Please set your exam date
Vital Signs
Study Questions
Practice Exercise 2
A nursing diagnosis of Ineffective peripheral tissue perfusion would be validated by which one of the following?
Explanation
The nursing diagnosis of Ineffective Peripheral Tissue Perfusion refers to a decrease in oxygen and nutrient supply to the body’s extremities, which can result from impaired arterial blood flow.
Rationale for correct answer:
D. Absent posterior tibial and pedal pulses: These are peripheral pulses, and their absence is a classic indicator of impaired arterial blood flow to the lower extremities.
Rationale for incorrect answers:
A. Bounding radial pulse: A bounding pulse indicates increased blood volume or pressure, not impaired tissue perfusion. Conditions like fever, anxiety, or fluid overload can cause bounding pulses.
B. Irregular apical pulse: An irregular apical pulse suggests a cardiac conduction issue (e.g., atrial fibrillation) but doesn’t directly validate peripheral tissue perfusion.
C. Carotid pulse stronger on the left side than the right: Asymmetrical carotid pulses can indicate localized vascular disease or structural abnormalities, but this reflects central circulation, not necessarily peripheral tissue perfusion.
Take-home points:
- Absent or diminished peripheral pulses (e.g., posterior tibial, dorsalis pedis) are hallmark signs of impaired tissue perfusion in the extremities.
- Cardiac irregularities or bounding pulses may reflect systemic or central issues but do not validate peripheral perfusion deficits.
Which client meets the criteria for selection of the apical site for assessment of the pulse rather than a radial pulse?
Explanation
The radial pulse is the most commonly used site for routine assessments because it is accessible and generally reliable in healthy individuals. However, when more accurate or detailed assessment is needed- such as detecting rate irregularities or evaluating heart function directly- the apical pulse is preferred.
Rationale for correct answer:
C. A client with an arrhythmia: The apical pulse is preferred when a client has an irregular heart rhythm (arrhythmia) because it provides a more accurate count of heartbeats, especially if some beats do not produce a palpable pulse at the radial site.
Rationale for incorrect answers:
A. A client who is in shock: In shock, peripheral perfusion is often poor, making the radial pulse weak or unpalpable. While that may seem like a reason to check the apical pulse, the priority in shock is rapid stabilization, not detailed pulse analysis.
B. A client whose pulse changes with body position changes: Pulse variations with postural changes (e.g., orthostatic hypotension) can still be accurately assessed using the radial pulse. The key in this scenario is to observe trends in heart rate and blood pressure during position changes.
D. A client who had surgery less than 24 hours ago: Postoperative clients are routinely monitored using the radial pulse unless there is a specific cardiovascular concern such as arrhythmia or instability.
Take-home points:
- The apical pulse should be assessed when accuracy is critical, such as in clients with arrhythmias or on cardiac medications that affect heart rate and rhythm.
- The radial pulse is sufficient for routine monitoring in stable clients without suspected irregularities in rhythm or perfusion deficits.
The measurement of blood that enters the aorta with each ventricular contraction is called the ______.
Explanation
The amount of blood ejected from the heart during each contraction (systole) reflects the heart’s pumping efficiency and directly affects tissue perfusion. This volume of blood plays a central role in determining cardiac output, blood pressure, and ultimately, oxygen delivery to organs.
Rationale for correct answer:
B. Stroke Volume (SV) is the amount of blood ejected by the left ventricle into the aorta with each contraction, typically about 60–100 mL per beat in a healthy adult.
Rationale for incorrect answers:
A. Pulse refers to the palpable rhythmic expansion of arteries as blood is ejected from the heart. It reflects heart rate and rhythm, but it is not a volume measurement.
C. Cardiac Output (CO) is the total volume of blood the heart pumps per minute and is calculated as:
CO = Stroke Volume × Heart Rate.
D. Pulse Pressure is the difference between systolic and diastolic blood pressures (e.g., 120/80 → pulse pressure = 40 mmHg).
Take-home points:
- Stroke volume is the volume of blood ejected from the ventricle per heartbeat, and it is a key determinant of cardiac performance.
- Cardiac output considers both stroke volume and heart rate and reflects the heart’s minute-to-minute output.
While taking an adult patient’s pulse, a nurse finds the rate to be 140 beats/min. What should the nurse do next?
Explanation
A rate of 140 bpm is classified as tachycardia, which can be caused by various conditions such as fever, dehydration, pain, anxiety, hypoxia, infection, hemorrhage, or cardiac arrhythmia.
Rationale for correct answer:
D. Report the rate: A pulse of 140 bpm is significantly abnormal and should be immediately reported to the provider or charge nurse.
Rationale for incorrect answers:
A. Check the pulse again in 2 hours: Delaying action for 2 hours could result in missed early intervention if the client is experiencing a medical emergency such as arrhythmia or sepsis.
B. Check the blood pressure: Checking blood pressure is a reasonable follow-up when a tachycardic pulse is noted, as it helps assess perfusion and cardiovascular stability. However, this step should be secondary to reporting the abnormal pulse.
C. Record the information: Documentation is important, but simply recording without reporting an abnormal rate of 140 bpm fails to meet the nurse's responsibility to act on critical findings.
Take-home points:
- A pulse rate of 140 bpm in an adult is tachycardia and could indicate a serious underlying problem-it must be reported immediately.
- Nurses should not delay action or rely solely on documentation; abnormal findings require clinical judgment and escalation.
Practice Exercise 3
When the nurse enters a client’s room to measure routine vital signs, the client is on the phone. What technique should the nurse use to determine the respiratory rate?
Explanation
Assessing respiratory rate is a key component of a full set of vital signs and offers important insights into a client’s oxygenation and metabolic status. Unlike other vital signs, respirations can be consciously controlled by the client, so the accuracy of measurement depends heavily on observation without alerting the client to the fact they are being observed.
Rationale for correct answer:
D. Since there is no evidence of distress or urgency, postpone the measurement until later: Since the client’s needs are always considered first, the measurement should be delayed unless the client is in distress or there are other urgent reasons.
Rationale for incorrect answers:
A. Count the respirations during conversational pauses: Respirations should be measured for 30 seconds to 1 minute and are affected by talking.
B. Ask the client to end the phone call now and resume it at a later time: This approach is unnecessarily intrusive for a non-urgent procedure like routine vital sign measurement. It may also damage rapport with the client.
C. Wait at the client’s bedside until the phone call is completed and then count respirations: While not incorrect in safety terms, this wastes time and can reduce nursing efficiency. Waiting may also make the client self-conscious, affecting the accuracy of later respiratory measurements.
Take-home points:
- Respiratory rate should be measured without alerting the client, as conscious control can distort the accuracy.
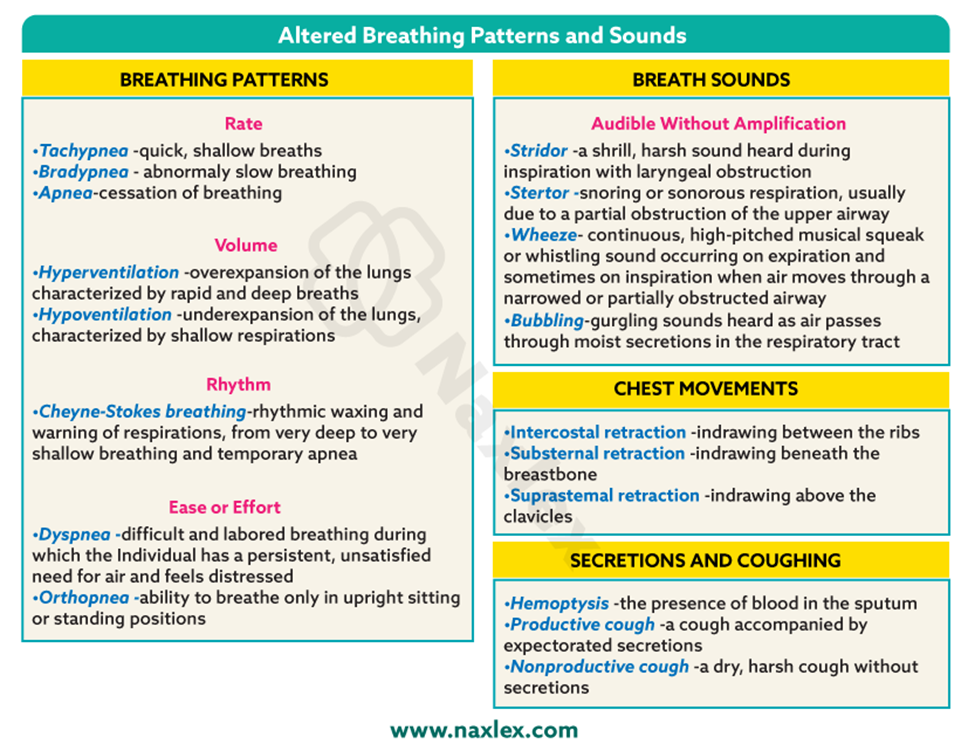
The nurse reports that the client has dyspnea when ambulating. The nurse is most likely to have assessed which of the following?
Explanation
Dyspnea is a subjective sensation of breathing difficulty, commonly described by clients as shortness of breath (SOB). It may occur at rest or during exertion, such as ambulation. Nurses play a key role in identifying signs of respiratory compromise by assessing breathing patterns, respiratory effort, oxygen saturation, lung sounds, and associated symptoms.
Rationale for correct answer:
C. Shortness of breath: Dyspnea is defined as shortness of breath, especially with exertion.
Rationale for incorrect answers:
A. Shallow respirations may accompany dyspnea, but it is not the defining feature.
B. Wheezing is a high-pitched sound during breathing, usually caused by narrowed airways (e.g., in asthma or bronchospasm).
D. Coughing up blood (hemoptysis) may indicate serious pulmonary pathology such as tuberculosis, pulmonary embolism, or cancer, but it is not a hallmark or required feature of dyspnea.
Take-home points:
- Dyspnea is best characterized by shortness of breath, especially on exertion like walking or climbing stairs.
- Nurses should differentiate related symptoms like wheezing or shallow breathing, but not confuse them as synonymous with dyspnea.
