Please set your exam date
Long-term Respiratory Dysfunction
Study Questions
Practice Exercise 1
Which laboratory result will provide the most important information regarding the respiratory status of a child with an acute asthma exacerbation?
Explanation
Asthma is a chronic respiratory condition that affects the airways in the lungs. In acute asthma exacerbation, airway obstruction and inflammation impair ventilation, leading to hypoxemia and, if severe, hypercapnia.
Rationale for correct answer:
2.ABGis the most important test to assess severity of asthma exacerbation. Early stages of the disease result in ↓ PaO₂, and ↓ PaCO₂ from hyperventilation. Late/severe stages cause ↓ PaO₂, ↑ PaCO₂ from respiratory failure. This provides guidance for oxygen therapy and need for escalation such as intubation.
Rationale for incorrect answers:
1. Complete blood count (CBC)may detect infection or eosinophilia, but it does not evaluate acute respiratory status.
3. Blood urea nitrogen (BUN)reflects kidney function, unrelated to asthma exacerbation.
4. Partial thromboplastin time (PTT)measures clotting time, not respiratory function.
Take home points
- ABGs are crucial in acute asthma to monitor oxygenation and CO₂ retention.
- Pulse oximetry is a quick bedside tool, but ABG confirms severity.
- Rising PaCO₂ in a child with asthma is a red flag for impending respiratory failure.
What is the most important piece of information that the nurse must ask the parent of a child in status asthmaticus?
Explanation
Status asthmaticusis a severe, prolonged asthma attack unresponsive to standard treatment such as inhaled β₂-agonists. It is a medical emergency requiring rapid intervention to prevent respiratory failure.
Rationale for correct answer:
4.Knowing when the child’s last dose of medication was administeredprovides essential, time-sensitive information to guide immediate treatment decisions. It helps avoid duplicating doses too soon and identifies whether medications were ineffective or if the attack worsened despite therapy.
Rationale for incorrect answers:
1. Knowing the last time the child ate is relevant if intubation or sedation might be required (aspiration risk), but not the most urgent information in status asthmaticus.
2. Knowing whether the child has been exposed to any of the usual asthma triggers is useful for long-term prevention and management, but not immediately life-saving during the acute crisis.
3. Asking when the child was last admitted to the hospital for asthma provides background history of severity but does not influence urgent management in the current emergency.
Take home points
- In status asthmaticus, always prioritize immediate treatment-related information (last dose of bronchodilators, steroids, or other meds).
- Exposure history and hospitalization history are important for long-term care, but life-saving interventions come first.
Nurses must gather information that directly impacts safe and effective acute management.
Which statement by the parent of a child using an albuterol inhaler leads the nurse to believe that further education is needed on how to administer the medication?
Explanation
Albuterol is a short-acting beta-agonist (SABA)used as a rescue medication during asthma attacks or before exercise to relax airway smooth muscle and relieve bronchospasm. Proper inhaler technique ensures the drug reaches the lower airways effectively.
Rationale for correct answer:
1. “I should administer two quick puffs of the albuterol inhaler using a spacer.”This is an incorrect technique. Parents should wait at least 1 minute between puffsto allow the first dose to dilate the airways, which helps the second puff penetrate deeper into the lungs. Administering “two quick puffs” without waiting decreases medication effectiveness.
Rationale for incorrect answers:
2. “I should always use a spacer when administering the albuterol inhaler.”Spacers help children coordinate inhalation and maximize delivery of medication to the lungs, reducing deposition in the mouth/throat.
3. “I should be sure that my child is in an upright position when administering the inhaler.”Upright positioning optimizes lung expansion and medication delivery to the lower airways.
4. “I should always shake the inhaler before administering a dose.”Shaking ensures the medication is properly mixed for accurate dosing.
Take home points
- Parents should wait at least 1 minute between puffs of albuterol.
- Using a spacer, upright positioning, and shaking the inhaler are all correct practices.
- Nurses must emphasize step-by-step technique to improve asthma control and avoid ineffective medication use.
Which should the nurse administer to provide quick relief to a child with asthma who is coughing, wheezing, and having difficulty catching her breath?
Explanation
Asthma is a chronic inflammatory airway diseasecharacterized by bronchoconstriction, airway inflammation, and increased mucus production. During acute symptoms such as wheezing, coughing, or shortness of breath, the immediate priority is to relieve bronchospasmand improve airflow.
Rationale for correct answer:
3.Albuterolis ashort-acting bronchodilatorthat works within minutes to provide rapid relief of acute bronchospasm, wheezing, and dyspnea. It is the first-line treatment for an asthma attack.
Rationale for incorrect answers:
1. Prednisoneis a corticosteroid used for longer-term control of inflammation in moderate to severe exacerbations but does not provide immediate relief. It can take several hours to days to be effective.
2. Montelukast (Singulair)is a leukotriene receptor antagonist used for long-term asthma control and prevention, not for acute symptom relief.
4. Fluticasone (Flovent)is an inhaled corticosteroid for daily maintenance therapy to reduce airway inflammation. It does not work quickly enough to treat acute attacks.
Take home points
- Albuterol (SABA) is the go-to rescue medication for acute asthma symptoms.
- Corticosteroids (oral or inhaled) are for long-term inflammation control, not acute relief.
- Montelukast is preventive, not a rescue drug.
- Nurses should teach families the difference between rescue medications used for immediate relief and controller medications used for long-term management.
Which child with asthma should the nurse see first?
Explanation
An asthma exacerbation, also called an asthma attackor flare-up, is a sudden worsening of asthma symptoms due to increased inflammation and narrowing of the airways.
Rationale for correct answer:
3.A 9-year-old who is quiet, pale, wheezing bilaterally with SpO₂ 92%: This child is the most critical. Quietness, hypoxemia, and pallorindicate severe obstruction with reduced air entry, suggesting impending respiratory failure. This requires immediate priority intervention such as oxygen, bronchodilator therapy, and possible escalation to advanced airway support.
Rationale for incorrect answers:
1. A 12-month-old, mild cry, pale, diminished breath sounds, SpO₂ 93%: This is concerning but not the most urgent. Diminished breath sounds are worrisome, but SpO₂ is still slightly higher (93%), and the child still has some cry showing air movement.
2. A 5-year-old, complete sentences, pink, wheezing bilaterally, SpO₂ 93%: This child is stable compared to the others. The ability to speak in complete sentencesand normal color indicate adequate air exchange. Wheezing is expected but not immediately life-threatening.
4. A 16-year-old, short sentences, wheezing, sitting upright, SpO₂ 93%: These symptoms indicate moderate distress, but the child is compensating by sitting upright and still moving air with SpO₂ 93%. Not as critical as the quiet 9-year-old with worsening hypoxemia.
Take home points
- Oxygen saturation ≤ 92% signals significant hypoxemia and the need for urgent treatment.
- Prioritization in asthma focuses on recognizing signs of impending respiratory failure: quiet chest, altered mental status, severe retractions, and hypoxemia.
- Always treat the sickest first, not the noisiest. Wheezing children are often moving more air than those who are quiet.
Which breathing exercises should the nurse have an asthmatic 3-year-old child do to increase her expiratory phase?
Explanation
Asthma is a chronic inflammatory airway disorder with air trappingcaused by bronchoconstriction, mucus production, and swelling. Young children often have difficulty with structured breathing techniques such as incentive spirometry. Instead, play-based breathing exercises which helps to mobilize trapped air and improve ventilation.
Rationale for correct answer:
3.Blow a pinwheelis a playful, age-appropriate exercise that helps the child lengthen the expiratory phase, promoting better airway clearance and reducing air trapping.
Rationale for incorrect answers:
1. Using an incentive spirometerrequires a level of cooperation and understanding not expected in a 3-year-old. It is more appropriate for older children and adults.
2. Breathing into a paper bagis not used in asthma; it is sometimes used for hyperventilation due to anxiety. In asthma, this could worsen hypoxemia by limiting oxygen intake.
4. Taking several deep breathswithout a focus on prolonged exhalation does not specifically target the problem of air trapping in asthma.
Take home points
- Age-appropriate, play-based breathing exercises (e.g., blowing bubbles, blowing a pinwheel) are best for young children with asthma.
- The goal is to prolong exhalation and help mobilize trapped air.
- Structured devices like incentive spirometry are best reserved for older, cooperative children.
- Never use techniques that limit oxygen intake (like paper bag breathing) in asthma.
The parents of a 6-year-old who has a new diagnosis of asthma ask the nurse what to do to make their home a more allergy-free environment. Which is the nurse’s best response?
Explanation
Asthma is a chronic inflammatory airway disorder with air trappingcaused by bronchoconstriction, mucus production, and swelling. Asthma can be triggered by environmental allergens such as dust mites, pet dander, mold, and pollen. Preventive management focuses on allergen avoidance in the home environment.
Rationale for correct answer:
4.“Avoid purchasing upholstered furniture.”Upholstered furniture collects dust and allergens, which can worsen asthma symptoms. Choosing non-upholstered, easy-to-clean furniture helps maintain a more allergy-free environment.
Rationale for incorrect answers:
1. “Use a humidifier in your child’s room.”Humidifiers can actually promote mold growth and dust mites, which are common asthma triggers. A dehumidifier may be more appropriate in damp environments.
2. “Have your carpet cleaned chemically once a month.”Carpet cleaning chemicals may irritate airways. Instead, minimizing carpet use and vacuuming with a HEPA filter vacuum is better for asthma management.
3. “Wash household pets weekly.”While washing pets may temporarily reduce dander, it does not eliminate exposure. The best approach is to keep pets out of the child’s bedroom and limit close contact if pet dander is a known trigger.
Take home points
- Best environmental control for asthma: limit dust-collecting items (upholstered furniture, heavy drapes, stuffed animals).
- Humidifiers and strong chemicals should be avoided as they can worsen symptoms.
- HEPA filters, regular cleaning, and minimizing carpet use are better strategies.
- Nurses should educate parents that asthma control involves both medication adherence and environmental allergen reduction.
Which characteristic distinguishes status asthmaticus from asthma?
Explanation
Status asthmaticusis a severe, life-threatening asthma exacerbation that does not respond to standard bronchodilator therapy. Unlike typical asthma attacks, it is continuous, progressive, and can lead to respiratory failure if not treated promptly in an emergency setting.
Rationale for correct answer:
4.Status asthmaticus is characterized by persistent bronchospasm and airway obstructiondespite treatment with short-acting bronchodilators, requiring emergency interventions such as IV medications, oxygen therapy, or mechanical ventilation.
Rationale for incorrect answers:
1. Several attacks per monthindicate moderate persistent asthma, not status asthmaticus.
2. Less than six attacks per yearindicate mild intermittent asthma, not status asthmaticus.
3. While partial nonresponse may occur in severe asthma, status asthmaticus is defined by complete or nearly complete lack of responseand constant symptoms, making option 4 more precise.
Take home points
- Status asthmaticus is a medical emergency requiring immediate intervention.
- Key distinguishing feature: persistent symptoms unrelieved by usual therapy.
- Early recognition and treatment prevent respiratory failure and hypoxia.
- Nurses should monitor oxygen saturation, respiratory effort, and response to therapy continuously.
An 8-year-old child, who has a history of asthma, is seen in the office of the school nurse with coughing
and wheezing. Which of the following actions should the nurse perform first?
Explanation
Cystic fibrosis (CF) is a genetic disorderthat primarily affects the lungs and digestive system, but can impact other organs as well. CF is caused by mutations in the CFTR gene, which regulates the movement of salt and water in and out of cells. These mutations lead to the production of thick, sticky mucus that clogs airways and ducts in various organs.
Rationale for correct answer:
1. Assess the child’s peak expiratory flow: Measuring PEF is the first action because it gives critical information about the child’s current respiratory status and helps prioritize care. Immediate assessment guides whether quick-relief medications or emergency interventions are needed.
Rationale for incorrect answers:
2.Educate the child to avoid triggers: Education is important for long-term asthma management, but it does not address the acute respiratory distress the child is experiencing.
3. Transport the child to the emergency department: Transport may be necessary if severe symptoms persist or worsen, but initial assessment is required to determine the severity and urgency.
4. Notify the child’s parents of his condition: Parental notification is important, but the child’s respiratory status takes priority. Immediate assessment ensures timely intervention.
Take home points
- In children with asthma, airway assessment is the priority during acute symptoms.
- Peak expiratory flow is a simple, objective measure of airway obstruction.
- Nurses must act rapidly to assess, intervene with quick-relief medications, and escalate care if needed.
- Education on triggers and long-term management follows stabilization.
A 10-year-old child has been prescribed an MDI administered bronchodilator. Which of the following actions should the nurse teach the child to perform when taking the medication?
Explanation
A metered-dose inhaler (MDI)delivers a precise dose of bronchodilator directly to the lungs. It is a handheld device that delivers a precise amount of medication directly to the lungs in the form of a mist or aerosol. Proper technique is critical to ensure maximum drug delivery and therapeutic effect.
Rationale for correct answer:
3.Exhaling fullyempties the lungs, allowing for maximum inhalation of the medication when the MDI is actuated. Proper timing between exhalation and inhalation ensures optimal delivery to the lower airways.
Rationale for incorrect answers:
1. The MDI must be shakento mix the medication and propellant before each dose.
2. The recommended wait time between puffsof the same bronchodilator is usually about 1 minute, not 10 seconds, to allow the first dose to take effect.
4. The canister is pressed once per puff, not continuously for 30 seconds. Holding it down for an extended time is not necessary and can waste medication.
Take home points
- Proper MDI technique involves shaking the inhaler, exhaling fully, actuating while inhaling slowly, holding breath 5–10 seconds, and waiting 1–2 minutes between puffs if a second dose is prescribed.
- Teaching children the correct technique improves drug delivery, asthma control, and reduces side effects.
- Use of a spacer is recommended for children to ensure better deposition of medication in the lungs.
Practice Exercise 2
How does the nurse interpret the laboratory analysis of a stool sample containing excessive amounts of azotorrhea and steatorrhea in a child with cystic fibrosis (CF)?
The values indicate the child is:
Explanation
Cystic fibrosis (CF)is an autosomal recessive disorder affecting the exocrine glands. Thick secretions obstruct the pancreatic ducts, preventing digestive enzymes from reaching the intestines. This results in malabsorption of fats and proteins, leading to steatorrheaand azotorrhea, that is, foul-smelling stools with undigested protein.
