Please set your exam date
Adverse Drug Reactions and Side Effects
Study Questions
Introduction
A nurse is reviewing the medication list of a client who has a history of allergic reactions to penicillin and sulfa drugs. The nurse should identify that which of the following medications is contraindicated for this client?
Explanation
Answer: A. Cefazolin is a cephalosporin antibiotic that has a cross-sensitivity with penicillin and should be avoided by clients who are allergic to penicillin.
B is incorrect because ciprofloxacin does not have cross-sensitivity with penicillin or sulfa drugs and can be safely administered to this client.
C is incorrect because vancomycin does not have cross-sensitivity with penicillin or sulfa drugs and can be safely administered to this client.
D is incorrect because Azithromycin does not have cross-sensitivity with penicillin or sulfa drugs and can be safely administered to this client.
A client who is receiving intravenous amphotericin B for a fungal infection reports feeling dizzy and having chills and fever. The nurse should recognize that these manifestations indicate which of the following adverse reactions?
Explanation
Infusion reaction is a common adverse effect of amphotericin B that occurs within 1 to 3 hours of starting the infusion and causes symptoms such as fever, chills, headache, nausea, vomiting, and hypotension.
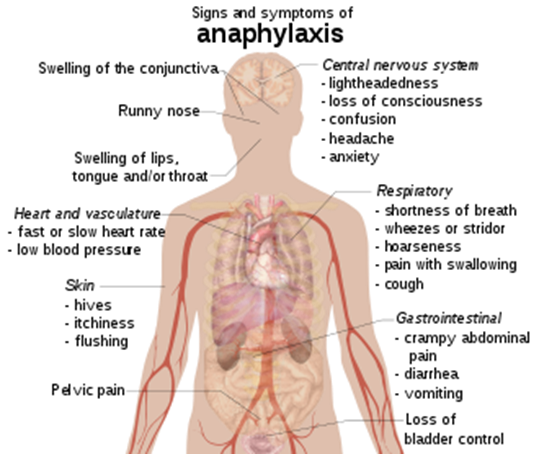
A is incorrect because anaphylaxis is a severe allergic reaction that causes symptoms such as urticaria, angioedema, bronchospasm, and shock.
C is incorrect because nephrotoxicity is another adverse effect of amphotericin B that causes renal impairment and electrolyte imbalances.
D is incorrect because ototoxicity is an adverse effect of some antibiotics such as gentamicin and vancomycin that causes hearing loss and tinnitus.
A nurse is preparing to administer epinephrine to a client who is experiencing anaphylaxis after a bee sting. The nurse should administer the medication by which of the following routes?
Explanation
Intramuscular injection is the preferred route for administering epinephrine in anaphylaxis because it provides rapid absorption and onset of action.
B is incorrect because subcutaneous injection has a slower absorption rate than intramuscular injection and may not provide adequate relief in an emergency situation.
C is incorrect because intravenous injection of epinephrine can cause severe adverse effects such as cardiac arrhythmias and hypertension and should be reserved for life-threatening situations when other routes are ineffective.
D is incorrect because oral administration of epinephrine is ineffective due to extensive first-pass metabolism in the liver.
A client who has a peanut allergy accidentally ingested a cookie that contained peanut butter. The client reports feeling anxious, having difficulty breathing, and having a tingling sensation in the mouth. The nurse should identify that these manifestations indicate which of the following types of hypersensitivity reactions?
Explanation
Type I hypersensitivity reaction is also known as immediate hypersensitivity or anaphylaxis and occurs within minutes of exposure to an allergen. It involves the activation of mast cells and basophils that release histamine and other inflammatory mediators that cause vasodilation, bronchoconstriction, edema, and pruritus.
B is incorrect because Type II hypersensitivity reaction is also known as cytotoxic hypersensitivity or antibody-mediated hypersensitivity and occurs when antibodies bind to antigens on the surface of cells and cause cell lysis or damage. An example of this type of reaction is hemolytic transfusion reaction.
C is incorrect because Type III hypersensitivity reaction is also known as immune complex-mediated hypersensitivity and occurs when antigen-antibody complexes deposit in tissues and cause inflammation and tissue damage. An example of this type of reaction is serum sickness.
D is incorrect because Type IV hypersensitivity reaction is also known as delayed hypersensitivity or cell-mediated hypersensitivity and occurs when sensitized T cells react with antigens and release cytokines that activate macrophages and cause inflammation and tissue damage. An example of this type of reaction is contact dermatitis.
A nurse is caring for a client who has a severe allergic reaction to a medication and requires immediate administration of diphenhydramine. The nurse should administer the medication by which of the following routes?
Explanation
Answer: C. Intravenous injection is the fastest route for administering diphenhydramine in a severe allergic reaction because it provides immediate onset of action and avoids the first-pass metabolism in the liver.
A and B are incorrect because intramuscular and subcutaneous injections have slower absorption rates than intravenous injection and may not provide adequate relief in an emergency situation.
D is incorrect because oral administration of diphenhydramine has the slowest absorption rate and onset of action and is subject to first-pass metabolism in the liver.
A client who is receiving a blood transfusion develops a fever, chills, headache, and back pain. The nurse should suspect that the client is experiencing which of the following types of transfusion reactions?
Explanation
B. Febrile transfusion reaction is a common type of transfusion reaction that occurs when the recipient's antibodies react with the donor's leukocytes and cause fever, chills, headache, and malaise.
A is incorrect because hemolytic transfusion reaction is a rare but serious type of transfusion reaction that occurs when the recipient's antibodies react with the donor's erythrocytes and cause hemolysis, hemoglobinuria, hypotension, tachycardia, and renal failure.
C is incorrect because allergic transfusion reaction is a type of transfusion reaction that occurs when the recipient's antibodies react with the donor's plasma proteins and cause urticaria, pruritus, angioedema, and anaphylaxis.
D is incorrect because circulatory overload is a type of transfusion complication that occurs when the infusion rate exceeds the recipient's cardiac output and causes dyspnea, orthopnea, crackles, tachycardia, hypertension, and pulmonary edema.
A nurse is teaching a client who has a history of anaphylaxis about the use of an epinephrine auto-injector. Which of the following instructions should the nurse include in the teaching?
Explanation
Holding the device at a 90-degree angle to the thigh ensures proper penetration and delivery of the medication into the vastus lateralis muscle.
A is incorrect because injecting the medication into the deltoid muscle may not provide adequate absorption and onset of action.
