Please set your exam date
Urinary Elimination
Study Questions
Practice Exercise 1
The nurse recognizes that urinary elimination changes may occur even in healthy older adults because of which of the following?
Explanation
Urinary elimination in older adults is often affected by age-related changes such as decreased bladder capacity, weakened pelvic floor muscles, and reduced kidney function, which can lead to issues like urinary frequency, urgency, nocturia, and incontinence. These changes increase the risk of infection, skin breakdown, and social isolation, making assessment and supportive interventions essential for maintaining health and quality of life.
Rationale for correct answer:
4. The amount of urine retained after voiding increases: This is known as post-void residual (PVR). As people age, the detrusor muscle weakens. This weakness, combined with changes in the pelvic floor and potential outlet obstruction (like an enlarged prostate in men), prevents the bladder from emptying completely.
Rationale for incorrect answers:
1. The bladder distends and its capacity increases: In older adults, the bladder wall becomes less elastic and more fibrous. This leads to a decrease in bladder capacity, not an increase. A smaller bladder capacity often results in increased frequency of urination and urgency.
2. Older adults ignore the need to void: This is a behavioral assumption rather than a physiological change. While some individuals with cognitive impairments like dementia may not recognize the sensation of a full bladder, it is not a normal physiological consequence of aging in a healthy adult. In fact, many older adults become more sensitive to the need to void due to reduced bladder capacity.
3. Urine becomes more concentrated: Aging affects the kidneys' ability to concentrate urine. Because there is a decrease in the number of functioning nephrons and a reduced response to antidiuretic hormone (ADH), the kidneys are actually less efficient at concentrating urine. This often leads to nocturia (waking up at night to urinate).
Test taking strategy:
- Focus on normal aging physiology, not disease or behavior.
- Eliminate answers that:
- Describe opposites of known age-related changes (e.g., increased bladder capacity, concentrated urine)
- Imply intentional or cognitive behavior rather than physical changes
Take home points:
- Normal aging leads to incomplete bladder emptying, resulting in increased post-void residual urine.
- Older adults have decreased ability to concentrate urine and decreased bladder capacity, contributing to frequency and nocturia.
During shift report, the nurse learns that an older female client is unable to maintain continence after she senses the urge to void and becomes incontinent on the way to the bathroom. Which nursing diagnosis is most appropriate?
Explanation
Urinary incontinence can be classified into several types: stress incontinence, where leakage occurs during activities that increase abdominal pressure such as coughing or lifting; urge incontinence, marked by a sudden, intense need to urinate due to overactive bladder contractions; mixed incontinence, which combines features of both stress and urge; overflow incontinence, caused by incomplete bladder emptying leading to dribbling; and functional incontinence, where physical or cognitive impairments prevent timely toileting.
Rationale for correct answer:
4. Urge urinary incontinence: This is defined as the involuntary loss of urine following a strong, sudden desire to void. The bladder (detrusor) muscle contracts prematurely. This is exactly what the prompt describes: she senses the urge but cannot “hold it” long enough to reach the toilet.
Rationale for incorrect answers:
1. Stress urinary incontinence occurs when physical pressure is put on the bladder-such as coughing, sneezing, laughing, or lifting. It is caused by weak pelvic floor muscles.
2. Reflex urinary incontinence: This occurs at predictable intervals when the bladder reaches a specific volume. Crucially, the patient lacks the sensation or urge to void. This is common in patients with spinal cord injuries.
3. Functional urinary incontinence: This occurs when the patient has bladder control but cannot reach the toilet in time due to environmental or physical barriers (e.g., a broken hip, dementia, or being in restraints).
Test taking strategy:
To differentiate types of incontinence, look for the trigger word in the question:
- If you see “sneeze/cough/jump” - Stress.
- If you see “strong urge/sudden need” - Urge.
- If you see “doesn't feel it/spinal injury” - Reflex.
- If you see “barrier/cannot walk/dementia” - Functional.
Take home points:
- If the problem is the bladder's inability to wait, it is Urge.
- If the problem is the person's inability to walk fast enough or unbutton pants, it is Functional.
A client is experiencing a fever and diaphoresis. What is the expected urine output?
Explanation
Urine output is influenced by multiple factors including fluid intake, diet, and hydration status, as well as physiological and pathological conditions; increased fluid consumption, diuretic foods or medications, and stress can raise output, while dehydration, low fluid intake, kidney disease, urinary tract obstruction, or heart failure can reduce it.
Rationale for correct answer:
1. Decreased and highly concentrated: Fever and diaphoresis cause insensible fluid loss. As the body loses water through the skin and respiratory tract, the total circulating blood volume decreases. The kidneys compensate by reabsorbing as much water as possible back into the bloodstream stimulated by Antidiuretic Hormone - ADH. This results in a lower volume of urine that is high in solutes.
Rationale for incorrect answers:
2. Decreased and highly dilute: This is a physiological contradiction. If urine volume is decreased because the body is holding onto water, the urine produced will be dark and concentrated (high specific gravity), not dilute.
3. Increased and concentrated: This is physically impossible under normal kidney function. To make urine concentrated, the kidneys must remove water; removing water naturally decreases the total volume of urine.
4. Increased and dilute: This occurs with high fluid intake or conditions like diabetes insipidus. In a client with fever and sweating, the body is trying to conserve fluid, not get rid of it.
Test taking strategy:
Identify fluid loss first.
- Fever and sweating - fluid loss.
Ask: “Does the body want to conserve or eliminate water?”
- Conserve: decreases urine output, increases concentration.
Take home points:
- When the body loses fluid through non-urinary routes (skin/lungs), the kidneys will always attempt to conserve fluid, leading to oliguria.
- A nurse should expect the urine specific gravity to be high (>1.030) in a febrile, diaphoretic patient, reflecting dehydration.
A nurse is caring for a client in the renal unit. Which of the following terms denotes a client’s inability to void even though the kidneys are producing urine that enters the bladder?
Explanation
Understanding these terms is essential in nursing practice, as they differentiate between various urinary problems: urgency refers to a sudden, strong need to urinate; retention is the inability to void despite bladder filling; oliguria indicates reduced urine output; and dysuria describes painful or difficult urination.
Rationale for correct answer:
2. Retention: Urinary retention is the state in which the bladder is full of urine, but the client is unable to move the urine out of the bladder. This can be caused by obstructions like an enlarged prostate or nerve issues.
Rationale for incorrect answers:
1. Urgency is the sudden, strong, and often uncontrollable desire to void immediately. It is a sensory symptom, not an inability to empty the bladder.
3. Oliguria refers to decreased urine production by the kidneys (typically less than 400 mL in 24 hours). In the scenario, the kidneys are producing urine, so the problem is not oliguria.
4. Dysuria is the medical term for painful or difficult urination, often described as a burning sensation. While it may accompany a struggle to void, it does not define the inability to empty a full bladder.
Test taking strategy:
When faced with terminology questions, match the “action” in the stem to the definition:
- “Producing urine” - Kidneys are working (eliminates oliguria).
- “Enters the bladder” - The tubes (ureters) are clear.
- “Inability to void” - The exit is blocked or the pump failed. This logical flow leads you directly to retention.
Take home points:
For a client with retention, the nurse will find a distended bladder on palpation or a high volume on a bladder scan, whereas in oliguria, the bladder will be empty.
The nurse should incorporate which of the following into the teaching plan for a client to promote healthy urinary functioning?
Explanation
A diet for healthy urinary functioning emphasizes hydration and balanced nutrition to support bladder and kidney health; drinking adequate water helps flush bacteria and toxins, while limiting bladder irritants such as caffeine, alcohol, carbonated drinks, and spicy foods reduces urgency and irritation. Including fiber-rich foods prevents constipation, which can worsen urinary symptoms, and consuming fruits and vegetables high in antioxidants (like berries and leafy greens) supports urinary tract resilience.
Rationale for correct answer:
4. Caffeine-containing beverages should be monitored to prevent excess intake: Caffeine is a known bladder irritant and a diuretic. It increases the urgency to void and causes the kidneys to produce more urine, which can lead to frequency and dehydration. Monitoring and limiting caffeine is a standard part of urinary health teaching.
Rationale for incorrect answers:
1. Drinking more than 2,000 mL of fluid per day will cause fluid retention: For a healthy adult with normal heart and kidney function, 2,000 mL (about 2 liters) is actually the recommended target. The body maintains homeostasis by excreting excess fluid as urine; it does not cause retention unless there is an underlying pathology like heart failure or renal failure.
2. The healthy adult should drink four to six 8-ounce glasses of water per day: This amount is too low. The standard recommendation is eight to ten 8-ounce glasses (approx. 2,000–2,400 mL) per day to ensure adequate kidney flushing and to prevent constipation.
3. Children need fewer reminders to drink because of greater thirst sensitivity: Children are actually at higher risk for dehydration because they often get distracted by play and may not recognize or respond to thirst cues as quickly as adults. They require frequent reminders to hydrate.
Test taking strategy:
- Look for prevention-based, realistic health teaching- Education that promotes balance and moderation.
- Eliminate absolute or misleading statements e.g. “Will cause fluid retention”
- Choose the option that applies across all age groups and settings.
Take home points:
- Unless a patient has a specific restriction, aim for at least 2 liters of fluid daily to maintain urinary health.
- Caffeine and alcohol are the two biggest triggers for urinary dysfunction.
Practice Exercise 2
The nurse is most likely to assess for which of the following during assessment of the client with urinary incontinence? Select all that apply
Explanation
Urinary incontinence is the involuntary leakage of urine, a common condition especially among women and older adults, caused by factors such as weakened pelvic muscles, overactive bladder, or obstruction, and it can present as stress, urge, mixed, overflow, or continuous incontinence; though not life-threatening, it significantly impacts quality of life and is managed through lifestyle changes, pelvic floor exercises, medications, or surgical interventions depending on severity and type.
Rationale for correct answers:
1. Perineal skin irritation: Chronic exposure to urine changes the skin's pH and creates a moist environment. This leads to incontinence-associated dermatitis, characterized by redness, itching, and skin breakdown. Assessing the skin is a priority to prevent secondary fungal infections or pressure ulcers.
2. Fluid Intake of Less than 1,500 mL/day: While it seems counterintuitive, patients with incontinence often restrict fluids to avoid “accidents.” However, low fluid intake leads to concentrated urine, which acts as a bladder irritant, increasing urgency and frequency. A healthy intake is typically 1,500–2,000 mL/day unless contraindicated.
4. History of frequent urinary tract infections (UTIs): A UTI is a leading cause of “transient” or acute incontinence. Inflammation of the bladder wall (cystitis) causes the bladder to become hyperactive, leading to a sudden, uncontrollable urge to void. Conversely, chronic incontinence can increase the risk of UTIs due to the use of pads or catheters.
5. A fecal impaction: The rectum and the bladder share the same pelvic floor space. An impacted mass of stool in the rectum can physically press against the bladder neck, obstructing flow (leading to overflow incontinence) or irritating the bladder (leading to urge incontinence). Relieving constipation often resolves the urinary issue.
Rationale for incorrect answers:
3. History of antihistamine intake: Many over-the-counter antihistamines have anticholinergic effects. These drugs can cause the bladder muscle (detrusor) to relax too much or the urethral sphincter to contract, leading to urinary retention.
Test taking strategy:
When faced with a “Select all that apply” (SATA) question regarding a symptom like incontinence, treat each option as a True/False statement and categorize them into two groups:
- Complications: Ask, “Is this a physical result of being incontinent?” (Choice 1 fits here).
- Etiologies (Causes): Ask, “Could this factor actually trigger or worsen bladder leakage?” (Choices 2, 4, and 5 fit here).
Take home points:
- Urinary incontinence assessment includes skin integrity, hydration, medications, infections, and bowel function.
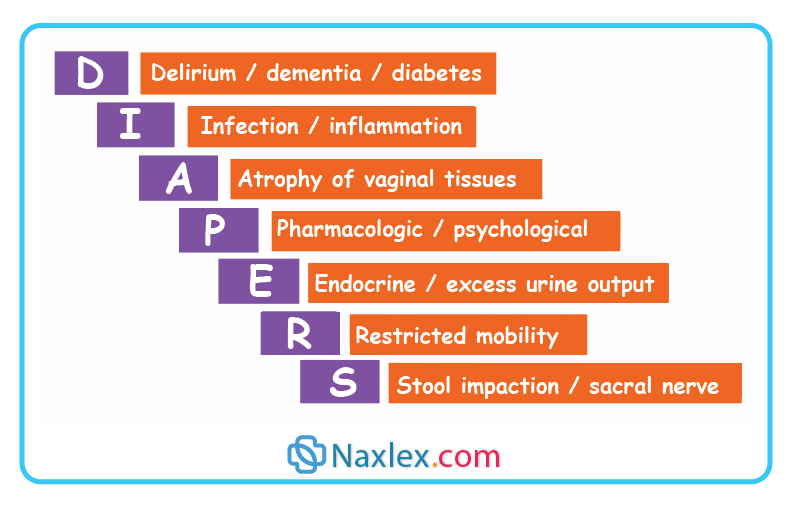
- Many causes of incontinence are reversible, making thorough nursing assessment essential. Always look for the DIAPPERS acronym to find treatable causes.
The nurse will need to assess the client’s performance of clean intermittent self-catheterization (CISC) for a client with which urinary diversion?
Explanation
Clean intermittent self-catheterization (CISC) is a technique where individuals insert a catheter into the bladder at regular intervals to drain urine, then remove it immediately afterward, rather than leaving it in place; it is commonly used for patients with neurogenic bladder, chronic urinary retention, or incomplete bladder emptying, and is preferred over long-term indwelling catheters because it reduces the risk of infection, preserves bladder function, and promotes independence.
Rationale for correct answer:
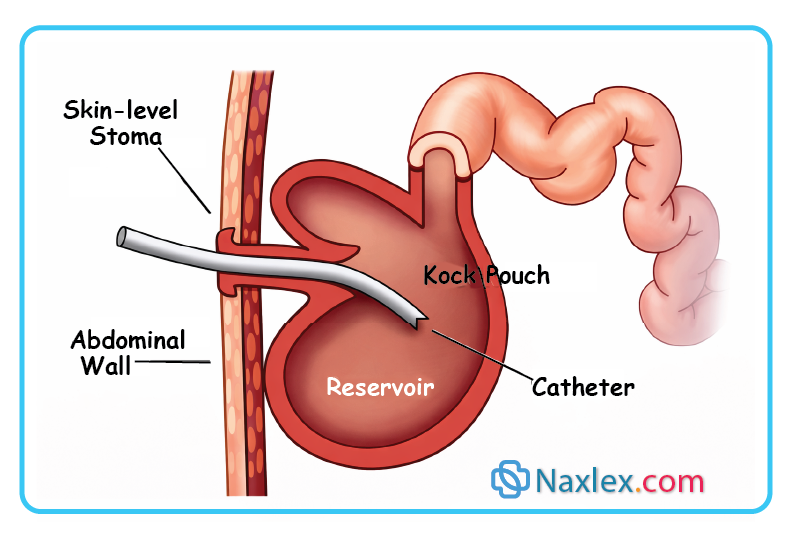
2. Kock pouch: This is a continent cutaneous urinary diversion. The surgeon creates an internal reservoir from the small intestine. A “nipple” valve is created so urine does not leak out. Because there is no external bag, the client must perform CISC every 4–6 hours to empty the internal pouch through the stoma.
Rationale for incorrect answers:
1. Ileal conduit: This is an incontinent urinary diversion. The ureters are connected to a piece of the ileum, which opens onto the abdominal wall as a stoma. Urine drains continuously into an external collection bag. No catheterization is required.