In the figure below, which number indicates the client’s oxygen saturation as measured by pulse oximetry? _____________
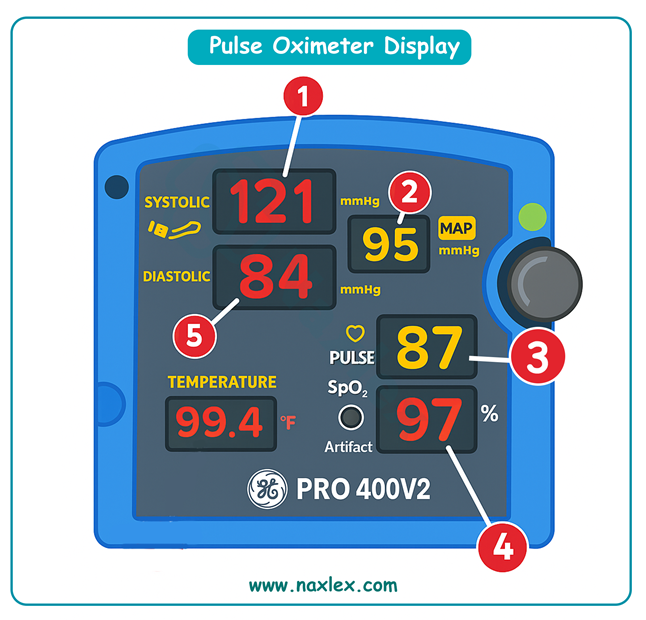
Explanation
One of the key components of vital signs measurement is oxygen saturation (SpO₂), which reflects the percentage of hemoglobin molecules carrying oxygen in the blood. This value is measured noninvasively using a pulse oximeter and is essential for assessing respiratory function and oxygen delivery.
Rationale for correct answer:
4. 97%: This is the SpO₂ or oxygen saturation reading from pulse oximetry. It represents the percentage of oxygen-bound hemoglobin and is essential in monitoring respiratory function.
Rationale for incorrect answers:
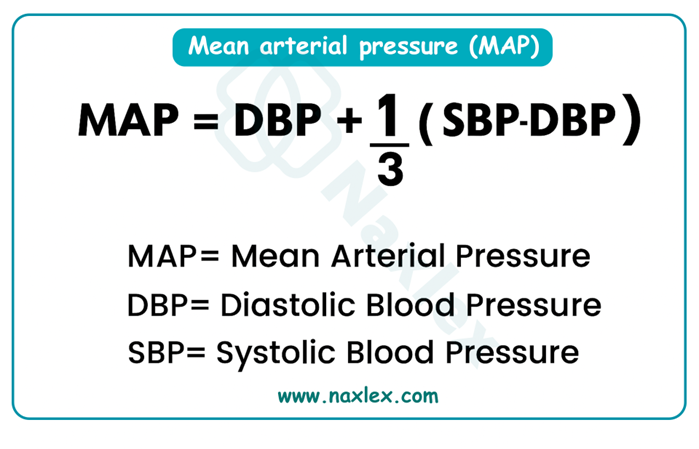
1. 121 mmHg: This is the systolic blood pressure, the pressure in arteries when the heart contracts. It is not related to oxygen saturation.
2. 95 mmHg: This is the MAP (Mean Arterial Pressure), which reflects average blood pressure during a cardiac cycle.
3. 87 BPM: This value indicates the heart rate in beats per minute (BPM).
5. 84 mmHg: This is the diastolic blood pressure, the pressure in arteries when the heart is at rest.
Which of the following patients are at most risk for tachypnea? Select all that apply
Explanation
Tachypnea, defined as a respiratory rate > 20 breaths per minute in adults, is a common clinical sign indicating respiratory distress or physiological stress. It may result from pain, hypoxia, fever, metabolic acidosis, pregnancy, pulmonary conditions, or neurologic impairment.
Rationale for correct answers:
A. Patient just admitted with four rib fractures: Rib fractures cause pain with inspiration, leading to shallow, rapid breathing (tachypnea) as the patient attempts to minimize chest movement.
B. Woman who is 9 months pregnant: In late pregnancy, the enlarged uterus pushes against the diaphragm, reducing lung expansion and causing compensatory increased respiratory rate.
E. Three-pack–per-day smoker with pneumonia: Pneumonia causes inflammation and fluid in the alveoli, impairing gas exchange and leading to hypoxia.
Rationale for incorrect answers:
C. A patient admitted with hypothermia: Hypothermia is associated with slowed metabolism, bradycardia, and slowed respirations - not tachypnea.
D. Postoperative patient waking from general anesthesia: Anesthesia often causes respiratory depression, especially in the immediate postoperative phase.
Take-home points:
- Tachypnea is a compensatory mechanism for impaired ventilation or oxygenation and often occurs with pain, pulmonary disease, or late pregnancy.
- Conditions that slow metabolism (e.g., hypothermia) generally reduce respiratory rate, not increase it.
Comprehensive Questions
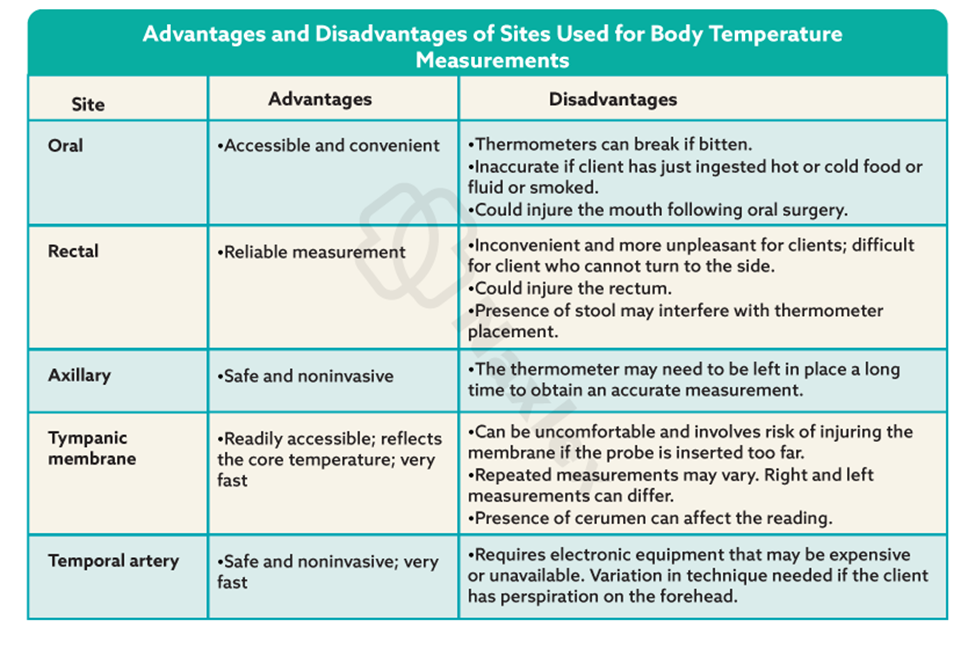
An 85-year-old client has had a stroke resulting in right-sided facial drooping, difficulty swallowing, and the inability to move self or maintain position unaided. The nurse determines that which sites are most appropriate for taking the temperature? Select all that apply
Explanation
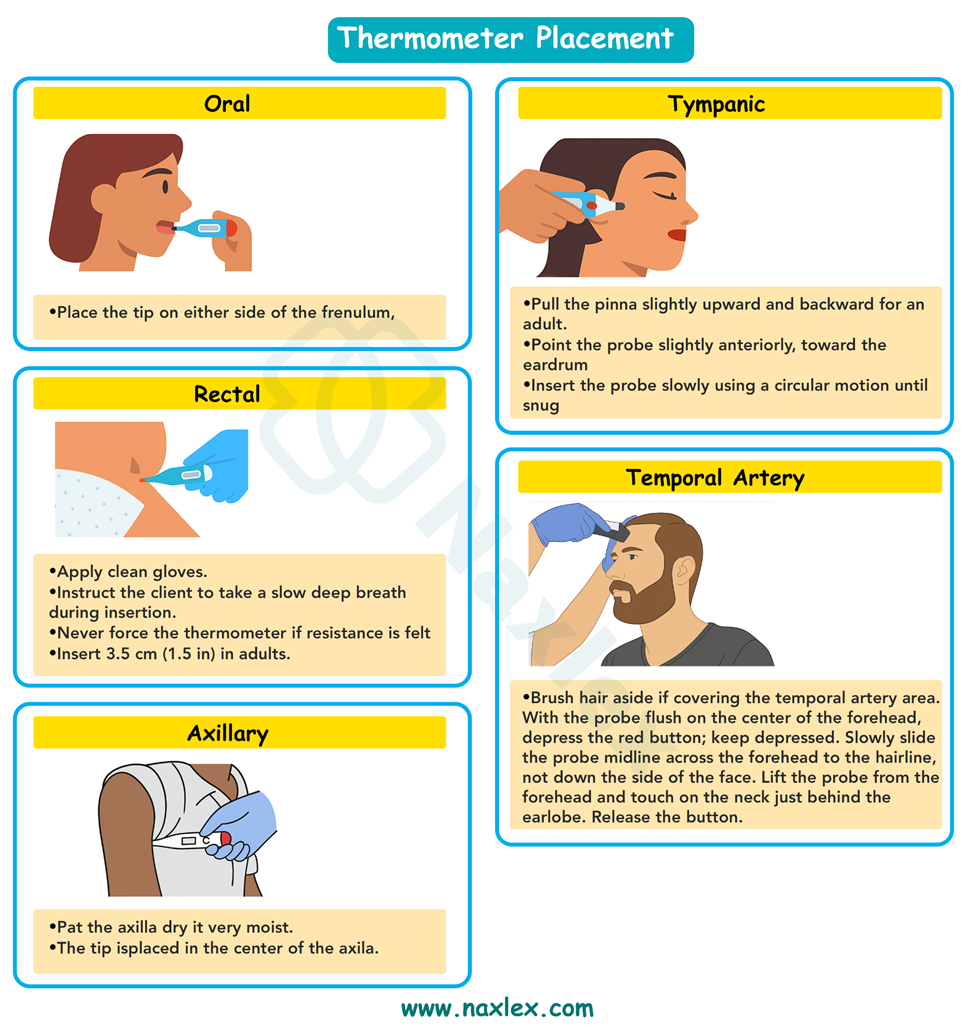
In clients who have had a stroke, especially those with facial drooping, dysphagia (difficulty swallowing), or immobility, the nurse must choose a method of taking temperature that minimizes risk (e.g., aspiration or injury) and provides consistent, accurate readings.
Rationale for correct answer:
C. Axillary: Safe, noninvasive, and easy to perform even in clients with limited mobility. While it is less accurate than core sites, it’s a reasonable alternative when oral and rectal sites are contraindicated.