C is incorrect because massaging the injection site may increase the risk of bleeding and bruising and may decrease the absorption of the medication.
D is incorrect because repeating the injection after 5 minutes may cause overdose and adverse effects such as hypertension, tachycardia, arrhythmias, and myocardial ischemia.
Causes and risk factors
A nurse is caring for a client who has a history of allergic reactions to penicillin. The client is prescribed cefazolin for a wound infection. Which of the following actions should the nurse take before administering the medication?
Explanation
Rationale: Cefazolin is a cephalosporin, which has a cross-sensitivity with penicillin. Therefore, the nurse should ask the client about any previous reactions to cephalosporins before administering the medication. This can help identify clients who are at risk of developing an allergic reaction to cefazolin.
B) is incorrect because administering an antihistamine is not a preventive measure for an allergic reaction, but rather a treatment for mild symptoms. Antihistamines do not prevent anaphylaxis, which is a life-threatening reaction that requires immediate intervention.
C) is incorrect because monitoring the client's vital signs for 15 minutes after the injection is not enough to detect an allergic reaction, which can occur up to 72 hours after exposure. The nurse should monitor the client for signs and symptoms of an allergic reaction throughout the course of therapy.
D) is incorrect because diluting the medication with normal saline does not reduce the risk of an allergic reaction, but rather the risk of phlebitis, which is inflammation of the vein. Phlebitis is a common adverse reaction to cefazolin, but it is not related to allergy.
A client is admitted to the emergency department with signs of anaphylaxis after being stung by a bee. The nurse should expect to administer which of the following medications first?
Explanation
Rationale: Epinephrine is the first-line medication for anaphylaxis, which is a severe allergic reaction that can cause bronchoconstriction, hypotension, and shock. Epinephrine acts as a bronchodilator and a vasoconstrictor, reversing the effects of histamine and other mediators released during anaphylaxis.
B) is incorrect because diphenhydramine is an antihistamine that can help relieve itching, hives, and urticaria, but it does not reverse bronchoconstriction or hypotension. Diphenhydramine can be given as an adjunct therapy after epinephrine.
C) is incorrect because albuterol is a beta2 agonist that can help relieve bronchospasm, but it does not affect blood pressure or other systemic effects of anaphylaxis. Albuterol can be given as an adjunct therapy after epinephrine.
D) is incorrect because hydrocortisone is a corticosteroid that can help reduce inflammation and prevent delayed reactions, but it does not have an immediate effect on anaphylaxis. Hydrocortisone can be given as an adjunct therapy after epinephrine.
A nurse is teaching a client who has a new prescription for warfarin about potential drug interactions. Which of the following over-the-counter medications should the nurse instruct the client to avoid?
Explanation
Rationale: Ibuprofen is a nonsteroidal anti-inflammatory drug (NSAID) that can increase the risk of bleeding when taken with warfarin, which is an anticoagulant. NSAIDs inhibit platelet aggregation and interfere with warfarin metabolism, leading to increased levels of warfarin and prolonged prothrombin time (PT) and international normalized ratio (INR).
A) is incorrect because acetaminophen is an analgesic and antipyretic that does not affect platelet function or warfarin metabolism. However, high doses or chronic use of acetaminophen can increase INR and cause liver toxicity, so the nurse should advise the client to limit acetaminophen intake and monitor liver function tests.
C) is incorrect because loratadine is an antihistamine that does not interact with warfarin or affect bleeding. Loratadine can be used safely by clients who have allergies and are taking warfarin.
D) is incorrect because calcium carbonate is an antacid and a calcium supplement that does not interact with warfarin or affect bleeding. However, calcium carbonate can interfere with the absorption of other medications, so the nurse should instruct the client to take it at least 2 hours before or after other medications.
A nurse is reviewing the medication list of a client who has hypertension and diabetes mellitus. The client reports experiencing a dry cough for several weeks. The nurse should identify that this adverse reaction is most likely caused by which of the following medications?
Explanation
Rationale: Lisinopril is an angiotensin-converting enzyme (ACE) inhibitor that can cause a dry, persistent cough as a common adverse reaction. The cough is due to the accumulation of bradykinin, which is a vasodilator and an inflammatory mediator that is normally degraded by ACE. The cough usually resolves after discontinuing the medication.
B) is incorrect because metformin is an antidiabetic agent that does not cause a cough as an adverse reaction. The most common adverse reactions of metformin are gastrointestinal disturbances, such as nausea, vomiting, diarrhea, and abdominal pain.
C) is incorrect because atenolol is a beta blocker that does not cause a cough as an adverse reaction. The most common adverse reactions of atenolol are bradycardia, hypotension, fatigue, and dizziness.
D) is incorrect because glipizide is a sulfonylurea that does not cause a cough as an adverse reaction. The most common adverse reactions of glipizide are hypoglycemia, weight gain, and skin rash.
A nurse is preparing to administer amoxicillin to a client who has a respiratory infection. The client states that he is allergic to penicillin and shows the nurse a medical alert bracelet. Which of the following actions should the nurse take?
Explanation
Amoxicillin is a penicillin derivative that has a high cross-reactivity with penicillin. Therefore, the nurse should hold the medication and notify the provider of the client's allergy. The provider may prescribe an alternative antibiotic that belongs to a different class, such as a macrolide or a fluoroquinolone.
A) is incorrect because administering the medication as prescribed and monitoring for signs of an allergic reaction can put the client at risk of developing a serious or life-threatening reaction, such as anaphylaxis. The nurse should not administer any medication that the client is allergic to.
C) is incorrect because asking the client about the type and severity of his allergic reaction to penicillin is not enough to prevent an allergic reaction to amoxicillin. Even if the client had a mild reaction to penicillin in the past, he may have a severe reaction to amoxicillin in the present. The nurse should avoid giving any medication that has cross-sensitivity with penicillin.
D) is incorrect because administering an antihistamine before giving the medication to prevent an allergic reaction is not a safe or effective practice. Antihistamines do not prevent anaphylaxis, which is a life-threatening reaction that requires immediate intervention. Antihistamines can also mask some signs of an allergic reaction, such as itching and hives, making it harder to detect and treat.
A nurse is assessing a client for risk factors of anaphylaxis. Which of the following factors should the nurse consider?
No explanation
A client asks the nurse about the risk factors associated with allergic reactions to medications. Which response by the nurse is correct?
