Please set your exam date
Oxygen Therapy and Respiratory Care (Oxygenation and Perfusion)
Study Questions
Introduction
A client with severe hypoxemia requires oxygen therapy. What is the appropriate delivery method for this client?
Explanation
Answer: d. Non-rebreather mask Explanation
A non-rebreather mask is the most suitable delivery method for a client with severe hypoxemia, as it provides the highest concentration of oxygen (up to 95%) by utilizing a reservoir bag and one-way valves to prevent the rebreathing of exhaled air.
Incorrect choices:
a. Nasal cannula delivers lower concentrations of oxygen and is more appropriate for clients with mild hypoxemia.
b. Simple face mask delivers moderate concentrations of oxygen and is suitable for clients with stable oxygen needs.
c. Venturi mask delivers precise concentrations of oxygen and is commonly used in clients with chronic respiratory conditions.
John: have a map of the level of serious of the illness and what device to use
When administering oxygen therapy, what should the nurse prioritize to ensure the safety of the client?
Explanation
Answer: b. Monitoring oxygen saturation levels Explanation:
Monitoring the client's oxygen saturation levels using a pulse oximeter is crucial to assess the effectiveness of oxygen therapy and ensure the client's oxygen needs are being met adequately.
Incorrect choices:
a. Assessing the client's respiratory rate is important but does not directly measure the adequacy of oxygen therapy.
c. Evaluating the client's level of dyspnea provides subjective information but does not quantify the client's oxygenation status.
d. Adjusting the oxygen flow rate as needed is a valid action, but monitoring oxygen saturation levels is essential to guide the adjustment accurately.
Which intervention should the nurse prioritize to promote effective airway clearance in a client with impaired oxygenation?
Explanation
Answer: c. Encouraging deep breathing and coughing Explanation:
Deep breathing and coughing help to mobilize and clear respiratory secretions, promoting effective airway clearance and improved oxygenation.
Incorrect choices:
a. Incentive spirometry exercises help promote lung expansion but are not directly aimed at airway clearance.
b. Bronchodilator medications are primarily used to alleviate bronchospasm and improve airflow, but they may not directly address airway clearance.
d. Positioning the client in high Fowler's position facilitates lung expansion and may improve oxygenation but does not directly address airway clearance.
A client with chronic obstructive pulmonary disease (COPD) is prescribed long-term oxygen therapy. What is the most important nursing consideration for this client?
Explanation
Answer: b. Monitoring the client's carbon dioxide levels
Explanation: Clients with COPD have a chronic retention of carbon dioxide, so monitoring carbon dioxide levels is essential to prevent the development of respiratory acidosis while providing long-term oxygen therapy.
Incorrect choices:
a. Assessing for signs of oxygen toxicity is important but is not specific to clients with COPD.
c. Proper humidification of oxygen is beneficial but does not take precedence over monitoring carbon dioxide levels in clients with COPD.
d.Ensuring an adequate supply of oxygen is a general consideration for all clients receiving oxygen therapy and is not specific to clients with COPD.
A client is receiving oxygen therapy via a nasal cannula. What is the appropriate flow rate for this client?
Explanation
Answer: b. 4-6 liters per minute
Explanation: The appropriate flow rate for oxygen therapy via a nasal cannula typically ranges from 1-6 liters per minute, with 4-6 liters per minute being a common range to achieve adequate oxygenation.
Incorrect choices:
a. 1-2 liters per minute may be appropriate for clients with mild hypoxemia or during rest.
c. 8-10 liters per minute is generally too high for a nasal cannula and may not be well-tolerated by the client.
d. 12-15 liters per minute is excessively high for a nasal cannula and may be more suitable for a higher flow oxygen delivery system such as a non-rebreather mask or Venturi mask.
Indications for Oxygen Therapy
A client with chronic obstructive pulmonary disease (COPD) presents with severe dyspnea and hypoxemia. What is the appropriate indication for initiating oxygen therapy in this client?
Explanation
Answer: d. Preventing complications of hypoxia
Explanation: Oxygen therapy is indicated in clients with COPD to prevent complications of hypoxia, such as tissue damage and respiratory failure.