D. Tympanic: Quick, noninvasive, and reflects core temperature well. Not affected by oral or facial dysfunctions. Can be performed even when the client has limited cooperation.
E. Temporal artery: Noninvasive, fast, and generally well tolerated. Can be used in immobile or neurologically impaired clients without requiring cooperation.
Rationale for incorrect answers:
A. Oral: Oral temperature measurement requires the client to close their mouth tightly around the probe, which is compromised by facial drooping and dysphagia.
B. Rectal: While rectal temperature is accurate, it is invasive and can be uncomfortable, particularly in older or immobile clients.
Take-home points:
- Avoid oral and rectal routes in clients with neurologic deficits, swallowing issues, or limited mobility due to safety concerns.
- Axillary, tympanic, and temporal artery methods are safe, noninvasive, and appropriate for clients with stroke-related impairments.
For a client with a previous blood pressure of 138/74 mmHg and pulse of 64 beats/min, approximately how long should the nurse take to release the blood pressure cuff in order to obtain an accurate reading?
Explanation
Accurate blood pressure (BP) measurement is a fundamental nursing skill. If the cuff is deflated too quickly, the nurse may miss the first Korotkoff sound (systolic BP) or inaccurately estimate diastolic pressure. Deflating the cuff too slowly can cause venous congestion, discomfort, and a falsely high diastolic reading. Best practice guidelines recommend a cuff deflation rate of 2–3 mmHg per second to ensure an accurate reading without patient discomfort.
Rationale for correct answer:
B. 30–45 seconds: This is the recommended time frame for releasing the cuff when using a 2–3 mmHg/second deflation rate, which allows clear identification of both systolic and diastolic sounds.
Rationale for incorrect answers:
A. 10–20 seconds: Deflating the cuff this quickly equates to a deflation rate that is too fast (greater than 5 mmHg per second). This may result in missing Korotkoff sounds and underestimating the true BP values, especially systolic pressure.
C. 1 -- A.5 minutes: Deflating the cuff this slowly would equate to less than 1 mmHg per second, which is unnecessarily prolonged. It can cause venous congestion, discomfort, and may lead to a falsely elevated diastolic pressure.
D. 3–C.5 minutes: This is excessively slow and not clinically appropriate.
Take-home points:
- The blood pressure cuff should be deflated at a rate of 2-3 mmHg per second, resulting in a total release time of approximately 30-45 seconds, depending on the pressure range.
- Incorrect deflation rates (too fast or too slow) can lead to inaccurate readings and impact clinical decisions.
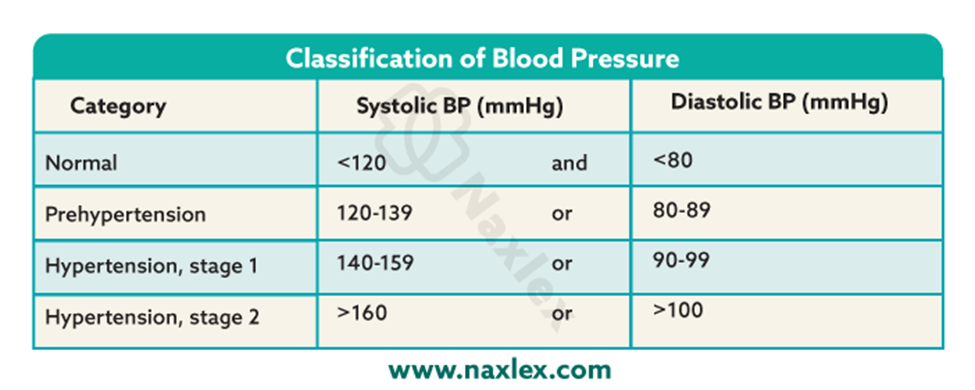
According to the JNC’s seventh report, a BP reading of 144/96 would be considered ______.
Explanation
The Joint National Committee (JNC 7) report provides evidence-based guidelines for the classification and management of blood pressure (BP) to reduce the risk of cardiovascular disease.
Rationale for correct answer:
C. Stage 1 Hypertension: Stage 1 hypertension is defined as: Systolic 140–159 mmHg or Diastolic 90–99 mmHg.
Rationale for incorrect answers:
A. Normal: According to JNC 7, normal BP is defined as less than 120/80 mmHg.
B. Prehypertension is defined as: Systolic 120–139 mmHg or Diastolic 80–89 mmHg.
D. Stage 2 Hypertension is defined as: Systolic ≥160 mmHg or Diastolic ≥100 mmHg.
Take-home points:
- According to JNC 7, Stage 1 Hypertension is defined as a systolic BP of 140–159 mmHg or diastolic of 90–99 mmHg.
- When systolic and diastolic values fall into different categories, the higher stage should determine the classification.
A healthy adult patient tells the nurse that he obtained his blood pressure in “one of those quick machines in the mall” and was alarmed that it was 152/7B. He immediately repeated the measurement, and the value was 158/80. His normal BP value ranges from 114/72 to 118/78. The nurse obtains a blood pressure of 116/76. What would account for the blood pressure of 152/72? Select all that apply
Explanation
Blood pressure (BP) measurement is a foundational clinical assessment, but its accuracy is highly influenced by technique, cuff size, body position, and external factors.
Rationale for correct answers:
A. Cuff too small on the device: A cuff that is too small for the client’s arm can result in falsely elevated systolic pressure.
D. Patient did not remove his long-sleeved shirt: Taking BP over clothing can interfere with cuff compression and cause falsely high readings, especially thicker or tight sleeves.
E. Insufficient time between measurements: Taking repeat BP readings too soon (e.g., within 1–2 minutes) doesn’t allow time for vascular recovery and can lead to falsely high results.
Rationale for incorrect answers:
B. Arm positioned above heart level: If the arm is above heart level, BP readings tend to be falsely low, not high. To avoid error, the arm should be at heart level.
C. Slow inflation of the cuff by the machine: Slow deflation, not inflation, affects BP accuracy.
Take-home points:
- Improper cuff size, measuring over clothing, and not waiting long enough between readings can all cause falsely elevated BP.
- BP measurement should be performed with the arm at heart level, cuff directly on skin, and with the correct-sized cuff to ensure accuracy.
The client’s temperature at 8:00 am using an oral electronic thermometer is 3F.1°C (97.2°F). If the respiration, pulse, and blood pressure were within normal range, what would the nurse do next?
Explanation
Vital signs provide critical information about a client's physiological status. When evaluating temperature, it's essential to consider normal ranges, the client’s baseline, and potential factors affecting the measurement (e.g., equipment error, recent food or fluid intake).
Rationale for correct answer:
B. Check what the client’s temperature was the last time it was taken: A single temperature reading may be normal or abnormal depending on the client's baseline pattern. Comparing previous readings helps determine whether this value is consistent or a new finding that might warrant further assessment.
Rationale for incorrect answers:
A. Wait 15 minutes and retake it: There is no indication that the initial temperature was affected by recent activity such as eating, drinking, or smoking, which could temporarily alter an oral temperature.
C. Retake it using a different thermometer: There’s no indication that the equipment is malfunctioning. If the reading had been inconsistent with the client’s condition, or if the thermometer showed an error, retaking with a different device would be reasonable.
D. Chart the temperature; it is normal: While 3F.1°C (97.2°F) is technically within the lower limit of normal, this option skips an important clinical validation step: checking for trends. The nurse may miss a developing pattern of hypothermia or a declining trend in temperature.
Take-home points:
- Always compare current vital signs with the client’s baseline and trends to determine clinical significance.
- Low-normal temperature readings require context- never assume they're acceptable without reviewing previous data and clinical presentation.
It would be appropriate to delegate the taking of vital signs of which client to unlicensed assistive personnel?
Explanation
According to the ANA and NCSBN guidelines, UAPs can take vital signs in stable clients, but the nurse is still responsible for interpreting the findings and taking action when needed. For clients who are unstable, newly admitted, or receiving high-risk treatments, vital signs should be taken by the nurse to allow for immediate clinical judgment.
Rationale for correct answer:
A. A client being prepared for elective facial surgery with a history of stable hypertension: This client is clinically stable and undergoing a planned, non-emergency procedure. The history of stable hypertension implies no acute instability, making it appropriate for the UAP to collect vital signs.
Rationale for incorrect answers:
B. A client receiving a blood transfusion with a history of transfusion reactions: This client is high risk due to a known history of transfusion reactions. Vital signs need to be monitored closely and frequently by a licensed nurse who can recognize early signs of a reaction.
C. A client recently started on a new antiarrhythmic agent: Starting a new antiarrhythmic introduces potential for serious adverse effects, including bradycardia, hypotension, or arrhythmias.
D. A client who is admitted frequently with asthma attacks: Although this client may be familiar to the unit, frequent asthma exacerbations place them at risk for acute respiratory deterioration. Vital signs should be taken by the nurse to assess signs of distress.
A 69-year-old woman is admitted with dizziness, confusion, and dyspnea. Which vital sign should not be delegated to trained ancillary personnel?
Explanation
In cases where a client presents with acute symptoms, the nurse must use clinical judgment to determine whether vital sign assessment requires nursing-level evaluation, particularly for parameters that require observation, interpretation, or correlation with clinical symptoms.
Rationale for correct answer:
C. Respiratory rate is the most sensitive indicator of deterioration and must often be assessed by a nurse, especially in clients with dyspnea or altered mental status.
Rationale for incorrect answers:
A. Temperature: Taking temperature is a simple, objective task that is appropriate to delegate to trained personnel.
B. Pulse can generally be delegated, especially when using automated equipment.
D. Blood Pressure is usually safe to delegate to trained personnel. While the nurse should evaluate the results, the act of measuring BP (especially with an automated device) does not require advanced assessment skills unless there's an abnormality.
Take-home points:
- Respiratory rate is often under-assessed but is critical for identifying early clinical deterioration, especially in clients with dyspnea or confusion.
- Delegation decisions must always factor in client stability, the complexity of the task, and the skill level required to interpret findings.
Prioritize your nursing interventions based on the vital signs.
Explanation
When multiple abnormal readings are present, the nurse must prioritize interventions based on the urgency, potential for deterioration, and underlying cause. The principle of ABC (Airway, Breathing, Circulation), followed by temperature regulation and pain control, guides prioritization.
Rationale for correct answer:
B. Heart rate 130 beats/min, apical: A heart rate of 130 bpm is significantly elevated and may indicate compensatory response to fever, pain, dehydration, or underlying cardiac stress.
