully.
Rationale for correct answers
B. Follicle-stimulating hormone (FSH) is released by the anterior pituitary gland and directly stimulates the growth and development of ovarian follicles. During the follicular phase, FSH levels are elevated, acting on granulosa cells within the follicles to promote their proliferation and the synthesis of estrogen. This specific action is what drives the maturation of the follicles.
Rationale for incorrect answers
A. Luteinizing hormone (LH) is primarily responsible for triggering ovulation, not the initial growth of the follicles. While LH is present during the follicular phase and acts synergistically with FSH to promote estrogen synthesis, its levels surge around day 14 of a typical cycle, leading to the rupture of the dominant follicle and the release of the oocyte. This LH surge is a key event marking the end of the follicular phase and the beginning of ovulation.
C. Progesterone is the dominant hormone of the luteal phase, which occurs after ovulation. Its main function is to prepare the uterine lining for implantation by increasing its vascularity and glandular secretions. It is secreted by the corpus luteum, the remnants of the ruptured follicle, and its levels are low during the follicular phase, making it incorrect as the stimulus for follicular growth.
D. Estrogen is produced by the growing follicles in response to FSH stimulation, not the other way around. Estrogen levels rise progressively during the follicular phase, and this increasing concentration has several effects, including the proliferation of the uterine endometrium and a positive feedback loop on FSH secretion, which eventually leads to the LH surge. Therefore, estrogen is a product of follicular growth, not its primary stimulant.
Take home points
- FSH is the primary driver of ovarian follicle growth.
- The LH surge triggers ovulation.
- Estrogen is produced by the growing follicles.
- Progesterone is the dominant hormone of the luteal phase.
What triggers the LH surge that leads to ovulation?
Explanation
Ovulation is the release of a mature oocyte from the dominant ovarian follicle. It occurs around day 14 of a typical 28-day menstrual cycle. This process is triggered by a sudden surge in luteinizing hormone (LH). The event is critical for conception, as the ovulated oocyte has a limited lifespan of about 12-24 hours. The entire process is a result of a complex interplay between the hypothalamus, pituitary gland, and ovaries, involving both positive and negative feedback loops.
Rationale for correct answers
B. High estrogen levels from the dominant follicle are the primary trigger for the LH surge. As the follicle matures during the follicular phase, it secretes increasing amounts of estrogen. When estrogen levels remain elevated for an extended period, they switch from a negative to a positive feedback mechanism on the hypothalamus and pituitary gland, leading to a massive release of GnRH and subsequently, LH.
Rationale for incorrect answers
A. Progesterone levels are low during the follicular phase, with a normal range of 0.1 to 0.7 ng/mL. It is produced in significant amounts by the corpus luteum after ovulation. Its primary role is to prepare the uterine lining for implantation and maintain pregnancy, and its rise is a consequence of the LH surge, not the cause. Therefore, high progesterone levels do not trigger the LH surge.
C. Follicle-stimulating hormone (FSH) levels are not low when the LH surge is triggered. In fact, there is a small, but significant, concurrent surge of FSH that is also caused by the high estrogen levels. The LH surge and this FSH surge both contribute to the final maturation of the oocyte and the process of ovulation. Low FSH would not support follicular development to the point where high estrogen levels could be produced.
D. Gonadotropin-releasing hormone (GnRH) levels do not drop before the LH surge. Instead, the high estrogen levels trigger a surge in GnRH from the hypothalamus, which in turn stimulates the anterior pituitary to release the LH surge. This is a positive feedback loop, where the high estrogen promotes more GnRH and LH secretion, leading to the cascade of events that result in ovulation.
Take home points
- The LH surge is the primary trigger for ovulation.
- High estrogen levels switch from negative to positive feedback to cause the LH surge.
- Progesterone levels rise after ovulation.
- GnRH levels surge, not drop, to cause the LH surge.
Which of the following are components of the Hypothalamic-Pituitary-Ovarian (HPO) Axis? Select all that apply.
Explanation
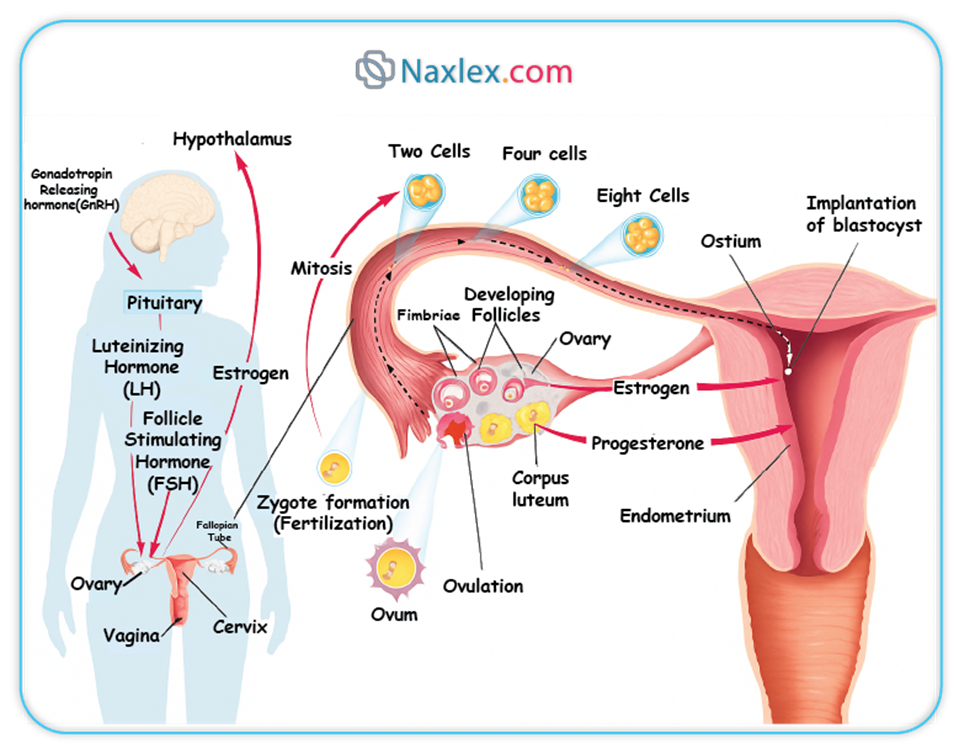
Hypothalamic-pituitary-ovarian (HPO) axis is a complex endocrine system responsible for regulating female reproductive function. It involves a coordinated interplay between three key components: the hypothalamus, the anterior pituitary gland, and the ovaries. The axis operates through a series of hormonal feedback loops, ensuring the proper timing of the menstrual cycle, including follicular development, ovulation, and preparing the uterus for pregnancy. Disruption of this axis can lead to various reproductive disorders.
Rationale for correct answers
B. The hypothalamus is the control center of the HPO axis. It secretes gonadotropin-releasing hormone (GnRH) in a pulsatile manner, which travels to the anterior pituitary gland and stimulates the release of gonadotropins. This is the first and most superior component of the axis.
C. The anterior pituitary gland is the second component. It responds to GnRH by producing and releasing follicle-stimulating hormone (FSH) and luteinizing hormone (LH). These gonadotropins then travel through the bloodstream to the ovaries to regulate their function.
D. The ovaries are the third and final component of the HPO axis. They are the target organs for FSH and LH. In response to these hormones, the ovaries produce estrogen and progesterone, which in turn exert feedback control on the hypothalamus and pituitary gland, completing the loop.
Rationale for incorrect answers
A. The thyroid gland is a part of the hypothalamic-pituitary-thyroid axis, which regulates metabolism through the production of thyroid hormones like triiodothyronine (T3) and thyroxine (T4). While thyroid function can affect reproductive health, it is not a direct component of the HPO axis. It operates as a distinct endocrine pathway.
E. The adrenal glands are part of the hypothalamic-pituitary-adrenal axis, responsible for the stress response through the production of cortisol and other corticosteroids. While adrenal hormones can influence reproductive function, especially under conditions of chronic stress, the adrenal glands are not considered a primary component of the HPO axis. They are a separate endocrine organ with a distinct regulatory pathway.
Take home points
- The HPO axis consists of the hypothalamus, pituitary, and ovaries.
- The hypothalamus releases GnRH.
- The pituitary releases FSH and LH.
- The ovaries release estrogen and progesterone.
Which of the following are events that occur during the follicular phase of the ovarian cycle? Select all that apply.
Explanation
Follicular phase is the first half of the ovarian cycle, initiated by the menstrual period and concluding with ovulation. The primary event is the maturation of ovarian follicles. It is driven by the hormone follicle-stimulating hormone (FSH), which is secreted by the anterior pituitary gland. During this phase, estrogen levels rise as the follicles grow and produce estrogen, leading to the thickening of the uterine lining. The selection of a dominant follicle is a crucial event, as this one follicle will be the source of the oocyte for ovulation.
Rationale for correct answers
A. Follicle-stimulating hormone (FSH) is the primary hormone that initiates the follicular phase. It is released by the anterior pituitary gland and stimulates the growth and development of a cohort of ovarian follicles. Without FSH, the follicles would not mature.
B. As the follicles grow and mature under the influence of FSH, they produce increasing amounts of estrogen. This rise in estrogen levels is a hallmark of the follicular phase and is responsible for the proliferation of the uterine endometrium, preparing it for a potential pregnancy.
E. Out of the several follicles that begin to develop, only one, typically, is selected to become the dominant follicle. This selection process is a crucial event during the mid-to-late follicular phase. The dominant follicle continues to grow and mature, while the others undergo atresia (degeneration).
