Please set your exam date
The Nursing Process In Pharmacology
Study Questions
Practice Exercise
A patient has a new prescription for a blood pressure medication that may cause him to feel dizzy during the first few days of therapy. Which is the best human needs statement for this situation?
Explanation
When starting a new antihypertensive medication, the patient may experience dizziness during the first few days due to orthostatic hypotension or initial adjustments to reduced blood pressure. This places the patient at increased risk for falls and injury, making physical safety the primary human need to address.
Rationale for correct answer:
B. Physical safety – Best choice because dizziness elevates the risk of falls and related injuries. Ensuring safety by teaching the patient to rise slowly, use handrails, and avoid sudden position changes directly addresses the immediate danger.
Rationale for incorrect answers:
A. Physical activity – While dizziness could temporarily limit mobility, activity level is not the most urgent concern. Preventing falls takes priority before encouraging activity.
C. Freedom from pain – The symptom described (dizziness) is not pain-related, so pain management is not the primary nursing focus in this scenario.
D. Interchange of gases – This relates to oxygen exchange and respiratory function, which are not affected by dizziness caused by antihypertensives.
Take-Home Points:
- Orthostatic hypotension from antihypertensives can cause dizziness and falls.
- Physical safety interventions are essential during medication initiation.
- Educating patients on gradual position changes reduces fall risk.
The nurse is compiling a drug history for a patient. Which questions from the nurse will obtain the most information from the patient? Select all that apply
Explanation
A thorough drug history involves asking questions that elicit detailed and relevant information about a patient’s medication use, allergies, and symptom management. This includes open-ended questions that encourage the patient to explain their experiences, ensuring the nurse gathers the most accurate and complete picture to promote safe and effective care.
Rationale for correct answers:
C. “When you have pain, what do you do to relieve it?” – Best question because it is open-ended and invites the patient to describe all pain-relief measures, including prescription drugs, OTC medications, herbal remedies, and non-drug approaches.
E. “Tell me about what happened when you had the allergic reaction to penicillin.” – Best choice as it provides essential details about the type and severity of the reaction, helping prevent future adverse events.
F. “What herbal products or over-the-counter medications do you use?” – Best choice because many patients take these products without considering them “medications,” and they can cause significant drug interactions.
Rationale for incorrect answers:
A. “Do you use sleeping pills to get to sleep?” – This yes/no question limits the amount of information obtained. An open-ended question would encourage more detail about the type, frequency, and duration of use.
B. “Do you have a family history of heart disease?” – While important for overall health assessment, it does not provide direct information for the drug history.
D. “Did you have the mumps as a child?” – This is a past illness history question, not directly related to current or previous drug use.
Take-Home Points:
- Favor open-ended over yes/no questions for medication history.
- Always include herbal and OTC product use in assessments.
- Document allergy type, reaction details, and severity to prevent harm.
A 77-year-old man who has been diagnosed with an upper respiratory tract infection tells the nurse that he is allergic to penicillin. Which is the most appropriate response by the nurse?
Explanation
A thorough drug allergy assessment is a critical part of safe medication administration. When a patient reports an allergy, the nurse must obtain specific, detailed information about the reaction to distinguish between true allergic hypersensitivity and non-allergic adverse effects. This distinction guides decisions on whether a drug or related compounds can be administered safely. Open-ended, clarifying questions help the nurse gather essential data on onset, symptoms, severity, and treatment of past reactions.
Rationale for correct answer:
C. “What type of reaction did you have when you took penicillin?” – Best choice because it invites the patient to describe the exact reaction, helping the nurse assess whether it was a true allergic event (e.g., rash, anaphylaxis) or a side effect. This information prevents dangerous re-exposure to the drug or related agents.
Rationale for incorrect answers:
A. “Many people are allergic to penicillin.” – This statement is vague and does not assess the patient’s reaction. It fails to gather information needed to determine allergy type, which is essential for safe prescribing.
B. “This allergy is not of major concern because the drug is given so often.” – The frequency of prescribing does not diminish the risk of severe allergic responses. Minimizing a patient’s reported allergy can result in unsafe medication administration and potentially life-threatening events.
D. “Drug allergies don't usually occur in older individuals due to built-up resistance to allergic reactions.” – This is inaccurate. Allergic responses can occur at any age, and prior exposure does not create resistance; in fact, repeated exposures may increase reaction risk.
Take-Home Points:
- Always clarify the nature of a reported drug allergy before proceeding with care.
- Differentiate between allergic reactions and adverse effects to guide safe prescribing.
- Age does not eliminate allergy risk; prior exposures can actually increase sensitivity.
The nurse is preparing a care plan for a patient who has been newly diagnosed with type 2 diabetes mellitus. Which of these reflect the correct order of the steps of the nursing process?
Explanation
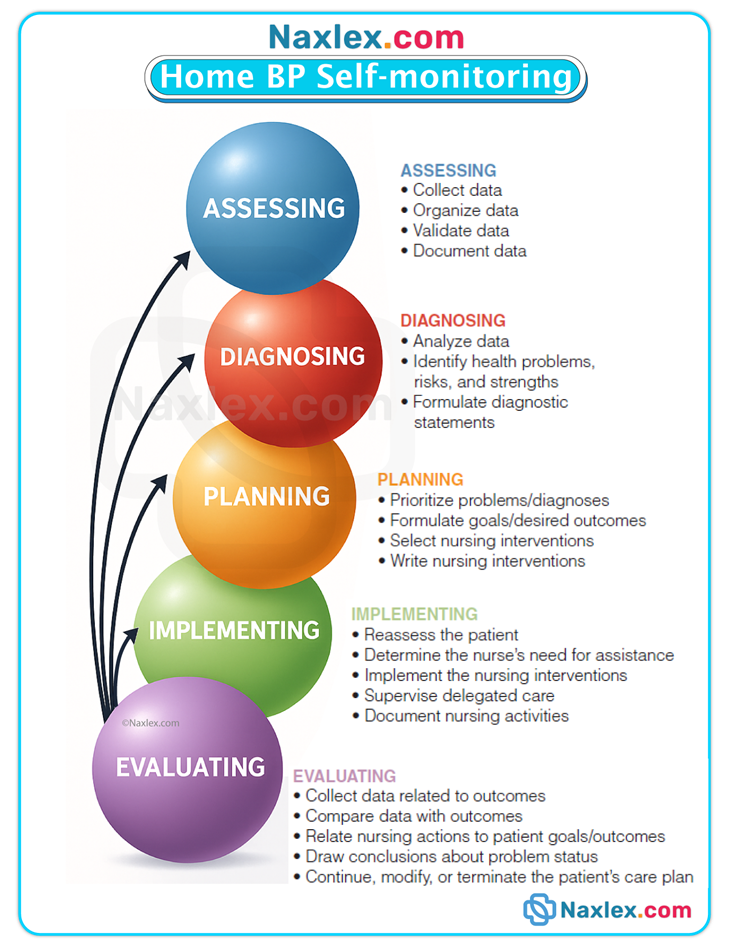
The nursing process is a systematic, patient-centered framework used by nurses to provide safe, effective, and individualized care. It follows a logical sequence that begins with gathering patient data and ends with evaluating the outcomes of care. Correct sequencing ensures that interventions are based on accurate information and tailored to patient needs.
Rationale for correct answer:
D. Assessment, human needs statement, planning, implementation, evaluation – This is the correct sequence: Assessment: Collect subjective and objective data. Human needs statement: Identify patient needs based on assessment data. Planning: Establish goals and choose interventions. Implementation: Carry out interventions. Evaluation: Determine if goals were met and modify care as needed.
Rationale for incorrect answers:
A. Assessment, planning, human needs statement, implementation, evaluation – This sequence skips the essential step of formulating the human needs statement immediately after assessment, which helps guide planning.
B. Evaluation, assessment, human needs statement, planning, implementation – This order starts with evaluation before any data collection or planning, which is illogical in the care process.
C. Human needs statement, assessment, planning, implementation, evaluation – Creating the human needs statement before conducting a thorough assessment risks basing care on incomplete or inaccurate information.
Take-Home Points:
- Always begin with a comprehensive assessment before identifying needs.
- The human needs statement (or nursing diagnosis) bridges assessment and planning.
- Evaluation is the final step, guiding ongoing adjustments to care.
The nurse is reviewing data collected from a medication history. Which of these data are considered objective data? Select all that apply
Explanation
Objective data are measurable, observable, and verifiable findings collected through direct examination, diagnostic tests, or equipment readings. They are not influenced by personal opinions and can be confirmed by other healthcare providers.
Rationale for correct answers:
A. White blood cell count 22,000 mm³ – This value comes from a laboratory test, making it a quantifiable and verifiable result, which is a hallmark of objective data.
B. Blood pressure 150/94 mm Hg – This is obtained using a blood pressure device, providing a measurable and reproducible physiologic reading, which qualifies it as objective.
E. Patient's weight is 68 kg – Weight is directly measured using a scale, making it objective and verifiable.
Rationale for incorrect answers:
C. Patient rates pain as an “8” on a 10-point scale – Pain scores are self-reported perceptions, meaning they are based on the patient’s feelings rather than measurable facts, making them subjective.
D. Patient's wife reports that the patient has been very sleepy during the day – This is second-hand information and represents subjective data from another observer, not a direct measurable finding.
Take-Home Points:
- Objective data are measurable facts like vital signs, lab values, and physical measurements.
- Subjective data are personal experiences or perceptions, reported by the patient or others.
- Distinguishing between the two ensures accurate assessment and care planning.
During a medication review session, a patient says, “I just do not know why I am taking all of these pills.” Based on this piece of subjective data, which diagnosis will the nurse identify?
Explanation
When a patient expresses uncertainty about their medication regimen, it suggests a gap in understanding that could affect adherence and safety. This falls under the nursing diagnosis of deficient knowledge, which is based on subjective data provided by the patient.
Rationale for correct answer:
B. Deficient knowledge – The patient’s comment reveals lack of understanding regarding the purpose of their medications, which is a knowledge deficit that may hinder compliance and therapeutic effectiveness.
Rationale for incorrect answers:
A. Risk for injury – This diagnosis applies when a patient is at potential harm due to environmental hazards, altered mobility, or side effects of medication. The patient’s statement does not directly indicate a hazard or unsafe condition.
C. Risk for aspiration – This is related to swallowing difficulties or impaired gag reflex, neither of which are indicated in the patient’s statement.
D. Anxiety – Although uncertainty can contribute to anxiety, the patient’s statement focuses on lack of information, not emotional distress or worry.
Take-Home Points:
- Deficient knowledge is identified when patients lack understanding of treatment, disease process, or self-care.
- Subjective statements from patients are crucial in forming accurate nursing diagnoses.
- Addressing knowledge gaps improves compliance, safety, and health outcomes.
The nurse is developing goals in collaboration with a patient. Which is the best goal statement?
Explanation
Goal-setting is a critical part of the nursing process, as it provides clear, measurable, and achievable outcomes for patient care. Effective goals should be specific, measurable, achievable, relevant, and time-bound (SMART). Collaborating with the patient ensures understanding, motivation, and adherence to the plan of care.
Rationale for correct answer:
C. The patient will independently self-administer the prescribed dose of albuterol by the end of the second teaching session.
This goal is specific (self-administer albuterol), measurable (independently by the end of the second session), achievable, and time-bound, aligning with SMART criteria and promoting patient autonomy.
Rationale for incorrect answers:
A. The patient will self-administer albuterol by tomorrow.
This goal lacks specificity about the correct dose and independence, making it less measurable and realistic.
B. The patient will self-administer the prescribed dose of albuterol by the end of the second teaching session.
Although time-bound and measurable, it does not emphasize independence, which is crucial for evaluating self-management.
D. The patient will organize her medications by tomorrow.
This goal addresses medication management, not the specific skill of self-administering albuterol, so it is not relevant to the immediate learning objective.