Explanation
Correct answer: Option D. Previous exposure to a medication is a significant risk factor for developing an allergic reaction. Sensitization to a particular medication can occur after the initial exposure, leading to an allergic response upon subsequent use.
Incorrect choices:
Option A: Age and gender are not direct risk factors for developing allergic reactions to medications.
Option B: Body weight is not directly related to the risk of allergic reactions to medications.
Option C: Dietary preferences may affect other aspects of health but are not directly associated with the risk of allergic reactions to medications.
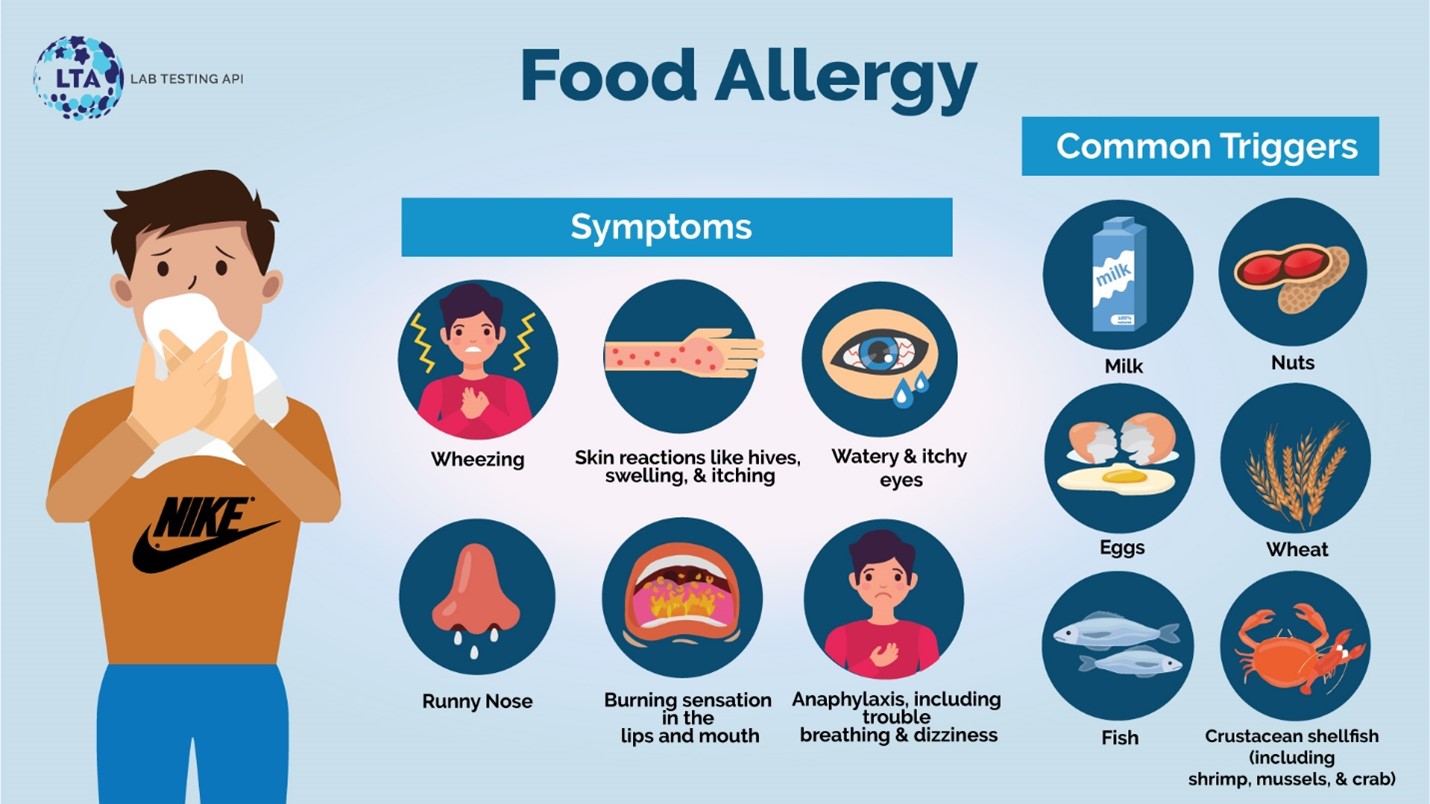
Signs and symptoms
A nurse is teaching a client who has a new prescription for warfarin about potential adverse effects of the medication. Which of the following statements by the client indicates an understanding of the teaching?
Explanation
- Correct answer: A) "I will report any signs of bleeding to my provider.": This statement indicates that the client understands the potential adverse effect of warfarin, which is an anticoagulant medication. The most significant concern with warfarin therapy is the risk of bleeding, so it is crucial for the client to promptly report any signs of bleeding to their healthcare provider.
- Incorrect answers:
- B) "I will take an antacid if I have stomach upset.": Antacids are not related to the adverse effects ofwarfarin. Stomach upset is not a commonly reported adverse effect of warfarin.
- C) "I will increase my intake of green leafy vegetables.": Increasing the intake of green leafy vegetables is not recommended for clients taking warfarin because these foods are high in vitamin K, which can interfere with the medication's anticoagulant effect.
- D) "I will use a heating pad for muscle aches.": Muscle aches are not a common adverse effect of warfarin. Using a heating pad would not address this medication-related concern.
A nurse is reviewing the medication administration record of a client who is receiving digoxin for heart failure. The nurse should identify that which of the following medications can increase the risk of digoxin toxicity in this client?
Explanation
Correct answer: D) Verapamil: Verapamil, a calcium channel blocker, can increase digoxin levels by inhibiting its clearance. This interaction can lead to digoxin toxicity, which manifests as symptoms such as nausea, vomiting, visual disturbances, and cardiac arrhythmias.
A) Furosemide: Furosemide, a loop diuretic, can cause electrolyte imbalances, but it does not directly increase the risk of digoxin toxicity.
B) Metoprolol: Metoprolol, a beta-blocker, does not have a significant interaction with digoxin that increases the risk of toxicity.
C) Lisinopril: Lisinopril, an angiotensin-converting enzyme (ACE) inhibitor, does not have a significant interaction with digoxin that increases the risk of toxicity.
A nurse is administering amoxicillin to a client who has a sinus infection. The client reports itching and difficulty breathing. The nurse should suspect that the client is experiencing which of the following types of adverse reactions?
Explanation
- Correct answer: B) Allergic reaction: The client's symptoms of itching and difficulty breathing are indicative of an allergic reaction. Allergic reactions occur when the immune system recognizes a drug as a foreign substance and launches an immune response, resulting in symptoms such as itching, hives, rash, and respiratory distress.
