Please set your exam date
Congenital heart diseases: Obstructive disorders
Study Questions
Practice Exercise 1
A client is diagnosed with coarctation of the aorta. Which finding should the nurse expect during an assessment?
Explanation
Coarctation of the aorta is a congenital obstructive cardiac defect characterized by a localized narrowing of the aortic lumen. This constriction typically occurs near the ductus arteriosus insertion site. It results in significant pressure gradients between the proximal and distal arterial systems. Compensatory collateral circulation often develops via intercostal arteries.
Rationale for correct answer:
B. Significant narrowing distal to the left subclavian artery increases afterload on the left ventricle. This causes a compensatory rise in systolic blood pressure within the vessels originating proximal to the obstruction. Consequently, hypertension is observed in the arms.
Rationale for incorrect answers:
A. A finding of normal blood pressure is highly unlikely in a symptomatic patient with this defect. The mechanical obstruction necessitates an increase in proximal pressure to maintain systemic perfusion. Blood pressure readings will typically reveal a significant discrepancy between limbs.
C. Blood pressure is not decreased in the upper extremities because they receive blood from pre-coarctation vessels. Decreased pressure is instead localized to the lower extremities and the descending aorta. The upper body remains hyperperfused relative to the lower body.
D. Pulses in the upper extremities are typically bounding rather than decreased or absent. This is due to the high volume and pressure generated proximal to the aortic narrowing. Absent pulses are a hallmark of the femoral arteries in this specific clinical context.
Test-taking strategy:
- Identify the pathophysiology: Recognize that coarctation is a constriction of the aorta, which naturally creates a "backup" of pressure before the site of narrowing.
- Apply anatomical knowledge: Determine that the upper body (head and arms) is supplied by vessels arising before the typical site of coarctation, while the lower body is supplied by the aorta after the narrowing.
- Use the principle of pressure gradients: In obstructive defects, blood pressure will always be higher proximal (before) the obstruction and lower distal (after) to it.
- Eliminate opposites: Since choice 2 and 3 are direct opposites, one of them is likely the correct answer based on the mechanical effects of the lesion.
Take home points
- Coarctation of the aorta results in hypertension in the upper extremities and hypotension in the lower extremities.
- Characteristic findings include weak or absent femoral pulses and a systolic murmur heard best at the left infraclavicular area.
- Rib notching may be visible on a chest X-ray due to enlarged collateral intercostal arteries.
- Post-operative nursing care focuses on monitoring for rebound hypertension and ensuring adequate lower extremity perfusion.
A nurse is caring for a child 24-hours post coarctation of the aorta repair. Which of the following is the priority nursing diagnoses at this point?
Explanation
Coarctation of the aorta is a localized constriction of the aortic lumen, typically near the insertion of the ductus arteriosus. This narrowing creates a significant pressure gradient, resulting in hypertension in the upper extremities and hypoperfusion of the lower body. Post-surgical repair involves the excision of the stenotic segment or patch aortoplasty, which requires cross-clamping of the aorta and carries a high risk for rebound hypertension and mesenteric inflammation.
Rationale for correct answer:
C. Maintaining systemic blood flow is the critical priority during the immediate post-operative period following an aortic reconstruction. The nurse must monitor for spinal cord ischemia, renal failure, and bowel ischemia that can occur due to altered hemodynamics or surgical manipulation. Ensuring adequate oxygen delivery to distal tissues prevents permanent organ damage and identifies potential complications like graft thrombosis or persistent narrowing.
Rationale for incorrect answers:
A. While the risk of surgical site infection is a valid concern, it is not the most life-threatening priority within the first 24 hours. Infection typically manifests several days after a procedure and does not pose the same immediate threat as vascular compromise. Standard aseptic techniques and prophylactic antibiotics are used to manage this risk while the nurse focuses on hemodynamic stability.
B. Impaired skin integrity related to the surgical incision is an expected finding rather than a priority diagnosis in the acute phase. Although the nurse must monitor for wound dehiscence or hematoma, these issues are secondary to the primary goal of maintaining vital organ perfusion. Skin integrity is a lower-level need on Maslow's hierarchy compared to the physiological necessity of adequate blood circulation.
D. Anxiety is a psychosocial diagnosis that, while important for holistic care, does not take precedence over hemodynamic monitoring. In the initial 24 hours, physiological stability is the focus to ensure patient survival and successful surgical outcomes. Psychosocial needs are addressed once the child is clinically stable and the immediate risks of the major vascular surgery have subsided.
Test-taking strategy:
- Apply Maslow's Hierarchy of Needs, prioritizing physiological stability (perfusion) over safety (infection) or psychosocial needs (anxiety).
- Use the ABCs (Airway, Breathing, Circulation) framework; in a vascular surgery case, "perfusion" is the primary representative of the "C" (Circulation) category.
- Distinguish between actual vs. risk diagnoses: While all are "risks," impaired tissue perfusion following an aortic cross-clamp is the most high-stakes complication.
- Focus on the surgical site: Since the aorta is the main vessel for systemic distribution, any surgery on it makes "Tissue Perfusion" the most specific and relevant priority.
- Evaluate the post-operative timeline: Within the first 24 hours, acute mechanical or hemodynamic failures are the priority; infectious processes typically require a longer incubation period.
Take home points
- Post-coarctation repair patients require frequent monitoring of blood pressure in all four extremities to identify gradients.
- A significant risk after this specific surgery is post-coarctation syndrome, which involves abdominal pain and intestinal ischemia.
- Antihypertensive medications are often required post-operatively to prevent the high pressure from damaging the new surgical anastomosis.
- Neurovascular checks of the lower extremities, including pedal pulses and capillary refill, are essential to confirm adequate distal perfusion.
A nurse is caring for a child after surgical repair of coarctation of the aorta. Which assessments are priorities in the immediate postoperative period? Select all that apply
Explanation
Postoperative care for coarctation of the aorta focuses on monitoring hemodynamic stability and assessing the patency of the new anastomosis. The sudden transition from chronic high resistance to perfused distal vascular beds can trigger a surge in sympathetic activity. This results in paradoxical hypertension, which must be managed to prevent tension on the suture line. Ensuring adequate renal perfusion is equally vital, as the kidneys adjust to normalized blood flow after years of hypoperfusion.
Rationale for correct answers:
A. Comparing blood pressure in upper and lower extremities is the most direct way to evaluate the success of the surgical repair. The nurse expects to see a significant reduction or total resolution of the preoperative pressure gradient. Persistent or worsening discrepancies may indicate surgical failure or acute thrombosis at the repair site.
B. Assessment of femoral pulse quality provides an immediate bedside indicator of distal aortic patency. Strong, palpable pulses in the lower extremities signify that blood is successfully traversing the repaired segment of the aorta. Weak or absent pulses post-surgery are red-flag findings that necessitate urgent surgical re-evaluation.
C. Urine output is a critical indicator of kidney perfusion and overall cardiac output in the immediate recovery phase. Because the renal arteries are located distal to the coarctation, they are sensitive to hemodynamic changes following the removal of the obstruction. A drop in output below 1 ml/kg/hr may signal low cardiac output or renal vascular complications.
Rationale for incorrect answers:
D. Monitoring for signs of infection at the incision site is a standard nursing intervention, but it is not a priority in the immediate (first 24 hours) postoperative period. Surgical site infections typically take days to manifest through erythema, warmth, or purulent drainage. Immediate concerns must focus on life-threatening hemodynamic instability rather than subacute inflammatory processes.
E. Daily weight trends are useful for long-term monitoring of fluid volume status and nutritional progress in pediatric patients. However, in the high-acuity immediate postoperative hours, hourly output and invasive pressure monitoring provide more actionable data. Weight changes over a 24-hour period are too slow to guide emergency interventions for acute surgical complications.
Test-taking strategy:
- Prioritize "Immediate" vs. "Long-term": When a question uses the word immediate, look for assessments that detect life-threatening or surgical-failure complications such as pulses and BP gradients.
- Focus on the specific defect: For coarctation, the most specific assessments always involve the gradient between the top and bottom of the body.
- Apply the ABCs and Perfusion: Urine output and pulse quality are direct measures of circulation, which is the priority in the immediate post-surgical window.
- Identify the "Normal" postoperative timeline: Rule out infection as an immediate priority because it is a complication that occurs later in the recovery trajectory.
Take home points
- The primary goal after coarctation repair is maintaining stable blood pressure to protect the anastomosis.
- Paradoxical hypertension occurs in many patients post-repair and requires aggressive vasodilator therapy.
- Abdominal pain should be assessed frequently to rule out mesenteric arteritis caused by sudden increased intestinal perfusion.
- A return of the pressure gradient between limbs suggests acute recoarctation or graft occlusion.
A nurse is reviewing the history of a client with newly diagnosed coarctation of the aorta. Which historical findings support this diagnosis? Select all that apply
Explanation
A. Frequent headaches result from chronic hypertension in the upper body. The vessels proximal to the aortic narrowing are exposed to elevated pressures. This cephalic congestion leads to persistent or recurrent cephalgia. This symptom reflects the vascular stress on the cerebral circulation.
B. Nosebleeds, or epistaxis, occur due to the fragility of the nasal mucosa vessels under high pressure. The upper body hyperperfusion caused by the obstruction increases the force against these small capillaries. It is a classic clinical manifestation of pre-stenotic hypertension.
E. Leg pain with exercise, or claudication, is caused by inadequate oxygen delivery to the lower limb muscles. During physical activity, the metabolic demand of the legs exceeds the restricted supply permitted by the narrowed aorta. This results in ischemic pain that subsides with rest.
Rationale for incorrect answers:
C. Bounding lower extremity pulses are not found in this condition. The narrowing specifically reduces the pulse volume and pressure distal to the site of coarctation. Femoral pulses are typically described as weak, delayed, or entirely absent upon palpation.
D. Cool upper extremities are inconsistent with the pathophysiology of this defect. The upper body receives blood from the aorta before the point of constriction and is therefore warm and well-perfused. It is the lower extremities that typically feel cool to the touch.
Test-taking strategy:
- Analyze the flow of blood: Visualize the aorta and remember that coarctation is a "kink" in the garden hose. Everything before the kink has high pressure, and everything after the kink has low pressure.
- Map symptoms to anatomy: Headaches and nosebleeds are "above the kink" due to high pressure. Leg pain and cold skin are "below the kink" result from the low pressure.
- Identify pulse characteristics: Bounding pulses always occur where the pressure is highest. Since the legs are after the obstruction, their pulses must be diminished, not bounding.
- Evaluate exercise intolerance: Recognize that "claudication" is a hallmark of any arterial obstruction. If blood cannot get through the narrow aorta fast enough to feed working leg muscles, pain will occur.
- Eliminate opposites: If you know the legs are poorly perfused, you must eliminate any choice suggesting strong pulses or warm skin in the lower body.
Take home points
- Upper body symptoms like headaches and epistaxis are caused by hypertension proximal to the narrowing.
- Lower body symptoms like leg cramps and cool skin are caused by hypotension distal to the narrowing.
- A hallmark physical exam finding is the "brachial-femoral delay," where the radial pulse is felt before the femoral pulse.
- In infants, the first sign may be acute heart failure or cardiogenic shock when the ductus arteriosus closes.
Practice Exercise 2
A child has been seen by the school nurse for dizziness since the start of the school term. It happens when standing in line for recess and homeroom. The child now reports that she would rather sit and watch her friends play hopscotch because she cannot count out loud and jump at the same time. When the nurse asks her if her chest ever hurts, she says yes. Based on this history, the nurse suspects that she has:
Explanation
Aortic stenosis is a congenital obstructive cardiac malformation characterized by a narrowing of the aortic valve orifice. This mechanical barrier restricts the ejection of oxygenated blood from the left ventricle into the systemic circulation, creating a high pressure gradient. This results in a relatively fixed cardiac output that cannot increase to meet the metabolic demands of physical exertion. Chronic pressure overload leads to compensatory hypertrophy of the left ventricular myocardium and increased oxygen consumption.
Rationale for correct answer:
B. The combination of dizziness, exercise intolerance, and exertional chest pain is highly indicative of aortic stenosis. These symptoms occur because the narrowed valve prevents the necessary increase in cardiac output during physical activity. The resulting myocardial ischemia and reduced cerebral perfusion lead to angina and syncope. These findings signify a clinically significant obstruction.
Rationale for incorrect answers:
A. Ventricular septal defect is a left-to-right shunt that increases pulmonary blood flow rather than obstructing systemic output. While large defects can cause exercise intolerance due to heart failure, they do not typically present with angina or dizziness. The primary symptoms involve tachypnea and poor weight gain in younger children. It is not an obstructive lesion.
C. Mitral valve prolapse is often asymptomatic or presents with vague palpitations and atypical chest pain that is not usually exertional. It involves the displacement of the mitral valve leaflets into the left atrium during systole. While common in adolescents, it does not typically cause the severe obstructive symptoms of syncope and exertional angina. It rarely restricts activity significantly.
D. Tricuspid atresia is a severe cyanotic heart defect where the tricuspid valve fails to develop. This results in decreased pulmonary blood flow and profound hypoxemia from birth. Children with this condition usually have a history of multiple palliative surgeries and baseline cyanosis. It does not manifest as new-onset exertional dizziness in a previously healthy school-aged child.
Test-taking strategy:
- Link symptoms to pathophysiology: Recognize that dizziness and fainting while standing or active suggest a failure of cardiac output to meet demand.
- Identify "red flag" signs: Exertional chest pain (angina) in a child is a hallmark indicator of an obstructive left-sided lesion like aortic stenosis.
- Assess activity level: The inability to "count out loud and jump" indicates a limitation in aerobic capacity due to a mechanical bottleneck in the heart.
- Differentiate shunt from obstruction: Rule out VSD and tricuspid atresia as they are primarily flow or shunting issues rather than outflow tract obstructions.
- Prioritize the most dangerous finding: While mitral valve prolapse can cause chest pain, aortic stenosis is the classic boards-tested cause of exertional syncope and angina.
Take home points
- Aortic stenosis prevents the heart from increasing cardiac output during physical exertion.
- Exertional chest pain and dizziness are critical symptoms indicating severe valvular obstruction.
- These children are at high risk for sudden cardiac death during strenuous activities or competitive sports.
- Physical assessment usually reveals a harsh systolic ejection murmur at the right upper sternal border.
A nurse is caring for a neonate with aortic stenosis. Which medication may be prescribed to maintain adequate systemic blood flow?
Explanation
Critical aortic stenosis in a neonate represents a life-threatening obstruction of the left ventricular outflow tract. In this severe form, the left ventricle is unable to maintain adequate systemic perfusion independently. The infant's survival becomes ductal-dependent, meaning systemic blood flow must be supplemented by a right-to-left shunt from the pulmonary artery. This bypass occurs through the ductus arteriosus, a fetal vascular structure that normally begins to close shortly after birth. Maintaining this channel is the highest therapeutic priority to prevent rapid circulatory collapse and metabolic acidosis.
Rationale for correct answer:
B. Prostaglandin E1 is a potent vasodilator used specifically to maintain the patency of the ductus arteriosus. In critical stenosis, it allows deoxygenated blood from the right ventricle to reach the descending aorta, bypassing the left-sided obstruction. This ensures that vital organs receive at least partial perfusion until surgical or transcatheter intervention. This medication is essential for stabilizing the neonate's hemodynamic status.
Rationale for incorrect answers:
A. Indomethacin is a nonsteroidal anti-inflammatory drug that acts as a prostaglandin inhibitor. It is used clinically to facilitate the closure of a patent ductus arteriosus in premature infants. Administering this to a neonate with critical aortic stenosis would be fatal as it would eliminate the only route for systemic blood flow. It is strictly contraindicated in ductal-dependent obstructive lesions.
C. Acetaminophen is an analgesic and antipyretic medication used to manage pain and fever. While safe for general use in neonates, it has no hemodynamic properties and does not affect the patency of fetal heart structures. It would be ineffective in addressing the primary pathophysiological crisis of systemic hypoperfusion. It lacks the pharmacological action required to manage an aortic obstruction.
D. Albuterol is a beta-2 agonist used to treat bronchospasm and improve airway resistance in respiratory conditions. It acts on the smooth muscle of the bronchioles rather than the vascular smooth muscle of the aorta or ductus arteriosus. It plays no role in the management of congenital heart defects or the maintenance of systemic circulation. It would not resolve the underlying cardiac output deficiency.
Test-taking strategy:
- Identify the physiological need: Recognize that "critical” stenosis means the heart cannot pump blood out; therefore, the baby needs an alternative path for blood to reach the body.
- Understand the "Ductal-Dependent" concept: Memorize that for left-sided obstructions, a patent ductus arteriosus (PDA) is the only thing keeping the infant alive.
- Recall the "Keep Open" drug: Associate prostaglandin E1 with the phrase "keep the ductus open" and indomethacin with "close the ductus."
- Apply the "Opposite Rule": Since Indomethacin and Prostaglandin E1 have opposite effects on the same structure, the answer is likely one of the two; in an obstruction, you never want to close the door.
- Prioritize life-saving interventions: Rule out choices 3 and 4 as they are supportive or respiratory drugs that do not address the immediate surgical/cardiovascular emergency.
Take home points
- Prostaglandin E1 is life-saving for neonates with ductal-dependent systemic blood flow.
- Signs of ductal closure in critical stenosis include sudden onset of grayish skin, diminished pulses, and metabolic acidosis.
- Continuous intravenous infusion of PGE1 requires close monitoring for apnea, a common side effect in neonates.
- The primary goal of PGE1 therapy is to bridge the patient to a balloon valvuloplasty or surgical valvotomy.
A nurse is assessing a child with untreated aortic stenosis. Which complication is the child most at risk for?
Explanation
Aortic stenosis is a congenital obstructive cardiac malformation involving the narrowing of the aortic valve. This mechanical barrier significantly increases afterload, requiring the left ventricle to generate higher pressures to maintain systemic perfusion. Chronic pressure overload leads to concentric remodeling as a compensatory mechanism. This structural change reduces ventricular compliance and increases myocardial oxygen consumption.
Rationale for correct answer:
C. Left ventricular hypertrophy is the most direct and common compensatory response to the chronic pressure overload of aortic stenosis. The myocardium thickens as it works against the obstructed valve to eject blood. This structural change is necessary to maintain cardiac output but eventually leads to decreased diastolic filling.
Rationale for incorrect answers:
A. Pulmonary edema is a clinical sign of congestive heart failure that occurs when the left ventricle fails. While it can occur in advanced stages of untreated stenosis, it is a secondary complication of pump failure. It is not the most immediate structural risk compared to the compensatory thickening of the heart wall.
B. Right-sided heart failure typically occurs as a sequela to long-standing left-sided failure or primary pulmonary disease. In isolated aortic stenosis, the primary pathological stress is localized to the left side of the heart. Right-sided involvement only happens after pulmonary hypertension develops due to chronic left-sided congestion.
D. Increased pulmonary blood flow is characteristic of acyanotic left-to-right shunts, such as a ventricular septal defect. Aortic stenosis is an obstructive lesion and does not involve an abnormal opening that redirects blood to the lungs. Instead, it creates a bottleneck for blood trying to exit the heart into the systemic circulation.
Test-taking strategy:
- Identify the primary chamber: Recognize that "aortic" refers to the exit from the left ventricle; therefore, the most immediate risk will affect that specific chamber.
- Understand "Compensatory vs. Failure": Distinguish between the mechanism of compensation (hypertrophy) and the result of failure (pulmonary edema). Hypertrophy happens first and most consistently.
- Match pathology to hemodynamics: Since stenosis is a "narrowing," think of the heart as a muscle lifting heavier and heavier weights; the muscle (ventricle) will naturally get bigger (hypertrophy).
- Rule out shunts: Eliminate choice 4 because it describes a volume problem (too much blood) rather than the pressure problem (difficulty pushing blood) found in stenosis.
- Prioritize local effects: Focus on the anatomical site of the defect (the valve) and choose the complication that occurs immediately "upstream" from that site.
Take home points
- Left ventricular hypertrophy is the hallmark compensatory response to chronic aortic stenosis.