3. Neobladder: A neobladder is an internal reservoir connected to the urethra. Ideally, the client voids by relaxing the pelvic floor and using the Valsalva maneuver (bearing down). While some neobladder patients may occasionally need to catheterize if they can't empty fully, it is not the standard primary method of emptying as it is for a Kock pouch.
4. Vesicostomy: This is a simple opening made directly from the bladder to the abdominal wall, common in pediatrics. It usually drains directly into a diaper or an appliance; while it can be catheterized, the Kock pouch is the definitive answer for a diversion requiring a formal CISC schedule.
Test taking strategy:
Ask: “How is urine emptied?”
- External bag - no catheter
- Internal pouch with stoma - catheter required
Continent diversions store urine thus needs to be emptied.
Take home points:
- An ileal conduit is “incontinent” - needs a bag.
- A Kock pouch is “continent” - needs a catheter.
- For patients with a Kock pouch, learning CISC is essential for survival and social continence, as the pouch can rupture if not emptied regularly.
A nurse is educating a client with a flaccid bladder. Which focus is the nurse most likely to teach this client?
Explanation
A flaccid bladder, also called a hypotonic or atonic bladder, is a condition where the bladder loses muscle tone and cannot contract effectively, leading to incomplete emptying and urinary retention. It is often caused by damage to the sacral spinal cord, peripheral nerves, or conditions such as diabetes mellitus and spinal cord injury. Because the bladder cannot generate enough pressure to expel urine, patients may experience overflow incontinence, frequent dribbling, and increased risk of urinary tract infections.
Rationale for correct answer:
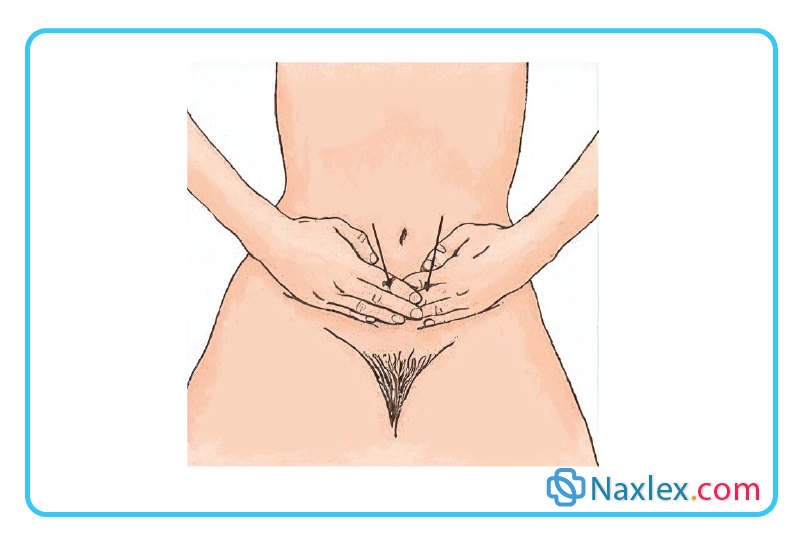
3. Credé’s maneuver: Apply gentle manual pressure to the lower abdomen. A flaccid bladder, often caused by lower motor neuron spinal cord injuries, lost its muscle tone (detrusor areflexia) and cannot contract to push urine out. Credé’s maneuver involves manually pressing down on the bladder to physically force the urine out.
Rationale for incorrect answers:
1. Habit training: Attempt voiding at specific time periods. Habit training (or timed voiding) is typically used for clients with functional incontinence or those with cognitive impairments (like dementia). It relies on a schedule to keep the client dry but does not solve the physical emptying problem of a flaccid bladder.
2. Bladder training: Delay voiding according to a prescheduled timetable. Bladder training is the primary intervention for urge incontinence (overactive bladder). The goal is to “teach” the bladder to hold more urine for longer periods. In a flaccid bladder, the muscle is already too relaxed (underactive), so delaying voiding would only lead to dangerous over-distention.
4. Kegel exercises: Contract the pelvic muscles. Kegel exercises strengthen the pelvic floor to help with stress incontinence (leakage during coughing or sneezing). While healthy, they do not assist the detrusor muscle in a flaccid bladder to actually empty.
Test taking strategy:
- When you see the word “flaccid,” think “weak/no contraction.” If the muscle won't contract, you need an outside force to help.
- Options 1, 2, and 4 all require the bladder or pelvic muscles to have some level of functional snap or control.
- Only Option 3 provides a mechanical, external solution for a muscle that cannot move on its own.
Take home points:
- The priority for a flaccid bladder is preventing urinary retention and the resulting kidney damage due to hydronephrosis.
- In a flaccid bladder, the “pump” is broken. One must use external force (Credé’s maneuver) or a catheter to empty it.
A nurse is assessing a client on a bladder training program. Which of the following behaviors indicates that the client has met the expected outcomes? Select all that apply
Explanation
A bladder training program is a behavioral therapy designed to help individuals with urinary incontinence or overactive bladder regain control by gradually increasing the time between voids; it involves scheduled toileting, resisting the urge to urinate immediately, and using techniques such as distraction or pelvic floor exercises to delay urination. Over time, the bladder’s capacity improves, urgency episodes decrease, and continence is enhanced. This program is often combined with lifestyle modifications.
Rationale for correct answers:
2. Practices slow, deep breathing until the urge decreases: This is a “distraction” or “urge-suppression” technique. Deep breathing helps the nervous system relax and prevents the detrusor muscle from contracting prematurely, allowing the client to wait until the scheduled voiding time.
5. Performs pelvic muscle exercises: Pelvic muscle exercises (Kegels) strengthen the muscles that support the bladder and help close the urethra. This physical strength is essential for successfully suppressing an urge and maintaining continence until the scheduled time.
Rationale for incorrect answers:
1. Voids each time there is an urge: This behavior is what the client is trying to stop doing. In bladder training, the goal is to resist the initial urge and wait for the scheduled time to increase bladder capacity. Voids at every urge reinforce “urge incontinence.”
3. Uses adult diapers, for “just in case.”: While seemingly practical, the use of diapers can be a psychological “crutch” that discourages the active effort required for bladder training. Clients are encouraged to use pads initially, but the goal is to return to regular underwear as confidence and control increase.
4. Drinks citrus juices and carbonated beverages: Citrus juices, caffeine, and carbonated beverages are known bladder irritants. They can trigger detrusor contractions and make the urge to void much stronger, which works against the goals of a training program.
Test taking strategy:
In “Expected outcomes” questions, look for behaviors that show the client is actively managing the condition using the specific techniques taught.
- If the training is about control, then giving in to the urge (1) or using a “safety net” like a diaper (3) are signs of failure or lack of progress.
- Look for the “Golden Pair”: urge suppression (2) and muscle strengthening (5).
Take home points:
- Bladder training is a behavioral therapy.
- Success is marked by using techniques (like deep breathing) to suppress the urge rather than giving in to it.
- Successful bladder management includes avoiding irritants (caffeine, alcohol, artificial sweeteners, and citrus).
The nurse keeps in mind which of the following when collecting a urine specimen for routine urinalysis from a client?
Explanation
Collecting a urine specimen for routine urinalysis involves obtaining a clean, midstream sample to ensure accuracy and reduce contamination; the patient is instructed to wash their hands, cleanse the genital area, begin urinating into the toilet, then collect the midstream portion in a sterile container, sealing it promptly and labeling it correctly. The specimen should be delivered to the laboratory as soon as possible - ideally within one hour - or refrigerated if delayed, since prolonged standing can alter results.
Rationale for correct answer:
2. Results may be altered if a sample is left standing at room temperature for a long time: If urine sits at room temperature for longer than 1 hour, it begins to decompose. Bacteria multiply, the pH becomes more alkaline as urea converts to ammonia, and glucose levels may drop as bacteria consume it. If the sample cannot be sent to the lab immediately, it must be refrigerated.
Rationale for incorrect answers:
1. A sterile specimen is required for collection: A routine urinalysis does not require a sterile specimen. It is a clean procedure, not a surgical one. A sterile specimen is only required for a urine culture and sensitivity to identify specific bacteria.
3. The external meatus requires cleaning with antiseptic soap and water before voiding: While the area should be generally clean, the formal “antiseptic wipe” procedure is specifically for a clean-catch midstream specimen. For a routine urinalysis, the client can simply void into a clean container.
4. A clean-catch midstream specimen is necessary: While a clean-catch is the “gold standard” for avoiding contamination, it is not strictly necessary for a routine screening urinalysis. A simple “random” specimen is usually sufficient unless the provider specifically orders a clean-catch or a culture.
Test taking strategy
- In nursing exams, look for the answer that addresses specimen integrity.
- Options 1, 3, and 4 are “best practice” for cultures, but Option 2 is a universal rule for all urine samples.
Take home points:
- Urine is a living medium; to get accurate results for pH, nitrites, and bacteria, the lab must receive the specimen within 1 hour or it must be cooled to pause bacterial growth.
- Always distinguish between a routine urinalysis (tests for chemistry/blood/protein) and a culture (tests for specific bacteria).
- Cultures require sterile technique; routine urinalysis do not.
Practice Exercise 3
The nurse is caring for a client wearing a condom catheter. Which action represents the appropriate nursing management?
Explanation
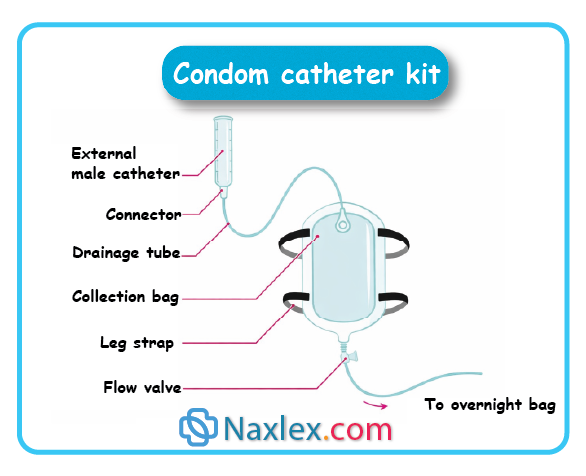
A condom catheter is a non-invasive urinary collection device used mainly for men with urinary incontinence; it fits over the penis like a condom and connects via tubing to a drainage bag strapped to the leg, offering a safer alternative to indwelling catheters since it does not enter the urethra and carries a lower risk of urinary tract infections, though it requires daily changes and proper hygiene to prevent skin irritation or leakage.
Rationale for correct answer:
2. Check the penis for adequate circulation 30 minutes after applying: This is a critical safety intervention. If the condom is too tight or the adhesive is applied improperly, it can act as a tourniquet. The nurse must assess for swelling, discoloration (cyanosis), or coolness to ensure blood flow is not compromised.
Rationale for incorrect answers:
1. Ensure that the tip of the penis fits snugly against the end of the condom: There should be a gap of about 1 to 2 inches (2.5 to 5 cm) between the tip of the penis and the end of the condom catheter. This prevents the head of the penis (glans) from rubbing against the rubber, which causes skin irritation and breakdown. It also prevents urine from pooling against the skin, which can lead to maceration.
3. Change the condom every 8 hours: Changing a condom catheter every 8 hours is unnecessary and can cause skin trauma from repeated adhesive removal. Standard practice is to change it daily (every 24 hours) or when it becomes soiled or dislodged.
4. Tape the collecting tubing to the lower abdomen: For male patients, the tubing of a condom catheter (or indwelling catheter) is typically secured to the upper thigh to prevent tension on the penis. Taping to the lower abdomen is more common for long-term suprapubic catheters to prevent penoscrotal fistulas, but it is not the standard for condom catheters.
Test taking strategy:
- When choosing between nursing actions, prioritize the one that involves assessment for potential injury.
- Option 2 is an assessment of “Circulation” which falls under the ABC (Airway, Breathing, Circulation) priority framework.
Take home points:
- Always leave space at the tip of a condom catheter to prevent skin erosion and allow for immediate drainage into the tube.
- Any external device applied to an extremity or organ (like a condom catheter or a restraint) requires a timed circulation check to prevent tissue necrosis.
A nurse is catheterizing a female client. The catheter slips into the vagina. The nurse should perform which action?
Explanation
Catheterization errors in females often occur due to anatomical challenges and technical mistakes, such as misidentifying the urethral opening, inserting the catheter into the vagina, inflating the balloon before the catheter reaches the bladder, or using the wrong catheter size; these errors can lead to complications including trauma, infection, leakage, or patient discomfort, but they are preventable with proper visualization, aseptic technique, correct equipment selection, and careful confirmation of urine flow before balloon inflation
Rationale for correct answer:
1. Leaves the catheter in place and gets a new sterile catheter: If the catheter enters the vagina, it is now contaminated. Leaving it there acts as a visual landmark. By leaving the “wrong” tube in the vaginal opening, the nurse can more easily identify the urinary meatus which is located just above it and avoid hitting the vagina a second time with the new, sterile kit.
Rationale for incorrect answers:
2. Leaves the catheter in place and asks another nurse to attempt the procedure: While you might eventually need help, the immediate nursing action is to maintain the landmark and prepare a sterile replacement. The nurse should attempt to correct their own technique before delegating, provided sterile technique is maintained.
3. Removes the catheter and redirects it to the urinary meatus: Once the catheter touches the vaginal mucosa, it is no longer sterile. Inserting a contaminated catheter into the bladder will introduce bacteria directly into the urinary tract, significantly increasing the risk of a catheter-associated urinary tract infection (CAUTI).
4. Removes the catheter, wipes it with a sterile gauze, and redirects it to the urinary meatus: Wiping a catheter with gauze does not resterilize it. Once the sterile field or equipment is breached by contact with non-sterile skin or mucous membranes, it must be discarded.
Test taking strategy:
In any question regarding a sterile procedure, immediately eliminate any answer that suggests reusing or cleaning equipment that has touched a non-sterile surface.
Take home points:
- The vagina is the most common “wrong turn” in female catheterization.
- Use the misplaced catheter as a placeholder to ensure the second attempt is successful.
- In nursing, if you even suspect a break in sterile technique, you must stop and start over.
The health care provider has ordered an indwelling catheter inserted in a hospitalized male client. The nurse is aware of which of the following considerations?
Explanation
An indwelling catheter, commonly called a Foley catheter, is a flexible tube inserted into the bladder through the urethra and left in place to provide continuous urine drainage; it is held in position by a small balloon inflated inside the bladder. Indwelling catheters are used when patients cannot empty their bladder naturally, such as in cases of urinary retention, surgery, severe incontinence, or critical illness requiring accurate urine output monitoring.
Rationale for correct answer:
1. The male urethra is more vulnerable to injury during insertion: The male urethra is significantly longer (approx. 20 cm) than the female urethra (approx. 4 cm) and has a double curve. It is more prone to trauma, especially in older men with an enlarged prostate (BPH) which can constrict the urethral passage, making catheter insertion difficult and potentially causing mucosal tears or false passages.
Rationale for incorrect answers:
2. In the hospital, a clean technique is used for catheter insertion: In an acute care or hospital setting, indwelling catheterization must be performed using sterile technique (surgical asepsis). Clean technique is only acceptable for intermittent self-catheterization in the home environment.
3. The catheter is inserted 2” to 3” into the meatus: This is the measurement for a female client. For a male client, the catheter should be inserted 7 to 9 inches (17 to 22.5 cm), or until urine flows, and then advanced another 1–2 inches to ensure the balloon is not inflated inside the urethra.
