Please set your exam date
Physiological Maternal Changes
Study Questions
Practice Exercise 1
Which physiological change in pregnancy contributes to physiological anemia?
Explanation
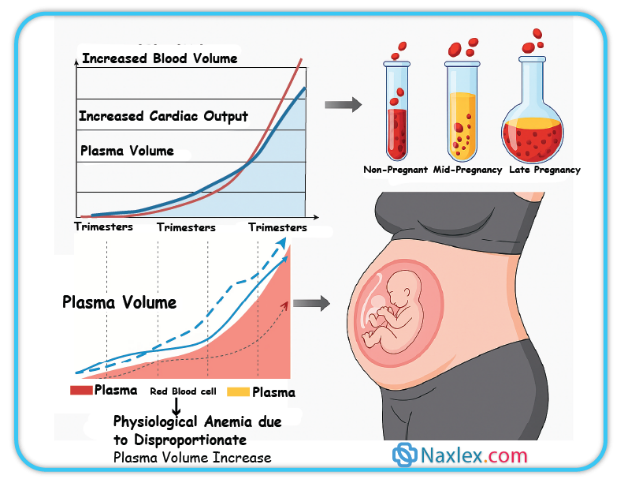
Physiological anemia in pregnancyis caused by an increased plasma volumerelative to red blood cell mass. Plasma volume expands by 40–50% while red blood cell mass rises only 20–30%, leading to hemodilution. The normal hemoglobin range in pregnancy is 11–13 g/dL, and hematocrit falls to 32–36%. This adaptation enhances uteroplacental perfusion but predisposes to symptoms like fatigueand paleness.
Rationale for correct answer
3.Plasma volume increases more than red blood cell mass, resulting in hemodilution and relative anemia. This explains the physiological anemia observed during pregnancy, which ensures optimal placental perfusion without true reduction in oxygen-carrying capacity.
Rationale for incorrect answers
1.Increased red blood cell mass does occur, but it is not sufficient to match the larger plasma volume expansion. Therefore, while it increases oxygen delivery, it does not cause anemia.
2.Decreased plasma volume is opposite of what occurs in pregnancy. Plasma volume expands significantly under estrogen and aldosterone influence, ensuring greater blood flow to the placenta.
4.Cardiac output increases by 30–50% in pregnancy due to increased stroke volume and heart rate. This enhances systemic and placental circulation but does not directly explain anemia.
Take home points
• Physiological anemia in pregnancy results from disproportionate plasma volume expansion.
• Hemoglobin values normally fall to 11–13 g/dL, hematocrit to 32–36% in pregnancy.
• Cardiac output and blood volume increase but oxygen-carrying capacity is maintained.
• Differentiate physiological anemia from iron-deficiency anemia, which lowers hemoglobin below 11 g/dL.
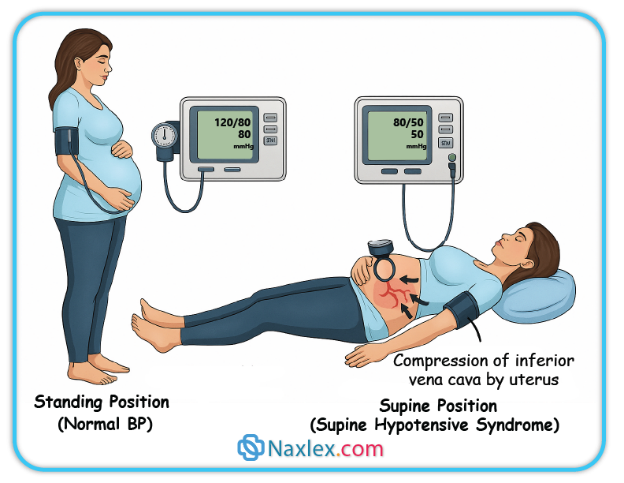
Supine hypotensive syndrome is caused by:
Explanation
Supine hypotensive syndromeoccurs when the gravid uterus causes compressionof the inferior vena cava, impairing venous return to the heart. This reduces preloadand cardiac output, leading to maternal hypotension, dizziness, pallor, and syncope. Normal systolic blood pressure in pregnancy is 100–120 mmHg, and diastolic is 60–80 mmHg. The condition appears after 20 weeks gestation when the uterus is large enough to obstruct venous return.
Rationale for correct answer
2.The gravid uterus compresses the inferior vena cava in the supine position, reducing venous return and cardiac output. This leads to hypotension and symptoms such as dizziness and pallor, defining supine hypotensive syndrome.
Rationale for incorrect answers
1.Compression of the aorta can occur in late pregnancy, but it does not primarily cause hypotension. Aortic compression mainly reduces uteroplacental perfusion and fetal oxygen delivery, not maternal blood pressure.
3.Peripheral vasodilation due to progesterone contributes to systemic vascular resistance reduction in pregnancy. However, it is a generalized adaptation of pregnancy, not the mechanism of acute hypotension in the supine position.
4.Cardiac output increases by 30–50% in pregnancy due to elevated stroke volume and heart rate. Supine position does not increase cardiac output but instead decreases it by restricting venous return.
Take home points
• Supine hypotensive syndrome results from inferior vena cava compression by the gravid uterus.
• It is most pronounced after 20 weeks gestation when the uterus is large.
• Symptoms include hypotension, dizziness, pallor, and syncope when lying supine.
• Management includes positioning the mother in the left lateral tilt to relieve vena cava compression.
What is the primary reason for increased tidal volume during pregnancy?
Explanation
Respiratory changes in pregnancyare driven mainly by the hormonalinfluence of progesteroneon the respiratory center in the medulla. Progesterone increases sensitivity to carbon dioxide, lowering arterial PaCO₂ to 27–32 mmHg (normal 35–45 mmHg). This causes increased tidal volumeand minute ventilation, ensuring adequate maternal oxygen delivery and fetal gas exchange despite unchanged respiratory rate.
Rationale for correct answer
2.Progesterone stimulates the central respiratory center, increasing sensitivity to carbon dioxide. This leads to deeper breaths, thereby increasing tidal volume and maternal minute ventilation, which supports enhanced oxygen transfer to the fetus.
Rationale for incorrect answers
1.Oxygen demand does not decrease in pregnancy; instead, it increases by about 20–30% due to fetal and maternal metabolic requirements. Therefore, decreased oxygen demand is not a cause of increased tidal volume.
3.Functional residual capacity decreases by about 20% during pregnancy because the enlarged uterus elevates the diaphragm. A reduced FRC does not cause increased tidal volume; rather, it reflects decreased lung volumes.
4.Chest wall compliance is not reduced in pregnancy. Rib cage expansion actually increases chest wall dimensions to accommodate the growing uterus, and this adaptation does not explain the rise in tidal volume.
Take home points
• Progesterone stimulates the maternal respiratory center, causing hyperventilation in pregnancy.
• Arterial PaCO₂ decreases to 27–32 mmHg as a normal pregnancy adaptation.
• Tidal volume and minute ventilation increase, but respiratory rate remains largely unchanged.
• Oxygen demand increases by 20–30% during pregnancy to meet maternal and fetal needs.
A pregnant client complains of nasal stuffiness and occasional nosebleeds. The nurse explains this is a common physiological change due to:
Explanation
Nasal congestion in pregnancyis primarily caused by estrogen-induced hyperemiaof the mucous membranes. Estrogen increases vascular engorgementand capillary permeability, leading to nasal stuffiness, epistaxis, and a sensation of obstruction. Normal blood volume increases by 40–50% during pregnancy, which enhances mucosal vascularity, further worsening nasal congestion. These changes are benign but commonly distressing to clients.
Rationale for correct answer
2.Estrogen increases vascular engorgement and hyperemia of the nasal mucosa. This leads to increased swelling and fragility of capillaries, causing stuffiness and frequent nosebleeds as a normal physiological change in pregnancy.
Rationale for incorrect answers
1.Blood volume does not decrease in pregnancy; instead, it increases by 40–50%. A decrease in blood volume would cause hypotension and poor perfusion, not nasal congestion or epistaxis.
3.Respiratory rate does not significantly decrease in pregnancy. It usually remains stable, while tidal volume increases. A reduced rate would impair gas exchange but does not cause nasal congestion or bleeding.
4.Increased clotting factors are a hematological change of pregnancy to reduce postpartum hemorrhage risk. While this creates a hypercoagulable state, it does not cause nasal stuffiness or epistaxis.
Take home points
• Estrogen increases nasal mucosal vascularity, causing congestion and nosebleeds in pregnancy.
• Blood volume increases 40–50% and contributes to mucosal engorgement.
• Respiratory rate remains stable, but tidal volume increases due to progesterone.
• Hypercoagulability in pregnancy prevents hemorrhage but does not cause nasal symptoms.
Which of the following are normal cardiovascular changes in pregnancy? Select all that apply.
Explanation
Cardiovascular changes in pregnancyare adaptive responses to support maternal and fetal needs. Blood volumeincreases by 40–50%, while heart raterises by 10–20 beats/minute, resulting in increased cardiac outputby 30–50%. Systemic vascular resistancedecreases due to progesterone-mediated smooth muscle relaxation. Hematocritdecreases to 32–36% because plasma volume increases more than red blood cell mass, causing physiological anemia.
Rationale for correct answers
1.Blood volume increases by 40–50% in pregnancy to meet the metabolic demands of the fetus and placenta. This expansion enhances perfusion and prepares for blood loss at delivery.
3.Heart rate increases by 10–20 beats/minute, which contributes to elevated cardiac output. This change helps maintain adequate circulation to the uterus and other maternal organs.
5.Hematocrit decreases to 32–36% because plasma volume expands more than red blood cell mass. This hemodilution results in physiological anemia of pregnancy.
Rationale for incorrect answers
2.Cardiac output does not decrease; it increases by 30–50% due to elevated stroke volume and heart rate. This adaptation ensures optimal uteroplacental perfusion.
4.Systemic vascular resistance does not increase; it decreases under the vasodilatory influence of progesterone, prostaglandins, and nitric oxide. This maintains normal to slightly lower blood pressure despite expanded blood volume.
Take home points
• Pregnancy increases blood volume by 40–50% and cardiac output by 30–50%.
• Heart rate rises by 10–20 beats/minute to maintain uteroplacental circulation.
• Hematocrit decreases to 32–36% due to plasma volume expansion.
• Systemic vascular resistance decreases under progesterone influence, keeping blood pressure stable or slightly reduced.
Practice Exercise 2
Which of the following gastrointestinal changes is typically attributed to the relaxation of the lower esophageal sphincter by progesterone?
