Please set your exam date
Health problems in children (infancy to adolescence)
Study Questions
Practice Exercise 1
Vitamin A may be administered in significant amounts to children with this childhood communicable illness to decrease morbidity and mortality:
Explanation
Measles is a highly contagious viral illness that can cause severe complications in children, especially in those who are malnourished or vitamin A–deficient. Vitamin A supplementation has been shown to significantly reduce measles-related morbidity and mortality by enhancing immune function, supporting epithelial integrity, and reducing the risk of severe complications like pneumonia and blindness.
Rationale for correct answer:
D. Measles virus can cause severe respiratory and systemic illness. Vitamin A deficiency worsens outcomes by impairing immune defenses and tissue repair. WHO and UNICEF recommend high-dose vitamin A for all children diagnosed with measles to reduce severity and fatality rates.
Rationale for incorrect answers:
A. Pertussis caused by Bordetella pertussis, it affects the respiratory tract but does not benefit from vitamin A supplementation in terms of morbidity or mortality reduction.
B. Varicella caused by the varicella-zoster virus, this usually has a mild course in healthy children and does not require vitamin A supplementation.
C. Rubella caused by the rubella virus, it is typically mild in children; prevention is via vaccination, and vitamin A is not part of management.
Take home points
- Measles can cause severe complications such as pneumonia, diarrhea, and blindness, particularly in vitamin A–deficient children.
- WHO recommends administering vitamin A to all children with measles to reduce morbidity and mortality.
- Early recognition and supportive care, including nutritional support, are essential in measles management.
A 10-year-old child with a peanut allergy would be expected to have which of these as an early manifestation of his allergy? Select all that apply
Explanation
Peanut allergy is an IgE-mediated hypersensitivity reaction that can occur within minutes of exposure. Early manifestations result from histamine and other inflammatory mediators causing respiratory, gastrointestinal, skin, and cardiovascular symptoms. Recognizing these early signs is critical to prevent progression to life-threatening anaphylaxis.
Rationale for correct answers:
A. Wheezing caused by bronchospasm and airway inflammation due to histamine release in an allergic reaction.
C. Trouble breathing result from airway swelling, bronchoconstriction, and laryngeal edema which may cause dyspnea and stridor, signaling early respiratory compromise.
E. Urticaria are raised, itchy hives are a classic skin manifestation of IgE-mediated allergic reactions.
Rationale for incorrect answer:
B. Gastrointestinal symptoms such as nausea, vomiting, or abdominal pain can occur as a late symptom unlike respiratory symptoms such as dyspnea.
C. Headache is not a typical early manifestation of peanut allergy. While headaches may occur later from hypoxia or hypotension in severe reactions, they are not an early sign.
Take home points
- Early symptoms of peanut allergy can involve the skin, respiratory tract, and gastrointestinal tract.
- Rapid recognition and prompt administration of epinephrine are critical to preventing progression to anaphylaxis.
- Education of caregivers and children on allergen avoidance and emergency action plans is essential.
The recommended treatment for cow’s milk protein allergy is the substitution of cow’s milk–based formula for:
Explanation
Cow’s milk protein allergy (CMPA) is an immune-mediated reaction to proteins such as casein and whey found in cow’s milk. Management involves eliminating cow’s milk protein from the diet and replacing it with a safe, nutritionally adequate alternative. Hydrolyzed formulas contain proteins broken down into smaller peptides, reducing allergenicity. Soy formula may be used in some cases for infants older than 6 months if tolerated.
Rationale for correct answer:
B. Extensively hydrolyzed formulas such as soy milk or a hydrolyzed formula are first-line for most infants with CMPA, as they minimize allergic reactions while providing complete nutrition. Soy formulas may be used in children over 6 months if there is no soy protein allergy.
Rationale for incorrect answers:
A. Goat’s milk is not recommended because it contains proteins similar to those in cow’s milk, which can trigger cross-reactivity.
C. Whole milk still contains cow’s milk proteins and would worsen symptoms.
D. Evaporated milk is derived from cow’s milk and therefore not safe for CMPA. It is also nutritionally inappropriate for infants without proper fortification.
Take home points
- CMPA requires strict elimination of all cow’s milk proteins from the diet.
- Extensively hydrolyzed formulas are preferred; amino acid–based formulas are used in severe or refractory cases.
- Soy formula may be considered for older infants if no soy sensitivity exists.
Which factors are considered protective factors for sudden infant death syndrome (SIDS)?
Explanation
Sudden infant death syndrome (SIDS) is the sudden, unexplained death of an apparently healthy infant, typically during sleep. Certain practices significantly reduce the risk by improving airway patency, lowering arousal thresholds, and supporting immune protection.
Rationale for correct answer:
D. Supine sleeping position keeps the airway clear and reduces the risk of suffocation compared to prone or side positions. Breastfeeding is associated with a lower incidence of SIDS, possibly due to immune benefits and improved arousability from sleep. Vaccination may reduce SIDS risk by preventing infections that could contribute to sudden death.
Rationale for incorrect answers:
A. Side sleeping position, breastfeeding, updated childhood immunization status: Side sleeping is unstable and increases the risk of rolling into a prone position.
B. Supine sleeping position, breastfeeding, soft bedding: Soft bedding increases suffocation and entrapment risk.
C. Prone sleeping position, exposure to maternal tobacco use, updated childhood immunization status: Prone sleeping and tobacco exposure are strong SIDS risk factors.
Take home points
- Place infants on their backs to sleep, on a firm surface, with no loose bedding or soft objects.
- Encourage breastfeeding and keep vaccinations up to date.
- Avoid smoke exposure, overheating, and unsafe sleep environments to reduce SIDS risk.
Practice Exercise 2
The mother of a 4-year-old health clinic patient asks the nurse about night terrors. Which statement by the mother reveals a need for further teaching? Select all that apply
Explanation
Night terrors are a type of parasomnia that typically occur in children aged 3–7 years during non-REM sleep. They are usually self-limiting and not remembered by the child. Management focuses on safety, reassurance, and maintaining good sleep hygiene, not on stimulating activities or co-sleeping.
Rationale for correct answers:
C. Watching TV before bedtime can stimulate the child and worsen sleep disturbances. Understanding “what is real” does not prevent night terrors.
E. Co-sleeping can disrupt sleep cycles and is not recommended as a treatment for night terrors. It may also increase safety risks, particularly in younger children.
Rationale for incorrect answers
A. This statement is true since most children outgrow night terrors by late childhood.
B. Getting into a specific routine is helpful and can be calming to my son is consistent bedtime routines improve sleep quality.
D. Helping the child with sleep by giving him his favorite stuffed animal or using a night-light is acceptable comfort measures that promote a sense of security without interfering with sleep.
Take home points
- Night terrors usually resolve without intervention as the child matures.
- Maintain a calm, consistent bedtime routine and ensure a safe environment.
- Avoid stimulating activities, screen time before bed, and unnecessary co-sleeping.
A child is brought to the emergency department by his parents after noted to be “acting funny” a few hours ago while he was being cared for by his grandmother. When she went to take her evening medication, the grandmother noted that her pill container had been opened and some pills were missing. The parents state that the grandmother has a heart condition. Anticipating the emergency care this child will receive, you know:
Explanation
In suspected pediatric ingestion of potentially cardiotoxic medication such as digoxin, beta-blockers, or calcium channel blockers, rapid assessment and stabilization take priority. Emergency interventions depend on the type of drug, time since ingestion, and clinical status.
Rationale for correct answers:
D. This scenario suggests a possible cardiac medication ingestion such as digoxin, beta-blockers, calcium channel blockers, all of which can cause life-threatening bradycardia, hypotension, arrhythmias, and altered mental status. In pediatric poisoning, airway, breathing, and circulation (ABCs) are the top priorities. Continuous vital sign and neurological assessments allow early detection of deterioration. Cardiac and respiratory support may be required, including supplemental oxygen, IV access, and possible advanced life support measures.
Rationale for incorrect answers:
A. The majority of medications having a specific antidote is false since most medications do not have specific antidotes, and treatment is supportive or involves decontamination methods.
B. Gastric lavage is rarely used today due to risk of aspiration and limited benefit, and is usually only considered within 1 hour of ingestion in life-threatening cases.
C. Activated charcoal should be mixed with water, not milk or juice, as these may reduce its effectiveness. It is used selectively based on drug type and presentation time.
Take home points
- In pediatric poisonings, stabilization of airway, breathing, and circulation comes before any decontamination efforts.
- Many ingestions, including cardiac medications, can cause rapid clinical deterioration.
- Antidotes are rare; most treatment is supportive.
- Activated charcoal should be used appropriately and never with milk or juice.
You are working with the family of a 4-year-old patient and have concerns about possible exposure to lead poisoning. Which information will determine whether follow-up is needed? Select all that apply
Explanation
Lead exposure in children can occur from multiple sources, especially in environments with deteriorating lead-based paint, contaminated dust, or renovations that release lead particles. Any history suggesting possible exposure warrants follow-up regardless of age.
Rationale for correct answers:
A. The child goes daily to the older home of a babysitter: Older homes (built before 1978 in the U.S.) are more likely to have lead-based paint and contaminated dust.
B. One of the child’s playmates in the neighborhood has lead poisoning: Shared environments or similar exposures increase risk, even if the child lives in a different home.
C. Although living in a newer neighborhood, one of the child’s playmates’ homes is being renovated: Renovations in older homes can release lead dust, posing a risk to visiting children.
Rationale for incorrect answers:
D. The child is out of the danger age range for screening (1 to 2 years old), so screening is not needed: While routine screening is most common at ages 1–2, older children with risk factors should also be screened.
E. Past BLL was 12, so no follow-up is needed at this time: A blood lead level (BLL) of 12 µg/dL is above the CDC reference value (currently C.5 µg/dL) and requires follow-up, environmental investigation, and monitoring until levels decrease.
Take home points
- Lead screening should be based on risk factors, not just age.
- Any suspected exposure, through older homes, renovations, or contact with affected individuals, warrants evaluation.
- Even mild elevations in BLL require intervention to prevent long-term neurodevelopmental harm.
When assessing a child’s injury in the emergency department, a nurse suspects physical abuse. Based on this suspicion, the nurse’s primary legal responsibility is to
Explanation
Child abuse refers to any intentional harm or mistreatment of a child under the age of 18. It can occur in various forms and often involves someone the child knows and trusts, such as a parent, caregiver, teacher, or family member.
Rationale for correct answer:
B. Reporting the case in which the abuse is suspected to the local authorities is the nurse’s primary legal duty. Reporting must be done immediately upon suspicion; proof is not required. Failure to report can result in legal consequences for the nurse.
Rationale for incorrect answers:
A. Assisting the family in identifying resources for support is important for long-term care, but not the immediate legal priority when abuse is suspected.
C. Documenting the child’s physical assessment findings accurately and thoroughly is essential for supporting the case, but documentation alone does not fulfill the legal reporting requirement.
D. Referring the family to the hospital support group may be helpful later but is not a legal mandate in the acute setting of suspected abuse.
Take home points
- Nurses must report suspected child abuse promptly; investigation is not the nurse’s role.
- Accurate documentation and cooperation with authorities support the legal process.
- The child’s safety takes priority over all other considerations in suspected abuse cases.
Practice Exercise 3
Which of the following conditions may lead to the development of obesity in children? Select all that apply
Explanation
Childhood obesity results from a combination of behavioral, environmental, and socioeconomic factors that influence caloric intake and energy expenditure. Early identification of risk factors is essential for prevention.
Rationale for correct answers:
A. Reduced physical activity decreases energy expenditure, contributing to a positive energy balance and weight gain.
B. Low socioeconomic status is often associated with limited access to healthy foods, safe play areas, and healthcare, increasing obesity risk.
C. Use of food as a positive reinforcement of desired behaviors encourages emotional eating patterns and overconsumption of calorie-dense foods.
D. Consumption of energy-dense foods and drinks, such as high-calorie, nutrient-poor foods and sugar-sweetened beverages contribute significantly to excess caloric intake.
Rationale for incorrect answer:
E. Positive self-esteem is not a risk factor for childhood obesity. In fact, children with obesity often experience low self-esteem due to stigma and body image concerns.
Take home points
- Childhood obesity is multifactorial, involving lifestyle, socioeconomic, and behavioral influences.
- Prevention strategies should focus on promoting physical activity, balanced nutrition, and healthy coping mechanisms.
- Avoid using food as a behavioral reward to prevent unhealthy eating habits.
Which child should receive further diagnostic testing for chronic abdominal pain? Select all that apply
Explanation
Chronic abdominal pain in children may be due to functional gastrointestinal disorders or underlying organic pathology. Chronic pain is generally defined as pain lasting ≥1 month that interferes with daily activities, or pain associated with alarming features such as gastrointestinal bleeding, persistent diarrhea, weight loss, or abnormal physical findings.
Rationale for correct answers:
A. An 11-year-old boy with a 1-month history of generalized periumbilical pain: This description is a classic presentation of functional abdominal pain. The pain is generalized and centered around the navel, and there are no other "red flag" symptoms like fever, weight loss, or specific location of pain. While it's chronic, lasting over a month, the nature of the pain does not strongly suggest an organic cause.
C. A 12-year-old girl with a 6-week history of constipation: Constipation lasting several weeks may indicate an underlying gastrointestinal disorder and requires further evaluation.
D. A 6-year-old boy with 1 month of diarrhea and a rectal fistula: Presence of a rectal fistula is an alarming sign suggestive of Crohn’s disease or other inflammatory bowel disease, necessitating prompt diagnostic workup.
Rationale for incorrect answer:
B. An 8-year-old girl with a 1-week history of right lower quadrant pain: This is acute rather than chronic abdominal pain; the priority would be to evaluate for acute appendicitis or other emergent causes rather than chronic pain workup.
Take home points
- Chronic abdominal pain workup is indicated when symptoms are persistent (weeks to months) or when there are red flag signs such as weight loss, gastrointestinal bleeding, persistent diarrhea, or abnormal examination findings.
- Conditions like inflammatory bowel disease, celiac disease, and chronic constipation are common organic causes.
- Acute localized pain requires urgent evaluation for surgical causes, not chronic pain assessment.
You are working with a family whose 7-year-old has just been diagnosed with attention-deficit/hyperactivity disorder. Which statements by the mother indicate a need for further teaching? Select all that apply
Explanation
Attention-deficit/hyperactivity disorder (ADHD) is best managed with structured routines, clear and concise communication, and consistent expectations. Misunderstandings about learning strategies or avoiding structure can hinder progress.