4. Since it uses a closed system, the risk for urinary tract infection is absent: While a closed drainage system reduces the risk of infection compared to an open system, the risk is never absent. An indwelling catheter is the primary cause of healthcare-associated UTIs (CAUTIs) because it provides a direct pathway for bacteria to enter the bladder via biofilm.
Test taking strategy:
- In Option 4, the word “absent” is an absolute. In nursing exams, risks are almost never absent or zero. This allows you to eliminate that choice immediately.
- By comparing the measurements in Option 3 to your knowledge of male vs. female anatomy, you can eliminate that as well.
- Choosing Option 1 recognizes the physiological reality of the male reproductive and urinary tract.
Take home points:
- The length and curvature of the male urethra require the nurse to insert the catheter almost to the “Y” bifurcation before inflating the balloon to ensure safety.
- Any invasive procedure in the hospital that enters a normally sterile body cavity (like the bladder) requires strict surgical asepsis.
A nurse is caring for a client with an indwelling urinary catheter. Which nursing intervention decreases the risk for catheter-associated urinary tract infection (CAUTI)?
Explanation
Catheter-associated urinary tract infection (CAUTI) is one of the most common healthcare-associated infections, occurring when bacteria enter the urinary tract via an indwelling catheter, often due to prolonged use. CAUTIs develop when microorganisms adhere to the catheter surface and form biofilms, leading to bacteriuria and sometimes symptomatic infection. They are classified as nosocomial infections and account for up to 80% of hospital-acquired UTIs
Rationale for correct answer:
2. Bag below the level of the bladder: This is the most critical intervention for preventing CAUTI. It utilizes gravity to maintain a one-way flow of urine. If the bag is raised above the bladder, contaminated urine from the bag or tubing can reflux back into the bladder, introducing bacteria.
Rationale for incorrect answers:
1. Cleansing with antiseptic 3-4 times daily: Current evidence-based practice suggests that aggressive cleansing with antiseptics (like povidone-iodine) can irritate the meatus and actually increase infection risk. Routine hygiene with mild soap and water during a bath is sufficient.
3. Emptying the bag daily: Emptying the bag only once a day is insufficient and increases the risk of bacterial overgrowth. The bag should be emptied whenever it is one-half to two-thirds full, or at least every 8 hours, to maintain flow and prevent tension.
4. Irrigating with sterile water: Routine irrigation breaks the closed drainage system. Every time the catheter is disconnected from the tubing to irrigate, you provide an entry point for bacteria. Irrigation should only be done if an obstruction is suspected (e.g., blood clots).
Test taking strategy:
- In nursing school, “below the level of” is a common theme for drainage systems (chest tubes, Foley bags, etc.).
- To prevent infection, you must prevent reflux. If you see an option that maintains a closed system or uses gravity, it is almost always the correct answer for infection control questions.
Take home points:
- Every time one opens the connection (to irrigate or change a bag), you increase the risk of CAUTI. Keep the system intact as much as possible.
- Always ensure there are no dependent loops in the tubing and that the bag is lower than the bladder to prevent the backflow of colonized urine.
A nurse is caring for a male client with a condom catheter. Which of the following is a nursing priority?
Explanation
A condom catheter is a non-invasive urinary collection device used mainly for men with urinary incontinence; it fits over the penis like a condom and connects via tubing to a drainage bag strapped to the leg, offering a safer alternative to indwelling catheters since it does not enter the urethra and carries a lower risk of urinary tract infections, though it requires daily changes and proper hygiene to prevent skin irritation or leakage.
Rationale for correct answer:
1. Preventing the tubing from kinking: The primary purpose of a condom catheter is to allow urine to flow away from the skin into a drainage bag. If the tubing kinks, urine pools within the condom sheath. This causes two major issues: skin breakdown (maceration) due to prolonged moisture contact and the high likelihood that the pressure will cause the condom to pop off or leak.
Rationale for incorrect answers:
2. Not removing the catheter for any reason: Condom catheters must be removed daily to perform thorough perineal care and to inspect the skin of the penis for signs of irritation, swelling, or decreased circulation.
3. Fastening the condom tightly: A condom catheter that is applied too tightly acts as a tourniquet. Because the penis can change in size due to erections or edema, a tight application can cut off blood flow, leading to tissue necrosis. There should always be a small gap (about 1–2 inches) between the tip of the penis and the end of the catheter.
4. Maintaining bed rest at all times: A condom catheter is not an indication for bed rest. In fact, it is often used for mobile patients to help them maintain independence. The drainage bag can be switched to a leg bag to allow for ambulation.
Test taking strategy:
- Identify the keyword: priority. Focus on safety and basic function.
- Use the process of elimination. Option 2 (for any reason) and Option 4 (at all times) use absolute language, which is rarely correct in nursing.
Take home points:
- The biggest risk with a condom catheter is skin breakdown or circulatory compromise; nursing care must focus on frequent inspection and dry skin.
- Like all urinary drainage systems, the bag must stay below the level of the bladder and the tubing must remain straight to prevent backflow and leaks.
Comprehensive Questions
A nurse is caring for home care client with a long-term indwelling catheter. Which statement indicates a need for further teaching?
Explanation
A long-term indwelling catheter, is a flexible tube inserted into the bladder via the urethra and left in place for continuous drainage of urine over weeks to months; it is indicated for patients with chronic urinary retention not manageable by other means, severe urinary incontinence causing skin breakdown, neurogenic bladder dysfunction, palliative care needs, or when accurate urine output monitoring is essential in long-term settings.
Rationale for correct answer:
3. “Soaking in a warm tub bath may ease the irritation associated with the catheter.” Clients with indwelling catheters should avoid tub baths because the water is not sterile and can easily travel up the outside of the catheter (the “wicking” effect) and enter the urethra, leading to a UTI. Showers are preferred over baths.
Rationale for incorrect answers:
1. “I will keep the collecting bag below the level of the bladder at all times.” Keeping the bag lower than the bladder uses gravity to prevent the backflow (reflux) of contaminated urine into the bladder, which is a primary cause of infection.
2. “Intake of cranberry juice may help decrease the risk of infection.” Cranberry juice contains compounds that can prevent E. coli bacteria from adhering to the bladder wall. While it doesn't cure an infection, it is a common preventative measure for home care clients.
4. “I should use clean technique when emptying the collecting bag.” In a home setting, clean technique (medical asepsis) is the standard for emptying the bag, provided the drainage spigot does not touch the collection container or the floor.
Test taking strategy:
- In “need for further teaching” questions, you are looking for the incorrect statement.
- Read each option and label it “True or False” regarding standard medical practice.
- The false statement is the correct answer. In this case, tub baths (F) stand out against three standard catheter care rules (T).
Take home points:
- Education should focus on showering and keeping the perineal area clean with mild soap and water.
- To prevent catheter-associated urinary tract infection (CAUTI), the drainage bag must always be lower than the bladder, even during transport or sleep.
A female client has a urinary tract infection (UTI). Which teaching points by the nurse would be helpful to the client? Select all that apply
Explanation
A urinary tract infection (UTI) is an infection that occurs anywhere along the urinary system-most commonly in the bladder (cystitis) or urethra, but sometimes affecting the kidneys (pyelonephritis); it is usually caused by bacteria such as Escherichia coli entering the urinary tract. Symptoms often include burning during urination, frequent or urgent need to urinate, cloudy or foul-smelling urine, and pelvic pain, while kidney involvement may cause fever, flank pain, or nausea.
Rationale for correct answers:
2. Review symptoms of UTI with the client: Education is vital for early detection. The nurse should ensure the client knows to watch for urgency, frequency, dysuria, hematuria, and flank pain which could indicate the infection has spread to the kidneys.
4. Wear cotton underclothes: Cotton is a breathable fabric that allows moisture to evaporate. Synthetic fabrics like nylon trap heat and moisture, creating a “greenhouse effect” that promotes bacterial growth.
Rationale for incorrect answers:
1. Limit fluids to avoid the burning sensation on urination: Patients should increase fluid intake ideally 2–3 L/day. Fluids help flush bacteria out of the urinary tract and dilute the urine, which can actually make the burning sensation less intense by reducing urine concentration.
3. Wipe the perineal area from back to front: This is a major risk factor for UTIs in females. Clients must be taught to wipe from front to back (cleanest to dirtiest) to avoid dragging E. coli and other fecal bacteria into the urethral opening.
5. Take baths rather than showers: Clients with UTIs should avoid baths and choose showers. Sitting in bath water especially with bubble bath or oils allows bacteria and chemical irritants to enter the urethra, potentially worsening or causing infections.
Test taking strategy:
- In select all that apply questions regarding infection, look for habits that either introduce bacteria or provide an environment for growth.
- Wiping back-to-front (3) and taking baths (5) both introduce bacteria or irritants.
- Limiting fluids (1) prevents the flushing of bacteria.
Take home points:
- Perineal hygiene is the cornerstone of UTI prevention in women due to the short length of the female urethra.
- Increasing water intake is one of the most effective non-pharmacological interventions to assist in resolving and preventing UTIs.
A nurse is caring for a client with an indwelling catheter. Nursing care for this client includes which of the following?
Explanation
An indwelling catheter, commonly called a Foley catheter, is a flexible tube inserted into the bladder through the urethra and left in place to provide continuous urine drainage; it is held in position by a small balloon inflated inside the bladder. Indwelling catheters are used when patients cannot empty their bladder naturally, such as in cases of urinary retention, surgery, severe incontinence, or critical illness requiring accurate urine output monitoring.
Rationale for correct answer:
3. Encouraging a generous fluid intake if not contraindicated by the client’s condition: High fluid intake if the client's heart and kidneys can handle it produces a high volume of urine. This provides a “natural irrigation” that flushes the bladder, keeps the tubing clear of sediment, and reduces the risk of catheter-associated urinary tract infection (CAUTI).
Rationale for incorrect answers:
1. Irrigation of the catheter with 30 mL of normal saline solution every 4 hours: Routine irrigation is not recommended because it breaks the closed system and significantly increases the risk of introducing bacteria into the bladder. Irrigation is only performed if there is an obstruction like blood clots or per a specific surgeon's order.
2. Disconnecting and reconnecting the drainage system quickly to obtain a urine specimen: You should never disconnect the catheter from the drainage tube to collect a specimen. Most modern catheters have a needleless sampling port on the tubing. Disconnecting the system creates a portal of entry for pathogens.
4. Telling the client that burning and irritation are normal, subsiding within a few days: While mild awareness of the catheter is common, persistent burning and irritation are not normal and can be signs of a UTI, urethral trauma, or a catheter that is improperly secured and pulling on the bladder neck.
Test taking strategy:
- When answering questions about invasive tubes (catheters, IVs, chest tubes), look for the answer that maintains the closed system.
- Any option that involves disconnecting, opening or irrigating (Options 1 and 2) increases infection risk and is usually the wrong nursing action unless an emergency obstruction exists.
Take home points:
- The integrity of the connection between the catheter and the drainage bag is the most important defense against infection.
- Increasing oral fluids is always safer than manual saline irrigation for keeping a catheter patent and the bladder healthy.
A client is having difficulty voiding after surgery. Which nursing action would most likely lead to an increased difficulty with voiding?
Explanation
Difficulty voiding after surgery, often called postoperative urinary retention, is a common complication where patients are unable to empty their bladder effectively; it can result from anesthesia, pain medications (especially opioids), surgical trauma near the urinary tract, or immobility, all of which interfere with bladder muscle contraction or nerve signaling. Patients may experience discomfort, bladder distension, or inability to urinate, and if untreated, this can lead to infection or kidney problems.
Rationale for correct answer:
2. Having the client ignore the urge to void until her bladder is full: This is the action most likely to increase difficulty. Ignoring the urge can lead to over-distention of the bladder. When the bladder muscle (detrusor) is stretched too far, it loses its ability to contract effectively, making it even harder for the patient to start the stream.
Rationale for incorrect answers:
1. Pouring warm water over the client’s fingers: This is a sensory stimuli technique. The sound and feel of running warm water can trigger the micturition reflex, helping the patient relax the urinary sphincter to initiate voiding.
3. Using a warm bedpan when the client feels the urge to void: A cold bedpan causes muscles to tense up (vasoconstriction and guarding). A warm bedpan promotes pelvic muscle relaxation, which is necessary to allow urine to pass.
4. Stroking the client’s leg or thigh: This is another form of tactile stimulation that can sometimes stimulate the nerves responsible for the voiding reflex in patients struggling with postoperative urinary retention.
Test taking strategy
- This is a Negative event question (which action would increase difficulty?). You are looking for the “bad” nursing intervention.
- Options 1, 3, and 4 are all facilitation techniques designed to help.
- Option 2 is a suppression technique. Since the goal is to encourage voiding, choosing the option that tells the patient to wait is logically the one that will cause the most harm in this context.
Take home points:
- In the postoperative period, the nurse should encourage the patient to attempt voiding the moment they feel the urge to prevent bladder atony (weakness) from over-filling.
- Post-surgical retention is often caused by anesthesia and pain.
- Nursing interventions should focus on comfort (warmth, privacy, position) to allow the sphincters to relax.
A male client with diabetes mellitus, has developed a UTI. He is 80 years old and has an indwelling catheter in place. Which factor is most likely the cause of his UTI?
Explanation
A urinary tract infection (UTI) is an infection that occurs anywhere along the urinary system-most commonly in the bladder (cystitis) or urethra, but sometimes affecting the kidneys (pyelonephritis); it is usually caused by bacteria such as Escherichia coli entering the urinary tract. Symptoms often include burning during urination, frequent or urgent need to urinate, cloudy or foul-smelling urine, and pelvic pain, while kidney involvement may cause fever, flank pain, or nausea.
Rationale for correct answer:
4. An indwelling catheter is the leading cause of healthcare-associated infections. It provides a direct superhighway (biofilm) for bacteria to bypass the body's natural defenses and enter the bladder. For a client who already has a catheter, this is statistically the primary culprit (CAUTI).
Rationale for incorrect answers:
1. The close proximity of the male genitalia to the rectum: While this is a major factor for female clients due to a short urethra and close proximity, it is less of a factor for males. The male urethra is longer, providing a greater distance for bacteria to travel to reach the bladder.
2. Decreased immunity: Being 80 years old and having diabetes mellitus does result in decreased immunity, making it harder for the body to fight an infection. However, decreased immunity is a predisposing factor, not the direct mechanical cause of the infection in this scenario.
3. A high urine glucose level: In diabetes, glucose in the urine (glycosuria) provides an excellent food source for bacteria to multiply. Like decreased immunity, this makes an infection more likely to thrive, but it is not the primary vehicle that introduces the bacteria.
Test taking strategy:
- When a question provides several correct sounding predisposing factors (diabetes, age, anatomy), look for the invasive device.
- An invasive foreign body (like a catheter, IV line, or ventilator) is almost always the most likely cause of a new infection because it breaks the body's natural protective barriers.
Take home points:
- In any clinical scenario where a patient has a catheter and develops a UTI, the catheter is considered the primary cause until proven otherwise.
- Diabetes and age (host factors) make the environment favorable for bacteria, but the catheter (the agent/vehicle) is what facilitates the entry.
A client who is an alert, ambulatory, older nursing home resident, voids frequently and has difficulty making it to the bathroom in time. The nurse planning her care is aware of which of the following?
Explanation
Urge incontinence is a type of urinary incontinence characterized by a sudden, intense urge to urinate followed by involuntary leakage before reaching a toilet; it is commonly caused by overactive bladder contractions due to neurological conditions, bladder irritation, or idiopathic factors. Patients often report frequent urination, nocturia, and difficulty delaying voiding, which can significantly impact daily life.