Rationale for correct answer:
2. Excessive steatorrhea and azotorrhea indicate that pancreatic enzymes are not being adequately delivered to the intestines. This strongly suggests that the child is either missing doses, taking them incorrectly, or underdosed.Compliance with enzyme replacement is critical to prevent growth failure and nutritional deficiencies in CF.
Rationale for incorrect answers:
1. Vitamin noncomplianceleads to deficiencies (A, D, E, K) but does not directly cause steatorrhea and azotorrhea.
3. A high-fat dietalone does not cause these findings if enzymes are taken as prescribed. Enzyme therapy allows CF patients to tolerate high-calorie, high-fat diets.
4. High fiber intakemay cause bloating or gas, but it does not cause fat and protein malabsorption.
Take home points
- Steatorrhea and azotorrhea results from inadequate pancreatic enzyme therapy in CF.
- Pancreatic enzyme replacement must be taken with all meals and snacks.
- Fat-soluble vitamin supplementation is important but does not directly prevent malabsorption symptoms.
- Nutritional management in CF includes a high-calorie, high-protein, high-fat diet with enzyme supplementation.
Which would the nurse explain to parents about the inheritance of cystic fibrosis?
Explanation
Cystic fibrosis (CF) is caused by mutations in the Cystic Fibrosis Transmembrane Conductance Regulator (CFTR gene). This gene controls the movement of salt and water in and out of cells. This leads to the production of thick, sticky mucus instead of thin, slippery secretions.
Rationale for correct answer:
4.If one parent has CF, that is, two defective genes and the other is a carrier, that is one defective gene there is a 50% chancethe child will have CF since the child inherits one defective gene from each parent. There is also a 50% chancethe child will be a carrier by inheriting one defective gene from the CF parent and one normal gene from the carrier parent.
Rationale for incorrect answers:
1. CF is an autosomal-dominant trait passed on from the child’s motheris incorrect because CF is autosomal recessive, not dominant.
2. CF is an autosomal-dominant trait passed on from the child’s fatheris inaccurate since inheritance is not dominant.
3. The child of parents who are both carriers having a 50% chance of acquiring CFis incorrect. If both parents are carriers 25% chance the child will have CF, 50% chance the child will be a carrier, and 25% chance the child will be unaffected.
Take home points
- CF is autosomal recessive. A child must inherit two defective CF genes to have the disease.
- Two carrier parents: 25% affected, 50% carrier, 25% unaffected.
- One parent with CF and one carrier parent: 50% affected, 50% carrier.
- Genetic counseling is important for families with a history of CF.
The parent of a 4-month-old with cystic fibrosis (CF) asks the nurse what time to begin the child’s first chest physiotherapy (CPT) each day. Which is the nurse’s best response?
Explanation
Cystic fibrosis (CF) causes thick, sticky mucus that clogs the airways and predisposes the child to respiratory infections. Chest physiotherapy (CPT)is used to mobilize secretions and improve airway clearance. Timing of CPT is important to optimize effectiveness and reduce complications such as vomiting or aspiration.
Rationale for correct answer:
1.Performing CPT 30 minutes before feedingis correct because airway clearance prior to eating reduces the risk of vomiting or aspirationduring therapy. It also helps open the airways, which improves oxygenation and overall tolerance of feeds.
Rationale for incorrect answers:
2.CPT is performed before suctioning, not after. CPT helps loosen secretions, and suctioning may then be used afterward if needed to clear mobilized mucus.
3.Performing CPT 30 minutes after feedingis incorrect because it increases the risk of regurgitation, vomiting, and aspiration, especially in infants.
4.CPT should not be limited to times of congestion or coughing. It is a routine, daily therapyto maintain airway clearance and prevent mucus plugging.
Take home points
- CPT should be scheduled before meals to minimize aspiration risk.
- Airway clearance therapy is a routine part of CF management, not just during illness.
- CPT helps loosen secretions, and suctioning may follow if secretions are not effectively expelled.
- Timing airway clearance correctly supports nutrition and lung function in infants with CF.
The parent of an infant with cystic fibrosis (CF) asks the nurse how to meet the child’s increased nutritional needs. Which is the nurse’s best suggestion?
Explanation
Infants with cystic fibrosis (CF) have increased energy requirementsbecause of the extra work of breathing and chronic lung infections. They also experience malabsorption of fats and proteins due to pancreatic enzyme insufficiency.
Rationale for correct answer:
3. A higher-calorie formulais appropriate because infants with CF need more calories than healthy infants to meet growth requirements. This ensures they receive enough energy to compensate for malabsorption and increased metabolic demands. Pancreatic enzymes are also given with feeds to aid digestion.
Rationale for incorrect answers:
1.Increasing fruits and vegetablesdoes not meet the high-calorie and high-protein needs of an infant with CF. While they are healthy foods, they are not calorie-dense enough to support growth in CF.
2.Advancing to whole cow’s milkbefore age 12 months is inappropriate. Infants under 1 year should receive breast milk or formula; cow’s milk lacks adequate iron and essential nutrients and may increase the risk of anemia.
4.Increasing carbohydrate intakealone is not sufficient. Infants with CF need balanced nutrition with adequate protein and fatto support tissue growth and energy needs.
Take home points
- Infants with CF need higher-calorie diets due to malabsorption and increased metabolic demands.
- Pancreatic enzymes must be given with feeds to aid digestion and nutrient absorption.
- Cow’s milk is not recommended before 12 months of age.
- Nutritional care in CF focuses on high-calorie, high-protein, high-fat foods once the child is on solids.
The parent of a child with cystic fibrosis (CF) is excited about the possibility of the child receiving a double lung transplant. What should the parent understand?
Explanation
Cystic fibrosis (CF) causes thick, sticky mucus that clogs the airways and predisposes the child to respiratory infections. It is a genetic, multisystem disorderthat primarily affects the lungs and digestive system.
Rationale for correct answer:
2.A double lung transplant can improverespiratory functionand quality of life, allowing the child to live longer. However, it does not correct the underlying genetic defect, so problems with digestion, pancreatic insufficiency, and other CF complications persist.
Rationale for incorrect answers:
1.Lung transplant doesnot cure CF; the genetic defect remains, and other organ complications continue.
3. Transplantation cannotreverse multisystem damagesuch as pancreatic insufficiency, liver disease, and infertility. These issues remain lifelong.
4.While transplantation may prolong life, it should not be described as the only chancefor survival or framed in terms of a specific milestone (like college graduation). This may create unrealistic expectations.
Take home points
- Lung transplantation improves survival in CF patients with end-stage lung disease but is not a cure.
- CF remains a multisystem disease; pancreatic and gastrointestinal issues persist after transplant.
- Families should be counseled about realistic expectations and ongoing care needs after transplant.
- Genetic counseling and continued multidisciplinary support remain essential in CF management.
A 2-year-old has just been diagnosed with cystic fibrosis (CF). The parents ask the nurse what early respiratory symptoms they should expect to see in their child. Which is the nurse’s best response?
Explanation
Cystic fibrosis (CF) is a genetic disorder that causes thick, sticky mucus production in the airways, leading to airway obstruction, inflammation, and infections. It is a genetic, multisystem disorder that primarily affects the lungs and digestive system.
Rationale for correct answer:
4.Wheezing respirationsare an early sign of airway obstruction due to mucus plugging in children with CF. Parents should be taught that recurrent wheezing is one of the first respiratory manifestations.
Rationale for incorrect answers:
1. Abarrel-shaped chestdevelops later in the disease from chronic air trapping and hyperinflation of the lungs. It is not an early sign.
2. Achronic productive coughis more typical in later stages, once recurrent lung infections and persistent mucus buildup have progressed.
3. Bronchiectasis, an irreversible dilation and damage of bronchi, is a long-term complication of repeated lung infections, not an early finding.
Take home points
- Early respiratory signs of CF include wheezing and recurrent respiratory infections.
- Progressive signs include chronic cough, barrel chest, and digital clubbing.
- Parents should report persistent wheezing, frequent cough, or recurrent infections early for prompt intervention.
- Early airway clearance therapy helps reduce progression of lung damage.
The parent of a child with cystic fibrosis (CF) asks the nurse what will be done to relieve the child’s constipation. Which is the nurse’s best response?
Explanation
Children with cystic fibrosis (CF) often develop gastrointestinal complications due to thick, sticky mucus secretions that block the intestines. Constipation is common and is usually managed with oral stool softeners or osmotic laxatives.
Rationale for correct answer:
3.MiraLAX (polyethylene glycol)is commonly prescribed for constipation in children with CF because it draws water into the stool, making it easier to pass. It is safe for long-term use and effective in relieving constipation caused by thick mucus secretions.
Rationale for incorrect answers:
1. Surgery isnot the first-line treatmentfor constipation in CF. Surgery is only considered for severe complications such as distal intestinal obstructive syndrome (DIOS)that does not respond to medical management.
2.IV fluidsmay be given if the child is dehydrated but are not the primary treatment for constipation. Hydration helps, but medications like MiraLAX are typically needed.
4.A clear liquid dietmay temporarily ease symptoms in severe obstruction but is not standard treatment for routine constipation in CF. Adequate nutrition is essential for growth and health.
Take home points
- Constipation in CF is usually managed with osmotic laxatives like MiraLAX.
- Surgery is reserved for severe, non-resolving intestinal obstruction (DIOS).
- Adequate hydration and enzyme therapy also help prevent constipation.
- GI symptoms in CF require ongoing monitoring to prevent complications.
What does the therapeutic management of cystic fibrosis (CF) patients include? Select all that apply
Explanation
Cystic fibrosis (CF) is a chronic, progressive genetic disorder affecting multiple systems, primarily the lungs and gastrointestinal tract. Therapeutic management focuses on maintaining adequate nutrition, promoting airway clearance, preventing infections, encouraging activity, and supporting adherence to prescribed therapies to improve quality of life and extend survival.
Rationale for correct answers:
1. Ahigh-protein, high-calorie dietis necessary because CF patients have increased metabolic demands and malabsorption due to pancreatic enzyme insufficiency.
3. Exerciseimproves lung function, enhances airway clearance, strengthens respiratory muscles, and promotes overall health.
4. Minimizing pulmonary complicationsis a cornerstone of CF management. This includes chest physiotherapy, airway clearance techniques, antibiotics, and vaccinations.
5. Medication complianceis critical for effectiveness of therapies such as pancreatic enzymes, fat-soluble vitamins, bronchodilators, mucolytics, antibiotics, and CFTR modulators.
Rationale for incorrect answers:
2.While CF patients require high-calorie and nutrient-rich diets, recommending a specifically high-fat, high-carbohydrate dietis misleading. Fat and carbohydrate intake should be balanced with protein, with pancreatic enzymes given to aid digestion. The emphasis is on high-calorie, high-protein nutrition, not excessive fat/carbs alone.
Take home points
- CF management requires a multidisciplinary approach (nutrition, respiratory therapy, medications).
- High-protein, high-calorie diets with enzyme supplementation support growth and development.
- Daily airway clearance + exercise improves lung function and reduces complications.
- Long-term survival depends heavily on adherence to prescribed therapies and consistent medical follow-up.
A chloride level greater than _____________________ is a positive diagnostic indicator of cystic fibrosis (CF).
Explanation
The sweat chloride testis the gold standard for diagnosing cystic fibrosis (CF). CF causes defective chloride transport across epithelial cells, leading to abnormally salty sweat. Elevated chloride levels in sweat confirm the diagnosis.
Rationale for correct answer:
3. Asweat chloride level ≥60 mEq/Lis a positive diagnostic indicator of CF in children and adults. This finding strongly supports CF when clinical features are present.
Rationale for incorrect answers:
1. 30 mEq/Lis below the diagnostic threshold. In infants under 6 months, values ≥30 mEq/L are considered suspicious but not diagnostic.
2. 25 mEq/Lis normal and does not indicate CF.
4. 50 mEq/Lis considered borderline/suspicious but not diagnostic. Additional testing (genetic testing or repeat sweat chloride test) would be required.
Take home points
- Sweat chloride level ≥60 mEq/L is diagnostic for CF.
- The sweat chloride test is most accurate when performed at a certified CF center.
A nurse is performing an assessment on a newborn with a possible diagnosis of cystic fibrosis. Which of the following is an early sign of the disease?
Explanation
Cystic fibrosis (CF) is a genetic disorderthat affects the lungs, digestive system, and other organs by causing the body to produce thick, sticky mucus. CF is caused by mutations in the CFTR gene, which regulates salt and water movement in and out of cells. These mutations disrupt the function of the CFTR protein, leading to mucus buildup.
Rationale for correct answer:
4.Meconium ileusoccurs in newborns with CF due to viscous intestinal secretions,and it may present as abdominal distention, failure to pass meconium within the first 24–48 hours, and bilious vomiting. Early recognition is crucial for prompt surgical or medical intervention.
Rationale for incorrect answers:
1. While CF can later cause intestinal blockages or constipation, it is not typically an early neonatal sign.
2. Decreased appetitemay occur later due to malabsorption, but it is not an early sign in newborns.
3.CF is not associated with elevated albumin levels. Instead, malabsorption can lead to hypoalbuminemiaover time.
Take home points
- Meconium ileus is a hallmark early sign of CF in newborns.
- Newborns with delayed meconium passage or abdominal distention should be evaluated for CF.
- Early detection allows for timely management of nutrition, pancreatic enzymes, and respiratory care.
- Newborn screening and sweat chloride testing confirm the diagnosis.
Which statement concerning pancreatic enzymes for a cystic fibrosis client is correct?
Explanation
Children with cystic fibrosis (CF)often have pancreatic insufficiency, leading to malabsorption of fats and proteins. Pancreatic enzyme supplements are essential to improve digestion and nutrient absorption. Proper timing and dosing of enzymes are critical to maximize their effectiveness.
Rationale for correct answer:
4.Pancreatic enzymes should be taken with every meal and snackto ensure that food is properly digested, reduce steatorrhea, and promote adequate growth and nutrition.
