Please set your exam date
Post-traumatic Stress Disorder
Study Questions
Practice Exercise 1
A recently discharged veteran reports symptoms of recurring intrusive thoughts, insomnia, and hypervigilance. Which mental health diagnosis would a nurse suspect for this client?
Explanation
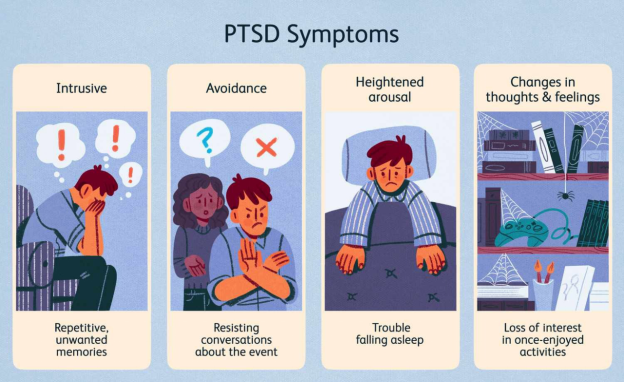
Posttraumatic stress disorderis a psychiatric condition triggered by exposure to actual or threatened death, serious injury, or sexual violence. It manifests through intrusive memories, hyperarousal, and avoidance behaviors. Symptoms must persist for over one month and cause significant distress or impairment. Individuals may experience flashbacks, nightmares, exaggerated startle responses, and emotional numbness. Sleep disturbances and hypervigilance are common. PTSD is more prevalent in populations exposed to combat, trauma, or violence, and often coexists with depression or substance use disorders.
Rationale for correct answers
2. Posttraumatic stress disorderinvolves persistent intrusive thoughts, insomnia, and hypervigilance following trauma. These symptoms reflect the DSM-5 criteria for PTSD, especially in veterans exposed to combat or life-threatening events.
Rationale for incorrect answers
1.Narcolepsy presents with sudden sleep attacks, cataplexy, and daytime sleepiness, not intrusive thoughts or hypervigilance. It is a neurological sleep disorder unrelated to trauma exposure.
3.Trichotillomania involves compulsive hair-pulling, often linked to tension relief or sensory gratification. It does not include hypervigilance or trauma-related intrusive thoughts.
4.Obsessive-compulsive disorder features obsessions and compulsions, such as repetitive checking or cleaning. While intrusive thoughts are present, they are not trauma-related and lack the hyperarousal seen in PTSD.
Take Home Points
- PTSD is characterized by trauma-related intrusive memories, avoidance, negative mood changes, and hyperarousal.
- It must be differentiated from OCD, which involves non-trauma-related obsessions and compulsions.
- Narcolepsy is a sleep disorder with cataplexy and sleep attacks, not psychiatric trauma symptoms.
- Trichotillomania is a body-focused repetitive behavior, distinct from trauma-related disorders.
A nurse is reviewing the treatment plan for a veteran of the war in Iraq who has been diagnosed with posttraumatic stress disorder (PTSD). Which of the following therapy regimens would most appropriately be ordered?
Explanation
Posttraumatic stress disorder (PTSD)is a chronic psychiatric condition triggered by exposure to traumatic events such as combat, assault, or disasters. It involves reexperiencing, hyperarousal, and avoidancesymptoms. First-line pharmacologic treatment includes SSRIslike paroxetine, which reduce intrusive thoughts and mood symptoms. Psychotherapy is essential, with group therapy offering peer support and normalization of trauma responses. Benzodiazepines like alprazolam and diazepam are discouraged due to dependency risks. Anticonvulsants like carbamazepine are not standard for PTSD unless comorbid conditions exist.
Rationale for correct answers
1. Paroxetine and group therapyis appropriate. Paroxetine, an SSRI, is FDA-approved for PTSD and reduces anxiety and depressive symptoms. Group therapy fosters shared experiences and emotional processing, enhancing recovery.
Rationale for incorrect answers
2.Diazepam is a benzodiazepine with high dependency risk and poor long-term efficacy in PTSD. Implosion therapy is rarely used and may worsen symptoms due to intense exposure.
3.Alprazolam is not recommended for PTSD due to tolerance and withdrawal risks. Behavior therapy alone lacks the trauma-focused component essential for PTSD recovery.
4.Carbamazepine is an anticonvulsant used for bipolar disorder and seizures, not PTSD. Cognitive therapy is effective, but carbamazepine has no role unless treating comorbid conditions.
Take Home Points
- SSRIs like paroxetine are first-line pharmacologic treatments for PTSD.
- Group therapy provides peer support and emotional validation in trauma recovery.
- Benzodiazepines are discouraged due to dependency and poor long-term outcomes.
- PTSD treatment should include trauma-focused psychotherapy, not general behavioral approaches.
Which of the following may be influential in the predisposition to posttraumatic stress disorder (PTSD)? Select all that apply.
Explanation
Posttraumatic stress disorder (PTSD)is a psychiatric condition triggered by exposure to traumatic events. It involves intrusive memories, hyperarousal, and negative mood alterations. Risk factors include early-life relational trauma, distorted cognition, and poor social support. Neurobiological changes include reduced hippocampal volume and altered serotoninand norepinephrine signaling. Severity of trauma and lack of support increase vulnerability. Elevated hemoglobin improves oxygen delivery but has no known influence on PTSD development or symptomatology.
Rationale for correct answers
1. Unsatisfactory parent–child relationshipPoor attachment disrupts emotional regulation and stress resilience, increasing PTSD risk through insecure coping and impaired trust development.
3. Distorted, negative cognitionsNegative beliefs about self and world maintain PTSD symptoms by reinforcing fear, guilt, and helplessness beyond the trauma.
4. Severity of the stressor and availability of support systemsGreater trauma intensity and lack of support impair recovery, increasing PTSD risk due to isolation and emotional dysregulation.
Rationale for incorrect answers
2.PTSD is associated with reduced serotonin activity, not excess. Elevated serotonin is not a recognized risk factor and may improve mood regulation.
5.Elevated hemoglobin improves oxygen delivery but has no established role in PTSD pathogenesis or emotional regulation mechanisms.
Take Home Points
- PTSD risk increases with severe trauma, poor support, and early relational disruptions.
- Distorted cognitions perpetuate PTSD symptoms and hinder recovery.
- Serotonin dysfunction contributes to emotional dysregulation but excess serotonin is not a risk factor.
- PTSD must be differentiated from acute stress disorder and depression, especially in early stages.