Rationale for correct answer:
3. Kegel exercises performed at regular intervals throughout the day may be helpful: Kegel exercises (pelvic floor muscle training) strengthen the pubococcygeus muscle group. This improves the ability of the urethral sphincter to remain closed and can help suppress the premature bladder contractions associated with the frequent voiding and difficulty making it in time.
Rationale for incorrect answers:
1. Incontinence is to be expected in a woman her age: This is a common myth. While the risk of incontinence increases with age due to physiological changes, it is not a normal or inevitable part of aging. It should always be investigated as a treatable condition rather than dismissed as expected.
2. One of every 10 nursing home residents is incontinent: This statistic is significantly underestimated. Research suggests that over 50% (and some studies suggest up to 75%) of nursing home residents experience some form of urinary incontinence.
4. An indwelling catheter should be inserted as soon as possible: This is a last resort intervention. Indwelling catheters carry a high risk of infection (CAUTI) and tissue trauma. They should never be used for the convenience of staff or as a first-line treatment for an ambulatory, alert client.
Test taking strategy:
In nursing care planning, always follow the least invasive to most invasive hierarchy.
- Kegels (3) are non-invasive and health-promoting.
- Catheters (4) are highly invasive and risky.
- Options 1 and 2 are passive statements that don't involve a nursing action.
Take home points:
- Never accept incontinence as a normal consequence of getting older. Nursing care should always focus on rehabilitation and bladder health.
- Pelvic floor exercises are a gold-standard, non-invasive intervention for both stress and urge incontinence, even in the elderly population.
A client who is an alert, ambulatory, older nursing home resident, voids frequently and has difficulty making it to the bathroom in time. The priority treatment option for this client would most likely involve which of the following?
Explanation
Urge incontinence is a type of urinary incontinence characterized by a sudden, intense urge to urinate followed by involuntary leakage before reaching a toilet; it is commonly caused by overactive bladder contractions due to neurological conditions, bladder irritation, or idiopathic factors. Management includes bladder training, pelvic floor exercises, lifestyle modifications such as reducing caffeine and alcohol, and medications like antimuscarinics or beta-3 agonists, with surgical options reserved for refractory cases.
Rationale for correct answer:
1. Behavioral techniques: For an alert and ambulatory client, behavioral techniques (such as bladder training, prompted voiding, and Kegel exercises) are the first-line, priority treatment. They have no side effects, cost nothing, and address the root cause of the frequent voiding and urgency.
Rationale for incorrect answers:
2. Pharmacologic measures: While medications like anticholinergics can be used for urge incontinence, they are considered second-line treatments. In older adults, these drugs often cause significant side effects like confusion, dry mouth, and constipation.
3. Surgical intervention: Surgery is usually reserved for specific structural issues like a prolapsed bladder or severe stress incontinence after conservative treatments have failed. It is the most invasive option and carries the highest risk for an older adult.
4. Use of absorbent products: Absorbent products (pads or diapers) are a management strategy, not a treatment. While they keep the client dry in the short term, they do not help fix the bladder issue and can lead to skin breakdown if used as a substitute for actual care.
Test taking strategy:
Nursing exams prioritize interventions that are safe, effective, and non-pharmacological first.
- Behavioral - Safest and least invasive.
- Pharmacologic - Risk of side effects or toxicity.
- Surgical - Risk of complications or infection.
- Absorbent Products - Avoidance of the problem.
Take home points:
- Nursing standards emphasize that behavioral therapies should be attempted before moving to medications or surgery.
- The facts that she is alert (can follow instructions) and ambulatory (can physically get to the toilet) make behavioral therapy the most logical and effective priority.
A client taking phenazopyridine should be cautioned that her urine may change to what color?
Explanation
Phenazopyridine is a urinary tract analgesic used to relieve discomfort such as burning, pain, urgency, and frequency associated with urinary tract infections or irritation; it works locally by exerting a soothing effect on the mucosa of the urinary tract but does not treat the underlying infection. It is typically taken orally for short-term use alongside antibiotics.
Rationale for correct answer:
3. Orange-red: Phenazopyridine is excreted directly into the urine, where it causes a very distinct, bright orange to reddish discoloration. This is a harmless, expected side effect, but it can be alarming to patients if they are not warned, as it can be mistaken for blood (hematuria).
Rationale for incorrect answers:
1. Pale yellow is the color of normal, dilute urine. Phenazopyridine is a potent dye that significantly alters the appearance of urine; it would not result in a normal appearance.
2. Green urine is less common and can be caused by certain medications (like amitriptyline or propofol), pseudomonas infections, or specific food dyes. It is not an expected side effect of phenazopyridine.
4. Brown or tea-colored urine is often associated with liver dysfunction, severe dehydration, or certain antibiotics like nitrofurantoin or metronidazole. While phenazopyridine can look very dark, its primary characteristic is the vibrant orange hue.
Test taking strategy:
- Categorize medications by their most famous distinguishing feature.
- In nursing exams, phenazopyridine is almost exclusively tested on its ability to turn secretions orange.
Take home points:
- Always warn patients that phenazopyridine will stain their urine (and potentially contact lenses or clothing) to prevent unnecessary anxiety.
- Remind patients that this medication only treats the pain of a UTI, not the infection itself. They must finish their entire course of antibiotics.
A nurse is caring for a client who is 60 years old and alert. He is timid and reluctant to talk about his urinary retention problem. Which part of this plan could create stress for the client and possibly increase his inability to urinate?
Explanation
Urinary retention is the inability to completely empty the bladder despite urine being produced by the kidneys and reaching the bladder; it may be acute, presenting suddenly with painful inability to void, or chronic, with gradual incomplete emptying and frequent dribbling. Causes include obstruction (such as enlarged prostate or urethral stricture), neurological disorders affecting bladder innervation, certain medications, or postoperative effects.
Rationale for correct answer:
3. Staying with him while voiding: For a client who is already timid and reluctant to discuss the issue, having a staff member stand over him or remain in the immediate vicinity while he tries to void can create significant performance anxiety. This stress triggers the sympathetic nervous system, which tightens the urinary sphincter and makes urination physically more difficult.
Rationale for incorrect answers:
1. Assisting him in assuming his normal voiding position: This is a positive intervention. For most men, standing is the natural position for urination. Using gravity and familiar body mechanics helps relax the urethral sphincter and facilitates bladder emptying.
2. Pulling curtains around him to provide privacy: This is a standard nursing intervention that reduces stress. Privacy is essential for relaxation; a lack of privacy is more likely to cause shy bladder (paruresis) and worsen retention.
4. Offering the urinal on a regular schedule: This is a helpful, proactive nursing action. Regular timed voiding helps prevent the bladder from overstretching, which can weaken the detrusor muscle and worsen retention.
Test taking strategy:
- Look at the options through the lens of patient privacy vs. observation.
- Options 1, 2, and 4 all promote comfort or routine. Option 3 is the only one that involves an invasive presence.
- In nursing, if a patient is alert, you should always choose the option that maximizes their privacy unless they are a high fall risk.
Take home points:
- Stress and embarrassment directly impact the body's ability to perform involuntary and semi-voluntary functions like voiding.
- For alert and oriented patients, maintaining dignity through privacy is often the most effective medical intervention for urinary issues.
A client has a nursing diagnosis of Impaired Urinary Elimination related to maturational enuresis. The nurse recognizes that their client is which of the following?
Explanation
Maturational enuresis refers to involuntary urination, most commonly bedwetting at night, that occurs in children beyond the age when bladder control is typically expected; it is considered a developmental delay rather than a pathological condition.
Rationale for correct answer:
2. A child older than 4 years: Enuresis is the medical term for bedwetting or involuntary voiding. “Maturational” implies that the child has reached an age typically age 4 or 5, where voluntary bladder control is developmentally expected, but has not yet achieved it. Before age 4, involuntary voiding is considered a normal developmental stage.
Rationale for incorrect answers:
1. An adult older than 65 years: Involuntary urination in an older adult is referred to as urinary incontinence. This is typically related to physical issues like weakened pelvic floor muscles, prostate enlargement, or cognitive decline.
3. A 12-month-old child: Involuntary urination is a normal physiological state for a 1-year-old. At this age, the nervous system has not matured enough to control the external urethral sphincter. Therefore, it cannot be diagnosed as impaired elimination or enuresis; it is simply developmental.
4. A client with neurologic damage: This is known as a neurogenic bladder. While it results in impaired elimination, the cause is structural or traumatic damage to the nerves (like a spinal cord injury), not a delay in the natural maturational process of growing up.
Test taking strategy:
- Focus on the keyword “maturational.” This points to developmental delay, not disease, injury, or aging.
- Eliminate extremes (very young infants and elderly adults).
- Ask yourself: “Who should normally have bladder control by now but doesn’t?”
Take home points:
- Enuresis is only considered a problem once the child has passed the age where bladder control is socially and physiologically expected (usually 4–5 years).
- Maturational specifically refers to the developmental timeline of the central nervous system's control over the bladder.
A nurse caring for an older client must collect data to evaluate the effectiveness of a plan to reduce urinary incontinence. Of the information below, which is least important for the evaluation process?
Explanation
Urinary incontinence is managed first with conservative measures such as pelvic floor muscle training (Kegel exercises), bladder training, weight reduction, and dietary adjustments. For urge incontinence, medications like anticholinergics or beta-3 agonists may be prescribed, while stress incontinence can benefit from pelvic floor physiotherapy, continence devices, or surgical options such as mid-urethral slings. Overflow incontinence often requires catheterization or addressing underlying obstruction, and functional incontinence is managed by treating the contributing cause (e.g., mobility issues).
Rationale for correct answer:
4. Age of the client: While age is a factor in health, incontinence is not a normal part of aging. Knowing the specific age does not help evaluate the effectiveness of a treatment plan. The focus should be on the client's functional status and symptoms, not their chronological age.
Rationale for incorrect answers:
1. The incontinence pattern: To evaluate if a plan is working, you must compare current data against the baseline. Knowing when, where, and how often the client is incontinent helps determine if the frequency has decreased or if the interventions like scheduled voiding are effective.
2. State of physical mobility: Functional incontinence is often caused by the inability to reach the toilet in time. If the plan includes mobility exercises or assistive devices, evaluating the client's current movement status is crucial to seeing if physical improvements are aiding continence.
3. Medications being taken: Many medications (diuretics, sedatives, or anticholinergics) can cause or worsen incontinence. Monitoring these is vital to see if pharmacological side effects are hindering the success of the nursing plan.
Test taking strategy:
- Strategic word recognition: Look for the word “Least.” This indicates you are looking for an outlier-the piece of data that does not change or provide dynamic feedback during an evaluation.
- Because the client is already identified as older, their specific age is a static demographic variable, whereas the other three options are dynamic clinical variables that change as the client's condition improves or declines.
Take home points:
- Never assume incontinence is an expected outcome of aging; it is always a symptom that requires assessment and intervention.
- Evaluation is about measuring change. Choose the options that represent measurable data points (patterns, mobility, meds) rather than fixed data points (age).
A client is scheduled to have an intravenous pyelogram (IVP) tomorrow morning. Which nursing measures should be implemented before the test? Select all that apply
Explanation
An Intravenous pyelogram (IVP) is an X-ray imaging test used to evaluate the urinary tract - including the kidneys, ureters, and bladder - by injecting a contrast dye into a vein, which highlights these structures as it flows through them. The procedure helps doctors assess the shape, size, and function of the urinary system and detect problems such as kidney stones, tumors, urinary tract blockages, infections, or congenital abnormalities.
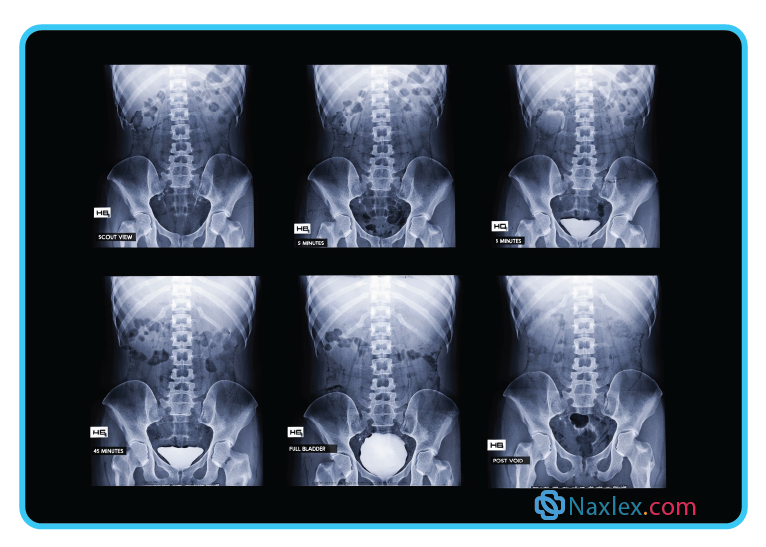
Rationale for correct answer:
1. Ask about allergies: An IVP involves injecting radiopaque contrast dye, which often contains iodine. The nurse must assess for allergies to iodine, shellfish, or previous reactions to contrast media to prevent anaphylaxis.
4. Informed consent: Since the procedure involves the injection of a contrast medium and carries risks (allergic reaction, kidney stress), the nurse must verify that the physician has explained the risks and the client has signed the consent form.
5. Facial flushing: It is a common, non-allergic side effect for clients to feel a sudden sensation of warmth, facial flushing, or a metallic taste in the mouth immediately after the dye is injected. Warning the client prevents anxiety during the test.
Rationale for incorrect answers:
2. Full bladder required: Unlike a pelvic ultrasound, an IVP does not require a full bladder. In fact, the client is usually asked to void before the procedure to ensure the bladder doesn't obstruct the view of the pelvic structures.
3. Save all urine: This is a requirement for a 24-hour urine collection, not an IVP. There is no need to save urine samples prior to this imaging test.
Test taking strategy:
- Recognize that an IVP is a contrast-dye study of the kidneys, ureters, and bladder.
- Whenever a question mentions contrast dye, your brain should immediately link to three things: allergies (iodine/shellfish), kidney function (creatinine), and expected sensations (flushing/warmth).
- Use the process of elimination to remove tasks related to other tests (like urine collection or ultrasounds).
Take home points:
- The priority nursing action for any contrast test (angiogram, pyelogram) using dye is always checking for allergies and protecting the kidneys.
- Warning a patient about the hot flash or metallic taste of contrast dye is a standard of care to ensure they don't panic and move during the imaging.
A nurse is inserting an indwelling catheter into a male client. What is a critical step?
Explanation
An indwelling catheter, commonly called a Foley catheter, is a flexible tube inserted into the bladder through the urethra and left in place to provide continuous urine drainage; it is held in position by a small balloon inflated inside the bladder. Indwelling catheters are used when patients cannot empty their bladder naturally, such as in cases of urinary retention, surgery, severe incontinence, or critical illness requiring accurate urine output monitoring.
Rationale for correct answer:
3. Advance to the bifurcation: In males, the urethra is significantly longer than in females. To ensure the balloon is entirely inside the bladder and not still within the prostatic urethra, the nurse must advance the catheter all the way to the Y connector (bifurcation). Inflating the balloon in the urethra can cause severe trauma and permanent scarring.
Rationale for incorrect answers:
1. Slowly inflate with sterile saline: While balloons are inflated with liquid, sterile water is used, not saline. Saline can crystallize over time, causing the balloon to get stuck or the valve to malfunction. Furthermore, inflation should only happen after correct placement is confirmed.
2. Secure to bedsheets: The drainage tubing should never be secured to the bedsheets because if the client moves, the catheter could be pulled or tensioned. The catheter should be secured to the client's thigh or abdomen to prevent urethral trauma.
