Please set your exam date
Drugs Used for Degenerative Diseases of the Nervous System
Study Questions
Practice Exericse 1
The nurse is assessing a patient who has begun therapy with amantadine (Symmetrel) for Parkinson's disease. The nurse will look for which possible adverse effects? Select all that apply
Explanation
Amantadine (Symmetrel) is an antiviral agent with dopaminergic properties used in Parkinson’s disease to reduce tremors and dyskinesias. Its mechanism involves enhancing dopamine release and blocking dopamine reuptake, which helps improve motor function. While effective, amantadine is associated with several central nervous system (CNS) and gastrointestinal adverse effects that require monitoring.
Rationale for correct answers:
A. Nausea
Amantadine may cause gastrointestinal upset, including nausea, due to its effect on the GI tract and central dopaminergic pathways.
C. Dizziness
Dizziness can result from orthostatic hypotension or CNS effects of increased dopaminergic activity, particularly in older adults.
D. Insomnia
CNS stimulation from amantadine may lead to insomnia or sleep disturbances, especially if taken late in the day.
Rationale for incorrect answers:
B. Hypertension
Amantadine does not typically cause hypertension; it is more commonly associated with hypotension or CNS effects rather than direct cardiovascular stimulation.
E. Fatigue
Fatigue is not a common adverse effect; amantadine usually has stimulatory effects, which may lead to insomnia rather than tiredness.
Take-home points:
- Amantadine can cause nausea, dizziness, and insomnia, requiring patient monitoring and education.
- Hypertension and fatigue are not typical adverse effects of this medication.
- Monitoring for CNS and GI effects is important, particularly in older adults.
The healthcare provider’s order reads, “Bromocriptine (Parlodel) 10 mg per day PO.” The medication is available in B.5-mg tablets. How many tablets will the nurse give per dose?
Explanation
Bromocriptine (Parlodel) is a dopamine agonist used in the management of Parkinson’s disease, a progressive neurodegenerative disorder characterized by dopamine deficiency in the basal ganglia. By directly stimulating dopamine receptors in the brain, bromocriptine helps improve motor function, reduce rigidity, tremors, and bradykinesia, and may be used alone in early-stage Parkinson’s or in combination with levodopa in more advanced cases to enhance therapeutic effects and reduce motor fluctuations.
Rationale for correct answer:
You need to determine how many B.5-mg tablets are needed to make a single 10-mg dose.
- Identify the ordered dose: The order is for 10 mg.
- Identify the available dose: The tablets are B.5 mg each.
- Calculate the number of tablets: Divide the ordered dose by the available dose per tablet.
- 10mg÷B.5mgpertablet=4tablets
The nurse will administer 4 tablets for this dose.
Take-home points:
- Always divide the ordered dose by the available strength to calculate the correct number of tablets.
- Bromocriptine is a dopamine agonist that improves motor symptoms in Parkinson’s disease.
- Verify dosage calculations carefully to ensure safe and accurate medication administration.
A patient who has been taking carbidopa-levodopa for Parkinson's disease for over 1 year wants to start a low carbohydrate/ high-protein weight-loss diet. The nurse tells the patient that this type of diet may have what effect on his drug therapy?
Explanation
Carbidopa-levodopa (Sinemet) is the gold-standard therapy for Parkinson’s disease, working by replenishing brain dopamine levels. Levodopa is absorbed in the small intestine and crosses the blood–brain barrier using the same transport channels as dietary amino acids. For this reason, diets that are high in protein can interfere with drug absorption and reduce its therapeutic effect. Nutritional counseling is essential to maximize the drug’s benefit.
Rationale for correct answer:
B. The high-protein diet can slow or prevent absorption of this medication
High-protein foods are rich in amino acids, which compete with levodopa for absorption in the gastrointestinal tract and for transport across the blood–brain barrier. This results in lower drug levels reaching the brain, leading to reduced symptom control. Patients may experience “off” periods with worsening tremors, rigidity, and bradykinesia when protein intake is high.
Rationale for incorrect answers:
A. There will be no problems with this diet while on this medication
This is incorrect because there is a well-established interaction between dietary protein and levodopa absorption. A high-protein diet almost always reduces effectiveness of the drug.
C. The high-protein diet may cause increased blood levels of this medication
The opposite is true—protein competes with levodopa, lowering rather than raising its absorption and blood levels.
D. The high-protein diet will cause no problems as long as the patient also takes pyridoxine (vitamin B6)
Vitamin B6 is relevant for levodopa without carbidopa, because it increases peripheral metabolism of levodopa. However, carbidopa prevents this breakdown, making pyridoxine less of a concern. Protein intake, not vitamin B6, is the major dietary issue here.
Take-home points:
- High-protein diets interfere with levodopa absorption, reducing its effectiveness in controlling Parkinson’s symptoms.
- Levodopa competes with amino acids for absorption and brain transport, causing “off” periods when protein intake is high.
- Clients should be counseled to spread protein intake throughout the day, rather than consuming large amounts with medication doses.
A patient requested an appointment with their healthcare provider to discuss the possibility that they were developing Parkinson disease, which runs in the family.
The nurse explained to the patient in the scenario that the symptoms of Parkinson disease are related to the levels of neurotransmitters in the brain and used which statement?
Explanation
Parkinson’s disease is a chronic, progressive neurodegenerative disorder characterized by motor symptoms such as tremors, rigidity, bradykinesia, and postural instability. It results from the degeneration of dopaminergic neurons in the substantia nigra of the brain. This loss of dopamine disrupts the delicate balance between dopamine and acetylcholine, two key neurotransmitters that regulate voluntary motor control.
Rationale for correct answer:
B. “Parkinson disease is related to an excess of acetylcholine and a deficiency of dopamine.”
In Parkinson’s disease, degeneration of dopaminergic neurons leads to a deficiency of dopamine. With less dopamine available, acetylcholine’s excitatory effects become unopposed, creating an imbalance. This imbalance between decreased dopamine (inhibitory) and relatively increased acetylcholine (excitatory) is the root cause of the motor symptoms seen in Parkinson’s disease.
Rationale for incorrect answers:
A. “Parkinson disease is related to an excess of serotonin and a deficiency of dopamine.”
Serotonin is involved in mood regulation, not in the pathophysiology of Parkinson’s motor symptoms. While depression may coexist with Parkinson’s, serotonin imbalance is not the primary issue.
C. “Parkinson disease is related to an excess of dopamine and a deficiency of acetylcholine.”
This is incorrect because Parkinson’s is marked by too little dopamine, not an excess. Increased dopamine is more characteristic of conditions like schizophrenia, not Parkinson’s disease.
D. “Parkinson disease is related to an excess of epinephrine and a deficiency of acetylcholine.”
Epinephrine primarily regulates cardiovascular responses and the fight-or-flight reaction. It is not a central neurotransmitter in Parkinson’s disease pathology.
Take-home points:
- Parkinson’s disease involves a deficiency of dopamine due to degeneration of substantia nigra neurons.
- The dopamine–acetylcholine imbalance causes the hallmark motor symptoms of the disease.
- Patient education should emphasize how drug therapies (dopaminergic drugs or anticholinergics) aim to restore this neurotransmitter balance.
A patient requested an appointment with their healthcare provider to discuss the possibility that they were developing Parkinson disease, which runs in the family.
The patient in the scenario was started on selegiline (Zelapar) therapy during the early treatment of Parkinson disease because this drug will have which effect?
Explanation
Selegiline (Zelapar) is a selective monoamine oxidase B (MAO-B) inhibitor used in the early stages of Parkinson’s disease. Its primary purpose is to enhance and prolong the effects of endogenous dopamine in the basal ganglia, improving motor function. By inhibiting MAO-B, selegiline slows the breakdown of dopamine, helping to maintain higher dopamine levels and reduce motor symptoms. Understanding its mechanism is essential for safe administration and patient education.
Rationale for correct answer:
C. Reduce the metabolism of dopamine
Selegiline selectively inhibits the MAO-B enzyme responsible for metabolizing dopamine in the brain. By decreasing dopamine breakdown, more dopamine remains available at synapses, which helps alleviate motor symptoms such as bradykinesia, rigidity, and tremors. This effect is particularly useful in the early stages of Parkinson’s disease or as an adjunct to levodopa therapy.
Rationale for incorrect answers:
A. Reduce excessive acetylcholine
Selegiline does not directly affect acetylcholine levels. Anticholinergic drugs, not MAO-B inhibitors, are used to counteract the relative excess of acetylcholine in Parkinson’s disease.
B. Decrease dopamine in the basal ganglia
This is incorrect because selegiline increases, not decreases, dopamine availability by slowing its breakdown.
D. Reduce the metabolism of levodopa, thereby making more available
Selegiline does not directly affect levodopa metabolism. It works on endogenous dopamine rather than levodopa. COMT inhibitors, like entacapone, affect levodopa metabolism.
Take-home points:
- Selegiline inhibits MAO-B, slowing dopamine metabolism and enhancing dopamine availability.
- It is useful in early Parkinson’s or as adjunct therapy to levodopa.
- It does not affect acetylcholine levels or levodopa metabolism directly.
- Monitoring for insomnia, hallucinations, or interactions with other serotonergic drugs is important during therapy.
Patient Scenario:
A patient requested an appointment with their healthcare provider to discuss the possibility that they were developing Parkinson disease, which runs in the family.
Choose the most likely option for the information missing from the following sentence by selecting from the list of options provided.
The nurse explains to the patient in the scenario that in the future the healthcare provider may start
Explanation
The nurse explains to the patient in the scenario that in the future the healthcare provider may start Rasagiline therapy in addition to Amantadine hydrochloride which is part of the drug class Monoamine oxidase type B inhibitors and Dopamine agonists , respectively.
Parkinson disease is a progressive neurodegenerative disorder characterized by motor symptoms such as tremors, rigidity, bradykinesia, and postural instability. Because dopamine deficiency is central to the disease process, treatment strategies often focus on enhancing dopamine activity or mimicking its effects.
Rationale for the correct answers:
Rasagiline is a MAO-B inhibitor that slows the breakdown of dopamine, helping increase and prolong dopamine activity in the brain.
Amantadine hydrochloride is classified as a dopamine agonist, which helps stimulate dopamine receptors and reduce motor symptoms like tremors and rigidity.
This combination may be used in early or adjunctive therapy in Parkinson disease to enhance dopamine levels and improve motor control without immediately relying on carbidopa-levodopa.
Take-home Points:
- MAO-B inhibitors (e.g., rasagiline) slow dopamine breakdown, preserving natural dopamine.
- Dopamine agonists (e.g., amantadine) directly stimulate dopamine receptors to improve symptoms.
- Early initiation of these therapies can delay the need for carbidopa-levodopa and help manage Parkinson disease progression.
A patient requested an appointment with their healthcare provider to discuss the possibility that they were developing Parkinson disease, which runs in the family.
The nurse knows that when anticholinergic agents are used, which of the following symptoms will show improvement? Select all that apply
Explanation
Anticholinergic agents, such as benztropine (Cogentin) and trihexyphenidyl, are used in Parkinson’s disease to reduce the effects of excess acetylcholine in the basal ganglia. Parkinson’s disease involves an imbalance between dopamine (deficient) and acetylcholine (relatively excessive), contributing to motor symptoms. By blocking acetylcholine, anticholinergic drugs help restore neurotransmitter balance, particularly improving tremors, rigidity, and salivation issues, while having minimal effect on bradykinesia.
Rationale for correct answers:
A. Tremors
Tremors in Parkinson’s are partly caused by excessive cholinergic activity. Anticholinergic agents reduce this activity, helping to control involuntary shaking, especially at rest.
B. Drooling
Drooling results from increased salivary secretion due to cholinergic overactivity. Anticholinergic drugs reduce saliva production, improving drooling.
E. Rigidity
Muscle rigidity is linked to cholinergic overactivity in the basal ganglia. Anticholinergic agents help relax muscles and improve stiffness.
Rationale for incorrect answers:
C. Cognition impairment
Anticholinergic drugs can actually worsen cognitive function, especially in older adults, because acetylcholine is critical for memory and learning.
D. Bradykinesia
Bradykinesia, or slowness of movement, is primarily due to dopamine deficiency, and anticholinergics have minimal impact on improving this symptom.
Take-home points:
- Anticholinergics improve tremors, drooling, and rigidity in Parkinson’s disease.
- Bradykinesia and cognitive function are not significantly improved; caution is needed in older adults.
- These drugs work by restoring the dopamine-acetylcholine balance in the basal ganglia.
A patient requested an appointment with their healthcare provider to discuss the possibility that they were developing Parkinson disease, which runs in the family.
The nurse is educating the family of an elderly patient on the mechanism of action for donepezil (Aricept). Which statement by the family indicates that further teaching is needed?
Explanation
Donepezil (Aricept) is a cholinesterase inhibitor used in the management of mild to moderate Alzheimer’s disease. It works by inhibiting the enzyme acetylcholinesterase, which breaks down acetylcholine in the brain. This increases the availability of acetylcholine, a neurotransmitter important for memory and cognition. Donepezil improves symptoms but does not stop or reverse neurodegeneration caused by Alzheimer’s disease.