Practice Exercise 2
A nurse is caring for a veteran of the war in Iraq who is diagnosed with posttraumatic stress disorder (PTSD). He experiences a nightmare during his first night in the hospital and explains to the nurse that he was dreaming about gunfire all around and people being killed. The nurse’s most appropriate initial intervention is to:
Explanation
Posttraumatic stress disorder (PTSD)is a psychiatric condition triggered by exposure to traumatic events such as combat, assault, or disasters. It involves hyperarousal, nightmares, and flashbacks. Individuals may experience intense fear, helplessness, or horror during episodes. Nightmares are a hallmark symptom, often replicating the trauma. Immediate nursing care focuses on safety, grounding, and emotional stabilization. Pharmacologic interventions like benzodiazepines are not first-line due to dependency risks. Supportive presence and reassurance are essential during acute episodes.
Rationale for correct answers
3. Stay and reassureis the most appropriate initial response. Presence reduces isolation and fear, while reassurance helps reorient the patient to the present and promotes psychological safety.
Rationale for incorrect answers
1.Alprazolam is a benzodiazepine used for acute anxiety but not first-line for PTSD due to risk of dependence and masking symptoms.
2.Calling the physician is premature. The episode is expected in PTSD and does not require immediate medical escalation unless safety is compromised.
4.Relaxation tapes are useful in structured therapy, but not during acute distress. The patient needs grounding and human connection first.
Take Home Points
- PTSD nightmares require immediate grounding and reassurance, not pharmacologic sedation.
- Benzodiazepines are not first-line for PTSD due to dependency and limited efficacy.
- Nurse presence during flashbacks or nightmares promotes safety and emotional regulation.
- Differentiate PTSD from panic disorder and generalized anxiety by presence of trauma-linked reexperiencing.
Leon, a veteran of the war in Iraq, has been diagnosed with posttraumatic stress disorder (PTSD). He has been hospitalized after swallowing a handful of his anti-panic medication. His physical condition has been stabilized in the emergency department, and he has been admitted to the psychiatric unit. In developing his initial plan of care, which is the priority nursing diagnosis that the nurse selects for the client?
Explanation
Risk for suicideis the priority nursing diagnosis when a client with PTSD has engaged in a potentially lethal act such as ingesting a handful of medication. This diagnosis reflects immediate danger, requiring urgent intervention to ensure safetyand prevent recurrence. PTSD increases suicide risk due to hopelessness, emotional dysregulation, and intrusive trauma-related thoughts. Veterans are particularly vulnerable due to combat exposure, survivor guilt, and limited support systems. Suicide risk must be addressed before other psychosocial or cognitive concerns.
Rationale for correct answers
2. Risk for suicideThis diagnosis takes precedence due to the client’s recent overdose, indicating active suicidal intent and immediate threat to life.
Rationale for incorrect answers
1.Post-trauma syndrome is relevant but not the priority when the client has demonstrated suicidal behavior requiring immediate safety interventions.
3.Complicated grieving may be present but does not supersede the urgency of suicide risk following a self-harm attempt.
4.Disturbed thought processes may contribute to PTSD symptoms but are not the most critical concern when suicide risk is evident.
Take Home Points
- Suicide risk is the highest priority in clients with PTSD who engage in self-harm.
- PTSD increases vulnerability to suicide due to emotional dysregulation and trauma-related distress.
- Post-trauma syndrome and complicated grieving are important but secondary to immediate safety concerns.
- Nursing care must prioritize stabilization and suicide prevention before addressing long-term psychological recovery.
A newly admitted client diagnosed with posttraumatic stress disorder is exhibiting recurrent flashbacks, nightmares, sleep deprivation, and isolation from others. Which nursing diagnosis takes priority?
Explanation
Risk for injuryis a priority nursing diagnosis when a client’s physiological or psychological state places them in danger of harm. In posttraumatic stress disorder (PTSD), sustained hyperarousal leads to sleep deprivation, impaired concentration, and exhaustion. These symptoms compromise physical safety and increase vulnerability to accidents, self-harm, or aggression. Sleep disruption in PTSD is linked to elevated cortisol and norepinephrine levels, which impair restorative sleep and heighten reactivity. Clients may experience dissociation, impulsivity, or poor judgment, especially when fatigued, making injury risk a critical concern.
Rationale for correct answers
4. Risk for injuryis the priority because sleep deprivation from nightmares and hyperarousal leads to physical exhaustion and impaired cognition. This increases the likelihood of falls, accidents, or impulsive behaviors, making safety the most urgent concern.
Rationale for incorrect answers
1.Posttrauma syndrome is a valid diagnosis but not the priority. It addresses emotional and psychological symptoms, which are secondary to immediate safety risks posed by exhaustion.
2.Social isolation is relevant but not life-threatening. While it affects emotional well-being, it does not pose an immediate physical danger compared to injury risk from sleep deprivation.
3.Ineffective coping due to alcohol use is serious but not the most acute concern in this scenario. The stem emphasizes exhaustion and flashbacks, not substance abuse behaviors.
Take Home Points
- Risk for injury is prioritized when PTSD symptoms impair physical safety, especially due to sleep deprivation and hyperarousal.
- PTSD clients may experience dissociation, impulsivity, and poor judgment, increasing injury risk.
- Posttrauma syndrome addresses emotional trauma but is secondary to physiological safety needs.
- PTSD must be differentiated from depression and substance use disorders when prioritizing nursing diagnoses.
Comprehensive Questions
A client with posttraumatic stress disorder (PTSD) is preparing for a family meeting. The nurse who is working with the client should encourage him to share which topic with family members?
Explanation
Posttraumatic stress disorder (PTSD)is a psychiatric condition triggered by exposure to actual or threatened death, serious injury, or sexual violence. It is characterized by intrusive memories, avoidance behaviors, and negative alterations in mood and cognition. Emotional detachment, also known as emotional numbing, is a hallmark symptom that impairs interpersonal relationships and is often misunderstood by family members. It reflects the brain’s protective mechanism against overwhelming trauma and is associated with decreased activity in the ventromedial prefrontal cortex and increased amygdala reactivity.
Rationale for correct answers
3. Emotional detachmentis a core symptom of PTSD and often leads to strained family relationships. Encouraging the client to share this with family promotes understanding and reduces misinterpretation of the client’s behavior as rejection or indifference.
Rationale for incorrect answers
1.People-pleasing behaviors are not diagnostic or central to PTSD. While they may reflect coping mechanisms, they are not typically the focus of family education in trauma recovery.
2.Survivor guilt is a significant symptom of PTSD, but discussing medication use in a family meeting may shift focus from emotional processing to pharmacologic management, which is better addressed in clinical settings.
4.Hallucinations are not a core symptom of PTSD. If present, they may indicate a comorbid psychotic disorder or severe dissociation, requiring specialized psychiatric evaluation rather than family discussion.
Take Home Points
- PTSD includes emotional detachment, hyperarousal, intrusive memories, and avoidance; emotional numbing often disrupts family bonds.
- Survivor guilt is common in PTSD but should be addressed therapeutically before being shared in family settings.