4. Advance until urine flows, then insert 1/4 inch more: This is a technique often used for female clients. For males, seeing urine flow only confirms the tip is in the bladder; however, since the balloon is further down the shaft, the catheter must be advanced much further to the bifurcation before inflation.
Test taking strategy:
- When a question specifies male vs female, the answer usually hinges on anatomical differences.
- The male urethra is roughly 7–8 inches long. If you only insert a small amount past the point of urine return, the balloon might still be in the urethra.
- Advancing to the bifurcation is the gold standard safety measure for male catheterization to prevent urethral injury.
Take home points:
- Advancing to the bifurcation in males ensures the balloon is in the bladder vault before inflation, protecting the prostatic urethra.
- Always use sterile water for balloon inflation to prevent the mechanical failure of the inflation valve due to salt crystallization.
The nurse is inserting a urinary catheter for a female client, and after the catheter has been inserted 3 inches, no urine is returned. What should the nurse do next?
Explanation
When a urinary catheter in females has been inserted about 3 inches and no urine is returned, it usually indicates that the catheter has not yet reached the bladder or accidentally placed in vagina. If a urinary catheter is accidentally inserted into the vagina instead of the urethra, no urine will return, since the catheter is not in the bladder.
Rationale for correct answer:
2. Leave it there and start over: If no urine returns after 3 inches, the catheter is likely in the vagina rather than the urethra. By leaving the wrongly placed catheter in the vaginal opening, it acts as a visual landmark. This helps the nurse avoid making the same mistake twice and ensures the new, sterile catheter is inserted into the meatus (which is located just above the vaginal opening).
Rationale for incorrect answers:
1. Remove and start over with a new kit: While you do need a new catheter, you don't necessarily need an entirely new sterile kit if your sterile field is still intact. More importantly, removing the misplaced catheter first loses your visual marker.
3. Pull back and reinsert at a different angle: Once the catheter has entered the vagina, it is considered contaminated. You cannot pull it back and put it into the sterile urethra; doing so would introduce vaginal bacteria into the urinary tract, significantly increasing the risk of infection.
4. Ask to bear down and insert farther: While bearing down can help relax the external sphincter, if the catheter is already in the vagina, pushing it farther will not produce urine and does not solve the placement error.
Test taking strategy:
- In nursing exams, when a catheter is accidentally placed in the vagina, the priority is infection control and accuracy.
- The answer is always to leave the first catheter in place as a “marker” for where not to go, then use a second sterile catheter to find the meatus.
Take home strategy:
- If a sterile object touches a non-sterile cavity like the vagina, it can never be used in a sterile cavity the bladder during that procedure.
- Leaving the misplaced catheter in the vagina is a physical strategy to block that path and help you visualize the correct anatomy for the second attempt.
A nurse should implement which nursing interventions when removing an indwelling urinary catheter in an adult client? Select all that apply
Explanation
Catheter removal is a simple but sterile procedure aimed at preventing infection and ensuring patient comfort. The process begins with hand hygiene and donning gloves, followed by deflating the retention balloon for indwelling catheters using a syringe to withdraw the sterile water. Once deflated, the catheter is gently and steadily withdrawn from the urethra without force. The patient is then observed for spontaneous urination, discomfort, or signs of urinary retention.
Rationale for correct answers:
2. Drain by gravity: To ensure the balloon is completely deflated and to avoid ridging the balloon which can cause urethral trauma, the nurse should pull back slightly on the plunger to start the flow and then allow the fluid to return into the syringe naturally by gravity.
3. Initiate a voiding record: After removal, the nurse must monitor for urinary retention. The client should be able to void within 6 to 8 hours. A voiding record (bladder diary) tracks the time and amount of the first few voids to ensure the bladder is functioning correctly after the catheter is gone.
Rationale for incorrect answers:
1. Attach a 3-mL syringe: Most indwelling catheter balloons are inflated with 5 mL to 10 mL of sterile water. Using a 3-mL syringe would be insufficient to fully deflate the balloon. You must check the size of the balloon usually printed on the inflation port and use a syringe large enough to hold all the fluid.
5. Clamp the catheter before removal: Bladder training by clamping the catheter before removal is an outdated practice and is no longer recommended by evidence-based guidelines, as it does not actually improve bladder tone and can increase infection risk.
Test taking strategy:
When removing an appliance, focus on two things: preventing trauma (deflating the balloon correctly) and evaluating function (monitoring the first void).
Take home points:
- Always ensure the volume of water removed matches the volume originally injected into the balloon to prevent pulling an inflated balloon through the urethra.
- After a catheter is removed, the clock starts. If the patient hasn't voided within 6 to 8 hours (or sooner if they are in pain), the nurse must assess for bladder distention.
Exams on Urinary Elimination
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
To:
- Describe the process of urination, from urine formation through micturition.
- Identify factors that influence urinary elimination.
- Identify common causes of selected urinary problems.
- Describe nursing assessment of urinary function, including subjective and objective data.
- Identify normal and abnormal characteristics and constituents of urine.
- Describe nursing interventions to maintain normal urinary elimination, prevent urinary tract infection, and manage urinary incontinence.
- Delineate ways to prevent urinary infection.
- Explain the care of clients with retention catheters or urinary diversions.
- Verbalize the steps used in: a. Applying an external urinary device. b. Performing urinary catheterization. c. Performing bladder irrigation.
Introduction
Elimination from the urinary tract helps to rid the body of waste products and materials that exceed bodily needs.
The client’s ability to manage urinary elimination and any cultural considerations related to urinary elimination patterns need to be assessed.
During acute illness, a patient may require urinary catheterization for close monitoring of urine output or to facilitate bladder emptying when bladder function is impaired.
Some patients require long-term indwelling urethral or suprapubic catheters when the bladder fails to empty effectively
Physiology of urinary elimination
1.1 PHYSIOLOGY OF URINARY ELIMINATION
Urinary elimination depends on the coordinated function of the upper urinary tract (kidneys and ureters) and the lower urinary tract (bladder, urethra, and pelvic floor).
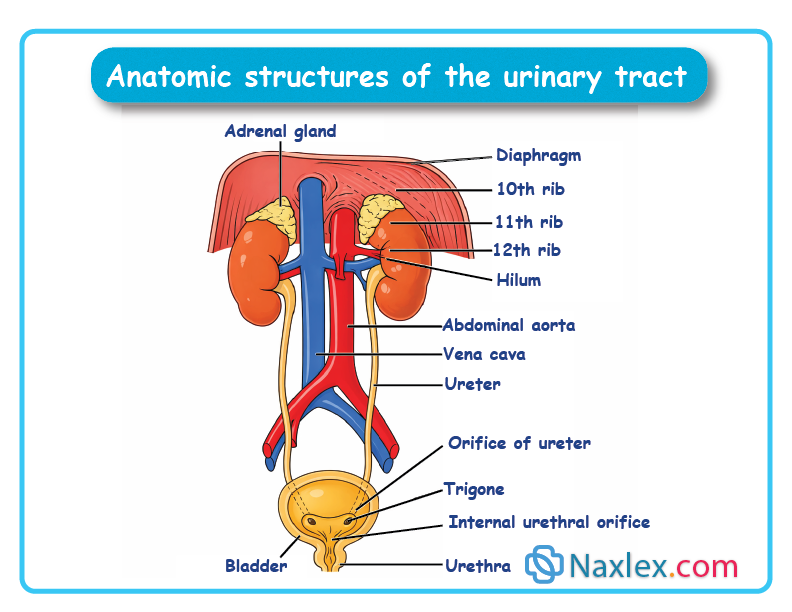
1. Kidneys
Location & Function
- Paired organs located on either side of the spine, behind the peritoneum. Right kidney sits slightly lower than the left due to the liver
- Primary functions:
- Regulate fluid balance
- Maintain acid–base balance
- Remove metabolic wastes
Blood Flow & Nephrons
- Receive ~21% of cardiac output (≈1,200 mL/min)
- Each kidney contains ~1 million nephrons
- Nephron is the functional unit of the kidney
Nephron Structure & Filtration
- Glomerulus: network of capillaries inside Bowman’s capsule
- Glomerular membrane is porous:
- Allows water, electrolytes, glucose, amino acids, and wastes to pass
- Blocks proteins and blood cells
- Resulting fluid = glomerular filtrate
Tubular Processing
- Proximal Convoluted Tubule
- Majority of water and electrolytes reabsorbed
- Loop of Henle
- Reabsorption of solutes (e.g., glucose)
- Secretion of substances - concentrates urine
- Distal Convoluted Tubule
- Final regulation of water and sodium under hormonal control
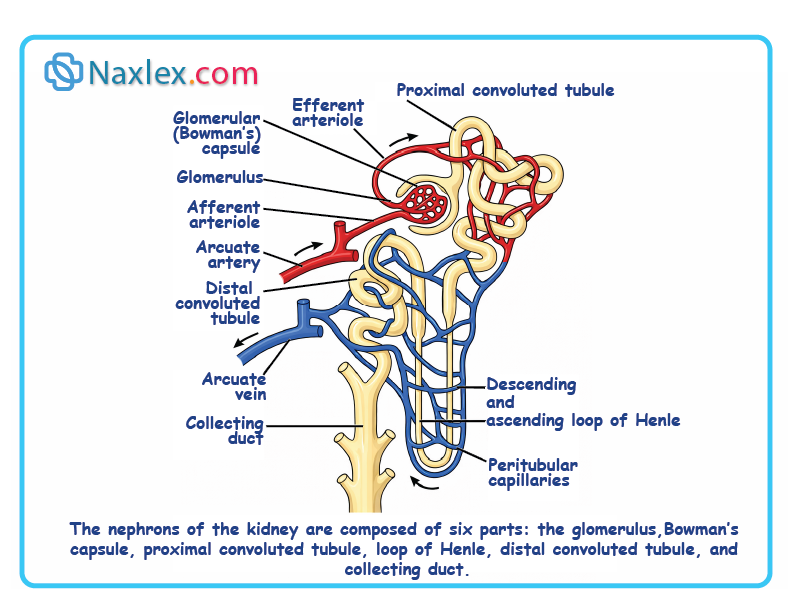
Hormonal Regulation
- Antidiuretic Hormone (ADH)
- Released when fluid intake is low or blood solutes are high. Increases water reabsorption - less urine. Suppressed when fluid intake is high - more urine
- Aldosterone
- Increases sodium and water reabsorption. Increases blood volume, decreased urinary output
2. Ureters
- Transport urine from kidneys to bladder. Length: 25–30 cm, diameter: ~1.25 cm
- Upper end: funnel-shaped at kidney. Enter bladder at posterior corners
- Flaplike valve at bladder entrance prevents reflux
3. Urinary Bladder
Structure & Location
- Hollow, muscular organ that: Stores urine, expels urine during voiding.
- Location:
- Men: anterior to rectum, above prostate
- Women: anterior to uterus and vagina
Bladder Wall Layers
- Mucous layer
- Connective tissue
- Detrusor muscle (3 smooth muscle layers)
- Serous layer
Detrusor Muscle
- Allows bladder to:
- Expand during filling
- Contract during voiding
Trigone
- Triangular area at base of bladder
- Formed by:
- Two ureter openings
- One urethral opening
Capacity
- Normal adult capacity: 300–600 mL
- Distention aided by rugae and elastic walls
- Overfilled bladder may rise above symphysis pubis
4. Urethra
Female Urethra
- Length: 3–4 cm
- Function: urine elimination only
- Short length and proximity to anus - increases UTI risk
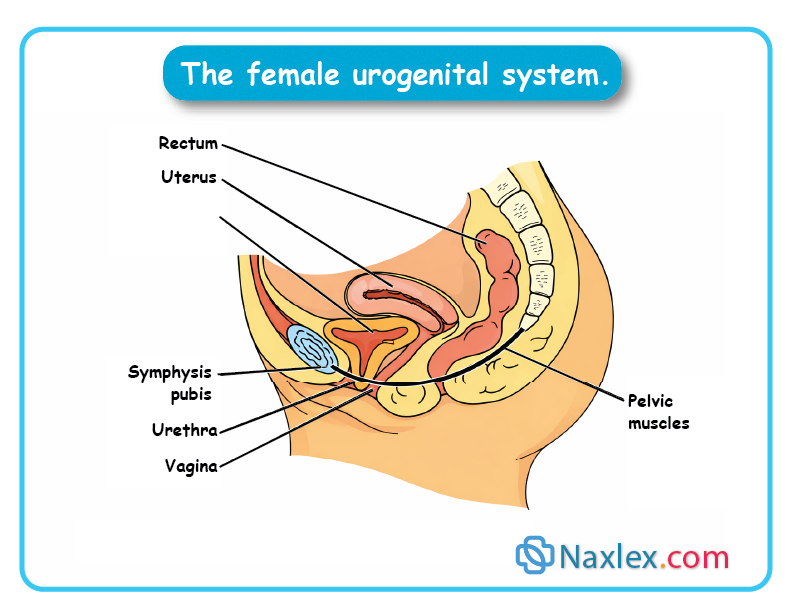
Male Urethra
- Length: ~20 cm. Function: passage for urine and semen
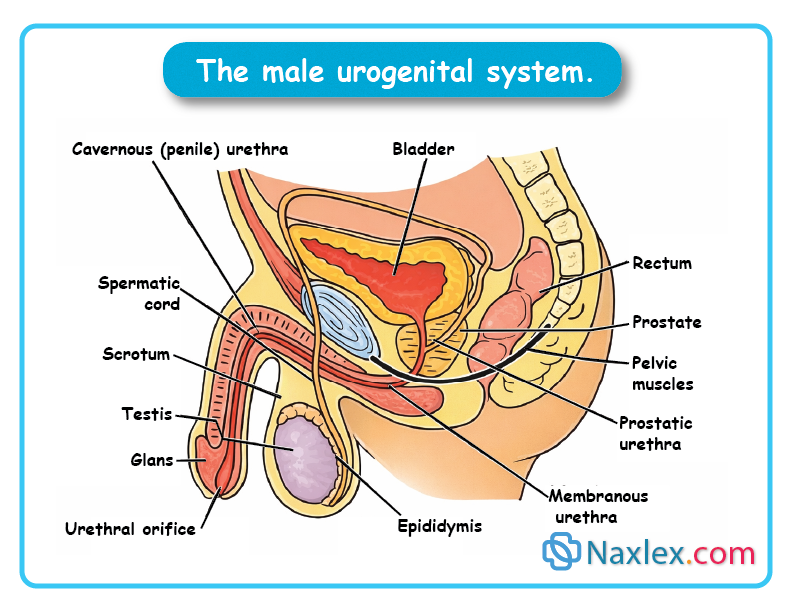
Infection Risk
- Mucosal lining continuous with bladder and ureters
- Infection can ascend to kidneys
- Women are more prone due to anatomy
5. Pelvic Floor & Sphincters
Pelvic Floor
- Muscle and ligament sling from symphysis pubis to coccyx
- Supports bladder, urethra, vagina, and rectum
Sphincters
- Internal Urethral Sphincter
- Smooth muscle
- Involuntary control
- Maintains urethral closure
- External Urethral Sphincter
- Skeletal muscle
- Voluntary control
- Allows conscious control of urination
6. Urination (Micturition)
Initiation
- Urine accumulates in bladder
- Stretch receptors activated at:
- Adults: 250–450 mL
- Children: 50–200 mL
Neural Control
- Stretch receptors send signals to sacral spinal cord (S2–S4) - voiding reflex center
- Effects:
- Internal sphincter relaxes
- Urge to void is perceived
Voluntary Control
- If appropriate:
- Cerebral cortex relaxes external sphincter
- Urination occurs
- If inappropriate:
- Reflex subsides until bladder fills more
Conditions affecting control
- Voluntary urination requires intact:
- Peripheral nerves
- Spinal cord pathways
- Brain motor centers
- Injury (e.g., stroke, spinal cord injury above sacral level): Causes involuntary bladder emptying.
