Please set your exam date
Generalized Anxiety Disorder
Study Questions
Practice Exercise 1
According to psychodynamic theory, what factors contribute to the development of generalized anxiety disorder? Select all that apply.
Explanation
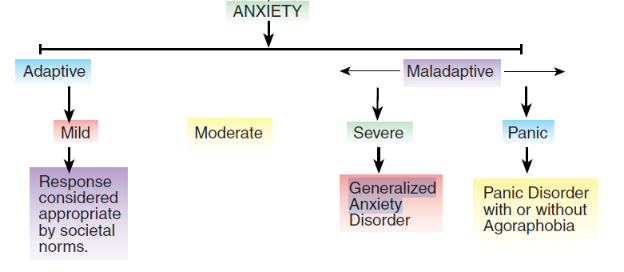
Generalized anxiety disorderis characterized by excessive, persistent worry that is difficult to control and affects daily functioning. Psychodynamic theory attributes its development to unconscious conflicts, impaired ego functioning, and maladaptive defense mechanisms. Early relational disruptions and poor emotional regulation contribute to vulnerability. The ego fails to mediate between internal drives and external reality, leading to anxiety symptoms.
Rationale for correct answers
1.Unresolved conflictsbetween parent and child create internal tension and unconscious fear, which manifest as chronic anxiety in adulthood.
2.Delayed egodevelopment impairs the ability to regulate impulses and manage stress, increasing vulnerability to anxiety disorders.
3.Defense mechanismsused excessively suppress emotional conflict but prevent resolution, leading to persistent anxiety symptoms.
Rationale for incorrect answers
4.High self-esteem reflects healthy ego strength and adaptive functioning, which are protective against anxiety disorders.
5.Rational problem-solving is a mature coping strategy that reduces anxiety by resolving stressors rather than avoiding them.
Take Home Points
- Psychodynamic theory links generalized anxiety disorder to unconscious conflict and impaired ego development.
- Excessive use of defense mechanisms prevents emotional resolution and perpetuates anxiety.
- Early relational disruptions, especially with caregivers, contribute to long-term anxiety vulnerability.
- Adaptive coping strategies and ego strength are protective against anxiety disorders.
Which brain structure is most involved in the regulation of emotional responses and is implicated in the pathophysiology of generalized anxiety disorder?
Explanation
Generalized anxiety disorderis a chronic psychiatric condition characterized by excessive, uncontrollable worry and heightened autonomic arousal. The hippocampus, amygdala, and prefrontal cortexare central to emotional regulation and fear processing. The hippocampus modulates contextual memory and stress responses via the hypothalamic-pituitary-adrenal axis. Neuroimaging consistently shows volume reduction and altered connectivity in the hippocampus in anxiety disorders.
Rationale for correct answers
2. Hippocampus.The hippocampus regulates stress responses and encodes emotional memory. Its dysfunction contributes to persistent worry and impaired fear extinction.
Rationale for incorrect answers
1.The occipital lobe processes visual stimuli and is not involved in emotional regulation or anxiety pathophysiology.
3.The cerebellum coordinates motor activity and balance; while it has emerging roles in cognition, it’s not central in anxiety.
4.The medulla oblongata controls autonomic functions like respiration and heart rate, not emotional processing or anxiety regulation.
Take Home Points
- The hippocampus is key in emotional memory and stress regulation, making it central in generalized anxiety disorder.
- Anxiety disorders show structural and functional changes in the hippocampus and amygdala.
- Occipital lobe and cerebellum are not primary structures in emotional regulation.
- Medulla oblongata governs autonomic functions, not emotional or cognitive processing.
According to cognitive theory, anxiety is maintained primarily due to:
Explanation
Cognitive theory of anxietyexplains that maladaptive thought patterns and negative interpretations of neutral stimuli perpetuate anxiety. Individuals with anxiety often exhibit automatic negative thoughts, catastrophic misinterpretations, and cognitive distortionsthat reinforce fear responses and avoidance behaviors.
Rationale for correct answers
2. Distorted thinking.Cognitive theory emphasizes that dysfunctional appraisals and irrational beliefs sustain anxiety by reinforcing perceived threats and avoidance.
Rationale for incorrect answers
1.Serotonin overactivity is implicated in mood disorders but is not the primary mechanism in cognitive theory’s explanation of anxiety.
3.While past trauma may contribute to anxiety, cognitive theory focuses on current thought patterns rather than stored memories.
4.Dopamine excess is more relevant to psychotic disorders and reward pathways, not central to anxiety maintenance in cognitive theory.
Take Home Points
- Cognitive theory attributes anxiety to distorted thinking and maladaptive interpretations of neutral or ambiguous stimuli.
- Serotonin and dopamine imbalances are biological models, not cognitive explanations for anxiety.
- Trauma may initiate anxiety but does not explain its maintenance in cognitive theory.
- Cognitive behavioral therapy targets dysfunctional thought patterns to reduce anxiety symptoms.
Which of the following are biological factors associated with generalized anxiety disorder? Select all that apply.
Explanation
GADis a chronic psychiatric condition characterized by persistent, excessive, and uncontrollable worry. It is associated with functional impairment in multiple neurotransmitter systems. Norepinephrine, serotonin, and GABAdysregulation play key roles in its pathophysiology. Increased sympathetic tone, impaired inhibition, and faulty modulation of emotional response circuits are observed. Benzodiazepines and SSRIs target these neurotransmitters to correct imbalances.
Rationale for correct answers
2. Overactive norepinephrinepathways are implicated in hyperarousal symptoms in GAD, including restlessness, irritability, and increased startle response.
3. Low serotoninlevels are associated with poor regulation of mood and anxiety, contributing to excessive worry and persistent anxious affect.
5. Decreased GABAactivity results in reduced inhibition of neural circuits, leading to heightened excitability and anxiety symptoms seen in GAD.
Rationale for incorrect answers
1.Elevated blood lactateis more closely associated with panic disorder than GAD; it can provoke panic attacks but is not a key factor in GAD.
4.Increased dopamineis not characteristic of GAD; excessive dopamine activity is more linked with psychotic disorders and some manic states, not anxiety.
Take Home Points
- GAD involves dysregulation in norepinephrine, serotonin, and GABA systems, causing excessive worry and somatic symptoms.
- It differs from panic disorder, which is more closely linked to lactate sensitivity and abrupt panic episodes.
- GABA deficits in GAD result in poor neural inhibition and increased anxiety; benzodiazepines enhance GABA function.
- SSRIs are first-line treatment due to their effect on serotonin levels, improving mood and anxiety regulation.
Which neurotransmitter is most directly involved in mediating arousal and anxiety symptoms in generalized anxiety disorder?
Explanation
Generalized Anxiety Disorder (GAD)is primarily linked to dysfunction in norepinephrine, GABA, and serotoninsystems. Of these, norepinephrine is the most directly responsible for arousalsymptoms like restlessness and heightened autonomic activity. The locus coeruleus, the brain’s primary norepinephrine center, triggers hyperarousal responses. Chronic noradrenergic overactivity contributes to persistent anxiety, muscle tension, insomnia, and irritability in GAD patients.
Rationale for correct answers
3. Norepinephrineis directly linked to arousal and stress response; its hyperactivity causes increased sympathetic output, triggering anxiety symptoms.
Rationale for incorrect answers
1.Acetylcholineis more involved in memory, attention, and voluntary movement; it has little role in the anxiety arousal pathway.
2.GABAinhibits neuronal activity and reduces anxiety, but it does not directly mediate arousal—it works by dampening overexcitation.
4.Dopamineis primarily related to reward, pleasure, and motor functions, not the physiological arousal symptoms seen in anxiety disorders.
Take Home Points
- Norepinephrine is the main neurotransmitter responsible for autonomic arousal and hyperactivity in GAD.
- GABA dysfunction contributes to GAD by reducing inhibition but doesn’t directly cause arousal.
- Dopamine and acetylcholine have minimal roles in GAD pathophysiology compared to norepinephrine.
- Targeting norepinephrine and GABA pathways helps alleviate both somatic and cognitive anxiety symptoms.
Practice Exercise 2
Which of the following is most characteristic of generalized anxiety disorder?
Explanation
GADis a chronic psychiatric disorder marked by persistent, excessive worrylasting at least 6 months. The worry is difficult to control and involves multiple domains like health, work, or finances. It must be accompanied by symptoms such as restlessness, fatigue, poor concentration, irritability, muscle tension, and sleep disturbance. It differs from other anxiety-related or psychotic disorders in both symptom profile and neurobiological underpinnings.
Rationale for correct answers
3. Excessive worryacross multiple situations is the hallmark of GAD. The worry is disproportionate and difficult to manage, occurring almost daily.
Rationale for incorrect answers
1.Hallucinationsare sensory perceptions without external stimuli and are characteristic of psychotic disorders, not anxiety disorders like GAD.
2.Obsessive thoughtsare intrusive and recurrent, typically linked to obsessive-compulsive disorder, not generalized anxiety.
4.Repetitive motorticsare involuntary movements seen in tic disorders like Tourette syndrome, not in GAD.
Take Home Points
- Persistent, excessive, and uncontrollable worry about multiple domains is the defining feature of GAD.
- GAD differs from OCD, which involves obsessions and compulsions, not general worry.
- Hallucinations suggest psychosis and are not a feature of GAD.