Rationale for correct answer:
D. “As I understand it, this medication will slow the progress of the neurodegeneration caused by Alzheimer disease.”
This statement is incorrect because donepezil does not slow the underlying neurodegeneration; it temporarily improves cognitive function by increasing acetylcholine levels but cannot alter disease progression.
Rationale for incorrect answers:
A. “This drug will improve the cognitive skills of my dad.”
Correct. Donepezil can improve memory, attention, and cognitive function in patients with Alzheimer’s disease.
B. “This drug is used in patients with mild to moderate dementia caused by Alzheimer disease.”
Correct. Donepezil is indicated for mild to moderate stages of Alzheimer’s disease.
C. “The enzyme that normally breaks down acetylcholine is inhibited by this medication.”
Correct. Donepezil inhibits acetylcholinesterase, preventing breakdown of acetylcholine and enhancing cholinergic transmission.
Take-home points:
- Donepezil improves cognition and daily functioning, but does not slow the underlying neurodegeneration.
- It works by inhibiting acetylcholinesterase, increasing acetylcholine availability in the brain.
- Education should focus on symptom management, not disease modification.
Practice Exercise 2
The nurse has initiated teaching for a family member of a patient with Alzheimer’s disease. The nurse realizes more teaching is needed if the family member makes which statement?
Explanation
Alzheimer’s disease is a progressive neurodegenerative disorder characterized by memory loss, personality changes, and cognitive decline. While medications such as cholinesterase inhibitors and NMDA receptor antagonists can help manage symptoms, there is currently no cure. Family education is essential to set realistic expectations and support long-term care planning.
Rationale for correct answer:
D. It may take several medications to cure the disease
This statement reflects a misunderstanding, since Alzheimer’s disease cannot be cured. Medications only slow symptom progression and improve quality of life but do not reverse or eliminate the disease. Believing there is a cure may lead to false hope and frustration, making this a teaching priority for the nurse.
Rationale for incorrect answers:
A. As the disease gets worse, the memory loss will get worse
Alzheimer’s disease is marked by progressive memory impairment, worsening as the disease advances.
B. There are several theories about the cause of the disease
Proposed causes include genetic factors, amyloid plaques, neurofibrillary tangles, and neurotransmitter imbalances.
C. Personality changes and hostility may occur
Behavioral changes, including irritability, aggression, and mood swings, are common as the disease progresses.
Take-home points:
- Alzheimer’s disease has no cure; treatments only manage symptoms.
- Memory loss, personality changes, and hostility are expected as the condition advances.
- Clear family education is essential to set realistic expectations and reduce caregiver frustration.
A patient is taking rivastigmine (Exelon). The nurse should teach the patient and family which information about rivastigmine?
Explanation
Rivastigmine (Exelon) is a cholinesterase inhibitor prescribed for mild to moderate Alzheimer’s disease and Parkinson’s dementia. By increasing acetylcholine levels in the brain, it helps improve memory, cognition, and functional ability. However, the same cholinergic action is responsible for frequent gastrointestinal side effects.
Rationale for correct answer:
C. That GI distress is a common side effect
Rivastigmine often causes nausea, vomiting, diarrhea, and decreased appetite due to increased cholinergic stimulation in the digestive tract. These effects are most pronounced during initiation or dose escalation. Administering the drug with food may help reduce discomfort.
Rationale for incorrect answers:
A. That hepatotoxicity may occur
Rivastigmine does not carry a risk of hepatotoxicity. This adverse effect is linked to other cholinesterase inhibitors such as tacrine, not rivastigmine.
B. That the initial dose is 6 mg t.i.d.
Rivastigmine should be started at A.5 mg twice daily, with gradual titration. Starting at 6 mg three times daily would be unsafe and increase the risk of severe side effects.
D. That weight gain may be a side effect
Rivastigmine is more often associated with weight loss, not weight gain, due to appetite suppression and GI distress.
Take-home points:
- GI distress is the most common adverse effect of rivastigmine.
- Dosing begins low and is titrated gradually to minimize side effects.
- Rivastigmine does not cause hepatotoxicity or weight gain.
A patient is taking rivastigmine (Exelon) to improve cognitive function. What should the nurse teach the patient/ family member to do? Select all that apply
Explanation
Rivastigmine (Exelon) is a cholinesterase inhibitor used in the management of Alzheimer’s disease and Parkinson’s dementia. By increasing acetylcholine levels in the brain, it can improve memory and cognition. However, it also carries risks such as orthostatic hypotension, dizziness, and falls, making patient and caregiver education critical for safety.
Rationale for correct answers:
A. Rise slowly to avoid dizziness
Rivastigmine can cause orthostatic hypotension and dizziness, increasing the risk of falls. Patients should be instructed to change positions slowly to reduce this risk.
B. Remove obstacles from pathways to avoid injury
Cognitive decline combined with dizziness places patients at high fall risk. Keeping walkways clear and using safety measures in the home environment helps prevent accidents.
C. Closely follow the drug dosing schedule
Rivastigmine requires strict adherence to the prescribed dosing schedule to maintain steady therapeutic levels and minimize side effects. Skipping or doubling doses can increase adverse effects or reduce drug effectiveness.
Rationale for incorrect answers:
D. Have frequent checks for hypertension
Rivastigmine is more commonly associated with hypotension, not hypertension. Monitoring for dizziness and low blood pressure is more relevant.
E. Receive regular liver function tests
Rivastigmine does not cause hepatotoxicity. Liver function monitoring was necessary with older agents like tacrine, but not with rivastigmine.
Take-home points:
- Orthostatic hypotension and dizziness are common, so patients should rise slowly.
- Environmental safety (removing obstacles) is crucial to reduce fall risk.
- Strict dosing adherence is needed for effectiveness and to minimize side effects.
Which of the following are major disadvantages to the use of tacrine? Select all that apply
Explanation
Tacrine (Cognex) was the first cholinesterase inhibitor approved for the treatment of Alzheimer’s disease, designed to improve cognitive function by increasing acetylcholine in the brain. However, its use declined significantly due to its serious side effects and inconvenient dosing schedule. Understanding these disadvantages helps nurses educate clients and caregivers about medication safety and adherence.
Rationale for correct answers:
A. It must be administered four times per day.
Tacrine requires frequent dosing (QID), which decreases adherence and makes it impractical for many clients, especially elderly patients with cognitive impairment who may struggle with complex regimens.
D. It may cause serious hepatic damage.
One of the most serious adverse effects of tacrine is hepatotoxicity, requiring frequent monitoring of liver function tests (LFTs). This risk led to its decline in use compared to newer cholinesterase inhibitors (e.g., donepezil, rivastigmine, galantamine), which have safer profiles.
Rationale for incorrect answers:
B. It causes weight gain.
Tacrine is not associated with weight gain; common side effects are more often related to the gastrointestinal system (e.g., nausea, vomiting, diarrhea).
C. It may cause vision difficulties.
Tacrine does not directly cause vision changes or ocular complications. This option may confuse it with other neuro or ophthalmic medications.
E. It may be purchased over the counter.
Tacrine is a prescription-only drug due to its risks and need for monitoring. It is not available over the counter.
Take-home points:
- Tacrine has limited use today due to frequent dosing requirements and serious liver toxicity.
- Safer alternatives like donepezil are now preferred in Alzheimer’s management.
- Nurses should monitor liver function tests closely if tacrine is prescribed.
A patient with Alzheimer’s disease is prescribed both rivastigmine and memantine. What is the primary rationale for this combination therapy?
Explanation
Combination therapy with rivastigmine (a cholinesterase inhibitor) and memantine (an NMDA receptor antagonist) is commonly used in moderate to severe Alzheimer’s disease. Rivastigmine increases acetylcholine availability to improve neurotransmission, while memantine reduces glutamate-induced excitotoxicity, protecting neurons from further damage. This complementary action addresses different pathological mechanisms of the disease to slow progression and improve cognitive function.
Rationale for correct answer:
B. To reduce excitotoxic neuronal damage while enhancing neurotransmission
Rivastigmine enhances cholinergic signaling, improving memory, attention, and cognition. Memantine blocks excessive NMDA receptor activity, preventing neuronal damage from glutamate excitotoxicity. Together, they target both neurotransmitter deficits and neurodegeneration, providing synergistic benefits in Alzheimer’s disease management.
Rationale for incorrect answers:
A. To completely cure Alzheimer’s disease
There is currently no cure for Alzheimer’s disease; medications slow progression and manage symptoms, but do not eliminate the disease.
C. To prevent cardiovascular side effects such as bradycardia and hypotension
Cardiovascular effects are possible adverse reactions of cholinesterase inhibitors but are not the primary reason for this combination therapy.
D. To immediately reverse cognitive deficits and memory loss
These medications improve cognition gradually; they do not produce immediate reversal of deficits.
Take-home points:
- Rivastigmine and memantine combination therapy enhances neurotransmission and protects neurons from excitotoxic damage.
- The goal is to slow progression and improve cognitive function, not cure Alzheimer’s disease.
- Immediate reversal of memory loss or cardiovascular protection are not primary benefits of this therapy.
Practice Exercise 3
The nurse discusses the disease process of multiple sclerosis with the client and caregiver. The client will begin taking glatiramer acetate (Copaxone), and the nurse is teaching the client about the drug. Which of the following points should be included?
Explanation
Multiple sclerosis (MS) is a chronic autoimmune disorder that damages the myelin sheath of the central nervous system, leading to progressive physical and cognitive impairment. Glatiramer acetate (Copaxone) is a disease-modifying therapy that helps reduce the frequency of relapses in MS by modifying the immune response. Teaching the client about its common effects and correct administration is vital for adherence and safe use.
Rationale for correct answer:
B. Local injection site irritation is a common effect.
Glatiramer acetate is given by subcutaneous injection, and the most common side effects include injection site reactions such as redness, pain, swelling, or itching. Clients should rotate injection sites and use proper technique to minimize irritation and prevent complications like lipoatrophy.
Rationale for incorrect answers:
A. Drink extra fluids while this drug is given.
Increased fluid intake is not required for glatiramer acetate therapy. Hydration does not influence the drug’s effectiveness or safety.
C. Take the drug with plenty of water and remain in an upright position for at least 30 minutes.
This teaching applies to oral bisphosphonates (e.g., alendronate) to prevent esophageal irritation, not to subcutaneous injections like glatiramer acetate.
D. The drug causes a loss of vitamin C so include extra citrus and foods containing vitamin C in the diet.
Glatiramer acetate does not deplete vitamin C, and no dietary supplementation is needed.
E. A client who has not responded well to other drug therapy for Alzheimer’s disease is placed on tacrine (Cognex).
This statement is unrelated and refers to Alzheimer’s disease treatment, not MS or glatiramer acetate. Including it here indicates a need for teaching clarification.
Take-home points:
- Injection site irritation is the most common side effect of glatiramer acetate.
- Clients should rotate subcutaneous injection sites to minimize skin reactions.
- Teaching should focus only on relevant drug effects and safe administration techniques.
Which oral disease-modifying therapy for MS requires strict pregnancy precautions due to teratogenicity?
Explanation
Teriflunomide (Aubagio) is an oral disease-modifying therapy for multiple sclerosis (MS) that works by inhibiting pyrimidine synthesis, reducing the proliferation of activated T and B lymphocytes. While effective in slowing MS progression, teriflunomide is highly teratogenic, requiring strict pregnancy precautions and reliable contraception for both women and men during treatment and until drug elimination is confirmed.
Rationale for correct answer:
C. Teriflunomide
- Teriflunomide is teratogenic and embryotoxic, associated with fetal malformations if taken during pregnancy.
- Pregnancy prevention programs are mandatory for patients of reproductive potential.
- If pregnancy occurs, accelerated elimination procedures using cholestyramine or activated charcoal may be required to reduce drug levels quickly.
Rationale for incorrect answers:
A. Fingolimod
- Fingolimod can also pose risks in pregnancy, but it is not the primary oral MS drug associated with strict teratogenic precautions; contraception is recommended, and it is contraindicated in pregnancy.
B. Dimethyl fumarate
- Dimethyl fumarate has limited human data but is not classified as highly teratogenic, though use is generally avoided in pregnancy.
D. Glatiramer acetate
- Glatiramer acetate is considered safe in pregnancy, with no known teratogenic effects.
Take-home points:
- Teriflunomide requires strict pregnancy precautions due to its teratogenic potential.
- Effective contraception and drug elimination protocols are critical for patients planning pregnancy.
- Other oral MS therapies may have pregnancy considerations, but teriflunomide carries the highest risk.
Comprehensive Questions
A nurse is providing information about pramipexole (Mirapex) to a client who has early Parkinson’s disease. Which of the following possible adverse effects should the nurse include in the information?
Explanation
Pramipexole (Mirapex) is a dopamine agonist commonly prescribed in the early stages of Parkinson’s disease to help reduce motor symptoms such as tremors, rigidity, and bradykinesia. While effective, dopamine agonists are associated with significant neuropsychiatric side effects, particularly due to overstimulation of dopamine receptors in the brain.
Rationale for correct answer:
A. Hallucinations
Pramipexole can cause hallucinations, especially in older adults, because it increases dopamine activity in the mesolimbic pathway. This overstimulation can lead to visual or auditory perceptual disturbances, which may worsen with higher doses or in clients with a history of cognitive impairment.