Incorrect choices: a. Maintaining oxygen saturation above 95% is not the primary indication for oxygen therapy in clients with COPD. Target oxygen saturation levels may be lower due to the risk of suppressing the respiratory drive.
b. Correcting underlying lung pathology may require other interventions but does not solely indicate oxygen therapy.
c. Relieving shortness of breath may be a beneficial outcome of oxygen therapy, but it is not the primary indication in this case.
A client with pneumonia exhibits signs of respiratory distress and decreased oxygen saturation. What is the primary indication for initiating oxygen therapy in this client?
Explanation
Answer: c. Improving oxygen delivery to tissues
Explanation: In a client with pneumonia, the primary indication for oxygen therapy is to improve oxygen delivery to tissues and alleviate hypoxia.
Incorrect choices: a. Promoting lung expansion is a goal of oxygen therapy but is not the primary indication in this case.
b. Enhancing antimicrobial therapy is essential for treating pneumonia but is not directly related to the need for oxygen therapy.
d. Reducing the risk of bacterial resistance is not an indication for oxygen therapy but rather a consideration for appropriate antibiotic use.
A client with congestive heart failure (CHF) experiences worsening dyspnea and peripheral edema. What is the primary indication for initiating oxygen therapy in this client?
Explanation
Answer: d. Improving myocardial oxygenation
Explanation: In clients with CHF, the primary indication for oxygen therapy is to improve myocardial oxygenation and relieve symptoms of myocardial ischemia.
Incorrect choices: a. Reducing the workload of the heart is a potential benefit of oxygen therapy but is not the primary indication in this case.
b. Decreasing peripheral edema is not a direct indication for oxygen therapy.
c. Preventing fluid overload is important in managing CHF but does not directly relate to the need for oxygen therapy.
A client with anemia presents with fatigue and decreased exercise tolerance. What is the primary indication for initiating oxygen therapy in this client?
Explanation
Answer: a. Increasing oxygen-carrying capacity
Explanation: In a client with anemia, the primary indication for oxygen therapy is to increase the oxygen-carrying capacity of the blood and improve tissue oxygenation.
Incorrect choices:
b. Reducing iron deficiency is a necessary intervention for managing anemia but is not the primary indication for oxygen therapy.
c. Promoting tissue healing may be a general benefit of adequate oxygenation, but it is not the primary indication in this case.
d. Enhancing erythropoiesis is important for treating anemia but does not directly relate to the need for oxygen therapy
A client with a traumatic brain injury (TBI) develops altered mental status and decreased oxygen saturation. What is the primary indication for initiating oxygen therapy in this client?
Explanation
Answer: d. Ensuring adequate oxygen supply to the brain
Explanation: In a client with a traumatic brain injury, the primary indication for oxygen therapy is to ensure adequate oxygen supply to the brain and prevent further neurological damage.
Incorrect choices:
a. Preventing cerebral edema is an important goal in managing a TBI, but it is not the primary indication for oxygen therapy.
b. Improving neurological function may be an eventual outcome of adequate oxygenation, but it is not the primary indication in this case.
c. Stabilizing blood pressure is crucial in TBI management, but it does not directly relate to the need for oxygen therapy.
Oxygen Delivery Devices
A nurse is providing oxygen therapy to a client with chronic obstructive pulmonary disease (COPD). Which oxygen delivery system would be most appropriate for this client?
Explanation
Explanation: The Venturi mask is the most appropriate oxygen delivery system for clients with COPD as it provides a precise and controlled oxygen concentration. This system allows for a specific amount of room air to mix with oxygen, ensuring a precise oxygen level is delivered without the risk of excessive oxygen concentration.
Incorrect choices: a. Nasal cannula delivers a lower oxygen concentration and may not provide sufficient oxygen for clients with severe COPD.
c. Non-rebreather mask delivers a high concentration of oxygen, which can potentially worsen the client's condition by reducing respiratory drive.
d. Oxygen tent is not commonly used in COPD management and is typically reserved for pediatric clients or those with specific respiratory conditions.
A client with pneumonia requires oxygen therapy. Which oxygen delivery system would be most appropriate for this client to improve oxygenation and reduce the work of breathing?
Explanation
Answer: c. High-flow nasal cannula
Explanation: High-flow nasal cannula delivers a high flow rate of humidified oxygen and provides consistent oxygenation while reducing the work of breathing. It is effective in improving oxygenation in clients with pneumonia.