- Tic disorders present with involuntary movements or sounds and are neurologically distinct from anxiety disorders.
Which population is statistically more likely to be diagnosed with generalized anxiety disorder (GAD)?
Explanation
Generalized anxiety disorder (GAD)is a chronic psychiatric condition characterized by excessive, persistent worry that interferes with daily functioning. It disproportionately affects women, especially those over 40, due to hormonal changes, psychosocial stressors, and neurochemical vulnerabilities. Estrogen fluctuations and caregiving burdens contribute to increased susceptibility.
Rationale for correct answers
2.Womenover 40 show increased prevalence due to hormonal shifts, caregiving stress, and higher rates of comorbid depression and anxiety disorders.
Rationale for incorrect answers
1.Men in their 20s have lower prevalence rates; GAD is less common in young adult males due to protective social and biological factors.
3.Men over 60 may experience anxiety, but GAD is less frequently diagnosed in this group compared to middle-aged women.
4.Children under 10 may show anxiety symptoms, but GAD diagnosis is rare due to developmental limitations in expressing persistent worry.
Take Home Points
- GAD is more prevalent in women, especially those over 40, due to hormonal and psychosocial factors.
- Estrogen fluctuations and caregiving roles increase vulnerability to anxiety disorders in middle-aged women.
- GAD is less common in children and older men due to developmental and diagnostic factors.
- Differentiation from panic disorder and OCD is essential due to overlapping symptoms but distinct diagnostic criteria.
An overuse or ineffective use of ego defense mechanisms, which results in a maladaptive response to anxiety, is an example of the ___________________ theory of generalized anxiety disorder development.
Explanation
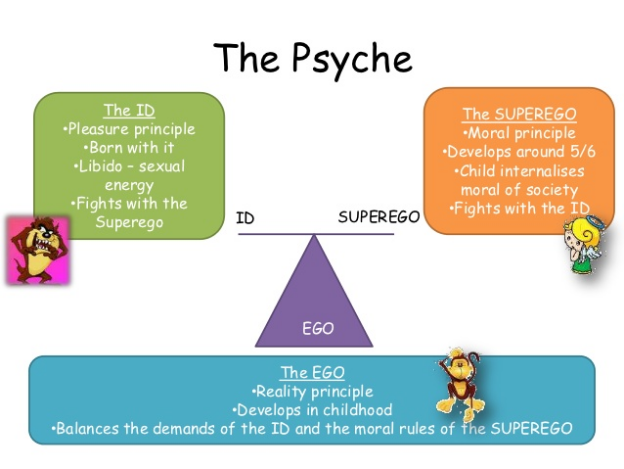
Psychodynamic theoryexplains the development of anxiety disorders through unconscious conflicts between internal drives and external demands. It emphasizes the role of ego defense mechanisms, which are unconscious strategies used to manage anxiety. When these defenses are overused or ineffective, they fail to contain internal conflict, leading to maladaptive symptoms such as chronic worry or somatic complaints. Anxiety is viewed as a signal to the ego of impending psychological danger, often rooted in early relational experiences or unresolved emotional trauma.
Rationale for correct answers
3.Psychodynamic theory attributes anxiety to unconscious conflict and the failure of defense mechanisms. When the ego cannot manage internal stressors, anxiety emerges as a symptom of unresolved psychic tension.
Rationale for incorrect answers
1.Cognitive theory focuses on distorted thinking patterns and negative automatic thoughts, not unconscious defense mechanisms.
2.Behavioral theory emphasizes learned responses to stimuli, such as avoidance or reinforcement, rather than internal psychological conflict.
4.Biological theory centers on neurochemical imbalances, genetic predisposition, and brain structure abnormalities, not psychological defenses.
Take Home Points
- Psychodynamic theory links anxiety to unconscious conflict and maladaptive defense mechanisms.
- Defense mechanisms like repression and denial are central to psychodynamic explanations of GAD.
- Cognitive and behavioral theories focus on conscious thought and learned behavior, not unconscious processes.
- Biological models explain anxiety through neurochemical and genetic factors, distinct from psychodynamic views.
Practice Exercise 3
Which of the following medications is commonly prescribed for long-term management of generalized anxiety disorder?
Explanation
Buspironeis a non-benzodiazepine anxiolytic used for the long-term managementof generalized anxiety disorder (GAD). It acts as a partial agonist at serotonin 5-HT1A receptors and has minimal sedative effects. Unlike benzodiazepines, buspirone does not cause dependence or withdrawal symptoms. It requires consistent dosing and may take 2–4 weeks to show full therapeutic effect. Common side effects include dizziness, headache, and nausea. It is contraindicated with monoamine oxidase inhibitors due to risk of hypertensive crisis.
Rationale for correct answers
2.Buspironeis FDA-approved for GAD and preferred for long-term use due to its non-sedating profile and low risk of dependence. It modulates serotonin without affecting GABA, making it suitable for chronic anxiety.
Rationale for incorrect answers
1.Alprazolamis a benzodiazepine used for short-term relief due to rapid onset. Long-term use risks tolerance, dependence, and withdrawal, making it unsuitable for chronic GAD management.
3.Haloperidolis an antipsychotic used for schizophrenia and agitation. It is not indicated for GAD and may worsen anxiety symptoms due to dopamine blockade and extrapyramidal side effects.
4.Lithiumis a mood stabilizer used in bipolar disorder. It is not approved for GAD and lacks evidence for efficacy in anxiety without comorbid mood instability.
Take Home Points
- Buspirone is the preferred long-term pharmacologic agent for GAD due to low abuse potential and serotonergic action.
- Benzodiazepines like alprazolam are effective short-term but carry significant risks with prolonged use.
- Antipsychotics and mood stabilizers are not first-line treatments for GAD unless comorbid conditions exist.
- SSRIs and SNRIs are also commonly used for long-term GAD management due to their efficacy and safety profile.
Which nursing interventions are appropriate for a client diagnosed with generalized anxiety disorder? Select all that apply.
Explanation
Generalized anxiety disorder (GAD)is a chronic psychiatric condition marked by excessive, uncontrollable worry occurring more days than not for at least six months. It affects multiple domains including cognition, behavior, and physiology. Clients often experience muscle tension, restlessness, and difficulty concentrating. Sleep disturbances, irritability, and fatigue are common. GAD is managed through a combination of pharmacologic therapy—typically SSRIs or SNRIs—and cognitive behavioral interventions. Benzodiazepines may be used short-term.
Rationale for correct answers
1.Verbal expression and emotional processing are essential in reducing internalized anxiety. Encouraging clients to articulate their feelings helps externalize worry and fosters therapeutic rapport.
2.Relaxation techniques and deep breathing activate the parasympathetic nervous system, reducing sympathetic overdrive. These methods decrease physical symptoms like tachycardia and hyperventilation.
4.Environmental stability and predictability reduce sensory overload and minimize triggers. A calm, structured setting lowers arousal levels and supports emotional containment.
5.Cognitive distortions such as catastrophizing and overgeneralization perpetuate anxiety. Challenging these through cognitive restructuring helps clients develop more adaptive thought patterns.
Rationale for incorrect answers
3.Stimulants exacerbate anxietysymptoms by increasing norepinephrine and dopamine activity. They heighten arousal, worsen insomnia, and may trigger panic responses. They are contraindicated in GAD unless comorbid ADHD is present and carefully managed.
Take Home Points
- GAD is characterized by persistent, excessive worry and somatic symptoms lasting at least six months.
- Nursing interventions should focus on emotional expression, cognitive restructuring, and environmental modulation.
- Relaxation techniques are first-line nonpharmacologic strategies to reduce autonomic hyperactivity.
- Stimulants are not appropriate for GAD management and may worsen symptoms unless used for comorbid conditions under strict supervision.
Which statement by a client taking buspirone for generalized anxiety disorder (GAD) indicates a need for further teaching?
Explanation
Buspironeis a non-benzodiazepine anxiolyticused for generalized anxiety disorder (GAD). It acts as a partial agonist at serotonin 5-HT1A receptors and requires consistent daily dosingto maintain therapeutic levels. Unlike PRN anxiolytics, buspirone does not provide immediate relief and takes 2–4 weeksfor full effect. It has low abuse potential, but abrupt discontinuation can lead to rebound anxiety. Alcohol should be avoided due to additive CNS effects. Buspirone must be tapered under medical supervision if discontinued.
Rationale for correct answers
4.Discontinuationwithout medical guidance is inappropriate. Buspirone requires gradual tapering to prevent rebound anxiety. Feeling better does not justify abrupt cessation, especially within one week of starting therapy.
Rationale for incorrect answers
1.Buspirone’sdelayed onset is well understood here. It typically takes 2–4 weeks to reach full efficacy, so this statement reflects accurate patient knowledge.
2.Daily administrationis essential for buspirone’s effectiveness. It is not used on an as-needed basis, so this statement shows proper understanding.
3.Alcoholcan potentiate CNS effects like dizziness and sedation. Avoiding alcohol is appropriate and indicates safe medication practices.
Take Home Points
- Buspirone must be taken consistently and not used as-needed for anxiety relief.
- Therapeutic effects of buspirone may take 2–4 weeks to manifest.
- Abrupt discontinuation can lead to rebound anxiety and should be avoided.
