Please set your exam date
ATTENTION-DEFICIT/HYPERACTIVITY DISORDER (ADHD)
Study Questions
Practice Exercise 1
A nurse is educating a group of parents about the causes of attention-deficit/hyperactivity disorder (ADHD). Which of the following factors should the nurse include as being attributed to the etiology of the disorder? Select all that apply
Explanation
Attention-deficit/hyperactivity disorder is a neurodevelopmental disorder characterized by persistent inattention, hyperactivity, and impulsivity. It involves geneticpredisposition, neurochemicaldysregulation, abnormal dopaminergicsignaling, and altered prefrontal cortexfunction. Symptoms include distractibility, poor executive function, and impaired working memory. Neuroimaging shows reduced cortical thickness and hypoactivity in fronto-striatal circuits. Environmental factors may exacerbate severity but are not primary etiologies.
Rationale for correct answers:
1.Genetic factors are strongly implicated, with heritability estimates ≥70%.Twin studies confirm familial aggregation. Specific polymorphisms in dopamine transporter and receptor genes increase vulnerability. The question stem highlights causative factors, making genetics a scientifically valid etiology. Geneticand heritabilityare central.
3.Neurochemical factors are critical, particularly dopamine and norepinephrine imbalance in fronto-striatal pathways. Reduced catecholamine activity impairs attention regulation. Pharmacologic evidence supports this, as stimulants normalize neurotransmission. The stem’s focus on etiology validates neurochemical dysregulation. Dopamineand norepinephrineare emphasized.
Rationale for incorrect answers:
2.Psychodynamic factors are not causative. They may explain behavioral manifestations but lack neurobiological evidence. ADHD is not rooted in unconscious conflict or early psychosexual stages. Reliance on psychodynamic theory misattributes etiology. Psychodynamicsand conflictare irrelevant.
4.Family dynamic factors influence symptom expression and management but are not etiologic. Dysfunctional parenting may worsen behavior but does not cause ADHD. Neurodevelopmental abnormalities precede environmental influences. Familyand environmentare contributory, not causal.
5.Dietary factors have limited evidence. Additives or sugar may exacerbate symptoms but are not primary causes. Controlled trials show inconsistent associations. Etiology remains neurobiological, not nutritional. Dietaryand additiveslack scientific causation.
Test-taking strategy
- Focus on etiologyrather than contributing or exacerbating factors.
- Rule out theories lacking neurobiological evidence such as psychodynamicexplanations.
- Distinguish between causativeversus influencingfactors.
- Use knowledge of geneticsand neurochemistryas established scientific bases.
- Eliminate options that describe environmental modifiers (family dynamics, diet) since they do not explain pathogenesis.
- Apply evidence-based reasoning: ADHD is a neurodevelopmental disorderwith strong heritability and neurotransmitter dysregulation.
- When faced with “select all that apply,” ensure each choice aligns with established pathophysiology.
- Avoid distractors that describe management or symptom exacerbation rather than causation.
- Remember that stimulant pharmacologysupports neurochemical etiology, reinforcing neurotransmitter imbalance as a correct answer.
- Genetic linkage studies provide definitive evidence, making genetics a reliable choice.
Take home points
- ADHD is a neurodevelopmental disorder with strong genetic heritability.
- Dopamine and norepinephrine dysregulation underlie attentional deficits and impulsivity.
- Family dynamics and diet may influence severity but are not causative.
- Psychodynamic theories lack scientific validity in explaining ADHD etiology.
A nurse is explaining the biological basis of attention-deficit/hyperactivity disorder (ADHD) to a group of nursing students. Which factor should the nurse identify as being associated with the genetic etiology of the disorder?
Explanation
Attention-deficit/hyperactivity disorder is a neurodevelopmental disorder with strong geneticpredisposition, involving abnormal dopaminergicsignaling, impairedprefrontal cortexregulation, and alteredcatecholaminepathways. Heritability is estimated at ≥70%, with family and twin studies confirming genetic transmission. Specific gene polymorphisms in dopamine transporter and receptor genes increase susceptibility.
Rationale for correct answer:
2.Having a sibling diagnosed with ADHD reflects familial aggregation and high heritability. Twin and family studies consistently show genetic transmission. The stem emphasizes genetic etiology, and sibling presence is a direct indicator of inherited vulnerability. Heritabilityand familiallinkage confirm this.
Rationale for incorrect answers:
1.Inborn error of metabolism is not implicated in ADHD pathogenesis. Metabolic disorders such as phenylketonuria cause cognitive impairment but do not specifically produce ADHD. ADHD is linked to neurotransmitter dysregulation, not metabolic enzyme defects. Metabolismand enzymeare irrelevant.
3.Dopamine neurotransmitter deficit is a neurochemical factor, not strictly genetic. While dopamine dysregulation contributes to symptoms, it represents biochemical imbalance rather than inherited etiology. The stem specifies genetic basis, making this option incorrect. Dopamineand neurochemicalare contributory, not genetic.
4.Arrested id development is a psychodynamic concept without biological evidence. ADHD is not explained by Freud’s structural theory of personality. Neurodevelopmental abnormalities, not unconscious conflict, underlie the disorder. Psychodynamicand idare scientifically invalid here.
Test-taking strategy
- Focus on the stem wording: it specifies genetic etiology, not biochemical or psychodynamic.
- Rule out options describing neurochemical imbalanceor psychodynamic theory, as these are not genetic.
- Eliminate distractors that describe unrelated conditions (inborn errors of metabolism).
- Recognize that family historyis the strongest genetic indicator.
- Use knowledge of heritability studies: ADHD shows sibling and twin concordance, confirming genetics.
- Apply principle: when asked about genetic basis, select familial aggregation rather than neurotransmitter imbalance.
- Remember that dopamine deficit is valid but belongs under neurochemical etiology, not genetic.
- Psychodynamic explanations are outdated and lack biological evidence, making them easy eliminations.
- Inborn errors of metabolism cause global cognitive deficits, not ADHD-specific pathology.
- Correct answer aligns with evidence-based geneticsin ADHD research.
Take home points
- ADHD has strong genetic heritability, with sibling concordance supporting familial transmission.
- Dopamine and norepinephrine dysregulation explain neurochemical basis but are not genetic causes.
- Psychodynamic theories do not explain ADHD etiology.
- Inborn errors of metabolism cause cognitive impairment but are not linked to ADHD.
A nurse reviews possible causes of attention-deficit/hyperactivity disorder (ADHD) with a parent. Which factor is most strongly associated with the development of ADHD?
Explanation
Attention-deficit/hyperactivity disorder is a neurodevelopmental disorder with strong geneticpredisposition, involving abnormal dopaminergicsignaling, impaired prefrontal cortexregulation, and altered catecholaminepathways. Heritability is estimated at ≥70%, with family and twin studies confirming genetic transmission. Specific gene polymorphisms in dopamine transporter and receptor genes increase susceptibility.
Rationale for correct answer:
1.Genetic predisposition involving first-degree relatives is the most stronglyassociated factor. Twin and family studies consistently demonstrate high heritability. The presence of ADHD in parents or siblings significantly increases risk. Geneticand heritabilityevidence confirm this as the primary etiology.
Rationale for incorrect answers:
2.Inconsistent parental discipline may exacerbate behavioral symptoms but does not cause ADHD. Parenting style influences symptom severity and management but lacks neurobiological causation. ADHD originates from neurodevelopmental abnormalities, not discipline patterns. Parenting and environment are contributory, not causal.
3.Exposure to stressful school environments may worsen inattention and hyperactivity but is not etiologic. Environmental stressors influence symptom expression but do not explain pathogenesis. ADHD develops from genetic and neurochemical abnormalities. Stressand schoolfactors are secondary.
4.Delayed toilet training during toddlerhood is unrelated to ADHD. Toilet training reflects developmental readiness and parental guidance, not neurobiological dysfunction. ADHD symptoms are linked to cortical and neurotransmitter dysregulation, not toileting milestones. Toilet and development are irrelevant.
Test-taking strategy
- Focus on the stem wording: it asks for the factor most strongly associated with ADHD development.
- Rule out options describing environmental influences or developmental milestones, as these are not causative.
- ADHD is a neurodevelopmental disorderwith high heritability; family history is the strongest predictor.
- Eliminate distractors that describe symptom exacerbation (school stress, parental discipline).
- Apply principle: when asked about strongest association, select genetic predispositionsupported by twin and family studies.
- Remember that neurotransmitter imbalance explains symptoms but the question specifies etiology, making genetics the correct choice.
- Use evidence-based reasoning: ADHD heritability ≥70% confirms genetic linkage.
- Distractors are environmental modifiers, not primary causes.
- Correct answer aligns with established scientific consensus on ADHD pathogenesis.
- Always prioritize biological evidencewhen asked about strongest associations.
Take home points
- ADHD is a neurodevelopmental disorder with strong genetic heritability.
- Family history, especially first-degree relatives, is the most significant risk factor.
- Environmental influences may worsen symptoms but are not causative.
- Developmental milestones such as toilet training are unrelated to ADHD etiology.
A nurse is providing an educational session for parents of children recently diagnosed with attention-deficit/hyperactivity disorder (ADHD). Which statement should the nurse include as an accurate description of the disorder?
Explanation
Attention-deficit/hyperactivity disorder is a neurodevelopmental disorder marked by inattention, hyperactivity, and impulsivity. It involves abnormal dopaminergicand noradrenergicsignaling within frontostriatal circuits, leading to impaired executive function. Symptoms persist ≥6 months, manifest before age 12, and cause functional impairment across settings.
Rationale for correct answer:
4.ADHD is characterized by a persistent pattern of inattention, often accompanied by hyperactivity and impulsivity. Diagnostic criteria require symptoms across ≥2 settings with significant impairment. The stem emphasizes accurate description, making this the correct choice. Inattentionand impulsivitydefine the disorder.
Rationale for incorrect answers:
1.Withdrawal into self describes autism spectrum disorder, not ADHD. ADHD involves externalizing behaviors such as distractibility and hyperactivity, not social withdrawal. Autismand withdrawalare distinct from ADHD pathology.
2.ADHD is not diagnosed before 2 years of age. Symptoms must be present before age 12, but reliable diagnosis typically occurs during school years. Ageand diagnosiscriteria exclude toddlers.
3.ADHD occurs more commonly in males than females, with a ratio of approximately 2:1 in childhood. Females often present with inattentive subtype, but prevalence is not equal. Genderand prevalencediffer.
Test-taking strategy
- Focus on DSM-5 diagnostic criteria: persistent inattention, hyperactivity, impulsivity.
- Rule out distractors describing other disorders (withdrawal → autism).
- Eliminate options inconsistent with diagnostic age criteria (<2 years).
- Apply epidemiology: ADHD is more common in males, not equal prevalence.
- Select the option that directly reflects the core symptom pattern.
- Use knowledge of diagnostic thresholds: symptoms ≥6 months, onset before 12 years, impairment in ≥2 settings.