Incorrect choices: a. Simple face mask does not provide precise oxygen concentrations and may not be as effective in improving oxygenation as other options.
b. Partial rebreather mask is not typically used in pneumonia management as it may impede effective coughing and clearance of secretions.
d. Transtracheal catheter is a more invasive oxygen delivery method and is not commonly used in pneumonia management.
A client with acute respiratory distress syndrome (ARDS) requires high levels of positive end-expiratory pressure (PEEP). Which oxygen delivery system would be most effective in providing the necessary PEEP?
Explanation
Answer: c. Continuous positive airway pressure (CPAP) mask
Explanation: CPAP mask provides positive pressure throughout the respiratory cycle, including expiration, and is effective in delivering the necessary PEEP in clients with ARDS.
Incorrect choices: a. Non-rebreather mask does not provide positive pressure and is not the appropriate choice for delivering PEEP.
b. Venturi mask is not designed to provide PEEP.
d. Bag-valve-mask device is typically used for manual ventilation and resuscitation, not for delivering continuous positive pressure.
A nurse is caring for a client with severe hypoxemia and requires precise oxygen titration. Which oxygen delivery system would be most appropriate for this client?
Explanation
Answer: d. High-flow nasal cannula
Explanation: High-flow nasal cannula is effective in delivering precise oxygen concentrations and provides consistent oxygenation for clients with severe hypoxemia.
Incorrect choices: a. Simple face mask, non-rebreather mask, and partial rebreather mask do not provide precise control over oxygen concentrations and may not be as effective in delivering accurate oxygenation in severe hypoxemia.
A client with sleep apnea requires positive pressure ventilation duringsleep. Which oxygen delivery system would be most appropriate for this client to ensure continuous positive airway pressure (CPAP)?
Explanation
Answer: d. CPAP mask
Explanation: A CPAP mask is the most appropriate oxygen delivery system for a client with sleep apnea who requires positive pressure ventilation. It delivers a continuous flow of air or oxygen at a constant pressure to keep the airway open during sleep.
Incorrect choices:
a. Nasal cannula does not provide positive pressure ventilation and is not suitable for addressing sleep apnea.
b. Venturi mask and c. Non-rebreather mask are not designed to deliver positive pressure ventilation and are not commonly used for sleep apnea management.
Nursing Considerations for Oxygen Therapy
A nurse is providing oxygen therapy to a client. What is an important nursing consideration when applying a nasal cannula for oxygen delivery?
Explanation
Answer: d. Administering humidified oxygen through the cannula
Explanation: Humidified oxygen should be administered through a nasal cannula to prevent drying of the nasal passages and promote client comfort. It is important for the nurse to ensure the oxygen is properly humidified to prevent mucosal irritation.
Incorrect choices:
a. Securing the cannula tightly around the client's head may cause discomfort and impede circulation.
b. Placing the cannula in the client's mouth is not the correct placement for a nasal cannula.
c. Assessing the client's skin behind the ears for pressure ulcers is important when using devices that apply pressure, such as oxygen masks or headgear, but not specific to the nasal cannula.
A nurse is assessing a client receiving oxygen therapy via a non-rebreather mask. What should the nurse do to ensure the mask is functioning effectively?
Explanation
Answer: c. Inflate the reservoir bag prior to inhalation.
Explanation: The reservoir bag of a non-rebreather mask should be inflated to ensure an adequate oxygen supply during inhalation. The inflated bag provides a reservoir of oxygen-rich air that is delivered during each breath.
Incorrect choices:
a. Ensuring the reservoir bag is fully deflated during inhalation would limit the amount of oxygen available for the client.
b. Adjusting the oxygen flow rate to the highest setting may lead to excessive oxygen concentrations and is not necessary for effective mask functioning.
d. Removing the one-way valve from the mask would compromise the integrity of the non-rebreather system and prevent effective oxygen delivery.
A nurse is caring for a client receiving oxygen therapy via a venturi mask. What is an important nursing consideration for this client?
Explanation
Answer: b. Monitoring the client for signs of oxygen toxicity.
Explanation: Oxygen toxicity can occur with prolonged exposure to high levels of oxygen. The nurse should closely monitor the client for signs of oxygen toxicity, such as substernal pain, respiratory distress, and changes in mental status.
Incorrect choices: a. Assessing the client's respiratory rate hourly is a general nursing assessment and not specific to venturi mask therapy.
c. Administering supplemental oxygen as needed is the purpose of providing oxygen therapy and is not a specific consideration for the venturi mask.
d. Ensuring the mask fits tightly over the client's nose and mouth is important for mask effectiveness but is not specific to the venturi mask.