Rationale for incorrect answers:
1. Many CF pancreatic enzyme capsules contain microbeads or microspheresthat can be sprinkled on soft foodsif the client cannot swallow capsules whole.
2. Crushing enzymes can destroy the enteric coating, making them ineffective and potentially irritating to the stomach.
3. While frequent meals and snacks are appropriate for nutrition, this alone does not address enzyme administration, which is the key point.
Take home points
- Administer pancreatic enzymes with all meals and snacks for proper digestion.
- Do not crush or chew enzyme capsules/microbeads unless specifically formulated to be sprinkled on soft food.
- Encourage a high-calorie, high-fat, high-protein diet to meet nutritional needs.
- Monitor stool characteristics and growth to assess enzyme effectiveness.
Which intervention is appropriate for care of the child with cystic fibrosis?
Explanation
Cystic fibrosis (CF) is a genetic disorderthat affects the lungs, digestive system, and other organs by causing the body to produce thick, sticky mucus. CF is caused by mutations in the CFTR gene, which regulates salt and water movement in and out of cells. These mutations disrupt the function of the CFTR protein, leading to mucus buildup.
Rationale for correct answer:
3.Chest physiotherapy (CPT)helps mobilize and clear secretions, improving airway clearance, lung function, and oxygenation. CPT is a primary therapy for CF. Regular sessions help prevent mucus plugging, reduce infection risk, and improve breathing.
Rationale for incorrect answers:
1. Exercise isencouragedin children with CF because it helps loosen mucus and maintain cardiopulmonary fitness.
2. Coughing is anatural mechanism for clearing mucus. Suppressants may worsen airway obstruction. Antihistamines are not routinely indicated unless allergies are present.
4. Bronchodilatorsare typically given before CPTto open airways, making airway clearance more effective.
Take home points
- Chest physiotherapy 2–4 times daily is essential in CF care.
- Administer bronchodilators before CPT to enhance mucus clearance.
- Encourage regular physical activity to support lung health.
- Avoid suppressing cough; coughing is an important mechanism for airway clearance.
Which statement is appropriate for a nurse to address to the parents of a child with cystic fibrosis who are planning to have a second child?
Explanation
Cystic fibrosis (CF) is a genetic disorderthat affects the lungs, digestive system, and other organs by causing the body to produce thick, sticky mucus. CF is caused by mutations in the CFTR gene, which regulates salt and water movement in and out of cells. These mutations disrupt the function of the CFTR protein, leading to mucus buildup.
Rationale for correct answer:
1. Cystic fibrosis (CF) is an autosomal recessive genetic disorder.Both parents must be carriers of the CF gene for a child to be affected. Genetic counselingprovides information on inheritance patterns, carrier status, and reproductive risks, helping families make informed decisions about future pregnancies.
Rationale for incorrect answers:
2.If both parents are carriers, the chance for a completely unaffected childis 25%, not 50%.
3. The chance of having an affected childwhen both parents are carriers is 25%, not 50%.
4. The chance of a child being a carrieris 50%, not 25%.
Take home points
- CF is autosomal recessive, meaning both parents must carry the gene for a child to be affected.
- Carrier status and inheritance risks should be discussed with a genetic counselor before future pregnancies.
- Understanding genetic risk helps parents plan and access prenatal testing or assisted reproductive options.
- Counseling provides psychosocial support in addition to medical information.
A child with CF should receive which vitamin supplements in his daily diet? Select all that apply
Explanation
Children with cystic fibrosis (CF) often have pancreatic insufficiency, which leads to malabsorption of fat-soluble vitamins. Supplementation is necessary to prevent deficiencies, maintain growth, support immune function, and promote bone health.
Rationale for correct answers:
1. Vitamin Ais essential for vision, skin integrity, and immune function. Fat malabsorption in CF can lead to deficiency.
3. Vitamin Dsupports calcium absorption and bone health. Children with CF are at risk for rickets and poor bone mineralization.
4. Vitamin Eis an antioxidantimportant for protecting cell membranes and preventing hemolytic anemia.
5. Vitamin Kis necessary for blood clotting.Deficiency can lead to bleeding disorders in children with CF.
Rationale for incorrect answers:
2.Vitamin Cis water-solubleand generally not deficient in CF if the child consumes a normal diet. Supplementation is not routinely required.
6. Vitamin B12is also water-soluble, and routine supplementation is usually unnecessary unless a deficiency is diagnosed.
Take home points
- Children with CF require daily supplementation of fat-soluble vitamins (A, D, E, K) due to malabsorption.
- Monitoring growth, bone health, and coagulation status helps ensure supplementation is effective.
- Caregivers should understand that water-soluble vitamins are generally obtained through diet, while fat-soluble vitamins need supplementation.
- Supplements should be given with meals containing fat to enhance absorption.
The parents of a child, who has had multiple respiratory infections since birth, tell the nurse, “When we kiss our child, all we can taste is salt.” It would be appropriate for the nurse to suggest to the primary health-care provider that the child be assessed for which of the following illnesses?
Explanation
Cystic fibrosis (CF)is a genetic disorder affecting exocrine glands, resulting in thick, sticky mucus in the lungs, pancreas, and other organs. Children with CF are also prone to recurrent respiratory infections due to mucus buildup and impaired airway clearance.
Rationale for correct answer:
1. Salty skin on the lips or skinis a classic early sign of cystic fibrosis, especially in children with a history of frequent respiratory infections. This warrants evaluation by the primary health-care provider and confirmatory testing such as a sweat chloride test.
Rationale for incorrect answers:
2.Asthmacauses wheezing, coughing, and shortness of breath but does not cause salty-tasting skin.
3. Bronchiolitisis an acute viral infection of the lower respiratory tract in infants, causing cough, wheezing, and congestion. Salty skin is not a feature.
4. Pharyngitisinvolves sore throat, fever, and inflammation of the pharynx, and does not cause salty-tasting skin.
Take home points
- Salty-tasting skin is a hallmark early sign of CF and should prompt further evaluation.
- Recurrent respiratory infections in infancy increase suspicion for CF.
- The sweat chloride test is the standard diagnostic tool.
Early diagnosis allows initiation of airway clearance, nutritional support, and infection prevention strategies.
Practice Exercise 3
An infant with chronic bronchopulmonary dysplasia (BPD) and a tracheostomy is being discharged on home oxygen therapy. Which statement by the mother indicates that further teaching is needed before discharge?
Explanation
Bronchopulmonary dysplasia (BPD)is a chronic lung disease of infancy, often seen in premature infants requiring prolonged ventilation or oxygen therapy. These infants frequently need home oxygen, tracheostomy care, and close monitoring. They are highly susceptible to respiratory infections, hypoxemia, and complications with high altitude.
Rationale for correct answer:
3.Camping trip to Yellowstone National Park:Yellowstone is at a high altitude, which has lower oxygen levels in the air. An infant with BPD on home oxygen is at high risk of severe hypoxemia and respiratory distress in such environments. Travel to high-altitude areas is contraindicated until the infant’s respiratory status is stable and cleared by the healthcare team.
Rationale for incorrect answers:
1. Calling the pediatrician if fever or increased secretions: These are early signs of infection or tracheostomy complications, and prompt medical evaluation is necessary.
2. Loosely covering the tracheostomy with a bib during feeding/outside:A loose cover protects the airway from food particles, wind, and debris without blocking airflow.
4. Notifying the power company about home oxygen use:This ensures the family has priority in case of a power outage since home oxygen is life-sustaining equipment.
Take home points
- Infants with BPD on home oxygen should not be exposed to high altitudes without medical clearance.
- Parents should be taught infection prevention, safe tracheostomy care, and oxygen safety.
- Backup power planning and emergency contacts are essential for families using home oxygen.
- Nurses must carefully assess caregiver understanding before discharge to ensure safety at home.
A neonate who has been exposed to ventilatory support with high positive airway pressure and oxygen during the first 2 weeks of life is at risk for developing which disorder?
Explanation
Bronchopulmonary dysplasia (BPD)is a chronic lung disease that primarily affects premature neonates who require prolonged ventilatory support or high concentrations of oxygen. It results from lung injury due to mechanical ventilation, oxygen toxicity, and inflammation, leading to impaired alveolar development, fibrosis, and airway remodeling.
Rationale for correct answer:
2.Exposure to high positive airway pressure and high oxygen concentrations during the first weeks of life can damage immature lungs and interfere with alveolar growth, leading to BPD.
Rationale for incorrect answers:
1. Bronchiolitisis an acute viral infectionof the lower respiratory tract, not caused by ventilatory support or oxygen therapy.
3. Asthmais a chronic inflammatory airway disease, usually diagnosed later in childhood, not directly caused by neonatal ventilatory support.
4. Cystic fibrosisis a genetic disorder caused by mutations in the CFTR gene, unrelated to ventilatory support or oxygen exposure.
Take home points
- Neonates exposed to high oxygen and positive pressure ventilation are at increased risk for BPD.
- BPD involves chronic lung inflammation, airway remodeling, and impaired alveolarization.
- Preventive strategies include gentle ventilation, minimizing oxygen exposure, and early surfactant therapy.
Which of these assessment findings, if identified in a young infant with bronchopulmonary dysplasia, should a nurse immediately report to the physician?
Explanation
Infants with bronchopulmonary dysplasia (BPD)have immature lungs with decreased compliance and impaired gas exchange. They are at risk for respiratory distress and failure. Key signs of acute respiratory compromiseinclude tachypnea, retractions, nasal flaring, grunting, and changes in oxygen saturation. Early recognition and prompt reporting are critical to prevent further deterioration.
Rationale for correct answer:
3.Respiratory rate greater than 60 breaths/minute with moderate sub-sternal retractions indicates increased work of breathing and possible hypoxemiadespite oxygen therapy. Immediate reporting is necessary because the infant may require escalation of respiratory supportor additional interventions to prevent respiratory failure.
Rationale for incorrect answers:
1. Pulse oximetry of 94% while receiving oxygen by nasal cannula is slightly lower than normal but generally acceptable for a BPD infant on supplemental oxygen; can be monitored, not emergent.
2. Decreased intake with last feedingis concerning for hydration/nutrition but not an immediate life-threatening issue; can be managed with feeding adjustments and monitoring.
4. Sleeping more than 3 hours at a time is normal for young infants; not an indication of acute respiratory compromise.
Take home points
- Tachypnea and retractions are early warning signs of respiratory distress in infants with BPD.
- Nurses should report changes in respiratory effort immediately, even if oxygen saturation is only mildly affected.
- Monitoring oxygen saturation, respiratory rate, retractions, and overall work of breathing is essential for infants with chronic lung disease.
- Prompt intervention can prevent progression to respiratory failure.
The nursing care plan for an infant with bronchopulmonary dysplasia includes the nursing diagnosis of Impaired gas exchange. Which nursing action would be most appropriate for a nurse to include?
Explanation
Bronchopulmonary dysplasia (BPD)is a chronic lung disease resulting from lung injury in premature infants. Impaired gas exchange occurs due to alveolar damage, inflammation, and mucus accumulation, leading to hypoxemia and increased work of breathing. Nursing care focuses on optimizing oxygenation and ventilation.
Rationale for correct answer:
1. Chest physiotherapyhelps mobilize secretions, improve airway clearance, and enhance ventilation, directly addressing impaired gas exchange. This intervention reduces atelectasis and facilitates better oxygenation.
Rationale for incorrect answers:
2.Enteral feedingssupport nutrition, which is important for growth, but they do not directly improve gas exchange.
3. Developmental activitiessupport neurodevelopment, but are secondary to airway and respiratory support in prioritization.
4. Bondingis important for psychosocial development, but it does not directly address impaired gas exchange.
Take home points
- Nursing interventions for impaired gas exchange in BPD should focus on airway clearance, oxygen therapy, and respiratory monitoring.
- Chest physiotherapy is a key intervention to remove secretions and improve alveolar ventilation.
- Supportive care (nutrition, developmental activities, and bonding) is important but secondary to ensuring adequate oxygenation.
- Continuous monitoring of respiratory rate, oxygen saturation, and work of breathing is essential to evaluate intervention effectiveness.
Which characteristic distinguishes allergies from colds?
Explanation
Allergiesare immune-mediated reactions to environmental antigens (allergens) such as pollen, dust, or pet dander. Coldsare viral infections that produce variable symptoms such as congestion, runny nose, and sometimes fever, usually resolving within 7–10 days.
Rationale for correct answer:
4.Sneezing in allergies occursrepetitively and predictably, often in response to exposure to a specific allergen, distinguishing it from the intermittent or variable sneezing seen in viral colds.
Rationale for incorrect answers:
1. Skin testsare used to identify allergens, not viral infections. Colds are diagnosed clinically based on symptoms.
2. Allergies do not causefever. Fever suggests an infectious process, such as a cold or flu.
3. Itchingis typical of allergies, not viral colds. Colds may cause nasal congestion or discharge but not persistent itching.
Take home points
- Allergies produce predictable, consistent, and non-infectious symptoms such as sneezing, nasal/eye itching, and clear rhinorrhea.
- Colds are caused by viruses and usually present with variable symptoms and possible fever.
- Diagnostic tests like skin testing or IgE levels can confirm allergies.
- Nurses should educate caregivers on differentiating allergy symptoms from infections to guide appropriate management.
A nurse is helping a client with obstructive sleep apnea to apply a continuous positive airway pressure (CPAP) mask before going to sleep. The nurse knows that CPAP is intended to:
Explanation
Obstructive sleep apnea (OSA) in children is a sleep-related breathing disorder where the upper airway becomes partially or completely blocked during sleep, causing repeated pauses in breathing throughout the night. The child may snore loudly, gasp, or stop breathing briefly, then resume with a snort or choke.
Rationale for correct answer:
4. Continuous positive airway pressure (CPAP) maintains positive airway pressure, which keeps alveoli and the upper airway patentduring sleep, improving oxygenation and reducing apneic events in clients with OSA.
Rationale for incorrect answers:
1. CPAPdoes not provide ventilation; it does not initiate breaths. It only maintains airway patency. Ventilators or BiPAP are used for assisted ventilation.
2. CPAP maintains positive pressure and may actually increase intrathoracic pressure slightly. Its goal is not to reduce it.
3. CPAP provides air at room concentration or supplemental oxygenif added, but the primary purpose is airway patency, not high oxygen delivery.