Explanation
Heartburn (pyrosis)occurs in pregnancy mainly due to progesterone-induced relaxationof the lower esophageal sphincter. This hormone lowers smooth muscle tone, allowing gastric acid to reflux into the esophagus. Symptoms include burning sensation behind the sternum, worsened after meals or lying down. Normal lower esophageal sphincter pressure ranges between 10–30 mmHg, but pregnancy reduces it to below 10 mmHg. Risk factors include increased intra-abdominal pressure from the enlarging uterus and delayed gastric emptying. Complications include esophagitis and sleep disturbance.
Rationale for correct answer
3.The presence of heartburn (pyrosis) in pregnancy is directly linked to progesterone’s smooth muscle relaxation, causing reduced lower esophageal sphincter tone and gastric acid reflux. The clinical presentation is a burning retrosternal discomfort, especially worsened after meals or lying supine. This directly aligns with the pathophysiology described.
Rationale for incorrect answers
1.Pica is an abnormal craving for non-nutritive substances like clay or ice. It is associated with iron deficiency anemia, not progesterone-induced smooth muscle relaxation. Its pathophysiology relates to altered dopamine pathways and iron metabolism, not gastrointestinal sphincter tone.
2.Constipation is common in pregnancy but results from decreased intestinal peristalsis due to progesterone and increased water absorption in the colon. It is not caused by relaxation of the lower esophageal sphincter but rather delayed transit time within the intestines.
4.Gingivitis in pregnancy is due to vascular changes and exaggerated inflammatory response to dental plaque under high estrogen and progesterone levels. It involves gum swelling, bleeding, and hyperemia, not esophageal sphincter relaxation.
Take home points
• Progesterone lowers lower esophageal sphincter pressure, leading to gastroesophageal reflux and heartburn.
• Constipation in pregnancy results from delayed intestinal transit, not sphincter relaxation.
• Gingivitis is hormonally mediated gum inflammation, unrelated to esophageal sphincter physiology.
• Pica is associated with iron deficiency anemia, not gastrointestinal smooth muscle tone changes.
A nurse is educating a pregnant patient about managing heartburn. Which recommendation is most appropriate?
Explanation
Heartburn in pregnancyis caused by progesterone-induced relaxationof the lower esophageal sphincterand increased intra-abdominal pressurefrom the enlarging uterus. Gastric acid reflux produces a burning retrosternal sensation. Normal gastric pH is 1.5–3.5, and when acid refluxes into the esophagus, mucosal irritation occurs. Risk factors include recumbency after meals, consumption of fatty or spicy foods, and delayed gastric emptying. Non-pharmacological interventions are first-line, with emphasis on dietary modifications and positional therapy to reduce acid exposure to the esophagus.
Rationale for correct answer
3.Consuming small, frequent meals reduces gastric volume, minimizing reflux into the esophagus. Smaller meals decrease gastric distension, lowering the pressure gradient across the lower esophageal sphincter and reducing the likelihood of acid regurgitation.
Rationale for incorrect answers
1.Increasing consumption of spicy foods exacerbates gastric acid secretion and directly irritates the esophageal mucosa, worsening heartburn symptoms. It increases mucosal sensitivity and reflux episodes rather than preventing them.
2.Eating large, infrequent meals distends the stomach, raising intragastric pressure and facilitating reflux through the weakened sphincter. This directly opposes recommended management.
4.Lying flat after eating increases the likelihood of acid reflux due to gravitational loss of barrier protection. The horizontal position facilitates acid movement from the stomach into the esophagus, worsening symptoms.
Take home points
• Heartburn in pregnancy results from progesterone-induced lower esophageal sphincter relaxation.
• Small, frequent meals are the best dietary modification to reduce reflux symptoms.
• Large meals, spicy foods, and lying flat exacerbate gastric reflux.
• Lifestyle changes precede pharmacologic interventions in management.
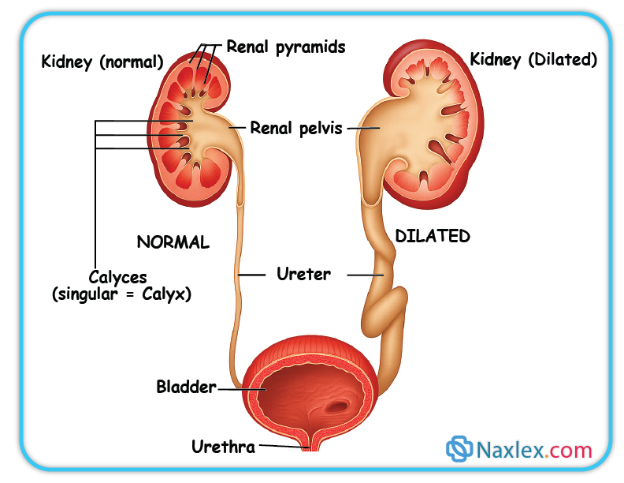
Urinary frequency in the first trimester is caused by:
Explanation
Urinary frequency in early pregnancyis due to uterine enlargementexerting pressure on the bladder, combined with hormonal effects of progesteroneand estrogen. Normal glomerular filtration rate (GFR) in non-pregnant adults is 90–120 mL/min, but in pregnancy, GFR actually increases by about 50% starting early in the first trimester. Plasma volume rises by 40–50%, and renal plasma flow increases by 50–80%, both enhancing urinary output. However, in the first trimester, the uterus remains a pelvic organ, directly compressing the bladder, leading to urinary frequency.
Rationale for correct answer
2.The enlarging uterus in the first trimester sits in the pelvis and presses on the bladder, reducing bladder capacity and causing urinary frequency. This mechanical pressure is the primary cause in early pregnancy before the uterus ascends into the abdominal cavity.
Rationale for incorrect answers
1.GFR does not decrease in pregnancy; instead, it increases significantly due to renal vasodilation and increased plasma volume. A decreased GFR would lower urine output, not increase urinary frequency.
3.Maternal blood volume does not reduce in pregnancy; it progressively increases by 40–50% to meet fetal and maternal needs. A reduced blood volume would impair renal perfusion, leading to oliguria, not urinary frequency.
4.Increased tubular reabsorption of fluid conserves body water and would reduce urine production. In pregnancy, although sodium and water retention occur, they do not directly cause urinary frequency in the first trimester.
Take home points
• First-trimester urinary frequency results from uterine pressure on the bladder.
• GFR increases in pregnancy, leading to greater renal clearance, not reduction.
• Maternal blood volume expands, not decreases, in pregnancy.
• Fluid reabsorption increases to maintain volume but does not cause frequency.
Which laboratory finding is expected in a healthy pregnant woman due to increased glomerular filtration rate?
Explanation
Renal physiology in pregnancyis altered due to increased glomerular filtration rate (GFR), elevated renal plasma flow, and hormonal changes involving progesteroneand estrogen. GFR increases by about 50% in early pregnancy, leading to enhanced clearance of creatinine, urea, and uric acid. Normal serum creatinine in non-pregnant adults is 0.6–1.1 mg/dL in women, but in pregnancy, it falls to 0.4–0.7 mg/dL. Mild glycosuria may occur due to reduced tubular reabsorption capacity, and small protein excretion (<300 mg/day) is considered normal. Elevated creatinine in pregnancy suggests renal impairment, not physiological adaptation.
Rationale for correct answer
2.Decreased serum creatinine is expected because increased GFR enhances filtration and clearance. A healthy pregnant woman often shows creatinine levels at the lower end of normal or slightly below, reflecting increased renal function.
Rationale for incorrect answers
1.Elevated serum creatinine is abnormal in pregnancy. It indicates impaired renal function, as physiologically creatinine should be reduced due to increased clearance. A creatinine >1.0 mg/dL in pregnancy is considered concerning.
3.Increased proteinuria beyond 300 mg/day is pathological and suggests preeclampsia or renal disease. Normal pregnancy allows only slight increases due to higher GFR, but not significant proteinuria.
4.Decreased glycosuria is not typical. Pregnancy often produces mild glycosuria due to increased GFR overwhelming tubular reabsorption, not a decrease. Persistent marked glycosuria, however, may indicate gestational diabetes.
Take home points
• GFR rises in pregnancy, lowering serum creatinine, urea, and uric acid levels.
• Elevated serum creatinine in pregnancy suggests renal impairment.
• Proteinuria >300 mg/day is abnormal and diagnostic for preeclampsia.
• Mild glycosuria is common in pregnancy due to tubular reabsorption changes.
Which of the following are true statements regarding renal system changes in pregnancy? Select all that apply.
Explanation
Renal system changes in pregnancyare driven by increased glomerular filtration rate (GFR), elevated renal plasma flow, and progesterone-mediated smooth muscle relaxation. GFR rises by ~50%, lowering serum creatinine (normal pregnancy 0.4–0.7 mg/dL) and blood urea nitrogen (BUN, normal pregnancy ~8–9 mg/dL). The enlarging uterus compresses the bladder causing urinary frequency. Progesterone relaxes ureters and renal pelvis, leading to dilation (hydronephrosis of pregnancy), urinary stasis, and increased urinary tract infection risk. Mild glycosuria is common due to decreased renal tubular reabsorption but does not always indicate gestational diabetes.
Rationale for correct answers
1.GFR increases significantly during pregnancy due to renal vasodilation and higher plasma volume. This enhances clearance of solutes, resulting in decreased serum creatinine and BUN.
2.Urinary frequency is common, especially in the first trimester due to bladder compression by the uterus and again in late pregnancy when the fetal head engages.
3.Dilation of renal pelves and ureters (hydronephrosis of pregnancy) occurs from progesterone-induced smooth muscle relaxation and uterine compression, causing urinary stasis and increased risk of UTI.
Rationale for incorrect answers
4.Serum creatinine and BUN do not increase in pregnancy. Both decrease due to increased GFR. Elevated values indicate abnormal renal function or preeclampsia.
5.Glycosuria is common due to increased filtered glucose load exceeding tubular reabsorptive capacity. It is not diagnostic of gestational diabetes unless persistent and associated with abnormal glucose tolerance testing.
Take home points
• GFR rises by ~50% in pregnancy, lowering creatinine and BUN levels.
• Urinary frequency occurs from uterine pressure on the bladder.
• Hydronephrosis of pregnancy predisposes to urinary tract infections.
• Mild glycosuria is common and not always diagnostic of gestational diabetes.
Practice Exercise 3
What is the primary role of human chorionic gonadotropin (hCG) in early pregnancy?
