Please set your exam date
Dementia And Alzheimer’s Disease
Study Questions
Practice Exercise 1
A family member of a client experiencing dementia and being treated for normal-pressure hydrocephalus asks the nurse, “Is my father’s dementia reversible?” Which nursing response indicates understanding of primary and secondary dementia? Select all that apply.
Explanation
Dementiais a progressive decline in cognition and memory. Primary dementiasuch as Alzheimer’s disease is irreversible due to neuronal degeneration, while secondary dementiamay improve if the underlying cause, like normal-pressure hydrocephalus or metabolic imbalance, is corrected.
Rationale for correct answers:
1.Secondary dementiaarises from conditions such as normal-pressure hydrocephalus, hypothyroidism, or vitamin B12 deficiency. These are potentially reversible because the cognitive decline is linked to a treatable pathology. Correcting the underlying disorder can restore cognitive function.
2.Primary dementiaresults from neurodegenerative processes such as beta-amyloid plaque and tau protein accumulation. These changes cause permanent neuronal damageand progressive decline. Current therapies only manage symptoms, making reversal of cognitive impairmentimpossible.
Rationale for incorrect answers:
3.Secondary dementia is not always irreversible. Disorders like hydrocephalus or metabolic disturbances can be corrected, leading to improvement in memory and cognition. Labeling it as never reversible disregards treatable causes.
4.Primary dementia cannot be reversed because it involves progressive neurodegeneration. No available treatment halts or reverses the disease process, so suggesting possible reversal is scientifically inaccurate.
5.Neither primary nor secondary dementia is always reversible. While secondary dementia may improve with treatment, primary dementia remains irreversible. Stating both are always reversible misrepresents the nature of dementia syndromes.
Test-taking strategy
- Identify whether the dementia is primary or secondary.
- Apply Maslow’s hierarchy: address physiological causes first.
- Recall DSM-5 classification: primary dementias are irreversible neurodegenerative disorders.
- Eliminate absolute statements such as “always” or “never” unless scientifically accurate.
Take Home Points
- Primary dementia such as Alzheimer’s disease is irreversible due to progressive neuronal degeneration.
- Secondary dementia may be reversible if the underlying cause is treated early.
- Normal-pressure hydrocephalus is a classic example of reversible secondary dementia.
- Differentiating primary from secondary dementia is essential for prognosis and family education.
A physician tells family members that their father, who is experiencing confusion and memory loss, has a reversible form of dementia. Which is the likely cause of this disorder?
Explanation
Reversible dementiaoccurs when systemic or metabolic abnormalities impair cognition. Electrolyte imbalance especially sodium, calcium, or potassium disturbances—can cause acute confusion, memory loss, and delirium. Correction of the imbalance often restores normal cognition, unlike neurodegenerative or vascular causes.
Rationale for correct answer:
3.Electrolyte imbalance alters neuronal excitabilityand neurotransmission. Severe hyponatremiaproduces cerebral edema and confusion, while hypercalcemia causes lethargy and impaired memory. These changes are reversible once corrected, making electrolyte imbalance the most likely cause of reversible dementia.
Rationale for incorrect answers:
1.Multiple sclerosis is a chronic demyelinating diseasewith progressive neurological decline. Cognitive impairment may occur, but axonal damage and demyelination are irreversible, so dementia from MS cannot be reversed.
2.Multiple small brain infarcts result in vascular dementia. Ischemic injury leads to permanent neuronal death. Once infarcts occur, cognitive deficits are fixed and cannot be reversed by medical treatment.
4.HIV disease can cause HIV-associated neurocognitive disorder. Although antiretroviral therapy may slow progression, neuronal injury from viral replicationand inflammationis not fully reversible, making this an incorrect option.
Test-taking strategy
- Identify whether the dementia is reversible or irreversible.
- Apply Maslow: prioritize physiological causes first.
- Electrolyte imbalance is a metabolic condition that can be corrected.
- Eliminate chronic, progressive, or irreversible conditions (MS, infarcts, HIV).
Take Home Points
- Reversible dementia is most often due to metabolic or systemic causes such as electrolyte imbalance, thyroid dysfunction, or vitamin deficiencies.
- Irreversible dementias include Alzheimer’s disease, vascular dementia, and neurodegenerative disorders.
- Electrolyte disturbances, especially sodium and calcium abnormalities, can mimic dementia but resolve with correction.
- Differentiating reversible from irreversible causes is critical for timely intervention and improved patient outcomes.
A client newly diagnosed with vascular dementia isolates themselves because of consistently poor role performance and increasing loss of independent functioning. Which nursing diagnosis reflects this client’s problem?
Explanation
Vascular dementiaresults from impaired cerebral circulationleading to progressive cognitive decline, executive dysfunction, and loss of independence. Clients often experience social isolationdue to poor role performance and inability to maintain previous functioning, which contributes to diminished self-worthand low self-esteem.
Rationale for correct answer:
4.Loss of independent functioning directly impacts the client’s self-esteem. Social isolationreflects withdrawal due to inability to perform roles, consistent with DSM-5 criteria for major neurocognitive disorder. Addressing self-esteemsupports psychosocial adaptation and prevents worsening depression.
Rationale for incorrect answers:
1.Disturbed thought processes are common in vascular dementia, but the stem emphasizes isolationand poor role performance, not disorientation. The problem is primarily psychosocialrather than cognitive in this context, making this less appropriate.
2.Risk for injury relates to impaired mobility, confusion, or unsafe behaviors. The stem highlights social withdrawaland role loss, not falls or physical hazards. Injury prevention is important but not the priority issuedescribed here.
3.Disturbed body image involves altered perception of the physical self, often linked to disfigurementor illness. Tearful affect here stems from loss of independenceand social isolation, not distorted body perception, so this diagnosis does not fit.
Test-taking strategy
- Identify the main issue in the stem: isolationdue to poor role performance.
- Apply Maslow: psychosocial needs after physiological stability.
- Match defining characteristics: social isolationand role loss align with low self-esteem.
- Eliminate options focusing on cognition, injury, or body image, as they do not match the stem.
Take Home Points
- Vascular dementia causes cognitive decline and executive dysfunction due to impaired cerebral circulation.
- Social isolation and poor role performance often manifest as low self-esteem in these clients.
- Disturbed thought processes and risk for injury are important but not the primary issue in this scenario.
- Differentiating psychosocial diagnoses from cognitive or physical ones ensures accurate nursing care planning.
A nurse is reviewing examples of treatable (reversible) forms of neurocognitive disorder (NCD). Which of the following causes are treatable? Select all that apply.
Explanation
Treatable (reversible) neurocognitive disordersresult from acute, correctable medical, metabolic, or nutritional conditionsthat cause cognitive impairment. Identifying and addressing these causes early can restore cognitive function, differentiating them from progressive, irreversible dementiaslike Alzheimer’s disease.
Rationale for correct answers:
3.Electrolyte imbalances(e.g., sodium, calcium, or potassium disturbances) can disrupt neuronal function, causing confusion or cognitive deficits. Correcting the imbalance often reverses cognitive impairmentquickly.
4.HIV-related cognitive impairmentcan be improved with antiretroviral therapy, especially in early stages, making it a reversible cause of NCDif treated appropriately.
5.Folate deficiencyimpairs DNA synthesis and neurotransmitter function, leading to cognitive decline. Supplementation with folic acidcan restore cognitive function if caught early.
Rationale for incorrect answers:
1.Multiple sclerosiscauses chronic, progressive demyelination; cognitive deficits are part of a non-reversible neurodegenerative process, so it is not fully treatable.
2.Multiple small brain infarcts(vascular dementia) lead to irreversible neuronal loss. While risk factors can be managed, existing cognitive deficits are generally not reversible.
Test-taking strategy
- Identify causes that are acute, correctable, or metabolic/nutritional.
- Differentiate progressive neurodegenerative disordersfrom reversible conditions.
- Focus on interventions that restore cognitive function.
Take Home Points
- Treatable NCDs often result from metabolic, infectious, or nutritional causes.
- Reversal is possible with early identification and treatment.
- Progressive disorders like MS or vascular dementiaare not reversible.
- Electrolyte, HIV, and folate deficiencies are key reversible contributors to cognitive impairment.
A client has been diagnosed with neurocognitive disorder (NCD) due to Alzheimer’s disease. The cause of this disorder is which of the following?
Explanation
Neurocognitive disorder (NCD) due to Alzheimer’s diseaseis a progressive, degenerative brain disordercharacterized by cognitive decline affecting memory, thinking, and daily functioning. The exact cause remains unknown, though it is associated with amyloid plaques, neurofibrillary tangles, and genetic risk factors.
Rationale for correct answer:
4.Alzheimer’s disease is considered idiopathic, meaning the precise etiology is not fully understood. While genetic, biochemical, and environmental factorscontribute to pathophysiology, there is no single identifiable cause.
Rationale for incorrect answers:
1.Multiple small brain infarcts cause vascular NCD, a different, usually treatable or preventable form of cognitive impairment, not Alzheimer’s disease.
2.Chronic alcohol abuse can lead to alcohol-related NCD(e.g., Wernicke-Korsakoff syndrome), which is distinct from Alzheimer’s.
3.A cerebral abscess is an infectious lesionthat may cause delirium or secondary NCD, but it is not related to Alzheimer’s disease.
Test-taking strategy
- Recognize that Alzheimer’s disease is progressive, degenerative, and idiopathic.
- Differentiate Alzheimer’s from vascular, substance-related, or infection-related NCDs.
- Focus on underlying pathophysiology (plaques, tangles) rather than external insults.
Take Home Points
- Alzheimer’s disease is a progressive, irreversible NCD.
- The precise cause remains unknown, though pathology involves plaques and tangles.
- Distinguish Alzheimer’s from vascular, substance-induced, or infection-related NCDs.
- Treatment focuses on symptom management and slowing progression, not curing the underlying cause.
Practice Excercise 2
A client diagnosed with Alzheimer’s disease is displaying signs and symptoms of anxiety, fear, and paranoia. An alteration in which area of the brain is responsible for these signs and symptoms?
Explanation
Alzheimer’s disease—amygdala dysfunctioninvolves disrupted limbic circuitry driving fear, anxiety, and threat misinterpretation. Amygdalar hyperreactivity and impaired prefrontal modulation amplify negative salience, producing paranoia, agitation, and heightened startle. Neurodegeneration also alters connectivity with hippocampus and insula, worsening emotional memory bias and autonomic arousal.
Rationale for correct answer:
4.The amygdalaassigns emotional salience to stimuli and orchestrates fear conditioning, threat detection, and autonomic responses. In Alzheimer’s, amygdalar dysfunction—combined with reduced top-down inhibition—produces exaggerated fear/anxietyand paranoid ideation, manifesting as hypervigilance, misinterpretation of cues, and agitation.
Rationale for incorrect answers:
1.The frontal lobe mediates executive function, judgment, and behavioral regulation. Its degeneration causes disinhibition and apathy rather than primary fear generation. While frontal impairment reduces control over limbic output, it does not originate the core anxiety/paranoia circuitry.
2.The parietal lobe integrates somatosensoryand visuospatial processing. Parietal involvement in Alzheimer’s leads to neglect, constructional apraxia, and spatial disorientation. These deficits may secondarily increase distress, but they do not drive the emotional salience and conditioned fear responses underlying paranoia.
3.The hippocampusencodes declarative memory and contextual binding. Hippocampal atrophy causes anterograde amnesia and impaired context retrieval, which can exacerbate confusion. However, the primary generator of fear/anxiety and threat appraisal is the amygdala, not hippocampal memory circuits.
Test-taking strategy
- Identify the symptom cluster—anxiety, fear, paranoia—then map to limbic structures.
- Prioritize the amygdalafor threat detection and fear conditioning.
- Differentiate hippocampus (memory), frontal lobe (executive control), parietal lobe (spatial/sensory).
- Apply pathophysiology: limbic hyperreactivity with reduced cortical inhibition.
Take Home Points
- Amygdala dysfunction in Alzheimer’s drives fear, anxiety, and paranoia via heightened threat salience and impaired regulation.
- Hippocampal atrophy primarily causes memory loss and contextual confusion, not core fear generation.
- Frontal lobe degeneration reduces inhibitory control, worsening limbic symptoms but is not the origin of fear.
- Parietal lobe involvement causes visuospatial deficits; emotional dysregulation stems mainly from limbic circuitry.
A client newly diagnosed with Alzheimer’s disease was admitted 72 hours ago. The client states, “Last night I went on a wonderful dinner cruise.” Which type of communication is this client expressing, and what is the underlying reason for its use?
Explanation
Confabulationis the unconscious fabrication of stories or experiences to fill memory gaps, commonly seen in Alzheimer’s disease. It is not intentional lying but a compensatory mechanism. The purpose is to protect the egofrom the distress of memory loss, allowing the client to maintain a sense of coherence and dignity despite cognitive decline.
Rationale for correct answer:
2.Confabulation arises when memory deficits prevent accurate recall, leading the brain to unconsciously generate plausible but false narratives. In Alzheimer’s, this protects the egoby preserving self-identityand reducing anxiety about memory gaps. The fabricated dinner cruise story reflects an attempt to maintain continuity of self and avoid embarrassment from admitting forgetfulness.
Rationale for incorrect answers:
1.Secondary gains involve external benefits such as attention or avoidance of responsibility. Confabulation in Alzheimer’s is not purposeful or manipulative; it is an unconscious defense, making secondary gainan inaccurate explanation.
3.Perseverationis the involuntary repetition of words, phrases, or behaviors due to impaired cortical inhibition. It does not involve creating new false memories. The dinner cruise narrative is fabricated, not repeated, ruling out perseveration.
4.Perseveration does not serve to maintain self-esteem; instead, it reflects neurological dysfunction. The client’s statement demonstrates confabulation, which specifically functions to protect self-esteem and ego, not perseveration.
Test-taking strategy
- Identify the communication: fabricated but plausible story → confabulation.
- Determine purpose: unconscious defense to protect ego.
- Eliminate perseveration (repetition, not fabrication).
- Eliminate secondary gain (external benefit, not unconscious defense).
- Apply Maslow: protecting ego relates to psychological needs of self-esteem.
Take Home Points
- Confabulation is unconscious fabrication of memories to fill gaps in dementia.
- It differs from lying or secondary gain, as it is not intentional.
- Perseveration involves repetition, not fabrication, and is distinct from confabulation.
- Recognizing confabulation helps differentiate Alzheimer’s communication patterns from other cognitive disorders.
A nurse documents that a client diagnosed with Alzheimer’s disease presents with aphasia while on a 24-hour assessment. Which client behavior supports this finding?
Explanation
Alzheimer’s disease with aphasiais a language impairmentcaused by progressive neurodegeneration especially in left temporal–parietal areas, affecting the production and comprehensionof speech. Aphasia in Alzheimer’s primarily affects word finding, naming, and fluency, though some patients may retain basic speech.
Rationale for correct answer:
3.Difficulty in forming words represents expressive language dysfunction, characteristic of aphasia in Alzheimer’s disease where the client struggles with word retrieval and constructing speech despite understanding and intent to communicate.
Rationale for incorrect answers:
1.Sadness and anhedonia reflect mood symptoms(depression) rather than a specific language production deficit; aphasia concerns speech and language processing, not emotional experience.
2.Emaciation and wasting relate to nutritional or systemic deterioration, not specifically to language ability; they do not reflect impaired speech production or comprehension.
4.“No longer able to speak” suggests mute behavior, which can be motor or severe, but aphasia describes disrupted language formulation rather than complete absence of speech output.
Test-taking strategy
- Identify key symptom: aphasia = language impairment.
- Differentiate language (aphasia) from mood (depression) and physical wasting.
- Exclude total mutism; focus on difficulty producing speech.
- Use elimination: only choice linked to language formationfits aphasia.
Take Home Points
- Aphasiain Alzheimer’s primarily affects word formation and language fluency.
- It does not inherently cause mood disordersor affect physical body mass.
- Distinguish speech production issuesfrom complete mutism.
- Language deficits reflect cortical degenerationin Alzheimer’s and impact communication ability.
A nurse understands that drastically reduced levels of acetylcholine are available in the brains of individuals diagnosed with Alzheimer’s disease. Which cognitive deficit is primarily associated with this reduction?
Explanation
Alzheimer’s disease and acetylcholine deficitinvolves marked reduction of acetylcholine, a neurotransmitter central to learning and memory consolidationin the hippocampus and cortex. Its depletion correlates most strongly with impaired memory encoding and recallin Alzheimer’s.
Rationale for correct answer:
1.Drastically reduced acetylcholine in Alzheimer’s disrupts hippocampal synaptic plasticityand cholinergic transmission critical for short-term memory formation and retrieval, leading primarily to loss of memory, especially recent events and new learning.
Rationale for incorrect answers:
2.Loss of purposeful movement reflects motor system dysfunctioninvolving basal ganglia, cerebellum, or motor cortex, not primarily due to cholinergic deficits in Alzheimer’s, which target cognitive circuitsrather than motor execution.
3.Loss of sensory ability to recognize objects (agnosia) involves association cortex dysfunction, especially in parietal and occipital regions; while present in Alzheimer’s, it is not the deficit most directly tied to acetylcholine reduction.
4.Loss of language ability (aphasia) arises from degeneration in language networks, particularly left temporal–parietal areas; acetylcholine depletion contributes to overall cognitive decline, but memory lossis the dominant deficit linked to cholinergic loss.