Take home points
- CPAP is first-line therapy for obstructive sleep apnea, particularly in adults and children with significant airway obstruction.
- The device prevents airway and alveolar collapse, improving oxygenation and sleep quality.
- Nurses should educate clients on proper mask fit, cleaning, and adherence to therapy.
- CPAP does not replace spontaneous breathing; it supports airway patency only.
Comprehensive Questions
Which statement by a school-aged client who has asthma indicates to the nurse an understanding of the use of a peak expiratory flow meter?
Explanation
A peak expiratory flow (PEF) metermeasures the maximum speed of expiration and is used to monitor airway obstruction in asthma. Daily use helps detect early changes in lung function before symptoms appear, allowing timely intervention and prevention of exacerbations.
Rationale for correct answer:
1. “My peak flow meter can tell me if an asthma episode might be coming, even though I might still be feeling okay.”The peak flow meter is an early warning tool. A decrease from the child’s personal best can indicate worsening airway obstruction before overt symptoms, prompting action according to the asthma action plan.
Rationale for incorrect answers:
2.“When I do my peak flow, it works best if I do three breaths without pausing in between breaths.”Peak flow measurements should be done with a deep inhalation followed by a single, forceful exhalation into the meter. Multiple breaths without pausing would invalidate the reading.
3. “I always start with the meter reading about halfway up. That way I don’t waste any breath.”The meter should always be set to zero before each attempt to ensure an accurate reading.
4. “If I use my peak flow meter every day, I will not have an asthma attack.”Using the meter does not prevent asthma attacks; it helps monitor airway status so early interventions can be taken if a decline is detected.
Take home points
- Peak flow meters detect early airway obstruction, even before symptoms appear.
- Proper technique: reset to zero, deep breath in, blow out as hard and fast as possible, repeat three times, record the highest value.
- Peak flow readings guide asthma action plans for timely medication adjustments.
Daily use helps prevent severe attacks but does not replace prescribed medications or other asthma management strategies.
A school-aged child with cystic fibrosis is hospitalized for a respiratory infection. Which documentation in the chart indicates to the nurse a need for counseling regarding nutrition and gastrointestinal complications? Select all that apply
Explanation
Cystic fibrosis (CF) affects the pancreas, leading to pancreatic enzyme insufficiencyand malabsorption of fats and proteins. This can cause nutritional deficiencies, steatorrhea (fatty stools), and poor growth. Proper nutrition with high-calorie, high-fat diets and enzyme supplementationis essential, especially during respiratory infections that increase metabolic demand.
Rationale for correct answers:
1. Frothy, foul-smelling stoolsindicates steatorrhea caused by fat malabsorption, suggesting the child may need enzyme dose adjustment or dietary counseling.
5. Children with CF require high-calorie, high-fat dietsto maintain growth and meet increased energy needs. A low-fat, low-calorie diet is inappropriate and increases the risk of malnutrition and poor growth.
Rationale for incorrect answers:
2.Weight remaining unchanged from yesterdaydoes not necessarily concerning in acute illness; short-term weight changes may not reflect chronic nutritional status.
3. Consuming 80% of breakfastis an acceptable intake for a hospitalized child. Indicates reasonable appetite.
4. Eating three snacks every dayis a positive behavior for caloric intake. Encouraged in CF nutrition plans.
Take home points
- Steatorrhea (frothy, foul-smelling stools) indicates inadequate fat absorption — assess enzyme use and dietary intake.
- Children with CF need high-calorie, high-fat diets; low-calorie diets are inappropriate.
- Nutrition counseling is essential to support growth, maintain weight, and meet increased metabolic demands during illness.
- Nurses should monitor stool characteristics, dietary intake, and weight trends for early identification of gastrointestinal complications.
Which nursing diagnosis is the priority for an infant with bronchopulmonary dysplasia?
Explanation
Bronchopulmonary dysplasia (BPD) is a chronic lung disease in infants, often following premature birth with prolonged oxygen therapy and mechanical ventilation. The primary pathophysiology involves alveolar damage, decreased lung compliance, and ventilation-perfusion mismatch, which can lead to hypoxemia and hypercapnia.
Rationale for correct answer:
3.Impaired gas exchange: The highest priority in nursing care is to ensure adequate oxygenation and ventilation. Without effective gas exchange, all other body systems are compromised. Interventions may include oxygen therapy, monitoring SpO₂, positioning, and respiratory support as needed.
Rationale for incorrect answers:
1. Imbalanced nutrition: Less than body requirements:This is important but secondary to addressing life-threatening respiratory compromise. Nutrition support is necessary once the infant is stable.
2. Effective breastfeeding: This is a goal/outcome rather than a diagnosis; important for growth and bonding but not immediately life-threatening.
4. Risk for imbalanced fluid volume:Preventive nursing concern; while fluid management is important, it is not as urgent as impaired gas exchange in an infant with BPD.
Take home points
- Airway and breathing always take priority over nutrition or fluid management in infants with chronic lung disease.
- Nursing interventions should focus on monitoring respiratory status, optimizing oxygenation, and minimizing work of breathing.
- Once the infant is stable, attention can shift to nutrition, fluid balance, and developmental care.
- ABCs (Airway, Breathing, Circulation) guide prioritization in critical pediatric care.
Which management strategy is recommended when caring for an infant with bronchopulmonary dysplasia?
Explanation
Bronchopulmonary dysplasia (BPD) is a chronic lung disease in infants, often following premature birth with prolonged oxygen therapy and mechanical ventilation. The primary pathophysiology involves alveolar damage, decreased lung compliance, and ventilation-perfusion mismatch, which can lead to hypoxemia and hypercapnia.
Rationale for correct answer:
3. Structured routinesensure that the infant receives adequate rest, nutrition, and care while minimizing unnecessary stress and energy expenditure, which is crucial for infants with compromised lungs.
Rationale for incorrect answers:
1. Provide frequent playful stimuli:While developmental stimulation is important, frequent stimulation can fatigue the infant, increasing oxygen needs and respiratory distress. Play should be balanced with rest.
2. Decrease oxygen during feedings: Oxygen should never be decreased during activities or feeding unless specifically ordered by the provider, as infants with BPD are at risk for desaturation.
4. Place the infant in an open crib: Open cribs may be inappropriate for infants needing thermal support or oxygen therapy. Isolette or semi-enclosed cribs may be preferred until the infant is stable.
Take home points
- Scheduled care helps conserve energy in infants with BPD.
- Balance rest, nutrition, and developmental activities to support growth and prevent fatigue.
- Oxygen therapy should always be maintained during all interventions.
- Nurses should plan care to minimize stress and optimize respiratory function while promoting normal development.
The nurse is planning care for a child admitted to the pediatric unit with bronchopulmonary dysplasia. Which symptom is the nurse most likely to assess?
Explanation
Bronchopulmonary dysplasia (BPD)is a chronic lung disease seen in premature infantswho required prolonged oxygen therapy or mechanical ventilation. The disease results in alveolar damage, airway inflammation, and impaired gas exchange, which manifest as increased work of breathing, tachypnea, and dyspnea.
Rationale for correct answer:
2.Infants and children with BPD often show rapid breathing, labored breathing, nasal flaring, retractions, and use of accessory musclesdue to compromised lung function and decreased oxygenation.
Rationale for incorrect answers:
1. BPD is characterized by increased work of breathing, not minimal effort.
3. Infants with BPD may become irritable or difficult to consoledue to discomfort, hypoxia, or fatigue from increased respiratory effort.
4. Hypotensionis not a typical early sign of BPD. Blood pressure is usually maintained unless there is severe illness or complications.
Take home points
- Tachypnea and dyspnea are hallmark signs of BPD and should guide nursing assessments.
- Nurses should monitor respiratory rate, effort, oxygen saturation, and work of breathing closely.
- Early identification of respiratory compromise allows timely interventions such as oxygen therapy, suctioning, and positioning to optimize ventilation.
- Supportive care should include nutrition, rest, and developmentally appropriate handling to minimize additional stress on the lungs.
Infants with bronchopulmonary dysplasia require frequent, prolonged rest periods. Which sign indicates overstimulation?
Explanation
Infants with bronchopulmonary dysplasia (BPD)have immature lungs and decreased respiratory reserve. Frequent handling and stimulation can increase oxygen demand and cause overstimulation, leading to hypoxemia, respiratory distress.
Rationale for correct answer:
3.Cyanosisindicates inadequate oxygenation, often a result of overstimulation or increased work of breathing. It is a serious sign that requires immediate intervention, such as pausing stimulation, providing supplemental oxygen, or repositioning.
Rationale for incorrect answers:
1. Increased alertnessis normal behavior and may indicate a healthy response to interaction rather than overstimulation.
2. Good eye contactis a positive developmental response and not a sign of respiratory distress or overstimulation.
4.While lethargycan indicate fatigue or illness, cyanosis is a more immediate indicator of overstimulation and oxygen compromise in BPD.
Take home points
- Infants with BPD need frequent rest periods to conserve energy and maintain oxygenation.
- Cyanosis, nasal flaring, retractions, and tachypnea are early signs of overstimulation and hypoxemia.
- Nurses should pace care, minimize handling, and cluster interventions to reduce stress.
- Immediate action is required if cyanosis occurs to ensure airway patency and adequate oxygen delivery.
Bronchopulmonary dysplasia can be classified into four categories. Which characteristic is noted during the early or first stage of the disease?
Explanation
Bronchopulmonary dysplasia (BPD)is a chronic lung disease primarily affecting premature infantswho required mechanical ventilation or high oxygen therapy. BPD is classified into four stagesbased on radiographic and clinical findings.
Rationale for correct answer:
4.During the initial stage of BPD, infants often present with signs of respiratory distress syndrome (RDS), such as tachypnea, retractions, grunting, and diffuse lung infiltrates on X-ray, before the development of chronic lung changes.
Rationale for incorrect answers:
1. Interstitial fibrosisis a feature of later stages of BPD, indicating chronic lung injury and scarring.
2. Signs of emphysemaoccur in advanced stages due to alveolar overdistension and chronic lung injury.
3. Hyperexpansion on chest X-raytypically appears in later stages, reflecting chronic air trapping and structural lung changes.
Take home points
- The early stage of BPD resembles RDS, requiring interventions similar to RDS management.
- Recognizing early-stage BPD is critical to prevent progression to chronic lung disease.
- Later stages show hyperexpansion, emphysema, and interstitial fibrosis, which indicate chronic structural damage.
- Nurses should monitor for respiratory distress, oxygen needs, and radiographic changes to guide appropriate care.
Which reason necessitates tracheostomy tube placement in long-term care of infants with bronchopulmonary dysplasia?
Explanation
Bronchopulmonary dysplasia (BPD)is a chronic lung disease resulting from lung injury in premature infants. Impaired gas exchange occurs due to alveolar damage, inflammation, and mucus accumulation, leading to hypoxemia and increased work of breathing.
Rationale for correct answer:
2.Tracheostomy is indicated when prolonged mechanical ventilation is necessaryand the infant cannot maintain adequate oxygenation or ventilation independently. It facilitates chronic respiratory support and allows the infant to transition to home care if stable.
Rationale for incorrect answers:
1. While tracheomalaciacan occur in BPD, it is not by itself an indication for tracheostomy unless it causes severe airway obstruction.
3. Gastrostomy tube placementdoes not require a tracheostomy; feeding tubes and tracheostomy are separate interventions.
4. Acute respiratory distressis managed with oxygen, medications, or short-term ventilation, not automatically with tracheostomy unless there is persistent ventilator dependence.
Take home points
- Tracheostomy is primarily indicated for long-term ventilator support in infants with BPD who cannot be weaned safely.
- It reduces risks associated with prolonged endotracheal intubation, such as subglottic stenosis and airway trauma.
- Care involves airway suctioning, tracheostomy tube care, and infection prevention.
- Nurses play a key role in monitoring respiratory status, maintaining airway patency, and educating caregivers for home care.
A nurse is caring for an 11-month-old infant diagnosed with bronchopulmonary dysplasia. The infant has a tracheostomy with 30% supplemental oxygen being provided via the tracheostomy. The infant has a decline in oxygen saturations from 96% to 87% and appears anxious and restless. Which action should be taken by the nurse?
Explanation
Bronchopulmonary dysplasia (BPD)is a chronic lung disease resulting from lung injury in premature infants. Impaired gas exchange occurs due to alveolar damage, inflammation, and mucus accumulation, leading to hypoxemia and increased work of breathing.
Rationale for correct answer:
3.The decline in oxygen saturation from 96% to 87%, along with anxiety and restlessness, suggests partial airway obstruction, likely from secretions. Immediate suctioningcan restore airway patency and improve oxygenation.
Rationale for incorrect answers:
1. Obtaining arterial blood gases (ABGs)provide information on gas exchange but do not immediately relieve airway obstruction, which is the priority.
2. Simply increasing oxygen rate from 30% to 50%will not resolve the underlying obstruction. Oxygen supplementation is supportive but secondary to clearing the airway.
4. Anxiety and restlessnessare likely secondary to hypoxemia, not primary pain. Administering medication without addressing the airway could worsen respiratory compromise.
Take home points
- In infants with BPD and tracheostomy, sudden drops in oxygen saturation require assessment for airway obstruction first.
- Priority interventions focus on clearing the airway before supportive measures such as oxygen or medications.
- Nurses must be skilled in tracheostomy suctioning, monitoring oxygen saturation, and recognizing early signs of respiratory distress.
The nurse is providing homecare instructions to the parents of a school-aged child with cystic fibrosis. Which statement by the parents indicates that they understand the treatment regimen? Select all that apply
Explanation
Cystic fibrosis (CF)is a chronic, multisystem disorder affecting the lungs, pancreas, and digestive system. Home care focuses on airway clearance, infection prevention, nutrition, and appropriate physical activity to maintain health and prevent complications.
Rationale for correct answers:
1. “We will perform chest physiotherapy and postural drainage four times a day.”Regular chest physiotherapy and postural drainage help mobilize secretions, prevent infection, and maintain lung function.
2. “We will keep our child home from school if there are any reportable communicable diseases in the school.”Children with CF have compromised pulmonary function and are at higher risk for complications from infections; avoiding exposure to communicable diseases is critical.