- Hallucinations are not typical of PTSD and may suggest comorbid conditions like psychosis or dissociative disorders.
- Family education should focus on core PTSD symptoms to foster empathy, reduce stigma, and support recovery.
During the night, a 50-year-old Vietnam veteran with posttraumatic stress disorder (PTSD) awakens shaking and tells you that someone is trying to smother him. What is the appropriate response for the nurse in this situation?
Explanation
Posttraumatic stress disorder (PTSD)is a psychiatric condition triggered by exposure to traumatic events such as combat, assault, or disasters. It is characterized by hypervigilance, nightmares, and flashbacks, often disrupting sleep and emotional regulation. Individuals may experience dissociation, intrusive thoughts, and exaggerated startle responses. Sleep disturbances are common, with nightmares being a hallmark symptom. The therapeutic approach emphasizes safety, trust-building, and grounding techniques. Supportive presence and reassurance during episodes of disorientation or fear are critical to de-escalate arousal and reorient the patient to the present.
Rationale for correct answers
1.Therapeutic presence and grounding are essential in managing acute PTSD symptoms. Staying with the patient and offering reassurance helps reorient them to reality and reduces fear. This approach validates the patient’s experience without challenging their perception, which is crucial during dissociative or hyperaroused states.
Rationale for incorrect answers
2.This response delays emotional processing and invalidates the patient’s current distress. PTSD-related episodes require immediate support, not postponement, as avoidance can reinforce fear and isolation.
3.Minimizing the experience by labeling it “only a dream” dismisses the patient’s perception and may increase feelings of alienation. PTSD nightmares often feel real and threatening; invalidation can worsen symptoms.
4.Offering medication prematurely without addressing the emotional crisis overlooks the importance of therapeutic engagement. Medication may be appropriate later, but immediate grounding and presence are the priority in acute episodes.
Take Home Points
- PTSD nightmares can trigger intense fear and disorientation; grounding and presence are first-line responses.
- Avoid minimizing or postponing emotional support during acute PTSD episodes.
- Therapeutic engagement should precede pharmacologic intervention in crisis moments.
- PTSD must be differentiated from other disorders with sleep disturbances, such as panic disorder or schizophrenia.
A school nurse is planning a school-based intervention program for children who lost their homes due to a tornado and are now residing in temporary housing. With which group should the nurse initially focus the intervention program because they are more likely to experience symptoms of mental health distress?
Explanation
Natural disasters like tornadoes can trigger significant psychological distressin children, often manifesting as post-traumatic stress, anxiety, or depression. Younger children, particularly those from lower socioeconomic backgrounds, face heightened vulnerability due to limited coping mechanisms and resource scarcity. Females may exhibit higher rates of internalizing symptoms, with prevalence of post-traumatic stress disorder ranging from 19.2% to 24.4% post-disaster. Social support significantly mitigates distress, while unstable housing exacerbates it.
Rationale for Correct Answers
3.Younger females from lower socioeconomicbackgrounds are more likely to experience mental healthdistress due to limited coping skills, higher sensitivity to trauma, and fewer resources in temporary housing, amplifying post-disaster stress.
Rationale for Incorrect Answers
1.Older females from higher socioeconomic backgrounds have better access to resources and more developed coping mechanisms, reducing their likelihood of severe mental health distress compared to younger, resource-scarce groups.
2.Older males from higher socioeconomic backgrounds are less vulnerable due to age-related resilience and resource availability, making them less likely to experience significant post-disaster mental health issues.
4.Younger males from lower socioeconomic backgrounds face risks due to age and resource scarcity, but males typically show lower rates of internalizing disorders like anxiety and depression compared to females.
Take Home Points
- Younger children are more vulnerable to mental health distress post-disaster due to limited coping skills.
- Females tend to exhibit higher rates of internalizing symptoms like post-traumatic stress and anxiety.
- Lower socioeconomic status exacerbates distress due to limited access to resources and support.
- Interventions should prioritize trauma-focused cognitive behavioral therapy and social support to mitigate distress.
A nurse is assessing a veteran of the war in Iraq who has been diagnosed with posttraumatic stress disorder (PTSD). He states, “I can’t figure out why God took my buddy instead of me.” From this statement, the nurse should recognize that the client is most likely experiencing which of the following?
Explanation
Survivor’s guiltis a psychological response to surviving a traumatic event in which others died. It is commonly seen in combat veterans, accident survivors, and disaster victims. Individuals may experience persistent feelings of guilt, questioning why they lived while others perished. This guilt often manifests as emotional distress, self-blame, and existential questioning. It is considered a cognitive/mood symptomof posttraumatic stress disorder and may coexist with depression, anxiety, or spiritual distress. Symptoms include rumination, impaired sleep, and difficulty finding meaning in survival.
Rationale for correct answers
2. Survivor’s guiltarises when individuals feel undeserving of survival after others have died. The veteran’s statement reflects existential questioning and emotional pain typical of this condition.
Rationale for incorrect answers
1.Repressed anger involves internalized hostility often leading to depression or passive-aggressive behavior. The veteran’s statement shows sorrow and guilt, not suppressed rage.
3.Intrusive thoughts are unwanted, distressing mental images or ideas, often linked to PTSD or OCD. The veteran’s reflection is deliberate and emotional, not involuntary or obsessive.
4.Spiritual distress involves loss of faith, meaning, or connection with a higher power. While the statement touches on existential themes, the dominant emotion is guilt over survival, not spiritual disconnection.
Take Home Points
- Survivor’s guilt is a common symptom of PTSD, especially in combat veterans.
- It involves emotional pain, self-blame, and questioning the fairness of survival.
- Differentiate from spiritual distress, which centers on loss of meaning or faith.
- Repressed anger and intrusive thoughts have distinct psychological profiles and symptom patterns.
A nurse is caring for a veteran of the war in Iraq who has been diagnosed with posttraumatic stress disorder (PTSD). The client, now receiving care at a VA outpatient clinic, reports experiencing panic attacks. Which of the following medications may be prescribed for the client to treat panic attacks?
Explanation
Panic attacks in PTSDare sudden episodes of intense fear accompanied by physical symptoms such as chest pain, palpitations, and shortness of breath. They result from hyperactivationof the amygdala, leading to exaggerated fear responses. Benzodiazepines like alprazolamact rapidly by enhancing GABAergic inhibition, reducing neuronal excitability and calming acute panic symptoms. However, they are recommended only for short-term use due to risks of dependence, tolerance, and interference with trauma processing.
Rationale for correct answers
1. AlprazolamAlprazolam is a fast-acting benzodiazepine that enhances GABA activity, reducing acute panic symptoms and promoting rapid anxiolysis.
Rationale for incorrect answers
2.Lithium is a mood stabilizer used primarily for bipolar disorder. It is not indicated for acute panic attacks and may take weeks to show effect.