Alcohol should be avoided due to additive CNS depressant effects.
What is a key advantage of buspirone compared to benzodiazepines in treating generalized anxiety disorder (GAD)?
Explanation
Buspironeis a non-benzodiazepine anxiolyticused for generalized anxiety disorder (GAD). It acts as a partial agonist at serotonin 5-HT1A receptors and lacks direct GABAergic activity, which distinguishes it from benzodiazepines. This mechanism contributes to its lower risk of dependence, making it suitable for long-term management. Buspirone does not cause sedation, tolerance, or withdrawal symptoms, and it requires consistent dosing over 2–4 weeks for therapeutic effect.
Rationale for correct answers
2.Dependence riskis significantly lower with buspirone because it does not act on GABA receptors. This avoids the tolerance and withdrawal seen with benzodiazepines, making it safer for chronic use.
Rationale for incorrect answers
1.Buspirone has a delayed onset of action, typically requiring 2–4 weeks for full effect. Benzodiazepines act within minutes to hours, making them more suitable for rapid relief.
3.Buspirone is not effective in acute panic episodesdue to its slow onset. Benzodiazepines are preferred in such cases for immediate symptom control.
4.Buspirone lacks sedative properties. Unlike benzodiazepines, it does not impair cognition or motor function, which is an advantage but not the correct answer in this context.
Take Home Points
- Buspirone is preferred for long-term GAD management due to low dependence risk.
- It does not act on GABA receptors, avoiding sedation and withdrawal.
- Benzodiazepines are more effective for acute anxiety but carry higher addiction potential.
- Buspirone requires consistent dosing and is not suitable for as-needed use.
Which non-pharmacological therapies are supported by evidence in the treatment of generalized anxiety disorder (GAD)? Select all that apply.
Explanation
Generalized anxiety disorder (GAD)is a chronic psychiatric condition marked by excessive, uncontrollable worry occurring more days than not for at least 6 months. It involves both psychological distressand somatic symptomssuch as restlessness, fatigue, and muscle tension. Non-pharmacological therapies aim to reduce autonomic hyperactivity and maladaptive cognitive patterns through behavioral and physiological retraining.
Rationale for correct answers
1.Cognitive behavioral therapy is the most evidence-based psychotherapy for GAD. It targets maladaptive thoughtsand promotes behavioral restructuring, reducing worry intensity and improving coping.
3.Biofeedback trains individuals to regulate autonomic responseslike heart rate and muscle tension. It improves self-awarenessand reduces physiological arousal associated with anxiety.
4.Relaxation training, including progressive muscle relaxation and breathing techniques, reduces sympathetic activationand enhances parasympathetic tone, lowering baseline anxiety levels.
Rationale for incorrect answers
2.Psychoanalysislacks robust evidence for GAD. It focuses on unconscious conflicts and early relational patterns, which are not primary drivers of GAD symptoms.
5.Hypnotherapyhas limited and inconsistent data for GAD. While it may aid in acute stress reduction, it is not considered a first-line or evidence-supported intervention for chronic anxiety disorders.
Take Home Points
- CBT is the gold standard non-pharmacological treatment for GAD due to its structured approach to cognitive and behavioral modification.
- Biofeedback and relaxation training are effective adjuncts that target physiological components of anxiety.
- Psychoanalysis and hypnotherapy are not supported by strong evidence for GAD and are not recommended as primary interventions.
- GAD management requires therapies that address both cognitive distortions and autonomic dysregulation.
Comprehensive Questions
A nurse is admitting a client diagnosed with generalized anxiety disorder. During the client’s assessment, the nurse determines that which findings would be consistent with generalized anxiety disorder? Select all that apply.
Explanation
Generalized anxiety disorder (GAD)is a chronic psychiatric condition characterized by excessive, uncontrollable worry occurring more days than not for at least 6 months. It affects both psychological and physiological domains, with hallmark features including restlessness, difficulty concentrating, and muscle tension. Adults must exhibit at least three of six DSM-5 criteria: restlessness, fatigue, difficulty concentrating, irritability, muscle tension, and sleep disturbance.
Rationale for correct answers
2.Restlessness or feeling keyed up is a core DSM-5 criterion. It reflects autonomic hyperactivityand heightened arousal, commonly seen in GAD.
3.Difficulty controlling anxiety is central to the diagnosis. Persistent worry is excessive and intrusive, often disproportionate to actual circumstances.
4.Irritability is a frequent emotional manifestation. It results from cognitive overloadand sustained psychological tension.
5.Muscle tension is a defining somatic symptom. Chronic neuromuscular contractionreflects prolonged sympathetic activation.
Rationale for incorrect answers
1.Expansive mood with pressured speechis characteristic of manic episodes in bipolar disorder, not GAD. It reflects elevated mood and increased goal-directed activity, which are absent in anxiety disorders.
Take Home Points
- GAD requires excessive worry lasting ≥6 months with ≥3 DSM-5 symptoms in adults.
- Somatic symptoms like muscle tension and restlessness reflect autonomic dysregulation.
- Emotional symptoms such as irritability and difficulty controlling worry are diagnostic hallmarks.
- GAD must be differentiated from mood disorders like bipolar disorder, which present with expansive mood and pressured speech.
After a nurse teaches a client with generalized anxiety disorder some strategies for coping with stressors, another goal for the client would be to:
Explanation
Generalized anxiety disorder (GAD)is a chronic psychiatric condition marked by excessive, uncontrollable worry occurring more days than not for at least 6 months. It involves both psychological distressand somatic symptomssuch as restlessness, fatigue, and muscle tension. Management includes pharmacologic and non-pharmacologic interventions, with emphasis on early recognitionof symptom escalation and implementation of coping strategies to prevent functional impairment.
Rationale for correct answers
2.Learning to obtain assistance when anxiety increases reflects insight and self-monitoring, which are essential for relapse prevention. It promotes adaptive copingand timely intervention before symptoms escalate.
Rationale for incorrect answers
1.Recognizing signs of elevated mood is relevant to bipolar disorder, not GAD. GAD is characterized by persistent worry, not mood elevation or pressured speech.
3.Decreasing manipulative peer behavior is unrelated to GAD. This goal aligns more with personality disorders or conduct-related interventions.
4.Facilitating self-care participation is more applicable to depressive disordersor severe psychosis where motivation and functioning are impaired. GAD clients typically maintain self-care but struggle with excessive worry.
Take Home Points
- GAD clients benefit from learning to recognize symptom escalation and seek support proactively.
- Elevated mood and pressured speech are features of bipolar disorder, not GAD.
- Goals should align with the client’s diagnosis and functional challenges specific to anxiety.
- Self-care deficits are not primary in GAD unless comorbid depression is present.
A nurse is caring for a client who has generalized anxiety disorder. Which statement about this client is true?
Explanation
Generalized anxiety disorder (GAD)is a chronic psychiatric condition marked by excessive, uncontrollable worry occurring more days than not for at least 6 months. It affects both psychological and physiological domains, with hallmark features including restlessness, difficulty concentrating, and muscle tension. Adults must exhibit at least three of six DSM-5 criteria: restlessness, fatigue, difficulty concentrating, irritability, muscle tension, and sleep disturbance. These symptoms must cause significant distress or impairment in functioning.
Rationale for correct answers
4.Anxiety lasting longer than 6 months is a diagnostic requirement for GAD. Persistent worry durationdistinguishes GAD from transient stress reactions and is central to DSM-5 criteria.
Rationale for incorrect answers
1.Regular obsessionsare characteristic of obsessive-compulsive disorder (OCD), not GAD. GAD involves excessive worry about realistic concerns, not intrusive, irrational thoughts.
2.Relaxation techniquesare helpful but not curative. GAD requires a multimodal approach including cognitive behavioral therapy and pharmacologic management.
3.Nightmares and flashbacksare hallmark symptoms of post-traumatic stress disorder (PTSD), not GAD. GAD is not trauma-based and lacks re-experiencing phenomena.
Take Home Points
- GAD diagnosis requires excessive worry lasting ≥6 months with ≥3 DSM-5 symptoms in adults.
- Obsessions and compulsions are specific to OCD and not present in GAD.
- Nightmares and flashbacks are core features of PTSD, not GAD.
- Relaxation techniques aid symptom control but are not curative for GAD.
After a nurse teaches a client with generalized anxiety disorder some strategies for coping with stressors, another goal for the client would be to:
Explanation
Generalized anxiety disorder (GAD)is a chronic psychiatric condition marked by excessive, uncontrollable worry occurring more days than not for at least 6 months. It involves both psychological distressand somatic symptomssuch as restlessness, fatigue, and muscle tension. Management includes pharmacologic and non-pharmacologic interventions, with emphasis on early recognitionof symptom escalation and implementation of coping strategies to prevent functional impairment.
Rationale for correct answers
2.Learning to obtain assistance when anxiety increases reflects insight and self-monitoring, which are essential for relapse prevention. It promotes adaptive copingand timely intervention before symptoms escalate.
Rationale for incorrect answers
1.Recognizing signs of elevated mood is relevant to bipolar disorder, not GAD. GAD is characterized by persistent worry, not mood elevation or pressured speech.
3.Decreasing manipulative peer behavior is unrelated to GAD. This goal aligns more with personality disorders or conduct-related interventions.