Test-taking strategy
- Recognize acetylcholine’s primary role in memorycircuits.
- Match options to functions: memory vs motor vs sensory recognition vs language.
- Eliminate choices not directly linked to cholinergic transmission.
- Choose the option most consistent with Alzheimer’s hallmark deficit.
Take Home Points
- Acetylcholineis essential for memory encoding and recallin Alzheimer’s.
- Cholinergic deficits correlate with early and prominent memory loss.
- Alzheimer’s also involves language and recognition issues, but not as primary cholinergic effects.
- Motor dysfunction is not a core feature of acetylcholine depletion in Alzheimer’s.
A nurse is caring for a client who states, “Lately I’m getting forgetful about things. I’m so afraid I’m getting Alzheimer’s disease.” Which response by the nurse is most therapeutic?
Explanation
Therapeutic communication in memory concernsinvolves validating client feelings, providing accurate information, and encouraging discussion. Normal aging can include minor memory lapses, but clients need a safe space to express concerns and explore further evaluation without fear or dismissal.
Rationale for correct answer:
3.This response acknowledges the client’s concernswhile providing factual information that some memory lapses are common. It invites further discussion, promotes trust, and encourages the client to share detailsthat may indicate normal aging or early cognitive changes.
Rationale for incorrect answers:
1.Dismissing the concern as normal aging invalidates the client’s feelingsand may discourage future disclosure of legitimate cognitive changes.
2.Self-disclosure by the nurse shifts focus away from the client, minimizing the client’s concerns and failing to address their anxiety about potential Alzheimer’s disease.
4.Overly complex explanations without listening can confuse or overwhelmthe client and negate the emotional componentof their concern, preventing therapeutic dialogue.
Test-taking strategy
- Use therapeutic communication principles: validate, clarify, and explore.
- Avoid dismissive, self-focused, or confusing statements.
- Encourage discussion to assess severity and impact.
- Focus on client feelings and education, not personal anecdotes.
Take Home Points
- Validate concerns while providing accurate informationabout normal vs pathological memory changes.
- Encourage discussion to assess cognitive status and emotional impact.
- Avoid dismissive or self-focused responses that minimize client anxiety.
- Therapeutic communication builds trust and facilitates early identificationof cognitive decline.
Practice Excercise 3
A nurse is assessing an older adult with the diagnosis of dementia. Which manifestations are expected in this client? Select all that apply.
Explanation
Test-taking strategy
- Identify hallmark cortical deficits—agnosia, apraxia, aphasia—over nonspecific behaviors.
- Prioritize objective, domain-specific impairments with functional impact per diagnostic criteria.
- Differentiate attentional complaints from memory encoding deficits.
- Exclude features more consistent with mood or personality rather than neurodegeneration.
Take Home Points
- Agnosia—failure to recognize familiar objects with intact sensation—is a classic cortical sign in dementia.
- Dementia requires cognitive decline with functional impairment across domains, not just behavioral preferences.
- Remote memory may be relatively preserved early; recent memory and new learning are disproportionately impaired.
- Differentiate dementia from depression and delirium by chronicity, attention, and presence of cortical deficits (aphasia, apraxia, agnosia).
A client says to the nurse: “I read an article about Alzheimer’s and it said the disease is hereditary. My mother has Alzheimer’s disease. Does that mean I’ll get it when I’m old?” The nurse bases her response on the knowledge that which factor is not associated with increased incidence of NCD due to Alzheimer’s disease?
Explanation
Neurocognitive disorder (NCD) due to Alzheimer’s diseaseis primarily influenced by age, genetics, and certain lifestyle or environmental factors. While some risk factors increase susceptibility, vascular events like small strokes are associated with vascular dementia, not Alzheimer’s disease, and do not directly increase the incidence of Alzheimer’s NCD.
Rationale for correct answer:
1.Multiple small strokescontribute to vascular neurocognitive disorderby causing cumulative brain infarcts. These are not a recognized risk factor for Alzheimer’s disease, so they do not increase its incidence.
Rationale for incorrect answers:
2.Family history of Alzheimer’s diseaseis a significant risk factor due to genetic predisposition, particularly in early-onset forms.
3.Head traumaincreases the risk of Alzheimer’s disease by accelerating amyloid deposition and neuronal injury, contributing to neurodegeneration.
4.Advanced ageis the strongest risk factor; incidence rises sharply after age 65, with prevalence increasing dramatically in older populations.
Test-taking strategy
- Identify risk factors specific to Alzheimer’s disease versus other forms of NCD.
- Exclude factors primarily associated with vascular or secondary dementias.
- Focus on well-established epidemiological and genetic risk factors.
Take Home Points
- Alzheimer’s disease risk increases with advanced age, family history, and head trauma.
- Multiple small strokes are primarily linked to vascular NCD, not Alzheimer’s.
- Understanding risk factors helps in patient education and preventive strategies.
- Genetic predisposition does not guarantee disease, but it elevates susceptibility.
A nurse is providing care for several clients who have a diagnosis of dementia. The nurse should adopt a common approach of care because these clients need to:
Explanation
Dementiais a progressive decline in cognition, memory, and orientation that interferes with daily functioning. Clients experience difficulty adapting to new environments or routines, and unfamiliar stimuli can trigger agitation or confusion. Maintaining sameness and consistency reduces stress, supports orientation, and preserves remaining abilities.
Rationale for correct answer:
4.Sameness and consistency in the environment are essential because dementia impairs the ability to process new information and adapt to change. A stable environment minimizes confusion, reduces agitation, and enhances safety by reinforcing familiar cues and routines that support residual cognitive function.
Rationale for incorrect answers:
1.Relating consistently to staff is supportive but secondary. The primary therapeutic need is environmental stability, as cognitive decline makes adaptation difficult. Staff consistency helps but does not address the core deficit of disorientation.
2.Learning that staff cannot be manipulated assumes intact reasoning and insight. Dementia clients lack the cognitive ability for such learning due to impaired executive functionand memory, making this rationale inappropriate.
3.Accepting controls that are concrete and fairly applied emphasizes discipline rather than therapeutic support. Dementia care focuses on minimizing stressors and maintaining orientation, not enforcing behavioral controls, which may increase agitation.
Test-taking strategy
- Identify the fundamental deficit in dementia: impaired memory and orientation.
- Apply Maslow’s hierarchy: safety and physiological needs take precedence.
- Eliminate options requiring intact reasoning or learning capacity.
- Select the option emphasizing environmental stability and sameness.
Take Home Points
- Dementia clients benefit most from consistent environments to reduce confusion and agitation.
- Cognitive decline limits ability to learn new rules or adapt to change.
- Staff consistency is supportive but not the primary therapeutic need.
- Differentiating dementia from delirium is critical: delirium requires acute medical management, while dementia requires long-term environmental and supportive care.
A 76-year-old client is admitted to a long-term-care facility with a diagnosis of Alzheimer’s-type dementia. The client has been wearing the same dirty clothes for several days, and the nurse contacts the family to bring in clean clothing. Which intervention would best prevent further regression in the client’s personal hygiene?
Explanation
Alzheimer’s-type dementiais a progressive neurocognitive disorder marked by decline in memory, executive function, and self-care abilities. Clients gradually lose independence in activities of daily living. Promoting retained abilities through encouragement of self-care helps preserve dignity, slows regression, and maintains functional capacity.
Rationale for correct answer:
1.Encouraging the client to perform as much self-care as possible maintains independence and prevents further decline in functional abilities. Preserving autonomysupports self-esteem, reduces learned helplessness, and aligns with rehabilitation principles in dementia care. This approach maximizes retained skills while providing assistance only when necessary.
Rationale for incorrect answers:
2.Making the client assume responsibility for physical care is unrealistic because dementia impairs judgmentand memory. Forcing responsibility may increase frustration and agitation, as clients lack the cognitive capacity to consistently manage hygiene independently.
3.Assigning a staff member to take over physical care fosters dependency and accelerates regression. Over-assistance diminishes opportunities for practice of retained abilities, leading to faster decline in activities of daily livingand loss of autonomy.
4.Accepting the client’s desire to go without bathing neglects basic physiological needsand compromises health. Poor hygiene increases risk of infection, skin breakdown, and social isolation. Maslow’s hierarchy prioritizes physical care needs, making this option unsafe and inappropriate.
Test-taking strategy
- Identify the goal in dementia care: preserve independence and dignity.
- Apply Maslow’s hierarchy: physiological needs (hygiene) must be met.
- Eliminate options requiring intact cognition or neglecting basic needs.
- Select the option that balances autonomy with supportive care.
Take Home Points
- Encouraging self-care in dementia preserves independence and slows decline in daily functioning.
- Over-assistance accelerates regression by removing opportunities to practice retained abilities.
- Neglecting hygiene compromises health and violates physiological needs.
- Dementia care should balance autonomy with safety, supporting dignity while meeting essential needs.
A nurse is planning care for a client who has a diagnosis of dementia. Which intervention should the nurse identify as the top priority for this client?
Explanation
Dementiais a progressive decline in cognition, memory, and judgment that impairs daily functioning. Clients are at high risk for injury due to disorientation, wandering, and poor safety awareness. Establishing a safe environment is the top priority because it addresses immediate physiological needs and prevents harm.
Rationale for correct answer:
4.Creating a safe environment is the priority because dementia clients are prone to wandering, falls, and accidents due to impaired judgmentand orientation. Safety interventions—secured areas, removal of hazards, supervision—directly prevent injury and preserve life, aligning with Maslow’s physiological and safety needs.
Rationale for incorrect answers:
1.Providing foods that are easy to eat supports nutrition but is not the top priority. While important, nutritional needs come after ensuring safety, as injury or accidents pose immediate threats to survival.
2.Providing rest and sleep promotes comfort and reduces agitation, but it does not address the immediate risk of harm. Sleep hygiene is supportive but secondary to environmental safety.
3.Keeping the incontinent client clean and dry maintains skin integrity and dignity, but it is not the highest priority. Hygiene needs are important but do not outweigh the immediate risk of injury from unsafe surroundings.
Test-taking strategy
- Apply Maslow’s hierarchy: physiological and safety needs come first.
- Identify dementia’s greatest risk: injury due to disorientation and wandering.
- Eliminate options that address comfort or hygiene but not immediate survival.
- Select the intervention that prevents harm and ensures safety.
Take Home Points
- Safety is the top priority in dementia care due to risk of injury and wandering.
- Nutrition, rest, and hygiene are important but secondary to immediate safety needs.
- Dementia impairs judgment and orientation, making environmental control essential.
- Differentiating dementia from delirium is critical: delirium requires acute medical stabilization, while dementia requires long-term safety and supportive care.
A nurse is planning care for a client who has a diagnosis of dementia. Which intervention should the nurse identify as the top priority for this client?
Explanation
Dementiais a progressive decline in cognition, memory, and judgment that impairs daily functioning. Clients are at high risk for injury due to disorientation, wandering, and poor safety awareness. Establishing a safe environment is the top priority because it addresses immediate physiological needs and prevents harm.
Rationale for correct answer:
4.Creating a safe environment is the priority because dementia clients are prone to wandering, falls, and accidents due to impaired judgmentand orientation. Safety interventions—secured areas, removal of hazards, supervision—directly prevent injury and preserve life, aligning with Maslow’s physiological and safety needs.
Rationale for incorrect answers:
1.Providing foods that are easy to eat supports nutrition but is not the top priority. While important, nutritional needs come after ensuring safety, as injury or accidents pose immediate threats to survival.
2.Providing rest and sleep promotes comfort and reduces agitation, but it does not address the immediate risk of harm. Sleep hygiene is supportive but secondary to environmental safety.
3.Keeping the incontinent client clean and dry maintains skin integrity and dignity, but it is not the highest priority. Hygiene needs are important but do not outweigh the immediate risk of injury from unsafe surroundings.
Test-taking strategy
- Apply Maslow’s hierarchy: physiological and safety needs come first.
- Identify dementia’s greatest risk: injury due to disorientation and wandering.
- Eliminate options that address comfort or hygiene but not immediate survival.
- Select the intervention that prevents harm and ensures safety.
Take Home Points
- Safety is the top priority in dementia care due to risk of injury and wandering.
- Nutrition, rest, and hygiene are important but secondary to immediate safety needs.
- Dementia impairs judgment and orientation, making environmental control essential.
- Differentiating dementia from delirium is critical: delirium requires acute medical stabilization, while dementia requires long-term safety and supportive care.
Practice Exercise 4
A client who has a neurocognitive disorder due to Alzheimer’s disease, says to the nurse, “I have a date tonight. I always have a date on Christmas.” Which of the following is the most appropriate response?
Explanation
Reality orientation in Alzheimer’s diseaseinvolves gently reorienting the client to the present time, place, and situationwhile minimizing confusion and anxiety. Clients with NCD often confabulate or misinterpret eventsdue to memory loss, and appropriate nursing responses should be truthful, calm, and reassuring.
Rationale for correct answer:
2.Providing the correct date and factual information about upcoming eventsgently reorients the client without confrontation. This approach reduces anxiety, maintains trust, and supports cognitive functioningwhile addressing the client’s confusion.
Rationale for incorrect answers:
1.Telling the client “Don’t be silly” is dismissive and confrontational, which may increase frustration or agitation.
3.Asking about the date without clarification reinforces the client’s confabulationand does not provide orientation or reassurance.
4.Suggesting the client needs more medication is dismissive, nontherapeutic, and inappropriate, as it blames the client rather than addressing confusion with reality orientation.
Test-taking strategy
- Use reality orientation techniques: correct gently, provide factual information.
- Avoid confrontation, sarcasm, or reinforcing confabulations.
- Focus on maintaining trust and reducing anxietywhile reorienting the client.
Take Home Points
- Reality orientation is key for clients with confusion and memory loss.
- Responses should be gentle, factual, and reassuring.
- Avoid dismissive, confrontational, or corrective statements that may increase agitation.
- Confabulations should be addressed calmly without reinforcing false memories.
A nurse is teaching the wife of a client who has mild symptoms of dementia how to more effectively communicate with her spouse. The teaching would be considered successful if the nurse observed the wife:
Explanation
ementiain its mild stage is characterized by memory impairment, difficulty with attention, and reduced ability to process complex communication. Effective strategies include maintaining eye contact, using simple sentences, and face-to-face interaction, which enhances comprehension and reduces confusion.
Rationale for correct answer:
1.Face-to-face conversation allows the client to use visual cuessuch as facial expressions and lip movements, which improve understanding. It also fosters connectionand reduces distraction, making communication clearer and more supportive in mild dementia.
Rationale for incorrect answers:
2.Talking quietly into the ear may reduce clarity and eliminate visual reinforcement. Clients with dementia often rely on visual cues, so this method increases confusion and does not enhance comprehension.
3.Discussing only past events limits communication and does not support orientation to the present. While reminiscence can be comforting, effective communication requires addressing both current and past topics to maintain orientationand engagement.
4.Speaking loudly and enunciating each word may appear confrontational and can increase agitation. Dementia clients benefit more from calm, clear, and supportive communication rather than exaggerated speech patterns.
Test-taking strategy
- Identify therapeutic communication principles: calm, supportive, clear, and face-to-face.
- Eliminate options that reduce clarity (quiet speech), limit scope (only past events), or increase agitation (loud speech).
- Select the option that enhances comprehension and connection.
Take Home Points
- Mild dementia requires communication strategies that use visual cues and simple language.
- Face-to-face interaction improves comprehension and reduces confusion.
- Loud or whispered speech increases agitation or reduces clarity.
- Reminiscence is supportive but should not replace orientation to present reality.
A client is experiencing acute confusion due to poisoning from an accidental exposure to toxic chemicals in the workplace. What type of behavior should the nurse expect this client to demonstrate upon admission to the nursing unit?
Explanation
Acute confusioncaused by toxic chemical exposure is a form of delirium, characterized by sudden onset of impaired attention, orientation, and communication. Neurotoxicity disrupts neurotransmitter balance and cerebral function, leading to difficulty organizing thoughts, expressing needs, and maintaining coherent speech.
Rationale for correct answer:
3.Toxic poisoning alters cognitive processingand language function, resulting in difficulty expressing ideas and needs. This is consistent with acute delirium, where impaired attention and disorganized thinking are hallmark features. The nurse should expect communication deficits upon admission.
Rationale for incorrect answers:
1.Nausea may occur with chemical exposure but is a gastrointestinal symptom, not the defining feature of acute confusion. The stem emphasizes cognitive impairment, making this option less appropriate.
2.Ambivalent feelings reflect emotional conflict but are not typical of acute delirium. The primary issue is disorganized thoughtand impaired communication, not frequent verbalization of mixed emotions.
4.Despondency in the presence of family suggests depressionor withdrawal. Acute confusion from poisoning presents with fluctuating cognition and communication deficits, not sustained despondency.
Test-taking strategy
- Identify the condition: acute confusion from toxic exposure = delirium.
- Apply Maslow: prioritize neurological and communication deficits over GI or emotional symptoms.
- Eliminate options that describe depression or emotional states.
- Select the option that reflects impaired communication and thought organization.
Take Home Points
- Acute confusion from toxic poisoning is a form of delirium with sudden cognitive impairment.
- Difficulty expressing ideas and needs is a hallmark of delirium due to disorganized thinking.