Rationale for incorrect answers:
A. Temperature 10B.4°F (39.1°C): This is a moderate to high-grade fever, likely contributing to the elevated HR and RR. The fever itself is not immediately life-threatening, but needs to be addressed with antipyretics.
C. Respiratory rate 25 breaths/min: Mild tachypnea may be a response to fever, pain, or anxiety, but could also signal early respiratory distress. Although not critically high, this rate warrants ongoing respiratory assessment.
D. BP 145/80: This is a mildly elevated systolic BP, possibly related to stress, fever, or pain. It is not immediately concerning in this clinical context
Take-home points:
- Always prioritize circulation and respiratory compromise first - HR and RR abnormalities can indicate early deterioration.
- Fever and elevated BP are important, but unless critical, they typically follow cardiac and respiratory concerns in priority.
A client is admitted with a head injury and may develop neurogenic fever. Which nursing diagnosis would be most appropriate for this client?
Explanation
The hypothalamus is the primary center for thermoregulation. When a client sustains a head injury, especially involving the hypothalamus or brainstem, the body may lose its ability to properly regulate temperature. This can lead to a neurogenic fever, which is a non-infectious fever caused by damage to the thermoregulatory center.
Rationale for correct answer:
D. Ineffective thermoregulation: This nursing diagnosis reflects an actual disruption in temperature regulation due to neurological impairment. It encompasses both fever and hypothermia, making it the most comprehensive and accurate for this client.
Rationale for incorrect answers:
A. Risk for imbalanced body temperature: This diagnosis is used when the risk factors are present, but the condition has not yet occurred.
B. Hyperthermia refers to an elevated body temperature due to external heat or failure of heat loss mechanisms (e.g., heatstroke, environmental exposure).
C. Hypothermia is defined as a core body temperature below 35°C (95°F). There’s no indication that the client is hypothermic, and with the mention of neurogenic fever, the temperature is expected to increase, not decrease.
Take-home points:
- Ineffective thermoregulation is the most appropriate nursing diagnosis for clients with neurologically driven temperature abnormalities, such as neurogenic fever.
- Nurses must differentiate between external causes of hyperthermia and central (neurogenic) causes, especially in clients with head injuries.
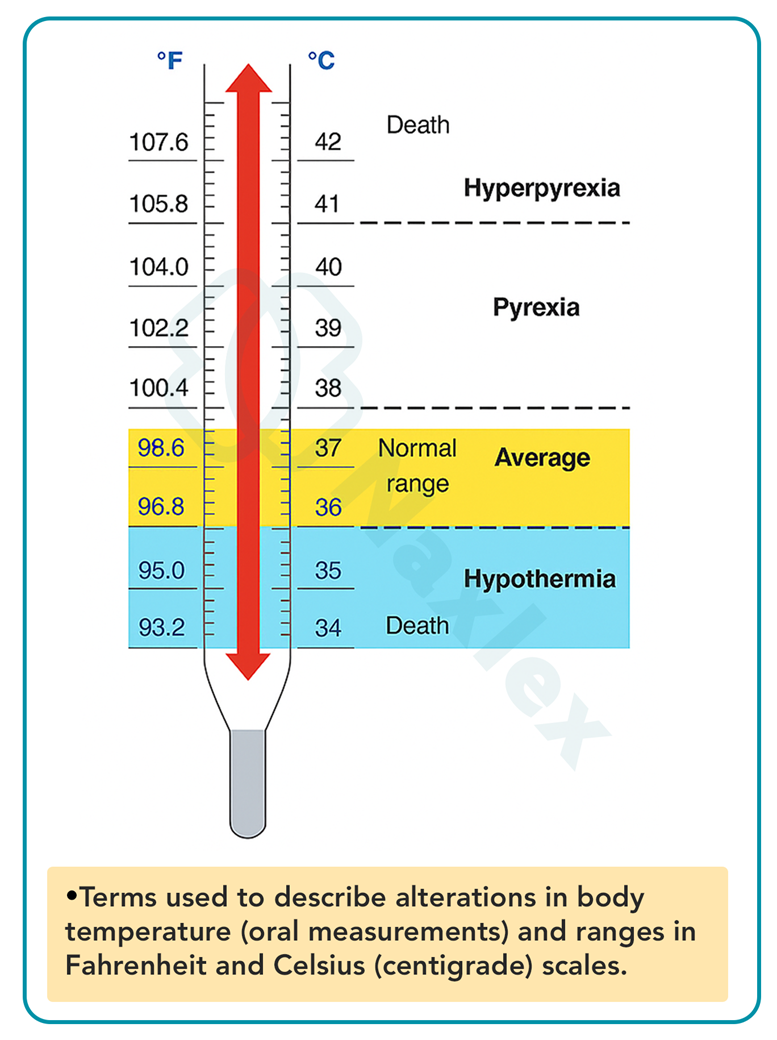
A nurse assesses an oral temperature for a patient as 38.5°C (10A.3°F). What term would the nurse use to report this temperature?
Explanation
Monitoring and interpreting body temperature is a fundamental nursing task used to assess homeostasis, detect infection, and guide treatment decisions. The normal oral temperature range for adults is typically between 3F.5°C to 37.5°C (97.7°F to 99.5°F).
Rationale for correct answer:
A. Fever (also called pyrexia) is defined as a body temperature above the normal range, typically greater than 38°C (100.4°F) when measured orally.
Rationale for incorrect answers:
B. Hypothermia refers to a core body temperature below 35°C (95°F).
C. Hypertension refers to elevated blood pressure, not body temperature.
D. Afebrile means without fever, or having a normal body temperature.
Take-home points:
- A temperature above 38°C (100.4°F) is classified as a fever and should be documented accordingly.
- Use accurate terminology for vital signs to ensure clear communication and proper follow-up care.
A patient complains of severe abdominal pain. When assessing the vital signs, the nurse would not be surprised to find what assessment?
Explanation
Pain, especially severe acute pain like abdominal pain, triggers a sympathetic nervous system (SNS) response, often referred to as the "fight or flight" reaction. This leads to measurable changes in vital signs.
Rationale for correct answer:
A. An increase in the pulse rate: Pain stimulates the sympathetic nervous system, resulting in tachycardia (increased heart rate).
Rationale for incorrect answers:
B. A decrease in body temperature: Pain does not typically cause a drop in temperature. Hypothermia is more likely in shock, exposure, or metabolic disorders-not as a direct result of pain.
C. A decrease in blood pressure: In the early stages of pain, the SNS response often causes a mild increase in blood pressure.
D. An increase in respiratory depth: Acute abdominal pain usually causes patients to take shallow breaths to minimize movement and discomfort (known as splinting).
Take-home points:
- Increased heart rate (tachycardia) is a common and expected physiological response to severe pain due to SNS activation.
- Nurses must interpret changes in vital signs in the context of the patient's symptoms to detect early signs of deterioration or complications.
A 52-year-old woman is admitted with pneumonia, dyspnea, and discomfort in her left chest when taking deep breaths. She has smoked for 35 years and recently lost over D.5 kg (10 lb). She is started on intravenous antibiotics, high protein shakes, and 2 L O2 via nasal cannula. Her vital signs at the start of treatment are HR 112, BP 138/82, RR 22, tympanic temperature 37.9°C (100.2°F), and oxygen saturation 94%. Which of the vital signs taken 4 hours later reflect a positive outcome of the treatment interventions? Select all that apply
Explanation
Pneumonia typically causes fever, tachypnea, increased heart rate, and reduced oxygen saturation. Treatment goals include reducing fever and infection, improving oxygenation, and relieving respiratory distress.
Rationale for correct answers:
A. Temperature: 37°C (98.6°F): This indicates that the fever has resolved, showing the antibiotics may be working and inflammation is decreasing.
B. Radial pulse: 98: The heart rate decreased from 112 to 98 bpm, reflecting reduced sympathetic response (less fever, improved oxygenation).
C. Respiratory rate: 18: A drop from 22 to 18 breaths/min indicates eased breathing, improved oxygen exchange, and reduced respiratory distress.
D. Oxygen saturation: 96%: An increase from 94% to 96% on 2 L oxygen suggests better gas exchange and alveolar function.
Rationale for incorrect answers:
E. Blood pressure: 134/78: Clinically stable but not the best indicator of pneumonia recovery. BP has remained within the normal range and is slightly lower than baseline (138/82).
Take-home points:
- Positive treatment outcomes in pneumonia include lowered fever, normalized respiratory rate, improved oxygen saturation, and decreasing heart rate.
- While blood pressure stability is important, it is less specific for tracking pneumonia recovery compared to respiratory and oxygenation parameters.
Which number marks the location where the nurse would auscultate the point of maximal impulse (PMI)?