3.Carbamazepine is an anticonvulsant and mood stabilizer used in bipolar disorder. It is not effective for treating panic attacks and has delayed onset.
4.Haldol (haloperidol) is a typical antipsychotic used for schizophrenia and agitation. It does not treat panic attacks and may worsen anxiety symptoms.
Take Home Points
- Alprazolam is effective for short-term relief of panic attacks due to its rapid GABAergic action.
- Benzodiazepines should be used cautiously in PTSD due to risk of dependence and interference with therapy.
- Lithium and carbamazepine are mood stabilizers, not first-line agents for panic symptoms.
- Haldol is reserved for psychotic symptoms and is not appropriate for panic or anxiety management.
When teaching a 6-year-old child with sickle cell disease and his family about pain management, which of the following should the nurse discuss? Select all that apply
Explanation
Pain management in sickle cell disease (SCD) is multimodal, involving medications, nonpharmacologic measures, and individualized care planning. Education for children and families emphasizes realistic expectations, self-advocacy tools like “passport cards,” and the collaborative nature of care decisions.
Rationale for correct answers:
B. Nonpharmacologic strategies complement medication therapy, help manage mild pain episodes, and promote relaxation and coping.
C. A sickle cell “passport” helps ensure consistent, timely, and informed care across healthcare settings, reducing delays in treatment.
E. Chronic pain management in SCD requires careful evaluation of medication type, dosing, side effects, tolerance, and the impact on daily functioning.
Rationale for incorrect answers:
A. Even with optimal therapy, pain may not be completely eliminated; the goal is to reduce intensity and improve function.
D. Pain management is a team approach, involving the patient, family, nurses, physicians, and other allied health professionals.
Take home points
- Sickle cell pain management combines pharmacologic and nonpharmacologic approaches.
- Pain passports improve communication and ensure faster, safer treatment.
- Complete elimination of pain is often not realistic — focus on control and quality of life.
- Management is collaborative, not physician-only.
How can the nurse prepare a child for a painful procedure? Select all that apply
Explanation
Preparing a child for a painful procedure involves honest communication, active coping strategies, and family involvement. Using age-appropriate explanations, distraction, positive self-talk, and guided imagery helps reduce anxiety and improves cooperation.
Rationale for correct answers:
A. Honesty builds trust and prevents loss of credibility. Use simple, accurate terms appropriate for the child’s developmental level.
B. Distraction helps shift the child’s focus away from the procedure, reducing anxiety and perceived pain.
D. Use of positive self-talk such as “When I go home, I will feel better and be able to see my friends” encourages coping and provides a sense of control and hope.
E. Use of guided imagery that involves recalling a previous pleasurable event can calm the child, decrease muscle tension, and promote relaxation during procedures.
Rationale for incorrect answers:
C. Parents are often a source of comfort and security; their presence can reduce the child’s fear. They should be given the choice to stay, rather than being asked to leave automatically.
Take home points
- Honest, age-appropriate communication fosters trust.
- Distraction, guided imagery, and positive self-talk are effective coping strategies for children.
- Parents should generally be encouraged to stay if it comforts the child.
- Preparation should be collaborative, supportive, and empowering for the child.
A nurse is caring for a client who is a veteran of the war in Iraq and has been diagnosed with posttraumatic stress disorder (PTSD). The client has been hospitalized on the psychiatric unit following an attempted suicide. In the middle of the night, the client wakes up yelling and tells the nurse he was having a flashback to when his unit transport drove over an improvised explosive device (IED) and most of his fellow soldiers were killed. He is breathing heavily, perspiring, and his heart is pounding. The nurse’s initial intervention is which of the following?
Explanation
Posttraumatic stress disorder (PTSD)is a psychiatric condition triggered by exposure to traumatic events such as combat, assault, or disasters. It involves intrusive memories, hyperarousal, and avoidance behaviors. Flashbacks are dissociative episodes where the individual re-experiences the trauma, often with intense autonomic symptoms like tachycardia and diaphoresis. During these episodes, grounding techniques and reassurance are essential. Immediate pharmacologic intervention is not first-line unless symptoms escalate or become psychotic. Safety and therapeutic presence are prioritized.
Rationale for correct answers
3. Stay and reassureThis is the most appropriate initial intervention during a flashback. The nurse’s presence provides psychological safetyand helps reorient the client to the present. Reassurance reduces autonomic arousal and prevents escalation.
Rationale for incorrect answers
1.Contacting the doctor is not the initial step. The nurse must first assess and stabilize the client. Reporting can follow once the client is calm and safe.
2.Chlorpromazine is an antipsychotic, not indicated for acute flashbacks unless psychosis is present. It may sedate but does not address the underlying dissociation or fear.
4.Having the client sit outside the nurses’ station may feel isolating and lacks therapeutic engagement. It does not provide the grounding or reassurance needed during a flashback.
Take Home Points
- PTSD flashbacks require immediate grounding and reassurance, not isolation or sedation.
- Chlorpromazine is not first-line for PTSD flashbacks; SSRIs and trauma-focused therapy are preferred.
- Nurse presence and verbal reassurance are critical during dissociative episodes.
- PTSD must be differentiated from panic disorder and acute stress reaction based on duration and symptom clusters.
A client diagnosed with posttraumatic stress disorder has a nursing diagnosis of disturbed sleep patterns related to nightmares. Which evaluation would indicate that the stated nursing diagnosis was resolved? Select all that apply.
Explanation
Posttraumatic stress disorder (PTSD)PTSD is a psychiatric condition triggered by exposure to traumatic events, leading to intrusive symptoms such as nightmares, hyperarousal, and avoidance. Sleep disturbances are common, with nightmares affecting REM sleep and contributing to daytime fatigueand impaired cognition. Effective management includes trauma-focused therapy, sleep hygiene, and medications like trazodone, which is often used off-label for insomnia in PTSD. Resolution is indicated by restored sleep architecture, improved daytime functioning, and reduced nightmare frequency.
Rationale for correct answers
3.Feeling rested and denying nightmares indicates restorative sleepand reduced trauma-related intrusions, confirming resolution of disturbed sleep patterns.
4.Avoiding daytime naps supports sleep hygiene, promoting consolidated nighttime sleep and reducing sleep fragmentation.
5.Improved concentration reflects enhanced cognitive functiondue to better sleep quality, suggesting resolution of sleep disturbance.
Rationale for incorrect answers
1.Expressing feelings about nightmares shows emotional processing but does not confirm resolution of sleep disturbance or improved sleep quality.
2.Requesting PRN trazodone suggests ongoing sleep difficulty, indicating the problem persists and the nursing diagnosis remains unresolved.
Take Home Points
- PTSD-related sleep disturbances often manifest as nightmares and fragmented sleep, impairing daytime functioning.