4.Facilitating self-care participation is more applicable to depressive disordersor severe psychosis where motivation and functioning are impaired. GAD clients typically maintain self-care but struggle with excessive worry.
Take Home Points
- GAD clients benefit from learning to recognize symptom escalation and seek support proactively.
- Elevated mood and pressured speech are features of bipolar disorder, not GAD.
- Goals should align with the client’s diagnosis and functional challenges specific to anxiety.
- Self-care deficits are not primary in GAD unless comorbid depression is present.
A nurse is caring for a client who has generalized anxiety disorder. Which statement about this client is true?
Explanation
Generalized anxiety disorder (GAD)is a chronic psychiatric condition marked by excessive, uncontrollable worry occurring more days than not for at least 6 months. It affects both psychological and physiological domains, with hallmark features including restlessness, difficulty concentrating, and muscle tension. Adults must exhibit at least three of six DSM-5 criteria: restlessness, fatigue, difficulty concentrating, irritability, muscle tension, and sleep disturbance. These symptoms must cause significant distress or impairment in functioning.
Rationale for correct answers
4.Anxiety lasting longer than 6 months is a diagnostic requirement for GAD. Persistent worry durationdistinguishes GAD from transient stress reactions and is central to DSM-5 criteria.
Rationale for incorrect answers
1.Regular obsessionsare characteristic of obsessive-compulsive disorder (OCD), not GAD. GAD involves excessive worry about realistic concerns, not intrusive, irrational thoughts.
2.Relaxation techniquesare helpful but not curative. GAD requires a multimodal approach including cognitive behavioral therapy and pharmacologic management.
3.Nightmares and flashbacksare hallmark symptoms of post-traumatic stress disorder (PTSD), not GAD. GAD is not trauma-based and lacks re-experiencing phenomena.
Take Home Points
- GAD diagnosis requires excessive worry lasting ≥6 months with ≥3 DSM-5 symptoms in adults.
- Obsessions and compulsions are specific to OCD and not present in GAD.
- Nightmares and flashbacks are core features of PTSD, not GAD.
- Relaxation techniques aid symptom control but are not curative for GAD.
A client diagnosed with generalized anxiety disorder is placed on clonazepam (Klonopin) and buspirone (BuSpar). Which client statement indicates teaching has been effective?
Explanation
Clonazepam and buspironeare commonly used together in the initial management of generalized anxiety disorder (GAD). Clonazepam is a benzodiazepinethat provides rapid relief of anxiety symptoms by enhancing GABA activity, but it carries risks of sedation, dependence, and tolerance. Buspirone is a non-benzodiazepine anxiolyticthat acts as a partial agonist at serotonin 5-HT1A receptors. It has a delayed onset of action, typically requiring 2–4 weeks for full therapeutic effect, and is preferred for long-term management due to its low abuse potentialand lack of sedation.
Rationale for correct answers
3.Clonazepam is used short-termto manage acute anxiety symptoms while waiting for buspirone’s delayed onsetto take effect. This approach minimizes benzodiazepine dependenceand supports transition to safer long-term therapy.
Rationale for incorrect answers
1.Long-term use of clonazepam is discouraged due to risk of tolerance, dependence, and withdrawal. It is not recommended as a sustained therapy alongside buspirone.
2.Buspirone does not cause sedationand is typically taken consistently, not necessarily at night. It lacks the sedative properties of benzodiazepines.
4.Buspirone does not lead to tolerancewith long-term use. It is considered safe for chronic anxiety management without risk of physical dependence.
Take Home Points
- Clonazepam is used short-term for acute anxiety relief while buspirone builds therapeutic effect.
- Buspirone is non-sedating and preferred for long-term GAD management due to low abuse potential.
- Benzodiazepines like clonazepam carry risks of dependence and are not suitable for chronic use.
- Buspirone does not cause tolerance or sedation, making it ideal for sustained anxiety control.
A client with a history of generalized anxiety disorder enters the emergency department complaining of restlessness, irritability, and exhaustion. Vital signs are blood pressure 140/90 mm Hg, pulse 96, and respirations 20.
Based on this assessed information, which assumption would be correct?
Explanation
Generalized anxiety disorderis a chronic psychiatric condition marked by excessive, persistent worry that is difficult to control. It presents with restlessness, irritability, and fatigue, often accompanied by somatic symptoms like muscle tension, sleep disturbance, and autonomic hyperactivity. Diagnostic criteria require symptoms to persist for at least six months and cause functional impairment. Exacerbations may occur during stress or illness, and vital signs may show mild sympathetic activation without reaching pathological thresholds.
Rationale for correct answers
1. Exacerbationof generalized anxiety disorder is supported by the client’s history and current symptoms—restlessness, irritability, and exhaustion—along with mildly elevated vital signs consistent with sympathetic arousal.
Rationale for incorrect answers
2.No evidence of acute medical illness is present; symptoms align with psychiatric etiologyrather than organic pathology.
3.While physical exams are routine, the client’s known diagnosis and symptom pattern already point to a psychiatric cause, making this less immediately relevant.
4.Dosage adjustment requires longitudinal assessment and evaluation of medication adherence, side effects, and therapeutic response—not assumed from a single ED visit.
Take Home Points
- Generalized anxiety disorder presents with chronic worry, restlessness, irritability, and fatigue.
- Mild sympathetic signs like elevated pulse and BP may occur during exacerbations.
- Diagnosis is clinical, based on DSM-5 criteria and exclusion of medical causes.
- Management includes psychotherapy and pharmacotherapy; dosage changes require careful evaluation.
Which of the following symptom assessments would validate the diagnosis of generalized anxiety disorder? Select all that apply.
Explanation
Generalized anxiety disorderis a chronic psychiatric condition marked by excessive worry, muscle tension, and autonomic hyperarousal. According to DSM-5, symptoms must persist for at least six months and include difficulty controlling worry, restlessness, fatigue, irritability, sleep disturbance, and somatic complaints. Feeling “keyed up” or “on edge” reflects persistent sympathetic activation. Muscle tension is a hallmark physical symptom. Hypersomnia and excessive energy are not typical features and may suggest alternative diagnoses like depression or bipolar disorder.
Rationale for correct answers
1. Excessive worryis the core diagnostic feature of generalized anxiety disorder. It must be present most days for at least six months and be difficult to control.
2. Muscle tensionis one of the six DSM-5 physical symptoms used to validate the diagnosis. It reflects chronic somatic arousal and is commonly reported.
5. Feeling “keyed up”or “on edge” indicates autonomic hyperactivity and is part of the DSM-5 criteria. It reflects the persistent restlessness and arousal seen in GAD.
Rationale for incorrect answers
3.Hypersomniais more characteristic of depressive disorders. GAD typically presents with insomnia or restless, unsatisfying sleep.
4.Excessive energyis not a symptom of GAD. It may suggest manic or hypomanic episodes seen in bipolar spectrum disorders.
Take Home Points
- Generalized anxiety disorder requires excessive, uncontrollable worry lasting at least six months.
- DSM-5 criteria include restlessness, fatigue, irritability, muscle tension, sleep disturbance, and difficulty concentrating.
- Feeling “keyed up” and muscle tension are hallmark signs of autonomic arousal in GAD.
During an assessment, a client diagnosed with generalized anxiety disorder rates anxiety as 9/10 and states, “I have thought about suicide because nothing ever seems to work out for me.” Based on this information, which nursing diagnosis takes priority?
Explanation
Risk for suicideis the most urgent concern when a client expresses suicidal ideation. Generalized anxiety disorder may elevate suicide risk, especially when compounded by hopelessness and impaired coping. According to DSM-5, suicidal thoughts in the context of anxiety signal acute distress and require immediate safety interventions. The priority in nursing care is always physiological safety, which aligns with Maslow’s hierarchy of needs—preserving life precedes addressing emotional or psychological concerns.
Rationale for correct answers
4. Risk for suicideis the priority diagnosis because the client has verbalized suicidal ideation. This poses an immediate threat to life and demands urgent intervention, including safety planning and continuous monitoring.
Rationale for incorrect answers
1.Hopelessnessis present but secondary to the suicide risk. While the statement reflects despair, it does not override the need to address the client’s safety first.
2.Ineffective copingmay contribute to suicidal ideation, but it is not the most critical concern. Coping strategies can be addressed after ensuring the client is safe.
3.Anxietyis evident, but it is not the priority when suicidal thoughts are expressed. The rating of 9/10 supports severity, but the suicide risk takes precedence.
Take Home Points
- Suicide risk always takes priority in nursing diagnoses when ideation is present.
- Generalized anxiety disorder can escalate to suicidal thoughts, especially when compounded by hopelessness.
- Maslow’s hierarchy places physiological safety above emotional needs.
- Nursing interventions must focus first on safety, then address underlying emotional and cognitive concerns.
The nurse has received an evening report. Which client would the nurse need to assess first?
Explanation
Acute anxiety escalationrequires immediate nursing attention due to its potential to progress into panic or behavioral dysregulation. When a client verbalizes a high anxiety rating (e.g. 8/10) and exhibits pacing, this signals autonomic hyperarousal, impaired coping, and possible risk of harm to self or others. Anxiety activates the sympathetic nervous system, leading to increased heart rate, blood pressure, and respiratory rate. If unaddressed, it can impair judgment, escalate into panic attacks, or trigger aggression. Nursing priority is guided by Maslow’s hierarchy—physiological and safety needscome first. Clients with acute symptoms must be stabilized before addressing chronic or less urgent concerns.