Rationale for correct answers:
A. Children with ADHD often have difficulty sustaining attention during lengthy verbal explanations. They benefit more from short, clear instructions, visual aids, and step-by-step guidance.
D. Structure and clear rules actually help children with ADHD. Avoiding rules or reducing structure can worsen symptoms.
Rationale for incorrect answers:
B. Proving the child with a consistent schedule for homework and activities helps him be organized structured routines improve focus and reduce forgetfulness.
C. Stimulant medications can affect appetite and growth, requiring frequent monitoring of the child’s growth.
E. Family counseling is appropriate and can help with coping strategies, stress reduction, and family support.
Take home points
- Children with ADHD benefit from structured environments, clear rules, and short, focused instructions.
- Both medical management and behavioral strategies are important.
Family counseling and collaboration with teachers support the child’s overall progress
A good understanding of enuresis will help the nurse work with children and their families. Which of the following teaching points should be included? Select all that apply
Explanation
Enuresis is involuntary urination beyond the age of expected bladder control, most commonly nocturnal. It is typically benign and often resolves spontaneously, but supportive strategies and sometimes pharmacologic therapy are used when it persists.
Rationale for correct answers:
A. Enuresis, particularly nocturnal enuresis (bed-wetting), is often related to a developmental delay in the nervous system's ability to coordinate bladder control during sleep. It is not caused by a serious disease and usually resolves on its own over time.
B. A significant number of children will stop bed-wetting without any specific intervention, which supports the "self-limiting" aspect of the condition. While the exact percentage can vary slightly in different studies, this figure is a good general approximation.
D. Desmopressin acetate (DDAVP) is a common and effective medical treatment for nocturnal enuresis. It works as an antidiuretic hormone, concentrating urine and decreasing the amount produced by the kidneys at night. This reduces the pressure on the bladder and lowers the likelihood of bed-wetting.
Rationale for incorrect answers:
C. The formula for estimating normal bladder capacity is indeed a child's age plus 2, not D. So, for a 6-year-old, the approximate bladder capacity is 8 ounces (240 ml). The calculation in the statement is incorrect, as 10 ounces is closer to 300 ml, not 600 ml. This makes the entire statement factually incorrect.
E. While enuresis is typically not a sign of a serious emotional disturbance, it is not a form of "willful misbehavior." The child is not doing it on purpose. Teaching parents that it's a behavioral issue can lead to punishment, shaming, and emotional distress for the child, which can in turn worsen the enuresis.
Take home points
- Enuresis is usually a developmental delay in bladder control, not misbehavior.
- Most cases resolve with time; reassurance and support are essential.
- Behavioral interventions, bladder training, and sometimes medications like desmopressin can be helpful.
Practice Exercise 4
What is the most common treatable cause of male-related impaired fertility, especially if diagnosed and treated early?
Explanation
A varicocele is an abnormal dilatation of the pampiniform plexus veins in the spermatic cord, often leading to increased scrotal temperature, oxidative stress, and impaired spermatogenesis. Early detection and surgical repair (varicocelectomy) can significantly improve sperm parameters and fertility outcomes.
Rationale for correct answer:
C. Idiopathic varicocele is strongly linked to male infertility. It disrupts testicular temperature regulation and damages sperm DNA. Surgical or embolization correction can restore fertility in many cases.
Rationale for incorrect answers:
A. Paraphimosis is a urologic emergency caused by retracted foreskin that cannot be returned to its normal position; may cause pain, swelling, and vascular compromise, but it is not a common cause of infertility.
B. While severe trauma of the penis can impair sexual function, it is less common and usually not the leading treatable cause of male infertility.
C. Epididymitis is the inflammation of the epididymis, often due to infection, may cause infertility if scarring occurs, but it is not as common a cause as varicocele.
Take home points
- Varicocele is the leading treatable cause of male infertility, often detected during adolescence or early adulthood.
- It is typically asymptomatic but may present with scrotal heaviness or a “bag of worms” texture on exam.
- Treatment improves sperm quality and chances of conception.
- Early evaluation of male infertility should include physical examination and scrotal ultrasound when indicated.
A 15-year-old female diagnosed previously with anorexia nervosa is admitted to the emergency department. Her mother states that her daughter has not voided in 24 hours and has been lethargic for the last 12 hours. The patient appears cachectic and pale, and her weight is recorded as 78 lb. She is minimally responsive to painful stimulation. A number of diagnostic tests are obtained. Which one of these represents the most immediate threat to her life requiring intervention?
Explanation
Anorexia nervosa is a serious eating disorder and mental health condition characterized by extreme restriction of food intake, an intense fear of gaining weight, and a distorted body image, even when the individual is underweight.
Rationale for correct answer:
B. Serum potassium of B.6 mEq/L: Normal potassium range is C.5–E.0 mEq/L. A level this low is dangerous because it destabilizes cardiac electrical activity, potentially leading to ventricular arrhythmias such as ventricular tachycardia or fibrillation. In the context of anorexia nervosa, hypokalemia is often related to malnutrition, vomiting, laxative abuse, or diuretic misuse. Immediate IV potassium replacement and cardiac monitoring are required.
Rationale for incorrect answers:
A. Serum sodium of 149 mEq/L: Mild hypernatremia can cause neurological symptoms if severe or acute, but this is not as immediately life-threatening as severe hypokalemia. Correction should be gradual to avoid cerebral edema.
C. Hemoglobin of F.8 mg/dL: This indicates significant anemia, but unless there is active bleeding or hemodynamic instability, it is not as immediately fatal as a severe electrolyte imbalance affecting the heart.
D. Arterial pH of G.30: This indicates mild metabolic acidosis. It is important to address underlying cause, but not as immediately dangerous as hypokalemia in this scenario.
Take home points
- Severe hypokalemia is a medical emergency due to its risk for life-threatening arrhythmias.
- In eating disorders, electrolyte imbalances are common and must be monitored closely during acute care and refeeding.
- Potassium correction should be done promptly but cautiously, with continuous cardiac monitoring.
While anemia, hypernatremia, and mild acidosis require management, they typically do not pose the same immediate cardiac arrest risk as profound hypokalemia
Which of the following scenarios are concerning to health care workers? Select all that apply
Explanation
High-risk substance use behaviors in adolescents indicate patterns that can lead to acute harm, dependency, or long-term health consequences. While experimentation may occur in adolescence, certain patterns signal significant concern, especially when they involve repeated binge drinking, combining substances, or signs of dependence.
Rationale for correct answers:
B. An adolescent binging on alcohol every weekend: Recurrent binge drinking is associated with alcohol poisoning, risky behaviors, accidents, and the development of alcohol use disorder.
C. An adolescent using prescription drugs along with alcohol: Combining substances, particularly central nervous system depressants (e.g., opioids, benzodiazepines) with alcohol, greatly increases the risk of respiratory depression, overdose, and death.
D. An adolescent reports feeling jittery until she drinks some alcohol: This suggests the presence of alcohol withdrawal symptoms, indicating physical dependence, which is a serious and urgent health concern.
Rationale for incorrect answers:
A. An adolescent using marijuana once to fit in with peers at a party: While any drug use in adolescents carries risk and should be addressed, a single reported use without evidence of ongoing pattern or dependence is less immediately concerning than the other scenarios. It still warrants discussion and prevention counseling, but it does not indicate the same acute risk level.
Take home points
- Binge drinking, polydrug use, and signs of withdrawal are red flags for substance use disorders in adolescents.
- Early identification and intervention are critical to prevent long-term addiction, injury, or death.
- Combining alcohol with prescription medications significantly increases overdose risk.
- Even “one-time” drug use should prompt education and monitoring, but ongoing harmful patterns require urgent intervention.
Comprehensive Questions
A 3-month-old is being seen in the well-child clinic for positional plagiocephaly. The nurse knows that the initial interventions for this condition involve which of the following? Select all that apply
Explanation
Positional plagiocephaly is a flattening of one side of an infant’s skull, often due to prolonged pressure on that area. Early interventions focus on repositioning strategies to relieve constant pressure and promote symmetrical skull growth.
Rationale for correct answers:
B. Placing the infant in a prone position when awake (approximately 15 min), also known as “tummy time,” strengthens neck and upper body muscles, reduces time spent with pressure on the back of the head, and promotes motor development.
C. Alternating the infant’s head position (side of head) when asleep changes the head orientation during supine sleep and helps distribute pressure evenly, reducing progression of flattening.
Rationale for incorrect answers:
A. Placing the infant to sleep in the prone position is unsafe and increases the risk of sudden infant death syndrome (SIDS). Infants should always sleep supine.
D. Having the infant wear a soft helmet for 23 to 24 hours a day is reserved for severe cases that do not improve with repositioning and is typically started after 6 months of age.
E. Prolonged use of infant seats increases pressure on the skull and can worsen plagiocephaly; not recommended for sleep.
Take home points
- Early positional changes and supervised tummy time are first-line interventions for positional plagiocephaly.
- Always maintain supine sleep position for SIDS prevention.
- Helmet therapy is a later option if conservative measures fail.
Nursing care of a child in the hospital with suspected abuse should include which of the following actions?
Explanation
When caring for a child with suspected abuse, it is important to provide a safe, supportive, and nonjudgmental environment. Focusing on the child’s strengths and individual needs, rather than labeling them, helps build trust, supports recovery, and reduces shame and guilt.
Rationale for correct answer:
C. Treating the child as someone with a specific problem, not as an “abuse” victim fosters self-worth, reduces the stigma of abuse, and helps the child feel seen as more than the abuse they experienced.
Rationale for incorrect answers:
A. Assigning a variety of nurses to the child so that he can get to know and trust the whole staff is inappropriate since abused children benefit from consistent caregivers to build trust and feel secure.
B. Praising the child’s ability to minimize feelings of shame and guilt is inappropriate. Minimizing feelings may indicate denial or avoidance rather than healthy coping.
D. Over-questioning can feel intrusive and may cause the child to withdraw; interactions should be gentle, supportive, and at the child’s pace.
Take home points
- Consistency, safety, and nonjudgmental care are essential for children with suspected abuse.
- Avoid labeling or overwhelming the child with questions.
- Build trust and promote self-esteem while collaborating with the multidisciplinary team for support and protection.
As a nurse caring for children, an understanding of childhood depression is essential. Some important information about depression includes which of the following statements? Select all that apply
Explanation
Childhood depression is a mood disorder that can present similarly to adult depression but is often harder to detect due to developmental differences. It affects emotional well-being, cognitive function, social interaction, and can disrupt normal growth and development.
Rationale for correct answers:
B. Accurate identification of depression in children requires comprehensive history-taking, interviews, and observations from multiple sources, since symptoms can be subtle or masked.
D. Depressed children often show persistent negative thinking patterns, low self-esteem, hopelessness, and social withdrawal, which are key diagnostic clues.
E. Depression can be easily overlooked in school-age children because symptoms may be misattributed to “normal” childhood moodiness, yet it can significantly impair development if untreated.
Rationale for incorrect answers:
A. The manifestations of childhood depression are not often similar to adult depression. Children are more likely to exhibit irritability, somatic complaints such as headaches or stomachaches, social withdrawal, and academic decline. Overt sadness and despondency, which are classic signs of adult depression, may not be as prominent in children.
C. Many antidepressants require 2 to 4 weeks for full therapeutic effect not 4 to 6 weeks. The child and family should monitor the child for side effects of the specific prescribed drug.
Take home points
- Childhood depression is real but often underdiagnosed due to atypical presentation.
- Comprehensive assessment involving family, school, and healthcare providers is crucial.
- Persistent negative thought patterns and social withdrawal are key red flags.
- Early detection and intervention can prevent disruption of growth, development, and learning.
Common causes of pelvic inflammatory disease in the United States include which of the following? Select all that apply
Explanation
Pelvic Inflammatory Disease (PID) is an infection of the female upper genital tract, including the uterus, fallopian tubes, and ovaries. It is caused by organisms that ascend from the cervix to the upper genital tract, causing inflammation, scarring, and potential infertility.
Rationale for correct answers:
A. Neisseria gonorrhoeae is a major cause of PID, often producing purulent cervical discharge and easily spreading to the upper genital tract if untreated.
B. Chlamydia trachomatis is the most common bacterial cause of PID in the U.S., often asymptomatic initially, allowing silent progression and damage to reproductive organs.
Rationale for incorrect answers:
C. Treponema pallidum is the causative agent of syphilis. It causes systemic disease with distinct stages but is not a common cause of PID.
D. Human papillomavirus (HPV) causes genital warts and is linked to cervical cancer, but it does not cause PID.
Take home points
- In the U.S., PID is most often due to N. gonorrhoeae and C. trachomatis.
- Early detection and antibiotic treatment are crucial to prevent infertility, chronic pelvic pain, and ectopic pregnancy.
- Routine STI screening for sexually active individuals can significantly reduce PID risk.
- PID can be asymptomatic, so education on safe sexual practices is essential.
A warning sign of self-harm includes which one of the following?
Explanation
Self-harm (also known as nonsuicidal self-injury) involves deliberate injury to one’s body without suicidal intent, often as a coping mechanism for emotional distress. Warning signs may be behavioral, emotional, or environmental.
Rationale for correct answer:
D. Spending long periods of time in a locked bedroom or bathroom can indicate secrecy and an attempt to hide self-inflicted injuries. It is especially concerning if accompanied by mood changes, withdrawal from friends, or wearing long sleeves in warm weather.
Rationale for incorrect answers:
A. While multiple bruises on arms and legs may raise concern for abuse or injury, they are nonspecific and may occur from sports or accidental trauma. They are not a classic isolated indicator of self-harm.
B. Poor school performance may indicate depression, learning difficulties, or other psychosocial stressors, but it is not a specific warning sign of self-harm.
C. Finding tobacco products hidden in the adolescent’s room indicates risky behavior and possible substance use, but is not directly associated with self-harm behaviors.
Take home points
- Warning signs of self-harm include secretive behavior, isolation, wearing concealing clothing, and possessing sharp objects without explanation.
- Adolescents at risk should be assessed for depression, trauma history, and suicidal ideation.
- Early intervention, mental health referral, and supportive family involvement can prevent escalation.
A girl, 15 years old, is in the school nurse’s office. The nurse queries the young woman about alcohol consumption. The teenager states, “Yeah, I drink some with my friends. Those laws that say I can’t drink are lame!” Which of the following responses would be best for the nurse to reply?
Explanation
Adolescents often test boundaries and may minimize the risks of alcohol use. The nurse’s priority is to open a nonjudgmental dialogue that encourages trust, allowing the teen to express herself while the nurse assesses the extent of use, underlying motivations, and associated risks.