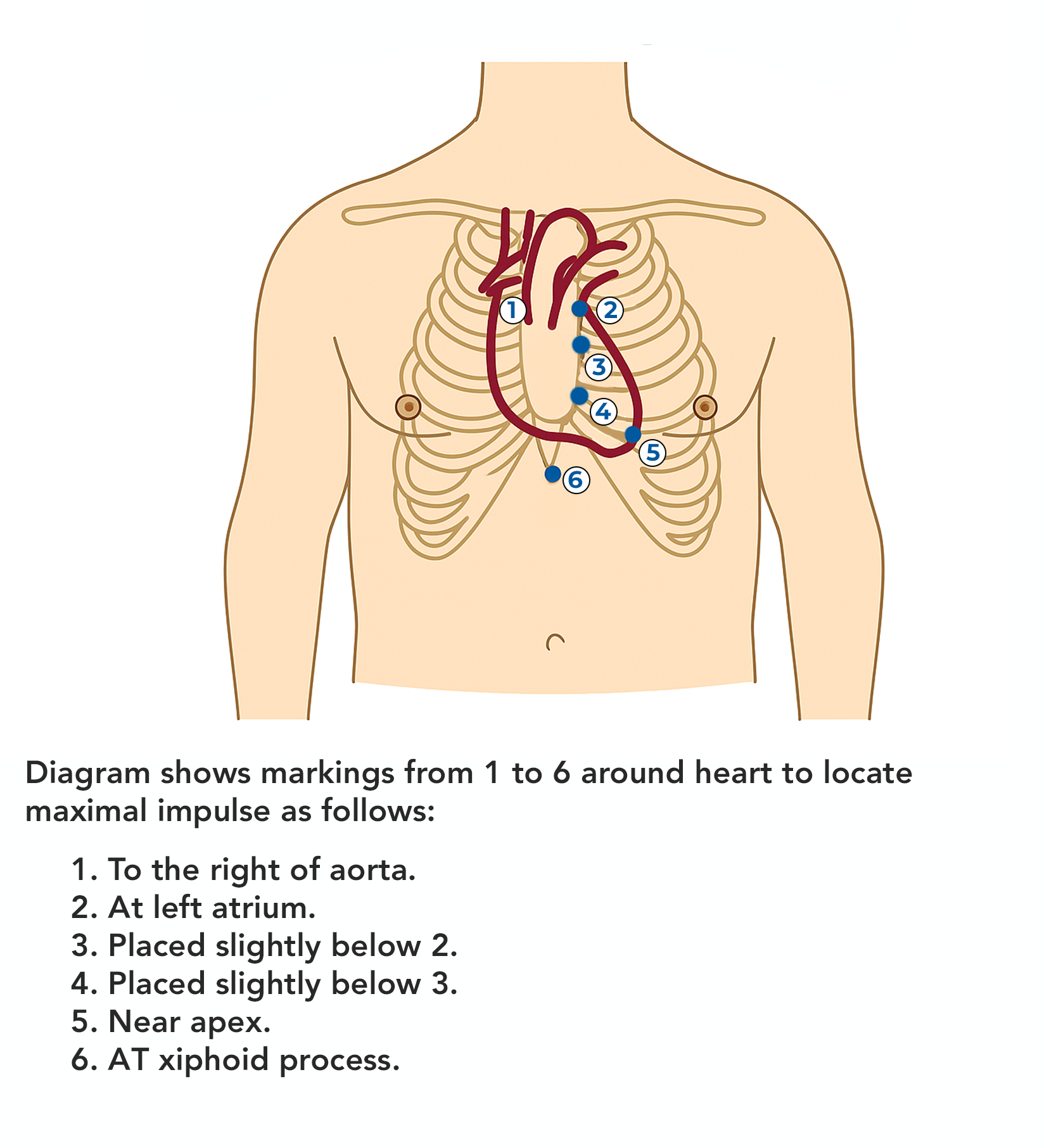
Explanation
The Point of Maximal Impulse (PMI), also referred to as the apical impulse, is the location on the chest wall where the heartbeat is most strongly felt or heard. It corresponds to the apex of the heart, typically located at the 5th intercostal space, midclavicular line in adults
Rationale for correct answers:
E. Near apex: This point corresponds to the 5th intercostal space at the midclavicular line, where the apex of the heart contacts the chest wall. It is the most accurate site for auscultating the apical pulse and evaluating left ventricular function.
Rationale for incorrect answers:
A. To the right of the aorta. This is in the right upper sternal border, typically used to auscultate the aortic valve area. It is not associated with the PMI or apex of the heart.
B. At left atrium: This is positioned more posteriorly in the chest and not palpable or auscultated directly from the anterior chest wall.
C. Placed slightly below 2: Still in the left parasternal area, likely over the pulmonic or tricuspid area, but not the apex.
D. Placed slightly below 3: This is near the left lower sternal border, where tricuspid sounds may be heard, but it's still not the apex.
F. At xiphoid process: This is the epigastric area, well below the heart’s apex, and is not used to assess apical pulse or PMI.
Take-home points:
- The PMI is best auscultated at the 5th intercostal space, midclavicular line, which corresponds to point 5 in the diagram.
- Accurate location of the PMI is essential in assessing left ventricular function and detecting cardiac enlargement or displacement.
During admission of an obese patient with heart failure the assistive personnel (AP) reports to the nurse that the blood pressure (BP) is 140/76 on the left arm and 128/72 on the right arm. What actions do you take on the basis of this information? Select all that apply
Explanation
A difference in blood pressure readings between arms can be a normal variation (up to 10 mm Hg) or a sign of vascular disease such as subclavian artery stenosis, aortic dissection, or peripheral arterial disease.
Rationale for correct answers:
B. Repeat the measurements on both arms using a stethoscope: The AP may have used an automated cuff, which can be less accurate in obese patients or those with arrhythmias.
E. Review the patient’s record for her baseline vital signs: Comparing with previous BP readings helps determine whether the difference is new, worsening, or chronic.
Rationale for incorrect answers:
A. Notify the health care provider immediately: A 12 mm Hg systolic difference may warrant further evaluation if persistent, but notifying the provider immediately is premature.
C. Ask the patient whether she has taken her blood pressure medications recently: BP medication doesn’t cause a discrepancy between the two limbs.
D. Obtain blood pressure measurements on lower extremities: Lower extremity BP may be needed if there is suspicion of aortic coarctation or severe vascular disease, but this is not routinely indicated for a 12 mm Hg arm difference.
Take-home points:
- A systolic BP difference of >10 mm Hg between arms should be manually verified and assessed in context of clinical history and baseline.
- Nurses must take a stepwise approach-recheck manually, gather history, review baseline-before escalating to a provider.
A patient with heart failure is one-day postoperative for major abdominal surgery. When the nurse and the assistive personnel raise the head of the bed to sit the patient on the side of the bed before ambulation, the patient immediately complains of dizziness and nausea. What are your immediate actions? Select all that apply
Explanation
Postoperative patients, especially those with heart failure, are at increased risk for orthostatic hypotension due to bedrest, anesthetic effects, and volume shifts. Orthostatic intolerance may manifest as dizziness, nausea, or fainting when the client is moved from lying to sitting or standing.
Rationale for correct answers:
A. Lower the head of the bed and return the patient to the supine position: This is the first and most important safety step to prevent fainting or falls. Returning to a supine position helps restore cerebral perfusion, relieving dizziness.
B. Obtain vital signs: Vital signs (especially blood pressure and heart rate) should be obtained to assess for orthostatic hypotension or other hemodynamic instability.
D. Allow the patient to rest for 20 to 30 minutes: After returning to a safe position, resting allows stabilization of blood pressure and heart rate. Many patients tolerate activity better after a brief rest period.
E. Raise the head of the bed again and obtain blood pressure readings: Gradually raising the head of the bed and monitoring orthostatic BPs is part of safely assessing tolerance to positional changes.
Rationale for incorrect answer:
C. Encourage the patient to try to sit on the side of the bed and then stand: Encouraging further movement while the patient is symptomatic is unsafe. Doing so may worsen symptoms and risk falls or cardiovascular collapse.
Take-home points:
- Immediate safety actions (return to supine, assess vitals) are essential when a patient becomes dizzy with movement.
- Orthostatic BP monitoring and gradual progression to activity can help prevent falls and guide safe ambulation.
It is important to have the appropriate cuff size when taking the blood pressure. What error may result from a cuff that is too large or too small?
Explanation
The American Heart Association recommends selecting a cuff size based on the circumference of the patient’s upper arm, not just age or weight.
Rationale for correct answer:
A. An incorrect reading: Using the wrong cuff size is the most common error in BP measurement. A cuff too small may falsely elevate the BP reading. A cuff too large may falsely lower the reading.
Rationale for incorrect answers:
B. Injury to the patient: While rare, prolonged or repeated inflation could cause discomfort, especially in fragile patients, but injury is uncommon due to cuff size alone.
C. Prolonged pressure on the arm: The duration of pressure is more related to how long the cuff is inflated, not its size.
D. Loss of Korotkoff sounds is typically related to improper stethoscope placement, cuff deflation speed, or poor technique, not cuff size alone.
Take-home points:
- Using the wrong cuff size results in inaccurate BP readings, which may lead to misdiagnosis and improper management.
- Always measure the mid-upper arm circumference and choose a cuff that covers 40% of the arm's width and 80% of its length for accuracy.
A patient has intravenous fluids infusing in the right arm. When taking a blood pressure on this patient, what would the nurse do in this situation?
Explanation
Site selection for BP measurement must be individualized and based on current clinical interventions, limb condition, and nursing judgment to ensure both safety and accuracy.
Rationale for correct answer:
B. Take the blood pressure in the left arm: The opposite limb (in this case, the left arm) should be used when an IV is infusing in the right arm. This ensures accurate BP measurement and protects the integrity of the IV site.
Rationale for incorrect answers:
A. Take the blood pressure in the right arm: Taking BP on the same arm as an active IV infusion may lead to: Occlusion or backflow in the IV-line, inaccurate readings due to fluid dynamics or risk of infiltration or discomfort.
C. Use the smallest possible cuff: Using a cuff that is too small can produce falsely high BP readings. The cuff size should be based on the client’s arm circumference, not the IV presence.
D. Report inability to take the blood pressure: There is no need to omit the BP assessment, as an alternative arm is available. Only if both arms are contraindicated (e.g., bilateral mastectomy, IVs, injuries) would the nurse need to report the inability and consider alternatives (e.g., leg BP).
Take-home points:
- Never take blood pressure in an arm with an active IV infusion unless absolutely necessary and no other options are available.
- Always assess for site limitations before taking BP and use the opposite limb when contraindications are present.
A patient has a blood pressure reading of 130/90 mm Hg when visiting a clinic. What would the nurse recommend to the patient?
Explanation
According to guidelines like JNC 7 and ACC/AHA, consistent elevated readings over multiple visits are necessary to diagnose hypertension. Nurses play a vital role in recognizing abnormal readings, educating patients, and guiding appropriate follow-up to prevent long-term complications like stroke or heart disease.
Rationale for correct answer:
A. Follow-up measurements of blood pressure: A single elevated BP does not confirm a diagnosis of hypertension. The nurse should recommend rechecking BP on separate occasions, as per guidelines, to determine if the elevation is persistent.
Rationale for incorrect answers:
B. Immediate treatment by a physician: Immediate treatment is not warranted based on a single mildly elevated BP unless the patient is symptomatic or has evidence of organ damage.
C. Nothing, because the nurse considers this reading is due to anxiety: While anxiety (white-coat hypertension) may cause temporary elevation, it should not be assumed without confirmation.
D. A change in dietary intake: Dietary changes (e.g., low sodium, DASH diet) are important in preventing or managing hypertension. However, before prescribing lifestyle changes, the first step is to confirm whether BP is consistently elevated.
Take-home points:
- A single reading of 130/90 mm Hg should prompt follow-up measurements, not immediate diagnosis or treatment.
- Nurses should avoid assumptions and use evidence-based protocols to guide BP assessment and education.
A student nurse is learning to assess blood pressure. What does the blood pressure measure?
Explanation
When nurses measure BP, they are not simply evaluating blood flow, but rather the pressure exerted by circulating blood on the walls of the arteries during the cardiac cycle.
Rationale for correct answer:
B. Force of blood against arterial walls: Blood pressure specifically refers to the force exerted by the blood on the walls of the arteries as the heart pumps. Systolic pressure is the peak force during ventricular contraction, while diastolic pressure is the residual force during relaxation.