- Nausea or emotional symptoms may occur but are not primary indicators of acute confusion.
- Differentiating delirium from depression or anxiety ensures accurate nursing assessment and intervention.
A client on an in-patient psychiatric unit is exhibiting extreme agitation. Using a behavioral approach, which nursing intervention should be implemented?
Explanation
Behavioral management of extreme agitationin psychiatric settings requires immediate interventions to reduce risk and ensure safety. When a client is highly agitated, physiological hyperarousal impairs rational thinking and behavioral control, so rapid stabilization is critical before implementing therapeutic behavioral strategies.
Rationale for correct answer:
3.Administering PRN medicationseffectively decreases anxiety and agitation, lowering the risk of harm to the client and others. This rapid, evidence-based interventionallows the client to regain self-control, enabling future behavioral or therapeutic interventions.
Rationale for incorrect answers:
1.Role-playing stressful situations requires cognitive engagement and calmness. Attempting this during extreme agitation is unsafe and may escalate behaviors.
2.Developing a stressor plan in a family meeting is long-term planning. It does not address the immediate risk of harmposed by extreme agitation.
4.Discussing emotional triggers requires reflection and cooperation, which is not possible during a hyperaroused state. Attempting this may increase agitationrather than reduce it.
Test-taking strategy
- Prioritize safety and immediate stabilizationover long-term behavioral interventions.
- Identify interventions that are rapidly effective and evidence-based.
- Reserve therapeutic and educational strategiesfor when the client is calm.
Take Home Points
- Extreme agitation requires immediate interventions for safety.
- PRN medications are appropriate for rapid reduction of physiological hyperarousal.
- Behavioral strategies (role-play, trigger discussions) are secondary interventions.
- Crisis management precedes therapeutic behavioral planningin inpatient psychiatric care.
Practice Exercise 5
A nurse is caring for a client diagnosed with Alzheimer’s disease who is prescribed cholinergic medications. Why do these medications help the client?
Explanation
Alzheimer’s diseaseis a progressive decline in memory, executive function, and orientation. A central feature is reduced acetylcholine due to degeneration of basal forebrain cholinergic neurons. Cholinergic medications inhibit acetylcholinesterase, increasing acetylcholine availability at synapses to improve cognition and daily functioning.
Rationale for correct answer:
1.Cholinergics increase acetylcholinein the brain by inhibiting acetylcholinesterase, the enzyme responsible for breakdown. This enhances synaptic transmissionin cortical and hippocampal regions, improving memory and attention. Although not curative, this mechanism temporarily slows decline and supports functional independence.
Rationale for incorrect answers:
2.Parasympathetic stimulation does not directly improve cognition. The therapeutic effect is specifically related to acetylcholine enhancementin the brain, not systemic parasympathetic activity such as bradycardia or increased secretions.
3.Sympathetic inhibition is not the mechanism of action. Cholinergic drugs act centrally to increase acetylcholine, not to suppress sympathetic nervous system activity. Autonomic effects are side effects, not therapeutic benefits.
4.Vasodilation and increased oxygen availability are not the primary therapeutic mechanism. Cognitive improvement is due to enhanced neurotransmission, not vascular changes. Cerebral perfusion is not significantly altered by cholinesterase inhibitors.
Test-taking strategy
- Identify the pathophysiology: Alzheimer’s involves acetylcholine deficiency.
- Eliminate options describing autonomic effects rather than central neurotransmission.
- Focus on the mechanism of cholinesterase inhibitors: increased acetylcholine in the brain.
- Select the option that directly addresses neurotransmitter restoration.
Take Home Points
- Alzheimer’s disease involves reduced acetylcholine due to degeneration of cholinergic neurons.
- Cholinesterase inhibitors increase acetylcholine by blocking its breakdown, improving cognition temporarily.
- Autonomic effects of cholinergics are side effects, not therapeutic mechanisms in dementia.
- Differentiating Alzheimer’s from other dementias is essential; treatment targets neurotransmitter deficits specific to Alzheimer’s pathology.
A nurse is teaching a client and family about the characteristics of dementia of the Alzheimer type. What characteristic should the nurse include?
Explanation
Alzheimer’s diseaseis a progressive neurocognitive disorder characterized by memory loss, impaired executive function, and cortical degeneration. A hallmark pathological feature is the presence of extracellular deposits known as senile plaques, composed primarily of beta-amyloid protein, which disrupt neuronal communication and contribute to neurodegeneration.
Rationale for correct answer:
4.Senile plaquesare areas of brain destruction formed by abnormal beta-amyloid deposits. These plaques interfere with synaptic transmission, trigger neuroinflammation, and contribute to neuronal death. Their presence, along with neurofibrillary tangles, defines the neuropathology of Alzheimer’s disease and explains the progressive cognitive decline.
Rationale for incorrect answers:
1.Periodic exacerbations are more characteristic of conditions with fluctuating courses, such as deliriumor multiple sclerosis. Alzheimer’s disease is progressive and irreversible, with steady decline rather than episodic worsening and recovery.
2.Aggressive acting-out behavior may occur in some clients due to frustration or disorientation, but it is not a defining characteristic. The hallmark features are cognitive declineand neuropathological changes, not behavioral aggression.
3.Hypoxia of selected brain tissue is not the primary mechanism in Alzheimer’s disease. While hypoxia can cause cognitive impairment, Alzheimer’s pathology is specifically linked to amyloid plaquesand neurofibrillary tangles, not vascular hypoxia.
Test-taking strategy
- Focus on hallmark pathological features of Alzheimer’s disease.
- Eliminate options describing nonspecific symptoms or unrelated mechanisms.
- Recall that Alzheimer’s is defined by plaques and tangles, not episodic or vascular changes.
- Select the option that directly addresses neuropathology.
Take Home Points
- Alzheimer’s disease is characterized by senile plaques and neurofibrillary tangles.
- The disease shows progressive, irreversible decline rather than episodic exacerbations.
- Behavioral changes may occur but are not defining features.
- Differentiate Alzheimer’s from vascular dementia, which involves ischemia and hypoxia of brain tissue.
A nurse is reviewing medications indicated for improvement in cognitive functioning in mild to moderate Alzheimer’s disease. Which medications are appropriate? Select all that apply.
Explanation
Cognitive enhancement in mild to moderate Alzheimer’s diseaseprimarily involves cholinesterase inhibitors, which increase acetylcholine availabilityin the brain, helping improve memory, attention, and overall cognitive function. These medications do not curethe disease but may slow cognitive decline.
Rationale for correct answers:
1.Donepezil (Aricept)is a cholinesterase inhibitor that prevents acetylcholine breakdown, improving synaptic transmission and enhancing cognitionin mild to moderate Alzheimer’s disease.
2.Rivastigmine (Exelon)inhibits both acetylcholinesterase and butyrylcholinesterase, increasing acetylcholine levels and improving memory, attention, and daily functioning.
5.Galantamine (Razadyne)is another cholinesterase inhibitor that enhances cholinergic transmissionand can modestly improve cognitive performance and behavioral symptoms.
Rationale for incorrect answers:
3.Risperidone (Risperdal)is an antipsychotic used for behavioral disturbancesin dementia (agitation, aggression), not for improving cognitive function.
4.Sertraline (Zoloft)is an SSRI antidepressant indicated for depression or anxiety; it does not directly enhance cognitionin Alzheimer’s disease.
Test-taking strategy
- Focus on cholinesterase inhibitorsfor cognitive improvement in mild to moderate Alzheimer’s.
- Exclude medications that are for behavioral or mood symptomsrather than cognition.
- Recall the mechanism: increase acetylcholine in the CNS.
Take Home Points
- Donepezil, Rivastigmine, and Galantamine are first-line cognitive enhancers.
- These medications slow cognitive declinebut do not cure Alzheimer’s disease.
- Antipsychotics and antidepressants address behavioral or mood symptoms, not cognition.
- Understanding mechanism of actionhelps differentiate medications for cognition versus behavior.
A client has a nursing diagnosis of disturbed sleep patterns related to increased anxiety as evidenced by an inability to fall asleep. Which short-term outcome is appropriate for this client?
Explanation
Disturbed sleep patterns related to anxietyinvolve difficulty initiating or maintaining sleep due to heightened physiological arousal and worry. Short-term outcomes should be specific, achievable, and directly linked to the presenting problem, focusing on immediate strategies to reduce anxiety and promote sleep.
Rationale for correct answer:
1.Using one coping skill before bedtimeis a specific, measurable, and realistic short-term outcomethat directly addresses the client’s inability to fall asleep caused by anxiety. It focuses on an immediate, achievable intervention.
Rationale for incorrect answers:
2.Sleeping 6–8 hours and feeling rested is a long-term goal, not a short-term, immediately achievable outcome, and may not be realistic without first addressing anxiety.
3.Asking for PRN medication is dependent on nurse/administered interventionsand is not a measure of the client’s own active coping or skill use; it is intervention-focused, not outcome-focused.
4.Verbalizing anxiety less than 3/10 is a cognitive outcome, which may take longer and does not directly measure the short-term goal of falling asleep.
Test-taking strategy
- Identify short-term, client-centered outcomesthat are specific and achievable.
- Focus on interventions that directly address the presenting problem(anxiety-induced sleep disturbance).
- Differentiate client behaviorsfrom long-term goals or dependent interventions.
- Use measurable actions (coping skills, relaxation techniques) for short-term outcomes.
Take Home Points
- Short-term outcomes should be specific, achievable, and measurable.
- Addressing the underlying causeof sleep disturbance (anxiety) is key.
- Client-directed actions (coping skills) are preferable for short-term goals.
- Long-term goals (sleep duration, feeling rested) are achieved after short-term interventionsare implemented.
A client diagnosed with primary dementia has a nursing diagnosis of altered thought process related to disorientation and confusion. Which nursing intervention should be implemented first?
Explanation
Assessment of cognitive status in primary dementiais the foundational step in care. Understanding the client’s level of disorientation and confusionguides safe, individualized interventions, prioritizes needs, and ensures appropriate strategies for safety, orientation, and agitation management.
Rationale for correct answer:
3.Assessing the client’s disorientation and confusionprovides critical baseline data to determine severity, triggers, and risks. Without assessment, interventions may be inappropriate or unsafe, and care cannot be tailored effectivelyto the client’s cognitive abilities.
Rationale for incorrect answers:
1.Using tranquilizers or restraints firstis inappropriate; these interventions are last-resort measuresand may worsen confusion or agitation if applied without prior assessment and justification.
2.Continual orientation is important, but its effectiveness depends on knowing the client’s current cognitive status; orientation strategies without assessment may be ineffective or frustrating.
4.Removing harmful objects improves safety, but prioritization requires knowing the client’s specific behaviors and level of risk, which comes from a proper assessment first.
Test-taking strategy
- Apply nursing process hierarchy: assessment precedes intervention.
- Determine baseline cognition, risk, and triggersbefore implementing strategies.
- Avoid immediate pharmacologic or restrictive interventions without evaluation.
- Prioritize data collection to guide safe, individualized care.
Take Home Points
- Assessment of disorientation and confusionis the first step in dementia care.
- Safety interventions and orientation strategies are guided by assessment findings.
- Pharmacologic or restrictive measures are last-resortand require justification.
- Accurate baseline assessment enables effective care planning and risk prevention.
Practice Exercise 6
A nurse is assessing a client with dementia. Which clinical manifestations are expected? Select all that apply.
Explanation
Dementiais a progressive decline in memory, reasoning, and attentionthat interferes with daily functioning. Clients often present with behavioral changes, impaired judgment, and difficulty with motor coordination. These manifestations reflect cortical and subcortical degeneration affecting multiple cognitive and functional domains.
Rationale for correct answers:
1.Agitationis common due to confusion, disorientation, and frustration with cognitive decline. Neurochemical changes and impaired coping mechanisms contribute to restlessness and irritability, often worsening in unfamiliar environments.
3.Short attention spanoccurs because dementia impairs concentration and the ability to sustain focus. Cortical degeneration disrupts attentional networks, leading to distractibility and difficulty completing tasks.
4.Disordered reasoningreflects impaired executive function. Clients struggle with problem-solving, judgment, and logical thought due to frontal lobe involvement, making decision-making unreliable and unsafe.
5.Impaired motor activitiesresult from apraxia, a cortical deficit where purposeful movement is disrupted despite intact motor strength. Clients may be unable to perform familiar tasks such as dressing or feeding themselves.
Rationale for incorrect answers:
2.Pessimism is not a defining manifestation of dementia. While mood changes such as depression can coexist, pessimism alone is not a diagnostic feature. Dementia is primarily characterized by cognitive and functional decline rather than personality outlook.
Test-taking strategy
- Identify hallmark features of dementia: memory loss, impaired reasoning, attention deficits, apraxia, and behavioral changes.
- Eliminate options that reflect mood or personality traits rather than cognitive decline.
- Apply DSM-5 criteria: decline in one or more cognitive domains with functional impairment.
- Select manifestations directly linked to cortical dysfunction.
Take Home Points
- Dementia manifests with agitation, short attention span, disordered reasoning, and impaired motor activities.
- Apraxia explains motor impairment despite intact strength.
- Mood traits like pessimism are not core diagnostic features.
- Differentiating dementia from delirium requires attention to chronicity and progressive decline versus acute onset.
A client in the early dementia stage of Alzheimer’s disease is admitted to a long-term care facility. Which activities must the nurse initiate? Select all that apply.
Explanation
Alzheimer’s diseasein the early dementia stage involves decline in memory, executive function, and orientation, but clients may still retain partial independence. Nursing care focuses on maintaining physical health, supporting structured routines, and promoting social engagement to slow regression and preserve dignity.
Rationale for correct answers:
1.Weekly weighingis important because dementia clients may forget meals, have altered appetite, or experience weight loss. Monitoring ensures nutritional status is maintained and allows early intervention for malnutrition or dehydration.
4.Establishing a schedule with rest periodssupports energy conservation and reduces agitation. Structured routines provide orientation cues, minimize confusion, and balance activity with rest, which is critical in early dementia care.
6.Weekly social entertainmentthrough senior groups promotes stimulation, reduces isolation, and maintains social skills. Engagement in structured activities helps preserve cognitive function and emotional well-being, slowing decline in early stages.
Rationale for incorrect answers:
2.Specialized rehabilitation equipment is not necessary in early dementia. The focus is on cognitive support and routine, not advanced physical rehabilitation, as motor strength is usually preserved at this stage.
3.Keeping the client in pajamas fosters dependency and disorientation. Normal clothing supports dignity, orientation to time of day, and maintenance of self-care abilities, which are essential in early dementia.
5.Reviewing budgets and community resources requires intact executive function, which is impaired in dementia. Expecting financial management is unrealistic and may cause frustration or errors, making this intervention inappropriate.
Test-taking strategy
- Apply Maslow’s hierarchy: prioritize physiological needs (nutrition, rest).
- Identify dementia care principles: structured routines, monitoring health, social stimulation.
- Eliminate options requiring intact executive function or promoting dependency.
- Select interventions that preserve independence and dignity while ensuring safety.
Take Home Points
- Early dementia care emphasizes structured routines, health monitoring, and social engagement.
- Nutrition and weight monitoring are critical due to risk of malnutrition.
- Social stimulation helps preserve cognition and emotional well-being.
- Avoid promoting dependency or expecting complex executive tasks in dementia clients.
A nurse is writing a plan of care for a client diagnosed with dementia. Which of the following are secondary prevention interventions? Select all that apply.
Explanation
Secondary preventionin dementia focuses on early detection and interventions that slow progression or minimize complications once the disease is present. It emphasizes maintaining cognitive function, reducing confusion, and supporting adaptation to deficits to prevent worsening disability.
Rationale for correct answers:
1.Reinforcing speech with nonverbal techniques supports communicationwhen verbal ability declines. This intervention reduces frustration and confusion, helping preserve cognitive interactionand slowing deterioration of functional abilities, which is consistent with secondary prevention.
2.Keeping surroundings simple by reducing clutterminimizes environmental stressors that worsen disorientation. A simplified environment enhances orientation and safety, preventing further confusion and behavioral disturbances, aligning with secondary prevention strategies.
4.Placing a large, visible clock and calendarprovides external cues that reinforce orientation to time and place. This intervention reduces disorientationand supports memory recall, helping stabilize cognitive decline rather than allowing worsening confusion.
Rationale for incorrect answers:
3.Offering family ethics consultation or hospice assistance is a tertiary preventionmeasure. It addresses advanced disease stages by focusing on comfort, end-of-life decisions, and quality of life rather than slowing progression.
5.Talking to family members about genetic predisposition is a primary preventionmeasure. It involves education and risk awareness before disease onset, not interventions for clients already diagnosed with dementia.
Test-taking strategy
- Differentiate prevention levels: primary (risk reduction), secondary (early detection and stabilization), tertiary (rehabilitation and end-of-life).
- Apply Maslow’s hierarchy: secondary prevention supports safety and orientation needs.
- Eliminate options that focus on pre-disease education or advanced-stage care.
- Select interventions that stabilize symptoms and prevent worsening confusion.
Take Home Points
- Secondary prevention in dementia emphasizes stabilizing cognition and preventing worsening disorientation.
- Environmental simplification and orientation cues are effective strategies to reduce confusion.
- Communication reinforcement helps maintain functional interaction and reduces frustration.
- Distinguishing primary, secondary, and tertiary prevention ensures appropriate interventions across disease stages.