Explanation
Human chorionic gonadotropin (hCG)is a glycoproteinhormone secreted by the syncytiotrophoblastduring early pregnancy. Its main function is to support the corpus luteum, ensuring continuous secretion of progesterone and estrogen until placental steroidogenesis is sufficient. Serum hCG normally doubles every 48–72 hours in early gestation and peaks at 100,000 IU/L around 10 weeks.
Rationale for correct answer
2.hCG maintains the corpus luteum in the first trimester. This prevents luteal regression and ensures sustained progesterone production, which maintains endometrial decidualization and prevents menstruation. The question stem asking about the primary role makes this the correct response.
Rationale for incorrect answers
1.Promoting insulin resistance is primarily mediated by human placental lactogen (hPL), not hCG. hPL increases maternal lipolysis and reduces insulin sensitivity, ensuring more glucose is available for the fetus. hCG has no direct role in glucose regulation.
3.hCG has mild thyrotropic activity due to structural similarity with thyroid-stimulating hormone (TSH), which may increase thyroid hormone levels in some women, but this is not its primary role. Normal TSH range is 0.4–4.0 mIU/L, and clinically significant changes are uncommon in healthy pregnancy.
4.Relaxation of smooth muscles, such as the uterus and gastrointestinal tract, is primarily mediated by progesterone, not hCG. Progesterone reduces uterine contractility and slows intestinal motility, leading to symptoms such as constipation and reflux. hCG does not mediate smooth muscle relaxation.
Take home points
• hCG is secreted by syncytiotrophoblasts and maintains the corpus luteum during early pregnancy.
• hPL regulates maternal glucose metabolism and causes insulin resistance, not hCG.
• Progesterone maintains uterine quiescence by relaxing smooth muscle.
• hCG has weak TSH-like activity but this is not its primary physiological role.
Which hormone is primarily responsible for relaxing smooth muscles throughout the body during pregnancy, leading to effects such as heartburn and constipation?
Explanation
Progesteroneis a steroid hormone secreted by the corpus luteumearly in pregnancy and later by the placenta. Its primary role is maintaining uterine quiescenceby relaxing smooth muscle and preventing contractions. It also decreases gastrointestinal motility, causing constipation, and lowers lower esophageal sphincter tone, contributing to reflux. Normal serum progesterone levels in the first trimester range from 10–44 ng/mL.
Rationale for correct answer
3.Progesterone relaxes smooth muscle by reducing myometrial excitability, lowering uterine contractility, and suppressing prostaglandin activity. This action prevents preterm uterine contractions while also leading to systemic smooth muscle relaxation effects like gastroesophageal reflux and constipation.
Rationale for incorrect answers
1.Estrogen primarily stimulates uterine growth, increases blood flow, and enhances oxytocin receptor expression in the myometrium. It does not relax smooth muscle but instead contributes to uterine excitability in later pregnancy.
2.Human chorionic gonadotropin (hCG) maintains the corpus luteum in early pregnancy, ensuring continued progesterone secretion. It does not directly act on smooth muscle relaxation.
4.Human placental lactogen (hPL) regulates maternal metabolism by promoting lipolysis and inducing insulin resistance, ensuring glucose availability for the fetus. It has no role in smooth muscle tone regulation.
Take home points
• Progesterone is the hormone that relaxes smooth muscles during pregnancy.
• Relaxed lower esophageal sphincter tone leads to heartburn and reflux.
• Reduced intestinal motility causes constipation in pregnancy.
• Estrogen, hCG, and hPL serve different roles and do not mediate smooth muscle relaxation.
Which hormone promotes insulin resistance in pregnancy?
Explanation
Human placental lactogen (hPL)is a peptide hormonesecreted by the syncytiotrophoblast. It modifies maternal metabolismby increasing insulin resistance, thereby reducing maternal glucose uptake and ensuring fetal glucose supply. hPL also promotes lipolysis, increasing free fatty acids for maternal energy use. Normal maternal serum hPL levels rise progressively to 5–7 mg/L at term.
Rationale for correct answer
2.hPL promotes insulin resistance by antagonizing insulin action in maternal tissues. This spares glucose for the fetus while shifting maternal metabolism toward lipolysis. The physiologic insulin resistance peaks in the second and third trimesters, helping maintain fetal growth.
Rationale for incorrect answers
1.Human chorionic gonadotropin (hCG) maintains the corpus luteum in early pregnancy and supports progesterone secretion. It does not influence insulin sensitivity or glucose regulation.
3.Estrogen promotes uterine growth, increases uteroplacental blood flow, and enhances myometrial oxytocin receptor expression. It does not play a significant role in maternal insulin resistance.
4.Progesterone relaxes smooth muscles, maintaining uterine quiescence and reducing gastrointestinal motility. While it indirectly affects glucose metabolism, it is not the primary hormone responsible for insulin resistance in pregnancy.
Take home points
• hPL is the main hormone that promotes insulin resistance in pregnancy.
• Insulin resistance spares glucose for the fetus and shifts maternal metabolism to fat utilization.
• Excessive insulin resistance may contribute to gestational diabetes mellitus.
• Estrogen, progesterone, and hCG serve other reproductive roles without directly altering insulin sensitivity.
The primary role of human placental lactogen (hPL) is to:
Explanation
Human placental lactogen (hPL)is a placental hormonestructurally related to growth hormoneand prolactin. Its primary action is to induce insulin resistancein maternal tissues, ensuring continuous fetal glucose availability. hPL also stimulates maternal lipolysis, increasing free fatty acids as an alternate maternal energy source. Normal maternal serum hPL levels rise steadily during pregnancy, reaching 5–7 mg/L at term.
Rationale for correct answer
3.hPL increases maternal insulin resistance, which decreases maternal glucose utilization and increases circulating glucose for fetal transport. This adaptive mechanism ensures that fetal energy needs are prioritized, especially during the second and third trimesters.
Rationale for incorrect answers
1.Relaxation of uterine smooth muscle is mediated by progesterone, not hPL. Progesterone maintains uterine quiescence by reducing myometrial excitability and preventing premature contractions.
2.Maintenance of the corpus luteum is the role of human chorionic gonadotropin (hCG), which supports progesterone production in early pregnancy. hPL has no direct function in corpus luteum support.
4.Cervical softening is mediated by prostaglandins and relaxin, which remodel collagen in cervical tissue. hPL does not directly influence cervical ripening.
Take home points
• hPL primarily induces maternal insulin resistance to increase glucose availability for the fetus.
• Progesterone relaxes uterine smooth muscle, preventing contractions.
• hCG maintains the corpus luteum and progesterone secretion in early pregnancy.
• Cervical softening is mainly regulated by prostaglandins and relaxin, not hPL.
Which of the following are hormonal changes that support pregnancy? Select all that apply.
Explanation
Hormonal changes in pregnancyare critical for maintaining implantation, fetal growth, and maternal adaptation. hCGmaintains the corpus luteum for early progesterone secretion, progesteronerelaxes uterine smooth muscle and prevents contractions, while hPLinduces insulin resistance and promotes fetal glucose supply. Estrogenrises progressively, stimulating uterine growth and increasing blood flow. Normal total estrogen levels increase 10–100 fold, progesterone rises from 10–44 ng/mL in the first trimester to >100 ng/mL at term, and hCG peaks around 100,000 IU/L by 10 weeks.
Rationale for correct answers
1.Increased hCG supports the corpus luteum in early pregnancy, ensuring continuous progesterone production until placental steroidogenesis becomes sufficient.
2.Increased hPL promotes maternal insulin resistance, sparing glucose for fetal use and enhancing maternal lipolysis for alternative energy sources.
4.Increased progesterone maintains uterine quiescence by reducing myometrial excitability, while also contributing to smooth muscle relaxation in other systems.
Rationale for incorrect answers
3.Estrogen does not decrease; it significantly increases during pregnancy, stimulating uterine growth, breast development, and increasing uteroplacental perfusion.
5.Thyroid hormone production does not decrease; in fact, mild increases occur due to hCG’s thyrotropic effect, with free thyroxine (T4) levels slightly rising in early pregnancy. Normal maternal free T4 range is 0.7–1.9 ng/dL.
Take home points
• hCG, hPL, estrogen, and progesterone all increase during pregnancy.
• Progesterone prevents uterine contractions and supports smooth muscle relaxation.
• hPL induces insulin resistance, sparing glucose for fetal development.
• Thyroid activity slightly increases due to hCG stimulation, not decreases.
Comprehensive Questions
The increase in uterine size during pregnancy is primarily due to:
Explanation
Uterine enlargement in pregnancyis primarily caused by hypertrophyof smooth muscle fibers accompanied by hyperplasiaunder the influence of estrogen and progesterone. Increased vascularizationsupports tissue growth and enlargement. The uterus grows from 70 g to about 1100 g by term. Uterine blood flow increases from 50 mL/min to 500–700 mL/min at term, with normal uterine artery resistance decreasing significantly.
Rationale for correct answer
2.Uterine growth occurs through hypertrophy, which is the increase in muscle cell size, and hyperplasia, which is the increase in the number of cells. Estrogen stimulates hyperplasia, while progesterone promotes hypertrophy. This dual mechanism explains the large size of the uterus at term.
Rationale for incorrect answers
1.Hyperplasia occurs in pregnancy, but atrophy does not. Atrophy is a reduction in cell size, which is opposite of what occurs in uterine enlargement. Muscle fibers increase in both number and size during pregnancy, making this option incorrect.
3.Uterine blood flow actually increases greatly in pregnancy. A decrease would compromise placental perfusion and fetal development. Normal blood flow rises from about 50 mL/min in nonpregnant state to 500–700 mL/min at term, therefore a decrease cannot explain uterine growth.
4.Development of new uterine cells from scratch does not occur. Instead, existing myometrial cells undergo hyperplasia and hypertrophy. Uterine cells are not newly created; the process is a modification of pre-existing smooth muscle fibers.
Take home points
• Uterine growth in pregnancy occurs through both hypertrophy and hyperplasia of smooth muscle.
• Estrogen primarily stimulates hyperplasia, while progesterone promotes hypertrophy.
• Uterine blood flow increases significantly to support placental perfusion and fetal growth.
• Atrophy and development of new cells from scratch are not physiological mechanisms in pregnancy.
A nurse is assessing a pregnant patient in the third trimester who reports dizziness when lying flat. What is the most likely cause?
Explanation
Supine hypotensive syndromeoccurs in late pregnancy when the gravid uteruscompresses the inferior vena cavawhile lying supine, reducing venous returnand decreasing cardiac output. This leads to maternal hypotension, dizziness, pallor, and tachycardia. Normal maternal cardiac output in pregnancy increases by 30–50% (from 4.5 L/min to 6–7 L/min).