Take-home points:
- Goals should follow the SMART criteria: Specific, Measurable, Achievable, Relevant, Time-bound.
- Emphasize patient independence to assess true competency.
- Goals should directly relate to the teaching or care objective being measured.
Practice Exercise 2
An 86-year-old patient is being discharged to home on drug therapy for hyperthyroidism and has very little information regarding the medication. Which statement best reflects a realistic outcome of patient teaching activities?
Explanation
Establishing realistic and achievable outcomes is essential in patient teaching, especially for older adults who may have limited prior knowledge of their medications. Outcomes should be measurable and focused on essential knowledge or skills that the patient can demonstrate before discharge to ensure safe medication administration at home.
Rationale for correct answer:
A. The patient and patient's daughter will state the proper way to take the drug.
This outcome is specific, measurable, and realistic for a discharge teaching session. It ensures that both the patient and a caregiver understand how to administer the medication safely, which is critical for adherence and preventing complications.
Rationale for incorrect answers:
B. The nurse will provide teaching about the drug's adverse effects.
This describes a nursing action, not a patient-centered outcome. Outcomes should reflect what the patient will demonstrate or achieve, not what the nurse will do.
C. The patient will state all the symptoms of toxicity of the drug.
Expecting the patient to recall all symptoms of toxicity may be unrealistic for a single teaching session, especially for older adults with limited prior knowledge.
D. The patient will call the prescriber if adverse effects occur.
While important, this outcome is not easily measurable during the teaching session and does not confirm that the patient understands how or why to respond.
Take-home points:
- Outcomes should be patient-centered, measurable, and achievable.
- Focus on essential skills or knowledge, such as proper drug administration.
- Avoid using outcomes that describe nursing actions rather than patient performance.
A patient's medical record includes an order that reads as follows: “Atenolol 25 mg once daily at 0900.” Which action by the nurse is correct?
Explanation
Safe medication administration requires clarity in the medication order, including the drug, dose, route, and timing. The order specifies atenolol 25 mg once daily at 0900 but does not indicate the route of administration. Since atenolol can be given orally or intravenously, the nurse must verify the route with the prescriber before administration to prevent errors and ensure patient safety. Following the rights of medication administration is a fundamental nursing responsibility.
Rationale for correct answer:
D. The nurse contacts the prescriber to clarify the dosage route –Verification ensures safe and accurate administration and demonstrates adherence to the nursing responsibilities of assessment, critical thinking, and patient safety.
Rationale for incorrect answers:
A. The nurse does not give the drug – While withholding the drug temporarily is safe, the priority action is to clarify the route rather than simply not administering it, which could delay necessary therapy.
B. The nurse gives the drug orally – Assuming the route is oral without verification could lead to a medication error, especially if the prescriber intended intravenous administration.
C. The nurse gives the drug intravenously – Administering IV without confirmation is unsafe and could cause serious complications, including dosing errors or adverse effects.
Take-home points:
- Always verify ambiguous medication orders before administration.
- Communication with the prescriber prevents medication errors and protects patient safety.
- Following the rights of medication administration—drug, dose, route, time, patient, and documentation—is essential in all clinical settings.
The nurse is reviewing new medication orders that have been written for a newly admitted patient. The nurse will need to clarify which orders? Select all that apply
Explanation
When reviewing new medication orders, the nurse must ensure that each order contains all essential components: the drug name, dose, route, frequency, and any specific instructions. Missing details can result in medication errors, patient harm, or delayed treatment. Orders lacking critical information must be clarified before administration to ensure patient safety and compliance with the rights of medication administration.
Rationale for correct answer:
B. Sitagliptin (Januvia) 50 mg daily – Missing the route of administration. Sitagliptin can be taken orally, but the nurse must confirm this with the prescriber to avoid assumptions and potential errors.
E. Docusate (Colace) as needed for constipation – Missing dose and route. “As needed” orders must include specific parameters, such as dose, route, and frequency, to prevent unsafe or excessive administration.
Rationale for incorrect answers:
A. Metformin (Glucophage) 1000 mg PO twice a day – This order is complete. It includes drug name, dose, route, and frequency, allowing the nurse to safely administer the medication.
C. Simvastatin (Zocor) 20 mg PO every evening – Order is complete. It specifies the drug, dose, route, and timing, which aligns with recommended administration at bedtime.
D. Irbesartan (Avapro) 300 mg PO once a day – This order is complete and provides all necessary details for safe administration.
Take-home points:
- Every medication order must include drug name, dose, route, frequency, and any special instructions.
- PRN (as needed) orders require a clear indication, dose, route, and frequency.
- Nurses must clarify incomplete or ambiguous orders before administration to prevent medication errors and uphold patient safety.
When developing an effective medication teaching plan, which component will the nurse identify as most essential?
Explanation
Effective medication teaching depends not only on the content delivered but also on the quality of the nurse–patient relationship. Establishing trust and rapport ensures that the patient feels comfortable asking questions, disclosing concerns, and adhering to the medication plan. Without trust, even the clearest instructions may not result in safe or effective medication use.
Rationale for correct answer:
B. Establish a trust relationship – Trust encourages open communication, patient engagement, and adherence. Patients are more likely to ask questions, report side effects, and follow the plan when they feel their nurse respects and understands them.
Rationale for incorrect answers:
A. Provide written instructions – Written materials support learning but are insufficient alone. Patients may misinterpret instructions or fail to read them, particularly if health literacy is limited.
C. Use colorful charts – Visual aids can enhance learning, but they are supplementary. Without trust, patients may ignore or misapply the information provided.
D. Review community resources – This helps reinforce education and support, but it is secondary to building a therapeutic relationship that fosters motivation and understanding.
Take-home points:
- A strong nurse–patient relationship is foundational for safe and effective medication education.
- Trust facilitates patient engagement, disclosure of concerns, and adherence to therapy.
- Written materials, visual aids, and community resources are valuable adjuncts, but they cannot replace a trusting relationship.
When developing an individualized medication teaching plan, which topics will the nurse include? Select all that apply
Explanation
An individualized medication teaching plan should focus on key aspects that ensure safe and effective drug therapy. This includes helping patients understand how and when to take their medications, the importance of adherence, monitoring for adverse effects, and recognizing the need for follow-up laboratory tests to evaluate therapeutic outcomes or detect toxicity. Education should be tailored to the patient’s literacy, cognitive ability, and health needs.
Rationale for correct answers:
A. Importance of adherence to the prescribed regimen – Adherence is critical for achieving therapeutic goals and preventing complications. Nonadherence can lead to treatment failure or disease progression.
B. How to administer medication(s) – Patients must understand the route, timing, and technique for each medication to ensure effectiveness and prevent errors.
C. What side/adverse effects to report to the health care provider – Teaching patients to recognize and report adverse reactions promptly improves safety and allows timely intervention.
E. Follow-up laboratory tests, if needed – Lab monitoring is necessary for some medications to evaluate efficacy or detect toxicity (e.g., anticoagulants, antidiabetics, or drugs affecting renal/hepatic function).
Rationale for incorrect answer:
D. Foods that must be eaten – While dietary considerations may be relevant for certain medications, this is not universally required for all drug regimens and is individualized based on the medication’s interactions.
Take-home points:
- Focus on adherence, correct administration, monitoring for adverse effects, and required follow-up in medication teaching.
- Tailor education to the patient’s cognitive abilities, literacy level, and health conditions.
- Reinforce understanding through demonstration, written instructions, and repeat-back methods.
The Guiding Principles for Patient engagement are most important for health care providers as they strive for which goal?
Explanation
Patient engagement is a core principle in modern healthcare, emphasizing that active partnerships between patients and all members of the healthcare team improve safety, quality, and overall health outcomes. Establishing therapeutic relationships allows providers to understand patients’ values, preferences, and needs, which informs clinical decision-making and enhances adherence to treatment plans.
Rationale for correct answer:
C. All health care providers to have patient relationships for cornerstone of safety and quality – Correct. Effective patient-provider relationships form the foundation of patient engagement, fostering communication, shared decision-making, and safety.
Rationale for incorrect answers:
A. Nurses to focus care on quality and safety – While nurses play a key role in quality and safety, patient engagement principles extend beyond nursing to all healthcare providers, ensuring comprehensive collaboration.
B. Confidentiality as determined by the patient – Maintaining confidentiality is vital, but patient engagement primarily aims to build collaborative relationships, not solely manage privacy.
D. Patient advocacy – Advocacy is part of engagement but represents only one aspect; the broader goal is partnership and collaboration across all care providers.
Take-home points:
- Patient engagement requires active partnerships between patients and all healthcare providers.
- Strong therapeutic relationships improve safety, adherence, and care quality.
- Engagement principles guide shared decision-making, communication, and collaborative care planning.
The QSEN focus on safety is best exemplified by which competency?
Explanation
The Quality and Safety Education for Nurses (QSEN) initiative emphasizes integrating safety and quality into everyday nursing practice. Patient-centered collaborative care demonstrates this focus by involving patients and healthcare team members in decision-making, identifying potential safety risks, and coordinating care effectively. This competency ensures that patient care is not only individualized but also minimizes errors and promotes safe outcomes.
Rationale for correct answer:
D. Patient-centered collaborative care – This competency highlights team-based, patient-focused care, reducing errors through communication, shared decision-making, and active patient involvement, directly reflecting QSEN’s safety emphasis.
Rationale for incorrect answers:
A. Patient advocacy – While advocacy supports patient safety, it focuses mainly on speaking up for patient needs, not on systematic collaboration across the healthcare team.
B. Technology-enhanced medication administration – Using technology (like barcode scanning) improves safety, but QSEN competencies are broader and include collaboration and communication, not just tools.
C. Quality improvement – This competency emphasizes evaluating and improving care processes, but it does not inherently ensure real-time safety through patient-centered collaboration.
Take-home points:
- QSEN safety competency is best achieved through collaborative, patient-centered care.
- Involving patients and the healthcare team reduces errors and promotes safe outcomes.
- Effective communication and shared decision-making are key to real-world patient safety.
Which teaching strategy is most likely to succeed in health teaching with the patient and family?
Explanation
Effective patient teaching relies on ensuring that the patient and family can perform the skill safely and correctly rather than just verbalizing understanding. Demonstration allows the nurse to observe technique, correct errors, and reinforce learning, which is especially important for medication administration, wound care, and use of medical devices. This method is considered a high-yield, evidence-based approach for assessing learning.
Rationale for correct answer:
C. Have patient demonstrate information – Correct. Demonstration allows the nurse to assess procedural competence, correct errors in real time, and reinforce proper technique, improving safety and adherence.
Rationale for incorrect answers:
A. Have patient verbalize understanding – Verbal feedback confirms comprehension but does not ensure the patient can perform the skill correctly, leaving room for mistakes in actual practice.
B. Have patient answer closed-ended questions – Yes/no or multiple-choice questions provide limited insight into practical skills or safe application, making this a less reliable teaching strategy.
D. Have patient identify pill by color – Recognizing appearance alone does not ensure correct administration, dosage, or understanding of side effects, and is inadequate for comprehensive teaching.
Take-home points:
- Demonstration is the most effective teaching strategy for skill-based patient education.
- Observing the patient perform the task ensures competence and safety.
- Always reinforce learning with feedback and repeat demonstration if necessary.
Comprehensive Questions
Which of the following are correct statements regarding nursing diagnoses? Select all that apply
Explanation
Nursing diagnoses are clinical judgments that identify the client’s response to actual or potential health and life processes. They focus on how the patient is affected by health conditions rather than the medical diagnosis itself. Nursing diagnoses assist in determining nursing interventions, guiding the nurse to select appropriate actions that promote health, prevent complications, and support recovery. By addressing these patient-centered problems, nurses create individualized care plans that improve outcomes.