- Remember that accurate descriptions must align with established definitions, not environmental or developmental factors.
- Distractors often describe associated conditions or misapplied features.
- Correct answer reflects the persistent symptom patterncentral to ADHD.
- Always prioritize evidence-based diagnostic language when evaluating descriptive statements.
Take home points
- ADHD is defined by persistent inattention, hyperactivity, and impulsivity.
- Diagnosis requires symptoms ≥6 months, onset before age 12, and impairment in multiple settings.
- Autism involves withdrawal into self, distinguishing it from ADHD.
- ADHD prevalence is higher in males, with females often showing inattentive subtype.
A nurse is performing a physical and behavioral assessment on a child. Which finding should the nurse recognize as a criterion for a diagnosis of attention-deficit/hyperactivity disorder (ADHD)?
Explanation
Attention-deficit/hyperactivity disorder is a neurodevelopmental disorder defined by inattention, hyperactivity, and impulsivity. It involves abnormal dopaminergicand noradrenergicsignaling in frontostriatal circuits, leading to impaired executive function. Symptoms must persist ≥6 months, begin before age 12, and cause impairment in ≥2 settings.
Rationale for correct answer:
1.Inattention is a DSM-5-TR diagnostic criterion for ADHD. It includes distractibility, difficulty sustaining tasks, forgetfulness, and disorganization. The stem specifies DSM-5-TR criteria, making inattention the accurate choice. Inattentionand disorganizationare core features.
Rationale for incorrect answers:
2.Recurrent intrusive thoughts are characteristic of obsessive-compulsive disorder, not ADHD. They involve unwanted, repetitive cognitions leading to compulsions. ADHD symptoms are attentional and behavioral, not intrusive thought patterns. Obsessionsand compulsionsare distinct.
3.Physical aggression is not a DSM-5-TR criterion for ADHD. Aggression may occur as a comorbidity with oppositional defiant disorder or conduct disorder but is not diagnostic. ADHD criteria focus on attention and activity regulation. Aggressionand conductare separate.
4.Anxiety and panic attacks are diagnostic of anxiety disorders, not ADHD. While ADHD may coexist with anxiety, panic attacks are not part of ADHD criteria. ADHD is defined by attentional and behavioral dysregulation. Anxietyand panicare unrelated.
Test-taking strategy
- Focus on DSM-5-TR diagnostic criteria: inattention, hyperactivity, impulsivity.
- Rule out distractors describing other psychiatric disorders (OCD, anxiety disorders, conduct disorders).
- Eliminate options that describe comorbidities rather than core diagnostic features.
- Apply principle: ADHD diagnosis requires symptoms ≥6 months, onset before 12 years, impairment in ≥2 settings.
- Select the option that directly reflects the core symptom pattern.
- Distractors often describe associated conditions but not diagnostic criteria.
- Correct answer aligns with established DSM-5-TR definitions.
- Always prioritize evidence-based diagnostic languagewhen evaluating descriptive statements.
- Use knowledge of comorbidities to rule out non-etiologic features.
- Inattention is the most accurate DSM-5-TR criterion in this context.
Take home points
- ADHD is diagnosed based on persistent inattention, hyperactivity, and impulsivity.
- DSM-5-TR requires symptoms ≥6 months, onset before age 12, impairment in multiple settings.
- Intrusive thoughts indicate OCD, not ADHD.
- Aggression and panic attacks are not diagnostic criteria but may occur as comorbidities.
Practice Excercise 2
A nurse obtains a health history for a client diagnosed with attention-deficit/hyperactivity disorder (ADHD). Which behaviors should the nurse expect? Select all that apply
Explanation
Attention-deficit/hyperactivity disorder is a neurodevelopmentalcondition characterized by inattention, hyperactivity, and impulsivity. It results from dysregulation of dopamineand norepinephrinepathways in the prefrontal cortex. Symptoms include distractibility, poor task completion, excessive verbalization, and impulsive actions. Onset occurs before age 12, with prevalence higher in males.
Rationale for correct answers:
1.Impulsivity is a hallmark of ADHDdue to impaired inhibitory control in the prefrontal cortex. Clients act without forethought, interrupt conversations, and engage in risk-taking behaviors. This stems from deficient executive functioning and altered catecholamine signaling. Impulsivity and executive dysfunctiondefine the disorder.
2.Excessive talking reflects hyperactivityand poor self-regulation. Clients often dominate conversations, interrupt others, and struggle with quiet activities. This behavior arises from cortical disinhibition and impaired attention modulation. Hyperactivity and disinhibition make this a classic ADHD manifestation.
6.Failure to complete tasks is a core feature of inattention. Clients begin activities but leave them unfinished due to distractibility and poor sustained focus. This results from impaired working memory and deficient organizational skills. Inattention and distractibility explain this presentation.
Rationale for incorrect answers:
3.Spiteful behavior is more consistent with oppositional defiant disorder, not ADHD. ADHD involves impulsivity and distractibility, but not intentional hostility. The underlying pathology is attentional dysregulation, not deliberate aggression. Hostility and vindictiveness are not diagnostic features of ADHD.
4.Deliberately annoying others is typical of oppositional defiant disorder. ADHD clients may irritate others unintentionally due to impulsivity, but purposeful provocation is not characteristic. The neurobiology involves attentional deficits, not intentional defiance. Provocation and defiance distinguish ODD from ADHD.
5.Prolonged video gaming is a behavioral choice, not a diagnostic criterion. While ADHD clients may struggle with time management, excessive gaming is not a defining feature. It reflects environmental reinforcement, not intrinsic pathology. Behavioral addiction and environmental influence explain this, not ADHD.
Test-taking strategy
- Identify core symptomsof ADHD: inattention, hyperactivity, impulsivity.
- Rule out behaviors linked to other disorders: oppositional defiant disorder involves hostility and deliberate provocation.
- Distinguish environmental behaviors (gaming) from diagnostic features.
- Focus on neurodevelopmental basis: ADHD arises from catecholamine dysregulation in the prefrontal cortex.
- Eliminate distractors by asking: Is this behavior intrinsic to attentional or inhibitory dysfunction?
- Correct answers must align with DSM-5 diagnostic criteria.
- Use elimination: spiteful and deliberately annoying behaviors → ODD; prolonged gaming → lifestyle, not pathology.
- Select impulsivity, excessive talking, and failure to complete tasks as they directly reflect ADHD’s triad of symptoms.
Take home points
- ADHD is defined by inattention, hyperactivity, and impulsivity.
- Oppositional defiant disorder involves deliberate hostility and provocation, not ADHD.
- Environmental behaviors like gaming are not diagnostic criteria.
- Differentiation requires understanding neurodevelopmental versus behavioral pathology.
A nurse assesses a client with the inattentive presentation of attention-deficit/hyperactivity disorder (ADHD). Which behavior is most consistent with this presentation?
Explanation
Attention-deficit/hyperactivity disorder, inattentive presentation, is defined by inattention, poor concentration, impaired working memory, and reduced organization. It is linked to dysfunction in prefrontal cortical circuits regulating dopamine and norepinephrine. Clients show distractibility, forgetfulness, and difficulty sustaining focus, without prominent hyperactivity or impulsivity.
Rationale for correct answer:
1.Difficulty sustaining attention during tasks is the hallmark of inattentive ADHD. Clients struggle with prolonged focus, make careless mistakes, and fail to follow through on instructions. This results from impaired executive functioning and deficient catecholamine signaling. Inattention and distractibilitydefine this subtype.
Rationale for incorrect answers:
2.Frequent physical restlessness is characteristic of hyperactive-impulsive ADHD. It involves fidgeting, inability to remain seated, and excessive motor activity. Inattentive presentation lacks prominent hyperactivity and motor agitation, making this inconsistent with the described subtype.
3.Excessive talking and interrupting others reflect hyperactive-impulsive ADHD. Clients with inattentive presentation do not display verbal overactivity. The pathology involves attentional deficits, not disinhibition or verbal impulsivity, so this is not consistent.
4.Engaging in risk-taking behaviors is linked to impulsivity and poor inhibitory control, typical of hyperactive-impulsive ADHD. Inattentive presentation is defined by distractibility and poor sustained focus, not impulsivity or risk-taking, making this incorrect.
Test-taking strategy
- Identify the presentation subtype: inattentive vs hyperactive-impulsive.
- Recall DSM-5 criteria: inattentive subtype requires ≥6 symptoms of inattention, such as poor focus, forgetfulness, and disorganization.
- Eliminate distractors by matching behaviors to hyperactive-impulsive features (restlessness, excessive talking, risk-taking).
- Focus on neurodevelopmental basis: inattentive ADHD stems from impaired prefrontal cortical regulation of attention, not motor or behavioral disinhibition.
- Correct answer must directly reflect attentional dysfunction, not hyperactivity or impulsivity.
- Use elimination: restlessness, talking, and risk-taking → hyperactive-impulsive; sustained attention difficulty → inattentive subtype.
Take home points
- Inattentive ADHD is defined by distractibility, poor focus, and disorganization.
- Hyperactive-impulsive ADHD involves restlessness, excessive talking, and impulsivity.
- Subtype differentiation is essential for accurate diagnosis and management.
- Neurobiology involves catecholamine dysregulation in prefrontal cortical circuits.
A nurse is assessing a client with the hyperactive-impulsive presentation of attention-deficit/hyperactivity disorder (ADHD). Which finding should the nurse expect?
Explanation
Attention-deficit/hyperactivity disorder, hyperactive-impulsive presentation, is characterized by hyperactivity, impulsivity, poor inhibitory control, and excessive motor activity. It results from dysregulation of catecholamine pathways in the prefrontal cortex and basal ganglia. Clients display restlessness, excessive talking, interrupting, and risk-taking behaviors without predominant inattention.
Rationale for correct answer:
1.Fidgeting and inability to remain seated are classic features of hyperactive-impulsive ADHD. Clients show constant movement, tapping, or squirming due to cortical disinhibition. This reflects impaired inhibitory control and excessive motor drive. Hyperactivityand restlessnessdefine this subtype.
Rationale for incorrect answers:
2.Daydreaming during conversations is typical of inattentive ADHD. It reflects distractibility and poor sustained focus, not hyperactivity. The pathology involves inattentionand cognitive drift, making this inconsistent with hyperactive-impulsive presentation.
3.Slow task completion is linked to inattentive ADHD due to poor organization and distractibility. Hyperactive-impulsive clients act quickly, often without forethought, but do not exhibit prolonged task delays. Disorganizationand inattentionexplain slow completion, not hyperactivity.
4.Avoidance of group activities is more consistent with social anxiety or autism spectrum disorder. Hyperactive-impulsive ADHD clients often seek stimulation and interaction, though disruptive. Social withdrawaland avoidanceare not defining features of this subtype.
Test-taking strategy
- Identify presentation subtype: hyperactive-impulsive vs inattentive.