Rationale for correct answer
2.Supine hypotensive syndrome results from compression of the inferior vena cava by the enlarged uterus, especially in the third trimester. This reduces venous return, lowers preload, and decreases cardiac output, causing dizziness when lying flat. Symptoms resolve when the woman turns to the left lateral position.
Rationale for incorrect answers
1.Increased cardiac output occurs in pregnancy due to increased blood volume and stroke volume, peaking at 30–50% above baseline. This increase improves tissue perfusion and does not cause dizziness when supine. Instead, reduced output from vena cava compression explains the symptom.
3.Physiological anemia in pregnancy results from plasma volume expansion exceeding red cell mass increase, leading to lower hematocrit values (normal pregnancy hemoglobin 11–12 g/dL, hematocrit 32–34%). It causes fatigue and pallor, not positional dizziness specific to lying supine.
4.Hyperventilation occurs due to progesterone-mediated respiratory drive increase, leading to mild respiratory alkalosis (PaCO₂ 28–32 mmHg, normal pregnancy pH 7.40–7.45). This causes dyspnea but not dizziness limited to supine position.
Take home points
• Supine hypotensive syndrome results from gravid uterine compression of the inferior vena cava.
• Symptoms include dizziness, pallor, hypotension, and tachycardia when lying flat.
• Turning to the left lateral position relieves symptoms by restoring venous return.
• Physiological anemia and hyperventilation are normal pregnancy changes but do not explain positional dizziness.
Goodell’s sign, the softening of the cervical tip, is primarily caused by:
Explanation
Goodell’s signis the softening of the cervical tipobserved around 6–8 weeks of pregnancy. It is caused by increased vascularity, hyperplasia, and hypertrophyof cervical glands due to estrogen and progesterone. Normal cervical tissue is firm, but with increased blood flow and edema, the cervix becomes softand pliable.
Rationale for correct answer
3.Goodell’s sign results from increased vascularity leading to engorgement, along with hyperplasia and hypertrophy of cervical glands. Estrogen increases blood flow and stimulates cervical tissue changes, causing the softening of the cervix detected on pelvic exam.
Rationale for incorrect answers
1.Decreased vascularity would make the cervix less perfused and firmer, not softer. Goodell’s sign specifically results from increased blood flow, not reduction.
2.Increased collagen content makes tissue more rigid and firm. In pregnancy, cervical collagen is remodeled and partially degraded, contributing to softening, not increased firmness.
4.Uterine contractions do not cause early cervical softening. Contractions influence cervical effacement and dilation during labor, but Goodell’s sign occurs in early pregnancy before labor begins.
Take home points
• Goodell’s sign is cervical softening detected at 6–8 weeks of pregnancy.
• It results from increased vascularity, hyperplasia, and hypertrophy of cervical glands.
• Increased collagen would firm the cervix, but in pregnancy collagen is remodeled for softness.
• Uterine contractions affect dilation in labor, not early pregnancy softening.
Which hematologic change increases the risk of thromboembolism in pregnancy?
Explanation
Hypercoagulability in pregnancydevelops as a protective adaptation to minimize hemorrhageat delivery, but it also increases the risk of thromboembolism. There is a marked rise in fibrinogenand several clotting factors(VII, VIII, IX, X, XII), while fibrinolytic activity decreases. Normal fibrinogen levels in nonpregnant women are 200–400 mg/dL, but in pregnancy, they rise to 400–650 mg/dL. This procoagulant state peaks in the third trimester and the puerperium.
Rationale for correct answer
2.Increased fibrinogen levels contribute to the hypercoagulable state of pregnancy. Elevated fibrinogen enhances clot formation and is a major factor in increasing the risk of venous thromboembolism, which is one of the leading causes of maternal morbidity and mortality.
Rationale for incorrect answers
1.Decreased clotting factors would reduce coagulation and increase the risk of bleeding, not thrombosis. Pregnancy is characterized by increased clotting factor activity, not reduction.
3.Reduced platelet count (gestational thrombocytopenia) can occur, but it is usually mild and not enough to outweigh the hypercoagulable changes. A lower platelet count actually tends toward bleeding risk, not thromboembolism.
4.Decreased white blood cell count is not typical in pregnancy. Instead, leukocytosis (WBC up to 12,000–15,000/µL, sometimes 25,000/µL in labor) is common. White blood cell levels are not directly related to thromboembolic risk in pregnancy.
Take home points
• Pregnancy is a hypercoagulable state due to increased fibrinogen and clotting factors.
• Elevated fibrinogen levels (400–650 mg/dL) significantly increase thromboembolism risk.
• Platelet count may slightly fall, but this does not negate the hypercoagulable effect.
• Thromboembolism is a major cause of maternal morbidity and mortality, especially postpartum.
Which of the following gastrointestinal discomforts is most likely caused by relaxation of the lower esophageal sphincter by progesterone?
Explanation
Heartburn in pregnancyis primarily due to progesterone-induced relaxationof the lower esophageal sphincter, which allows gastric acid refluxinto the esophagus. Progesterone also delays gastric emptying and decreases gastrointestinal motility. Normal lower esophageal sphincter pressure decreases progressively during pregnancy, predisposing to gastroesophageal reflux. Symptoms usually peak in the second and third trimesters.
Rationale for correct answer
1.Heartburn is the burning substernal sensation caused by reflux of gastric acid. Progesterone relaxes the lower esophageal sphincter, allowing backflow of stomach contents. This is the most direct gastrointestinal discomfort linked with progesterone-induced relaxation.
Rationale for incorrect answers
2.Constipation in pregnancy is caused by decreased bowel motility and prolonged transit time due to progesterone’s effect on smooth muscle. However, it is not due to lower esophageal sphincter relaxation but rather intestinal smooth muscle relaxation.
3.Nausea is primarily related to increased human chorionic gonadotropin and estrogen levels, especially in the first trimester. It is not due to esophageal sphincter changes.
4.Gingivitis results from increased vascularity, edema, and hormonal effects on gingival tissue, often leading to bleeding gums. It is unrelated to sphincter relaxation or acid reflux.
Take home points
• Heartburn in pregnancy results from progesterone-induced relaxation of the lower esophageal sphincter.
• Constipation is also progesterone-related but involves reduced intestinal motility, not sphincter relaxation.
• Nausea is linked to elevated hCG and estrogen levels, particularly in early pregnancy.
• Gingivitis arises from vascular and hormonal changes in gingival tissues, not gastrointestinal reflux.
Which respiratory change is normal in pregnancy?
Explanation
Respiratory adaptations in pregnancyinclude increased minute ventilation, driven mainly by elevated tidal volumedue to progesterone stimulation of the respiratory center. Normal tidal volume increases by about 30–40% (from 500 mL to ~650–700 mL), while minute ventilation increases by 30–50%. Oxygen consumption rises by 20–30% to meet maternal–fetal demands. Functional residual capacity decreases by ~20% due to upward displacement of the diaphragm by the gravid uterus.
Rationale for correct answer
2.Increased minute ventilation occurs because tidal volume rises while respiratory rate remains relatively stable. Progesterone increases sensitivity to CO₂, lowering PaCO₂ to 28–32 mmHg and causing mild respiratory alkalosis, a normal physiological adaptation.
Rationale for incorrect answers
1.Tidal volume does not decrease in pregnancy; it increases by 30–40% due to progesterone. A decrease would impair oxygen delivery, which is incompatible with normal pregnancy physiology.
3.Oxygen consumption increases by 20–30% to support maternal metabolism and fetal growth. A reduction would compromise oxygen delivery to both mother and fetus.
4.Functional residual capacity decreases by about 20% because the diaphragm is elevated up to 4 cm by the gravid uterus. An increase is not possible due to reduced thoracic space.
Take home points
• Minute ventilation increases in pregnancy due to higher tidal volume.
• Progesterone drives hyperventilation, lowering maternal PaCO₂ to 28–32 mmHg.
• Oxygen consumption increases 20–30% to meet maternal and fetal needs.
• Functional residual capacity decreases due to diaphragmatic elevation by the enlarged uterus.
The relaxation and increased mobility of pelvic ligaments and joints during pregnancy are primarily caused by the hormone:
Explanation
Relaxinis a peptide hormonesecreted mainly by the corpus luteum, decidua, and placenta during pregnancy. It increases collagen remodelingand connective tissue elasticity, promoting relaxation of pelvic ligaments and increased joint mobility to facilitate childbirth. Relaxin levels peak in the first trimester and again near term. Normal effects also include softening of the cervix and inhibition of uterine contractions to maintain early pregnancy.
Rationale for correct answer
3.Relaxin causes relaxation and softening of pelvic ligaments and joints, especially the pubic symphysis and sacroiliac joints. This increases pelvic mobility and prepares the birth canal for labor. It also contributes to cervical ripening through collagen breakdown and connective tissue remodeling.
Rationale for incorrect answers
1.Oxytocin stimulates uterine smooth muscle contractions during labor and milk ejection from the breast. It does not influence ligament relaxation or pelvic joint mobility.
2.Prolactin is primarily involved in mammary gland development and initiation of lactation. It has no role in pelvic ligament relaxation or connective tissue changes in pregnancy.
4.Cortisol regulates metabolism and has a role in fetal lung maturation, but it does not act on pelvic ligaments or joints. Its effects are primarily catabolic and immunomodulatory, not structural relaxation.
Take home points
• Relaxin softens pelvic ligaments and joints to facilitate delivery.
• It is secreted by the corpus luteum, decidua, and placenta.
• Cervical ripening and inhibition of uterine contractions are additional effects.
• Oxytocin, prolactin, and cortisol have different physiological roles unrelated to ligament relaxation.
Which hormone is primarily responsible for mood swings in pregnancy?
Explanation
Estrogenis a steroid hormonethat rises significantly in pregnancy, produced mainly by the placentaafter the first trimester. It influences neurotransmitter regulation, particularly serotonin and dopamine, which are involved in mood control. Rapidly increasing estrogen levels contribute to mood swings, irritability, and emotional lability often reported during pregnancy. Normal estradiol levels increase from ~50–350 pg/mL (follicular phase) to >10,000–40,000 pg/mL in late pregnancy.
Rationale for correct answer
2.Estrogen fluctuations and high levels alter central nervous system neurotransmission, especially serotonin, leading to emotional instability and mood swings. This is the primary hormonal factor for psychological changes during pregnancy.