4. “The relay races and swimming at the school picnic next week will be good exercise for her.”Moderate exercise is beneficial for children with CF, improving pulmonary function, endurance, and overall health.
Rationale for incorrect answers:
3.“If her bowel movements are normal and her appetite is good, she does not need her pancreatic enzymes.”Pancreatic enzyme supplementation is required with every meal or snack in children with CF who have pancreatic insufficiency, regardless of bowel movement or appetite status.
5. “My child will not need any special dietary intake.”Children with CF need a high-calorie, high-protein, high-fat diet to meet increased energy demands and compensate for malabsorption.
Take home points
- Home care for CF includes regular airway clearance, infection prevention, appropriate exercise, and optimal nutrition.
- Pancreatic enzymes must be taken with all meals/snacks if pancreatic insufficiency is present.
- Caregivers should understand the importance of balancing activity with rest and preventing exposure to infections.
- Education should reinforce daily adherence to treatment and monitoring for signs of infection or nutritional issues.
A nurse is caring for a 17-year-old female client with cystic fibrosis who has been admitted to the hospital to receive I.V. antibiotic and respiratory treatment for exacerbation of a lung infection. The client has questions about her future and the consequences of the disease. Which statements about the course of cystic fibrosis are true? Select all that apply
Explanation
Cystic fibrosis (CF) is a genetic, multisystem diseasethat primarily affects the lungs and pancreas. Adolescents with CF may experience delayed puberty, reproductive challenges, and risk of diabetes. Education about the disease helps adolescents and their families understand expectations and self-management.
Rationale for correct answers:
1. Delayed pubertyis common in females with CF due to malnutrition and chronic illness, which can slow growth and development.
2. Cystic fibrosis-related diabetes (CFRD)can develop during adolescence due to pancreatic damage, and screening should begin around age 10.
4. With appropriate education and support, adolescents with CF can have normal sexual relationships, although fertility may be affected, particularly in males.
Rationale for incorrect answers:
3. Fertility can beimpaired, especially in males, and pregnancy in females with CF requires careful planning and monitoring due to health risks.
5. CF is an autosomal recessive disorder, so both males and females can inherit and carry the gene.
6. CF is progressive, and respiratory treatment frequency usually remains high or may increaseover time; it is rarely decreased.
Take home points
- Adolescents with CF may experience delayed puberty and growth delays.
- CFRD screening is essential starting around age 10.
- With education and support, normal social and sexual relationships are possible, but fertility may be affected.
- CF management remains intensive throughout life, and treatment adherence is critical.
The arterial blood gas analysis of a child with asthma shows a pH of 7.30, PCO2, of 56 mm Hg, and HCO3 of 25 mEq/L. The nurse determines that the child has which condition?
Explanation
Asthma exacerbationscan lead to airway obstruction, causing hypoventilation and carbon dioxide retention. Respiratory acidosis occurs when the lungs fail to remove CO₂ effectively, leading to low pH and elevated PCO₂. Prompt recognition and treatment are essential to prevent respiratory failure.
Rationale for correct answer:
3.The ABG shows pH 7.30 which is acidic (normal 7.35–7.45), PCO₂ 56 mm Hg which is elevated (normal 35–45 mm Hg), and HCO₃⁻ 25 mEq/L is within normal ranges (22–26 mEq/L). This pattern indicates acuterespiratory acidosis, caused by hypoventilation from airway obstruction during an asthma attack.
Rationale for incorrect answers:
1. Metabolic acidosisshows low pH with low HCO₃⁻, which is not present here.
2. Metabolic alkalosisshows elevated pH and elevated HCO₃⁻; both are not present.
4. Respiratory alkalosisshows elevated pH and low PCO₂, the opposite of this ABG.
Take home points
- ABG interpretation requires assessing pH, PCO₂, and HCO₃⁻ to determine acid-base status.
- In acute asthma exacerbations, watch for CO₂ retention, which signals respiratory acidosis and worsening airway obstruction.
- Early intervention with bronchodilators, oxygen, and monitoring is critical to prevent respiratory failure.
Which neonate is at high risk for developing bronchopulmonary dysplasia?
Explanation
Bronchopulmonary dysplasia (BPD)is a chronic lung disease most common in premature infants who require mechanical ventilation and high concentrations of oxygen. Immature lungs are vulnerable to injury, and prolonged respiratory support can lead to alveolar and airway damage, resulting in BPD.
Rationale for correct answer:
3.Extreme prematurity (≤28 weeks)and prolonged high-pressure ventilationare the primary risk factors for BPD. These factors increase susceptibility to lung injury, inflammation, and chronic oxygen dependence.
Rationale for incorrect answers:
1. A neonate born at 38 weeks’ gestation receiving 1 to 4 L oxygen during feedingsis a term infant and generally has mature lungs, and low-flow oxygen for brief periods does not typically cause BPD.
2. A premature neonate born at 36 weeks’ gestation receiving supplemental oxygenis a late preterm infant (34–36 weeks) have relatively mature lungs, and short-term oxygen therapy rarely leads to BPD.
4. A neonate born at 42 weeks’ gestation who requires treatments for respiratory syncytial virus is apost-term infant. Post-term infants may have acute respiratory illness, but they are not at high risk for BPD because their lungs are mature.
Take home points
- Extreme prematurity and mechanical ventilation are the most significant risk factors for BPD.
- BPD results from lung injury caused by oxygen toxicity and barotrauma.
- Early identification of at-risk neonates allows for preventive strategies, including minimizing ventilator pressures and oxygen exposure.
- Infants with BPD require long-term monitoring for growth, oxygen needs, and respiratory complications.
The parents of a 10-year-old child recently diagnosed with asthma ask if the child can continue to play sports. Which response is most appropriate?
Explanation
Children with well-controlled asthma can safely participate in most physical activities and sports, which help improve cardiopulmonary fitness, lung function, and overall health. Proper medication use, warm-up routines, and trigger management allow participation without increasing the risk of asthma exacerbations.
Rationale for correct answer:
4. Exercise isbeneficialfor children with asthma. With adequate control, medication adherence, and monitoring, participation in sports is safe and supports overall physical and emotional well-being.
Rationale for incorrect answers:
1. Exercise cantrigger bronchospasm(exercise-induced asthma), so precautions are necessary.
2. Limiting activity unnecessarilycan negatively impact fitness, socialization, and quality of life.
3. Swimming isoften recommendedfor children with asthma because warm, humid air reduces airway irritation.
Take home points
- Encourage regular physical activity in children with controlled asthma.
- Ensure pre-exercise medication if prescribed (e.g., short-acting bronchodilator).
- Educate on recognizing early signs of asthma during activity.
- Promote inclusion and participation in sports to support physical and psychosocial health.
Which intervention by the parents is appropriate to “allergy proof’ the home?
Explanation
Asthmain children is a chronic lung condition that causes inflammation and narrowing of the airways, making it difficult to breathe. For children with asthma or allergies, allergen avoidancein the home is critical.
Rationale for correct answer:
4.Foam rubber pillows and synthetic blanketsdo not trap dust mites and allergens like natural fibers do, making them a practical intervention for “allergy-proofing” the child’s sleeping environment.
Rationale for incorrect answers:
1. Carpetstrap dust, pollen, and other allergens, which can worsen asthma and allergy symptoms.
2. Basementsmay have higher humidity and mold, which can increase allergen exposure rather than reduce it.
3. Cleaningtwice a month is insufficient; frequent cleaning, at least weekly, is needed to maintain a low-allergen environment.
Take home points
- Use allergen-resistant bedding and synthetic materials to reduce exposure to dust mites and allergens.
- Avoid carpets, upholstered furniture, and natural-fiber pillows that can harbor allergens.
- Combine with frequent cleaning, vacuuming with HEPA filters, and humidity control for optimal asthma management.
A neonate has been diagnosed with cystic fibrosis. The nurse should educate the parents regarding which of the following dietary needs of their baby?
Explanation
Infants with cystic fibrosis (CF)often have pancreatic insufficiency, leading to malabsorption of fats and proteins. To support adequate growth and nutrition, these infants require high-calorie, nutrient-dense, and predigested formulas that are easier to absorb. This helps prevent failure to thrive and supports overall development.
Rationale for correct answer:
4.The baby must consume a predigested formula that is high in calories: Predigested (hydrolyzed) formulas are easier to absorb, and high-calorie content meets the increased energy needs of infants with CF. This is a key component of nutritional management for growth and development.
Rationale for incorrect answers:
1. The baby must receive a dose of folic acid three times each day: Routine folic acid supplementation is not a primary dietary requirement for CF unless specifically prescribed.
2. The baby must never consume any milk or milk products: Milk and milk products are not contraindicated; they may be part of the diet as long as pancreatic enzymes are provided to aid digestion.
3. The baby must receive pancreatic enzymes before bedtime every night: Pancreatic enzymes should be given with every meal and snack, not just at bedtime, to ensure proper digestion of nutrients.
Take home points
- Infants with CF require high-calorie, predigested or enzyme-supplemented formulas to meet nutritional needs.
- Pancreatic enzyme therapy should accompany each feeding to enhance nutrient absorption.
- Proper nutrition supports growth, immune function, and overall health in infants with CF.
- Caregiver education should emphasize timing of enzyme administration and monitoring weight gain and growth parameters.
A 10-year-old child has cystic fibrosis. It would be appropriate for the nurse to advise the parents that the child should be monitored yearly for which of the following illnesses?
Explanation
Cystic fibrosis (CF) is a genetic disorderthat primarily affects the lungs and digestive system, but can impact other organs as well. CF is caused by mutations in the CFTR gene, which regulates the movement of salt and water in and out of cells. These mutations lead to the production of thick, sticky mucus that clogs airways and ducts in various organs.
Rationale for correct answer:
4.Children with cystic fibrosis (CF) are at risk for developing cystic fibrosis-related diabetes (CFRD)due to damage to the pancreas, which affects both insulin production and glucose metabolism. Annual screening for diabetes is recommended starting around age 10, even in asymptomatic children, to allow for early detection and management. Early monitoring allows for timely intervention with dietary management, insulin therapy, and glucose monitoringto prevent complications.
Rationale for incorrect answers:
1. Lupusis an autoimmune disorder not specifically associated with CF.
2. Arthritisis not a routine comorbidity in children with CF.
3. Hyperthyroidismis not linked to CF, and routine screening is not indicated.
Take home points
- Children with CF should have annual screening for diabetes starting at 10 years of age.
- CFRD differs from type 1 or type 2 diabetes but requires similar management strategies.
- Early detection helps maintain nutrition, growth, and overall health in children with CF.
- Nurses should educate families on recognizing signs of hyperglycemia, including increased thirst, urination, and weight loss.
The nurse is caring for a child with cystic fibrosis who receives pancreatic enzymes. Which statement by the child's mother indicates an understanding of how to administer the supplemental enzymes?
Explanation
Children with cystic fibrosis (CF) often have pancreatic insufficiency, leading to malabsorption of fats, proteins, and carbohydrates. Pancreatic enzyme supplementationis essential to aid digestion and ensure proper nutrition.
Rationale for correct answer:
4.“The enzymes should be given at the beginning of each meal and snack”Administering enzymes with the first bite of food maximizes digestion of nutrients and reduces steatorrhea and malnutrition.
Rationale for incorrect answers:
1. “I will stop the enzymes if my child is receiving antibiotics”Antibiotics do not affect enzyme use, and stopping enzymes could lead to malabsorption and nutritional deficiencies.
2. “I will decrease the dose by half if my child is having frequent, bulky stools”Stopping or reducing enzymes without provider guidance can worsen malabsorption. Stool changes should be reported to the provider for proper dose adjustment.
3. “Between meals is the best time for me to give the enzymes”Giving enzymes between meals is ineffective, as there is little food to digest; enzymes work only when food is present.
Take home points
- Pancreatic enzymes are essential for digestion in children with CF and must be given with every meal and snack.
- Proper timing reduces gastrointestinal symptoms such as foul-smelling, greasy stools.
- Parents should never alter the dose without consulting the provider, even if stools appear normal.
- Education should include signs of malabsorption, proper dosing, and administration techniques.
An infant with a positive newborn screen for pancreatic enzyme immunoreactive trypsinogen (IRT) is scheduled to have a sweat test. After speaking to the healthcare provider, the mother asks the nurse to explain again the purpose of this test. Which response by the nurse would best reinforce the healthcare provider’s explanation?
Explanation
A sweat chloride testis the gold standard for diagnosing cystic fibrosis (CF). CF is a genetic disorder affecting chloride transport across epithelial cells, leading to abnormally salty sweat. A positive newborn screen (elevated IRT) indicates the need for confirmatory testing with a sweat test.
Rationale for correct answer:
4.“This will diagnose whether the infant has cystic fibrosis.”The sweat test directly measures chloride concentration in sweat. Values ≥60 mEq/Lin infants confirm CF, while borderline values require further testing.
Rationale for incorrect answers:
1. “This will determine if your child is dehydrated.”The sweat test does not evaluate hydration status.
2. “This will assess whether your child’s sweat glands are functioning.”While sweat is collected during the test, the purpose is not to assess gland function, but to measure chloride concentration for CF diagnosis.
3. “This will help us to identify the infectious organism.”The sweat test is not a microbiology test and cannot detect infections.
Take home points
- Sweat chloride test confirms CF after a positive newborn screen.
- Abnormal chloride levels (≥60 mEq/L) indicate cystic fibrosis.
- The test is safe and noninvasive, but requires trained personnel.
- Nurses should educate caregivers on the purpose, procedure, and interpretation of the sweat test.
Exams on Long-term Respiratory Dysfunction
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
- Describe the incidence, pathophysiology, etiology, clinical manifestations, diagnostic evaluations, and formulate therapeutic and nursing management plans for children with asthma.
- Identify and manage acute exacerbations, such as status asthmaticus.
- Understand the incidence, pathophysiology, etiology, clinical manifestations, diagnostic evaluations, and formulate therapeutic and nursing management plans for children with cystic fibrosis (CF)
- Describe the incidence, pathophysiology, etiology, clinical manifestations, diagnostic evaluations, and formulate therapeutic and nursing management plans for children with allergic rhinitis.