A nurse is working with clients with late-stage Alzheimer’s dementia. Which is a priority intervention?
Explanation
Alzheimer’s disease (late-stage)involves severe cognitive decline, functional dependence, and high risk of dysphagia, aspiration, and electrolyte imbalance. Progressive neurodegeneration impairs swallowing, appetite, and recognition of hunger/thirst, making hydration and nutrition essential to prevent delirium, arrhythmias, and acute kidney injury.
Rationale for correct answer:
1.Late-stage Alzheimer’s commonly causes impaired swallowing and reduced intake, leading to dehydrationand electrolyte imbalancethat precipitate delirium, cardiac instability, and renal dysfunction. Prioritizing fluids and food addresses physiological survival needs first and reduces aspiration risk with supervised feeding and texture modification.
Rationale for incorrect answers:
2.Frequent reorientation is minimally effective in late-stage disease due to profound memory encoding deficits. Over-reorientation can heighten agitationand distress; supportive validation and environmental cues are preferable, but they do not supersede immediate physiological needs like hydration and nutrition.
3.Encouraging independent ADLs supports dignity earlier in the course, but late-stage patients have severe apraxiaand dependence. Pushing independence may increase fatigue, frustration, and unsafeattempts, while failing to address urgent risks from inadequate intake and metabolic derangements.
4.Fall prevention is important, yet ambulation assistance is secondary when dysphagiaand dehydrationthreaten acute medical instability. If the patient is weak or hypotensive from poor intake, ambulation may increase falland syncoperisk; stabilize fluids and nutrition first, then implement mobility safety.
Test-taking strategy
- Identify the stage: late-stage implies severe cognitive and functional decline.
- Apply Maslow: prioritize physiological needs—airway, breathing, circulation, hydration, nutrition.
- Recognize immediate risks: dysphagia, dehydration, electrolyte imbalance.
- Safety is vital but follows stabilization of basic physiological needs.
- Reorientation is less effective late-stage; validation and comfort are supportive, not priority.
Take Home Points
- Late-stage Alzheimer’s often presents with dysphagia and poor intake; prioritize hydration and nutrition to prevent metabolic and cardiac complications.
- Reorientation has limited utility in severe cognitive impairment; use validation and calm environments to reduce distress.
- Promote independence earlier in disease; late-stage care focuses on comfort, safety, and assisted ADLs.
- Differentiate priorities: physiological stabilization (fluids/food) precedes fall prevention and cognitive strategies in advanced neurocognitive disorder.
A client is in the hospital with a diagnosis of vascular neurocognitive disorder (NCD). In explaining this disorder to the client’s family, which statement by the nurse is correct?
Explanation
Vascular neurocognitive disorder (vascular NCD)results from cerebrovascular disease, including multiple small strokes or chronic ischemia, leading to cognitive decline that progresses in a step-wise pattern. Unlike Alzheimer’s disease, symptoms may remain stable for periods and then suddenly worsenafter vascular events.
Rationale for correct answer:
2.The step-wise progressionrefers to the characteristic pattern of vascular NCD, where cognitive function may remain stable for weeks or months, then suddenly declineafter additional cerebrovascular insults. This explains why the client sometimes appears relatively normalbetween episodes.
Rationale for incorrect answers:
1.Survival is variableand depends on comorbidities; vascular NCD does not consistently result in longer survival than Alzheimer’s disease.
3.Plaques and tangles are characteristic of Alzheimer’s disease, not vascular NCD, which is caused by ischemic or hemorrhagic brain injury.
4.The cause of vascular NCD is well understood—it results from cerebrovascular disease, not an unknown etiology.
Test-taking strategy
- Differentiate Alzheimer’s disease vs vascular NCD: plaques/tangles vs ischemic injury.
- Recognize the step-wise cognitive declineas hallmark of vascular NCD.
- Use progression patterns to guide family education.
Take Home Points
- Vascular NCD results from cerebrovascular insults.
- Cognitive decline is step-wise, not gradual like Alzheimer’s.
- Plaques and tangles are Alzheimer’s-specific pathology, not vascular NCD.
- Educate families about possible sudden changes and variability in symptoms.
Comprehensive Questions
A nurse is attempting to assess the behavior of an older adult diagnosed with vascular dementia. The nurse considers that the client probably is:
Explanation
Vascular dementiais a progressive decline in cognition, reasoning, and memorycaused by cerebrovascular disease. Clients often show stepwise deterioration with focal deficits. Because of impaired adaptability, they rely heavily on previously established coping styles, often exaggerating old defense mechanisms rather than developing new ones.
Rationale for correct answer:
3.Clients with vascular dementia make exaggerated use of old, familiar mechanismsbecause cognitive decline limits the ability to adapt or create new strategies. Reliance on past coping styles reflects impaired executive functionand reduced flexibility, leading to rigid, repetitive behaviors that provide a sense of security.
Rationale for incorrect answers:
1.Saying clients are not capable of using any defense mechanisms is inaccurate. Even with dementia, individuals retain some psychological coping strategies, though they are limited and often maladaptive.
2.Using one method of defense for every situation oversimplifies behavior. While reliance on familiar defenses is common, clients may still vary responses depending on context, though exaggerated patterns dominate.
4.Attempting to develop new defense mechanisms is unlikely because dementia impairslearningand adaptability. Neurocognitive decline prevents the creation of novel coping strategies, making this option inconsistent with disease progression.
Test-taking strategy
- Focus on the pathophysiology: vascular dementia causes impaired adaptability and executive dysfunction.
- Eliminate options suggesting absence of defenses or creation of new ones.
- Select the option emphasizing reliance on exaggerated familiar coping styles.
- Apply Maslow’s hierarchy: psychological security is maintained through familiar routines and defenses.
Take Home Points
- Vascular dementia clients rely on exaggerated old defense mechanisms due to impaired adaptability.
- Cognitive decline prevents development of new coping strategies.
- Defense mechanisms remain but are rigid and repetitive.
- Differentiating vascular dementia from Alzheimer’s: vascular dementia often shows stepwise decline linked to cerebrovascular events.
A nurse is planning care for a client with vascular dementia. What should be included in the plan of care?
Explanation
Vascular dementiais a progressive decline in memory, reasoning, and executive functioncaused by cerebrovascular disease. Clients often experience stepwise deterioration, focal neurological deficits, and impaired adaptability. Care planning focuses on supportive measures that maintain comfort, dignity, and safety rather than reeducation or new learning, which are limited by cognitive decline.
Rationale for correct answer:
2.Supportive careis the most appropriate intervention because vascular dementia clients cannot relearn or adapt effectively due to impaired cognitionand poor executive function. Supportive care emphasizes maintaining physical health, ensuring safety, and providing emotional support, which directly addresses the progressive and irreversible nature of the disease.
Rationale for incorrect answers:
1.A reeducation program is ineffective because dementia impairs the ability to learn new information. Neurocognitive decline prevents successful reeducation, making this option unrealistic and inappropriate.
3.Introducing new leisure-time activities requires intact learningand adaptability, which are compromised in dementia. Clients benefit more from familiar routines and activities that reinforce existing skills rather than new ones.
4.Group therapy sessions may be overwhelming due to impaired communicationand reasoning. While social support is valuable, structured supportive care tailored to individual needs is more effective than group therapy in advanced cognitive decline.
Test-taking Strategy
- Identify the pathophysiology: vascular dementia involves irreversible cognitive decline.
- Eliminate options requiring new learning or adaptation.
- Apply Maslow’s hierarchy: prioritize supportive care that ensures safety and comfort.
- Select the option that aligns with realistic, evidence-based dementia management.
Take Home Points
- Vascular dementia requires supportive care focused on safety, comfort, and dignity.
- Reeducation and new activities are ineffective due to impaired learning capacity.
- Group therapy may overwhelm clients with severe cognitive decline.
- Differentiating vascular dementia from Alzheimer’s: vascular dementia often shows stepwise decline linked to cerebrovascular events.
A nurse is assessing a client and attempting to distinguish between dementia and delirium. Which factors are unique to delirium? Select all that apply.
Explanation
Deliriumis an acute, fluctuatingneurocognitive syndrome characterized by impaired attention. Unlike the irreversible decline seen in dementia, this state is typically temporary and results from an underlying physiological disturbanceor toxicity.
Rationale for correct answer:
6.This represents the defining clinical characteristicdifferentiating the two states. While patients with dementia remain alert and stable, those in an acute confusional state exhibit a waxing and waningof awareness and arousal levels throughout the day.
Rationale for incorrect answers:
1.This sign is frequently observed during acute metabolic encephalopathydue to global brain dysfunction. However, it is not exclusively unique because it also manifests in end-stage dementiaor as a side effect of various psychotropic medications.
2.Rapid changes in affect are highly common during acute confusion episodes. Nevertheless, this symptom overlaps significantly with various neurodegenerative disorders, particularly frontotemporal dementia, where emotional dysregulation is a prominent feature rather than a unique identifier.
3.The loss of remote information is a hallmark of chronic neurocognitive deterioration. In the acute syndrome, the patient experiences a sudden inability to encode new informationdue to inattention, rather than a primary loss of long-established memories.
4.Sensory disturbances often occur when the brain is under acute toxic stress. However, they are also a core diagnostic feature of Lewy Body dementia, meaning they cannot be considered strictly unique to the acute confusional condition.
5.This term describes a slow and subtletransition into cognitive impairment over several years. This temporal pattern is the hallmark of progressive dementia, whereas the acute syndrome is defined by a sudden, rapid onset of symptoms.
Test-taking strategy
- Identify the core difference between acute and chronic cognitive impairment.
- Apply the principle of stability versus fluctuation.
- Eliminate symptoms common to both or specific to dementia.
- Select the answer reflecting the most significant physiological difference in consciousness.
Take Home Points
- The hallmark of delirium is an acute change in mental status with a fluctuating course and impaired attention.
- Dementia is distinguished by its gradual, insidious onset and a level of consciousness that remains stable until the final stages.
- Delirium is often reversible once the underlying medical cause, such as infection or electrolyte imbalance, is identified and corrected.
- Nurses must prioritize physical safety and physiological stability while performing a thorough assessment to identify the trigger of sudden confusion.
A nurse’s best approach when caring for a confused, older client is to provide an environment with:
Explanation
Confusional statesin older adults often involve fluctuations in cholinergic activityand neurotransmitter imbalances. Providing a stable environment helps regulate cortisol levels, reducing the physiological stress response and preventing the cognitive exhaustion that occurs with overstimulation.
Rationale for correct answer:
3.Developing a consistent therapeutic allianceprovides the psychological safety required to mitigate anxiety in cognitively impaired patients. A reliable caregiver relationship facilitates accurate clinical assessmentand emotional stability, which are vital for maintaining the client's remaining functional and cognitive abilities.
Rationale for incorrect answers:
1.Granting excessive seclusion often results in sensory deprivation, which can paradoxically worsen disorientation and trigger hallucinations in the geriatric population. Clients with diminished cognitive capacity require frequent environmental cuesand social orientation to maintain a connection with their immediate reality.
2.Engaging in complex social interactions frequently leads to sensory overstimulation, overwhelming the patient’s limited processing capacity and potentially causing agitation. Therapeutic activities should be highly structuredand tailored to the individual’s cognitive threshold rather than relying on group dynamics.
4.Exposure to a wide variety of tasks or changes in routine can lead to cognitive fragmentationand significant frustration. For those with impaired memory and orientation, a predictable and repetitiveschedule is essential to reduce the neurological demand and prevent behavioral outbursts.
Test-taking strategy
- Identify the client's primary need as safety and security within Maslow's hierarchy.
- Analyze the environmental requirements for a patient with cognitive deficits.
- Eliminate choices that increase cognitive load or environmental complexity.
- Select the option that prioritizes stability and the development of a therapeutic relationship.
Take Home Points
- Environmental management for confused older adults focuses on maximizing safety and minimizing stressors to prevent cognitive overload.
- Consistency in staffing and daily routines provides the necessary structure to help orient patients and reduce their level of agitation.
- Overstimulation from varied activities or group settings can trigger catastrophic reactions in individuals with moderate to severe dementia.
Effective geriatric nursing care utilizes a calm, supportive approach that prioritizes the establishment of a trusting, predictable relationship with the patient.
An older adult on the mental health unit begins acting out while in the day room. What is a nurse’s initial intervention?
Explanation
Behavioral agitationinvolves an acute state of neuropsychiatric dysregulationwhere a patient loses impulse control. This condition requires immediate de-escalation techniquesto stabilize the autonomic nervous system and ensure environmental safety without using provocative stimuli.
Rationale for correct answer:
3.Delivering clear, low-frequency auditory cueshelps stabilize a patient’s heightened arousal by avoiding the high-pitched tonesoften associated with alarm or aggression. This technique provides external cognitive structureand calm direction, which is vital for patients experiencing an acute loss of emotional self-regulation.
Rationale for incorrect answers:
1.Issuing a command to be quiet is a punitive communication stylethat frequently exacerbates agitation by inducing feelings of threat. This approach fails to address the underlying distressand lacks the necessary therapeutic support to help the client regain internal behavioral control.
2.Passive observation during an outburst is a safety violationthat places the client and others at risk for physical harm. It ignores the hemodynamic strainand potential for metabolic exhaustionthat occurs during prolonged periods of intense physical or emotional acting out.
4.Touching an agitated patient can be misinterpreted as a hostile physical restraint, potentially triggering a violent defensive response. In geriatric psychiatry, maintaining personal spaceis critical during de-escalation to prevent the client from feeling trapped or physically threatened.
Test-taking strategy
- Prioritize the least restrictive and safest intervention for an agitated client.
- Apply de-escalation principles that avoid physical contact and authoritarianism.
- Recognize that high-pitched sounds can escalate anxiety in confused older adults.
- Select the option that utilizes therapeutic communication to provide immediate redirection.
Take Home Points
- De-escalation in the geriatric population focuses on reducing environmental stimuli and providing calm, clear, and non-threatening verbal directions.
- Physical touch should be avoided during acute agitation as it may be perceived as a threat, potentially escalating the client’s behavior into physical aggression.
- The nurse’s primary goal during an outburst is to maintain the safety of the client and others while helping the individual regain emotional control.
- Firm, low-pitched vocalizations are more effective than high-pitched or loud commands because they are easier for older adults to process without triggering a fear response.
A 76-year-old client is admitted to a long-term-care facility with a diagnosis of Alzheimer’s-type dementia. The client has been wearing the same dirty clothes for several days, and the nurse contacts the family to bring in clean clothing. Which intervention would best prevent further regression in the client’s personal hygiene?
Explanation
Alzheimer’s-type dementiainvolves a neurodegenerative process characterized by amyloid plaques. This leads to synaptic failurein the cortex, impacting the patient's motor planningand the ability to complete complex sequencesof daily living.
Rationale for correct answer:
1.Supporting functional autonomyprevents the rapid loss of learned motor skills. Encouraging participation utilizes muscle memoryand maintains dignity, which is essential to prevent the psychological and physical regressioncommon in chronic cognitive decline.
Rationale for incorrect answers:
2.Demanding complete self-reliancefrom a cognitively impaired individual is developmentally inappropriate. Since the condition involves severe executive dysfunction, the client lacks the neural capacity to organize and execute the necessary hygiene tasks independently.
3.Total staff intervention fosters learned helplessness, accelerating the loss of physical capability. When the nurse performs every action, the client’s remaining neural pathwaysfor self-care undergo atrophy due to a lack of use.
4.Allowing poor hygiene violates infection controlstandards and basic health needs. Neglecting hygiene allows for the accumulation of pathogens, leading to dermal complicationsand potential systemic illness, which ignores the client's underlying physiological vulnerability.
Test-taking strategy
- Prioritize independence to maintain function.
- Use Maslow's hierarchy to address hygiene without removing autonomy.
- Avoid the extremes of total neglect or total care.
- Focus on interventions that preserve the client's current skill level.
Take Home Points
- Maintaining functional independence is the primary goal to slow the physical and cognitive regression associated with neurodegenerative disorders.
- The use of verbal prompts and physical cues allows clients to complete familiar tasks without experiencing the frustration of total failure.
- Complete dependence on staff for activities of daily living should be avoided as it contributes to the loss of overlearned motor skills.
- Hygiene interventions must balance the client’s psychiatric symptoms with the physiological need to prevent skin breakdown and infection.
An adult daughter of a client manifesting dementia expresses concern about her elderly father still driving his car. Which response by the nurse will educate the woman about mild dementia?
Explanation
Mild dementiainvolves a decline in executive functioningand visuospatial orientation. This stage is characterized by short-term memorydeficits and a reduced ability to process complex environmentalstimuli effectively.
Rationale for correct answer:
1.During the early stages of cognitive decline, the brain struggles with sustained attentionand spatial navigation. The inability to process simultaneous cueswhile driving, combined with geographic disorientation, represents a critical safety risk that stems directly from cortical impairment.
Rationale for incorrect answers:
2.While behavioral changes occur, severe aggression is more characteristic of the moderate stagerather than mild impairment. Predicting a specific emotional reaction is secondary to addressing the immediate safety hazardposed by the client’s failing cognitive and motor coordination.
3.Chronic sleep disturbances are common in neurodegeneration but are not the primary diagnostic indicatorfor driving cessation. The most significant risk factor is the loss of judgment and reactiontime, rather than fatigue-related recklessness typical of younger populations.