Rationale for incorrect answers:
A. Flow of blood through the circulation: Blood pressure is related to blood flow but does not measure it directly.
C. Force of blood against venous walls: While venous pressure exists, it is much lower than arterial pressure and is not what is measured during routine BP assessment.
D. Flow of blood through the heart: This refers to cardiac output or blood volume, not pressure. Blood pressure reflects resistance and force in the arteries, not the amount of blood passing through the heart chambers.
Take-home points:
- Blood pressure is the force of blood against the arterial walls, not a direct measure of blood flow or heart volume.
- Accurate understanding of BP helps nurses assess for hypertension, hypotension, and perfusion status, and supports safe clinical decision-making.
Exams on Vital Signs
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
- Describe the physiological mechanisms governing temperature, pulse, respiration, and blood pressure.
- Identify the normal age-related variations for vital sign measurements.
- Select the appropriate equipment used to take vital signs and perform a physical examination.
- Describe the correct positioning of the client for performing a physical examination.
- Identify the sites for measuring vital signs.
- Assess temperature, pulse, respiration, and blood pressure.
Introduction
The most frequent and routine measurements obtained by health care providers are those of temperature, pulse, blood pressure (BP), respiratory rate, and oxygen saturation.
These measurements reflect a patient’s health status by indicating the effectiveness of circulatory, respiratory, neural, and endocrine body functions.
Because of their importance, they are referred to as vital signs (VS). Pain, a subjective symptom, is often called another vital sign and is frequently measured with the others.
An alteration in vital signs signals a change in physiological function.
Assessment of vital signs provides data to identify nursing diagnoses, implement planned interventions, and evaluate outcomes of care.
Acceptable Ranges For Adults
Temperature range
- Average temperature range: 36° to 38°C (96.8° to 100.4°F)
- Average oral/tympanic: 37°C (98.6°F)
- Average rectal: 37.5°C (99.5°F)
- Axillary: 36.5°C (97.7°F)
Pulse
- 60 to 100 beats/min, strong and regular
Pulse oximetry (SpO2)
- Normal: SpO2 ≥95%
Respirations
- 12 to 20 breaths/min, deep and regular
Blood pressure
- Systolic <120 mm Hg
- Diastolic <80 mm Hg
- Pulse pressure: 30 to 50 mm Hg
Capnography (EtCO2)
- Normal: 35-45 mm Hg
When to Measure Vital Signs:
- On admission to a health care agency
- When assessing a patient during home care visits
- In a clinic setting before a health care provider examines the patient and after any invasive procedures
- In a hospital on a routine schedule according to the health care provider’s order or hospital standards of practice
- Before, during, and after a surgical procedure or invasive diagnostic/treatment procedure
- Before, during, and after a transfusion of any type of blood product
- Before, during, and after the administration of medication or therapies that affect cardiovascular, respiratory, or temperature-control functions
- Before, during, and after nursing interventions influencing a vital sign (e.g., before and after a patient previously on bed rest ambulates, before and after the patient performs range-of-motion exercises)
- When a patient reports nonspecific symptoms of physical distress (e.g., feeling “funny” or “different”)
- When a patient’s general physical condition changes (e.g., loss of consciousness or increased intensity of pain)
Body Temperature
Body temperature reflects the balance between the heat produced and the heat lost from the body, and is measured in heat units called degrees. 2 kinds:
- Core temperature is the temperature of the deep tissues of the body, such as the abdominal cavity and pelvic cavity. It remains relatively constant.
- Surface temperature is the temperature of the skin, the subcutaneous tissue, and fat. It, by contrast, rises and falls in response to the environment.
Factors affecting body’s heat production:
- Basal metabolic rate-younger the person, the higher the BMR
- Muscle activity-shivering
- Thyroxine output-increases the rate of cellular metabolism
- Epinephrine, norepinephrine, and sympathetic stimulation/ stress response
- Fever- increases the cellular metabolic rate
Heat is lost from the body through radiation, conduction, convection, and evaporation.
Regulation of body temperature:
The system that regulates body temperature has three main parts:
- sensors in the periphery and in the core- sensory receptors
- an integrator in the hypothalamus
- an effector system that adjusts the production and loss of heat.
The hypothalamic integrator is the center that controls the core temperature. When the integrator detects heat, it sends out signals intended to reduce the temperature, that is, to decrease heat production and increase heat loss. In contrast, when the cold sensors are stimulated, the integrator sends out signals to increase heat production and decrease heat loss.
Factors affecting body temperature:
-
Age: Older adults are also particularly sensitive to extremes in the environmental temperature due to decreased thermoregulatory controls. Infants are greatly influenced by the temperature of the environment and must be protected from extreme changes.
- Diurnal variations (circadian rhythms): Body temperatures normally change throughout the day, varying as much as 1.0°C (1.8°F) between the early morning and the late afternoon.
- Exercise: Hard work or strenuous exercise can increase body temperature to as high as 38.3°C to 40°C.
- Hormones: Ovulation raises body temperature by about 0.3°C to 0.6°C (0.5°F to 1.0°F) above basal temperature.
- Stress: Stimulation of the sympathetic nervous system can increase the production of epinephrine and norepinephrine, thereby increasing metabolic activity and heat production.
- Environment: Extremes in environmental temperatures can affect a person’s temperature regulatory systems.
Alterations in Body temperature:
The normal range for adults is considered to be between 36°C and 37.5°C (96.8°F to 99.5°F).
There are two primary alterations in body temperature: pyrexia and hypothermia.
1. Pyrexia
A body temperature above the usual range is called pyrexia, hyperthermia, or (in lay terms) fever.
A very high fever, such as 41°C (105.8°F), is called hyperpyrexia.
4 common types of fever:
- Intermittent-body temperature alternates at regular intervals
- Remittent- wide range of temperature fluctuations within 24hrs
- Relapsing- short febrile periods of a few days are interspersed with periods of 1 or 2 days of normal temperature
- Constant- body temperature fluctuates minimally but always remains above normal
In some conditions, an elevated temperature is not a true fever. Two examples are heat exhaustion and heat stroke.
Heat exhaustion: paleness, dizziness, nausea, vomiting, fainting, and a moderately increased temperature (38.3°C to 38.9°C [101°F to 102°F]).
Heat stroke- generally have been exercising in hot weather, have warm, flushed skin, and often do not sweat. They usually have a temperature of 41.1°C (106°F) or higher, and may be delirious, unconscious, or having seizures.
Nursing interventions for clients with fever:
- Monitor vital signs.
- Assess skin color and temperature.
- Monitor white blood cell count, hematocrit value, and other pertinent laboratory reports for indications of infection or dehydration.
- Remove excess blankets when the client feels warm, but provide extra warmth when the client feels chilled.
- Provide adequate nutrition and fluids (e.g., 2,500–3,000 mL/ day) to meet the increased metabolic demands and prevent dehydration.
- Measure intake and output.
- Reduce physical activity to limit heat production, especially during the flush stage.
- Administer antipyretics (drugs that reduce the level of fever) as ordered.
- Provide oral hygiene to keep the mucous membranes moist.
- Provide a tepid sponge bath to increase heat loss through conduction.
- Provide dry clothing and bed linens.
2. Hypothermia
Hypothermia is a core body temperature below the lower limit of normal. The three physiological mechanisms of hypothermia are
- excessive heat loss
- inadequate heat production to counteract heat loss
- impaired hypothalamic thermoregulation.
Hypothermia may be induced or accidental.
Induced hypothermia is the deliberate lowering of the body temperature to decrease the need for oxygen by the body tissues such as during certain surgeries.
Accidental hypothermia can occur as a result of (a) exposure to a cold environment, (b) immersion in cold water, and (c) lack of adequate clothing, shelter, or heat.
Clinical manifestations:
- Decreased body temperature, pulse, and respirations
- Severe shivering (initially)
- Feelings of cold and chills
- Pale, cool, waxy skin
- Frostbite (discolored, blistered nose, fingers, toes)
- Hypotension
- Decreased urinary output
- Lack of muscle coordination
- Disorientation
- Drowsiness progressing to coma
Nursing interventions for clients with hypothermia:
- Provide a warm environment.
- Provide dry clothing.
- Apply warm blankets.
- Keep limbs close to the body.
- Cover the client’s scalp with a cap or turban.
- Supply warm oral or intravenous fluids.
- Apply warming pads.
Assessing body temperature
Sites:
The most common sites for measuring body temperature are oral, rectal, axillary, tympanic membrane, and skin/temporal artery.
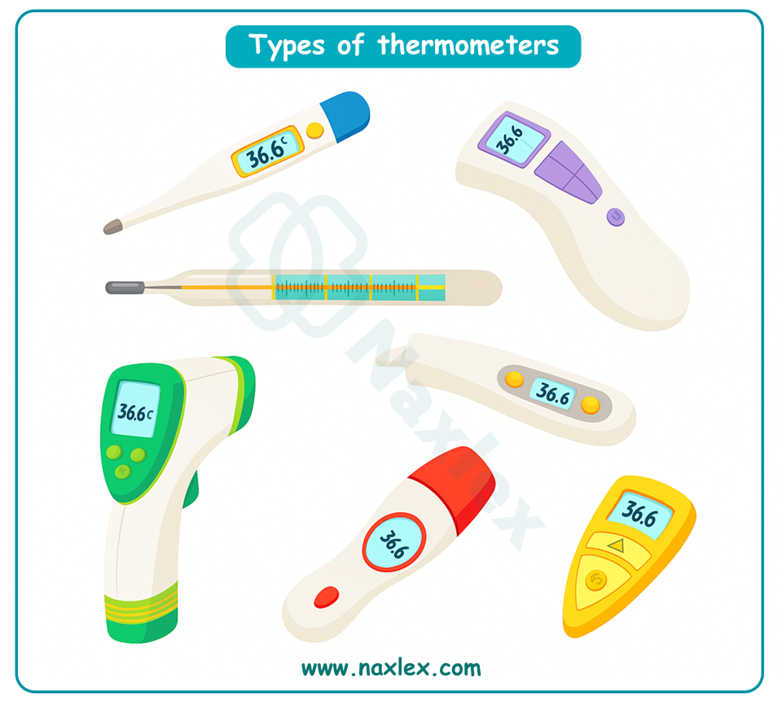
Types of thermometers:
- Mercury-in glass thermometers.