Rationale for correct answers:
C. They identify the client’s response to actual or potential health and life processes:
Nursing diagnoses describe the human response to health problems, such as anxiety, risk for falls, or impaired gas exchange. This guides holistic care by addressing the client’s physical, emotional, and psychosocial needs, both actual and potential.
D. They assist in determining nursing interventions:
Once a nursing diagnosis is made, it directly influences the planning of nursing interventions. For example, identifying a diagnosis of “Ineffective Airway Clearance” leads to interventions like positioning, suctioning, and encouraging deep breathing exercises to support airway management.
Rationale for incorrect answers:
A. They identify the medical problem experienced by the client:
Medical problems such as pneumonia or diabetes are addressed through medical diagnoses, not nursing diagnoses. Nursing diagnoses focus on how the client responds to these medical conditions rather than the conditions themselves.
B. They are identified for the client by the nurse:
Nurses develop nursing diagnoses, but these diagnoses are formulated in collaboration with the client’s input during assessment. Nursing diagnoses reflect shared care planning rather than the nurse acting alone.
E. They remain the same throughout the client’s healthcare encounter to ensure continuity of care:
Nursing diagnoses are dynamic and should be updated as the client’s condition changes. Frequent reassessment allows for accurate care planning and reflects improvements or complications in the client’s status.
Take-home points:
- Nursing diagnoses describe the client’s responses to health problems, not the medical condition itself.
- Nursing diagnoses guide the selection of individualized nursing interventions.
- Nursing diagnoses are updated regularly based on changes in the client’s condition.
Which of the following represents an appropriate outcome established during the planning phase?
Explanation
An appropriate outcome established during the planning phase is a specific, measurable goal that guides nursing interventions and evaluates patient progress. For example, “The client will demonstrate self-administration of the medication, using a preloaded syringe into the subcutaneous tissue of the thigh, prior to discharge.” This outcome clearly defines the expected patient behavior, the conditions under which it will occur, and the timeframe for achievement, supporting safe and effective medication management.
Rationale for correct answer:
B. The client will demonstrate self-administration of the medication, using a preloaded syringe into the subcutaneous tissue of the thigh, prior to discharge:
This is a clear, measurable, time-framed outcome focused on the client’s behavior. It reflects the client’s ability to perform a critical self-care task and allows the nurse to objectively assess whether the goal has been met before discharge.
Rationale for incorrect answers:
A. The nurse will teach the client to recognize and respond to adverse effects from the medication:
This is a nursing intervention, describing what the nurse will do rather than what the client will accomplish. Outcomes should be client-focused and measurable.
C. The nurse will teach the client to accurately prepare the dose of medication:
This describes an action performed by the nurse, not the client’s resulting ability or performance. Nursing outcomes must reflect patient behavior or achievement, not nursing actions.
D. The client will be able to self-manage his disease and medications:
Although this reflects an overall goal, it is too broad and vague. Effective outcomes should be specific, measurable, achievable, relevant, and time-bound (SMART), making it easier to evaluate the client’s success.
Take-home points:
- Nursing outcomes should describe what the client will do, not the nurse’s actions.
- Effective outcomes are specific, measurable, and time-framed to evaluate client learning.
- Broad goals like "self-manage disease" need to be broken into clear, achievable steps.
A 15-year-old adolescent with a history of diabetes is treated in the emergency department for complications related to skipping her medication for diabetes. She confides in the nurse that she deliberately skipped some of her medication doses because she did not want to gain weight and she is afraid of needle marks. Before establishing a diagnosis of “Noncompliance,” what should the nurse assess?
Explanation
Before establishing a diagnosis of “Noncompliance,” the nurse must first assess whether the client received adequate teaching about the prescribed medication and whether the client understands the instructions provided. This step ensures that the client’s actions are not due to a knowledge deficit or misunderstandings about the treatment plan, helping the nurse select the most accurate and appropriate nursing diagnosis.
Rationale for correct answer:
A. Whether the client received adequate teaching related to her medication and expresses an understanding of that teaching:
Assessing the client's understanding is the first priority before concluding noncompliance. If the adolescent lacks proper education about the purpose and benefits of her medications, her behavior may reflect a knowledge deficit rather than willful nonadherence. Education should address fears about weight gain and needle marks to promote informed, autonomous self-care.
Rationale for incorrect answers:
B. Whether the client was encouraged to skip her medication by a family member or friend:
Peer or family influence is important but is not the first concern when evaluating the reason for nonadherence. The nurse must first establish whether the client understands why the medication is needed and how to manage her fears or misconceptions.
C. Whether the client is old enough to understand the consequences of her actions:
At 15 years old, the adolescent likely has the cognitive ability to understand the consequences of her actions. The primary concern is whether she has received developmentally appropriate education about her condition and medications.
D. Whether the provider will write another prescription because the client refused to take the medication the first time:
Obtaining a new prescription is a separate concern and does not address the client’s understanding or the reasons behind her decision to skip medications. The nurse should focus on resolving the underlying barriers to adherence.
Take-home points:
- Assessing the client’s understanding of their medication is essential before concluding noncompliance.
- Knowledge deficits must be addressed before evaluating external influences or cognitive ability.
- Nonadherence may stem from fear or misconceptions that education can help resolve.
Which factor is most important for the nurse to assess when evaluating the effectiveness of a client’s drug therapy?
Explanation
When evaluating the effectiveness of a client’s drug therapy, the nurse assesses for evidence of therapeutic benefit from the medication. This involves comparing the client’s current condition to expected outcomes to determine whether the drug has achieved its intended effect. If the medication is effective, the client should show improvement in symptoms or lab values as planned in the therapeutic goals.
Rationale for correct answer:
D. Evidence of therapeutic benefit from the medication:
The most critical factor in determining drug therapy effectiveness is whether the medication achieves its intended health outcomes. This includes symptom relief, improvement in lab values, or stabilization of a chronic condition. Without evidence of benefit, therapy may need adjustment regardless of compliance or satisfaction.
Rationale for incorrect answers:
A. The client’s promise to comply with drug therapy:
While compliance is critical to the success of drug therapy, the nurse must assess whether the medication is actually producing the desired physiological or clinical effects, beyond the client’s intention to adhere.
B. The client’s satisfaction with the drug:
Client satisfaction can improve adherence but does not directly reflect whether the drug is effectively treating the condition. A satisfied client might still experience no therapeutic benefit.
C. The cost of the medication:
Although affordability affects access and adherence to treatment, the primary focus when evaluating effectiveness is the medication's actual therapeutic impact on the client’s health status.
Take-home points:
- Therapeutic benefit is the primary indicator of drug therapy effectiveness.
- Client satisfaction and compliance are important but secondary to clinical outcomes.
- Cost impacts adherence but does not measure the drug’s physiological effect.
Which method may offer the best opportunity for client teaching?
Explanation
An effective method for client teaching during pharmacotherapy is to provide education each time medications are administered. This approach allows for frequent, consistent reinforcement of key concepts about drug purpose, administration, and potential side effects. Repeated teaching moments help improve client understanding, promote medication adherence, and create opportunities for the nurse to assess and clarify the client’s knowledge.
Rationale for correct answer:
D. Providing education about the client’s medications each time the nurse administers the drugs:
This approach integrates teaching into daily care, reinforcing learning through repetition. By linking the medication to its purpose and potential side effects during administration, the nurse provides practical, context-specific education when the client is most attentive.
Rationale for incorrect answers:
A. Providing detailed written information when the client is discharged:
Written information is helpful for reference but may be overwhelming at discharge when the client is focused on leaving the facility. The effectiveness of learning is reduced without verbal reinforcement or opportunities to ask questions.
B. Providing the client with Internet links to conduct research on drugs:
Internet resources can supplement learning, but they require the client to independently seek out information. The nurse’s direct teaching ensures accurate, personalized explanations and provides immediate clarification of misunderstandings.
C. Referring the client to external health care groups that provide client education, such as the American Heart Association:
External resources are valuable for ongoing support but should not replace bedside teaching. Nurses play a key role in providing timely and tailored education that addresses the client’s immediate learning needs during hospitalization.
Take-home points:
- Teaching during medication administration provides timely, relevant learning opportunities.
- Written information and internet links are helpful but less effective without interactive teaching.
- Ongoing nurse-client discussions reinforce medication understanding and safe use.
During the evaluation phase of drug administration, the nurse completes which responsibilities?
Explanation
The evaluation phase of drug administration involves assessing whether the medication has achieved the desired therapeutic outcomes and monitoring for any adverse effects. During this phase, the nurse compares the client’s current health status to the expected outcomes and determines if adjustments to the medication regimen are needed. Continuous evaluation helps ensure medication safety, therapeutic effectiveness, and early detection of potential complications.
Rationale for correct answer:
C. Monitors the client for therapeutic and adverse effects:
This responsibility falls within the evaluation phase, where the nurse determines whether the medication achieved the desired effects and identifies any harmful reactions. This assessment informs decisions on continuing, adjusting, or discontinuing therapy.
Rationale for incorrect answers:
A. Prepares and administers drugs correctly:
This responsibility occurs during the implementation phase of the nursing process, when the nurse carries out interventions, including safe medication administration. It does not reflect the evaluation phase.
B. Establishes goals and outcome criteria related to drug therapy:
Goal setting and establishing outcome criteria are part of the planning phase, where the nurse collaborates with the client to develop measurable goals related to drug therapy outcomes.
D. Gathers data in a drug and dietary history:
Collecting a medication and dietary history is part of the assessment phase. This step helps establish a baseline for planning drug therapy but is not part of evaluating drug effectiveness.
Take-home points:
- Evaluation focuses on monitoring therapeutic benefits and adverse effects after drug administration.
- Drug preparation and administration are part of the implementation phase, not evaluation.
- Gathering histories and setting goals belong to the assessment and planning phases, respectively.
What is the nurse evaluating during the evaluation step of the nursing process?
Explanation
During the evaluation step of the nursing process, the nurse assesses whether the outcome statement has been achieved. This involves comparing the client’s actual response to the expected therapeutic goals outlined during the planning phase. By evaluating the client’s progress toward the outcome, the nurse determines the effectiveness of nursing interventions and decides if the care plan requires continuation, modification, or revision.
Rationale for correct answer:
C. The outcome statement:
During evaluation, the nurse determines if the client has met the established outcomes. This step assesses whether the client’s condition has improved, remained the same, or worsened based on the goals set during the planning phase.
Rationale for incorrect answers:
A. The nursing diagnosis:
The nursing diagnosis is determined during the analysis phase of the nursing process. It is not what the nurse evaluates but rather what the nurse uses to guide planning and interventions.
B. The interventions:
Interventions are implemented during the action phase of the nursing process. Although the nurse may reflect on their effectiveness, the primary focus of evaluation is on whether the desired outcomes have been achieved, not on the actions themselves.
D. The medical diagnosis:
The medical diagnosis is outside the scope of nursing evaluation. Physicians establish and update medical diagnoses, while nurses evaluate progress toward nursing-specific outcomes and overall client health goals.
Take-home points:
- The nurse evaluates if the client outcomes set during planning have been met.
- Nursing evaluation focuses on the client's progress, not the interventions or medical diagnosis.
- Outcome statements guide the nurse in determining the success of the care plan.
Arrange the components of the nursing process in the proper order.
Explanation
Correct answer: B→C→E→A→D
(Assessment → Diagnosis → Planning → Implementation → Evaluation)
The nursing process is a systematic, step-by-step approach to delivering safe and effective patient care. The proper order of the components is Assessment, Diagnosis, Planning, Implementation, and Evaluation (ADPIE). Each step builds upon the previous one, guiding nurses from gathering data to evaluating patient outcomes, and ensuring that nursing care is organized, evidence-based, and patient-centered.
Rationale for correct answer:
2. Assessment:
The nurse begins by collecting and analyzing data about the client’s health status. This forms the foundation for all subsequent steps in the nursing process.
3. Diagnosis:
After gathering data, the nurse identifies the client’s actual or potential health problems, forming nursing diagnoses that guide care priorities.