A nurse is providing oxygen therapy to a client using a face mask. What is an important nursing consideration for this client?
Explanation
Answer: d. Assessing the client for skin breakdown around the mask.
Explanation: When using a face mask for oxygen therapy, the nurse should assess the client's skin for any signs of irritation or breakdown due to prolonged mask use. It is important to ensure proper mask fit and periodically assess the skin integrity to prevent pressure ulcers or skin breakdown.
Incorrect choices:
a. Encouraging the client to remove the mask during meals may compromise oxygen delivery and is not recommended unless otherwise specified by the healthcare provider.
b. Adjusting the mask to cover the client's mouth only may not provide adequate oxygen delivery and is not the correct technique for using a face mask.
c. Checking the client's oxygen saturation every 4 hours is a general nursing assessment and not specific to face mask oxygen therapy. The frequency of oxygen saturation monitoring should be based on the client's condition and healthcare provider's orders.
A nurse is caring for a client receiving oxygen therapy through a transtracheal catheter. What is an important nursing consideration for this client?
Explanation
c. The nurse should closely monitor the client for signs of oxygen toxicity, such as substernal pain, respiratory distress, and changes in mental status.
Incorrect choices:
a. Ensuring the catheter is placed in the client's nostrils is incorrect as a transtracheal catheter is inserted directly into the trachea, bypassing the nose.
b. Assessing the client's respiratory rate every 15 minutes is too frequent for routine assessment and may disrupt the client's care.
d. While teaching coughing and deep breathing techniques can be important for clients with respiratory issues, it is not the most immediate or critical nursing consideration for clients using a transtracheal catheter.
Complications and Interventions
A nurse is caring for a client receiving high-flow oxygen therapy via a noninvasive positive pressure ventilation (NPPV) device. What is an important nursing intervention for this client?
Explanation
Answer: c. Providing frequent oral care to prevent dry mouth.
Explanation: NPPV devices, such as continuous positive airway pressure (CPAP) or bilevel positive airway pressure (BiPAP), can cause dry mouth. Providing frequent oral care, such as mouth rinses and moisturizing agents, helps alleviate discomfort and prevent oral complications.
Incorrect choices: a. Assessing the client's oxygen saturation every 4 hours is not specific to NPPV therapy and does not address the unique nursing intervention required for this intervention.
b. Monitoring the client's respiratory rate every 15 minutes may not be necessary for all clients receiving NPPV therapy and should be based on the client's condition and healthcare provider's orders.
d. Administering oxygen at a flow rate of 1-2 L/min is not appropriate for NPPV therapy, which delivers a higher flow of pressurized air to support ventilation.
A nurse is caring for a client receiving oxygen therapy via a nasal cannula. What is an important complication associated with prolonged use of a nasal cannula?
Explanation
Answer: a. Dry nasal passages
Explanation: Prolonged use of a nasal cannula can lead to dryness and discomfort in the nasal passages due to the direct flow of oxygen. The nurse should provide humidification to prevent or alleviate dryness and nasal irritation.
Incorrect choices: b. Hypoventilation is not a common complication associated with the use of a nasal cannula, which is a low-flow oxygen delivery device.
c. Hyperoxygenation refers to an excessive supply of oxygen, which is not typically associated with nasal cannula use, as the flow rate is relatively low.
d. Increased risk of infection is not directly associated with nasal cannula use. However, proper infection control practices should be followed during oxygen therapy to minimize the risk of infection.
A nurse is caring for a client receiving oxygen therapy via a mask. What is an important nursing intervention to prevent pressure ulcers on the client's face?
Explanation
Answer: c. Placing padding between the mask and the client's skin.
Explanation: Placing padding between the oxygen mask and the client's skin helps distribute pressure and reduce the risk of pressure ulcers. It provides a cushioning effect and helps prevent direct contact between the mask and the skin.
Incorrect choices: a. Frequently adjusting the mask to relieve pressure may disrupt the proper fit and seal of the mask, leading to ineffective oxygen delivery.
b. Applying petroleum jelly to the areas of skin contact is not recommended as it may interfere with the mask's fit and compromise oxygen delivery.
d. Assessing the client's facial skin integrity regularly is important but does not directly address the prevention of pressure ulcers. Placing padding is a proactive measure to prevent skin breakdown.