Rationale for incorrect answers
C. The luteinizing hormone (LH) surge is the event that marks the end of the follicular phase and triggers ovulation. This surge is caused by a positive feedback loop from the high estrogen levels produced by the dominant follicle. It does not occur during the main follicular growth period but rather at its conclusion.
D. The corpus luteum forms after ovulation, during the luteal phase. After the dominant follicle ruptures and releases the oocyte, the remaining follicular cells transform into the corpus luteum under the influence of LH. The corpus luteum's main function is to produce progesterone, which is essential for maintaining the uterine lining. Its formation is a key event of the post-ovulatory phase.
Take home points
- The follicular phase is characterized by follicle growth.
- FSH stimulates follicle development.
- Rising estrogen levels are a key feature of this phase.
- The LH surge and corpus luteum formation occur after the follicular phase.
Practice Exercise 2
Which physical sign is commonly associated with ovulation?
Explanation
Ovulation is the process where a mature ovum is released from the dominant follicle into the fallopian tube. It is triggered by the luteinizing hormone (LH) surge and typically occurs around day 14 of a 28-day cycle. This event is a critical component of female fertility. Associated physical signs are a result of hormonal fluctuations, primarily the peak in estrogen leading to the LH surge. These signs can be tracked to help predict the timing of ovulation.
Rationale for correct answers
B. Mittelschmerz, a German term meaning "middle pain," is a physical sign commonly associated with ovulation. It is a one-sided lower abdominal or pelvic pain that can occur just before, during, or after ovulation. The pain is believed to be caused by the swelling of the dominant follicle before rupture, or by the irritation of the peritoneal lining from the fluid and blood released during follicular rupture.
Rationale for incorrect answers
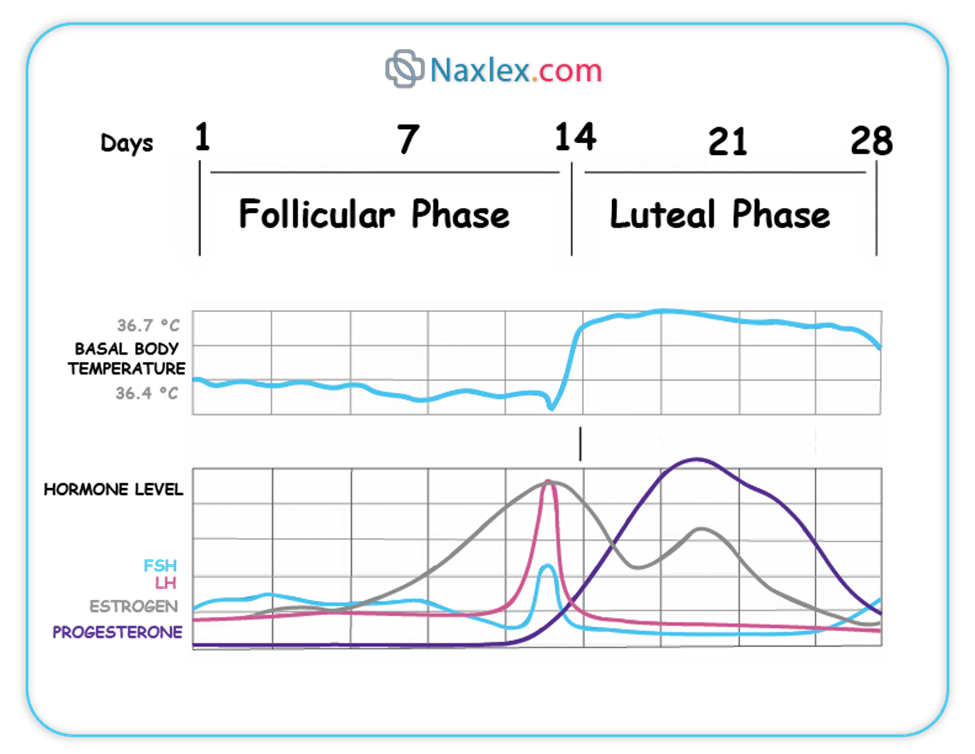
A. A decrease in basal body temperature (BBT) is not associated with ovulation. In fact, BBT remains low during the follicular phase, and then rises by approximately 0.5 to 1.0°F (0.3 to 0.6°C) after ovulation. This temperature increase is due to the thermogenic effects of progesterone, which is produced by the corpus luteum in the luteal phase. Therefore, a rise, not a decrease, in BBT is the correct physical sign.
C. Cervical mucus does change during ovulation, but the change is not a generalized thickening. Under the influence of rising estrogen, cervical mucus becomes thin, clear, and stretchy, resembling raw egg whites. This "fertile" mucus, known as EWM (egg white mucus), facilitates the movement of sperm through the cervix and into the uterus. After ovulation, progesterone causes the mucus to become thick and opaque.
D. Endometrial shedding is the process of menstruation, which is the beginning of the menstrual cycle, not an event of ovulation. Ovulation occurs mid-cycle, following the follicular phase where the uterine lining (endometrium) has thickened. Endometrial shedding is the result of the breakdown of the uterine lining due to a drop in progesterone and estrogen levels when pregnancy does not occur.
Take home points
- Ovulation can be accompanied by a one-sided pelvic pain called mittelschmerz.
- Basal body temperature rises after ovulation.
- Cervical mucus becomes thin and stretchy, like egg whites, during ovulation.
- Endometrial shedding is menstruation, which marks the start of a new cycle.
What is the typical volume of blood loss during menstruation?
Explanation
Menstruation is the cyclical shedding of the uterine endometrium, resulting in vaginal bleeding. It is the final phase of the menstrual cycle when pregnancy does not occur. The bleeding, which consists of blood, tissue, and mucus, typically lasts for 2 to 7 days. The average volume of blood lost is a crucial parameter for evaluating a woman's reproductive health. Menstrual blood loss is defined as heavy, or menorrhagia, if the volume exceeds 80 mL per cycle, which can lead to iron deficiency anemia.
Rationale for correct answers
B. The typical volume of blood lost during a menstrual period is between 30 and 80 mL. A volume of 30-80 mL is considered the normal range and is a key parameter for defining what is considered a healthy menstrual cycle. Values below this range are considered light and may indicate an issue, while values above 80 mL are considered heavy, or menorrhagia.
Rationale for incorrect answers
A. A blood loss volume of 10–20 mL is considered a very light period, also known as hypomenorrhea. While some women may naturally have lighter periods, a consistently low volume can be a sign of underlying hormonal imbalances, a very thin endometrial lining, or other medical conditions. It does not represent the average or typical blood loss for most menstruating individuals.
C. A blood loss volume of 80–120 mL falls into the range of heavy menstrual bleeding or menorrhagia. Menorrhagia is defined as menstrual blood loss exceeding 80 mL per cycle. This can be caused by various factors, including uterine fibroids, hormonal imbalances, and bleeding disorders. It is not considered a typical or normal volume and can lead to symptoms of anemia, such as fatigue.
D. A blood loss volume of 120–150 mL is significantly higher than the normal range and is a clear indicator of menorrhagia. This level of blood loss can be clinically significant, potentially causing iron deficiency anemia and interfering with a woman's daily life. It requires medical evaluation to identify and treat the underlying cause.
Take home points
- The normal range for menstrual blood loss is 30–80 mL per cycle.
- Menorrhagia is defined as blood loss greater than 80 mL per cycle.
- Heavy bleeding can lead to iron deficiency anemia.
- Abnormal bleeding can be caused by hormonal imbalances or structural issues like uterine fibroids.
What is the term for painful menstruation?
Explanation
Dysmenorrhea is the medical term for painful menstruation. It is a common gynecological complaint, with prevalence rates ranging from 45% to 95% among menstruating women. The pain, typically cramping, is caused by the release of prostaglandins in the uterus, which trigger uterine contractions. Dysmenorrhea is categorized into two types: primary dysmenorrhea, which has no underlying pathology, and secondary dysmenorrhea, which is caused by an underlying pelvic condition.
Rationale for correct answers
C. Dysmenorrhea is the correct medical term for painful menstruation. The pain is primarily caused by uterine contractions mediated by prostaglandins released during the menstrual period. This is a very common condition, and the pain can range from mild to severe, sometimes interfering with daily activities.
Rationale for incorrect answers
A. Amenorrhea refers to the absence of menstruation. It is defined as a lack of menstruation for at least 3 consecutive cycles in a woman who has previously menstruated (secondary amenorrhea) or the failure to start menstruating by age 15 (primary amenorrhea). It is a distinct condition from painful menstruation.
B. Oligomenorrhea refers to infrequent or light menstruation, characterized by menstrual cycles that are longer than 35 days. This condition is often associated with anovulation and can be caused by hormonal imbalances. It describes the frequency of periods, not the presence of pain during them.
D. Menorrhagia refers to abnormally heavy or prolonged menstrual bleeding, which is defined as a blood loss of more than 80 mL or a duration of more than 7 days. While menorrhagia can be associated with pain (dysmenorrhea), the term itself specifically describes the volume and duration of bleeding, not the pain.
Take home points
- Dysmenorrhea is the medical term for painful menstruation.
- Primary dysmenorrhea has no underlying cause.
- Secondary dysmenorrhea is due to an underlying condition like endometriosis.
- Other terms like amenorrhea, oligomenorrhea, and menorrhagia describe different menstrual cycle abnormalities.
Which of the following are signs of ovulation? Select all that apply.
Explanation
Ovulation is the release of a mature ovum from a Graafian follicle due to a luteinizing hormone (LH) surge around day 14 of a typical 28-day menstrual cycle. LH rises from baseline to peak levels of 20–100 mIU/mL just before ovulation. Cervical mucus changes to an estrogen-dominant, clear, stretchy consistency. Basal body temperature rises post-ovulation due to progesterone, increasing by 0.4–1.0°F from a normal pre-ovulatory 97.0–98.0°F. Mittelschmerz, a one-sided pelvic pain, may occur during follicular rupture. There is no endometrial shedding at ovulation; that occurs during menstruation.