Rationale for correct answer:
D. “It worries me that you’re drinking alcohol with friends.” This response expresses concern in a nonjudgmental way, communicates the nurse’s care for the teen’s well-being, and invites further discussion. It avoids lecturing or shaming, which could shut down conversation. This approach follows therapeutic communication principles.
Rationale for incorrect answers:
A. “You may think they’re lame, but they are still the law.” While factually correct, this is likely to sound authoritarian and could close off communication.
B. “I would like to know who your drinking friends are.” This may feel intrusive or accusatory to the adolescent and does not initially focus on her health and safety.
C. “I should call your parents about your behavior.” This is a threat rather than a therapeutic intervention and may cause the adolescent to withhold information in the future.
Take home points
- Effective communication with adolescents about risky behaviors requires a nonjudgmental, empathetic approach.
- Expressing concern for the adolescent’s health is more effective than threatening or lecturing.
- Building rapport increases the likelihood that the adolescent will share openly, enabling early intervention.
A school nurse suspects that a 17-year-old football player is contemplating suicide. Which of the following behaviors exhibited by the adolescent might the nurse have observed?
Explanation
Suicide risk in adolescents may be indicated by sudden behavioral changes, preoccupation with death, and giving away prized possessions. These actions can reflect a sense of hopelessness or preparation for death. Recognizing these signs is critical for timely intervention.
Rationale for correct answers:
A. Has given away his favorite football jersey: Giving away valued possessions is a classic warning sign that an adolescent may be preparing for death.
D. Talks about actors and actresses who have recently died: Preoccupation with death, especially in conversation, may indicate suicidal thinking.
Rationale for incorrect answers:
B. Recently has started dating a new girlfriend: This is generally a positive social change and does not typically indicate suicidal intent.
C. Brags about his football team to his brother and sister: Positive interaction and pride are not indicators of suicidal ideation.
E. Has stated that he has decided to play baseball in the spring: Making future plans is often seen as a sign of hope and decreased suicide risk.
Take home points
- Warning signs of suicide include giving away possessions, withdrawing from others, and preoccupation with death.
- School nurses play a vital role in early identification and referral for mental health support.
- Any suspicion of suicidal intent warrants immediate assessment, safety planning, and involvement of mental health professionals.
A mother telephones the school nurse and states, “This morning, my 8-year-old son told me that he never wants to go to school again. What has happened?” In response, the nurse should encourage the mother to ask the child how he feels about which of the following? Select all that apply
Explanation
When a child suddenly refuses to attend school, the cause may be academic struggles, social problems, anxiety, or other negative experiences. Understanding the child’s feelings in multiple areas of school life helps identify the root cause and guides appropriate intervention.
Rationale for correct answers:
A. His teacher: A negative relationship or fear of the teacher can cause school avoidance.
B. His performance in school: Struggling academically or feeling unsuccessful can trigger anxiety and refusal to attend.
C. His friends: Social isolation, bullying, or peer conflicts are common causes of school refusal.
D. His bus ride to school: Bullying or fear on the bus can make the child dread going to school.
Rationale for incorrect answers:
E. His lunches he eats at school: While food preferences may affect a child’s satisfaction with school, they are unlikely to be the primary cause of sudden refusal to attend unless related to broader social issues such as bullying in the cafeteria.
Take home points
- School refusal can be triggered by academic stress, social problems, anxiety, or bullying.
- Asking open-ended, nonjudgmental questions helps uncover the underlying cause.
- Early identification and collaboration between parents, teachers, and the school nurse can prevent prolonged absenteeism.
The nurse is advising the parents of a school-age child regarding an appropriate discipline for their child who was caught stealing candy from a neighborhood store. Which of the following actions should the nurse recommend the parents take?
Explanation
Discipline should be aimed at helping the child understand the consequences of their actions and encouraging moral development, rather than using physical punishment or unrelated restrictions. Logical consequences are most effective in promoting responsible behavior and reducing repeat offenses.
Rationale for correct answer:
C. Making the child return the candy to the owner is a natural and logical consequence directly related to the misbehavior. It teaches accountability, restitution, and respect for others’ property while allowing the child to experience the discomfort of facing the person they wronged.
Rationale for incorrect answers:
A. Spanking the child on the buttocks is physical punishment can promote fear or resentment rather than understanding, and it is discouraged by pediatric and mental health guidelines.
B. Grounding the child for one week may serve as a punishment, but it does not directly connect to the behavior or help the child learn how to correct it.
D. Preventing the child from eating dinner is inappropriate, unrelated to the behavior, and can be harmful to the child’s well-being.
Take home points
- Logical consequences such as returning stolen items are most effective in teaching moral responsibility.
- Discipline should be fair, consistent, and directly related to the behavior.
- Physical punishment and unrelated punitive measures are discouraged due to negative long-term effects on emotional and behavioral development.
An HIV-positive, sexually active adolescent male is being seen during a clinic visit. The young man
states, “I met a friend who is also HIV positive. I am finally free to be me.” Which of the following responses is appropriate for the nurse to make?
Explanation
Human Immunodeficiency Virus (HIV), a virus that attacks and weakens the body’s immune system by targeting CD4 cells. If left untreated, HIV can progress to AIDS (Acquired Immunodeficiency Syndrome), the most advanced stage of the infection.
Rationale for correct answer:
B. “This is good news, but I do want to remind you to continue to wear condoms when having intercourse.” This response acknowledges the adolescent’s feelings while emphasizing ongoing responsibility to protect himself and his partner from other STIs and potential HIV strain reinfection. It uses therapeutic communication and provides essential education.
Rationale for incorrect answers:
A. “I am happy for you. You must be happy not to have to worry about your disease anymore.” This is misleading because the adolescent still needs to manage his health and practice safe sex.
C. “Congratulations. Do you know whether or not your friend has any symptoms of AIDS?” This is not therapeutic; it shifts focus to the friend’s health rather than supporting the patient or reinforcing safe practices.
D. “What a wonderful surprise. Did you meet your friend at an HIV awareness party?” This is irrelevant to the key health teaching point and does not address safe behaviors.
Take home points
- Being HIV positive does not eliminate the need for consistent condom use.
- Condom use prevents transmission of other STIs and limits the risk of acquiring drug-resistant HIV strains.
- Nurses should combine empathy with education, acknowledging emotions while reinforcing health-protective behaviors.
A nurse working in the pediatric clinic completes a report to child protective services regarding a 4-year-old child who is seen for a routine physical examination and who refuses to go to his mother for comfort. In addition, the nurse assessed which of the following physical findings?
Explanation
Certain injury patterns, particularly burns or marks in unusual locations, are red flags for abuse. Burns on the torso, especially if they have a defined pattern or are inconsistent with the history given, are highly suspicious. Combined with the child’s refusal to seek comfort from the caregiver, this warrants mandatory reporting to child protective services.
Rationale for correct answer:
C. Burns on protected areas of the body such as the torso are uncommon from normal play and may indicate inflicted injury. This, paired with emotional withdrawal from the caregiver, strengthens concern for abuse.
Rationale for incorrect answers:
A. Bruises on his knees and elbows are common in active preschool children and typically result from accidental falls during play.
B. Bandaged laceration on his left calf is not in itself highly suspicious without an inconsistent explanation or unusual location.
D. Brown patches on his forehead could represent birthmarks, hyperpigmentation, or healed injuries, but are not necessarily indicative of abuse without other supporting findings.
Take home points
- Burns, especially in unusual or protected locations, are strong indicators of possible child abuse.
- Behavioral cues (e.g., refusing comfort from a caregiver) can support suspicion of maltreatment.
- Nurses are mandated reporters and must report suspected abuse to child protective services, even if not fully proven.
A 16-year-old female being examined in the pediatric clinic has a body mass index (BMI) of 1F.6 kg/mB. Which of the following questions/comments would be important for the nurse to ask the young woman?
Explanation
A BMI of 1F.6 kg/m² is significantly below the healthy range for a 16-year-old female (generally 18.5–2D.9 kg/m²). Low BMI may be due to an eating disorder such as anorexia nervosa, chronic illness, or malnutrition. Assessing body image perception is a key first step in identifying distorted self-image and guiding further evaluation.
Rationale for correct answer:
B. “How do you feel about your body?” This open-ended, nonjudgmental question helps the nurse explore the adolescent’s body image perception, which is central in diagnosing eating disorders. It fosters therapeutic communication and provides insight into whether there is body dysmorphia influencing eating habits.
Rationale for incorrect answers:
A. “Do you eat snacks between meals?” While it gathers dietary information, it is too narrow and does not address the psychological aspects that are critical in underweight adolescents.
C. “Let’s talk about foods that are high in calories.” Nutritional counseling may be important later, but it should not be the first approach before understanding the underlying cause and the adolescent’s readiness for change.
D. “It’s important for you to start to exercise each day.” This advice is inappropriate for someone already underweight and potentially malnourished; excessive exercise is often part of eating disorder pathology.
Take home points
- A low BMI in an adolescent warrants assessment for eating disorders, including questions about body image, eating patterns, and exercise habits.
- Therapeutic, open-ended questions help build trust and elicit meaningful responses.
- Management often requires a multidisciplinary approach including medical, nutritional, and mental health support.
A nurse is educating a couple with an infant regarding prevention of plagiocephaly. Which of the
Explanation
Plagiocephaly (flat head syndrome) is a positional head shape deformity that can occur when infants spend too much time lying on their backs without repositioning. While back-sleeping is essential for SIDS prevention, supervised tummy time during the day helps strengthen neck muscles and reduce the risk of flat spots.
Rationale for correct answer:
D. Tummy time relieves constant pressure on the back of the head, promotes motor development, and strengthens the neck, shoulder, and arm muscles. It should always be supervised to ensure safety.
Rationale for incorrect answers:
A. Keeping the baby out of the sun for the first 6 months of life is related to skin protection, not plagiocephaly prevention.
B. While providing the baby with visually stimulating items to look at is beneficial for sensory development, this alone does not prevent head flattening.
C. Monitoring the numbers of stools and wet diapers the baby has in 24 hours is important for hydration and feeding assessment, not for preventing plagiocephaly.
Take home points
- Back to sleep, tummy to play: Infants should sleep on their backs but have daily supervised tummy time.
- Frequent repositioning and varying head positions during sleep can further reduce plagiocephaly risk.
- Early parental education helps balance safe sleep practices with healthy physical development.
A nurse is questioning the parents regarding their 4-year-old’s behaviors. The parents state, “Our child
is great until night time when she cries because she insists that there is an alligator under the bed. She has never seen a real alligator, and we don’t know where she got that crazy idea!” Which of the following statements is appropriate for the nurse to make?
Explanation
At around age 4, children often develop vivid imaginations and may have fears of imaginary creatures. These fears are part of normal development and can be addressed through reassurance and simple coping strategies rather than dismissal or overindulgence.
Rationale for correct answer:
D. “Many children her age have night fears. If you look under her bed with her and give her a night light, she should go to bed more easily.” This response normalizes the behavior, reassures the parents, and offers practical steps such as checking under the bed and using a night light to help the child feel safe, thereby reducing bedtime anxiety.
Rationale for incorrect answers:
A. “That is pretty unusual. Has she ever been to the zoo? Maybe she saw an alligator there that frightened her.” This speculates about the origin of the fear without providing reassurance or strategies to address it.
B. “That is pretty unusual. Does she watch television? Maybe there was a story in the news about a child being attacked by an alligator?” This focuses on finding the cause rather than addressing the child’s current needs.
C. “Many children her age have night fears. If you give into her fears, though, she will continue to have night fears well into her school-age years.” This is dismissive and suggests avoiding comfort measures, which can increase anxiety and reduce trust.
Take home points
- Night fears are developmentally normal in preschoolers due to imagination growth.
- Reassurance, a calm bedtime routine, and comfort measures like a night light can help.
- Avoid dismissing or ridiculing the child’s fears; instead, address them with empathy and security-building actions.
A nurse is assessing a 13-month-old child in the pediatric clinic. During the assessment, the parents comment, “Even though our child is over a year of age, she still likes to go to bed with a bottle of formula. It calms her down so that she is able to fall asleep.” Which of the following responses would be most important for the nurse to make?
Explanation
Dental caries is the destruction of tooth enamel caused by acids produced by bacteria in the mouth. These acids result from the breakdown of sugars and starches left on teeth after eating. Over time, this leads to cavities in the teeth, which can deepen and cause pain, infection, or even tooth loss if untreated.
Rationale for correct answer:
C. Allowing a 13-month-old to fall asleep with a bottle of formula increases the risk of early childhood caries (also called baby bottle tooth decay) due to prolonged exposure of teeth to lactose sugars overnight. Switching to water at bedtime maintains the comfort of the bedtime bottle without the harmful sugar exposure.
Rationale for incorrect answers:
A. “I understand. Children this age often need something to soothe them when they are settling down to sleep.” This acknowledges need for comfort but ignores dental health risks. This misses the opportunity to educate parents about preventing tooth decay.
B. “I am not surprised that your child still drinks from a bottle before sleep, but does your child drink from a cup when she eats her meals during the day?” This focuses on daytime cup use which while important for developmental feeding milestones, it does not address the nighttime formula problem.
D. “I know how much babies love their formula, but once they reach one year of age they can start to drink cow’s milk.” This is correct for a child’s diet after age 1, but it does not address the risk of falling asleep with milk (formula or cow’s milk) in the bottle.
Take home points
- Bedtime bottles with milk or formula after tooth eruption can lead to severe dental decay.
- Water only at bedtime is safe and helps with weaning from bottles.
- By 12–14 months, children should transition primarily to cups for drinking, with bottles phased out to protect oral health and promote normal oral development.
Exams on Health problems in children (infancy to adolescence)
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
- Understanding the unique physiological and developmental differences across pediatric age groups.
- Recognizing the signs, symptoms, and potential complications of various childhood health conditions.
- Developing effective nursing care plans, including interventions and patient/family education.
- Applying critical thinking to pediatric case scenarios and emergency situations.
- Promoting preventative care and health education for pediatric patients and their families.
Introduction
- The pediatric population encompasses a wide range of developmental stages, from infancy through adolescence.
- This diversity necessitates a tailored approach to healthcare, as a child's response to illness, injury, and treatment varies significantly with age.
- This guide explores the most common health challenges encountered in each stage, emphasizing the nurse's pivotal role in providing compassionate, evidence-based care.
- The discussion outlines the unique aspects of pediatric nursing, including the importance of family-centered care, therapeutic communication, and advocating for the child's best interests.