- Recall DSM-5 criteria: hyperactive-impulsive requires ≥6 symptoms of hyperactivity/impulsivity such as fidgeting, excessive talking, interrupting, and inability to remain seated.
- Eliminate distractors by matching behaviors to inattentive features (daydreaming, slow task completion) or unrelated conditions (avoidance of group activities).
- Focus on motor restlessnessand impulsivityas diagnostic hallmarks.
- Correct answer must directly reflect excessive motor activity and poor inhibitory control.
- Use elimination: daydreaming and slow tasks → inattentive; avoidance → social withdrawal; fidgeting → hyperactive-impulsive.
Take home points
- Hyperactive-impulsive ADHD is defined by restlessness, impulsivity, and excessive motor activity.
- Inattentive ADHD involves distractibility, daydreaming, and poor task completion.
- Social withdrawal is not a feature of ADHD but may suggest other conditions.
- Subtype recognition is essential for accurate diagnosis and tailored interventions.
A nurse is selecting an intervention for a client with attention-deficit/hyperactivity disorder (ADHD). Which activity is most appropriate for a client with ADHD?
Explanation
Attention-deficit/hyperactivity disorder is a neurodevelopmentaldisorder marked by hyperactivity, impulsivity, and inattention. Clients benefit from structured activities with clear rules, short attention demands, and opportunities for physical activity. Such interventions channel excess energy, improve focus, and reduce disruptive behaviors.
Rationale for correct answer:
2.Volleyball is appropriate because it provides structured rules, teamwork, and continuous physical movement. The activity channels hyperactivity into organized play, enhances attention through rapid responses, and promotes social interaction. Structureand movementmake it ideal for ADHD management.
Rationale for incorrect answers:
1.Monopoly requires prolonged attention, strategic planning, and sustained focus, which ADHD clients struggle with. The slow pace and extended cognitive demand exacerbate distractibility. Inattentionand poor concentrationmake this unsuitable.
3.Pool swimming, while physically engaging, lacks the structured group interaction and rapid attention shifts that benefit ADHD clients. It may reduce hyperactivity but does not reinforce social skillsor teamwork, limiting therapeutic value.
4.Checkers demands sustained concentration and patience, which ADHD clients often lack. The sedentary nature fails to channel hyperactivity, and the cognitive load may increase frustration. Distractibilityand restlessnessmake this inappropriate.
Test-taking strategy
- Identify interventions that match ADHD symptomatology: hyperactivity, impulsivity, inattention.
- Apply principles: activities should be structured, short in duration, and involve physical movement.
- Rule out sedentary, prolonged, or cognitively demanding activities (Monopoly, Checkers).
- Consider therapeutic value: group sports enhance socializationand attention regulation.
- Eliminate options that do not address hyperactivity or require sustained focus.
- Select volleyball because it combines structure, movement, and teamwork, aligning with ADHD needs.
Take home points
- ADHD interventions should emphasize structure, movement, and short attention demands.
- Sedentary, prolonged activities worsen distractibility and frustration.
- Group sports enhance social skills and channel hyperactivity positively.
- Differentiating interventions requires matching activity demands to ADHD symptom profile.
A nurse anticipates that a client with attention-deficit/hyperactivity disorder (ADHD) may be learning-disabled. This means the client:
Explanation
Learning disability refers to perceptual difficultiesthat interfere with information processing, despite normal intelligenceand adequate opportunity. It involves dysfunction in brain regions responsible for language, reading, or mathematics. Clients may struggle with decoding, comprehension, or written expression, independent of intellectual impairment.
Rationale for correct answer:
3.Experiences perceptual difficulties that interfere with learning defines a learning disability. Clients have intact intelligence but impaired processing of auditory or visual input. This leads to difficulties in reading, writing, or mathematics. Perceptionand processing deficitsare central features.
Rationale for incorrect answers:
1.Not being self-directed reflects motivational or behavioral issues, not learning disability. Learning disability is neurologically based, involving processing deficits, not lack of initiative or independence.
2.Intellectual impairment is distinct from learning disability. Clients with learning disabilities have normal intelligence but specific deficits in processing. Cognitionand IQremain intact, differentiating it from intellectual disability.
4.Performing two grade levels below age norms may be a consequence of learning disability but is not its definition. The defining feature is impaired information processing, not academic performance alone.
Test-taking strategy
- Focus on the definitionof learning disability: intact intelligence with impaired perceptual processing.
- Rule out distractors that describe intellectual disability (choice 2) or behavioral issues (choice 1).
- Recognize that academic underperformance (choice 4) is a result, not the defining feature.
- Correct answer must directly reflect the neurological basis of learning disability.
- Use elimination: lack of self-direction → behavioral; intellectual impairment → separate disorder; grade-level deficit → consequence, not definition.
- Select perceptual difficulties interfering with learning as the precise definition.
Take home points
- Learning disability involves perceptual and processing deficits, not low intelligence.
- ADHD often coexists with learning disabilities, complicating academic performance.
- Intellectual disability differs by global cognitive impairment, not specific processing deficits.
- Academic underachievement may result from learning disability but is not diagnostic.
Practice Exercise 3
A nurse reviews the criteria for attention-deficit/hyperactivity disorder (ADHD). Which requirement must be met for diagnosis?
Explanation
Attention-deficit/hyperactivity disorder is a neurodevelopmentaldisorder characterized by inattention, hyperactivity, and impulsivity. According to DSM-5-TR, symptoms must be present before age 12, persist for ≥6 months, and cause impairment in multiple settings such as home, school, or work. Functional impairmentacross contexts is essential for diagnosis.
Rationale for correct answer:
1.Symptoms must be present in two or more settings is a DSM-5-TR requirement. ADHD must cause impairment in at least two domains (e.g., school and home) to confirm pervasive dysfunction. Cross-situationaland functional impairmentvalidate the diagnosis.
Rationale for incorrect answers:
2.Symptoms resolving with behavioral therapy alone is not a diagnostic requirement. ADHD often requires multimodal treatment including pharmacotherapy. Persistenceand neurobiologydefine the disorder, not treatment response.
3.Symptoms accompanied by psychosis are not part of ADHD criteria. Psychosis indicates a separate psychiatric disorder. ADHD involves attention deficitsand impulsivity, not hallucinations or delusions.
4.Symptoms beginning after school enrollment contradict DSM-5-TR. ADHD must present before age 12. Onset after school entry suggests other conditions. Early onsetand developmental trajectoryare required.
Test-taking strategy
- Recall DSM-5-TR diagnostic criteria: onset before age 12, persistence ≥6 months, impairment in ≥2 settings.
- Eliminate distractors: treatment response is not diagnostic, psychosis is unrelated, and onset after school enrollment is too late.
- Focus on cross-situational impairmentas the defining requirement.
- Correct answer must align with DSM-5-TR standards, not treatment outcomes or unrelated psychiatric features.
- Use elimination: therapy response → management, not diagnosis; psychosis → separate disorder; late onset → inconsistent.
Take home points
- ADHD requires symptoms in ≥2 settings for diagnosis.
- Onset must occur before age 12.
- Psychosis is not part of ADHD diagnostic criteria.
- Treatment response does not define diagnosis; persistence and impairment do.
A nurse uses assessment scales when evaluating a client for attention-deficit/hyperactivity disorder (ADHD). Which tool is commonly used to support diagnosis?
Explanation
Attention-deficit/hyperactivity disorder is a neurodevelopmentaldisorder characterized by persistent inattention, hyperactivity, and impulsivitybeginning before age 12. It involves dysfunction of dopaminergicand noradrenergic pathways, with genetic predisposition and environmental triggers. Symptoms include distractibility, poor task completion, fidgeting, and impulsive behaviors. ADHD is associated with academic underachievement, social impairment, and increased risk of comorbid psychiatric disorders.
Rationale for correct answer:
1.The Vanderbilt Assessment Scale is specifically designed to evaluate ADHD symptoms in children. It assesses both inattentionand hyperactivity, with teacher and parent input. It also screens for comorbidities such as oppositional defiant disorder and conduct disorder, making it clinically appropriate for diagnostic support.
Rationale for incorrect answers:
2.The Mini-Mental State Examination evaluatescognitionin adults, focusing on orientation, memory, and language. It is used for dementia and delirium screening, not ADHD. Its structure lacks sensitivity for attentional deficits in pediatric populations, making it unsuitable for ADHD diagnosis.
3.The Beck Depression Inventory measuresdepressivesymptomsincluding mood, guilt, and suicidal ideation. It is validated for major depressive disorder but does not assess hyperactivity or impulsivity. ADHD requires evaluation of attentional and behavioral domains, which this tool does not address.
4.The Glasgow Coma Scale assesses consciousness in acute neurological injury, measuring eye, verbal, and motor responses. It is used in trauma and critical care settings. ADHD is a chronic neurodevelopmental disorder, not an acute alteration of consciousness, so this scale is irrelevant.
Test-taking strategy
- Identify the main conditionin the stem: ADHD.
- Recall that ADHD requires specialized behavioral assessment tools.
- Rule out tools unrelated to ADHD:
- MMSE is for dementia.
- Beck Depression Inventory is for depression.
- Glasgow Coma Scale is for consciousness.
- Focus on the tool that specifically evaluates inattentionand hyperactivityin children.
- Use elimination methodology:
- Remove tools assessing cognition, mood, or consciousness.
- Retain the one validated for ADHD diagnosis.
- Correct answer emerges by matching the tool to the disorder’s core symptoms.
Take home points
- ADHD is a neurodevelopmental disorder with onset before age 12.
- Vanderbilt Assessment Scale is validated for ADHD diagnosis in children.
- MMSE, Beck Depression Inventory, and Glasgow Coma Scale assess other conditions.
- Differentiating ADHD from mood disorders and cognitive impairment is essential.
A nurse is differentiating combined presentation attention-deficit/hyperactivity disorder (ADHD) from other conditions. Which feature supports a combined presentation?
Explanation
Attention-deficit/hyperactivity disorder combined presentation involves both inattentionand hyperactivity-impulsivitypersisting ≥6 months, with onset before age 12, across ≥2 settings. Dysfunction in dopamineand norepinephrinepathways underlies impaired executive function, manifesting as distractibility, fidgeting, poor sustained attention, and impulsive behaviors.
Rationale for correct answer:
1.Combined presentation requires ≥6 months of both inattentionand hyperactivitysymptoms, present in multiple environments. This aligns with DSM-5 criteria, confirming diagnosis. The persistence and dual symptom clusters distinguish combined ADHD from inattentive or hyperactive-impulsive types.
Rationale for incorrect answers:
2.Symptoms limited to the classroom indicate situational behavioralissues, not ADHD. ADHD requires impairment in ≥2 settings (home, school, social). Restriction to one environment excludes diagnosis of combined presentation.
3.Onset after age 12 contradicts DSM-5 criteria. ADHD must begin before age 12. Later onset suggests other psychiatricor cognitive disorders, not combined ADHD.