- Incorrect answers:
- A) Idiosyncratic reaction: Idiosyncratic reactions are unpredictable and
uncommon responses to a medication that is unrelated to the medication's known pharmacological effects. They do not typically manifest as itching and difficulty breathing.
- C) Teratogenic reaction: Teratogenic reactions refer to the harmful effects of medications on a developing fetus during pregnancy and are not applicable in this situation.
- D) Toxic reaction: Toxic reactions occur when a medication accumulates to toxic levels in the body. The symptoms described by the client are more consistent with an allergic reaction than a toxic reaction.
A nurse is providing discharge instructions to a client who has a new prescription for phenytoin for seizure control. The nurse should instruct the client to report which of the following adverse effects of phenytoin to the provider?
Explanation
- Correct answer: A) Gingival hyperplasia: Phenytoin is known to cause gingival hyperplasia, an overgrowth of gum tissue. This side effect should be reported to the provider for appropriate management.
- Incorrect answers:
- B) Diarrhea: Diarrhea is not a common adverse effect of phenytoin. It is not necessary to report it to the provider unless it becomes severe or persistent.
- C) Insomnia: Insomnia is not a common adverse effect of phenytoin. It is not necessary to report it to the provider unless it becomes severe or significantly impacts the client's well-being.
- D) Tinnitus: Tinnitus, or ringing in the ears, is not a common adverse effect of phenytoin. It is not necessary to report it to the provider unless it becomes severe or persistent.
Diagnosis and treatment
A nurse is caring for a client who has a history of allergic reactions to penicillin. The client is prescribed cefazolin for a wound infection. Which of the following actions should the nurse take before administering the medication?
Explanation
Rationale: Cefazolin is a cephalosporin antibiotic, which has a cross-sensitivity with penicillin. Therefore, the nurse should ask the client about any previous reactions to cephalosporins before giving the medication.
Option B is incorrect because an antihistamine will not prevent a severe allergic reaction, such as anaphylaxis, which requires epinephrine.
Option C is incorrect because monitoring vital signs after the injection is not enough to prevent or treat an allergic reaction.
Option D is incorrect because diluting the medication will not affect its potential to cause an allergic reaction.
A client is admitted to the emergency department with signs of anaphylaxis after being stung by a bee. Which of the following medications should the nurse administer first?
Explanation
Rationale: Epinephrine is the first-line medication for anaphylaxis, as it reverses bronchoconstriction, vasodilation, and edema that can compromise the airway and circulation.
Option B is incorrect because diphenhydramine is an antihistamine that can help relieve itching and hives, but it does not act fast enough to treat anaphylaxis.
Option C is incorrect because albuterol is a bronchodilator that can help with wheezing, but it does not address the other manifestations of anaphylaxis. Option
D is incorrect because prednisone is a corticosteroid that can help reduce inflammation, but it has a delayed onset of action and is not effective for acute anaphylaxis.
A nurse is reviewing the medication list of a client who has hypertension and diabetes mellitus. The client reports experiencing a dry cough since starting lisinopril. Which of the following actions should the nurse take?
Explanation
Rationale: Lisinopril is an ACE inhibitor that can cause a dry cough as a common side effect. The nurse should notify the provider and request a prescription for an ARB, which has a similar antihypertensive effect but does not cause a dry cough.
Option A is incorrect because drinking more fluids and using lozenges may not relieve the cough caused by lisinopril.
Option B is incorrect because switching to another ACE inhibitor will likely result in the same side effect.
Option D is incorrect because stopping lisinopril abruptly can cause rebound hypertension and worsen the client's condition.
Nursing interventions and care
A nurse is caring for a client who has developed an allergic reaction to a medication. Which of the following actions should the nurse take first?
Explanation
Assess the client's respiratory status and oxygen saturation. This is the correct answer because the nurse should follow the ABC (airway, breathing, circulation) priority-setting framework when caring for a client who has an allergic reaction. The nurse should first assess the client's respiratory status and oxygen saturation to determine if they are in respiratory distress or have signs of anaphylaxis, which is a life-threatening emergency. The other actions are also important, but they are not the first priority.
A) Administer an antihistamine as prescribed. This is an incorrect answer because although administering an antihistamine can help reduce the symptoms of an allergic reaction, it is not the first action that the nurse should take. The nurse should first assess the client's respiratory status and oxygen saturation to determine if they are in respiratory distress or have signs of anaphylaxis.
B) Stop the medication infusion and disconnect the IV tubing. This is an incorrect answer because although stopping the medication infusion and disconnecting the IV tubing can prevent further exposure to the allergen, it is not the first action that the nurse should take. The nurse should first assess the client's respiratory status and oxygen saturation to determine if they are in respiratory distress or have signs of anaphylaxis.
D) Notify the provider and document the incident. This is an incorrect answer because although notifying the provider and documenting the incident are important steps in managing an allergic reaction, they are not the first actions that the nurse should take. The nurse should first assess the client's respiratory status and oxygen saturation to determine if they are in respiratory distress or have signs of anaphylaxis.
A client who has a history of penicillin allergy is prescribed cefazolin for a bacterial infection. The client asks the nurse why they can take cefazolin if they are allergic to penicillin. Which of the following responses should the nurse give?
Explanation
Answer: C. Cefazolin is a similar type of antibiotic to penicillin, but it has a lower risk of causing an allergic reaction than penicillin. This is the correct answer because cefazolin belongs to the same class of antibiotics as penicillin, which are called beta-lactams. However, cefazolin is a first-generation cephalosporin, which has less cross-reactivity with penicillin than other cephalosporins. This means that clients who are allergic to penicillin have a lower chance of having an allergic reaction to cefazolin than to other beta-lactam antibiotics. The nurse should explain this to the client and monitor them for any signs of an allergic reaction.
A) "Cefazolin is a different type of antibiotic than penicillin, so you will not have an allergic reaction to it." This is an incorrect answer because cefazolin is not a different type of antibiotic than penicillin; they both belong to
the beta-lactam class of antibiotics. Therefore, there is still a possibility that the client could have an allergic reaction to cefazolin if they are allergic to penicillin.
B) "Cefazolin is a synthetic version of penicillin, so it does not contain any of the allergens that cause your reaction." This is an incorrect answer because cefazolin is not a synthetic version of penicillin; they are both derived from natural sources. Therefore, cefazolin could still contain some of the allergens that cause the client's reaction to penicillin.