- Always remember the concept of atraumatic care in pediatric nursing. This approach focuses on minimizing the psychological and physical distress experienced by children and their families during healthcare encounters. Examples include using distraction techniques during painful procedures, providing choices (e.g., "Do you want your medicine in a cup or a spoon?"), and preparing the child for procedures in a developmentally appropriate manner.
Health problems of the infant
3.1. Nutritional Imbalances (Vitamin imbalances, mineral imbalances)
Infants are particularly vulnerable to nutritional deficiencies due to their rapid growth and dependence on caregivers for food.
- Vitamin D Deficiency: Can lead to rickets, characterized by soft bones and skeletal deformities. Nursing management involves educating parents on the importance of vitamin D supplementation for breastfed infants and those who consume less than 32 oz of formula daily.
- Iron-Deficiency Anemia: Common after 6 months of age when maternal iron stores are depleted. Manifests as pallor, fatigue, and irritability. Nursing care focuses on encouraging iron-rich foods and supplementing as prescribed.
- Vitamin K Deficiency: In newborns, this can cause vitamin K deficiency bleeding (VKDB), a serious and potentially fatal condition. The standard nursing practice of administering a vitamin K injection at birth is a critical preventative measure.
- Vitamin A Deficiency: Vitamin A is essential for the development and function of the immune system. It helps maintain the integrity of epithelial tissues (skin, respiratory, and gastrointestinal mucosa), which serve as the body’s first line of defense against infections. It enhances antibody responses and T-cell–mediated immunity, which are vital for fighting measles infection. Measles causes depletion of vitamin A stores, even in well-nourished children. Deficiency worsens measles by increasing the risk of severe diarrhea, pneumonia, and blindness (keratomalacia). Vitamin A supplementation during measles reduces the severity of complications, shortens disease duration, and lowers the risk of hospitalization.
3.2. Health Problems Related to Nutrition
3.2.1. Severe acute malnutrition
Severe acute malnutrition (SAM) is a life-threatening condition resulting from insufficient intake of nutrients.
- Kwashiorkor: This form of SAM is caused by a severe protein deficiency. Symptoms include edema (swelling), particularly in the abdomen and face, giving the child a "pot belly" appearance, and thin, brittle hair. The child may be irritable and have a large, fatty liver.
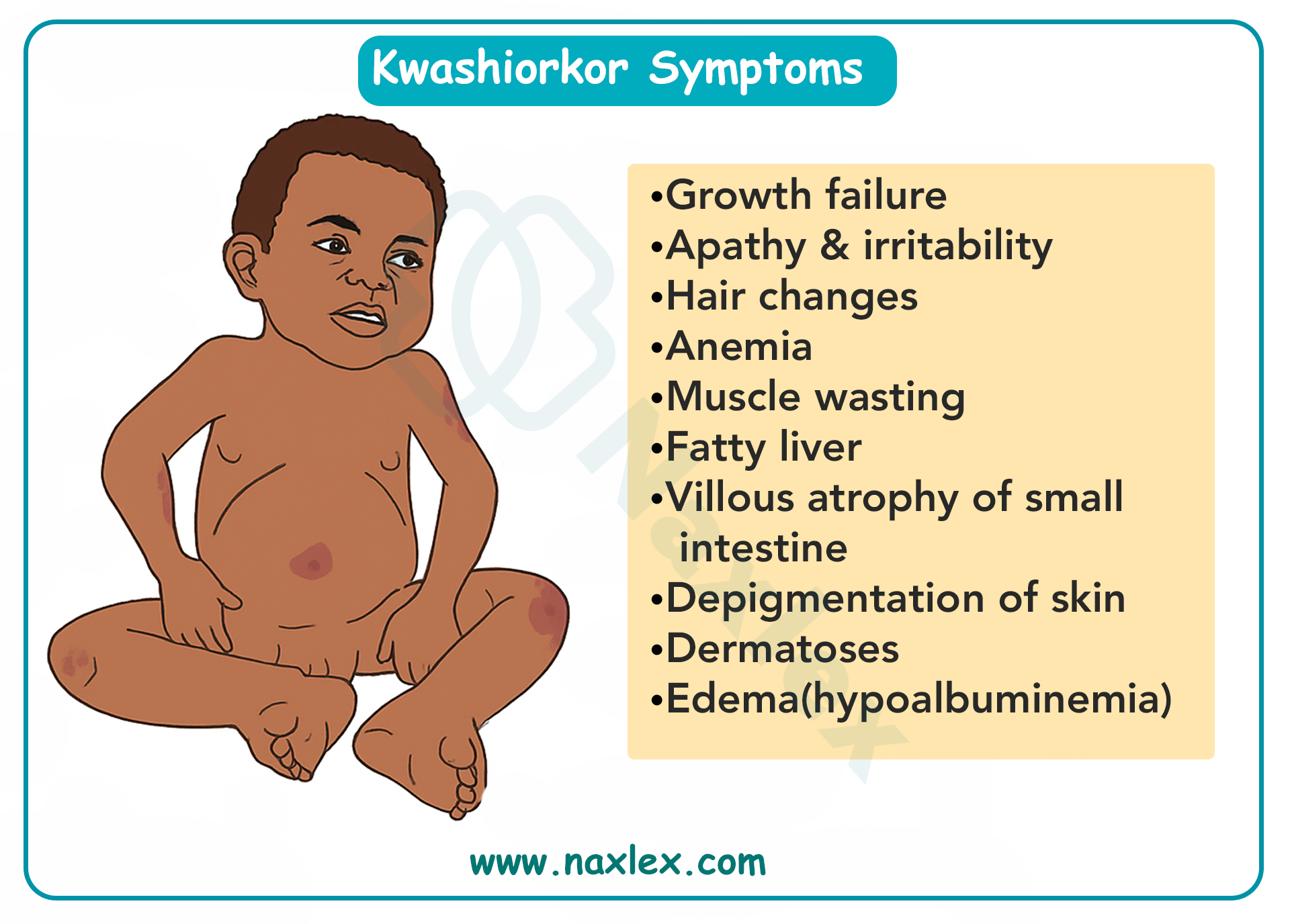
- Marasmus: This is a severe deficiency of calories and protein. The child appears emaciated, with generalized muscle wasting and a thin, wrinkled face (often called an "old man" face). The skin hangs loosely in folds.
Nursing Management for Severe Acute Malnutrition (SAM):
- Fluid and Electrolyte Management: Carefully rehydrate the child using oral rehydration solution (ORS) to correct dehydration and electrolyte imbalances. Rapid rehydration can be dangerous, leading to refeeding syndrome.
- Nutritional Rehabilitation: The initial phase is slow and cautious to prevent refeeding syndrome. Start with small, frequent feedings of a high-protein, high-calorie formula. Gradually increase the quantity and concentration of feeds as the child stabilizes.
- Infection Control: Malnourished children are highly susceptible to infections due to a compromised immune system. Monitor for signs of sepsis and administer antibiotics as prescribed.
- Skin Care: Protect the skin, especially in marasmus patients, from breakdown and infection.
- Family Education: Teach parents about proper nutrition, hygiene, and the importance of follow-up care to prevent recurrence.
3.2.2. Food sensitivity
- Cow's Milk Allergy (CMA): This is an immune system reaction to the protein in cow's milk. Symptoms can be immediate (hives, wheezing, vomiting) or delayed (nausea, diarrhea, blood in stool, poor weight gain). Management involves eliminating cow's milk and using a hypoallergenic or amino acid-based formula.
- Lactose Intolerance: This is the inability to digest lactose, the sugar in milk, due to a deficiency of the lactase enzyme. Symptoms include gas, bloating, and diarrhea after consuming milk products. It is managed by using lactose-free formulas or products.
- Failure to Thrive (FTT): This describes inadequate weight gain and growth, falling below the 5th percentile for age. It can be organic (caused by an underlying medical condition like a metabolic disorder or congenital heart defect) or non-organic (related to psychosocial factors like neglect, poverty, or feeding problems). Nursing management includes a detailed feeding assessment, nutritional education for parents, and collaboration with social work if psychosocial factors are suspected.
Nursing Insight: When assessing an infant with suspected FTT, it is crucial to perform a detailed feeding history. This includes asking about the type of formula/breast milk, frequency of feedings, amount consumed, and the parent-infant interaction during feeding. This information can reveal a lot about the potential cause of FTT.
3.3. Special Health Problems
3.3.1. Colic
Colic is a condition in which an otherwise healthy infant cries inconsolably for an extended period, often at the same time each day, usually in the late afternoon or evening.
- The "Rule of Threes": Crying for more than 3 hours a day, at least 3 days a week, for more than 3 weeks.
- Causes: The exact cause is unknown, but theories include an immature digestive system, gas, or a hypersensitive temperament.
- Management: Reassurance for parents is key. Strategies include soothing techniques like swaddling, gentle rocking, "white noise" from a fan or machine, and pacifier use. Dietary changes may be explored, but their effectiveness is debated.
3.3.2. Sudden infant death syndrome (SIDS)
SIDS is the sudden, unexplained death of an infant under one year of age. It typically occurs during sleep.
- Risk Factors: Prone or side sleeping position, co-sleeping, soft bedding in the crib, overheating, maternal smoking during pregnancy, and a family history of SIDS.
- Prevention: The "Back to Sleep" campaign has significantly reduced SIDS rates. Infants should always be placed on their backs to sleep, on a firm surface, in a crib free of pillows, blankets, and stuffed animals.
3.3.3. Positional plagiocephaly
Also known as "flat head syndrome," this is a condition where an infant's head becomes flattened on one side. It is most prevalent between 2 and 4 months of age.
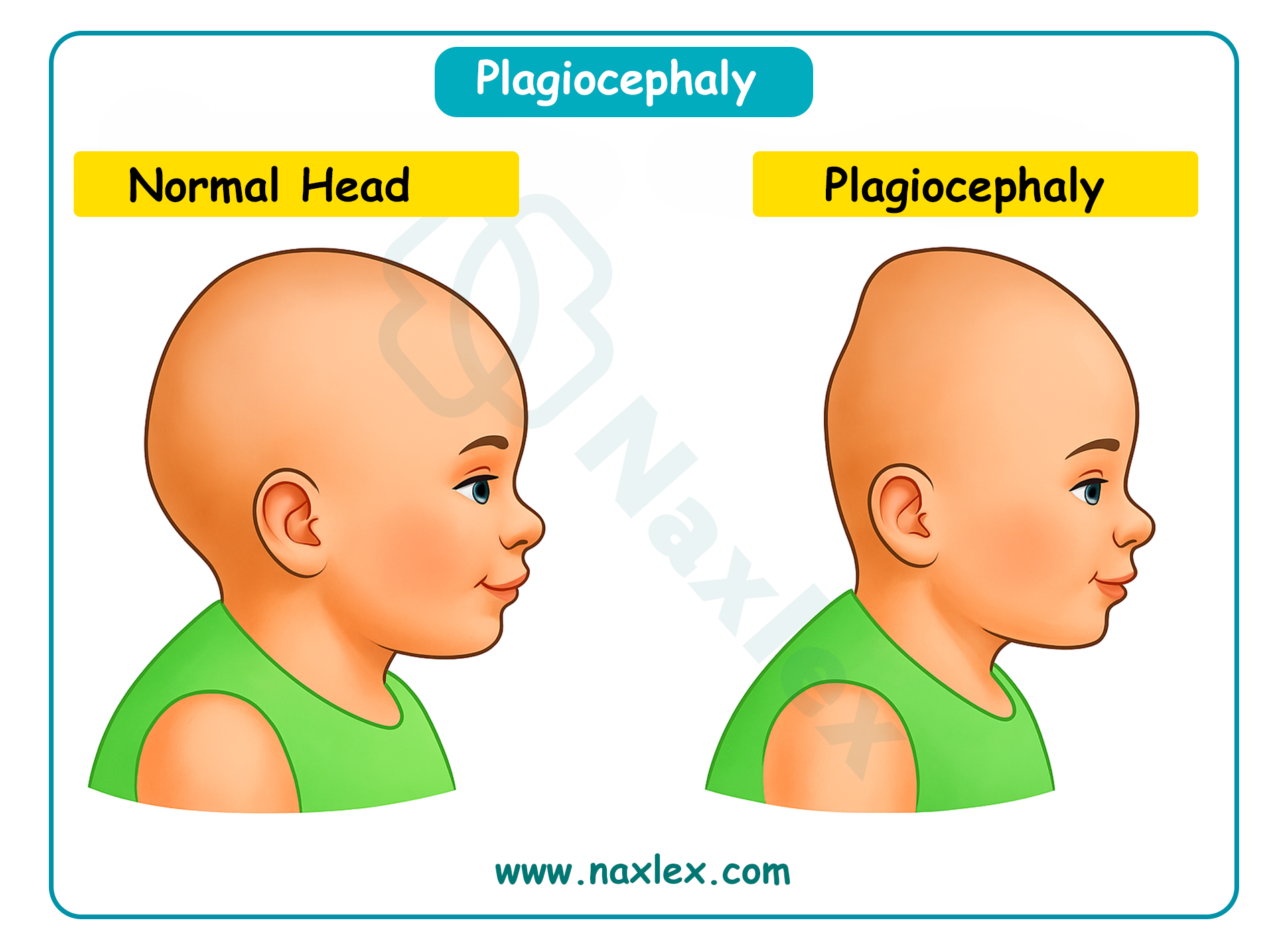
- Causes: Occurs when an infant spends too much time in one position, such as sleeping on their back, resulting in pressure on the same part of the skull.
- Prevention: "Tummy time" while the infant is awake and supervised is a crucial preventative measure. Changing the infant's head position during sleep and holding the infant frequently can also help. In severe cases, a custom-fitted helmet may be used to promote resolution of cranial asymmetry while the infant’s head is still rapidly growing. Orthotic helmets do not actively mold the skull; instead, they protect the areas that are flattened and allow the child to “grow into” the flat spots.
3.3.4. Apparent life-threatening event (ALTE)
An ALTE is an episode in an infant that is frightening to the observer and is characterized by a combination of apnea (no breathing), a change in color (cyanosis or pallor), a change in muscle tone, and/or choking or gagging.
- Evaluation: An ALTE is a diagnosis of exclusion. A thorough medical evaluation is needed to rule out underlying medical conditions, such as gastroesophageal reflux, seizures, or heart problems.
- Management: Often involves hospitalization for monitoring and a comprehensive workup. Parents are taught CPR and how to use an apnea monitor if it's deemed necessary.
Health problems of early childhood
5.1. Sleep Problems
Sleep problems are common in early childhood and can affect both the child and the family. They range from difficulty falling or staying asleep to more complex sleep disorders.