- Electronic thermometers
- Chemical disposable thermometers
- Temperature-sensitive tape
- Infrared thermometers
- Temporal artery thermometers
Temperature scales:
To convert from Fahrenheit to Celsius, deduct 32 from the Fahrenheit reading and then multiply by the fraction 5/9; that is:
C = (Fahrenheit temperature - 32) × 5/9
To convert from Celsius to Fahrenheit, multiply the Celsius reading by the fraction 9/5 and then add 32; that is:
F = (Celsius temperature × 9/5) + 32
Nursing insights
Lifespan considerations:
1. Infants/ children:
The body temperature of newborns is extremely labile, and newborns must be kept warm and dry to prevent hypothermia.
The tympanic route is fast and convenient. Place the infant supine and stabilize the head. Pull the pinna straight back and slightly downward. Remember that the pinna is pulled upward for children over 3 years of age and adults, but downward for children younger than age 3.
Avoid the tympanic route in a child with active ear infections or tympanic membrane drainage tubes.
2. Older adults:
Older adults’ temperatures are strongly influenced by both environmental and internal temperature changes. Their thermoregulation control processes are not as efficient as when they were younger, and they are at higher risk for both hypothermia and hyperthermia.
Pulse
The pulse is a wave of blood created by contraction of the left ventricle of the heart. Generally, the pulse wave represents the stroke volume output or the amount of blood that enters the arteries with each ventricular contraction.
- A peripheral pulse is a pulse located away from the heart, for example, in the foot or wrist.
- The apical pulse, in contrast, is a central pulse; that is, it is located at the apex of the heart. It is also referred to as the point of maximal impulse (PMI).
Factors affecting the pulse:
-
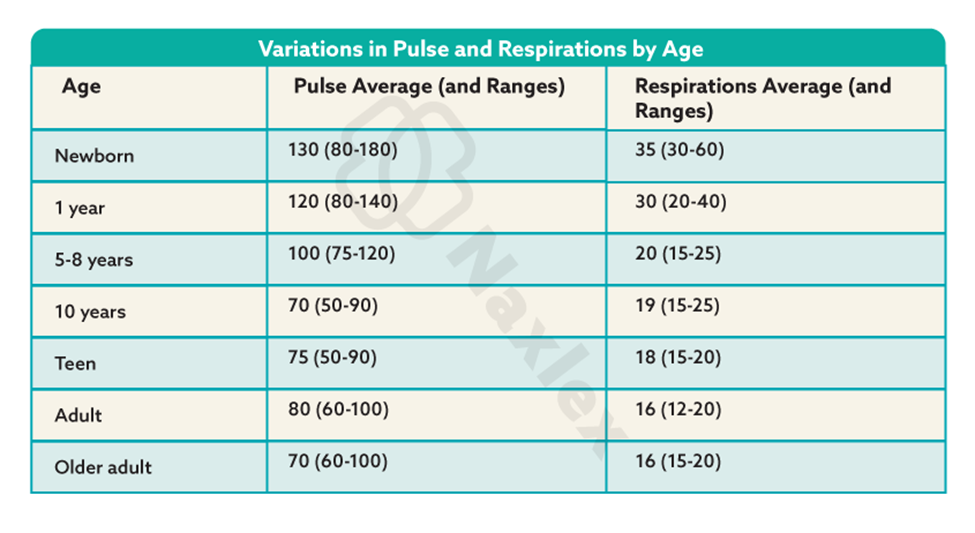
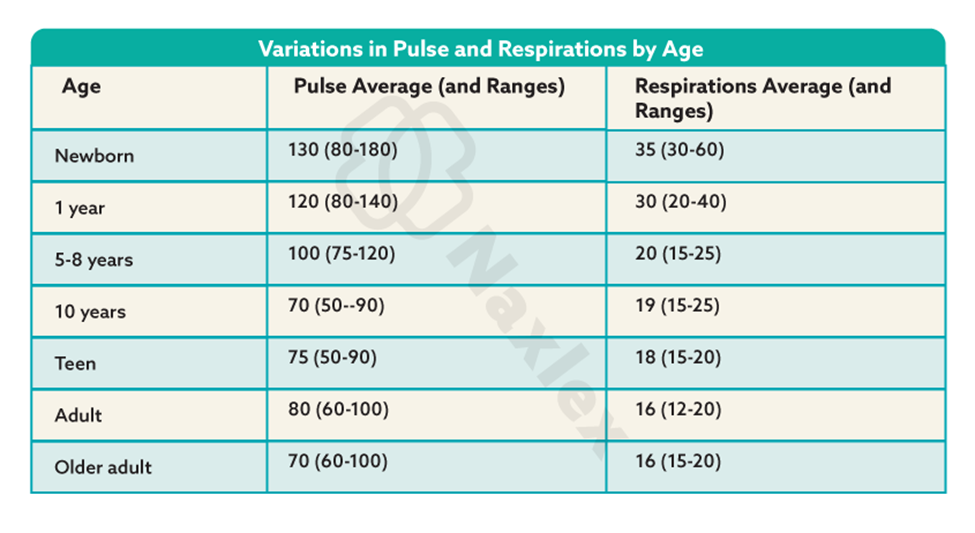
Age: As age increases, the pulse rate gradually decreases overall.
- Sex: After puberty, the average male’s pulse rate is slightly lower than the female’s.
- Exercise: The pulse rate normally increases with activity.
- Fever: Increases (a) in response to the lowered blood pressure that results from peripheral vasodilation associated with elevated body temperature and (b) because of the increased metabolic rate.
- Medications: Some medications decrease the pulse rate, and others increase it.
- Hypovolemia/dehydration: Loss of blood from the vascular system increases the pulse rate.
- Stress: In response to stress, sympathetic nervous stimulation increases the overall activity of the heart.
- Position: When a person is sitting or standing, blood usually pools in dependent vessels of the venous system- transient increase in heart rate.
- Pathology: Certain diseases such as some heart conditions or those that impair oxygenation can alter the resting pulse rate.
Pulse sites:
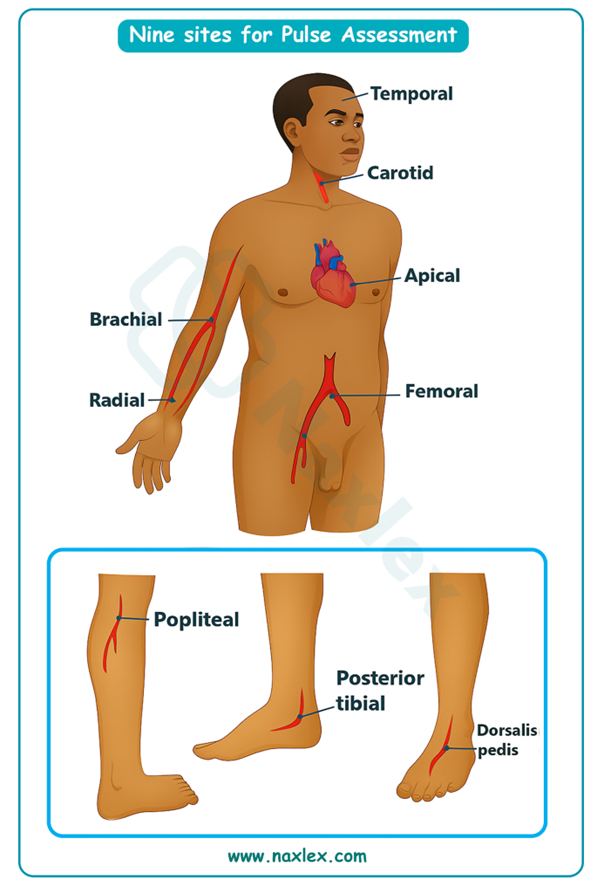
Assessing the pulse:
A pulse is commonly assessed by palpation (feeling) or auscultation (hearing).
A stethoscope is used for assessing apical pulses.
A Doppler ultrasound stethoscope is used for pulses that are difficult to assess.
When assessing the pulse, the nurse collects the following data:
- the rate
- rhythm
- volume
- arterial wall elasticity
- presence or absence of bilateral equality
Abnormalities of pulse:
An excessively fast heart rate (e.g., over 100 beats/min in an adult) is referred to as tachycardia. A heart rate in an adult of less than 60 beats/min is called bradycardia.
A pulse with an irregular rhythm is referred to as a dysrhythmia or arrhythmia.
Pulse volume, also called the pulse strength or amplitude, refers to the force of blood with each beat. It can range from absent to bounding.
Apical-radial pulse assessment
Normally, the apical and radial rates are identical.
Any discrepancy between the two pulse rates is called a pulse deficit and needs to be reported promptly.
Respirations
Respiration is the act of breathing.
Inhalation or inspiration refers to the intake of air into the lungs. Exhalation or expiration refers to breathing out or the movement of gases from the lungs to the atmosphere.
Ventilation is also used to refer to the movement of air in and out of the lungs.
There are basically two types of breathing:
- costal (thoracic) breathing- involves the external intercostal muscles and other accessory muscles.
- diaphragmatic (abdominal) breathing- involves the contraction and relaxation of the diaphragm.
Assessing respirations:
Resting respirations should be assessed when the client is relaxed.
Before assessing a client’s respirations, a nurse should be aware of the following:
- The client’s normal breathing pattern
- The influence of the client’s health problems on respirations
- Any medications or therapies that might affect respirations
- The relationship of the client’s respirations to cardiovascular function
The rate, depth, rhythm, quality, and effectiveness of respirations should be assessed.
Abnormally slow respirations are referred to as bradypnea, and abnormally fast respirations are called tachypnea or polypnea. Apnea is the absence of breathing.
Altered Breathing Patterns and Sounds:
Nursing insights
Lifespan considerations:
- An infant or child who is crying will have an abnormal respiratory rate and rhythm and needs to be quieted before respirations can be accurately assessed.
- Infants and young children use their diaphragms for inhalation and exhalation. If necessary, place your hand gently on the infant’s abdomen to feel the rapid rise and fall during respirations.
- Most newborns are complete nose breathers, so nasal obstruction can be life threatening.
- Older adults experience anatomic and physiological changes that cause the respiratory system to be less efficient. Any changes in rate or type of breathing should be reported immediately.
Oxygen Saturation
A pulse oximeter is a noninvasive device that estimates a client’s arterial blood oxygen saturation (SaO2) by means of a sensor attached to the client’s finger, toe, nose, earlobe, or forehead (or around the hand or foot of a neonate).
The pulse oximeter’s sensor has two parts:
- two light-emitting diodes (LEDs)- one red, the other infrared-that transmit light through nails, tissue, venous blood, and arterial blood.