A nurse is caring for a client receiving oxygen therapy via a non-rebreather mask. What is an important nursing intervention for this client?
Explanation
Answer: a. Ensuring the reservoir bag remains inflated at all times.
Explanation: The nurse should ensure that the reservoir bag attached to the non-rebreather mask remains inflated at all times. The inflated bag provides a reservoir of oxygen and ensures a high concentration of oxygen is delivered to the client during inhalation.
Incorrect choices: b. Adjusting the oxygen flow rate based on the client's preference is not appropriate without healthcare provider orders. The flow rate should be prescribed based on the client's oxygen needs.
c. Checking the client's oxygen saturation every 2 hours may not be necessary for all clients receiving oxygen therapy via a non-rebreather mask. The frequency of oxygen saturation monitoring should be based on the client's condition and healthcare provider's orders.
d. Encouraging the client to remove the mask during meals is not recommended unless otherwise specified by the healthcare provider. Removing the mask during meals may compromise oxygen delivery and should be avoided.
A nurse is caring for a client receiving oxygen therapy via a Venturi mask. What is an important nursing intervention for this client?
Explanation
Answer: b. Adjusting the oxygen flow rate as prescribed.
Explanation: The nurse should adjust the oxygen flow rate on the Venturi mask according to the prescribed percentage of inspired oxygen (FiO2). The specific flow rate and FiO2 will be specified in the healthcare provider's orders.
Incorrect choices: a. Monitoring the client's oxygen saturation continuously may not be necessary for all clients receiving oxygen therapy via a Venturi mask. The frequency of oxygen saturation monitoring should be based on the client's condition and healthcare provider's orders.
c. Assessing the client's lung sounds every shift is a general nursing assessment and may not be directly related to the use of a Venturi mask.
d. Placing the mask loosely over the client's face may compromise the delivery of the precise FiO2 and should be avoided. The mask should be properly secured to ensure accurate oxygen administration.
More Questions on This Topic
When administering oxygen therapy, which intervention should the nurse prioritize to ensure the delivery of the prescribed oxygen concentration?
Explanation
Answer: c. Monitoring the client's oxygen saturation continuously.
Explanation: Continuous monitoring of the client's oxygen saturation allows the nurse to assess the effectiveness of oxygen therapy and ensure the prescribed oxygen concentration is being delivered. It helps in making timely adjustments to the oxygen therapy to maintain adequate oxygenation.
Incorrect choices: a. Assessing the client's respiratory rate every hour is important but does not directly ensure the delivery of the prescribed oxygen concentration.
b. Checking the oxygen flow rate every 4 hours is important for monitoring equipment functionality but does not directly ensure the delivery of the prescribed oxygen concentration.
d. Adjusting the oxygen mask snugly on the client's face is important for proper fit and oxygen delivery, but it does not directly ensure the delivery of the prescribed oxygen concentration.
Which statement by a client on oxygen therapy indicates the need for further education?
Explanation
Answer: b. "I will secure the oxygen tubing under furniture legs."
Explanation: Securing the oxygen tubing under furniture legs can create a potential safety hazard by causing the tubing to become twisted or pulled, disrupting the oxygen flow. It is important to educate the client about keeping the tubing free from obstructions and ensuring it is positioned safely.
Incorrect choices: a. "I should avoid smoking while using oxygen" is a correct statement, as smoking near oxygen can be extremely dangerous and increase the risk of fire.
c. "I will keep the oxygen equipment away from open flames" is a correct statement, as oxygen supports combustion and can cause a fire if exposed to open flames.
d. "I will use a water-based moisturizer for dry nasal passages" is a correct statement, as oxygen therapy can cause dryness in the nasal passages, and using a water-based moisturizer can help alleviate discomfort.
When caring for a client receiving oxygen therapy, the nurse identifies condensation in the oxygen tubing. What action should the nurse take?
Explanation
Answer: b. Disconnect the tubing and drain the condensation.
Explanation: Condensation in the oxygen tubing can impede the flow of oxygen and reduce the effectiveness of oxygen therapy. The nurse should disconnect the tubing and drain the condensation before reconnecting and continuing oxygen therapy.