Rationale for correct answers
A. Mittelschmerz is the mid-cycle pelvic pain occurring during ovulation as the follicle ruptures and releases the oocyte. It typically localizes to one side and is brief, supporting its association with ovulation.
B. Basal body temperature increases post-ovulation due to the thermogenic effect of progesterone. The rise is measurable the day after ovulation and signals corpus luteum activity.
D. Clear, stretchy cervical mucus (spinnbarkeit) occurs under estrogen influence, which peaks before ovulation. This mucus promotes sperm motility and indicates fertility.
Rationale for incorrect answers
C. Thick cervical mucus is a progesterone-dominant change seen post-ovulation. It acts as a barrier to sperm and is not a sign of impending ovulation but rather luteal phase.
E. Endometrial shedding is menstruation, which occurs if fertilization does not happen. It marks the end of the luteal phase, not ovulation.
Take home points
- Clear, stretchy mucus signals estrogen peak and ovulation.
- Basal body temperature rise occurs after ovulation due to progesterone.
- Mittelschmerz is a physical symptom of follicle rupture.
- Endometrial shedding marks menstruation, not ovulation.
Which of the following are characteristics of the cervical mucus during the proliferative phase, under estrogen’s influence? Select all that apply.
Explanation
Proliferative phase cervical mucus
The proliferative phase occurs from day 5 to ovulation in a 28-day cycle and is dominated by estrogen secreted by developing follicles. Estrogen stimulates endometrial regeneration, proliferation of glands, and changes in cervical mucus. Under its influence, cervical mucus becomes thin, watery, clear, and alkaline to facilitate sperm motility and survival. The mucus shows “spinnbarkeit” and ferning when dried. Normal vaginal pH is 3.8–4.5, but during this phase, cervical mucus becomes alkaline (pH >7) to protect sperm from vaginal acidity. Thick, sticky mucus and mucus plug formation are progesterone effects seen in the luteal phase or pregnancy.
Rationale for correct answers
B. Estrogen causes cervical mucus to become clear, which indicates its low viscosity and readiness for sperm passage. Clarity is an essential feature of fertile mucus.
C. Watery consistency is due to high estrogen levels. This low viscosity mucus enhances sperm motility through the cervix.
D. Cervical mucus becomes alkaline under estrogen’s influence, neutralizing the acidic vaginal environment (pH 3.8–4.5) to support sperm survival and transport.
Rationale for incorrect answers
A. Thick and sticky mucus is a progesterone-driven effect in the luteal phase. It inhibits sperm movement and indicates non-fertile cervical conditions.
E. A mucus plug forms in the cervical canal during pregnancy under sustained progesterone influence. It acts as a mechanical barrier and is unrelated to the proliferative phase.
Take home points
- Estrogen makes cervical mucus clear, watery, and sperm-friendly.
- Alkalinity of cervical mucus increases during the proliferative phase.
- Thick, sticky mucus indicates luteal or non-fertile phases.
- Mucus plug formation is a progesterone effect in pregnancy.
Practice Exercise 3
Which condition is characterized by the absence of menstruation for ≥3 months in a woman with previously regular cycles?
Explanation
Secondary amenorrhea is the absence of menses for ≥3 months in a woman with previously regular menstrual cycles. It results from hypothalamic-pituitary-ovarian axis disruption, often due to pregnancy, stress, weight loss, or hyperprolactinemia. Normal menstrual cycles occur every 21–35 days, and bleeding lasts 2–7 days. Serum prolactin should be <20 ng/mL; FSH 4.7–21.5 mIU/mL in reproductive-age women. Causes include polycystic ovarian syndrome, hypothyroidism, and premature ovarian insufficiency. Workup includes β-hCG, TSH, prolactin, and FSH levels.
Rationale for correct answers
C. Secondary amenorrhea is defined as the absence of menstruation for ≥3 consecutive months in a woman with previously normal cycles. This clinical definition distinguishes it from other menstrual abnormalities.
Rationale for incorrect answers
A. Oligomenorrhea is infrequent menstruation, with cycles longer than 35 days but less than 90 days. It does not meet the ≥3-month criterion for amenorrhea.
B. Menorrhagia refers to excessively heavy or prolonged menstrual bleeding, typically >80 mL per cycle or lasting >7 days. It involves presence, not absence, of menstruation.
D. Dysmenorrhea is painful menstruation caused by prostaglandin-induced uterine contractions. It is a disorder of menstrual discomfort, not cycle absence.
Take home points
- Secondary amenorrhea is ≥3 months of absent menses in previously regular cycles.
- Common causes include pregnancy, hypothalamic suppression, and endocrine disorders.
- Oligomenorrhea is defined by long but not absent cycles.
- Dysmenorrhea and menorrhagia both involve active bleeding, not its absence.
Which condition is characterized by excessive menstrual bleeding (>80 mL)?
Explanation
Menorrhagia
Menorrhagia is prolonged or excessive menstrual bleeding exceeding 80 mL per cycle or lasting longer than 7 days. It is often due to hormonal imbalance, uterine fibroids, adenomyosis, or coagulopathies. Normal menstrual blood loss is 30–40 mL per cycle, with an upper limit of 80 mL. Iron-deficiency anemia is a common complication. Normal cycle frequency ranges from 21 to 35 days. Diagnostic evaluation may include complete blood count, pelvic ultrasound, and coagulation profile.
Rationale for correct answers
B. Menorrhagia is defined by menstrual blood loss greater than 80 mL per cycle or bleeding lasting more than 7 days. It reflects abnormal uterine bleeding due to various structural or hormonal causes.
Rationale for incorrect answers
A. Hypomenorrhea refers to light or scanty menstrual flow, typically with shortened duration or minimal blood loss (<20 mL per cycle), not excessive bleeding.
C. Oligomenorrhea is infrequent menstruation, with cycles occurring more than 35 days apart. It concerns frequency, not volume of bleeding.
D. Amenorrhea is the complete absence of menstruation for at least 3 months (secondary) or by age 15 (primary). It involves no bleeding, not excessive bleeding.
Take home points
- Menorrhagia is blood loss >80 mL or >7 days per cycle.
- Normal menstrual loss is 30–40 mL per cycle.
- Hypomenorrhea means light periods; oligomenorrhea means infrequent periods.
- Amenorrhea is absence of menstruation, not heavy flow.
What is the term for the permanent cessation of menstruation, typically diagnosed after 12 consecutive months of amenorrhea?
Explanation
Menopause is the permanent cessation of menstruation resulting from ovarian failure, typically diagnosed after 12 consecutive months of amenorrhea without pathological cause. It usually occurs between ages 45 and 55, with a mean age of 51 years. It involves depletion of ovarian follicles, leading to decreased estrogen and progesterone and elevated FSH levels (>30 mIU/mL). Symptoms include hot flashes, night sweats, vaginal atrophy, and mood changes. It marks the end of reproductive capability and increases risks for osteoporosis and cardiovascular disease due to estrogen loss.
Rationale for correct answers
D. Menopause is diagnosed after 12 months of continuous amenorrhea due to natural decline in ovarian function. It signifies the end of menstrual and reproductive activity.
Rationale for incorrect answers
A. Dysmenorrhea refers to painful menstruation caused by uterine contractions mediated by prostaglandins. It does not involve cessation of menses.
B. Amenorrhea is absence of menstruation, either primary or secondary, but is a symptom, not a natural permanent physiological stage like menopause.
C. Perimenopause is the transition phase leading up to menopause, characterized by menstrual irregularity and vasomotor symptoms, but not complete cessation.
Take home points
- Menopause is confirmed after 12 consecutive months of amenorrhea.
- Average age of menopause is 51 years.
- Elevated FSH and low estrogen levels are typical.
- Perimenopause is the transitional stage before menopause.
Which conditions may cause menstrual irregularities? Select all that apply.
Explanation
Menstrual irregularities result from disruptions in the hypothalamic-pituitary-ovarian axis, leading to abnormal bleeding patterns. Hormonal imbalances, such as altered estrogen, progesterone, or prolactin, are common causes. Normal menstrual cycle length is 21–35 days with bleeding lasting 2–7 days. TSH ranges from 0.4–4.0 mIU/L, prolactin < 20 ng/mL, LH 5–20 IU/L. Elevated androgens and metabolic dysfunctions can also disturb ovulation and endometrial stability.
Rationale for correct answers
A. Polycystic ovary syndrome causes chronic anovulation due to elevated LH and hyperandrogenism. It leads to irregular, infrequent, or absent periods. Serum LH is typically >10 IU/L with an LH:FSH ratio >2:1.
B. Thyroid dysfunction alters the release of GnRH from the hypothalamus, affecting FSH and LH secretion. Both hypothyroidism and hyperthyroidism can lead to amenorrhea or menorrhagia due to endometrial instability.
C. Endometriosis involves ectopic endometrial tissue causing inflammation, fibrosis, and hormonal imbalance, leading to spotting, menorrhagia, or intermenstrual bleeding despite ovulation being mostly preserved.
E. Hyperprolactinemia inhibits GnRH secretion, leading to decreased FSH and LH levels. This suppresses ovulation and results in secondary amenorrhea or oligomenorrhea. Normal prolactin is <20 ng/mL in nonpregnant women.
Rationale for incorrect answers
D. Normal ovulation maintains a stable hormonal environment that supports predictable endometrial shedding. It is regulated by coordinated release of FSH and LH. Progesterone secreted post-ovulation stabilizes the endometrium and supports regular cycles. It does not cause menstrual irregularities.