- Describe the incidence, pathophysiology, etiology, clinical manifestations, diagnostic evaluations, and formulate therapeutic and nursing management plans for children with obstructive sleep apnea (OSA).
- Describe the incidence, pathophysiology, etiology, clinical manifestations, diagnostic evaluations, and formulate therapeutic and nursing management plans for children with bronchopulmonary dysplasia (BPD).
- Educate children and caregivers on disease management, including proper medication administration, trigger avoidance, and promoting an allergy-free environment.
- Understand the unique challenges and nursing considerations for infants with BPD, including tracheostomy care, and for adolescents transitioning to adulthood with chronic conditions like CF.
Introduction
- Long-term respiratory dysfunction in children refers to chronic conditions affecting the lungs and airways, often leading to persistent symptoms, impaired quality of life, and potential long-term morbidity.
- These conditions range from common allergic responses to life-limiting genetic disorders. Pediatric respiratory systems have unique anatomical differences.
- Children have smaller, more compliant airways that are easily obstructed by inflammation, mucus, or foreign objects. Their short, narrow trachea and enlarged tonsil/adenoid tissue increase the risk of airway compromise.
- Infants are obligate nose breathers, and young children rely heavily on the diaphragm, making them prone to fatigue during periods of increased respiratory effort. They also have fewer alveoli and less surface area for gas exchange compared to adults.
- These vulnerabilities mean that chronic conditions like asthma, cystic fibrosis, and bronchopulmonary dysplasia present unique, complex challenges.
- Nursing care is pivotal in managing these chronic diseases, focusing on patient and family education, acute symptom control, minimizing complications, and maximizing developmental and quality-of-life outcomes.
Asthma
- Asthma is a chronic inflammatory disorder of the airways characterized by recurrent episodes of wheezing, breathlessness, chest tightness, and coughing, particularly at night or in the early morning. These episodes are usually associated with widespread, but variable, airflow obstruction that is often reversible spontaneously or with treatment.
Incidence
- It is the most common chronic disease of childhood, affecting millions of children globally.
- Incidence varies but is higher in lower socioeconomic groups and certain ethnic populations.
- It is a leading cause of school absenteeism and pediatric hospital visits.
Pathophysiology
- Airway Inflammation: Chronic inflammation, driven by IgE-mediated responses to triggers (allergens or irritants), involves immune cells (mast cells, eosinophils, T-lymphocytes).
- Bronchoconstriction (Bronchospasm): Smooth muscles surrounding the airways constrict acutely in response to inflammatory mediators (e.g., histamine, leukotrienes), leading to narrowing.
- Increased Mucus Production: Mucosal edema and hypersecretion of thick, tenacious mucus further plug the airways.
The combination of these three factors leads to airway hyper-responsiveness (exaggerated bronchoconstriction in response to various stimuli) and airflow obstruction, primarily affecting the expiratory phase, trapping air in the alveoli (air trapping).
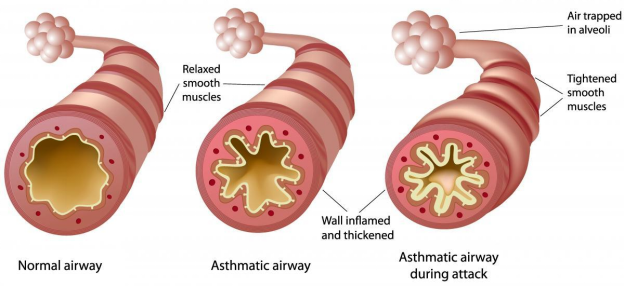
Etiology and Triggers
The exact etiology is multifactorial, involving a complex interplay of genetic predisposition (a family history of atopy or asthma is a major risk factor) and environmental factors.
|
Etiology/Triggers |
Examples |
|
Allergens |
Pollen, dust mites, mold, animal dander, cockroach droppings. |
|
Irritants |
Tobacco smoke (most significant), air pollution, strong odors, cleaning products. |
|
Infections |
Viral upper respiratory infections (most common trigger for exacerbations in children). |
|
Exercise |
Especially in cold or dry air. (Exercise-induced bronchoconstriction/asthma). |
|
Other |
Cold air, strong emotions/stress (crying, laughing), gastroesophageal reflux (GERD). |
Clinical Manifestations
Symptoms often vary in severity and frequency:
- Classic Triad: Cough (non-productive, hacking, worse at night), Wheezing (high-pitched musical sound on expiration), and Dyspnea (shortness of breath).
- Chest tightness: More common in older children).
- Prolonged expiratory phase: The time the child takes to exhale is longer than normal.
- Use of accessory muscles: Retractions, nasal flaring in infants/toddlers.
- Tachypnea, Tachycardia.
Restlessness/Irritability: These are early signs of hypoxia.
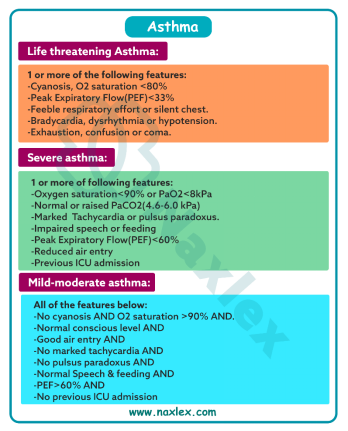
Diagnostic Evaluation
- History and Physical Exam: Recurrent symptoms, family history, and characteristic lung sounds (wheezing).
- Pulmonary Function Tests (PFTs)/Spirometry (usually for children ≥5−6 years): Measures forced expiratory volume in 1 second (FEV1) and forced vital capacity (FVC). A significant reversibility (e.g., 12% or greater improvement in FEV1 after a bronchodilator) supports the diagnosis.
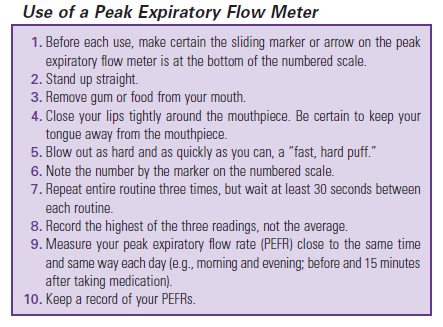
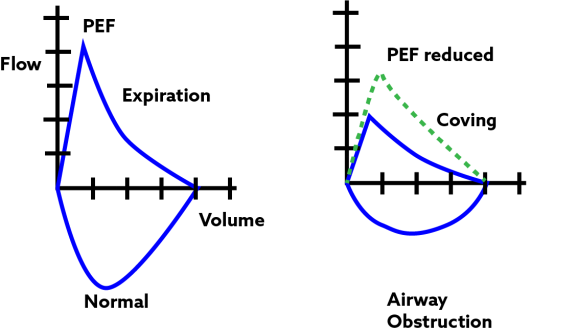
- Peak Expiratory Flow Rate (PEFR): Measured using a Peak Flow Meter. Compares the child's result to their personal best or predicted normal. Used for daily monitoring and in the Asthma Action Plan (Green, Yellow, Red Zones).
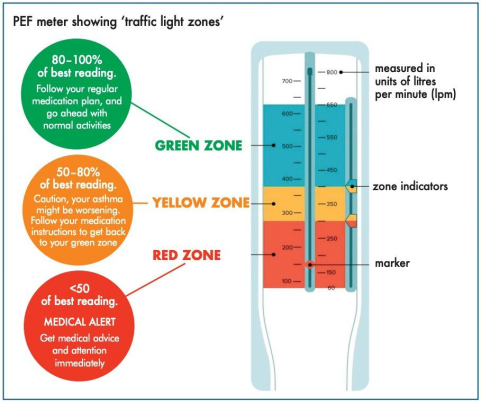
- Allergy Testing (Skin or Blood): To identify specific triggers.
- Arterial Blood Gases (ABGs): Not routine, but critical in severe exacerbations (status asthmaticus).
- Early: Respiratory Alkalosis (↓PaCO2, ↑pH) due to hyperventilation (compensatory mechanism).
- Worsening/Fatigue: Normalizing PaCO2 (This is a danger sign indicating respiratory fatigue and impending failure, as the child is no longer able to hyperventilate.
- Late/Failure: Respiratory Acidosis (↑PaCO2, ↓pH) indicating CO2 trapping and poor gas exchange.
Therapeutic Management
Management is guided by the severity and frequency of symptoms, following a stepwise approach (e.g., National Asthma Education and Prevention Program guidelines).
- Pharmacologic:
- Quick-Relief (Rescue) Medications:
- Short-Acting Beta Agonists (SABAs): Albuterol (Salbutamol). Used for acute symptoms and before exercise. Relaxes bronchial smooth muscle.
- Long-Term Control (Preventer) Medications:
- Inhaled Corticosteroids (ICS): The most effective long-term control therapy. Reduces inflammation and hyper-responsiveness. (e.g., Fluticasone, Budesonide).
- Long-Acting Beta Agonists (LABAs): Used only in combination with an ICS for moderate/severe persistent asthma. (e.g., Salmeterol, Formoterol).
- Leukotriene Modifiers: Oral medications (e.g., Montelukast). Blocks inflammatory leukotrienes.
- Combination Inhalers: ICS + LABA (e.g., Budesonide/Formoterol).
- Quick-Relief (Rescue) Medications:
Step-wise Approach for Asthma Management
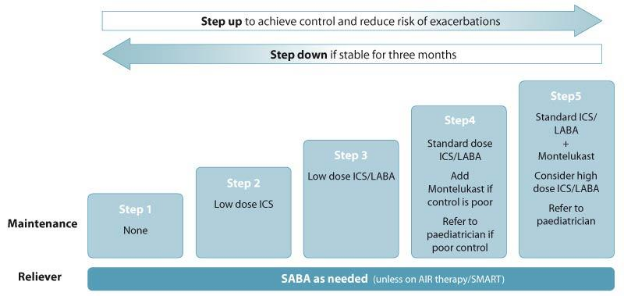
Prevention and Nursing Care Management
I. Asthma Action Plan
- Crucial for self-management. Color-coded zones based on symptoms and PEFR to guide treatment (medication, when to call the provider, when to go to the Emergency Department).
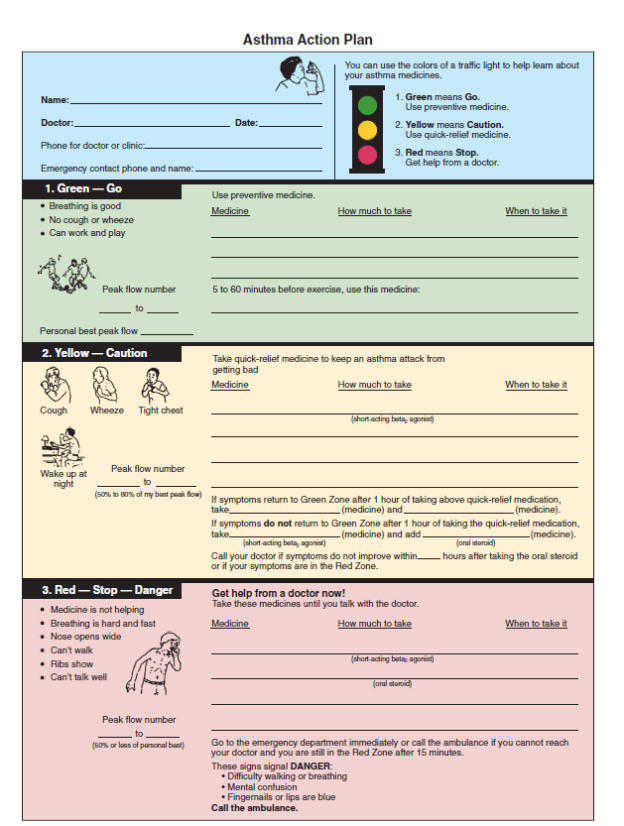
II. Proper MDI Use -
A Metered-Dose Inhaler (MDI) should almost always be used with a spacer/holding chamber for children to ensure proper drug delivery and minimize side effects (like thrush from ICS).
MDI Use with Spacer
MDI Use without Spacer
1. Shake the inhaler well and remove the cap.
1. Shake the inhaler well and remove the cap.
2. Insert the mouthpiece of the MDI into the spacer end.
2. Tilt the head back slightly.
3. Place the mask (for infants/toddlers) or mouthpiece (older children) over the face/in the mouth, ensuring a tight seal.
3. Breathe out gently (empty lungs).
4. Press the canister once to release the medication into the spacer.
4. Place the mouthpiece 1-2 inches in front of the mouth or seal lips around the mouthpiece.
5. Slowly inhale 5-10 deep breaths from the spacer, holding the last breath for 10 seconds if possible. (For mask, hold for 30 seconds or 5-10 breaths).
5. Start to breathe in slowly and deeply through the mouth, and press the canister once.
6. Wait 30-60 seconds between puffs if more than one is ordered.
6. Continue to inhale slowly for 3-5 seconds, then hold breath for 10 seconds if possible.
A spacer improves lung deposition and reduces oropharyngeal deposition.
This is less effective delivery; requires perfect coordination.
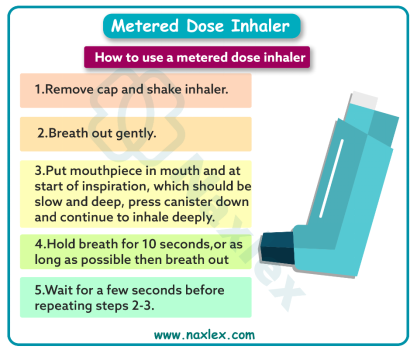
III. Ways to Increase Expiratory Phase
The goal is to encourage a prolonged, forced expiration to help clear trapped air and secretions.
- Blowing a Pinwheel or Bubbles: Fun, simple activities that require a sustained expiratory effort.
- Playing a wind instrument (e.g., harmonica, recorder).
- Blowing up balloons (for older, stable children).
- "Huffy" or "Foggy" breathing exercises: Exhaling as if trying to fog up a mirror.
IV. Home Allergy-Free Environment
Education focuses on eliminating common triggers:
- Dust Mites: Use allergen-proof covers on mattresses, box springs, and pillows. Wash bedding weekly in hot water (≥130∘F). Remove carpets, or vacuum with a HEPA filter vacuum.
- Pets: Keep pets out of the child's bedroom and off upholstered furniture. Regular bathing of pets may help but is less effective than removal.