- Over time, the thickened heart muscle becomes less efficient, leading to diastolic dysfunction.
- Significant hypertrophy increases the risk of myocardial ischemia because the coronary arteries cannot supply the thickened wall.
- EKG findings in these children typically show left axis deviation and increased QRS voltage.
A nurse is planning care for a child with aortic stenosis. Which nursing actions are appropriate? Select all that apply
Explanation
Aortic stenosis is a congenital obstructive cardiac malformation involving the narrowing of the aortic valve. This mechanical barrier restricts the outflow of blood from the left ventricle into the systemic circulation, creating a high pressure gradient. This results in a relatively fixed cardiac output that cannot increase to meet elevated metabolic demands. Chronic exposure to this high afterload leads to compensatory concentric left ventricular hypertrophy and increased myocardial oxygen consumption.
Rationale for correct answers:
C. Assessing for chest pain or syncope is a priority because these symptoms indicate critical myocardial ischemia or inadequate cerebral perfusion. In adolescents, exertional syncope is a major warning sign for potential sudden cardiac death. Frequent monitoring allows the nurse to evaluate the severity of the outflow obstruction and the risk for lethal arrhythmias.
D. Educating parents about activity limitations is essential to prevent episodes of ischemia triggered by physical exertion. Children with moderate to severe stenosis must avoid competitive sports and isometric exercises to protect the heart. This instruction reduces the risk of syncope and sudden cardiac arrest during high-demand activities.
E. Monitoring blood pressure regularly is necessary to track the child's systemic perfusion and evaluate for complications like heart failure. While the pressure gradient occurs across the valve, the nurse must ensure the systolic pressure is sufficient to meet peripheral demands. It also provides a baseline for evaluating the effectiveness of any pharmacological interventions or surgical repairs.
Rationale for incorrect answers:
A. Monitoring for signs of increased cardiac output is unnecessary because aortic stenosis typically leads to a decreased or fixed cardiac output. The narrowed valve acts as a bottleneck that prevents the heart from pumping more blood. Nurses should instead monitor for signs of low cardiac output, such as poor peripheral pulses and fatigue.
B. Providing a high sodium diet is contraindicated because it promotes fluid retention and increases circulating volume. This places additional volume overload on a left ventricle that is already struggling against a high-pressure obstruction. A sodium-restricted diet is more likely to be ordered if the child shows signs of congestive heart failure.
F. Requesting a prescription for indomethacin is inappropriate because this drug is used to close a patent ductus arteriosus. In some cases of critical aortic stenosis, the infant actually requires the ductus to stay open to maintain systemic flow. Indomethacin would have no therapeutic benefit for valvular narrowing and could be dangerous in ductal-dependent lesions.
Test-taking strategy
- Focus on safety risks: Identify that chest pain and activity levels are the most direct safety concerns in obstructive heart defects.
- Identify the physiological limit: Remember that stenosis is a "blockage"; therefore, the heart cannot increase output, it can only struggle to maintain it.
- Link diet to heart failure: In almost all cardiac conditions involving a pump problem, you would limit sodium rather than increase it.
- Differentiate drug actions: Recall that indomethacin is for closing holes, whereas stenosis is a problem of a valve being too tight.
- Select based on surveillance: Blood pressure is a standard nursing assessment for any child with a cardiovascular diagnosis.
Take home points
- The primary nursing goals for aortic stenosis are managing activity levels and monitoring for signs of low cardiac output.
- Exertional chest pain is a medical emergency in these patients and suggests severe myocardial oxygen mismatch.
- Physical education and sports participation must be strictly guided by the child's specific pressure gradient.
- Accurate blood pressure monitoring helps detect the onset of left-sided heart failure.
A nurse is explaining the pathophysiology of aortic stenosis to a parent. Which explanation is most accurate?
Explanation
Aortic stenosis is a congenital obstructive cardiac malformation where the aortic valve is narrowed or stiff. This creates a mechanical bottleneck that disrupts the normal flow of oxygenated blood. Because the exit is smaller than it should be, the heart must generate much higher pressures to force blood out, leading to significant hemodynamic stress on the primary pumping chamber.
Rationale for correct answer:
B. The left ventricle is the chamber responsible for pumping oxygenated blood to the entire body. In aortic stenosis, the narrowed valve creates increased resistance. To overcome this "kink in the hose," the left ventricle must pump harder and under higher pressure, which eventually causes the heart muscle to hypertrophy and potentially fail.
Rationale for incorrect answers:
A. Blood does not flow directly from the lungs into the aorta. In a normal heart, and in aortic stenosis, blood travels from the lungs to the left atrium, then the left ventricle, and then into the aorta. This choice describes an incorrect anatomical pathway.
C. Blood mixing between the atria is the definition of an atrial septal defect (ASD). Aortic stenosis is a valvular problem on the left side of the heart; it does not typically involve a hole or "mixing" between the upper chambers of the heart.
D. Pulmonary circulation becoming overloaded is characteristic of left-to-right shunts, such as a ventricular septal defect (VSD) or patent ductus arteriosus (PDA). While severe, long-term aortic stenosis can eventually cause backup into the lungs, its primary pathophysiology is an outflow obstruction, not a volume overload of the pulmonary circuit.
Test-taking strategy:
- Identify the "Stenosis" keyword: Whenever you see "stenosis," think of narrowing, obstruction, or resistance.
- Locate the chamber: Aortic = left ventricle. Therefore, the correct answer must involve the left ventricle working harder.
- Visualize the flow: Think of the heart as a pump. If the "exit pipe" (aorta) is narrow, the "pump" (ventricle) has to work with more force.
- Eliminate shunts: If the answer choice mentions "mixing" or "holes," it’s likely describing a different category of defect like VSD or ASD.
Take home points
- Aortic stenosis causes increased afterload for the left ventricle.
- The most common structural result in aortic stenosis is left ventricular hypertrophy.
- The primary symptom is a systolic murmur caused by turbulent blood flow through the narrow opening.
Practice Exercise 3
A nurse is educating a group of nurses on congenital heart defects. Which statement best describes a characteristic of valvular pulmonic stenosis?
Explanation
Valvular pulmonic stenosis is a congenital obstructive right-sided heart defect where the pulmonary valve leaflets are malformed, thickened, or fused. This mechanical barrier restricts the flow of deoxygenated blood from the right ventricle into the pulmonary artery, creating a high-pressure gradient. To overcome this resistance and maintain pulmonary perfusion, the right ventricle must work significantly harder, leading to hemodynamic changes and structural remodeling of the right heart.
Rationale for correct answer:
D. In the most common form of valvular pulmonic stenosis, the divisions between the cusps (leaflets) are fused, often forming a dome-shaped structure with a tiny central opening. This fusion prevents the valve from opening fully during systole, creating the "bottleneck" that characterizes the defect.
Rationale for incorrect answers:
A. The valve is not normal. By definition, stenosis implies a structural abnormality, either the valve is bicuspid, thickened, or the leaflets are fused. A normal valve would allow unobstructed blood flow to the lungs.
B. The right ventricle is typically hypertrophied that is thickened, not hypoplastic which means underdeveloped. Because it must pump against high resistance, the muscle grows larger to compensate. A hypoplastic right ventricle is more characteristic of pulmonary atresia or tricuspid atresia.
C. Right ventricular hypertrophy develops, not left. The pulmonary valve is the exit for the right ventricle. Therefore, the workload increase and subsequent muscle thickening occur exclusively on the right side of the heart.
Test-taking strategy:
- Anatomy match: Connect "pulmonic" to the right ventricle and "aortic" to the left ventricle. This helps you eliminate choice C.
- Defining "stenosis": Recognize that stenosis is a physical narrowing. Choice 4 provides the specific anatomical reason for that narrowing (fused cusps).
- Muscle logic: Think of the heart as a muscle at the gym. If the right ventricle is "lifting heavier weights" due to an obstruction, it will get bigger (hypertrophy), not smaller (hypoplastic).
Take home points
- Pulmonic stenosis causes right ventricular hypertrophy due to pressure overload.
- The hallmark physical finding is a systolic ejection murmur heard at the upper left sternal border.
- Severe cases may cause cyanosis if the high right-sided pressure forces deoxygenated blood through a patent foramen ovale (PFO).
A nurse is assessing a client with moderate pulmonary stenosis. Which findings are consistent with this condition? Select all that apply
Explanation
Pulmonary stenosis is an obstructive heart defect where the valve between the right ventricle and the pulmonary artery is narrowed. This creates a mechanical "bottleneck" that prevents the heart from efficiently sending deoxygenated blood to the lungs. Because the right side of the heart must pump against this high resistance, it eventually thickens and may fail, leading to symptoms associated with decreased oxygenation and systemic backup.
Rationale for correct answers:
A. A systolic murmur at the left upper sternal border is the hallmark physical finding. As the right ventricle squeezes blood through the narrow, tight valve during systole, it creates significant turbulence. This is heard loudest at the "pulmonic area", that is the second intercostal space, left sternal border.
B. Fatigue with feeding occurs because the heart cannot increase blood flow to the lungs to meet the body's increased oxygen demand. In infants, the act of sucking and swallowing is their primary form of exercise, and a fixed cardiac output results in rapid exhaustion.
E. Decreased blood flow to the lungs is the primary hemodynamic consequence of the narrowing. Since the exit is obstructed, less blood reaches the pulmonary capillary beds for gas exchange. In severe cases, this leads to hypoxemia and cyanosis.
Rationale for incorrect answers:
C. Increased pulmonary congestion is characteristic of left-to-right shunts like VSD or left-sided failure like aortic stenosis. In pulmonary stenosis, the problem is that not enough blood is getting to the lungs; therefore, the lungs typically appear clear or under-circulated on a chest X-ray.
D. Left ventricular hypertrophy results in obstruction on the right side of the heart. The workload increases for the right ventricle, leading to right ventricular hypertrophy (RVH). The left ventricle is generally unaffected in size unless a secondary complication occurs.
Test-taking strategy:
- Right vs. Left: Always associate the pulmonary valve with the right side of the heart and the aorta with the left side. This helps you eliminate choice D.
- Volume vs. Obstruction: If a valve is narrow (stenosis), blood flow after that valve will be decreased. If there is a hole (shunt), blood flow is usually increased.
- Remember that systolic murmurs are common in all "stenosis" defects because they occur when the heart is actively ejecting blood past the blockage.
Take home points
- Moderate pulmonary stenosis limits the heart's ability to oxygenate blood during stress or activity.
- The lungs will typically appear "darker" or less vascular on imaging due to reduced flow.
- Clinical management focuses on relieving the pressure gradient, often through balloon valvuloplasty.
A nurse is reviewing diagnostic studies for pulmonary stenosis. Which test is most definitive?
Explanation
Pulmonary stenosis is a valvular obstructive lesion that impairs right ventricular outflow. The definitive diagnosis relies on high-resolution imaging to visualize the anatomic structure and quantify the pressure gradient across the valve. Advanced diagnostics allow for the assessment of ventricular hypertrophy and the exclusion of associated defects like a patent foramen ovale or septal defects.
Rationale for correct answer:
C. Echocardiography is the gold standard because it provides real-time visual confirmation of valve morphology and leaflet mobility. Utilizing Doppler technology, clinicians can calculate the pressure gradient across the stenotic area to determine severity. It is a non-invasive, definitive tool that accurately measures right ventricular function and chamber dimensions without exposing the infant to radiation or invasive catheters.
Rationale for incorrect answers:
A. A chest x-ray provides a silhouette of the heart but cannot visualize internal structures like the pulmonary valve. While it may show prominent pulmonary segments due to post-stenotic dilation, it lacks the specificity required for a definitive diagnosis. It serves as a supportive screening tool rather than a confirmatory diagnostic for the exact site or degree of stenosis.
B. An electrocardiogram (ECG) detects electrical activity and may show right axis deviation or right ventricular hypertrophy in chronic cases. However, these findings are secondary changes and do not provide a direct assessment of the valve itself. Many other conditions, such as pulmonary hypertension, can produce similar ECG patterns, making it non-pathognomonic for pulmonary stenosis.
D. Pulse oximetry measures the percentage of hemoglobin saturation but does not diagnose the underlying structural cause of hypoxemia. In mild pulmonary stenosis, the oxygen saturation may remain within normal limits (≥ 95%), providing a false sense of security. It is a physiological monitoring tool used to assess clinical stability rather than a definitive diagnostic test for valvular pathology.
Test-taking strategy:
- Distinguish between screening tools and confirmatory tests. X-rays and ECGs suggest a problem, but imaging (echo) confirms the specific anatomical defect.
- Focus on the anatomy-function link: Since pulmonary stenosis is a physical blockage, the test that "sees" the physical valve (echocardiogram) is the most definitive.
- Apply the non-invasive gold standard rule: In pediatric cardiology, the echocardiogram is almost always the definitive non-invasive test for structural heart disease.
- Evaluate specificity vs. sensitivity: While pulse oximetry is sensitive to low oxygen, it is not specific to the pulmonary valve; an echo is highly specific to the valvular structure.
- Remember the Doppler effect: Any question asking for the "degree" or "severity" of a valve issue will point toward ultrasound-based diagnostics like the echocardiogram.
Take home points
- Echocardiography uses ultrasound waves to produce images of the heart's chambers, valves, and surrounding structures.
- The Doppler component of the echo is essential for measuring the velocity of blood flow to calculate the stenotic gradient.
- Mild stenosis is usually defined by a peak gradient < 25 mmHg, whereas severe stenosis exceeds 50 mmHg.
- This diagnostic modality is also used post-operatively to monitor the success of a balloon valvuloplasty or surgical repair.
A nurse is planning teaching for parents of a child with pulmonary stenosis. Which topics should be included? Select all that apply
Explanation
Pulmonary stenosis is a chronic congenital heart defect that requires long-term management rather than an immediate "cure." Education for parents focuses on maintaining the child's hemodynamic stability, monitoring for the progression of the obstruction, and ensuring the family can identify signs of decreasing cardiac reserve. Because the right ventricle must work significantly harder to pump blood to the lungs, the family's ability to monitor daily physiological tolerance is a cornerstone of safe home care.
Rationale for correct answers:
A. Importance of follow-up cardiology care is critical because pulmonary stenosis can be progressive. Regular echocardiograms are necessary to monitor the pressure gradient across the valve. As the child grows, the degree of stenosis may worsen, or the heart muscle may show signs of strain such as right ventricular hypertrophy that require surgical or interventional timing adjustments.
B. Recognition of activity intolerance allows parents to gauge the severity of the obstruction during daily life. Symptoms like shortness of breath, fatigue during play, or taking frequent breaks are indicators that the heart is unable to meet the body's oxygen demands. Teaching parents to spot "subtle" fatigue ensures that worsening conditions are reported before a cardiac crisis occurs.
E. Medication adherence is vital if the child has been prescribed drugs to manage symptoms or prevent complications. This may include diuretics to reduce the workload on the right side of the heart or medications to manage heart failure if the stenosis is severe. Even if the child appears healthy, maintaining the steady-state of these medications prevents sudden decompensation.
Rationale for incorrect answers:
C. Pulmonary stenosis is typically managed very successfully with balloon valvuloplasty or surgical valvotomy. A heart transplant is a last-resort treatment for end-stage heart failure or complex defects like Hypoplastic Left Heart Syndrome, not for a localized valvular obstruction like pulmonary stenosis.
D. Children with congenital heart defects are at a higher risk for complications from respiratory illnesses like the flu or pertussis. Staying up-to-date on immunizations is essential to protect them from infections that would further stress their cardiovascular system.
Test-taking strategy
- Identify the "acuity" of the defect: Pulmonary stenosis is an obstruction, but it is rarely a reason for a transplant. Look for treatments that match the defect that is repairing the valve.
- General health principles: In pediatric nursing, you almost never delay vaccinations for a cardiac defect; if anything, the child needs them more urgently to prevent added stress.
- Chronic vs. Acute: Follow-up care and monitoring are the "gold standards" for any parent education regarding a congenital structural heart issue.
Take home points
- Pulmonary stenosis is an obstructive lesion, meaning the heart has a "plumbing" problem that limits flow to the lungs.
- Education should emphasize that the child can often lead a relatively normal life with proper monitoring.
- Parents should be taught to report any cyanosis immediately, as this may indicate the shunt has reversed due to high right-sided pressure.
A nurse is providing discharge teaching to the caregiver of a child with pulmonary stenosis. Which of the following caregiver statements indicate correct understanding? Select all that apply
Explanation
Pulmonary stenosis is a narrowing of the pulmonary valve that causes the right ventricle to work harder to pump blood to the lungs. Discharge teaching focuses on monitoring for decreased cardiac output, ensuring hemodynamic stability, and preventing long-term complications like right-sided heart failure.
Rationale for correct answers:
C. “I will keep all scheduled cardiology follow-up appointments.” Pulmonary stenosis is often a progressive condition. Even if a child has had a successful balloon valvuloplasty, the valve can re-narrow as the child grows (restenosis). Regular echocardiograms are the only way to monitor the pressure gradient and ensure the right ventricle isn't becoming dangerously thick.
D. “I should notify the provider of any signs of shortness of breath.” Shortness of breath is a hallmark sign that the heart is unable to provide enough oxygenated blood to the body. It can also indicate that the right ventricle is beginning to fail. Early reporting allows for medical adjustments before the child reaches a state of critical decompensation.
Rationale for incorrect answers:
A. “It is normal for the child to be easily fatigued during feeding.” While fatigue is a symptom of the disorder, it is never normal or acceptable. Fatigue during feeding is a red-flag sign of heart failure in infants. It indicates that the heart cannot even handle the metabolic demand of eating, which is a sign that the stenosis is likely severe and needs intervention.
B. “I will encourage the child to participate in competitive sports in school.” Children with moderate to severe stenosis are usually restricted from competitive or high-intensity sports. Strenuous activity increases the demand for oxygenated blood, because the valve is narrowed, the heart has a fixed output and cannot meet that demand, which can lead to fainting or even sudden cardiac arrest.
E. “I will discontinue medications once the child appears asymptomatic.” Cardiac medications such as diuretics or afterload reducers must be taken exactly as prescribed. Often, a child appears asymptomatic because the medication is working. Abruptly stopping these drugs can lead to a rapid return of symptoms and acute heart failure.
Test-taking strategy:
- The "normal" trap: Be wary of any answer choice that calls a pathological symptom like fatigue or cyanosis normal.
- Safety first: In pediatric cardiology, exercise restrictions are common for obstructive defects. If the valve is tight, the output is limited, making competitive sports a high-risk activity.
- Chronic management: Follow-up and medication adherence are standard for almost all congenital heart defects (CHDs).
Take home points
- Pulmonary stenosis severity is determined by the pressure gradient measured across the valve during an echocardiogram.
- Caregivers must be educated to recognize subtle signs of failure to thrive and respiratory distress as indicators of worsening obstruction.
- Infective endocarditis prophylaxis may be required for certain dental procedures depending on the specific anatomy and repair status.
- Activity levels must be individualized based on the degree of stenosis and the presence of ventricular hypertrophy.
Comprehensive Questions
A nurse is teaching parents of a child with repaired coarctation of the aorta. Which long-term concerns should the nurse include? Select all that apply
Explanation
Coarctation of the aorta repair requires lifelong vigilance due to the high incidence of residual cardiovascular sequelae. Even after successful surgical or transcatheter intervention, patients remain predisposed to vasculopathy and altered arterial compliance. The structural integrity of the anastomosis can be compromised by somatic growth or intimal hyperplasia. Chronic hemodynamic stress on the left ventricle necessitates consistent longitudinal follow-up to prevent secondary organ damage.
Rationale for correct answers:
A. Systemic hypertension persists in a significant percentage of patients despite a successful anatomical repair. This is often attributed to permanent changes in baroreceptor sensitivity or residual narrowing of the aortic arch. Persistent hypertension increases the long-term risk for premature atherosclerosis and stroke.
B. Recoarctation refers to the restenosis of the aorta at the previous surgical or balloon angioplasty site. It is most common in infants who underwent repair but can occur at any age due to fibrotic scarring. Frequent screening is necessary to detect a returning pressure gradient before significant symptoms develop.