Rationale for incorrect answers:
B. Memory loss
While Parkinson’s disease itself may contribute to cognitive decline, memory loss is not a common adverse effect of pramipexole. The drug primarily affects motor and perceptual pathways rather than memory functions.
C. Diarrhea
Pramipexole is more commonly associated with nausea, orthostatic hypotension, and drowsiness, not diarrhea. Gastrointestinal upset may occur but diarrhea is not a recognized adverse effect requiring teaching.
D. Discoloration of urine
Urine discoloration is linked with drugs such as levodopa, not dopamine agonists like pramipexole. Therefore, this is not an expected effect for this medication.
Take-home points:
- Pramipexole may cause hallucinations due to increased dopamine activity in the brain.
- Memory loss, diarrhea, and urine discoloration are not typical adverse effects of pramipexole.
- Careful monitoring is important, especially in older adults who are more vulnerable to neuropsychiatric side effects.
A nurse is reviewing food interactions with a client who is taking levodopa/carbidopa (Sinemet) for Parkinson’s disease. Which of the following instructions should the nurse include?
Explanation
Levodopa/carbidopa (Sinemet) is the cornerstone therapy for Parkinson’s disease, helping to restore dopamine in the brain and improve motor function. Because levodopa is absorbed in the small intestine and competes with dietary proteins and certain foods, clients must be educated on food-drug interactions to optimize effectiveness and reduce symptom fluctuations.
Rationale for correct answer:
D. May take the medication crushed in apple juice
Levodopa/carbidopa tablets can be crushed and mixed with a non-protein food or drink, such as apple juice, to aid swallowing without affecting drug absorption. This method ensures medication bioavailability and is safe for clients who may have difficulty swallowing whole tablets.
Rationale for incorrect answers:
A. Eat large amounts of protein-rich foods with the medication
High-protein foods interfere with levodopa absorption because amino acids compete with the drug for transport across the intestinal wall and blood-brain barrier, reducing its therapeutic effect.
B. May take the medication with whole-grain cereal
Whole-grain cereal contains pyridoxine (vitamin B6), which enhances peripheral breakdown of levodopa, making it less available to the brain and decreasing its effectiveness.
C. Consider eating a banana with the medication
Bananas also contain vitamin B6, which can reduce the therapeutic effect of levodopa if consumed in significant amounts. This interaction makes bananas unsuitable to take alongside the medication.
Take-home points:
- Levodopa absorption is reduced by protein-rich foods and vitamin B6–containing foods such as bananas and cereals.
- Apple juice is safe for administering crushed levodopa/carbidopa, ensuring effectiveness.
- Dietary education is essential for clients on Sinemet to maximize drug benefit and reduce symptom fluctuations.
Which of the following assessment findings could the nurse see in a patient with parkinsonism? Select all that apply
Explanation
Parkinsonism is a neurologic syndrome characterized by motor symptoms that result from dopamine deficiency in the basal ganglia. Classic features include muscle rigidity, resting tremors, and bradykinesia. These hallmark findings are essential for diagnosis and guide both pharmacologic and non-pharmacologic management.
Rationale for correct answers:
B. Muscle rigidity
One of the cardinal features of parkinsonism, rigidity is caused by increased muscle tone leading to stiffness and resistance to movement. It contributes to the “cogwheel” phenomenon often noted during passive movement of the limbs.
C. Involuntary tremors
A resting tremor (“pill-rolling” motion of the fingers) is another hallmark symptom. These tremors often improve with voluntary activity but worsen with stress or fatigue.
D. Bradykinesia
This refers to slowness of voluntary movement and difficulty initiating actions, making routine activities such as walking, eating, or dressing challenging. Bradykinesia significantly contributes to disability in Parkinson’s disease.
Rationale for incorrect answers:
A. An abrupt onset of symptoms
Parkinsonism develops gradually and progressively, not abruptly. An acute onset would suggest another neurologic condition, such as stroke.
E. Bilateral muscle weakness
Weakness is not a typical feature of parkinsonism. The condition involves motor control deficits rather than true muscle weakness.
Take-home points:
- Rigidity, tremors, and bradykinesia are the cardinal features of parkinsonism.
- Symptoms develop gradually, not suddenly.
- Weakness is not characteristic of parkinsonism; motor control, not muscle strength, is impaired.
this drug?
Explanation
Carbidopa-levodopa is the gold standard treatment for Parkinson’s disease, as it restores dopamine levels in the brain. However, both dopaminergic drugs and anticholinergics used in Parkinson’s management carry important contraindications and side effects.
Rationale for correct answer:
D. Dopaminergics and anticholinergics are contraindicated in patients with glaucoma
Anticholinergic drugs can increase intraocular pressure by blocking parasympathetic stimulation in the eye. In patients with glaucoma, this can worsen the condition and lead to vision loss.
Rationale for incorrect answers:
A. Carbidopa-levodopa may lead to hypertension
Carbidopa-levodopa is more commonly associated with orthostatic hypotension, not hypertension. Blood pressure monitoring is still important, but hypertension is not the expected effect.
B. Carbidopa-levodopa may lead to excessive salivation
This drug more often causes dry mouth (xerostomia) rather than excessive salivation. Drooling can occur as a symptom of Parkinson’s itself, not as a direct effect of the medication.
C. Dopaminergic and anticholinergic therapy may lead to drowsiness and sedation
Dopaminergics may cause dyskinesia, nausea, and orthostatic hypotension, while anticholinergics can cause dry mouth, blurred vision, and constipation. Drowsiness or sedation is not a defining adverse effect for these medications.
Take-home points:
- Glaucoma is a contraindication for dopaminergic and anticholinergic Parkinson’s drugs.
- Carbidopa-levodopa is more likely to cause orthostatic hypotension, not hypertension.
- Dry mouth, not excessive salivation, is a common effect of anticholinergic therapy.
Which is a nursing intervention for a patient taking carbidopa-levodopa for parkinsonism?
Explanation
Carbidopa-levodopa is a dopaminergic combination drug used to manage symptoms of Parkinson’s disease by restoring dopamine levels in the brain. While highly effective, it has several important side effects and nursing considerations. Patient education is essential to help clients recognize expected effects, avoid harmful interactions, and maintain adherence to therapy.
Rationale for correct answer:
B. Inform the patient that perspiration may be dark and stain clothing
Carbidopa-levodopa can cause dark discoloration of body fluids such as urine, saliva, and sweat. This is a harmless but sometimes distressing side effect. The nurse should reassure the patient about this possibility and explain that while staining of clothing may occur, it is not dangerous.
Rationale for incorrect answers:
A. Encourage the patient to adhere to a high-protein diet
A high-protein diet interferes with levodopa absorption, since amino acids compete with the drug for transport across the intestinal lining and blood-brain barrier. Protein intake should be balanced and timed away from medication doses.
C. Advise the patient that glucose levels should be checked with urine testing
Blood glucose should be monitored using blood testing, not urine testing, for accuracy. This is not a primary nursing intervention related to carbidopa-levodopa.
D. Warn the patient that it may take 4 to 5 days before symptoms are controlled
Carbidopa-levodopa generally takes weeks, not days, to achieve therapeutic effects. Telling the patient 4–5 days could create false expectations and frustration.
Take-home points:
- Carbidopa-levodopa can cause dark discoloration of urine, saliva, and sweat, which may stain clothing but is harmless.
- Protein-rich foods interfere with levodopa absorption and should be timed carefully.
- Symptom control usually takes weeks, not just a few days, after starting therapy.
What would the nurse teach a patient who is taking anticholinergic therapy for parkinsonism? Select all that apply
Explanation
Anticholinergic drugs are sometimes used in the management of parkinsonism, especially for reducing tremors and rigidity. These medications work by blocking acetylcholine, thereby restoring the balance between dopamine and acetylcholine in the brain. However, they also produce peripheral anticholinergic side effects, which require careful patient education to ensure safety and comfort.
Rationale for correct answers:
A. Avoid alcohol, cigarettes, and caffeine
These substances can increase gastric acidity and decrease medication effectiveness. They may also worsen restlessness, anxiety, or insomnia in patients taking anticholinergics.
B. Relieve dry mouth with hard candy or ice chips
Dry mouth (xerostomia) is a common anticholinergic side effect due to decreased salivary secretions. Sucking on sugar-free candy, ice chips, or chewing gum helps provide relief.
C. Use sunglasses to reduce photophobia
Anticholinergics can cause pupil dilation and blurred vision, leading to light sensitivity. Sunglasses help minimize discomfort and protect the eyes.
E. Receive routine eye examinations
Anticholinergics may increase intraocular pressure, making glaucoma a concern. Regular ophthalmologic evaluations are important for early detection and prevention of vision complications.
Rationale for incorrect answer:
D. Urinate 2 hours after taking the drug
Anticholinergics can cause urinary retention, not increased urination. The nurse should teach the patient to report difficulty voiding rather than scheduling urination after doses.
Take-home points:
- Lifestyle adjustments (avoiding alcohol, caffeine, and smoking) help improve tolerance to anticholinergics.
- Dry mouth and photophobia are common side effects, manageable with simple interventions.
- Routine eye exams are essential because of the risk of increased intraocular pressure and glaucoma.
Which of the following client statements indicates that the levodopa/carbidopa (Sinemet) is effective?
Explanation
Levodopa/carbidopa (Sinemet) is a dopaminergic medication used in the treatment of Parkinson’s disease. Levodopa is converted into dopamine in the brain, while carbidopa prevents its premature breakdown in the periphery, allowing more dopamine to reach the central nervous system. The primary goal of this therapy is to improve motor function and independence in activities of daily living (ADLs).
Rationale for correct answer:
C. “I’m able to shower by myself.”
This statement indicates that the medication has improved the client’s mobility, coordination, and ability to perform self-care activities. Regaining independence in ADLs is a key measure of effectiveness in Parkinson’s treatment.
Rationale for incorrect answers:
A. “I’m sleeping a lot more, especially during the day.”
Daytime sleepiness is a side effect, not a sign of therapeutic effectiveness. Levodopa/carbidopa may actually cause drowsiness in some clients.
B. “My appetite has improved.”
While appetite changes can occur with improved well-being, increased appetite is not a primary goal or indicator of drug effectiveness in Parkinson’s disease.
D. “My skin doesn’t itch anymore.”
Resolution of itching is unrelated to the therapeutic purpose of levodopa/carbidopa. This symptom is not typically connected with Parkinson’s disease or Sinemet treatment.
Take-home points:
- Improved motor function and independence in ADLs are the best indicators of Sinemet’s effectiveness.
- Daytime sleepiness is a common side effect, not a therapeutic goal.
- Improvements unrelated to movement (like appetite or itching) are not valid measures of drug effectiveness.
The client asks what can be expected from the levodopa/ carbidopa (Sinemet) he is taking for treatment of parkinsonism. What is the best response by the nurse?
Explanation
Levodopa/carbidopa (Sinemet) is the cornerstone therapy for Parkinson’s disease. While it does not cure or halt disease progression, it effectively reduces symptoms such as rigidity, tremors, and bradykinesia, enabling patients to regain independence in daily living activities. Patient teaching must set realistic expectations to promote adherence and prevent disappointment.
Rationale for correct answer:
B. “Symptoms can be reduced and the ability to perform ADLs can be improved.”
This response accurately describes the purpose of Sinemet therapy. By restoring dopamine levels in the brain, it improves motor control, reduces symptoms, and enhances quality of life, especially in terms of performing activities of daily living (ADLs).
Rationale for incorrect answers:
A. “A cure can be expected within 6 months.”
Parkinson’s disease is chronic and progressive. Sinemet manages symptoms but does not cure the disease.
C. “Disease progression will be stopped.”
Sinemet does not slow or halt disease progression. The neurodegenerative process continues despite symptom control.
D. “EPS will be prevented.”
Extrapyramidal symptoms (EPS) are typically associated with antipsychotic medications, not Parkinson’s itself. Sinemet does not serve to prevent EPS but rather treats the movement symptoms of Parkinson’s disease.
Take-home points:
- Sinemet reduces symptoms and improves ADLs, but it is not a cure.
- The disease continues to progress despite treatment.
- Client teaching should emphasize realistic expectations to support adherence.
Levodopa (Larodopa) is prescribed for a client with Parkinson’s disease. At discharge, which of the following teaching points should the nurse include?
Explanation
Levodopa (Larodopa) is a dopamine precursor used to manage motor symptoms of Parkinson’s disease. Because dietary proteins compete with levodopa for absorption in the small intestine and across the blood–brain barrier, proper administration is crucial to maximize effectiveness. Patient teaching at discharge should therefore emphasize timing with meals, safe monitoring, and correct dosage practices.
Rationale for correct answer:
C. Take the pill on an empty stomach or 2 hours after a meal containing protein.
High-protein meals interfere with the absorption and transport of levodopa, reducing its therapeutic effect. Taking it on an empty stomach or separating it from protein-rich meals improves bioavailability and symptom control. This teaching is key to ensuring consistent and optimal drug effectiveness.
Rationale for incorrect answers:
A. Monitor blood pressure every 2 hours for the first 2 weeks.
While levodopa may cause orthostatic hypotension, routine home monitoring every 2 hours is impractical and unnecessary. Clients should instead be taught to rise slowly and report persistent dizziness or fainting.