4.Increased confusion during evening hours, known as nocturnal wanderingor sundowning, typically intensifies as the disease progresses to middle stages. In the mild stage, the primary concern is the daytime failureof navigation and the inability to handle unexpected traffic variables.
Test-taking strategy
- Focus on the hallmark symptoms of early-stage dementia.
- Connect cognitive deficits (memory/orientation) to functional activities like driving.
- Distinguish between early, middle, and late-stage symptoms.
- Prioritize safety and orientation over behavioral or sleep issues.
Take Home Points
- Mild dementia is often first noticed through a loss of complex instrumental activities of daily living, such as managing finances or driving.
- Executive dysfunction in early cognitive decline impairs the ability to make rapid decisions and navigate familiar routes safely.
- Families should be educated that getting lost in familiar places is a red flag indicating that the client's spatial memory is compromised.
- Driving cessation is a multidisciplinary decision based on the client's objective inability to concentrate and react to changing environmental stimuli.
A daughter of an 82-year-old client with Alzheimer’s contacts a clinic because the client has been unwilling to drink any fluids for over 24 hours. Which instruction by the nurse is most appropriate?
Explanation
Dehydrationin geriatric patients leads to rapid extracellular fluiddepletion and electrolyte shifts. This condition often results from an impaired thirst mechanismor the inability to communicate physiological needs, potentially causing hemodynamic instabilityin a very short period.
Rationale for correct answer:
3.The nurse must first perform a comprehensive assessmentto determine the severity of the fluid deficit. Identifying secondary symptoms like altered mental status, orthostatic hypotension, or concentrated urine helps distinguish between a mild refusal and a life-threatening crisis.
Rationale for incorrect answers:
1.Directing the client to the emergency department is premature without first evaluating the clinical presentation. While fluid replacement may be necessary, the nurse must first gather assessment datato justify such a high-intensity intervention for a cognitively impaired individual.
2.Requesting laboratory work is an appropriate secondary step, but it should not precede a symptomatic evaluation. Laboratory values like blood urea nitrogenand creatinine levels confirm the diagnosis, but the initial telephone interaction must focus on the patient's immediate physiological state.
4.Delaying further contact until the following day is dangerous for a patient who has already been fluid-deprivedfor 24 hours. Given the diminished physiological reservein an 82-year-old, waiting another day could lead to acute kidney injury or severe electrolyte imbalances.
Test-taking strategy
- Always follow the nursing process by assessing before intervening.
- Apply Maslow’s hierarchy by prioritizing the physiological need for hydration.
- Recognize the vulnerability of the elderly to rapid fluid loss.
- Eliminate options that delay care or provide an intervention without data.
Take Home Points
- Assessment is the priority nursing action when a caregiver reports a significant change in the physiological status of a geriatric patient.
- Dehydration in older adults can manifest as sudden confusion, which may be mistaken for a progression of their dementia.
- Skin turgor is an unreliable indicator of hydration in the elderly; instead, nurses should assess mucous membranes and postural blood pressure.
- Early intervention for fluid refusal involves identifying the underlying cause, such as oral pain, swallowing difficulties, or an acute infection.
A home-care nurse is visiting the home of a client diagnosed with Alzheimer’s disease. Which question by the nurse is most appropriate when attempting to assess the level of depression that the client’s husband is experiencing as the primary caregiver?
Explanation
Caregiver role strainis a multidimensional stress response that often leads to depressive disordersin those managing chronic illness. This state results from an imbalance between environmental demandsand the caregiver's coping resources, frequently manifesting as anhedoniaand social isolation.
Rationale for correct answer:
2.This inquiry specifically targets anhedonia, a core diagnostic criterion for clinical depression. By asking about leisure, the nurse assesses whether the husband still experiences pleasure in activities, which provides a direct window into his emotional well-beingand the presence of depressive symptoms.
Rationale for incorrect answers:
1.Focusing on the need for help addresses resource allocationrather than the caregiver's internal emotional state. While it identifies a need for respite care, it does not provide diagnostic information regarding the husband’s neurovegetative or moodsymptoms.
3.Asking if a situation is stressful often prompts a defensive or socially desirableresponse. Stress is an expected component of caregiving, but it is not synonymous with clinical depression, and this closed-ended approach may fail to uncover deeper psychological distress.
4.This statement is a presumptive generalizationthat can be perceived as judgmental or dismissive of the caregiver's devotion. Using declarative statementsinstead of therapeutic questions blocks the client from expressing their true feelings and can damage the therapeutic rapport.
Test-taking strategy
- Use therapeutic communication techniques that identify symptoms of depression.
- Look for the option that assesses for anhedonia or loss of interest.
- Eliminate closed-ended questions that lead to "yes/no" answers.
- Avoid making assumptions about the caregiver's feelings or lifestyle.
Take Home Points
- Assessment of caregiver depression should focus on identifying loss of interest in previously enjoyed activities and social withdrawal.
- Caregivers of Alzheimer's patients are at high risk for physical and mental health decline due to the chronic nature of the disease.
- Open-ended questions are the most effective tool for allowing caregivers to voice their emotional burdens without feeling guilty.
- Identifying caregiver strain early is essential to ensure the safety of both the caregiver and the patient with dementia.
An elderly client with Alzheimer’s dementia is being admitted from a postanesthesia unit following a hip hemiarthroplasty to treat a hip fracture. Which intervention should a nurse initially plan for the client’s pain control?
Explanation
Alzheimer’s dementiaaffects the prefrontal cortex, which significantly impairs a patient's ability to interpret and communicate pain. This neurological deficit often leads to the under-treatment of pain, which can manifest as increased agitation, aggression, or a rapid decline in functional status.
Rationale for correct answer:
4.Providing preventative analgesiais the standard of care for patients with significant cognitive impairment. Since the client cannot reliably report pain or recall the need for medication, around-the-clock administrationensures a therapeutic blood level of the drug, preventing the cyclical escalationof post-surgical distress.
Rationale for incorrect answers:
1.Utilizing a transdermal delivery system is inappropriate for acute post-operative painmanagement. These patches have a slow onset of action, often taking 12 to 24 hoursto reach a steady state, making them unsuitable for the immediate, intense pain following a major orthopedic procedure.
2.Self-directed analgesia requires the patient to have the cognitive capacityto understand the relationship between pain and the demand button. A client with advanced neurodegeneration lacks the executive functionto use a PCA pump safely or effectively, leading to either overdose or significant pain.
3.Relying on a subjective report is ineffective because dementia patients may have aphasia or agnosia, preventing them from vocalizing discomfort. Waiting for the client to ask for medication violates the principle of proactive pain managementand ignores the physiological reality of the patient’s sensory and cognitive barriers.
Test-taking strategy
- Prioritize physiological needs using Maslow's hierarchy for a post-operative patient.
- Recognize that "PRN" or "report of pain" is inappropriate for cognitively impaired clients.
- Eliminate options that require high-level cognitive functioning (PCA).
- Select the most proactive and consistent method of delivery for acute pain.
Take Home Points
- Patients with dementia require objective pain assessment tools, such as the PAINAD scale, which focuses on breathing, vocalization, and body language.
- Around-the-clock (ATC) dosing is the preferred strategy for postoperative analgesia in patients who cannot utilize self-report mechanisms.
- Untreated pain in the elderly is a leading cause of postoperative delirium and can significantly delay the rehabilitation process.
- Intravenous opioids must be monitored closely for side effects like respiratory depression and constipation, particularly in the opioid-naive geriatric population.
An older adult is brought to the clinic by a family member because of increasing confusion over the past week. What can a nurse ask the client to assess orientation to place?
Explanation
Spatial orientationis a cognitive function that relies on the integration of hippocampal processingand cortical awareness. It requires the brain to retrieve environmental dataand compare it with the individual's current physical location to maintain a continuous sense of geographic awareness.
Rationale for correct answer:
3.Asking the client to name their current location assesses situational awarenessand the ability to process immediate environmental cues. This specific question tests orientation to place, which is a fundamental component of a mental status examination and often the first to be lost in acute confusion.
Rationale for incorrect answers:
1.Interpreting a metaphorical statement evaluates abstract reasoningrather than spatial orientation. This task involves the higher-order processingof the frontal lobe and is used to assess intellectual depth and judgment rather than the client's awareness of their physical surroundings.
2.Recalling one's birthplace measures long-term remote memorystored in the temporal cortex. While this provides information about the client's history, it does not determine if they are currently oriented to the presentlocation or understand their current environment in the clinic.
4.Mentioning recent dietary intake is a test of short-term memoryand recent recall. Although memory deficits often accompany disorientation, being able to remember a meal does not confirm that the client knows where they arephysically located at the time of the assessment.
Test-taking strategy
- Focus on the specific domain of the mental status exam requested (place).
- Distinguish between memory (past events) and orientation (current facts).
- Eliminate tasks related to abstract thinking or long-term retrieval.
- Select the option that directly links the client to their current geographic environment.
Take Home Points
- Orientation is traditionally assessed in the sequence of person, place, time, and situation, with time typically being the first orientation lost.
- Assessing orientation to place requires the client to identify their current immediate environment, such as the name of the building or the city.
- A sudden change in orientation over one week strongly suggests an acute condition, such as delirium, rather than the slow progression of dementia.
- Disorientation is a physiological sign of cerebral dysfunction and necessitates further investigation into metabolic, infectious, or toxic causes.
A client has been diagnosed with a neurocognitive disorder (NCD) due to Alzheimer’s disease. Which primary nursing intervention should the nurse implement when working with the client?
Explanation
Primary nursing care for clients with NCD due to Alzheimer’s diseasefocuses on safety and injury prevention, as cognitive decline leads to impaired judgment, memory loss, and disorientation, increasing the risk for falls, wandering, and accidents. Maintaining a secure environmentis foundational before addressing secondary needs.
Rationale for correct answer:
2.Ensuring the environment is safedirectly reduces the risk of injury due to wandering, confusion, or impaired judgment. Safety is the highest priority interventionbecause cognitive decline compromises the client’s ability to recognize hazards.
Rationale for incorrect answers:
1.Providing preferred foods addresses nutrition, which is important but secondary to safety, and does not prevent acute risks.
3.Encouraging socialization helps prevent isolation and improves emotional well-being, but safety takes precedence over social needs in NCD.
4.Supporting ADLs promotes independence, but forcing or prioritizing self-care in advanced Alzheimer’s may increase frustration or risk, making safety the primary concern first.
Test-taking strategy
- Apply Maslow’s hierarchy: physiological and safety needs first.
- Prioritize interventions that prevent harm or injury.
- Differentiate primary (safety) from secondary (nutrition, socialization, ADLs) interventions.
Take Home Points
- Safety is the highest priorityfor clients with Alzheimer’s due to cognitive decline.
- Environmental modifications reduce the risk of falls, wandering, and accidents.
- Nutritional, social, and ADL support are secondary but important.
- Nursing care should prioritize life-threatening or injury risks first.
A client is displaying behaviors consistent with stage 2 Alzheimer’s disease. The client can no longer recognize family members and requires assistance with personal hygiene and dressing. The client is frequently incontinent of both urine and feces and displays violent outbursts during these times. Which nursing diagnoses should the nurse give highest priority to when developing the client’s care plan?
Explanation
Stage 2 Alzheimer’s disease and behavioral managementinvolves severe cognitive decline, including loss of recognition, dependence in ADLs, incontinence, and agitation. During this stage, safety is the top priority, especially when the client displays violent behaviors that could harm self or others.
Rationale for correct answer:
1.Violence directed at self or others poses an immediate safety risk, which supersedes other care needs. Clients with stage 2 Alzheimer’s may react aggressively due to fear, confusion, or frustration, making preventing injurythe highest priority nursing focus.
Rationale for incorrect answers:
2.Incontinence requires ongoing careand hygiene maintenance, but it does not pose an immediate threat to safetycompared with violent outbursts.
3.Self-care deficits in hygiene, dressing, and toileting are significant for quality of life, yet they are secondary to ensuring the client and others remain safeduring episodes of aggression.
4.Altered thought processes with impaired memory are inherent in stage 2 Alzheimer’s, but cognitive impairment alone is less urgentthan the risk of harm from violent behavior.
Test-taking strategy
- Prioritize using Maslow’s hierarchy: safety first.
- Identify which problem poses the most immediate risk.
- Recognize that behavioral violencecan cause injury, while self-care deficits or incontinence, though important, are secondary priorities.
- Apply ABC (Airway, Breathing, Circulation) plus safetyreasoning in dementia care.
Take Home Points
- In stage 2 Alzheimer’s, violent behavior can be sudden and dangerous.
- Safety always takes precedence over self-care or comfort needs.
- Incontinence and self-care deficits impact quality of life but are secondary in acute risksituations.
Understanding the progression of cognitive declinehelps prioritize nursing interventions effectively.
A home health nurse caring for a client diagnosed with Alzheimer’s disease is attempting to determine whether the client’s daughter understands the client’s prognosis. Which of the daughter’s questions to the nurse will most accurately assess the daughter’s understanding of Alzheimer’s disease and its prognosis?
Explanation
Alzheimer’s disease prognosis and caregiver understandinginvolves progressive neurodegenerationthat currently has no cure. The focus is on supportive care, symptom management, and caregiver resources. Understanding prognosis includes recognizing that functional decline is inevitable, and planning for long-term care is essential.
Rationale for correct answer:
1.Asking about support servicesdemonstrates that the daughter understands Alzheimer’s is progressive and incurable, and that care focuses on assistance, safety, and quality of life, not reversing memory loss. It reflects realistic comprehension of prognosis.
Rationale for incorrect answers:
2.Asking how to improve memoryindicates a misunderstanding of prognosis; Alzheimer’s causes irreversible cognitive decline, and no interventions can restore memory fully.
3.Asking about medication effectiveness suggests the daughter expects a cure or rapid improvement, which is inconsistent with the progressive, degenerative natureof the disease.
4.Asking about the “best treatment program” implies an expectation of curative or advanced intervention, rather than understanding that care is supportive and long-term.
Test-taking strategy
- Identify questions reflecting realistic understanding of progressive, incurable disease.
- Distinguish between supportive care vs curative expectations.
- Use cues from the question to determine focus on prognosis comprehension.
- Eliminate answers focused on memory improvement or rapid treatment outcomes.
Take Home Points
- Alzheimer’s disease is progressive and currently incurable; care focuses on support.
- Understanding prognosis includes recognizing the need for support servicesfor the patient and family.
- Caregivers often misunderstand medications or interventions as curative; education is key.
- Assessment of caregiver understanding guides planning for safety, long-term care, and resources.
A client says to the nurse: “I read an article about Alzheimer’s and it said the disease is hereditary. My mother has Alzheimer’s disease. Does that mean I’ll get it when I’m old?” The nurse bases her response on the knowledge that which factor is not associated with increased incidence of NCD due to Alzheimer’s disease?
Explanation
Neurocognitive disorder (NCD) due to Alzheimer’s diseaseis primarily influenced by age, genetics, and certain lifestyle or environmental factors. While some risk factors increase susceptibility, vascular events like small strokes are associated with vascular dementia, not Alzheimer’s disease, and do not directly increase the incidence of Alzheimer’s NCD.
Rationale for correct answer:
1.Multiple small strokescontribute to vascular neurocognitive disorderby causing cumulative brain infarcts. These are not a recognized risk factor for Alzheimer’s disease, so they do not increase its incidence.
Rationale for incorrect answers:
2.Family history of Alzheimer’s diseaseis a significant risk factor due to genetic predisposition, particularly in early-onset forms.
3.Head traumaincreases the risk of Alzheimer’s disease by accelerating amyloid deposition and neuronal injury, contributing to neurodegeneration.
4.Advanced ageis the strongest risk factor; incidence rises sharply after age 65, with prevalence increasing dramatically in older populations.
Test-taking strategy
- Identify risk factors specific to Alzheimer’s diseaseversus other forms of NCD.
- Exclude factors primarily associated with vascular or secondary dementias.
- Focus on well-established epidemiological and genetic risk factors.
Take Home Points
- Alzheimer’s disease risk increases with advanced age, family history, and head trauma.
- Multiple small strokes are primarily linked to vascular NCD, not Alzheimer’s.
- Understanding risk factors helps in patient education and preventive strategies.
- Genetic predisposition does not guarantee disease, but it elevates susceptibility.
Exams on Dementia And Alzheimer’s Disease
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
- Objectives
- Introduction
- Definition And Classification Of Dementia
- Practice Exercise 1
- Alzheimer’s Disease
- Practice Excercise 2
- Differences Between Dementia And Alzheimer’s Disease
- Nursing Management Of Dementia
- Practice Excercise 3
- Pharmacological Management Of Dementia And Alzheimer’s Disease
- Psychosocial And Behavioral Management
- Practice Exercise 4
- Complications And Prognosis
- Ethical And Legal Considerations In Dementia Care
- Practice Exercise 5
- Prevention And Health Education
- Role Of The Nurse In Community And Institutional Care
- Practice Exercise 6
- Summary
- Comprehensive Questions
Notes Highlighting is available once you sign in. Login Here.
Objectives
At the end of this topic, the learner should be able to:
- Define dementia and classify its types scientifically.
- Describe the epidemiology of dementia, including global and regional prevalence, incidence, and demographic patterns.
- Explain the etiology and major risk factors contributing to the development of dementia.