Take home points
- PCOS causes menstrual irregularities due to chronic anovulation and androgen excess.
- Thyroid hormones influence menstrual cycles by modulating GnRH and ovarian function.
- Hyperprolactinemia suppresses ovulation through inhibition of GnRH.
- Normal ovulation results in regular menstrual cycles and is not a cause of irregularity.
Which of the following are reasons why hormonal contraceptives are effective in preventing pregnancy? Select all that apply.
Explanation
Hormonal contraceptives prevent pregnancy by altering the hypothalamic-pituitary-ovarian axis, leading to suppressed gonadotropins, inhibited ovulation, and changes to the endometrial and cervical environments. Combined oral contraceptives contain estrogen and progestin. Estrogen suppresses FSH (normal: 3–20 IU/L), while progestin suppresses LH (normal: 5–20 IU/L) and inhibits GnRH pulsatility. These agents also thicken cervical mucus and thin the endometrium, reducing sperm penetration and implantation potential. Progesterone levels remain low (normal mid-luteal: 5–20 ng/mL), preventing ovulation.
Rationale for correct answers
A. Hormonal contraceptives suppress GnRH release from the hypothalamus, disrupting the normal pulsatile release needed to stimulate FSH and LH secretion. This halts the ovarian follicular cycle and prevents ovulation.
B. By suppressing LH surge, hormonal contraceptives inhibit ovulation. Without the LH peak (normally around day 14), the dominant follicle fails to rupture, preventing release of the ovum.
D. Progestin in contraceptives thickens cervical mucus, making it viscous and impenetrable to sperm. This mechanical barrier further reduces the chance of fertilization.
Rationale for incorrect answers
C. Hormonal contraceptives make the endometrium less receptive to implantation by causing thinning and glandular atrophy. Progestins suppress endometrial proliferation. A highly receptive endometrium is required for implantation and is stimulated by natural estradiol and progesterone cycles, which are disrupted by contraceptives.
E. Hormonal contraceptives do not stimulate sperm production. Spermatogenesis occurs in males and is regulated by FSH and LH acting on Sertoli and Leydig cells, respectively. Female contraceptives have no physiological role in male gametogenesis.
Take home points
- Contraceptives suppress GnRH, preventing LH and FSH secretion and ovulation.
- Progestin thickens cervical mucus, blocking sperm entry.
- The endometrium becomes thin and hostile to implantation.
- Sperm production is unrelated to female hormonal contraceptives.
Comprehensive Questions
What is the primary function of the corpus luteum?
Explanation
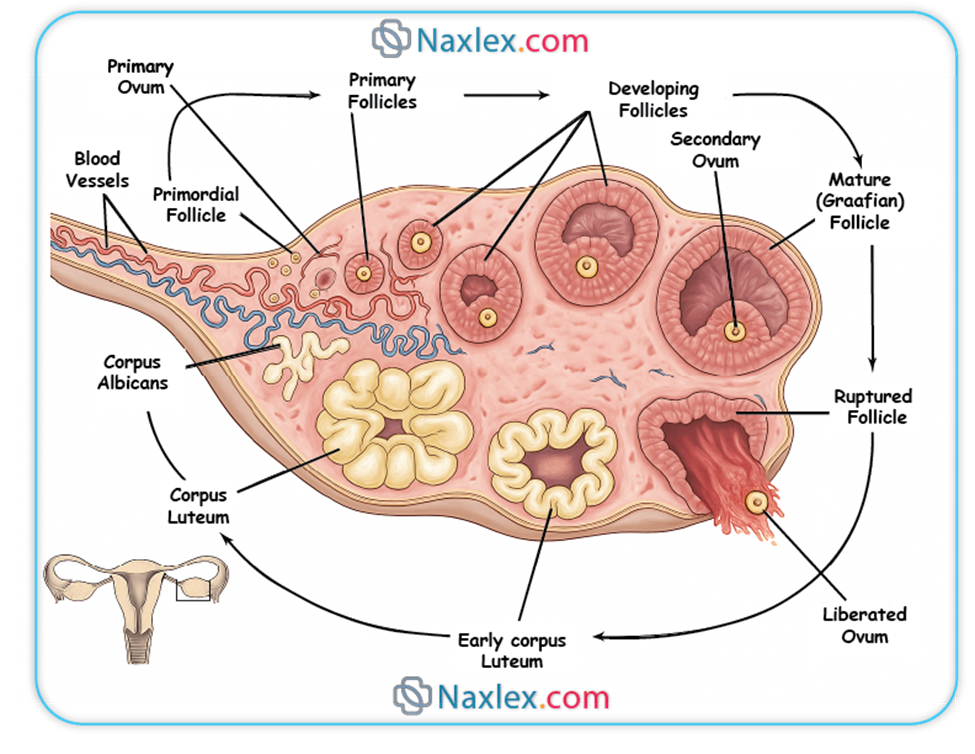
Corpus luteum
The corpus luteum is a temporary endocrine structure formed from the ruptured Graafian follicle after ovulation. It secretes high levels of progesterone, moderate estrogen, and minimal inhibin A to maintain the luteal phase of the menstrual cycle. Progesterone levels peak around day 21 of a 28-day cycle and range from 5–20 ng/mL in the mid-luteal phase. Its main role is to stabilize the endometrial lining for potential implantation and to inhibit GnRH, FSH, and LH via negative feedback. If fertilization does not occur, it regresses into the corpus albicans, causing a drop in hormones and onset of menstruation.
Rationale for correct answer
B. The corpus luteum secretes progesterone during the luteal phase to maintain the endometrium for possible implantation. It forms after ovulation and is hormonally dependent on LH for function.
Rationale for incorrect answers
A. Estrogen is secreted mainly by the dominant follicle during the follicular phase, not by the corpus luteum. The follicular phase precedes ovulation, and the corpus luteum forms after ovulation.
C. The ovum is released by the ruptured follicle due to the LH surge, not by the corpus luteum. The corpus luteum forms after ovulation and plays no direct role in ovum release.
D. GnRH is secreted by the hypothalamus and regulated by sex steroid feedback. The corpus luteum does not stimulate GnRH; in fact, progesterone from the corpus luteum inhibits it.
Take home points
- The corpus luteum secretes progesterone to maintain the endometrium.
- It forms after ovulation from the ruptured follicle.
- It does not release the ovum; that happens before it forms.
- Its hormones inhibit GnRH, FSH, and LH to prevent further ovulation.
Which phase of the menstrual cycle involves the shedding of the endometrium?
Explanation
The menstrual cycle is divided into the menstrual, follicular, ovulatory, and luteal phases, regulated by hormonal fluctuations of estrogen, progesterone, FSH, and LH. The menstrual phase begins on day 1 of the cycle and lasts about 3–7 days, during which the functional layer of the endometrium is shed due to a sudden drop in progesterone (from normal mid-luteal values of 5–20 ng/mL to <1 ng/mL) after corpus luteum regression. FSH (normal: 3–20 IU/L) begins to rise to recruit new follicles. Blood loss ranges from 30–80 mL, and prostaglandins contribute to uterine contractions and cramping.
Rationale for correct answer
D. The menstrual phase involves the shedding of the functional layer of the endometrium due to the withdrawal of progesterone and estrogen. It marks the beginning of a new cycle.
Rationale for incorrect answers
A. The follicular phase follows menstruation and involves regeneration of the endometrium under the influence of rising estrogen levels from developing follicles.
B. Ovulation is the release of an ovum due to the LH surge, around day 14. The endometrium is not shed during this phase; it continues to thicken in preparation for implantation.
C. The luteal phase occurs after ovulation and is marked by progesterone secretion from the corpus luteum to maintain the endometrium. Shedding occurs only if implantation does not happen.
Take home points
- The menstrual phase is when endometrial shedding occurs due to hormonal withdrawal.
- Estrogen and progesterone drop sharply, triggering menstruation.
- The follicular phase is for endometrial regeneration, not shedding.
- Luteal phase maintains the endometrium; shedding starts only if it ends.
What is the primary role of estrogen in the menstrual cycle?
Explanation
Estrogen function in the menstrual cycle
Estrogen is a key steroid hormone secreted primarily by the granulosa cells of the developing follicle. It plays a central role in the follicular phase of the menstrual cycle by stimulating endometrial proliferation, enhancing FSH receptor expression in follicles, and exerting negative feedback on FSH and positive feedback on LH as ovulation approaches. Normal estradiol (E2) levels range from 30–400 pg/mL, peaking around 200–300 pg/mL just before ovulation. Estrogen also supports cervical mucus thinning to facilitate sperm transport and primes the endometrium for possible implantation.
Rationale for correct answer
C. Estrogen stimulates mitotic activity and proliferation of the endometrial functional layer during the follicular phase. This prepares the uterine lining for potential implantation post-ovulation.
Rationale for incorrect answers
A. Ovulation is triggered by a surge in LH, not directly by estrogen. Estrogen contributes indirectly by reaching a threshold that induces the LH surge, but it does not trigger ovulation by itself.
B. Maintenance of the corpus luteum is supported by LH and, if pregnancy occurs, human chorionic gonadotropin (hCG). Estrogen does not sustain corpus luteum function.
D. Estrogen initially inhibits FSH secretion via negative feedback, but this is not its primary role. Its main function is endometrial proliferation and preparing the body for ovulation.
Take home points
- Estrogen stimulates the endometrial lining to proliferate during the follicular phase.
- LH, not estrogen, is the primary trigger for ovulation.
- Corpus luteum maintenance depends on LH or hCG, not estrogen.