- Resolution is best assessed through subjective sleep quality and objective improvements in cognition and mood.
- Trazodone is commonly used for sleep in PTSD but ongoing use may indicate unresolved symptoms.
- Differentiating PTSD from acute stress disorder involves symptom duration and functional impairment.
A construction worker is on duty when a nearly completed wall suddenly falls, crushing a number of co-workers. Although badly shaken initially, the client seemed to be coping well. About two weeks after the tragedy, the client begins to experience tremors, nightmares, and periods during which he feels numb or detached from his environment. He finds himself frequently thinking about the tragedy and feeling guilty that he was spared while many others died. Which statement about this situation is most accurate?
Explanation
Acute stress disorder (ASD)is a trauma-related condition that occurs within 3 days to 1 monthafter exposure to a traumatic event. It includes symptoms such as dissociation, intrusive memories, and hyperarousal. Individuals may experience emotional numbing, nightmares, and guilt. ASD differs from PTSD in duration and symptom persistence. Early pharmacologic treatment may include benzodiazepinesor SSRIsto manage anxiety and sleep disturbances. Psychotherapy, especially cognitive-behavioral therapy, is also effective in reducing progression to PTSD.
Rationale for correct answers
1. Acute stress disorderThe client’s symptoms began within two weeks of the trauma and include dissociation, nightmares, and guilt, consistent with ASD. Antianxiety medications such as benzodiazepinesor SSRIs may help reduce hyperarousal and facilitate sleep and emotional regulation.
Rationale for incorrect answers
2.PTSD requires symptoms to persist for more than one month. This client’s symptoms began within two weeks, which is too early for a PTSD diagnosis.
3.While anxiety and grief are present, the client’s dissociation and nightmares exceed normal grief reactions and meet criteria for ASD, requiring intervention.
4.The symptoms described—numbness, guilt, and nightmares—are not consistent with mild anxiety or normal grief alone. Lack of intervention risks progression to PTSD.
Take Home Points
- Acute stress disorder occurs within 3 days to 1 month after trauma and includes dissociation, nightmares, and hyperarousal.
- ASD must be differentiated from PTSD, which requires symptoms lasting longer than one month.
- Early treatment with SSRIs or benzodiazepines may reduce symptom severity and prevent progression to PTSD.
- ASD includes emotional numbing and guilt, which are more severe than typical grief reactions.
In which situation would benzodiazepines be prescribed appropriately?
Explanation
Benzodiazepinesare central nervous system depressants that enhance GABAactivity, producing anxiolytic, sedative, and muscle-relaxant effects. They are indicated for short-termmanagement of acute anxiety, alcohol withdrawal, and procedural sedation. Long-term use is discouraged due to risks of dependence, tolerance, and cognitive impairment. They are not first-line for chronic psychiatric conditions like PTSD or bipolar disorder. In alcohol withdrawal, long-acting agents like diazepam are preferred. For preoperative sedation, short-acting agents like midazolam are used. Benzodiazepines are contraindicated in chronic use for PTSD and essential hypertension.
Rationale for correct answers
2. Short-term treatmentBenzodiazepines are appropriate for generalized anxiety disorder, alcohol withdrawal, and preoperative sedationwhen used short-term. Their rapid onset and calming effects make them suitable for acute symptom relief in these conditions.
Rationale for incorrect answers
1.Long-term use in PTSD is contraindicated due to risk of worsening symptoms and dependence. Alcohol withdrawal requires short-term use only, and convulsive disorders are better managed with antiepileptics.
3.Benzodiazepines are not indicated for essential hypertension. OCD is treated with SSRIs and CBT. Muscle spasms may be treated with benzodiazepines, but not in this combination.
4.Long-term use for panic disorder and bipolar mania is discouraged due to addiction risk. Alcohol dependence requires abstinence strategies, not benzodiazepines.
Take Home Points
- Benzodiazepines are appropriate for short-term use in anxiety, alcohol withdrawal, and procedural sedation.
- Long-term use increases risk of dependence, tolerance, and cognitive impairment.
- PTSD and bipolar disorder are not treated with benzodiazepines as first-line therapy.
- Essential hypertension and OCD require different pharmacologic approaches.
A client diagnosed with posttraumatic stress disorder is close to discharge. Which client statement would indicate that teaching about the psychosocial cause of posttraumatic stress disorder was effective?
Explanation
Posttraumatic stress disorder (PTSD)PTSD is a psychiatric condition triggered by exposure to actual or threatened death, serious injury, or sexual violence. It involves persistent re-experiencing of the trauma, avoidance of reminders, negative alterations in cognition and mood, and hyperarousal. Psychosocial factorssuch as coping style, personality traits, and social supportsignificantly influence symptom severity and recovery. The disorder is diagnosed when symptoms persist for more than one month and cause functional impairment. Treatment includes trauma-focused cognitive behavioral therapy and pharmacotherapy with SSRIs.
Rationale for correct answers
1. Psychosocial understandingThis statement reflects accurate insight into the psychosocial model of PTSD, which emphasizes the role of the traumatic event, individual coping mechanisms, and the availability of a support systemin influencing disease progression.
Rationale for incorrect answers
2.Avoidance is a behavioral response and part of the symptom cluster of PTSD, not a psychosocial cause. It reflects maladaptive coping rather than understanding of etiology.
3.Natural opioid release during trauma is a biological response. While it may contribute to dissociation, it does not explain the psychosocial origin of PTSD.
4.Negative worldview and hopelessness are cognitive distortions common in PTSD but represent psychological consequences, not the psychosocial cause of the disorder.
Take Home Points
- PTSD arises from trauma exposure and is influenced by coping style and social support.
- Psychosocial models focus on how individuals process trauma and the role of interpersonal resources.
- Avoidance behaviors and cognitive distortions are symptoms, not causes, of PTSD.
- Differentiating psychosocial, biological, and cognitive models is essential for accurate patient education.
A client diagnosed with posttraumatic stress disorder states to the nurse, “All those wonderful people died, and yet I was allowed to live.” Which experience is the client most likely demonstrating?
Explanation
Posttraumatic stress disorder (PTSD)is a psychiatric condition triggered by exposure to actual or threatened death, serious injury, or sexual violence. It manifests through intrusive memories, hyperarousal, and avoidance behaviors. A subset of individuals with PTSD experience survivor’s guilt, where they feel unworthy of survival and blame themselves for others’ deaths. This guilt can intensify symptoms and impair recovery. Emotional numbness, self-blame, and persistent sadness are common. Up to 90% of trauma survivors report some form of guilt, especially when others perished in the same event.
Rationale for correct answers
4. Survivor’s guiltis evident when the client expresses distress over surviving while others died. This reflects internalized blame and emotional conflict, hallmark featuresof survivor’s guilt in PTSD.