- Discuss the pathophysiological mechanisms underlying dementia.
- Differentiate between various forms of dementia based on their neuropathological and clinical features.
- Describe Alzheimer’s disease as the most common cause of dementia.
- Identify the stages, clinical manifestations, diagnostic criteria, and management strategies of Alzheimer’s disease.
- Explain the pharmacological and non-pharmacological approaches used in the treatment and nursing care of patients with dementia and Alzheimer’s disease.
- Discuss the nurse’s role in the management, rehabilitation, and health education of patients with dementia and Alzheimer’s disease.
- Demonstrate knowledge of ethical and legal principles guiding dementia care.
- Apply evidence-based nursing interventions in the care of individuals with cognitive decline and their families.
Introduction
- Dementia represents a syndrome of chronic and progressive deterioration in cognitive function, beyond what is expected from normal aging.
- It involves impairment in memory, thinking, orientation, comprehension, calculation, learning capacity, language, and judgment, often accompanied by deterioration in emotional control, social behavior, or motivation.
- Alzheimer’s disease (AD) is the most prevalent form of dementia, accounting for approximately 60–80% of all cases.
- It is characterized by neurodegenerative changes that lead to irreversible loss of neurons and synapses, especially in the cerebral cortex and hippocampus, resulting in progressive decline in cognitive and functional abilities.
- Dementia is a major public health concern with increasing global prevalence due to aging populations.
- According to the World Health Organization (WHO), more than 55 million people worldwide are currently living with dementia, with nearly 10 million new cases annually. It is a leading cause of disability and dependency among older adults.
- From a nursing perspective, dementia poses complex challenges that require multidisciplinary management, including accurate assessment, symptom control, psychological support, family education, and promotion of quality of life.
- Nurses play a vital role in early detection, compassionate care, prevention of complications, and maintaining patient dignity.
Definition And Classification Of Dementia
- Dementia is a chronic, acquired, and progressive syndrome characterized by impairment in multiple higher cortical functions such as memory, intellect, language, and executive functioning, severe enough to interfere with daily life and social functioning, in the absence of altered consciousness.
- Dementia is not a single disease but rather a clinical syndrome resulting from various brain disorders that affect cognition and behavior.
1.1 Types of Dementia
Dementias can be classified based on etiology, pathophysiological mechanisms, or clinical presentation.
A. Based on Etiology:
- Primary Dementias:
- The dementia itself is the main disorder, due to intrinsic neurodegenerative processes.
- Examples:
- Alzheimer’s disease
- Frontotemporal dementia (Pick’s disease)
- Lewy body dementia
- Parkinson’s disease dementia
- Huntington’s disease - Secondary Dementias:
- Cognitive impairment occurs as a consequence of another underlying systemic or cerebral disorder.
- Examples:
- Vascular dementia (post-stroke dementia)
- Dementia due to infections (HIV, neurosyphilis, Creutzfeldt-Jakob disease)
- Dementia due to toxins (chronic alcohol use, heavy metals)
- Dementia due to metabolic or endocrine disorders (hypothyroidism, vitamin B₁₂ deficiency)
Alzheimer’s Dementia
- Etiology:
- Caused by progressive neurodegeneration and neuronal loss.
- Associated with amyloid plaque accumulation and neurofibrillary tangles.
- Genetic factors, including APOE-e4 allele, increase risk.
- Key Features:
- Gradual, insidious onset of cognitive decline.
- Memory impairment is typically the earliest and most prominent symptom.
- Progressive decline in language, executive function, and visuospatial skills.
- Clinical Manifestations:
- Early-stage: mild memory loss, difficulty performing complex tasks, subtle personality changes.
- Middle-stage: increased disorientation, language impairments, behavioral disturbances such as agitation and wandering.
- Late-stage: profound cognitive loss, inability to communicate, total dependence for ADLs.
- Nursing Implications:
- Focus on safety, cognitive stimulation, structured routines, and caregiver education.
- Early intervention improves quality of life and slows functional decline.
Vascular Dementia
- Etiology:
- Results from cerebrovascular disease, including stroke, chronic ischemia, or microvascular injury.
- Cognitive decline is due to reduced cerebral blood flow and neuronal damage.
- Key Features:
- Onset may be abrupt or stepwise after a stroke or transient ischemic attack.
- Cognitive deficits often correlate with location and extent of vascular lesions.
- Memory may be less affected initially compared to Alzheimer’s, but executive dysfunction is prominent.
- Clinical Manifestations:
- Impaired judgment, slowed thinking, and difficulty with planning and decision-making.
- Emotional lability or depression is common.
- Focal neurological deficits (e.g., hemiparesis, visual field deficits) may be present.
- Nursing Implications:
- Focus on stroke prevention, management of cardiovascular risk factors, and safety planning.
- Cognitive and functional support should be individualized based on neurological deficits.
Lewy Body Dementia (LBD)
- Etiology:
- Caused by abnormal deposition of alpha-synuclein proteins (Lewy bodies) in cortical neurons.
- Key Features:
- Fluctuating cognition, pronounced attention deficits, and visual hallucinations.
- Parkinsonian motor symptoms (rigidity, bradykinesia) often appear.
- REM sleep behavior disorder may precede cognitive symptoms.
- Clinical Manifestations:
- Recurrent visual hallucinations and delusions.
- Variations in alertness and attention throughout the day.
- Parkinsonian signs including shuffling gait and tremor.
- Nursing Implications:
- Monitor for falls due to motor impairment.
- Avoid antipsychotics if possible, as clients with LBD are highly sensitive to extrapyramidal side effects.
- Focus on environmental modifications, reassurance, and caregiver support.
Frontotemporal Dementia (FTD)
- Etiology:
- Degeneration of frontal and/or temporal lobes of the brain.
- Genetic mutations in MAPT or progranulin genes may contribute.
- Key Features:
- Early behavioral changes or language deficits rather than memory loss.
- Two primary variants:
- Behavioral variant FTD: marked changes in personality, social conduct, and judgment.
- Primary progressive aphasia: progressive language and communication impairments.
- Clinical Manifestations:
- Socially inappropriate behaviors, impulsivity, and apathy.
- Loss of empathy and insight into own behavior.
- Difficulty naming objects, constructing sentences, or understanding language.
- Nursing Implications:
- Emphasize behavioral management, caregiver education, and environmental modifications.
- Support communication strategies for language deficits.
- Focus on safety due to impulsive or disinhibited behaviors.
Mixed Dementia
- Etiology:
- Combination of two or more types of dementia, most commonly Alzheimer’s disease and vascular dementia.
- Key Features:
- Cognitive decline reflects contributions from multiple pathologies.
- Symptoms may overlap and complicate diagnosis.
- Clinical Manifestations:
- Memory impairment, executive dysfunction, mood disturbances, and possible motor deficits.
- Fluctuating cognitive abilities may be observed.
- Nursing Implications:
- Care must address all contributing pathologies, including cardiovascular risk management.
- Tailored interventions for both cognitive and functional deficits are necessary.
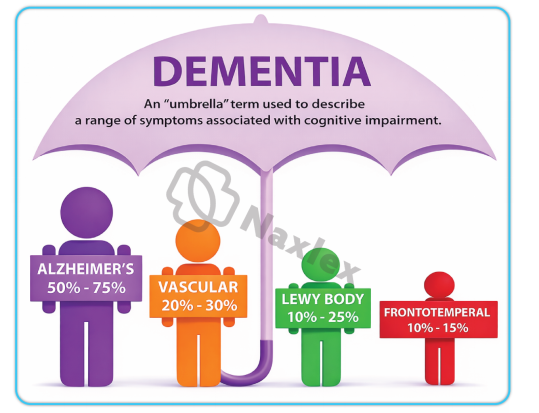
B. Based on Affected Brain Regions:
- Cortical Dementias: Primarily involve the cerebral cortex.
- Manifested by language disturbances, memory loss, and reasoning difficulties.
- Examples: Alzheimer’s disease, frontotemporal dementia. - Subcortical Dementias: Affect basal ganglia, thalamus, and brainstem structures.
- Manifested by psychomotor slowing and mood changes.
- Examples: Parkinson’s disease dementia, Huntington’s disease dementia. - Mixed Dementias: Show features of both cortical and subcortical involvement.
- Example: Vascular dementia with Alzheimer’s pathology.
1.2 Epidemiology of Dementia
- Global Prevalence:
- >55 million people are living with dementia worldwide.
- Alzheimer’s disease accounts for ≈60–80% of all dementia cases.
- Prevalence increases exponentially with age:
- ~5% among people aged ≥65 years
- ~25–50% among those aged ≥85 years - Gender Distribution:
- Women are more commonly affected than men due to longer life expectancy and possible hormonal influences. - Geographic Variation:
- Higher prevalence in developed nations, but a growing burden in low- and middle-income countries due to increased life expectancy. - Mortality:
- Dementia is among the top 10 causes of death globally.
- Average survival after diagnosis ranges from 4–8 years, depending on type and severity. -
Nursing Insights:
- Nurses must recognize that early detection and diagnosis of dementia allow better planning and improved outcomes.
- Community health nurses play a key role in screening older adults for early cognitive impairment using tools such as the Mini-Mental State Examination (MMSE) and Montreal Cognitive Assessment (MoCA).
- Understanding epidemiological patterns helps nurses prioritize at-risk populations and educate families on preventive measures such as controlling vascular risk factors.
1.3 Etiology and Risk Factors of Dementia
A. Etiological Categories:
- Neurodegenerative causes: Alzheimer’s disease, Parkinson’s disease, Huntington’s disease, and frontotemporal lobar degeneration.
- Vascular causes: Multi-infarct dementia, subcortical ischemic vascular dementia.
- Infectious causes: HIV-associated dementia, neurosyphilis, prion diseases.
- Metabolic and toxic causes: Chronic alcoholism, hypoglycemia, hepatic encephalopathy, thyroid disorders, vitamin deficiencies (e.g., B₁₂, thiamine).
- Traumatic causes: Chronic traumatic encephalopathy (CTE) in repetitive head injuries.
- Neoplastic causes: Primary brain tumors or metastases affecting cortical and limbic structures.
B. Major Risk Factors:
- Age: Risk doubles every 5 years after age 65.
- Genetics:
- APOE-ε4 allele increases risk of late-onset Alzheimer’s disease.
- Mutations in APP, PSEN1, PSEN2 genes cause early-onset familial Alzheimer’s disease. - Gender: Female sex is associated with a higher risk.
- Vascular risk factors: Hypertension, diabetes mellitus, hyperlipidemia, smoking, and obesity.
- Lifestyle factors: Physical inactivity, poor diet, social isolation, and low educational attainment.
- Head trauma: Repeated traumatic brain injuries increase dementia risk.
- Chronic stress and depression: Associated with neuroendocrine and inflammatory changes that promote cognitive decline.
Nursing Insights:
- Nurses should educate patients on modifiable risk factors, emphasizing the importance of controlling blood pressure, glucose, and cholesterol levels, and maintaining active mental and social engagement.
- During patient assessment, always take a comprehensive history, including family history, occupational exposure, and lifestyle habits to identify potential contributing factors.
- Nursing interventions should focus on primary prevention, such as community education on healthy brain aging.
1.4 Pathophysiology of Dementia
Dementia results from progressive neuronal loss and synaptic dysfunction in regions of the brain responsible for cognition, memory, and behavior.
Key Pathophysiological Mechanisms:
- Neuronal Degeneration: Loss of neurons and synapses in cortical and subcortical regions impairs signal transmission.
- Neurotransmitter Imbalance:
- ↓ Acetylcholine (ACh) is particularly important in Alzheimer’s disease, leading to memory impairment.
- Dopamine and serotonin imbalances contribute to behavioral and psychotic symptoms. - Cerebrovascular Pathology: In vascular dementia, multiple infarctions or chronic ischemia cause white matter lesions and neuronal death.
- Amyloid Plaques and Neurofibrillary Tangles:
- Extracellular deposition of β-amyloid peptides and intracellular aggregation of hyperphosphorylated tau protein disrupt neuronal communication.
- These are hallmark features of Alzheimer’s disease. - Oxidative Stress and Inflammation:
- Excess reactive oxygen species (ROS) cause mitochondrial dysfunction and neuronal apoptosis.
- Microglial activation releases pro-inflammatory cytokines (IL-1β, TNF-α). - Synaptic Dysfunction:
- Progressive loss of dendritic spines impairs neuronal plasticity and learning.
Table: Major Pathophysiological Changes in Dementia
|
Mechanism |
Resulting Effect |
Example Disorder |
|
β-Amyloid accumulation |
Disrupts synaptic transmission |
Alzheimer’s disease |
|
Tau hyperphosphorylation |
Neuronal cytoskeletal collapse |
Alzheimer’s disease |
|
Ischemic injury |
White matter damage, infarcts |
Vascular dementia |
|
Lewy bodies (α-synuclein) |
Neuronal death in cortex |
Lewy body dementia |
|
Neurotransmitter depletion |
Cognitive and behavioral impairment |
Various dementias |
Nursing Insights:
- Understanding pathophysiology assists nurses in interpreting symptoms (e.g., memory loss due to hippocampal damage).
- It also guides pharmacologic care—cholinesterase inhibitors (e.g., donepezil) are prescribed to enhance acetylcholine levels in Alzheimer’s disease.
- Nurses should closely monitor adverse drug effects such as bradycardia, dizziness, and gastrointestinal disturbances.
- Patient and family education should include explaining the biological basis of symptoms, helping to reduce stigma and enhance cooperation with care.
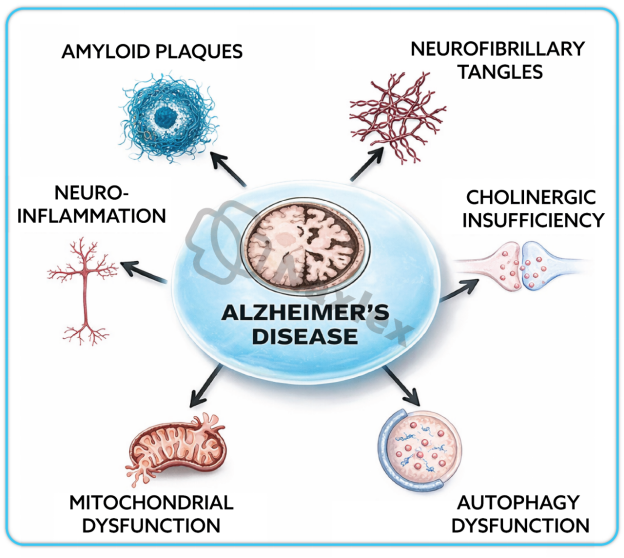
Alzheimer’s Disease
1.1 Definition of Alzheimer’s Disease
- Alzheimer’s disease (AD) is a progressive, irreversible neurodegenerative disorder characterized by cognitive decline, memory impairment, and behavioral disturbances due to widespread neuronal degeneration and synaptic loss, particularly in the cerebral cortex and hippocampus.
- It is the most common cause of dementia, accounting for approximately 60–80% of all dementia cases globally.
- Alzheimer’s disease results from the accumulation of abnormal proteins in the brain, specifically β-amyloid plaques and neurofibrillary tangles composed of hyperphosphorylated tau protein.
- The hallmark features include loss of cholinergic neurons, cerebral atrophy, and ventricular enlargement.
- Nurses should understand that Alzheimer’s disease leads to irreversible loss of cognitive and functional abilities and requires long-term multidisciplinary management.
- Early recognition and accurate diagnosis are crucial for planning appropriate interventions, supporting caregivers, and improving patient outcomes.
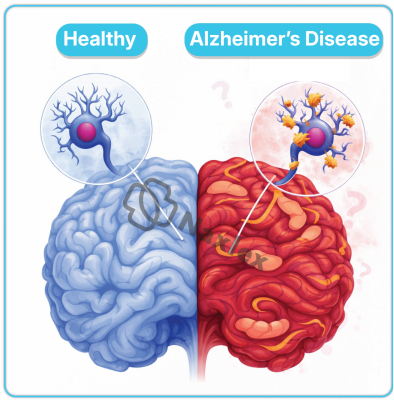
1.2 Epidemiology of Alzheimer’s Disease
- Prevalence:
- Alzheimer’s disease affects over 35 million people globally, with prevalence increasing sharply with age.
- Approximately 1 in 9 individuals aged ≥65 years and nearly one-third of those aged ≥85 years have Alzheimer’s disease. - Gender Distribution:
- Women are at higher risk than men, partly due to longer life expectancy and hormonal changes after menopause. - Geographic and Socioeconomic Factors:
- Higher prevalence in high-income countries due to longer lifespans, but incidence is rising rapidly in low- and middle-income countries. - Mortality:
- Alzheimer’s disease is among the top 5 causes of death in adults over 65 years.
- The average survival period after diagnosis is 4–8 years, though some may live up to 20 years. -
Nursing Insights:
- Nurses in geriatrics and community health should identify high-risk populations for early screening.
- Awareness programs should emphasize healthy aging, lifestyle modifications, and regular cognitive assessments in elderly patients.
1.3 Etiology and Risk Factors of Alzheimer’s Disease
Alzheimer’s disease results from a complex interaction of genetic, environmental, and lifestyle factors leading to neuronal degeneration.
A. Genetic Factors:
- Familial (Early-Onset) Alzheimer’s Disease:
- Occurs before 65 years, accounting for <5% of cases.