- Older adults with cognitive impairment- may not recognize or respond to urge to void.
1.2 FACTORS AFFECTING VOIDING
Numerous factors affect the volume and characteristics of the urine produced and the manner in which it is excreted.
|
Factor |
Key Points |
|
Developmental – Infants |
• Urine output: 250–500 mL/day by 1 year |
|
Developmental – Preschoolers |
• Independent toileting begins |
|
Developmental – School-age Children |
• Kidneys double in size (ages 5–10) |
|
Developmental – Older Adults |
• Kidney function declines with age |
|
Psychosocial Factors |
• Voiding aided by privacy, normal position, sufficient time, running water |
|
Fluid & Food Intake |
• Fluid intake increases - urine output increases |
|
Medications |
• Autonomic drugs may cause retention |
|
Muscle Tone |
• Good detrusor tone - proper filling/emptying |
|
Pathologic Conditions |
• Kidney disease - protein/blood in urine or renal failure |
|
Surgical & Diagnostic Procedures |
• Cystoscopy - urethral swelling |
1.3 ALTERED URINE PRODUCTION
Although people’s patterns of urination are highly individual, most people void about five to six times a day. People usually void when they first awaken in the morning, before they go to bed, and around mealtimes.
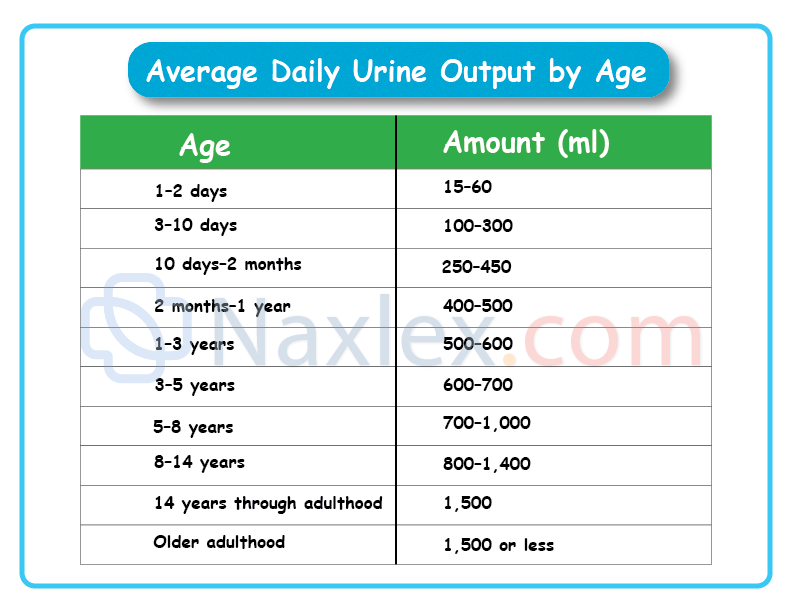
Polyuria
Polyuria (or diuresis) refers to the production of abnormally large amounts of urine by the kidneys, often several liters more than the client’s usual daily output.
Polyuria can follow excessive fluid intake, a condition known as polydipsia, or may be associated with diseases such as diabetes mellitus, diabetes insipidus, and chronic nephritis.
Polyuria can cause excessive fluid loss, leading to intense thirst, dehydration, and weight loss.
Oliguria and Anuria
The terms oliguria and anuria are used to describe decreased urinary output.
Oliguria is low urine output, usually less than 500 mL a day or 30 mL an hour for an adult. Although oliguria may occur because of abnormal fluid losses or a lack of fluid intake, it often indicates impaired blood flow to the kidneys or impending renal failure and should be promptly reported to the primary care provider.
Anuria refers to a lack of urine production. Should the kidneys become unable to adequately function, some mechanism of filtering the blood is necessary to prevent illness and death. This filtering is done through the use of renal dialysis, a technique by which fluids and molecules pass through a semipermeable membrane according to the rules of osmosis.
1.4 ALTERED URINARY ELIMINATION
Despite normal urine production, a number of factors or conditions can affect urinary elimination.
Frequency and Nocturia
Urinary frequency is voiding at frequent intervals, that is, more than four to six times per day. An increased intake of fluid causes some increase in the frequency of voiding. Conditions such as UTI, stress, and pregnancy can cause frequent voiding of small quantities (50 to 100 mL) of urine. Total fluid intake and output may be normal.
Nocturia is voiding two or more times at night. Like frequency, it is usually expressed in terms of the number of times the person gets out of bed to void.
Urgency
Urgency is the sudden, strong desire to void. There may or may not be a great deal of urine in the bladder, but the person feels a need to void immediately. Urgency accompanies psychological stress and irritation of the trigone and urethra. It is also common in people who have poor external sphincter control and unstable bladder contractions.
Dysuria
Dysuria means voiding that is either painful or difficult. It can accompany a stricture (decrease in caliber) of the urethra, urinary infections, and injury to the bladder and urethra. Often clients will say they have to push to void or that burning accompanies or follows voiding. The burning may be described as severe, like a hot poker, or more subdued, like a sunburn.
Often, urinary hesitancy (a delay and difficulty in initiating voiding) is associated with dysuria.
Enuresis
Enuresis is involuntary urination in children beyond the age when voluntary bladder control is normally acquired, usually 4 or 5 years of age.
Nocturnal enuresis often is irregular in occurrence and affects boys more often than girls. Diurnal (daytime) enuresis may be persistent and pathologic in origin. It affects women and girls more frequently.
Urinary Incontinence
Urinary incontinence (UI), or involuntary leakage of urine or loss of bladder control, is a health symptom, not a disease. The four main types of UI are stress urinary incontinence, urge urinary incontinence, mixed urinary incontinence, and overflow incontinence.
- Stress urinary incontinence (SUI) occurs because of weak pelvic floor muscles and/or urethral hypermobility, causing urine leakage with such activities as laughing, coughing, sneezing, or any body movement that puts pressure on the bladder. Facts that make women more likely to experience SUI include shorter urethras, the trauma to the pelvic floor associated with childbirth, and changes related to menopause. For men, SUI may result after a prostatectomy.
- Urge urinary incontinence: This type of incontinence is described as an urgent need to void and the inability to stop micturition (passage of urine). The urine leakage can range from a few drops to soaking of undergarments. Urge incontinence is a major symptom of an overactive bladder.
- Mixed urinary incontinence: Mixed incontinence is diagnosed when symptoms of both stress UI and urgency UI are present. It is very common among middle-age and older women.
- Overflow incontinence: This is continuous involuntary leakage or dribbling of urine that occurs with incomplete bladder emptying. It can be seen in men with an enlarged prostate and clients with a neurologic disorder (e.g., multiple sclerosis, Parkinson’s disease, spinal cord injury). An impaired neurologic function can interfere with the normal mechanisms of urine elimination, resulting in a neurogenic bladder. The client with a neurogenic bladder does not perceive bladder fullness and is therefore unable to control the urinary sphincters. The bladder may become flaccid and distended or spastic, with frequent involuntary urination.
Urinary Retention
When emptying of the bladder is impaired, urine accumulates and the bladder becomes overdistended, a condition known as urinary retention. Overdistention of the bladder causes poor contractility of the detrusor muscle, further impairing urination. Common causes of urinary retention include prostatic hypertrophy (enlargement), surgery, and some medications.
Nursing management of urinary function
1.1 Assessing
- Components:
- Nursing history
- Physical assessment (GU system, hydration, skin, urine exam)
- Relating findings to diagnostic tests
- Nursing History:
- Normal voiding pattern/frequency
- Urine appearance & recent changes
- Past/current urinary problems
- Presence of ostomy
- Influencing factors (fluid intake, habits, stress)
- Physical Assessment:
- Percussion of kidneys (tenderness)
- Palpation/percussion of bladder
- Inspect urethral meatus (swelling, discharge, inflammation)
- Assess skin (color, turgor, edema, perineal irritation if incontinent)
Assessing Urine
- Composition:
- 96% water, 4% solutes
- Organic: urea (chief), ammonia, creatinine, uric acid
- Inorganic: Na⁺, Cl⁻, K⁺, sulfate, Mg²⁺, phosphorus
- Normal Output:
- ~60 mL/hr (≈1,500 mL/day)
- <30 mL/hr - report (possible hypovolemia or renal malfunction)
- Color Variations:
- Normal pale yellow Abnormal: red (blood/beets), dark (bilirubin), cloudy (infection)
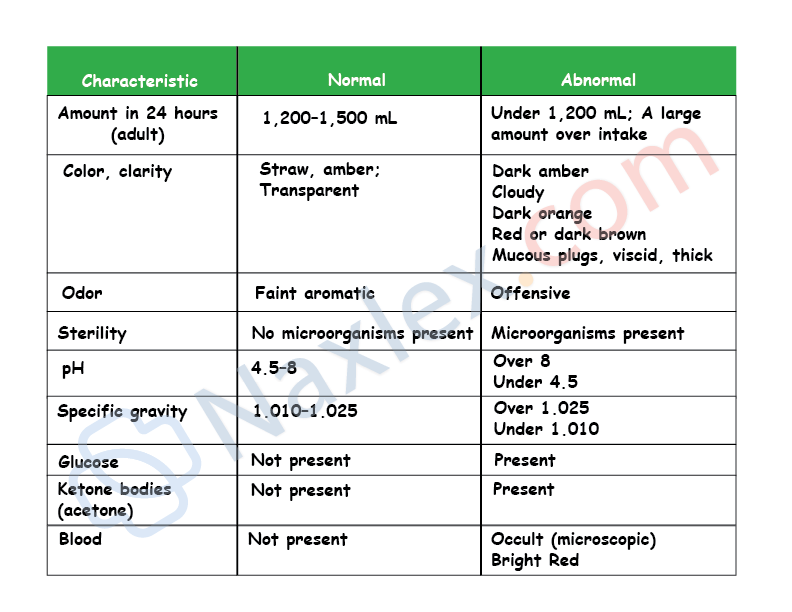
Measuring Urinary Output
- General Steps:
- Gloves, clean collection device
- Keep urine separate from feces/toilet paper
- Pour into calibrated container, read at eye level
- Record on I&O sheet
- Rinse equipment, hand hygiene
- Document totals per shift & 24 hrs
- Catheterized Clients:
- Gloves, calibrated container under bag spout
- Drain urine without contaminating sterile system
- Record as above
Measuring Residual Urine (PVR)
- Normal: 50–100 mL
- Abnormal: increased retention due to obstruction (e.g., enlarged prostate) or poor bladder tone
- Manifestations: frequent small voids (<100 mL), stasis, UTI
- Measurement: post-void catheterization or bladder scan
- Intervention: indwelling catheter if PVR exceeds threshold
1.2 Diagnosing
Diagnostic Tests
- Blood Urea Nitrogen (BUN): end product of protein metabolism
- Serum Creatinine: constant production by muscles
- Creatinine Clearance: 24-hr urine + serum creatinine - GFR (sensitive renal function indicator)
- Other: urine specimens, specific gravity, imaging/visualization procedures
NANDA Labels
- General:
- Impaired Urinary Elimination
- Readiness for Enhanced Urinary Elimination
- Specific:
- Functional, Overflow, Reflex, Stress, Urge Incontinence
- Risk for Urge Incontinence
- Urinary Retention
- Associated Problems:
- Risk for Infection (retention, invasive procedures)
- Low Self-Esteem / Social Isolation (incontinence)
- Risk for Impaired Skin Integrity (urine-soaked linens)
- Toileting Self-Care Deficit
- Fluid Volume Imbalance
- Disturbed Body Image (ostomy)
- Deficient Knowledge (self-care skills)
- Caregiver Role Strain
1.3 Planning
Planning Goals
- Maintain/restore normal voiding pattern
- Regain normal urine output
- Prevent risks: infection, skin breakdown, electrolyte imbalance, low self-esteem
- Promote independent toileting (with/without devices)
- Contain urine appropriately (catheter, ostomy, absorbent products)
Planning for Home Care
- Discharge Planning:
- Assess client/family resources & abilities
- Financial resources
- Need for referrals/home health services
- Client Teaching:
- Self-care skills (e.g., ostomy management)
- Hygiene practices
- Monitoring output
- When to seek help (e.g., retention, infection signs)
1.4 Implementation
I. Maintaining normal urinary elimination
Most interventions are independent nursing functions aimed at promoting natural function and preventing complications.
- Fluid Intake:
- Goal: Average 1,500 mL/day for healthy adults.
- High Risk (UTI/Stones): Increase to 2,000–3,000 mL/day to dilute urine and flush the system.
- Increased Needs: Clients with diaphoresis (sweating), vomiting, diarrhea, or wound drainage.
- Contraindications: Fluid restrictions are required for clients with kidney failure or heart failure to prevent edema/overload.
- Voiding Habits: Help clients maintain their normal routine even when hospitalized.
- Assisting with Toileting: Stay with fall-risk clients.
- Ensure access to call signals and handrails.
- Provide bedside equipment (urinals, commodes) if the bathroom is inaccessible.
II. Preventing urinary tract infections (UTIs)
Women are at higher risk due to a shorter urethra and proximity to the anus. Most infections are caused by E. coli.
Patient Education Checklist:
- Hygiene: Always wipe front to back.
- Hydration: Drink eight 8-ounce glasses of water daily.
- Voiding Habits: Void every 2–4 hours and immediately after intercourse.
- Clothing: Wear cotton underwear (not nylon) and avoid tight-fitting pants.
- Avoid Irritants: No harsh soaps, bubble baths, or perineal sprays.
- Showers over Baths: Prevents bacteria in bathwater from entering the urethra.
III. Managing Urinary incontinence (UI)
Note: UI is NOT a normal part of aging.
- Assessment Tip: Clients may deny incontinence due to stigma. Ask specifically: “Do you leak urine when you cough or sneeze?”
- Bladder Retraining:
- Used for urge incontinence.
- Goal: Gradually lengthen intervals between voiding.
- Technique: Use deep, slow breathing to inhibit the premature urge to void.
- Habit Training: Scheduled toileting (e.g., every 2–4 hours) to keep bedridden or cognitively impaired clients dry.
- Pelvic Floor Muscle (Kegel) Exercises: Identify muscles by squeezing the anal sphincter.
- Perform quick (2-sec) and slow (up to 10-sec) contractions.
- Skin Integrity: Urine converts to ammonia, causing skin breakdown (maceration).
- Action: Clean with mild soap/no-rinse cleanser; apply barrier creams; use absorbent pads that keep the surface dry.
IV. Urinary Catheterization
Catheterization is a last resort due to the high risk of CAUTI (Catheter-Associated Urinary Tract Infection).