Rationale for correct answers
3.Elevated anxiety and pacing behavior indicate acute distress. The client is actively symptomatic and may be at risk for decompensation. Immediate assessment allows for early intervention, de-escalation, and prevention of harm.
Rationale for incorrect answers
1.Although newly admitted clients require prompt assessment, a history of panic attacks alone does not indicate current instability. Without active symptoms, this client is not the highest priority.
2.Sleep disruption due to flashbacks suggests PTSD-related distress, but the client is not currently exhibiting acute behavioral or physiological symptoms. This is important but not urgent.
4.A client awaiting discharge with a diagnosis of GAD is likely stable and has already been evaluated for readiness. Discharge planning is a lower priority compared to acute symptom management.
Take Home Points
- Clients with acute anxiety symptoms (e.g. pacing, high self-reported anxiety) require immediate assessment to prevent escalation.
- Prioritization is based on physiological and safety needs per Maslow’s hierarchy.
- History alone does not determine urgency—current presentation is key.
- Sleep disruption and chronic anxiety are important but not prioritized over acute behavioral signs.
A client diagnosed with generalized anxiety disorder has a nursing diagnosis of panic anxiety related to altered perceptions. Which of the following short-term outcomes is most appropriate for this client?
Explanation
Panic anxietyis an acute, intense episode of fear or discomfort that peaks within minutes and is often accompanied by somatic symptoms such as chest pain, palpitations, and shortness of breath. It stems from altered perceptionsand distorted cognitive processing, leading to catastrophic misinterpretations of bodily sensations or environmental cues. Management includes rapid symptom containment, cognitive restructuring, and grounding techniques. Short-term goals focus on stabilization and symptom reduction, while long-term goals address coping and insight. SSRIs are first-line pharmacologic agents; benzodiazepines may be used short-term.
Rationale for correct answers
2.Verbalizing anxietyand tracking symptom change are measurableand achievablewithin 48 hours. This outcome reflects early therapeutic engagement and emotional awareness, which are critical in managing panic anxiety. It allows the nurse to monitor progress and adjust interventions accordingly.
Rationale for incorrect answers
1.Intervening before panic escalation is a long-term behavioral goalrequiring insight, skill acquisition, and practice. It is not realistic as a short-term outcome, especially for a client with altered perceptions.
3.Effective problem-solving reflects higher-order cognitive functioningand emotional regulation. This is a long-term adaptive goal, not suitable for acute-phase planning.
4.Voluntary group participation is a discharge-level goal indicating improved social functioningand reduced avoidance. It does not address immediate symptom relief or emotional stabilization.
Take Home Points
- Panic anxiety involves acute fear with distorted perceptions and intense somatic symptoms.
- Short-term goals should focus on symptom awareness and reduction, not behavioral mastery.
- Verbalizing anxiety levels is a realistic and measurable early outcome.
- Long-term goals include cognitive restructuring, coping skill development, and social reintegration.
Which assessment information would be evaluated as objective data?
Explanation
Objective datarefers to measurable, observable findings obtained through physical examination, diagnostic tests, or standardized tools. It is not influenced by personal feelings or interpretations. Objective data includes vital signs, lab results, and scores from validated assessment tools. These findings are reproducible and consistent across observers, making them essential for clinical decision-making.
Rationale for correct answers
1.A CIWA score is derived from a standardized assessment tool used to quantify alcohol withdrawal severity. It is measurableand reproducible, qualifying it as objective data.
Rationale for incorrect answers
2.Statements of anxiety are subjectivebecause they reflect the client’s personal experience and emotional state, which cannot be directly measured or verified by others.
3.Complaints of anorexia are subjectiveas they rely on the client’s perception of appetite loss, which may vary and cannot be quantified without further diagnostic evaluation.
4.The statement about disorganized thoughts is subjective, reflecting the client’s internal cognitive experience, which cannot be objectively validated without formal testing.
Take Home Points
- Objective data includes measurable findings like scores from validated tools and diagnostic results.
- Subjective data reflects the client’s personal experience and cannot be independently verified.
- CIWA is a validated tool used to assess alcohol withdrawal severity objectively.
- Differentiating objective from subjective data is critical for accurate nursing documentation and care planning.
In which situation would benzodiazepines be prescribed appropriately?
Explanation
Benzodiazepinesare central nervous system depressants that enhance the effect of gamma-aminobutyric acid (GABA), producing sedative, anxiolytic, anticonvulsant, and muscle relaxant effects. They are indicated for short-termmanagement of anxiety, alcohol withdrawal, and procedural sedation. Long-term use is discouraged due to risks of dependence, tolerance, and cognitive impairment. Common side effects include drowsiness, confusion, and respiratory depression. Contraindications include sleep apnea, substance use disorders, and concurrent use with opioids or alcohol due to synergistic CNS depression.
Rationale for correct answers
2.Benzodiazepines are appropriate for short-term treatment of generalized anxiety disorder, alcohol withdrawal, and preoperative sedationdue to their rapid onset and calming effects. These uses align with their pharmacologic profile and safety guidelines for limited duration.
Rationale for incorrect answers
1.Long-term use for PTSD and convulsive disorders is discouraged due to risk of dependenceand tolerance. While benzodiazepines may be used acutely in alcohol withdrawal, chronic use is not recommended.
3.Benzodiazepines are not first-line for obsessive-compulsive disorder or essential hypertension. They may relieve muscle spasms but are not indicated for long-termmanagement of these conditions.
4.Long-term treatment of panic disorder and bipolar mania with benzodiazepines is not standard due to risk of addiction. Alcohol dependence requires structured withdrawal protocols, not maintenance benzodiazepine therapy.
Take Home Points
- Benzodiazepines are best suited for short-term use in anxiety, alcohol withdrawal, and procedural sedation.
- Long-term use increases risk of dependence, tolerance, and cognitive decline.
- They are contraindicated in patients with substance use disorders or respiratory compromise.
- SSRIs and other non-addictive agents are preferred for chronic anxiety and mood disorders.
A client recently diagnosed with generalized anxiety disorder is prescribed clonazepam
(Klonopin), buspirone (BuSpar), and citalopram (Celexa). Which assessment related to
the concurrent use of these medications is most important?
Explanation
Concurrent use of serotonergic agentslike clonazepam, buspirone, and citalopramrequires careful monitoring due to additive central nervous system and serotonergic effects. Clonazepam is a benzodiazepine with sedative and anxiolytic properties. Buspirone is a non-benzodiazepine anxiolytic that modulates serotonin and dopamine receptors. Citalopram is a selective serotonin reuptake inhibitor (SSRI) used for depression and anxiety. When combined, these drugs may increase the risk of serotonin syndrome, CNS depression, and altered mental status. Symptoms may include tremor, diaphoresis, tachycardia, and confusion. Monitoring is essential, especially during initiation or dosage changes.
Rationale for correct answers
2.The combination of citalopram and buspirone increases serotonergic activity, while clonazepam adds CNS depressant effects. This triad can lead to serotonin syndromeand autonomic instability, making it critical to monitor for tremor, diaphoresis, tachycardia, and mental status changes.
Rationale for incorrect answers
1.While worsening depression and suicidal ideation are concerns with SSRIs like citalopram, this is not the most immediate risk when combined with buspirone and clonazepam. The primary concern is serotonin syndromeand CNS effects.
3.Hyperpyrexia, dystonia, and rigidity are more characteristic of neuroleptic malignant syndrome, typically associated with antipsychotics, not the medications listed.
4.Facial spasms and bizarre movements suggest extrapyramidal symptomsor tardive dyskinesia, which are not common with SSRIs, buspirone, or benzodiazepines.
Take Home Points
- Combining SSRIs, buspirone, and benzodiazepines increases risk of serotonin syndrome and CNS depression.
- Serotonin syndrome presents with tremor, tachycardia, diaphoresis, and altered mental status.
- Neuroleptic malignant syndrome and extrapyramidal symptoms are not typical risks with these agents.
- Close monitoring is essential during initiation or dose changes of serotonergic and CNS depressant drugs.
Which client would the charge nurse assign to an agency nurse who is new to a psychiatric setting?
Explanation
Algophobiais an irrational and persistent fear of pain that may lead to avoidance behaviors and heightened anxiety. It is classified under specific phobias and typically does not involve acute psychiatric instability. Clients with algophobia are often cognitively intact and oriented, and their care focuses on gradual exposure therapy, reassurance, and anxiety-reducing techniques. Unlike disorders with active psychosis or medication initiation, algophobia rarely requires complex psychiatric interventions
Rationale for correct answers
3.Stable conditionand low riskmake this client appropriate for a nurse new to psychiatric care. The client has been admitted for several days, reducing the likelihood of unpredictable behavior or urgent needs. Care involves routine monitoring and supportive communication.
Rationale for incorrect answers
1.Flashbacksin posttraumatic stress disorder may involve dissociation, aggression, or re-experiencing trauma. These episodes require skilled de-escalation techniques and familiarity with trauma-informed care, which may overwhelm a new psychiatric nurse.
2.Initiating benzodiazepinesrequires close monitoring for sedation, paradoxical reactions, and respiratory depression. A newly admitted client also presents with unknown behavioral patterns, increasing the complexity of care.