- Estrogen has a dual feedback effect on FSH depending on its concentration and timing.
What happens to the corpus luteum if fertilization does not occur?
Explanation
The corpus luteum is formed from the ruptured ovarian follicle after ovulation and functions as a temporary endocrine gland, primarily secreting progesterone (5–20 ng/mL mid-luteal) and smaller amounts of estrogen. It maintains the endometrium in preparation for implantation. If fertilization and implantation do not occur, the absence of human chorionic gonadotropin (hCG) causes the corpus luteum to degenerate around day 24–26 of a typical 28-day cycle. It then becomes a fibrous scar tissue called the corpus albicans, leading to a drop in progesterone and estrogen levels, and triggering menstruation.
Rationale for correct answer
B. If fertilization does not occur, the corpus luteum degenerates due to lack of hCG support and transforms into the corpus albicans. This structural regression leads to hormonal withdrawal and menstruation.
Rationale for incorrect answers
A. Progesterone secretion continues only if fertilization occurs and hCG is produced by the trophoblast. Without hCG, the corpus luteum involutes and stops secreting hormones.
C. The corpus luteum forms after ovulation; it does not trigger it. Ovulation is triggered by the LH surge prior to corpus luteum formation.
D. The corpus luteum secretes some estrogen, but its primary function is progesterone production. After degeneration, it no longer produces either hormone in significant amounts.
Take home points
- The corpus luteum regresses into the corpus albicans without fertilization.
- Hormonal support from hCG is necessary to sustain the corpus luteum.
- Progesterone levels drop, triggering menstruation.
- The corpus luteum does not cause ovulation; it follows it.
Which phase of the endometrial cycle coincides with the luteal phase?
Explanation
The endometrial cycle aligns with the ovarian cycle and consists of three main phases: menstrual, proliferative, and secretory. The secretory phase coincides with the luteal phase of the ovarian cycle and spans approximately days 15–28. It is regulated primarily by progesterone (normal mid-luteal: 5–20 ng/mL) secreted by the corpus luteum. Progesterone stimulates the endometrial glands to secrete glycogen and other nutrients, making the endometrium thick, vascular, and receptive to implantation. Without fertilization, progesterone levels fall, leading to endometrial breakdown and the start of menstruation.
Rationale for correct answer
C. The secretory phase is driven by progesterone from the corpus luteum and prepares the endometrium for possible implantation. It occurs during the luteal phase of the ovarian cycle.
Rationale for incorrect answers
A. The menstrual phase coincides with the early follicular phase, not the luteal phase. It involves shedding of the functional layer of the endometrium due to hormone withdrawal.
B. The proliferative phase occurs during the follicular phase of the ovarian cycle. It is estrogen-driven and involves rebuilding the endometrium after menstruation.
D. The regenerative phase is not a standard term in the clinical classification of the endometrial cycle. The correct phases are menstrual, proliferative, and secretory.
Take home points
- The secretory phase matches the luteal phase and prepares the uterus for implantation.
- Progesterone from the corpus luteum drives the secretory changes.
- The proliferative phase aligns with follicular phase and is estrogen-dependent.
- Menstrual phase begins with hormone withdrawal and marks the end of the luteal phase.
What is the typical duration of menstruation?
Explanation
Menstruation marks the beginning of the menstrual cycle and involves the shedding of the functional layer of the endometrium due to the decline of progesterone and estrogen. It is triggered by corpus luteum regression in the absence of fertilization. Normal menstrual bleeding lasts 3–7 days, with average blood loss between 30–80 mL. Levels of FSH (3–20 IU/L) begin to rise to recruit new follicles for the next cycle. Prostaglandins are released, causing vasoconstriction and myometrial contractions, leading to menstrual cramps and tissue expulsion.
Rationale for correct answer
B. The normal duration of menstruation is 3–7 days. This range is physiologically typical and supported by stable hormone withdrawal patterns and normal endometrial responses.
Rationale for incorrect answers
A. A duration of 1–3 days is shorter than the normal range and may indicate hypomenorrhea or hormonal insufficiency, though still considered normal if consistent and asymptomatic.
C. Bleeding for 7–10 days exceeds the upper normal limit and may suggest menorrhagia or coagulation abnormalities, requiring evaluation.
D. A menstrual duration of 10–14 days is abnormal and often pathological. It may suggest hormonal imbalance, fibroids, endometrial hyperplasia, or bleeding disorders.
Take home points
- Normal menstruation lasts 3–7 days with 30–80 mL blood loss.
- Bleeding <3 days or >7 days may indicate hormonal or structural pathology.
- Menstruation occurs due to hormonal withdrawal after corpus luteum regression.
- Prostaglandins play a role in endometrial shedding and cramping.
Which hormone is primarily responsible for preparing the endometrium for implantation during the secretory phase of the uterine cycle?
Explanation
The secretory phase follows ovulation and spans days 15–28 of a typical 28-day menstrual cycle. It is driven by progesterone secreted by the corpus luteum. Progesterone transforms the previously estrogen-primed proliferative endometrium into a thick, vascular, and glandular lining capable of supporting implantation. Endometrial glands become coiled and secrete glycogen-rich fluid to nourish a potential embryo. Progesterone levels typically peak at 5–20 ng/mL in the mid-luteal phase. If implantation does not occur, progesterone falls sharply, leading to menstruation.
Rationale for correct answer
D. Progesterone is the main hormone that prepares the endometrium during the secretory phase. It induces glandular secretion, stromal edema, and vascularization to support early pregnancy if fertilization occurs.
Rationale for incorrect answers
A. Estrogen plays a primary role in the proliferative phase, promoting regeneration of the endometrium but not in its secretory transformation. It works before ovulation, not after.
B. FSH stimulates follicular development and estrogen secretion during the follicular phase, but it does not act on the endometrium directly and is not dominant in the luteal/secretory phase.
C. LH triggers ovulation and supports the formation of the corpus luteum, which secretes progesterone, but LH itself does not directly act on the endometrium during the secretory phase.
Take home points
- Progesterone transforms the endometrium into a receptive state during the secretory phase.
- Estrogen prepares the endometrium in the proliferative phase, not the secretory.
- FSH and LH regulate ovarian activity but have no direct endometrial action in the luteal phase.
- Secretory changes include gland coiling, glycogen secretion, and stromal edema.
The menstrual cycle is typically counted from which day?
Explanation
The menstrual cycle is a recurring sequence of hormonal and physiological events typically lasting 21–35 days, with an average of 28 days. It is counted from day 1, which is defined as the first day of menstrual bleeding—the visible onset of endometrial shedding. This marks the start of the follicular phase, during which FSH (normal range: 3–20 IU/L) rises to stimulate follicular development. Bleeding lasts about 3–7 days, and estrogen levels gradually increase to rebuild the endometrium. Ovulation generally occurs around day 14, followed by the luteal phase.
Rationale for correct answer
B. The first day of menstrual bleeding is considered day 1 of the cycle. It marks the beginning of the follicular phase and is used clinically to track ovulation, fertility windows, and menstrual regularity.
Rationale for incorrect answers
A. Ovulation typically occurs around day 14 of a 28-day cycle, not at the beginning. It is a mid-cycle event and not used as the starting point for cycle calculation.
C. The last day of menstruation varies among individuals and does not consistently mark the start of a new hormonal cycle, making it an unreliable reference point.
D. The LH surge precedes ovulation by 24–36 hours and occurs around day 13–14, mid-cycle. It is not the beginning of the menstrual cycle and occurs much later than day 1.
Take home points
- Day 1 of the menstrual cycle is the first day of menstrual bleeding.
- This marks the start of the follicular phase and FSH rise.
- Ovulation and the LH surge occur mid-cycle, not at the beginning.
- Accurate cycle tracking begins with the first day of menstruation.
What is the role of human chorionic gonadotropin (hCG) if pregnancy occurs?
Explanation
hCG is a glycoprotein hormone secreted by the trophoblast cells of the developing embryo shortly after implantation, typically detectable in maternal serum by day 8–10 post-ovulation. Its primary role is to rescue the corpus luteum, preventing its degeneration and allowing continued secretion of progesterone and estrogen. These hormones maintain the decidualized endometrium, preventing menstruation and supporting early pregnancy. hCG shares structural similarity with LH and binds to LH receptors on the corpus luteum. Peak serum hCG levels reach 100,000–200,000 mIU/mL by 10 weeks gestation.
Rationale for correct answer
C. hCG prevents luteolysis by acting on LH receptors of the corpus luteum, maintaining its progesterone production. This sustains the endometrial lining for implantation and early embryonic development.
Rationale for incorrect answers
A. hCG does not stimulate new follicle development. In fact, high progesterone and estrogen levels maintained by the corpus luteum inhibit FSH, preventing new folliculogenesis during early pregnancy.
B. hCG prevents menstruation by maintaining the corpus luteum and its hormone output. Menstruation is triggered by progesterone withdrawal, which hCG directly prevents.
D. hCG supports the continued production of progesterone, not its inhibition. It ensures the endometrial lining remains intact until the placenta takes over hormone production around week 10–12.
Take home points
- hCG maintains the corpus luteum during early pregnancy.
- It prevents menstruation by supporting progesterone production.
- hCG mimics LH and binds to LH receptors on luteal cells.
- It does not promote follicle development or suppress progesterone.
Which hormone, when at consistently high levels for a sustained period, switches from negative to positive feedback on GnRH and LH, leading to the LH surge?
Explanation
Estrogen, specifically estradiol (E2), plays a dual role in the hypothalamic-pituitary-ovarian axis through both negative and positive feedback mechanisms. During the late follicular phase, when estradiol levels remain consistently high—typically >200 pg/mL for at least 50 hours—the feedback on the hypothalamus and anterior pituitary shifts from negative to positive. This stimulates a GnRH surge, which triggers a massive LH release (LH surge), leading to ovulation. The LH surge also initiates the transformation of the ruptured follicle into the corpus luteum.