Incorrect choices: a. Increasing the oxygen flow rate does not address the issue of condensation and may lead to unnecessary oxygen supplementation.
c. Replacing the oxygen tubing with a new one immediately may not be necessary if the condensation can be resolved by draining it.
d. Placing a heat-moisture exchanger (HME) on the oxygen tubing is not necessary for managing condensation but can be used to provide humidification for clients receiving high-flow oxygen therapy.
The nurse is caring for a client receiving oxygen therapy via a simple face mask. Which nursing intervention is important to prevent skin breakdown?
Explanation
Answer: c. Padding the pressure points on the client's face with soft material.
Explanation: Oxygen masks, especially those that exert pressure on specific areas of the face, can cause skin breakdown and pressure ulcers. Padding the pressure points with soft material helps distribute the pressure more evenly and reduces the risk of skin damage.
Incorrect choices: a. Changing the position of the mask every 2 hours is important for preventing pressure ulcers related to prolonged pressure on the skin but may not directly address the pressure points created by the mask.
b. Applying a protective barrier cream to the client's face is not specifically indicated for preventing pressure ulcers caused by oxygen masks. It is more commonly used for preventing moisture-associated skin damage.
d. Encouraging the client to remove the mask intermittently for facial skin care may compromise oxygen delivery and is not recommended unless otherwise specified by the healthcare provider.
The nurse is caring for a client receiving oxygen therapy via a nasal cannula. Which action by the nurse is appropriate when providing oral care to the client?
Explanation
Answer: a. Removing the nasal cannula during oral care.
Explanation: To ensure effective oral care, the nurse should temporarily remove the nasal cannula while performing oral care procedures. This allows better access to the client's mouth and prevents interference with oral hygiene.
Incorrect choices: b. Increasing the oxygen flow rate during oral care is not necessary and may lead to unnecessary oxygen supplementation.
c. Applying petroleum jelly to the client's lips before oral care may be helpful for preventing dryness and chapping but is not directly related to the administration of oral care.
d. Instructing the client to breathe through the mouth during oral care is not necessary if the nasal cannula is temporarily removed to facilitate oral hygiene.
The nurse is caring for a client with chronic obstructive pulmonary disease (COPD) receiving long-term oxygen therapy at home. What should the nurse include in the client's teaching regarding oxygen safety?
Explanation
Answer: c. "Avoid using electric heating devices in your home."
Explanation: Oxygen supports combustion, and using electric heating devices in the presence of oxygen therapy can pose a significant fire hazard. It is important to educate clients with long-term oxygen therapy about the importance of avoiding open flames and electric heating devices to ensure their safety.
Incorrect choices: a. Ensuring a fire extinguisher is readily available is a good general safety practice but may not directly address the specific risk associated with oxygen therapy.
b. Keeping the oxygen tubing loose may increase the risk of tangling and accidental disconnection. The tubing should be appropriately secured and free from obstructions.
d. Using an oxygen concentrator for outdoor activities may not be necessary for all clients and should be based on individual needs and healthcare provider recommendations.
The nurse is assessing a client who is receiving high-flow oxygen therapy via a non-rebreather mask. Which finding requires immediate intervention?
Explanation
Answer: d. Loose fit of the mask on the client's face.
Explanation: A loose fit of the mask on the client's face can result in a significant reduction in the delivery of high-flow oxygen therapy. It is essential to ensure a proper seal and fit of the mask to maximize the effectiveness of oxygen therapy. Immediate intervention is needed to readjust and secure the mask properly.
Incorrect choices: a. An oxygen flow rate of 10 L/min may be appropriate for high-flow oxygen therapy, depending on the client's condition and prescribed treatment.
b. An oxygen saturation of 95% indicates adequate oxygenation and is within the target range for most clients.
c. Condensation in the mask can be managed by draining it appropriately and does not necessarily require immediate intervention unless it significantly obstructs oxygen flow.
The nurse is caring for a client with a tracheostomy receiving oxygen therapy. Which intervention should the nurse prioritize to prevent infection and ensure proper oxygen delivery?
Explanation
Answer: c. Applying a sterile dressing over the tracheostomy site.
Explanation: Applying a sterile dressing over the tracheostomy site helps prevent infection by providing a barrier against microorganisms. It also ensures a clean environment for optimal oxygen delivery and promotes wound healing.