Rationale for incorrect answers
1.Human placental lactogen regulates maternal glucose metabolism and increases insulin resistance to ensure fetal glucose supply. It does not act directly on neurotransmitters or cause mood swings.
3.Insulin regulates blood glucose by facilitating cellular glucose uptake. While hypoglycemia or hyperglycemia can cause irritability, insulin itself is not the hormonal cause of mood swings in pregnancy.
4.Thyroxine (T4) regulates metabolism and oxygen consumption. Abnormal thyroid hormone levels can cause anxiety or depression, but normal pregnancy mood swings are not primarily due to thyroxine.
Take home points
• Estrogen is the main hormone responsible for mood swings in pregnancy.
• High estrogen levels affect serotonin and dopamine pathways in the brain.
• Human placental lactogen and insulin regulate glucose, not emotions.
• Thyroxine regulates metabolism; abnormal levels may mimic mood changes but are not typical causes.
Diastasis recti abdominis is:
Explanation
Diastasis recti abdominisis the separationof the rectus abdominismuscles along the linea alba, usually due to stretching from the enlarging uterus and hormonal effects on connective tissue. The gap may exceed 2 cm, measured at the umbilicus. It presents with a midline bulge when abdominal muscles are contracted but does not involve a true fascial defect as in hernia. Risk factors include multiparity, multiple gestations, and advanced maternal age.
Rationale for correct answer
2.Diastasis recti abdominis is specifically defined as the separation of the rectus abdominis muscles along the linea alba. It occurs due to mechanical stretching of the abdominal wall during pregnancy combined with hormonal softening of connective tissues. This makes the option scientifically accurate.
Rationale for incorrect answers
1.Pregnancy-induced hypertension is a hypertensive disorder occurring after 20 weeks of gestation, defined as blood pressure ≥140/90 mmHg on two occasions. It has no relation to abdominal muscle separation and involves vascular pathophysiology, not musculoskeletal changes.
3.Neurological disorders affecting balance involve dysfunction of the cerebellum, vestibular system, or proprioception. Diastasis recti is purely a musculoskeletal and connective tissue condition and does not affect neural pathways or balance.
4.A permanent abdominal muscle tear implies actual rupture of muscle fibers. Diastasis recti does not involve tearing but rather stretching and thinning of the linea alba with separation of muscle bellies. It may improve postpartum with exercises or persist without complications of a true tear.
Take home points
• Diastasis recti abdominis is the separation of rectus muscles along the linea alba.
• The condition is due to uterine expansion and hormonal effects on connective tissue.
• It differs from hernia and muscle tears, as no fascial defect or rupture occurs.
• Risk factors include multiple pregnancies, advanced maternal age, and increased intra-abdominal pressure.
What is the expected increase in maternal blood volume during pregnancy?
Explanation
Maternal blood volume increase in pregnancyoccurs to meet increased metabolic demands, uteroplacental circulation, and fetal development. Plasma volumerises by 40–50% and red blood cell massrises by 20–30%. This results in hemodilutioncalled physiologic anemia. Normal hematocrit in pregnancy is 32–42%, hemoglobin 11–12 g/dL, and normal non-pregnant hematocrit is 36–46%. Increased cardiac outputand reduced systemic vascular resistance maintain adequate perfusion.
Rationale for correct answer
2.Maternal blood volume increases by 30–50% during pregnancy. This expansion supports uteroplacental perfusion and compensates for blood loss at delivery. The stem asked for the expected increase, which directly aligns with this physiologic range.
Rationale for incorrect answers
1.A 10–20% increase is too low and would not meet pregnancy demands. Such a small increase could not sustain placental blood flow or provide reserve for intrapartum hemorrhage. Scientific data consistently report expansion closer to 40–50%.
3.A 60–80% increase would be excessive and pathologic. This degree of hypervolemia would lead to severe hemodilution, pulmonary edema, and possible high-output cardiac failure. Physiologically, maternal cardiovascular adaptation plateaus at about 50%.
4.A 90–100% increase is not physiologically possible. Doubling blood volume would cause circulatory overload and profound cardiopulmonary compromise. Such levels are not compatible with normal adaptation in pregnancy.
Take home points
• Maternal blood volume increases by 30–50% during pregnancy.
• Hemodilution results in physiologic anemia with hemoglobin 11–12 g/dL and hematocrit 32–42%.
• Increased plasma volume supports uteroplacental circulation and compensates for delivery blood loss.
• Differentiation is important from pathologic hypervolemia such as preeclampsia or heart failure.
Which of the following are common physiological changes affecting the cardiovascular system during pregnancy? Select all that apply.
Explanation
Cardiovascular changes in pregnancyare adaptive responses that maintain maternal and fetal perfusion. Blood volumerises by 30–50% and cardiac outputincreases by 30–50% due to higher stroke volume and heart rate. Systemic vascular resistancedecreases from progesterone-mediated vasodilation. Physiological anemiaresults from disproportionate plasma expansion. The maternal state becomes hypercoagulableto prevent postpartum hemorrhage, with increased clotting factors VII, VIII, IX, X, and fibrinogen.
Rationale for correct answers
1.Blood volume increases 30–50% to sustain uteroplacental circulation and provide a reserve for delivery blood loss. This is a normal physiologic change.
3.Physiological anemia occurs because plasma volume rises more than red cell mass. Hematocrit falls to 32–42% and hemoglobin to 11–12 g/dL, producing dilutional anemia.
5.Pregnancy is a hypercoagulable state due to increased coagulation factors and fibrinogen, which lowers fibrinolytic activity. This adaptation reduces postpartum hemorrhage risk but raises thromboembolism risk.
Rationale for incorrect answers
2.Cardiac output does not decrease. Instead, it rises by 30–50% from increased heart rate and stroke volume, peaking in mid-pregnancy. A decrease would compromise placental perfusion.
4.Systemic vascular resistance does not increase. Progesterone and prostaglandins cause vasodilation, lowering resistance to accommodate higher blood volume without severe hypertension. An increase would predispose to preeclampsia.
Take home points
• Blood volume and cardiac output increase significantly in pregnancy.
• Physiologic anemia develops due to disproportionate plasma expansion.
• Pregnancy induces a hypercoagulable state to prevent hemorrhage but raises clotting risk.
• Systemic vascular resistance decreases, distinguishing normal adaptation from hypertensive disorders.
Which of the following are normal respiratory changes in pregnancy? Select all that apply.
Explanation
Respiratory changes in pregnancyare driven by hormonal and mechanical factors to meet higher oxygen demand. Progesteroneincreases respiratory center sensitivity to CO₂, raising tidal volumeby about 30–40%. Minute ventilationrises by 30–50%, leading to mild respiratory alkalosis with PaCO₂ 28–32 mmHg (normal non-pregnant PaCO₂ 35–45 mmHg). Oxygen consumptionincreases by 15–20% due to fetal and maternal metabolic needs. The enlarging uterus elevates the diaphragm, reducing functional residual capacityby 20%. Respiratory rateremains unchanged or slightly increased, not decreased.
Rationale for correct answers
1.Tidal volume increases by 30–40% from progesterone stimulation of the respiratory center. This enhances alveolar ventilation and maintains maternal-fetal gas exchange.
3.Oxygen consumption increases 15–20% to meet maternal and fetal metabolic demands. This adaptation ensures sufficient oxygen delivery across the placenta.
4.Functional residual capacity decreases by about 20% due to diaphragm elevation from the gravid uterus. This lowers lung reserve volume and contributes to dyspnea in late pregnancy.
Rationale for incorrect answers
2.Minute ventilation does not decrease. Instead, it increases by 30–50% because of higher tidal volume. A decrease would cause hypercapnia and impair placental gas exchange.
5.Respiratory rate does not decrease. It usually remains stable or slightly increases by 1–2 breaths/min. A decrease would reduce alveolar ventilation and worsen hypoxemia risk.
Take home points
• Pregnancy increases tidal volume and minute ventilation, not respiratory rate.
• Oxygen consumption rises by 15–20% to support maternal-fetal metabolism.
• Functional residual capacity decreases due to diaphragm elevation.
• Maternal PaCO₂ is reduced to 28–32 mmHg, causing mild compensated respiratory alkalosis.
Which of the following endocrine glands or organs undergo significant functional changes during pregnancy? Select all that apply.
Explanation
Endocrine changes in pregnancyare crucial for maternal adaptation and fetal development. The placentaacts as a temporary endocrine organ producing hCG, hPL, progesterone, and estrogens. The pituitary glandenlarges due to lactotroph hyperplasia, increasing prolactin. The thyroid glandincreases hormone output with total T4 and T3 rising, though free T4 remains within 0.8–1.8 ng/dL. Adrenal glandsproduce more cortisol and aldosterone, elevating total plasma cortisol to 16–29 µg/dL. The pancreasincreases insulin secretion, but maternal tissues develop insulin resistance from hPL, predisposing to gestational diabetes.
Rationale for correct answers
1.The placenta functions as an endocrine organ, producing hCG to maintain the corpus luteum, progesterone to support gestation, estrogens for uterine growth, and hPL to induce insulin resistance.
2.The pituitary gland enlarges by about 30% in pregnancy, driven by lactotroph proliferation, which increases prolactin secretion to prepare for lactation.
4.The adrenal glands increase secretion of cortisol, corticosterone, and aldosterone. Cortisol rises progressively, reaching up to 2–3 times non-pregnant levels, modulating immune tolerance and metabolism.
5.The pancreas increases β-cell mass and insulin secretion. Peripheral insulin resistance develops from placental hormones, particularly hPL, which ensures glucose availability to the fetus.
Rationale for incorrect answers
3.The thyroid gland Enlarges slightly and increases production of thyroxine (T4)and triiodothyronine (T3). This maintains metabolic support for pregnancy.
Take home points
• The placenta is a temporary endocrine organ producing hCG, hPL, progesterone, and estrogens.
• The pituitary enlarges and prolactin secretion rises for lactation.
• The thyroid and adrenal glands increase hormone output to meet maternal-fetal demands.
• The pancreas adapts with increased insulin secretion but maternal insulin resistance develops.
Which of the following are appropriate interventions to prevent constipation in pregnancy? Select all that apply.
Explanation
Constipation in pregnancyis common due to hormonal and mechanical factors. Progesteronerelaxes smooth muscle, slowing colonic transit, while the enlarging uterus compresses the intestines. Normal bowel movement frequency ranges from 3 times/day to 3 times/week. Low fiberintake (<25 g/day), reduced activity, and inadequate hydrationworsen symptoms. Typical clinical features are infrequent stools, straining, and hard stool consistency. Preventive strategies include dietary fiber >25–30 g/day, fluid intake >2 L/day, regular exercise, and meal pattern adjustment.