Rationale for correct answer
C. Estrogen at sustained high levels switches to positive feedback, stimulating GnRH and causing the LH surge. This is the critical hormonal trigger for ovulation around day 14 of a typical 28-day cycle.
Rationale for incorrect answers
A. Progesterone exerts only negative feedback on GnRH, FSH, and LH throughout the cycle, especially during the luteal phase. It does not cause the LH surge and actually prevents further ovulation.
B. FSH is regulated by negative feedback via estrogen and inhibin. It does not trigger the LH surge and is not part of the positive feedback loop leading to ovulation.
D. Inhibin is secreted by granulosa cells and specifically suppresses FSH release via negative feedback. It plays no role in triggering the LH surge or stimulating GnRH.
Take home points
- High sustained estrogen levels trigger positive feedback on GnRH and LH.
- The LH surge causes ovulation and luteinization of the follicle.
- Progesterone and inhibin exert negative feedback and suppress further ovulation.
- FSH supports follicle growth but is not involved in the LH surge trigger.
Which hormones are secreted by the anterior pituitary to regulate the menstrual cycle? Select all that apply.
Explanation
The anterior pituitary secretes follicle-stimulating hormone (FSH) and luteinizing hormone (LH), two key gonadotropins that regulate the ovarian cycle and control the secretion of ovarian hormones (estrogen and progesterone). FSH (normal: 3–20 IU/L) promotes follicular growth and estrogen production during the follicular phase, while LH (normal: 5–20 IU/L) triggers ovulation and stimulates the formation and function of the corpus luteum during the luteal phase. Their secretion is stimulated by GnRH from the hypothalamus in a pulsatile manner.
Rationale for correct answers
A. FSH is secreted by the anterior pituitary and stimulates the growth and maturation of ovarian follicles and the synthesis of estradiol by granulosa cells.
B. LH is also released from the anterior pituitary and is responsible for triggering ovulation and maintaining the corpus luteum, which secretes progesterone during the luteal phase.
Rationale for incorrect answers
C. GnRH is not secreted by the anterior pituitary—it is secreted by the hypothalamus and acts on the anterior pituitary to stimulate the release of FSH and LH.
D. Estrogen is produced by granulosa cells of the ovarian follicles, not by the anterior pituitary. Its secretion is regulated by FSH.
E. Progesterone is secreted by the corpus luteum in the ovary after ovulation. It is not an anterior pituitary hormone.
Take home points
- FSH and LH are the two anterior pituitary hormones that regulate the menstrual cycle.
- GnRH is from the hypothalamus, not the anterior pituitary.
- Estrogen and progesterone are secreted by the ovaries under pituitary control.
- Pituitary hormones initiate and regulate ovulation and corpus luteum function.
Which hormones are produced by the ovaries during the menstrual cycle? Select all that apply.
Explanation
The ovaries are the primary source of estrogen and progesterone during the menstrual cycle. These steroid hormones regulate endometrial development, ovulation, and feedback control of the hypothalamic-pituitary axis. Estrogen is mainly secreted by granulosa cells of developing follicles during the follicular phase, reaching peak levels of 200–300 pg/mL pre-ovulation. Progesterone is produced by the corpus luteum in the luteal phase, with mid-luteal levels of 5–20 ng/mL, stabilizing the endometrium for implantation.
Rationale for correct answers
A. Estrogen is produced by ovarian granulosa cells during follicular development. It promotes endometrial proliferation and regulates FSH and LH secretion via feedback.
B. Progesterone is secreted by the corpus luteum after ovulation. It prepares and maintains the endometrium for implantation and inhibits GnRH, FSH, and LH secretion to prevent further ovulation.
Rationale for incorrect answers
C. FSH is secreted by the anterior pituitary, not the ovaries. It stimulates follicular growth in the ovaries and estrogen production.
D. LH is also secreted by the anterior pituitary, not the ovaries. It triggers ovulation and supports the corpus luteum.
E. GnRH is secreted by the hypothalamus, not the ovaries. It regulates the release of FSH and LH from the pituitary.
Take home points
- The ovaries produce estrogen (follicular phase) and progesterone (luteal phase).
- FSH and LH come from the anterior pituitary, not the ovaries.
- GnRH originates in the hypothalamus and regulates pituitary hormones.
- Ovarian hormones regulate endometrial changes and provide feedback control.
Which of the following are functions of progesterone in the menstrual cycle? Select all that apply.
Explanation
Progesterone in the menstrual cycle Progesterone is a steroid hormone produced by the corpus luteum after ovulation during the luteal phase. Its primary role is to prepare the endometrium for implantation. Progesterone maintains the uterine lining, inhibits uterine contractions, and increases basal body temperature. Normal serum progesterone levels vary across the cycle: follicular phase <1 ng/mL, luteal phase 5–20 ng/mL, postmenopausal <0.5 ng/mL. It is also critical in modulating immune tolerance during early pregnancy.
Rationale for correct answers
B. Progesterone converts the endometrium from the proliferative to the secretory phase, enhancing glandular secretion and stromal edema to support implantation.
C. It inhibits myometrial contractions by reducing prostaglandin synthesis and promoting uterine quiescence during the luteal phase, preventing embryo expulsion.
E. Progesterone increases basal body temperature typically by 0.3–0.5°C due to its thermogenic effect on the hypothalamic temperature-regulating center.
Rationale for incorrect answers
A. Endometrial proliferation occurs during the follicular phase and is mediated primarily by estradiol. Progesterone opposes proliferation and promotes secretory transformation.
D. Ovulation is triggered by a surge in luteinizing hormone (LH), not progesterone. Progesterone secretion rises only after ovulation has occurred.
Take home points
- Progesterone maintains a secretory endometrium essential for embryo implantation.
- It inhibits uterine contractility by downregulating prostaglandins.
- Progesterone elevation correlates with the post-ovulatory rise in body temperature.
- Estradiol governs the proliferative phase; LH surge triggers ovulation.
Which of the following are changes that occur in the uterine endometrium during the secretory phase? Select all that apply.
Explanation
Secretory phase of the menstrual cycle The secretory phase follows ovulation and is driven by progesterone from the corpus luteum, transforming the proliferative endometrium into a receptive environment for implantation. The endometrial glands become tortuous and begin secreting glycogen, while stromal edema and increased vascularity aid embryo nourishment. Spiral arteries elongate and become more coiled, and normal endometrial thickness during this phase ranges from 7–14 mm. Progesterone levels peak around 5–20 ng/mL in the mid-luteal phase.
Rationale for correct answers
A. Endometrial glands become tortuous due to progesterone influence, increasing their secretory capacity in preparation for embryo implantation.
B. Glycogen and mucus are secreted into the lumen to create a nutrient-rich medium essential for the survival and implantation of the embryo.
C. Progesterone enhances vascular permeability and stromal edema, making the endometrium highly vascular and edematous to support embryo development.
Rationale for incorrect answers
D. Shedding of the functional layer occurs during menstruation, not the secretory phase. Menstrual shedding begins only if fertilization does not take place, leading to corpus luteum regression and progesterone withdrawal.
E. Spiral arteries become more prominent and coiled during the secretory phase to support increased blood flow. Less prominence is incorrect; their hypertrophy is critical for placental development if implantation occurs.
Take home points
- Secretory phase is progesterone-dominant and follows ovulation.
- Tortuous glands and glycogen secretion prepare the endometrium for implantation.
- Spiral arteries elongate and coil for enhanced perfusion.
- Functional layer shedding occurs only in menstruation, not in the secretory phase.
Which of the following are characteristics of the menstrual phase of the uterine cycle? Select all that apply.
Explanation
Menstrual phase of the uterine cycle The menstrual phase marks the beginning of the uterine cycle and is initiated by a sudden drop in estrogen and progesterone levels due to corpus luteum regression in the absence of implantation. This hormonal decline leads to vasoconstriction of spiral arteries, ischemia, and shedding of the functional layer of the endometrium. Normal menstrual flow lasts 3–5 days, and blood loss averages 30–40 mL. Spiral artery spasms result in tissue necrosis, and rising estrogen levels only commence after menstruation is complete.
Rationale for correct answers
A. The withdrawal of estrogen and progesterone at the end of the luteal phase triggers endometrial breakdown and onset of menstrual bleeding.
B. The functional layer of the endometrium undergoes necrosis and is shed through the cervix and vagina as menstrual fluid.
C. Spiral arteries undergo intense vasoconstriction, leading to ischemia and necrosis of the endometrium, which causes menstruation.
D. The menstrual phase typically spans Days 1 to 5 of the cycle, marking the beginning of the uterine cycle before follicular estrogen rise.
Rationale for incorrect answers
E. Rising estrogen levels occur during the proliferative phase, which begins after menstruation. The menstrual phase is marked by low estrogen and progesterone levels.
Take home points
- Menstrual phase starts with progesterone and estrogen withdrawal.
- Endometrial shedding is due to spiral artery ischemia.
- Menstrual flow usually lasts 3–5 days.
- Rising estrogen levels define the proliferative phase, not the menstrual phase.
Exams on The Menstrual Cycle
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
- Objectives
- Introduction
- Hormonal Regulation Of The Menstrual Cycle
- Ovarian Phases Of The Menstrual Cycle
- Uterine Phases Of The Menstrual Cycle
- Practice Exercise 1
- Physiological Changes And Clinical Manifestations
- Clinical Implications And Patient Education
- Practice Exercise 2
- Nursing Considerations In Menstrual Cycle Management
- Practice Exercise 3
- Summary
- Comprehensive Questions
Notes Highlighting is available once you sign in. Login Here.