B. Report the development of diarrhea.
Diarrhea is not a typical adverse effect of levodopa. More common side effects include nausea, vomiting, dyskinesia, and hypotension.
D. If tremors seem to worsen, take a double dose for two doses and call the provider.
Doubling the dose can lead to toxicity, severe dyskinesias, and cardiovascular complications. Clients should never self-adjust the dosage without medical guidance.
Take-home points:
- Separate levodopa from protein-rich meals to improve absorption and effectiveness.
- Teach clients about orthostatic hypotension but avoid unrealistic home monitoring expectations.
- Clients should never change their dose independently; adjustments must be made by the provider.
An early sign(s) of levodopa toxicity is (are) which of the following?
Explanation
Levodopa is a cornerstone treatment for Parkinson’s disease, as it restores dopamine balance in the brain and improves motor function. However, with long-term therapy or higher doses, patients are at risk of developing toxicity. Recognizing the early signs of levodopa toxicity allows timely adjustment of the drug regimen to prevent complications.
Rationale for correct answer:
C. Spasmodic eye winking and muscle twitching.
Early signs of levodopa toxicity include involuntary movements (dyskinesias) such as spasmodic eye winking, facial grimacing, or muscle twitching. These occur because of excess dopamine activity in the brain. Identifying these symptoms early is crucial so the dose can be reduced before more severe adverse effects develop.
Rationale for incorrect answers:
A. Orthostatic hypotension.
While orthostatic hypotension is a common side effect of levodopa, it is not a sign of toxicity. It results from dopamine’s effect on peripheral vasculature.
B. Drooling.
Drooling is more commonly associated with Parkinson’s disease itself due to impaired swallowing and muscle control, not levodopa toxicity.
D. Nausea, vomiting, and diarrhea.
Gastrointestinal upset is a frequent side effect of levodopa therapy, particularly when starting treatment, but it does not signal toxicity.
Take-home points:
- Dyskinesias such as spasmodic eye winking and twitching indicate early levodopa toxicity.
- Side effects like nausea and orthostatic hypotension are common but not toxic signs.
- Nurses must monitor patients on levodopa closely and report involuntary movements promptly.
Which condition will alert the nurse to a potential caution or contraindication regarding the use of a dopaminergic drug for treatment of mild Parkinson's disease?
Explanation
Dopaminergic drugs, such as levodopa/carbidopa, are widely used to treat Parkinson’s disease by replenishing dopamine and improving motor function. However, these medications can have systemic effects that make them unsafe in certain conditions. Knowing the major contraindications helps nurses promote safe medication use.
Rationale for correct answer:
C. Angle-closure glaucoma.
Dopaminergic drugs can increase intraocular pressure due to their effects on neurotransmitter balance. In patients with angle-closure glaucoma, this can worsen the condition and potentially lead to vision loss. For this reason, glaucoma is considered a major contraindication or caution for dopaminergic therapy.
Rationale for incorrect answers:
A. Diarrhea.
While unpleasant, diarrhea is not a contraindication for dopaminergic therapy and is not directly related to the drug’s action.
B. Tremors.
Tremors are one of the primary symptoms of Parkinson’s disease, and dopaminergic drugs are prescribed to reduce them, not contraindicated by them.
D. Unstable gait.
An unsteady gait is a common manifestation of Parkinson’s disease, and treatment aims to improve mobility, not avoid therapy.
Take-home points:
- Angle-closure glaucoma is a key contraindication for dopaminergic therapy.
- Parkinson’s symptoms such as tremors and unstable gait are expected and treated with these drugs.
- Nurses should carefully review ocular history before starting dopaminergic medications.
A patient is taking entacapone (Comtan) as part of the therapy for Parkinson's disease. Which intervention by the nurse is appropriate at this time?
Explanation
Entacapone (Comtan) is a catechol-O-methyltransferase (COMT) inhibitor prescribed with levodopa/carbidopa in Parkinson’s disease. It prolongs the action of levodopa, improving motor control. Nurses must educate patients about expected harmless side effects, such as urine discoloration, and provide reassurance.
Rationale for Correct Answer:
A. Notify the patient that this drug causes discoloration of the urine.
Entacapone commonly causes orange-brown urine discoloration, which is harmless and expected. Patients should be reassured so they do not mistake it for blood or infection.
Rationale for Incorrect Answers:
B. Limit the patient’s intake of tyramine-containing foods.
Tyramine restrictions are needed with MAO inhibitors (e.g., selegiline), not COMT inhibitors. Entacapone does not interact with dietary tyramine.
C. Monitor the results of renal studies because this drug can seriously affect renal function.
Entacapone is metabolized by the liver, not the kidneys. Renal monitoring is unnecessary for this drug.
D. Force fluids to prevent dehydration.
While hydration is healthy, entacapone does not increase dehydration risk, so this is not a specific nursing intervention.
Take-home Points:
- Entacapone may cause harmless orange-brown urine discoloration.
- Tyramine restrictions apply to MAOIs, not COMT inhibitors.
- The nurse should reassure patients and monitor motor symptom control.
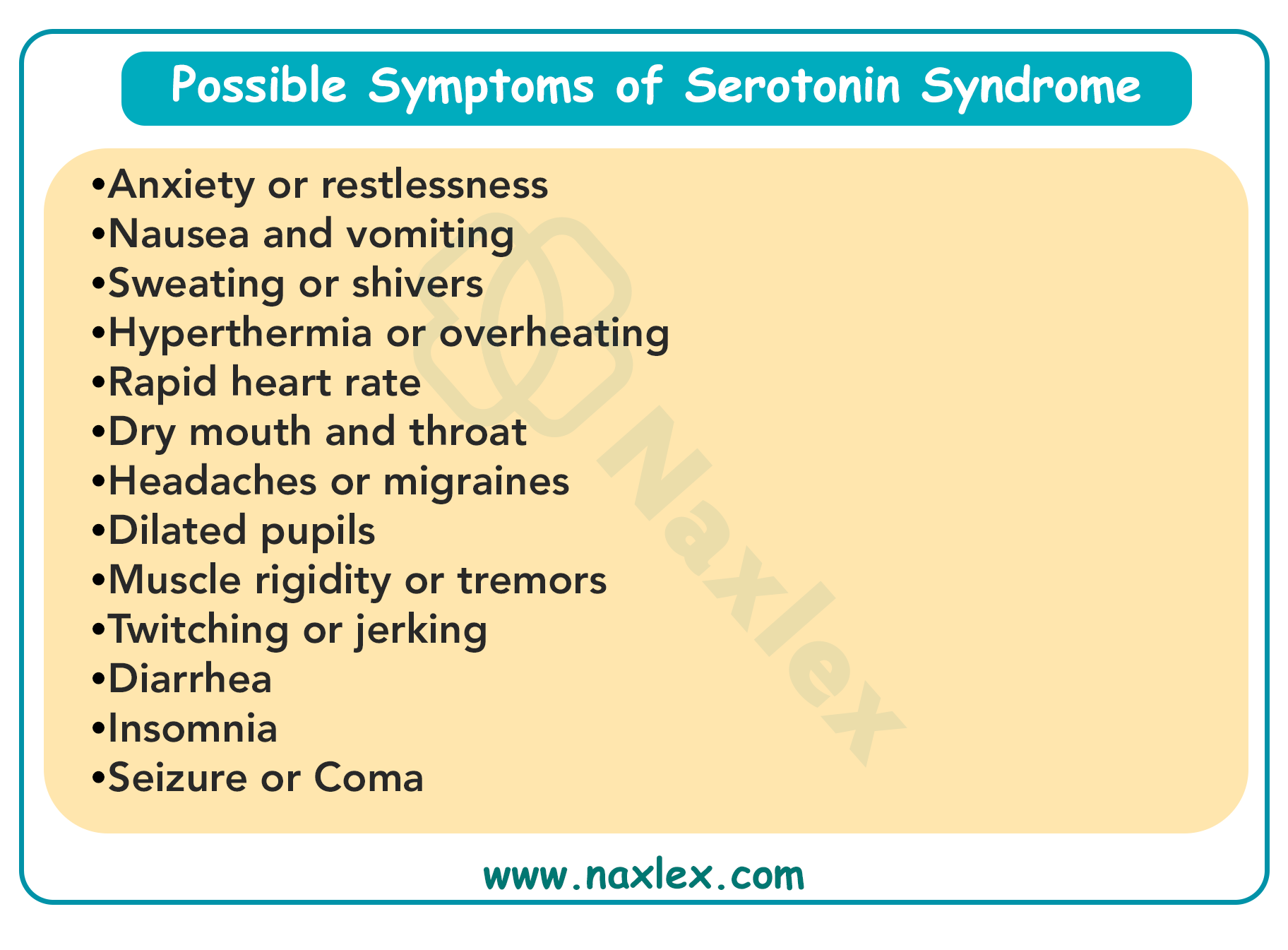
The nurse is reviewing the medication orders for a patient who has been taking selegiline (Eldepryl). Which of these medications or medication classes, if ordered, would cause a problem due to an interaction? Select all that apply
Explanation
Selegiline (Eldepryl) is a monoamine oxidase B (MAO-B) inhibitor used in the treatment of Parkinson’s disease. While it helps by inhibiting dopamine breakdown, it carries significant drug interaction risks, especially with medications that affect serotonin or opioid pathways. Nurses must recognize these risks to prevent life-threatening complications.
Rationale for Correct Answers:
B. Meperidine (Demerol)
Combining selegiline with meperidine can cause severe, potentially fatal reactions, including hyperthermia, muscle rigidity, and agitation. This combination is strictly contraindicated.
C. A cough syrup that contains dextromethorphan
Dextromethorphan has serotonergic activity. When combined with selegiline, it increases the risk of serotonin syndrome (confusion, hypertension, fever, tremors).
D. Serotonergic antidepressants
Drugs like SSRIs, SNRIs, and TCAs can also trigger serotonin syndrome when taken with selegiline. Patients should be carefully monitored, and concurrent use is usually avoided.
Rationale for Incorrect Answers:
A. Warfarin (Coumadin)
Selegiline does not have a significant interaction with warfarin. Monitoring INR is always important with anticoagulants, but there is no dangerous interaction here.
E. Erythromycin
Erythromycin primarily causes CYP3A4 interactions, not MAO-related issues. It does not pose a direct interaction risk with selegiline.
Take-home Points:
- Avoid opioids (e.g., meperidine) with selegiline due to life-threatening reactions.
- Dextromethorphan and serotonergic antidepressants can cause serotonin syndrome when combined with selegiline.
- Not all drugs interact — focus on serotonin-related and opioid interactions.
A patient will be taking selegiline (Eldepryl), 5 mg daily, in addition to dopamine replacement therapy for Parkinson's disease. The nurse will implement which precautions regarding selegiline?
Explanation
Selegiline (Eldepryl) is an MAO-B inhibitor used as adjunct therapy in Parkinson’s disease. At low doses, it selectively inhibits MAO-B, enhancing dopamine availability in the brain. Unlike nonselective MAO inhibitors, it generally does not require strict dietary restrictions at therapeutic doses. However, it can cause cardiovascular side effects, especially dizziness and orthostatic hypotension, which require close monitoring.
Rationale for Correct Answer:
B. Monitor for dizziness and orthostatic hypotension
Selegiline may impair blood pressure regulation, leading to orthostatic hypotension, particularly when combined with levodopa. Nurses should teach patients to rise slowly and report persistent dizziness or fainting.
Rationale for Incorrect Answers:
A. Teach the patient to avoid foods containing tyramine
Tyramine interactions are a concern with nonselective MAO inhibitors, but at standard doses (5–10 mg/day), selegiline is MAO-B selective and does not typically require tyramine restrictions.
C. Inform the patient that this drug may cause urine discoloration
Urine discoloration is associated with entacapone, not selegiline.
D. Monitor for weight gain
Weight gain is not a common adverse effect of selegiline.
Take-home Points:
- Monitor for dizziness and orthostatic hypotension with selegiline.
- Tyramine restrictions are unnecessary at standard MAO-B inhibitor doses.
- Differentiate side effects of Parkinson’s drugs to provide accurate teaching.
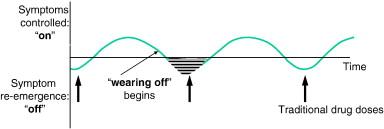
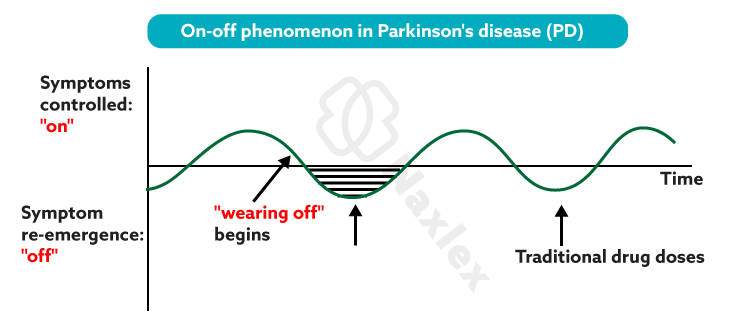
A patient with Parkinson's disease will start taking entacapone (Comtan) along with the carbidopa-levodopa (Sinemet) he has been taking for a few years. The nurse recognizes that which of these is an advantage of taking entacapone?