D) "Cefazolin is a newer type of antibiotic than penicillin, so it has fewer side effects and less potential for causing an allergic reaction." This is an incorrect answer because cefazolin is not a newer type of antibiotic than penicillin; they were both discovered in the 1940s. Therefore, the age of the antibiotic does not determine its side effects or potential for causing an allergic reaction.
A nurse is teaching a client who has a severe peanut allergy about how to use an epinephrine auto-injector in case of anaphylaxis. Which of the following instructions should the nurse include in the teaching?
Explanation
Answer: A. Inject the epinephrine into your thigh muscle and hold it for 10 seconds. This is the correct answer because the thigh muscle is the preferred site for administering epinephrine in case of anaphylaxis. The thigh muscle has a large blood supply and can absorb the medication quickly. The nurse should instruct the client to inject the epinephrine into the middle of the outer thigh, at a 90-degree angle, and hold it for 10 seconds to ensure that the full dose is delivered.
B) Inject the epinephrine into your upper arm muscle and hold it for 5 seconds. This is an incorrect answer because the upper arm muscle is not a recommended site for administering epinephrine in case of anaphylaxis. The upper arm muscle has a smaller blood supply and may not absorb the medication as quickly as the thigh muscle. The nurse should instruct the client to inject the epinephrine into the thigh muscle instead.
C) Inject the epinephrine into your abdomen and hold it for 15 seconds. This is an incorrect answer because the abdomen is not a recommended site for administering epinephrine in case of anaphylaxis. The abdomen has more fat tissue and may not absorb the medication as quickly as the thigh muscle. The nurse should instruct the client to inject the epinephrine into the thigh muscle instead.
D) Inject the epinephrine into your buttock and hold it for 20 seconds. This is an incorrect answer because the buttock is not a recommended site for administering epinephrine in case of anaphylaxis. The buttock has more fat tissue and may not absorb the medication as quickly as the thigh muscle. The nurse should instruct
the client to inject the epinephrine into the thigh muscle instead.
A nurse is reviewing the medication list of a client who is scheduled for surgery. The client reports that they are allergic to latex, iodine, and aspirin. Which of the following medications should the nurse alert the provider about?
No explanation
A nurse is caring for a client who is experiencing an allergic reaction to a medication. Which of the following interventions should the nurse prioritize?
Explanation
Explanation: When a client experiences an allergic reaction, monitoring vital signs is a priority nursing intervention. An allergic reaction can lead to systemic manifestations, such as respiratory distress, hypotension, or tachycardia. Monitoring vital signs allows the nurse to assess the client's overall condition, identify any worsening symptoms, and provide prompt intervention.
A) Administering an antihistamine
While antihistamines may be a part of the treatment plan for allergic reactions, they should not be the nurse's initial priority. The nurse should first assess the client's vital signs and overall stability before administering any medication.
B) Notifying the healthcare provider
While it is important to communicate with the healthcare provider, especially in severe cases, immediate intervention to monitor vital signs and ensure client stability should take precedence before notifying the healthcare provider.
D) Applying a cool compress to the affected area
Applying a cool compress may provide local relief for symptoms such as itching or redness. However, in the case of an allergic reaction, systemic manifestations require immediate attention. Therefore, monitoring vital signs takes priority over local comfort measures.
A client is experiencing an anaphylactic reaction. Which of the following actions should the nurse take first?
Explanation
Explanation: When a client is experiencing an anaphylactic reaction, ensuring airway patency is the nurse's first priority. Airway obstruction due to swelling or bronchospasm can rapidly lead to respiratory distress and hypoxia. Assessing airway patency allows the nurse to determine the severity of the situation and initiate appropriate interventions.
A) Administering epinephrine
Epinephrine is a critical medication for treating anaphylaxis, but the nurse must first ensure airway patency before administering any medication. The administration of epinephrine would follow the assessment and confirmation of airway patency.
B) Calling for emergency assistance
While calling for emergency assistance is essential in managing anaphylactic reactions, it should not take precedence over assessing airway patency. The nurse must first assess the client's immediate condition and initiate interventions to secure the airway.
D) Positioning the client in a supine position
Positioning the client in a supine position may be appropriate in some situations, but it is not the first priority when managing an anaphylactic reaction. Airway assessment and intervention should be the initial focus to address potential airway obstruction.
A nurse is providing education to a client about self-management of allergic reactions.
Which of the following statements by the client indicates understanding of the teaching?
Explanation
Explanation: Carrying an epinephrine auto-injector is a crucial self-management strategy for individuals with known allergies. In case of an allergic reaction, epinephrine can be administered promptly to counteract severe symptoms and potentially prevent anaphylaxis. This response demonstrates the client's understanding of the importance of being prepared to manage allergic reactions.
A) "I will avoid all potential allergens to prevent any reaction."
While avoiding known allergens is an essential aspect of managing allergies, it is often challenging to avoid all potential allergens. Some allergens may be difficult to identify or encounter unexpectedly. Carrying an epinephrine auto-injector provides a more comprehensive approach to self-management.
C) "I will take antihistamine medication every day to prevent reactions."
Antihistamines are primarily used for relieving symptoms of allergic reactions, such as itching or congestion, rather than preventing reactions. Taking antihistamines every day is not the recommended approach for preventing allergic reactions.
D) "I will self-administer corticosteroid injections during allergic reactions."
Corticosteroid injections are generally administered by healthcare professionals and are not intended for self-administration during allergic reactions. Corticosteroids may be part of the treatment plan for severe allergic reactions but are typically prescribed and administered under medical supervision.
Prevention and education
A nurse is providing education to a client about preventing allergic reactions to medications. Which of the following statements by the client indicates a correct understanding of the teaching?
Explanation
This statement indicates that the client understands the importance of informing their healthcare provider about any known drug allergies. By providing this information, healthcare providers can take appropriate measures to avoid prescribing medications that may cause an allergic reaction and choose alternatives if necessary. It promotes patient safety and helps prevent adverse reactions.
A) "I will always stop taking the medication if I experience mild itching."
This response is incorrect because mild itching alone may not indicate a severe allergic reaction. It is important for the client to communicate with their healthcare provider to determine the appropriate course of action.
C) "Allergic reactions to medications are rare and unlikely to happen to me."
This response is incorrect because allergic reactions to medications can occur and vary in frequency among individuals. It is important for clients to be aware of the potential risks and take necessary precautions.