4.Hallucinations and delusions are features of psychosis, not ADHD. ADHD involves attentional and behavioral dysregulation, not perceptual disturbances. Psychotic symptoms indicate schizophrenia or mood disorders with psychotic features.
Test-taking strategy
- Identify the main condition: ADHD combined presentation.
- Recall DSM-5 diagnostic criteria: onset before 12, symptoms ≥6 months, impairment in ≥2 settings.
- Rule out distractors:
- Classroom-only symptoms = situational.
- Onset after 12 = not ADHD.
- Hallucinations = psychosis.
- Focus on the option describing both inattentionand hyperactivitypersisting ≥6 months.
- Use elimination methodology: remove answers inconsistent with ADHD diagnostic framework.
- Correct answer emerges by matching DSM-5 criteria to combined presentation.
Take home points
- Combined ADHD requires both inattention and hyperactivity symptoms ≥6 months.
- Symptoms must occur in ≥2 settings, not restricted to one.
- Onset must be before age 12 for ADHD diagnosis.
- Psychotic features differentiate schizophrenia from ADHD.
A nurse differentiates attention-deficit/hyperactivity disorder (ADHD) from anxiety disorders. Which finding is more consistent with ADHD?
Explanation
Attention-deficit/hyperactivity disorder is a neurodevelopmentaldisorder characterized by persistent inattention, hyperactivity, and impulsivityacross multiple settings, with onset before age 12. Dysfunction in dopamineand norepinephrine pathways impairs executive function, leading to distractibility, poor sustained attention, fidgeting, and impulsive behaviors. ADHD differs from anxiety disorders, which are marked by excessive worry, fear, and autonomic hyperarousal.
Rationale for correct answer:
1.ADHD presents with persistent difficulty sustainingattentionacross settings such as home, school, and social environments. This impairment is not situational but pervasive. The presence of both attentional deficits and behavioral dysregulation supports ADHD rather than anxiety disorders.
Rationale for incorrect answers:
2.Excessive worry about future events is characteristic of generalized anxiety disorder. It reflects cognitive preoccupation with potential threats, not attentional deficits. ADHD involves distractibility and impulsivity, not chronic worry.
3.Fear of social situations indicates socialanxiety disorder. It involves avoidance due to fear of embarrassment or scrutiny. ADHD does not primarily manifest as social fear but as inattentive and hyperactive behaviors.
4.Avoidance of school due to panic reflects panicdisorderor school refusal linked to anxiety. ADHD does not cause panic attacks or avoidance behaviors; instead, it causes poor task completion and impulsivity across settings.
Test-taking strategy
- Identify the main condition: ADHD versus anxiety disorders.
- Recall ADHD diagnostic criteria: inattention, hyperactivity, impulsivity, onset before 12, symptoms ≥6 months, impairment in ≥2 settings.
- Rule out distractors:
- Excessive worry = generalized anxiety.
- Social fear = social anxiety.
- School avoidance due to panic = panic disorder.
- Focus on the option describing attention deficitsacross multiple environments.
- Use elimination methodology: remove answers linked to anxiety-specific features.
- Correct answer emerges by matching ADHD’s hallmark symptom of persistent inattentionacross settings.
Take home points
- ADHD involves persistent inattention and hyperactivity across ≥2 settings.
- Anxiety disorders are defined by excessive worry, fear, or panic.
- ADHD onset is before age 12, anxiety may occur later.
- Differentiating ADHD from anxiety requires focus on attentional versus emotional symptoms.
Practice Exercise 4
A nurse is caring for a 9-year-old client with attention-deficit/hyperactivity disorder. Which medication is most frequently prescribed for ADHD?
Explanation
Attention-deficit/hyperactivity disorder is a neurodevelopmentaldisorder treated primarily with stimulantmedications that enhance dopamineand norepinephrinetransmission in the prefrontal cortex, improving attention and impulse control. Methylphenidate is the most frequently prescribed stimulant for children, with proven efficacy in reducing hyperactivity and improving focus.
Rationale for correct answer:
3.Methylphenidate (Ritalin) is the first-line stimulant for ADHD. It increases synaptic dopamine and norepinephrine, improving attention span and reducing impulsivity. It is widely prescribed in pediatric ADHD due to strong evidence of efficacy and safety.
Rationale for incorrect answers:
1.Lorazepam (Ativan) is a benzodiazepineused for anxiety and acute agitation. It enhances GABA activity, causing sedation. It does not improve attention or hyperactivity, making it inappropriate for ADHD management.
2.Haloperidol (Haldol) is a typical antipsychoticused for schizophrenia and severe agitation. It blocks dopamine receptors, which may worsen attentional deficits. It is not indicated for ADHD and carries risk of extrapyramidal side effects.
4.Methocarbamol (Robaxin) is a muscle relaxantused for musculoskeletal pain. It acts centrally to reduce muscle spasms but has no role in ADHD treatment. It does not affect attention or impulsivity.
Test-taking strategy
- Identify the main condition: ADHD in a pediatric client.
- Recall first-line pharmacologic treatment: stimulants(methylphenidate, amphetamines).
- Rule out distractors:
- Benzodiazepines treat anxiety, not ADHD.
- Antipsychotics treat psychosis, not ADHD.
- Muscle relaxants treat musculoskeletal pain, not ADHD.
- Focus on the option that directly improves dopamineand norepinephrinesignaling in the prefrontal cortex.
- Use elimination methodology: remove drugs unrelated to attentional regulation.
- Correct answer emerges by matching stimulant therapy to ADHD pathophysiology.
Take home points
- Methylphenidate is the most frequently prescribed stimulant for ADHD in children.
- ADHD treatment targets dopamine and norepinephrine pathways to improve attention.
- Benzodiazepines, antipsychotics, and muscle relaxants are not indicated for ADHD.
- Differentiating ADHD pharmacotherapy from other psychiatric and neurologic drugs is essential.
A nurse is caring for a client with attention-deficit/hyperactivity disorder (ADHD) who is prescribed methylphenidate (Ritalin). Which symptoms should the nurse monitor as potential side effects? Select all that apply
Explanation
Methylphenidate is a stimulantmedication that enhances dopamineand norepinephrineactivity in the prefrontal cortex, improving attention and impulse control. Common adverse effects include insomnia, decreased appetite, headache, abdominal pain, and potential risk of seizures. Cardiovascular effects usually involve mild hypertension or tachycardia, not hypotension.
Rationale for correct answers:
2.Decreased appetite is a frequent side effect due to stimulant-induced suppression ofdopaminergicpathwaysregulating hunger. This can lead to weight loss in children, requiring monitoring of growth and nutritional intake.
4.Insomnia occurs because stimulantsincrease CNS activity. Evening dosing exacerbates sleep disturbance. Nurses should advise morning administration and monitor sleep hygiene to reduce impact on rest.
5.Headache is a common adverse effect linked to stimulant-induced changes inneurotransmitterbalance. It is usually mild but can interfere with adherence, requiring symptomatic management.
6.Seizures are a rare but serious adverse effect. Stimulants lower the seizure threshold, especially in clients with preexisting epilepsy. Monitoring neurological status is essential to detect early warning signs.
Rationale for incorrect answers:
1.Hypotension is not typical of methylphenidate. Stimulants usually cause hypertension or tachycardia due to sympathetic activation. Monitoring blood pressure is important, but hypotension is not expected.
3.Sedation is inconsistent with stimulant pharmacology. Methylphenidate increases alertness and activity, not drowsiness. Sedationwould suggest another drug effector comorbidity, not methylphenidate.
Test-taking strategy
- Identify the main drug: methylphenidate, a stimulant.
- Recall stimulant side effects: insomnia, appetite suppression, headache, abdominal pain, possible seizures.
- Rule out distractors:
- Hypotension is not expected; stimulants raise blood pressure.
- Sedation contradicts stimulant pharmacology.
- Focus on adverse effects consistent with CNS stimulationand appetite suppression.
- Use elimination methodology: remove options inconsistent with stimulant effects.
- Correct answers emerge by matching stimulant pharmacodynamics to expected clinical manifestations.
Take home points
- Methylphenidate commonly causes decreased appetite, insomnia, and headache.
- Seizures are rare but serious adverse effects requiring monitoring.
- Hypotension and sedation are not expected with stimulant therapy.
- Nurses must monitor growth, sleep, and neurological status in children on methylphenidate.
A nurse is caring for a 10-year-old client prescribed dextroamphetamine (Dexedrine) who has a nursing diagnosis of imbalanced nutrition: less than body requirements related to anorexia. Which nursing intervention addresses this problem?
Explanation
Dextroamphetamine is a stimulantthat enhances dopamineand norepinephrineactivity, improving attention and impulse control in ADHD. However, it frequently causes anorexiaand weight loss due to appetite suppression. Administering the drug after meals helps reduce nutritional impact by allowing adequate intake before appetite suppression begins.
Rationale for correct answer:
3.Administering dextroamphetamine after meals minimizesanorexiaby ensuring the child eats before appetite suppression occurs. This intervention directly addresses imbalanced nutrition and supports growth and weight maintenance in pediatric ADHD clients.
Rationale for incorrect answers:
1.Monitoring output and sleep patterns daily is important for stimulant therapy but does not directly addressnutrition. It helps detect insomnia or urinary changes, yet it fails to correct anorexia-related weight loss.
2.Administering medication with food prevents nausea, not anorexia. Stimulants primarily suppress appetite rather than cause gastrointestinal upset. This intervention does not resolve the nutritional deficit associated with dextroamphetamine.
4.Increasing fiber and fluid intake prevents constipation, a possible side effect of stimulants. While beneficial, it does not address anorexia or weight loss, which are the primary nutritional concerns in this scenario.
Test-taking strategy
- Identify the main issue: imbalanced nutrition due to anorexia from stimulant therapy.
- Recall stimulant side effects: appetite suppression, insomnia, headache, abdominal pain.
- Rule out distractors:
- Monitoring sleep/output = general care, not nutrition.
- With food = prevents nausea, not anorexia.
- Fiber/fluid = prevents constipation, not anorexia.
- Focus on the intervention that directly improves nutritional intake.
- Correct answer emerges by matching anorexia management with timing of medication administration.
Take home points
- Stimulants like dextroamphetamine suppress appetite, leading to anorexia and weight loss.
- Administering medication after meals helps preserve nutritional intake.
- Other interventions address side effects but not anorexia.
- Nurses must monitor growth and weight in children on stimulant therapy.
A nurse educates parents about non-stimulant medications used to treat attention-deficit/hyperactivity disorder (ADHD). Which medication is a non-stimulant option?
Explanation
Non-stimulant therapy for ADHD includes atomoxetine, a selective norepinephrinereuptake inhibitor. Unlike stimulants, it does not directly increase dopamine release but modulates norepinephrine transmission, improving attention and impulse control. Atomoxetine is useful in patients with contraindications to stimulants, comorbid anxiety, or risk of substance misuse.