Types of catheters:
|
Type |
Description |
Use Case |
|
Straight |
Single lumen; drained then removed. |
Intermittent emptying, sterile specimen. |
|
Foley (Retention) |
Double lumen (one for urine, one for balloon). |
Continuous drainage. |
|
Coudé |
Curved, stiff tip. |
Men with hypertrophied prostate. |
|
Condom Catheter |
External device for males. |
Preferred over indwelling; lower UTI risk. |
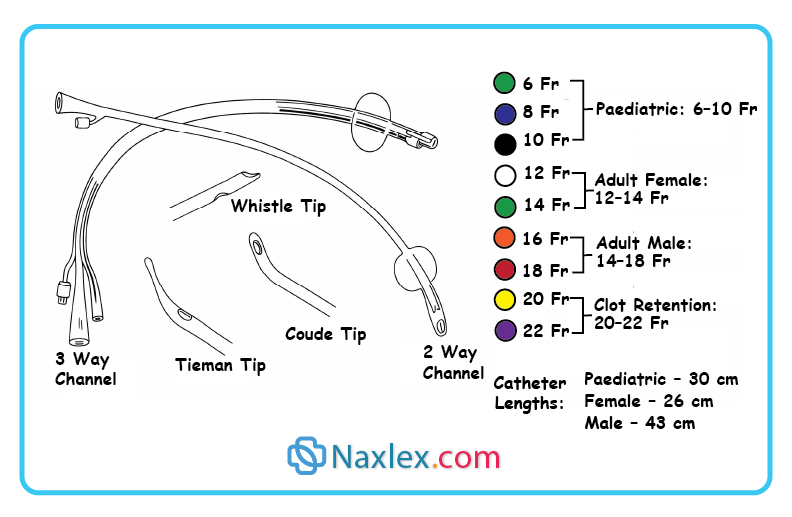
Key safety points:
- Sizing: Measured on the French (Fr) scale (larger number = larger diameter).
- Balloon Safety: Follow manufacturer guidelines; do not pretest silicone balloons as they may crease and cause urethral trauma.
- CAUTI Prevention: The risk of infection increases by 5% for every day the catheter remains in. Remove as soon as medically unnecessary.
- Male Insertion: Position the penis perpendicular to the body to straighten the urethra and reduce trauma.
V. Managing Urinary Retention
- Cholinergic Drugs: e.g., Bethanechol chloride (Urecholine) to stimulate bladder contraction.
- Credé’s Maneuver: Manual pressure on the bladder. Requires a provider’s order; used only for flaccid bladders.
- Intermittent Catheterization: Often preferred over indwelling catheters to reduce UTI risk.
VI. Care of clients with indwelling catheters
Nursing care focuses on preventing infection (CAUTI) and maintaining patency.
- Fluid Management: Encourage up to 3,000 mL/day. High output flushes the bladder, prevents stasis, and keeps sediment from clogging the tube.
- Urinary Acidity: Acidic urine reduces UTI and stone risk.
- Acidifying Foods: Eggs, cheese, meat, whole grains, cranberries, prunes, tomatoes.
- Alkalizing Foods: Most other fruits/veggies, legumes, milk.
- Maintenance: Perform routine perineal hygiene (no special meatal cleaners required).
- Do not change catheters or bags on a routine schedule; change only if sediment accumulates, drainage is impaired, or the system is compromised.
VI. Catheter Removal & Post-Care
- Bladder Retraining: For long-term catheters, the bladder may lose muscle tone. Clamping the catheter for 2–4 hours before removal helps “re-train” the bladder to distend and contract.
- Removal Procedure:
- Deflation: Use a syringe to withdraw all fluid. Note: Rapid “active” deflation causes more “cuffing” (ridges on the balloon) which can cause discomfort. Passive autodeflation is gentler.
- Post-Removal Monitoring: Record time, amount, and clarity of the first void.
- Retention Check: If the client voids < 100 mL at a time, check Post-Void Residual (PVR) with a bladder scanner. PVR > 200 mL usually requires a straight catheter.
VII. Specialized Catheterization & Irrigations
- Clean Intermittent Self-Catheterization (CISC):
- Used for neurogenic bladder (e.g., MS, spinal cord injury).
- Technique: Medical asepsis (clean technique) at home.
- Criteria: Client needs manual dexterity, mental capacity, and a bladder capacity > 100 mL.
- Bladder Irrigations:
- Closed System (Preferred): Uses a triple-lumen (three-way) catheter. Common after GU surgery to prevent blood clots from occluding the tube.
- Open System: Higher infection risk; only used to restore patency when the catheter is blocked by thick mucous or clots.
VIII. Suprapubic catheters
Inserted surgically through the abdominal wall above the symphysis pubis.
- Indications: Long-term use or when the urethra is bypassed (trauma/surgery).
- Site Care: Use sterile technique for dressings until the tract is healed (6 weeks to 6 months).
- Emergency: If a temporary suprapubic catheter falls out, it must be replaced within 30 minutes to prevent the tract from closing.
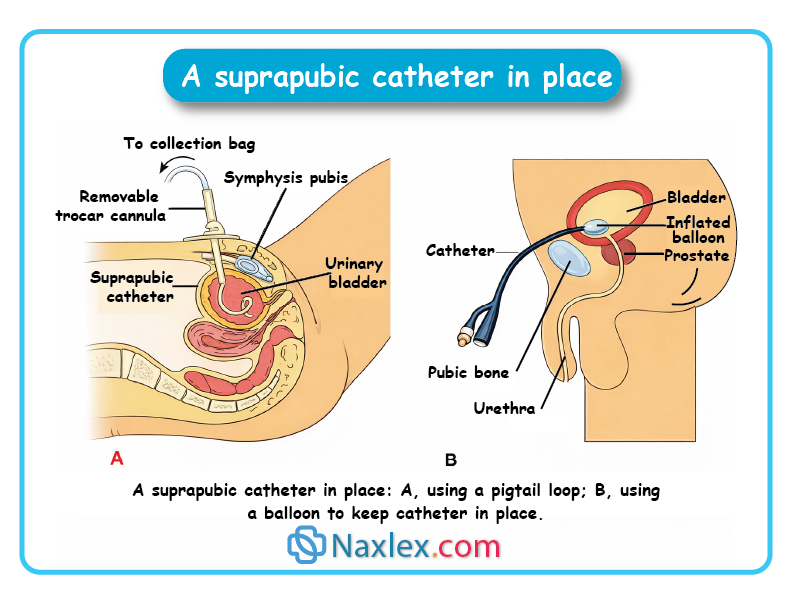
IX. Urinary Diversions
Surgical rerouting of urine, common in bladder cancer (cystectomy).
1. Incontinent Diversions (Require an external bag)
- Ileal Conduit (most common): A loop of the ileum (small intestine) is used as a passageway for urine to a stoma. Note: Mucous shreds in urine are normal due to the intestinal lining.
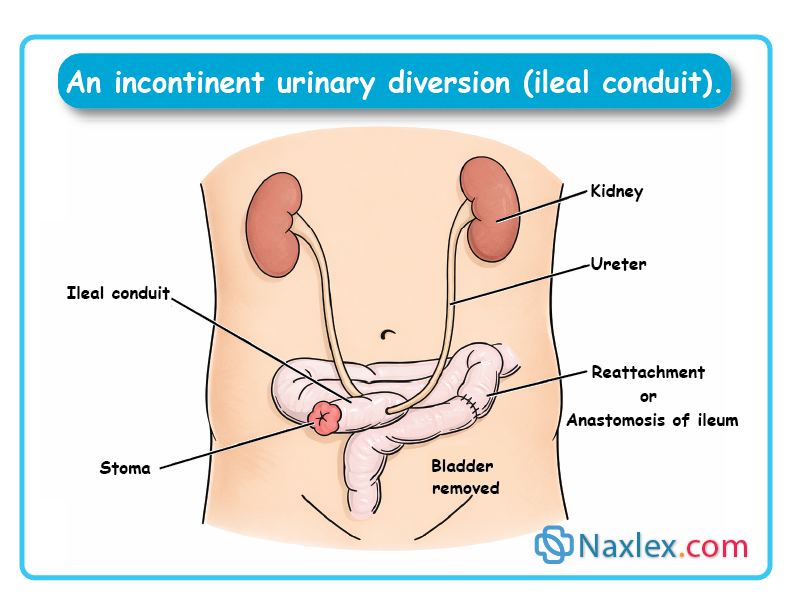
- Nephrostomy: A tube goes directly into the renal pelvis of the kidney.
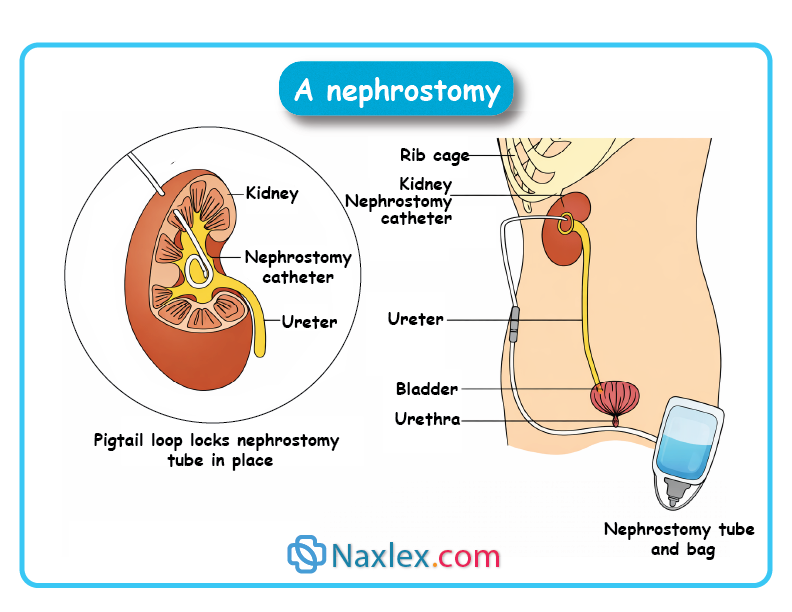
- Vesicostomy: Bladder is intact but sutured to an opening in the skin.
2. Continent Diversions (Client controls drainage)
- Kock Pouch: An internal ileal reservoir with “valves.” The client must self-catheterize the stoma every 2–6 hours.
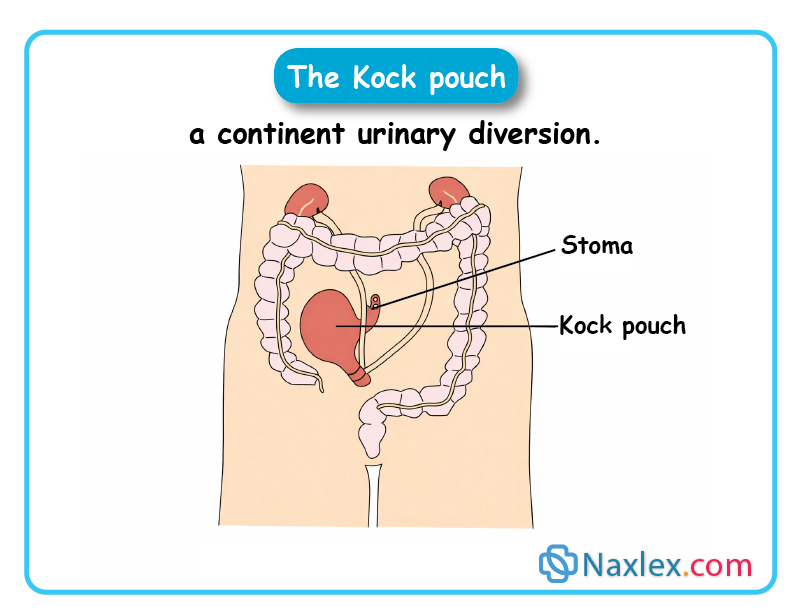
- Neobladder: A new bladder is made from the intestine and sutured to the functional urethra. The client voids by relaxing sphincters and using abdominal straining.
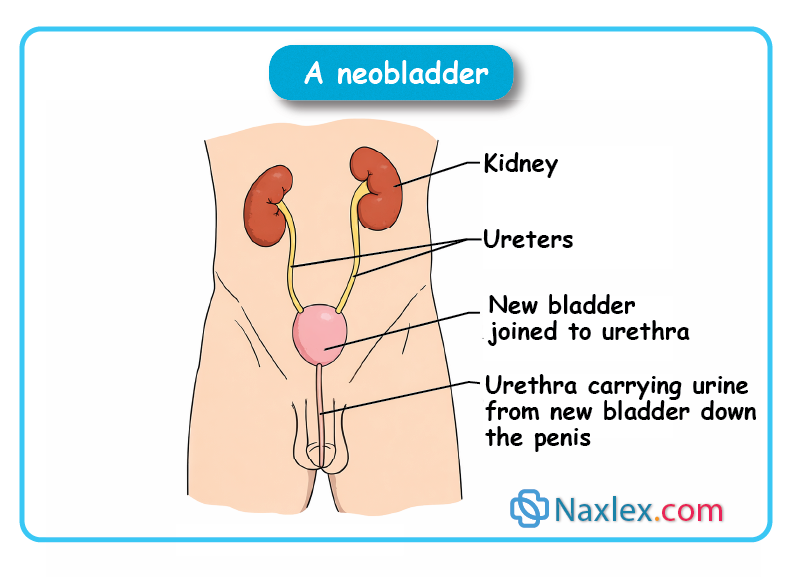
Nursing Care for Diversions:
- Stoma Health: Should be moist and pink/red. Assess peristomal skin for irritation.
- Wicking: Use gauze or a tampon over an incontinent stoma during appliance changes to keep skin dry while fitting the new bag.
- Psychosocial: Address body image and sexuality concerns.
1.5 Evaluating
Using the overall goals and desired outcomes identified in the planning stage, the nurse collects data to evaluate the effectiveness of nursing activities. If the desired outcomes are not achieved, explore the reasons before modifying the care plan. For example, if the outcome “Remains dry between voidings and at night” is not met, examples of questions that need to be considered include:
- What is the client’s perception of the problem?
- Does the client understand and comply with the health care instructions provided?
- Is access to toilet facilities a problem?
- Can the client manipulate clothing for toileting? Can adjustments be made to allow easier disrobing?
- Are scheduled toileting times appropriate?
- Is there adequate transition lighting for night-time toileting?
- Are mobility aids such as a walker, elevated toilet seat, or grab bar needed? If currently used, are they appropriate or adequate?
- Is the client performing pelvic floor muscle exercises appropriately as scheduled?
- Is the client’s fluid intake adequate? Does the timing of fluid intake need to be adjusted (e.g., restricted after dinner)?
- Is the client restricting caffeine, citrus juice, carbonated beverages, and artificial sweetener intake?
- Is the client taking a diuretic? If so, when is the medication taken? Do the times need to be adjusted (e.g., taking second dose no later than 4 pm)?
- Should continence aids such as a condom catheter or absorbent pads be used?
Skills
1.1 SKILL I: Performing Urinary Catheterization
Purpose
Urinary catheterization is performed to:
- Relieve bladder distention or provide gradual decompression
- Measure postvoid residual urine
- Obtain a sterile urine specimen
- Empty the bladder before surgery
- Allow continuous or intermittent bladder drainage
- Accurately monitor urinary output (e.g., critically ill clients)
- Prevent urine contact with perineal or surgical incisions
Assessment
- Determine the appropriate catheter type based on purpose:
- Straight catheter: one-time specimen, residual urine measurement, temporary decompression
- Indwelling catheter: continuous drainage, bladder must remain empty, intermittent catheterization contraindicated
- Review the provider’s order (catheter size, amount to drain)
- Assess the client’s:
- Ability to cooperate and remain still
- Level of discomfort or anxiety
- Determine last voiding time
- If urinary retention is suspected, perform a bladder scan when possible
- Urinary retention is often ≥ 500–800 mL
Planning
- Allow adequate time (procedure may take longer than expected)
- Avoid performing just before or after meals
- Consider client comfort, privacy, and cultural preferences
- If gender concerns exist, obtain consent and follow agency policy regarding a same-gender presence
Delegation
- Do NOT delegate catheter insertion to UAP
- Requires sterile technique and anatomical knowledge
Equipment
- Sterile catheterization kit or individual sterile supplies:
- Sterile catheter (correct size and extra)
- Sterile gloves
- Waterproof drape(s)
- Antiseptic solution and cleansing balls
- Forceps
- Water-soluble lubricant
- Urine receptacle and specimen container
- For indwelling catheter:
- Prefilled syringe with sterile water (balloon inflation)
- Drainage bag and tubing
- Additional supplies:
- Clean gloves
- Perineal care supplies
- Adequate lighting
- Optional: Xylocaine gel for male clients (per policy)
Client positioning
- Female: Supine, knees flexed, feet apart, hips slightly externally rotated
- Male: Supine, thighs slightly abducted
Implementation:
Preparation
- Perform perineal care with clean gloves
- Locate urinary meatus (especially in female clients)
- Perform hand hygiene before sterile setup
Sterile Procedure
- Maintain strict sterile technique
- Lubricate catheter:
- Females: 2.5–5 cm (1–2 in.)