D) "I can safely take any over-the-counter medication without consulting a healthcare provider."
This response is incorrect because even over-the-counter medications can cause allergic reactions or interact with other medications. It is important for clients to consult with their healthcare provider or pharmacist before taking any new medication.
A client asks the nurse about the use of an antihistamine medication for the prevention of allergic reactions. Which of the following responses by the nurse is correct?
Explanation
Antihistamines are commonly used to relieve symptoms of allergic reactions, such as itching, sneezing, and runny nose. However, they are not typically used for prevention purposes. Antihistamines work by blocking histamine receptors in the body but do not prevent the initial allergic response. Other preventive measures, such as avoiding known allergens, are more appropriate for allergy prevention.
B) "You should take an antihistamine before being exposed to potential allergens to prevent an allergic reaction."
This response is incorrect because taking an antihistamine before exposure to potential allergens is not a standard recommendation for prevention. Antihistamines are typically used for symptom relief after an allergic reaction has occurred.
C) "Antihistamines should only be used after experiencing an allergic reaction, not for prevention."
This response is incorrect because antihistamines can be used for symptom relief after an allergic reaction, but they are not limited to post-reaction use only.
D) "Taking antihistamines regularly can increase your risk of developing allergies."
This response is incorrect because regular use of antihistamines does not increase the risk of developing allergies. Antihistamines are generally safe and effective for relieving allergy symptoms when used as directed.
A nurse is educating a client with a known penicillin allergy about cross-reactivity with other antibiotics. Which of the following statements by the nurse is correct?
Explanation
Cross-reactivity between penicillin and other antibiotics is relatively uncommon. While some antibiotics may have a similar chemical structure to penicillin and potentially trigger a cross-reaction, the risk is generally low. However, it is important for clients with a known penicillin allergy to inform their healthcare provider about their allergy to ensure safe prescribing practices.
A) "If you are allergic to penicillin, you are also allergic to all other antibiotics."
This response is incorrect because not all antibiotics share the same chemical structure or have the potential for cross-reactivity. Each antibiotic has its own distinct chemical composition, and an allergy to one antibiotic does not necessarily mean an allergy to all others.
C) "You should avoid all antibiotics to prevent a cross-reaction if you have a penicillin allergy."
This response is incorrect because it is overly cautious and not necessary in all cases. While it is important for individuals with a penicillin allergy to be cautious and inform their healthcare provider, avoiding all antibiotics may not be appropriate or necessary for every situation.
D) "It is safe to take any antibiotic if you have a documented penicillin allergy."
This response is incorrect because taking any antibiotic without consulting a healthcare provider can be risky for individuals with a documented penicillin allergy. It is important for individuals with allergies to work closely with their healthcare provider to determine safe alternative antibiotics if needed.
A client is prescribed a new medication and asks the nurse about potential allergic reactions. Which of the following responses by the nurse is correct?
Explanation
This statement indicates that the client understands the importance of informing their healthcare provider about any known drug allergies. By providing this information, healthcare providers can take appropriate measures to avoid prescribing medications that may cause an allergic reaction and choose alternatives if necessary. It promotes patient safety and helps prevent adverse reactions.
A) "I will always stop taking the medication if I experience mild itching."
This response is incorrect because mild itching alone may not indicate a severe allergic reaction. It is important for the client to communicate with their healthcare provider to determine the appropriate course of action.
C) "Allergic reactions to medications are rare and unlikely to happen to me."
This response is incorrect because allergic reactions to medications can occur and vary in frequency among individuals. It is important for clients to be aware of the potential risks and take necessary precautions.
D) "I can safely take any over-the-counter medication without consulting a healthcare provider."
A client asks the nurse about the use of an antihistamine medication for the prevention of allergic reactions. Which of the following responses by the nurse is correct?
No explanation
A nurse is educating a client about the importance of reading medication labels for potential allergens. Which of the following instructions should the nurse provide?
Explanation
"Skipping or altering medication doses can increase the risk of adverse reactions."
Explanation: Skipping or altering medication doses can disrupt the therapeutic effects of medications and increase the risk of adverse reactions. It is important for clients to follow the prescribed dosing schedule and not make changes to their medication regimen without consulting their healthcare provider. This statement emphasizes the importance of medication adherence in preventing adverse reactions.
A) "Taking multiple medications simultaneously can reduce the risk of adverse reactions."
This response is incorrect because taking multiple medications simultaneously does not inherently reduce the risk of adverse reactions. In fact, the use of multiple medications can increase the complexity of medication regimens and the potential for drug interactions or adverse reactions.
C) "Stopping the medication as soon as symptoms improve can prevent adverse reactions."
This response is incorrect because abruptly stopping a medication without medical guidance can have unintended consequences and may not prevent adverse reactions. Medications should be taken for the prescribed duration unless instructed otherwise by a healthcare provider.
D) "Taking medications with grapefruit juice can enhance their effectiveness and reduce adverse reactions."
This response is incorrect because grapefruit juice can interact with certain medications, affecting their metabolism and potentially increasing the risk of adverse reactions. It is generally recommended to avoid consuming grapefruit juice with specific medications to ensure safety and effectiveness.
Summary
A nurse is monitoring a client who has gout and is receiving indomethacin (Indocin), a nonselective COX inhibitor. What are some of the adverse effects that the nurse should watch for?
Explanation
D. All of the above
This is because indomethacin can cause gastrointestinal, renal, and cardiovascular effects as a result of its nonselective inhibition of cyclooxygenase (COX) enzymes². COX enzymes are responsible for producing prostaglandins that have different functions in different tissues. By blocking both COX-1 and COX-2 enzymes, indomethacin can interfere with the protective, regulatory, and homeostatic roles of prostaglandins in various organs². Indomethacin is a nonsteroidal anti-inflammatory drug (NSAID) that is used to treat gout and other inflammatory conditions by reducing pain, swelling, and joint stiffness¹. It works by blocking the production of prostaglandins, which are chemical messengers that cause inflammation and pain¹. However, it can also cause some adverse effects that the nurse should watch for.