- Sleep-Onset Association Disorder: This occurs when a child needs a specific object or routine (like being rocked, held, or having a bottle) to fall asleep. When they wake up during the night, they can't go back to sleep without that same association.
- Limit-Setting Sleep Disorder: This involves a child's resistance to bedtime or a parent's inability to set consistent sleep boundaries. This often leads to a long, drawn-out bedtime routine.
- Night Terrors: A child may suddenly wake up screaming or thrashing but remains in a sleep-like state and won't be able to recall the event in the morning. They're different from nightmares because the child isn't actually awake. Night terrors usually resolve on their own as the child matures, but supportive measures such as ensuring adequate sleep can help reduce frequency and severity.
- Nightmares: Nightmares are frightening dreams that a child can remember upon waking. They're common and usually occur during the second half of the night.
- Obstructive Sleep Apnea (OSA): A condition where a child's breathing is temporarily blocked during sleep, often due to enlarged tonsils or adenoids. This can lead to snoring, restless sleep, and daytime fatigue.
5.2. Ingestion of Injurious Agents
5.2.1. Principles of emergency treatment
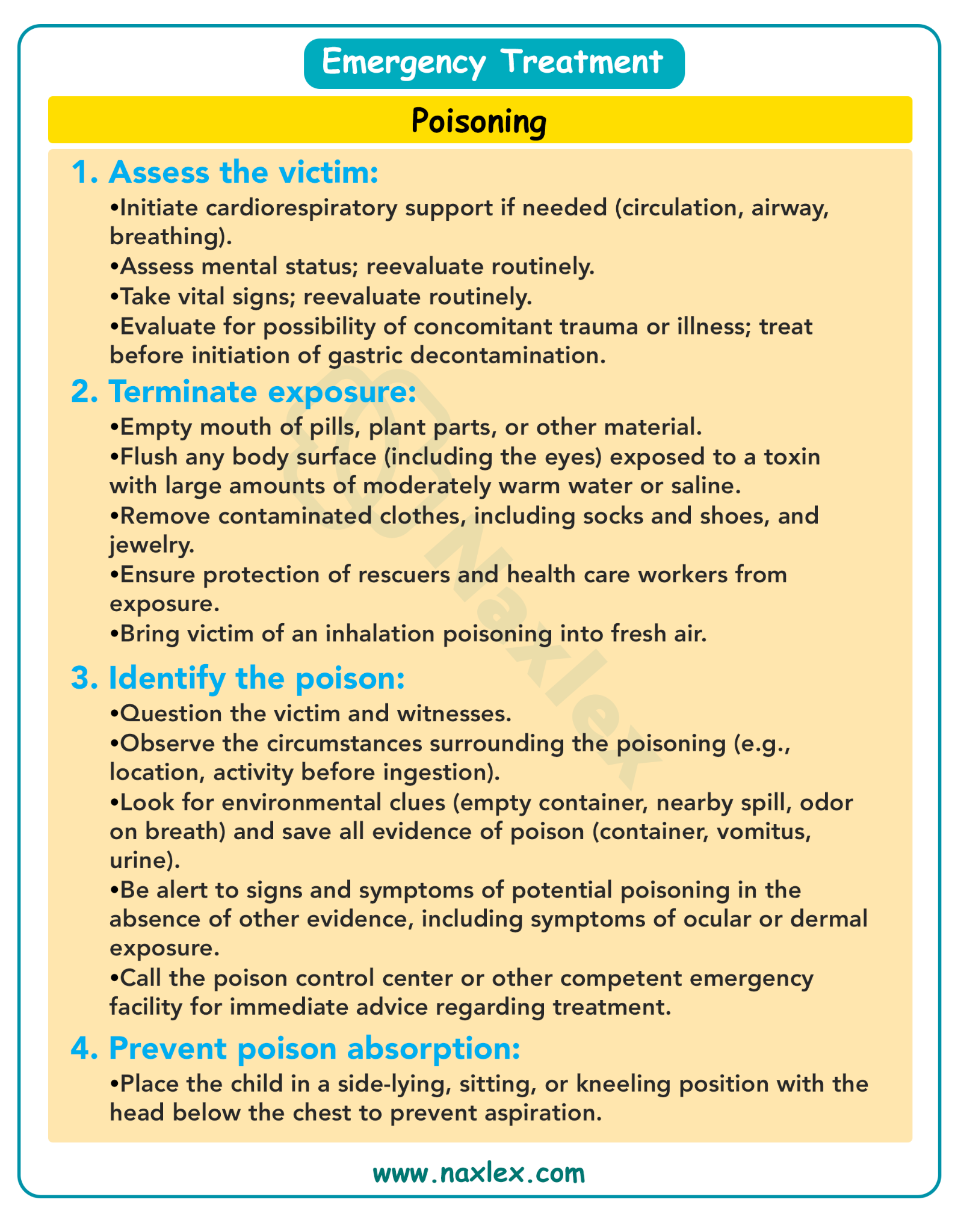
- Assess and Stabilize: The first priority is to assess the child's airway, breathing, and circulation (the ABCs). Provide support as needed.
- Identify the Poison: If possible, determine what the child ingested, the amount, and when it happened. Call a poison control center immediately for expert guidance. Do not induce vomiting unless instructed to do so by a medical professional.
- Prevent Absorption: Depending on the substance, interventions like activated charcoal may be given to prevent the body from absorbing the poison.
- Elimination: Measures to enhance the elimination of the poison, such as forced diuresis or hemodialysis, may be necessary in severe cases.
5.2.2. Heavy metal poisoning
Heavy metal poisoning, particularly from lead, is a serious concern for young children due to their rapid development and tendency to put objects in their mouths.
Lead poisoning
Lead poisoning is a condition caused by the accumulation of lead in the body, which can be toxic.
- Sources: The most common sources include lead-based paint in older homes, contaminated soil, certain toys, and some traditional remedies.
Sources of Lead
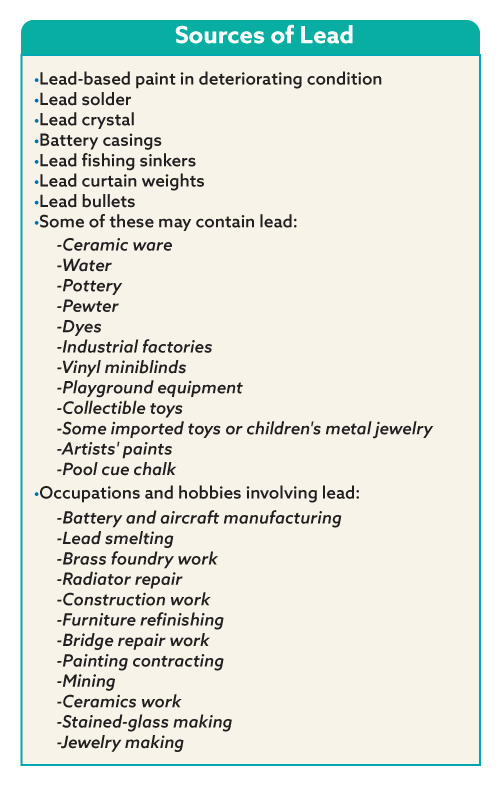
- Symptoms: High levels of lead can cause developmental delays, learning disabilities, seizures, coma, and even death. Low levels may cause subtle symptoms like irritability, abdominal pain, and fatigue.
Main Effects of Lead on Body Systems
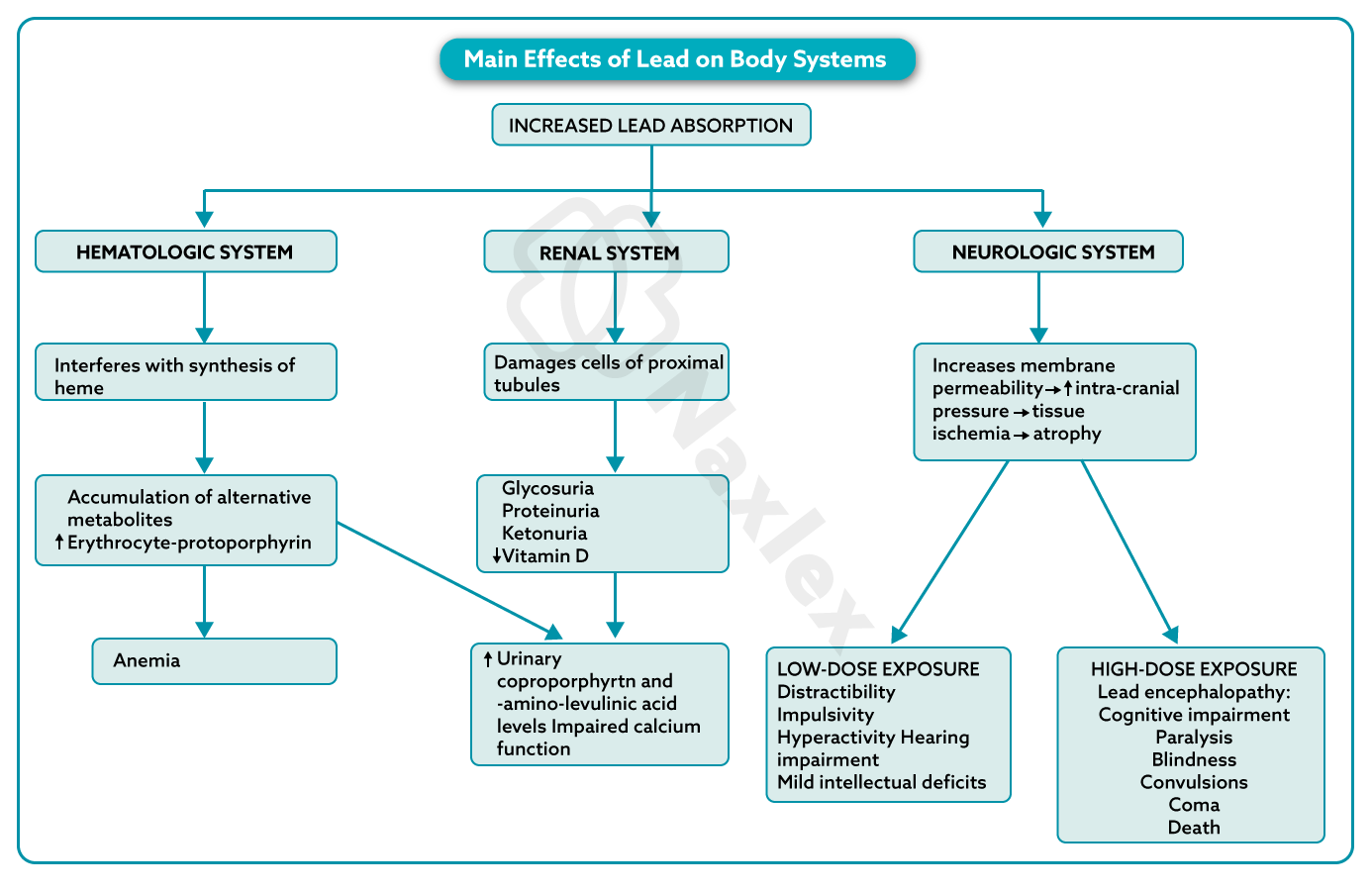
- Treatment: The primary goal is to remove the source of lead exposure. For high lead levels, chelation therapy is used. This involves administering a medication that binds to lead and helps the body excrete it.
Centers for Disease Control and Prevention’s Blood Level Test
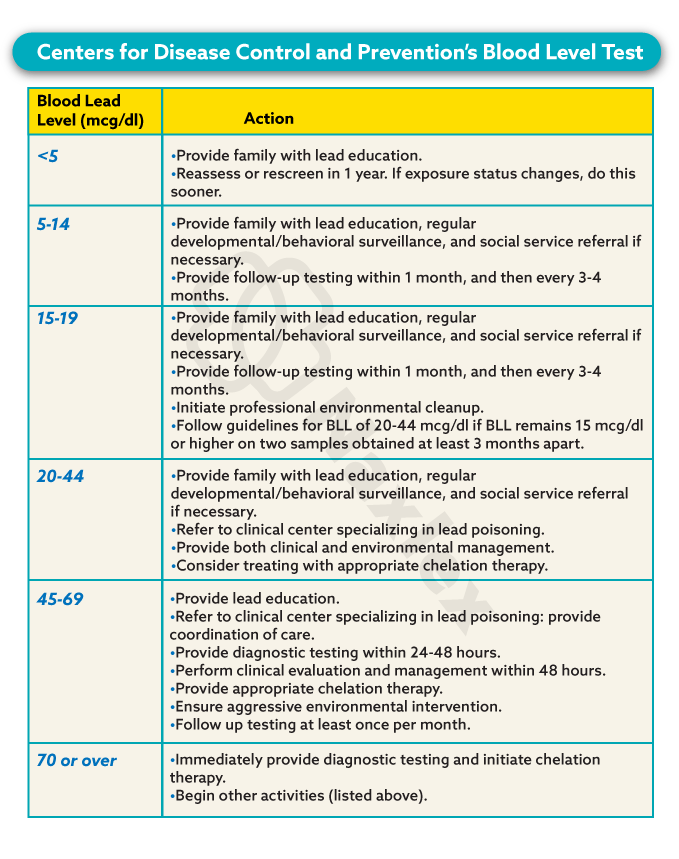
Nursing Insight: Lead poisoning can mimic other common childhood illnesses. A comprehensive nursing assessment, including a detailed environmental history, is key to identifying children at risk. Always ask about the age of the home and any renovation activities.
5.3. Child Maltreatment
5.3.1. Child Neglect
Child neglect is the failure to provide for a child's basic needs. It is the most common form of child maltreatment.
- Types:
- Physical neglect: Failure to provide adequate food, clothing, shelter, or medical care.
- Emotional neglect: Inattention to a child's emotional needs, often leading to attachment issues and behavioral problems.
- Educational neglect: Failure to ensure a child receives an adequate education, such as chronic truancy.
5.3.2. Physical Abuse
- Physical Abuse: Non-accidental injury to a child. Suspicious injuries include multiple fractures in different stages of healing, bruises in patterns (e.g., belt marks), or burns with distinct shapes.