5. Planning:
The nurse develops specific, measurable goals and selects evidence-based interventions tailored to the client’s diagnoses and overall condition.
1. Implementation:
This phase involves carrying out the planned interventions, such as administering medications, providing education, or assisting with activities of daily living.
4. Evaluation:
Finally, the nurse determines whether the client’s goals were met and assesses the effectiveness of the interventions, modifying the care plan as needed.
Take-home points:
- The correct sequence of the nursing process is Assessment, Diagnosis, Planning, Implementation, and Evaluation.
- Assessment gathers client data, and Evaluation determines if outcomes were achieved.
- Each step builds on the previous one to ensure comprehensive, client-centered care.
The nurse applies the nursing process by gathering client information to assess the client using which of the following methods? Select all that apply
Explanation
The nurse applies the nursing process during the assessment phase by systematically gathering client data through multiple approaches. This includes a body systems assessment, a head-to-toe assessment, and the use of structured frameworks such as Gordon’s Functional Health Patterns Model. These methods help the nurse obtain comprehensive subjective and objective data, forming the foundation for identifying health concerns and planning safe, effective nursing care.
Rationale for correct answers:
A. Body systems assessment:
This method organizes assessment findings based on specific physiological systems (e.g., respiratory, cardiovascular). It helps the nurse collect focused data and identify abnormalities efficiently.
B. Head-to-toe assessment:
The head-to-toe approach systematically reviews each body area, ensuring comprehensive data collection. It promotes thorough assessment and reduces the risk of missing significant findings.
E. Gordon’s Functional Health Patterns Model:
This holistic assessment framework organizes client information into patterns of function, such as nutrition, activity, and coping. It promotes a comprehensive understanding of the client’s overall health and life processes.
Rationale for incorrect answers:
C. Critical pathway:
A critical pathway outlines a multidisciplinary plan of care but does not describe a method for gathering assessment data. It is used later to guide interventions and monitor progress.
D. Evidence-based practice:
Evidence-based practice informs nursing interventions and clinical decisions but is not a direct method of assessing client data. It guides care planning and evaluation rather than initial assessment.
Take-home points:
- Client assessment uses structured approaches like body systems, head-to-toe, and Gordon’s Functional Health Patterns.
- Critical pathways and evidence-based practice guide care but are not used for initial data collection.
- Thorough assessment helps form accurate nursing diagnoses and care plans.
The nurse understands it is important to know the difference between a nursing diagnosis and a medical diagnosis because of which factor?
Explanation
A key difference between a nursing diagnosis and a medical diagnosis lies in their focus. A medical diagnosis identifies a specific disease or pathology, such as pneumonia or diabetes. In contrast, a nursing diagnosis describes the client’s response to the illness, such as ineffective airway clearance or risk for unstable blood glucose levels. This distinction allows nurses to focus on holistic, patient-centered care that addresses the client’s physical, emotional, and psychosocial needs.
Rationale for correct answer:
C. The nursing diagnosis refers to how the client is responding to an illness identified in the medical diagnosis:
Nursing diagnoses focus on the human response to health problems. This includes physical, emotional, and psychosocial reactions to medical conditions, guiding nursing-specific care and interventions.
Rationale for incorrect answers:
A. The nursing diagnosis needs to match the medical diagnosis:
The nursing diagnosis does not need to match the medical diagnosis. Instead, it complements the medical diagnosis by focusing on the client’s holistic needs and responses to illness.
B. The nursing diagnosis needs to be approved by the primary health care provider before use:
Nurses independently identify nursing diagnoses based on their assessments and clinical judgment. They do not require approval from the healthcare provider to establish or implement nursing diagnoses.
D. The medical diagnosis refers to how the client is recovering from the illness that the nursing diagnosis has established:
Medical diagnoses identify the disease or condition itself, not the client’s recovery process. Recovery and progress are monitored through nursing evaluations, but the nursing diagnosis does not create the illness.
Take-home points:
- Nursing diagnoses describe the client's responses to medical conditions and guide individualized nursing care.
- Medical diagnoses identify the actual disease or disorder, while nursing diagnoses focus on holistic client needs.
- Nurses independently develop nursing diagnoses based on assessment and clinical judgment.
The use of evidence-based practice to guide the formulation of nursing interventions based on research and clinical expertise is part of which component of the nursing process?
Explanation
In the Planning phase of the nursing process, the nurse applies evidence-based practice to select appropriate interventions that are supported by current research and clinical expertise. This ensures that the planned nursing actions are scientifically sound, tailored to the patient’s needs, and designed to achieve safe, effective therapeutic outcomes. Evidence-based interventions help improve patient care quality and promote optimal health results.
Rationale for correct answer:
A. Planning:
During the planning phase, the nurse selects interventions that are supported by evidence-based practice. These interventions aim to achieve the desired outcomes and are chosen based on clinical guidelines, scientific research, and the nurse’s expertise.
Rationale for incorrect answers:
B. Assessment:
The assessment phase involves collecting client data to understand their health status. Although evidence-based tools may be used during assessment, this phase does not focus on selecting interventions.
C. Evaluation:
Evaluation is the process of determining whether the planned interventions achieved the desired client outcomes. While evidence-based criteria may be used to assess success, the formulation of interventions happens earlier in the planning stage.
D. Nursing diagnosis:
Nursing diagnosis involves analyzing the assessment data to identify the client’s health problems and responses. It guides the planning phase but does not involve selecting specific evidence-based interventions.
Take-home points:
- Evidence-based nursing interventions are selected during the planning phase to achieve desired client outcomes.
- The planning phase integrates clinical expertise, client needs, and scientific evidence to guide care.
- Assessment, diagnosis, and evaluation inform or follow planning but do not involve selecting interventions.
Nurses need to use the nursing process to provide quality client care. Using the parts of the nursing process of goal planning and creating an outcome statement, as well as writing interventions, mark an X under the column to identify which statement is a nursing intervention and which is an outcome statement.
Explanation
Rationale for correct answer:
In the Planning phase of the nursing process, nurses differentiate between outcome statements and nursing interventions. An outcome statement describes the desired result or goal that the patient will achieve, often written as SMART goals. A nursing intervention outlines the specific actions the nurse will take to help the patient meet that outcome. During planning, the nurse creates both components, ensuring that each intervention supports the achievement of the outcome.
Monitoring for potential complications
This is a nursing intervention because it involves the nurse actively observing and assessing the client for any signs of developing problems in order to prevent deterioration or manage risks early.
Changes observed in the client behavior
This is an outcome statement as it reflects how the client responds to nursing care over time, and it helps the nurse determine whether the intended health goals are being met.
Specific actions to be performed
These are nursing interventions—concrete, nurse-initiated steps taken to achieve the client’s care goals, such as administering medication, turning the patient, or teaching about diet.
Prioritized goals to be identified
This is part of the outcome planning process, where the nurse determines what improvements or targets are most important for the client to achieve during the course of care.
Expected responses to be observed
This is an outcome statement because it defines the anticipated results of nursing interventions—such as stable vital signs or pain reduction—that indicate progress toward recovery.
Take-home points:
- Nursing interventions describe what the nurse will do to help the client achieve goals, such as monitoring or performing actions.
- Outcome statements describe expected client responses or changes that result from nursing care.
- Outcome planning involves setting measurable goals that reflect the client’s health improvements or behavioral changes.
When the nurse decides that the client needs to rest before ambulating, the decision is based on what factor?
Explanation
When the nurse determines that the client should rest before ambulating, the decision reflects the prioritization of physiologic needs, an essential part of clinical judgment. According to Maslow’s hierarchy of needs, physiologic needs such as rest, oxygenation, and energy conservation take priority over activities like ambulation. In the nursing process, this decision occurs during the Planning phase, where the nurse sets priorities to promote patient safety and optimal recovery.
Rationale for correct answer:
C. The prioritization of physiologic needs:
Physiologic needs, such as rest and oxygenation, form the foundation of Maslow’s hierarchy and are prioritized before activities like ambulation. Ensuring the client is rested prevents fatigue, falls, or other complications.
Rationale for incorrect answers:
A. The client’s wishes:
While client preferences are important in planning care, the nurse’s clinical judgment must prioritize safety and physical needs. If ambulation would cause harm due to fatigue, physiologic needs take precedence.
B. The family’s influences:
Family input is valuable but secondary to the client’s immediate physiological condition. The nurse uses clinical assessment to determine if the client is physically ready for activity.
D. The healthcare provider’s orders:
Healthcare provider’s orders may provide activity guidelines, but nurses are responsible for assessing the client’s readiness before performing an activity. Clinical decisions should adjust to the client’s current physiologic state.
Take-home points:
- Physiologic needs such as rest and safety must be prioritized before activities like ambulation.
- Nurses use clinical judgment to assess readiness for activity, even when orders allow ambulation.
- Client and family preferences are considered but do not override immediate physical safety concerns.
The nurse understands that the actions the nurse takes can be determined to be from various sources. For each nursing action indicate with an X whether it is a dependent, an interdependent, or an independent action.
Explanation
In nursing practice, actions are categorized as independent, dependent, or interdependent, reflecting the nurse’s scope of practice and collaboration with the healthcare team. Independent actions are nursing interventions initiated without a provider’s order, such as teaching or repositioning. Dependent actions require a healthcare provider’s prescription, such as administering medications. Interdependent actions involve collaboration with other disciplines, like coordinating physical therapy.
Rationale for correct answer:
Administering medications
This is a dependent nursing action because it requires a prescription or order from a licensed healthcare provider. Nurses carry out the administration, but they do not independently choose the medication.
Educating a client on discharge medications
This is an independent action within the nurse’s scope of practice. Nurses can independently provide teaching on medication usage, timing, and side effects to ensure client understanding and promote safe self-care after discharge.
Documenting the client’s response to a medication
This is an independent nursing action since nurses are responsible for observing, recording, and reporting client outcomes related to medications. It is a critical part of ongoing clinical assessment and care evaluation.
Consulting the pharmacist about a medication order
This is an interdependent action involving collaboration between the nurse and pharmacist. Nurses consult pharmacists to clarify, verify, or adjust medication orders to ensure safe and accurate drug administration.
Discussing with the healthcare provider the client’s medication change request
This is also an interdependent action, requiring collaborative communication with the provider. Nurses advocate for client concerns and help ensure that care decisions reflect client needs while staying within legal practice boundaries.
Take-home points:
- Dependent actions require a provider’s prescription, while independent actions fall within the nurse’s autonomous scope.
- Interdependent actions involve collaboration with healthcare team members like providers or pharmacists.
- Nurses independently educate and document, but consult and medication administration rely on orders or teamwork.
Match the step of the nursing process with the actions of the nurse.
|
NURSING PROCESS |
NURSING ACTIONS |
|
Assessment |
dropdown
|
|
Diagnosis |
dropdown
|
|
Planning |
dropdown
|
|
Interventions |
dropdown
|
|
Evaluation |
dropdown
|
Explanation
The nursing process is a systematic, patient-centered framework used to deliver safe and effective care. It consists of five steps: Assessment, where the nurse collects and analyzes patient data; Diagnosis, identifying actual or potential patient responses to health problems; Planning, setting measurable goals and selecting interventions; Implementation, performing the planned nursing actions; and Evaluation, determining whether the patient goals were met and revising the care plan as needed.
Rationale for correct answer:
Assessment → Take a drug history
In the assessment phase, nurses gather comprehensive information, including a detailed drug history. This helps identify current medications, potential interactions, allergies, and baseline client data essential for safe care.
Diagnosis → Analysis of the client data to determine client need
During diagnosis, the nurse critically analyzes assessment data to identify actual or potential health issues, including medication-related problems. This guides formulation of appropriate nursing diagnoses to direct care.
Planning → Determine client education needed for medication side effects
In the planning phase, nurses set goals and choose appropriate actions, including teaching the client about possible side effects. This ensures the client is informed, safe, and prepared to manage their medications after discharge.