- Males: 15–17.5 cm (6–7 in.)
- Cleanse the meatus:
- Female: Labia majora → labia minora → meatus (front to back). Use your nondominant hand to spread the labia so that the meatus is visible. Establish firm but gentle pressure on the labia. The antiseptic may make the tissues slippery but the labia must not be allowed to return over the cleaned meatus.
- Male: Use your nondominant hand to grasp the penis just below the glans. If necessary, retract the foreskin. Hold the penis firmly upright, with slight tension. The antiseptic may make the tissues slippery but the foreskin must not be allowed to return over the cleaned meatus nor the penis be dropped.
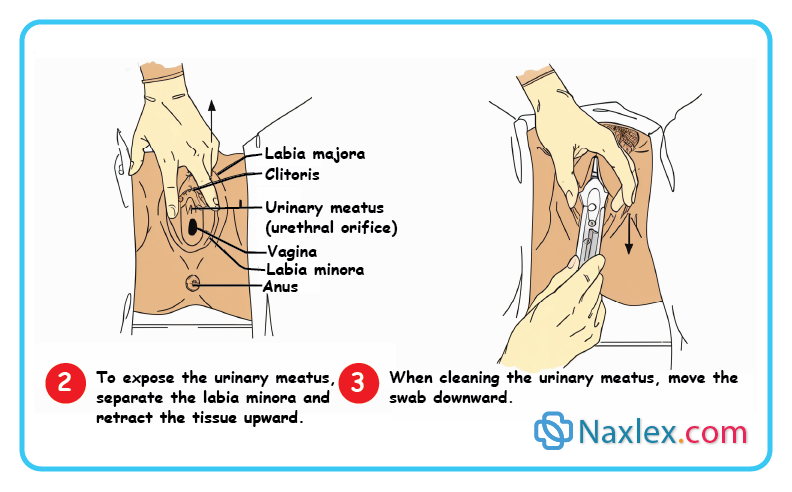
Insertion
- Insert catheter during exhalation
- Expect slight resistance at the sphincter
- Advance catheter 5 cm (2 in.) after urine flows
- For males, may advance to the Y-bifurcation (per policy)
- If catheter enters the vagina - discard and use a new sterile catheter. The contaminated catheter may be left in the vagina until the new catheter is inserted to help avoid mistaking the vaginal opening for the urethral meatus.
Balloon Inflation (Indwelling)
- Inflate balloon with manufacturer-specified volume
- If pain occurs:
- Deflate balloon
- Advance catheter further
- Reinflate
- Gently pull until resistance is felt (balloon seated in trigone)
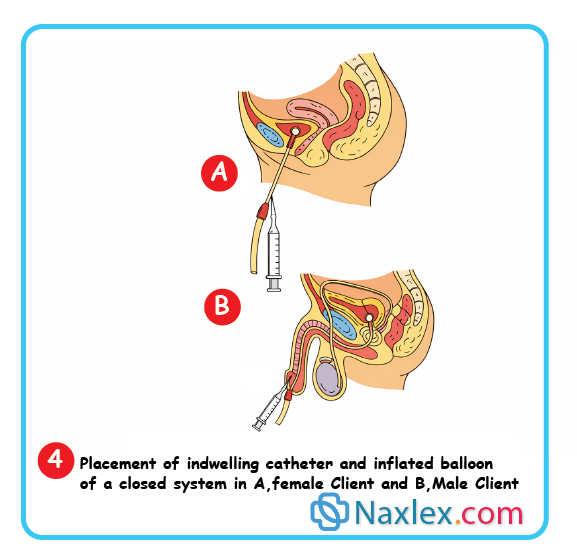
Urine drainage & aftercare
- Collect specimen if ordered (20–30 mL for straight catheter)
- Drain urine gradually if large volumes present
- Often limit to 750–1,000 mL at one time
- Secure catheter:
- Female: thigh
- Male: upper thigh or lower abdomen
- Keep drainage bag below bladder level
- Ensure tubing does not loop below the bag
- Clean perineal area and reposition client comfortably
Documentation
Document:
- Type of catheter and size
- Amount, color, and clarity of urine
- Client response and tolerance
- Any difficulties or complications
- Specimen collection (if applicable)
1.2 SKILL II: Performing Bladder Irrigation
Purposes
Bladder irrigation is performed to:
- Maintain catheter patency (closed continuous irrigation)
- Remove clots, mucus, or debris from catheter or tubing (open intermittent irrigation)
- Prevent catheter obstruction and ensure adequate urinary drainage
Assessment
- Identify the current urinary drainage system (two-way vs three-way catheter)
- Review intake and output (I&O) records
- Assess:
- Urine amount, color, clarity
- Presence of clots, mucus, or sediment
- Client discomfort, bladder spasms, or distention
- Review previous irrigation results
Planning
Before irrigation, verify:
- Reason for irrigation
- Provider’s order (required in most agencies)
- Type of irrigation:
- Continuous vs intermittent
- Solution details:
- Type, strength, amount, temperature
- Rate (if continuous)
- Catheter type:
- Two-way (intermittent/open)
- Three-way (continuous/closed)
- Follow agency protocol if details are unclear
Delegation
- Not delegated to UAP
- Requires sterile/aseptic technique
- UAP may:
- Monitor drainage with continuous irrigation
- Report abnormal findings to the nurse
Equipment (varies by type)
Common supplies include:
- Clean gloves (2 pairs)
- Indwelling catheter in place
- Drainage tubing and bag
- Antiseptic swabs
- Sterile irrigating solution (room temperature or warmed)
- Clearly labeled: Bladder Irrigation, additives, date/time, nurse initials
- Infusion tubing and IV pole
- Sterile receptacle or basin
- Irrigation syringe (30–50 mL) for open irrigation
Implementation
General STEPS
- Verify client identity; explain procedure
- Irrigation should not be painful
- Perform hand hygiene and provide privacy
- Apply clean gloves
- Empty and measure drainage bag
- Establish baseline urine characteristics
- Discard urine and gloves; perform hand hygiene
CLOSED CONTINUOUS BLADDER IRRIGATION (CBI)
Used with a three-way catheter
- Flush irrigation tubing before connecting (removes air)
- Connect:
- Irrigation tubing - irrigation port
- Drainage tubing - drainage port
- Open urinary drainage clamp
- Regulate irrigant flow:
- As prescribed or 40–60 gtt/min if not specified
- Monitor drainage:
- Output should equal irrigant + urine
- Empty bag frequently (≤ half full)
- Assess for:
- Color, clarity
- Bladder distention or spasms
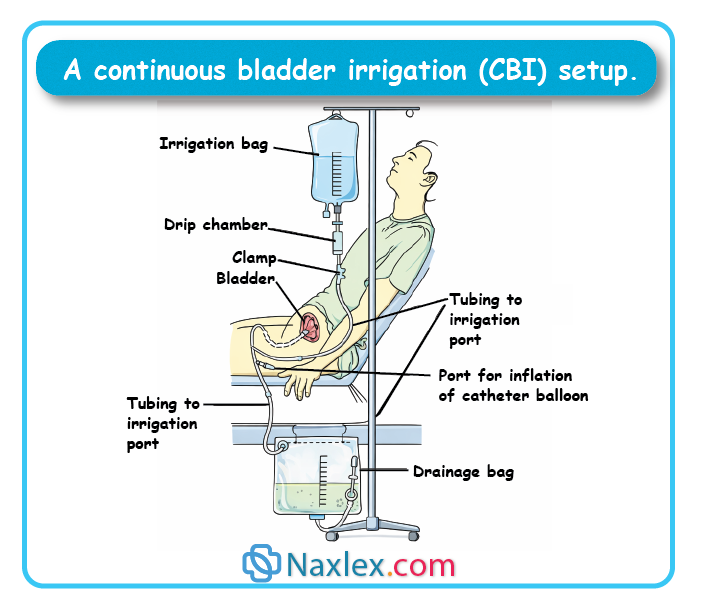
CLOSED INTERMITTENT IRRIGATION
- Determine if solution is to:
- Remain in bladder (instillation)
- Flush catheter only
- Clamp drainage tubing if solution is to dwell
- Instill ordered amount via:
- Three-way catheter infusion port OR
- Two-way catheter injection port with syringe
- After dwell time, unclamp tubing and allow drainage
- Assess output and urine characteristics
OPEN INTERMITTENT IRRIGATION (TWO-WAY CATHETER)
- Use aseptic technique
- Disconnect catheter from drainage tubing
- Cap drainage tubing to maintain sterility
- Instill irrigant gently:
- Rate: ~3 mL/sec
- Volumes:
- Catheter irrigation: 30–40 mL
- Bladder irrigation/instillation: 100–200 mL
- Allow solution to drain back by gravity
- Repeat until:
- Ordered volume is used OR
- Return is clear and clots are removed
- Reconnect catheter and drainage tubing
Post-procedure care
- Assess client comfort
- Measure drainage:
- Subtract irrigant volume from total output
- Observe for:
- Blood clots
- Mucus shreds
- Pus or abnormal color
- Perform hand hygiene
Documentation
Document:
- Type of irrigation and catheter
- Solution type, amount, and rate
- Appearance of urine and drainage
- Net urine output (after subtracting irrigant)
- Client tolerance and any complications
Evaluation
- Compare findings to baseline and prior assessments
- Report abnormal findings promptly
- Adjust care plan based on:
- Persistent clots
- Reduced output
- Client discomfort or bladder spasms
1.3 SKILL III: Applying an External Urinary Device
Purposes
External urinary devices are used to:
- Collect urine and manage urinary incontinence (UI)
- Allow physical activity while controlling UI
- Protect skin and prevent irritation or breakdown from urine exposure
Assessment
- Review client record for:
- Voiding patterns
- History of skin breakdown
- Latex sensitivity or allergy
- Assess if the client has:
- Previously used an external catheter
- Experienced leakage, skin irritation, or discomfort
- Inspect the penis for:
- Swelling, excoriation, or impaired circulation
- Conditions that may contraindicate use
Planning
- Discuss the device with the client and/or family
- Condom catheters are often more comfortable and associated with lower UTI risk than indwelling catheters
- Select the correct size using manufacturer’s guide
- Choose latex-free silicone for clients with latex allergy
- Complete activities best done without the catheter (e.g., weighing)
- Assemble drainage system (leg bag or bedside bag)
Delegation
- Application may be delegated to UAP
- Nurse must:
- Assess for special needs (e.g., impaired circulation, latex allergy)
- Validate and interpret abnormal findings
Equipment
- Condom sheath (correct size; self-adhering or secured with Velcro/elastic strip)
- Leg bag (ambulatory) or bedside drainage bag with tubing
- Clean gloves
- Basin with warm water, soap
- Washcloth and towel

Implementation
Preparation
- Assemble drainage bag
- Roll condom outward if not pre-rolled
Procedure
- Verify client identity and explain procedure
- Perform hand hygiene and provide privacy
- Position client supine or sitting
- Apply clean gloves
- Clean and dry the penis thoroughly
- Reduces skin irritation and excoriation
- Apply the condom catheter
- Roll smoothly over the penis
- Leave 2.5 cm (1 in.) space between tip of penis and drainage tube
- Secure snugly but not tightly
- Do not use ordinary tape (risk of impaired circulation)
- Attach drainage system
- Ensure condom is not twisted
- Bedside bag - attach to bed frame
- Ambulatory client - attach leg bag
- Remove gloves and perform hand hygiene
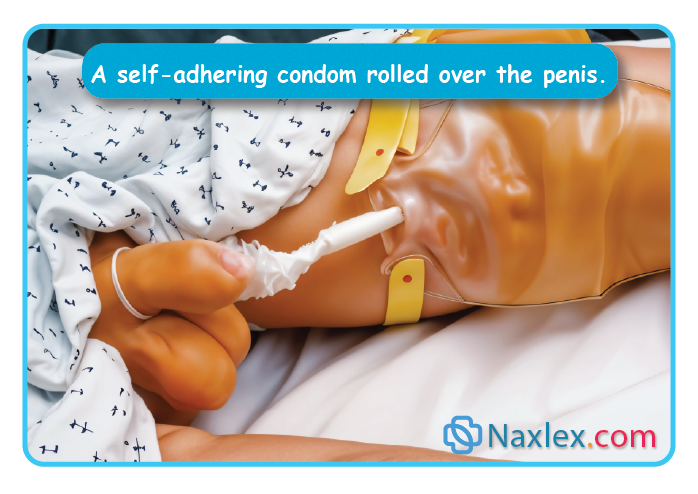
Client teaching
- Keep drainage bag below condom level
- Avoid kinks or loops in tubing
- Report:
- Pain
- Swelling
- Redness
- Wetness or leakage
Ongoing assessment & care
- Inspect penis:
- 30 minutes after application
- At least every 4 hours
- Assess for:
- Swelling or discoloration (too tight)
- Adequate urine flow
- Redness or blistering (possible latex allergy)
- Change condom daily (or per agency policy)
- Provide skin care with each change
Evaluation
- Compare findings to baseline
- Report significant abnormalities to the provider
- Reapply new condom after skin care
Documentation
Document:
- Time and date of application
- Skin condition of penis
- Type and size of condom catheter
- Client education provided
- Any irritation, swelling, or leakage
Summary
- Urinary elimination depends on normal functioning of the upper urinary tract’s kidneys and ureters and the lower urinary tract’s urinary bladder, urethra, and pelvic floor.
- Urine is formed in the nephron, the functional unit of the kidney, through a process of filtration, reabsorption, and secretion. Hormones such as antidiuretic hormone (ADH) and aldosterone affect the reabsorption of sodium and water, thus affecting the amount of urine formed.
- In the adult, urination generally occurs after 250 to 450 mL of urine has collected in the bladder.
- Alterations in urine production and elimination include polyuria, oliguria, anuria, frequency, nocturia, urgency, dysuria, enuresis, incontinence, and retention. Each may have various influencing and associated factors that need to be identified.
- The four main types of urinary incontinence are stress urinary incontinence, urge urinary incontinence, mixed urinary incontinence, and overflow incontinence.
- Urinary catheterization is frequently required for clients with urinary retention but is only performed when all other measures to facilitate voiding fail. Sterile technique is essential to prevent urinary infections.
- Clients with urinary retention may be taught to perform clean intermittent self-catheterization to enhance their independence, reduce the risk of infection, and eliminate incontinence.
- Bladder or catheter irrigations may be used to apply medication to bladder walls or maintain catheter patency.
- A urinary diversion is the surgical rerouting of urine from the kidneys to a site other than the bladder. There are two categories of diversions: incontinent and continent.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Urinary Elimination
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