- Mold: Fix leaks, use a dehumidifier to keep relative humidity below 50%.
- Smoke: No smoking in the home or car. Avoid wood-burning stoves/fireplaces.
- Pollen: Keep windows and doors closed, especially during high pollen seasons. Use air conditioning.
Status Asthmaticus
- Definition: A severe, life-threatening asthma episode that is refractory to initial treatment such as initial SABA treatments.
- Manifestations: Severe respiratory distress, poor air movement ("silent chest"), impending respiratory failure indicated by cyanosis, decreased level of consciousness, and normalizing or rising PaCO2.
- Nursing Care:
- Continuous Monitoring: SpO2, HR, RR, LOC, and ABGs.
- Oxygen: Administer to maintain SpO2≥92%.
- Medications: Continuous or frequent nebulized SABA (Albuterol/Salbutamol), IV or oral Systemic Corticosteroids (e.g., Methylprednisolone or Prednisone), and consider IV Magnesium Sulfate (a potent smooth muscle relaxant).
- Airway Management: Prepare for intubation and mechanical ventilation if respiratory failure is imminent.
Nursing Insight: A "silent chest" following wheezing is a dire emergency! It means air movement has stopped due to severe airway obstruction and requires immediate, aggressive intervention.
Cystic Fibrosis
- Cystic Fibrosis is an autosomal recessive genetic disease that affects the exocrine glands, leading to the production of abnormally thick and sticky mucus that obstructs ducts and passages in multiple body systems, most notably the respiratory, digestive, and reproductive systems.
Incidence
- It is the most common fatal inherited disease in Caucasians in the United States.
- Improvements in treatment have significantly extended the median life expectancy to ∼40−50 years.
Pathophysiology / Inheritance Pattern
- Inheritance Pattern: Autosomal Recessive.
- The child must inherit two copies of the mutated gene (one from each carrier parent) to have CF.
- If both parents are carriers (Cc), there is a 25% (1 in 4) chance with each pregnancy that the child will have CF (cc).
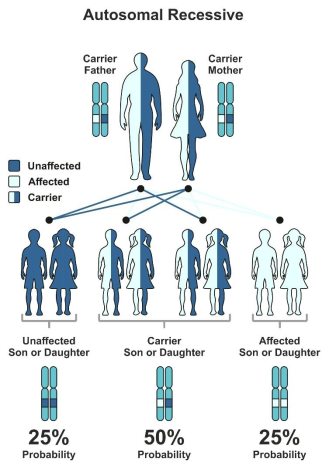
Etiology
A mutation in the Cystic Fibrosis Transmembrane Conductance Regulator (CFTR) gene on chromosome 7.
- The CFTR protein acts as a chloride ion channel in epithelial cells.
- In CF, the defective CFTR protein fails to transport chloride out of the cells.
This lack of chloride secretion and increased sodium and water reabsorption into the cells leads to dehydrated, viscous secretions in the sweat ducts, lungs, pancreas, liver, and intestine.
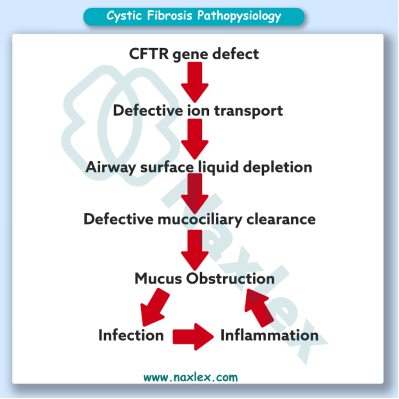
Clinical Manifestations per Body System
- Respiratory:
- Thick mucus obstructs bronchioles, leading to air trapping, atelectasis, and recurrent infections (chronic cough, wheezing, barrel chest, clubbing).
- Infections often involve specific bacteria, like Staphylococcus aureus and later Pseudomonas aeruginosa.
- Chronic colonization leads to bronchiectasis (irreversible dilation and destruction of the bronchial walls).
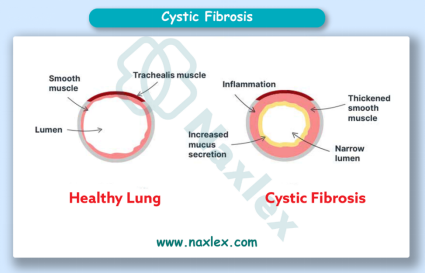
- Gastrointestinal (Pancreas):
- Thick secretions block the pancreatic ducts, preventing the release of digestive enzymes (lipase, amylase, protease) into the small intestine.
- Results in malabsorption of fats, proteins, and fat-soluble vitamins (A, D, E, K).
- Clinical Signs: Steatorrhea (foul-smelling, fatty, bulky stools), failure to thrive, malnutrition.
- Can lead to CF-related diabetes (CFRD) due to pancreatic damage.
- Gastrointestinal (Intestine/Liver):
- Meconium Ileus: The initial presentation in ∼10−20% of newborns; thick meconium causes intestinal obstruction.
- Biliary obstruction leading to focal biliary cirrhosis.
- Integumentary/Sweat Glands:
- Defective CFTR in the sweat ducts prevents reabsorption of chloride and sodium.
- Results in abnormally high concentrations of salt in the sweat.
- Clinical Sign: Parents often report their child "tastes salty" when kissed.
- Reproductive:
- Males are typically infertile due to congenital bilateral absence of the vas deferens.
- Females have reduced fertility due to thickened cervical mucus.
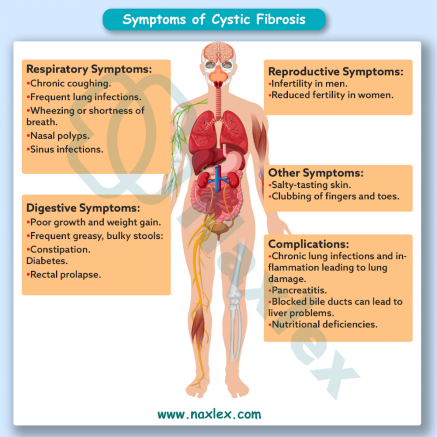
Diagnostic Evaluation
- Newborn Screening: All U.S. states screen for CF. Initial test measures Pancreatic Enzyme Immunoreactive Trypsinogen (IRT) in a blood spot; high IRT indicates further testing.
- Sweat Chloride Test (Gold Standard): Measures the chloride concentration in the sweat.
- Procedure: Pilocarpine iontophoresis is used to stimulate localized sweating, and the sweat is collected and analyzed.
- Diagnostic Levels:
- Positive/Diagnostic: ≥60 mEq/L
- Intermediate: 30−59 mEq/L (requires further genetic testing)
- Normal: ≤29 mEq/L
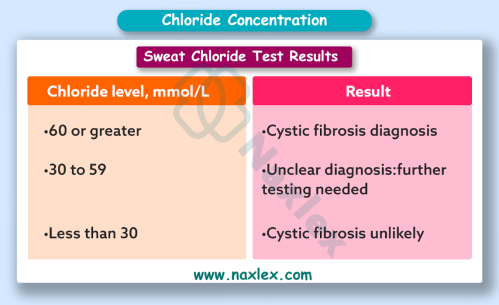
- Stool Analysis: Measures fecal fat content to confirm fat malabsorption.
Therapeutic Management
I. Chest Physiotherapy (CPT) and Airway Clearance
- The cornerstone of management. Helps to mobilize and clear thick mucus from the airways.
- Techniques: Percussion, vibration, postural drainage, High-Frequency Chest Wall Oscillation (HFCWO) vest, positive expiratory pressure (PEP) mask, and active cycle of breathing techniques.
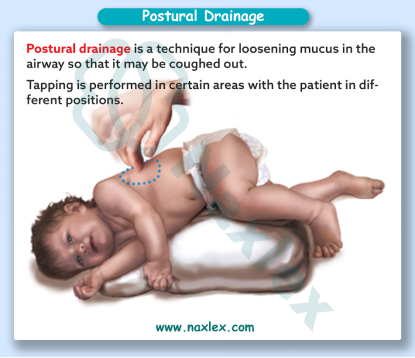
- Appropriate Timings: 1-3 times per day (and sometimes more during exacerbations), usually before meals or at least one hour after meals to avoid regurgitation/vomiting.
- Medications: Dornase Alfa (Pulmozyme) decreases mucus viscosity and hypertonic saline mobilizes secretions.
II. Nutrition
- High-Calorie, High-Protein Diet: To counteract malabsorption and meet increased metabolic demands due to chronic infection/work of breathing.
- Fat-Soluble Vitamin Supplementation: Daily supplements of A, D, E, K.
III. Pancreatic Enzyme Replacement Therapy (PERT)
- Enzyme capsules containing lipase, amylase, protease must be taken with all meals and snacks to digest food and absorb nutrients.
- How and When to Take Them: Swallow capsules whole, or open and sprinkle on small amount of acidic food (e.g., applesauce) immediately before eating. Do not chew or mix with alkaline foods.
- Dosing: Individually titrated based on weight, fat intake, and stool consistency (goal is 1-2 formed stools/day).
IV. Treatment of Constipation/Distal Intestinal Obstruction Syndrome (DIOS)
- DIOS is a partial or complete obstruction of the small intestine or ileocecal valve by thick stool and mucus.
- Treatment: Oral laxatives like Polyethylene Glycol (Miralax), osmotic solutions, and sometimes enemas are used to relieve the obstruction.
V. Lung Transplant
- Considered for patients with advanced lung disease, typically when FEV1<30% of predicted.
Complications
- Respiratory complications: Chronic lung infections, bronchiectasis, respiratory failure, pneumothorax, hemoptysis, and allergic bronchopulmonary aspergillosis (ABPA).
- Nutritional complications: Malnutrition, growth failure, vitamin deficiencies, and osteoporosis.
- Reproductive complications: Infertility in males due to absence of the vas deferens.
- Psychosocial complications: Depression, anxiety, social isolation, and decreased quality of life.
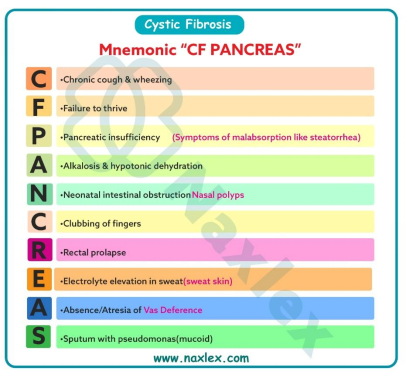
Nursing Care Management
- Infection Control: Strict hand hygiene; patients with CF should be separated from one another ("Six-foot rule" or distance ≥6 feet) to prevent cross-contamination of resistant organisms.
- Monitor Nutritional Status: Daily weights, growth charts, BMI, and serum albumin.
- Hydration: Encourage fluids to thin secretions.
- Psychosocial Support: CF is a major chronic illness; support groups and mental health resources are vital.
Transitioning to Adulthood
- Focus: Shifting responsibility for care from parent/guardian to the adolescent/young adult.
- Goals: Medication self-administration, scheduling CPT, managing appointments, understanding insurance, discussing fertility and reproductive health.
Nursing Insight: Due to the risk of Pseudomonas transmission, patients with CF should never share equipment like nebulizers and should maintain a physical distance from others with CF in healthcare settings.
Allergic Rhinitis
- Allergic Rhinitis, often called "hay fever," is an IgE-mediated inflammatory condition of the nasal mucosa, typically triggered by exposure to inhalant allergens.
Incidence
- Very common, affecting 10−30% of the world's population.
- Onset often occurs in childhood or adolescence.
Pathophysiology
- Sensitization: Initial exposure to an allergen leads to the production of IgE antibodies, which bind to mast cells in the nasal mucosa.
- Re-exposure: Subsequent exposure causes the allergen to bind to the IgE on mast cells.
- Mediator Release: Mast cells release inflammatory mediators, primarily histamine, causing vasodilation, increased capillary permeability, and stimulation of sensory nerves.
- Symptoms: This results in edema, rhinorrhea, sneezing, and pruritus.

Etiology and Triggers
- Etiology: Genetic predisposition including a family history of atopy (allergic rhinitis, asthma, and eczema).
- Triggers:
- Seasonal (SAR): Pollens (trees, grasses, weeds) and outdoor molds.
- Perennial (PAR): Indoor allergens like dust mites, animal dander, indoor molds, and cockroach droppings.
Clinical Manifestations
- Nasal Symptoms: Clear, watery rhinorrhea, repeated sneezing (paroxysmal), nasal congestion/stuffiness, and pruritus of the nose, palate, and throat.
- Ocular Symptoms: Itchy, red, watery eyes (allergic conjunctivitis).
- Systemic Symptoms: Fatigue, irritability, and headache.
- Physical Signs:
- Allergic Salute/allergic nasal crease: Upward rubbing of the nose with the palm, creating a transverse crease across the bridge of the nose.
- Allergic Shiners: Dark circles/edema beneath the eyes.
- Dennie-Morgan lines: These are extra creases or double folds of skin that appear directly below the lower eyelid, seen in clients with conditions such as allergic rhinitis.
Facial Signs of Allergic Rhinitis
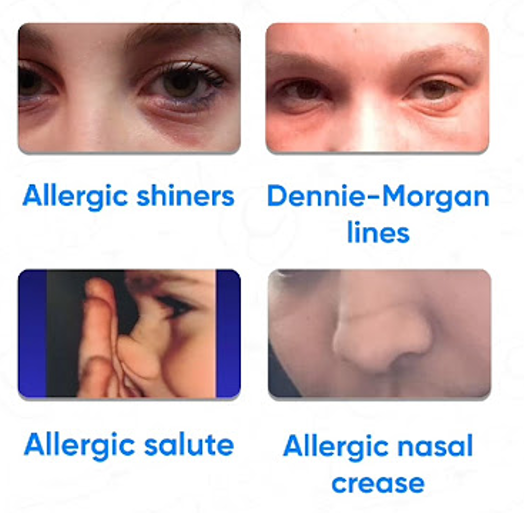
- Nasal Mucosa: Pale, boggy, and swollen.
- Postnasal Drip: May cause a chronic cough.
Diagnostic Evaluation
- Clinical History and Physical Exam: Most diagnoses are based on a history of recurrent symptoms and physical findings.