Interventions → Identify the client and administer medications
This step involves executing planned nursing actions, such as correctly identifying the client using two identifiers and safely administering medications according to standards and provider orders.
Evaluation → Identify the therapeutic intent of the medication
In evaluation, the nurse determines whether the expected outcomes of medication therapy have been achieved. Understanding the therapeutic intent helps assess if the medication is effective or if adjustments are needed.
Take-home points:
- Assessment involves collecting data like drug history to form the foundation of the care plan.
- Planning includes determining client education needs, while interventions involve safely administering medications.
- Evaluation focuses on assessing the medication’s therapeutic intent to determine if goals are met.
Exams on The Nursing Process In Pharmacology
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
- Define the nursing process in pharmacology and its purpose in medication safety.
- Identify key components of patient assessment before and during pharmacotherapy.
- Formulate common nursing diagnoses related to medication management.
- Establish SMART pharmacologic goals and patient-centered outcomes.
- Describe safe medication administration and patient education strategies.
- Monitor and evaluate therapeutic effects and adverse drug reactions.
- Apply the nursing process dynamically across diverse populations.
- Emphasize critical thinking, collaboration, and documentation in pharmacologic care.
Introduction
- Purpose and Scope: The nursing process in pharmacology provides a structured, evidence-based pathway for nurses to deliver safe and effective medication therapy. It integrates critical thinking, clinical reasoning, and creativity to translate patient data into sound pharmacologic decisions.
- ADPIE is Dynamic, Not Linear: Although taught in steps, Assessment, Diagnosis, Planning, Implementation, and Evaluation continually overlap and inform one another. For example, when evaluating an analgesic’s effect, the nurse simultaneously conducts a focused reassessment of pain and side effects to refine the plan.
- Interdisciplinary Nature: Pharmacotherapy is an interdisciplinary effort; nurses coordinate with prescribers, pharmacists, and therapists to mitigate risks (e.g., drug interactions), remove barriers (e.g., cost, access), and support adherence.
- Patient-Centeredness: At each phase, the nurse ensures care is individualized, culturally respectful, and aligned with patient priorities and readiness to learn.
- Medication Safety Emphasis: Because drug therapy carries inherent risks, the nursing process anchors medication safety, patient education, and outcome monitoring as core responsibilities of nursing practice.
Phases Of The Nursing Process
Assessment Phase
Purpose:
- The assessment phase systematically collects, organizes, validates, and documents patient data to form a safe, individualized pharmacotherapy plan. Data collection starts at first contact and continues at every encounter, ensuring current decisions reflect current patient status.
Key Components:
- Health History (Subjective Data):
- Allergies and Hypersensitivities: The nurse identifies drug, food, and environmental allergies and explicitly documents the reaction (e.g., “hives and wheeze to amoxicillin,” not simply “penicillin allergy”), because reaction type guides risk.
- Prescription and OTC Medications: The nurse collects the drug name, dose, route, time/frequency, indication, and duration for all current medications, including recently discontinued ones that may still affect physiology.
- Herbal/Dietary Supplements: The nurse asks specifically about herbals, nutraceuticals, and vitamins, because these can interact with prescribed drugs or alter labs.
- Past Medical History and Prior Adverse Drug Reactions: The nurse explores chronic illnesses (e.g., hepatic/renal disease, cardiac conditions) and documented ADRs to predict altered pharmacokinetics or sensitivities.
- Personal and Social History: The nurse assesses alcohol, tobacco, caffeine, and illicit substances that can induce/inhibit metabolism, complicate adherence, or increase risk.
- Reproductive Health: For patients of child-bearing potential, the nurse clarifies pregnancy intent/status and lactation, since both require risk–benefit analysis and possibly alternative therapies.
- Family History and Pharmacogenetics: The nurse screens for family responses to medications (e.g., atypical anesthetic response) that may hint at genetic metabolizer variants.
- Access, Cost, and Logistics: The nurse identifies insurance coverage, medication affordability, transportation, and pharmacy access, which frequently determine adherence.
- Physical Assessment (Objective Data):
- The nurse obtains baseline vital signs and focused system exams relevant to the medication (e.g., apical heart rate before beta-blockers, respiratory rate before opioids).
- The nurse records height, weight, and BMI—especially crucial for weight-based dosing (pediatrics) and renal dosing (older adults).
- The nurse reviews baseline laboratory data such as renal function (BUN/creatinine), hepatic enzymes (AST/ALT), electrolytes (Na⁺, K⁺, Ca²⁺, Mg²⁺), and therapeutic drug levels when applicable, because these direct dosing and monitor toxicity.
- Ongoing Assessment During Pharmacotherapy:
- The nurse tracks therapeutic response (e.g., trending BP after antihypertensives, fever curve and WBC after antibiotics) using consistent measures and timing.
- The nurse detects adverse effects and toxicity (e.g., sedation after opioids, bleeding after anticoagulants) and correlates findings with peak/trough times where relevant.
- The nurse assesses adherence and self-administration capacity (cognition, dexterity, vision/hearing, numeracy), because even the “right drug” fails if the patient cannot self-manage.
- The nurse validates patient perceptions of effects, because subjective changes (e.g., dizziness, palpitations) often precede objective derangements.
- Critical Thinking in Assessment:
- The nurse compares baseline to current data, seeking trends (improving, stable, worsening) that influence dosing intervals and escalation/de-escalation decisions.
- The nurse reconciles discrepancies between reports and findings (e.g., “no pain” while grimacing or guarding), using clarifying questions and objective measures to avoid error.
- The nurse anticipates population-specific variations (e.g., reduced renal function in older adults) and pre-emptively adjusts monitoring.
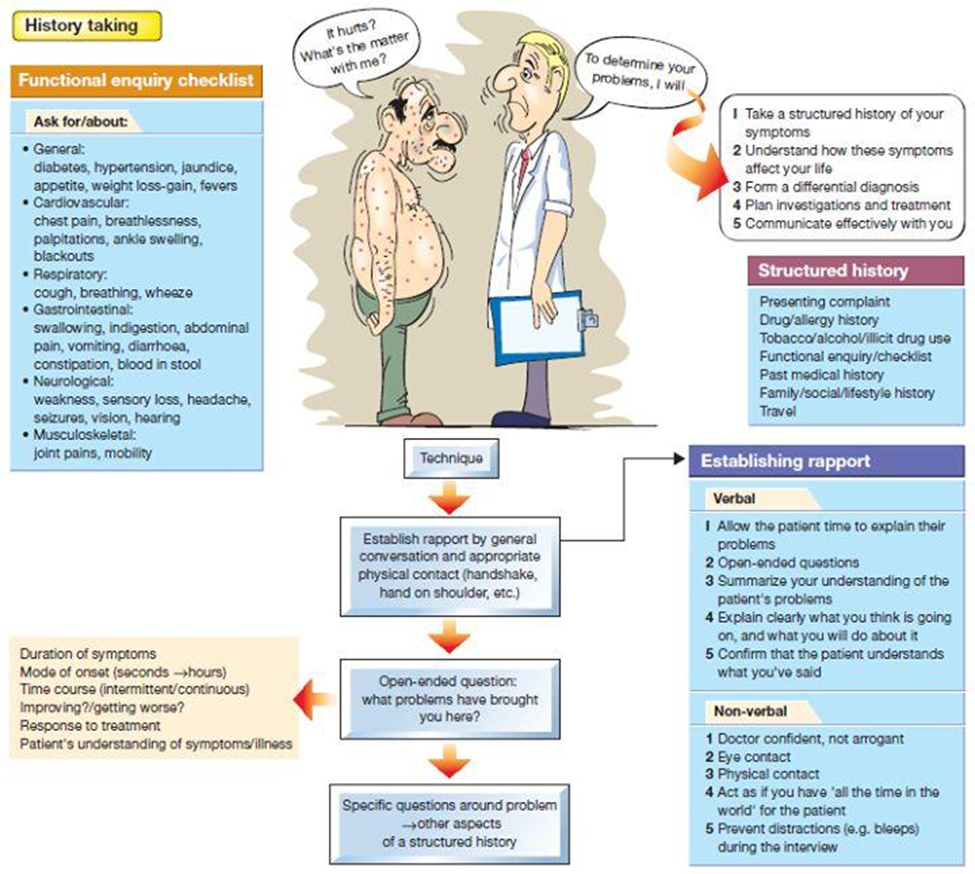
Structured Assessment Questions
- Chief Complaint: “How do you feel today?” “Are you having pain, nausea, dizziness, palpitations, shortness of breath, itching, headache, or fatigue?”
- Allergies: “Are you allergic to any medications, foods, tape/cleansers, or environmental triggers? What happens when you are exposed?”
- Past Medical History: “Do you have diabetes, heart/lung/neurologic/dermatologic conditions? How are these treated now?”
- Family History: “Has anyone in your family had unusual problems with medications or anesthesia?”
- Drug History: “List all prescription and OTC drugs you take (name/dose/frequency). Have you taken any new or stopped any meds in the last 2 months? Any side effects?”
- Herbal/Supplements: “Do you use any herbals, homeopathic remedies, or vitamins?”
- Health Management: “Who are your providers? What is your usual diet and sleep pattern?”
- Reproductive: “Is there any chance you are pregnant? Are you currently breastfeeding?”
- Personal–Social: “Do you smoke, drink alcohol, or use caffeine? Do you use street drugs? What is your occupation and schedule? Any cultural or religious practices that affect medications? Any concerns about cost or coverage?”
- Health Risks: “Any history of depression or other mental health conditions?”
Nursing Insights:
- What is unsaid matters. Nonverbal cues (e.g., guarding, facial grimace) can contradict verbal reports and must be reconciled.
- Storage and safety planning are part of assessment. The nurse determines if home storage, child safety, refrigeration, or sharps disposal considerations are required.
- Readiness to learn is assessed by exploring health literacy, numeracy, preferred language, and sensory needs, which drive how the nurse will teach.
Diagnosis Phase
Definition and Focus:
- A nursing diagnosis is a clinical judgment about individual, family, or community responses to actual or potential health/life processes. In pharmacology, diagnoses promote therapeutic effects, minimize adverse effects/toxicity, and maximize self-care capacity.
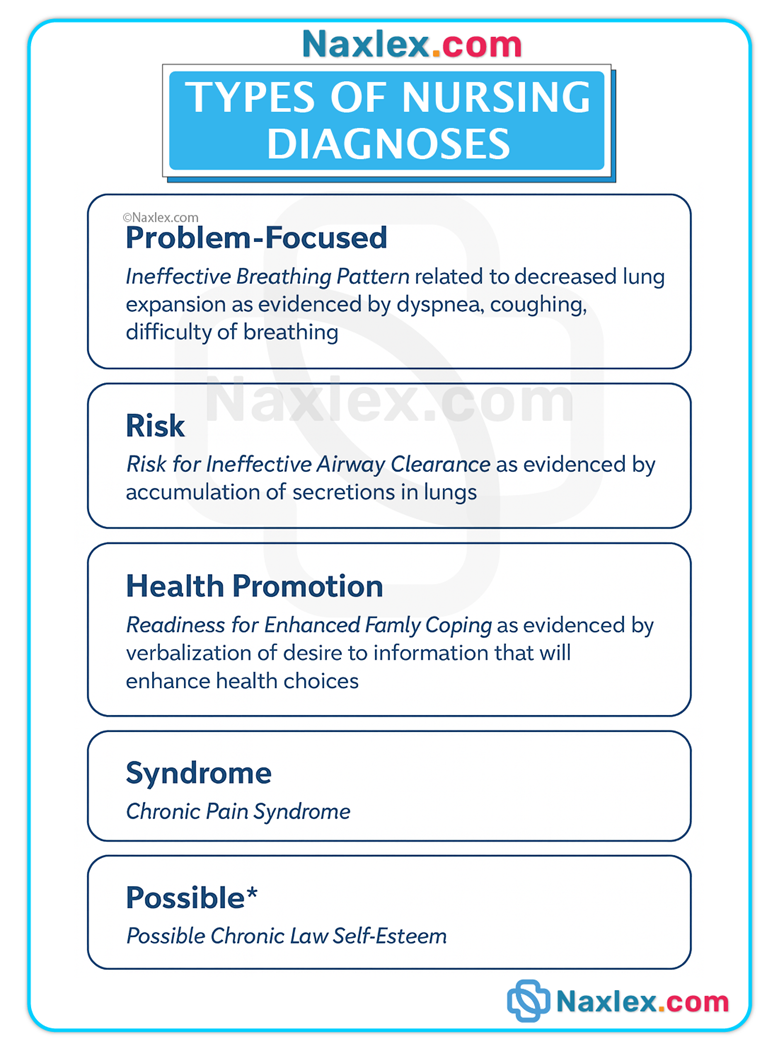
Structure of Nursing Diagnoses:
- One-part (Wellness): e.g., Readiness for Enhanced Self-Health Management related to new understanding of insulin use.