Rationale for incorrect answers
1.Denial involves refusal to accept reality or facts, often seen early in grief. The client is acknowledging the deaths and their survival, not denying them.
2.Social isolation is characterized by withdrawal from others and lack of interaction. The client’s statement reflects emotional turmoil, not behavioral withdrawal.
3.Anger in PTSD may be directed outward or inward, but the client’s tone suggests sorrow and guilt, not irritability or rage.
Take Home Points
- Survivor’s guilt is a common and distressing symptom in PTSD, especially after mass casualty events.
- It involves self-blame, feelings of unworthiness, and intrusive thoughts about the traumatic event.
- Differentiating survivor’s guilt from depression, anger, or denial is essential for targeted interventions.
- Treatment includes trauma-focused therapy, cognitive restructuring, and addressing maladaptive guilt.
Which of the following would the nurse expect to assess in a client diagnosed with posttraumatic stress disorder? Select all that apply.
Explanation
Posttraumatic stress disorder (PTSD)PTSD is a psychiatric condition triggered by exposure to actual or threatened death, serious injury, or sexual violence. It involves intrusive symptoms, avoidance behaviors, and negative alterations in mood. Dissociative events such as depersonalization and derealization may occur, especially in the dissociative subtype. Intense emotional responses like fear and helplessness are common during re-experiencing episodes. Avoidance of trauma-related stimuli—activities, places, or conversations—is a core diagnostic criterion. A full range of affect is typically absent; instead, emotional numbing and restricted affect are common.
Rationale for correct answers
1. Dissociative eventsClients with PTSD may experience depersonalizationor derealization, especially in the dissociative subtype. These episodes reflect altered consciousness and detachment from reality.
2. Intense fear and helplessnessThese are hallmark emotional responses during trauma re-experiencing. They reflect activation of the sympathetic nervous systemand are central to PTSD diagnosis.
5. Avoidance of trauma-related activitiesAvoidance is a core symptom cluster in PTSD. Clients may avoid activities, places, or conversations that trigger traumatic memories to reduce distress.
Rationale for incorrect answers
3.Excessive attachment and dependence are not typical features of PTSD. PTSD is more often associated with emotional withdrawal and detachment from others.
4.Clients with PTSD often exhibit restricted affect, emotional numbing, and inability to experience positive emotions. A full range of affect is not commonly present.
Take Home Points
- PTSD includes dissociative symptoms like depersonalization and derealization in some subtypes.
- Intense fear and helplessness are common during trauma re-experiencing episodes.
- Avoidance of trauma-related stimuli is a diagnostic criterion and impairs daily functioning.
- PTSD is marked by restricted affect, not a full emotional range.
When treating individuals with posttraumatic stress disorder, which variables are included in the recovery environment?
Explanation
Posttraumatic stress disorder (PTSD)PTSD recovery is influenced not only by the trauma itself but also by the recovery environment, which includes psychological resilience, social context, and interpersonal support. Among these, social supportsplay a critical role in buffering stress, enhancing coping, and improving treatment outcomes. Support from family, peers, and community fosters emotional regulation and reduces isolation. The presence of a cohesive and protective support system is consistently associated with better prognosis and reduced symptom severity. Recovery is less dependent on the trauma’s characteristics and more on post-trauma adaptation.
Rationale for correct answers
2. Social supportsAvailability of social supportsis a key variable in the recovery environment. Supportive relationships enhance emotional stability, reduce isolation, and promote engagement in treatment, improving long-term outcomes.
Rationale for incorrect answers
1.Ego strength is an internal psychological trait, not an environmental variable. While it affects coping, it is not part of the recovery environment.
3.Severity and duration of the stressor are characteristics of the trauma itself, not the recovery environment. They influence risk but are not modifiable environmental factors.
4.Control over reoccurrence relates to perceived safety and future risk, but it is not a consistent or direct component of the recovery environment.
Take Home Points
- Social support is a central environmental factor influencing PTSD recovery and resilience.
- Recovery environment includes interpersonal and societal influences, not internal traits or trauma characteristics.
- Ego strength and trauma severity affect vulnerability but are not part of the recovery environment.
- Enhancing social connectedness improves emotional regulation and treatment engagement in PTSD.
A newly admitted client is diagnosed with posttraumatic stress disorder. Which behavioral symptom would the nurse expect to assess? Select all that apply.
Explanation
Posttraumatic stress disorder (PTSD)is a psychiatric condition triggered by exposure to traumatic events such as violence, disasters, or abuse. It manifests through intrusive memories, avoidance behaviors, and negative mood alterations. Symptoms must persist for over one month and cause functional impairment. Behavioral signs include flashbacks, emotional numbing, hypervigilance, and detachment. DSM-5 criteria require at least one intrusion symptom, one avoidance symptom, two cognition/mood symptoms, and two arousal/reactivity symptoms.
Rationale for correct answers
1. Recurrent flashbacksare a hallmark of PTSD’s intrusion symptoms. These vivid, distressing recollections often feel like reliving the trauma and are triggered by sensory cues or internal thoughts.
3. Diminished participationin significant activities reflects negative alterations in mood and cognition. It indicates emotional numbing and loss of interest in previously enjoyed experiences, common in PTSD.
4. Detachment from othersis a behavioral symptom tied to emotional numbing and estrangement. It arises from avoidance and altered mood, impairing interpersonal relationships and social functioning.
Rationale for incorrect answers
2.Intense fear, helplessness, and horror are emotional responses during the traumatic event, not behavioral symptoms assessed after diagnosis. DSM-5 removed this as a diagnostic criterion.
5.While some individuals with PTSD may exhibit reckless or self-destructive behaviors (which could be seen as impulsive), hyperactivity is not a core symptom. It is sometimes seen in children with PTSD and can be confused with other disorders like ADHD.
Take Home Points
- PTSD behavioral symptoms include flashbacks, emotional numbing, and social withdrawal.
- DSM-5 criteria emphasize persistent symptoms across intrusion, avoidance, mood, and arousal domains.
- PTSD must be differentiated from acute stress disorder, which lasts less than one month.
- Emotional detachment and diminished interest are key indicators of PTSD-related mood alterations.
The nurse teaches an anxious client diagnosed with posttraumatic stress disorder a breathing technique. Which action by the client would indicate that the teaching was successful?
Explanation
Posttraumatic Stress Disorder (PTSD)is a psychiatric condition triggered by exposure to traumatic events such as violence, disasters, or abuse. It manifests through hyperarousal, intrusive memories, and avoidance behaviors. Individuals often experience escalating anxiety, flashbacks, and physiological dysregulation. Breathing techniques like diaphragmatic breathing and SKY Breath Meditation help modulate the autonomic nervous system, reduce cortisol levels, and activate the parasympathetic response, thereby lowering anxiety intensity and improving emotional regulation.