4.Obsessive-compulsive disorderoften involves compulsions that interfere with daily functioning. A newly admitted client may exhibit rituals, anxiety, or resistance to care, requiring experienced psychiatric assessment and intervention strategies.
Take Home Points
- Algophobia is a specific phobia characterized by fear of pain, typically managed with reassurance and exposure therapy.
- Clients with PTSD experiencing flashbacks may require trauma-informed care and advanced psychiatric skills.
- Benzodiazepine initiation demands close monitoring for adverse effects and behavioral changes.
- Newly admitted psychiatric clients often present with unpredictable symptoms requiring experienced nursing judgment.
During an intake assessment, a client diagnosed with generalized anxiety disorder rates mood at 3/10, rates anxiety at 8/10, and states, “I’m thinking about suicide.” Which nursing intervention takes priority?
Explanation
Suicidal ideationin the context of generalized anxiety disorder (GAD) is a psychiatric emergency requiring immediate risk assessment. GAD is characterized by excessive, persistent worry and physiological symptoms such as restlessness, fatigue, and sleep disturbance. When suicidal thoughts are present, especially with high anxiety and low mood ratings, the priority is to determine intent and plan. This guides the urgency of intervention and safety measures.
Rationale for correct answers
2.Suicide riskand intent assessmentmust be addressed first. Determining whether the client has a plan helps evaluate lethality and immediacy. This guides whether one-to-one observation, hospitalization, or other protective measures are needed.
Rationale for incorrect answers
1.Teaching relaxation techniques is inappropriatewhen suicide risk is active. It does not address the immediate safety concern and assumes the client is stable enough to engage in coping strategies.
3.Calling for a PRN anxiolytic may help reduce anxiety but does not address the suicidal ideation directly. Medication alone is insufficientwithout assessing intent and planning.
4.Encouraging group participation is a long-term therapeuticstrategy. It is not suitable during acute suicidal ideation and may overwhelm the client or increase distress.
Take Home Points
- Suicide risk assessment begins with direct questioning about intent and plan.
- Generalized anxiety disorder increases suicide risk, especially with comorbid depression.
- Immediate safety interventions take precedence over therapeutic or pharmacologic measures.
- Relaxation and group therapy are supportive but secondary to crisis evaluation.
In the United States, which diagnosis has the lowest percentage of occurrence?
Explanation
Schizophreniais a chronic psychiatric disorder marked by delusions, hallucinations, and disorganized thinking. It affects approximately 0.25% to 0.64% of the U.S. population annually, making it one of the least prevalent major mental illnesses. Onset typically occurs in late adolescence or early adulthood, with males often presenting earlier than females. The condition involves disturbances in perception, cognition, and affect, and is associated with significant functional impairment
Rationale for correct answers
4.Low prevalenceand chronic coursedistinguish schizophrenia from other listed conditions. Its lifetime prevalence is significantly lower than depressive or anxiety disorders, making it the least common among the options.
Rationale for incorrect answers
1.Major depressive disorder affects approximately 8.3% of U.S.adults annually. It is the most prevalent psychiatric diagnosis, characterized by persistent low mood, anhedonia, and functional impairment.
2.Generalized anxiety disorder has an annual prevalence of around 2.7%.It involves excessive worry and physical symptoms such as restlessness and muscle tension, often co-occurring with other psychiatric conditions.
3.Obsessive-compulsive disorder affects about 1.2%of the population annually. It is marked by intrusive thoughts and repetitive behaviors, with significant distress and impairment in daily functioning.
Take Home Points
- Schizophrenia has the lowest prevalence among major psychiatric disorders in the U.S.
- It presents with psychotic symptoms and requires long-term antipsychotic treatment.
- Major depressive disorder is the most common psychiatric diagnosis.
- OCD and GAD have higher prevalence rates than schizophrenia and involve anxiety-related symptoms.
A client diagnosed with generalized anxiety disorder is getting ready for discharge. Which statement evaluates the client’s cognitive response to nursing interventions?
Explanation
Cognitive responserefers to how a client processes, interprets, and applies information or strategies learned during care. In generalized anxiety disorder (GAD), cognitive responses are essential for long-term management and include identifying triggers, restructuring thoughts, and recognizing maladaptive patterns. GAD is marked by excessive worry, restlessness, and difficulty concentrating, often accompanied by somatic symptoms. Cognitive-behavioral therapy (CBT) is the gold standard, targeting distorted thinking and promoting adaptive coping. A key goal is helping clients identify negative self-talk, which perpetuates anxiety and impairs functioning. Discharge planning should assess whether clients can apply these cognitive strategies independently.
Rationale for correct answers
3.Thought recognitionand self-awarenessreflect cognitive processing. The ability to identify negative self-talk indicates the client has internalized cognitive strategies taught during therapy, showing readiness for discharge and independent coping.
Rationale for incorrect answers
1.This describes physiological stability, not cognitive processing. While calm demeanor and normal vitals are positive, they do not reflect the client’s internal thought patterns or ability to manage anxiety cognitively.
2.This reflects behavioral feedback, not cognitive restructuring. While breathing techniques are helpful, stating their effectiveness does not demonstrate insight into thought patterns or triggers.
4.Journaling is an expressive and emotional outlet. It supports emotional regulation but does not directly evaluate cognitive restructuring or thought monitoring, which are central to cognitive response.
Take Home Points
- Cognitive response involves recognizing and restructuring maladaptive thoughts that fuel anxiety.
- Physiological and behavioral improvements do not confirm cognitive readiness for discharge.
- Identifying negative self-talk is a key marker of cognitive progress in GAD.
Journaling and relaxation techniques support emotional regulation but are not direct indicators of cognitive restructuring.
Exams on Generalized Anxiety Disorder
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
- Describe the diagnostic criteria and clinical manifestations of Generalized Anxiety Disorder (GAD) in adults.
- Explain etiological perspectives (psychodynamic, cognitive, biological) relevant to the development of GAD.
- Identify key symptoms (psychological and somatic) associated with chronic anxiety and worry in GAD.
- Formulate nursing interventions, including assessment strategies and therapeutic approaches, for patients with GAD.
- Discuss common pharmacological treatments for GAD (e.g., SSRIs, buspirone) and essential patient education points.
- Construct a sample nursing care plan addressing anxiety reduction and coping enhancement for a client with GAD.
Introduction
- Generalized Anxiety Disorder (GAD) is a chronic psychiatric condition characterized by persistent, excessive, and unrealistic worry that is non-specific and pervasive.
- GAD differs from normal anxiety in its intensity, duration (typically at least six months), and impact on daily functioning.
- Patients with GAD often anticipate disaster in multiple domains of life – such as health, work, or relationships – even in the absence of clear threats.
- The anxiety in GAD is often described as “free-floating” because it is not tied to a single situation or phobia.
- Over time, this excessive worry impairs social, occupational, and personal functioning, leading to significant distress.
- Prevalence data suggest GAD is one of the most common anxiety disorders seen in primary care settings (many patients present to family physicians rather than psychiatrists) due to its chronic, somatic symptom profile.
- GAD involves excessive worry and anxiety about a variety of events or activities on more days than not for at least six months.
- Common worry topics include interpersonal relationships, job performance, finances, and health of loved ones.
- Physical symptoms (e.g., muscle tension, insomnia) and cognitive symptoms (e.g., poor concentration) accompany the chronic anxiety.
- Onset can occur at any age but often begins in adolescence or early adulthood and tends to run a chronic course with exacerbations during stress.
Pathophysiology Of Gad
1 Psychodynamic Theory
Psychodynamic theory attributes GAD to unresolved intrapsychic conflicts and immature ego defenses. Key points include:
- Ego weakness and conflict: Anxiety arises when the ego cannot mediate between the id’s instinctual demands and the superego’s moral constraints. Chronic anxiety indicates a failure of the ego to resolve these internal conflicts.
- Delayed ego development: An unsatisfactory early parent-child relationship or conditional love may hinder full ego maturation, leaving the individual less able to cope with stress.
- Overuse of defense mechanisms: To control unbearable anxiety, the individual may rely excessively on primitive defenses (e.g., repression, denial, avoidance) which are maladaptive in the long run. Over time, this leads to chronic anxiety and difficulty adjusting to reality.
Nursing Insight:
- From a nursing perspective, recognize that excessive worry often serves as a coping mechanism for deeper emotional conflicts.
Nurses should create a supportive environment where patients feel safe to express underlying fears, and should avoid reinforcing maladaptive defenses.
2 Cognitive Theory
Cognitive theory emphasizes faulty thinking patterns and appraisals in GAD. The central idea is that distorted cognitions cause and maintain anxiety. Key concepts include:
- Catastrophic thinking: Patients interpret minor events as catastrophic. For example, difficulty concentrating may be seen as evidence of impending mental collapse.
- All-or-nothing and overgeneralization: Thinking patterns such as “I must perform perfectly” or “Everything bad happens to me” perpetuate worry.
- Persistent negative appraisal: Individuals habitually view situations as threatening or unsolvable. This distortions cause a feeling of vulnerability and helplessness.
- Reduced reasoning ability: Intense anxiety impairs concentration and problem-solving, reinforcing a sense that situations cannot be controlled.