- Two-part (Risk): e.g., Risk for Injury related to sedative effects of benzodiazepines.
- Three-part (Actual—PES format): Problem related to Etiology as evidenced by Signs/Symptoms; e.g., Deficient Knowledge related to new anticoagulant prescription as evidenced by patient incorrectly stating dose and food interactions.
Common Nursing Diagnoses in Pharmacology
- Deficient Knowledge: The patient lacks essential information about purpose, dose, timing, interactions, or side effects, which can lead to misuse or harm.
- Noncompliance (Nonadherence): The patient chooses not to follow the regimen after adequate education; the nurse explores barriers (cost, beliefs, side effects, complexity).
- Risk for Injury/Falls: Medications that lower BP, impair cognition, or cause hypoglycemia increase injury risk requiring fall precautions and monitoring.
- Pain / Acute Pain / Chronic Pain: Pharmacologic and nonpharmacologic strategies are coordinated to relieve pain while minimizing opioid adverse effects.
- Nausea/Diarrhea/Constipation: The nurse anticipates GI effects from antibiotics, opioids, iron, or chemo and plans prophylaxis and monitoring.
- Impaired Gas Exchange / Ineffective Breathing Pattern: Sedatives/opioids may depress respiration, requiring close respiratory assessment.
- Ineffective Therapeutic Regimen Management: The regimen is too complex or poorly integrated into daily life; simplification and supports are needed.
- Risk for Infection: Immunosuppressants or steroids raise infection risk; the nurse reinforces hygiene and monitoring.
- Impaired Skin Integrity / Risk for Bleeding: Anticoagulants and steroids increase bruising/bleeding; injections and skin care require precautions.
- Impaired Swallowing / Imbalanced Nutrition: Dysphagia or anorexia from meds may limit safe oral dosing and nutritional intake.
- Risk for Impaired Liver Function / Urinary Retention / Excess/Deficient Fluid Volume: Hepatotoxic or anticholinergic drugs necessitate organ-system surveillance.
- (Additional NANDA-I diagnoses such as Anxiety, Fatigue, Sleep Disturbance, Impaired Thermoregulation, Ineffective Health Maintenance, Risk for Suicide, etc., are selected when supported by the assessment and medication profile.)
Nursing Focus:
- Patient-centered needs drive diagnosis selection; the nurse avoids making the medication the “problem” and instead articulates the patient’s response to therapy.
- Interprofessional collaboration is initiated for multidisciplinary problems (e.g., pharmacist consult for polypharmacy; social worker for affordability).
Nursing Insights:
- Avoid assumptions. Validate diagnoses with robust data.
- Co-create priorities with the patient, which improves engagement and adherence.
- Revise diagnoses as clinical status, labs, and responses evolve.
Planning Phase
Purpose:
- The planning phase prioritizes diagnoses, establishes SMART goals, and selects interventions that ensure safe, effective medication use and informed self-care.
Goal Types:
- Short-Term Goals provide near-term targets (e.g., “Patient will report pain ≤3/10 within 60 minutes of oral analgesic”).
- Long-Term Goals emphasize sustained self-management (e.g., “Patient will demonstrate accurate insulin self-administration and hypoglycemia management within 72 hours”).
SMART Outcomes (with medication focus):
- Outcomes clearly specify who does what, under what conditions, to what standard, and by when (e.g., “Patient will name warfarin indication, dose, timing, and 3 foods high in vitamin K by discharge tomorrow.”).
- Outcomes also include safety parameters (e.g., “Patient will verbalize when to hold metoprolol (HR < 60 bpm) and notify provider today.”).
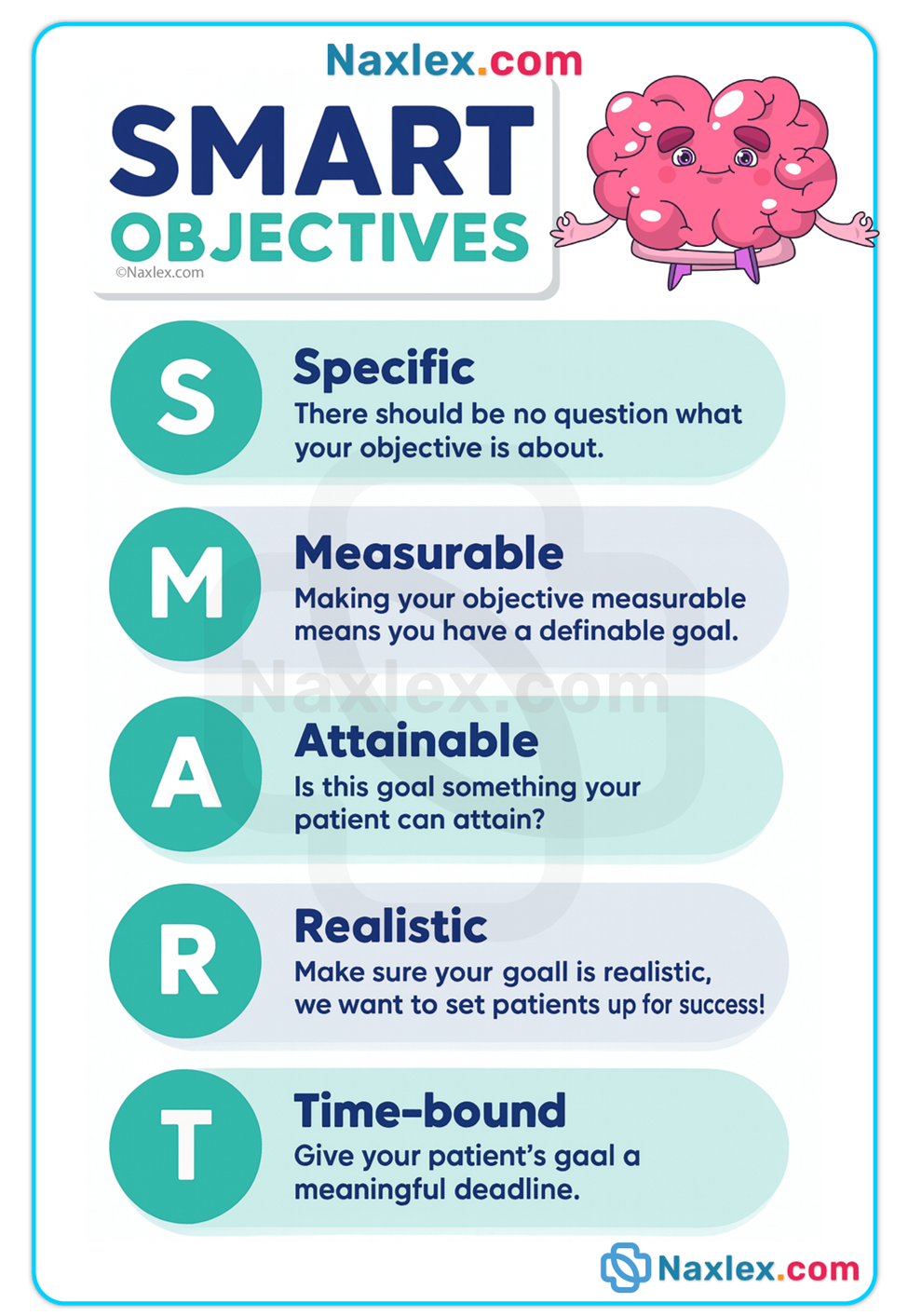
Pharmacotherapy Planning Priorities:
- Therapeutic Targets: The nurse sets measurable endpoints (e.g., SBP 120–140; afebrile 24 hours; trough within range).
- Adverse-Effect Prevention: The nurse anticipates predictable side effects and embeds prophylaxis (e.g., stool softener with opioids).
- Patient Education Plan: The nurse designs tailored teaching (preferred language, legible handouts, teach-back) and return-demonstrations (e.g., eyedrops, inhaler use).
- Monitoring Plan: The nurse schedules focused reassessments (e.g., pain at 30–60 minutes post-dose; BP before/after new antihypertensive) and lab intervals (e.g., renal panel after ACE inhibitor initiation).
- Safety Parameters/Orders: The nurse clarifies hold parameters (e.g., anticoagulant with platelet count thresholds), rescue medications, and when to escalate (e.g., persistent RR < 10/min).
Examples of Planning by Drug Class:
- Antibiotics: Emphasize full course completion, track fever and WBC trends, and teach signs of C. difficile to report promptly.
- Anticoagulants: Plan bleeding precautions, drug–diet education (vitamin K with warfarin), and lab monitoring as ordered; include fall prevention.
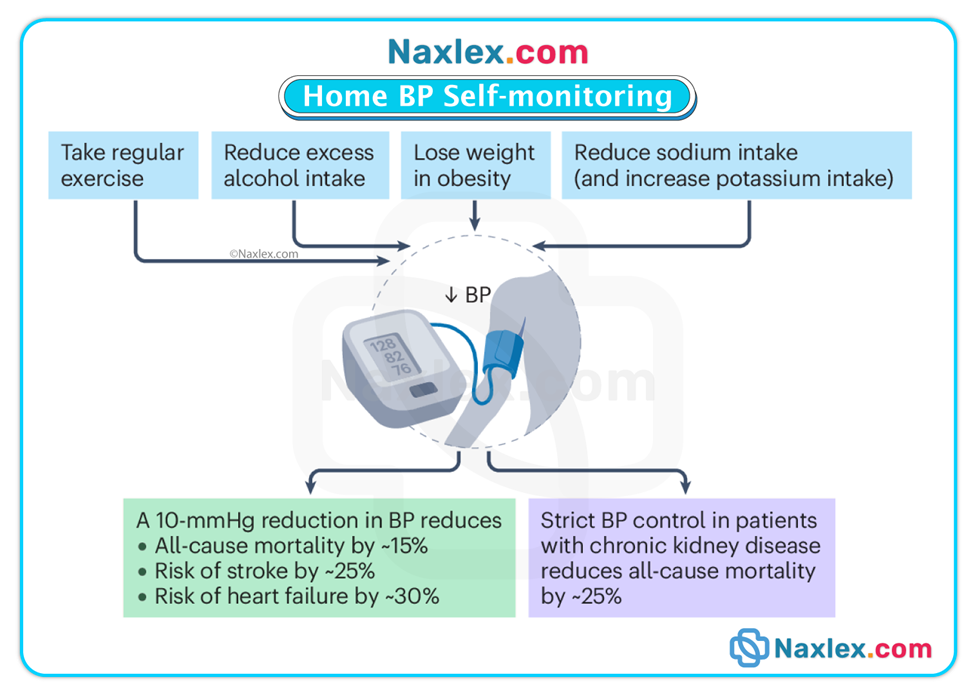
- Antihypertensives: Include orthostatic BP precautions, daily weights if diuretics are used, and home BP self-monitoring technique.