D. Routine blood pressure monitoring is the cornerstone of post-repair surveillance for these pediatric patients. It allows for the early detection of both systemic hypertension and potential re-narrowing of the aorta. Measurements should be obtained in both upper and lower extremities to ensure ongoing vascular patency.
Rationale for incorrect answers:
C. Lifelong oxygen therapy is not indicated because coarctation of the aorta is an obstructive lesion rather than a primary hypoxemic lung disease. Once the mechanical narrowing is corrected, systemic oxygenation typically remains within normal limits. Oxygen is generally reserved for cyanotic heart defects or chronic pulmonary hypertension.
E. Development of cyanosis with activity is not an expected finding following a successful repair of an obstructive cardiac defect. Coarctation does not involve a right-to-left shunt that would cause deoxygenated blood to enter the systemic circulation. New onset cyanosis would suggest an entirely different pathology or severe acute heart failure.
Test-taking strategy:
- Differentiate cardiac defects that cause cyanosis vs. those that do not cause cyanosis: Eliminate options involving oxygen or cyanosis because coarctation is a left-sided obstructive lesion, not a shunting defect.
- Focus on the "mechanical" nature: Since the defect is a physical narrowing, the two biggest risks are that the narrowing comes back or that the high pressure caused by the narrowing doesn't go away.
- Identify standard surveillance: In any cardiovascular repair, blood pressure is the most basic and vital parameter to track for the rest of the patient's life.
- Consider growth factors: Remember that as a child grows, a surgical site that does not grow at the same rate will inevitably lead to recoarctation.
Take home points
- Children with repaired coarctation require annual cardiology follow-up throughout their entire lives.
- Persistent hypertension must be treated aggressively with antihypertensives to protect the brain and kidneys.
- Exercise testing may be used during follow-up to evaluate the blood pressure response to physical stress.
- Endocarditis prophylaxis is generally no longer required unless there is a residual defect or prosthetic material.
A nurse is reviewing the history of a client with newly diagnosed coarctation of the aorta. Which historical findings support this diagnosis? Select all that apply
Explanation
A. Frequent headaches result from chronic hypertension in the upper body. The vessels proximal to the aortic narrowing are exposed to elevated pressures. This cephalic congestion leads to persistent or recurrent cephalgia. This symptom reflects the vascular stress on the cerebral circulation.
B. Nosebleeds, or epistaxis, occur due to the fragility of the nasal mucosa vessels under high pressure. The upper body hyperperfusion caused by the obstruction increases the force against these small capillaries. It is a classic clinical manifestation of pre-stenotic hypertension.
E. Leg pain with exercise, or claudication, is caused by inadequate oxygen delivery to the lower limb muscles. During physical activity, the metabolic demand of the legs exceeds the restricted supply permitted by the narrowed aorta. This results in ischemic pain that subsides with rest.
Rationale for incorrect answers:
C. Bounding lower extremity pulses are not found in this condition. The narrowing specifically reduces the pulse volume and pressure distal to the site of coarctation. Femoral pulses are typically described as weak, delayed, or entirely absent upon palpation.
D. Cool upper extremities are inconsistent with the pathophysiology of this defect. The upper body receives blood from the aorta before the point of constriction and is therefore warm and well-perfused. It is the lower extremities that typically feel cool to the touch.
Test-taking strategy:
- Analyze the flow of blood: Visualize the aorta and remember that coarctation is a "kink" in the garden hose. Everything before the kink has high pressure, and everything after the kink has low pressure.
- Map symptoms to anatomy: Headaches and nosebleeds are "above the kink" due to high pressure. Leg pain and cold skin are "below the kink" result from the low pressure.
- Identify pulse characteristics: Bounding pulses always occur where the pressure is highest. Since the legs are after the obstruction, their pulses must be diminished, not bounding.
- Evaluate exercise intolerance: Recognize that "claudication" is a hallmark of any arterial obstruction. If blood cannot get through the narrow aorta fast enough to feed working leg muscles, pain will occur.
- Eliminate opposites: If you know the legs are poorly perfused, you must eliminate any choice suggesting strong pulses or warm skin in the lower body.
Take home points
- Upper body symptoms like headaches and epistaxis are caused by hypertension proximal to the narrowing.
- Lower body symptoms like leg cramps and cool skin are caused by hypotension distal to the narrowing.
- A hallmark physical exam finding is the "brachial-femoral delay," where the radial pulse is felt before the femoral pulse.
- In infants, the first sign may be acute heart failure or cardiogenic shock when the ductus arteriosus closes.
A nurse is caring for a child after surgical repair of coarctation of the aorta. Which assessments are priorities in the immediate postoperative period? Select all that apply
Explanation
Postoperative care for coarctation of the aorta focuses on monitoring hemodynamic stability and assessing the patency of the new anastomosis. The sudden transition from chronic high resistance to perfused distal vascular beds can trigger a surge in sympathetic activity. This results in paradoxical hypertension, which must be managed to prevent tension on the suture line. Ensuring adequate renal perfusion is equally vital, as the kidneys adjust to normalized blood flow after years of hypoperfusion.
Rationale for correct answers:
A. Comparing blood pressure in upper and lower extremities is the most direct way to evaluate the success of the surgical repair. The nurse expects to see a significant reduction or total resolution of the preoperative pressure gradient. Persistent or worsening discrepancies may indicate surgical failure or acute thrombosis at the repair site.
B. Assessment of femoral pulse quality provides an immediate bedside indicator of distal aortic patency. Strong, palpable pulses in the lower extremities signify that blood is successfully traversing the repaired segment of the aorta. Weak or absent pulses post-surgery are red-flag findings that necessitate urgent surgical re-evaluation.
C. Urine output is a critical indicator of kidney perfusion and overall cardiac output in the immediate recovery phase. Because the renal arteries are located distal to the coarctation, they are sensitive to hemodynamic changes following the removal of the obstruction. A drop in output below 1 ml/kg/hr may signal low cardiac output or renal vascular complications.
Rationale for incorrect answers:
D. Monitoring for signs of infection at the incision site is a standard nursing intervention, but it is not a priority in the immediate (first 24 hours) postoperative period. Surgical site infections typically take days to manifest through erythema, warmth, or purulent drainage. Immediate concerns must focus on life-threatening hemodynamic instability rather than subacute inflammatory processes.
E. Daily weight trends are useful for long-term monitoring of fluid volume status and nutritional progress in pediatric patients. However, in the high-acuity immediate postoperative hours, hourly output and invasive pressure monitoring provide more actionable data. Weight changes over a 24-hour period are too slow to guide emergency interventions for acute surgical complications.
Test-taking strategy:
- Prioritize "Immediate" vs. "Long-term": When a question uses the word immediate, look for assessments that detect life-threatening or surgical-failure complications such as pulses and BP gradients.
- Focus on the specific defect: For coarctation, the most specific assessments always involve the gradient between the top and bottom of the body.
- Apply the ABCs and Perfusion: Urine output and pulse quality are direct measures of circulation, which is the priority in the immediate post-surgical window.
- Identify the "Normal" postoperative timeline: Rule out infection as an immediate priority because it is a complication that occurs later in the recovery trajectory.
Take home points
- The primary goal after coarctation repair is maintaining stable blood pressure to protect the anastomosis.
- Paradoxical hypertension occurs in many patients post-repair and requires aggressive vasodilator therapy.
- Abdominal pain should be assessed frequently to rule out mesenteric arteritis caused by sudden increased intestinal perfusion.
- A return of the pressure gradient between limbs suggests acute recoarctation or graft occlusion.
A child with coarctation of the aorta experiences a postsurgical re-coarctation. Which treatment should the nurse expect the physician to recommend?
Explanation
Recurrent coarctation, or re-coarctation, is a frequent postoperative complication involving the narrowing of the aortic lumen at the previous surgical site. This condition often results from intimal hyperplasia or inadequate growth of the anastomosis in pediatric patients. It manifests as a return of the pressure gradient between upper and lower extremities. Percutaneous intervention is the preferred primary management strategy for recurrence.
Rationale for correct answer:
C. Balloon angioplasty is the preferred treatment for re-coarctation due to its minimally invasive nature and high success rate. It effectively dilates the stenotic area using a catheter-guided balloon to disrupt the fibrotic tissue. This procedure avoids the significant morbidity associated with a repeat thoracotomy.
Rationale for incorrect answers:
A. A bypass graft repair is typically reserved for complex or long-segment primary coarctation in older patients. It involves using a synthetic tube to shunt blood around the narrow segment. This is rarely the first choice for recurrent narrowing when less invasive options exist.
B. Patch aortoplasty involves the surgical widening of the aorta using a synthetic or prosthetic material to enlarge the lumen. While effective for primary repair, it carries a long-term risk of aneurysm formation at the repair site. It is not the standard approach for simple postoperative re-coarctation.
D. Left subclavian flap angioplasty is a surgical technique primarily used in neonates for the initial repair of the defect. It utilizes the patient's own subclavian artery to patch the narrowed aortic area. It is technically difficult and less effective for addressing fibrotic re-coarctation.
Test-taking strategy:
- Distinguish between primary and secondary repair: Recognize that the question specifies a postsurgical recurrence, which changes the preferred medical hierarchy of interventions.
- Prioritize least invasive methods: In modern pediatric cardiology, interventional radiology (catheter-based) is favored over repeat open-chest surgery for simple restenosis.
- Recognize "Gold Standard" for recurrence: Memorize that balloon angioplasty (with or without stenting) is the specific treatment of choice for a narrowing that occurs after an initial surgical fix.
- Eliminate neonatal-specific procedures: Rule out the subclavian flap if the context implies a child who has already undergone an initial surgery, as that flap has already been used or bypassed.
- Assess surgical risk: Consider that repeat thoracotomy carries higher risks of bleeding and nerve damage, making non-surgical options like choice 3 more desirable.
Take home points
- Balloon angioplasty is the first-line treatment for post-surgical re-coarctation in children.
- Re-coarctation is suspected when the blood pressure gradient between arms and legs exceeds 20 mmHg.
- Stent placement may be combined with angioplasty in older children to provide structural support to the vessel.
- Long-term follow-up with MRI or CT angiography is essential to monitor for restenosis or aneurysm formation.
A nurse is assessing a child with suspected coarctation of the aorta. Which of the following factors is a necessary part of the assessment?
Explanation
Coarctation of the aorta involves a constriction of the distal aortic arch which creates a significant hemodynamic pressure differential. This mechanical obstruction leads to cephalic hypertension and reduced systemic perfusion to the lower body. Clinical assessment must prioritize detecting gradients between pre-stenotic and post-stenotic vascular beds. Accurate manometry is vital to quantify the severity of the aortic narrowing.
Rationale for correct answer:
D. Evaluating blood pressure in four extremities is the gold standard for detecting the characteristic pressure gradient. A significant discrepancy where the upper extremities are hypertensive compared to the lower extremities confirms the diagnosis. At least a 20 mmHg systolic difference is clinically significant for this cardiac defect.
Rationale for incorrect answers:
A. Assessment of skin turgor is used to evaluate hydration status and fluid volume deficit in pediatric patients. While important in general pediatrics, it does not provide specific diagnostic data regarding the presence of an aortic obstruction. It reflects interstitial fluid rather than the mechanical output of the left ventricle.
B. Body temperature is a vital sign used to identify infection or inflammatory processes like endocarditis. Although children with cardiac defects are at higher risk for infections, temperature does not confirm the structural presence of a coarctation. It is a nonspecific indicator of metabolic or immunological activity.
C. Pupil size and reaction to light assess neurological function and cranial nerve integrity. These findings are relevant in cases of increased intracranial pressure or head trauma but are not primary indicators of a congenital heart defect. They do not correlate with the vascular narrowing found in the aorta.
Test-taking strategy
- Focus on the pathophysiology: Since coarctation is an obstructive defect affecting blood flow distribution, the assessment must measure that distribution directly.
- Prioritize the "classic" sign: The definitive assessment for coarctation of the aorta is always the comparison of upper and lower extremity pressures.
- Rule out general assessments: While temperature and skin turgor are part of a comprehensive head-to-toe exam, they are not "necessary" to identify this specific structural defect.
- Look for hemodynamic data: Choice 4 is the only option that addresses the hemodynamics of the aorta and the specific pressure changes caused by the lesion.
Take home points
- A systolic blood pressure higher in the arms than the legs is pathognomonic for coarctation of the aorta.
- Radial pulses may be bounding while femoral pulses are weak, delayed, or entirely absent.
- Infants may present with signs of congestive heart failure, while older children may be asymptomatic until a routine screening.
- Accurate assessment requires using appropriately sized blood pressure cuffs on both arms and both legs.
A nurse is caring for a client post-operative for a coarctation of the aorta repair. Which intervention is recommended?
Explanation
Post-operative management following repair of aortic coarctation requires meticulous hemodynamic monitoring to prevent paradoxical hypertension. This phenomenon occurs due to sudden exposure of the distal vascular bed to high pressure and activation of the renin-angiotensin system. Ensuring vascular stability is the primary goal in the immediate recovery phase.
Rationale for correct answer:
C. Maintaining a normal to low blood pressure is essential to protect the anastomosis site from excessive mechanical stress. High systemic pressures can lead to catastrophic hemorrhage or the development of postoperative mesenteric arteritis. Vasodilators like nitroprusside are frequently utilized to achieve these specific hemodynamic targets.
Rationale for incorrect answers:
A. Administering a vasoconstrictor would be contraindicated as it exacerbates hypertension and increases afterload on the left ventricle. This would place undue tension on the surgical repair site and increase the risk of vascular injury. It would further stimulate the already overactive sympathetic response seen after this specific surgery. Instead, vasodilators like nitroprusside are frequently used to maintain normal to low blood pressure.
B. Maintaining hypothermia is not a standard intervention for postoperative coarctation repair and can cause shivering. Shivering significantly increases oxygen consumption and metabolic demand, placing unnecessary stress on the heart. It can also cause peripheral vasoconstriction, which counterintuitively raises the systemic blood pressure.
D. Giving a bolus of I.V. fluids is generally avoided unless the patient shows clear signs of hypovolemia. Rapid volume expansion can trigger or worsen postoperative hypertension by increasing stroke volume against a healing aorta. Careful fluid restriction or maintenance rates are usually preferred to prevent fluid overload.
Test-taking strategy
- Identify the primary surgical risk: Recognize that the most dangerous postoperative complication after an aortic repair is bleeding or rupture at the suture line.
- Link physiology to intervention: Understand that high pressure equals high stress on the vessel wall; therefore, lowering the pressure is the logical protective measure.
- Evaluate the "Paradoxical" effect: Remember that the body often reacts to coarctation repair with a spike in sympathetic tone, making blood pressure control a high-priority nursing action.
- Apply safety principles: In any vascular surgery, hemostasis and suture integrity are prioritized through the avoidance of hypertensive crises.
Take home points
- Postoperative hypertension must be aggressively managed to prevent mesenteric ischemia and bowel necrosis.
- Abdominal pain and distension after surgery should be reported immediately as signs of intestinal complications.
- Sodium nitroprusside or esmolol are the preferred intravenous agents for rapid titration of blood pressure.
- The nurse must frequently assess the strength and symmetry of pulses in both upper and lower extremities.
The school nurse has been following a child who comes to the office frequently for vague complaints of dizziness and headache. Today, she is brought in after fainting in the cafeteria following a nosebleed. Her BP is 122/85, and her radial pulses are bounding. The nurse suspects she has:
Explanation
Coarctation of the aorta is a congenital obstructive cardiac defect involving a localized constriction of the aortic arch. This narrowing typically occurs distal to the left subclavian artery, resulting in a significant pressure disparity between the cephalic and pedal circulations. Chronic exposure to high arterial pressure in the upper body leads to secondary hypertension and compensatory left ventricular hypertrophy.
Rationale for correct answers:
B. Recurrent headaches, dizziness, and spontaneous epistaxis are classic signs of upper body hypertension caused by the aortic narrowing. The finding of bounding radial pulses indicates high stroke volume and pressure in the vessels proximal to the obstruction. This clinical constellation specifically points to the hemodynamic pattern of coarctation.
Rationale for incorrect answers
A. Transposition of the great vessels is a cyanotic lesion presenting shortly after birth with profound hypoxemia. It involves the complete reversal of the aorta and pulmonary artery, creating two parallel circulatory loops. It does not typically manifest with isolated hypertension and bounding upper pulses in an older school-aged child.
C. Aortic stenosis results from a narrowed aortic valve, which obstructs the total outflow from the left ventricle. This leads to a global decrease in systemic perfusion and weak or thready pulses throughout all extremities. It does not produce the localized discrepancy between upper and lower body pressures seen in this case.
D. Pulmonic stenosis involves an obstruction of blood flow from the right ventricle to the pulmonary artery. This causes right-sided heart strain and decreased pulmonary perfusion rather than systemic hypertension. Symptoms usually include exertional dyspnea and cyanosis rather than bounding radial pulses and nosebleeds.
Test-taking strategy:
- Correlate symptoms with vascular regions: Recognize that headaches and epistaxis are results of "too much pressure" in the head, while dizziness and fainting can occur from poor autoregulation of that high pressure.
- Match pulse quality to anatomy: Bounding pulses in the arms combined with signs of high blood pressure indicates an obstruction occurring after the branch points of the arms.
- Use the "Pathognomonic" rule: The combination of upper body hypertension and epistaxis in a child is a classic indicator for coarctation of the aorta.
- Rule out right-sided defects: Eliminate pulmonic stenosis because it affects the lungs and venous system, not the systemic arterial pressure or radial pulse quality.
- Distinguish valvular from vascular: Rule out aortic stenosis because it would make all pulses weak rather than making the radial pulses bounding.
Take home points
- Coarctation of the aorta should be suspected in any child presenting with unexplained hypertension or frequent nosebleeds.
- Bounding pulses in the upper extremities contrasted with weak or absent femoral pulses is a hallmark physical finding.
- Fainting or dizziness in these patients often results from transient cerebral hypertensive crises or exercise-induced discrepancies.
- The primary goal of assessment is to quantify the blood pressure gradient between the arms and the legs.
A nurse attended a staff education program on congenital heart defects (CHDS). In which CHD would the nurse need to take upper and lower extremity BPs?
Explanation
Coarctation of the aorta is a congenital obstructive cardiac malformation involving a focal narrowing of the aortic lumen. This constriction most commonly occurs at the juxtaductal position, immediately distal to the origin of the left subclavian artery. It results in a significant hemodynamic disparity between the pre-stenotic and post-stenotic arterial systems.
Rationale for correct answer:
C. Measurement of blood pressure in both upper and lower extremities is the definitive clinical assessment for coarctation. The mechanical obstruction prevents adequate systolic pressure from reaching the descending aorta. This creates a characteristic gradient where the arms are hypertensive and the legs are hypotensive.
Rationale for incorrect answers:
A. Transposition of the great vessels is a mixed cardiac defect where the aorta and pulmonary artery are switched. This creates two independent, parallel circuits rather than a systemic obstruction. Assessment focuses on oxygen saturation and the presence of a mixing lesion like an ASD. Blood pressure gradients between limbs are not a diagnostic feature.
B. Aortic stenosis involves narrowing of the aortic valve itself, which restricts blood flow out of the left ventricle. This causes a global decrease in cardiac output affecting all systemic arteries equally. While it results in narrow pulse pressures, it does not create a discrepancy between the upper and lower extremities.
D. Tetralogy of Fallot is characterized by a ventricular septal defect, pulmonary stenosis, right ventricular hypertrophy, and an overriding aorta. The primary clinical concern is right-to-left shunting leading to severe cyanosis and "tet spells." It does not involve a focal constriction of the aorta that would necessitate four-limb blood pressure monitoring.
Test-taking strategy:
- Identify the mechanical problem: Recognize that among the listed defects, only coarctation involves a physical narrowing of the vessel that supplies the lower body.
- Match the assessment to the defect: Remember that "upper and lower BP" is the classic nursing board answer specifically linked to the term coarctation.