Explanation
Entacapone (Comtan) is a COMT inhibitor prescribed as an adjunct to carbidopa-levodopa therapy in Parkinson’s disease. By inhibiting COMT, it slows the breakdown of levodopa in the periphery, leading to more consistent dopamine levels in the brain. This helps reduce “wearing-off” and “on-off” fluctuations, which are common in long-term levodopa therapy.
Rationale for Correct Answer:
A. The entacapone can reduce on-off effects
Entacapone prolongs levodopa’s half-life, reducing motor fluctuations between doses. This improves mobility and overall quality of life in patients with advanced Parkinson’s disease.
Rationale for Incorrect Answers:
B. The levodopa may be stopped in a few days
Entacapone is never used alone; it only enhances the effect of levodopa and does not replace it.
C. There is less GI upset with entacapone
Entacapone does not reduce GI upset. Nausea and GI symptoms are more related to levodopa.
D. It does not cause the cheese effect
The cheese effect (hypertensive crisis from tyramine-rich foods) occurs with nonselective MAO inhibitors, not COMT inhibitors.
Take-home Points:
- Entacapone reduces “wearing-off” and on-off fluctuations in levodopa therapy.
- It cannot replace levodopa; it must be used in combination.
- COMT inhibitors do not cause the cheese effect.
Exams on Drugs Used for Degenerative Diseases of the Nervous System
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
- Objectives
- Introduction
- Overview of degenerative neurological diseases
- Parkinson’s disease (PD)
- Parkinson’s disease pharmacotherapy
- Practice Exericse 1
- Alzheimer’s disease (AD)
- Alzheimer’s disease (AD) pharmacotherapy
- Practice Exercise 2
- Multiple sclerosis (MS)
- Multiple sclerosis (MS) pharmacotherapy
- Practice Exercise 3
- Summary
- Comprehensive Questions
Notes Highlighting is available once you sign in. Login Here.
Introduction
- Explain the pathophysiology and clinical manifestations of Parkinson’s Disease, Alzheimer’s Disease, and Multiple Sclerosis.
- Identify the key neurotransmitters and receptors involved in degenerative neurological diseases.
- Describe the pharmacologic goals for managing PD, AD, and MS.
- Outline the mechanism of action, indications, and adverse effects of dopaminergic agents in PD.
- Discuss the use, benefits, and nursing considerations of MAO-B inhibitors, COMT inhibitors, and anticholinergic agents in PD management.
- Explain the role of acetylcholinesterase inhibitors and NMDA receptor antagonists in treating Alzheimer’s Disease.
- Identify disease-modifying therapies (DMTs) for MS and their mechanisms, administration routes, and monitoring requirements.
- Describe pharmacologic strategies for symptomatic management in MS, including spasticity, fatigue, neuropathic pain, bladder dysfunction, and walking impairment.
- Apply nursing principles in medication administration, monitoring therapeutic and adverse effects, and patient/caregiver education.
- Evaluate patient outcomes and adjust care plans to optimize functional independence, safety, and quality of life in degenerative neurological disorders.
-
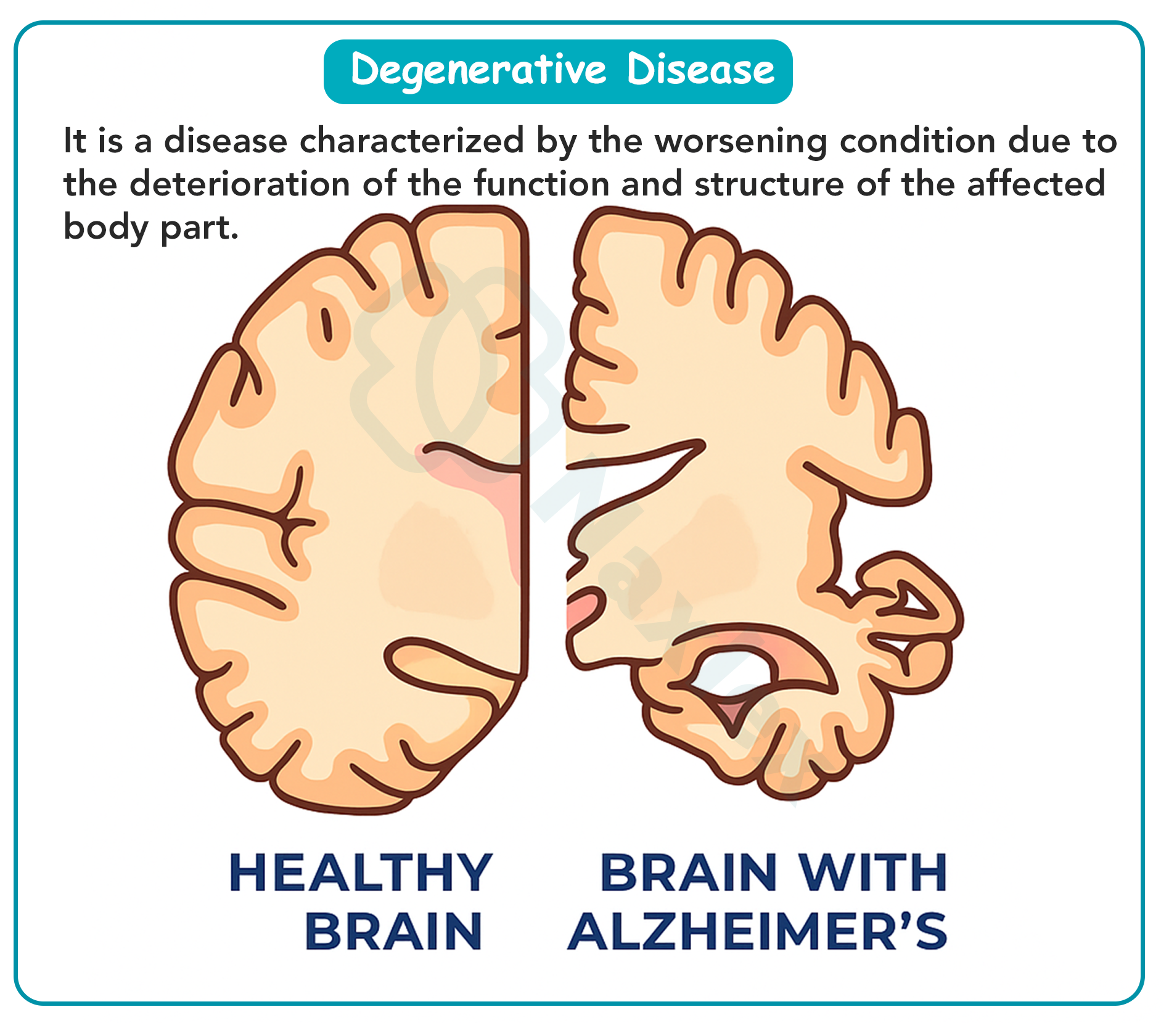
Degenerative diseases of the nervous system are a group of progressive, chronic, and largely irreversible disorders that affect the structure and function of neurons.
These diseases result in a gradual decline of motor, cognitive, and sensory abilities, profoundly affecting patients’ daily lives, independence, and overall quality of life.
The most common conditions in this category include Parkinson’s Disease (PD), Alzheimer’s Disease (AD), and Multiple Sclerosis (MS).
Pharmacologic management for these conditions is complex and tailored to symptom control, slowing disease progression, and enhancing patient function, rather than curing the disease. Medications target the underlying neurotransmitter imbalances, modulate immune responses, or reduce excitotoxic neuronal damage.
The nurse plays a pivotal role in the care of these patients. Key nursing responsibilities include:
- Ensuring safe medication administration, including correct timing, dose, and route.
- Vigilant monitoring for therapeutic responses, side effects, and adverse drug interactions.
- Patient and caregiver education on medication purposes, expected outcomes, side effects, dietary considerations, and lifestyle modifications.
- Supporting psychosocial needs of patients and families, providing guidance on coping strategies, safety precautions, and functional independence.
-
Understanding the pathophysiology of each disease, the pharmacologic principles, and the specific nursing interventions is essential to optimizing outcomes and maintaining patient safety.
Overview of degenerative neurological diseases
-
Degenerative diseases of the nervous system are a group of progressive, chronic, and largely irreversible disorders that affect the structure and function of neurons.
Degenerative diseases primarily affect the Central Nervous System (CNS), leading to progressive neuronal loss.
The exact causes of many of these conditions are not fully understood but involve a combination of genetic, environmental, and immunological factors.
These disorders are challenging to diagnose and manage due to their chronic and progressive nature.
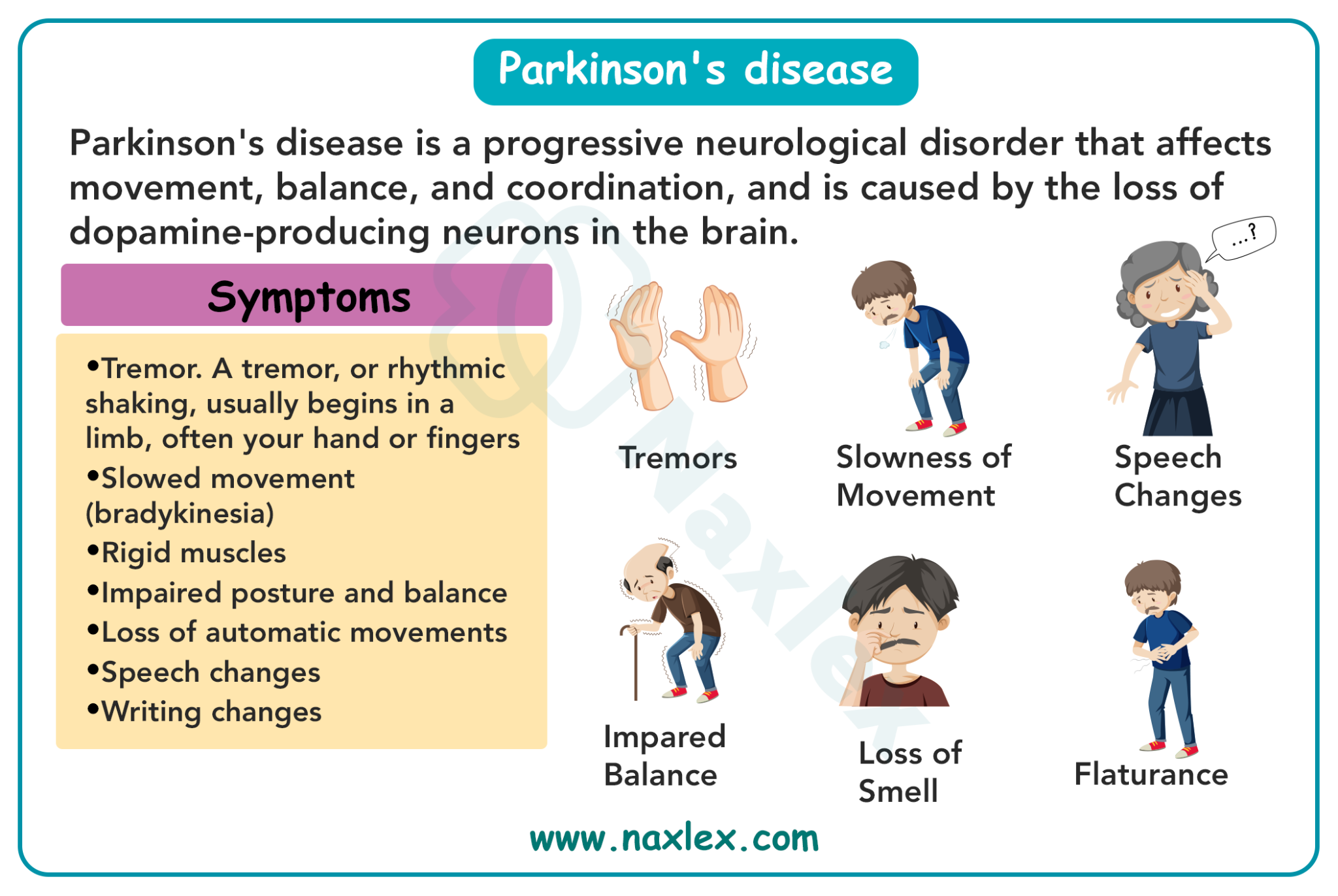
Parkinson’s Disease (PD)
- PD is characterized by the degeneration of dopamine-producing neurons in the substantia nigra, a brain region crucial for regulating voluntary and involuntary movement.
- Dopamine deficiency in the nigrostriatal pathway leads to a disruption of the delicate balance between dopamine (inhibitory) and acetylcholine (excitatory), resulting in motor dysfunction.
- Common symptoms include resting tremor, bradykinesia, muscle rigidity, postural instability, and gait disturbances.
-
AD involves progressive loss of cholinergic neurons in the cerebral cortex and hippocampus, leading to memory impairment and cognitive decline.
-
Accumulation of beta-amyloid plaques and neurofibrillary tangles further disrupts neural communication and accelerates neuronal death.