- Insulin/Antidiabetics: Schedule glucose checks, hypoglycemia teaching, and meal–med timing to align peak actions with food intake.
- Inhaled Therapies: Plan bronchodilator before corticosteroid, mouth rinse after steroid, and spacer use if indicated.
Collaboration and Prioritization:
- The nurse includes the patient/caregiver in goal setting to align with values and capacity.
- High-risk issues (airway/breathing/circulation, severe reactions) take priority over less urgent teaching topics.
Nursing Insights:
- Time medication around activities/food to optimize absorption and minimize adverse effects.
- Anticipate barriers (cost, transport, memory) and pre-plan supports (90-day fills, pill organizers, alarms).
Implementation Phase
Purpose:
- Implementation is the action phase, where the nurse gives medications safely, monitors responses, prevents complications, and teaches continuously to build self-management capacity.
Safe Administration—Core Actions:
- The nurse follows the 6 Rights of Medication Administration—right patient, right drug, right dose, right route, right time, and right documentation—and many institutions extend these with right reason/indication, right response/evaluation, right education, and the patient’s right to refuse.
-
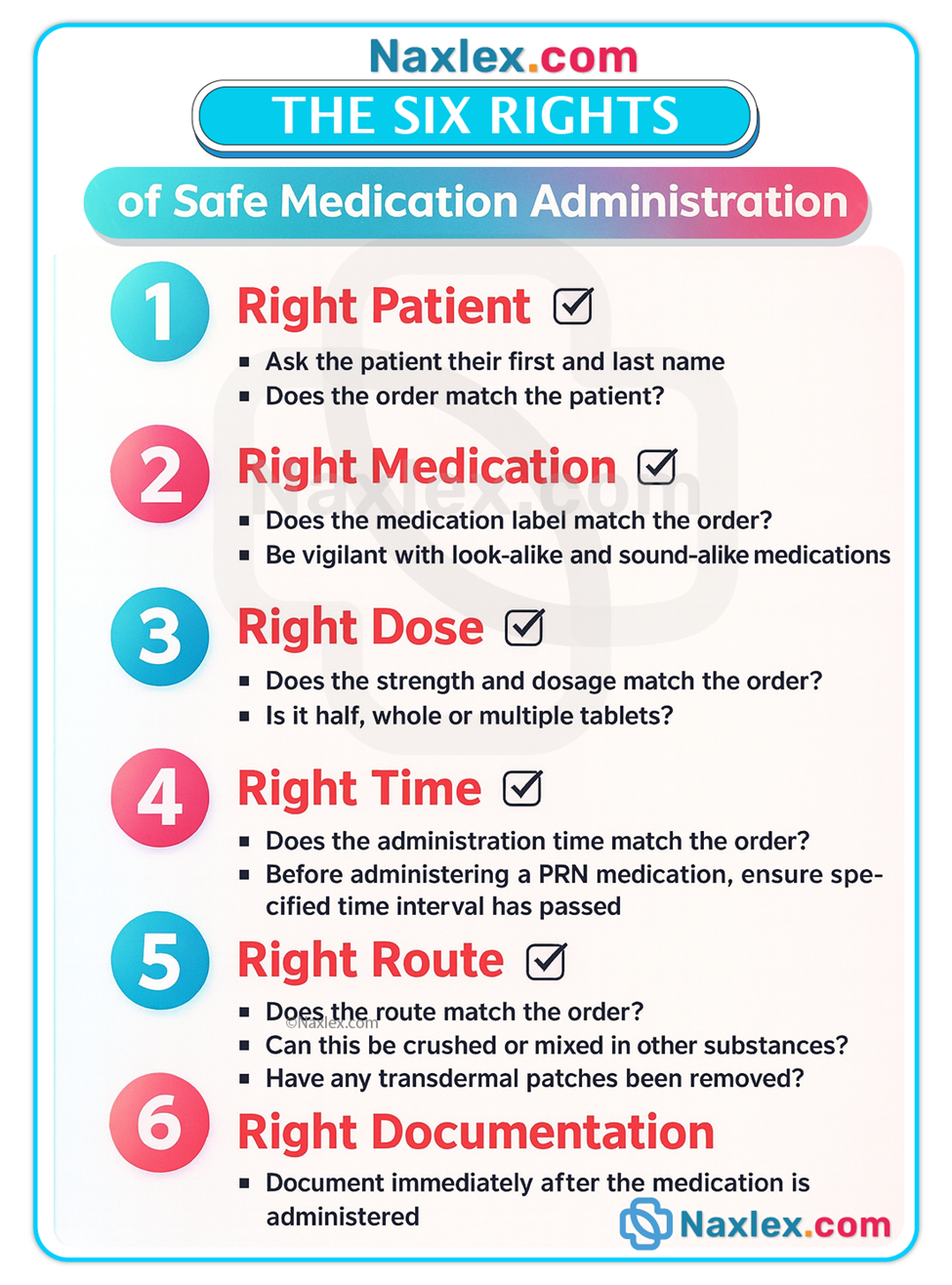
- Pre-administration verification includes checking allergies, indication, vital signs/labs (e.g., apical HR for digoxin, K⁺ for diuretics), and compatibilities for IV medications.
- High-alert medications (e.g., insulin, anticoagulants, chemotherapy, concentrated electrolytes) often require independent double-checks and smart-pump safeguards; the nurse adheres strictly to local policy.
- The nurse calculates doses carefully, uses weight-based dosing when ordered, and clarifies unclear orders before administration.
- The nurse uses bar-code scanning or other verification technologies where available, but still thinks critically and does not bypass alerts without cause.
Monitoring and Response:
- The nurse monitors for therapeutic effect at expected onset/peak and documents objective and subjective responses (e.g., pain score change, BP reduction, improved airflow).
- The nurse surveils for adverse effects and implements safety measures (e.g., fall precautions after first-dose antihypertensive; nausea prophylaxis before chemotherapy).
- The nurse acts promptly for serious reactions (e.g., airway, anaphylaxis protocol) and notifies the provider with concise clinical data.
Patient and Caregiver Education:
- Purpose and Expected Effects: The nurse explains why the medication is prescribed and how success will be measured (“You’ll know lisinopril helps when your home BPs trend toward the target without dizziness or cough.”).
- Side vs. Adverse Effects: The nurse differentiates self-manageable effects (mild nausea, transient flushing) from report-now effects (bleeding, wheeze, swelling, rash).
- Administration Details: The nurse clarifies dose, timing, relation to food, missed-dose protocol, storage, and special techniques (e.g., eyedrops without touching the eye; insulin rotation; inhaler spacing and rinse).
- Interactions and Precautions: The nurse identifies drug–drug and drug–food issues (e.g., NSAIDs with anticoagulants; grapefruit with certain statins) and activity restrictions (e.g., alcohol with CNS depressants).
- Self-Monitoring: The nurse teaches what and when to monitor (e.g., home BP, glucose), how to record, and when to call.
- Teach-Back and Return-Demonstration: The nurse verifies understanding by asking the patient to explain or show the steps back, which reveals learning gaps to address immediately.
- Written Materials: The nurse provides clear, concise, large-print handouts in the patient’s preferred language, aligning with health literacy needs.
Special Populations:
- Pediatrics: The nurse confirms weight-based doses, uses oral syringes, avoids calling medicine “candy,” and involves caregivers with simple, step-wise instructions.
- Older Adults: The nurse screens for polypharmacy, simplifies regimens, uses pill organizers/alarms, and assesses vision/hearing/cognition that may impede adherence.
- Pregnancy/Lactation: The nurse verifies risk–benefit, selects safer alternatives when possible, and times doses to minimize fetal/infant exposure.
Documentation:
- The nurse documents drug name, dose, route, time, site (if parenteral), pre-checks, and patient response (including PRN effectiveness).
- The nurse records adverse effects, refusals, education provided, teach-back results, and provider notifications, ensuring a clear clinical record.
Medication Safety and Quality:
- Medication Reconciliation is performed at every transition of care to detect duplications, omissions, dosing differences, and interactions.
- Event Reporting (non-punitive) is completed for errors or near misses to support system improvement and prevent recurrence.
Evaluation Phase
Purpose:
- Evaluation determines whether goals and outcomes were met and what modifications are required to optimize therapy.
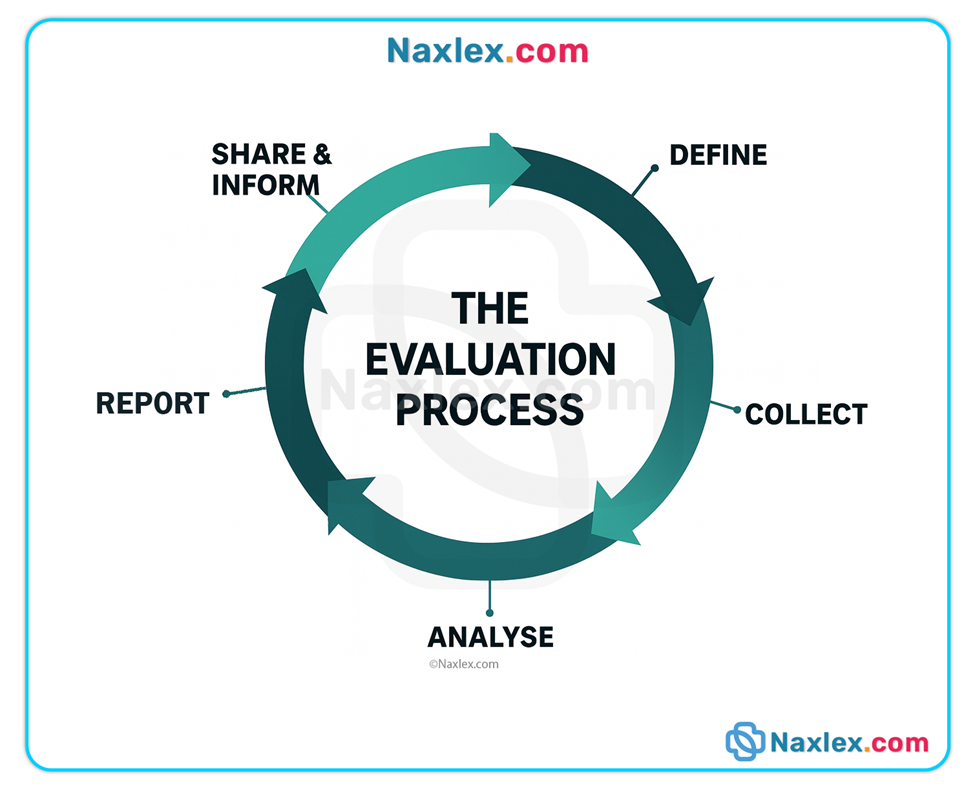
Evaluation Criteria:
- Therapeutic Outcomes: The nurse verifies that the target effect occurred (e.g., pain relief within timeframe, BP reduction to goal, infection signs resolving).
- Safety Outcomes: The nurse assesses whether adverse effects were prevented or minimized, and whether hold parameters and precautions were effective.
- Learning and Self-Care: The nurse confirms the patient can explain and demonstrate medication use and knows when to seek help.
- Adherence and Barriers: The nurse evaluates refill patterns, cost/access issues, regimen complexity, and beliefs that may hinder continued use.
Next Steps:
- If goals are met, the nurse continues the plan and establishes ongoing monitoring intervals.
- If partially met or unmet, the nurse reassesses, revises diagnoses, alters the regimen (after provider consult), or modifies teaching to address the gap.
- Evaluation is continuous; each cycle informs the next, sustaining patient safety and therapeutic success.
Nursing Insights:
- No effect ≠ patient failure. It may indicate dose/timing issues, drug selection mismatch, kinetics changes, or adherence barriers that the nurse can help resolve.
- Every evaluation closes a loop—the nurse returns to reassessment, adjusts the plan, and strengthens the education and safety net.