- Differentiate between types of stenosis: Understand that aortic stenosis is a central pump problem (valve), whereas coarctation is a peripheral distribution problem (vessel).
- Use the "Four-Limb" rule: Any question mentioning blood pressure in all four extremities is screening for obstructive lesions of the aortic arch.
Take home points
- Coarctation of the aorta is the only defect that causes a blood pressure mismatch between the upper and lower body.
- A systolic pressure difference greater than 20 mmHg between the arms and legs is highly suggestive of the defect.
- Physical exam should also include simultaneous palpation of the radial and femoral pulses to check for femoral delay.
- Failure to diagnose coarctation early can lead to left ventricular failure and severe systemic hypertension.
The nurse is preparing a staff education program about congenital heart defects. Which heart defect and hemodynamic change pairing is correct?
Explanation
Aortic stenosis is a congenital obstructive left-sided heart defect involving the narrowing of the aortic valve. This mechanical restriction increases afterload on the left ventricle as it struggles to eject blood into the systemic circulation. Chronic pressure overload leads to significant myocardial hypertrophy and decreased coronary perfusion. Effective cardiac output depends on the severity of the valvular orifice narrowing.
Rationale for correct answer:
A. Aortic stenosis represents a classic obstruction to systemic blood flow originating from the left ventricle. The narrowed valve increases the pressure gradient required to move blood into the aorta. This directly causes a decrease in stroke volume and can lead to pulmonary congestion. It is the primary example of a ventricular outflow tract obstruction.
Rationale for incorrect answers:
B. Ventricular septal defect is a left-to-right shunt that increases pulmonary blood flow rather than decreasing it. Blood moves from the high-pressure left ventricle into the lower-pressure right ventricle. This over-perfusion of the lungs can lead to pulmonary hypertension. It does not cause a decrease in flow unless severe pulmonary vascular disease develops.
C. Tricuspid atresia involves the complete absence of the tricuspid valve, which diminishes pulmonary blood flow. Because blood cannot pass from the right atrium to the right ventricle, it must shunt through an atrial opening. This results in severe cyanosis because very little blood reaches the lungs for oxygenation. It is categorized as a decreased pulmonary flow defect.
D. Atrioventricular canal defect is primarily classified as an increased pulmonary blood flow lesion. While some mixing occurs due to the large central septal opening, the dominant hemodynamic shift is a left-to-right shunt. "Mixed blood flow" is the formal classification for complex lesions like transposition of the great arteries.
Test-taking strategy:
- Categorize by hemodynamic effect: Group defects into increased pulmonary flow, decreased pulmonary flow, obstructive, or mixed.
- Identify the keyword "Stenosis": In medical jargon, stenosis always refers to an obstruction or narrowing of a passage.
- Analyze shunt directions: Remember that simple septal holes (VSD/ASD) usually cause left-to-right shunting, which increases flow to the lungs.
- Distinguish between "Mixing" and "Shunting": Although most defects have some mixing, only specific complex anomalies like truncus arteriosus are officially labeled as "Mixed" defects in nursing curricula.
- Use the process of elimination: Rule out choices where the anatomy like atresia clearly prevents blood flow, making "increased flow" impossible.
Take home points
- Aortic stenosis creates a pressure gradient that results in left ventricular hypertrophy and potential failure.
- Left-to-right shunts like VSD lead to pulmonary over-circulation and signs of congestive heart failure.
- Right-to-left shunts or atretic valves cause desaturated blood to enter the system, leading to cyanosis.
- Complex defects like transposition of the great arteries require "mixing" for survival until surgical intervention.
A 2-day-old infant was just diagnosed with aortic stenosis. What is the most likely nursing assessment finding?
Explanation
Aortic stenosis is a congenital obstructive cardiac defect involving the narrowing of the aortic valve orifice. This structural anomaly impedes the ejection of blood from the left ventricle into the systemic circulation, creating a significant pressure gradient. In neonates, this restriction increases myocardial workload and can lead to rapid decompensation if the stenosis is critical. The primary clinical indicator of this turbulent flow is a specific auscultatory finding heard during the systolic phase of the cardiac cycle.
Rationale for correct answers:
D. A systolic ejection murmur is the most common and likely finding in a 2-day-old infant with this defect. The sound is produced by turbulent blood flow being forced through the narrow, stenotic valvular opening. It is typically heard loudest at the upper right sternal border and may radiate to the carotid arteries.
Rationale for incorrect answers:
A. A gallop rhythm and rales are clinical manifestations of acute congestive heart failure and pulmonary edema. While these can occur in cases of critical neonatal aortic stenosis, they are secondary complications rather than the primary diagnostic sign. They indicate a more advanced state of ventricular dysfunction rather than the defect itself.
B. Blood pressure discrepancies between the upper and lower extremities are the hallmark of coarctation of the aorta. In aortic stenosis, the obstruction is at the valvular level, which affects the entire systemic circulation equally. Therefore, there is no differential in pressure between the arms and the legs.
C. Right ventricular hypertrophy on an ECG is characteristic of defects that increase right-sided afterload, such as pulmonic stenosis. Aortic stenosis primarily affects the left side of the heart, leading to left ventricular hypertrophy. The ECG would reflect an increased mass of the left ventricle rather than the right.
Test-taking strategy:
- Identify the defect type: Recognize aortic stenosis as an obstructive lesion on the left side of the heart.
- Match sound to pathology: In any "stenosis" question, a murmur is almost always the initial and most frequent finding due to the physics of fluid moving through a narrow gap.
- Rule out limb discrepancies: Immediately associate "blood pressure discrepancies" with coarctation, not stenosis.
- Link anatomy to ECG: Remember that aortic equals left ventricle; therefore, right-sided hypertrophy is anatomically incorrect for this diagnosis.
- Assess for acuity: While rales can happen, they represent failure, whereas a murmur represents the structural defect present from birth.
Take home points
- A harsh systolic ejection murmur is the classic physical finding for aortic stenosis.
- Infants with critical stenosis may present with decreased peripheral pulses and grayish skin color.
- Chest pain and exercise intolerance are more common findings in older children than in neonates.
- The definitive diagnosis is typically made via echocardiography to measure the pressure gradient across the valve.
A nurse is caring for a 16-year-old client with aortic stenosis. Which finding is associated with aortic stenosis when the child is active?
Explanation
Aortic stenosis is a congenital obstructive left-sided heart defect characterized by the narrowing of the aortic valve. This structural anomaly restricts the ejection of blood from the left ventricle into the systemic circulation, creating a significant pressure gradient. During periods of high metabolic demand, the heart must work harder to overcome this resistance. The resulting mismatch between myocardial oxygen supply and demand leads to ischemia. Severe cases can result in syncope or sudden cardiac death during strenuous physical exertion.
Rationale for correct answer:
A. Chest pain or angina occurs during activity because the hypertrophied left ventricle requires more oxygen than the restricted coronary flow can provide. The narrowed valve limits the increase in cardiac output needed for exercise. This creates an ischemic environment within the myocardium. This is a critical warning sign in adolescents.
Rationale for incorrect answers:
B. Right ventricular failure is not typically associated with primary aortic stenosis. This defect places a direct pressure load on the left ventricle, causing left-sided hypertrophy. While chronic left-sided failure can eventually lead to pulmonary hypertension and right-sided involvement, it is not the primary active finding.
C. Increased cardiac output is what the body attempts to achieve during activity, but aortic stenosis prevents this from happening. The mechanical obstruction acts as a fixed output barrier regardless of the heart rate. Consequently, the child may experience fatigue or fainting rather than an effective increase in circulation.
D. While a loud systolic murmur is present, it is described as an ejection murmur rather than a regurgitant one. A regurgitant murmur is characteristic of valvular insufficiency, such as mitral or aortic regurgitation. A thrill may be palpable, but the timing and type of murmur in the choice are technically incorrect.
Test-taking strategy:
- Connect symptoms to demand: Recognize that "activity" increases the heart's need for oxygen. If there is an "obstruction," the supply cannot meet that demand.
- Identify the primary chamber: Aortic equals left ventricle. Therefore, any choice involving the right side is anatomically secondary and less likely to be the correct answer.
- Differentiate murmur types: Memorize that stenosis causes ejection murmurs (pushing through a narrow gap), while regurgitation causes backflow murmurs (leaking through a loose gap).
- Assess for emergencies: In adolescent cardiology, chest pain and syncope are the most dangerous and prioritized symptoms of aortic stenosis.
- Understand "Fixed Output": Recognize that obstructive lesions limit the heart's ability to increase output, which is why symptoms appear during exercise.
Take home points
- Exercise-induced chest pain in aortic stenosis is a sign of critical myocardial ischemia.
- Sudden death can occur during vigorous sports due to decreased coronary perfusion and arrhythmias.
- Adolescents with moderate to severe stenosis are often restricted from competitive or isometric sports.
- Dizziness and fainting during activity are additional indicators of an inadequate cardiac output response.
A nurse is teaching the parents of a child with congenital aortic stenosis. Which statement should the nurse include in her teaching about this disorder?
Explanation
Aortic stenosis is a mechanical obstruction of the left ventricular outflow tract that can be congenital or acquired. The pathology involves a narrowing of the aortic valve orifice, which significantly increases the workload of the left ventricle to maintain systemic circulation. Chronic pressure overload leads to concentric hypertrophy of the myocardium. In the pediatric population, it most frequently occurs as a bicuspid aortic valve, though secondary causes related to inflammatory processes are clinically significant.
Rationale for correct answer:
A. While often congenital, aortic stenosis can be an acquired condition resulting from rheumatic heart disease. This follows a poorly treated infection with Group A streptococci, leading to cross-reactivity and inflammation of the endocardium. The valve leaflets become scarred and fused, resulting in progressive stenosis.
Rationale for incorrect answers:
B. Aortic stenosis does not account for 25% of all congenital defects. It actually accounts for approximately 5% to 10% of congenital heart disease cases. Ventricular septal defects are the most common, making up about 25% to 30% of cardiac anomalies.
C. This condition causes a decrease in cardiac output, especially during periods of increased metabolic demand. The mechanical narrowing acts as a fixed resistance that prevents the heart from pumping more blood. Patients often experience fatigue because the heart cannot meet the body's systemic needs.
D. Aortic stenosis is classified as an acyanotic obstructive defect, not one with increased pulmonary blood flow. Defects with increased pulmonary flow involve shunting from left to right, such as an atrial septal defect. In stenosis, blood flow is impeded leaving the heart, which does not directly flood the lungs.
Test-taking strategy:
- Distinguish between classifications: Group defects into obstructive, increased pulmonary flow, decreased pulmonary flow, or mixed. Aortic stenosis is strictly obstructive.
- Verify epidemiological data: Remember that VSDs are the most common (approx. 25-30%), making choice 2 statistically incorrect for stenosis.
- Identify causal relationships: Recognize that rheumatic fever is a classic boards-tested cause for acquired valvular damage, including both stenosis and regurgitation.
- Apply hemodynamic logic: An obstruction by definition limits flow; therefore, an increased cardiac output is physiologically impossible in a stenotic environment.
- Evaluate shunt vs. block: Understand that increased pulmonary blood flow requires a hole (shunt) that isn't present in isolated aortic stenosis.
Take home points
- Aortic stenosis can be either a congenital structural defect or an acquired complication of rheumatic fever.
- The primary hemodynamic effect is a reduction in systemic cardiac output and increased left ventricular afterload.
- Clinical signs include a systolic ejection murmur and, in severe cases, exertional chest pain or syncope.
- Unlike septal defects, this is an obstructive lesion and does not typically result in pulmonary over-perfusion.
A nurse is caring for a client with aortic stenosis. Which instruction would be most appropriate for this client?
Explanation
Aortic stenosis is a congenital obstructive cardiac malformation involving the narrowing of the aortic valve orifice. This structural anomaly restricts the ejection of blood from the left ventricle into the systemic circulation, creating a significant pressure gradient. This mechanical barrier results in a relatively fixed cardiac output that cannot increase to meet elevated metabolic demands. Chronic exposure to this high afterload leads to compensatory concentric left ventricular hypertrophy and increased myocardial oxygen consumption.
Rationale for correct answer:
A. Restricting exercise is the most appropriate instruction to prevent sudden cardiac death and myocardial ischemia. Strenuous physical activity increases the demand for oxygenated blood that the obstructed valve cannot provide. This mismatch can trigger life-threatening ventricular arrhythmias or syncopal episodes. High-intensity competitive sports and isometric exercises are particularly hazardous for these patients.
Rationale for incorrect answers:
B. Avoiding prostaglandin E is not a standard instruction for all clients with this condition and may be incorrect for neonates. In cases of critical aortic stenosis in newborns, prostaglandin E1 is actually life-saving. It maintains the patency of the ductus arteriosus to ensure systemic perfusion via a right-to-left shunt. Restricting its use in that context would be fatal.
C. Avoiding digoxin and diuretics is generally not recommended as these medications are often essential for managing heart failure. Digoxin increases myocardial contractility, while diuretics reduce pulmonary venous congestion by decreasing preload. While they must be monitored for toxicity, they are standard components of the medical regimen for symptomatic obstructive defects.
D. Allowing the child to exercise freely is dangerous and potentially fatal in the presence of moderate to severe stenosis. The mechanical obstruction prevents the necessary rise in stroke volume during physical exertion. This leads to a drop in systemic blood pressure and coronary hypoperfusion. Free exercise increases the risk of exercise-induced syncope and sudden death.
Test-taking strategy:
- Identify the safety priority: In pediatric cardiology, sudden death is the greatest risk associated with obstructive left-sided lesions like aortic stenosis.
- Recognize the "Fixed Output" limitation: Understand that the narrowed valve acts as a bottleneck; the heart cannot pump more blood when the body asks for it during exercise.
- Match the intervention to the risk: Since exercise increases oxygen demand and the heart cannot supply it, the only logical preventative measure is to limit the demand by restricting activity.
- Rule out pharmacological absolutes: Avoid choices that suggest avoiding heart failure medications such as diuretics and digoxin unless there is a specific contraindication mentioned.
- Evaluate the neonate context: Remember that prostaglandin is a friend, not a foe, in ductal-dependent cardiac obstructions.
Take home points
- Exercise restriction is mandatory for children with moderate to severe aortic stenosis to prevent sudden cardiac collapse.
- Chest pain, dizziness, or fainting during activity are red-flag symptoms indicating critical obstruction.
- Monitoring for left ventricular hypertrophy via regular ECGs and echocardiograms is essential for tracking disease progression.
- Avoidance of dehydration is important to maintain adequate preload and prevent a precipitous drop in cardiac output.
A nurse is assessing a group of pediatric clients. During the assessment of a child with pulmonic stenosis, which finding is most common?
Explanation
Pulmonic stenosis is an obstructive heart defect where the pulmonary valve is narrowed, restricting blood flow from the right ventricle to the lungs. This creates significant turbulence as the heart forces blood through the constricted opening. The primary clinical manifestation of this turbulent flow is a distinct sound heard during the contraction phase of the heart.
Rationale for correct answer:
C. A systolic ejection murmur is the classic and most frequent finding in pulmonic stenosis. It is a harsh, medium-to-high pitched sound heard best at the upper left sternal border, the pulmonic area. This sound occurs specifically during systole as the right ventricle pumps blood past the obstruction.
Rationale for incorrect answers:
A. Hyperactivity is not a characteristic finding. In fact, if the stenosis is severe, children are more likely to exhibit exercise intolerance or fatigue because they cannot efficiently oxygenate enough blood to meet high metabolic demands.
B. A normal respiratory rate is unlikely in symptomatic cases. Children with significant pulmonic stenosis often have dyspnea or tachypnea during activity because the heart cannot pump enough blood to the lungs to keep up with the body's oxygen needs.
D. Capillary refill of more than 2 seconds signifies delayed refill and is a sign of poor systemic perfusion or shock. While severe pulmonic stenosis can eventually lead to right-sided heart failure and decreased cardiac output, it is not the most common or initial finding compared to the nearly universal presence of a murmur.
Test-taking strategy:
- The "stenosis = murmur" rule: In almost every pediatric nursing question, if the defect name ends in "stenosis," look for "murmur" in the answer choices. Narrowing always creates turbulence.
- Location matters: Remember that pulmonic issues are heard on the left side of the chest (2nd intercostal space), while aortic issues are heard on the right.
- Physiology of obstruction: Think of the path of blood. If the "exit" to the lungs is blocked, the symptoms will be related to low oxygenation (fatigue) and heart sounds (murmurs), not behavioral changes like hyperactivity.
Take home points
- Pulmonic stenosis causes right ventricular hypertrophy as the heart muscle thickens to push against the resistance.
- In newborns, if the stenosis is "critical," they may appear cyanotic because blood cannot reach the lungs effectively.
- Treatment often involves a balloon valvuloplasty, where a catheter is used to stretch the narrowed valve open.
A nurse is caring for a child with pulmonic stenosis. Which finding is seen during cardiac catheterization of this client?
Explanation
Pulmonic stenosis is a congenital obstructive defect involving the narrowing of the pulmonary valve. This mechanical barrier forces the right ventricle to generate extremely high pressures to eject blood into the pulmonary artery. In many cases, this elevated pressure on the right side of the heart exceeds the pressure on the left.
Rationale for correct answer:
A. During cardiac catheterization of a child with significant pulmonic stenosis, right-to-left shunting is a common finding. Because the stenotic valve creates a "backlog" of pressure in the right atrium and ventricle, deoxygenated blood is pushed through any existing septal openings, like a patent foramen ovale, into the left side of the heart. This is why children with severe pulmonic stenosis may present with cyanosis.
Rationale for incorrect answers:
B. Left-to-right shunting is typical of defects like VSD or ASD where there is no outflow obstruction. In those cases, blood flows from the high-pressure left side to the low-pressure right side. In pulmonic stenosis, the right-sided pressures are often too high to allow this flow pattern.
C. Decreased pressure in the right side of the heart is the opposite of what occurs. Pulmonic stenosis causes increased pressures in the right ventricle as it struggles to overcome the valvular obstruction.
D. Increased oxygenation in the left side of the heart is not possible in this scenario. If anything, oxygenation on the left side decreases because deoxygenated blood is shunting over from the right side, diluting the saturated blood.
Test-taking strategy
- Follow the Pressure: In cardiac questions, blood always flows from high pressure to low pressure. Since stenosis creates high pressure on the right, the shunt must move toward the left.
- Identify the "Obstruction" Effect: Any time a valve is stenosed, the chamber behind that valve (the right ventricle) will have increased pressure. This helps you immediately eliminate choice C.
- Think cyanosis: Pulmonic stenosis is one of the few acyanotic defects that can become cyanotic. Cyanosis is caused by right-to-left shunting.
Take home points
- Pulmonic stenosis increases right ventricular afterload.
- The pressure gradient created can reopen a patent foramen ovale, leading to shunting.
- Cardiac catheterization is used to measure the exact pressure gradient across the valve to determine if surgery or balloon valvuloplasty is needed.
A nurse is reviewing diagnostic results for a client with suspected pulmonary stenosis. Which findings support the diagnosis? Select all that apply
Explanation
Pulmonary stenosis is a valvular obstruction characterized by the narrowing of the outflow tract between the right ventricle and the pulmonary artery. This mechanical resistance necessitates an increase in ventricular pressure to eject blood into the pulmonary circulation. Chronic pressure overload leads to compensatory myocardial thickening and can eventually manifest as right-sided heart failure if the obstruction is not relieved surgically or via balloon valvuloplasty.
Rationale for correct answers:
A. Increased resistance to blood flow forces the right ventricle to contract with greater force against a fixed afterload. Over time, the cardiac muscle fibers undergo pathologic remodeling, resulting in right ventricular hypertrophy. This thickening is clearly visualized during an echocardiogram, providing evidence of the chronic workload placed on the right side of the heart by the stenotic valve.
B. Turbulent blood flow across a narrowed or malformed pulmonary valve creates a characteristic systolic murmur. This sound is typically heard best at the left upper sternal border, often accompanied by a palpable thrill in severe cases. The timing and anatomical location of the murmur are classic clinical markers used to differentiate pulmonary stenosis from other congenital cardiac defects.