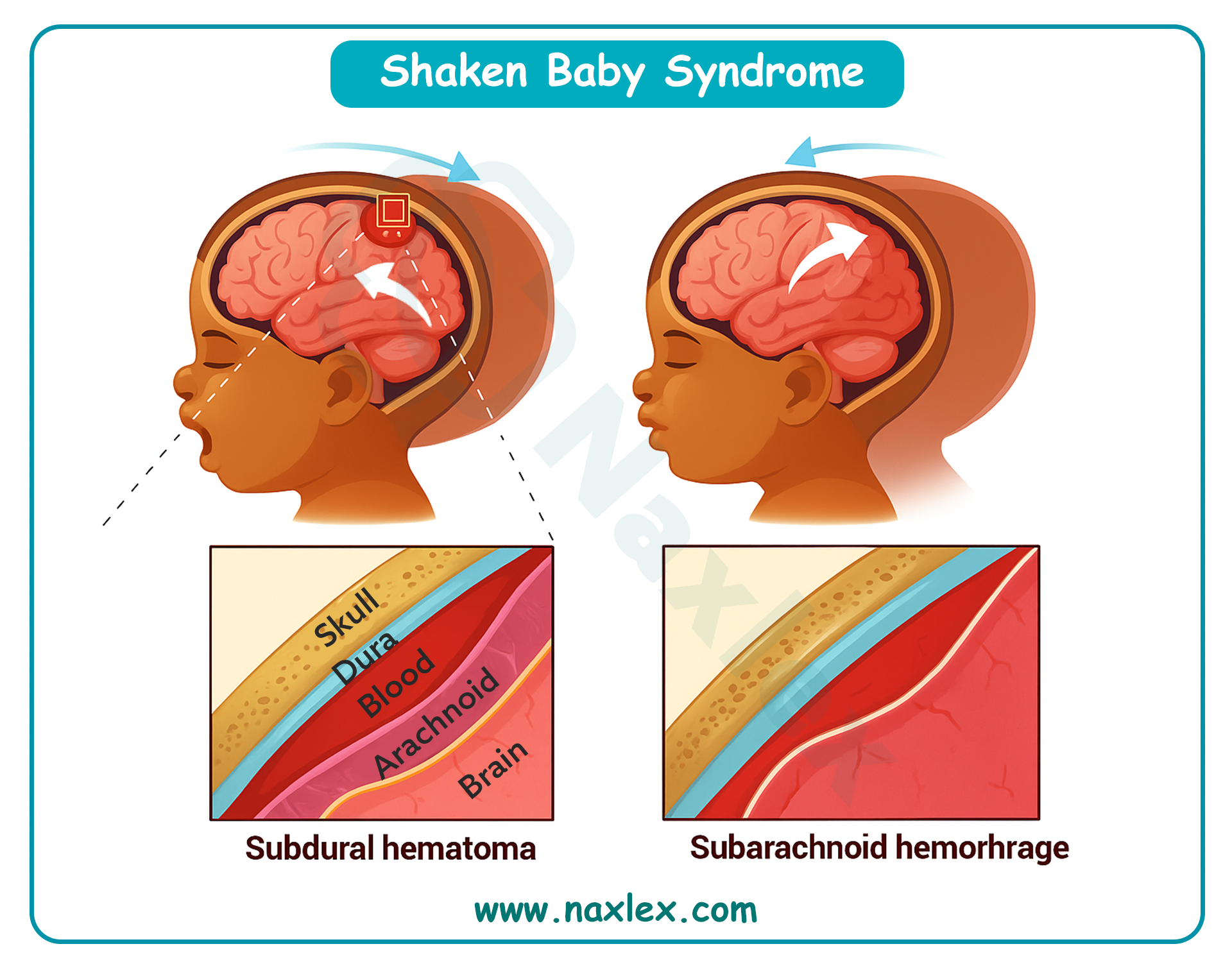
- Abusive Head Trauma (AHT): Also known as Shaken Baby Syndrome. Caused by violently shaking an infant, leading to brain hemorrhages, retinal hemorrhages, and often permanent brain damage, blindness, or death. Nurses should educate parents on coping with a crying baby.
- Munchausen Syndrome by Proxy (MSBP): A caregiver, usually the mother, fabricates or induces illness in a child. The nurse's role is to act as the child's advocate, identifying inconsistent signs and symptoms and reporting suspicions to child protective services.
5.3.3. Sexual Abuse
Sexual abuse is any sexual act or exploitation imposed on a child by an adult or an older child. It can be physical, emotional, or psychological. It's often difficult to identify because children may not disclose the abuse, and physical signs aren't always present.
1.3.4 Nursing Care of the Maltreated Child
- Recognize and Report: Nurses are mandatory reporters and must be able to recognize the signs and symptoms of abuse and neglect. These can include unexplained injuries, a delay in seeking medical care, or a child's fear of a caregiver.
- Create a Safe Environment: Provide a safe, non-judgmental space for the child to be examined and interviewed.
- Document: Document all injuries, observations, and conversations with the child and family in a detailed, objective manner.
- Support the Child: Provide comfort and emotional support to the child.
- Collaborate: Work with a multidisciplinary team, including social workers, child protective services, and law enforcement, to ensure the child's safety and well-being.
Nursing Insight: When documenting injuries, use objective, non-judgmental language. Instead of writing "The father's story doesn't make sense," document the specific details of the father's explanation and the discrepancy with the physical findings. For example, "Father states the child fell from a chair, but the child has a spiral fracture of the femur."
Health problems of the school-aged child
Health problems of the school-age chil
7.1. Obesity
Obesity is a serious health problem characterized by an excessive accumulation of body fat. In school-age children, it's typically defined as having a Body Mass Index (BMI) at or above the 95th percentile for their age and sex. Childhood obesity is a significant predictor of adult obesity and is linked to numerous health complications.
Complex Relationships in Childhood obesity
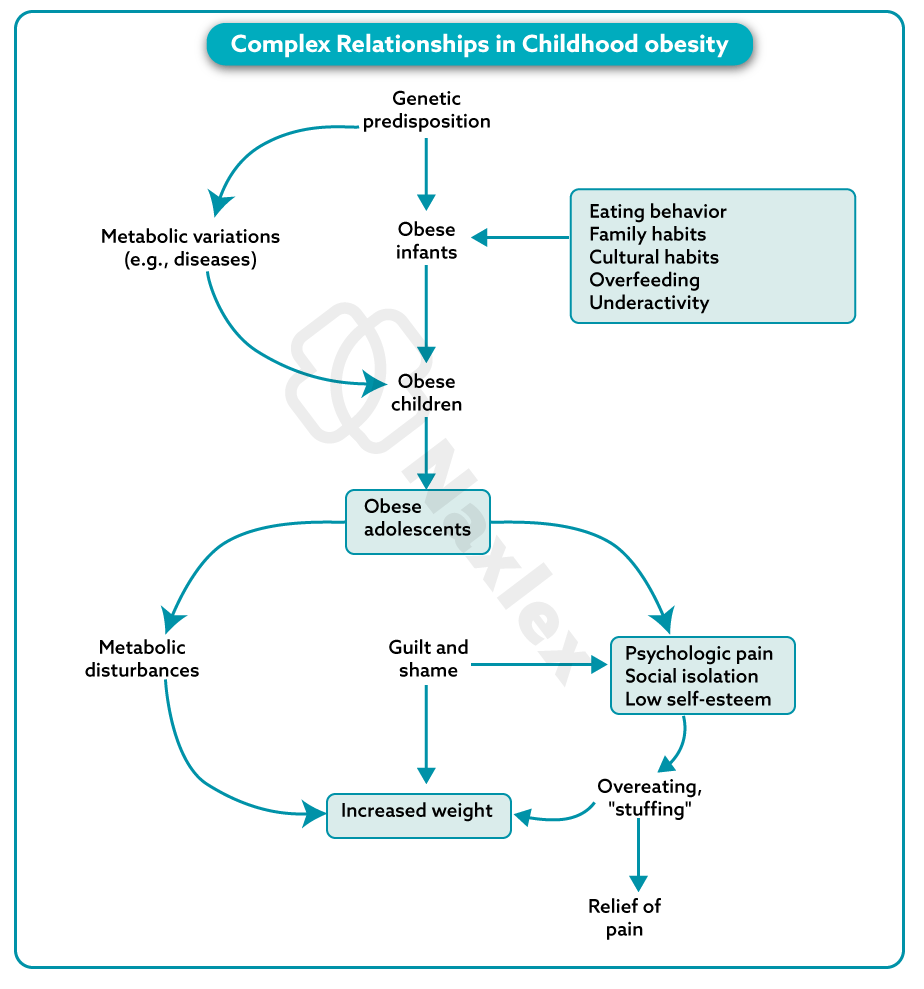
Complications
Obesity in childhood can lead to a wide range of short-term and long-term health problems affecting nearly every body system. These include:
- Cardiovascular: High blood pressure (hypertension), high cholesterol, and early development of atherosclerosis.
- Metabolic: Type 2 diabetes, insulin resistance, and non-alcoholic fatty liver disease (NAFLD).
- Musculoskeletal: Increased risk of fractures, flat feet, and joint pain, particularly in the hips and knees (e.g., slipped capital femoral epiphysis).
- Respiratory: Sleep apnea and asthma.
- Psychosocial: Low self-esteem, depression, anxiety, social isolation, and bullying.
Treatment
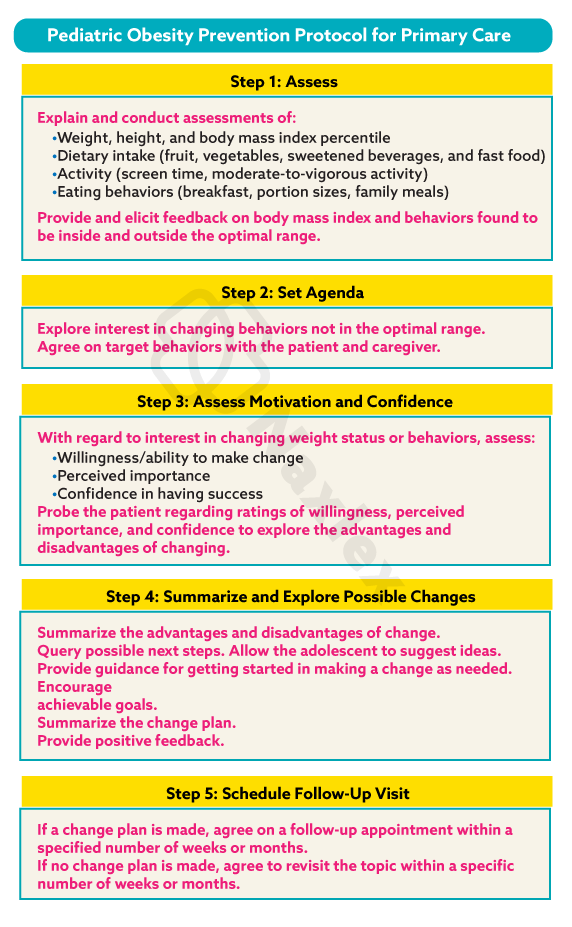
Treatment for childhood obesity is a multifaceted approach that involves the child, family, and healthcare providers. It focuses on lifestyle changes rather than rapid weight loss.
- Dietary Changes: Emphasize a balanced diet rich in fruits, vegetables, and whole grains while limiting sugary drinks, processed foods, and high-fat snacks. A registered dietitian can provide personalized guidance.
- Physical Activity: Encourage at least 60 minutes of moderate-to-vigorous physical activity daily. This can include sports, active play, or family activities. Screen time should be limited to less than two hours per day.
- Behavioral Therapy: Cognitive-behavioral therapy (CBT) can help children and families address emotional eating, build problem-solving skills, and develop a positive body image. Family involvement is crucial for long-term success.
Prevention
Preventing childhood obesity starts early and is a community-wide effort.
- Healthy Habits: Promote healthy eating and regular physical activity from a young age.
- Parental Modeling: Parents and caregivers should model healthy behaviors, such as eating nutritious meals and being physically active.
- Community Support: Schools, community centers, and healthcare providers should offer resources and programs that support healthy lifestyles.
- Policy: Policies that promote healthy food choices and safe places to play are essential for creating a supportive environment.
Nursing Insight: When discussing weight with a child and their family, use a positive, non-judgmental approach. Focus on "healthy choices" and "being strong and active" rather than "losing weight." This helps prevent the development of body image issues.
Pediatric Obesity Prevention Protocol for Primary Care
7.2. Dental Disorders
Dental health is a key component of a child's overall well-being. Poor oral hygiene and diet can lead to several common dental disorders.
Dental Caries (Cavities)
Dental caries is the irreversible breakdown of tooth enamel due to acid-producing bacteria in plaque. These bacteria metabolize sugars from food, creating acids that demineralize the tooth surface.
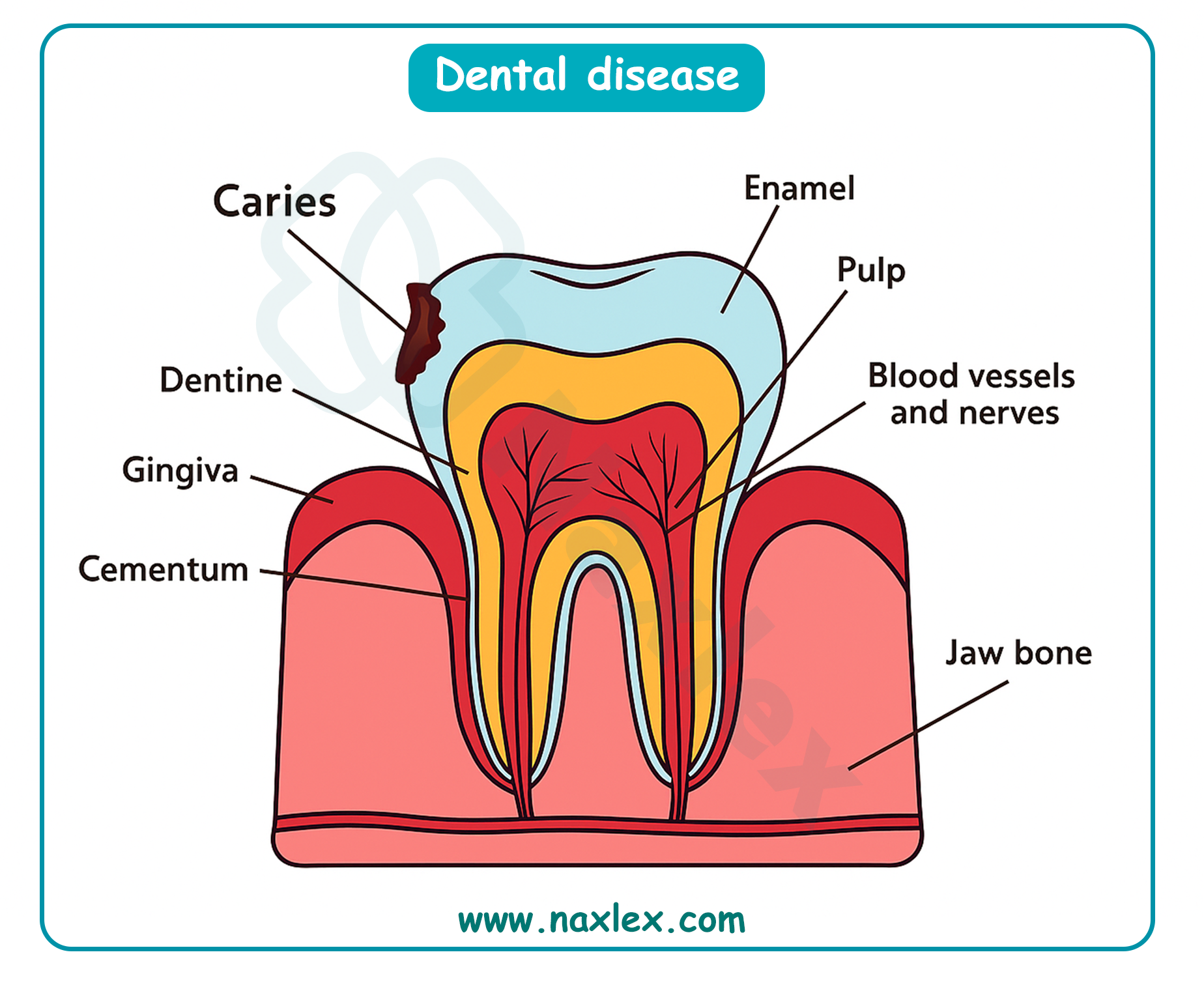
- Causes: Poor oral hygiene, a diet high in sugar and carbohydrates, and inadequate fluoride exposure.