Objectives
Upon completion of this module, the nursing student will be able to:
- Describe the key hormones involved in regulating the menstrual cycle and their respective functions.
- Differentiate between the ovarian and uterine phases of the menstrual cycle, outlining the major events occurring in each.
- Explain the feedback mechanisms that control the release of reproductive hormones throughout the menstrual cycle.
- Identify the normal physiological changes associated with each phase of the menstrual cycle.
- Relate the hormonal and physical changes of the menstrual cycle to common signs and symptoms experienced by women.
- Apply knowledge of the menstrual cycle to patient education regarding reproductive health, contraception, and fertility.
- Recognize deviations from a normal menstrual cycle and their potential clinical implications.
Introduction
The menstrual cycle is a complex, hormonally regulated process that prepares the female reproductive system for potential pregnancy. It involves intricate interactions between the hypothalamus, anterior pituitary, ovaries, and uterus, resulting in cyclic changes in the ovarian and endometrial tissues. The average menstrual cycle lasts 21–35 days, with menstruation typically occurring for 3–7 days. Understanding the menstrual cycle is fundamental for nurses to provide effective patient education, assess reproductive health, and identify abnormalities that may require medical intervention. These comprehensive notes aim to equip nursing students with a detailed understanding of the menstrual cycle, emphasizing hormonal regulation, physiological changes, clinical manifestations, and nursing considerations.
Hormonal Regulation Of The Menstrual Cycle
Key Hormones and Their Functions
The menstrual cycle is orchestrated by a cascade of hormones that regulate ovarian and uterine functions. These hormones include gonadotropin-releasing hormone (GnRH), follicle-stimulating hormone (FSH), luteinizing hormone (LH), estrogen, progesterone, and inhibin.
• Gonadotropin-Releasing Hormone (GnRH):
➤ Secreted by the hypothalamus in a pulsatile manner, GnRH stimulates the anterior pituitary to release FSH and LH.
➤ The pulsatility of GnRH is critical for maintaining the cyclic nature of the menstrual cycle.
• Follicle-Stimulating Hormone (FSH):
➤ Produced by the anterior pituitary, FSH stimulates the growth and maturation of ovarian follicles during the follicular phase.
➤ FSH promotes granulosa cell proliferation and estrogen synthesis within the follicles.
• Luteinizing Hormone (LH):
➤ Also secreted by the anterior pituitary, LH triggers ovulation by causing the rupture of the mature Graafian follicle.
➤ LH supports the transformation of the ruptured follicle into the corpus luteum, which secretes progesterone.
• Estrogen:
➤ Primarily produced by the ovarian follicles and corpus luteum, estrogen stimulates endometrial proliferation during the proliferative phase.
➤ Estrogen also influences cervical mucus changes, facilitating sperm transport during ovulation.
• Progesterone:
➤ Secreted by the corpus luteum during the luteal phase, progesterone prepares the endometrium for implantation by promoting glandular secretion and vascularization.
➤ Progesterone inhibits uterine contractions and maintains pregnancy if fertilization occurs.
• Inhibin:
➤ Produced by granulosa cells, inhibin selectively inhibits FSH secretion, preventing the development of additional follicles during the cycle.
Nursing Insights:
• Nurses must understand the specific roles of each hormone to interpret laboratory results and assess hormonal imbalances.
• Monitoring hormone levels, such as FSH and LH, can aid in diagnosing conditions like polycystic ovary syndrome (PCOS) or premature ovarian failure.
• Educating patients about hormonal contraceptives involves explaining how synthetic estrogen and progesterone mimic natural hormones to suppress ovulation.
Hypothalamic-Pituitary-Ovarian Axis
The hypothalamic-pituitary-ovarian (HPO) axis is the central regulatory system governing the menstrual cycle. This axis integrates neural and endocrine signals to coordinate reproductive functions.
• Hypothalamus:
➤ Releases GnRH in a pulsatile pattern, which stimulates the anterior pituitary.
➤ External factors, such as stress or excessive exercise, can disrupt GnRH pulsatility, leading to menstrual irregularities.
• Anterior Pituitary:
➤ Responds to GnRH by secreting FSH and LH, which act on the ovaries to regulate folliculogenesis and ovulation.
• Ovaries:
➤ Produce estrogen, progesterone, and inhibin, which exert feedback on the hypothalamus and pituitary to modulate hormone release.
➤ The ovaries are the primary site of follicular development, ovulation, and corpus luteum formation.
Nursing Insights:
• Nurses should assess for factors that disrupt the HPO axis, such as stress, malnutrition, or thyroid dysfunction, as these can lead to amenorrhea or irregular cycles.
• When counseling patients, nurses must explain how lifestyle factors, like extreme weight loss or excessive exercise, can impair HPO axis function.
• Understanding the HPO axis is crucial for interpreting diagnostic tests, such as serum FSH levels, to evaluate ovarian reserve.
Feedback Mechanisms
The menstrual cycle is regulated by both negative and positive feedback mechanisms that control hormone release.
• Negative Feedback:
➤ During the follicular phase, low levels of estrogen and progesterone exert negative feedback on the hypothalamus and pituitary, maintaining steady FSH and LH secretion.
➤ In the luteal phase, high progesterone levels inhibit GnRH, FSH, and LH, preventing further follicular development.
• Positive Feedback:
➤ During the late follicular phase, high estrogen levels trigger a positive feedback loop, leading to an LH surge that induces ovulation.
➤ This surge is critical for the rupture of the dominant follicle and release of the mature ovum.
Nursing Insights:
• Nurses must recognize that disruptions in feedback mechanisms, such as hyperprolactinemia, can inhibit GnRH release and cause anovulatory cycles.
• Patient education should include how hormonal contraceptives manipulate feedback mechanisms to prevent ovulation.
• Monitoring for signs of positive feedback, such as the LH surge, is essential when assisting patients with ovulation predictor kits (OPKs).
Ovarian Phases Of The Menstrual Cycle
Follicular Phase
The follicular phase, spanning from day 1 to approximately day 14 of a 28-day cycle, is characterized by follicular growth and estrogen production.
• Folliculogenesis:
➤ FSH stimulates the development of multiple primordial follicles, with one becoming the dominant Graafian follicle.
➤ Non-dominant follicles undergo atresia, a process of degeneration.
• Estrogen Production:
➤ Granulosa cells within the developing follicles produce estrogen, which peaks as the dominant follicle matures.
➤ Estrogen stimulates endometrial proliferation and cervical mucus changes.
• Duration Variability:
➤ The follicular phase is the most variable in length, ranging from 7 to 21 days, depending on individual hormonal profiles.
Nursing Insights:
• Nurses should educate patients using ovulation predictor kits to detect the LH surge, which typically occurs 24–36 hours before ovulation.
• Assessing the follicular phase duration is critical for fertility planning, as prolonged phases may indicate delayed ovulation.
• Patients with irregular follicular phases may require referral to a reproductive endocrinologist for further evaluation.
Ovulatory Phase
The ovulatory phase, lasting 24–36 hours, is marked by the rupture of the Graafian follicle and release of the mature ovum.
• LH Surge:
➤ A peak in estrogen levels triggers a positive feedback loop, resulting in a surge of LH from the anterior pituitary.
➤ The LH surge causes the follicle wall to weaken and rupture, releasing the secondary oocyte into the fallopian tube.
• Oocyte Maturation:
➤ The oocyte completes meiosis I just before ovulation, forming a secondary oocyte and a polar body.
➤ Meiosis II is completed only if fertilization occurs in the fallopian tube.
Nursing Insights:
• Nurses should teach patients to recognize signs of ovulation, such as mittelschmerz or changes in cervical mucus, to optimize conception timing.
• Ovulation predictor kits detect the LH surge, assisting patients in identifying their fertile window.
• Understanding the ovulatory phase is essential for counseling patients on natural family planning methods.
Luteal Phase
The luteal phase, lasting approximately 12–16 days, begins after ovulation and is characterized by corpus luteum formation and progesterone secretion.
• Corpus Luteum Formation:
➤ The ruptured follicle transforms into the corpus luteum under LH influence, secreting progesterone and some estrogen.
➤ If fertilization does not occur, the corpus luteum degenerates into the corpus albicans, leading to a decline in hormone levels.
• Progesterone Effects:
➤ Progesterone prepares the endometrium for implantation and inhibits uterine contractions.
➤ Progesterone also causes a rise in basal body temperature, a key indicator of ovulation.
Nursing Insights:
• Nurses should monitor basal body temperature charts to confirm ovulation in patients attempting to conceive.
• A shortened luteal phase (<10 days) may indicate a luteal phase defect, associated with recurrent early pregnancy loss.
• Educating patients about progesterone’s role in maintaining early pregnancy is crucial for those undergoing fertility treatments.
Uterine Phases Of The Menstrual Cycle
Menstrual Phase
The menstrual phase, lasting 3–7 days, involves the shedding of the endometrial functional layer due to declining hormone levels.
• Hormonal Trigger:
➤ A sharp decline in estrogen and progesterone removes negative feedback, initiating endometrial breakdown.
➤ Prostaglandins cause spasms of spiral arteries, leading to ischemia and shedding of the functional layer.
• Blood Loss:
➤ Normal menstrual blood loss ranges from 30–80 mL, with excessive bleeding (>80 mL) termed menorrhagia.
➤ The basal layer of the endometrium remains intact to regenerate the endometrium in the next phase.
Nursing Insights:
• Nurses must assess menstrual flow volume and duration to identify abnormalities like menorrhagia or hypomenorrhea.