D. The primary anatomical defect in this condition is the physical narrowing of the pulmonary valve leaflets or the subvalvular region. This restriction limits the volume of blood that can reach the pulmonary arteries for oxygenation. Identifying this structural abnormality through imaging or cardiac catheterization is the definitive requirement for confirming a diagnosis of pulmonary stenosis.
Rationale for incorrect answers:
C. In pulmonary stenosis, there is typically a decrease in blood flow reaching the lungs, leading to decreased pulmonary vascular markings. Chest x-rays often show a "clear" lung field because the obstruction prevents adequate blood volume from entering the pulmonary circuit. Increased markings are more indicative of left-to-right shunts, such as a ventricular septal defect, which cause pulmonary overcirculation.
E. Pulmonary stenosis specifically impacts the right side of the heart, therefore, left ventricular pressures generally remain within normal limits. The pathology is isolated to the right ventricle and the pulmonary valve, whereas elevated left-sided pressure would suggest systemic hypertension or aortic valve disease. Measurement of intracardiac pressures during catheterization would show high right ventricular pressure but normal left-sided hemodynamics.
Test-taking strategy:
- Identify the anatomical location of the defect: Pulmonary stenosis affects the right heart and the path to the lungs; therefore, symptoms will be right-sided.
- Apply the pressure-flow principle: Obstruction (stenosis) leads to high pressure behind the block that is the right ventricle and low flow ahead of the block in the lungs.
- Differentiate between murmur locations: A murmur at the left upper sternal border is typical for pulmonary issues, whereas the right upper sternal border is typical for aortic issues.
- Rule out left-sided findings: If the question specifies a right-sided valve (pulmonary), eliminate any choices mentioning the left ventricle or systemic circulation.
- Evaluate radiographic findings: Connect "stenosis" (narrowing) with "decreased" lung markings due to the physical limitation of blood reaching the pulmonary tissue.
Take home points
- Pulmonary stenosis results in a systolic ejection murmur often preceded by a "click" as the stiff valve opens.
- Right ventricular hypertrophy is a compensatory response to the high afterload created by the narrowed valve.
- Radiographic findings typically include a prominent main pulmonary artery segment due to post-stenotic dilation despite decreased lung markings.
- Severe cases may present with cyanosis in neonates if a right-to-left shunt develops through a patent foramen ovale.
A nurse is working with a family with a child who has a congenital heart defect. Future surgery is planned, and the nurse is teaching the parent how to reduce cardiac demands. The parent needs more teaching when she says which of the following?
Explanation
Congenital heart defects often result in increased metabolic demands due to inefficient oxygen delivery and compensatory cardiac hypertrophy. Management focuses on optimizing cardiac output while minimizing the workload of the myocardium to prevent congestive heart failure. Nursing interventions emphasize structured rest periods and nutritional support that does not exhaust the infant's limited energy reserves.
Rationale for correct answer:
A. Frequent awakenings for feedings significantly increase energy expenditure and prevent necessary restorative sleep cycles. Infants with cardiac defects require uninterrupted rest to decrease myocardial oxygen consumption. Feedings should be provided on a demand schedule or every 3 to 4 hours, utilizing high-calorie density formulas to maximize intake while minimizing the physical effort of sucking.
Rationale for incorrect answers:
B. Digoxin administration requires strict adherence to safety protocols due to its narrow therapeutic index and potential for toxicity. Auscultating the apical pulse for 1 full minute ensures the nurse or parent identifies bradycardia or arrhythmias before dosing. This practice is essential to prevent administering the medication when the heart rate is below the age-specific threshold, usually 90 to 110 beats per minute in infants.
C. Children with structural heart defects are at high risk for cardiovascular collapse if they contract respiratory syncytial virus or other infections. Respiratory illnesses increase pulmonary vascular resistance and oxygen demand, which a compromised heart cannot meet. Protecting the child from ill contacts is a standard preventive measure to avoid complications like pneumonia or infective endocarditis.
D. Monitoring urine output via diaper counts is a critical non-invasive method to assess fluid balance and renal perfusion. Excessive weight gain or decreased wet diapers can indicate fluid retention, a hallmark sign of worsening heart failure. Conversely, adequate output suggests that the heart is effectively circulating blood to the kidneys and that diuretic therapy, if prescribed, is functioning appropriately.
Test-taking strategy:
- Identify the negative polarity of the question; "needs more teaching" means you must select the incorrect or unsafe parental statement.
- Apply the rest vs. effort principle for cardiac patients: In a child with limited cardiac reserve, any activity, including feeding or waking, must be balanced against the need for metabolic rest.
- Evaluate the digoxin protocol: Safety standards for pediatric digoxin always include a full minute of apical pulse monitoring to ensure clinical accuracy.
- Use infection control priorities: For patients with compromised physiology, preventing secondary stressors like respiratory infections is always a correct and necessary action.
- Utilize fluid assessment basics: Diaper counts are the primary way parents track output; recognizing this as a correct action allows you to rule it out as the answer.
Take home points
- Feedings should be limited to 20 or 30 minutes to prevent exhaustion and excessive caloric expenditure during the act of feeding.
- Maximizing rest is the primary strategy for reducing cardiac workload in pediatric patients with congenital defects.
- Digoxin toxicity in children often presents as vomiting, poor feeding, or bradycardia, necessitating careful pulse checks.
- Daily weights and monitoring the number of wet diapers provide the most accurate home assessment of a child's fluid status.
A nurse is evaluating an infant with pulmonary stenosis. Which finding is expected during the assessment of this client?
Explanation
Pulmonary stenosis involves a narrowing of the pulmonary valve or outflow tract, obstructing blood flow from the right ventricle into the pulmonary artery. This mechanical obstruction increases afterload on the right side of the heart, eventually leading to right ventricular hypertrophy. When the right ventricle can no longer compensate for the pressure gradient, right-sided heart failure occurs, resulting in systemic venous congestion and visceral engorgement.
Rationale for correct answer:
C. Right-sided heart failure causes blood to back up into the systemic circulation, leading to venous hypertension. The liver becomes enlarged and palpable below the costal margin due to passive congestion of the hepatic sinusoids. In infants, this hepatomegaly is a primary clinical indicator that the right heart is failing to pump effectively against the stenotic valve.
Rationale for incorrect answers:
A. Infants with significant congenital heart defects typically present as underweight rather than overweight. The increased metabolic work of breathing and the high energy required for the heart to pump against obstruction lead to failure to thrive. Caloric intake often cannot keep pace with the massive energy expenditure required for basic physiological maintenance.
B. Tachycardia, not bradycardia, is the expected compensatory response to decreased cardiac output. The sympathetic nervous system is activated to maintain systemic perfusion, leading to an increased heart rate. Bradycardia is usually a late, pre-arrest sign of hypoxia or exhaustion in an infant rather than a standard finding of pulmonary stenosis.
D. An infant with pulmonary stenosis is likely to exhibit an increased respiratory rate to compensate for inadequate pulmonary blood flow. Tachypnea occurs as the body attempts to improve gas exchange and manage the hypoxemia resulting from restricted blood delivery to the lungs. A decreased respiratory rate would be atypical and indicative of neurological depression or impending respiratory failure.
Test-taking strategy
- Distinguish between left-sided and right-sided heart failure symptoms. Right-sided failure involves systemic backup such as edema, and hepatomegaly, while left-sided involves pulmonary backup such as crackles and dyspnea.
- Apply the hemodynamic flow principle: If the "door" to the lungs (pulmonary valve) is narrow, pressure builds up behind it in the right ventricle, right atrium, and eventually the liver.
- Evaluate the infant metabolic profile: Most congenital heart defects lead to high-energy states; therefore, "overweight" or "slow heart rate" are rarely correct answers in this population.
- Use physiological compensation logic: The body rarely slows down (bradycardia/low respiratory rate) when faced with an obstruction; it speeds up to try and maintain homeostasis.
- Recognize organ-specific signs: In pediatrics, the liver is a very sensitive indicator of fluid volume status and central venous pressure.
Take home points
- Pulmonary stenosis causes a systolic ejection murmur best heard at the upper left sternal border.
- Severe stenosis leads to right ventricular hypertrophy as the muscle thickens to overcome high valvular resistance.
- Clinical manifestations range from asymptomatic in mild cases to cyanosis and heart failure in critical neonatal stenosis.
- Prostaglandin E1 may be administered in critical cases to maintain ductal patency and ensure adequate pulmonary blood flow.
Exams on Congenital heart diseases: Obstructive disorders
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
- Classify obstructive congenital heart diseases based on hemodynamic patterns, specifically identifying defects that impede blood flow exiting the heart.
- Describe the anatomical differences between coarctation of the aorta, aortic stenosis, and pulmonic stenosis and their respective effects on ventricular workload.
- Identify the clinical hallmark of coarctation of the aorta, specifically the disparity in blood pressure and pulse strength between upper and lower extremities.
- Explain the pathophysiology of critical left-sided obstructions and the vital role of the patent ductus arteriosus (PDA) in maintaining systemic perfusion until surgical intervention.
- Interpret diagnostic findings, such as echocardiograms and chest X-rays, specific to obstructive lesions.
- Outline the primary therapeutic interventions, including balloon angioplasty, valvuloplasty, and surgical resection/anastomosis.
- Develop a nursing care plan for pediatric patients with obstructive defects.
- Recognize potential complications following surgical or interventional repairs, such as recoarctation, rebound hypertension, or restenosis.
Introduction
- Obstructive congenital heart disorders (CHDs) comprise a category of structural defects where blood flow exiting the heart is physically impeded.
- Unlike defects that cause shunting, these anomalies involve a narrowing or constriction of the heart valves or the great vessels.
- This obstruction creates a significant pressure gradient: the heart chamber behind the blockage must generate abnormally high pressures to force blood through the narrowed opening, while the areas beyond the obstruction receive diminished flow.
- The primary pathophysiological hallmark of obstructive lesions, such as coarctation of the aorta, aortic stenosis, and pulmonic stenosis, is an increased "afterload" on the myocardium.
- The clinical manifestation of these disorders depends heavily on the severity of the narrowing.
- In cases of pulmonic stenosis, patients may exhibit cyanosis due to decreased pulmonary perfusion. In contrast, left-sided obstructions like coarctation of the aorta present a unique diagnostic profile.
- A critical nursing assessment involves comparing the upper and lower extremities; nurses will often find hypertension and bounding pulses in the arms, contrasted with hypotension, weak or absent femoral pulses, and cool skin in the lower body.
- In neonates with "critical" obstructive lesions, systemic perfusion may depend entirely on the patent ductus arteriosus (PDA). When the ductus begins to close shortly after birth, these infants can rapidly spiral into cardiogenic shock.
- The nurse’s role is vital in the early identification of decreased cardiac output and the management of life-saving infusions, such as Prostaglandin E1, to maintain ductal patency until surgical or balloon intervention can be performed.
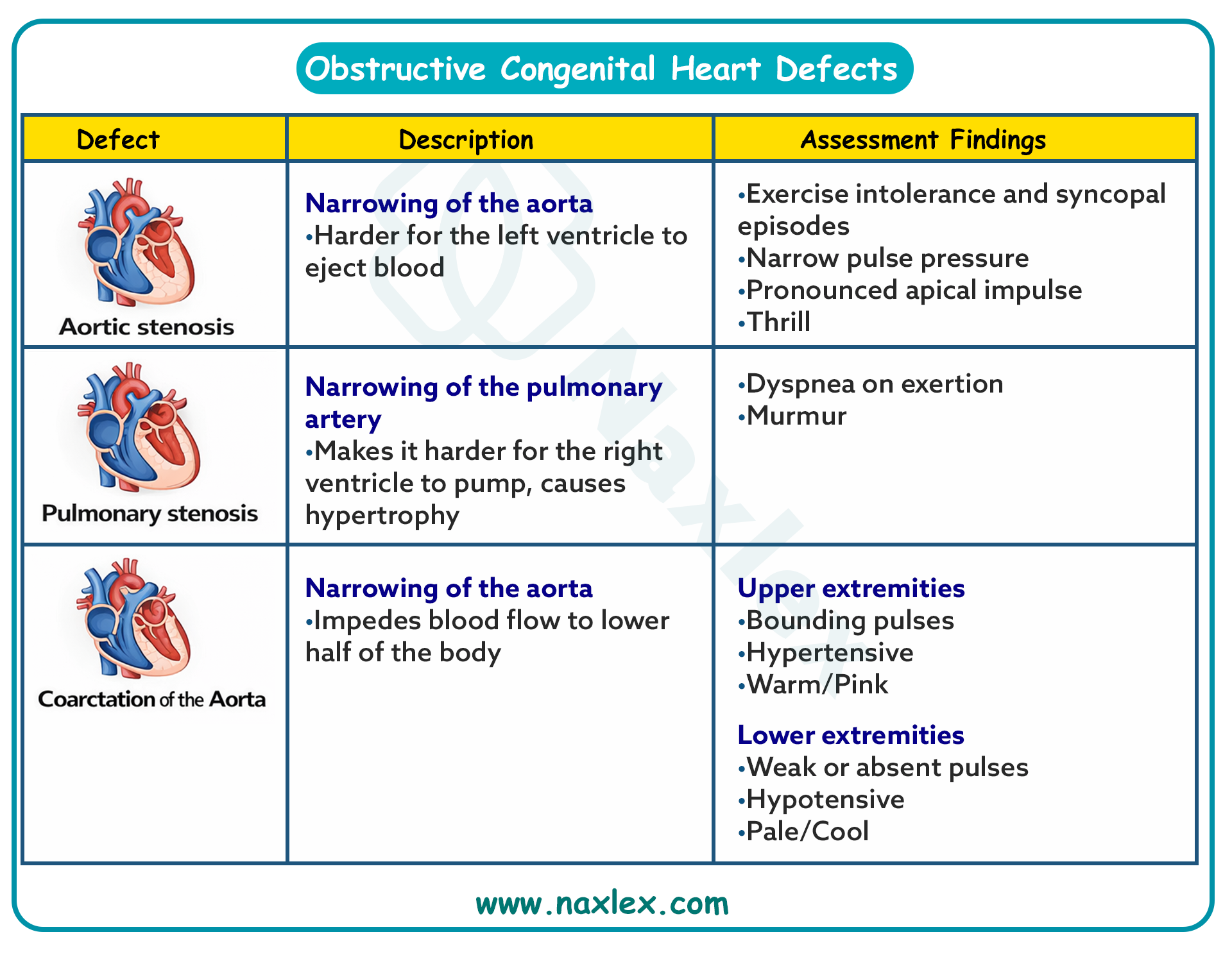
Coarctation of the aorta
Definition
- Coarctation of the aorta (CoA) is a localized narrowing of the aortic lumen, typically occurring in the area of the ductus arteriosus (juxtaductal). This obstructive defect results in increased pressure proximal to the stenosis (upper body) and decreased pressure distal to the stenosis (lower body).
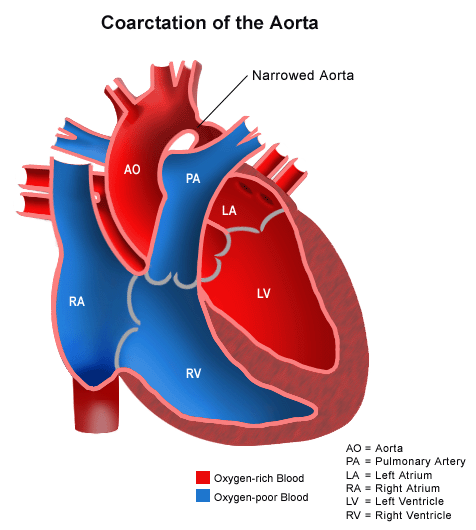
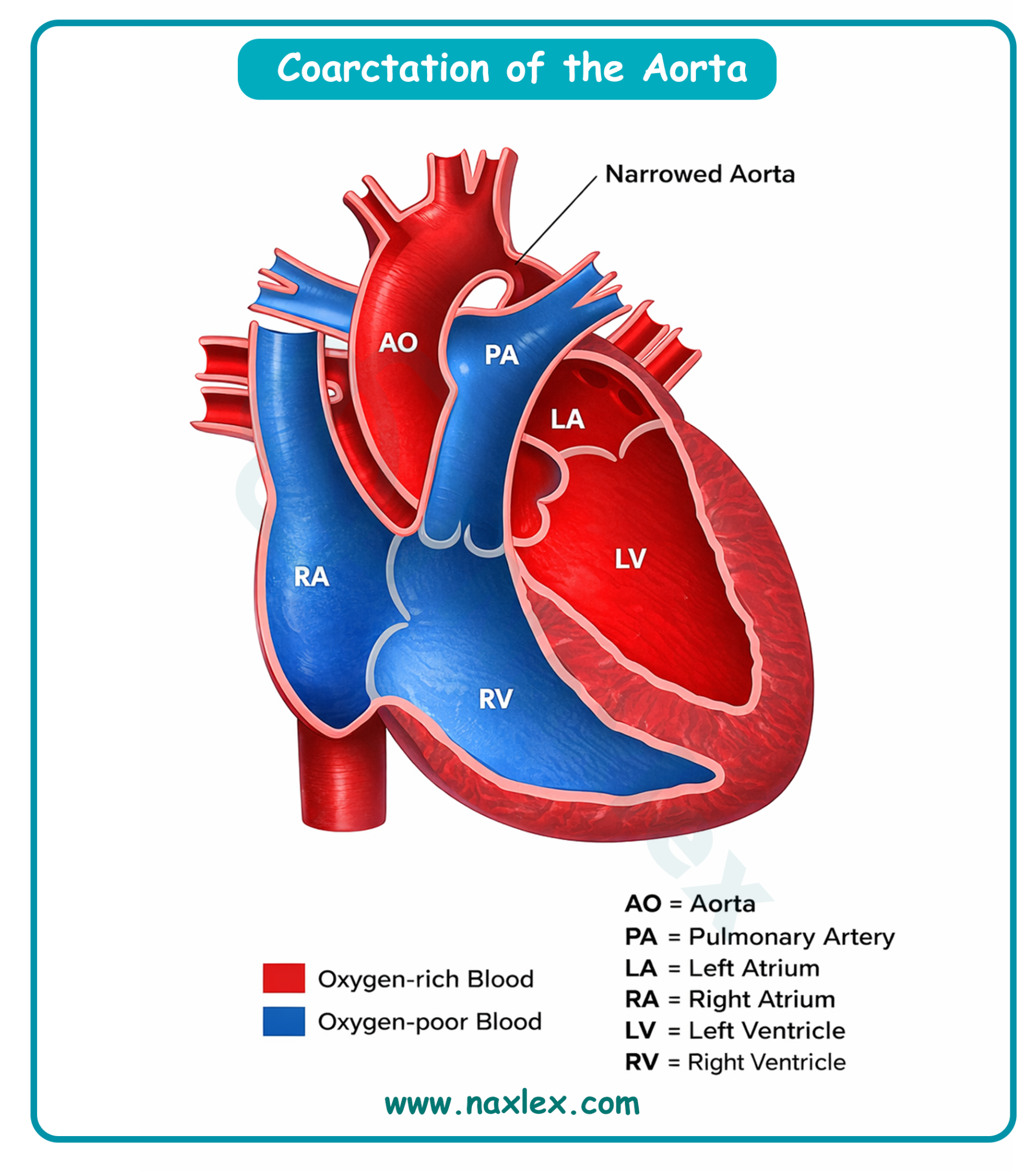
Epidemiology
- CoA accounts for 6% to 8% of all congenital heart defects.
- It occurs in approximately 4 per 10,000 live births.
- There is a significant male predominance, with a ratio of 2:1.
- It is frequently associated with Turner syndrome, occurring in 15% to 20% of affected females.
Etiology
- Congenital: The most common cause is the "Ductal Tissue Theory," where ectopic ductal tissue migrates into the aortic wall; as the ductus closes after birth, the tissue contracts, narrowing the aorta. It is often associated with bicuspid aortic valve (up to 85% of cases) and ventricular septal defects.