- Gastrointestinal effects such as nausea, vomiting, ulceration, bleeding, and perforation
These are the most common and serious side effects of indomethacin and other NSAIDs²³. They occur because indomethacin blocks the production of prostaglandins that protect the gastric mucosa from acid and pepsin, maintain the mucosal blood flow, and promote healing of ulcers². The risk of these effects is higher in older adults, those with a history of peptic ulcer disease or gastrointestinal bleeding, those who use alcohol or tobacco, and those who take other drugs that irritate the stomach, such as corticosteroids or anticoagulants²³. The nurse should advise the client to take indomethacin with food or milk, avoid alcohol and tobacco, report any signs of gastrointestinal bleeding (such as black or tarry stools, abdominal pain, vomiting blood), and use the lowest effective dose for the shortest duration possible²³.
- Renal effects such as reduced glomerular filtration rate, sodium and water retention, edema, hypertension, and acute renal failure
These are less common but potentially serious side effects of indomethacin and other NSAIDs²⁴. They occur because indomethacin blocks the production of prostaglandins that regulate renal blood flow, glomerular filtration rate, sodium excretion, and water balance². The risk of these effects is higher in those with preexisting renal impairment, heart failure, liver cirrhosis, dehydration, or hypovolemia, and those who use diuretics or angiotensin-converting enzyme inhibitors²⁴. The nurse should monitor the client's fluid intake and output, body weight, blood pressure, electrolytes, and renal function tests, and report any signs of renal dysfunction (such as oliguria, anuria, edema) or worsening heart failure (such as dyspnea, fatigue) to the doctor²⁴.
- Cardiovascular effects such as increased risk of myocardial infarction and stroke due to platelet aggregation and vasoconstriction
These are rare but potentially fatal side effects of indomethacin and other NSAIDs²⁵. They occur because indomethacin blocks the production of prostaglandins that inhibit platelet aggregation and vasodilation². The risk of these effects is higher in those with a history of cardiovascular disease or risk factors such as hypertension, diabetes mellitus, hyperlipidemia, smoking, or obesity²⁵. The nurse should assess the client's cardiovascular status and history before starting indomethacin therapy and advise the client to seek immediate medical attention if they experience any signs of a heart attack (such as chest pain or pressure) or a stroke (such as sudden weakness or numbness on one side of the body) while taking this drug²⁵.
Exams on Adverse Drug Reactions and Side Effects
Custom Exams
Login to Create a Quiz
Click here to loginAdverse Drug Reactions and Side Effects
Lessons
 Naxlex
Just Now
Naxlex
Just Now
Login to View Adverse Drug Reactions and Side Effects Study Video
Notes Highlighting is available once you sign in. Login Here.
Objectives
- Define adverse reactions and side effects of medications, allergic reactions, and anaphylaxis
- Identify the causes and risk factors for adverse drug reactions
- Recognize the signs and symptoms of adverse drug reactions, allergic reactions, and anaphylaxis
- Explain the diagnosis and treatment of adverse drug reactions, allergic reactions, and anaphylaxis
- Describe the nursing interventions and care for patients with adverse drug reactions, allergic reactions, and anaphylaxis
- Educate patients and families on how to prevent and manage adverse drug reactions, allergic reactions, and anaphylaxis
Introduction
- Adverse reactions and side effects of medications are unwanted or harmful effects that occur when a medication is taken as prescribed or directed
- Allergic reactions are hypersensitivity responses of the immune system to a foreign substance (allergen) that is usually harmless to most people
- Anaphylaxis is a severe and potentially life-threatening allergic reaction that involves multiple organ systems and requires immediate medical attention
- Adverse drug reactions, allergic reactions, and anaphylaxis can affect anyone at any age, but some people are more susceptible than others
- Adverse drug reactions, allergic reactions, and anaphylaxis can have serious consequences for the patient's health and quality of life and may result in hospitalization, disability, or death

Causes and risk factors
a. Some common risk factors for adverse drug reactions include:
- Age: older adults and children are more prone to adverse drug reactions due to changes in metabolism, organ function, body weight and drug interactions
- Gender: women may experience more adverse drug reactions than men due to hormonal fluctuations, pregnancy, breastfeeding and use of oral contraceptives
- Medical history: patients with chronic diseases, multiple comorbidities, impaired renal or hepatic function, or history of previous adverse drug reactions are more likely to have adverse drug reactions
- Medication factors: the type, dose, route, frequency, duration, combination and formulation of the medication may affect the risk of adverse drug reactions
- Lifestyle factors: smoking, alcohol consumption, diet, exercise and stress may influence the metabolism and elimination of medications and affect the risk of adverse drug reactions
b. Some common risk factors for allergic reactions include:
- Family history: having a parent or sibling with allergies increases the likelihood of developing allergies
- Personal history: having a history of allergies to other substances increases the risk of developing new allergies or crossreactivity to related substances
- Exposure: repeated or prolonged exposure to an allergen may sensitize the immune system and trigger an allergic reaction
- Allergen factors: some allergens are more potent than others and may cause more severe allergic reactions
- Environmental factors: pollution, temperature changes, humidity and seasonal variations may affect the exposure and response to allergens
c. Some common risk factors for anaphylaxis include:
- Previous anaphylaxis: having a history of anaphylaxis increases the risk of recurrence with subsequent exposure to the same or similar allergen
- Severity of allergy: having a severe allergy to a substance increases the risk of anaphylaxis with exposure to that substance
- Type of allergen: some allergens are more likely to cause anaphylaxis than others, such as food (e.g., peanuts, shellfish), insect stings (e.g., bees, wasps), medications (e.g., penicillin, antibiotics), latex and contrast media
- Cofactors: some factors may enhance or trigger anaphylaxis in combination with an allergen exposure, such as exercise, alcohol, infection, stress or menstruation
Signs and symptoms
a. Allergic reactions
- Type A: predictable pharmacological effects that are dosedependent and related to the known action of the medication (e.g., nausea, drowsiness, hypotension)
- Type B: unpredictable immunological effects that are doseindependent and related to the individual's hypersensitivity to the medication (e.g., rash, urticaria, angioedema)
- Type C: chronic effects that occur after longterm use of the medication (e.g., liver damage, osteoporosis)
- Type D: delayed effects that occur after discontinuation or withdrawal of the medication (e.g., rebound hypertension, withdrawal syndrome)
- Type E: endof-dose effects that occur when the medication level falls below the therapeutic range (e.g., breakthrough pain, breakthrough seizures)
- Type F: failure effects that occur when the medication fails to achieve the desired therapeutic outcome (e.g., treatmentresistant depression, antibiotic resistance)
b. Allergic Reactions
- Type I: immediate hypersensitivity reactions that occur within minutes to hours of exposure to the allergen and involve the release of histamine and other mediators from mast cells and basophils (e.g., anaphylaxis, allergic rhinitis, allergic asthma, allergic conjunctivitis, urticaria, angioedema)
- Type II: cytotoxic reactions that occur within hours to days of exposure to the allergen and involve the binding of antibodies to antigens on the surface of cells, leading to cell lysis or dysfunction (e.g., hemolytic anemia, thrombocytopenia, transfusion reactions, druginduced hemolytic anemia)
- Type III: immune complex reactions that occur within hours to days of exposure to the allergen and involve the formation of antigenantibody complexes that deposit in tissues and activate complement, leading to inflammation and tissue damage (e.g., serum sickness, glomerulonephritis, vasculitis)
- Type IV: delayed hypersensitivity reactions that occur within days to weeks of exposure to the allergen and involve the activation of T cells and macrophages, leading to cellmediated immunity and tissue destruction (e.g., contact dermatitis, tuberculin reaction, granulomatous inflammation)
c. Anaphylaxis
- The signs and symptoms of anaphylaxis vary depending on the severity and organ system involved. Anaphylaxis is characterized by a rapid onset of symptoms that may affect the skin, respiratory system, cardiovascular system, gastrointestinal system, nervous system or genitourinary system.