Rationale for correct answer:
1.Atomoxetine (Strattera) is a non-stimulant norepinephrinereuptake inhibitor approved for ADHD. It improves attentional control without the abuse potential of stimulants. It is particularly beneficial in children with comorbid anxiety or those intolerant to stimulant side effects.
Rationale for incorrect answers:
2.Methylphenidate (Ritalin) is a stimulantthat blocks dopamine and norepinephrine reuptake. It is first-line therapy for ADHD but not classified as non-stimulant.
3.Dextroamphetamine (Dexedrine) is a stimulantthat increases dopamine and norepinephrine release. It is effective for ADHD but carries abuse potential, making it unsuitable as a non-stimulant option.
4.Lisdexamfetamine (Vyvanse) is a stimulantprodrug of dextroamphetamine. It is long-acting and effective for ADHD but remains a stimulant, not a non-stimulant medication.
Test-taking strategy
- Identify the main concept: non-stimulant ADHD medication.
- Recall that stimulants (methylphenidate, amphetamines) are first-line but not non-stimulant.
- Rule out distractors:
- Methylphenidate = stimulant.
- Dextroamphetamine = stimulant.
- Lisdexamfetamine = stimulant.
- Focus on the option that is FDA-approved as a non-stimulant.
- Correct answer emerges by matching atomoxetine to non-stimulant pharmacology.
Take home points
- Atomoxetine is the primary non-stimulant approved for ADHD.
- Stimulants include methylphenidate, dextroamphetamine, and lisdexamfetamine.
- Atomoxetine is preferred in patients with anxiety or substance misuse risk.
- Differentiating stimulant from non-stimulant therapy is essential in ADHD management.
A nurse monitors a client prescribed atomoxetine for attention-deficit/hyperactivity disorder (ADHD). Which adverse effect should the nurse assess for?
Explanation
Atomoxetine is a non-stimulantselective norepinephrinereuptake inhibitor used in ADHD management. Unlike stimulants, it lacks abuse potential but carries risk of liverinjury. Clinicians must monitor hepatic function, as atomoxetine can cause elevated transaminases, jaundice, and rare cases of hepatic failure.
Rationale for correct answer:
1.Atomoxetine may causeliver dysfunction, including hepatotoxicity with elevated ALT/AST and jaundice. Monitoring liver enzymes and clinical signs such as dark urine or right upper quadrant pain is essential to detect early hepatic injury.
Rationale for incorrect answers:
2.Severe hypoglycemia is not associated with atomoxetine. Hypoglycemia is linked toinsulinor oral hypoglycemics, not norepinephrine reuptake inhibition. Atomoxetine does not alter glucose metabolism significantly.
3.Respiratory depression is a risk with opioidsor sedatives, not atomoxetine. Atomoxetine does not depress respiratory drive, as it lacks GABAergic or opioid receptor activity.
4.Constipation is not a major adverse effect of atomoxetine. While mild gastrointestinalupset may occur, constipation is not a clinically significant or frequent finding compared to hepatic risk.
Test-taking strategy
- Identify the main drug: atomoxetine, a non-stimulant norepinephrine reuptake inhibitor.
- Recall its unique adverse effect profile: liver dysfunctionis the most clinically significant.
- Rule out distractors:
- Hypoglycemia = insulin-related.
- Respiratory depression = opioids/sedatives.
- Constipation = not common with atomoxetine.
- Focus on the adverse effect requiring routine monitoring.
- Correct answer emerges by matching atomoxetine’s pharmacology to its known hepatotoxic risk.
Take home points
- Atomoxetine is a non-stimulant ADHD medication acting via norepinephrine reuptake inhibition.
- Liver dysfunction is the most important adverse effect requiring monitoring.
- Hypoglycemia and respiratory depression are unrelated to atomoxetine.
- Differentiating stimulant versus non-stimulant adverse effects is essential in ADHD pharmacology.
Practice Exercise 5
A nurse is evaluating the effectiveness of parental teaching for a 10-year-old client diagnosed with attention-deficit/hyperactivity disorder (ADHD). Which parental statement indicates that further teaching is needed?
Explanation
Attention-deficit/hyperactivity disorder is a neurodevelopmental disorder characterized by persistent patterns of inattention, hyperactivity, and impulsivity that interfere with functioning. Pathophysiology involves dysregulation of dopamine, norepinephrine, and prefrontal cortexcircuits. Symptoms include distractibility, poor organization, fidgeting, and impulsive actions. Diagnosis requires ≥6 symptoms persisting ≥6 months. Management includes behavioral therapy, structured routines, and pharmacologic agents such as stimulants.
Rationale for correct answer:
1.Restricting sugar and food-coloring additives is not evidence-basedin ADHD management. Scientific studies show no consistent link between dietary sugar or artificial coloring and hyperactivity. The parental statement reflects a misconception, requiring further teaching. The correct approach emphasizes behavioral interventionsand pharmacologic therapy.
Rationale for incorrect answers:
2.Behavioral contracts are effective in ADHD because they provide structured reinforcement and accountability. They help children with poor organizational skills by linking specific behaviors to rewards. This aligns with evidence-basedbehavioral modificationstrategies.
3.Goal charts with star rewards are appropriate positive reinforcement techniques. They enhance motivation and track progress, supporting executive function deficits in ADHD. This structured system is consistent with recommended behavioral therapyinterventions for pediatric ADHD.
4.Setting limits and encouraging recreational activities are valid strategies. Clear boundaries reduce impulsivity, while physical activity channels hyperactivity constructively. These interventions are consistent with non-pharmacologic management and improve behavioral regulationand social functioningin affected children.
Test-taking strategy
To answer this question, the nurse must differentiate between evidence-based interventions and misconceptions. The strategy involves:
- Identifying scientifically supported interventionssuch as behavioral contracts, reward charts, and structured recreational activities.
- Recognizing that dietary restrictionsinvolving sugar and food coloring lack empirical support in ADHD management.
- Applying elimination methodology: rule out options that align with behavioral therapy principles, leaving the one based on outdated or unsupported beliefs.
- Using clinical reasoning: ADHD requires structured behavioral interventions and pharmacologic therapy, not dietary elimination.
- Focus on patient education: nurses must correct misconceptions and reinforce evidence-based strategies to ensure effective parental teaching.
This systematic approach ensures accurate identification of the statement needing further teaching.
Take home points
• ADHD is a neurodevelopmental disorder involving dopamine and norepinephrine dysregulation.
• Evidence-based management includes behavioral therapy, structured routines, and stimulant medications.
• Dietary sugar and food-coloring restrictions are not scientifically supported interventions.
• Differentiation from conditions like oppositional defiant disorder and anxiety disorders is essential in clinical practice.
Exams on ATTENTION-DEFICIT/HYPERACTIVITY DISORDER (ADHD)
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
- Objectives
- Introduction
- Etiology And Pathophysiology Of Adhd
- Practice Exercise 1
- Clinical Manifestations And Diagnostic Criteria
- Practice Excercise 2
- Diagnostic Evaluation And Differential Diagnosis
- Practice Exercise 3
- Pharmacological Interventions
- Practice Exercise 4
- Nursing Management And Psychosocial Interventions
- Practice Exercise 5
- Summary
- Comprehensive Questions
Notes Highlighting is available once you sign in. Login Here.
Objectives
- Analyze the complex interplay of genetic, neurobiological, and environmental factors in the etiology of Attention-Deficit/Hyperactivity Disorder to understand its chronic nature.
- Evaluate the specific neuroanatomical structures and neurotransmitter pathways, specifically dopamine and norepinephrine, involved in the pathophysiology of executive dysfunction.
- Assess the impact of prenatal, perinatal, and environmental risk factors on the developing neonatal brain and their subsequent contribution to ADHD symptoms.
- Synthesize the relationship between hereditary transmission and clinical presentation to facilitate accurate family history taking during nursing assessments.
- Formulate a foundational scientific understanding of ADHD to provide high-level patient education regarding the biological basis of the disorder, reducing stigma for the patient and family.
- Distinguish between the behavioral manifestations of ADHD and other neurodevelopmental or psychiatric mimics to ensure diagnostic accuracy.
- Compare the mechanisms of action between various pharmacological classes to anticipate potential side effects and therapeutic outcomes.
- Design nursing interventions that utilize environmental modification and behavioral reinforcement to bridge the gap in executive functioning.
- Integrate legal and ethical considerations regarding the administration of controlled substances in the pediatric population.
Introduction
- Attention-Deficit/Hyperactivity Disorder (ADHD) is classified as a persistent, chronic neurodevelopmental disorder.
- The condition is characterized by an age-inappropriate and pervasive pattern of inattention, hyperactivity, and impulsivity.
- Symptoms must result in significant functional impairment across multiple domains, including social, academic, or occupational settings.
- Longitudinal data confirms that ADHD is not exclusively a childhood disorder; it persists into adulthood for approximately 50% to 60% of patients.
- In adults, the presentation often shifts from overt physical hyperactivity to internal restlessness and profound executive dysfunction.
- The disorder is rooted in physiological dysfunction of the prefrontal cortex and associated subcortical structures rather than being a mere "behavioral problem."
- Global prevalence is estimated at 5% to 7% in school-aged children, with a higher diagnostic frequency in males (3:1 ratio).
- Females are frequently underdiagnosed as they often present with predominantly inattentive symptoms rather than disruptive hyperactive behaviors.
- Multimodal management is the gold standard, requiring a combination of pharmacological therapy, behavioral modification, and environmental restructuring.
Etiology And Pathophysiology Of Adhd
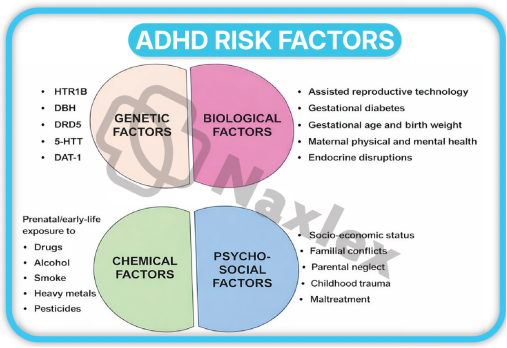
- The etiology of ADHD is multifactorial, involving a sophisticated interaction between high heritability and environmental "hits" during critical periods of neurodevelopment.
- It is categorized as a neurobiological condition where the brain's "brakes" (inhibitory control) fail to regulate the "accelerator" (impulses and motor activity).
1 Genetic Predisposition and Hereditability
ADHD is among the most heritable psychiatric conditions, often showing strong familial clustering.
- Heritability Coefficients:
- Scientific studies indicate a heritability rate of approximately 75% to 91%.
- This suggests that genetic factors play a predominant role in the manifestation of the disorder compared to environmental factors alone.
- Polygenic Inheritance:
- ADHD is not caused by a single "ADHD gene" but rather by the cumulative effect of multiple risk alleles.
- DRD4 and DRD5 Genes: These genes code for dopamine receptors; variations here are linked to reduced receptor sensitivity in the reward centers of the brain.