- Acquired: Rare in pediatrics. Can result from inflammatory vasculitis (e.g., Takayasu arteritis) or following trauma/surgical scarring of the aorta.
Pathophysiology
- Obstructed Flow: The narrowing creates a mechanical obstruction to blood flow leaving the left ventricle.
- Pressure Gradient: This creates hypertension in the vessels of the head and arms (pre-ductal) and hypotension in the lower extremities and abdominal viscera (post-ductal).
- Left Ventricular Afterload: The left ventricle must work harder to pump against the high resistance, leading to left ventricular hypertrophy (LVH).
- Collateral Circulation: In older children, the body develops collateral vessels (intercostal, internal mammary, and scapular arteries) to bypass the obstruction and supply the lower body.
Image Title: Pathophysiology of Coarctation of the Aorta (CoA)
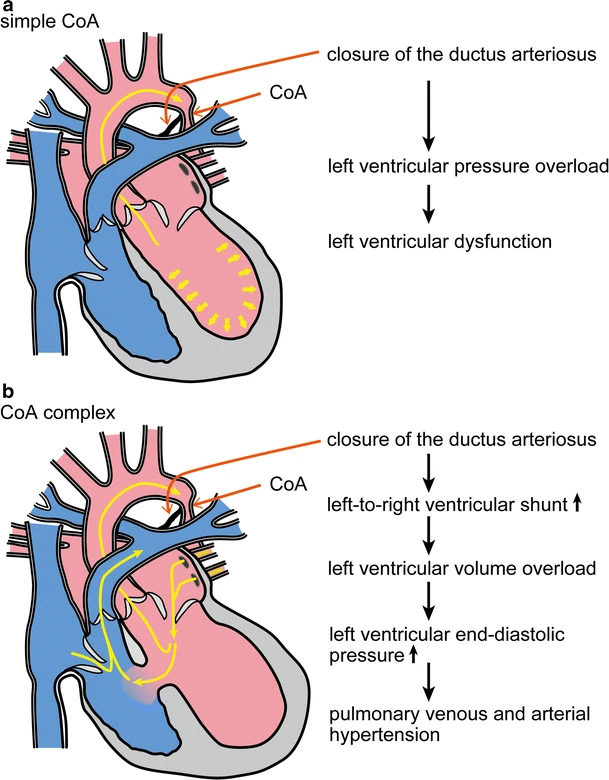
Clinical Manifestations
- Neonates (Critical Coarctation)
- Symptoms often appear as the ductus arteriosus closes.
- Sudden onset of congestive heart failure (CHF) and cardiogenic shock.
- Pale skin, irritability, heavy sweating, and dyspnea.
- Weak or absent femoral pulses compared to strong brachial/radial pulses.
- Severe metabolic acidosis and oliguria.
- Older Infants and Children (Non-Critical)
- Often asymptomatic initially, discovered during routine physical exams.
- Leg aches or cramps (claudication) during exercise.
- Frequent headaches, nosebleeds (epistaxis), or dizziness.
- Discrepancy in blood pressure and pulse quality between upper and lower extremities.
- Cardiac Auscultation Features
- S2: Usually single and loud.
- Murmur: A systolic ejection murmur, best heard at the left infraclavicular area and in the left interscapular area (back).
- Click: An apical systolic ejection click may be heard if a bicuspid aortic valve is also present.
Diagnostic Evaluation
- Blood Pressure (BP) Measurements: The hallmark is a systolic BP difference of > 20 mmHg between the upper and lower extremities (upper > lower).
- Pulse Oximetry: May show differential cyanosis if a PDA is present, where the lower body has lower oxygen saturation than the upper body.
- Echocardiogram (ECHO): Confirms the site of narrowing, measures the pressure gradient across the coarctation, and assesses LV function.
- Electrocardiogram (ECG): In neonates, shows Right Ventricular Hypertrophy (RVH); in older children, shows Left Ventricular Hypertrophy (LVH).
- Chest X-Ray (CXR): May show cardiomegaly. In older children, "notching of the ribs" (3rd to 8th ribs) is seen due to erosion by dilated collateral intercostal arteries. The "3 sign" may be visible on the aorta.
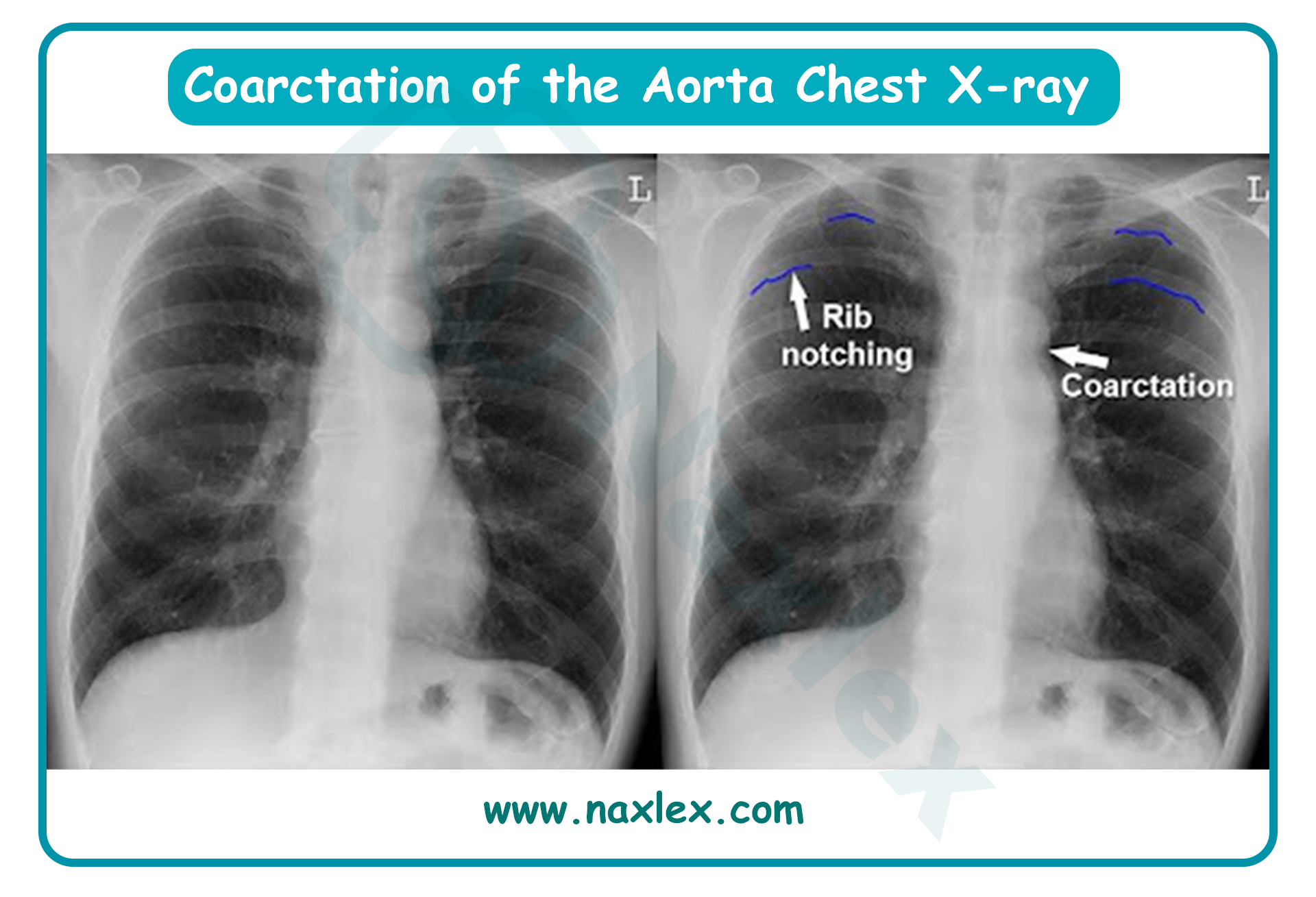
Therapeutic Management
- Management for Neonates with Critical Coarctation
- Prostaglandin E1 (Alprostadil) Infusion: Crucial to maintain patency of the ductus arteriosus (PDA) to provide blood flow to the lower body distal to the coarctation.
- Stabilization: Intubation and mechanical ventilation to reduce myocardial oxygen demand.
- Correction of Acidosis: Administration of sodium bicarbonate and fluid resuscitation.
- Management for Non-Critical Coarctation
- Elective surgical repair or balloon angioplasty usually performed between 2 and 5 years of age.
- Medical Management
- Inotropic Support: Dopamine or Dobutamine for neonates in shock.
- Diuretics: Furosemide to manage pulmonary congestion.
- Antihypertensives: Beta-blockers or ACE inhibitors (e.g., Captopril) used pre-operatively and sometimes post-operatively to control rebound hypertension.
- Surgical Management
- Resection with End-to-End Anastomosis: The narrowed segment is removed and the two healthy ends of the aorta are sewn together.
- Subclavian Flap Aortoplasty: Uses the left subclavian artery as a flap to widen the narrowed aortic area.
Image Title: Coarctation of Aorta Surgical Management
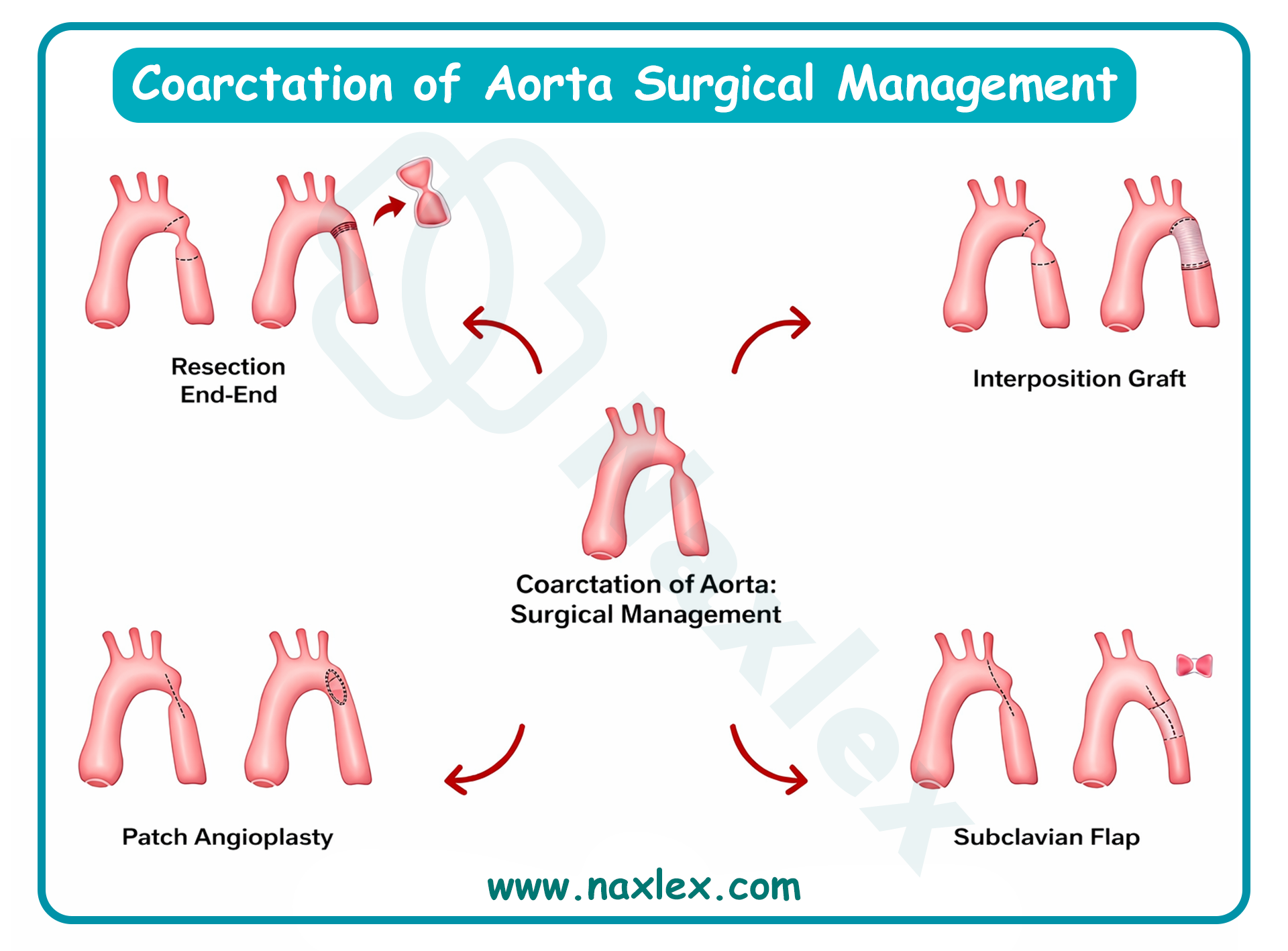
- Balloon Angioplasty / Stenting: Often the primary choice for recoarctation or in older children.
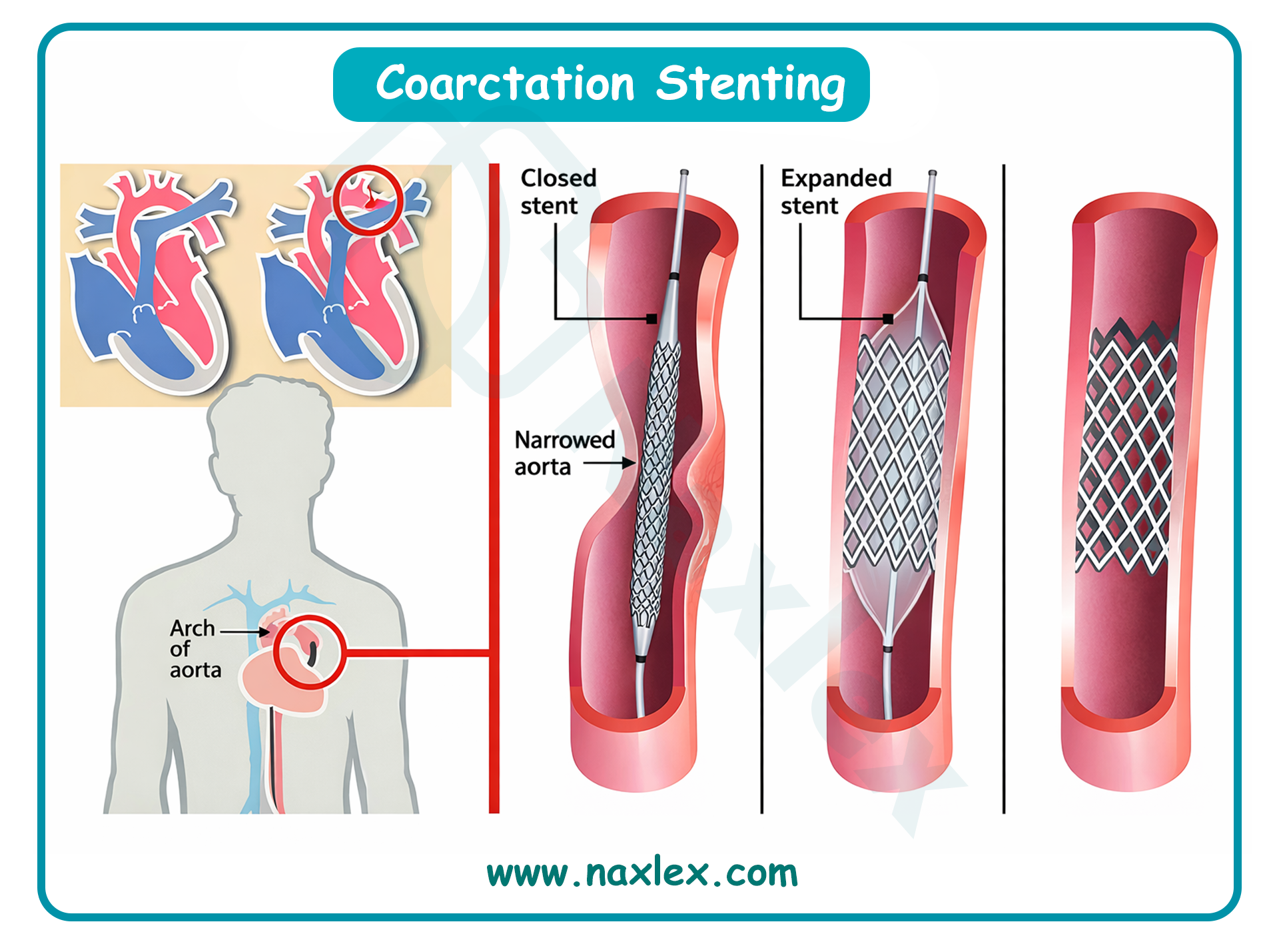
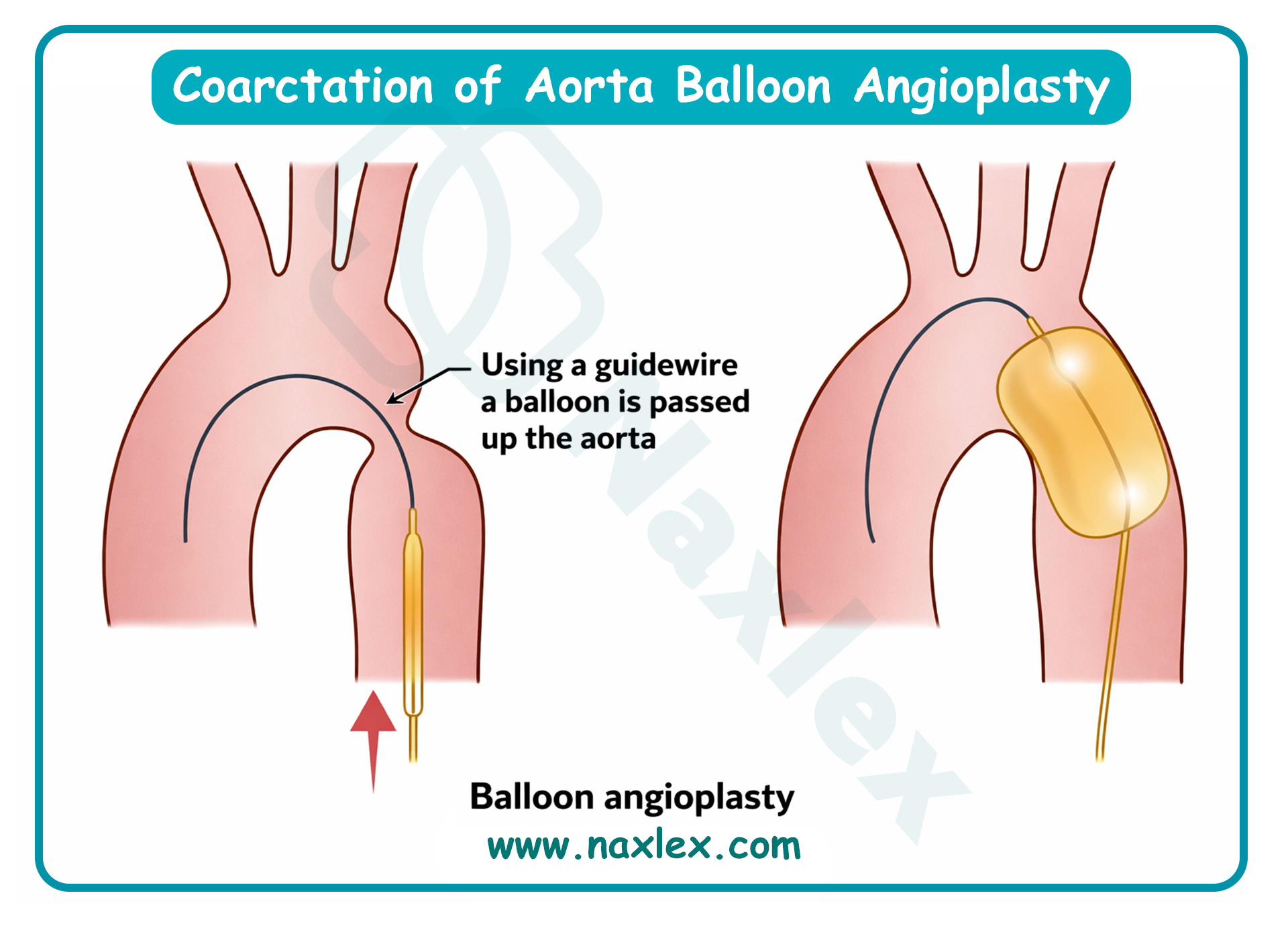
Post-Operative Nursing Interventions
- Post-Op Day 1 to 2:
- BP Monitoring: Use of an arterial line (usually right radial) for continuous monitoring. Monitor for "Paradoxical Hypertension" (rebound hypertension) which can cause suture line stress.