Incorrect choices: a. Regularly suctioning the tracheostomy tube is important for maintaining airway patency but may not directly address infection prevention or oxygen delivery.
b. Assessing the client's respiratory rate every hour is important for monitoring respiratory status but does not specifically address infection prevention or oxygen delivery.
d. Administering humidified oxygen through the tracheostomy tube may be necessary to provide moistened air to the client's lungs but does not directly address infection prevention.
The nurse is caring for a client receiving oxygen therapy via a Venturi mask. Which assessment finding indicates the need for adjustment of the oxygen flow rate?
Explanation
Answer: c. Client reporting nasal dryness and discomfort.
Explanation: The client reporting nasal dryness and discomfort indicates inadequate humidification of the oxygen. The nurse should assess and adjust the oxygen flow rate or consider providing humidified oxygen to alleviate the client's discomfort.
Incorrect choices: a. An oxygen saturation of 98% indicates adequate oxygenation and does not necessitate an adjustment in the oxygen flow rate.
b. A respiratory rate of 16 breaths per minute within the normal range does not indicate a need for adjustment of the oxygen flow rate.
d. An oxygen flow rate set at 4 L/min may be appropriate for a Venturi mask, depending on the prescribed oxygen concentration and the client's needs.
The nurse is caring for a client receiving oxygen therapy via a face tent. Which action by the nurse is important to ensure proper oxygen delivery?
Explanation
Answer: c. Frequently checking for condensation inside the face tent.
Explanation: Checking for condensation inside the face tent is important to ensure that the oxygen is effectively delivered to the client. Condensation can obstruct the flow ofoxygen and reduce its effectiveness. The nurse should frequently check for condensation and take appropriate measures to maintain proper oxygen delivery.
Incorrect choices: a. Adjusting the face tent to fit snugly around the client's face may cause discomfort and impede proper oxygen delivery. The face tent should be loosely fitted to allow adequate airflow.
b. Ensuring the client breathes through the nose during oxygen therapy is not necessary with a face tent, as it covers both the nose and mouth, allowing the client to breathe through either.
d. Monitoring the client's oxygen saturation every 8 hours is not frequent enough for clients receiving oxygen therapy. Continuous or regular monitoring is typically necessary to assess the effectiveness of oxygen therapy and adjust as needed.
Exams on Oxygen Therapy and Respiratory Care (Oxygenation and Perfusion)
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
Notes Highlighting is available once you sign in. Login Here.
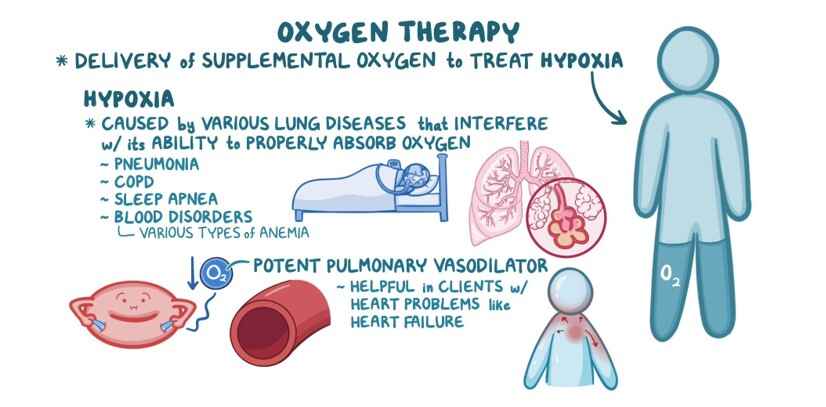
Introduction
Oxygen therapy is a crucial component of respiratory care, aimed at improving oxygenation and perfusion in clients with various respiratory conditions or inadequate oxygen levels.
The goal of oxygen therapy is to maintain adequate oxygen saturation in tissues and organs, ensuring proper cellular function and preventing hypoxia-related complications. Nurses play a vital role in assessing clients, administering oxygen, and monitoring their response to therapy.
Indications for Oxygen Therapy
- Hypoxemia: Low arterial oxygen levels, defined as PaO2 < 60 mm Hg or SaO2 < 90% on room air.
- Respiratory Distress: Clients experiencing difficulty breathing or respiratory failure.
- Acute or Chronic Respiratory Conditions: Such as pneumonia, chronic obstructive pulmonary disease (COPD), asthma, and acute respiratory distress syndrome (ARDS).