- Associated with mutations in genes encoding:
- Amyloid precursor protein (APP)
- Presenilin 1 (PSEN1)
- Presenilin 2 (PSEN2) - Sporadic (Late-Onset) Alzheimer’s Disease:
- Accounts for >95% of cases.
- The APOE-ε4 allele is the strongest genetic risk factor.
B. Non-Genetic Risk Factors:
- Age: Risk doubles every 5 years after age 65.
- Gender: Women more frequently affected.
- Vascular and Metabolic Conditions: Hypertension, diabetes, obesity, and dyslipidemia increase susceptibility.
- Head Trauma: Repeated concussions or severe brain injury accelerate pathology.
- Lifestyle Factors: Sedentary lifestyle, poor diet, smoking, and social isolation.
- Neuroinflammation: Chronic activation of microglia leads to progressive neuronal damage.
- Low Education Level: Reduced cognitive reserve predisposes to earlier symptom onset.
Nursing Insights:
- Nurses should perform comprehensive health assessments to identify modifiable risk factors.
- Patient education should focus on vascular health, dietary habits (Mediterranean diet), and physical and mental activity as preventive strategies.
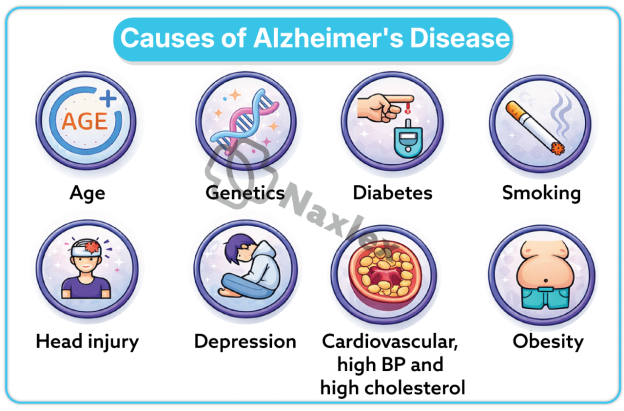
1.4 Pathophysiology of Alzheimer’s Disease
The pathogenesis of Alzheimer’s disease involves accumulation of toxic proteins, neuronal death, and neurotransmitter depletion.
A. Amyloid Cascade Hypothesis:
- The β-amyloid (Aβ) peptide, derived from abnormal cleavage of amyloid precursor protein (APP), accumulates extracellularly forming amyloid plaques.
- These plaques disrupt synaptic communication and trigger neuroinflammation and oxidative stress.
B. Tau Protein Abnormality:
- Hyperphosphorylated tau protein aggregates intracellularly into neurofibrillary tangles (NFTs).
- This disrupts the neuronal cytoskeleton, leading to impaired axonal transport and neuronal death.
C. Neurotransmitter Deficiency:
- Marked reduction in acetylcholine (ACh) due to degeneration of cholinergic neurons in the basal forebrain.
- This correlates with severity of cognitive impairment.
D. Brain Structural Changes:
- Cortical atrophy, ventricular enlargement, and hippocampal degeneration are prominent features.
- Loss of synaptic density leads to decline in neural plasticity.
E. Neuroinflammation and Oxidative Stress:
Activated microglia release cytokines (IL-1β, TNF-α) and reactive oxygen species (ROS), perpetuating neuronal injury.
|
Pathological Feature |
Description |
Functional Consequence |
|
β-Amyloid plaques |
Extracellular aggregates |
Synaptic dysfunction |
|
Neurofibrillary tangles |
Intracellular tau accumulations |
Neuronal death |
|
Loss of cholinergic neurons |
Decreased acetylcholine |
Memory loss |
|
Cortical atrophy |
Shrinking of cerebral tissue |
Cognitive decline |
Nursing Insights:
- Understanding these mechanisms helps nurses correlate clinical symptoms with brain pathology.
- Explaining these changes to families can improve understanding and empathy for patient behavior.
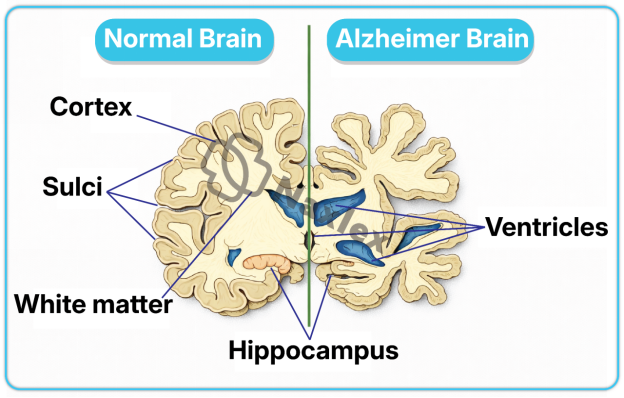
1.5 Stages of Alzheimer’s Disease
Alzheimer’s disease progresses through three major clinical stages:
1. Mild (Early Stage):
- Memory lapses, especially short-term memory.
- Difficulty with words, names, and recent events.
- Mild disorientation in familiar places.
- Preserved independence in basic activities of daily living (ADLs).
2. Moderate (Middle Stage):
- Increasing confusion and forgetfulness.
- Impairment in complex tasks (finances, meal preparation).
- Behavioral changes: agitation, wandering, aggression, hallucinations.
- Assistance required for most ADLs.
3. Severe (Late Stage):
- Loss of ability to communicate.
- Incontinence, inability to ambulate, and profound dependence.
- Dysphagia, muscle rigidity, and cachexia.
- Death often due to complications such as infections or aspiration pneumonia.
Nursing Insights:
- Nurses must tailor interventions to disease stage—safety and orientation in mild stages; behavioral management and full assistance in late stages.
- Family education on progressive care needs is essential.
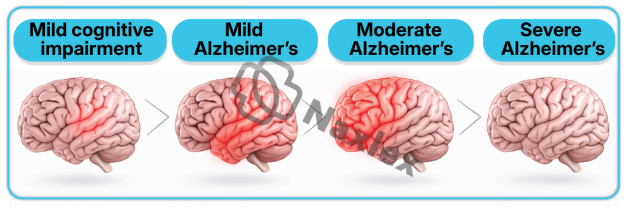
1.6 Clinical Manifestations of Alzheimer’s Disease
A. Cognitive Symptoms:
- Memory loss (initially short-term, later long-term).
- Disorientation to time, place, and person.
- Impaired judgment and problem-solving.
- Aphasia (language difficulties).
- Apraxia (difficulty performing motor tasks).
- Agnosia (inability to recognize objects or people).
B. Behavioral and Psychological Symptoms:
- Agitation, irritability, depression, and anxiety.
- Paranoia, delusions, and hallucinations.
- Wandering, sundowning (worsening confusion at dusk).
C. Physical and Functional Changes:
- Gait disturbance, rigidity, and loss of coordination.
- Difficulty swallowing, leading to aspiration risk.
- Bladder and bowel incontinence.
Nursing Insights:
- Nurses should monitor for behavioral triggers (e.g., pain, overstimulation, fatigue).
- Gentle reorientation, calm tone, and consistent routine help minimize agitation.
1.7 Diagnostic Evaluation of Alzheimer’s Disease
A. Clinical Assessment:
- Detailed history from patient and caregivers.
- Cognitive screening:
- Mini-Mental State Examination (MMSE)
- Montreal Cognitive Assessment (MoCA)
- Clock drawing test - Functional status evaluation using Activities of Daily Living (ADL) and Instrumental ADL scales.
B. Laboratory Tests:
- Complete blood count (CBC), electrolytes, thyroid function, vitamin B₁₂ levels to rule out reversible causes.
C. Neuroimaging:
- MRI/CT Scan: Cortical atrophy, ventricular enlargement, hippocampal shrinkage.
- PET Scan: Decreased glucose metabolism in temporoparietal areas.
D. Biomarkers (advanced settings):
- CSF analysis for ↓Aβ42 and ↑tau proteins.
- Amyloid PET imaging to detect β-amyloid deposition.
Nursing Insights:
- Nurses play a vital role in preparing patients for neuroimaging, ensuring cooperation and comfort.
- During assessment, nurses should evaluate for delirium, depression, or medication effects which may mimic dementia.
1.8 Medical Management of Alzheimer’s Disease
A. Pharmacologic Management:
- Cholinesterase Inhibitors: Donepezil, Rivastigmine, Galantamine
- Increase acetylcholine levels, improving cognition and daily function. - NMDA Receptor Antagonist: Memantine
- Reduces excitotoxic neuronal damage. - Adjunctive Medications:
- Antidepressants (SSRIs) for mood disturbances.
- Antipsychotics (Risperidone, Quetiapine) for agitation or psychosis.
- Benzodiazepines used cautiously for anxiety. -
B. Non-Pharmacologic Management:
- Cognitive stimulation therapy and memory training.
- Reality orientation and reminiscence therapy.
- Physical activity, balanced diet, and structured routines.
- Environmental modifications to prevent wandering and injury.
-
Nursing Insights:
- Nurses should monitor for adverse drug reactions (bradycardia, dizziness, GI upset).
- Encourage caregiver support programs to prevent burnout.
- Regularly evaluate medication efficacy and side effects.
1.9 Nursing Management of Alzheimer’s Disease
1.9.1 Nursing Assessment
- Assess level of consciousness, orientation, and cognitive status.
- Evaluate memory, judgment, speech, and emotional status.
- Assess ability to perform ADLs.
- Observe for behavioral and psychotic symptoms.
- Review medications, nutrition, sleep patterns, and safety risks.
1.9.2 Nursing Diagnosis
- Impaired memory related to neuronal degeneration.
- Risk for injury related to confusion and wandering.
- Self-care deficit related to cognitive decline.
- Caregiver role strain related to patient dependency.
1.9.3 Nursing Planning and Implementation
- Promote Safety:
- Remove hazardous objects, use identification bracelets.
- Maintain a consistent, familiar environment. - Enhance Orientation:
- Display clocks, calendars, and labels on rooms.
- Use simple, clear communication. - Promote Independence:
- Encourage participation in self-care within ability limits.
- Provide step-by-step instructions for tasks. - Support Family and Caregivers:
- Offer education on disease progression and coping strategies.
- Facilitate support group referrals. - Manage Behavioral Symptoms:
- Use distraction, reassurance, and avoid confrontation.
- Provide activities that reduce restlessness.
1.9.4 Nursing Evaluation
- Patient demonstrates improved orientation and reduced agitation.
- ADLs maintained to maximum ability.
- Safety maintained with no falls or injuries.
- Caregiver demonstrates understanding and coping skills.
2.0 Complications of Alzheimer’s Disease
- Medical Complications:
- Malnutrition and dehydration
→ Due to dysphagia and neglect of self-care.
- Aspiration pneumonia
→ From impaired swallowing reflex.
- Pressure ulcers
→ Due to immobility and incontinence.
- Falls and fractures
→ From disorientation and poor coordination. - Psychological Complications:
- Depression, psychosis, social withdrawal. - Caregiver Complications:
- Fatigue, depression, and emotional exhaustion. -
Nursing Insights:
- Nurses must anticipate complications and initiate preventive measures, such as regular repositioning, nutritional monitoring, and fall prevention strategies.
-
Continuous caregiver assessment and support are essential to sustain effective long-term care.
Differences Between Dementia And Alzheimer’s Disease
- ementia and Alzheimer’s disease are closely related but not synonymous.
- Dementia is a broad clinical syndrome characterized by impairment in cognitive function severe enough to interfere with daily activities, while Alzheimer’s disease (AD) is a specific neurodegenerative disorder and the most common cause of dementia.
- Understanding their differences is crucial for accurate diagnosis, appropriate management, and nursing care planning.
1.1 Comparative Table: Dementia vs. Alzheimer’s Disease
|
Feature |
Dementia |
Alzheimer’s Disease |
|
Definition |
A clinical syndrome involving decline in cognitive function affecting memory, thinking, and social abilities due to various brain disorders. |
A specific neurodegenerative disease that causes 60–80% of all dementia cases, characterized by β-amyloid plaques and neurofibrillary tangles. |
|
Nature |
A symptom complex or umbrella term. |
A distinct pathological condition. |
|
Causes |
Multiple causes: Alzheimer’s, vascular, Lewy body, Parkinson’s, frontotemporal, infections, toxins, etc. |
Caused by accumulation of β-amyloid and tau proteins leading to neuronal death. |
|
Onset |
May be sudden (vascular) or gradual (degenerative). |
Gradual and insidious onset. |
|
Progression |
Depends on underlying cause; may be stable or progressive. |
Always progressive and irreversible. |
|
Memory Impairment |
Variable depending on cause; not always early. |
Early and prominent symptom. |
|
Reversibility |
Some forms are reversible (e.g., metabolic, drug-induced). |
Irreversible. |
|
Diagnosis |
Based on identifying the underlying cause. |
Confirmed by clinical evaluation, neuroimaging, and biomarkers. |
|
Treatment |
Depends on etiology; may include treating underlying condition. |
Symptomatic management only; no cure available. |
|
Prognosis |
Varies with cause. |
Chronic progressive deterioration leading to death. |
Nursing Insights:
- Nurses must recognize that all Alzheimer’s disease causes dementia, but not all dementia is Alzheimer’s disease.
- Accurate differentiation helps direct appropriate care strategies and medication use.
- During assessment, always rule out reversible causes of dementia before diagnosing Alzheimer’s disease.
Nursing Management Of Dementia
Nursing management of dementia focuses on maintaining patient safety, preserving functional abilities, supporting cognitive function, and providing emotional and psychosocial support to both patients and caregivers.
1.1 Nursing Assessment of Dementia
The nurse performs a comprehensive and holistic assessment to determine the degree of cognitive impairment and the impact on daily living.
- Cognitive Function:
- Assess orientation to time, place, person, and situation.
- Evaluate memory (short-term, long-term), attention, and problem-solving abilities. - Behavioral and Psychological Symptoms:
- Observe for agitation, aggression, delusions, hallucinations, wandering, or sleep disturbances. - Functional Status:
- Determine ability to perform Activities of Daily Living (ADLs) and Instrumental ADLs. - Physical Examination:
- Assess for neurological deficits, nutrition, hydration, mobility, and continence status. - Environmental Assessment:
- Evaluate home safety, fall hazards, lighting, and noise levels. - Family and Social Support:
- Assess caregiver burden, coping mechanisms, and available support systems.
Nursing Insights:
- Nurses should recognize behavioral changes as a form of communication rather than intentional defiance.
- Early detection of functional decline can guide interventions to maintain independence longer.
1.2 Nursing Diagnoses in Dementia
Common nursing diagnoses include:
- Impaired memory related to progressive neuronal degeneration.
- Chronic confusion related to disorientation and cognitive decline.
- Risk for injury related to impaired judgment and wandering.
- Impaired verbal communication related to aphasia.
- Self-care deficit related to impaired cognitive function.
- Caregiver role strain related to continuous supervision demands.
1.3 Nursing Interventions and Rationales
A. Promote Safety:
- Provide a secure and hazard-free environment.
- Install door alarms, remove clutter, and use nightlights.
- Ensure supervision during ambulation and meals to prevent falls and choking.
B. Enhance Cognitive Function:
- Provide structured routines to reduce confusion.
- Use calendars, clocks, and labeled items for orientation.
- Encourage memory exercises and familiar activities.
C. Manage Behavioral Symptoms:
- Maintain calm, reassuring communication; avoid arguing.
- Use distraction and redirection when agitation occurs.
- Provide rest periods to prevent fatigue and irritability.
D. Support Daily Functioning:
- Encourage self-care with assistance as needed.
- Simplify tasks into small, achievable steps.
- Provide adaptive devices to foster independence.
E. Promote Nutrition and Hydration:
- Offer finger foods if utensils are difficult to use.
- Monitor intake to prevent malnutrition and dehydration.
F. Provide Emotional and Family Support:
- Educate caregivers about disease progression and coping strategies.
- Encourage participation in support groups.
- Provide information on respite care services.
Nursing Insights:
- Nurses should adopt a patient-centered approach, focusing on dignity, respect, and comfort.
- Avoid overstimulation—use calm environments and familiar caregivers.
- Recognize caregiver fatigue early and provide resources for stress management.
1.4 Nursing Evaluation of Dementia Care
- Patient demonstrates improved orientation and reduced episodes of agitation.
- Safety maintained with no falls or injuries.
- Nutritional and hydration status stable.
- Family verbalizes understanding of disease and demonstrates coping ability.
- Patient maintains optimal level of independence in ADLs.
Pharmacological Management Of Dementia And Alzheimer’s Disease
- Pharmacologic treatment aims to slow disease progression, stabilize symptoms, and improve quality of life.
- Medications are primarily symptomatic, addressing neurotransmitter imbalances and behavioral disturbances.
1.1 Cholinesterase Inhibitors
- Mechanism of Action:
- Inhibit acetylcholinesterase enzyme, increasing acetylcholine levels in synaptic clefts.
- Enhance communication between neurons, improving memory and cognition. - Common Agents:
- Donepezil (Aricept): Used in mild to severe AD; once daily dosing.
→ Adverse effects: nausea, bradycardia, diarrhea.
- Rivastigmine (Exelon): Available as oral or transdermal patch; reduces GI effects.
- Galantamine (Razadyne): Also enhances nicotinic receptor activity. - Nursing Responsibilities:
- Monitor heart rate for bradycardia.