Rationale for correct answers
1.Increased fiber intake enhances stool bulk and water retention, stimulating peristalsis. Daily intake of 25–30 g is recommended for pregnant women to prevent constipation.
3.Regular exercise improves bowel motility by stimulating colonic activity. Activities like walking 30 minutes daily are safe and effective in pregnancy.
5.Promoting small, frequent meals helps regulate digestion, prevents gastric overfilling, and maintains steady bowel function. This supports peristalsis and reduces bloating.
Rationale for incorrect answers
2.Reducing fluid intake worsens constipation. Adequate hydration (≥2 L/day) softens stools and supports normal bowel function. Low fluid intake results in harder stools and straining.
4.Avoiding stool softeners is incorrect. Stool softeners such as docusate sodium are considered safe in pregnancy and may be used when lifestyle measures are insufficient. They reduce straining without systemic absorption.
Take home points
• Progesterone-induced smooth muscle relaxation slows bowel transit in pregnancy.
• Adequate fiber, fluids, and exercise are first-line preventive strategies.
• Small frequent meals regulate digestion and reduce bloating.
• Stool softeners are safe in pregnancy if lifestyle changes are inadequate.
Which of the following are true statements regarding renal system changes in pregnancy? Select all that apply.
Explanation
Renal changes in pregnancyoccur due to hormonal and mechanical effects. Glomerular filtration rate (GFR)increases by 40–50% from early pregnancy, lowering serum creatinine (0.4–0.7 mg/dL) and blood urea nitrogen (BUN) (7–12 mg/dL vs non-pregnant 10–20 mg/dL). Urinary frequencyresults from increased GFR and bladder compression by the uterus. Progesteronecauses smooth muscle relaxation, leading to dilation of the renal pelvesand ureters, increasing stasis and risk for urinary tract infections. Mild glycosuriamay appear due to lower renal glucose threshold but does not always indicate gestational diabetes.
Rationale for correct answers
1.GFR increases 40–50% beginning early in pregnancy due to renal vasodilation and higher plasma volume. This is a physiologic adaptation.
2.Urinary frequency is common because of increased GFR and mechanical compression of the bladder by the enlarging uterus.
3.Dilation of renal pelves and ureters, known as hydronephrosis of pregnancy, occurs from progesterone-induced smooth muscle relaxation and uterine pressure. This increases UTI risk.
Rationale for incorrect answers
4.Serum creatinine and BUN do not increase. Instead, both decrease due to higher GFR. Normal serum creatinine in pregnancy is 0.4–0.7 mg/dL compared to 0.6–1.1 mg/dL in non-pregnant women. BUN decreases to 7–12 mg/dL.
5.Glycosuria does not always indicate gestational diabetes. It is often physiologic due to decreased renal threshold for glucose excretion. Only persistent or high-level glycosuria warrants further evaluation with glucose tolerance testing.
Take home points
• GFR increases 40–50% in pregnancy, lowering creatinine and BUN levels.
• Urinary frequency is due to both increased filtration and uterine compression.
• Ureteral and pelvic dilation increase the risk for urinary tract infections.
• Mild glycosuria is physiologic, but persistent glycosuria needs evaluation for gestational diabetes.
Exams on Physiological Maternal Changes
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
• To describe in detail the physiological maternal adaptations of the cardiovascular, respiratory, gastrointestinal, renal, and endocrine systems during pregnancy.
• To explain the clinical significance of these physiological changes in relation to maternal and fetal well-being.
• To provide nursing insights that highlight high-yield facts essential for clinical practice and nursing examinations.
• To link theoretical knowledge to practical nursing interventions in real patient care.
• To reinforce learning with selected practice questions and comprehensive review questions.
Introduction
Pregnancy is characterized by profound physiological changes across multiple organ systems. These adaptations occur to sustain the growing fetus, prepare the maternal body for labor, and protect the mother against the physiological stress of delivery. The changes are primarily mediated by hormonal influences, mechanical effects of the enlarging uterus, and the metabolic demands of the fetus.
Understanding these changes is essential for nurses, as they often mimic pathological conditions but are within the spectrum of normal pregnancy physiology. For instance, a decreased hematocrit may suggest anemia, but in pregnancy, it often reflects hemodilution. Similarly, shortness of breath may be due to increased tidal volume rather than cardiopulmonary pathology.
The nurse must be able to differentiate normal physiological changes from pathological conditions, implement appropriate nursing interventions, and educate patients regarding
Cardiovascular System
1.1 Hemodynamic Changes
• The cardiovascular system undergoes dramatic adaptations to accommodate the increased metabolic demands of the fetus and placenta.
• Blood volume increases progressively, beginning as early as the first trimester, and peaks around the 32nd to 34th week of gestation.
• Maternal heart rate increases by 10–20 beats per minute, ensuring adequate perfusion of uteroplacental circulation.
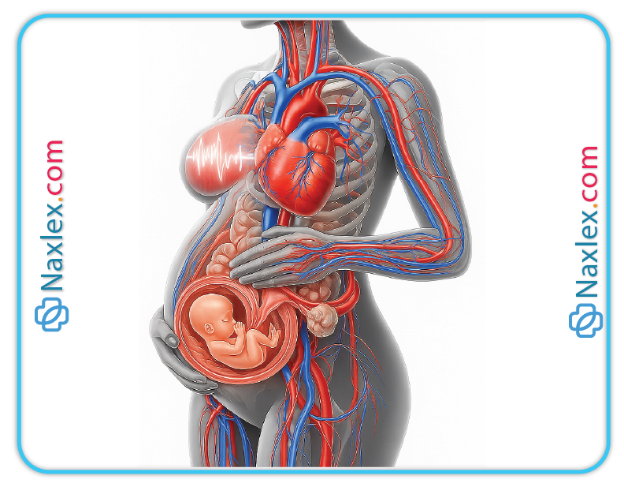
1.2 Blood Volume and Cardiac Output
• Maternal blood volume increases by approximately 30–50% above pre-pregnancy levels.
➤ Plasma volume increases disproportionately compared to red blood cell mass.
➤ This leads to physiological (dilutional) anemia of pregnancy.
• Cardiac output increases by 30–50%, peaking around mid-pregnancy.
➤ Increased stroke volume and increased heart rate contribute to the rise.
➤ Enhanced cardiac output ensures optimal placental perfusion.
1.3 Vascular Resistance and Blood Pressure
• Systemic vascular resistance decreases due to the vasodilatory effects of progesterone, nitric oxide, and relaxin.
• Blood pressure generally decreases in the second trimester (notably diastolic BP), then returns to baseline by the third trimester.
• Decreased afterload facilitates increased cardiac output without excessive cardiac strain.
1.4 Hematologic Changes
• Plasma volume increases by 40–50%, while red cell mass increases by only 20–30%, resulting in hemodilution.
• Hemoglobin and hematocrit values decrease, a normal adaptation known as physiological anemia of pregnancy.
• Leukocytosis is common, with WBC counts rising up to 15,000–20,000/mm³ in late pregnancy and labor.
• Hypercoagulability is induced by increased clotting factors (fibrinogen, factors VII, VIII, IX, X, and XII) and decreased fibrinolytic activity.
➤ This adaptation reduces postpartum hemorrhage risk but increases thromboembolic risk.
1.5 Supine Hypotensive Syndrome
• In the supine position, the gravid uterus compresses the inferior vena cava, reducing venous return to the heart.
• This leads to decreased preload, reduced cardiac output, hypotension, dizziness, and syncope.
• Supine hypotension is most common in the third trimester.
• The left lateral recumbent position is the preferred posture to optimize venous return and uteroplacental perfusion.
1.6 Clinical Nursing Considerations
• Nurses must assess maternal cardiovascular status frequently, especially in women with pre-existing cardiac disease.
• Orthostatic hypotension should be anticipated due to vascular tone changes.
• Nurses should educate patients to avoid lying flat on their back in late pregnancy.
• Increased clotting potential requires vigilance for signs of deep vein thrombosis (DVT).
Nursing Insights
• Physiological anemia is due to plasma volume expansion outpacing red blood cell mass increase.
• Supine hypotension should always be corrected by turning the patient to the left lateral position.
• The normal heart murmur of pregnancy (systolic ejection murmur) results from increased blood flow and usually requires no intervention.
• Pregnant women are at higher risk for thromboembolism due to the hypercoagulable state; nurses must assess for unilateral leg swelling, redness, and warmth.
• Knowledge of normal blood volume increase (30–50%) and cardiac output rise (30–50%) is high-yield for exams.
Respiratory System
1.1 Anatomical Adaptations
• The enlarging uterus elevates the diaphragm by approximately 4 cm during late pregnancy.
➤ Despite elevation, diaphragmatic excursion increases due to thoracic cage expansion.
• The chest circumference expands by 5–7 cm, and the subcostal angle widens from approximately 68° to 103°.
• The diaphragm becomes the primary muscle of respiration, with less reliance on abdominal musculature.
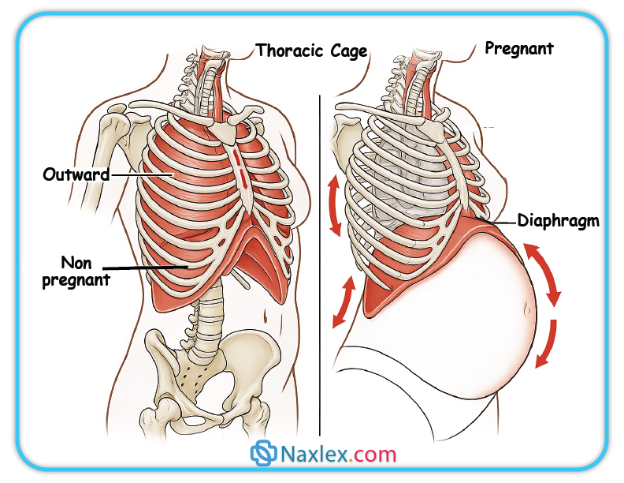
1.2 Functional Respiratory Changes
• Tidal volume increases by 30–40% due to the stimulatory effect of progesterone on the medullary respiratory center.
• Minute ventilation rises by 30–50%, primarily from increased tidal volume, not respiratory rate.
• Respiratory rate remains relatively stable or increases slightly.
• Functional residual capacity (FRC) decreases due to reduced expiratory reserve volume and residual volume.
• Oxygen consumption increases by 15–20% to meet maternal and fetal metabolic demands.