- Cardiovascular Conditions: Clients with heart failure or other cardiac issues that can lead to decreased tissue oxygenation.
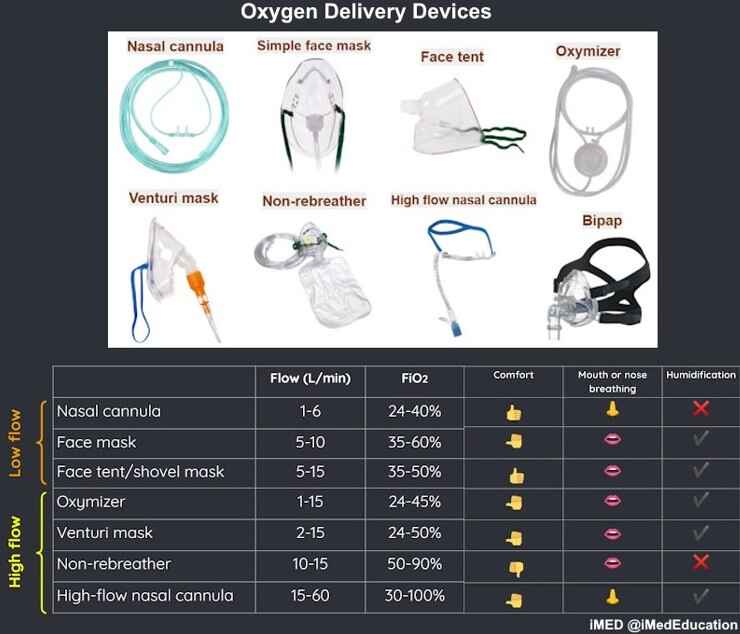
Oxygen Delivery Devices
Various oxygen delivery devices are available, depending on the client's condition and needs:
- Nasal Cannula: Low-flow device delivering 1-6 L/min, providing 24-44% oxygen concentration.
- Simple Face Mask: Moderate-flow device delivering 5-10 L/min, providing approximately 40-60% oxygen concentration.
- Venturi Mask: High-flow device with specific adapters delivering precise oxygen concentrations (24-60%) based on color-coded valves.
- Non-Rebreather Mask: High-flow device with a reservoir bag ensuring the client breathes pure oxygen, delivering 60-100% oxygen concentration.
- High-Flow Nasal Cannula (HFNC): Delivers heated and humidified oxygen at flow rates of up to 60 L/min, maintaining constant oxygen concentration and reducing airway resistance.
Nursing Considerations for Oxygen Therapy
- Oxygen Assessment: Regularly monitor oxygen saturation (SpO2) using pulse oximetry, and assess respiratory rate, depth, and effort.
- Safety Precautions: Avoid smoking or open flames near oxygen sources due to increased fire risk.
- Humidification: Consider adding humidification to high-flow oxygen delivery systems to prevent mucosal drying and irritation.
- Mobility: Ensure safe mobility with portable oxygen delivery systems or cylinders.
- Monitoring: Continuously assess client response to therapy, looking for signs of improvement or deterioration.
- Education: Educate clients and their families about proper use, maintenance, and potential risks associated with oxygen therapy.
Complications and Interventions
- Oxygen Toxicity: High FiO2 levels (> 50%) for extended periods can cause lung damage. Adjust oxygen levels as prescribed.
- Hypoventilation: Monitor for signs of hypoventilation (e.g., confusion, cyanosis) in clients with chronic hypercapnia and COPD.
- Dry Mucous Membranes: Provide humidification to prevent dryness and discomfort.
- Skin Breakdown: Inspect the skin around nasal cannulas or masks regularly and use skin protectants to prevent breakdown.
- Carbon Dioxide Narcosis: In clients with chronic hypercapnia, high levels of oxygen may reduce the respiratory drive. Monitor for signs of hypoventilation.
Conclusion
Oxygen therapy is a fundamental aspect of respiratory care, aimed at maintaining adequate oxygenation and perfusion in clients with respiratory or cardiac conditions. Nurses should be knowledgeable about the different oxygen delivery devices, client assessment, and potential complications. By providing appropriate oxygen therapy, nurses can significantly improve client outcomes and enhance overall respiratory function. Regular monitoring, prompt interventions, and client education are essential
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Oxygen Therapy and Respiratory Care (Oxygenation and Perfusion)
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