-
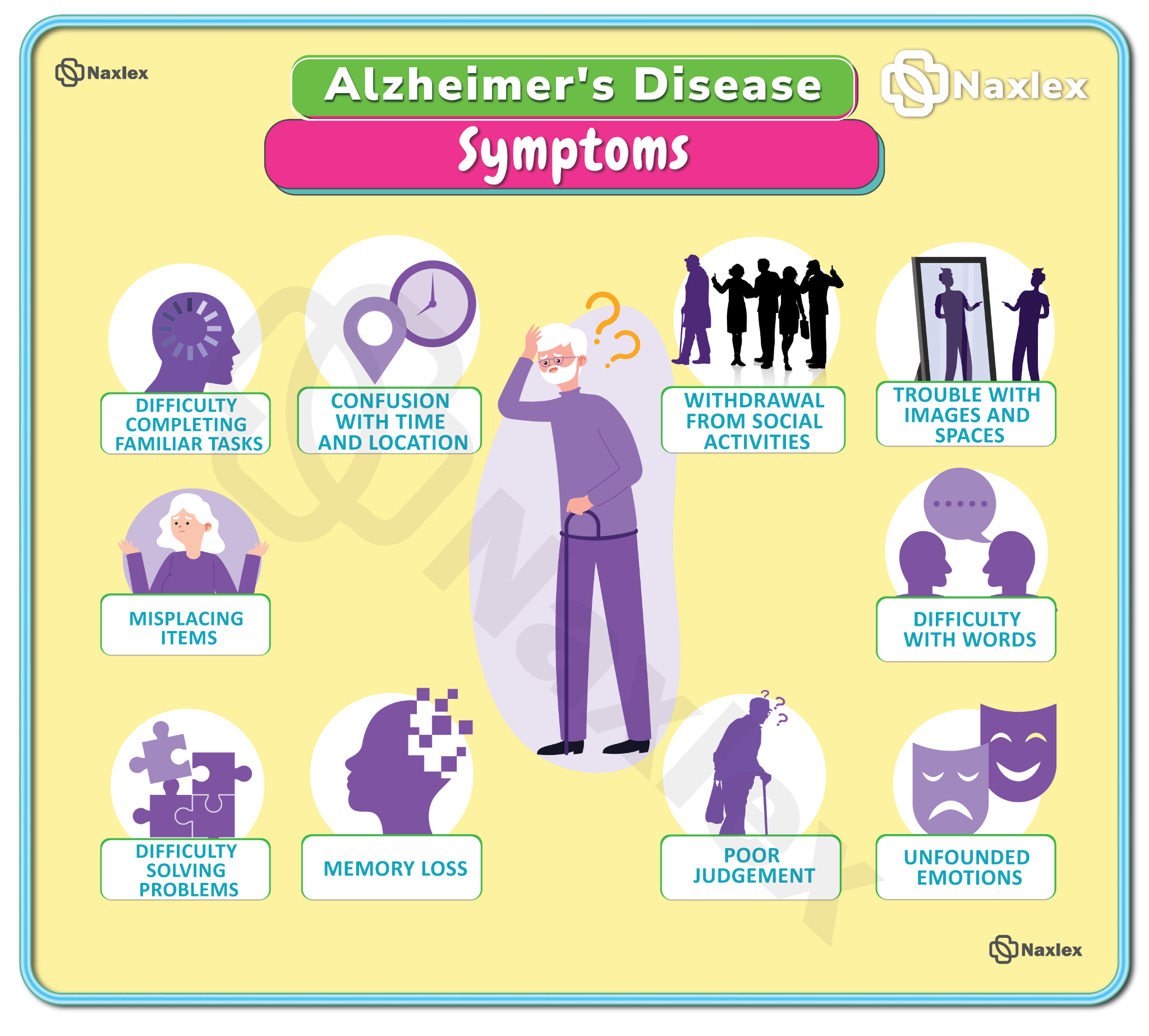
Clinically, patients exhibit memory loss, confusion, disorientation, personality changes, and eventually loss of independence in performing ADLs.
-
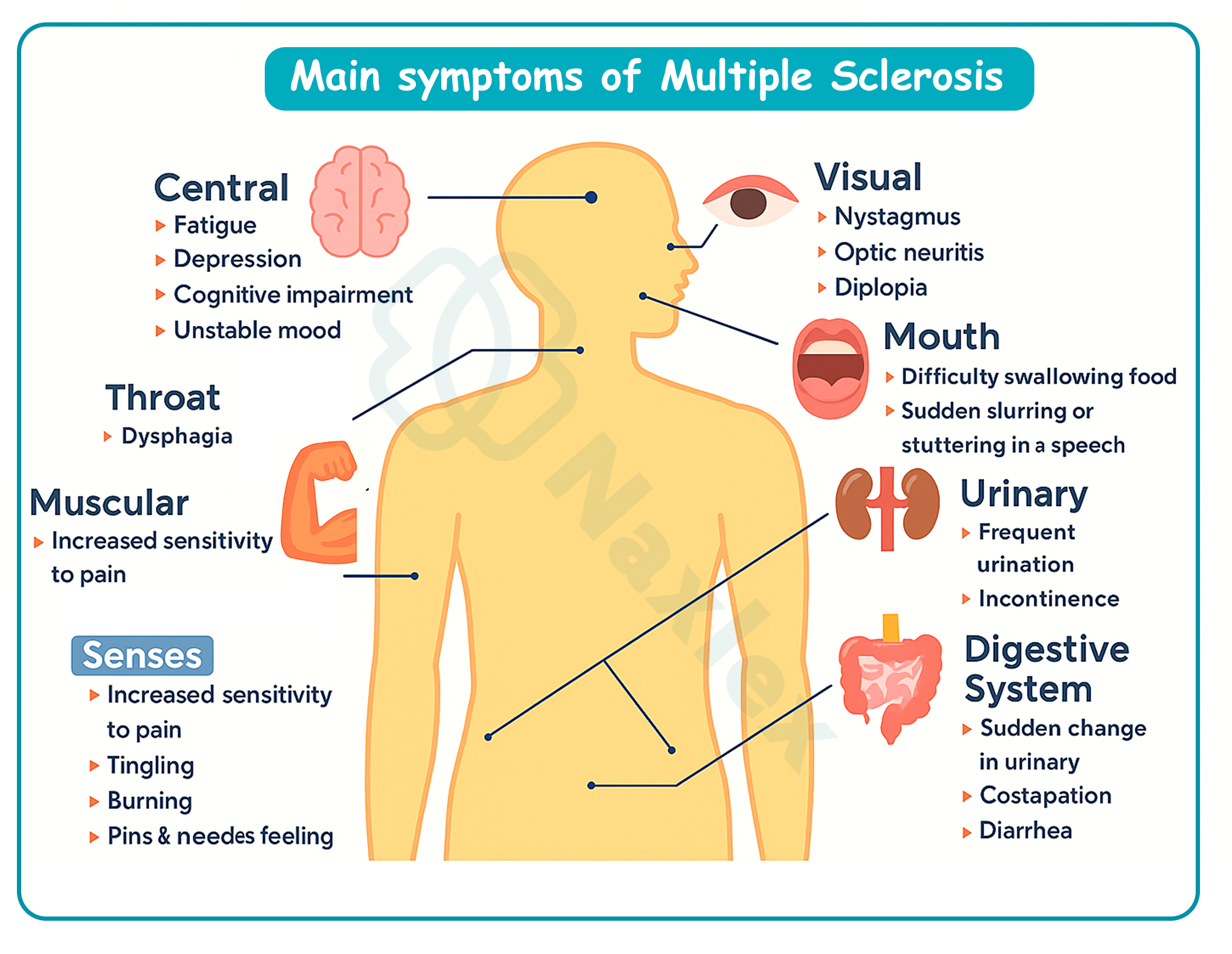
MS is an autoimmune demyelinating disease where T-cells and antibodies attack myelin, the protective sheath around CNS neurons.
-
This demyelination causes impaired nerve conduction, resulting in muscle weakness, spasticity, fatigue, sensory disturbances, and cognitive deficits.
-
The disease course varies: Relapsing-Remitting, Secondary-Progressive, Primary-Progressive, and Progressive-Relapsing, with each requiring specific treatment and monitoring strategies.
-
The nervous system and neurotransmitters
A firm understanding of the nervous system structure and neurotransmitters is crucial for comprehending drug action in degenerative diseases.
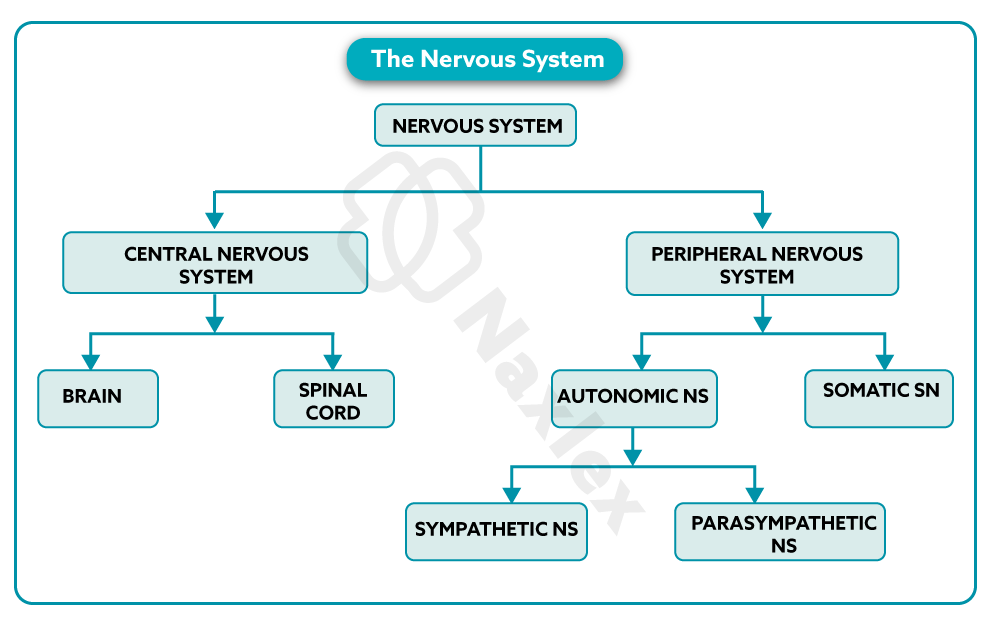
Nervous System Overview
-
Central Nervous System (CNS): Consists of the brain and spinal cord, which integrates information and coordinates responses. Neurodegenerative diseases primarily affect CNS neurons.
-
Peripheral Nervous System (PNS): Comprises all nerves outside the CNS. The PNS transmits signals to and from the body and is divided into:
-
Somatic Nervous System: Controls voluntary movement through skeletal muscles.
-
Autonomic Nervous System (ANS): Regulates involuntary activities, including heart rate, digestion, respiratory rate, and glandular secretions.
-
-
Neurotransmitters and Receptors
Key neurotransmitters targeted in treatment:
-
Dopamine: Regulates movement, emotion, and cognition. Deficiency causes motor symptoms in PD.
-
Acetylcholine (ACh): Vital for cognition and memory; loss leads to AD.
-
Glutamate: Overactivity results in excitotoxicity and neuronal death.
-
GABA: Inhibitory neurotransmitter that balances neuronal excitability.
-
Receptors:
-
Dopaminergic receptors (D1–D5): Targeted by dopaminergic agents and agonists in PD.
-
Cholinergic receptors (muscarinic and nicotinic): Targeted by AChE inhibitors in AD.
-
NMDA receptors: Blocked by memantine to prevent glutamate-induced excitotoxicity.
-
These diseases result in a gradual decline of motor, cognitive, and sensory abilities, profoundly affecting patients’ daily lives, independence, and overall quality of life.
The most common conditions in this category include Parkinson’s Disease (PD), Alzheimer’s Disease (AD), and Multiple Sclerosis (MS).
Pharmacologic management for these conditions is complex and tailored to symptom control, slowing disease progression, and enhancing patient function, rather than curing the disease. Medications target the underlying neurotransmitter imbalances, modulate immune responses, or reduce excitotoxic neuronal damage.
The nurse plays a pivotal role in the care of these patients. Key nursing responsibilities include:
-
Ensuring safe medication administration, including correct timing, dose, and route.
-
Vigilant monitoring for therapeutic responses, side effects, and adverse drug interactions.
-
Patient and caregiver education on medication purposes, expected outcomes, side effects, dietary considerations, and lifestyle modifications.
-
Supporting psychosocial needs of patients and families, providing guidance on coping strategies, safety precautions, and functional independence.
-
Understanding the pathophysiology of each disease, the pharmacologic principles, and the specific nursing interventions is essential to optimizing outcomes and maintaining patient safety.
Parkinson’s disease (PD)
-
Pathophysiology and Clinical Presentation
Parkinson’s Disease (PD) is a progressive neurodegenerative disorder primarily affecting the basal ganglia, specifically the substantia nigra pars compacta, where dopamine-producing neurons are lost. Dopamine is a critical neurotransmitter that inhibits excessive motor activity, and its deficiency leads to a relative excess of excitatory acetylcholine activity. This neurotransmitter imbalance manifests as motor dysfunction and non-motor complications.