Rationale for correct answers
3.Recognizing signs of escalating anxiety reflects self-awarenessand emotional regulation, which are key outcomes of successful breathing technique training. This ability allows the client to intervene early using the technique before anxiety intensifies.
Rationale for incorrect answers
1.Anxiety cannot be completely eliminated; the goal of breathing techniques is to reduce intensity and improve coping, not eradicate the emotion.
2.Performing ADLs independently may reflect functional improvement but does not directly indicate mastery of a breathing technique or its use in anxiety regulation.
4.Maintaining a 3/10 anxiety level without medication is desirable, but it lacks specificity. It does not confirm the client is using the breathing technique effectively or consistently to manage anxiety.
Take Home Points
- PTSD involves dysregulation of the autonomic nervous system, often leading to chronic hyperarousal and anxiety.
- Breathing techniques activate the parasympathetic system, reducing cortisol and promoting calm.
- Successful use of breathing techniques is evidenced by early recognition and management of escalating anxiety.
PTSD must be differentiated from panic disorder and generalized anxiety disorder, which have different triggers and symptom profiles.
Exams on Post-traumatic Stress Disorder
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
- Define post-traumatic stress disorder (PTSD) and its core symptom clusters.
- Review the DSM-5 diagnostic criteria for PTSD and differentiate it from acute stress reactions.
- Identify common traumatic stressors, risk factors, and populations at risk for PTSD.
- Outline a systematic nursing assessment for a patient with PTSD, including subjective and objective findings.
- Describe evidence-based nursing interventions, including pharmacologic and nonpharmacologic therapies, for managing PTSD.
- Emphasize the nurse’s role in patient education, prevention of complications, and coordination of mental health resources.
Introduction
- Post-traumatic stress disorder (PTSD) is a severe, chronic anxiety disorder that develops after exposure to traumatic events.
- It occurs after direct experience of trauma or witnessing it. Common precipitating events include combat exposure, physical or sexual assault, serious accidents, and natural or man-made disasters.
- The disorder is characterized by persistent, intrusive memories or flashbacks of the trauma, nightmares, avoidance of trauma reminders, hypervigilance, and other re-experiencing symptoms.
- These symptoms typically begin within weeks of the trauma but can emerge later. Symptoms must persist for at least one month to meet PTSD criteria, distinguishing it from acute stress disorder.
- PTSD can affect people of any age, but it is about twice as common in women as men. Early recognition and intervention are critical to prevent chronic dysfunction.
Nursing Insight:
- Nurses should remember that PTSD can result from many types of trauma, including medical and obstetric events. For example, complicated childbirth or severe postpartum complications are known risk factors for PTSD (peripartum maternal morbidity).
- Awareness of high-risk patients (e.g., veterans, abuse survivors, critical care patients, and new mothers after a traumatic birth) helps ensure timely screening and support.
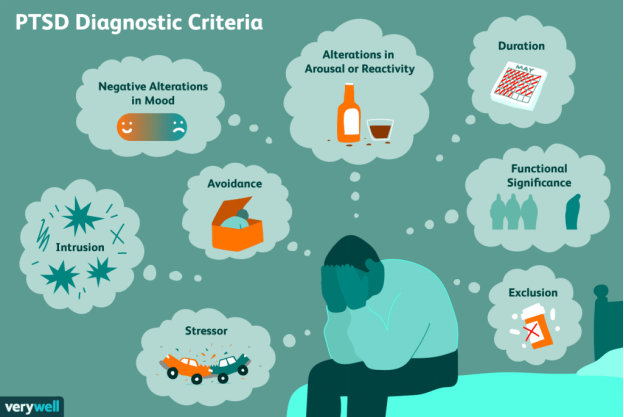
Diagnosis
PTSD is diagnosed using DSM-5 criteria. Nurses should know these criteria to assist in assessment and documentation. Criteria include:
- Criterion A (Stressor Exposure): The patient experienced, witnessed, or was confronted with an event involving actual or threatened death, serious injury, or sexual violence.
- Criterion B (Intrusion): Recurrent, involuntary, and intrusive distressing memories of the event, such as nightmares, flashbacks, or intense distress at exposure to reminders.
- Criterion C (Avoidance): Persistent avoidance of stimuli associated with the trauma (e.g., avoiding thoughts, conversations, or external reminders that trigger distress).
- Criterion D (Negative Alterations in Cognition/Mood): Negative beliefs about oneself or the world, distorted blame of self or others, persistent negative emotional state (fear, guilt, shame), diminished interest in activities, and feelings of detachment or estrangement.
- Criterion E (Arousal/Reactivity): Marked alterations in arousal and reactivity, such as irritability or angry outbursts, reckless or self-destructive behavior, hypervigilance, exaggerated startle response, difficulty concentrating, or sleep disturbance.
- Criterion F (Duration): Symptoms from Criteria B, C, D, and E last more than one month.
- Criterion G (Impairment): The symptoms cause significant distress or impairment in social, occupational, or other important areas of functioning.
- Criterion H (Exclusion): The symptoms are not due to the physiological effects of a substance or another medical condition.
If all criteria are met, a PTSD diagnosis is confirmed. Symptoms lasting less than one month would indicate Acute Stress Disorder instead. Delayed onset PTSD can occur months after the trauma.
Key signs and symptoms
• Anxiety
• Flashbacks of the traumatic experience
• Nightmares about the traumatic experience
• Poor impulse control
• Social isolation
• Survivor guilt

Nursing Insight:
- Use a sensitive, patient-centered interview to uncover trauma history and symptoms. Patients may minimize or avoid details of the trauma.
- Employ PTSD screening tools (e.g., the PTSD Checklist for DSM-5, PCL-5) to clarify symptom presence.
- Always assess for comorbid depression, substance use, or suicidality, which commonly accompany PTSD.
Stressors
Understanding the precipitating stressors is essential in PTSD care. Key points:
- Types of Traumatic Events: Includes personal threat (assault, abuse), combat or military exposure, serious accidents, witnessing severe injury or death, natural disasters (earthquakes, floods), and terror acts.
- Chronic and Repeated Trauma: Prolonged abuse (domestic violence, torture) or multiple traumatic exposures can result in complex PTSD.
- Occupational Exposure: First responders, soldiers, and emergency care providers may develop PTSD from repeated trauma exposure.
- Medical and Obstetric Stressors: Severe illnesses, ICU stays, or invasive procedures; traumatic childbirth (e.g., emergent cesarean, obstetric hemorrhage) can trigger PTSD symptoms in patients and postpartum mothers.
- Risk Factors: Female sex, history of previous trauma or mental illness, lack of social support, and the severity or unexpected nature of the event increase risk.