- DAT1 (SLC6A3): This gene encodes the dopamine transporter protein, which is responsible for the reuptake of dopamine from the synaptic cleft.
- Familial Risk:
- A child with a parent or sibling diagnosed with ADHD has a 2 to 8 times higher risk of developing the disorder.
- Twin studies show significantly higher concordance rates in monozygotic (identical) twins compared to dizygotic (fraternal) twins.
Nursing Insights
- When conducting a health history, the nurse must meticulously document the psychiatric history of first-degree relatives.
- If a parent exhibits signs of undiagnosed ADHD (e.g., constant interrupting, inability to sit still during the interview, or poor follow-through), the nurse must adapt education materials.
- Education should be concise, written, and delivered in "chunks" as the parent may struggle to process long, complex verbal instructions.
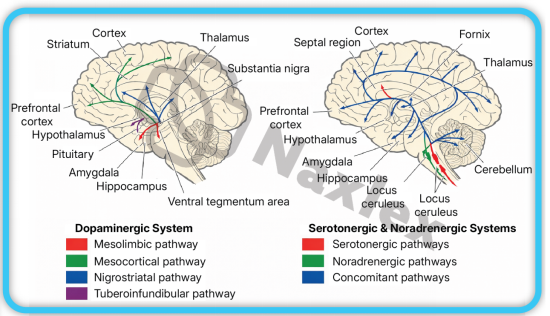
2 Neuroanatomical Disruption and Neurotransmitter Dysregulation
The core of ADHD pathology lies in the structural and functional deficiencies of the circuits connecting the prefrontal cortex to the basal ganglia.
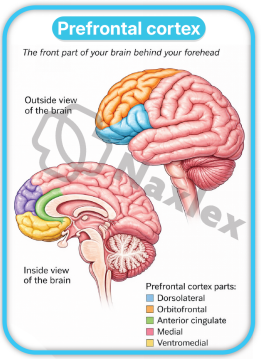
- The Prefrontal Cortex (PFC):
- This area is the "CEO" of the brain, responsible for "Executive Functions."
- Functions include working memory, impulse inhibition, and organization.
- Patients with ADHD often show delayed cortical thickening and reduced metabolic activity in this region.
- The Basal Ganglia and Cerebellum:
- These subcortical structures regulate motor control and timing.
- Reduced volume in the caudate nucleus is frequently observed in neuroimaging, which correlates strongly with hyperactive symptoms.
- The Catecholamine Hypothesis:
- The primary biochemical theory involves a deficit in the transmission of Dopamine and Norepinephrine.
- Dopamine (DA): Essential for reward, motivation, and attention. Low levels in the nucleus accumbens lead to "reward deficiency," where the patient seeks high-stimulation activities to achieve a normal level of arousal.
- Norepinephrine (NE): Crucial for modulating the "signal-to-noise" ratio. Deficient NE prevents the brain from filtering out irrelevant environmental stimuli, leading to distractibility.
- Default Mode Network (DMN) Interference:
- In a healthy brain, the DMN deactivates when a person focuses on a task.
- In ADHD, the DMN stays active, causing internal "mind-wandering" even when the patient is attempting to concentrate on a specific task.
Nursing Insights
- It is vital for the nurse to explain to parents that ADHD is a "performance disorder," not a "knowledge disorder."
- The child often knows what to do but their brain lacks the chemical "bridge" (Dopamine/Norepinephrine) to execute the action in the moment.
- Nurses should advocate for the use of external cues—such as timers, checklists, and visual prompts—to compensate for these internal neurological deficits.
- Recognize that "laziness" is a misnomer; the patient's brain requires a higher threshold of stimulation to engage in mundane tasks.
3 Environmental and Psychosocial Influences
-
While genetics set the stage, environmental "insults" can trigger or exacerbate the severity of ADHD symptoms.
- Prenatal Exposures:
- Maternal Substance Use: Exposure to nicotine, alcohol, or cocaine in utero is strongly correlated with disrupted neurogenesis and subsequent ADHD.
- Maternal Stress: High levels of maternal cortisol during pregnancy can affect fetal brain development, particularly the hypothalamic-pituitary-adrenal (HPA) axis.
- Perinatal and Postnatal Factors:
- Prematurity and Low Birth Weight: Infants born < 32 weeks gestation or < 1500g have a significantly increased risk due to potential hypoxic-ischemic brain injury to the white matter.
- Lead Exposure: Even low levels of lead (Pb) in the blood are neurotoxic and specifically interfere with the development of the prefrontal cortex and synaptic pruning.
- Psychosocial Stressors:
- Severe early deprivation (e.g., institutionalization) can lead to "ADHD-like" symptoms.
- Family discord or low socioeconomic status do not "cause" ADHD in a vacuum but can worsen the clinical trajectory and increase the risk of comorbid conduct disorders.
- Nurses working in community health or pediatric clinics should prioritize screening for environmental toxins like lead.
- Assess the home environment for stability and routine; while chaos doesn't cause ADHD, a structured environment is the primary non-pharmacological treatment.
- Identifying these secondary contributors allows for a more comprehensive treatment plan that addresses the patient's environment alongside their biology.
Clinical Manifestations And Diagnostic Criteria
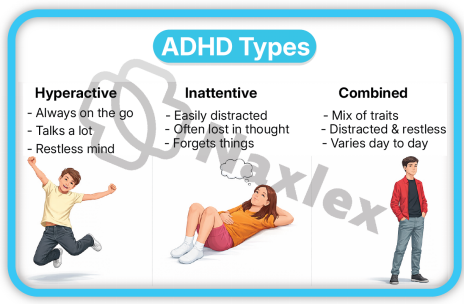
- The clinical presentation of ADHD is heterogeneous and categorized into three distinct presentations based on the predominance of symptoms over the previous 6 months.
- To meet diagnostic thresholds, symptoms must be present before age 12, occur in two or more settings (e.g., home and school), and clearly interfere with social, academic, or occupational functioning.
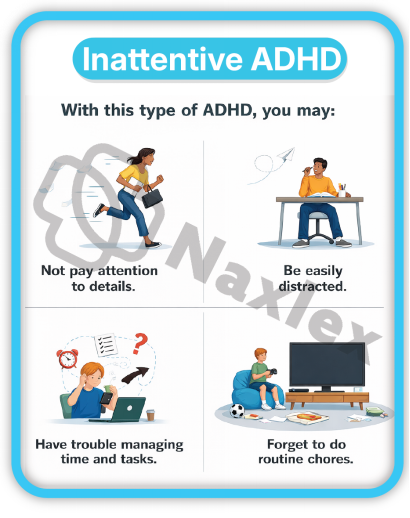
1. Inattentive Presentation
This presentation is characterized by a primary failure in the brain's "filtering" system, where the individual cannot prioritize relevant stimuli over irrelevant distractions.
- Diagnostic Requirements:
- For children up to age 16, at least 6 symptoms of inattention must be present.
- For adolescents 17 and older and adults, at least 5 symptoms are required.
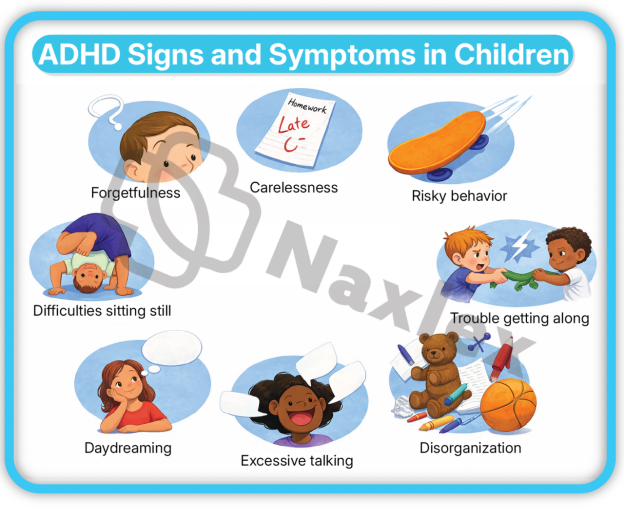
- Key Clinical Manifestations:
- Failure to Give Close Attention to Detail: The patient makes "careless" mistakes in schoolwork or professional tasks because the brain does not sustain focus on the minutiae of the assignment.
- Difficulty Sustaining Attention: Inability to remain focused during lengthy lectures, conversations, or long reading assignments.
- Apparent Listening Deficits: The individual often seems "elsewhere" or as if their mind is wandering, even in the absence of obvious external distraction.
- Poor Follow-through: Failure to finish schoolwork, chores, or workplace duties; the patient starts tasks but quickly loses focus and becomes easily sidetracked.
- Executive Dysfunction in Organization: Significant difficulty managing sequential tasks, keeping materials/belongings in order, and poor time management (missing deadlines).
- Avoidance of Mentally Effortful Tasks: A persistent reluctance to engage in tasks that require sustained mental effort (e.g., preparing reports, completing forms, or long-term projects).
- Frequent Loss of Items: Losing essential tools such as school assignments, wallets, keys, eyeglasses, or mobile phones.
- Distractibility: Easily diverted by extraneous stimuli (e.g., a car driving by, a conversation in the hallway).
- Forgetfulness in Daily Activities: Missing appointments, forgetting to return calls, or neglecting daily chores/obligations.
Nursing Insights
- Recognize that Inattentive Presentation is the most common form in females and is frequently misidentified as "daydreaming," "shyness," or "lack of motivation."
- When providing patient education, use the "TEACH-BACK" method to ensure the patient has processed the information, as their internal distractibility may prevent them from encoding the entire conversation.
- Nurses should assess for "masking" in older students, where they expend massive amounts of energy to appear focused, leading to extreme fatigue and burnout after the school day.
2. Hyperactive-Impulsive Presentation
This presentation involves a lack of behavioral inhibition and "top-down" regulation of motor activity and verbal output.
- Diagnostic Requirements:
- Similar to inattention, 6 or more symptoms are required for children.
- 5 or more for individuals 17 and older.
- Key Clinical Manifestations of Hyperactivity:
- Fidgeting and Squirming: Constant movement of hands or feet; inability to sit still in a chair.
- Inability to Remain Seated: Leaving the seat in situations where remaining seated is expected (e.g., classroom, office, or dinner table).
- Inappropriate Physical Activity: Running or climbing in situations where it is inappropriate (in adolescents or adults, this may manifest as a subjective feeling of "internal restlessness").
- Inability to Play Quietly: Difficulty engaging in leisure activities or hobbies in a calm manner.
- "Driven by a Motor": Appearing to be constantly on the go; the patient is uncomfortable being still for extended periods.
- Excessive Volubility: Talking excessively regardless of social cues or the need for silence.
- Key Clinical Manifestations of Impulsivity:
- Blurting Out Answers: Completing people's sentences or answering before a question has been fully asked.
- Difficulty Waiting Turns: Demonstrating profound impatience in lines or during group games.