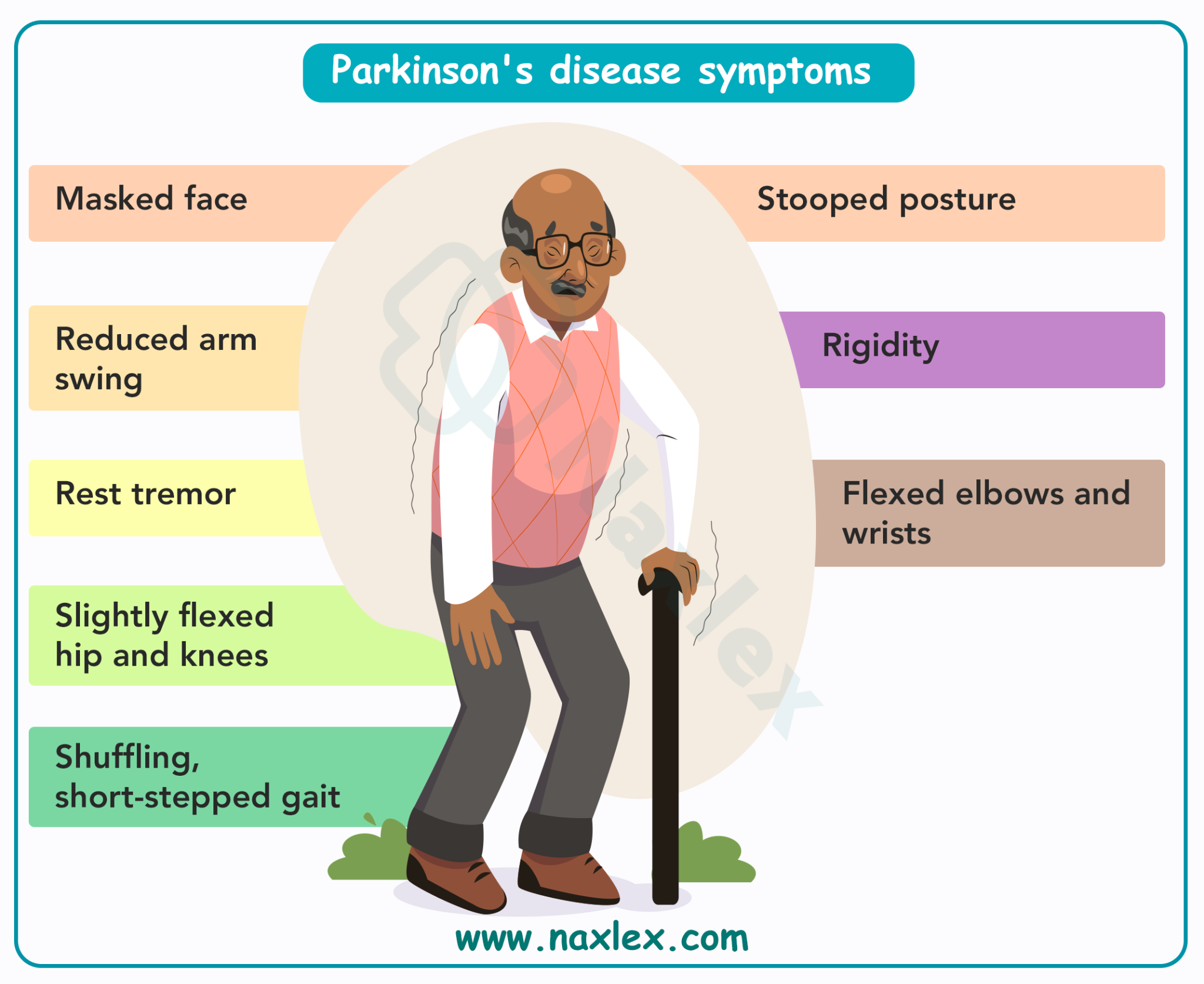
Motor symptoms include:
- Resting tremor: Often described as a “pill-rolling” movement of the fingers, prominent at rest and decreasing with voluntary movement.
- Bradykinesia/Akinesia: Slowed initiation and execution of voluntary movements. Clinically observed as shuffling gait, reduced arm swing, and diminished facial expression (“masked face”).
- Muscle Rigidity: Increased muscle tone causing stiffness and resistance to passive movement, often described as “cogwheel rigidity.”
- Postural instability: Impaired balance and coordination, contributing to an increased risk of falls and injuries.
-
Non-motor symptoms are often under-recognized but significantly impact quality of life:
- Neuropsychiatric: Depression, anxiety, apathy, hallucinations, and impulse-control disorders.
- Cognitive: Dementia, slowed processing speed, attention deficits.
- Autonomic dysfunction: Orthostatic hypotension, constipation, urinary retention, sexual dysfunction.
-
Pharmacologic Goal: PD treatment is not curative but aims to:
- Restore dopaminergic function in the basal ganglia to improve motor symptoms.
- Reduce cholinergic overactivity, which contributes to tremors.
- Improve functional independence and quality of life.
- Sleep disorders: Insomnia, REM sleep behavior disorder, excessive daytime sleepiness.
Parkinson’s disease pharmacotherapy
Medication choice is individualized, considering disease severity, age, comorbidities, and risk for adverse effects. Nurses must monitor both therapeutic response and drug-related complications, and educate patients/families for optimal adherence and safety.
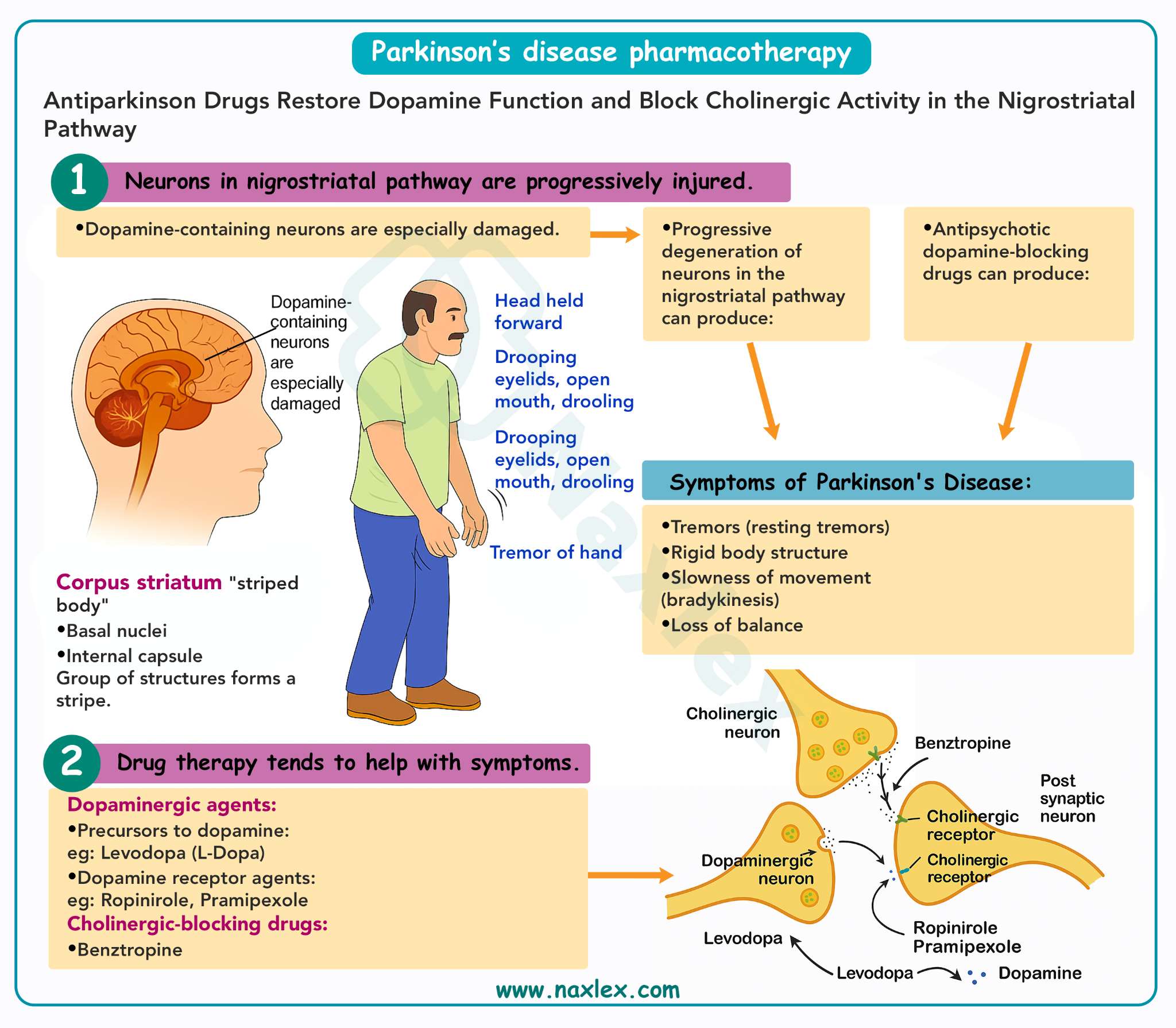
Levodopa/Carbidopa
Mechanism of Action:
- Levodopa is a metabolic precursor of dopamine that crosses the blood-brain barrier, where it is decarboxylated to dopamine, replenishing depleted neurotransmitter levels.
- Carbidopa is a peripheral decarboxylase inhibitor that prevents levodopa conversion in the periphery, enhancing CNS delivery and reducing peripheral adverse effects like nausea and hypotension.
- Pharmacokinetics: Levodopa is rapidly absorbed in the small intestine; its bioavailability is affected by gastric emptying and competition with dietary amino acids.

Indications: First-line therapy for moderate to severe motor symptoms, particularly bradykinesia and rigidity.
Adverse Effects:
- Peripheral: Nausea, vomiting, orthostatic hypotension, anorexia, benign dark urine or sweat discoloration.
- Central: Dyskinesias (involuntary writhing or choreiform movements), hallucinations, agitation, confusion.
- Motor Fluctuations:
- “Wearing-off” phenomenon: Return of symptoms near the end of a dosing interval.
- “On-off” phenomenon: Sudden, unpredictable transitions between mobility and immobility, often unrelated to dosing.
Nursing Insights:
- Administer on an empty stomach 30–60 minutes before meals; high-protein meals reduce absorption.
- Monitor for early signs of dyskinesia, psychosis, or orthostatic hypotension.
- Educate patients and caregivers to document symptom changes, recognize dyskinesias, and report sudden immobility or hallucinations.
- Abrupt withdrawal can trigger neuroleptic malignant-like syndrome, characterized by fever, rigidity, altered mental status, and autonomic dysfunction – a medical emergency.
Prototypes: Pramipexole, Ropinirole, Apomorphine.
Mechanism of Action:
- Directly stimulate dopamine D2 and D3 receptors, bypassing presynaptic dopamine neurons.
- Can be used as monotherapy in early PD to delay levodopa-related motor complications or as adjuncts in advanced stages.
Adverse Effects:
- Cardiovascular: Orthostatic hypotension, especially with the first dose.
- CNS: Sedation, hallucinations, impulse-control disorders (compulsive gambling, shopping, hypersexuality), confusion.
- Sleep attacks: Sudden, uncontrollable sleep episodes, posing safety risks.
- Apomorphine specific: Subcutaneous injection for acute “off” episodes; causes severe nausea without antiemetic pretreatment.
Nursing Insights:
- Monitor blood pressure, mental status, and behavior changes.
- Educate patients about sleep safety, driving restrictions, and reporting compulsive behaviors.
- Administer antiemetic pre-treatment for apomorphine and monitor for rapid hypotension.
Prototypes: Selegiline, Rasagiline.

Mechanism of Action:
- Selectively inhibit monoamine oxidase B (MAO-B), the CNS enzyme that metabolizes dopamine, prolonging synaptic dopamine activity.
- Rasagiline is more potent and lacks amphetamine-like metabolites, reducing insomnia and agitation.
Adverse Effects:
- Insomnia, dizziness, headache, mild hypertension.
- Rare hypertensive crisis when combined with high tyramine intake or certain medications (SSRIs, TCAs, sympathomimetics).
Nursing Insights:
- Administer early in the day to prevent insomnia.
- Monitor for drug interactions, especially with serotonergic agents, to avoid serotonin syndrome.
- Educate patients on avoiding large amounts of tyramine-rich foods (aged cheeses, cured meats).
Prototypes: Entacapone, Tolcapone.
Mechanism of Action:
-
Inhibit catechol-O-methyltransferase (COMT) in the periphery, preventing levodopa metabolism and prolonging CNS dopamine availability.
Adverse Effects:
-
Diarrhea, orange urine discoloration, orthostatic hypotension.
-
Tolcapone carries risk of hepatotoxicity, necessitating liver function monitoring.
Nursing Insights:
-
Administer with levodopa/carbidopa.
-
Monitor liver enzymes regularly for signs of hepatotoxicity.
-
Educate patients about harmless urine discoloration and report persistent diarrhea or jaundice immediately.
Prototypes: Benztropine, Trihexyphenidyl.
Mechanism of Action:
-
Block central muscarinic cholinergic receptors, reducing acetylcholine activity to restore dopamine/ACh balance.