- Allergy Testing: Skin Prick Test or blood test (measuring specific IgE levels) to identify the specific allergens.
Therapeutic Management
- Allergen Avoidance
- Pharmacologic:
- Intranasal Corticosteroids (e.g., Fluticasone): Most effective single treatment for all major symptoms. Used daily.
- Antihistamines: Second-generation oral (e.g., Cetirizine, Loratadine) are preferred due to less sedation than first-generation (e.g., Diphenhydramine).
- Leukotriene Modifiers (e.g., Montelukast): Effective for co-existing asthma and rhinitis.
- Allergen Immunotherapy (Allergy Shots/Sublingual Tablets): Long-term treatment involving gradual exposure to allergens to desensitize the immune system.
Prevention and Nursing Care Management
- Prevention: Environmental control is key similar to asthma environment section:
- Reduce dust mites and pet dander.
- Keep windows closed during high pollen season.
- Nursing Care:
- Education: Teach proper technique for intranasal corticosteroid sprays (aim spray away from the nasal septum to prevent irritation/epistaxis).
- Symptom Management: Encourage nasal saline flushes/washes to rinse allergens from the nasal mucosa.
- Anticipatory Guidance: Counsel parents on the difference between AR symptoms such as clear discharge and itching) and a cold symptoms including thick discharge, fever, and sore throat.
Nursing Insight:
To distinguish allergies from colds, be aware that:
- Allergies occur repeatedly and are often seasonal.
- Allergies are seldom accompanied by fever.
- Allergies often involve itching in the eyes and nose.
- Allergies usually trigger constant and consistent bouts of sneezing.
- Allergies are often accompanied by ear and eye problems.
Nursing Insight: Uncontrolled AR can worsen asthma control and may predispose a child to recurrent otitis media due to Eustachian tube dysfunction. Treating AR is part of comprehensive asthma care.
Obstructive Sleep Apnea
- Obstructive Sleep Apnea in children is characterized by recurrent episodes of partial or complete upper airway obstruction during sleep, leading to reduced ventilation and disrupted sleep patterns.
Incidence
- Estimated to affect 1−5% of children.
- Most prevalent in preschool-aged children (2−8 years).
Pathophysiology
- During sleep, the muscles that hold the pharynx open naturally relax.
- In children with OSA, this relaxation, combined with a narrowed airway most commonly due to adenotonsillar hypertrophy, leads to partial (hypopnea) or complete (apnea) airway collapse.
- The obstruction causes a drop in blood oxygen saturation (hypoxemia) and a rise in CO2 (hypercapnia).
- The brain briefly wakes the child to restore muscle tone and open the airway, often accompanied by a snort or gasp, before falling back to sleep.
- This cycle severely disrupts sleep architecture, leading to daytime dysfunction.
Pathophysiology of Obstructive Sleep Apnea
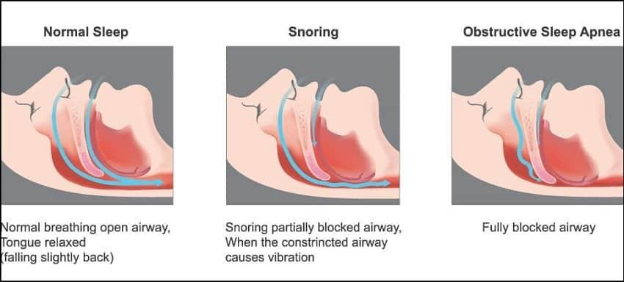
Etiology and Triggers
- Primary Etiology: Adenotonsillar Hypertrophy is the main cause in children.
Adenotonsillar Hypertrophy
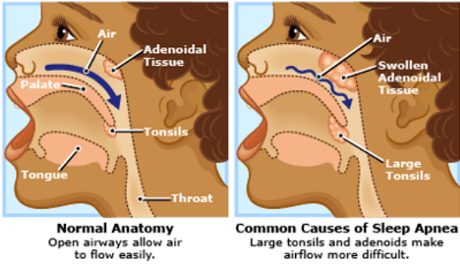
- Risk Factors/Triggers:
- Obesity is increasingly common.
- Craniofacial abnormalities (e.g., Down syndrome, Pierre Robin sequence) or neuromuscular disorders.
- Allergic Rhinitis/Chronic Nasal Congestion worsens obstruction.
Clinical Manifestations
- Nighttime Symptoms:
- Loud, habitual snoring often with pauses, snorts, or gasps.
- Labored/mouth breathing during sleep.
- Restless sleep including sleeping in unusual positions, like hyperextended neck.
- Night sweats, enuresis.
- Daytime Symptoms (often different from adults):
- Behavioral/Neurocognitive Issues: Hyperactivity, ADHD-like symptoms, aggression, poor concentration, and school performance.
- Daytime Sleepiness is less common than in adults but can occur.
- Morning headaches due to nocturnal CO2 retention.
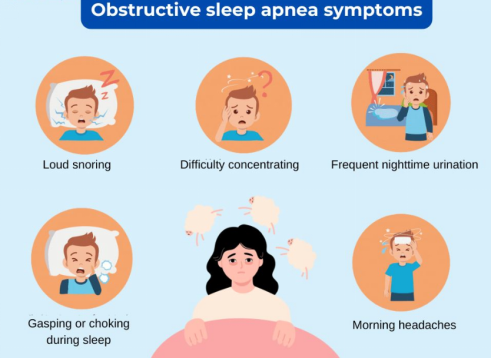
Diagnostic Evaluation
- Gold Standard: Polysomnography (Sleep Study): An overnight study in a sleep lab that monitors EEG (brain waves), EOG (eye movement), EMG (muscle activity), breathing effort, airflow, HR, and SpO2.
- Apnea-Hypopnea Index (AHI): The number of apneas and hypopneas per hour of sleep; used to grade severity.
Therapeutic Management
- First-Line Treatment for most children with enlarged tonsils/adenoids: Adenotonsillectomy (T&A). Often curative.
- Continuous Positive Airway Pressure (CPAP): Used when T&A is not indicated or ineffective, especially in children with obesity or craniofacial syndromes. The machine delivers pressurized air via a mask to keep the airway open.
- Weight Loss: Essential for obese children.
- Allergy Treatment: Intranasal corticosteroids may be used if AR contributes to nasal congestion.
Prevention and Nursing Care Management
- Prevention: Maintaining a healthy weight; management of allergies.
- Nursing Care:
- Post-T&A Care: Monitoring for hemorrhage indicated by frequent swallowing/clearing throat is a sign, pain control, and encouraging cool liquids.
- CPAP Adherence: Education and support for families regarding mask fitting and compliance, which can be challenging for young children. Start slowly and make it a routine.
Nursing Insight: Always take a child's report of habitual snoring seriously. Unlike adults, OSA in children often presents as hyperactivity or inattention, not just daytime sleepiness.
Bronchopulmonary Dysplasia
- Bronchopulmonary Dysplasia is a chronic lung disease that affects premature infants. It results from damage to the lungs caused by mechanical ventilation, oxygen therapy, and inflammation, leading to abnormal lung development.
Bronchopulmonary Dysplasia
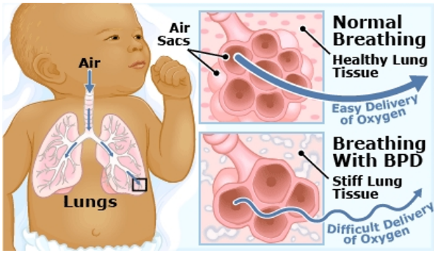
Incidence
- Primarily affects very premature infants born before 30 weeks gestation and those with low birth weight.
Pathophysiology
- Immature Lungs: Premature infants have lungs with fewer, larger alveoli and less developed supporting vasculature.
- Initial Injury: The immature lungs, often with insufficient surfactant, are injured by factors like high oxygen concentrations (causing free radical damage) and positive pressure from mechanical ventilation (barotrauma/volutrauma).
- Abnormal Development: This injury leads to chronic inflammation, scarring, and arrested alveolar and vascular development.
- Clinical Outcome: The lungs become less elastic, and the airways are prone to collapse, resulting in chronic respiratory distress and oxygen dependence.
Etiology and Triggers
- Primary Etiology: Prematurity and low birth weight.
- Contributory Factors: Respiratory Distress Syndrome (RDS), mechanical ventilation, prolonged high-concentration oxygen therapy, pre/postnatal infection (sepsis, pneumonia).
- Triggers for Exacerbation: Respiratory infections (RSV, influenza), fluid overload.
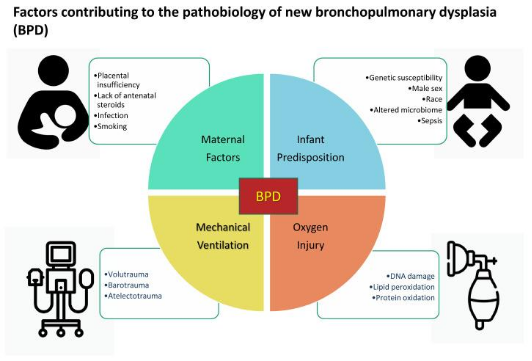
Clinical Manifestations
- Persistent respiratory distress including signs such as tachypnea, retractions, and nasal flaring.
- Oxygen dependence often for weeks or months after the expected due date.
- Abnormal Chest X-ray: Areas of hyperinflation and fibrosis/atelectasis.
- Pulmonary Hypertension and potential for Cor Pulmonale (right-sided heart failure).
- Growth Failure/Failure to Thrive due to high caloric demands from the work of breathing.
Classification of Bronchopulmonary Dysplasia (BPD) based on radiological features and clinical manifestations
|
Stage |
Age (Postnatal Days) |
Radiological Features |
Clinical Manifestations |
Key Pathophysiological Features |
|
Stage I (Acute Phase) |
1–3 days |
- Diffuse fine granular or ground-glass appearance resembling hyaline membrane disease (RDS) |
- Respiratory distress soon after birth |
- Surfactant deficiency |
|
Stage II (Early Injury Phase) |
4–10 days |
- Coarse, patchy infiltrates |
- Persistent oxygen dependency |
- Lung injury due to oxygen toxicity and barotrauma |
|
Stage III (Established Injury Phase) |
10–20 days |
- Cystic lucencies and linear densities giving a “bubbly” or sponge-like appearance |
- Continued oxygen need |
- Alveolar simplification |
|
Stage IV (Chronic Phase / Established BPD) |
>28 days (or 36 weeks postmenstrual age) |
- Marked hyperinflation and cystic changes |
- Chronic respiratory insufficiency |
- Chronic lung disease with fibrosis |
Diagnostic Evaluation
- Clinical Definition: Requirement for supplemental oxygen for at least 28 days of life, typically confirmed at 36 weeks post-menstrual age.
- Chest X-ray: Diffuse areas of hyperinflation, scarring, and atelectasis.
Therapeutic Management
- Respiratory Support: Minimal effective oxygen, gentle ventilation, and gradual weaning.
- Medications:
- Diuretics (e.g., Furosemide): To treat pulmonary edema and improve lung compliance.
- Bronchodilators: To decrease airway resistance.
- Inhaled/Systemic Corticosteroids: To reduce inflammation (use is cautious due to side effects).
- Nutrition: High-calorie feeds/supplementation to support growth.
- Infection Prevention: RSV prophylaxis (e.g., Palivizumab/Synagis) is crucial for at-risk infants.
Nursing Care Management
- Oxygen Management: Careful monitoring and titration of O2 to prevent retinopathy of prematurity or oxygen toxicity, while maintaining target SpO2.
- Fluid Management: Strict intake and output monitoring to prevent fluid overload and pulmonary edema (a common complication).
- Developmental Care: Minimize stress, clustering care, and promoting adequate rest.
- Tracheostomy Care (for severe BPD needing long-term ventilation/airway support):
- Suctioning: Sterile technique. Suction only as needed (not routinely). Use appropriate length/pressure. Pre-oxygenate and limit suction pass to <5−10 seconds.
- Cleaning: Clean around the stoma daily with saline or mild soap and water. Ensure the faceplate and skin are dry. Inspect the skin for breakdown.
- Dressing/Tie Change: Change the tracheostomy tie/holder daily or when soiled (requires a two-person technique for safety, one to hold the tube, one to change the tie.
- Emergency: Keep a replacement trach tube of the same size and one smaller size at the bedside. Know the facility's procedure for tube dislodgement or occlusion.
- Discharge Planning: Extensive education for home care, equipment use (ventilator/trach supplies/oxygen), and emergency protocols.
Nursing Insight: Infants with BPD are at high risk for RSV and other respiratory infections, which can lead to rapid deterioration. Vaccination (for age) and strict infection control measures are non-negotiable.
Summary
- Long-term respiratory dysfunctions in children, such as Asthma, Cystic Fibrosis, Allergic Rhinitis, Obstructive Sleep Apnea, and Bronchopulmonary Dysplasia, represent a diverse group of chronic conditions requiring highly specialized and family-centered nursing care.
- Management focuses on preventing acute exacerbations, controlling symptoms through pharmacologic and physical therapies, optimizing nutrition and growth, providing extensive patient/family education, and facilitating a smooth transition to adult care.
- Nurses serve as vital educators, monitors, and emotional supports, helping children live full lives despite chronic disease.
- Asthma requires meticulous trigger avoidance and adherence to a stepwise pharmacologic regimen. The core nursing goal is ensuring proper delivery of medication (especially MDI with a spacer) and teaching families to use the Asthma Action Plan for timely intervention.
- Cystic fibrosis (CF) management is resource-intensive, centered on airway clearance and aggressive nutritional support.
- Allergic rhinitis (AR), though often milder, its chronicity impacts sleep, concentration, and asthma control. Effective management hinges on consistent use of intranasal corticosteroids and simple, effective environmental control measures.
- Obstructive sleep apnea (OSA) primarily manifests in children as daytime behavioral and neurocognitive issues.
- Bronchopulmonary dysplasia (BPD), a disease of prematurity requiring complex, long-term support. Nursing care prioritizes gentle oxygen weaning, strict fluid management, and extensive home health education, particularly for patients requiring a tracheostomy, where competent suctioning and emergency tube change skills are life-saving.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Long-term Respiratory Dysfunction
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