- Symptoms: White spots on the teeth (early sign), brown or black spots, tooth sensitivity, and pain.
- Prevention: Brushing with a fluoride toothpaste twice daily, flossing, limiting sugary foods and drinks, regular dental check-ups, and dental appointments.
Periodontal Disease (Gum Disease)
Periodontal disease is an inflammation of the gums and supporting structures of the teeth. It's rare in its severe form in children but gingivitis (mild gum inflammation) is very common.
- Causes: Plaque buildup, poor oral hygiene, and genetic factors.
- Symptoms: Red, swollen, and bleeding gums.
- Prevention: Proper brushing and flossing to remove plaque and regular dental cleanings.
Malocclusion
Malocclusion refers to an improper alignment of the teeth and jaws. This can be hereditary or caused by habits like thumb-sucking or prolonged pacifier use.
- Types:
- Class I: The bite is normal, but teeth are crowded, spaced, or rotated.
- Class II (Overbite): The upper jaw and teeth protrude over the lower jaw.
- Class III (Underbite): The lower jaw and teeth protrude past the upper jaw.
- Treatment: Orthodontic treatment, such as braces or retainers.
Dental Trauma
Dental trauma is an injury to the teeth, gums, or supporting structures. It's common in school-age children due to falls, sports injuries, or accidents.
- Common Injuries: Fractured teeth, luxated (displaced) teeth, or avulsed (knocked-out) teeth.
- Action: Immediate dental care is essential. For a knocked-out permanent tooth, it's crucial to find the tooth, rinse it gently with milk or saline, and attempt to re-implant it or transport it to the dentist in a container of milk.
7.3. Disorders of Continence
These disorders involve the involuntary loss of urine or feces and can be a source of significant distress for children and their families.
Enuresis (Bedwetting)
Enuresis is the involuntary urination by a child who is past the age of toilet training. It's classified as primary (the child has never been consistently dry) or secondary (the child has a period of dryness lasting at least six months before the onset of enuresis).
- Causes: A combination of factors, including a small bladder capacity, a delay in the maturation of the nervous system, a family history of enuresis, and deep sleep patterns. Psychological factors can also play a role, especially in secondary enuresis.
- Treatment:
- Behavioral: Motivational therapy (e.g., star charts), fluid restriction before bedtime, and bladder training.
- Enuresis Alarms: These devices are highly effective and wake the child at the first sign of wetness, helping to condition them to wake up and use the toilet.
- Medication: Desmopressin, which reduces urine production at night, may be used for short-term management.
Encopresis (Fecal Incontinence)
Encopresis is the voluntary or involuntary passage of feces into inappropriate places by a child older than four years. It's often associated with chronic constipation.
- Causes: Chronic constipation leads to a buildup of hard stool in the rectum (impaction). This stretches the rectum, causing a loss of sensation. Liquid stool from higher up in the colon leaks around the impacted stool, resulting in soiling.
- Treatment:
- Stool Removal: The first step is to clear the impacted stool using laxatives or enemas.
- Maintenance: A long-term regimen of high-fiber diet, increased fluids, and laxatives is needed to prevent re-impaction.
- Behavioral: Positive reinforcement and a regular toileting schedule are important.
7.4. Disorders With Behavioral Components
7.4.1. Attention-Deficit/Hyperactivity Disorder (ADHD)
Description: A neurodevelopmental disorder characterized by persistent patterns of inattention, hyperactivity, and impulsivity that interfere with functioning or development.
- Symptoms:
- Inattention: Difficulty sustaining attention, is easily distracted, seems not to listen, and struggles with organization.
- Hyperactivity: Fidgets, talks excessively, can't sit still, and has trouble engaging in quiet activities.
- Impulsivity: Acts without thinking, interrupts others, and has difficulty waiting their turn.
Clinical Characteristics of ADHD
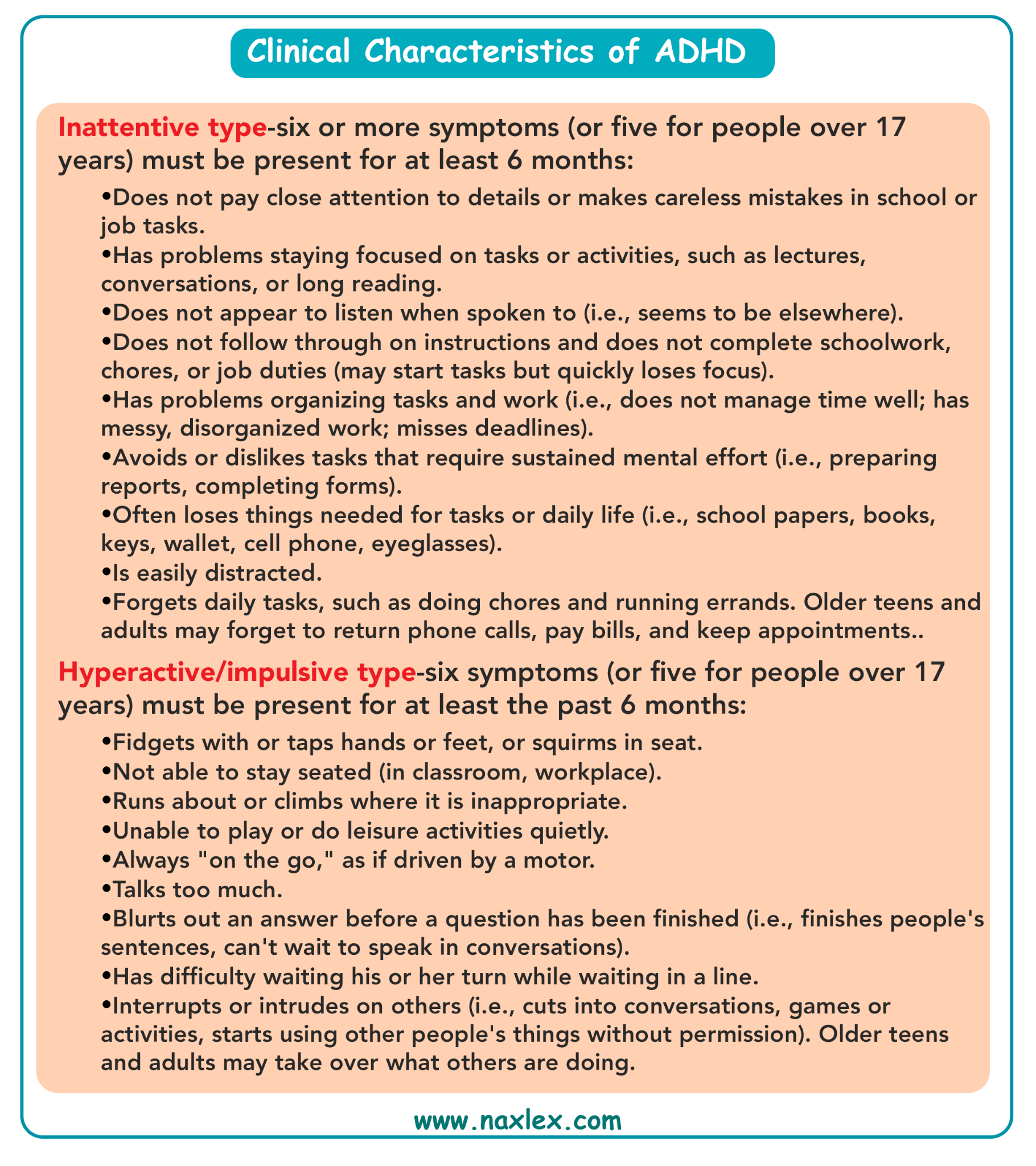
- Management:
- Medication: CNS stimulants (e.g., methylphenidate, amphetamine) are often used to improve focus and reduce hyperactivity.
- Behavioral Therapy: Strategies include creating a structured environment, using clear and consistent rules, providing positive reinforcement, and teaching social skills.
- Nursing Care: Educate parents and teachers on the disorder, administer medications, and monitor for side effects. Advocate for school accommodations (e.g., extended time on tests).
ADHD is a neurodevelopmental disorder characterized by persistent patterns of inattention, hyperactivity, and/or impulsivity.
- Core Symptoms:
- Inattention: Difficulty sustaining attention, being easily distracted, forgetfulness, and organizational problems.
- Hyperactivity: Fidgeting, restlessness, excessive talking, and difficulty remaining seated.
- Impulsivity: Acting without thinking, interrupting others, and difficulty waiting for one's turn.
- Treatment: A combination of medication (stimulants or non-stimulants) and behavioral therapy. Behavioral therapy focuses on developing organizational skills, time management, and social skills. Parent training is also a crucial component.
7.4.2 Learning Disability
A Learning Disability is a neurological disorder that affects a person's ability to receive, process, analyze, or store information. It's not a sign of low intelligence.
- Types:
- Dyslexia: Difficulty with reading, including decoding words, reading fluency, and comprehension.
- Dysgraphia: Difficulty with writing, including handwriting, spelling, and organizing thoughts on paper.
- Dyscalculia: Difficulty with math, including understanding number concepts and performing calculations.
- Intervention: Specialized educational programs, accommodations in the classroom (e.g., extra time on tests), and one-on-one tutoring.
7.4.3. Tic Disorders
Tics are sudden, rapid, recurrent, non-rhythmic movements or vocalizations. They can be simple (e.g., eye blinking, throat clearing) or complex (e.g., jumping, repeating phrases).
- Treatment: In most cases, tics are mild and don't require treatment. However, when tics are disruptive, behavioral therapies (e.g., habit reversal training) and sometimes medication may be used.
7.4.4 Gilles De La Tourette Syndrome
Tourette's Syndrome is a complex tic disorder characterized by the presence of both multiple motor tics and at least one vocal tic for more than one year.
- Associated Conditions: Tourette's is often associated with other conditions, including ADHD, Obsessive-Compulsive Disorder (OCD), and anxiety.
- Treatment: Primarily symptomatic. Behavioral therapies like Habit Reversal Training (HRT) and Comprehensive Behavioral Intervention for Tics (CBIT) are the first-line treatment. Medications are used when tics are severe and interfere with daily functioning.
7.4.5 Post-Traumatic Stress Disorder (PTSD)
PTSD is a disorder that develops in some people who have experienced a shocking, scary, or dangerous event. In children, it may present differently than in adults.
- Symptoms:
- Re-experiencing: Flashbacks, nightmares, and intrusive thoughts about the event.
- Avoidance: Avoiding places, people, or activities that remind them of the trauma.
- Negative Changes in Mood/Thinking: Negative beliefs about themselves, difficulty with positive emotions, and memory problems.
- Increased Arousal: Irritability, difficulty sleeping, and being easily startled.
- Treatment: Trauma-focused cognitive-behavioral therapy (TF-CBT) is a highly effective treatment for children with PTSD. Family therapy and play therapy are also used.
7.4.6 School Phobia
School phobia, or school refusal, is an extreme, irrational fear of attending school. It's often a symptom of an underlying anxiety disorder, such as separation anxiety or social anxiety.
- Symptoms: Physical complaints (stomachaches, headaches) that disappear on weekends or school breaks, panic attacks, and crying spells before school.
- Treatment: The goal is a gradual return to school. Treatment involves a multi-pronged approach with the child, family, and school. Cognitive-behavioral therapy (CBT) helps the child understand and manage their anxiety.
7.4.7 Functional Abdominal Pain (FAP)
FAP is a chronic or recurrent abdominal pain that has no identifiable organic cause. It's often linked to psychological stress or anxiety.
- Symptoms: Diffuse, crampy pain around the belly button, with no other signs of illness. It doesn't typically wake the child at night.
- Treatment: Reassurance and education are key. Treatment focuses on managing the pain and coping with the symptoms, often using CBT, relaxation techniques, and sometimes dietary changes.
7.4.8 Childhood Depression
Childhood depression is a serious mood disorder that can affect how a child feels, thinks, and behaves. It's more than just a passing sadness.
- Symptoms: Persistent sadness or irritability, loss of interest in activities they once enjoyed, changes in appetite or sleep, fatigue, feelings of worthlessness or guilt, and thoughts of self-harm or suicide.
- Treatment: Cognitive-behavioral therapy (CBT) and Interpersonal Therapy (IPT) are effective. In moderate-to-severe cases, medication (antidepressants) may be used in combination with therapy, with careful monitoring.
7.4.9 Childhood Schizophrenia
Childhood schizophrenia is a rare but severe psychiatric disorder characterized by psychosis, including hallucinations and delusions. Its onset is typically later in adolescence, but in rare cases, it can begin in childhood.
- Symptoms: Hallucinations (e.g., hearing voices), delusions (false beliefs), disorganized thinking, and social withdrawal.
- Treatment: A combination of antipsychotic medication, psychotherapy (individual and family), and social skills training. Early intervention is crucial for a better prognosis.