- Some common signs and symptoms of anaphylaxis include:
- Skin: flushing, itching, urticaria, angioedema, erythema
- Respiratory: dyspnea, wheezing, coughing, stridor, bronchospasm, laryngeal edema
- Cardiovascular: hypotension, tachycardia, arrhythmias, shock, cardiac arrest
- Gastrointestinal: nausea, vomiting, diarrhea, abdominal cramps, oral or pharyngeal swelling
- Nervous: headache, dizziness, confusion, anxiety, seizures
- Genitourinary: dysuria, urinary incontinence, uterine contractions
Diagnosis and treatment
- The diagnosis of adverse drug reactions is based on:
- the history of medication use
- the onset and duration of symptoms
- the type and severity of symptoms
- the exclusion of other possible causes
- the response to discontinuation or reversal of the medication
- Some tests that may be used to confirm or rule out adverse drug reactions include:
- Skin tests: used to detect type I or type IV hypersensitivity reactions to medications by applying a small amount of the suspected medication or its metabolite to the skin and observing for a local reaction
- Blood tests: used to measure the level of the medication or its metabolite in the blood and assess its pharmacokinetic profile
- Serological tests: used to detect antibodies or immune complexes against medications or their metabolites in the blood and assess their immunological profile
- Genetic tests: used to identify genetic variants that may affect the metabolism or response to medications and assess their pharmacogenetic profile
- The treatment of adverse drug reactions depends on:
- the type
- severity and mechanism of the reaction
- Some general principles for treating adverse drug reactions include:
- Discontinuation or reduction of the medication: this is usually the first step in managing adverse drug reactions unless it is contraindicated or impractical
- Symptomatic and supportive care: this involves providing oxygen, fluids, antihistamines, corticosteroids, bronchodilators, vasopressors or other medications as needed to relieve symptoms and stabilize vital signs
- Specific antidotes or reversal agents: these are substances that can bind to or inhibit the action of the medication or its metabolite and reverse its effects (e.g., naloxone for opioid overdose, and flumazenil for benzodiazepine overdose)
- Desensitization or immunotherapy: these are procedures that can reduce or eliminate the hypersensitivity response to a medication by gradually exposing the patient to increasing doses of the medication or its allergen under close medical supervision (e.g., penicillin desensitization, allergy shots)
- The diagnosis of allergic reactions is based on the history of exposure to allergens, the onset of symptoms and severity.
- The treatment of allergic reactions and anaphylaxis is aimed at reversing the immune response and preventing further exposure to the allergen.
- It may include administering epinephrine (adrenaline), antihistamines, corticosteroids, or other drugs, providing oxygen and fluids, or performing cardiopulmonary resuscitation if needed.
Nursing interventions and care
- Administering the prescribed treatment
- Providing comfort and reassurance,
- Educating the patient about the drug and its effects.
- Assessing the patient's airway, breathing, and circulation
- Maintaining the patient's vital signs and oxygen saturation
- Preventing further exposure to the allergen
- Preparing for possible emergency transport.

Prevention and education
- Reviewing the patient's medical history and allergies before prescribing a drug,
- Informing the patient about the possible adverse reactions and side effects of the drug and how to manage them,
- Instructing the patient on how to take the drug correctly and safely,
- Advising the patient to report any new or worsening symptoms to the healthcare provider
- Encouraging the patient to follow up regularly.
- The prevention and education for patients with allergic reactions and anaphylaxis include:
- Identifying the patient's triggers and sensitivities through testing or elimination diets,
- Educating the patient about the signs and symptoms of an allergic reaction and anaphylaxis and how to recognize them early,
- Prescribing an epinephrine auto-injector (epipen) for the patient to carry at all times and teaching them how to use it properly,
- Instructing the patient to wear a medical alert bracelet or necklace that states their allergy,
- Advising the patient to inform their family members, friends, co-workers, teachers, or caregivers about their allergy and what to do in case of a reaction,
- Recommending the patient to consult an allergist or immunologist for further evaluation and treatment.
Conclusion
- Adverse reactions and side effects of medications, allergic reactions and anaphylaxis,
- And monitoring and managing adverse drug reactions are important topics for nursing students to learn and master
- Adverse drug reactions can have serious consequences for a patient's health and wellbeing
- Nurses have a key role in preventing, detecting, reporting, and managing adverse drug reactions
- Allergic reactions and anaphylaxis are rare but serious and require immediate attention.
- Nurses play a vital role in diagnosing, treating, caring for, preventing, and educating patients with these conditions.
Summary
- Introduction: Unwanted effects of medications, allergic reactions, and anaphylaxis
- Causes and risk factors: Age, gender, medical history, medication factors, lifestyle, family history, personal history, exposure, allergen factors, environmental factors
- Signs and symptoms: Various types of allergic reactions (Type AF), anaphylaxis symptoms affecting multiple organ systems
- Diagnosis and treatment: History, symptom assessment, tests (skin, blood, serological, genetic), discontinuation, symptomatic care, antidotes, desensitization
- Nursing interventions and care: Treatment administration, comfort, education, assessment, vital signs, prevention, emergency preparedness
- Prevention and education: Medical history review, informing patients, correct usage instruction, follow-up, trigger identification, epinephrine use, allergen awareness
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Adverse Drug Reactions and Side Effects
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