- Neurovascular Checks: Assess all 4 extremities for pulse strength, temperature, and capillary refill hourly.
- Pain Management: Continuous IV opioid infusion (Fentanyl or Morphine).
- Chest Tube: Monitor for chylothorax (milky drainage) if the thoracic duct was injured during surgery.
- Post-Op Day 3 to 5:
- Abdominal Assessment: Monitor for "Post-coarctectomy Syndrome" (mesenteric arteritis). Assess for abdominal pain, distension, and ileus caused by sudden increased perfusion to the gut.
- Activity: Gradual increase in ambulation; keep the head of the bed elevated.
- Wound Care: Monitor thoracotomy site for signs of infection.
Nursing Diagnosis (Post-Op)
- Post-Op Day 1 to 2:
- Risk for Ineffective Peripheral Tissue Perfusion related to surgical manipulation of the aorta and potential thrombus.
- Decreased Cardiac Output related to afterload changes and myocardial depression from bypass.
- Acute Pain related to thoracotomy and chest tube placement.
- Post-Op Day 3 to Discharge:
- Risk for Ineffective Gastrointestinal Tissue Perfusion related to mesenteric arteritis secondary to increased systemic pressure.
- Deficient Knowledge (Caregiver) related to long-term antihypertensive medication and activity restrictions.
- Risk for Infection related to surgical incision and invasive lines.
Complications
- Recurrent Coarctation: Occurs in up to 10% of infants repaired early.
- Post-Coarctectomy Syndrome: Mesenteric inflammation due to sudden changes in blood flow; can lead to bowel infarction if not managed.
- Paradoxical Hypertension: Extreme hypertension in the immediate post-operative period requiring IV nitroprusside or esmolol.
- Permanent Spinal Cord Ischemia: Rare; due to interruption of blood supply during aortic clamping.
Prognosis
- Generally excellent survival rate (> 98%).
- Life-long follow-up is mandatory as systemic hypertension can persist or develop years after a successful repair.
- Increased risk for premature coronary artery disease and cerebral aneurysms later in life.
Aortic valve stenosis
Definition
- Coarctation of the aorta (CoA) is a localized narrowing of the aortic lumen, typically occurring in the area of the ductus arteriosus (juxtaductal). This obstructive defect results in increased pressure proximal to the stenosis (upper body) and decreased pressure distal to the stenosis (lower body).
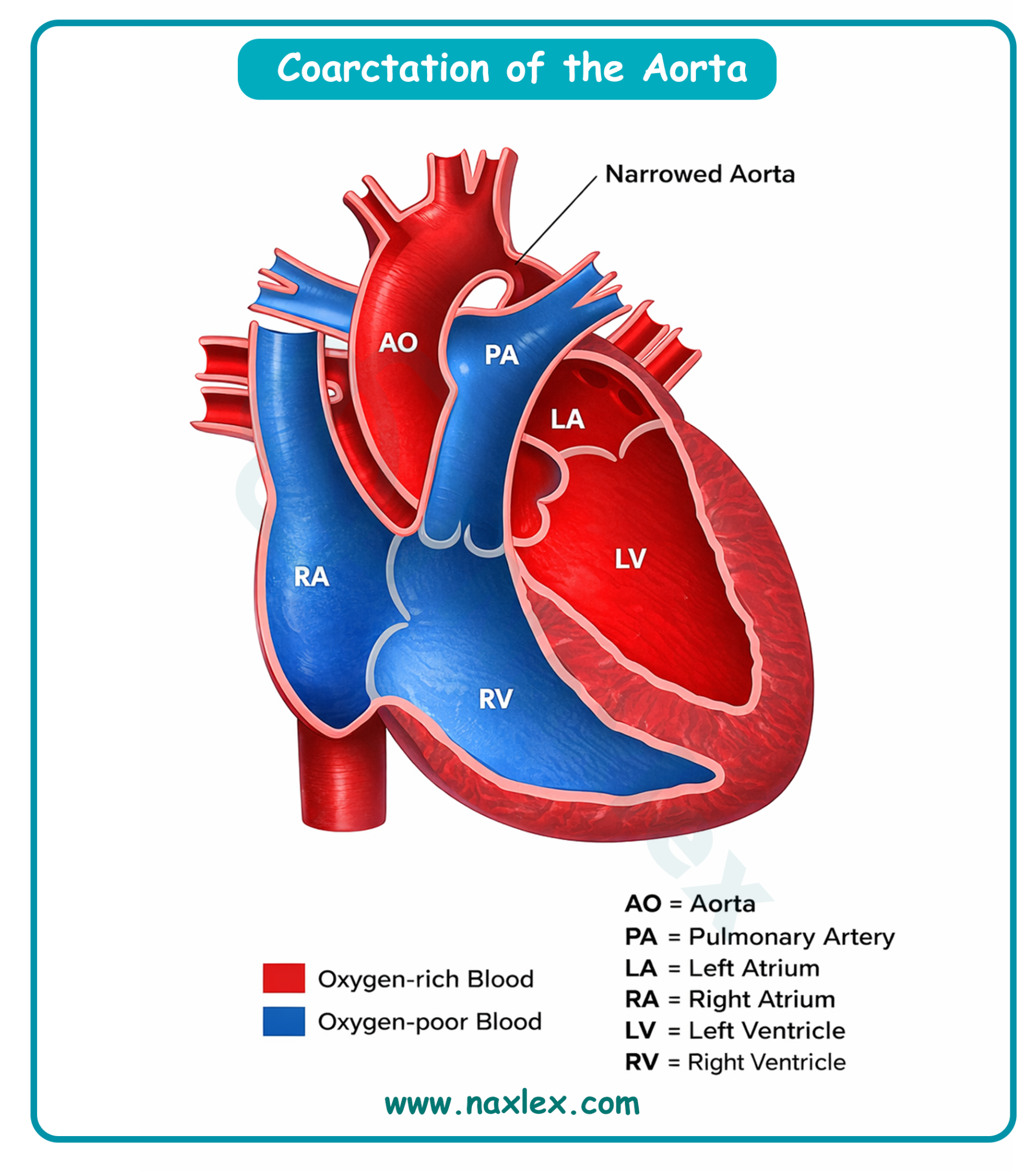
Epidemiology
- CoA accounts for 6% to 8% of all congenital heart defects.
- It occurs in approximately 4 per 10,000 live births.
- There is a significant male predominance, with a ratio of 2:1.
- It is frequently associated with Turner syndrome, occurring in 15% to 20% of affected females.
Etiology
- Congenital: The most common cause is the "Ductal Tissue Theory," where ectopic ductal tissue migrates into the aortic wall; as the ductus closes after birth, the tissue contracts, narrowing the aorta. It is often associated with bicuspid aortic valve (up to 85% of cases) and ventricular septal defects.
- Acquired: Rare in pediatrics. Can result from inflammatory vasculitis (e.g., Takayasu arteritis) or following trauma/surgical scarring of the aorta.
Pathophysiology
- Obstructed Flow: The narrowing creates a mechanical obstruction to blood flow leaving the left ventricle.
- Pressure Gradient: This creates hypertension in the vessels of the head and arms (pre-ductal) and hypotension in the lower extremities and abdominal viscera (post-ductal).
- Left Ventricular Afterload: The left ventricle must work harder to pump against the high resistance, leading to left ventricular hypertrophy (LVH).
- Collateral Circulation: In older children, the body develops collateral vessels (intercostal, internal mammary, and scapular arteries) to bypass the obstruction and supply the lower body.
Clinical Manifestations
- Neonates (Critical Coarctation)
- Symptoms often appear as the ductus arteriosus closes.
- Sudden onset of congestive heart failure (CHF) and cardiogenic shock.
- Pale skin, irritability, heavy sweating, and dyspnea.
- Weak or absent femoral pulses compared to strong brachial/radial pulses.
- Severe metabolic acidosis and oliguria.
- Older Infants and Children (Non-Critical)
- Often asymptomatic initially, discovered during routine physical exams.
- Leg aches or cramps (claudication) during exercise.
- Frequent headaches, nosebleeds (epistaxis), or dizziness.
- Discrepancy in blood pressure and pulse quality between upper and lower extremities.
- Cardiac Auscultation Features
- S2: Usually single and loud.
- Murmur: A systolic ejection murmur, best heard at the left infraclavicular area and in the left interscapular area (back).
- Click: An apical systolic ejection click may be heard if a bicuspid aortic valve is also present.
Diagnostic Evaluation
- Blood Pressure (BP) Measurements: The hallmark is a systolic BP difference of > 20 mmHg between the upper and lower extremities (upper > lower).
- Pulse Oximetry: May show differential cyanosis if a PDA is present, where the lower body has lower oxygen saturation than the upper body.
- Echocardiogram (ECHO): Confirms the site of narrowing, measures the pressure gradient across the coarctation, and assesses LV function.
- Electrocardiogram (ECG): In neonates, shows Right Ventricular Hypertrophy (RVH); in older children, shows Left Ventricular Hypertrophy (LVH).
- Chest X-Ray (CXR): May show cardiomegaly. In older children, "notching of the ribs" (3rd to 8th ribs) is seen due to erosion by dilated collateral intercostal arteries. The "3 sign" may be visible on the aorta.
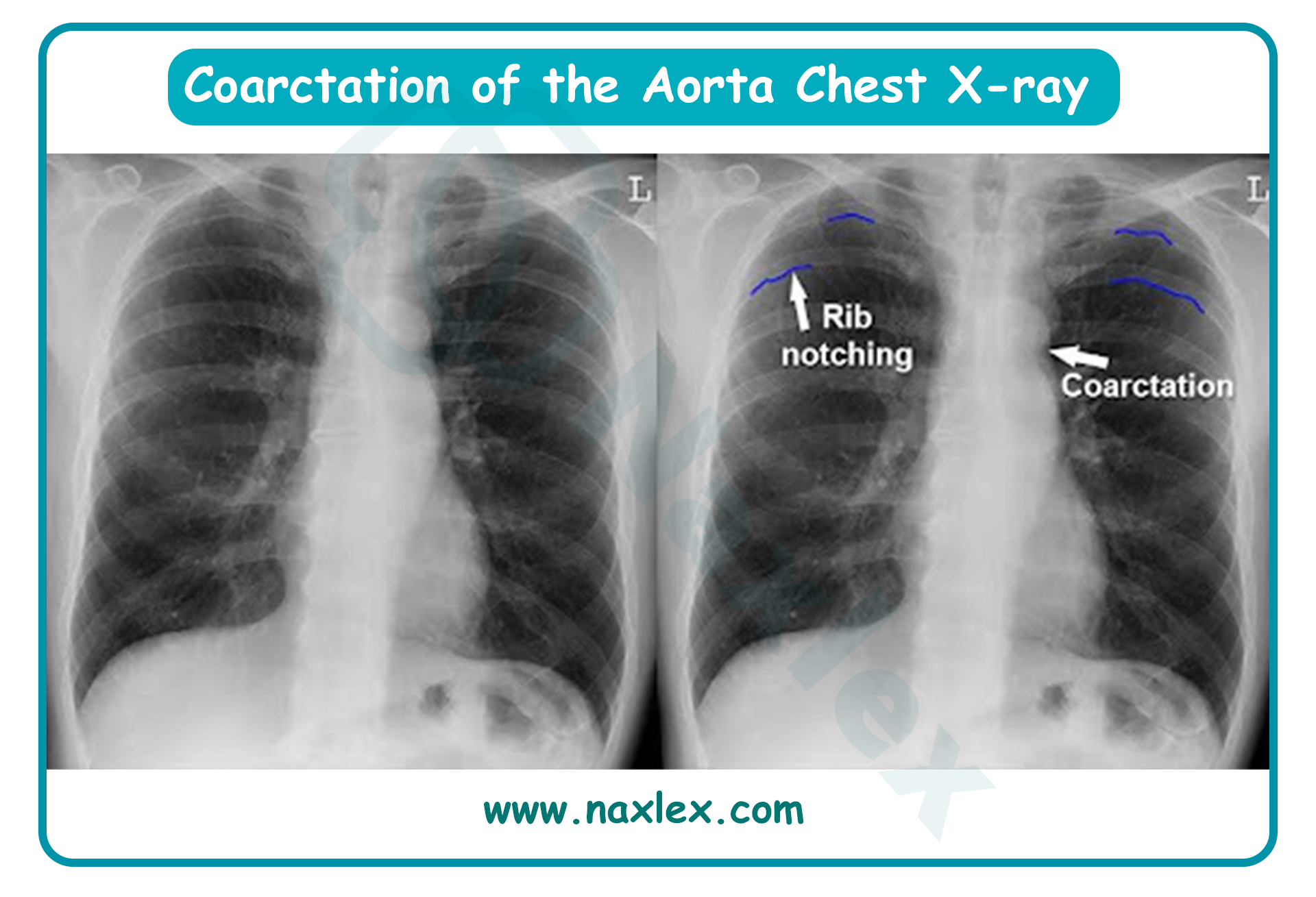
Therapeutic Management
- Management for Neonates with Critical Coarctation
- Prostaglandin E1 (Alprostadil) Infusion: Crucial to maintain patency of the ductus arteriosus (PDA) to provide blood flow to the lower body distal to the coarctation.
- Stabilization: Intubation and mechanical ventilation to reduce myocardial oxygen demand.
- Correction of Acidosis: Administration of sodium bicarbonate and fluid resuscitation.
- Management for Non-Critical Coarctation
- Elective surgical repair or balloon angioplasty usually performed between 2 and 5 years of age.
- Medical Management
- Inotropic Support: Dopamine or Dobutamine for neonates in shock.
- Diuretics: Furosemide to manage pulmonary congestion.
- Antihypertensives: Beta-blockers or ACE inhibitors (e.g., Captopril) used pre-operatively and sometimes post-operatively to control rebound hypertension.
- Surgical Management
- Resection with End-to-End Anastomosis: The narrowed segment is removed and the two healthy ends of the aorta are sewn together.
- Subclavian Flap Aortoplasty: Uses the left subclavian artery as a flap to widen the narrowed aortic area.
Image Title: Coarctation of Aorta Surgical Management
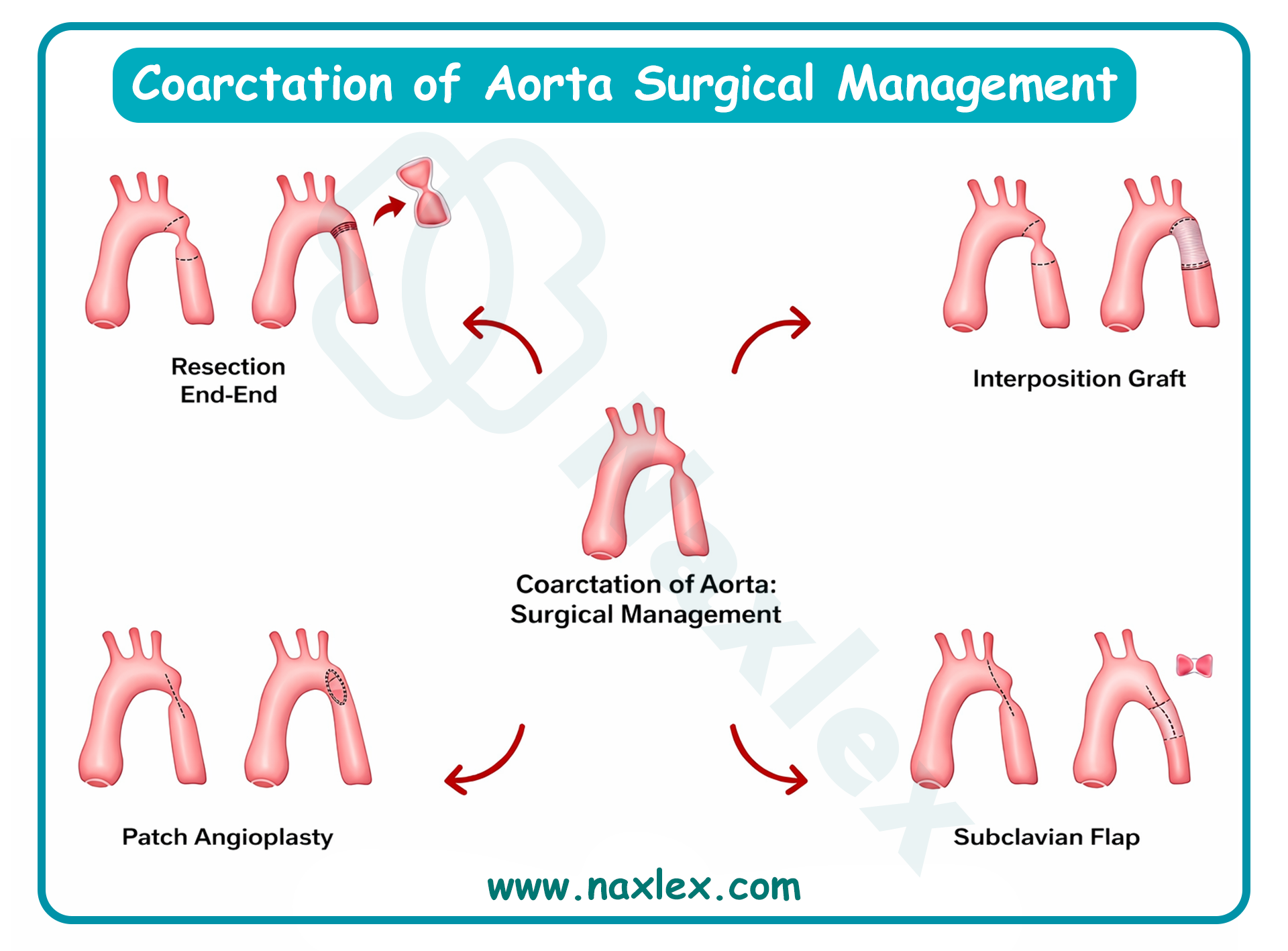
- Balloon Angioplasty / Stenting: Often the primary choice for recoarctation or in older children.