- a photodetector placed directly opposite the LEDs (e.g., the other side of the finger, toe, or nose).
Factors affecting oxygen saturation readings:
-
Hemoglobin. If the hemoglobin is fully saturated with oxygen, the SpO2 will appear normal even if the total hemoglobin level is low.
- Circulation. The oximeter will not return an accurate reading if the area under the sensor has impaired circulation.
- Activity. Shivering or excessive movement of the sensor site may interfere with accurate readings.
- Carbon monoxide poisoning. Pulse oximeters cannot discriminate between hemoglobin saturated with carbon monoxide versus oxygen.
Nursing insights
Lifespan considerations:
INFANTS • If an appropriate-sized finger or toe sensor is not available, consider using an earlobe or forehead sensor.
CHILDREN •Instruct the child that the sensor does not hurt. Disconnect the probe whenever possible to allow for movement.
OLDER ADULTS •Use of vasoconstrictive medications, poor circulation, or thickened nails may make finger or toe sensors inaccurate.
Blood Pressure
Arterial blood pressure is a measure of the pressure exerted by the blood as it flows through the arteries. Because the blood moves in waves, there are two blood pressure measurements.
- The systolic pressure is the pressure of the blood as a result of contraction of the ventricles, that is, the pressure of the height of the blood wave.
- The diastolic pressure is the pressure when the ventricles are at rest.
The difference between the diastolic and the systolic pressures is called the pulse pressure. A normal pulse pressure is about 40 mmHg but can be as high as 100 mmHg during exercise.
Blood pressure is measured in millimeters of mercury (mmHg) and recorded as a fraction: systolic pressure over the diastolic pressure.
Mean arterial pressure (MAP): this represents the pressure actually delivered to the body’s organs. A normal MAP is 70 to 110 mmHg.
Determinants of Blood pressure:
- Pumping action of the heart: When the pumping action of the heart is weak, less blood is pumped into arteries (lower cardiac output), and the blood pressure decreases.
- Peripheral vascular resistance: Peripheral resistance can increase blood pressure.
- Blood volume: When the blood volume decreases (for example, as a result of a hemorrhage or dehydration), the blood pressure decreases because of decreased fluid in the arteries.
- Blood viscosity: Blood pressure is higher when the blood is highly viscous (thick)- higher hematocrit.
Factors affecting blood pressure:
-
Age. Newborns have a systolic pressure of about 75 mmHg. The pressure rises with age, reaching a peak at the onset of puberty, and then tends to decline somewhat.
- Exercise. Physical activity increases the cardiac output and hence the blood pressure.
- Stress. Stimulation of the sympathetic nervous system increases cardiac output and vasoconstriction of the arterioles, thus increasing the blood pressure reading.
- Race. African Americans older than 35 years tend to have higher blood pressures than European Americans of the same age.
- Sex. After puberty, females usually have lower blood pressures than males of the same age.
- Medications. Many medications, including caffeine, may increase or decrease the blood pressure.
- Obesity. Both childhood and adult obesity predispose hypertension.
- Diurnal variations. Pressure is usually lowest early in the morning, when the metabolic rate is lowest.
- Medical conditions. Any condition affecting the cardiac output, blood volume, blood viscosity, and/or compliance of the arteries has a direct effect on the blood pressure.
- Temperature. Because of increased metabolic rate, fever can increase blood pressure.
Hypertension:
A blood pressure that is persistently above normal is called hypertension.
- An elevated blood pressure of unknown cause is called primary hypertension.
- An elevated blood pressure of known cause is called secondary hypertension.
Hypotension:
Hypotension is a blood pressure that is below normal, that is, a systolic reading consistently between 85 and 110 mmHg in an adult whose normal pressure is higher than this.
Orthostatic hypotension is a blood pressure that decreases when the client sits or stands.
Assessing Blood pressure:
Blood pressure is measured with a blood pressure cuff, a sphygmomanometer, and a stethoscope.
There are two types of sphygmomanometers: aneroid and digital.
Doppler ultrasound stethoscopes are also used to assess blood pressure. These are of particular value when blood pressure sounds are difficult to hear, such as in infants, obese clients, and clients in shock.
Sites for assessment:
Client’s upper arm using the brachial artery and a standard stethoscope.
Blood pressure is not measured on a particular client’s limb in the following situations:
- The shoulder, arm, or hand (or the hip, knee, or ankle) is injured or diseased.
- A cast or bulky bandage is on any part of the limb.
- The client has had surgical removal of breast or axillary (or inguinal) lymph nodes on that side.
- The client has an intravenous infusion or blood transfusion in that limb.
- The client has an arteriovenous fistula (e.g., for renal dialysis) in that limb.
Methods:
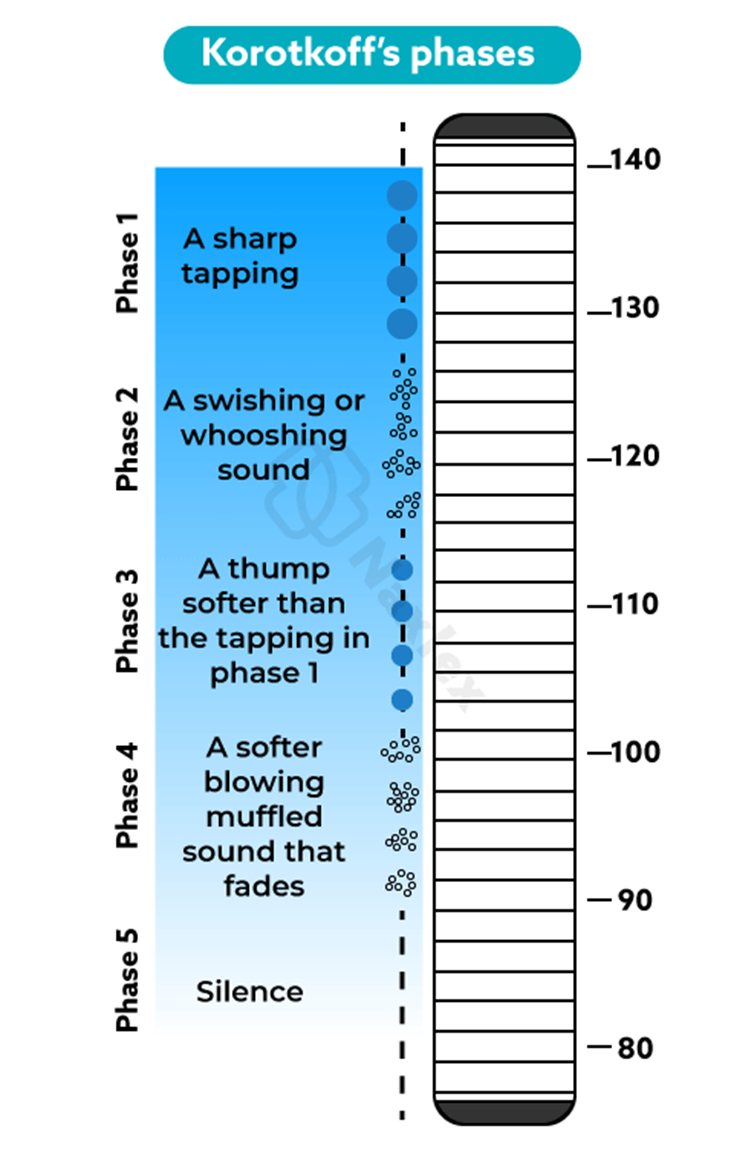
When taking a blood pressure using a stethoscope, the nurse identifies phases in the series of sounds called Korotkoff’s sounds.
The systolic pressure is the point where the first tapping sound is heard (phase 1). In adults, the diastolic pressure is the point where the sounds become inaudible (phase 5).
An auscultatory gap, which occurs particularly in hypertensive clients, is the temporary disappearance of sounds normally heard over the brachial artery when the cuff pressure is high followed by the reappearance of the sounds at a lower level.
Korotkoff’s sounds:
Phase 1: The pressure level at which the first faint, clear tapping or thumping sounds are heard. These sounds gradually become more intense. To ensure that they are not extraneous sounds, the nurse should identify at least two consecutive tapping sounds. The first tapping sound heard during deflation of the cuff is the systolic blood pressure.
Phase 2: The period during deflation when the sounds have a muffled, whooshing, or swishing quality.
Phase 3: The period during which the blood flows freely through an increasingly open artery and the sounds become crisper and more intense and again assume a thumping quality but softer than in phase 1.
Phase 4: The time when the sounds become muffled and have a soft, blowing quality.
Phase 5: The pressure level when the last sound is heard. This is followed by a period of silence. The pressure at which the last sound is heard is the diastolic blood pressure in adults.
Common errors in assessing Blood pressure
- Bladder cuff too narrow/ Bladder cuff too wide
- Arm unsupported
- Insufficient rest before the assessment
- Repeating assessment too quickly
- Cuff wrapped too loosely or unevenly
- Deflating cuff too quickly/ Deflating cuff too slowly
- Failure to use the same arm consistently
- Arm above level of the heart
- Assessing immediately after a meal or while client smokes or has pain
- Failure to identify auscultatory gap
Nursing insights
Lifespan considerations:
Infants
- Use a pediatric stethoscope with a small diaphragm.
- The lower edge of the blood pressure cuff can be closer to the antecubital space of an infant.
- The systolic blood pressure of a newborn averages about 75 mmHg
Children:
- Explain each step of the process and what it will feel like. Demonstrate on a doll.
- In children, the diastolic pressure is considered to be the onset of phase 4, where the sounds become muffled.
- Take the blood pressure prior to other uncomfortable procedures so that the blood pressure is not artificially elevated by the discomfort.
Older adults:
Medications that cause vasodilation (antihypertensive medications) and also the loss of baroreceptor efficiency in older clients place them at increased risk for having orthostatic hypotension.
Summary
- Vital signs reflect changes in body function that otherwise might not be observed.
- Body temperature is the balance between heat produced by and heat lost from the body.
- Factors affecting body temperature include age, diurnal variations, exercise, hormones, stress, and environmental temperatures.
- Pulse rate and volume reflect the stroke volume output, the compliance of the client’s arteries, and the adequacy of blood flow.
- The difference between the apical and radial pulses is called the pulse deficit.
- Blood pressure reflects the pumping action of the heart, peripheral vascular resistance, blood volume, and blood viscosity.
- A pulse oximeter measures the percent of hemoglobin saturated with oxygen. A normal result is 95% to 100%.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Vital Signs
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