- The person with GAD may think, “If I make a mistake at work, I will be fired,” even though this is unlikely. This erroneous appraisal fuels worry and anxiety.
- Feeling “keyed up” is often accompanied by an inability to silence repetitive, anxious thoughts (rumination).
Nursing Insight:
- In clinical practice, help patients identify and challenge their cognitive distortions. Cognitive-behavioral strategies are especially effective: teaching patients to reframe negative thoughts can reduce anxiety.
- Nurses should use therapeutic communication to gently question irrational beliefs (e.g., “What evidence do you have that you will fail?”).
3 Biological Factors
- Research suggests that biological factors contribute significantly to anxiety disorders. This includes genetic predisposition, neuroanatomical findings, biochemical triggers, and neurotransmitter imbalances.
- Nurses should consider these factors when assessing and educating patients.
3.1 Genetic Factors
- Family history: There is a notable genetic component. Individuals with a first-degree relative who has GAD or related anxiety disorders are at higher risk. Twin studies estimate about a 30% concordance rate in identical twins for panic and anxiety disorders.
- Genetic markers: Research has identified potential genetic variations (e.g., in the cholecystokinin gene) that may influence anxiety sensitivity. These genes can affect neurotransmitter systems that regulate mood and arousal.
- A positive family history of anxiety or panic suggests that biological predisposition should be considered in the patient’s assessment.
Nursing Insight:
- When obtaining history, be sure to ask about family mental health. A patient may not volunteer that “everyone in my family is anxious,” but this pattern is an important clue to genetic susceptibility.
3.2 Neuroanatomical Factors
- Limbic system involvement: Structures such as the amygdala and hippocampus (part of the limbic system) are critical in fear processing and memory. Overactivity or dysregulation in these areas can generate persistent anxiety responses to stress.
- Temporal lobe abnormalities: Some imaging studies have found changes in temporal lobe structures (e.g., hippocampus volume) in anxiety disorders. The hippocampus is involved in regulating emotional responses and the stress hormone axis.
- Diencephalon and brainstem: The hypothalamus and thalamus mediate autonomic and endocrine responses to stress. Overactivity of the hypothalamic-pituitary-adrenal (HPA) axis can contribute to chronic anxiety.
- Chronic GAD may be associated with hyperarousal of neural circuits; this can manifest as increased baseline tension and reactivity.
Nursing Insight:
- A biological basis for anxiety means that we should not dismiss GAD as “just psychological.” Stress-reduction interventions can modulate these neural pathways.
- Educating patients that their symptoms have a biological component can reduce self-blame and stigma.
3.3 Biochemical Factors
- Lactate sensitivity: Patients prone to panic and anxiety show increased sensitivity to sodium lactate infusions, which can trigger panic-like symptoms. Elevated blood lactate levels have been observed in anxious individuals. The exact mechanism is unclear, but lactate may stimulate chemoreceptors that trigger a fight-or-flight response.
- Cortisol and stress hormones: Chronic anxiety often co-occurs with elevated cortisol from prolonged HPA axis activation. High cortisol can lead to many of the physical symptoms of anxiety (e.g., insomnia, muscle weakness).
- Physiologic arousal (e.g., rapid heartbeat, hyperventilation) can sometimes begin with purely biochemical stimuli. Nurses should measure vital signs and consider lab tests (thyroid, metabolic panels) to rule out medical contributors to anxiety.
3.4 Neurochemical Factors
- Norepinephrine (NE): Excessive NE activity (sympathetic nervous system dominance) leads to hyperarousal. Drugs like yohimbine, which increase NE, reliably induce anxiety in predisposed individuals.
- Serotonin (5-HT): Low serotonergic activity is implicated in anxiety. Serotonin modulates mood and anxiety; deficits can remove inhibitory control over stress circuits. SSRIs (Selective Serotonin Reuptake Inhibitors) help by increasing serotonin and are effective in GAD.
- Gamma-aminobutyric acid (GABA): GABA is the chief inhibitory neurotransmitter. Reduced GABA function (or GABA receptor sensitivity) leads to decreased inhibition and increased neuronal excitability. Benzodiazepines (e.g., lorazepam) potentiate GABA and rapidly reduce anxiety.
- Other neurotransmitters: Imbalances in dopamine and other neuromodulators may also play minor roles in the anxiety spectrum.
- Many anti-anxiety medications target these pathways (e.g., SSRIs for 5-HT, benzodiazepines for GABA, beta-blockers address peripheral NE effects).
-
Nursing Insight:
- Understanding the neurochemical basis helps nurses explain medication effects.
- For example, tell patients that SSRIs gradually balance serotonin levels to reduce anxiety over weeks, whereas benzodiazepines immediately enhance GABA to calm nerves. This knowledge helps set realistic expectations and improve adherence.
Clinical Features Of Gad
1. Excessive Worry and Anxiety
- GAD is defined by uncontrollable, excessive worry about everyday events on most days for at least six months. This worry is broad, persistent, and not limited to specific situations.
- Patients often report constant mental chatter: fearing the worst even when evidence suggests things are likely to be fine. The intensity of anxiety is out of proportion to the actual likelihood of events.
- Because of this chronic worry, individuals frequently feel on edge or keyed-up and may dwell on hypothetical problems. They anticipate disasters in multiple areas (work, health, relationships) simultaneously.
- Example: A person might worry for weeks about a possible job layoff, focusing on minor criticisms from a supervisor and assuming the worst outcome.
- The worry is ego-dystonic (the person recognizes it as excessive) but feels uncontrollable.
- Decision-making can be difficult because the patient expects negative outcomes, leading to indecisiveness or procrastination.
Nursing Insight:
- When assessing anxiety, distinguish normal worry from GAD: GAD worry persists over months and invades many parts of life, whereas normal worry is usually tied to a specific recent stressor and is temporary.
2. Associated Psychological Symptoms
- Restlessness or feeling keyed up: Patients often cannot relax; they may pace or fidget constantly.
- Fatigability: Chronic anxiety is exhausting. Patients feel tired even without physical exertion due to sustained mental strain.
- Irritability: Small stresses can trigger disproportionate irritability or frustration. Loved ones may note the patient is “on edge” or “snaps easily.”
- Difficulty concentrating: Anxiety fills the mind with worries, leading to a sense of “blanking out” or distraction. This affects academic or work performance.
- Procrastination and avoidance: Because of fear of poor outcomes, individuals might delay decisions or avoid tasks (e.g., being late or absent at work/school).
- Excessive reassurance seeking: Patients frequently seek confirmation from friends or family that “everything will be okay,” yet this only temporarily relieves anxiety.
- These symptoms often feed each other (e.g., poor sleep leads to irritability; irritability increases worry). Nurses should assess each symptom systematically.
Nursing Insight:
- Interview patients about sleep and concentration specifically. Even subtle admission of poor focus or feeling tired all day can be clues to GAD.
- Ask open-ended questions like, “Tell me about your sleep routine,” or “What thoughts keep you awake at night?”
3. Physical and Physiological Symptoms
- Muscle tension: Chronic stress causes the patient to hold muscles tightly. Common complaints include headaches, neck/shoulder pain, and overall achiness.
- Autonomic hyperactivity: Symptoms may include heart palpitations, sweating, trembling, dry mouth, dizziness, or shortness of breath. These are manifestations of a persistent fight-or-flight state.
- Sleep disturbance: Difficulty falling or staying asleep (insomnia) is very common. Even when sleep occurs, it may be restless or non-restorative. The mind often races with worries at bedtime.
- Somatic complaints: Frequent complaints of gastrointestinal upset, nausea, diarrhea, or frequent urination can occur due to stress. These symptoms often lead patients to seek medical rather than psychiatric help.
- General health impact: Because of poor sleep and stress, GAD patients may have low energy and be more susceptible to medical illnesses.
- Routine vital signs may show mild tachycardia or hypertension if the anxiety is severe. However, ensure to rule out medical causes (e.g., hyperthyroidism) for these signs.
Nursing Insight:
- Document all somatic symptoms carefully. Patients with GAD often become “doctor shoppers” looking for physical causes.
- A thorough review of systems is essential to identify which symptoms are anxiety-driven versus organic.
4. Course and Comorbidity
- GAD often begins gradually in adolescence or early adulthood, but it can start later in life. The course is usually chronic; symptoms wax and wane but rarely fully remit without treatment.
- Stress exacerbates symptoms: during life crises (job loss, health scare), anxiety levels spike. In calmer periods, the patient may function better but still feels underlying tension.
- Comorbidity: Major depressive disorder is the most common comorbid condition (often >50% lifetime comorbidity). Substance use disorders and other anxiety disorders (like panic disorder or social anxiety) frequently co-occur.
- Gender differences: GAD is more common in females than males. Age trends show increasing lifetime prevalence through adulthood.
- Impact on function: Chronic worry and avoidance behaviors lead to impaired relationships, missed work, and social withdrawal. Patients may feel “disabled” by their anxiety.
- Quality of life is significantly reduced; older adults with GAD, in particular, report poorer health and functioning compared to their peers.
- Because symptoms are diffuse, patients often present to primary care with somatic issues; GAD is under-diagnosed when physical symptoms predominate.
Nursing Insight:
- Pay attention to functional impairment: Ask, “How have your worries affected your job performance or daily activities?”
- GAD often flies under the radar until its impact on daily life is documented. Encourage patients to keep a symptom diary to illustrate the pattern of anxiety.