Nursing Insight:
- Thoroughly explore the patient’s trauma history. Even events not traditionally considered “life-threatening” (such as loss of a child or severe illness) may be traumatic to the individual. Identifying stressors and risk factors helps the nurse anticipate PTSD and provide early interventions.
Assessment
A comprehensive nursing assessment for PTSD includes:
- Subjective Data: Patient reports may include:
- Recurring intrusive thoughts, flashbacks, or nightmares of the trauma.
- Avoidance of reminders (avoiding discussions, places, or people related to the trauma).
- Feelings of detachment or emotional numbness.
- Persistent negative thoughts or beliefs (e.g., “I am unsafe,” “I did something terrible”) and intense guilt or shame.
- Hyperarousal (feeling “on edge”), irritability, or angry outbursts.
- Sleep disturbances (insomnia, nightmares) and concentration difficulties.
- Changes in behavior, such as new or increased substance use to cope.
- Objective Data: Observation and objective signs may include:
- Startle responses, scanning environment for danger, or excessive alertness.
- Blunted affect or visible tension when discussing the trauma.
- Physical signs of anxiety (tachycardia, sweating) during the interview.
- Evidence of self-harm (scars, wounds) or disordered self-care.
- Signs of comorbid conditions (depressive affect, poor hygiene, or intoxication).
- Note vital signs and consider medical workup to rule out other causes of symptoms (e.g., thyroid dysfunction).
- Screening Tools: Use standardized instruments like the PCL-5 to assess symptom severity. Screen also for comorbid depression, anxiety, and suicidal ideation.
ASSESSMENT FINDINGS
- Anger
- Anxiety
- Apathy
- Avoidance of people involved in the trauma
- Avoidance of places where the trauma occurred
- Chronic tension
- Detachment
- Difficulty concentrating
- Difficulty falling or staying asleep
- Emotional numbness
- Flashbacks of the traumatic experience
- Hyper alertness
- Inability to recall details of the traumatic event
- Labile affect
- Nightmares about the traumatic experience
- Poor impulse control
- Social isolation
- Survivor guilt
Nursing Insight:
- Always assess patient safety. PTSD patients may have increased suicide risk or self-harm behaviors, especially if they feel hopeless or trapped.
- Ensure that any risk of self-harm is addressed immediately, and help create a safety plan if needed.
Interventions
Nursing interventions for PTSD focus on safety, symptom management, and coping. These include:
Key interventions
• Help the client to identify stressors.
• Provide for client safety.
• Encourage the client to explore the traumatic event and the meaning of the event.
• Assist the client with problem solving and resolving guilt.
- Safety and Trust: Establish a stable, reassuring environment. Build rapport through empathetic communication; listen actively and calmly. Maintain patient confidentiality and a nonjudgmental stance. Ensure the physical setting minimizes anxiety (e.g., quiet, private room).
- Psychoeducation: Teach the patient (and family) about PTSD. Explain that symptoms are common responses to trauma, not a sign of weakness. Provide information on symptom patterns and reassure that recovery is possible.
- Coping Skills: Instruct on relaxation techniques (deep breathing, progressive muscle relaxation, guided imagery) to reduce anxiety. Encourage structured daily routines, balanced nutrition, and regular sleep. Identify positive coping mechanisms and encourage their use (e.g., exercise, hobbies, social support).
- Drug therapy: Benzodiazepines: alprazolam (Xanax),lorazepam (Ativan), clonazepam (Klonopin), Beta-adrenergic blocker: propranolol(Inderal), MAOIs: phenelzine (Nardil), tranylcypromine(Parnate), SSRIs: fluoxetine (Prozac), paroxetine(Paxil), sertraline (Zoloft), TCAs: imipramine (Tofranil), amitriptyline(Elavil)
- Encourage Expression: Support the patient in expressing feelings about the trauma when ready. This may be through talking with the nurse or therapist, journaling, art therapy, or other outlets. Validate their feelings and acknowledge their strength in sharing.
- Referral to Therapy: Facilitate referrals for trauma-focused psychotherapy. Examples include cognitive-behavioral therapy (CBT) with exposure techniques, eye movement desensitization and reprocessing (EMDR), or group therapy. Collaborate with mental health professionals to integrate these therapies into the care plan.
- Medication Management: Administer and monitor prescribed medications. First-line pharmacologic treatments are SSRIs such as sertraline or paroxetine. Other medications may include SNRIs (e.g., venlafaxine) or adjunctive agents like prazosin for trauma-related nightmares. Monitor efficacy and side effects; educate the patient about the importance of adherence and the delayed onset of medication benefits.
- Community Resources: Provide information on support groups, therapists, crisis lines, and community mental health services. Coordinate referrals to social work if needed (e.g., for housing or financial assistance).
- Family Support: Involve family or significant others (with consent) in education. Teach them about PTSD symptoms and how to provide emotional support, encourage treatment adherence, and assist with stress management at home.
- Follow-up: Arrange regular follow-up to monitor progress. Reassess symptoms, coping skills, and risk factors at each visit. Adjust the care plan as needed based on patient progress and feedback.
- Key treatments
• Cognitive behavioral therapy
• Group therapy
• Systematic desensitization
• Benzodiazepines: alprazolam (Xanax), lorazepam (Ativan), clonazepam (Klonopin)
• TCAs: imipramine (Tofranil), amitriptyline (Elavil)
Nursing Insight:
- Recovery from PTSD often requires long-term management. Nurses should reinforce coping strategies and support networks consistently.
- Collaboration with an interdisciplinary team (psychiatry, psychology, social work) ensures comprehensive care and helps maintain continuity as the patient transitions from acute care to outpatient therapy.
Summary
- PTSD is a chronic mental health condition following trauma, featuring intrusive recollections (flashbacks, nightmares), avoidance behaviors, negative changes in mood/thought, and hyperarousal.
- Diagnosis is clinical, based on DSM-5 criteria A through H. Nurses must gather a detailed trauma history and symptom assessment to confirm the diagnosis.
- Stressors include combat, violence, disasters, accidents, and even medical or obstetric emergencies. Recognize risk factors (e.g., female gender, previous trauma, lack of support) that predispose patients to PTSD.
- Assessment findings include patient reports of nightmares, flashbacks, avoidance, and irritability, as well as observed hypervigilance, startle response, or numbing.
- Interventions are multi-dimensional: ensure safety, provide trauma-informed care, teach coping/relaxation techniques, and coordinate trauma-specific therapies and medications.
- Collaborative care and education are essential. Nurses should involve the patient’s support system, manage comorbid conditions, and plan for long-term follow-up.
- Nursing Insight: Effective care for PTSD integrates empathy with evidence-based practice. By addressing triggers, reinforcing coping strategies, and ensuring ongoing support, nurses help patients rebuild a sense of safety and improve long-term outcomes.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Post-traumatic Stress Disorder
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