1.3 Gas Exchange and Oxygen Demand
• Maternal arterial PaCO₂ decreases to approximately 28–32 mmHg (compared to 40 mmHg in non-pregnant women).
➤ This mild respiratory alkalosis facilitates the transfer of CO₂ from fetus to mother.
• Bicarbonate concentration decreases to partially compensate for alkalosis.
• Increased alveolar ventilation ensures adequate oxygen delivery to both maternal and fetal tissues.
1.4 Clinical Nursing Considerations
• Pregnant women often report dyspnea, especially in the third trimester, due to increased tidal volume and elevated diaphragm.
• Nurses must differentiate between physiological dyspnea and pathological conditions such as pulmonary embolism or pneumonia.
• Nasal congestion and epistaxis are common due to estrogen-induced hyperemia and vascular engorgement of mucous membranes.
• Women should be advised to sleep with the head of the bed elevated if respiratory discomfort occurs.
• Hyperventilation during labor is normal, but excessive hyperventilation may cause respiratory alkalosis, leading to lightheadedness and tingling.
Nursing Insights
• The primary reason for increased tidal volume in pregnancy is progesterone’s effect on the respiratory center, not increased oxygen demand alone.
• Decreased PaCO₂ is a normal compensatory change that enhances fetal CO₂ clearance across the placenta.
• Shortness of breath is expected, but sudden onset of chest pain with dyspnea should alert the nurse to possible pulmonary embolism.
• Nurses should anticipate an increased need for oxygen during labor and immediate postpartum recovery.
• Knowledge of increased minute ventilation and decreased functional residual capacity is essential for anesthesia management in obstetrics.
Gastrointestinal System
1.1 Hormonal Influence on the GI Tract
• The gastrointestinal (GI) system is significantly affected by the hormonal environment of pregnancy, particularly progesterone and estrogen.
• Progesterone relaxes smooth muscle, leading to delayed gastric emptying and decreased intestinal motility.
• Estrogen increases vascularity and may cause hyperemia of the gums and mucous membranes, contributing to gingivitis and bleeding gums.
1.2 Changes in Appetite, Nausea, and Vomiting
• Nausea and vomiting are common in the first trimester, often referred to as “morning sickness,” though symptoms may occur at any time of day.
➤ This is associated with elevated hCG and estrogen levels.
➤ Usually subsides by the second trimester.

• Some women may develop hyperemesis gravidarum, a severe and persistent form of nausea and vomiting that leads to dehydration, electrolyte imbalance, and weight loss.
• Appetite may increase in the second and third trimesters due to the growing caloric demands of the fetus.
1.3 Gastric and Intestinal Motility
• Progesterone-induced relaxation of the lower esophageal sphincter (LES) predisposes pregnant women to gastroesophageal reflux and heartburn (pyrosis).
• Gastric emptying is delayed, especially during labor, which increases the risk of aspiration under anesthesia.
• Intestinal transit time is prolonged, enhancing absorption of nutrients but also contributing to constipation.
• Hemorrhoids are common due to increased venous pressure from the enlarging uterus and constipation.
1.4 Common Gastrointestinal Symptoms
• Ptyalism (excessive salivation): may occur in early pregnancy.
• Gingivitis and bleeding gums: due to estrogen-mediated vascular changes in the oral cavity.
• Constipation: due to decreased bowel motility, reduced activity, and increased iron supplementation.
• Gallbladder hypomotility: increases risk of gallstone formation.
• Altered taste and smell perceptions may lead to food aversions or cravings, sometimes extending to pica (eating non-nutritive substances).
Nursing Insights
• Nurses should encourage small, frequent meals and advise against lying flat after eating to reduce heartburn.
• Constipation prevention strategies: high-fiber diet, adequate fluid intake, and moderate exercise are essential.
• Hyperemesis gravidarum requires immediate intervention to prevent electrolyte imbalance and maternal-fetal complications.
• Iron supplementation contributes to constipation, so nurses should pair patient teaching with dietary management strategies.
• Any severe abdominal pain, hematemesis, or persistent vomiting should not be attributed to “normal pregnancy changes” but evaluated for pathology.
Renal System
1.1 Anatomical Changes
• The kidneys enlarge slightly, and the renal pelvis and ureters dilate under the influence of progesterone.
• The right ureter is more dilated than the left due to uterine dextrorotation and compression by the gravid uterus.
• Ureteral dilation and urinary stasis predispose to urinary tract infections (UTIs).
• The bladder becomes displaced upward and anteriorly by the growing uterus.
1.2 Functional Changes (GFR, Renal Plasma Flow)
• Renal plasma flow increases by 50–80% during mid-pregnancy.
• Glomerular filtration rate (GFR) rises by 30–50%, leading to decreased serum levels of creatinine, blood urea nitrogen (BUN), and uric acid.
• Glycosuria may occur due to increased GFR and reduced tubular reabsorption, but persistent or high levels require evaluation for gestational diabetes.
• Mild proteinuria may occur but significant proteinuria suggests pathology such as preeclampsia.
1.3 Electrolyte and Fluid Balance
• Sodium retention occurs due to increased aldosterone activity, helping to maintain expanded plasma volume.
• Water retention increases total body fluid by about 6–8 liters, supporting fetal, placental, and maternal tissue growth.
• Increased filtration predisposes to mild hyponatremia in some women.
1.4 Susceptibility to Urinary Tract Infections
• Urinary stasis and ureteral dilation increase susceptibility to UTIs and pyelonephritis.
• Asymptomatic bacteriuria is more common in pregnancy and should always be treated to prevent ascending infection.
• UTIs are associated with risks of preterm labor, low birth weight, and maternal sepsis if untreated.
Nursing Insights
• Normal pregnancy is associated with decreased serum creatinine; elevated creatinine should alert the nurse to renal pathology.
• Glycosuria can be normal, but persistent findings require further testing to rule out gestational diabetes mellitus.
• Nurses should teach pregnant women to maintain hydration and practice proper perineal hygiene to reduce UTI risk.
• Routine urine dipstick testing in prenatal care is essential for detecting proteinuria or glycosuria early.
• Pregnant women should be educated on the importance of promptly reporting dysuria, frequency, urgency, or flank pain.
Endocrine System
1.1 Placental Hormones
• The placenta becomes a major endocrine organ during pregnancy, producing hormones essential for fetal growth and maternal adaptation.
• Human chorionic gonadotropin (hCG):
➤ Produced by trophoblastic cells as early as implantation.
➤ Maintains the corpus luteum until the placenta takes over progesterone and estrogen production at 10–12 weeks.
➤ Basis for most pregnancy tests.
• Progesterone:
➤ Maintains the endometrium and prevents uterine contractions.
➤ Relaxes smooth muscle, contributing to GI hypomotility and urinary stasis.
➤ Facilitates breast gland development for lactation.
• Estrogen:
➤ Stimulates uterine growth and blood flow.
➤ Increases vascularity, leading to nasal congestion, gum hyperemia, and spider angiomas.
➤ Promotes breast ductal system development.
• Human placental lactogen (hPL):
➤ Produced by syncytiotrophoblast cells.
➤ Antagonizes insulin, promoting maternal insulin resistance.
➤ Ensures glucose availability for the fetus by reducing maternal glucose uptake.
• Relaxin:
➤ Softens pelvic ligaments and joints to facilitate childbirth.
➤ Relaxes the cervix in preparation for labor.
1.2 Pituitary Adaptations
• Anterior pituitary:
➤ Increases production of prolactin to prepare breasts for lactation.
➤ Growth hormone secretion is suppressed as placental hPL predominates.
• Posterior pituitary:
➤ Stores and releases oxytocin, which stimulates uterine contractions and milk ejection.
➤ Oxytocin activity is inhibited during pregnancy but rises significantly at term and during labor.
1.3 Thyroid and Parathyroid Changes
• Thyroid gland:
➤ Enlarges slightly and increases production of thyroxine (T4) and triiodothyronine (T3).
➤ Enhanced thyroid hormone levels support maternal basal metabolic rate and fetal brain development.
• Parathyroid glands:
➤ Secrete increased parathyroid hormone (PTH) to regulate calcium and phosphorus metabolism.
➤ Calcium demands are greatest in the third trimester when fetal bone mineralization is maximal.
1.4 Adrenal and Pancreatic Changes
• Adrenal glands:
➤ Cortisol secretion increases to support glucose metabolism and fetal organ maturation.
➤ Aldosterone levels rise, promoting sodium and fluid retention.
• Pancreas:
➤ Early pregnancy is characterized by increased insulin sensitivity.
➤ As pregnancy progresses, placental hormones (hPL, progesterone, cortisol, estrogen) induce insulin resistance.
➤ This ensures adequate glucose availability for the fetus but predisposes the mother to gestational diabetes mellitus (GDM) if pancreatic function cannot meet increased insulin demand.
Nursing Insights
• Nurses must educate patients that hCG is responsible for nausea and vomiting in early pregnancy, while hPL causes insulin resistance in later pregnancy.
• Normal pregnancy is a diabetogenic state; thus, screening for gestational diabetes is recommended between 24–28 weeks.
• Maternal thyroid function is essential for fetal neurodevelopment; untreated hypothyroidism can impair cognitive outcomes in the fetus.
• Prolactin prepares the breasts, but milk secretion is inhibited by high progesterone and estrogen until after delivery.
• Relaxin and progesterone together account for many musculoskeletal and GI discomforts reported during pregnancy.
Integumentary System
1.1 Pigmentation Changes
• Melasma (Chloasma): Also known as the “mask of pregnancy,” characterized by irregular brown hyperpigmented patches over the cheeks, forehead, and nose.
➤ Caused by increased melanocyte-stimulating hormone, estrogen, and progesterone.
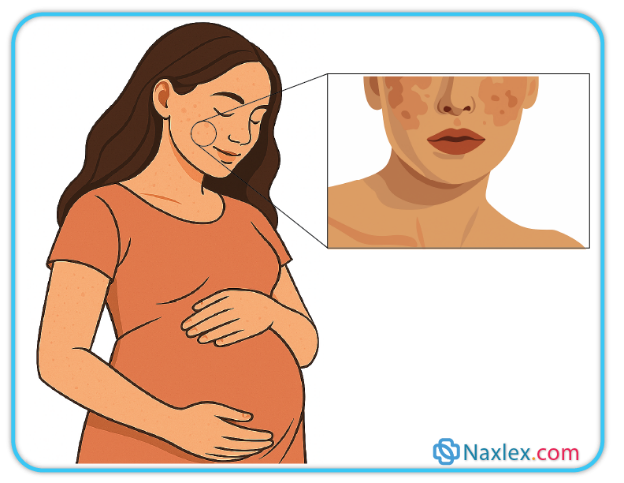
• Linea nigra: A hyperpigmented line running from the symphysis pubis to the xiphoid process.