Nursing Management Of Gad
1. Assessment and Diagnosis
- Conduct a thorough psychosocial assessment focusing on the pattern of anxiety. Confirm that the patient experiences excessive worry on more days than not, for at least six months.
- Evaluate the content of the worry: Note which domains (health, work, relationships) are involved and how persistent the worry is.
- Use standardized tools as appropriate (e.g., GAD-7 questionnaire) to quantify severity of anxiety. This helps in monitoring progress.
- Physical assessment: Rule out medical causes of anxiety symptoms. Check thyroid function tests, electrolytes, and substance use (caffeine, stimulants, medication side effects). Some arrhythmias or endocrine disorders can mimic anxiety.
- Functional assessment: Determine how anxiety affects daily life (e.g., school, work, family). Look for evidence of social withdrawal, job absences, or reliance on medication/alcohol.
- Mental status examination: Assess for restlessness, irritability, attention/concentration, mood (often worried or tense), sleep patterns.
Nursing Insight:
- Patients may not recognize excessive worry as a problem; they may complain only of physical symptoms (like headaches).
- Nurses should use open-ended questions to uncover hidden anxiety, for example: “What worries have been on your mind lately?” rather than asking only about headaches or heartburn.
2. Psychosocial Interventions/Non-Pharmacological Interventions
- Therapeutic communication: Remain calm and nonjudgmental. Provide reassurance with realism (avoid platitudes). Listen actively and acknowledge the patient’s feelings.
- Educate the patient: Explain that anxiety has physiological and psychological components. Inform them that GAD is a recognized medical condition (reduces stigma). Discuss the chronic nature of GAD and that gradual improvement is the goal.
- Cognitive-behavioral techniques: Encourage identification of negative thoughts and rational reappraisal. For example, challenge catastrophizing: “What is the worst that can happen?” “What evidence supports or refutes this thought?”
- Relaxation training: Teach techniques such as deep breathing exercises, progressive muscle relaxation, guided imagery, or meditation to reduce autonomic arousal. Practice these together in sessions.
- Sleep hygiene: Counsel on good sleep practices (regular bedtime, avoidance of caffeine before bed, limited screen time). Chronic anxiety often disrupts sleep.
- Lifestyle interventions: Encourage regular physical activity (exercise can reduce anxiety) and balanced meals. Advise on limiting caffeine and alcohol, as these can worsen anxiety.
- Social support: Involve family or friends in therapy if appropriate (family education about GAD). Support groups or peer groups can also be helpful for some patients.
- Small, achievable goals: Help the patient break tasks into manageable steps to avoid overwhelming worry (e.g., “Today I will complete the first 5 minutes of my work task”).
Nursing Insight:
- A calm therapeutic environment helps. Nurses should provide a safe space for expressing fears and discourage avoidance behaviors gradually (e.g., short exposure to feared social situations with support).
3. Pharmacological Treatments
- First-line treatments: Selective serotonin reuptake inhibitors (SSRIs, e.g., escitalopram, paroxetine) and serotonin-norepinephrine reuptake inhibitors (SNRIs, e.g., venlafaxine, duloxetine) have a 30-50% response rate and target serotonin and norepinephrine imbalances.
- Adjunctive treatments: Benzodiazepines (e.g., diazepam, clonazepam) provide short-term relief but are avoided in patients with a history of substance abuse due to dependence risk.
- Alternative treatments: Buspirone, a non-benzodiazepine anxiolytic, is effective with a 2-3 week onset and no dependency risk.
- Selective Serotonin Reuptake Inhibitors (SSRIs): Common choices include paroxetine, escitalopram, or sertraline. SSRIs are first-line for GAD as they improve anxiety and have a favorable safety profile.
- Action: Increase serotonin availability over weeks, reducing anxiety gradually.
- Nursing considerations: Educate that full effect takes 4–6 weeks; continue even if early improvement is slight. Monitor for side effects (nausea, insomnia, sexual dysfunction). Warn about potential initial increase in anxiety or jitteriness when starting or adjusting dose.
- Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs): Examples include venlafaxine and duloxetine. These target both serotonin and norepinephrine. They are effective for GAD and often chosen if SSRIs fail.
- Nursing considerations: Similar to SSRIs. Monitor blood pressure (venlafaxine can raise BP) and inform about side effects.
- Buspirone: An anxiolytic specifically indicated for GAD. It acts on serotonin (and dopamine) receptors.
- Advantages: Non-sedating and non-habit-forming (unlike benzodiazepines).
- Nursing considerations: It also takes ~2-4 weeks to take effect. Advise patient to take regularly (not PRN) and not to use with grapefruit juice (which can increase drug levels).
- Benzodiazepines: Such as lorazepam or alprazolam can rapidly reduce acute anxiety and tension.
- Uses: Short-term relief during severe exacerbations or until SSRIs/buspirone take effect.
- Risks: Sedation, dependency, tolerance. Use is limited due to abuse potential, especially in patients with substance use history.
- Nursing considerations: Administer lowest effective dose for short duration. Monitor for signs of oversedation and educate patient about not driving or operating machinery. Taper slowly if discontinuing after long-term use to avoid rebound anxiety/withdrawal.
- Other medications: Occasionally beta-blockers (like propranolol) are used to control somatic symptoms (tremor, tachycardia) in anxiety situations (e.g., prior to a public speech).
Nursing Insight:
- Medication teaching is crucial. Nurses should emphasize adherence (even when feeling better) and schedule follow-up appointments to evaluate effectiveness and side effects.
- For instance, advise patients that SSRI-induced anxiolysis is not immediate, so they should use coping skills in the interim.
4. Nursing Care Plan Example
Coordination of Care
GAD is best managed by a multidisciplinary team, including:
- Mental health nurse: Provides direct care, education, and support.
- Psychiatrist: Prescribes and monitors pharmacotherapy.
- Psychologist: Delivers CBT or other psychotherapies.
- Social worker: Addresses social determinants, such as housing or financial stress.
- Primary care provider: Rules out medical causes of anxiety and manages comorbidities.
A sample nursing care plan for GAD may include:
- Nursing Diagnosis: Anxiety related to overwhelming and uncontrollable worry about multiple life circumstances.
- Desired Outcome: Client will demonstrate decreased anxiety (e.g., reduced muscle tension, improved sleep) and utilize effective coping strategies (e.g., relaxation techniques, positive self-talk).
- Nursing Interventions:
- Encourage the client to verbalize feelings and worries.
- Rationale: Expressing fears often reduces their intensity and helps identify distorted thoughts.
- Teach and practice a relaxation exercise (e.g., diaphragmatic breathing) during each session.
- Rationale: Relaxation lowers sympathetic arousal and provides the patient with a self-help tool to counter anxiety.
- Break complex tasks into smaller, manageable steps.
- Rationale: This reduces the likelihood of feeling overwhelmed and helps the client experience success with gradual progress.
- Educate the client on the importance of following the prescribed medication regimen.
- Rationale: Consistent pharmacotherapy (SSRIs/SNRIs) reduces neurochemical imbalances underlying anxiety; irregular use can lead to relapse.
- Limit caffeine and stimulants in the client’s diet.
- Rationale: These substances can exacerbate anxiety symptoms and interfere with sleep.
- Encourage the client to verbalize feelings and worries.
- Evaluation:
- Monitor the client’s self-reported anxiety level (use of a scale, e.g., 1–10).
- Observe for increased usage of learned coping strategies (e.g., the client takes three deep breaths when anxious).
- Assess improvements in sleep patterns and ability to concentrate on tasks.
Discharge Planning
Discharge planning should include:
- Scheduling follow-up appointments with clinicians (e.g., psychiatrist, therapist).
- Providing resources for ongoing support, such as helplines or support groups.
- Reinforcing lifestyle modifications, including avoiding caffeine, alcohol, and illicit drugs, and maintaining sleep hygiene.
- Encouraging a healthy diet and regular physical activity.
Summary
- Generalized Anxiety Disorder is a long-term condition characterized by excessive and pervasive worry.
- By definition, the anxiety is present on more days than not for at least six months and is accompanied by physical and psychological symptoms (muscle tension, restlessness, insomnia, irritability, poor concentration, and fatigue).
- The worry is broad and not confined to a single event or situation.
- Etiology of GAD is understood through multiple lenses:
- Psychodynamic factors: Unconscious conflicts and weak ego defenses lead to chronic anxiety.
- Cognitive factors: Distorted thinking patterns (catastrophizing, pessimism) maintain a cycle of worry.
- Biological factors: Genetic predisposition, overactive limbic pathways, and neurotransmitter imbalances (norepinephrine, serotonin, GABA) contribute to a hyper-aroused state.
- Nursing assessment must be comprehensive, screening for duration and scope of worries, comorbid depression, and medical conditions that mimic anxiety. Essential nursing interventions include:
- Using a calm, supportive approach and therapeutic communication to build trust.
- Teaching relaxation techniques and encouraging regular exercise and sleep hygiene.
- Applying cognitive-behavioral strategies to challenge unrealistic fears.
- Pharmacotherapy with SSRIs/SNRIs or buspirone is considered first-line; benzodiazepines are reserved for short-term relief. Education on medication adherence and potential side effects is critical.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Generalized Anxiety Disorder
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