• Patient education should include proper hygiene practices during menstruation to prevent infections.
• Monitoring for signs of anemia, such as fatigue or pallor, is essential in patients with heavy menstrual bleeding.
Proliferative Phase
The proliferative phase, coinciding with the follicular phase, involves endometrial regeneration under estrogen influence.
• Endometrial Growth:
➤ Estrogen stimulates the proliferation of the endometrial functional layer, increasing its thickness and vascularity.
➤ Endometrial glands elongate, and spiral arteries develop to support potential implantation.
• Cervical Mucus Changes:
➤ Estrogen causes cervical mucus to become thin, clear, watery, and alkaline, facilitating sperm transport.
Nursing Insights:
• Nurses should educate patients about cervical mucus changes as a natural indicator of fertility.
• Assessing endometrial thickness via ultrasound may be necessary in patients with infertility concerns.
• Understanding the proliferative phase aids in counseling patients about the timing of fertility treatments.
Secretory Phase
The secretory phase, aligning with the luteal phase, prepares the endometrium for implantation under progesterone influence.
• Endometrial Maturation:
➤ Progesterone stimulates endometrial glands to become tortuous and secrete glycogen and mucus.
➤ The endometrium becomes edematous and highly vascular, optimizing conditions for embryo implantation.
• Hormonal Maintenance:
➤ If pregnancy occurs, human chorionic gonadotropin (hCG) maintains the corpus luteum, sustaining progesterone production.
➤ In the absence of pregnancy, declining progesterone triggers menstruation.
Nursing Insights:
• Nurses should counsel patients about the importance of progesterone in maintaining early pregnancy.
• Monitoring for luteal phase defects involves assessing cycle length and progesterone levels.
• Patients undergoing in vitro fertilization (IVF) may require progesterone supplementation to support the secretory phase.
Physiological Changes And Clinical Manifestations
Normal Physiological Changes
Each phase of the menstrual cycle is associated with distinct physiological changes that prepare the reproductive system for potential pregnancy.
• Follicular Phase:
➤ Rising estrogen levels stimulate endometrial proliferation and cervical mucus changes.
➤ Basal body temperature remains low, typically 36.1–36.6°C (97–98°F).
• Ovulatory Phase:
➤ The LH surge triggers ovulation, accompanied by a slight rise in basal body temperature.
➤ Cervical mucus becomes clear, stretchy, and forms “ferning” patterns under a microscope.
• Luteal Phase:
➤ Progesterone secretion causes a sustained rise in basal body temperature by 0.4–0.8°C (0.7–1.4°F).
➤ The endometrium becomes secretory, with increased glandular activity and vascularity.
• Menstrual Phase:
➤ Declining hormone levels lead to endometrial shedding and menstrual bleeding.
➤ Prostaglandin-induced uterine contractions may cause mild cramping.
Nursing Insights:
• Nurses must teach patients to track basal body temperature to confirm ovulation, as a biphasic pattern indicates a normal luteal phase.
• Assessing cervical mucus changes can help patients identify their fertile window for conception or contraception.
• Understanding normal physiological changes allows nurses to reassure patients about expected symptoms, such as mild ovulatory pain.
Common Signs and Symptoms
The menstrual cycle is associated with various signs and symptoms that reflect hormonal and physiological changes.
• Mittelschmerz:
➤ Mid-cycle pelvic pain, often unilateral, caused by follicular rupture during ovulation.
➤ Typically lasts a few hours to a day and may be accompanied by light spotting.
• Cervical Mucus Changes:
➤ During ovulation, cervical mucus is clear, stretchy, and slippery, resembling egg whites.
➤ Post-ovulation, progesterone causes mucus to become thick and opaque, forming a barrier.
• Basal Body Temperature:
➤ A rise in basal body temperature post-ovulation is a reliable indicator of progesterone activity.
• Menstrual Symptoms:
➤ Common symptoms include bloating, breast tenderness, mood changes, and mild cramping due to prostaglandin release.
Nursing Insights:
• Nurses should educate patients to differentiate normal symptoms, like mittelschmerz, from pathological conditions, such as ovarian cysts.
• Patients reporting severe menstrual pain should be assessed for secondary dysmenorrhea, which may indicate endometriosis.
• Tracking symptoms in a menstrual diary can aid in diagnosing cycle irregularities and planning interventions.
Clinical Implications And Patient Education
Deviations from Normal Menstrual Cycle
Deviations from a normal menstrual cycle may indicate underlying pathology and require thorough assessment.
• Amenorrhea:
➤ Primary amenorrhea is the absence of menstruation by age 15 in the presence of secondary sexual characteristics.
➤ Secondary amenorrhea is the cessation of menstruation for ≥3 months in women with previously regular cycles.
➤ Causes include pregnancy, stress, excessive exercise, PCOS, or thyroid dysfunction.
• Oligomenorrhea:
➤ Characterized by infrequent cycles (>35 days), often associated with anovulation or hormonal imbalances.
• Menorrhagia:
➤ Excessive menstrual bleeding (>80 mL) may lead to anemia and requires evaluation for fibroids or coagulopathies.
• Dysmenorrhea:
➤ Primary dysmenorrhea involves painful menstruation without underlying pathology, managed with NSAIDs.
➤ Secondary dysmenorrhea is associated with conditions like endometriosis or adenomyosis.
Nursing Insights:
• Nurses must conduct a thorough menstrual history, including cycle length, flow volume, and associated symptoms, to identify abnormalities.
• Patients with amenorrhea should be assessed for pregnancy first, followed by evaluation of hormonal or anatomical causes.
• Referral to a gynecologist is warranted for persistent irregularities or severe symptoms.
Patient Education on Reproductive Health
Effective patient education enhances reproductive health literacy and empowers women to make informed decisions.
• Fertility Awareness:
➤ Educate patients on tracking ovulation signs, such as cervical mucus changes and basal body temperature, to optimize conception.
➤ Explain the fertile window, typically 5 days before and 1 day after ovulation.
• Contraception:
➤ Discuss how hormonal contraceptives suppress ovulation and alter cervical mucus to prevent pregnancy.
➤ Address potential side effects, such as breakthrough bleeding or mood changes.
• Menstrual Hygiene:
➤ Advise on proper hygiene practices, such as changing sanitary products frequently, to prevent infections like toxic shock syndrome.
• Health Maintenance:
➤ Encourage regular gynecological exams and screening for conditions like PCOS or endometrial hyperplasia.
Nursing Insights:
• Nurses should use clear, non-judgmental language when discussing reproductive health to build trust with patients.
• Providing written materials or apps for tracking menstrual cycles can enhance patient compliance with fertility awareness methods.
• Cultural sensitivity is essential when addressing menstrual health, as beliefs and practices vary widely.
Nursing Considerations In Menstrual Cycle Management
Assessment and Monitoring
Accurate assessment of the menstrual cycle is critical for identifying abnormalities and guiding interventions.
• Menstrual History:
➤ Obtain a detailed history, including cycle length, duration, flow volume, and associated symptoms.
➤ Document age at menarche, regularity of cycles, and any recent changes.
• Physical Assessment:
➤ Perform a general assessment for signs of anemia, thyroid dysfunction, or hirsutism, which may indicate hormonal imbalances.
➤ Pelvic exams may be necessary to evaluate for structural abnormalities.
• Diagnostic Tests:
➤ Serum hormone levels (FSH, LH, estrogen, progesterone) can identify ovulatory dysfunction.
➤ Ultrasound may assess endometrial thickness or ovarian cysts.
Nursing Insights:
- Nurses should use standardized tools, such as menstrual cycle questionnaires, to ensure comprehensive data collection.
- Monitoring vital signs and hemoglobin levels is essential in patients with menorrhagia to detect anemia.
- Collaborate with healthcare providers to order appropriate diagnostic tests based on clinical findings.
Nursing Interventions
Nursing interventions focus on symptom management, patient education, and referral for specialized care.
• Symptom Management:
➤ Administer NSAIDs for dysmenorrhea, as prescribed, to reduce prostaglandin-induced pain.
➤ Provide iron supplementation for patients with menorrhagia-related anemia.
• Patient Support:
➤ Offer emotional support for patients experiencing menstrual irregularities, as they may cause anxiety or distress.
➤ Refer patients to counseling or support groups for conditions like PCOS or endometriosis.
• Health Promotion:
➤ Encourage a balanced diet, regular exercise, and stress management to support HPO axis function.
➤ Advise on smoking cessation and weight management to reduce menstrual irregularities.
Nursing Insights:
- Nurses should tailor interventions to the patient’s specific needs, considering cultural and socioeconomic factors.
- Educating patients about over-the-counter remedies, such as heating pads for cramps, can enhance comfort.
- Document all interventions and patient responses to ensure continuity of care.
Summary
The menstrual cycle is a highly regulated process involving the interplay of the hypothalamus, anterior pituitary, ovaries, and uterus through the HPO axis. Key hormones, including GnRH, FSH, LH, estrogen, progesterone, and inhibin, orchestrate follicular development, ovulation, and endometrial preparation. The ovarian cycle consists of the follicular, ovulatory, and luteal phases, while the uterine cycle includes the menstrual, proliferative, and secretory phases. Feedback mechanisms, both negative and positive, ensure precise hormonal control. Nurses must understand these processes to assess menstrual health, recognize deviations such as amenorrhea or menorrhagia, and provide patient education on fertility, contraception, and menstrual hygiene. Practical nursing interventions include symptom management, health promotion, and collaboration with healthcare providers to address abnormalities. Mastery of these concepts is essential for delivering evidence-based care to women across the reproductive lifespan.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on The Menstrual Cycle
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