-
More effective for tremor than bradykinesia or rigidity.
Adverse Effects:
-
Dry mouth, blurred vision, constipation, urinary retention, tachycardia, sedation, cognitive impairment, hallucinations (especially in elderly).
Nursing Insights:
-
Limit use in older adults due to risk of confusion and falls.
-
Encourage hydration and fiber intake to prevent constipation.
-
Monitor for urinary retention and glaucoma exacerbation.
-
Educate patients to report new confusion or memory changes.
Mechanism:
-
Enhances dopamine release from presynaptic neurons and may block NMDA glutamate receptors, reducing excitotoxicity.
-
Provides mild symptomatic relief and is often used for levodopa-induced dyskinesias.
Adverse Effects:
-
Livedo reticularis (mottled skin), ankle edema, hallucinations, confusion, hypotension.
Nursing Insights:
-
Monitor CNS status, skin changes, and edema.
-
Educate patients and families to report confusion, hallucinations, or skin mottling.
Alzheimer’s disease (AD)
Pathophysiology
- Loss of cholinergic neurons in the basal forebrain leads to acetylcholine deficiency, contributing to cognitive decline.
- Accumulation of beta-amyloid plaques and neurofibrillary tau tangles disrupts synaptic transmission and induces neuronal death.
- Clinically manifests as memory loss, confusion, disorientation, impaired judgment, personality changes, and eventual loss of independence.
-
Enhance cholinergic neurotransmission to temporarily improve cognitive function.
- Reduce excitotoxic damage from glutamate overactivity.
- Manage behavioral and psychological symptoms of dementia, including agitation, anxiety, and psychosis.
Alzheimer’s disease (AD) pharmacotherapy
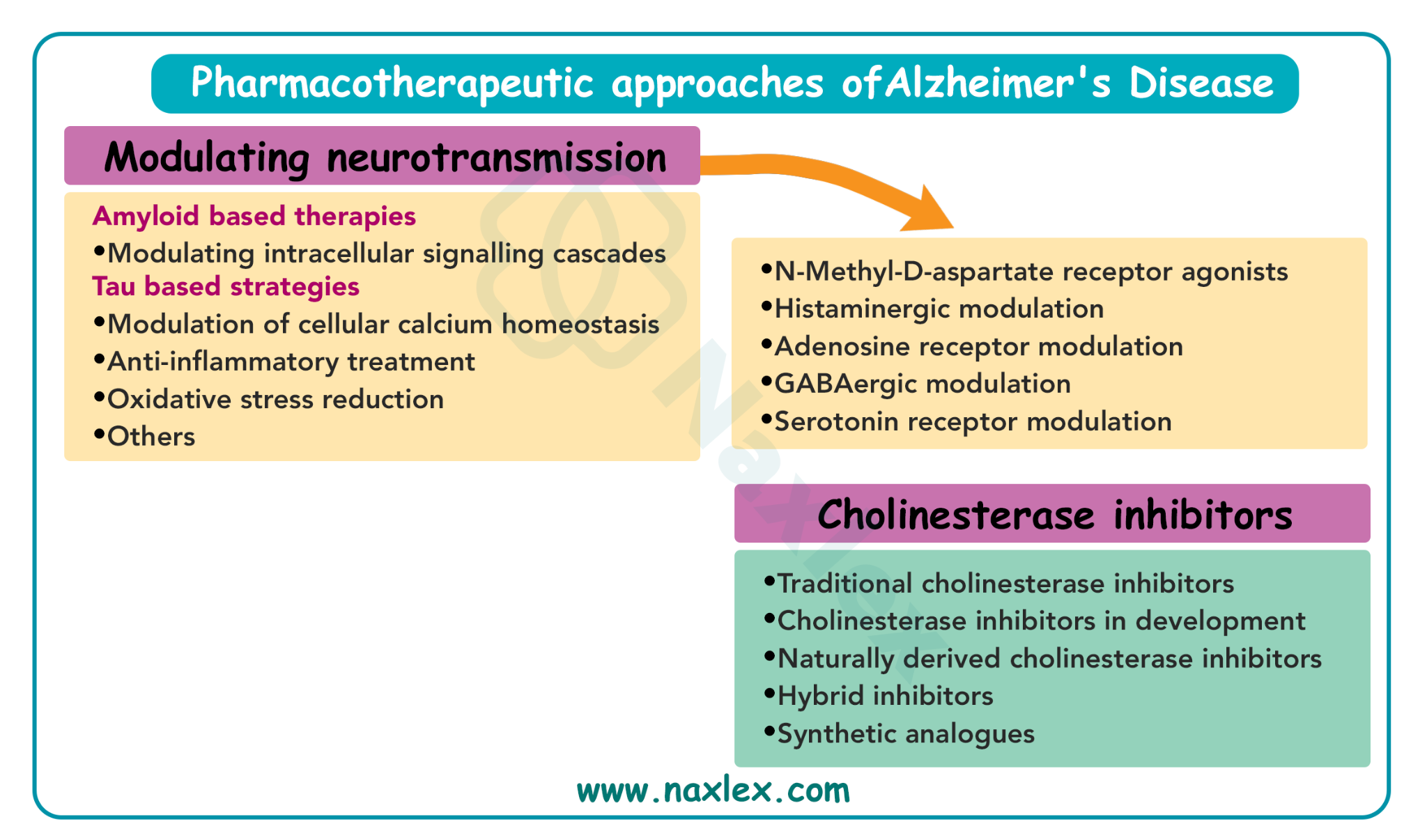
Acetylcholinesterase Inhibitors (AChEIs)
Prototypes: Donepezil, Rivastigmine, Galantamine.
Mechanism:
- Reversibly inhibit acetylcholinesterase, increasing acetylcholine levels at synapses.
- Improve cognitive symptoms and may slow functional decline in early to moderate AD.
Adverse Effects:
- GI: nausea, vomiting, diarrhea, anorexia, weight loss.
- Cardiac: bradycardia, syncope, conduction abnormalities.
- CNS: dizziness, headache, sleep disturbances.
Nursing Insights:
- Titrate doses gradually to minimize GI upset.
- Monitor weight and cardiac status, especially in patients with arrhythmias or hypotension.
- Educate caregivers about adherence, monitoring for side effects, and strategies to improve medication tolerance.
Prototype: Memantine.
Mechanism:
- Non-competitive NMDA receptor antagonist, reducing excessive calcium influx, preventing excitotoxic neuronal damage.
- Used for moderate to severe AD, often with AChEIs.
Adverse Effects:
- Dizziness, confusion, headache, constipation, occasional hypertension.
Nursing Insights:
- Educate caregivers on fall prevention and monitoring for CNS changes.
- Advantage: Does not cause cholinergic adverse effects like nausea or bradycardia.
Multiple sclerosis (MS)
- MS is an immune-mediated demyelinating disorder, leading to impaired nerve conduction and CNS inflammation.
- Disease courses:
- Relapsing-Remitting (RRMS): Acute flares with full or partial recovery.
- Secondary-Progressive (SPMS): Gradual worsening after initial relapsing phase.
- Primary-Progressive (PPMS): Continuous decline without remissions.
- Progressive-Relapsing (PRMS): Progressive course with acute relapses.
Symptoms: muscle weakness, spasticity, fatigue, sensory disturbances, neuropathic pain, bladder/bowel dysfunction, cognitive deficits.
- Disease-Modifying Therapies (DMTs): Slow disease progression and reduce relapse frequency.
- Symptomatic Management: Address spasticity, fatigue, neuropathic pain, urinary issues, and mobility impairments.
Multiple sclerosis (MS) pharmacotherapy
Injectables:
- Interferon Beta-1a/1b: Immunomodulatory, reduces T-cell activation. Adverse effects: flu-like symptoms, elevated LFTs, injection site reactions. Nursing: premedicate with NSAIDs, teach injection technique, monitor labs and mood.
- Glatiramer Acetate: Mimics myelin, shifts immune response to anti-inflammatory phenotype. AE: injection reactions, transient chest tightness. Nursing: teach proper injection and monitor post-injection reactions.
Oral DMTs:
- Fingolimod: Sequesters lymphocytes; AE: bradycardia, macular edema, infection risk. Nursing: first-dose observation, ECG, educate on infection precautions.
- Dimethyl Fumarate: Activates Nrf2 antioxidant pathway; AE: flushing, GI upset, lymphopenia. Nursing: take with food, monitor CBC.
- Teriflunomide: Inhibits T/B cell proliferation; AE: hepatotoxicity, alopecia, teratogenic. Nursing: pregnancy precautions, monitor LFTs, educate patient.
Infusion DMTs:
- Natalizumab: Monoclonal antibody blocking lymphocyte CNS entry; AE: PML risk. Nursing: JC virus testing, strict monitoring.
- Ocrelizumab: CD20 B-cell depletion; AE: infusion reactions, infections. Nursing: premedicate, monitor infection risk.
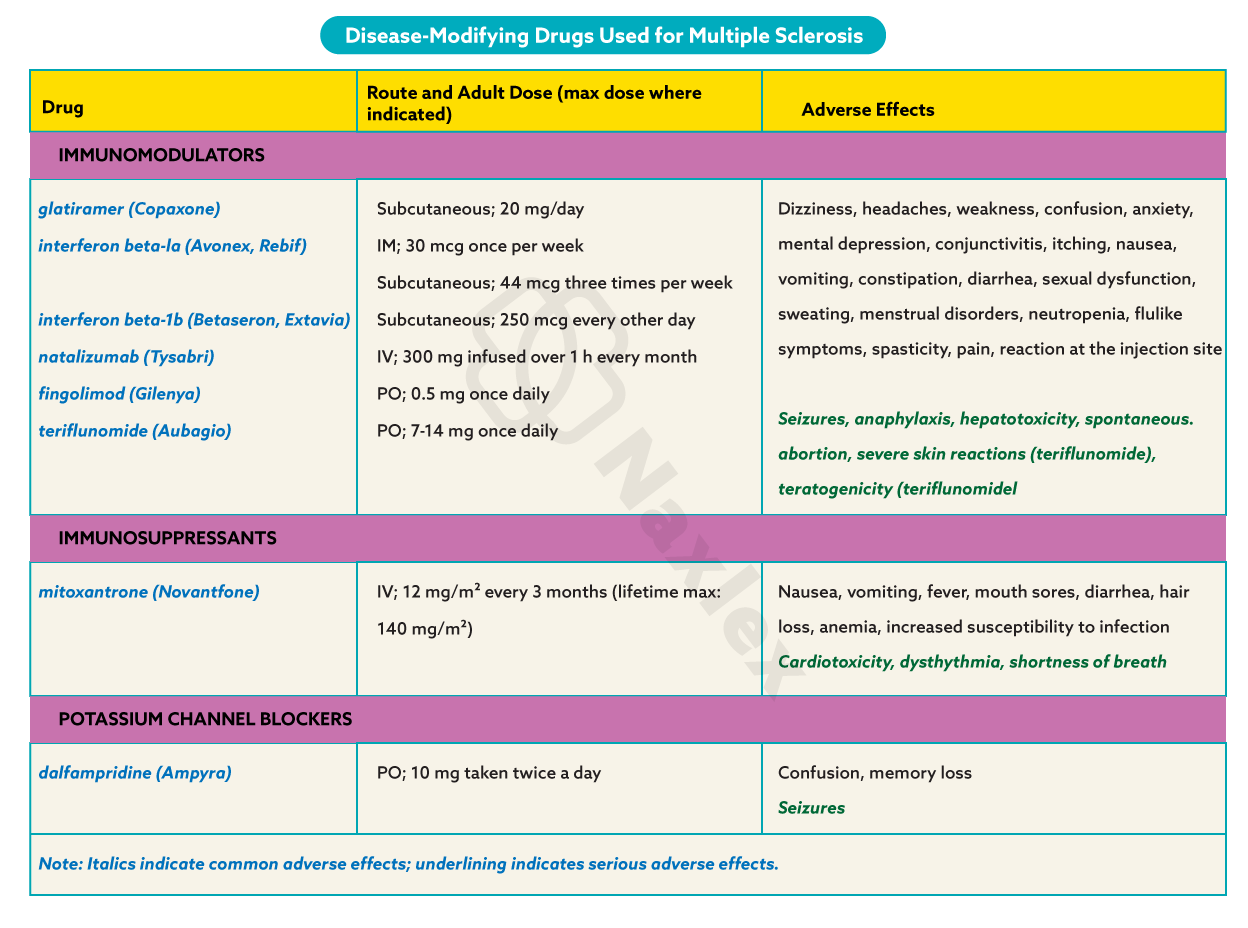
-
Spasticity: Baclofen, Tizanidine, Diazepam, Dantrolene. Monitor muscle tone, sedation, and liver function.
- Fatigue: Amantadine, Modafinil. Monitor CNS effects and BP.
- Neuropathic Pain: Gabapentin, Pregabalin, Amitriptyline, Duloxetine. Monitor sedation and mood.
- Bladder Dysfunction: Oxybutynin, Tolterodine (overactive), Bethanechol (retention). Monitor voiding patterns and post-void residual.
- Walking Impairment: Dalfampridine; monitor for seizures and educate about adherence.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Drugs Used for Degenerative Diseases of the Nervous System
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