- Intrusiveness: Interrupting or intruding on others' conversations, games, or activities; may start using other people's things without asking.
- In the clinical setting, the hyperactive patient is at a higher risk for accidental injury. The nurse must prioritize safety assessments and environment-proofing.
- Impulsivity can lead to "social rejection" by peers. The nurse should assess the patient's self-esteem, as repeated negative feedback from teachers and peers regarding their behavior can lead to comorbid depression or anxiety.
- In adults, physical hyperactivity often transforms into "verbal hyperactivity" or a constant need to be busy, which can be misdiagnosed as mania or high-energy anxiety.
3. Combined Presentation
- Definition: This is the most common clinical presentation. It occurs when the individual meets the diagnostic threshold (6 symptoms for children, 5 for adults) for both Inattention and Hyperactivity-Impulsivity.
- Clinical Profile: These patients represent the "classic" ADHD case. They struggle simultaneously with staying focused and remaining physically still.
- Functional Impact: Because both domains are affected, these individuals often face the highest level of impairment in academic settings and social relationships.
- Developmental Shift: It is common for a child to be diagnosed with Combined Presentation in elementary school, but as they age, the hyperactive symptoms may diminish, leaving them with a predominantly Inattentive Presentation in adulthood.
|
Feature |
Inattentive |
Hyperactive-Impulsive |
Combined |
|
Primary Deficit |
Selective Attention & Working Memory |
Behavioral Inhibition & Motor Control |
Both Cognitive & Motor Regulation |
|
Common Misnomer |
"Spacey" or "Lazy" |
"Disruptive" or "Wild" |
"Difficult" or "Uncontrollable" |
|
Gender Trend |
More common in Females |
More common in Males |
Most common clinical diagnosis |
|
Academic Impact |
Missed instructions, incomplete work |
Classroom disruption, unfinished tests |
Severe global academic impairment |
Nursing Insights
- For the Combined Presentation, the nurse must coordinate a "multimodal" plan. Medication often targets the physiological hyperactivity, but behavioral therapy is necessary to teach the organizational skills missed due to inattention.
- Nurses should monitor for "rebound" symptoms in the late afternoon when medication wears off; the combined symptoms may return with increased intensity, leading to "meltdowns" or high-risk impulsive behaviors during evening hours.
Diagnostic Evaluation And Differential Diagnosis
- The diagnostic process for ADHD is a meticulous clinical synthesis rather than a singular laboratory event.
- Because there is no definitive biological marker, such as a blood test or neuroimaging scan, for a definitive diagnosis, the clinician relies on a comprehensive history, objective data from multiple informants, and the exclusion of other medical and psychiatric conditions.
1. DSM-5-TR Diagnostic Criteria
The Diagnostic and Statistical Manual of Mental Disorders, 5th Edition, Text Revision (DSM-5-TR) establishes the standardized gold standard for diagnosis, emphasizing chronicity, pervasiveness, and impairment.
- Symptom Thresholds and Age Adjustments:
- Pediatric Population (<17 years): Requires the presence of at least 6 symptoms of inattention or 6 symptoms of hyperactivity-impulsivity.
- Adolescent/Adult Population (≥17 years): Requires a minimum of 5 symptoms in either category, acknowledging that hyperactivity often attenuates with age.
- Chronicity Requirements:
- Symptoms must have been persistent for at least 6 months to a degree that is maladaptive and inconsistent with the individual’s developmental level.
- Early Onset:
- Several inattentive or hyperactive-impulsive symptoms must have been present prior to the age of 12 years. This distinguishes ADHD from adult-onset conditions like Generalized Anxiety Disorder (GAD).
- Pervasiveness Across Environments:
- Symptoms must be manifest in two or more settings (e.g., home and school; work and social gatherings).
- If symptoms are localized to only one environment, the nurse must investigate environmental stressors, such as an abusive home or a specific learning disability at school.
- Functional Interference:
- There must be clear evidence that the symptoms interfere with, or reduce the quality of, social, academic, or occupational functioning.
Nursing Insights
- When gathering a history, the nurse should specifically ask parents for "archival data" such as elementary school report cards.
- Common red flags in early records include comments like "talks too much," "does not follow directions," or "frequently loses materials," which provide the objective evidence of symptoms before age 12 required by the DSM-5-TR.
- Nurses must be aware of "masking" in high-IQ patients who may use sheer cognitive effort to compensate for executive deficits until the complexity of higher education or professional life exceeds their coping mechanisms.
2 Assessment Scales and Clinical Observation
Objective measurement tools are utilized to quantify the severity of behaviors and compare them to age-matched norms.
- Standardized Rating Scales:
- Vanderbilt Assessment Scales: These are the most common primary care tools; they include parent and teacher versions and screen for comorbidities such as Oppositional Defiant Disorder (ODD), Conduct Disorder (CD), and Anxiety/Depression.
- Conners Rating Scales: A highly detailed tool used often in neuropsychological evaluations to assess specific domains like cognitive instability and restlessness.
- Adult ADHD Self-Report Scale (ASRS): A validated 6-item screening tool for adults used to identify the likelihood of adult ADHD.
- Clinical Observation Strategies:
- Clinic Behavior: The nurse should observe the patient's behavior in the waiting room and during the interview. Does the child climb on furniture? Does the adult interrupt the nurse or lose the thread of the conversation?
- The "One-on-One" Effect: Note that children with ADHD often perform well in the novelty of a doctor's office or a one-on-one setting. A lack of symptoms during a 20-minute office visit does not rule out ADHD.
- Neuropsychological and Cognitive Testing:
- Continuous Performance Test (CPT): A computerized task measuring sustained attention and impulsivity (omission and commission errors).
- IQ and Achievement Testing: Vital for identifying a "discrepancy" between a child's potential (IQ) and their actual academic performance.
-
Nursing Insights
- The nurse is the "Coordinator of Information." Ensure that rating scales are collected from all primary environments. If only a parent completes the form, the diagnosis is incomplete.
- Nurses must verify that the teacher completing the form has known the child for at least 2 to 3 months to ensure the observations are representative of the child's baseline.
- Be cautious of "Symptom Over-reporting" by parents seeking a specific diagnosis or "Under-reporting" by teachers who may have a very high tolerance for disruptive behavior.
-
7.3 Differential Diagnosis: Ruling Out Mimics
ADHD symptoms are non-specific; therefore, the nurse must assist the provider in ruling out "The Great Mimics" to avoid misdiagnosis.
- Physiological and Medical Mimics:
- Sleep-Disordered Breathing (SDB): Chronic hypoxia from enlarged tonsils or sleep apnea leads to daytime irritability and "brain fog" that mimics ADHD.
- Absence Seizures (Petit Mal): Brief episodes of staring and unresponsiveness can be mistaken for "inattentive" daydreaming.
- Thyroid Dysfunction: Hyperthyroidism presents with restlessness and tachycardia; Hypothyroidism presents with cognitive sluggishness.
- Iron Deficiency Anemia: Low ferritin levels are associated with restless leg symptoms and decreased cognitive focus.
- Lead Poisoning: Chronic exposure to lead (Pb) is neurotoxic to the prefrontal cortex, causing permanent deficits in impulse control.
- Psychiatric and Psychosocial Mimics:
- Anxiety Disorders: A child who is "worried" may appear inattentive because they are ruminating on fears rather than the teacher's lesson.
- Post-Traumatic Stress Disorder (PTSD): Hypervigilance and a "startle response" can be mistaken for hyperactivity.
- Bipolar Disorder: Mania involves high energy and impulsivity, but unlike the chronic, daily nature of ADHD, Bipolar symptoms occur in distinct, cyclical "episodes."
|
Condition |
Distinguishing Clinical Feature |
|
Learning Disability (LD) |
Struggle is task-specific (e.g., only with reading or math). |
|
Absence Seizures |
Sudden "stare" with lip-smacking or eyelid fluttering; no memory of the gap. |
|
Chronic Sleep Deprivation |
Symptoms resolve entirely when the child gets 10+ hours of sleep. |
|
Fetal Alcohol Syndrome |
Associated with distinct facial dysmorphology and global cognitive delay. |
Nursing Insights
- The Vision and Hearing Rule: No child should be diagnosed with ADHD until the nurse confirms a recent vision and hearing screening. A child who cannot see the board or hear instructions will invariably appear "off-task."
- The Snore Question: Always ask parents, "Does your child snore loudly or gasp for air at night?" If yes, refer to an ENT or Sleep Study before initiating stimulants.
- Trauma Screening: Always assess for "Adverse Childhood Experiences" (ACEs). Toxic stress in the home environment can over-activate the amygdala, leading to a state of constant "Fight or Flight" that perfectly mimics ADHD hyperactivity.
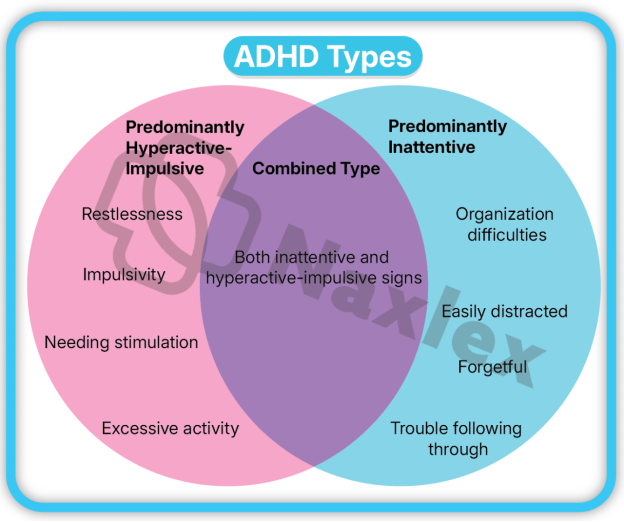
Pharmacological Interventions
- Pharmacotherapy is considered the first-line treatment for moderate to severe ADHD in school-aged children, adolescents, and adults.
- The primary goal of pharmacological intervention is to normalize the catecholaminergic neurotransmission within the prefrontal cortex and basal ganglia to enhance executive function and behavioral inhibition.
1. Stimulant Medications: Methylphenidates and Amphetamines
Stimulants are the most widely researched and frequently prescribed medications for ADHD, demonstrating a high effect size (approximately 1.0) in symptom reduction.
- Mechanism of Action (MOA):
- Methylphenidates: Block the reuptake of Dopamine (DA) and Norepinephrine (NE) by inhibiting the transport proteins (DAT and NET), thereby increasing the concentration of these neurotransmitters in the synaptic cleft.
- Amphetamines: Act as both reuptake inhibitors and "releasers." They enter the presynaptic neuron and induce the release of DA and NE from storage vesicles into the synapse, making them slightly more potent than methylphenidates.
- Classification by Duration:
- Short-Acting (Immediate Release): Effective for 3 to 5 hours (e.g., Ritalin, Focalin, Adderall IR). Requires multiple daily dosing, which can lead to "peaks and valleys" in focus and poor school-day compliance.