7.4.10. Anxiety Disorders
Anxiety disorders are the most common mental health problems in children. They are characterized by excessive fear, worry, and avoidance behaviors.
- Types:
- Separation Anxiety: Excessive worry about being away from home or attachment figures.
- Generalized Anxiety Disorder (GAD): Persistent and excessive worry about multiple things (e.g., school performance, future events).
- Social Anxiety Disorder: Intense fear of social situations and being judged by others.
- Specific Phobias: Irrational fear of a specific object or situation (e.g., dogs, needles, heights).
- Treatment: Cognitive-behavioral therapy (CBT) is the gold standard for treating anxiety disorders in children. It helps them identify and challenge anxious thoughts and gradually face their fears.
7.4.11 Conduct Disorders
Conduct Disorder is a behavioral disorder characterized by a persistent pattern of violating the rights of others or major age-appropriate societal norms or rules.
- Symptoms: Aggression toward people and animals, destruction of property, deceitfulness or theft, and serious violations of rules.
- Treatment: Parent Management Training (PMT), in which parents learn techniques to manage their child's behavior, and Multisystemic Therapy (MST), which addresses the child's entire social environment (family, school, community).
Nursing Insight: When a child presents with somatic symptoms like stomachaches or headaches with no organic cause, always consider psychosocial stressors like school phobia, anxiety, or bullying. A thorough psychosocial assessment is as important as a physical one.
d
Health problems of the adolescent
9.1. Health Conditions of the Male Reproductive System
9.1.1. Penile Conditions
Adolescent males may experience various penile conditions. Phimosis is a condition where the foreskin can't be retracted, while paraphimosis is a medical emergency where the retracted foreskin is trapped behind the glans, causing swelling. Balanitis is an inflammation of the head of the penis, often caused by poor hygiene.
9.1.2. Varicocele
A varicocele is an enlargement of the veins within the scrotum, similar to a varicose vein in the leg.
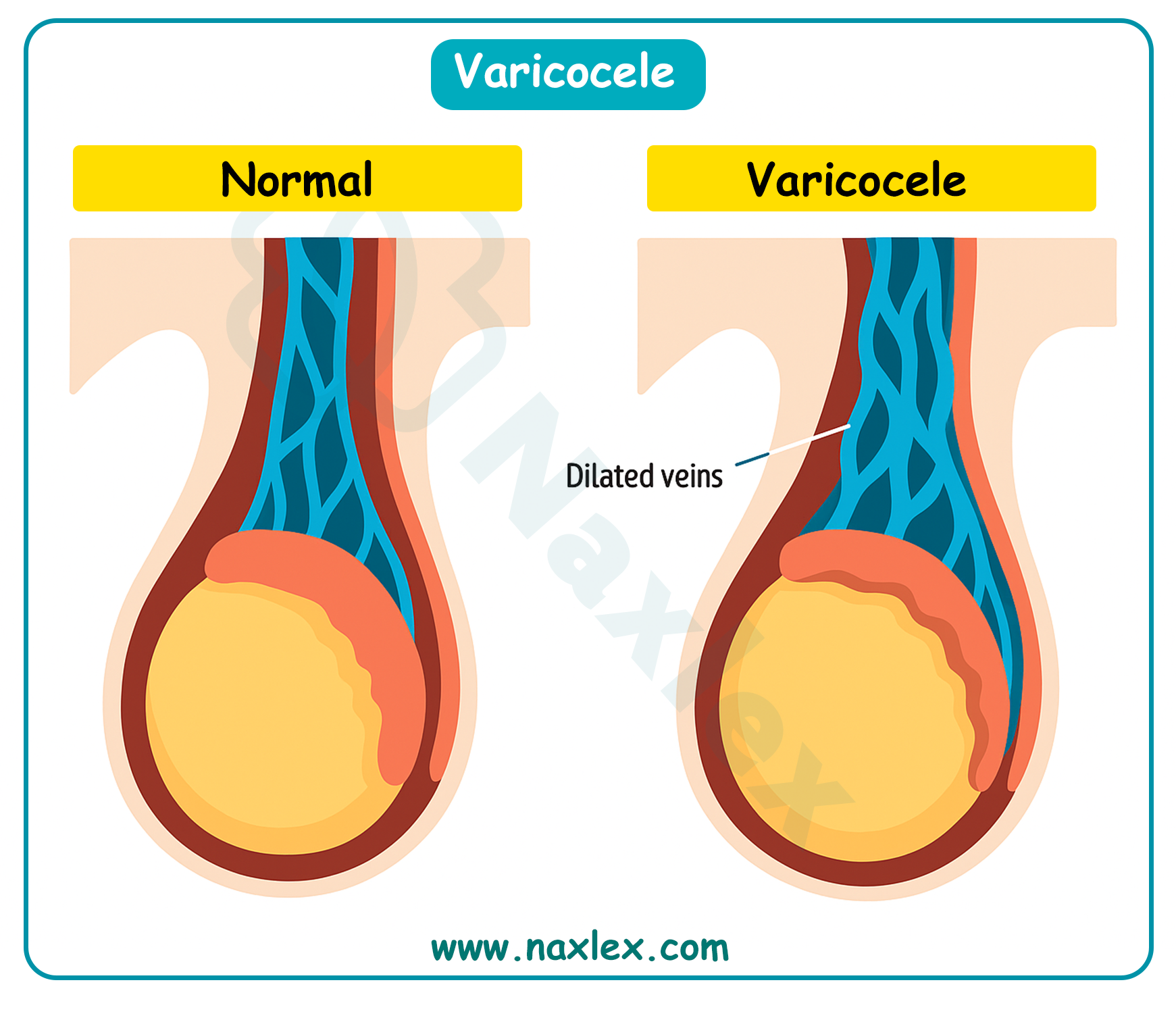
It's a common cause of low sperm production and decreased sperm quality, which can lead to infertility. It often feels like a "bag of worms." Treatment is usually only necessary if the varicocele causes pain, testicular atrophy, or infertility.
9.1.3. Epididymitis
- Epididymitis is an inflammation of the epididymis, the coiled tube at the back of the testicle that stores and carries sperm.
- It's often caused by a bacterial infection, including sexually transmitted infections (STIs) like chlamydia or gonorrhea.
- Symptoms include testicular pain, redness, and swelling, often accompanied by fever. Treatment involves antibiotics and supportive care.
9.1.4. Testicular Torsion
- Testicular torsion is a medical emergency where the spermatic cord, which provides blood to the testicle, twists. This cuts off blood supply and can lead to the death of the testicle.
- Symptoms include a sudden onset of severe testicular pain, swelling, and redness. It requires immediate surgical intervention to save the testicle.
9.1.5. Gynecomastia
Gynecomastia is the benign enlargement of male breast tissue. It's common during puberty due to hormonal imbalances. It usually resolves on its own, but in some cases, it can persist and cause psychological distress. In such cases, surgical removal of the excess tissue may be considered.
9.2. Health Conditions of the Female Reproductive System
9.2.1. Gynecologic Examination
- The first gynecologic exam for an adolescent is typically recommended between ages 13 and 15, unless there's a specific health concern. The first exam usually doesn't include a Pap test unless the adolescent is sexually active. The exam focuses on providing education about reproductive health, menstrual cycles, and contraception.
Nursing Insight: To make the gynecologic exam less intimidating for an adolescent, a nurse should explain each step of the process clearly and respectfully. Offering the option of a chaperone and ensuring privacy are also vital.
9.2.2. Menstrual Disorders
- Amenorrhea: The absence of menstruation. Primary amenorrhea is when menstruation hasn't started by age 16. Secondary amenorrhea is the cessation of menstruation for more than three to six months in someone who has previously had periods. Causes can include hormonal imbalances, excessive exercise, or eating disorders.
- Dysmenorrhea: Painful menstruation. Primary dysmenorrhea is common and caused by prostaglandins, which cause uterine contractions. It's treated with NSAIDs. Secondary dysmenorrhea is caused by an underlying medical condition, such as endometriosis or fibroids.
9.2.3. Endometriosis
Endometriosis is a condition in which tissue similar to the lining of the uterus grows outside the uterus. This can cause severe pelvic pain, especially during menstruation, and may lead to infertility. Diagnosis often involves a laparoscopy.
9.2.4. Premenstrual Syndrome (PMS)
PMS is a group of physical and emotional symptoms that occur in the one to two weeks before menstruation. Symptoms can include bloating, breast tenderness, mood swings, and irritability. Lifestyle changes, such as diet and exercise, can help manage symptoms.
9.2.5. Abnormal Uterine Bleeding
This refers to any deviation from a normal menstrual cycle, including bleeding between periods, a very heavy flow, or an unusually long period. It can be caused by hormonal imbalances, uterine fibroids, or infections.
9.2.6. Vaginal Infections
- Bacterial Vaginosis (BV): An imbalance of bacteria in the vagina, characterized by a thin, gray discharge with a "fishy" odor. It's treated with antibiotics.
- Candidiasis (Yeast Infection): An overgrowth of the Candida fungus, causing itching, burning, and a thick, white discharge. It's treated with antifungal medications.
9.2.7. Sexually Transmitted Infections (STIs)
Adolescents are a high-risk group for STIs.
- HIV: A virus that attacks the immune system.
- Trichomoniasis: A parasitic infection causing a foul-smelling, greenish-yellow discharge.
- Chlamydia and Gonorrhea: Both are bacterial infections that often have no symptoms, making them easy to spread. They can lead to pelvic inflammatory disease (PID).
- Syphilis: A bacterial infection that progresses through stages and can cause serious long-term complications if left untreated.
- Pelvic Inflammatory Disease (PID): An infection of the female reproductive organs, often a complication of untreated chlamydia or gonorrhea.
- HPV (Human Papillomavirus): The most common STI. Some strains cause genital warts, while others can lead to cervical cancer. A vaccine is available for prevention.
- Herpes Simplex Virus (HSV): Causes painful blisters on the genitals, mouth, or surrounding areas. It's a lifelong infection.
- Hepatitis: A viral infection of the liver, with types B and C being transmitted sexually.
Nursing Insight: When discussing sexual health with adolescents, use a non-judgmental, confidential, and straightforward approach. Use the "5 P's" as a framework for your assessment: Partners, Practices, Protection from STIs, Past history of STIs, and Pregnancy plans.
9.3. Health Conditions Related to Reproduction
9.3.1. Adolescent Pregnancy
Teen pregnancy is associated with higher risks for both the mother and the infant, including pre-term birth, low birth weight, and higher infant mortality rates. Social and economic consequences for the mother are also significant.
9.3.2. Adolescent Abortion
Adolescents may seek abortion due to lack of support, financial instability, or wanting to continue their education. They require compassionate, non-judgmental care and counseling.
9.3.3. Contraception
Adolescents need access to comprehensive education about contraception, including methods like condoms, birth control pills, and long-acting reversible contraception (LARC) such as IUDs and implants. Condoms are the only method that also protects against STIs.
9.3.4. Sexual Assault
Sexual assault is a serious crime and a devastating experience for an adolescent. Nurses must provide sensitive, trauma-informed care. This includes providing a safe space, physical assessment, and collection of forensic evidence, as well as offering emotional support and resources for counseling.
9.4. Health Conditions with a Behavioral Component
9.4.1. Anorexia Nervosa and Bulimia Nervosa
Description: Eating disorders characterized by a distorted body image.
- Anorexia Nervosa: Involves a refusal to maintain a healthy body weight, an intense fear of gaining weight, and a distorted perception of body shape.
- Bulimia Nervosa: Involves cycles of binge eating followed by compensatory behaviors like self-induced vomiting, excessive exercise, or laxative abuse.
- Management: Requires a multidisciplinary team approach including medical stabilization, nutritional counseling, and psychotherapy.
9.4.2. Substance Abuse
Substance abuse is the harmful use of psychoactive substances. Adolescents may be particularly vulnerable due to peer pressure and a developing brain.
- Tobacco: Nicotine is highly addictive. Vaping and e-cigarettes are also a major concern.
- Alcohol: Can impair judgment and lead to risky behaviors, as well as long-term health problems.
- Cocaine: A powerful stimulant that can be highly addictive.
- Narcotics: Opioids like heroin and prescription painkillers are highly addictive and carry a high risk of overdose.
- CNS Depressants: Drugs like benzodiazepines that slow brain activity.
- CNS Stimulants: Drugs like amphetamines that speed up brain activity.
- Mind-altering drugs: Hallucinogens like LSD and PCP.
9.4.3. Self-Harm
Description: A coping mechanism for intense emotional pain, not necessarily a suicide attempt. It includes cutting, burning, or scratching oneself.
- Management: Nurses must assess for suicidal ideation and provide a safe environment. Teaching alternative coping strategies and referring the adolescent to a mental health professional is crucial.
9.4.4. Suicide
Description: Suicide is a leading cause of death in adolescents.
- Risk factors: Depression, substance abuse, previous suicide attempts, and a family history of suicide.
- Management:
- Nursing Insight: If an adolescent discloses thoughts of self-harm or suicide, the nurse's priority is to assess the immediate risk. Ask direct questions like, "Are you thinking about hurting yourself?" and "Do you have a plan?" If a plan exists, the adolescent is at high risk and should not be left alone. Initiate a safety contract and contact the appropriate mental health services.
Summary
- Infants are vulnerable to nutritional deficiencies (vitamin D, iron, vitamin K), malnutrition (kwashiorkor, marasmus), and food sensitivities (CMA, lactose intolerance, FTT).
- Other issues include colic, SIDS, and positional plagiocephaly. Management involves nutrition support, infection control, safe sleep practices, parental education, and preventive measures like tummy time and vitamin supplementation.
- Early childhood health issues include sleep problems such as sleep-onset association disorder, night terrors, and obstructive sleep apnea, which disrupt rest and development.
- Ingestion of injurious agents, including lead poisoning, requires prompt assessment, poison control consultation, and prevention strategies. Child maltreatment including neglect, physical abuse, and sexual abuse, necessitates recognition, reporting, documentation, and multidisciplinary collaboration.
- Nurses play a critical role in early detection, intervention, and ensuring a safe environment for affected children.
- Adolescent health issues include male reproductive conditions such as phimosis, varicocele, epididymitis, testicular torsion, and gynecomastia, and female concerns like menstrual disorders, endometriosis, PMS, and STIs.
- Reproductive health topics include teen pregnancy, abortion, contraception, and sexual assault. Behavioral health challenges include eating disorders, substance abuse, self-harm, and suicide risk.
- Nursing care focuses on prevention, early detection, education, emotional support, and multidisciplinary intervention.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Health problems in children (infancy to adolescence)
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