Application In Pharmacology
Ongoing Process
- The nursing process is cyclical and iterative. Evaluation feeds back into Assessment, prompting updated Diagnosis, revised Planning, and refined Implementation. This constant feedback loop is essential for safe medication use, especially when patient status or regimens change.
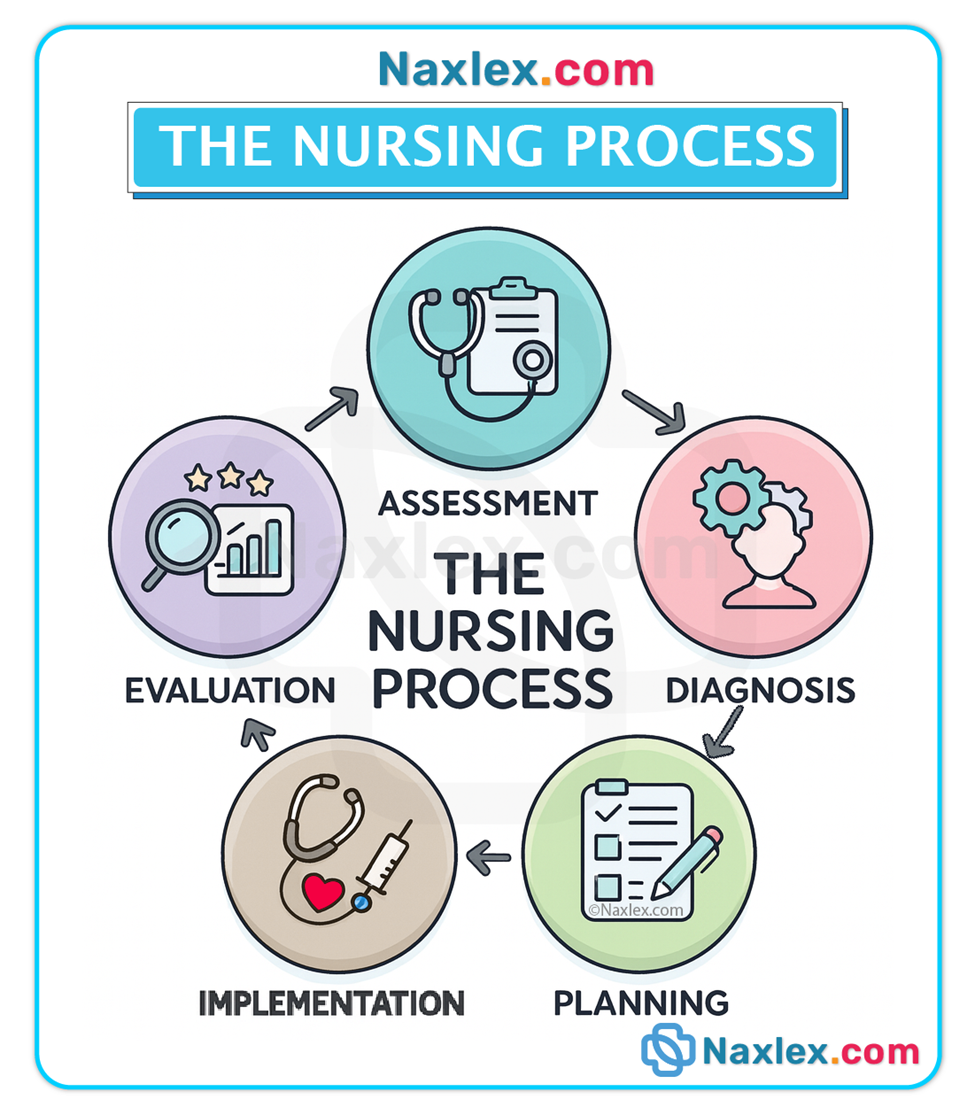
Sample Assessment Questions for Nursing Practice
- Health History (before/during therapy):
- “Are you allergic to any medications, foods, tape, or cleansers—and what exactly happens if you are exposed?”
- “Which prescription and OTC medications are you taking now, including herbals and vitamins? How much, how often, and why do you take each?”
- “Is there any chance you are pregnant or breastfeeding?”
- “Do you use alcohol, tobacco, caffeine, or recreational drugs? How often?”
- “Can you afford your medications and get to the pharmacy? Which pharmacy do you use?”
- Physical Assessment (pre/post dose):
- “What are the baseline vital signs and relevant labs (e.g., creatinine, AST/ALT, electrolytes, drug levels)?”
- “Is the patient at risk for falls due to sedatives, antihypertensives, or hypoglycemics?”
- “Are there signs of adverse effects such as rash, bleeding, respiratory depression, confusion, or diarrhea?”
Expanded Teaching Focus Areas
- Therapeutic Use & Outcomes: The nurse asks, “What is this medication for, and how will you know it’s working?” The patient identifies measurable indicators (e.g., fewer wheezing episodes, BP log trending downward).
- Side & Adverse Effects: The nurse clarifies, “Which effects can you self-manage, and which require a call right away?” The patient distinguishes common, mild effects from serious warning signs (e.g., black stools on anticoagulants).
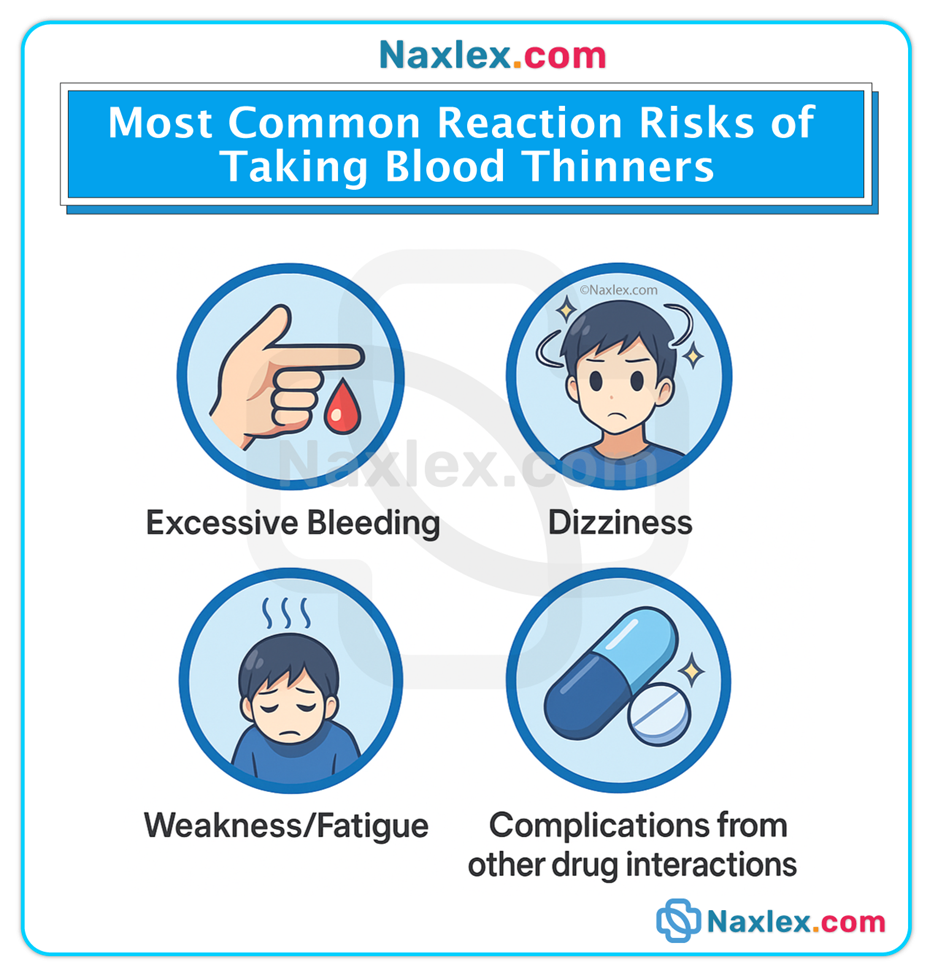

- Medication Administration: The nurse confirms, “How much do you take, how often, and do you take it with food or water?” The patient states and demonstrates the correct technique (e.g., eyedrop placement, SC injection).
- Drug Interactions & Precautions: The nurse reviews, “Are there foods, drinks, or drugs you must avoid?” The patient can name specific restrictions and timing considerations (e.g., spacing antacids from certain meds).
- Self-Monitoring Requirements: The nurse explains, “What do you need to check at home, how will you record it, and when will you call?” The patient engages in BP/glucose monitoring and brings logs to visits.
- Missed-Dose Protocols & Storage: The nurse asks, “What will you do if you miss a dose, and where/how will you store this medication?” The patient states correct steps and storage needs (e.g., refrigeration, away from light).
Key Principles Across All Phases
- Critical Thinking: The nurse synthesizes patient data, drug knowledge, and trends to anticipate problems and adapt promptly.
- Collaboration: The nurse coordinates with prescribers, pharmacists, and social workers to optimize regimens, costs, and supports.
- Patient-Centered Care: The nurse respects patient values, culture, language, and preferences, tailoring teaching and schedules accordingly.
- Safety First: The nurse prevents errors via the 6 Rights, medication reconciliation, independent double-checks for high-alert meds, and timely escalation.
- Documentation: The nurse provides clear, timely, complete records of administration, responses, education, and communications.
The 5 Phases Applied to Pharmacology
- Assessment: The nurse collects a complete medication and allergy history, performs focused exams, and reviews labs to establish baselines and anticipate risk.
- Diagnosis: The nurse identifies medication-related problems (e.g., Deficient Knowledge, Risk for Injury, Ineffective Regimen Management) that nursing interventions can address.
- Planning: The nurse sets SMART goals for therapeutic targets, safety, monitoring, and education, prioritizing high-risk concerns first.
- Implementation: The nurse administers medications safely, monitors therapeutic and adverse responses, and teaches continuously using teach-back and return-demo.
- Evaluation: The nurse determines if outcomes were achieved, identifies barriers, and modifies the plan to improve safety, adherence, and effectiveness.
Summary
- Structured, Patient-Centered Framework: The Nursing Process in Pharmacology (ADPIE) is a systematic, cyclical approach that anchors medication safety and therapeutic effectiveness.
- Assessment: Nurses gather comprehensive subjective and objective data, including complete medication profiles, allergy details, baseline vitals/labs, functional capacity, and learning needs.
- Nursing Diagnosis: Nurses identify actual and potential problems such as Deficient Knowledge, Noncompliance, and Risk for Injury, translating data into actionable nursing priorities.
- Planning: Nurses set SMART, patient-centered goals for medication outcomes, safety precautions, and education, embedding monitoring schedules and hold parameters.
- Implementation: Nurses execute safe medication administration using the 6 Rights, continuously monitor responses, and deliver clear, tailored teaching with teach-back and return-demo.
- Evaluation: Nurses verify therapeutic success, prevent or minimize adverse effects, assess learning and adherence, and revise the plan as needed—closing the loop and beginning the next cycle.
- Safety and Collaboration: Throughout, nurses reconcile medications, document precisely, collaborate across disciplines, and advocate for patients, ensuring that pharmacotherapy remains effective, equitable, and safe.
Clinical Pearls
- Always verify drug allergies with reaction details before administering medications.
- Ask specifically about OTCs, herbals, and supplements; these often go unreported yet can change therapy outcomes.
- Time your reassessments to expected onset/peak for the medication to capture true therapeutic and adverse responses.
- Use teach-back every time you educate about a medication; assume variability in health literacy and tailor accordingly.
- Start low, go slow in older adults; adjust doses to renal/hepatic function and monitor closely for atypical presentations.
- Perform medication reconciliation at every transition of care to prevent duplication, omission, and interactions.
- Document completely: include education given, patient response, refusals, and provider communications; if you didn’t document it, it didn’t happen.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on The Nursing Process In Pharmacology
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