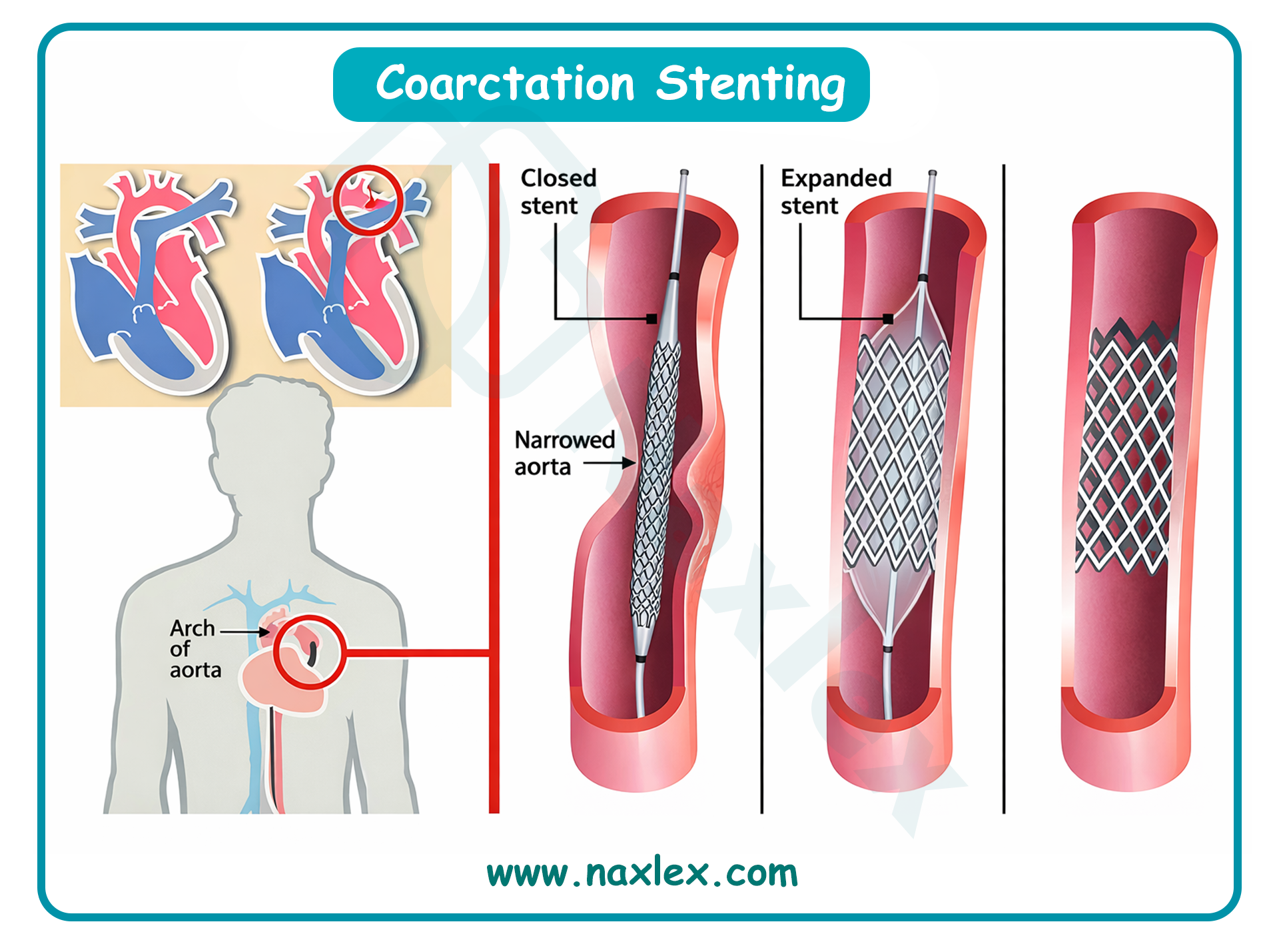
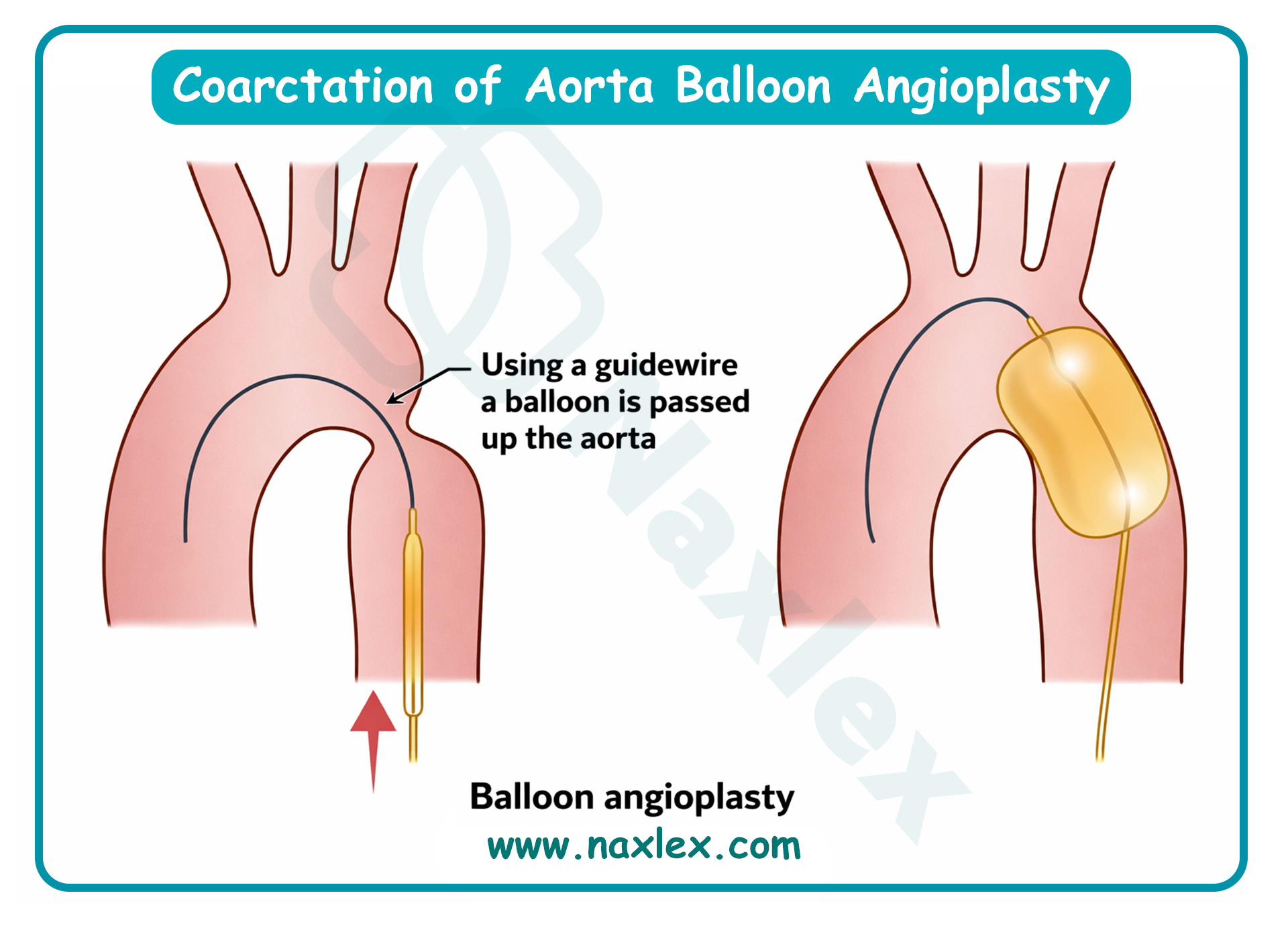
Post-Operative Nursing Interventions
- Post-Op Day 1 to 2:
- BP Monitoring: Use of an arterial line (usually right radial) for continuous monitoring. Monitor for "Paradoxical Hypertension" (rebound hypertension) which can cause suture line stress.
- Neurovascular Checks: Assess all 4 extremities for pulse strength, temperature, and capillary refill hourly.
- Pain Management: Continuous IV opioid infusion (Fentanyl or Morphine).
- Chest Tube: Monitor for chylothorax (milky drainage) if the thoracic duct was injured during surgery.
- Post-Op Day 3 to 5:
- Abdominal Assessment: Monitor for "Post-coarctectomy Syndrome" (mesenteric arteritis). Assess for abdominal pain, distension, and ileus caused by sudden increased perfusion to the gut.
- Activity: Gradual increase in ambulation; keep the head of the bed elevated.
- Wound Care: Monitor thoracotomy site for signs of infection.
Nursing Diagnosis (Post-Op)
- Post-Op Day 1 to 2:
- Risk for Ineffective Peripheral Tissue Perfusion related to surgical manipulation of the aorta and potential thrombus.
- Decreased Cardiac Output related to afterload changes and myocardial depression from bypass.
- Acute Pain related to thoracotomy and chest tube placement.
- Post-Op Day 3 to Discharge:
- Risk for Ineffective Gastrointestinal Tissue Perfusion related to mesenteric arteritis secondary to increased systemic pressure.
- Deficient Knowledge (Caregiver) related to long-term antihypertensive medication and activity restrictions.
- Risk for Infection related to surgical incision and invasive lines.
Complications
- Recurrent Coarctation: Occurs in up to 10% of infants repaired early.
- Post-Coarctectomy Syndrome: Mesenteric inflammation due to sudden changes in blood flow; can lead to bowel infarction if not managed.
- Paradoxical Hypertension: Extreme hypertension in the immediate post-operative period requiring IV nitroprusside or esmolol.
- Permanent Spinal Cord Ischemia: Rare; due to interruption of blood supply during aortic clamping.
Prognosis
- Generally excellent survival rate (> 98%).
- Life-long follow-up is mandatory as systemic hypertension can persist or develop years after a successful repair.
- Increased risk for premature coronary artery disease and cerebral aneurysms later in life.
Pulmonary valve stenosis
Definition
- Pulmonary valve stenosis (PS) is a right-sided obstructive congenital heart defect characterized by the narrowing of the pulmonary valve orifice. This obstruction impedes blood flow from the right ventricle into the pulmonary artery, necessitating higher right ventricular pressures to maintain pulmonary circulation.
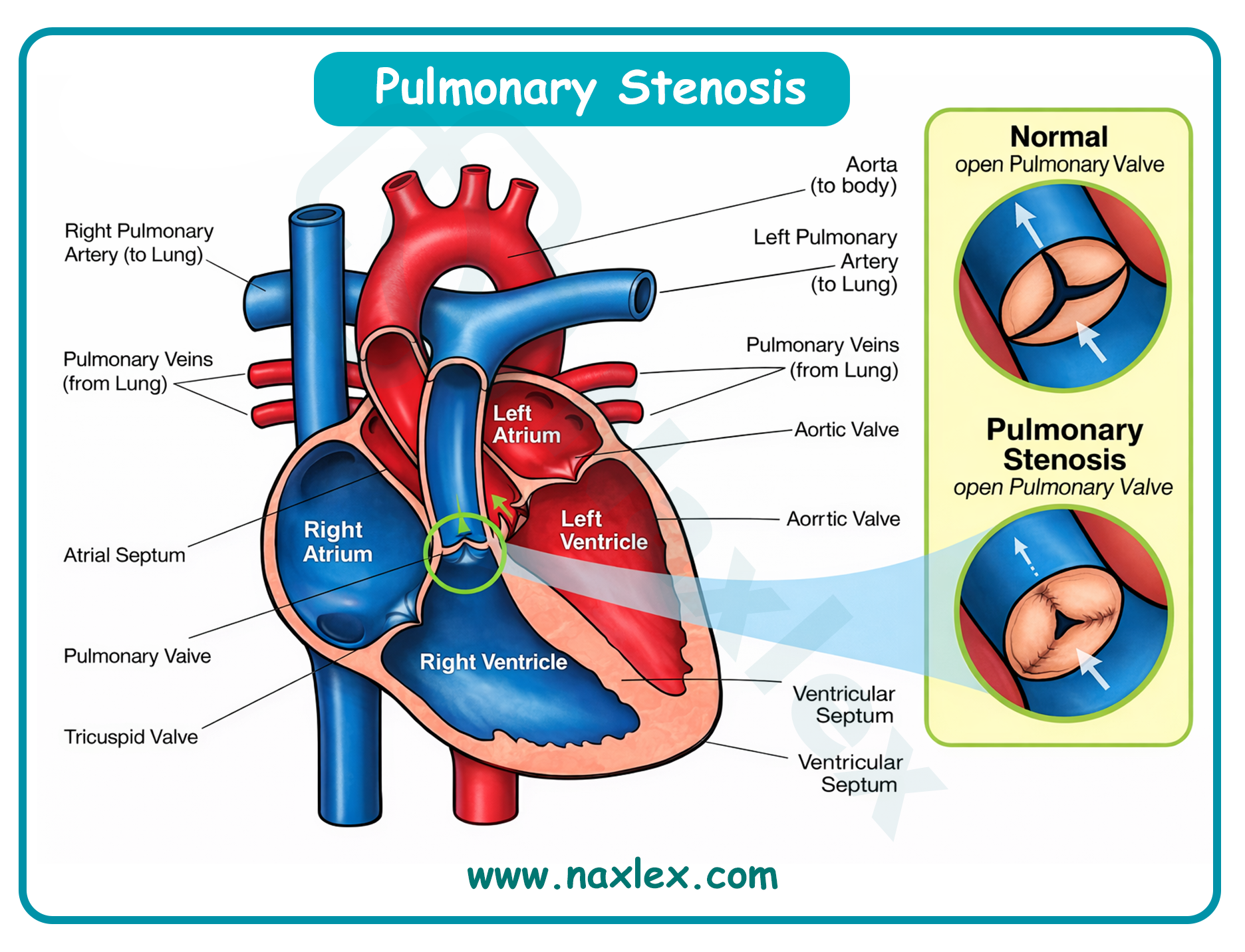
Epidemiology
- PS accounts for approximately 8% to 10% of all congenital heart defects.
- It occurs in roughly 1 in 2,000 live births.
- There is no strong gender predilection, though some studies suggest a slightly higher incidence in females.
- It frequently occurs as an isolated defect but can be associated with complex lesions like Tetralogy of Fallot.
Etiology
- Genetic Factors: Highly associated with Noonan Syndrome (approximately 50% of Noonan patients have PS, often with a dysplastic valve). Also linked to Alagille Syndrome and Williams Syndrome.
- Embryological Failure: Result of abnormal development of the pulmonary valve leaflets during the 6th to 9th week of gestation, leading to fused or thickened commissures.
- Environmental Factors: Maternal rubella infection is a known risk factor for peripheral pulmonary artery stenosis.
Pathophysiology
- Right Ventricular Afterload: The stenotic valve creates a pressure gradient. The right ventricle (RV) must generate higher systolic pressure to force blood through the narrowing.
- Right Ventricular Hypertrophy (RVH): Chronic pressure overload leads to compensatory concentric hypertrophy of the RV wall to maintain stroke volume.
- Right-Sided Heart Failure: As the RV becomes increasingly non-compliant and thick, end-diastolic pressure rises. Eventually, the RV fails, leading to right atrial (RA) enlargement.
- Shunting: If the RA pressure exceeds left atrial pressure, deoxygenated blood may shunt right-to-left through a patent foramen ovale (PFO), causing systemic cyanosis.
- Post-Stenotic Dilation: The high-velocity "jet" of blood passing through the stenotic valve can cause the wall of the main pulmonary artery to bulge or dilate.
Clinical Manifestations
Clinical presentation varies from asymptomatic to severe neonatal distress based on the degree of obstruction.
- Mild to Moderate PS: Usually asymptomatic; growth and development are often normal.
- Severe/Critical PS: Newborns present with "critical PS," appearing cyanotic (due to right-to-left shunting at the atrial level) and tachypneic.
- Exercise Intolerance: Older children may experience dyspnea on exertion, fatigue, and occasionally chest pain or syncope.
- Cardiac Auscultation Features:
- S2: Often widely split with a soft or absent pulmonic component (P2).
- Systolic Ejection Click: A high-pitched sound heard at the left upper sternal border that characteristically decreases in intensity during inspiration (the only right-sided sound to do so).
- Murmur: A harsh, crescendo-decrescendo systolic ejection murmur heard best at the 2nd left intercostal space.
- Radiation: The murmur may radiate toward the left clavicle and the back.
Diagnostic Evaluation
- Echocardiography (ECHO): The definitive diagnostic tool. It quantifies the pressure gradient (Mild: < 40 mmHg; Moderate: 40 to 79 mmHg; Severe: > 80 mmHg), visualizes valve morphology, and assesses RV function.
- Electrocardiogram (ECG): Reveals Right Axis Deviation (RAD) and Right Ventricular Hypertrophy (RVH), often characterized by tall R-waves in the right precordial leads (V1).
- Chest X-Ray (CXR): Often shows a prominent main pulmonary artery segment (post-stenotic dilation) and a "boot-shaped" appearance if RVH is significant, though heart size may be normal in mild cases.
- Pulse Oximetry: Saturations may be normal in isolated PS but will be low (cyanosis) in critical PS with an atrial right-to-left shunt.
Therapeutic Management
- Medical Management
- Prostaglandin E1 (Alprostadil): Indicated for neonates with critical PS to maintain patency of the ductus arteriosus, ensuring pulmonary blood flow until the valve can be opened.
- Diuretics: Used if signs of right-sided heart failure (hepatomegaly, edema) are present.
- Inotropic Support: May be required in neonates with RV dysfunction.
- Surgical/Interventional Management
- Percutaneous Balloon Pulmonary Valvuloplasty (BPV): The procedure of choice. A catheter is used to dilate the valve. It is highly successful with low recurrence rates.
- Surgical Valvotomy: Indicated if BPV is unsuccessful or if the valve is severely dysplastic (common in Noonan syndrome). Performed via cardiopulmonary bypass.
- Transventricular Valvotomy (Brock Procedure): A closed-heart surgical approach used in rare emergencies.
Post-Operative Nursing Interventions
- Post-Op Day 1 (Interventional/Surgical):
- Access Site Monitoring: If post-BPV, monitor the femoral site for hematoma, hemorrhage, or loss of distal pulses. Keep the affected extremity straight for 4 to 6 hours.
- Hemodynamic Monitoring: Observe for "Suicide Right Ventricle" (dynamic infundibular obstruction) where the thickened RV muscle obstructs its own outflow once the valve is opened.
- Arrhythmia Assessment: Monitor for Right Bundle Branch Block (RBBB) or ventricular ectopy.
- Post-Op Day 2 to 3:
- Fluid Balance: Monitor for right-sided failure symptoms (ascites, periorbital edema).
- Pain Management: Transition from IV to oral analgesics.
- Respiratory Support: Encourage incentive spirometry to prevent basal atelectasis.
Nursing Diagnosis (Post-Op)
- Post-Op Day 1:
- Risk for Ineffective Peripheral Tissue Perfusion related to femoral artery/vein catheterization or surgical bypass.
- Decreased Cardiac Output related to right ventricular diastolic dysfunction or arrhythmias.
- Impaired Gas Exchange related to altered pulmonary blood flow and anesthesia effects.
- Post-Op Day 2 to 3:
- Acute Pain related to surgical incision or invasive lines.
- Risk for Infection related to the presence of central lines or the sternotomy site.
- Deficient Knowledge (Caregiver) related to home monitoring and follow-up ECHO schedules.
Complications
- Pulmonary Regurgitation (PR): Common after BPV or surgery; usually well-tolerated but may lead to RV dilation over decades.
- Infective Endocarditis: Risk remains higher than the general population; necessitates education on dental hygiene.
- Residual Stenosis: May require repeat balloon dilation.
- Tricuspid Regurgitation: Due to high RV pressures or surgical manipulation.
Prognosis
- The prognosis is excellent for most children following BPV or surgery, with survival rates near 99%.
- Most children lead completely normal, active lives without exercise restrictions.
- Long-term follow-up is necessary to monitor for progressive pulmonary regurgitation or RV dilation in adulthood.
Summary
- Obstructive congenital heart disorders are characterized by a physical narrowing within the heart chambers, valves, or great vessels that impedes the exit of blood. This category primarily includes coarctation of the aorta, aortic stenosis, and pulmonic stenosis.
- The fundamental hemodynamic consequence is a significant increase in afterload. To overcome the resistance caused by the obstruction, the affected ventricle must work harder, eventually leading to compensatory muscular hypertrophy and, if untreated, potential heart failure.
- Clinical manifestations vary based on the site of the lesion. Left-sided obstructions (aortic stenosis and coarctation of the aorta) reduce systemic perfusion, often resulting in diminished cardiac output, exercise intolerance, and, in the case of coarctation, a distinct blood pressure gradient between the upper and lower extremities.
- Right-sided obstructions such as pulmonic stenosis, result in decreased pulmonary blood flow and may cause cyanosis in severe cases.
- Nursing management focuses on early detection of decreased cardiac output and monitoring for signs of systemic or pulmonary congestion.
- In critical neonatal cases, maintaining the patent ductus arteriosus (PDA) with prostaglandin therapy is a vital bridge to definitive treatment, which typically involves balloon valvuloplasty or surgical resection.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Congenital heart diseases: Obstructive disorders
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