- Intermediate-Acting: Effective for 6 to 8 hours (e.g., Ritalin SR, Metadate ER).
- Long-Acting (Extended Release): Effective for 8 to 12+ hours (e.g., Concerta, Adderall XR, Vyvanse). These utilize sophisticated delivery systems like OROS (osmotic release) or prodrug technology to provide a steady therapeutic level.
- Common Compounds:
- Methylphenidate (MPH): Ritalin, Concerta, Daytrana (transdermal patch), Quillivant XR (liquid).
- Amphetamine Salts (AMP): Adderall, Vyvanse (Lisdexamfetamine—a prodrug that must be metabolized in the blood to become active, reducing abuse potential).
Nursing Insights
- Educate parents that stimulants are "Schedule II" controlled substances; they require a new hard-copy or secure electronic prescription every 30 days and cannot be refilled via telephone.
- For the "Daytrana" patch, teach the family to apply it to the hip 2 hours before the effect is needed and to rotate sites daily to prevent skin irritation.
- Explain the "Holiday" or "Medication Break" concept: Some providers recommend stopping stimulants during summer or school breaks to allow for "catch-up" growth, although this is debated if the child has severe social impairment.
2. Non-Stimulant Medications: Alpha-2 Agonists and SNRIs
Non-stimulants are indicated for patients who do not tolerate stimulants, have a history of substance abuse, or have comorbid conditions like Tic disorders or severe aggression.
- Selective Norepinephrine Reuptake Inhibitors (SNRIs):
- Atomoxetine (Strattera): The first non-stimulant FDA-approved for ADHD.
- MOA: Specifically inhibits the reuptake of Norepinephrine. Unlike stimulants, it is not a controlled substance and takes 2 to 4 weeks to reach full therapeutic effect.
- Alpha-2 Adrenergic Agonists:
- Guanfacine (Intuniv) and Clonidine (Kapvay):
- MOA: These were originally antihypertensives. They stimulate Alpha-2A receptors in the prefrontal cortex, strengthening the "signal" of neurotransmission to improve working memory and impulse control.
- Utility: Particularly effective for "Hyperactive-Impulsive" symptoms and for patients with co-occurring sleep disturbances or Tourette’s syndrome.
- Atomoxetine carries a "Black Box Warning" for increased suicidal ideation in children and adolescents; the nurse must monitor for mood changes and "dark" thoughts during the first month of therapy.
- Alpha-2 agonists can cause significant hypotension and bradycardia. Nurses must check blood pressure and heart rate before titration and educate parents not to discontinue these medications abruptly, as this can cause "rebound hypertension."
3. Side Effect Management and Monitoring
Effective nursing care involves the proactive identification and mitigation of adverse effects to ensure long-term treatment adherence.
- Anorexia and Weight Loss: Stimulants suppress the appetite center in the hypothalamus.
- Nursing Intervention: Monitor height and weight on a growth chart at every visit. Encourage "mechanical eating" (eating by the clock, not by hunger) and provide high-calorie, nutrient-dense "Power Breakfasts" before the medication kicks in.
- Insomnia: Especially common if long-acting stimulants are taken too late in the day.
- Nursing Intervention: Administer the dose early in the morning (e.g., 0700). Assess for "rebound" hyperactivity in the evening which may be mistaken for insomnia.
- Cardiovascular Effects: Increased heart rate and blood pressure.
- Nursing Intervention: Screen for family history of sudden cardiac death or arrhythmias. Baseline and periodic ECGs may be required for high-risk patients.
- Growth Suppression: Some studies show a temporary slowing of growth velocity in children on long-term stimulants.
- Nursing Intervention: Document growth trajectories meticulously. Most children eventually reach their predicted adult height.
- Tics and Agitation: Stimulants can unmask underlying motor tics.
- Nursing Intervention: Observe for repetitive eye-blinking, shoulder-shrugging, or throat-clearing.
|
Side Effect |
Management Strategy |
|
Appetite Suppression |
Dose after meals; offer calorie-dense snacks in the evening when the med wears off. |
|
Gastrointestinal Upset |
Administer medication with food. |
|
"Zombie-like" Affect |
Indicates the dose is too high; report to the provider for a dose reduction. |
|
Dry Mouth (Xerostomia) |
Encourage frequent sips of water or sugar-free gum (common with Atomoxetine). |
Nursing Insights
- Teach the "Concerta Ghost": In the Concerta OROS delivery system, the tablet shell may appear in the stool after the medication has been absorbed.
- Parents should be warned so they do not think the pill was not digested.
- Stimulants may lower the seizure threshold. If a patient has a known seizure disorder, the nurse must monitor for increased seizure frequency during titration.
Nursing Management And Psychosocial Interventions
- Nursing management of ADHD involves a multi-dimensional approach that extends beyond the clinical setting. The nurse acts as a liaison between the family, the school, and the medical provider, ensuring that the patient’s environment is optimized to compensate for their neurobiological deficits.
1. Behavioral Therapy and Parent Training
Behavioral therapy is the first-line recommendation for preschool-aged children (ages 4–5) before initiating medication, and it remains a core component of "Multimodal Treatment" for older children and adults.
- Principles of Behavior Modification: * Positive Reinforcement: Immediate rewards for desired behaviors (e.g., staying seated for 10 minutes).
- Token Economies: A systematic use of points or stickers that can be exchanged for larger privileges (e.g., extra screen time).
- Time-Outs/Response Cost: Consistent consequences for non-compliance or aggressive behaviors.
- Parent Management Training (PMT): * Nurses teach parents to shift from a "reactive" parenting style to a "proactive" one.
- Focus on "The 3 Cs": Clear, Concise, and Consistent commands.
- Emphasis on maintaining a highly structured daily routine (fixed times for meals, homework, and sleep).
- Social Skills Training: Group-based interventions to help the patient recognize social cues, practice turn-taking, and manage frustration without impulsivity.
Nursing Insights
- Explain to parents that behavioral therapy does not "cure" the ADHD brain; rather, it creates an "external prosthetic" for the child's missing executive functions.
- Nurses must encourage parents to "Catch the child being good." Children with ADHD receive significantly more negative feedback than their peers, which destroys self-esteem.
- The nurse should help parents identify "High-Yield Rewards." A child with ADHD has a low dopamine response; therefore, rewards must be frequent, immediate, and meaningful to be effective.
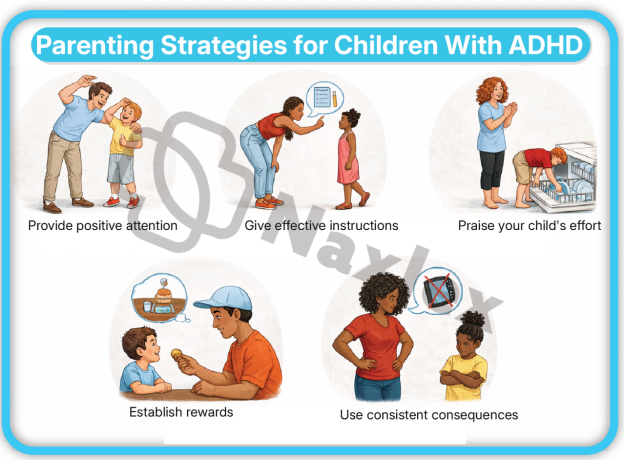
2. Classroom Management and Academic Accommodations
The school environment is often the most challenging domain for the ADHD patient due to the requirement for sustained mental effort and physical stillness.
- Environmental Restructuring:
- Preferential Seating: Seating the student near the teacher and away from high-distraction areas like windows, pencil sharpeners, or busy hallways.
- "Wiggle Room": Allowing for "planned movement breaks" (e.g., the student is assigned the job of taking a note to the office) to expend excess motor energy.
- Academic Modifications (Individualized Education Program - IEP or 504 Plan):
- Extended Time: Providing 50% to 100% more time on tests to account for slow processing and distractibility.
- Reduced Workload: Focusing on "quality over quantity" (e.g., having the student complete only every second math problem to demonstrate mastery).
- Visual Aids: Using graphic organizers, color-coded folders, and daily planners to assist with organizational deficits.
- Instructional Strategies:
- Breaking down long-term projects into "micro-goals" with individual deadlines.
- Providing written instructions to supplement verbal directions.
Nursing Insights
- The nurse should advocate for the "504 Plan" or "IEP." These are legally binding documents under the Individuals with Disabilities Education Act (IDEA).
- Advise teachers and parents to use a "Home-School Communication Log." Consistency across both environments is the strongest predictor of academic success.
- Nurses should educate school staff that ADHD is a disability of "self-regulation," not "disrespect." A child blurting out an answer is a symptom of poor impulse control, not an intentional act of defiance.
3. Nursing Process: Assessment, Nursing Diagnosis, and Interventions
The nursing process provides a systematic framework for managing the care of a patient with ADHD, focusing on safety, compliance, and functional improvement.
- Nursing Assessment:
- Subjective Data: Reports from parents/teachers regarding attention span, activity levels, and social interactions. Assessment of the patient's self-perception.
- Objective Data: Vital signs (BP/HR), height/weight growth velocity, and observation of motor activity during the exam.
- Common Nursing Diagnoses:
- Risk for Injury: Related to impulsive behaviors and lack of danger awareness.
- Impaired Social Interaction: Related to intrusiveness, inability to wait turns, and verbal impulsivity.
- Ineffective Coping (Family): Related to the chronic stress of managing a child with disruptive behavior.
- Non-compliance (Therapeutic Regimen): Related to medication side effects or forgetfulness.
- Nursing Interventions:
- Promote Safety: Instruct the family to keep medications locked away (due to stimulant abuse potential) and provide a supervised, clutter-free environment.
- Enhance Self-Esteem: Assist the child in identifying a "strength" (e.g., art, sports, or computers) to build confidence outside of academics.
- Medication Education: Teach the patient and family about the importance of morning dosing and the management of "rebound" symptoms.
|
Phase |
Nursing Action |
|
Assessment |
Check baseline BMI and EKG if indicated before starting stimulants. |
|
Planning |
Establish a "Behavior Contract" with the child with clear, attainable goals. |
|
Implementation |
Administer stimulants with or immediately after breakfast to mitigate appetite suppression. |
|
Evaluation |
Monitor the Vanderbilt Scale scores every 3–6 months to assess treatment efficacy. |
Nursing Insights
- The 1800-Rule: Stimulants should generally not be administered after 1800 (6:00 PM) to prevent severe insomnia, unless a very small "booster" dose is prescribed for evening homework.
- During follow-up appointments, always ask the child: "How do you feel on the medicine?" Listen for reports of "feeling like a robot" or "losing my personality," which indicates the dose is too high.
- For the nursing student: Remember that Safety is always the priority. If a question asks about an impulsive child running toward a street, the nursing intervention is immediate physical intervention/supervision.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on ATTENTION-DEFICIT/HYPERACTIVITY DISORDER (ADHD)
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