• Darkening of nipples, areolae, vulva, and perineum occurs due to increased melanin deposition.
1.2 Connective Tissue and Skin Changes
• Striae gravidarum (stretch marks): Caused by stretching and tearing of dermal connective tissue with collagen disruption.
➤ Typically appear on abdomen, breasts, thighs, and buttocks.
• Spider angiomas and palmar erythema: Due to estrogen-mediated vascular changes.
• Vascular nevi and varicosities: Commonly develop in the legs, vulva, and rectum (hemorrhoids).
1.3 Hair and Nail Changes
• Hair: Increased estrogen prolongs the anagen (growth) phase of hair, leading to thicker hair during pregnancy.
➤ Postpartum telogen effluvium (hair shedding): Occurs 2–4 months after delivery when estrogen levels drop.
• Nails: May become softer, more brittle, or grow faster.
Nursing Insights
• Hyperpigmentation and striae are common, and nurses should provide anticipatory guidance to reduce cosmetic concerns.
• Melasma may worsen with sun exposure; advise sun protection to minimize pigmentation.
• Varicosities and hemorrhoids improve postpartum but can cause significant discomfort; nurses should recommend support stockings, elevation of legs, and high-fiber diet.
• Postpartum hair loss is temporary and resolves within months; reassurance is an important nursing role.
Musculoskeletal System
1.1 Postural and Structural Changes
• The enlarging uterus shifts the maternal center of gravity forward, leading to compensatory changes.
• Lumbar lordosis develops to balance body weight, often causing low back pain.
• Relaxin and progesterone relax ligaments and joints, particularly in the pelvis.
➤ Increases mobility but predisposes to joint discomfort and instability.
1.2 Abdominal Wall Changes
• Diastasis recti abdominis: Separation of the rectus abdominis muscles along the midline due to uterine enlargement.
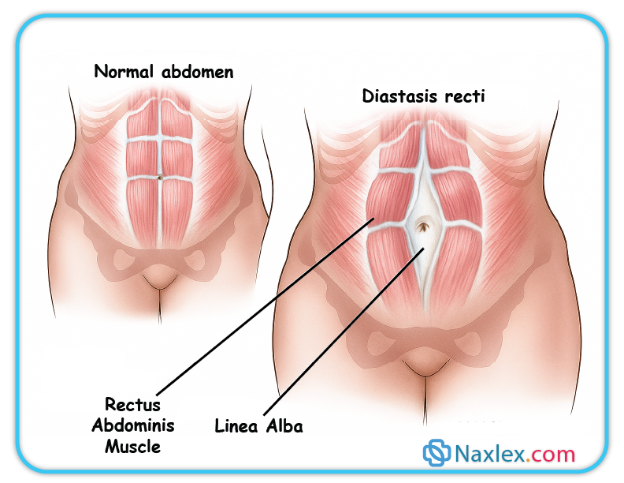
• Abdominal muscle tone decreases, contributing to poor posture and discomfort.
1.3 Pelvic Adaptations
• Softening of pelvic ligaments and widening of the symphysis pubis prepare for delivery.
• These changes, while beneficial for childbirth, may cause pelvic girdle pain.
1.4 Common Musculoskeletal Complaints
• Low back pain: Due to increased lordosis and ligament relaxation.
• Leg cramps: Related to altered calcium and magnesium balance, pressure on nerves, and circulatory changes.
• Carpal tunnel syndrome: Compression of the median nerve from fluid retention.
Nursing Insights
• Encourage proper posture and use of supportive footwear to reduce back strain.
• Pelvic tilt exercises and prenatal yoga can strengthen muscles and relieve discomfort.
• Side-lying rest positions relieve strain on the back and pelvis.
• Nurses should advise women to avoid high-impact activities late in pregnancy to prevent injury.
• Management of leg cramps includes stretching the calf muscle, adequate hydration, and calcium/magnesium intake.
• Carpal tunnel symptoms often resolve postpartum but may require splinting or activity modification during pregnancy.
Psychological Maternal Changes
The gestational period involves profound psychological transformations mediated by hormonal fluctuations, psychosocial stressors, and evolving self-concepts. Expectant mothers oscillate among feelings of ambivalence and acceptance, experience emotional lability, confront shifts in body image, and gradually develop a relationship with the fetus. Understanding these dynamics is essential for nurses to deliver holistic, empathetic, and evidence-based care. The following sections present a deeply scientific exploration of each psychological change, enriched with Nursing Insights and practical application.
1.1 Ambivalence
Ambivalence in early pregnancy refers to the coexistence of conflicting emotions toward the pregnancy, such as joy and anxiety, desire and fear, or acceptance and doubt.
- Definition and Mechanism
• Ambivalence occurs due to neuroendocrine adjustments (e.g., fluctuations in estrogen, progesterone, and oxytocin) interacting with the mother’s pre-existing psychological state, social expectations, and personal readiness.
• Full-scientific description: The expectant woman may concurrently experience positive anticipatory emotions and irrational fears stemming from adaptive physiological stress responses and psychological defense mechanisms. - Manifestations
• Verbal expressions of uncertainty (“I care about this baby, but I’m also terrified of what it means”).
• Somatic signs such as insomnia, mild anorexia, or tension headaches related to psychosomatic stress.
• Cognitive dissonance visible in oscillatory planning: both nesting behaviors and procrastination.
Nursing Insights
Expectant mothers commonly articulate ambivalence early in prenatal visits. It is crucial to actively listen without judgment, validate the complexity of their feelings, and normalize ambivalence as a common, adaptive psychological state. Use reflective statements such as, “It seems you both want and worry about this pregnancy—those feelings are very common.” These actions foster therapeutic rapport and resilience.
1.2 Acceptance
Acceptance describes the progression from uncertainty toward integration of the pregnancy into the mother’s identity and life narrative.
- Definition and Mechanism
• Biologically, stabilization of hormonal milieu (e.g., steady progesterone and estrogen levels) supports mood regulation and adaptation.
• Psychologically, cognitive restructuring helps the woman internalize fetal existence as part of herself and her future. - Manifestations
• Expressions such as “I feel a bond with my baby” or “I’m preparing for her arrival.”
• Initiating tangible preparations: prenatal care adherence, birth planning, discussing fetal sex.
• Emotional consistency and calm projection during consultations or daily life.
Nursing Insights
When a woman demonstrates acceptance, reinforce her adaptive coping by encouraging journaling, prenatal education engagement, and exploring her birth expectations. Acknowledge her evolving identity as a mother and facilitate continuity of care discussions—e.g., “I see how connected you feel—I can refer you to prenatal classes that support this positive adaptation.”
1.3 Emotional Lability
Emotional lability refers to rapid and intense fluctuations in mood, often incongruent with situational stimuli, due to hormonal and psychological volatility.
- Definition and Mechanism
• Hormonal surges, especially hCG, estrogen, and progesterone, can affect neurotransmitter pathways (e.g., serotonin, GABA) leading to affective dysregulation.
• Psychological factors such as fatigue, sleep disturbance, and stress amplify susceptibility to mood swings. - Manifestations
• Sudden crying during a routine conversation; abrupt shifts from laughter to tears.
• Irritability disproportionate to provocation.
• Difficulty concentrating or maintaining emotional equilibrium.
Nursing Insights
When faced with emotional lability, provide a calm, safe environment; use soothing tone; offer brief grounding techniques (e.g., guided deep breathing). Educate that these mood shifts are common and typically reflect endocrine changes, not personal weakness. Document mood patterns, and if extreme, consult mental health resources.
1.4 Body Image
Body image refers to the expectant mother’s perception, feelings, and attitudes toward her changing body.
- Definition and Mechanism
• Morphological changes—uterine enlargement, weight gain, skin changes—can challenge pre-existing body schema.
• Sociocultural ideals and personal self-esteem influence the internalized response. - Manifestations
• Expressions such as “I don’t recognize myself” or “I feel unattractive.”
• Preoccupation with weight gain or visible stretch marks.
• Avoidance of full-length mirrors, refusal of photos, or excessive clothing.
Nursing Insights
Validate feelings of body conflation and provide education on physiologic changes. Encourage positive self-talk, gentle exercise, and maternal support groups. Offer tailored reassurance: “Your body is nurturing life; each change has a purpose—and you’re doing beautifully.”
1.5 Relationship with Fetus
This subtopic describes how a woman develops emotional ties and maternal attachment to her unborn baby.
- Definition and Mechanism
• Through maternal-fetal attachment theory: initially cognitive (fantasy), then affective (feeling), culminating in behavioral (interaction).
• Influenced by fetal movements, ultrasound visualization, and psychosocial bonding rituals. - Manifestations
• Talking or singing to the fetus.
• Attending ultrasounds with evident maternal verbalization (“Look how strong you are”).
• Planning postnatal care with fondness (“I’ll brush your hair”, “I’m choosing your name”).
Nursing Insights
Encourage bond-building behaviors: “Noticing you speak to your baby, that’s a wonderful expression of attachment.” Recommend journaling or prenatal bonding rituals (e.g., playing music to fetus), which foster maternal identity and postnatal transition.
Summary
Pregnancy is a dynamic physiological state requiring adaptation across multiple systems to sustain the mother and the developing fetus.
• Cardiovascular: Increased blood volume (30–50%), cardiac output, and hypercoagulability. Decreased systemic vascular resistance and risk of supine hypotensive syndrome.
• Respiratory: Diaphragmatic elevation with increased tidal volume and minute ventilation, decreased PaCO₂ for fetal CO₂ clearance. Mild dyspnea is normal; sudden chest pain is not.
• Gastrointestinal: Progesterone-induced smooth muscle relaxation causes delayed gastric emptying, constipation, and reflux. Morning sickness is common in early pregnancy.
• Renal: Increased GFR and renal plasma flow lower serum creatinine. Urinary stasis increases UTI risk. Mild glycosuria can be normal; persistent glycosuria suggests gestational diabetes.
• Endocrine: Placental hormones regulate maternal adaptation—hCG maintains the corpus luteum, progesterone maintains pregnancy, estrogen promotes uterine growth, and hPL induces insulin resistance. The thyroid, adrenal, and pancreas adjust to meet maternal and fetal metabolic needs.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Physiological Maternal Changes
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