- Administer with food to minimize GI upset.
- Assess cognitive function periodically for drug effectiveness.
Nursing Insights:
- Early initiation improves outcomes; however, these drugs do not halt disease progression.
- Nurses should educate families on adherence and expected benefits (symptom stabilization, not cure).
1.2 NMDA Receptor Antagonists
- Agent: Memantine (Namenda)
- Mechanism:
- Blocks excessive glutamate activity at NMDA receptors, preventing excitotoxicity and neuronal death. - Indication: Moderate to severe Alzheimer’s disease, alone or combined with cholinesterase inhibitors.
- Side Effects: Dizziness, headache, constipation, confusion.
- Nursing Responsibilities:
- Monitor for cognitive changes and side effects.
- Ensure adequate hydration and slow dosage titration.
Nursing Insights:
- Combination therapy (Memantine + Donepezil) often provides greater functional stability in moderate to severe disease.
1.3 Adjunctive Medications (Antidepressants, Antipsychotics, etc.)
- Antidepressants (SSRIs):
- For depressive symptoms; e.g., sertraline, citalopram. - Antipsychotics:
- Used cautiously for severe agitation, hallucinations, or aggression (e.g., risperidone, quetiapine).
- Monitor for extrapyramidal symptoms and sedation. - Anxiolytics:
- Short-term use for anxiety or restlessness (avoid long-term benzodiazepines). - Sleep Aids:
- Non-pharmacologic sleep hygiene preferred; melatonin may be used.
Nursing Insights:
- Nurses should prioritize non-drug behavioral interventions before pharmacologic options.
- Always monitor for adverse reactions, particularly in elderly patients with comorbidities.
Psychosocial And Behavioral Management
Psychosocial interventions aim to preserve cognitive abilities, reduce behavioral disturbances, and enhance emotional well-being.
1.1 Cognitive Stimulation Therapy
- Involves structured group activities designed to improve thinking, concentration, and memory.
- Activities may include word games, music, puzzles, and discussion of current events.
- Evidence shows it improves quality of life and cognitive function in mild to moderate dementia.
Nursing Insights:
- Nurses can facilitate sessions in day-care or residential settings.
- Participation should be voluntary and enjoyable to promote engagement.
1.2 Reality Orientation
- A therapeutic approach using verbal and visual cues to reinforce person, place, and time orientation.
- Tools include clocks, calendars, labeled objects, and regular reminders.
- Enhances environmental familiarity and reduces confusion.
Nursing Insights:
- Should be applied gently; avoid correcting the patient harshly.
- Consistent caregivers help reinforce stability and trust.
1.3 Reminiscence Therapy
- Uses past experiences, photographs, and music to stimulate long-term memory.
- Strengthens identity, reduces anxiety, and improves social interaction.
Nursing Insights:
- Particularly beneficial in later stages when short-term memory is impaired.
- Nurses can use old songs, family albums, or cultural stories to elicit positive emotions.
1.4 Family and Caregiver Support
- Provide education on disease process, prognosis, and care strategies.
- Encourage respite care and support groups to prevent caregiver burnout.
- Offer guidance on managing financial, ethical, and legal aspects of long-term care.
Nursing Insights:
- Nurses serve as primary educators, advocates, and emotional support for caregivers.
- Recognizing caregiver stress early prevents neglect and improves patient care outcomes.
Complications And Prognosis
- Dementia and Alzheimer’s disease are chronic, progressive neurodegenerative disorders that lead to a multitude of complications affecting multiple systems.
- As the disease advances, patients experience deterioration in cognitive, functional, behavioral, and physiological domains.
- Understanding the potential complications and overall prognosis enables nurses to plan anticipatory care and provide holistic, evidence-based management.
1.1 Short-Term and Long-Term Complications
A. Short-Term Complications
Short-term complications commonly arise during the early to moderate stages of the disease due to impaired cognition and behavioral instability.
- Falls and Injuries:
- Disorientation, poor balance, and wandering behavior increase fall risk.
- Visual-perceptual deficits cause difficulty navigating environments.
- Fractures, head injuries, and soft tissue damage are common outcomes. - Nutritional Deficiencies:
- Forgetfulness and inability to recognize hunger or thirst lead to poor intake.
- Dysphagia and motor dysfunction may cause aspiration pneumonia. - Infections:
- Poor hygiene, urinary retention, and immobility predispose to urinary tract infections (UTIs) and respiratory infections. - Behavioral and Psychological Disturbances (BPSD):
- Includes agitation, aggression, anxiety, hallucinations, and depression.
- May lead to social isolation and caregiver burnout. - Sleep Disturbances:
- Fragmented sleep and nocturnal wandering increase fatigue and confusion. - Medication Side Effects:
- Polypharmacy heightens the risk of adverse drug reactions and delirium.
B. Long-Term Complications
These occur in the advanced stages when the patient becomes fully dependent and physiological systems decline.
- Severe Malnutrition and Dehydration:
- Progressive dysphagia and anorexia reduce intake, leading to cachexia. - Aspiration Pneumonia:
- Loss of gag reflex and poor swallowing coordination cause aspiration. - Pressure Ulcers:
- Immobility, incontinence, and poor nutrition lead to skin breakdown. - Sepsis:
- Secondary to pressure ulcers, pneumonia, or urinary infections. - Contractures and Muscle Wasting:
- Prolonged immobility leads to atrophy and deformities. - Functional Incontinence:
- Due to lack of awareness or inability to locate restrooms. - Social Isolation and Institutionalization:
- Family caregivers may be unable to manage advanced cases, resulting in long-term care placement.
Nursing Insights:
- Nurses must vigilantly monitor for early signs of infection, aspiration, and nutritional decline, which are major causes of morbidity.
- Preventive measures such as frequent repositioning, assisted feeding, fall precautions, and infection control are essential in advanced care.
- Emotional support to families during the terminal stage is crucial in providing compassionate, dignified end-of-life care.
1.2 Prognosis of Dementia and Alzheimer’s Disease
- Disease Course:
- Alzheimer’s disease is progressive and irreversible, typically spanning 8–12 years after diagnosis.
- The course may vary depending on comorbidities, genetics, and quality of care. - Mortality:
- Leading causes of death include pneumonia, sepsis, and malnutrition.
- Advanced dementia is a terminal condition with gradual decline in all body functions. - Factors Influencing Prognosis:
- Age: Older patients deteriorate faster.
- Sex: Women show higher prevalence and slightly slower decline.
- Comorbidities: Diabetes, hypertension, and cardiovascular disease accelerate progression.
- Early Diagnosis and Intervention: Early initiation of cholinesterase inhibitors may prolong function and delay institutionalization. - Functional Decline:
- Cognitive and physical abilities deteriorate progressively until complete dependency is reached.
Nursing Insights:
- Nurses should counsel families that dementia is a life-limiting illness requiring palliative and supportive care approaches.
The focus of care should shift gradually from curative to comfort, dignity, and quality of life.
Ethical And Legal Considerations In Dementia Care
- Ethical and legal challenges frequently arise in dementia care due to cognitive impairment, loss of decision-making capacity, and dependence on others for daily needs.
- Nurses play a key role in upholding ethical principles—autonomy, beneficence, nonmaleficence, and justice—while ensuring the patient’s rights are respected.
1.1 Informed Consent
- Definition:
- Informed consent refers to a patient’s voluntary agreement to treatment after receiving adequate information about the procedure, benefits, risks, and alternatives. - Challenges in Dementia:
- As cognitive function declines, the patient’s capacity to understand and consent diminishes.
- Consent may need to be obtained from a legally authorized representative or next of kin. - Nurse’s Role:
- Ensure that the patient is informed in a manner consistent with their cognitive level.
- Verify comprehension by asking the patient to restate the information.
- Document all discussions related to consent.
- Advocate for patient rights if coercion or misunderstanding is suspected.
Nursing Insights:
- Nurses should always assess for fluctuating levels of capacity, as mild dementia patients may still be capable of making simple decisions.
- Involve family members, but prioritize the patient’s preferences wherever possible.
1.2 Patient Autonomy and Capacity Assessment
- Patient Autonomy:
- Refers to the right of individuals to make decisions regarding their care and treatment.
- Dementia progressively impairs autonomy due to cognitive decline. - Capacity Assessment:
- Must be task-specific and time-specific, evaluated for each decision.
- A competent patient should be able to:
→ Understand relevant information.
→ Appreciate the consequences of decisions.
→ Communicate a consistent choice.
→ Reason about treatment options. - Legal Provisions:
- When capacity is lost, legal mechanisms such as power of attorney, guardianship, or advance directives are implemented.
Nurse’s Role:
- Collaborate with physicians and legal representatives in capacity evaluation.
- Support patient participation in decisions to the fullest extent possible.
- Respect cultural and individual values regarding autonomy and dependence.
Nursing Insights:
- Nurses should be familiar with local laws and institutional policies governing capacity and guardianship.
- Advocacy for the patient’s best interests is paramount, especially in cases of neglect or exploitation.
1.3 End-of-Life Decision-Making
End-of-life care in dementia involves making decisions about resuscitation, artificial nutrition, hydration, and life-prolonging interventions as cognitive decline progresses.
- Advance Directives:
- Legal documents expressing the patient’s wishes regarding treatment when they lose decision-making capacity.
- May include Do Not Resuscitate (DNR) orders and preferences for comfort-focused care. - Palliative and Hospice Care:
- Focus on symptom control, comfort, and dignity rather than curative treatment.
- Prioritizes management of pain, dyspnea, and agitation. - Ethical Dilemmas:
- Conflicts may arise between family desires for aggressive treatment and professional recommendations for comfort care.
- Nurses must balance beneficence (doing good) and nonmaleficence (avoiding harm).
Nurse’s Role:
- Facilitate discussions between healthcare providers and families regarding goals of care.
- Ensure that the patient’s prior wishes, cultural beliefs, and dignity are respected.
- Provide emotional support to families during bereavement.
Nursing Insights:
- Nurses are critical in ensuring that end-of-life care aligns with ethical principles and the patient’s known or presumed wishes.
- Compassionate communication and empathy are key to helping families accept the natural course of dementia.
Prevention And Health Education
- Dementia and Alzheimer’s disease are major global public health issues with no definitive cure, making prevention and health education critical in reducing incidence, delaying onset, and mitigating complications.
- Nurses have a central role in educating individuals, families, and communities about risk reduction strategies, early detection, and maintenance of brain health.
1.1 Primary Prevention
Primary prevention targets individuals before disease onset to minimize risk factors that predispose to dementia and Alzheimer’s disease.
A. Lifestyle Modifications:
- Cognitive Stimulation:
- Encourage mental exercises such as reading, puzzles, crosswords, and learning new languages to enhance neuroplasticity. - Physical Activity:
- Regular aerobic and resistance exercises improve cerebral circulation and reduce vascular dementia risk.
- Recommendations: ≥150 minutes of moderate exercise weekly. - Balanced Diet:
- Adoption of the Mediterranean diet rich in fruits, vegetables, whole grains, nuts, fish, and olive oil.
- Limit saturated fats, refined sugars, and processed foods. - Social Interaction:
- Promote regular engagement in social activities and community participation to prevent isolation and depression. - Cardiovascular Health:
- Manage hypertension, diabetes, obesity, and dyslipidemia to reduce cerebrovascular injury. - Avoidance of Neurotoxins:
- Discourage smoking, excessive alcohol consumption, and exposure to environmental toxins (e.g., heavy metals).
B. Public Health Measures:
- Conduct community education programs on maintaining brain health.
- Encourage periodic screening for cognitive decline in older adults.
- Support vaccination programs against infections that may precipitate delirium (e.g., influenza, pneumococcal vaccines).
Nursing Insights:
- Nurses should integrate brain health education into community outreach and primary care consultations.
- Early identification of at-risk individuals enables preventive interventions before irreversible neuronal damage occurs.
1.2 Secondary Prevention
Secondary prevention aims to detect early disease and slow its progression through timely diagnosis and intervention.
A. Early Detection:
- Utilize cognitive screening tools such as MMSE, MoCA, and Clock Drawing Test in routine assessments for elderly clients.
- Recognize early warning signs such as forgetfulness, apathy, irritability, and decreased problem-solving ability.
B. Prompt Intervention:
- Initiate cholinesterase inhibitors (Donepezil, Rivastigmine, Galantamine) early in mild cases.
- Start cognitive stimulation therapy and structured routines to maintain independence.
C. Management of Comorbidities:
- Optimize control of hypertension, diabetes, dyslipidemia, and heart disease.
- Encourage smoking cessation and moderate alcohol use.
D. Family Education:
- Provide teaching on the significance of early consultation and regular follow-up.
- Direct families to support services, day-care programs, and local memory clinics.
Nursing Insights:
- Nurses are instrumental in detecting subtle cognitive changes that may go unnoticed in clinical settings.
- Early intervention can delay institutionalization and preserve patient autonomy longer.
1.3 Tertiary Prevention
Tertiary prevention seeks to reduce disability, prevent complications, and improve quality of life for patients with established dementia or Alzheimer’s disease.
A. Supportive and Rehabilitative Care:
- Maintain patient mobility through physiotherapy and regular ambulation.
- Provide occupational therapy to promote independence in daily activities.
B. Complication Prevention:
- Prevent falls by using bed alarms, clear pathways, and proper footwear.
- Prevent aspiration by ensuring correct positioning during meals and providing texture-modified diets.
- Implement turning schedules to avoid pressure injuries.
C. Caregiver and Family Support:
- Offer psychological support, respite care, and education on symptom management.
- Teach stress reduction and coping strategies to prevent burnout.
D. Long-Term Planning:
- Assist families in planning for advanced disease stages, including palliative care options.
- Collaborate with social services for long-term care placement when necessary.
Nursing Insights:
- The focus in tertiary prevention should shift toward comfort, dignity, and functional maintenance.
- Nurses must regularly assess for caregiver fatigue and connect families to community-based resources.
Role Of The Nurse In Community And Institutional Care
- Nurses function as educators, caregivers, advocates, and coordinators across all settings of dementia care.
- Their role spans prevention, clinical management, rehabilitation, and support for patients and caregivers both in the community and institutional environments.
1.1 Health Promotion in the Community
A. Community Health Education:
- Conduct awareness campaigns about dementia risk factors, symptoms, and prevention strategies.
- Dispel myths and stigma surrounding mental health and aging.
B. Screening and Early Detection:
- Participate in community outreach programs offering cognitive assessments for older adults.
- Facilitate referrals to specialized memory clinics.
C. Support Group Initiatives:
- Establish and facilitate caregiver support groups to share experiences and coping techniques.
- Promote social interaction for both patients and caregivers.
D. Advocacy:
- Advocate for accessible mental health services, dementia-friendly environments, and policies that protect elderly rights.
E. Home-Based Care and Follow-Up:
- Conduct home visits to assess environmental safety, nutrition, and caregiver competency.
- Provide education on behavioral management and medication adherence.
Nursing Insights:
- Community nurses are essential in maintaining continuity of care between hospital and home.
- Empathy and effective communication foster trust, adherence, and improved outcomes.
1.2 Institutional Support and Multidisciplinary Team Role
A. Institutional Care Settings:
- Ensure a safe, structured, and supportive environment tailored to dementia patients.
- Incorporate therapeutic activities such as music therapy, reminiscence, and reality orientation.
B. Multidisciplinary Collaboration:
- Physician: Diagnosis, medical treatment, and disease monitoring.
- Psychiatrist/Psychologist: Manage behavioral and emotional issues.
- Physiotherapist/Occupational Therapist: Support functional mobility and independence.
- Dietitian: Develop nutrition plans preventing malnutrition and dehydration.
- Social Worker: Provide counseling, coordinate financial and social resources.
- Nurse: Monitor daily health status, administer medications, educate families, and coordinate team communication.
C. Role of the Nurse:
- Implement individualized care plans and ensure holistic attention to physical, emotional, and spiritual needs.
- Prevent complications through vigilant observation and early intervention.
- Serve as the primary advocate for patient dignity, respect, and comfort.
Nursing Insights:
- Nurses bridge communication gaps between the patient, family, and multidisciplinary team, ensuring seamless and compassionate care.
- Institutional nurses must regularly reassess care goals and adapt interventions as the disease progresses.
Summary
- Dementia is a progressive, irreversible cognitive decline impairing memory, reasoning, and daily functioning.
- Alzheimer’s disease is the leading cause of dementia, characterized by β-amyloid plaque accumulation and neurofibrillary tangles leading to neuronal loss.
- Pathophysiology involves acetylcholine deficiency, synaptic degeneration, and cortical atrophy.
- Clinical presentation includes progressive memory loss, disorientation, behavioral changes, and eventual dependency.
- Diagnosis utilizes cognitive tests, neuroimaging, and laboratory assessments to exclude reversible causes.
- Management combines pharmacologic therapy (cholinesterase inhibitors, NMDA antagonists) with psychosocial and nursing interventions.
- Complications such as aspiration, infections, pressure ulcers, and caregiver burnout require proactive nursing care.
- Ethical and legal aspects involve respecting autonomy, ensuring informed consent, and guiding end-of-life decisions.
- Preventive measures—primary, secondary, and tertiary—are essential to reduce disease burden.
- Nurses serve as advocates, educators, and caregivers in both community and institutional contexts, ensuring holistic, compassionate, and patient-centered dementia care.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Dementia And Alzheimer’s Disease
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


